User login
The Need for a Multidisciplinary Approach for Successful High-Risk Pulmonary Embolism Treatment
The Need for a Multidisciplinary Approach for Successful High-Risk Pulmonary Embolism Treatment
Pulmonary embolism (PE) is a common cause of morbidity and mortality in the general population.1 The incidence of PE has been reported to range from 39 to 115 per 100,000 persons per year and has remained stable.2 Although mortality rates have declined, they remain high.3 The clinical presentation is nonspecific, making diagnosis and management challenging. A crucial and difficult aspect in the management of patients with PE is weighing the risks vs benefits of treatment, including thrombolytic therapy and other invasive procedures, which carry inherent risks. These factors have led to the development of PE response teams (PERTs) in some hospitals to implement effective multidisciplinary protocols that facilitate prompt diagnosis, management, and follow-up.4
CASE PRESENTATIONS
Case 1
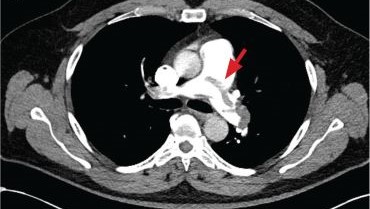
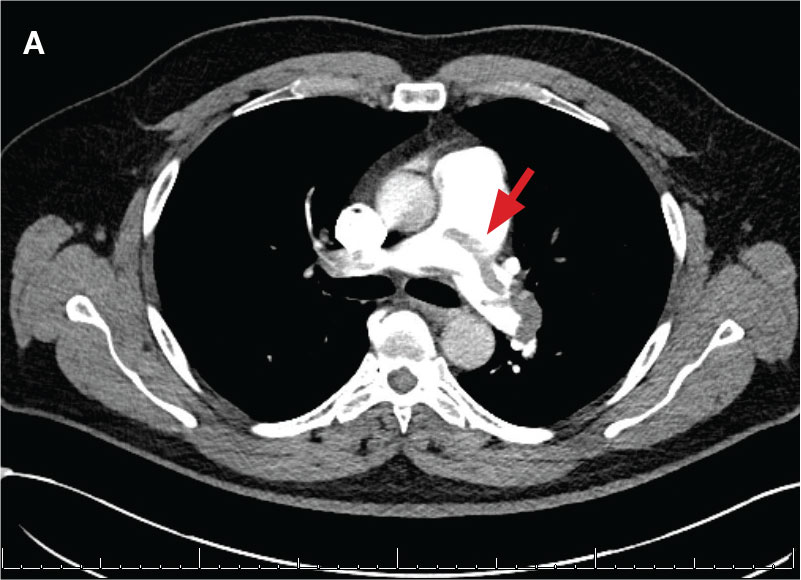
New onset seizures and cardiac arrest in the treatment of saddle PE. A 54-year-old male who worked as a draftsman and truck driver with a history of hypertension and nephrolithiasis presented to the emergency department (ED) with progressive shortness of breath for 2 weeks. On the morning of ED presentation the patient experienced an episode of severe shortness of breath, lightheadedness, and chest pressure. He reported no other symptoms such as palpitations, nausea, vomiting, abdominal discomfort, or extremity pain or swelling. He reported no recent travel, immunization, falls, or surgery. Upon evaluation, the patient was found to be in no acute distress, with stable vital signs and laboratory results except for 2 elevated results: > 20 μg/mL D-dimer (reference range, < 0.5 μg/mL) and N-terminal prohormone brain natriuretic peptide (proBNP) level, 3455 pg/mL (reference range, < 125 pg/mL for patients aged < 75 years). Electrocardiogram showed T-wave inversions in leads V2 to V4. Imaging revealed a saddle PE and left popliteal deep venous thrombosis (Figure 1). The patient received an anticoagulation loading dose and was started on heparin drip upon admission to the medical intensive care unit (MICU) for further management and monitoring. The Interventional Radiology Service recommended full anticoagulation with consideration of reperfusion therapies if deterioration developed.
indicated by arrows in the pulmonary trunk extending to the left pulmonary artery (A),
and obliterating right pulmonary artery and branches of left pulmonary artery (B).
indicated by arrows in the pulmonary trunk extending to the left pulmonary artery (A),
and obliterating right pulmonary artery and branches of left pulmonary artery (B).
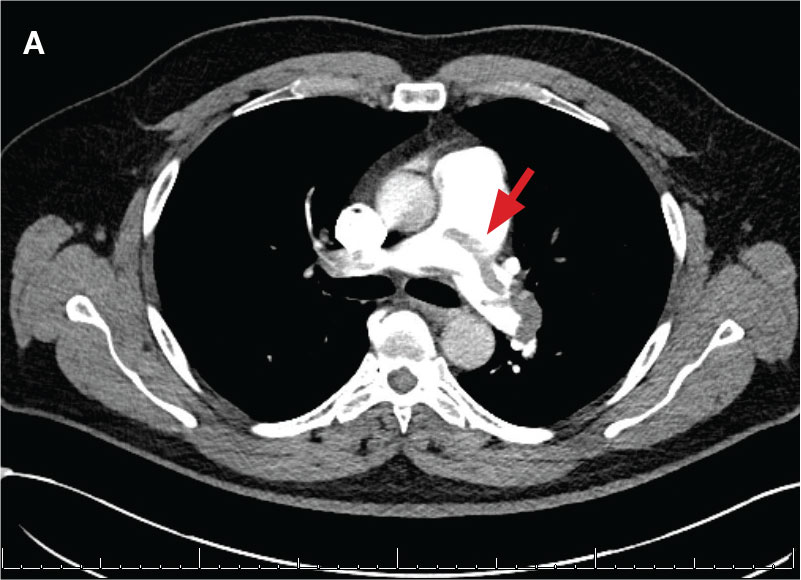
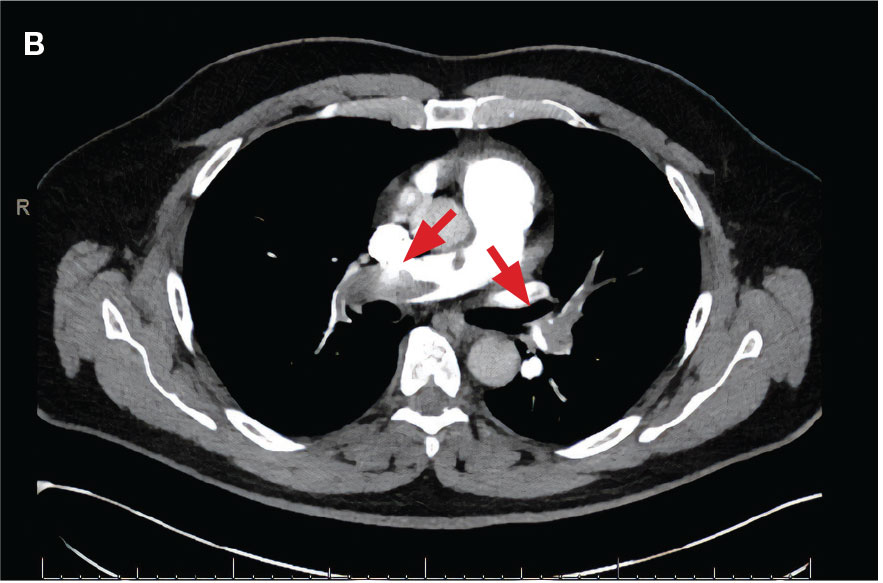
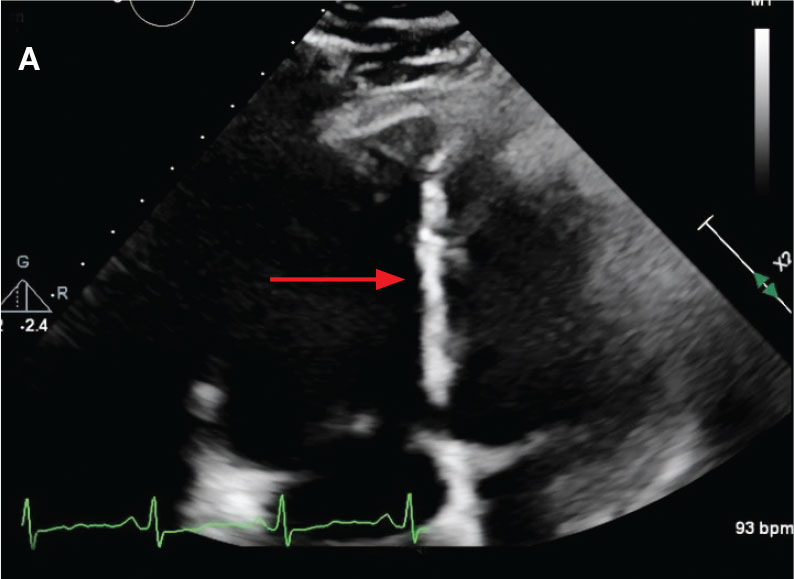
While in the MICU, point-of-care ultrasound findings were confirmed with official echocardiogram by the cardiology service, which demonstrated a preserved ejection fraction of 60% to 65%, a D-shaped left ventricle with septal wall hypokinesis secondary to right heart strain (Figure 2), a markedly elevated right ventricular systolic pressure (RVSP) of 73 mm Hg, and a mean pulmonary artery pressure (mPAP) of 38 mm Hg. The patient’s blood pressure progressively decreased, heart rate increased, and he required increased oxygen supplementation. The case was discussed with the Pharmacy Service, and since the patient had no contraindications to thrombolytic therapy, the appropriate dosage was calculated and 100 mg intravenous (IV) tissue plasminogen activator (tPA) was administered over 2 hours.
flattening and deviation to left in direction (A) and septal deviation to left with
formation of D-sign (B).
flattening and deviation to left in direction (A) and septal deviation to left with
formation of D-sign (B).
About 40 minutes into tPA infusion, the patient suddenly experienced marked shortness of breath, diaphoresis, and anxiety with seizure-like involuntary movements; as a result, the infusion was stopped. He also had episodes of posturing, mental status decline, and briefly going in and out of consciousness, which lasted about 3 minutes before he lost consciousness and pulse. High-quality advanced cardiac life support was initiated, followed by endotracheal intubation. Despite a secured airway and return of spontaneous circulation, the patient remained hypotensive and continued to have seizure-like activity.
The patient was administered a total of 8 mg of lorazepam, sedated with propofol, initiated at 5 μg/kg/min, titrated to stop seizure activity at 15μg/kg/min, and later maintained at 10 μg/kg/min, for a RASS of -1, and started on norepinephrine 0.1 μg/kg/min for acute stabilization. Head computed tomography without contrast showed no acute intracranial pathology as etiology of seizures. Seizure etiology differential at this time was broad; however, hypoxemia due to PE and medication adverse effects were strongly suspected.
The patient’s condition improved, and vasopressor therapy was tapered off the next day. Four days later, the patient was weaned from mechanical ventilation and transferred to the step-down unit. Echocardiogram obtained 48 hours after tPA infusion showed essentially normal left ventricular function (60%-65%), a RVSP of 17 mm Hg and mPAP of 13 mm Hg. The patient’s ProBNP levels markedly decreased to 137 pg/mL. Postextubation, the neurologic examination was at baseline. The Neurology Service recommended temporary treatment with levetiracetam, 1000 mg every 12 hours, and the Hematology Service recommended transitioning to direct oral anticoagulation with follow-up. The patient presented significant clinical and respiratory improvement and was referred for home-based physical rehabilitation as recommended by the physical medicine and rehabilitation service before being discharged.
Case 2
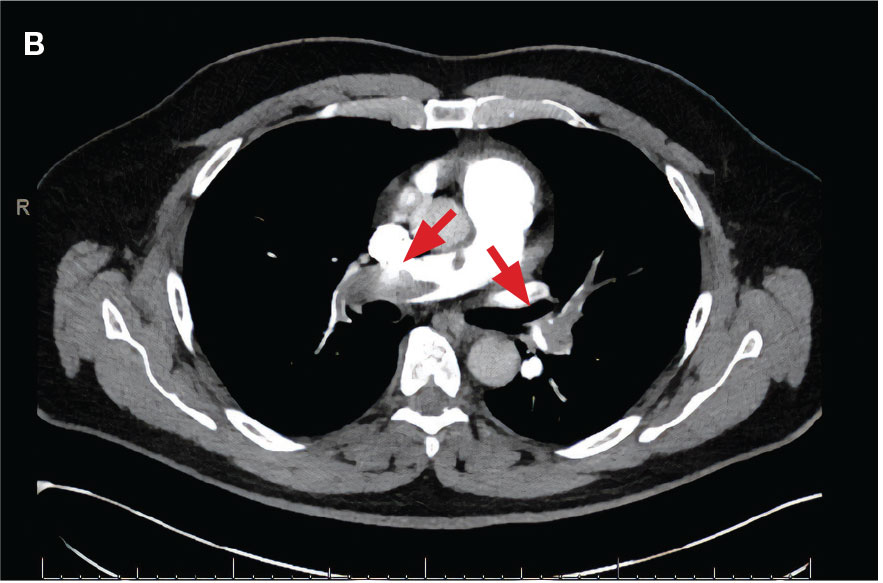
Localized tPA infusion for bilateral PEs via infusion catheters. A 91-year-old male with no history of smoking and a medical history of hypertension, diabetes mellitus, prostate cancer (> 20 years postradiotherapy) and severe osteoarthritis was receiving treatment in the medical ward for medication-induced liver injury secondary to an antibiotic for a urinary tract infection. During the night the patient developed hypotension (86/46 mm Hg), shortness of breath, tachypnea, desaturation, nonradiating retrosternal chest pain, and tachycardia. The hypotension resolved after a 500-mL 0.9 normal saline bolus, and hypoxemia improved with supplemental oxygen via Venturi mask. Chest computed tomography angiography was performed immediately and revealed extensive bilateral acute PE, located most proximally in the right main pulmonary artery (PA) and on the left in the proximal lobar branches, with associated right heart strain. The patient was started on IV heparin with a bolus of 5000 units (80 u/kg) followed by a drip with a partial thromboplastin time goal of 62-103 seconds and transferred to MICU.
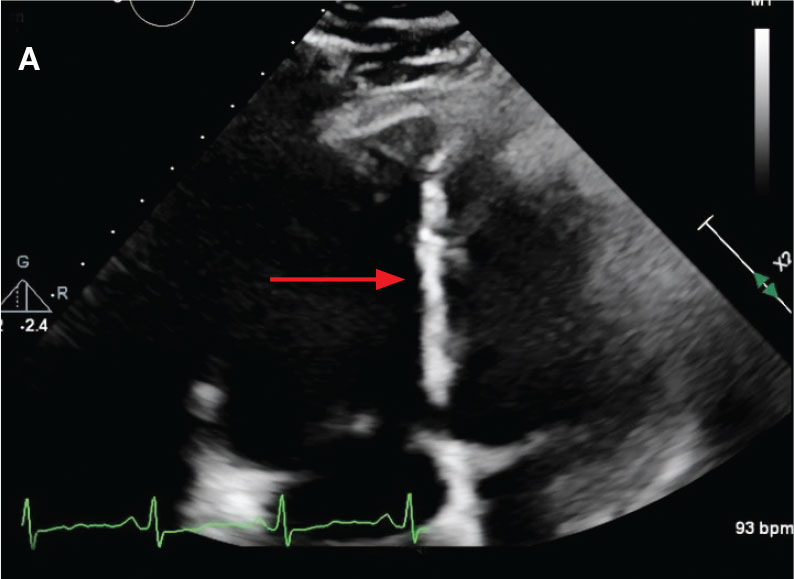
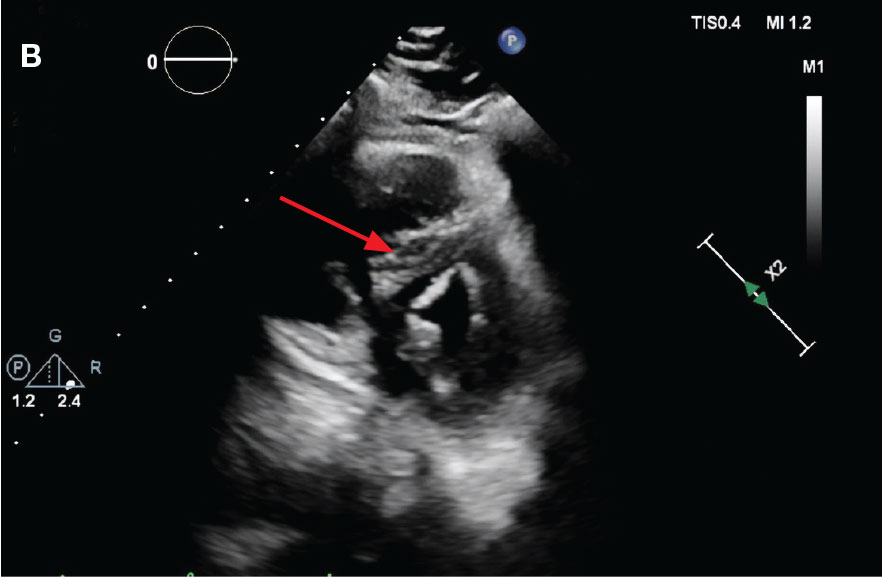
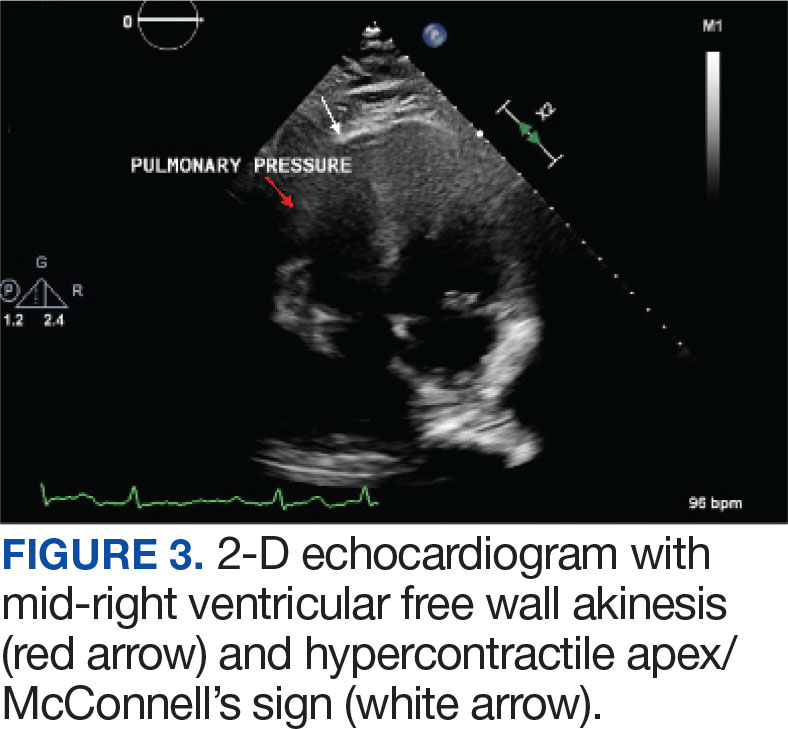
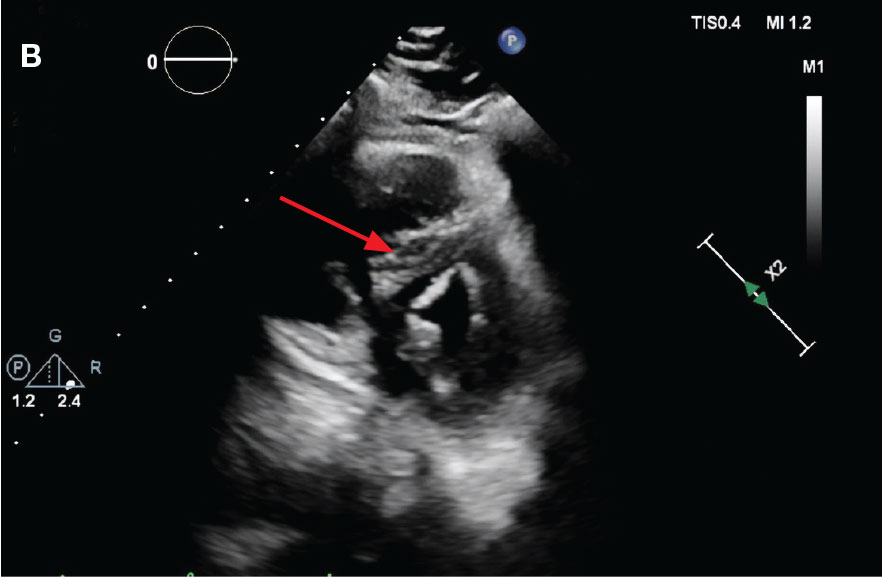
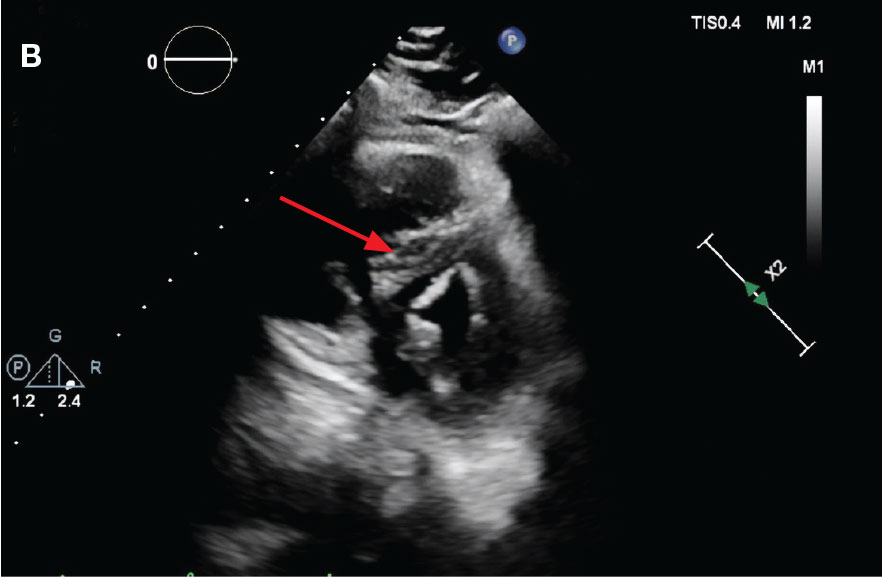
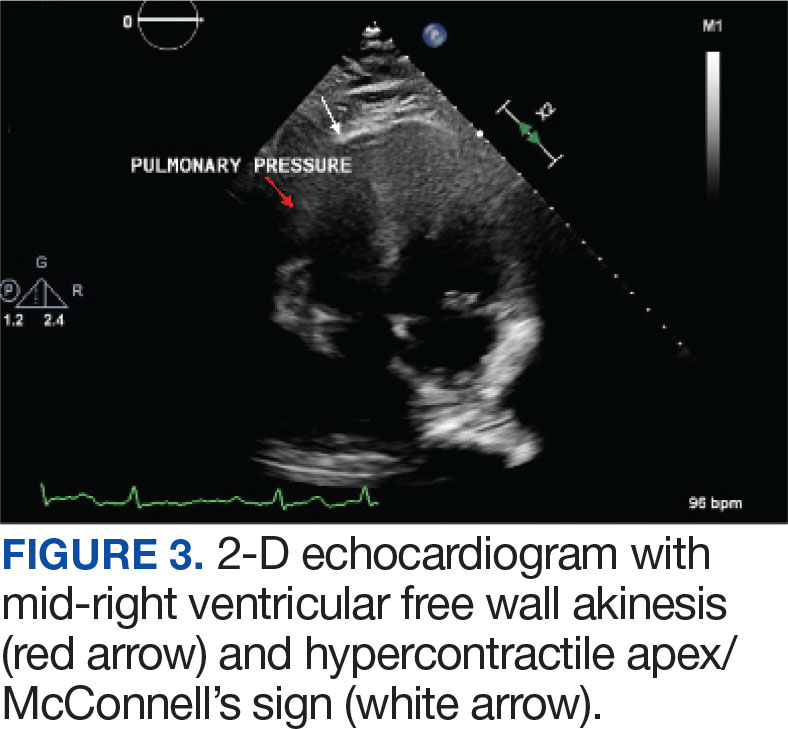
Laboratory findings were notable for proBNP that increased from 115 pg/mL to 4470 pg/mL (reference range, < 450 pg/mL for patients aged 75 years) and elevated troponin levels at 218 ng/L to 295 ng/L (reference range, < 22 ng/L), exhibiting chemical evidence of right heart strain. Initial echocardiogram showed mid-right ventricular free wall akinesis with a hypercontractile apex, suggestive of PE (McConnell’s sign) (Figure 3). Interventional Radiology Service was consulted and recommended tPA infusion given that the patient had bilateral PEs and stable blood pressure.
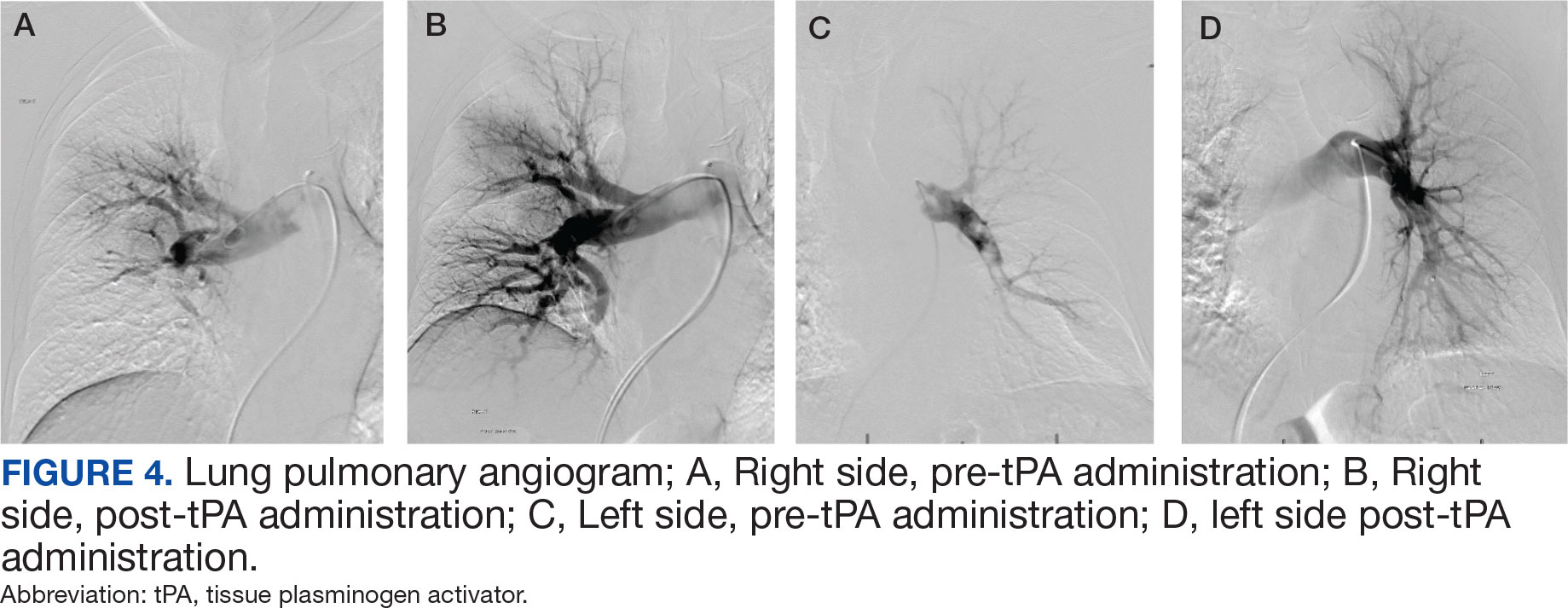
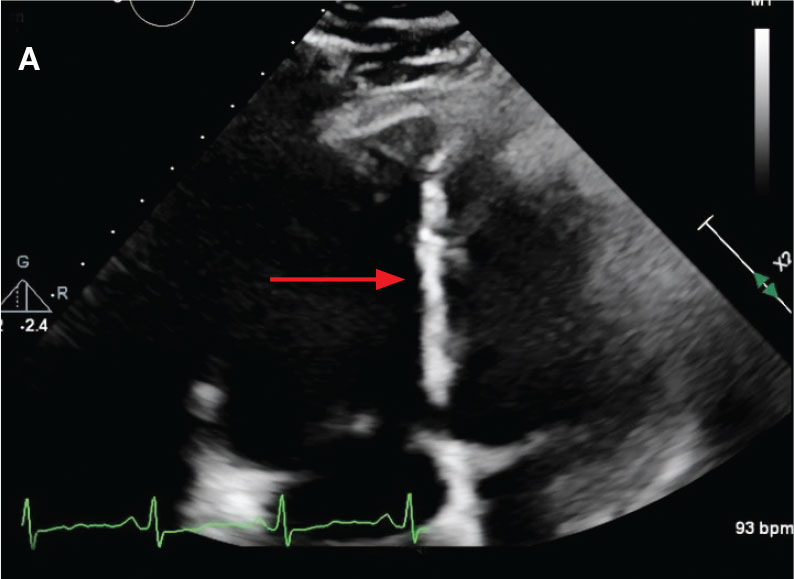
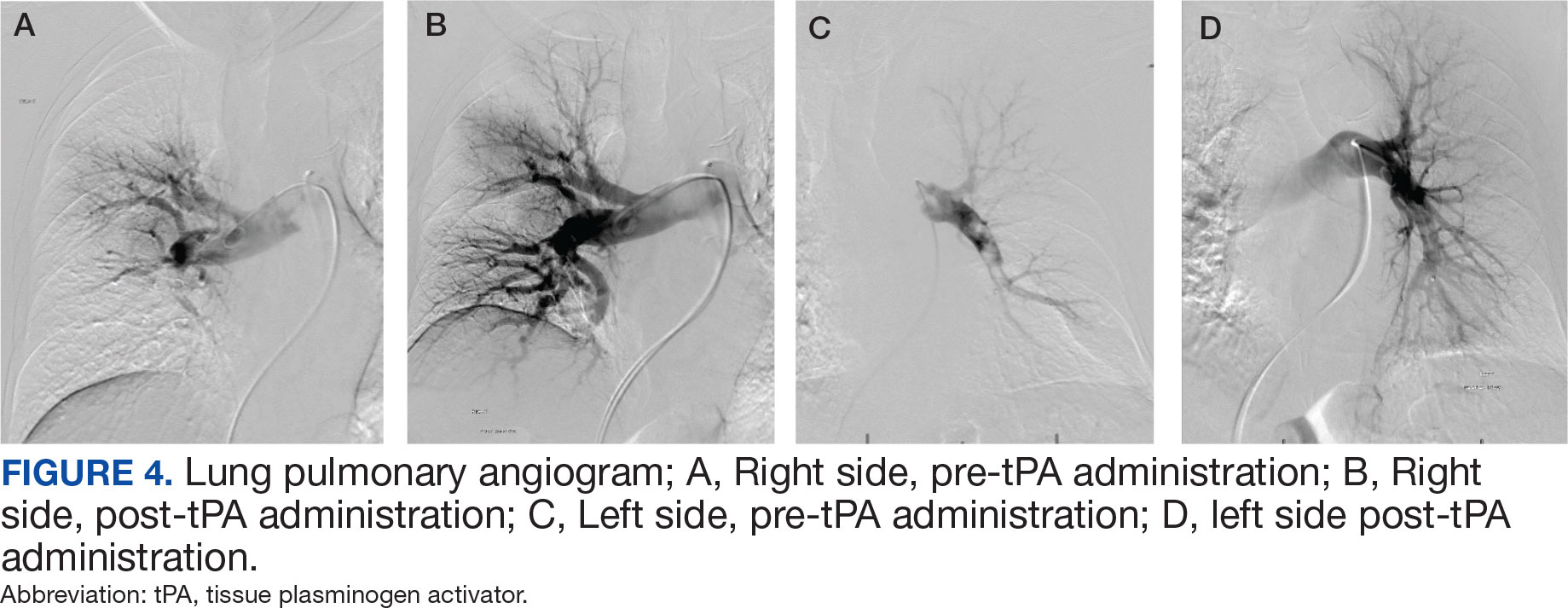
Pulmonary angiogram showed elevated pressures in the right PA of 64/21 mm Hg and the left PA pressures of 63/20 mm Hg. Mechanical disruption of the larger right lower PA thrombus was achieved via a pigtail catheter followed by bilateral catheter bolus infusions of 2 mg tPA (alteplase) and a continuous tPA infusion 0.5 mg/h for 24 hours, in conjunction with a heparin infusion.
After 24 hours of tPA infusion, the catheters were removed, with posttreatment pulmonary angiography demonstrating right and left PA pressures of 42/15 mm Hg and 40/16 mm Hg, respectively. Pre- and postlocalized tPA infusion treatment images are provided for visual comparison (Figure 4). An echocardiogram performed after tPA infusion showed no signs of pulmonary hypertension. The Hematology Service provided recommendations regarding anticoagulation, and after completion of tPA infusion, the patient was transitioned to an unfractioned heparin infusion and subsequently to direct oral anticoagulation prior to transfer back to the medical ward, hemodynamically stable and asymptomatic.
DISCUSSION
PE management can be a straightforward decision when the patient meets criteria for hemodynamic instability, or with small PE burden. In contrast, management can be more challenging in intermediate-risk (submassive) PE when patients remain hemodynamically stable but show signs of cardiopulmonary stress, such as right heart strain, elevated troponins, or increased proBNP levels.2 In these situations, case-by- case evaluation is warranted. A PERT can assess the most beneficial treatment approach by considering factors such as right ventricular dysfunction, hemodynamic status, clot burden, and clinical deterioration despite appropriate anticoagulation. The evidence supporting the benefits these organized teams can provide is growing. These case reports emphasize the need for a multidisciplinary and systematic approach in these complex cases, especially in the management of intermediate-risk PE patients.
Currently, the Veterans Affairs Caribbean Healthcare System does not have an organized PERT, although a multidisciplinary approach was applied in the management of these patients. A systematic, structured team could have decreased time to interventions and alleviated the burden of physician decision-making. Having such a team would streamline the diagnostic pathway for patients presenting from a ward or emergency department with suspected PE.
We present 2 cases of patients found to have a high clot burden from PEs. The patients were initially hemodynamically stable (intermediate-risk PE), but later required systemic or localized thrombolysis due to hemodynamic deterioration despite adequate anticoagulation. Despite similar diagnoses and etiologies, these patients were successfully managed using different approaches, yielding positive outcomes. This reflects the complexity and variability in diagnosing and managing intermediate-risk PE in patients with different comorbidities and clot burden effects. In Case 1, our multidisciplinary approach was obtained via consults to selected services such as interventional radiology, cardiology, and direct involvement of pharmacy. An organized PERT conceivably would have allowed quicker discussions among these services, including hematology, to provide recommendations and collaborative support upon the patient’s arrival to the ED. Additionally, with a PERT team, a systematic approach to these patients could have allowed for an earlier official echocardiogram report for evaluation of right heart strain and develop an adequate therapeutic plan in a timely manner.
In Case 2, consultation with the Interventional Radiology Service yielded a better therapeutic plan, utilizing localized tPA infusion for this older adult patient with increased risk of bleeding with systemic tPA infusion. Having a PERT presents an opportunity to optimize PE management through early recognition, diagnosis, and treatment by institutional consensus from an interdisciplinary team.5,6 These response teams may improve outcomes and prognosis for patients with PE, especially where diagnosis and management is not clear.
The definite etiology of seizure activity in the first case pre- and postcardiac arrest, in the context of no acute intracranial process, remains unknown. Reports have emerged about postreperfusion seizures in acute ischemic stroke, as well as cases of seizures masquerading as PE as the primary presentation. 7,8 However, there were no reports of patients developing seizures post tPA infusion for the treatment of PE. This report may shed light into possible complications secondary to tPA infusion, raising awareness among physicians and encouraging further investigation into its possible etiologies.
CONCLUSIONS
Management of PE can be challenging in patients that meet criteria for intermediate risk. PERTs are a tool that allow for a multidisciplinary, standardized and systematic approach with a diagnostic and treatment algorithm that conceivably would result in a better consensus and therapeutic approach.
- Thompson BT, Kabrhel C. Epidemiology and pathogenesis of acute pulmonary embolism in adults. UpToDate. Wolters Kluwer. Updated December 4, 2023. Accessed February 26, 2025. https://www.uptodate.cn/contents/epidemiology-and-pathogenesis-of-acute-pulmonary-embolism-in-adults
- Kulka HC, Zeller A, Fornaro J, Wuillemin WA, Konstantinides S, Christ M. Acute pulmonary embolism– its diagnosis and treatment from a multidisciplinary viewpoint. Dtsch Arztebl Int. 2021;118(37):618-628. doi:10.3238/arztebl.m2021.0226
- Zghouzi M, Mwansa H, Shore S, et al. Sex, racial, and geographic disparities in pulmonary embolism-related mortality nationwide. Ann Am Thorac Soc. 2023;20(11):1571-1577. doi:10.1513/AnnalsATS.202302-091OC
- Channick RN. The pulmonary embolism response team: why and how? Semin Respir Crit Care Med. 2021;42(2):212-217. doi:10.1055/s-0041-1722963
- Rosovsky R, Zhao K, Sista A, Rivera-Lebron B, Kabrhel C. Pulmonary embolism response teams: purpose, evidence for efficacy, and future research directions. Res Pract Thromb Haemost. 2019;3(3):315-330. doi:10.1002/rth2.12216
- Glazier JJ, Patiño-Velasquez S, Oviedo C. The pulmonary embolism response team: rationale, operation, and outcomes. Int J Angiol. 2022;31(3):198-202. doi:10.1055/s-0042-1750328
- Lekoubou A, Fox J, Ssentongo P. Incidence and association of reperfusion therapies with poststroke seizures: a systematic review and meta-analysis. Stroke. 2020;51(9):2715-2723.doi:10.1161/STROKEAHA.119. 028899
- Alemany M, Nuñez A, Falip M, et al. Acute symptomatic seizures and epilepsy after mechanical thrombectomy. A prospective long-term follow-up study. Seizure. 2021;89:5-9. doi:10.1016/j.seizure.2021.04.011
Pulmonary embolism (PE) is a common cause of morbidity and mortality in the general population.1 The incidence of PE has been reported to range from 39 to 115 per 100,000 persons per year and has remained stable.2 Although mortality rates have declined, they remain high.3 The clinical presentation is nonspecific, making diagnosis and management challenging. A crucial and difficult aspect in the management of patients with PE is weighing the risks vs benefits of treatment, including thrombolytic therapy and other invasive procedures, which carry inherent risks. These factors have led to the development of PE response teams (PERTs) in some hospitals to implement effective multidisciplinary protocols that facilitate prompt diagnosis, management, and follow-up.4
CASE PRESENTATIONS
Case 1
New onset seizures and cardiac arrest in the treatment of saddle PE. A 54-year-old male who worked as a draftsman and truck driver with a history of hypertension and nephrolithiasis presented to the emergency department (ED) with progressive shortness of breath for 2 weeks. On the morning of ED presentation the patient experienced an episode of severe shortness of breath, lightheadedness, and chest pressure. He reported no other symptoms such as palpitations, nausea, vomiting, abdominal discomfort, or extremity pain or swelling. He reported no recent travel, immunization, falls, or surgery. Upon evaluation, the patient was found to be in no acute distress, with stable vital signs and laboratory results except for 2 elevated results: > 20 μg/mL D-dimer (reference range, < 0.5 μg/mL) and N-terminal prohormone brain natriuretic peptide (proBNP) level, 3455 pg/mL (reference range, < 125 pg/mL for patients aged < 75 years). Electrocardiogram showed T-wave inversions in leads V2 to V4. Imaging revealed a saddle PE and left popliteal deep venous thrombosis (Figure 1). The patient received an anticoagulation loading dose and was started on heparin drip upon admission to the medical intensive care unit (MICU) for further management and monitoring. The Interventional Radiology Service recommended full anticoagulation with consideration of reperfusion therapies if deterioration developed.
indicated by arrows in the pulmonary trunk extending to the left pulmonary artery (A),
and obliterating right pulmonary artery and branches of left pulmonary artery (B).
indicated by arrows in the pulmonary trunk extending to the left pulmonary artery (A),
and obliterating right pulmonary artery and branches of left pulmonary artery (B).
While in the MICU, point-of-care ultrasound findings were confirmed with official echocardiogram by the cardiology service, which demonstrated a preserved ejection fraction of 60% to 65%, a D-shaped left ventricle with septal wall hypokinesis secondary to right heart strain (Figure 2), a markedly elevated right ventricular systolic pressure (RVSP) of 73 mm Hg, and a mean pulmonary artery pressure (mPAP) of 38 mm Hg. The patient’s blood pressure progressively decreased, heart rate increased, and he required increased oxygen supplementation. The case was discussed with the Pharmacy Service, and since the patient had no contraindications to thrombolytic therapy, the appropriate dosage was calculated and 100 mg intravenous (IV) tissue plasminogen activator (tPA) was administered over 2 hours.
flattening and deviation to left in direction (A) and septal deviation to left with
formation of D-sign (B).
flattening and deviation to left in direction (A) and septal deviation to left with
formation of D-sign (B).
About 40 minutes into tPA infusion, the patient suddenly experienced marked shortness of breath, diaphoresis, and anxiety with seizure-like involuntary movements; as a result, the infusion was stopped. He also had episodes of posturing, mental status decline, and briefly going in and out of consciousness, which lasted about 3 minutes before he lost consciousness and pulse. High-quality advanced cardiac life support was initiated, followed by endotracheal intubation. Despite a secured airway and return of spontaneous circulation, the patient remained hypotensive and continued to have seizure-like activity.
The patient was administered a total of 8 mg of lorazepam, sedated with propofol, initiated at 5 μg/kg/min, titrated to stop seizure activity at 15μg/kg/min, and later maintained at 10 μg/kg/min, for a RASS of -1, and started on norepinephrine 0.1 μg/kg/min for acute stabilization. Head computed tomography without contrast showed no acute intracranial pathology as etiology of seizures. Seizure etiology differential at this time was broad; however, hypoxemia due to PE and medication adverse effects were strongly suspected.
The patient’s condition improved, and vasopressor therapy was tapered off the next day. Four days later, the patient was weaned from mechanical ventilation and transferred to the step-down unit. Echocardiogram obtained 48 hours after tPA infusion showed essentially normal left ventricular function (60%-65%), a RVSP of 17 mm Hg and mPAP of 13 mm Hg. The patient’s ProBNP levels markedly decreased to 137 pg/mL. Postextubation, the neurologic examination was at baseline. The Neurology Service recommended temporary treatment with levetiracetam, 1000 mg every 12 hours, and the Hematology Service recommended transitioning to direct oral anticoagulation with follow-up. The patient presented significant clinical and respiratory improvement and was referred for home-based physical rehabilitation as recommended by the physical medicine and rehabilitation service before being discharged.
Case 2
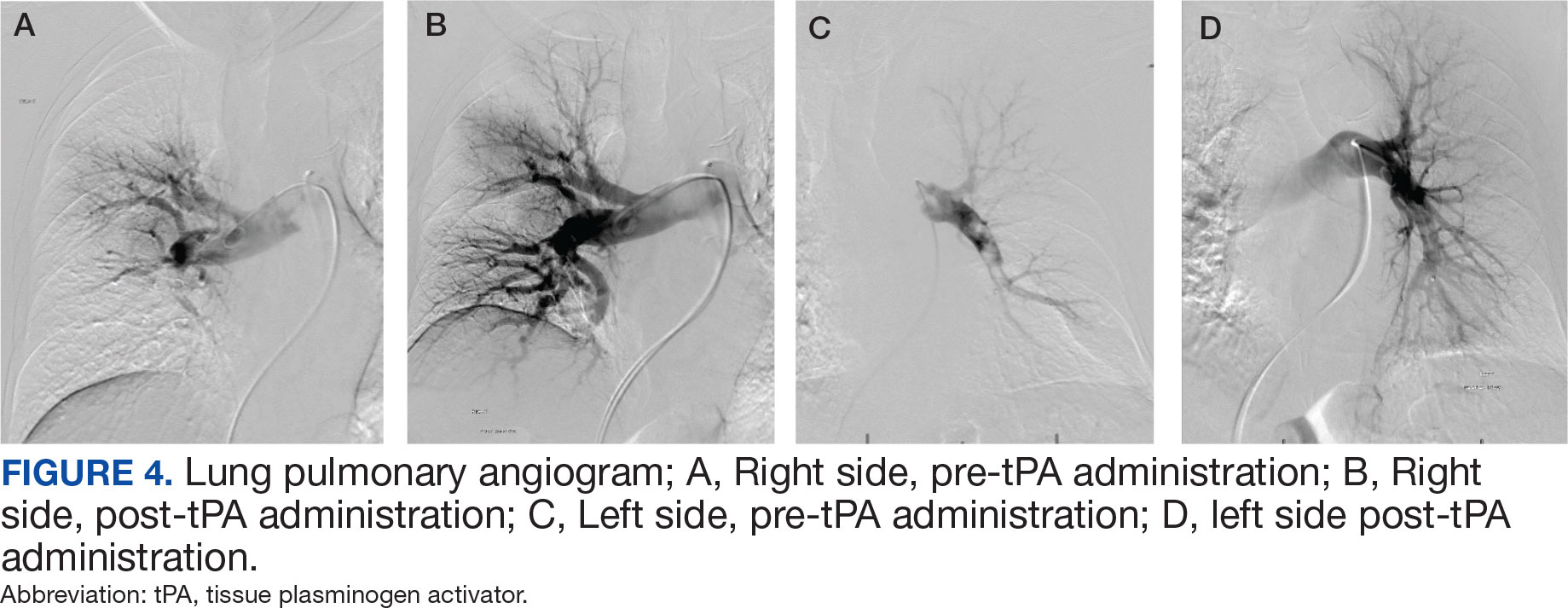
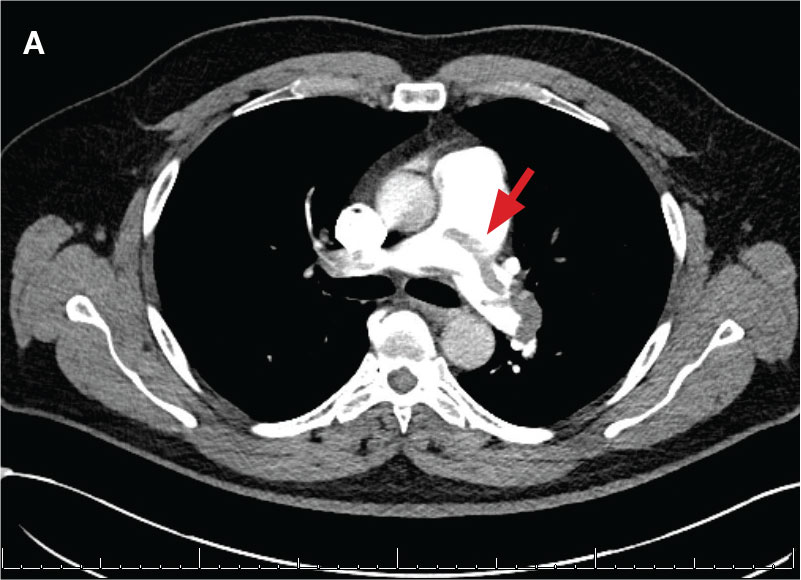
Localized tPA infusion for bilateral PEs via infusion catheters. A 91-year-old male with no history of smoking and a medical history of hypertension, diabetes mellitus, prostate cancer (> 20 years postradiotherapy) and severe osteoarthritis was receiving treatment in the medical ward for medication-induced liver injury secondary to an antibiotic for a urinary tract infection. During the night the patient developed hypotension (86/46 mm Hg), shortness of breath, tachypnea, desaturation, nonradiating retrosternal chest pain, and tachycardia. The hypotension resolved after a 500-mL 0.9 normal saline bolus, and hypoxemia improved with supplemental oxygen via Venturi mask. Chest computed tomography angiography was performed immediately and revealed extensive bilateral acute PE, located most proximally in the right main pulmonary artery (PA) and on the left in the proximal lobar branches, with associated right heart strain. The patient was started on IV heparin with a bolus of 5000 units (80 u/kg) followed by a drip with a partial thromboplastin time goal of 62-103 seconds and transferred to MICU.
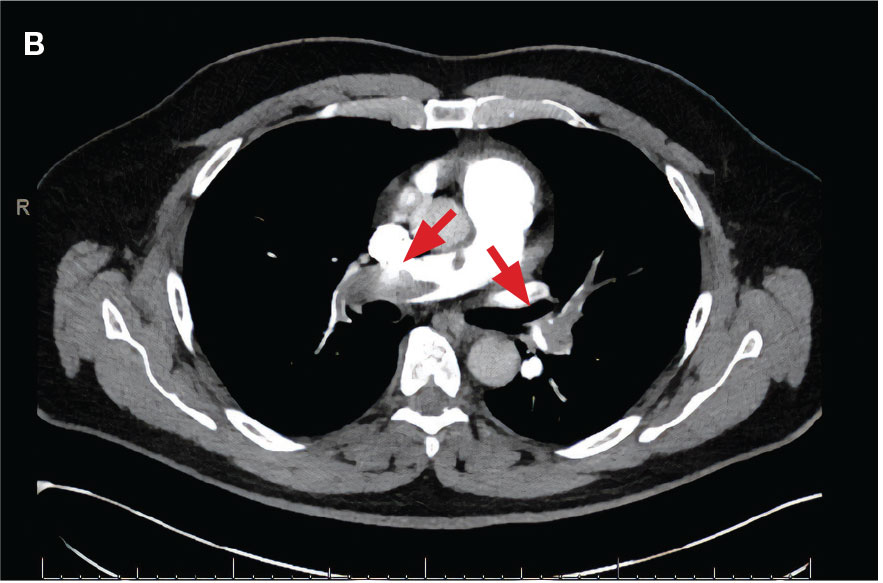
Laboratory findings were notable for proBNP that increased from 115 pg/mL to 4470 pg/mL (reference range, < 450 pg/mL for patients aged 75 years) and elevated troponin levels at 218 ng/L to 295 ng/L (reference range, < 22 ng/L), exhibiting chemical evidence of right heart strain. Initial echocardiogram showed mid-right ventricular free wall akinesis with a hypercontractile apex, suggestive of PE (McConnell’s sign) (Figure 3). Interventional Radiology Service was consulted and recommended tPA infusion given that the patient had bilateral PEs and stable blood pressure.
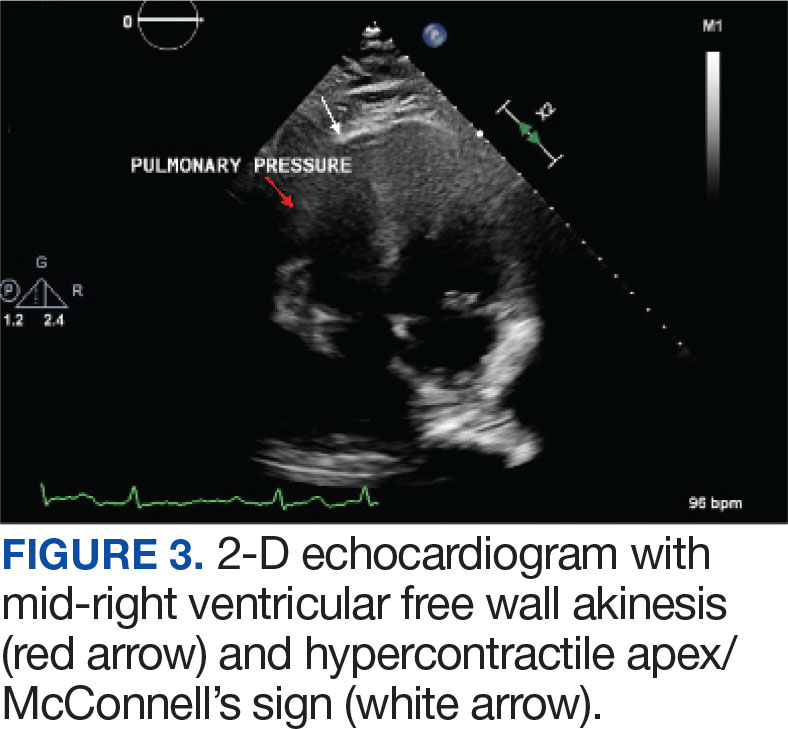
Pulmonary angiogram showed elevated pressures in the right PA of 64/21 mm Hg and the left PA pressures of 63/20 mm Hg. Mechanical disruption of the larger right lower PA thrombus was achieved via a pigtail catheter followed by bilateral catheter bolus infusions of 2 mg tPA (alteplase) and a continuous tPA infusion 0.5 mg/h for 24 hours, in conjunction with a heparin infusion.
After 24 hours of tPA infusion, the catheters were removed, with posttreatment pulmonary angiography demonstrating right and left PA pressures of 42/15 mm Hg and 40/16 mm Hg, respectively. Pre- and postlocalized tPA infusion treatment images are provided for visual comparison (Figure 4). An echocardiogram performed after tPA infusion showed no signs of pulmonary hypertension. The Hematology Service provided recommendations regarding anticoagulation, and after completion of tPA infusion, the patient was transitioned to an unfractioned heparin infusion and subsequently to direct oral anticoagulation prior to transfer back to the medical ward, hemodynamically stable and asymptomatic.
DISCUSSION
PE management can be a straightforward decision when the patient meets criteria for hemodynamic instability, or with small PE burden. In contrast, management can be more challenging in intermediate-risk (submassive) PE when patients remain hemodynamically stable but show signs of cardiopulmonary stress, such as right heart strain, elevated troponins, or increased proBNP levels.2 In these situations, case-by- case evaluation is warranted. A PERT can assess the most beneficial treatment approach by considering factors such as right ventricular dysfunction, hemodynamic status, clot burden, and clinical deterioration despite appropriate anticoagulation. The evidence supporting the benefits these organized teams can provide is growing. These case reports emphasize the need for a multidisciplinary and systematic approach in these complex cases, especially in the management of intermediate-risk PE patients.
Currently, the Veterans Affairs Caribbean Healthcare System does not have an organized PERT, although a multidisciplinary approach was applied in the management of these patients. A systematic, structured team could have decreased time to interventions and alleviated the burden of physician decision-making. Having such a team would streamline the diagnostic pathway for patients presenting from a ward or emergency department with suspected PE.
We present 2 cases of patients found to have a high clot burden from PEs. The patients were initially hemodynamically stable (intermediate-risk PE), but later required systemic or localized thrombolysis due to hemodynamic deterioration despite adequate anticoagulation. Despite similar diagnoses and etiologies, these patients were successfully managed using different approaches, yielding positive outcomes. This reflects the complexity and variability in diagnosing and managing intermediate-risk PE in patients with different comorbidities and clot burden effects. In Case 1, our multidisciplinary approach was obtained via consults to selected services such as interventional radiology, cardiology, and direct involvement of pharmacy. An organized PERT conceivably would have allowed quicker discussions among these services, including hematology, to provide recommendations and collaborative support upon the patient’s arrival to the ED. Additionally, with a PERT team, a systematic approach to these patients could have allowed for an earlier official echocardiogram report for evaluation of right heart strain and develop an adequate therapeutic plan in a timely manner.
In Case 2, consultation with the Interventional Radiology Service yielded a better therapeutic plan, utilizing localized tPA infusion for this older adult patient with increased risk of bleeding with systemic tPA infusion. Having a PERT presents an opportunity to optimize PE management through early recognition, diagnosis, and treatment by institutional consensus from an interdisciplinary team.5,6 These response teams may improve outcomes and prognosis for patients with PE, especially where diagnosis and management is not clear.
The definite etiology of seizure activity in the first case pre- and postcardiac arrest, in the context of no acute intracranial process, remains unknown. Reports have emerged about postreperfusion seizures in acute ischemic stroke, as well as cases of seizures masquerading as PE as the primary presentation. 7,8 However, there were no reports of patients developing seizures post tPA infusion for the treatment of PE. This report may shed light into possible complications secondary to tPA infusion, raising awareness among physicians and encouraging further investigation into its possible etiologies.
CONCLUSIONS
Management of PE can be challenging in patients that meet criteria for intermediate risk. PERTs are a tool that allow for a multidisciplinary, standardized and systematic approach with a diagnostic and treatment algorithm that conceivably would result in a better consensus and therapeutic approach.
Pulmonary embolism (PE) is a common cause of morbidity and mortality in the general population.1 The incidence of PE has been reported to range from 39 to 115 per 100,000 persons per year and has remained stable.2 Although mortality rates have declined, they remain high.3 The clinical presentation is nonspecific, making diagnosis and management challenging. A crucial and difficult aspect in the management of patients with PE is weighing the risks vs benefits of treatment, including thrombolytic therapy and other invasive procedures, which carry inherent risks. These factors have led to the development of PE response teams (PERTs) in some hospitals to implement effective multidisciplinary protocols that facilitate prompt diagnosis, management, and follow-up.4
CASE PRESENTATIONS
Case 1
New onset seizures and cardiac arrest in the treatment of saddle PE. A 54-year-old male who worked as a draftsman and truck driver with a history of hypertension and nephrolithiasis presented to the emergency department (ED) with progressive shortness of breath for 2 weeks. On the morning of ED presentation the patient experienced an episode of severe shortness of breath, lightheadedness, and chest pressure. He reported no other symptoms such as palpitations, nausea, vomiting, abdominal discomfort, or extremity pain or swelling. He reported no recent travel, immunization, falls, or surgery. Upon evaluation, the patient was found to be in no acute distress, with stable vital signs and laboratory results except for 2 elevated results: > 20 μg/mL D-dimer (reference range, < 0.5 μg/mL) and N-terminal prohormone brain natriuretic peptide (proBNP) level, 3455 pg/mL (reference range, < 125 pg/mL for patients aged < 75 years). Electrocardiogram showed T-wave inversions in leads V2 to V4. Imaging revealed a saddle PE and left popliteal deep venous thrombosis (Figure 1). The patient received an anticoagulation loading dose and was started on heparin drip upon admission to the medical intensive care unit (MICU) for further management and monitoring. The Interventional Radiology Service recommended full anticoagulation with consideration of reperfusion therapies if deterioration developed.
indicated by arrows in the pulmonary trunk extending to the left pulmonary artery (A),
and obliterating right pulmonary artery and branches of left pulmonary artery (B).
indicated by arrows in the pulmonary trunk extending to the left pulmonary artery (A),
and obliterating right pulmonary artery and branches of left pulmonary artery (B).
While in the MICU, point-of-care ultrasound findings were confirmed with official echocardiogram by the cardiology service, which demonstrated a preserved ejection fraction of 60% to 65%, a D-shaped left ventricle with septal wall hypokinesis secondary to right heart strain (Figure 2), a markedly elevated right ventricular systolic pressure (RVSP) of 73 mm Hg, and a mean pulmonary artery pressure (mPAP) of 38 mm Hg. The patient’s blood pressure progressively decreased, heart rate increased, and he required increased oxygen supplementation. The case was discussed with the Pharmacy Service, and since the patient had no contraindications to thrombolytic therapy, the appropriate dosage was calculated and 100 mg intravenous (IV) tissue plasminogen activator (tPA) was administered over 2 hours.
flattening and deviation to left in direction (A) and septal deviation to left with
formation of D-sign (B).
flattening and deviation to left in direction (A) and septal deviation to left with
formation of D-sign (B).
About 40 minutes into tPA infusion, the patient suddenly experienced marked shortness of breath, diaphoresis, and anxiety with seizure-like involuntary movements; as a result, the infusion was stopped. He also had episodes of posturing, mental status decline, and briefly going in and out of consciousness, which lasted about 3 minutes before he lost consciousness and pulse. High-quality advanced cardiac life support was initiated, followed by endotracheal intubation. Despite a secured airway and return of spontaneous circulation, the patient remained hypotensive and continued to have seizure-like activity.
The patient was administered a total of 8 mg of lorazepam, sedated with propofol, initiated at 5 μg/kg/min, titrated to stop seizure activity at 15μg/kg/min, and later maintained at 10 μg/kg/min, for a RASS of -1, and started on norepinephrine 0.1 μg/kg/min for acute stabilization. Head computed tomography without contrast showed no acute intracranial pathology as etiology of seizures. Seizure etiology differential at this time was broad; however, hypoxemia due to PE and medication adverse effects were strongly suspected.
The patient’s condition improved, and vasopressor therapy was tapered off the next day. Four days later, the patient was weaned from mechanical ventilation and transferred to the step-down unit. Echocardiogram obtained 48 hours after tPA infusion showed essentially normal left ventricular function (60%-65%), a RVSP of 17 mm Hg and mPAP of 13 mm Hg. The patient’s ProBNP levels markedly decreased to 137 pg/mL. Postextubation, the neurologic examination was at baseline. The Neurology Service recommended temporary treatment with levetiracetam, 1000 mg every 12 hours, and the Hematology Service recommended transitioning to direct oral anticoagulation with follow-up. The patient presented significant clinical and respiratory improvement and was referred for home-based physical rehabilitation as recommended by the physical medicine and rehabilitation service before being discharged.
Case 2
Localized tPA infusion for bilateral PEs via infusion catheters. A 91-year-old male with no history of smoking and a medical history of hypertension, diabetes mellitus, prostate cancer (> 20 years postradiotherapy) and severe osteoarthritis was receiving treatment in the medical ward for medication-induced liver injury secondary to an antibiotic for a urinary tract infection. During the night the patient developed hypotension (86/46 mm Hg), shortness of breath, tachypnea, desaturation, nonradiating retrosternal chest pain, and tachycardia. The hypotension resolved after a 500-mL 0.9 normal saline bolus, and hypoxemia improved with supplemental oxygen via Venturi mask. Chest computed tomography angiography was performed immediately and revealed extensive bilateral acute PE, located most proximally in the right main pulmonary artery (PA) and on the left in the proximal lobar branches, with associated right heart strain. The patient was started on IV heparin with a bolus of 5000 units (80 u/kg) followed by a drip with a partial thromboplastin time goal of 62-103 seconds and transferred to MICU.
Laboratory findings were notable for proBNP that increased from 115 pg/mL to 4470 pg/mL (reference range, < 450 pg/mL for patients aged 75 years) and elevated troponin levels at 218 ng/L to 295 ng/L (reference range, < 22 ng/L), exhibiting chemical evidence of right heart strain. Initial echocardiogram showed mid-right ventricular free wall akinesis with a hypercontractile apex, suggestive of PE (McConnell’s sign) (Figure 3). Interventional Radiology Service was consulted and recommended tPA infusion given that the patient had bilateral PEs and stable blood pressure.
Pulmonary angiogram showed elevated pressures in the right PA of 64/21 mm Hg and the left PA pressures of 63/20 mm Hg. Mechanical disruption of the larger right lower PA thrombus was achieved via a pigtail catheter followed by bilateral catheter bolus infusions of 2 mg tPA (alteplase) and a continuous tPA infusion 0.5 mg/h for 24 hours, in conjunction with a heparin infusion.
After 24 hours of tPA infusion, the catheters were removed, with posttreatment pulmonary angiography demonstrating right and left PA pressures of 42/15 mm Hg and 40/16 mm Hg, respectively. Pre- and postlocalized tPA infusion treatment images are provided for visual comparison (Figure 4). An echocardiogram performed after tPA infusion showed no signs of pulmonary hypertension. The Hematology Service provided recommendations regarding anticoagulation, and after completion of tPA infusion, the patient was transitioned to an unfractioned heparin infusion and subsequently to direct oral anticoagulation prior to transfer back to the medical ward, hemodynamically stable and asymptomatic.
DISCUSSION
PE management can be a straightforward decision when the patient meets criteria for hemodynamic instability, or with small PE burden. In contrast, management can be more challenging in intermediate-risk (submassive) PE when patients remain hemodynamically stable but show signs of cardiopulmonary stress, such as right heart strain, elevated troponins, or increased proBNP levels.2 In these situations, case-by- case evaluation is warranted. A PERT can assess the most beneficial treatment approach by considering factors such as right ventricular dysfunction, hemodynamic status, clot burden, and clinical deterioration despite appropriate anticoagulation. The evidence supporting the benefits these organized teams can provide is growing. These case reports emphasize the need for a multidisciplinary and systematic approach in these complex cases, especially in the management of intermediate-risk PE patients.
Currently, the Veterans Affairs Caribbean Healthcare System does not have an organized PERT, although a multidisciplinary approach was applied in the management of these patients. A systematic, structured team could have decreased time to interventions and alleviated the burden of physician decision-making. Having such a team would streamline the diagnostic pathway for patients presenting from a ward or emergency department with suspected PE.
We present 2 cases of patients found to have a high clot burden from PEs. The patients were initially hemodynamically stable (intermediate-risk PE), but later required systemic or localized thrombolysis due to hemodynamic deterioration despite adequate anticoagulation. Despite similar diagnoses and etiologies, these patients were successfully managed using different approaches, yielding positive outcomes. This reflects the complexity and variability in diagnosing and managing intermediate-risk PE in patients with different comorbidities and clot burden effects. In Case 1, our multidisciplinary approach was obtained via consults to selected services such as interventional radiology, cardiology, and direct involvement of pharmacy. An organized PERT conceivably would have allowed quicker discussions among these services, including hematology, to provide recommendations and collaborative support upon the patient’s arrival to the ED. Additionally, with a PERT team, a systematic approach to these patients could have allowed for an earlier official echocardiogram report for evaluation of right heart strain and develop an adequate therapeutic plan in a timely manner.
In Case 2, consultation with the Interventional Radiology Service yielded a better therapeutic plan, utilizing localized tPA infusion for this older adult patient with increased risk of bleeding with systemic tPA infusion. Having a PERT presents an opportunity to optimize PE management through early recognition, diagnosis, and treatment by institutional consensus from an interdisciplinary team.5,6 These response teams may improve outcomes and prognosis for patients with PE, especially where diagnosis and management is not clear.
The definite etiology of seizure activity in the first case pre- and postcardiac arrest, in the context of no acute intracranial process, remains unknown. Reports have emerged about postreperfusion seizures in acute ischemic stroke, as well as cases of seizures masquerading as PE as the primary presentation. 7,8 However, there were no reports of patients developing seizures post tPA infusion for the treatment of PE. This report may shed light into possible complications secondary to tPA infusion, raising awareness among physicians and encouraging further investigation into its possible etiologies.
CONCLUSIONS
Management of PE can be challenging in patients that meet criteria for intermediate risk. PERTs are a tool that allow for a multidisciplinary, standardized and systematic approach with a diagnostic and treatment algorithm that conceivably would result in a better consensus and therapeutic approach.
- Thompson BT, Kabrhel C. Epidemiology and pathogenesis of acute pulmonary embolism in adults. UpToDate. Wolters Kluwer. Updated December 4, 2023. Accessed February 26, 2025. https://www.uptodate.cn/contents/epidemiology-and-pathogenesis-of-acute-pulmonary-embolism-in-adults
- Kulka HC, Zeller A, Fornaro J, Wuillemin WA, Konstantinides S, Christ M. Acute pulmonary embolism– its diagnosis and treatment from a multidisciplinary viewpoint. Dtsch Arztebl Int. 2021;118(37):618-628. doi:10.3238/arztebl.m2021.0226
- Zghouzi M, Mwansa H, Shore S, et al. Sex, racial, and geographic disparities in pulmonary embolism-related mortality nationwide. Ann Am Thorac Soc. 2023;20(11):1571-1577. doi:10.1513/AnnalsATS.202302-091OC
- Channick RN. The pulmonary embolism response team: why and how? Semin Respir Crit Care Med. 2021;42(2):212-217. doi:10.1055/s-0041-1722963
- Rosovsky R, Zhao K, Sista A, Rivera-Lebron B, Kabrhel C. Pulmonary embolism response teams: purpose, evidence for efficacy, and future research directions. Res Pract Thromb Haemost. 2019;3(3):315-330. doi:10.1002/rth2.12216
- Glazier JJ, Patiño-Velasquez S, Oviedo C. The pulmonary embolism response team: rationale, operation, and outcomes. Int J Angiol. 2022;31(3):198-202. doi:10.1055/s-0042-1750328
- Lekoubou A, Fox J, Ssentongo P. Incidence and association of reperfusion therapies with poststroke seizures: a systematic review and meta-analysis. Stroke. 2020;51(9):2715-2723.doi:10.1161/STROKEAHA.119. 028899
- Alemany M, Nuñez A, Falip M, et al. Acute symptomatic seizures and epilepsy after mechanical thrombectomy. A prospective long-term follow-up study. Seizure. 2021;89:5-9. doi:10.1016/j.seizure.2021.04.011
- Thompson BT, Kabrhel C. Epidemiology and pathogenesis of acute pulmonary embolism in adults. UpToDate. Wolters Kluwer. Updated December 4, 2023. Accessed February 26, 2025. https://www.uptodate.cn/contents/epidemiology-and-pathogenesis-of-acute-pulmonary-embolism-in-adults
- Kulka HC, Zeller A, Fornaro J, Wuillemin WA, Konstantinides S, Christ M. Acute pulmonary embolism– its diagnosis and treatment from a multidisciplinary viewpoint. Dtsch Arztebl Int. 2021;118(37):618-628. doi:10.3238/arztebl.m2021.0226
- Zghouzi M, Mwansa H, Shore S, et al. Sex, racial, and geographic disparities in pulmonary embolism-related mortality nationwide. Ann Am Thorac Soc. 2023;20(11):1571-1577. doi:10.1513/AnnalsATS.202302-091OC
- Channick RN. The pulmonary embolism response team: why and how? Semin Respir Crit Care Med. 2021;42(2):212-217. doi:10.1055/s-0041-1722963
- Rosovsky R, Zhao K, Sista A, Rivera-Lebron B, Kabrhel C. Pulmonary embolism response teams: purpose, evidence for efficacy, and future research directions. Res Pract Thromb Haemost. 2019;3(3):315-330. doi:10.1002/rth2.12216
- Glazier JJ, Patiño-Velasquez S, Oviedo C. The pulmonary embolism response team: rationale, operation, and outcomes. Int J Angiol. 2022;31(3):198-202. doi:10.1055/s-0042-1750328
- Lekoubou A, Fox J, Ssentongo P. Incidence and association of reperfusion therapies with poststroke seizures: a systematic review and meta-analysis. Stroke. 2020;51(9):2715-2723.doi:10.1161/STROKEAHA.119. 028899
- Alemany M, Nuñez A, Falip M, et al. Acute symptomatic seizures and epilepsy after mechanical thrombectomy. A prospective long-term follow-up study. Seizure. 2021;89:5-9. doi:10.1016/j.seizure.2021.04.011
The Need for a Multidisciplinary Approach for Successful High-Risk Pulmonary Embolism Treatment
The Need for a Multidisciplinary Approach for Successful High-Risk Pulmonary Embolism Treatment
Renal Replacement Therapy in a Patient Diagnosed With Pancreatitis Secondary to Severe Leptospirosis
In areas where the zoonotic disease leptospirosis is endemic, reduced morbidity and mortality is strongly linked to quick initiation of renal replacement therapy.
Leptospirosis (LS) is considered the most common and widespread zoonotic disease in the world. Numerous outbreaks have occurred in the past 10 years. Due to its technically difficult diagnosis, LS is severely underrecognized, underdiagnosed, and therefore, underreported.1,2 The Centers for Disease Control and Prevention (CDC) estimate 100 to 150 cases of LS are identified annually in the US, with about 50% of those cases occurring in Puerto Rico (PR).3 Specifically in PR, about 15 to 100 cases of suspected LS were reported annually between 2000 and 2009, with 59 cases and 1 death reported in 2010. The data are thought to be severely underreported due to a lack of widespread diagnostic testing availability in PR and no formal veterinary and environmental surveillance programs to monitor the incidence of animal cases and actual circulating serovars.4
A recent systematic review of 80 studies from 34 countries on morbidity and mortality of LS revealed that the global incidence and mortality is about 1.03 million cases and 58,900 deaths every year. Almost half of the reported deaths were adult males aged 20 to 49 years.5 Although mild cases of LS are not associated with an elevated mortality, icteric LS with renal failure (Weil disease) carries a mortality rate of 10%.6 In patients who develop hemorrhagic pneumonitis, mortality may be as high as 50 to 70%.7 Therefore, it is pivotal that clinicians recognize the disease early, that novel modalities of treatment continue to be developed, and that their impact on patient morbidity and mortality are studied and documented.
Case Presentation
A 43-year-old man with a medical history of schizophrenia presented to the emergency department at the US Department of Veterans Affairs (VA) Caribbean Healthcare System in San Juan, PR, after experiencing 1 week of intermittent fever, myalgia, and general weakness. Emergency medical services had found him disheveled and in a rodent-infested swamp area several days before admission. Initial vital signs were within normal limits.
On physical examination, the patient was afebrile, without acute distress, but he had diffuse jaundice and mild epigastric tenderness without evidence of peritoneal irritation. His complete blood count was remarkable for leukocytosis with left shifting, adequate hemoglobin levels but with 9 × 103 U/L platelets. The complete metabolic panel demonstrated an aspartate aminotransferase level of 564 U/L, alanine transaminase level of 462 U/L, total bilirubin of 12 mg/dL, which 10.2 mg/dL were direct bilirubin, and an alkaline phosphate of 345 U/L. Lipase levels were measured at 626 U/L. Marked coagulopathy also was present. The toxicology panel, including acetaminophen and salicylate acid levels, did not reveal the presence of any of the tested substances, and chest imaging did not demonstrate any infiltrates.
An abdominal ultrasound was negative for acute cholestatic pathologies, such as cholelithiasis, cholecystitis, or choledocholithiasis. Nonetheless, a noncontrast abdominopelvic computed tomography was remarkable for peripancreatic fat stranding, which raised suspicion for a diagnosis of pancreatitis.
Once the patient was transferred to the intensive care unit, he developed several episodes of hematemesis, leading to hemodynamical instability and severe respiratory distress. Due to anticipated respiratory failure and need for airway securement, endotracheal intubation was performed. Multiple packed red blood cells were transfused, and the patient was started in vasopressor support.
Diagnosis
A presumptive diagnosis of LS was made due to a considerable history of rodent exposure. The patient was started on broad-spectrum parenteral antibiotics, vancomycin 750 mg every 24 hours, metronidazole 500 mg every 8 hours, and ceftriaxone 2 g IV daily for adequate coverage against Leptospira spp. Despite 72 hours of antibiotic treatment, the patient’s clinical state deteriorated. He required high dosages of norepinephrine (1.5 mcg/kg/min) and vasopressin (0.03 U/min) to maintain adequate organ perfusion. Despite lung protective settings with low tidal volume and a high positive end-expiratory pressure, there was difficulty maintaining adequate oxygenation. Chest imaging was remarkable for bilateral infiltrates concerning for acute respiratory distress syndrome (ARDS).
The coagulopathy and cholestasis continued to worsen, and the renal failure progressed from nonoliguric to anuric. Because of this progression, the patient was started on continuous renal replacement therapy (CRRT) by hemodialysis. Within 24 hours of initiating CRRT, the patient’s clinical status improved dramatically. Vasopressor support was weaned, the coagulopathy resolved, and the cholestasis was improving. The patient’s respiratory status improved in such a manner that he was extubated by the seventh day after being placed on mechanical ventilation. The urine and blood samples sent for identification of Leptospira spp. through polymerase chain reaction (PCR) returned positive by the ninth day of admission. While on CRRT, the patient’s renal function eventually returned to baseline, and he was discharged 12 days after admission.
Discussion
The spirochetes of the genus Leptospira include both saprophytic and pathogenic species. These pathogenic Leptospira spp. have adapted to a grand variety of zoonotic hosts, the most important being rodents. They serve as vectors for the contraction of the disease by humans. Initial infection in rodents by Leptospira spp. causes a systemic illness followed by a persistent colonization of renal tubules from which they are excreted in the urine and into the environment. Humans, in turn, are an incidental host unable to induce a carrier state for the transmission of the pathogenic organism.1 The time from exposure to onset of symptoms, or incubation phase, averages 7 to 12 days but may range from 3 to 30 days.8
LS has been described as having 2 discernable but often coexisting phases. The first, an acute febrile bacteremic phase, has been noted to last about 9 days in about 85% of patients, although a minority have persistent fever from 2 weeks to > 30 days. A second phase, the immune or inflammatory phase, is characterized by a second fever spike preceded by 1 to 5 afebrile days in which there is presence of IgM antibodies and resolution of leptospiremia but positive urine cultures.9 Weil disease may present as the second phase of the disease or as a single, progressive illness from its first manifestation. It is characterized by a triad of jaundice, renal failure, and hemorrhage or coagulopathy.10 Weil disease is of great concern and importance due to its associated higher mortality than that found with the mildest form of the disease.
There are studies that advocate for RRT as an intricate part of the treatment regimen in LS to remove the inflammatory cytokines produced as a reaction to the spirochete.11 In tropical countries with a higher incidence of the disease, leptospirosis is an important cause of acute kidney injury (AKI), depending on multiple factors, including the AKI definition that is used.12 Renal invasion by Leptospira spp. produces acute tubular necrosis (ATN) and cell edema during the first week and then could progress to acute interstitial nephritis (AIN) in 2 to 3 weeks. It is believed that the mechanism for the Leptospira spp. invasion of the tubules that results in damage is associated with the antigenic components in its outer membrane; the most important outer membrane protein expressed during infection is LipL32. This protein increases the production of proinflammatory proteins, such as inducible nitric oxide synthase, monocyte chemotactic protein-1 (CCL2/MCP-1), T cells, and tumor necrosis factor.13
Although doxycycline has been recommended for the prophylaxis and treatment of mild LS, the preferred agent and the conferred benefits of antibiotic treatment overall for the severe form of the disease has been controversial. Traditionally, penicillin G sodium has been recommended as the first-line antibiotic treatment for moderate-to-severe LS.14 Nonetheless, there has been an increasing pattern of penicillin resistance among Leptospira spp. that has prompted the study and use of alternative agents.
An open-label, randomized comparison of parenteral cefotaxime, penicillin G sodium, and doxycycline for the treatment of suspected severe leptospirosis conducted by Suputtamongkol and colleagues showed no difference in mortality, defervescence, or time to resolution of abnormal laboratory findings.15 Current CDC recommendations include the use of parenteral penicillin 1.5 MU every 6 hours as the drug of choice, with ceftriaxone 1 g administered IV every 24 hours equally as effective.3
In addition to antimicrobial therapy, supportive care has shifted to include hemodialysis in those patients who develop AKI as part of the disease. Andrade and colleagues conducted a study of 33 patients with LS in Brazil that was set to compare the impact of door-to-dialysis time and dosage of hemodialysis on mortality. In patients with a quicker door-to-dialysis time and daily hemodialysis sessions, there was a 50% (16.7% vs 66.7%) absolute mortality reduction when compared with those with delayed initiation and alternate-day hemodialysis sessions.11 A follow-up prospective study compared the use of traditional sustained low-efficiency dialysis (SLED) with the use of extended SLED via hemodiafiltration in patients with LS presenting with ARDS and AKI. Although hemodiafiltration resulted in a relative decrease in serum levels of interleukin (IL)-17, IL-7, and CCL2/MCP-1, there was no significant difference in mortality.16 The most important prognostic factor in severe LS presenting with AKI and relating to RRT is a shorter door-to-dialysis time and increased dose, not the mode of dialysis clearance. Nonetheless, both RRT methods resulted in a progressive decrease in inflammatory mediators that have been associated with ATN and AIN in the context of LS.16 The authors argue that using CRRT instead of SLED via hemodiafiltration could have accentuated the effects of the reduction that inflammatory mediators may have on mortality in patients with severe LS.
Conclusions
LS continues to be of interest due to its current status as the most common zoonotic disease and its widespread prevalence throughout the globe. Novel treatment modalities for LS, specifically for Weil disease, continue to be developed with the goal of reducing the current mortality rate associated with the disease.
In endemic areas, prompt recognition is essential to initiate the recommended therapy. Parenteral antibiotics, such as penicillin G sodium and ceftriaxone, continue to be the mainstay of treatment and constitute the current CDC recommendations. Nonetheless, early initiation of CRRT has been shown to greatly reduce the mortality associated with Weil disease and, when available, should be considered in these patients.
Our patient failed to improve while receiving parenteral antibiotics alone but showed marked improvement after being placed on CRRT. Furthermore, initiation of CRRT resulted in near-complete resolution of his organ dysfunction and eventual discharge from the hospital. This case serves to further support the use of early CRRT as part of the standard of care in severe LS.
1. Ko AI, Goarant C, Picardeau M. Leptospira: the dawn of the molecular genetics era for an emerging zoonotic pathogen. Nat Rev Microbiol. 2009;7(10):736-747. doi:10.1038/nrmicro2208
2. Hartskeerl RA, Collares-Pereira M, Ellis WA. Emergence, control and re-emerging leptospirosis: dynamics of infection in the changing world. Clin Microbiol Infect. 2011;17(4):494-501. doi:10.1111/j.1469-0691.2011.03474.x
3. Centers for Disease Control and Prevention. Leptospirosis fact sheet for clinicians, CS287535B. https://www.cdc.gov/leptospirosis/pdf/fs-leptospirosis-clinicians-eng-508.pdf. Published January 30, 2018. Accessed October 9, 2020.
4. Martinez-Recio C, Rodriguez-Cintron W, Galarza-Vargas S, et al. The brief case: cases from 3 hospitals in Puerto Rico. ACP Hosp. https://acphospitalist.org/archives/2014/09/briefcase.htm. Published September 2014. Accessed October 9, 2020.
5. Costa F, Hagan JE, Calcagno J, et al. Global morbidity and mortality of leptospirosis: a systematic review. PLoS Negl Trop Dis. 2015;9(9):e0003898. doi:10.1371/journal.pntd.0003898
6. Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14(2):296-326. doi:10.1128/CMR.14.2.296-326.2001
7. Vijayachari P, Sugunan AP, Shriram AN. Leptospirosis: an emerging global public health problem. J Biosci. 2008;33(4):557-569. doi:10.1007/s12038-008-0074-z
8. Haake DA, Levett PN. Leptospirosis in humans. In: Adler B, ed. Leptospira and Leptospirosis. Berlin, Heidelberg: Springer-Verlag Berlin Heidelberg; 2015:65-97. doi:10.1007/978-3-662-45059-8_5
9. Berman SJ. Sporadic anicteric leptospirosis in South Vietnam: a study in 150 patients. Ann Intern Med. 1973;79(2):167. doi:10.7326/0003-4819-79-2-167
10. Bharti AR, Nally JE, Ricaldi JN, et al. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis. 2003;3(12):757-771. doi:10.1016/S1473-3099(03)00830-2
11. Andrade L, Cleto S, Seguro AC. Door-to-dialysis time and daily hemodialysis in patients with leptospirosis: impact on mortality. Clin J Am Soc Nephrol. 2007;2(4):739–744. doi: 10.2215/CJN.00680207
12. Mathew A, George J. Acute kidney injury in the tropics. Ann Saudi Med. 2011;31(5):451-456. doi:10.4103/0256-4947.84620
13. Daher EF, Silva GB Jr, Karbage NNN, et al. Predictors of oliguric acute kidney injury in leptospirosis. Nephron Clin Pract. 2009;112(1):c25-c30. doi:10.1159/000210571
14. Panaphut T, Domrongkitchaiporn S, Vibhagool A, Thinkamrop B, Susaengrat W. Ceftriaxone compared with sodium penicillin g for treatment of severe leptospirosis. Clin Infect Dis. 2003;36(12):1507-1513. doi:10.1086/375226
15. Suputtamongkol Y, Niwattayakul K, Suttinont C, et al. An open, randomized, controlled trial of penicillin, doxycycline, and cefotaxime for patients with severe leptospirosis. Clin Infect Dis. 2004;39(10):1417-1424. doi:10.1086/425001
16. Cleto SA, Rodrigues CE, Malaque CM, Sztajnbok J, Seguro AC, Andrade L. Hemodiafiltration decreases serum levels of inflammatory mediators in severe leptospirosis: a prospective study. PLoS ONE. 2016;11(8):e0160010. doi:10.1371/journal.pone.0160010
In areas where the zoonotic disease leptospirosis is endemic, reduced morbidity and mortality is strongly linked to quick initiation of renal replacement therapy.
In areas where the zoonotic disease leptospirosis is endemic, reduced morbidity and mortality is strongly linked to quick initiation of renal replacement therapy.
Leptospirosis (LS) is considered the most common and widespread zoonotic disease in the world. Numerous outbreaks have occurred in the past 10 years. Due to its technically difficult diagnosis, LS is severely underrecognized, underdiagnosed, and therefore, underreported.1,2 The Centers for Disease Control and Prevention (CDC) estimate 100 to 150 cases of LS are identified annually in the US, with about 50% of those cases occurring in Puerto Rico (PR).3 Specifically in PR, about 15 to 100 cases of suspected LS were reported annually between 2000 and 2009, with 59 cases and 1 death reported in 2010. The data are thought to be severely underreported due to a lack of widespread diagnostic testing availability in PR and no formal veterinary and environmental surveillance programs to monitor the incidence of animal cases and actual circulating serovars.4
A recent systematic review of 80 studies from 34 countries on morbidity and mortality of LS revealed that the global incidence and mortality is about 1.03 million cases and 58,900 deaths every year. Almost half of the reported deaths were adult males aged 20 to 49 years.5 Although mild cases of LS are not associated with an elevated mortality, icteric LS with renal failure (Weil disease) carries a mortality rate of 10%.6 In patients who develop hemorrhagic pneumonitis, mortality may be as high as 50 to 70%.7 Therefore, it is pivotal that clinicians recognize the disease early, that novel modalities of treatment continue to be developed, and that their impact on patient morbidity and mortality are studied and documented.
Case Presentation
A 43-year-old man with a medical history of schizophrenia presented to the emergency department at the US Department of Veterans Affairs (VA) Caribbean Healthcare System in San Juan, PR, after experiencing 1 week of intermittent fever, myalgia, and general weakness. Emergency medical services had found him disheveled and in a rodent-infested swamp area several days before admission. Initial vital signs were within normal limits.
On physical examination, the patient was afebrile, without acute distress, but he had diffuse jaundice and mild epigastric tenderness without evidence of peritoneal irritation. His complete blood count was remarkable for leukocytosis with left shifting, adequate hemoglobin levels but with 9 × 103 U/L platelets. The complete metabolic panel demonstrated an aspartate aminotransferase level of 564 U/L, alanine transaminase level of 462 U/L, total bilirubin of 12 mg/dL, which 10.2 mg/dL were direct bilirubin, and an alkaline phosphate of 345 U/L. Lipase levels were measured at 626 U/L. Marked coagulopathy also was present. The toxicology panel, including acetaminophen and salicylate acid levels, did not reveal the presence of any of the tested substances, and chest imaging did not demonstrate any infiltrates.
An abdominal ultrasound was negative for acute cholestatic pathologies, such as cholelithiasis, cholecystitis, or choledocholithiasis. Nonetheless, a noncontrast abdominopelvic computed tomography was remarkable for peripancreatic fat stranding, which raised suspicion for a diagnosis of pancreatitis.
Once the patient was transferred to the intensive care unit, he developed several episodes of hematemesis, leading to hemodynamical instability and severe respiratory distress. Due to anticipated respiratory failure and need for airway securement, endotracheal intubation was performed. Multiple packed red blood cells were transfused, and the patient was started in vasopressor support.
Diagnosis
A presumptive diagnosis of LS was made due to a considerable history of rodent exposure. The patient was started on broad-spectrum parenteral antibiotics, vancomycin 750 mg every 24 hours, metronidazole 500 mg every 8 hours, and ceftriaxone 2 g IV daily for adequate coverage against Leptospira spp. Despite 72 hours of antibiotic treatment, the patient’s clinical state deteriorated. He required high dosages of norepinephrine (1.5 mcg/kg/min) and vasopressin (0.03 U/min) to maintain adequate organ perfusion. Despite lung protective settings with low tidal volume and a high positive end-expiratory pressure, there was difficulty maintaining adequate oxygenation. Chest imaging was remarkable for bilateral infiltrates concerning for acute respiratory distress syndrome (ARDS).
The coagulopathy and cholestasis continued to worsen, and the renal failure progressed from nonoliguric to anuric. Because of this progression, the patient was started on continuous renal replacement therapy (CRRT) by hemodialysis. Within 24 hours of initiating CRRT, the patient’s clinical status improved dramatically. Vasopressor support was weaned, the coagulopathy resolved, and the cholestasis was improving. The patient’s respiratory status improved in such a manner that he was extubated by the seventh day after being placed on mechanical ventilation. The urine and blood samples sent for identification of Leptospira spp. through polymerase chain reaction (PCR) returned positive by the ninth day of admission. While on CRRT, the patient’s renal function eventually returned to baseline, and he was discharged 12 days after admission.
Discussion
The spirochetes of the genus Leptospira include both saprophytic and pathogenic species. These pathogenic Leptospira spp. have adapted to a grand variety of zoonotic hosts, the most important being rodents. They serve as vectors for the contraction of the disease by humans. Initial infection in rodents by Leptospira spp. causes a systemic illness followed by a persistent colonization of renal tubules from which they are excreted in the urine and into the environment. Humans, in turn, are an incidental host unable to induce a carrier state for the transmission of the pathogenic organism.1 The time from exposure to onset of symptoms, or incubation phase, averages 7 to 12 days but may range from 3 to 30 days.8
LS has been described as having 2 discernable but often coexisting phases. The first, an acute febrile bacteremic phase, has been noted to last about 9 days in about 85% of patients, although a minority have persistent fever from 2 weeks to > 30 days. A second phase, the immune or inflammatory phase, is characterized by a second fever spike preceded by 1 to 5 afebrile days in which there is presence of IgM antibodies and resolution of leptospiremia but positive urine cultures.9 Weil disease may present as the second phase of the disease or as a single, progressive illness from its first manifestation. It is characterized by a triad of jaundice, renal failure, and hemorrhage or coagulopathy.10 Weil disease is of great concern and importance due to its associated higher mortality than that found with the mildest form of the disease.
There are studies that advocate for RRT as an intricate part of the treatment regimen in LS to remove the inflammatory cytokines produced as a reaction to the spirochete.11 In tropical countries with a higher incidence of the disease, leptospirosis is an important cause of acute kidney injury (AKI), depending on multiple factors, including the AKI definition that is used.12 Renal invasion by Leptospira spp. produces acute tubular necrosis (ATN) and cell edema during the first week and then could progress to acute interstitial nephritis (AIN) in 2 to 3 weeks. It is believed that the mechanism for the Leptospira spp. invasion of the tubules that results in damage is associated with the antigenic components in its outer membrane; the most important outer membrane protein expressed during infection is LipL32. This protein increases the production of proinflammatory proteins, such as inducible nitric oxide synthase, monocyte chemotactic protein-1 (CCL2/MCP-1), T cells, and tumor necrosis factor.13
Although doxycycline has been recommended for the prophylaxis and treatment of mild LS, the preferred agent and the conferred benefits of antibiotic treatment overall for the severe form of the disease has been controversial. Traditionally, penicillin G sodium has been recommended as the first-line antibiotic treatment for moderate-to-severe LS.14 Nonetheless, there has been an increasing pattern of penicillin resistance among Leptospira spp. that has prompted the study and use of alternative agents.
An open-label, randomized comparison of parenteral cefotaxime, penicillin G sodium, and doxycycline for the treatment of suspected severe leptospirosis conducted by Suputtamongkol and colleagues showed no difference in mortality, defervescence, or time to resolution of abnormal laboratory findings.15 Current CDC recommendations include the use of parenteral penicillin 1.5 MU every 6 hours as the drug of choice, with ceftriaxone 1 g administered IV every 24 hours equally as effective.3
In addition to antimicrobial therapy, supportive care has shifted to include hemodialysis in those patients who develop AKI as part of the disease. Andrade and colleagues conducted a study of 33 patients with LS in Brazil that was set to compare the impact of door-to-dialysis time and dosage of hemodialysis on mortality. In patients with a quicker door-to-dialysis time and daily hemodialysis sessions, there was a 50% (16.7% vs 66.7%) absolute mortality reduction when compared with those with delayed initiation and alternate-day hemodialysis sessions.11 A follow-up prospective study compared the use of traditional sustained low-efficiency dialysis (SLED) with the use of extended SLED via hemodiafiltration in patients with LS presenting with ARDS and AKI. Although hemodiafiltration resulted in a relative decrease in serum levels of interleukin (IL)-17, IL-7, and CCL2/MCP-1, there was no significant difference in mortality.16 The most important prognostic factor in severe LS presenting with AKI and relating to RRT is a shorter door-to-dialysis time and increased dose, not the mode of dialysis clearance. Nonetheless, both RRT methods resulted in a progressive decrease in inflammatory mediators that have been associated with ATN and AIN in the context of LS.16 The authors argue that using CRRT instead of SLED via hemodiafiltration could have accentuated the effects of the reduction that inflammatory mediators may have on mortality in patients with severe LS.
Conclusions
LS continues to be of interest due to its current status as the most common zoonotic disease and its widespread prevalence throughout the globe. Novel treatment modalities for LS, specifically for Weil disease, continue to be developed with the goal of reducing the current mortality rate associated with the disease.
In endemic areas, prompt recognition is essential to initiate the recommended therapy. Parenteral antibiotics, such as penicillin G sodium and ceftriaxone, continue to be the mainstay of treatment and constitute the current CDC recommendations. Nonetheless, early initiation of CRRT has been shown to greatly reduce the mortality associated with Weil disease and, when available, should be considered in these patients.
Our patient failed to improve while receiving parenteral antibiotics alone but showed marked improvement after being placed on CRRT. Furthermore, initiation of CRRT resulted in near-complete resolution of his organ dysfunction and eventual discharge from the hospital. This case serves to further support the use of early CRRT as part of the standard of care in severe LS.
Leptospirosis (LS) is considered the most common and widespread zoonotic disease in the world. Numerous outbreaks have occurred in the past 10 years. Due to its technically difficult diagnosis, LS is severely underrecognized, underdiagnosed, and therefore, underreported.1,2 The Centers for Disease Control and Prevention (CDC) estimate 100 to 150 cases of LS are identified annually in the US, with about 50% of those cases occurring in Puerto Rico (PR).3 Specifically in PR, about 15 to 100 cases of suspected LS were reported annually between 2000 and 2009, with 59 cases and 1 death reported in 2010. The data are thought to be severely underreported due to a lack of widespread diagnostic testing availability in PR and no formal veterinary and environmental surveillance programs to monitor the incidence of animal cases and actual circulating serovars.4
A recent systematic review of 80 studies from 34 countries on morbidity and mortality of LS revealed that the global incidence and mortality is about 1.03 million cases and 58,900 deaths every year. Almost half of the reported deaths were adult males aged 20 to 49 years.5 Although mild cases of LS are not associated with an elevated mortality, icteric LS with renal failure (Weil disease) carries a mortality rate of 10%.6 In patients who develop hemorrhagic pneumonitis, mortality may be as high as 50 to 70%.7 Therefore, it is pivotal that clinicians recognize the disease early, that novel modalities of treatment continue to be developed, and that their impact on patient morbidity and mortality are studied and documented.
Case Presentation
A 43-year-old man with a medical history of schizophrenia presented to the emergency department at the US Department of Veterans Affairs (VA) Caribbean Healthcare System in San Juan, PR, after experiencing 1 week of intermittent fever, myalgia, and general weakness. Emergency medical services had found him disheveled and in a rodent-infested swamp area several days before admission. Initial vital signs were within normal limits.
On physical examination, the patient was afebrile, without acute distress, but he had diffuse jaundice and mild epigastric tenderness without evidence of peritoneal irritation. His complete blood count was remarkable for leukocytosis with left shifting, adequate hemoglobin levels but with 9 × 103 U/L platelets. The complete metabolic panel demonstrated an aspartate aminotransferase level of 564 U/L, alanine transaminase level of 462 U/L, total bilirubin of 12 mg/dL, which 10.2 mg/dL were direct bilirubin, and an alkaline phosphate of 345 U/L. Lipase levels were measured at 626 U/L. Marked coagulopathy also was present. The toxicology panel, including acetaminophen and salicylate acid levels, did not reveal the presence of any of the tested substances, and chest imaging did not demonstrate any infiltrates.
An abdominal ultrasound was negative for acute cholestatic pathologies, such as cholelithiasis, cholecystitis, or choledocholithiasis. Nonetheless, a noncontrast abdominopelvic computed tomography was remarkable for peripancreatic fat stranding, which raised suspicion for a diagnosis of pancreatitis.
Once the patient was transferred to the intensive care unit, he developed several episodes of hematemesis, leading to hemodynamical instability and severe respiratory distress. Due to anticipated respiratory failure and need for airway securement, endotracheal intubation was performed. Multiple packed red blood cells were transfused, and the patient was started in vasopressor support.
Diagnosis
A presumptive diagnosis of LS was made due to a considerable history of rodent exposure. The patient was started on broad-spectrum parenteral antibiotics, vancomycin 750 mg every 24 hours, metronidazole 500 mg every 8 hours, and ceftriaxone 2 g IV daily for adequate coverage against Leptospira spp. Despite 72 hours of antibiotic treatment, the patient’s clinical state deteriorated. He required high dosages of norepinephrine (1.5 mcg/kg/min) and vasopressin (0.03 U/min) to maintain adequate organ perfusion. Despite lung protective settings with low tidal volume and a high positive end-expiratory pressure, there was difficulty maintaining adequate oxygenation. Chest imaging was remarkable for bilateral infiltrates concerning for acute respiratory distress syndrome (ARDS).
The coagulopathy and cholestasis continued to worsen, and the renal failure progressed from nonoliguric to anuric. Because of this progression, the patient was started on continuous renal replacement therapy (CRRT) by hemodialysis. Within 24 hours of initiating CRRT, the patient’s clinical status improved dramatically. Vasopressor support was weaned, the coagulopathy resolved, and the cholestasis was improving. The patient’s respiratory status improved in such a manner that he was extubated by the seventh day after being placed on mechanical ventilation. The urine and blood samples sent for identification of Leptospira spp. through polymerase chain reaction (PCR) returned positive by the ninth day of admission. While on CRRT, the patient’s renal function eventually returned to baseline, and he was discharged 12 days after admission.
Discussion
The spirochetes of the genus Leptospira include both saprophytic and pathogenic species. These pathogenic Leptospira spp. have adapted to a grand variety of zoonotic hosts, the most important being rodents. They serve as vectors for the contraction of the disease by humans. Initial infection in rodents by Leptospira spp. causes a systemic illness followed by a persistent colonization of renal tubules from which they are excreted in the urine and into the environment. Humans, in turn, are an incidental host unable to induce a carrier state for the transmission of the pathogenic organism.1 The time from exposure to onset of symptoms, or incubation phase, averages 7 to 12 days but may range from 3 to 30 days.8
LS has been described as having 2 discernable but often coexisting phases. The first, an acute febrile bacteremic phase, has been noted to last about 9 days in about 85% of patients, although a minority have persistent fever from 2 weeks to > 30 days. A second phase, the immune or inflammatory phase, is characterized by a second fever spike preceded by 1 to 5 afebrile days in which there is presence of IgM antibodies and resolution of leptospiremia but positive urine cultures.9 Weil disease may present as the second phase of the disease or as a single, progressive illness from its first manifestation. It is characterized by a triad of jaundice, renal failure, and hemorrhage or coagulopathy.10 Weil disease is of great concern and importance due to its associated higher mortality than that found with the mildest form of the disease.
There are studies that advocate for RRT as an intricate part of the treatment regimen in LS to remove the inflammatory cytokines produced as a reaction to the spirochete.11 In tropical countries with a higher incidence of the disease, leptospirosis is an important cause of acute kidney injury (AKI), depending on multiple factors, including the AKI definition that is used.12 Renal invasion by Leptospira spp. produces acute tubular necrosis (ATN) and cell edema during the first week and then could progress to acute interstitial nephritis (AIN) in 2 to 3 weeks. It is believed that the mechanism for the Leptospira spp. invasion of the tubules that results in damage is associated with the antigenic components in its outer membrane; the most important outer membrane protein expressed during infection is LipL32. This protein increases the production of proinflammatory proteins, such as inducible nitric oxide synthase, monocyte chemotactic protein-1 (CCL2/MCP-1), T cells, and tumor necrosis factor.13
Although doxycycline has been recommended for the prophylaxis and treatment of mild LS, the preferred agent and the conferred benefits of antibiotic treatment overall for the severe form of the disease has been controversial. Traditionally, penicillin G sodium has been recommended as the first-line antibiotic treatment for moderate-to-severe LS.14 Nonetheless, there has been an increasing pattern of penicillin resistance among Leptospira spp. that has prompted the study and use of alternative agents.
An open-label, randomized comparison of parenteral cefotaxime, penicillin G sodium, and doxycycline for the treatment of suspected severe leptospirosis conducted by Suputtamongkol and colleagues showed no difference in mortality, defervescence, or time to resolution of abnormal laboratory findings.15 Current CDC recommendations include the use of parenteral penicillin 1.5 MU every 6 hours as the drug of choice, with ceftriaxone 1 g administered IV every 24 hours equally as effective.3
In addition to antimicrobial therapy, supportive care has shifted to include hemodialysis in those patients who develop AKI as part of the disease. Andrade and colleagues conducted a study of 33 patients with LS in Brazil that was set to compare the impact of door-to-dialysis time and dosage of hemodialysis on mortality. In patients with a quicker door-to-dialysis time and daily hemodialysis sessions, there was a 50% (16.7% vs 66.7%) absolute mortality reduction when compared with those with delayed initiation and alternate-day hemodialysis sessions.11 A follow-up prospective study compared the use of traditional sustained low-efficiency dialysis (SLED) with the use of extended SLED via hemodiafiltration in patients with LS presenting with ARDS and AKI. Although hemodiafiltration resulted in a relative decrease in serum levels of interleukin (IL)-17, IL-7, and CCL2/MCP-1, there was no significant difference in mortality.16 The most important prognostic factor in severe LS presenting with AKI and relating to RRT is a shorter door-to-dialysis time and increased dose, not the mode of dialysis clearance. Nonetheless, both RRT methods resulted in a progressive decrease in inflammatory mediators that have been associated with ATN and AIN in the context of LS.16 The authors argue that using CRRT instead of SLED via hemodiafiltration could have accentuated the effects of the reduction that inflammatory mediators may have on mortality in patients with severe LS.
Conclusions
LS continues to be of interest due to its current status as the most common zoonotic disease and its widespread prevalence throughout the globe. Novel treatment modalities for LS, specifically for Weil disease, continue to be developed with the goal of reducing the current mortality rate associated with the disease.
In endemic areas, prompt recognition is essential to initiate the recommended therapy. Parenteral antibiotics, such as penicillin G sodium and ceftriaxone, continue to be the mainstay of treatment and constitute the current CDC recommendations. Nonetheless, early initiation of CRRT has been shown to greatly reduce the mortality associated with Weil disease and, when available, should be considered in these patients.
Our patient failed to improve while receiving parenteral antibiotics alone but showed marked improvement after being placed on CRRT. Furthermore, initiation of CRRT resulted in near-complete resolution of his organ dysfunction and eventual discharge from the hospital. This case serves to further support the use of early CRRT as part of the standard of care in severe LS.
1. Ko AI, Goarant C, Picardeau M. Leptospira: the dawn of the molecular genetics era for an emerging zoonotic pathogen. Nat Rev Microbiol. 2009;7(10):736-747. doi:10.1038/nrmicro2208
2. Hartskeerl RA, Collares-Pereira M, Ellis WA. Emergence, control and re-emerging leptospirosis: dynamics of infection in the changing world. Clin Microbiol Infect. 2011;17(4):494-501. doi:10.1111/j.1469-0691.2011.03474.x
3. Centers for Disease Control and Prevention. Leptospirosis fact sheet for clinicians, CS287535B. https://www.cdc.gov/leptospirosis/pdf/fs-leptospirosis-clinicians-eng-508.pdf. Published January 30, 2018. Accessed October 9, 2020.
4. Martinez-Recio C, Rodriguez-Cintron W, Galarza-Vargas S, et al. The brief case: cases from 3 hospitals in Puerto Rico. ACP Hosp. https://acphospitalist.org/archives/2014/09/briefcase.htm. Published September 2014. Accessed October 9, 2020.
5. Costa F, Hagan JE, Calcagno J, et al. Global morbidity and mortality of leptospirosis: a systematic review. PLoS Negl Trop Dis. 2015;9(9):e0003898. doi:10.1371/journal.pntd.0003898
6. Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14(2):296-326. doi:10.1128/CMR.14.2.296-326.2001
7. Vijayachari P, Sugunan AP, Shriram AN. Leptospirosis: an emerging global public health problem. J Biosci. 2008;33(4):557-569. doi:10.1007/s12038-008-0074-z
8. Haake DA, Levett PN. Leptospirosis in humans. In: Adler B, ed. Leptospira and Leptospirosis. Berlin, Heidelberg: Springer-Verlag Berlin Heidelberg; 2015:65-97. doi:10.1007/978-3-662-45059-8_5
9. Berman SJ. Sporadic anicteric leptospirosis in South Vietnam: a study in 150 patients. Ann Intern Med. 1973;79(2):167. doi:10.7326/0003-4819-79-2-167
10. Bharti AR, Nally JE, Ricaldi JN, et al. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis. 2003;3(12):757-771. doi:10.1016/S1473-3099(03)00830-2
11. Andrade L, Cleto S, Seguro AC. Door-to-dialysis time and daily hemodialysis in patients with leptospirosis: impact on mortality. Clin J Am Soc Nephrol. 2007;2(4):739–744. doi: 10.2215/CJN.00680207
12. Mathew A, George J. Acute kidney injury in the tropics. Ann Saudi Med. 2011;31(5):451-456. doi:10.4103/0256-4947.84620
13. Daher EF, Silva GB Jr, Karbage NNN, et al. Predictors of oliguric acute kidney injury in leptospirosis. Nephron Clin Pract. 2009;112(1):c25-c30. doi:10.1159/000210571
14. Panaphut T, Domrongkitchaiporn S, Vibhagool A, Thinkamrop B, Susaengrat W. Ceftriaxone compared with sodium penicillin g for treatment of severe leptospirosis. Clin Infect Dis. 2003;36(12):1507-1513. doi:10.1086/375226
15. Suputtamongkol Y, Niwattayakul K, Suttinont C, et al. An open, randomized, controlled trial of penicillin, doxycycline, and cefotaxime for patients with severe leptospirosis. Clin Infect Dis. 2004;39(10):1417-1424. doi:10.1086/425001
16. Cleto SA, Rodrigues CE, Malaque CM, Sztajnbok J, Seguro AC, Andrade L. Hemodiafiltration decreases serum levels of inflammatory mediators in severe leptospirosis: a prospective study. PLoS ONE. 2016;11(8):e0160010. doi:10.1371/journal.pone.0160010
1. Ko AI, Goarant C, Picardeau M. Leptospira: the dawn of the molecular genetics era for an emerging zoonotic pathogen. Nat Rev Microbiol. 2009;7(10):736-747. doi:10.1038/nrmicro2208
2. Hartskeerl RA, Collares-Pereira M, Ellis WA. Emergence, control and re-emerging leptospirosis: dynamics of infection in the changing world. Clin Microbiol Infect. 2011;17(4):494-501. doi:10.1111/j.1469-0691.2011.03474.x
3. Centers for Disease Control and Prevention. Leptospirosis fact sheet for clinicians, CS287535B. https://www.cdc.gov/leptospirosis/pdf/fs-leptospirosis-clinicians-eng-508.pdf. Published January 30, 2018. Accessed October 9, 2020.
4. Martinez-Recio C, Rodriguez-Cintron W, Galarza-Vargas S, et al. The brief case: cases from 3 hospitals in Puerto Rico. ACP Hosp. https://acphospitalist.org/archives/2014/09/briefcase.htm. Published September 2014. Accessed October 9, 2020.
5. Costa F, Hagan JE, Calcagno J, et al. Global morbidity and mortality of leptospirosis: a systematic review. PLoS Negl Trop Dis. 2015;9(9):e0003898. doi:10.1371/journal.pntd.0003898
6. Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14(2):296-326. doi:10.1128/CMR.14.2.296-326.2001
7. Vijayachari P, Sugunan AP, Shriram AN. Leptospirosis: an emerging global public health problem. J Biosci. 2008;33(4):557-569. doi:10.1007/s12038-008-0074-z
8. Haake DA, Levett PN. Leptospirosis in humans. In: Adler B, ed. Leptospira and Leptospirosis. Berlin, Heidelberg: Springer-Verlag Berlin Heidelberg; 2015:65-97. doi:10.1007/978-3-662-45059-8_5
9. Berman SJ. Sporadic anicteric leptospirosis in South Vietnam: a study in 150 patients. Ann Intern Med. 1973;79(2):167. doi:10.7326/0003-4819-79-2-167
10. Bharti AR, Nally JE, Ricaldi JN, et al. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis. 2003;3(12):757-771. doi:10.1016/S1473-3099(03)00830-2
11. Andrade L, Cleto S, Seguro AC. Door-to-dialysis time and daily hemodialysis in patients with leptospirosis: impact on mortality. Clin J Am Soc Nephrol. 2007;2(4):739–744. doi: 10.2215/CJN.00680207
12. Mathew A, George J. Acute kidney injury in the tropics. Ann Saudi Med. 2011;31(5):451-456. doi:10.4103/0256-4947.84620
13. Daher EF, Silva GB Jr, Karbage NNN, et al. Predictors of oliguric acute kidney injury in leptospirosis. Nephron Clin Pract. 2009;112(1):c25-c30. doi:10.1159/000210571
14. Panaphut T, Domrongkitchaiporn S, Vibhagool A, Thinkamrop B, Susaengrat W. Ceftriaxone compared with sodium penicillin g for treatment of severe leptospirosis. Clin Infect Dis. 2003;36(12):1507-1513. doi:10.1086/375226
15. Suputtamongkol Y, Niwattayakul K, Suttinont C, et al. An open, randomized, controlled trial of penicillin, doxycycline, and cefotaxime for patients with severe leptospirosis. Clin Infect Dis. 2004;39(10):1417-1424. doi:10.1086/425001
16. Cleto SA, Rodrigues CE, Malaque CM, Sztajnbok J, Seguro AC, Andrade L. Hemodiafiltration decreases serum levels of inflammatory mediators in severe leptospirosis: a prospective study. PLoS ONE. 2016;11(8):e0160010. doi:10.1371/journal.pone.0160010