User login
Culture change can improve NP, PA practice
Creating an atmosphere conducive to productive teamwork can help maximize nurse practitioners’ and physician assistants’ potential, say experts presenting at the Tuesday session “How Best NP/PA and MD Hospitalists Can Work Together.”
Session leaders Brian Wolfe, MD, FHM, a general internist at the University of Michigan, Ann Arbor, and Tracy Cardin, ACNP-BC,SFHM, the associate director of clinical integration at Adfinitas Health, Hanover, Md., will break down strategies to help incorporate different perspectives into your practice to improve its culture.
“I think culture beats strategy any day of the week, and the cultural threads we can draw from our different experiences are a lot more powerful, and a lot more translatable, across different institutions,” Dr. Wolfe said in an interview. “The purpose of this session is to get away from saying ‘Well, this is the way we do it,’ and instead say, ‘This is what kind of cultural vision we have for our NPs and PAs, and this is where we succeed, and these are the ways we fail.’ ”
Attendees will learn about what PAs and NPs are looking for in their work, what some providers are doing to change their hospital culture, and the business data behind those decisions.
“NPs and PAs are looking for autonomy, mastery, and purpose,” said Dr. Wolfe. “While some of that comes from where you work and how long your hours are, a lot of it has to do with how the culture treats you as a nurse practitioner or physician assistant and where your place is.”
Following Dr. Wolfe’s initial presentation, the facilitators will analyze cases with evident structural problems in order to uncover the underlying cultural issues.
By hearing about concrete, everyday examples, attendees will be able to recognize some of the problems within their own networks that they might deal with on a regular basis and come away with long-term solutions.
“Nobody really acknowledges these issues on a day-to-day basis, but they can be extremely influential,” Ms. Cardin said in an interview. “Once you’re aware of the cultural impacts on the functionality of your group, then you can begin chipping away at them and altering culture to provide for a more successful path.”
Attendees will leave the session with solutions that can boost productivity and spending, according to Dr. Wolfe.
“As a physician leader, you want to recruit and retain high-level people who can operate at the top of their licenses and can push your practice beyond its structures,” said Dr. Wolfe. “The other piece is that there is no defined cost for retraining, and if you don’t address the issues that will drive your PAs and NPs to leave, you’ll be stuck with a constant turnover, which leads to lower performance and less efficiency.”
How Best NP/PA and MD Hospitalists Can Work Together:
Incorporating NPs/PAs into the workforce and Workplace Culture
Tuesday, 4:30-6 p.m.
Grand Ballroom 1-3
Creating an atmosphere conducive to productive teamwork can help maximize nurse practitioners’ and physician assistants’ potential, say experts presenting at the Tuesday session “How Best NP/PA and MD Hospitalists Can Work Together.”
Session leaders Brian Wolfe, MD, FHM, a general internist at the University of Michigan, Ann Arbor, and Tracy Cardin, ACNP-BC,SFHM, the associate director of clinical integration at Adfinitas Health, Hanover, Md., will break down strategies to help incorporate different perspectives into your practice to improve its culture.
“I think culture beats strategy any day of the week, and the cultural threads we can draw from our different experiences are a lot more powerful, and a lot more translatable, across different institutions,” Dr. Wolfe said in an interview. “The purpose of this session is to get away from saying ‘Well, this is the way we do it,’ and instead say, ‘This is what kind of cultural vision we have for our NPs and PAs, and this is where we succeed, and these are the ways we fail.’ ”
Attendees will learn about what PAs and NPs are looking for in their work, what some providers are doing to change their hospital culture, and the business data behind those decisions.
“NPs and PAs are looking for autonomy, mastery, and purpose,” said Dr. Wolfe. “While some of that comes from where you work and how long your hours are, a lot of it has to do with how the culture treats you as a nurse practitioner or physician assistant and where your place is.”
Following Dr. Wolfe’s initial presentation, the facilitators will analyze cases with evident structural problems in order to uncover the underlying cultural issues.
By hearing about concrete, everyday examples, attendees will be able to recognize some of the problems within their own networks that they might deal with on a regular basis and come away with long-term solutions.
“Nobody really acknowledges these issues on a day-to-day basis, but they can be extremely influential,” Ms. Cardin said in an interview. “Once you’re aware of the cultural impacts on the functionality of your group, then you can begin chipping away at them and altering culture to provide for a more successful path.”
Attendees will leave the session with solutions that can boost productivity and spending, according to Dr. Wolfe.
“As a physician leader, you want to recruit and retain high-level people who can operate at the top of their licenses and can push your practice beyond its structures,” said Dr. Wolfe. “The other piece is that there is no defined cost for retraining, and if you don’t address the issues that will drive your PAs and NPs to leave, you’ll be stuck with a constant turnover, which leads to lower performance and less efficiency.”
How Best NP/PA and MD Hospitalists Can Work Together:
Incorporating NPs/PAs into the workforce and Workplace Culture
Tuesday, 4:30-6 p.m.
Grand Ballroom 1-3
Creating an atmosphere conducive to productive teamwork can help maximize nurse practitioners’ and physician assistants’ potential, say experts presenting at the Tuesday session “How Best NP/PA and MD Hospitalists Can Work Together.”
Session leaders Brian Wolfe, MD, FHM, a general internist at the University of Michigan, Ann Arbor, and Tracy Cardin, ACNP-BC,SFHM, the associate director of clinical integration at Adfinitas Health, Hanover, Md., will break down strategies to help incorporate different perspectives into your practice to improve its culture.
“I think culture beats strategy any day of the week, and the cultural threads we can draw from our different experiences are a lot more powerful, and a lot more translatable, across different institutions,” Dr. Wolfe said in an interview. “The purpose of this session is to get away from saying ‘Well, this is the way we do it,’ and instead say, ‘This is what kind of cultural vision we have for our NPs and PAs, and this is where we succeed, and these are the ways we fail.’ ”
Attendees will learn about what PAs and NPs are looking for in their work, what some providers are doing to change their hospital culture, and the business data behind those decisions.
“NPs and PAs are looking for autonomy, mastery, and purpose,” said Dr. Wolfe. “While some of that comes from where you work and how long your hours are, a lot of it has to do with how the culture treats you as a nurse practitioner or physician assistant and where your place is.”
Following Dr. Wolfe’s initial presentation, the facilitators will analyze cases with evident structural problems in order to uncover the underlying cultural issues.
By hearing about concrete, everyday examples, attendees will be able to recognize some of the problems within their own networks that they might deal with on a regular basis and come away with long-term solutions.
“Nobody really acknowledges these issues on a day-to-day basis, but they can be extremely influential,” Ms. Cardin said in an interview. “Once you’re aware of the cultural impacts on the functionality of your group, then you can begin chipping away at them and altering culture to provide for a more successful path.”
Attendees will leave the session with solutions that can boost productivity and spending, according to Dr. Wolfe.
“As a physician leader, you want to recruit and retain high-level people who can operate at the top of their licenses and can push your practice beyond its structures,” said Dr. Wolfe. “The other piece is that there is no defined cost for retraining, and if you don’t address the issues that will drive your PAs and NPs to leave, you’ll be stuck with a constant turnover, which leads to lower performance and less efficiency.”
How Best NP/PA and MD Hospitalists Can Work Together:
Incorporating NPs/PAs into the workforce and Workplace Culture
Tuesday, 4:30-6 p.m.
Grand Ballroom 1-3
Levothyroxine may increase mortality in older patients
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
With increased mortality and similar prevalence of atrial fibrillation and femoral fractures between study and control groups, physicians may want to reevaluate giving their elderly patients levothyroxine until more information is available, according to presenter Joseph Meyerovitch, MD, of Schneider Children’s Medical Center, Ramat Hasharon, Israel.
The case-control study included 416 patients 65 years or older with TSH levels of 4.2-10 mIU/L who died between 2012 and 2016, and 1,461 patients with comparable TSH levels who did not die during that time.
Most of the patients in both the control and study group were women. The average age of the patients was 84 years, and most had some form of dementia or senility (86.4%).
Mortality was 19% more likely in the group taking levothyroxine, according to an analysis by Dr. Meyerovitch and his fellow investigators.
When broken down further, presence of certain comorbidities increased mortality dramatically, including dementia (odds ratio, 1.61), heart failure (OR, 2.67), chronic renal failure (OR, 1.89), and cerebrovascular disease (OR, 1.94).
There was no significant difference in prevalence of atrial fibrillation between the test and control groups with thyroid stimulating hormone (TSH) testing, nor any difference in femur fracture prevalence.
Patients were given a TSH test three times during follow-up and showed significantly lower TSH levels compared with controls, according to Dr. Meyerovitch.
Dr. Meyerovitch acknowledged that the data he and his team used did not include the reason for a TSH evaluation, nor why patients began levothyroxine treatment. This leaves unanswered questions about the initial baseline mortality risk in patients included in the study.
“This may have resulted in treatment of patients with a higher risk, since we don’t know the reason for the treatment,” he said. “There may have been other reasons that were not included in the database that caused the physician to treat with levothyroxine.”
Details on the cause of death were not included.
Despite these limitations, Dr. Meyerovitch and his team stressed the need for more research before continuing to recommend this treatment to their elderly patients.
Dr. Meyerovitch reported no relevant financial disclosures.
Source: Meyerovitch J et al. ENDO 2018 Abstract OR34-2.
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
With increased mortality and similar prevalence of atrial fibrillation and femoral fractures between study and control groups, physicians may want to reevaluate giving their elderly patients levothyroxine until more information is available, according to presenter Joseph Meyerovitch, MD, of Schneider Children’s Medical Center, Ramat Hasharon, Israel.
The case-control study included 416 patients 65 years or older with TSH levels of 4.2-10 mIU/L who died between 2012 and 2016, and 1,461 patients with comparable TSH levels who did not die during that time.
Most of the patients in both the control and study group were women. The average age of the patients was 84 years, and most had some form of dementia or senility (86.4%).
Mortality was 19% more likely in the group taking levothyroxine, according to an analysis by Dr. Meyerovitch and his fellow investigators.
When broken down further, presence of certain comorbidities increased mortality dramatically, including dementia (odds ratio, 1.61), heart failure (OR, 2.67), chronic renal failure (OR, 1.89), and cerebrovascular disease (OR, 1.94).
There was no significant difference in prevalence of atrial fibrillation between the test and control groups with thyroid stimulating hormone (TSH) testing, nor any difference in femur fracture prevalence.
Patients were given a TSH test three times during follow-up and showed significantly lower TSH levels compared with controls, according to Dr. Meyerovitch.
Dr. Meyerovitch acknowledged that the data he and his team used did not include the reason for a TSH evaluation, nor why patients began levothyroxine treatment. This leaves unanswered questions about the initial baseline mortality risk in patients included in the study.
“This may have resulted in treatment of patients with a higher risk, since we don’t know the reason for the treatment,” he said. “There may have been other reasons that were not included in the database that caused the physician to treat with levothyroxine.”
Details on the cause of death were not included.
Despite these limitations, Dr. Meyerovitch and his team stressed the need for more research before continuing to recommend this treatment to their elderly patients.
Dr. Meyerovitch reported no relevant financial disclosures.
Source: Meyerovitch J et al. ENDO 2018 Abstract OR34-2.
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
With increased mortality and similar prevalence of atrial fibrillation and femoral fractures between study and control groups, physicians may want to reevaluate giving their elderly patients levothyroxine until more information is available, according to presenter Joseph Meyerovitch, MD, of Schneider Children’s Medical Center, Ramat Hasharon, Israel.
The case-control study included 416 patients 65 years or older with TSH levels of 4.2-10 mIU/L who died between 2012 and 2016, and 1,461 patients with comparable TSH levels who did not die during that time.
Most of the patients in both the control and study group were women. The average age of the patients was 84 years, and most had some form of dementia or senility (86.4%).
Mortality was 19% more likely in the group taking levothyroxine, according to an analysis by Dr. Meyerovitch and his fellow investigators.
When broken down further, presence of certain comorbidities increased mortality dramatically, including dementia (odds ratio, 1.61), heart failure (OR, 2.67), chronic renal failure (OR, 1.89), and cerebrovascular disease (OR, 1.94).
There was no significant difference in prevalence of atrial fibrillation between the test and control groups with thyroid stimulating hormone (TSH) testing, nor any difference in femur fracture prevalence.
Patients were given a TSH test three times during follow-up and showed significantly lower TSH levels compared with controls, according to Dr. Meyerovitch.
Dr. Meyerovitch acknowledged that the data he and his team used did not include the reason for a TSH evaluation, nor why patients began levothyroxine treatment. This leaves unanswered questions about the initial baseline mortality risk in patients included in the study.
“This may have resulted in treatment of patients with a higher risk, since we don’t know the reason for the treatment,” he said. “There may have been other reasons that were not included in the database that caused the physician to treat with levothyroxine.”
Details on the cause of death were not included.
Despite these limitations, Dr. Meyerovitch and his team stressed the need for more research before continuing to recommend this treatment to their elderly patients.
Dr. Meyerovitch reported no relevant financial disclosures.
Source: Meyerovitch J et al. ENDO 2018 Abstract OR34-2.
REPORTING FROM ENDO 2018
Key clinical point: Levothyroxine is associated with increased mortality in hypothyroidism patients 65 years and older.
Major finding: Patients who were treated with levothyroxine had an increased rate of mortality of 19% (HR = 1.19) compared to those treated with other methods.
Data source: Case-control study of 416 hypothyroidism patients 65 years or older who died between 2012 and 2016, compared with 1,461 hypothyroidism patients treated in the same period who did not die.
Disclosures: Dr. Meyerovitch reported no relevant financial disclosures.
Source: Meyerovitch J et al. ENDO 2018 Abstract OR34-2.
2018 FNIH Lurie Prize awarded for DNA immune response discovery
The Foundation of the National Institutes of Health has awarded according to a statement released Tuesday, April 3.
“We are proud to honor Dr. Chen with the 2018 Lurie Prize in Biomedical Sciences for the discovery of the cGAS enzyme and pathway and their unique role in immune and inflammatory response,” Maria C. Freire, PhD, president and executive director of the FNIH, said in a press release. “Dr. Chen joins five other Lurie Prize winners, who are shaping the future of human health through their profound biomedical research.”
While scientists have known for some time that DNA had a role in activating the immune response, the specifics of the process eluded explanation.
Through their work, Dr. Chen and his team uncovered that cGAS was the enzyme used to spark the reaction.
“[cGAS] is a protein sensor that detects DNA as a danger signal that then triggers the immune response,” said Dr. Chen. “When DNA gets into the cytoplasm, cGAS becomes activated and catalyzes the synthesis of a small molecule, called cGAMP, which then functions as a messenger that activates the immune response pathway.”
While the cGAS enzyme can help defend against infectious disease or cancer, the enzyme can also trigger autoimmune diseases such as rheumatoid arthritis.
Dr. Chen is the George L. MacGregor Distinguished Chair in Biomedical Science and professor of molecular biology at the University of Texas Southwestern Medical Center, Dallas, and an investigator for the Howard Hughes Medical Institute, Chevy Chase, Md. He completed his undergraduate study in biology at Fujian (China) Normal University, after which he went on to earn his PhD from State University of New York at Buffalo.
The prize includes a $100,000 honorarium, donated to the FNIH by philanthropist Ann Lurie, who serves as president of the Ann and Robert H. Lurie Foundation and president of Lurie Holdings, according to the press release.
“This is a tremendous honor and is a strong endorsement of the work discovered by the scientists in my lab; it is very exciting,” said Dr. Chen. “We hope to continue our work to deepen our understanding of this pathway, as the mechanisms of the pathway are not yet completely understood, as well as look more into how we can harness the immunity pathway to develop treatments for cases like autoimmune diseases or cancer.”
The Foundation of the National Institutes of Health has awarded according to a statement released Tuesday, April 3.
“We are proud to honor Dr. Chen with the 2018 Lurie Prize in Biomedical Sciences for the discovery of the cGAS enzyme and pathway and their unique role in immune and inflammatory response,” Maria C. Freire, PhD, president and executive director of the FNIH, said in a press release. “Dr. Chen joins five other Lurie Prize winners, who are shaping the future of human health through their profound biomedical research.”
While scientists have known for some time that DNA had a role in activating the immune response, the specifics of the process eluded explanation.
Through their work, Dr. Chen and his team uncovered that cGAS was the enzyme used to spark the reaction.
“[cGAS] is a protein sensor that detects DNA as a danger signal that then triggers the immune response,” said Dr. Chen. “When DNA gets into the cytoplasm, cGAS becomes activated and catalyzes the synthesis of a small molecule, called cGAMP, which then functions as a messenger that activates the immune response pathway.”
While the cGAS enzyme can help defend against infectious disease or cancer, the enzyme can also trigger autoimmune diseases such as rheumatoid arthritis.
Dr. Chen is the George L. MacGregor Distinguished Chair in Biomedical Science and professor of molecular biology at the University of Texas Southwestern Medical Center, Dallas, and an investigator for the Howard Hughes Medical Institute, Chevy Chase, Md. He completed his undergraduate study in biology at Fujian (China) Normal University, after which he went on to earn his PhD from State University of New York at Buffalo.
The prize includes a $100,000 honorarium, donated to the FNIH by philanthropist Ann Lurie, who serves as president of the Ann and Robert H. Lurie Foundation and president of Lurie Holdings, according to the press release.
“This is a tremendous honor and is a strong endorsement of the work discovered by the scientists in my lab; it is very exciting,” said Dr. Chen. “We hope to continue our work to deepen our understanding of this pathway, as the mechanisms of the pathway are not yet completely understood, as well as look more into how we can harness the immunity pathway to develop treatments for cases like autoimmune diseases or cancer.”
The Foundation of the National Institutes of Health has awarded according to a statement released Tuesday, April 3.
“We are proud to honor Dr. Chen with the 2018 Lurie Prize in Biomedical Sciences for the discovery of the cGAS enzyme and pathway and their unique role in immune and inflammatory response,” Maria C. Freire, PhD, president and executive director of the FNIH, said in a press release. “Dr. Chen joins five other Lurie Prize winners, who are shaping the future of human health through their profound biomedical research.”
While scientists have known for some time that DNA had a role in activating the immune response, the specifics of the process eluded explanation.
Through their work, Dr. Chen and his team uncovered that cGAS was the enzyme used to spark the reaction.
“[cGAS] is a protein sensor that detects DNA as a danger signal that then triggers the immune response,” said Dr. Chen. “When DNA gets into the cytoplasm, cGAS becomes activated and catalyzes the synthesis of a small molecule, called cGAMP, which then functions as a messenger that activates the immune response pathway.”
While the cGAS enzyme can help defend against infectious disease or cancer, the enzyme can also trigger autoimmune diseases such as rheumatoid arthritis.
Dr. Chen is the George L. MacGregor Distinguished Chair in Biomedical Science and professor of molecular biology at the University of Texas Southwestern Medical Center, Dallas, and an investigator for the Howard Hughes Medical Institute, Chevy Chase, Md. He completed his undergraduate study in biology at Fujian (China) Normal University, after which he went on to earn his PhD from State University of New York at Buffalo.
The prize includes a $100,000 honorarium, donated to the FNIH by philanthropist Ann Lurie, who serves as president of the Ann and Robert H. Lurie Foundation and president of Lurie Holdings, according to the press release.
“This is a tremendous honor and is a strong endorsement of the work discovered by the scientists in my lab; it is very exciting,” said Dr. Chen. “We hope to continue our work to deepen our understanding of this pathway, as the mechanisms of the pathway are not yet completely understood, as well as look more into how we can harness the immunity pathway to develop treatments for cases like autoimmune diseases or cancer.”
FDA recalls kratom products for salmonella contamination
The Food and Drug Administration on April 3 recalled all products containing kratom manufactured by Triangle Pharmanaturals LLC, after a number of supplements tested positive for salmonella.
The FDA advises consumers to get rid of products including Raw Form Organics Maeng Da Kratom Emerald Green, Raw Form Organics Maeng Da Kratom Ivory White, and Raw Form Organics Maeng Da Kratom Ruby Red.
Evidence of the contamination was found after two samples were collected from a retail store in Oregon by the Oregon Public Health Division and tested positive for salmonella.
The recall was ordered after Triangle Pharmanaturals did not comply with a March 30 formal request from the FDA to voluntarily recall their products.
“This action is based on the imminent health risk posed by the contamination of this product with salmonella, and the refusal of this company to voluntarily act to protect its customers and issue a recall, despite our repeated requests and actions,” said FDA Commissioner Scott Gottlieb, M.D., said in a statement. “The action today is based on the risks posed by the contamination of this particular product with a potentially dangerous pathogen.”
At press time, Triangle Pharmanaturals did not respond to a request for comment.
This is the most recent in a list recalls of kratom products as part of an ongoing investigation of a salmonella outbreak by the FDA; however Triangle Pharmanaturals’ noncompliance is unique to the agency, according to an FDA representative.
“This is the first time the agency has issued a mandatory recall order to protect Americans from contaminated food products,” Michael Felberbaum, an FDA press officer, said in an interview. “This is the third time the FDA has invoked its mandatory recall authority, but the first time the agency ordered a mandatory recall because a company has opted not to voluntarily recall after the FDA’s notification of an opportunity to initiate a voluntary recall.”
Earlier in March, the CDC reported 87 people in 35 states infected with either Salmonella Javiana, Salmonela Okatie, or Salmonella Thompson, which have been associated with the outbreak.
While salmonella was identified in Triangle Pharmanaturals’ products, the strains identified are not currently linked to the outbreak.
Kratom, a plant that commonly grows in South East Asian countries like Thailand, Malaysia, Indonesia, and Papua New Guinea, has recently been used to produce food supplements and marketed as an alternative to addictive pain medication like opioids, as well as used to help treat opioid withdrawal symptoms.
Use of the food supplement has fired debate among physicians, patients, and public officials as all sides continue to determine its efficacy and how, or whether, it should be given a drug classification.
The Food and Drug Administration on April 3 recalled all products containing kratom manufactured by Triangle Pharmanaturals LLC, after a number of supplements tested positive for salmonella.
The FDA advises consumers to get rid of products including Raw Form Organics Maeng Da Kratom Emerald Green, Raw Form Organics Maeng Da Kratom Ivory White, and Raw Form Organics Maeng Da Kratom Ruby Red.
Evidence of the contamination was found after two samples were collected from a retail store in Oregon by the Oregon Public Health Division and tested positive for salmonella.
The recall was ordered after Triangle Pharmanaturals did not comply with a March 30 formal request from the FDA to voluntarily recall their products.
“This action is based on the imminent health risk posed by the contamination of this product with salmonella, and the refusal of this company to voluntarily act to protect its customers and issue a recall, despite our repeated requests and actions,” said FDA Commissioner Scott Gottlieb, M.D., said in a statement. “The action today is based on the risks posed by the contamination of this particular product with a potentially dangerous pathogen.”
At press time, Triangle Pharmanaturals did not respond to a request for comment.
This is the most recent in a list recalls of kratom products as part of an ongoing investigation of a salmonella outbreak by the FDA; however Triangle Pharmanaturals’ noncompliance is unique to the agency, according to an FDA representative.
“This is the first time the agency has issued a mandatory recall order to protect Americans from contaminated food products,” Michael Felberbaum, an FDA press officer, said in an interview. “This is the third time the FDA has invoked its mandatory recall authority, but the first time the agency ordered a mandatory recall because a company has opted not to voluntarily recall after the FDA’s notification of an opportunity to initiate a voluntary recall.”
Earlier in March, the CDC reported 87 people in 35 states infected with either Salmonella Javiana, Salmonela Okatie, or Salmonella Thompson, which have been associated with the outbreak.
While salmonella was identified in Triangle Pharmanaturals’ products, the strains identified are not currently linked to the outbreak.
Kratom, a plant that commonly grows in South East Asian countries like Thailand, Malaysia, Indonesia, and Papua New Guinea, has recently been used to produce food supplements and marketed as an alternative to addictive pain medication like opioids, as well as used to help treat opioid withdrawal symptoms.
Use of the food supplement has fired debate among physicians, patients, and public officials as all sides continue to determine its efficacy and how, or whether, it should be given a drug classification.
The Food and Drug Administration on April 3 recalled all products containing kratom manufactured by Triangle Pharmanaturals LLC, after a number of supplements tested positive for salmonella.
The FDA advises consumers to get rid of products including Raw Form Organics Maeng Da Kratom Emerald Green, Raw Form Organics Maeng Da Kratom Ivory White, and Raw Form Organics Maeng Da Kratom Ruby Red.
Evidence of the contamination was found after two samples were collected from a retail store in Oregon by the Oregon Public Health Division and tested positive for salmonella.
The recall was ordered after Triangle Pharmanaturals did not comply with a March 30 formal request from the FDA to voluntarily recall their products.
“This action is based on the imminent health risk posed by the contamination of this product with salmonella, and the refusal of this company to voluntarily act to protect its customers and issue a recall, despite our repeated requests and actions,” said FDA Commissioner Scott Gottlieb, M.D., said in a statement. “The action today is based on the risks posed by the contamination of this particular product with a potentially dangerous pathogen.”
At press time, Triangle Pharmanaturals did not respond to a request for comment.
This is the most recent in a list recalls of kratom products as part of an ongoing investigation of a salmonella outbreak by the FDA; however Triangle Pharmanaturals’ noncompliance is unique to the agency, according to an FDA representative.
“This is the first time the agency has issued a mandatory recall order to protect Americans from contaminated food products,” Michael Felberbaum, an FDA press officer, said in an interview. “This is the third time the FDA has invoked its mandatory recall authority, but the first time the agency ordered a mandatory recall because a company has opted not to voluntarily recall after the FDA’s notification of an opportunity to initiate a voluntary recall.”
Earlier in March, the CDC reported 87 people in 35 states infected with either Salmonella Javiana, Salmonela Okatie, or Salmonella Thompson, which have been associated with the outbreak.
While salmonella was identified in Triangle Pharmanaturals’ products, the strains identified are not currently linked to the outbreak.
Kratom, a plant that commonly grows in South East Asian countries like Thailand, Malaysia, Indonesia, and Papua New Guinea, has recently been used to produce food supplements and marketed as an alternative to addictive pain medication like opioids, as well as used to help treat opioid withdrawal symptoms.
Use of the food supplement has fired debate among physicians, patients, and public officials as all sides continue to determine its efficacy and how, or whether, it should be given a drug classification.
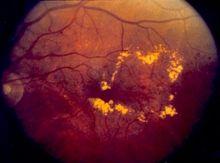
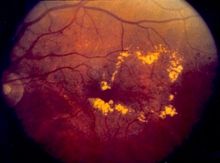
Robocalls increase diabetic retinopathy screenings in low-income patients
CHICAGO – according to a presentation at the annual meeting of the Endocrine Society.
Patients with diabetes require routine diabetic retinopathy (DR) screenings as it is usually asymptomatic until vision loss, explained presenter Eli K. Ipp, MD, professor of medicine at the University of California, Los Angeles. Sending robocalls is an easy, relatively cheap solution to encourage patients to seek screening, especially for certain populations that may be less inclined to spend the time and money to do so.
Investigators used EHRs to randomly selected 350 patients with diabetes to receive either a prerecorded message 1-7 days ahead of an existing appointment or a phone call from a staff member reminding patients of an upcoming appointment, during the course of 7 weeks.
Patients included were aged 54-58 years, and 70% were Hispanic and 30% were African American, with more than half this population having less than a high school education and three-quarters having an income less than $25,000.
Overall show rate for screenings was almost 14% higher in the robocall group (59.9%) than in the control group (46.3%).
Among African Americans, the program worked especially well, closing the gap with Hispanic patients, who reported attending their appointments nearly twice as often as did African American patients the previous year.
“Automated robocall reminders are an effective, potentially low-cost approach to appointment reminders in safety-net clinics,” Dr. Ipp explained to attendees. “Robocall almost eliminated the African American disparity seen with usual care in this population.”
Implementation of the robocalls is also relatively simple since the programs used to find the patients and create the calls are readily available, although investigators chose to gather the data for this study by hand, according to Dr. Ipp.
Screening rates in the United States are disconcertingly low, Dr. Ipp pointed out. While screening rates were around 70% in Medicare patients, rates among Medicaid and commercially insured patients hovered between 47.5%-54.9%, according to data collected by the National Committee for Quality Assurance.
Rates are especially low among minorities, as seen by a difference in screenings between minorities and non-Hispanic whites that ranged from 7% to15% during 2002-2009, according to a study cited by Dr. Ipp.
Dr. Ipp reported no relevant financial disclosures.
SOURCE: Mehranbod C et al. ENDO 2018, Abstract OR27-4.
CHICAGO – according to a presentation at the annual meeting of the Endocrine Society.
Patients with diabetes require routine diabetic retinopathy (DR) screenings as it is usually asymptomatic until vision loss, explained presenter Eli K. Ipp, MD, professor of medicine at the University of California, Los Angeles. Sending robocalls is an easy, relatively cheap solution to encourage patients to seek screening, especially for certain populations that may be less inclined to spend the time and money to do so.
Investigators used EHRs to randomly selected 350 patients with diabetes to receive either a prerecorded message 1-7 days ahead of an existing appointment or a phone call from a staff member reminding patients of an upcoming appointment, during the course of 7 weeks.
Patients included were aged 54-58 years, and 70% were Hispanic and 30% were African American, with more than half this population having less than a high school education and three-quarters having an income less than $25,000.
Overall show rate for screenings was almost 14% higher in the robocall group (59.9%) than in the control group (46.3%).
Among African Americans, the program worked especially well, closing the gap with Hispanic patients, who reported attending their appointments nearly twice as often as did African American patients the previous year.
“Automated robocall reminders are an effective, potentially low-cost approach to appointment reminders in safety-net clinics,” Dr. Ipp explained to attendees. “Robocall almost eliminated the African American disparity seen with usual care in this population.”
Implementation of the robocalls is also relatively simple since the programs used to find the patients and create the calls are readily available, although investigators chose to gather the data for this study by hand, according to Dr. Ipp.
Screening rates in the United States are disconcertingly low, Dr. Ipp pointed out. While screening rates were around 70% in Medicare patients, rates among Medicaid and commercially insured patients hovered between 47.5%-54.9%, according to data collected by the National Committee for Quality Assurance.
Rates are especially low among minorities, as seen by a difference in screenings between minorities and non-Hispanic whites that ranged from 7% to15% during 2002-2009, according to a study cited by Dr. Ipp.
Dr. Ipp reported no relevant financial disclosures.
SOURCE: Mehranbod C et al. ENDO 2018, Abstract OR27-4.
CHICAGO – according to a presentation at the annual meeting of the Endocrine Society.
Patients with diabetes require routine diabetic retinopathy (DR) screenings as it is usually asymptomatic until vision loss, explained presenter Eli K. Ipp, MD, professor of medicine at the University of California, Los Angeles. Sending robocalls is an easy, relatively cheap solution to encourage patients to seek screening, especially for certain populations that may be less inclined to spend the time and money to do so.
Investigators used EHRs to randomly selected 350 patients with diabetes to receive either a prerecorded message 1-7 days ahead of an existing appointment or a phone call from a staff member reminding patients of an upcoming appointment, during the course of 7 weeks.
Patients included were aged 54-58 years, and 70% were Hispanic and 30% were African American, with more than half this population having less than a high school education and three-quarters having an income less than $25,000.
Overall show rate for screenings was almost 14% higher in the robocall group (59.9%) than in the control group (46.3%).
Among African Americans, the program worked especially well, closing the gap with Hispanic patients, who reported attending their appointments nearly twice as often as did African American patients the previous year.
“Automated robocall reminders are an effective, potentially low-cost approach to appointment reminders in safety-net clinics,” Dr. Ipp explained to attendees. “Robocall almost eliminated the African American disparity seen with usual care in this population.”
Implementation of the robocalls is also relatively simple since the programs used to find the patients and create the calls are readily available, although investigators chose to gather the data for this study by hand, according to Dr. Ipp.
Screening rates in the United States are disconcertingly low, Dr. Ipp pointed out. While screening rates were around 70% in Medicare patients, rates among Medicaid and commercially insured patients hovered between 47.5%-54.9%, according to data collected by the National Committee for Quality Assurance.
Rates are especially low among minorities, as seen by a difference in screenings between minorities and non-Hispanic whites that ranged from 7% to15% during 2002-2009, according to a study cited by Dr. Ipp.
Dr. Ipp reported no relevant financial disclosures.
SOURCE: Mehranbod C et al. ENDO 2018, Abstract OR27-4.
REPORTING FROM ENDO 2018
Key clinical point: Robocalls increase diabetic retinopathy screenings in low-income, minority patients.
Major finding: Overall rate of patients who showed up to DR screenings increased from 46.3% to 59.9% in the robocall test group (P = .036).
Data source: Controlled study of 301 patients who received a robocall over 7 weeks.
Disclosures: Dr. Ipp reported no relevant financial disclosures.
Source: Mehranbod C et al. ENDO 2018, Abstract OR27-4.
Declining androgen levels correlated with increased frailty
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The findings provide more evidence of the relationship between function and lower levels of androgens such as testosterone and introduce the possibility of using hormones to offset frailty in older patients.
“The decline in total and free [testosterone] and DHEA-S [dehydroepiandrosterone sulfate] was significantly associated with small deteriorations in physical function and worsening frailty,” according to presenter Frederick C. Wu, MD, an endocrinologist at the University of Manchester (England). “The present results are consistent with and support our hypothesis that the decline in these hormones can contribute to a worsening physical function and frailty in the elderly.”
Investigators gathered data on 2,278 men from eight centers across Europe to conduct an observational study of their physical functions.
Patients were all men, an average of 58 years old, and had an average body mass index of 27.6 kg/m2 and average free testosterone and DHEA-S levels at 16.9 nmol/L and 4.7 micromol/L, respectively.
At follow-up, which was on average conducted 4.4 years later, average age was 63 years, and average testosterone and DHEA-S levels had dropped to 287.3 nmol/L and 4 micromol/L respectively, which Dr. Wu described as a moderate drop.
Decreases of free testosterone or DHEA-S by one standard deviation – 86.8 nmol/L and 2.6 micromol/L, respectively – accounted for 11%-17% of the average rate of deterioration of physical function, according to Dr. Wu.
Patients with lower levels of free testosterone and DHEA-S experienced worsening 15-meter walk time, five chair-stands, physical quality of life, and overall worsening of frailty phenotypes at follow up.
Dr. Wu and his colleagues measured frailness in patients by looking for the presence of frailty phenotypes, which include slowness, sarcopenia, exhaustion, low activity, and weakness.
If one-two of these criteria were present, patients would be considered “prefrail,” and if three or more were present, patients would be deemed “frail.”
Patients experienced an average 2.5% increase in frailty per year during the time between baseline and follow up, Dr. Wu told attendees.
Investigators used the mean of 60 years old to adjust for age, Dr. Wu explained in response to a question from the audience; however, this may have been an overadjustment as free testosterone and DHEA-S are age dependent, Dr. Wu admitted.
Investigators also incorporated a frailty index of 39 health deficits – 16 physical or cognitive, 11 comorbidities, and 12 clinical – measuring on a 0-1 scale in order to measure different levels of frailty.
While the link between these androgens and frailty are evident, the potential benefits of hormonal intervention in elderly men are still in the air and demand further study.
“The decline in androgen levels in the physiological range, because of the modest degree of change, is unlikely to be the single greatest cause of deterioration in the majority of aging men in the population,” said Dr. Wu. “Therefore, the possible therapeutic roles of androgens in improving physical health may be limited to a minority of men with very low levels of testosterone.”
Dr. Wu is on the advisory board of Bayer-Schering, Eli Lilly, and Besins Healthcare. Dr. Wu is a research supporter or consultant for Repros Therapeutics, Merck Serono, and Mereo Biopharma. Investigators reported no additional relevant financial disclosures.
SOURCE: Wu F C et al. ENDO 2018, Abstract OR15-1.
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The findings provide more evidence of the relationship between function and lower levels of androgens such as testosterone and introduce the possibility of using hormones to offset frailty in older patients.
“The decline in total and free [testosterone] and DHEA-S [dehydroepiandrosterone sulfate] was significantly associated with small deteriorations in physical function and worsening frailty,” according to presenter Frederick C. Wu, MD, an endocrinologist at the University of Manchester (England). “The present results are consistent with and support our hypothesis that the decline in these hormones can contribute to a worsening physical function and frailty in the elderly.”
Investigators gathered data on 2,278 men from eight centers across Europe to conduct an observational study of their physical functions.
Patients were all men, an average of 58 years old, and had an average body mass index of 27.6 kg/m2 and average free testosterone and DHEA-S levels at 16.9 nmol/L and 4.7 micromol/L, respectively.
At follow-up, which was on average conducted 4.4 years later, average age was 63 years, and average testosterone and DHEA-S levels had dropped to 287.3 nmol/L and 4 micromol/L respectively, which Dr. Wu described as a moderate drop.
Decreases of free testosterone or DHEA-S by one standard deviation – 86.8 nmol/L and 2.6 micromol/L, respectively – accounted for 11%-17% of the average rate of deterioration of physical function, according to Dr. Wu.
Patients with lower levels of free testosterone and DHEA-S experienced worsening 15-meter walk time, five chair-stands, physical quality of life, and overall worsening of frailty phenotypes at follow up.
Dr. Wu and his colleagues measured frailness in patients by looking for the presence of frailty phenotypes, which include slowness, sarcopenia, exhaustion, low activity, and weakness.
If one-two of these criteria were present, patients would be considered “prefrail,” and if three or more were present, patients would be deemed “frail.”
Patients experienced an average 2.5% increase in frailty per year during the time between baseline and follow up, Dr. Wu told attendees.
Investigators used the mean of 60 years old to adjust for age, Dr. Wu explained in response to a question from the audience; however, this may have been an overadjustment as free testosterone and DHEA-S are age dependent, Dr. Wu admitted.
Investigators also incorporated a frailty index of 39 health deficits – 16 physical or cognitive, 11 comorbidities, and 12 clinical – measuring on a 0-1 scale in order to measure different levels of frailty.
While the link between these androgens and frailty are evident, the potential benefits of hormonal intervention in elderly men are still in the air and demand further study.
“The decline in androgen levels in the physiological range, because of the modest degree of change, is unlikely to be the single greatest cause of deterioration in the majority of aging men in the population,” said Dr. Wu. “Therefore, the possible therapeutic roles of androgens in improving physical health may be limited to a minority of men with very low levels of testosterone.”
Dr. Wu is on the advisory board of Bayer-Schering, Eli Lilly, and Besins Healthcare. Dr. Wu is a research supporter or consultant for Repros Therapeutics, Merck Serono, and Mereo Biopharma. Investigators reported no additional relevant financial disclosures.
SOURCE: Wu F C et al. ENDO 2018, Abstract OR15-1.
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The findings provide more evidence of the relationship between function and lower levels of androgens such as testosterone and introduce the possibility of using hormones to offset frailty in older patients.
“The decline in total and free [testosterone] and DHEA-S [dehydroepiandrosterone sulfate] was significantly associated with small deteriorations in physical function and worsening frailty,” according to presenter Frederick C. Wu, MD, an endocrinologist at the University of Manchester (England). “The present results are consistent with and support our hypothesis that the decline in these hormones can contribute to a worsening physical function and frailty in the elderly.”
Investigators gathered data on 2,278 men from eight centers across Europe to conduct an observational study of their physical functions.
Patients were all men, an average of 58 years old, and had an average body mass index of 27.6 kg/m2 and average free testosterone and DHEA-S levels at 16.9 nmol/L and 4.7 micromol/L, respectively.
At follow-up, which was on average conducted 4.4 years later, average age was 63 years, and average testosterone and DHEA-S levels had dropped to 287.3 nmol/L and 4 micromol/L respectively, which Dr. Wu described as a moderate drop.
Decreases of free testosterone or DHEA-S by one standard deviation – 86.8 nmol/L and 2.6 micromol/L, respectively – accounted for 11%-17% of the average rate of deterioration of physical function, according to Dr. Wu.
Patients with lower levels of free testosterone and DHEA-S experienced worsening 15-meter walk time, five chair-stands, physical quality of life, and overall worsening of frailty phenotypes at follow up.
Dr. Wu and his colleagues measured frailness in patients by looking for the presence of frailty phenotypes, which include slowness, sarcopenia, exhaustion, low activity, and weakness.
If one-two of these criteria were present, patients would be considered “prefrail,” and if three or more were present, patients would be deemed “frail.”
Patients experienced an average 2.5% increase in frailty per year during the time between baseline and follow up, Dr. Wu told attendees.
Investigators used the mean of 60 years old to adjust for age, Dr. Wu explained in response to a question from the audience; however, this may have been an overadjustment as free testosterone and DHEA-S are age dependent, Dr. Wu admitted.
Investigators also incorporated a frailty index of 39 health deficits – 16 physical or cognitive, 11 comorbidities, and 12 clinical – measuring on a 0-1 scale in order to measure different levels of frailty.
While the link between these androgens and frailty are evident, the potential benefits of hormonal intervention in elderly men are still in the air and demand further study.
“The decline in androgen levels in the physiological range, because of the modest degree of change, is unlikely to be the single greatest cause of deterioration in the majority of aging men in the population,” said Dr. Wu. “Therefore, the possible therapeutic roles of androgens in improving physical health may be limited to a minority of men with very low levels of testosterone.”
Dr. Wu is on the advisory board of Bayer-Schering, Eli Lilly, and Besins Healthcare. Dr. Wu is a research supporter or consultant for Repros Therapeutics, Merck Serono, and Mereo Biopharma. Investigators reported no additional relevant financial disclosures.
SOURCE: Wu F C et al. ENDO 2018, Abstract OR15-1.
REPORTING FROM ENDO 2018
Key clinical point: Declining androgen levels correlates with lower physical function in elder men.
Major finding: Decline in testosterone by one standard deviation accounted for 11%-17% of the average population rate of physical function deterioration.
Data source: Prospective study of 2,278 men gathered from eight European centers.
Disclosures: Frederick C. Wu is on the advisory board of Bayer-Schering, Eli Lilly, and Besins Healthcare. Dr. Wu is a research supporter or consultant for Repros Therapeutics, Merck Serono, and Mereo Biopharma.
Source: Wu F C et al. ENDO 2018 OR15-1.
Oral SGLT-2 inhibitor reduced liver fat in diabetics with NAFLD
CHICAGO – and improved ALT in patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus, according to a study presented at the annual meeting of the Endocrine Society.
As insulin resistance is the mechanism for NAFLD development, this new addition to the list of drugs on offer to patients with diabetes could help decrease the chance of developing metabolic syndrome and cardiovascular disease.
“SGLT-2 inhibitors are newer antidiabetic agents that reduce blood glucose by promoting urinary glucose excretion,” said presenter Mohammad Shafi Kuchay, MD, DM, an endocrinologist at Medanta The Medicity, Gurugram, India. “NAFLD, which also increases the risk of type 2 diabetes, often responds to strategies that improve hyperglycemia.”
Dr. Kuchay and fellow investigators conducted a small, 20-week randomized controlled trial of 42 patients with type 2 diabetes and NAFLD.
Patients in the test group were mostly male and on average 50 years old, with baseline AST, ALT, and gamma-glutamyltransferase scores of 44.6 U/L, 64.3 U/L, and 65.8 U/L, respectively. Those randomized to the control group had similar characteristics.
After adding 10 mg of empagliflozin to their diabetes regimen, liver fat density in test patients decreased from 16.2% to 11.3% (P less than or equal to .0001). The drop stands in sharp contrast to the control group, which decreased from 16.4% to 15.5% (P = .054). Measurement of liver fat density was made by MRI-derived proton density fat fraction (MRI-PDFF). This method has higher sensitivity for detecting changes in liver fat, compared with histology, explained Dr. Kuchay.
When broken down by individual liver fat, 25% of patients in the control group increased in liver fat, 50% had no significant change, and 25% decreased in liver fat, according to Dr. Kuchay.
In comparison, 77% of patients in the empagliflozin group had a decrease in liver fat, 23% had no change, and no patients saw an increase in liver fat.
When comparing levels of hemoglobin A1c between the two groups, both had a similarly significant reduction of around 2%, which Dr. Kuchay attributes to deliberate intervention by investigators.
Further studies will need to be conducted regarding the long-term effects of this treatment; however, using SGLT-2 to reduce liver fat could be a boon to preventing more serious liver diseases, concluded Dr. Kuchay.
“There are studies in which liver fat reduction led to improvement in inflammation and fibrosis,” said Dr. Kuchay in response to a question from the audience. “Because liver fat accumulation is the first inhibitor in the pathogenesis of more severe forms of liver disease, reducing liver fat should help improve patient outcomes.”
Dr. Kuchay reported no relevant financial disclosures.
Source: M. Kuchay et al. ENDO 2018, Abstract OR27-2.
CHICAGO – and improved ALT in patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus, according to a study presented at the annual meeting of the Endocrine Society.
As insulin resistance is the mechanism for NAFLD development, this new addition to the list of drugs on offer to patients with diabetes could help decrease the chance of developing metabolic syndrome and cardiovascular disease.
“SGLT-2 inhibitors are newer antidiabetic agents that reduce blood glucose by promoting urinary glucose excretion,” said presenter Mohammad Shafi Kuchay, MD, DM, an endocrinologist at Medanta The Medicity, Gurugram, India. “NAFLD, which also increases the risk of type 2 diabetes, often responds to strategies that improve hyperglycemia.”
Dr. Kuchay and fellow investigators conducted a small, 20-week randomized controlled trial of 42 patients with type 2 diabetes and NAFLD.
Patients in the test group were mostly male and on average 50 years old, with baseline AST, ALT, and gamma-glutamyltransferase scores of 44.6 U/L, 64.3 U/L, and 65.8 U/L, respectively. Those randomized to the control group had similar characteristics.
After adding 10 mg of empagliflozin to their diabetes regimen, liver fat density in test patients decreased from 16.2% to 11.3% (P less than or equal to .0001). The drop stands in sharp contrast to the control group, which decreased from 16.4% to 15.5% (P = .054). Measurement of liver fat density was made by MRI-derived proton density fat fraction (MRI-PDFF). This method has higher sensitivity for detecting changes in liver fat, compared with histology, explained Dr. Kuchay.
When broken down by individual liver fat, 25% of patients in the control group increased in liver fat, 50% had no significant change, and 25% decreased in liver fat, according to Dr. Kuchay.
In comparison, 77% of patients in the empagliflozin group had a decrease in liver fat, 23% had no change, and no patients saw an increase in liver fat.
When comparing levels of hemoglobin A1c between the two groups, both had a similarly significant reduction of around 2%, which Dr. Kuchay attributes to deliberate intervention by investigators.
Further studies will need to be conducted regarding the long-term effects of this treatment; however, using SGLT-2 to reduce liver fat could be a boon to preventing more serious liver diseases, concluded Dr. Kuchay.
“There are studies in which liver fat reduction led to improvement in inflammation and fibrosis,” said Dr. Kuchay in response to a question from the audience. “Because liver fat accumulation is the first inhibitor in the pathogenesis of more severe forms of liver disease, reducing liver fat should help improve patient outcomes.”
Dr. Kuchay reported no relevant financial disclosures.
Source: M. Kuchay et al. ENDO 2018, Abstract OR27-2.
CHICAGO – and improved ALT in patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus, according to a study presented at the annual meeting of the Endocrine Society.
As insulin resistance is the mechanism for NAFLD development, this new addition to the list of drugs on offer to patients with diabetes could help decrease the chance of developing metabolic syndrome and cardiovascular disease.
“SGLT-2 inhibitors are newer antidiabetic agents that reduce blood glucose by promoting urinary glucose excretion,” said presenter Mohammad Shafi Kuchay, MD, DM, an endocrinologist at Medanta The Medicity, Gurugram, India. “NAFLD, which also increases the risk of type 2 diabetes, often responds to strategies that improve hyperglycemia.”
Dr. Kuchay and fellow investigators conducted a small, 20-week randomized controlled trial of 42 patients with type 2 diabetes and NAFLD.
Patients in the test group were mostly male and on average 50 years old, with baseline AST, ALT, and gamma-glutamyltransferase scores of 44.6 U/L, 64.3 U/L, and 65.8 U/L, respectively. Those randomized to the control group had similar characteristics.
After adding 10 mg of empagliflozin to their diabetes regimen, liver fat density in test patients decreased from 16.2% to 11.3% (P less than or equal to .0001). The drop stands in sharp contrast to the control group, which decreased from 16.4% to 15.5% (P = .054). Measurement of liver fat density was made by MRI-derived proton density fat fraction (MRI-PDFF). This method has higher sensitivity for detecting changes in liver fat, compared with histology, explained Dr. Kuchay.
When broken down by individual liver fat, 25% of patients in the control group increased in liver fat, 50% had no significant change, and 25% decreased in liver fat, according to Dr. Kuchay.
In comparison, 77% of patients in the empagliflozin group had a decrease in liver fat, 23% had no change, and no patients saw an increase in liver fat.
When comparing levels of hemoglobin A1c between the two groups, both had a similarly significant reduction of around 2%, which Dr. Kuchay attributes to deliberate intervention by investigators.
Further studies will need to be conducted regarding the long-term effects of this treatment; however, using SGLT-2 to reduce liver fat could be a boon to preventing more serious liver diseases, concluded Dr. Kuchay.
“There are studies in which liver fat reduction led to improvement in inflammation and fibrosis,” said Dr. Kuchay in response to a question from the audience. “Because liver fat accumulation is the first inhibitor in the pathogenesis of more severe forms of liver disease, reducing liver fat should help improve patient outcomes.”
Dr. Kuchay reported no relevant financial disclosures.
Source: M. Kuchay et al. ENDO 2018, Abstract OR27-2.
REPORTING FROM ENDO 2018
Key clinical point: Empagliflozin reduced liver fat in patients with NAFLD and type 2 diabetes.
Major finding: MRI-PDFF in test patients decreased from 16.2% to 11.3% (P less than or equal to .0001), compared with control patients, who saw a decrease from 19.4% to 15.5% (P = .057)
Data source: Prospective, randomized, controlled trial of 60 patients with type 2 diabetes and NAFLD.
Disclosures: Dr. Kuchay reported no relevant financial disclosures.
Source: Kuchay M et al. ENDO 2018, Abstract OR27-2.
Is kratom the answer to the opioid crisis?
As the opioid epidemic continues to ravage the United States, patients and physicians are looking for less-addictive alternatives for pain control.
For a growing number of U.S. patients, top among the contenders is kratom, a plant-based product that shows a dose-dependent opioidlike effect. For physicians, toxicologists – and federal regulators, however – the absence of evidence-based studies on the herb’s effectiveness and safety is raising concerns.
“
Petros Levounis, MD, an addiction psychiatrist who has treated kratom users, said an inherent challenge is countering patients’ perceptions about the substance.
“Somehow, in the popular culture, kratom has a reputation as being a mild opioid. And we’re not sure about that,” said Dr. Levounis, a member of the American Academy of Addiction Psychiatry. “But the fact that people think it’s more natural and therefore it must be safer is very problematic.”
The uncertainty around kratom raises the stakes when it comes to treating patients. “From a medical perspective, one of the trickiest issues is we’re not sure that naloxone reverses the opioid effects,” said Dr. Levounis, also chair of psychiatry at Robert Wood Johnson Medical School, New Brunswick. “We do use naloxone, but it is not clear that it works as an antidote. This is probably the most problematic area about kratom.”
Origins, demographics
A member of the coffee family, kratom (Mitragyna speciosa) grows in Thailand, Malaysia, Indonesia, and Papua New Guinea, and has been used throughout southeast Asia for many years to manage pain and bolster energy, according to the National Center for Complementary and Integrative Health.
Dr. Grundmann conducted an anonymous survey last year about kratom and found that most users are white, married or partnered, and employed for wages. Dr. Grundmann’s survey of 8,049 kratom users also found that a majority of users reported having some college. However, the survey found an inverse relationship between years of education and the tendency to use kratom (Drug Alcohol Depend. 2017 Jul 1;176:63-70).
“The more education somebody has, the less likely they are to use kratom for prescription medicine dependency or for an emotional or mental condition,” Dr. Grundmann said.
Anecdotal evidence
One study conducted by David Galbis-Reig, MD, president-elect of the Wisconsin Society of Addiction Medicine, followed a 37-year-old woman who experienced kratom addiction.
“The mitragynine and 7-Hydroxymitragynine very clearly have partial opioid agonist activity with kappa antagonist activity, which is very similar to buprenorphine,” said Dr. Galbis-Reig, who is also with American Society of Addiction Medicine.
A major concern that Dr. Galbis-Reig’s case brings up is the use of liquid kratom extract.
“My biggest concern is we just don’t know what the stimulant properties of the drug are,” Dr. Galbis-Reig said. “If it turns out the properties are more in line with an amphetamine, I’m not sure that’s a great drug to use in a clinical setting for many conditions.”
But Murray A. Holcomb, MD, an acute care surgeon at Seton Healthcare Family Center, Round Rock, Tex., offered a different take. He said he and his family were first highly skeptical when they first heard about kratom. But after years of trying to help his son overcome his depression and substance abuse, Dr. Holcomb said he was ready to try anything.
After researching and consulting with his colleagues, Dr. Holcomb helped his son acquire the plant. What was expected to be another substance that overpromised and underdelivered turned out to be the real thing.
“Out of desperation, [my son] tried kratom, and within a few short days, he began to experience remission of his symptoms – which was immediately noticeable to all of us who knew him,” said Dr. Holcomb. “It is important to note that kratom does not make him high, loopy, or anything but normal. He lives independently, works full time, maintains healthy relationships, is pleasant and responsible, reestablished contact with his sister and brother, and is largely a happy normal person.”
Not only was his son able to return to his normal life, but the costs for his dose of kratom were within his budget while making minimum wage, similar to a majority of users – who make $35,000-$50,000 per year, Dr. Grundmann’s survey results suggest.
For people with substance use disorder, the issue of addiction always is present, Dr. Holcomb believes, and if that is the case, it’s better to be using kratom than another drug,
“If people steer themselves to kratom rather than something else, that’s probably a good thing, because if someone wants to abuse something, you can’t stop them; you can’t regulate intent,“ Dr. Holcomb said. “Kratom is a partial agonist. It doesn’t make you euphorically high, it doesn’t make you quit breathing, and you don’t really have any withdrawal symptoms, and no one is going to overdose on a natural plant – because it will make them sick to their stomach.”
In a systematic review of studies related to kratom use, investigators found that the product “may be useful for analgesia, mood elevation, anxiety reduction, and may aid opioid withdrawal management. Negative themes also emerged, including unfavorable side effects, especially stomach upset and vomiting,” wrote Marc T. Swogger, PhD, and his colleagues (J Psychoactive Drugs. 2015 Nov-Dec;47[5]:360-7).
“As an opioid substitute, it seems to be used in good effect to decrease opioid withdrawal symptoms, including cravings for more opioids,” said Dr. Swogger, clinical psychologist at the University of Rochester (N.Y.). “People are able to use kratom as a way to get through systemic hoops to get the medicine they need.”
The regulatory fight
In 2016, the Drug Enforcement Administration announced its intentions to classify mitragynine and 7-Hydroxymitragynine, the active ingredients in kratom, as a schedule I drug in order to “avoid an imminent hazard to public safety” after two cases of kratom exposure were reported to the American Association for Poison Control Centers, according to a statement released by the DEA.
In November 2017, Scott Gottlieb, MD, commissioner of the Food and Drug Administration, issued a public health advisory reporting that kratom-related calls to U.S. poison control centers soared 10-fold during 2010-2015. It also said that 36 people have died after using products containing kratom. In light of those developments and with the absence of evidence showing that the substance is safe, the agency is taking action, he wrote.
“To fulfill our public health obligations, we have identified kratom products on two import alerts and we are working to actively prevent shipments of kratom from entering the U.S.,” Dr. Gottlieb wrote. “Kratom is already a controlled substance in 16 countries, including 2 of its native countries of origin, Thailand and Malaysia, as well as Australia, Sweden, and Germany. Kratom is also banned in several states, specifically Alabama, Arkansas, Indiana, Tennessee, and Wisconsin, and several others have pending legislation to ban it.”
In December 2017, a group comprising 17 members of Congress responded wrote a letter to Dr. Gottlieb imploring the Trump administration to recognize the merits of the substance and to drop its intention to make it more difficult to procure.
“Given that numerous stakeholders, former opioid addicts, and scientific researchers vouch for kratom’s safety and support its use, and responsible manufacturers of kratom products ensure that their products are properly labeled for adult-only consumption, we respectfully request that the FDA reconsider its stance and take a closer look at the facts and recent science regarding this plant,” the members wrote in the letter. After the letter was received by the FDA, the DEA decided to hold off on its scheduling.
But controversy surrounding the botanical product continues. Earlier this year, the FDA ordered the recall and destruction of kratom-containing dietary supplements made by a company in Grain Valley, Mo., the agency said in a statement. The FDA also is investigating a possible association between kratom intake and an outbreak of salmonella in North Dakota and Utah, in which 17 of 24 patients reported taking products thought to contain kratom before becoming sick, the agency wrote. Meanwhile, in late March, the FDA reported that it was investigating a multistate outbreak of salmonella infections tied to products that were reported to contain kratom. For example, the agency said, it is "reporting four additional products tested by Oregon Health Authority identified as positive for salmonella in four additional product samples collected from the retailer Torched Illusions." As of March 15, the FDA said, the Centers for Disease Control and Prevention reported that 87 people had been infected with outbreak strains of salmonella reported from 35 states.*
Dr. Gottlieb had issued a statement a few weeks earlier, in February, saying that the agency was able to confirm that kratom contains opioids. “The extensive scientific data we’ve evaluated about kratom provides conclusive evidence that compounds contained in kratom are opioids and are expected to have similar addictive effects as well as risks of abuse, overdose and, in some cases, death. At the same time, there’s no evidence to indicate that kratom is safe or effective for any medical use,” Dr. Gottlieb wrote. “To protect the public health, we’ll continue to affirm the risks associated with kratom, warn consumers against its use, and take aggressive enforcement action against kratom-containing products.”
For physicians like Dr. Levounis, who treat kratom users in emergency departments, patients should heed those warnings. “People erroneously feel that herbal products are milder than other products,” he said. “Nature can manufacture incredibly strong stuff – for good and for bad.”
*This story was updated 3/23/2018.
Dr. Goldberger, Dr. Levounis, Dr. Grundmann, and Dr. Holcomb had no disclosures. Dr. Galbis-Reig disclosed in his study that he is the owner of stock in GW Pharmaceuticals and Cortex Pharmaceuticals, Pfizer bonds, and has spousal ownership of stock in AbbVie, Abbott Pharma, and Hospira. Dr. Swogger and other authors of the systematic review reported serving as consultants for the American Kratom Association, as well as sponsors of other kratom products.
As the opioid epidemic continues to ravage the United States, patients and physicians are looking for less-addictive alternatives for pain control.
For a growing number of U.S. patients, top among the contenders is kratom, a plant-based product that shows a dose-dependent opioidlike effect. For physicians, toxicologists – and federal regulators, however – the absence of evidence-based studies on the herb’s effectiveness and safety is raising concerns.
“
Petros Levounis, MD, an addiction psychiatrist who has treated kratom users, said an inherent challenge is countering patients’ perceptions about the substance.
“Somehow, in the popular culture, kratom has a reputation as being a mild opioid. And we’re not sure about that,” said Dr. Levounis, a member of the American Academy of Addiction Psychiatry. “But the fact that people think it’s more natural and therefore it must be safer is very problematic.”
The uncertainty around kratom raises the stakes when it comes to treating patients. “From a medical perspective, one of the trickiest issues is we’re not sure that naloxone reverses the opioid effects,” said Dr. Levounis, also chair of psychiatry at Robert Wood Johnson Medical School, New Brunswick. “We do use naloxone, but it is not clear that it works as an antidote. This is probably the most problematic area about kratom.”
Origins, demographics
A member of the coffee family, kratom (Mitragyna speciosa) grows in Thailand, Malaysia, Indonesia, and Papua New Guinea, and has been used throughout southeast Asia for many years to manage pain and bolster energy, according to the National Center for Complementary and Integrative Health.
Dr. Grundmann conducted an anonymous survey last year about kratom and found that most users are white, married or partnered, and employed for wages. Dr. Grundmann’s survey of 8,049 kratom users also found that a majority of users reported having some college. However, the survey found an inverse relationship between years of education and the tendency to use kratom (Drug Alcohol Depend. 2017 Jul 1;176:63-70).
“The more education somebody has, the less likely they are to use kratom for prescription medicine dependency or for an emotional or mental condition,” Dr. Grundmann said.
Anecdotal evidence
One study conducted by David Galbis-Reig, MD, president-elect of the Wisconsin Society of Addiction Medicine, followed a 37-year-old woman who experienced kratom addiction.
“The mitragynine and 7-Hydroxymitragynine very clearly have partial opioid agonist activity with kappa antagonist activity, which is very similar to buprenorphine,” said Dr. Galbis-Reig, who is also with American Society of Addiction Medicine.
A major concern that Dr. Galbis-Reig’s case brings up is the use of liquid kratom extract.
“My biggest concern is we just don’t know what the stimulant properties of the drug are,” Dr. Galbis-Reig said. “If it turns out the properties are more in line with an amphetamine, I’m not sure that’s a great drug to use in a clinical setting for many conditions.”
But Murray A. Holcomb, MD, an acute care surgeon at Seton Healthcare Family Center, Round Rock, Tex., offered a different take. He said he and his family were first highly skeptical when they first heard about kratom. But after years of trying to help his son overcome his depression and substance abuse, Dr. Holcomb said he was ready to try anything.
After researching and consulting with his colleagues, Dr. Holcomb helped his son acquire the plant. What was expected to be another substance that overpromised and underdelivered turned out to be the real thing.
“Out of desperation, [my son] tried kratom, and within a few short days, he began to experience remission of his symptoms – which was immediately noticeable to all of us who knew him,” said Dr. Holcomb. “It is important to note that kratom does not make him high, loopy, or anything but normal. He lives independently, works full time, maintains healthy relationships, is pleasant and responsible, reestablished contact with his sister and brother, and is largely a happy normal person.”
Not only was his son able to return to his normal life, but the costs for his dose of kratom were within his budget while making minimum wage, similar to a majority of users – who make $35,000-$50,000 per year, Dr. Grundmann’s survey results suggest.
For people with substance use disorder, the issue of addiction always is present, Dr. Holcomb believes, and if that is the case, it’s better to be using kratom than another drug,
“If people steer themselves to kratom rather than something else, that’s probably a good thing, because if someone wants to abuse something, you can’t stop them; you can’t regulate intent,“ Dr. Holcomb said. “Kratom is a partial agonist. It doesn’t make you euphorically high, it doesn’t make you quit breathing, and you don’t really have any withdrawal symptoms, and no one is going to overdose on a natural plant – because it will make them sick to their stomach.”
In a systematic review of studies related to kratom use, investigators found that the product “may be useful for analgesia, mood elevation, anxiety reduction, and may aid opioid withdrawal management. Negative themes also emerged, including unfavorable side effects, especially stomach upset and vomiting,” wrote Marc T. Swogger, PhD, and his colleagues (J Psychoactive Drugs. 2015 Nov-Dec;47[5]:360-7).
“As an opioid substitute, it seems to be used in good effect to decrease opioid withdrawal symptoms, including cravings for more opioids,” said Dr. Swogger, clinical psychologist at the University of Rochester (N.Y.). “People are able to use kratom as a way to get through systemic hoops to get the medicine they need.”
The regulatory fight
In 2016, the Drug Enforcement Administration announced its intentions to classify mitragynine and 7-Hydroxymitragynine, the active ingredients in kratom, as a schedule I drug in order to “avoid an imminent hazard to public safety” after two cases of kratom exposure were reported to the American Association for Poison Control Centers, according to a statement released by the DEA.
In November 2017, Scott Gottlieb, MD, commissioner of the Food and Drug Administration, issued a public health advisory reporting that kratom-related calls to U.S. poison control centers soared 10-fold during 2010-2015. It also said that 36 people have died after using products containing kratom. In light of those developments and with the absence of evidence showing that the substance is safe, the agency is taking action, he wrote.
“To fulfill our public health obligations, we have identified kratom products on two import alerts and we are working to actively prevent shipments of kratom from entering the U.S.,” Dr. Gottlieb wrote. “Kratom is already a controlled substance in 16 countries, including 2 of its native countries of origin, Thailand and Malaysia, as well as Australia, Sweden, and Germany. Kratom is also banned in several states, specifically Alabama, Arkansas, Indiana, Tennessee, and Wisconsin, and several others have pending legislation to ban it.”
In December 2017, a group comprising 17 members of Congress responded wrote a letter to Dr. Gottlieb imploring the Trump administration to recognize the merits of the substance and to drop its intention to make it more difficult to procure.
“Given that numerous stakeholders, former opioid addicts, and scientific researchers vouch for kratom’s safety and support its use, and responsible manufacturers of kratom products ensure that their products are properly labeled for adult-only consumption, we respectfully request that the FDA reconsider its stance and take a closer look at the facts and recent science regarding this plant,” the members wrote in the letter. After the letter was received by the FDA, the DEA decided to hold off on its scheduling.
But controversy surrounding the botanical product continues. Earlier this year, the FDA ordered the recall and destruction of kratom-containing dietary supplements made by a company in Grain Valley, Mo., the agency said in a statement. The FDA also is investigating a possible association between kratom intake and an outbreak of salmonella in North Dakota and Utah, in which 17 of 24 patients reported taking products thought to contain kratom before becoming sick, the agency wrote. Meanwhile, in late March, the FDA reported that it was investigating a multistate outbreak of salmonella infections tied to products that were reported to contain kratom. For example, the agency said, it is "reporting four additional products tested by Oregon Health Authority identified as positive for salmonella in four additional product samples collected from the retailer Torched Illusions." As of March 15, the FDA said, the Centers for Disease Control and Prevention reported that 87 people had been infected with outbreak strains of salmonella reported from 35 states.*
Dr. Gottlieb had issued a statement a few weeks earlier, in February, saying that the agency was able to confirm that kratom contains opioids. “The extensive scientific data we’ve evaluated about kratom provides conclusive evidence that compounds contained in kratom are opioids and are expected to have similar addictive effects as well as risks of abuse, overdose and, in some cases, death. At the same time, there’s no evidence to indicate that kratom is safe or effective for any medical use,” Dr. Gottlieb wrote. “To protect the public health, we’ll continue to affirm the risks associated with kratom, warn consumers against its use, and take aggressive enforcement action against kratom-containing products.”
For physicians like Dr. Levounis, who treat kratom users in emergency departments, patients should heed those warnings. “People erroneously feel that herbal products are milder than other products,” he said. “Nature can manufacture incredibly strong stuff – for good and for bad.”
*This story was updated 3/23/2018.
Dr. Goldberger, Dr. Levounis, Dr. Grundmann, and Dr. Holcomb had no disclosures. Dr. Galbis-Reig disclosed in his study that he is the owner of stock in GW Pharmaceuticals and Cortex Pharmaceuticals, Pfizer bonds, and has spousal ownership of stock in AbbVie, Abbott Pharma, and Hospira. Dr. Swogger and other authors of the systematic review reported serving as consultants for the American Kratom Association, as well as sponsors of other kratom products.
As the opioid epidemic continues to ravage the United States, patients and physicians are looking for less-addictive alternatives for pain control.
For a growing number of U.S. patients, top among the contenders is kratom, a plant-based product that shows a dose-dependent opioidlike effect. For physicians, toxicologists – and federal regulators, however – the absence of evidence-based studies on the herb’s effectiveness and safety is raising concerns.
“
Petros Levounis, MD, an addiction psychiatrist who has treated kratom users, said an inherent challenge is countering patients’ perceptions about the substance.
“Somehow, in the popular culture, kratom has a reputation as being a mild opioid. And we’re not sure about that,” said Dr. Levounis, a member of the American Academy of Addiction Psychiatry. “But the fact that people think it’s more natural and therefore it must be safer is very problematic.”
The uncertainty around kratom raises the stakes when it comes to treating patients. “From a medical perspective, one of the trickiest issues is we’re not sure that naloxone reverses the opioid effects,” said Dr. Levounis, also chair of psychiatry at Robert Wood Johnson Medical School, New Brunswick. “We do use naloxone, but it is not clear that it works as an antidote. This is probably the most problematic area about kratom.”
Origins, demographics
A member of the coffee family, kratom (Mitragyna speciosa) grows in Thailand, Malaysia, Indonesia, and Papua New Guinea, and has been used throughout southeast Asia for many years to manage pain and bolster energy, according to the National Center for Complementary and Integrative Health.
Dr. Grundmann conducted an anonymous survey last year about kratom and found that most users are white, married or partnered, and employed for wages. Dr. Grundmann’s survey of 8,049 kratom users also found that a majority of users reported having some college. However, the survey found an inverse relationship between years of education and the tendency to use kratom (Drug Alcohol Depend. 2017 Jul 1;176:63-70).
“The more education somebody has, the less likely they are to use kratom for prescription medicine dependency or for an emotional or mental condition,” Dr. Grundmann said.
Anecdotal evidence
One study conducted by David Galbis-Reig, MD, president-elect of the Wisconsin Society of Addiction Medicine, followed a 37-year-old woman who experienced kratom addiction.
“The mitragynine and 7-Hydroxymitragynine very clearly have partial opioid agonist activity with kappa antagonist activity, which is very similar to buprenorphine,” said Dr. Galbis-Reig, who is also with American Society of Addiction Medicine.
A major concern that Dr. Galbis-Reig’s case brings up is the use of liquid kratom extract.
“My biggest concern is we just don’t know what the stimulant properties of the drug are,” Dr. Galbis-Reig said. “If it turns out the properties are more in line with an amphetamine, I’m not sure that’s a great drug to use in a clinical setting for many conditions.”
But Murray A. Holcomb, MD, an acute care surgeon at Seton Healthcare Family Center, Round Rock, Tex., offered a different take. He said he and his family were first highly skeptical when they first heard about kratom. But after years of trying to help his son overcome his depression and substance abuse, Dr. Holcomb said he was ready to try anything.
After researching and consulting with his colleagues, Dr. Holcomb helped his son acquire the plant. What was expected to be another substance that overpromised and underdelivered turned out to be the real thing.
“Out of desperation, [my son] tried kratom, and within a few short days, he began to experience remission of his symptoms – which was immediately noticeable to all of us who knew him,” said Dr. Holcomb. “It is important to note that kratom does not make him high, loopy, or anything but normal. He lives independently, works full time, maintains healthy relationships, is pleasant and responsible, reestablished contact with his sister and brother, and is largely a happy normal person.”
Not only was his son able to return to his normal life, but the costs for his dose of kratom were within his budget while making minimum wage, similar to a majority of users – who make $35,000-$50,000 per year, Dr. Grundmann’s survey results suggest.
For people with substance use disorder, the issue of addiction always is present, Dr. Holcomb believes, and if that is the case, it’s better to be using kratom than another drug,
“If people steer themselves to kratom rather than something else, that’s probably a good thing, because if someone wants to abuse something, you can’t stop them; you can’t regulate intent,“ Dr. Holcomb said. “Kratom is a partial agonist. It doesn’t make you euphorically high, it doesn’t make you quit breathing, and you don’t really have any withdrawal symptoms, and no one is going to overdose on a natural plant – because it will make them sick to their stomach.”
In a systematic review of studies related to kratom use, investigators found that the product “may be useful for analgesia, mood elevation, anxiety reduction, and may aid opioid withdrawal management. Negative themes also emerged, including unfavorable side effects, especially stomach upset and vomiting,” wrote Marc T. Swogger, PhD, and his colleagues (J Psychoactive Drugs. 2015 Nov-Dec;47[5]:360-7).
“As an opioid substitute, it seems to be used in good effect to decrease opioid withdrawal symptoms, including cravings for more opioids,” said Dr. Swogger, clinical psychologist at the University of Rochester (N.Y.). “People are able to use kratom as a way to get through systemic hoops to get the medicine they need.”
The regulatory fight
In 2016, the Drug Enforcement Administration announced its intentions to classify mitragynine and 7-Hydroxymitragynine, the active ingredients in kratom, as a schedule I drug in order to “avoid an imminent hazard to public safety” after two cases of kratom exposure were reported to the American Association for Poison Control Centers, according to a statement released by the DEA.
In November 2017, Scott Gottlieb, MD, commissioner of the Food and Drug Administration, issued a public health advisory reporting that kratom-related calls to U.S. poison control centers soared 10-fold during 2010-2015. It also said that 36 people have died after using products containing kratom. In light of those developments and with the absence of evidence showing that the substance is safe, the agency is taking action, he wrote.
“To fulfill our public health obligations, we have identified kratom products on two import alerts and we are working to actively prevent shipments of kratom from entering the U.S.,” Dr. Gottlieb wrote. “Kratom is already a controlled substance in 16 countries, including 2 of its native countries of origin, Thailand and Malaysia, as well as Australia, Sweden, and Germany. Kratom is also banned in several states, specifically Alabama, Arkansas, Indiana, Tennessee, and Wisconsin, and several others have pending legislation to ban it.”
In December 2017, a group comprising 17 members of Congress responded wrote a letter to Dr. Gottlieb imploring the Trump administration to recognize the merits of the substance and to drop its intention to make it more difficult to procure.
“Given that numerous stakeholders, former opioid addicts, and scientific researchers vouch for kratom’s safety and support its use, and responsible manufacturers of kratom products ensure that their products are properly labeled for adult-only consumption, we respectfully request that the FDA reconsider its stance and take a closer look at the facts and recent science regarding this plant,” the members wrote in the letter. After the letter was received by the FDA, the DEA decided to hold off on its scheduling.
But controversy surrounding the botanical product continues. Earlier this year, the FDA ordered the recall and destruction of kratom-containing dietary supplements made by a company in Grain Valley, Mo., the agency said in a statement. The FDA also is investigating a possible association between kratom intake and an outbreak of salmonella in North Dakota and Utah, in which 17 of 24 patients reported taking products thought to contain kratom before becoming sick, the agency wrote. Meanwhile, in late March, the FDA reported that it was investigating a multistate outbreak of salmonella infections tied to products that were reported to contain kratom. For example, the agency said, it is "reporting four additional products tested by Oregon Health Authority identified as positive for salmonella in four additional product samples collected from the retailer Torched Illusions." As of March 15, the FDA said, the Centers for Disease Control and Prevention reported that 87 people had been infected with outbreak strains of salmonella reported from 35 states.*
Dr. Gottlieb had issued a statement a few weeks earlier, in February, saying that the agency was able to confirm that kratom contains opioids. “The extensive scientific data we’ve evaluated about kratom provides conclusive evidence that compounds contained in kratom are opioids and are expected to have similar addictive effects as well as risks of abuse, overdose and, in some cases, death. At the same time, there’s no evidence to indicate that kratom is safe or effective for any medical use,” Dr. Gottlieb wrote. “To protect the public health, we’ll continue to affirm the risks associated with kratom, warn consumers against its use, and take aggressive enforcement action against kratom-containing products.”
For physicians like Dr. Levounis, who treat kratom users in emergency departments, patients should heed those warnings. “People erroneously feel that herbal products are milder than other products,” he said. “Nature can manufacture incredibly strong stuff – for good and for bad.”
*This story was updated 3/23/2018.
Dr. Goldberger, Dr. Levounis, Dr. Grundmann, and Dr. Holcomb had no disclosures. Dr. Galbis-Reig disclosed in his study that he is the owner of stock in GW Pharmaceuticals and Cortex Pharmaceuticals, Pfizer bonds, and has spousal ownership of stock in AbbVie, Abbott Pharma, and Hospira. Dr. Swogger and other authors of the systematic review reported serving as consultants for the American Kratom Association, as well as sponsors of other kratom products.
What’s in the way of you and new tech?
BOSTON – Bringing new technology to your practice is not as simple as flipping a switch, as attendees of the Thursday afternoon AGA Tech Summit session “Physician Perspective on Barriers to Incorporating New Technology” learned. The Tech Summit is sponsored by the AGA Center for GI Innovation and Technology.
“As physicians think about being a part of taking on new technology, there are varying perspectives, including the perspective they have about their patients and the perspective they have for themselves,” Richard Rothstein, MD, chair of the department of medicine at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. “However, there are other perspectives as well, like the perspectives of the hospital or the ambulatory endoscopy center in which they work.”
He presented an intriguing historical example. Within months of the first demonstration of anesthetized surgery in 1846, the use of ether and the machine to deliver it were spreading rapidly through hospitals in large U.S. cities. European adoption soon followed.
However, decades passed before there was wide acceptance of Lister’s ideas on carbolic acid as a surgical antiseptic.
“Why was one technology adopted early and one later? Incentives to adopt both went in the same direction – improved patient outcomes. Both were based on ideas that violated prior beliefs. Both were technically complex. But one combatted a visible and immediate problem: pain. The other combatted an invisible and unproven problem: germs. Both made life better for the patient – but only one made life better for the surgeon. And that one, anesthesia, was the one that was quickly adopted.”
Even today, clinicians are the main drivers of the adoption of novel medical technology. They fall into two general categories, Dr. Rothstein said: early adopters, who want to be the first to offer an exciting new procedure, and late adopters, who wait for more information and want all the issues of that technology to be sorted out before diving in.
Each one stands in the same circle, however, forced to evaluate the issues that come along with adopting new tech, including training, credentialing and insurance, facility support, and how the new tool or procedure might affect the entire clinical team
Facilities have to tussle with these issues, too, Dr. Rothstein said.
Administrations wonder, “‘Will I get paid for this? Will it displace something else that’s equally effective that could be making more money? What resources do I need to implement it? Will it impact malpractice insurance rates for clinicians who work at my facility?’”
Patient choice also plays into the matter. Third-party payers may or may not have cutting-edge tech on their payment ledger. The specter of a self-pay procedure, no matter how potentially effective, is an enormous deterrent for patients, especially when figuring in the possibility of footing the bill for any associated complications. And of course, new technology and procedures lack the deep pool of efficacy and safety data that established ones lean upon – another potential sticking point for both clinicians and patients, Dr. Rothstein said.
“There are a lot of great ideas out there, and a lot of innovative devices, but without addressing the barriers to adoption, the technology will never get to the targeted goal of delivering better care to our patients,” he said.
BOSTON – Bringing new technology to your practice is not as simple as flipping a switch, as attendees of the Thursday afternoon AGA Tech Summit session “Physician Perspective on Barriers to Incorporating New Technology” learned. The Tech Summit is sponsored by the AGA Center for GI Innovation and Technology.
“As physicians think about being a part of taking on new technology, there are varying perspectives, including the perspective they have about their patients and the perspective they have for themselves,” Richard Rothstein, MD, chair of the department of medicine at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. “However, there are other perspectives as well, like the perspectives of the hospital or the ambulatory endoscopy center in which they work.”
He presented an intriguing historical example. Within months of the first demonstration of anesthetized surgery in 1846, the use of ether and the machine to deliver it were spreading rapidly through hospitals in large U.S. cities. European adoption soon followed.
However, decades passed before there was wide acceptance of Lister’s ideas on carbolic acid as a surgical antiseptic.
“Why was one technology adopted early and one later? Incentives to adopt both went in the same direction – improved patient outcomes. Both were based on ideas that violated prior beliefs. Both were technically complex. But one combatted a visible and immediate problem: pain. The other combatted an invisible and unproven problem: germs. Both made life better for the patient – but only one made life better for the surgeon. And that one, anesthesia, was the one that was quickly adopted.”
Even today, clinicians are the main drivers of the adoption of novel medical technology. They fall into two general categories, Dr. Rothstein said: early adopters, who want to be the first to offer an exciting new procedure, and late adopters, who wait for more information and want all the issues of that technology to be sorted out before diving in.
Each one stands in the same circle, however, forced to evaluate the issues that come along with adopting new tech, including training, credentialing and insurance, facility support, and how the new tool or procedure might affect the entire clinical team
Facilities have to tussle with these issues, too, Dr. Rothstein said.
Administrations wonder, “‘Will I get paid for this? Will it displace something else that’s equally effective that could be making more money? What resources do I need to implement it? Will it impact malpractice insurance rates for clinicians who work at my facility?’”
Patient choice also plays into the matter. Third-party payers may or may not have cutting-edge tech on their payment ledger. The specter of a self-pay procedure, no matter how potentially effective, is an enormous deterrent for patients, especially when figuring in the possibility of footing the bill for any associated complications. And of course, new technology and procedures lack the deep pool of efficacy and safety data that established ones lean upon – another potential sticking point for both clinicians and patients, Dr. Rothstein said.
“There are a lot of great ideas out there, and a lot of innovative devices, but without addressing the barriers to adoption, the technology will never get to the targeted goal of delivering better care to our patients,” he said.
BOSTON – Bringing new technology to your practice is not as simple as flipping a switch, as attendees of the Thursday afternoon AGA Tech Summit session “Physician Perspective on Barriers to Incorporating New Technology” learned. The Tech Summit is sponsored by the AGA Center for GI Innovation and Technology.
“As physicians think about being a part of taking on new technology, there are varying perspectives, including the perspective they have about their patients and the perspective they have for themselves,” Richard Rothstein, MD, chair of the department of medicine at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. “However, there are other perspectives as well, like the perspectives of the hospital or the ambulatory endoscopy center in which they work.”
He presented an intriguing historical example. Within months of the first demonstration of anesthetized surgery in 1846, the use of ether and the machine to deliver it were spreading rapidly through hospitals in large U.S. cities. European adoption soon followed.
However, decades passed before there was wide acceptance of Lister’s ideas on carbolic acid as a surgical antiseptic.
“Why was one technology adopted early and one later? Incentives to adopt both went in the same direction – improved patient outcomes. Both were based on ideas that violated prior beliefs. Both were technically complex. But one combatted a visible and immediate problem: pain. The other combatted an invisible and unproven problem: germs. Both made life better for the patient – but only one made life better for the surgeon. And that one, anesthesia, was the one that was quickly adopted.”
Even today, clinicians are the main drivers of the adoption of novel medical technology. They fall into two general categories, Dr. Rothstein said: early adopters, who want to be the first to offer an exciting new procedure, and late adopters, who wait for more information and want all the issues of that technology to be sorted out before diving in.
Each one stands in the same circle, however, forced to evaluate the issues that come along with adopting new tech, including training, credentialing and insurance, facility support, and how the new tool or procedure might affect the entire clinical team
Facilities have to tussle with these issues, too, Dr. Rothstein said.
Administrations wonder, “‘Will I get paid for this? Will it displace something else that’s equally effective that could be making more money? What resources do I need to implement it? Will it impact malpractice insurance rates for clinicians who work at my facility?’”
Patient choice also plays into the matter. Third-party payers may or may not have cutting-edge tech on their payment ledger. The specter of a self-pay procedure, no matter how potentially effective, is an enormous deterrent for patients, especially when figuring in the possibility of footing the bill for any associated complications. And of course, new technology and procedures lack the deep pool of efficacy and safety data that established ones lean upon – another potential sticking point for both clinicians and patients, Dr. Rothstein said.
“There are a lot of great ideas out there, and a lot of innovative devices, but without addressing the barriers to adoption, the technology will never get to the targeted goal of delivering better care to our patients,” he said.
REPORTING FROM 2018 AGA TECH SUMMIT
Interleukin-1 antagonist boosts testosterone in obese men
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The treatment helps patients by targeting testosterone deficiency associated with metabolic syndrome as well as inflammation associated with hypogonadism.
“Antagonism of the interleukin inflammatory pathway led to improved endogenous testosterone production,” said presenter Fahim Ebrahimi, MD, of the University Hospital Basel, Switzerland. “Even with a clinical period so short, only 4 weeks, we have seen reduced blood pressure and increased grip strength.”
A total of 70 men with metabolic syndrome and hypergonadism from the University Hospital in Basel and Kantonsspital Aarau, Switzerland, were included in the randomized, double-blind, placebo-controlled study.
Patients were mostly white, 54-year-old men with an average body mass index of 37 kg/m2.
Testosterone levels at baseline were an average of 9.6 nmol/L in the placebo group and 9.1 nmol/L in the test group.
Dr. Ebrahimi and his colleagues randomly assigned patients to either the IL-1 antagonist treatment anakinra, or a placebo for 4 weeks.
Total testosterone levels in the treatment group rose 11% over 4 weeks, ending the trial with an average level 0.96 nmol/L higher than the placebo group, according to the investigators.
Evidence of the positive effects of the anti-inflammatory were clear when patients were broken into subgroups based on baseline inflammation levels.
Patients who did not have baseline inflammation did not respond to treatment, while patients with a baseline CRP level higher than 2 mg/l had an increase of 2.14 nmol/L, explained Dr. Ebrahimi.
Treatment response also increased with increased body mass index, with patients who had a BMI above 40 kg/m2 seeing testosterone levels improve by 2.64 nmol/L.
Along with higher testosterone, patients in the test group experienced improved grip strength and blood pressure.
Investigators chose targeting IL-1 receptor antagonist specifically because of previous successes with other conditions.
“We chose IL-1 because it has shown previous, very beneficial effects on glucose metabolism, with reductions of A1c, and is well tolerated,” Dr. Ebrahimi said in response to a question from the audience.
Dr. Ebrahimi and fellow investigators believe this study will help open the door on unanswered questions related to the cardiovascular safety of this kind of treatment.
“These data will have a clinical impact, especially against the background of the recently published data from the large randomized trial, which has shown that IL-1 antagonism in these patients lead to a significant reduction in cardiovascular mortality,” Dr. Ebrahimi said. “We also still do not know if this treatment is possibly harmful to the patient on cardiovascular outcomes.”
The investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Ebrahimi F. et al. ENDO 2018, Abstract OR15-6.
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The treatment helps patients by targeting testosterone deficiency associated with metabolic syndrome as well as inflammation associated with hypogonadism.
“Antagonism of the interleukin inflammatory pathway led to improved endogenous testosterone production,” said presenter Fahim Ebrahimi, MD, of the University Hospital Basel, Switzerland. “Even with a clinical period so short, only 4 weeks, we have seen reduced blood pressure and increased grip strength.”
A total of 70 men with metabolic syndrome and hypergonadism from the University Hospital in Basel and Kantonsspital Aarau, Switzerland, were included in the randomized, double-blind, placebo-controlled study.
Patients were mostly white, 54-year-old men with an average body mass index of 37 kg/m2.
Testosterone levels at baseline were an average of 9.6 nmol/L in the placebo group and 9.1 nmol/L in the test group.
Dr. Ebrahimi and his colleagues randomly assigned patients to either the IL-1 antagonist treatment anakinra, or a placebo for 4 weeks.
Total testosterone levels in the treatment group rose 11% over 4 weeks, ending the trial with an average level 0.96 nmol/L higher than the placebo group, according to the investigators.
Evidence of the positive effects of the anti-inflammatory were clear when patients were broken into subgroups based on baseline inflammation levels.
Patients who did not have baseline inflammation did not respond to treatment, while patients with a baseline CRP level higher than 2 mg/l had an increase of 2.14 nmol/L, explained Dr. Ebrahimi.
Treatment response also increased with increased body mass index, with patients who had a BMI above 40 kg/m2 seeing testosterone levels improve by 2.64 nmol/L.
Along with higher testosterone, patients in the test group experienced improved grip strength and blood pressure.
Investigators chose targeting IL-1 receptor antagonist specifically because of previous successes with other conditions.
“We chose IL-1 because it has shown previous, very beneficial effects on glucose metabolism, with reductions of A1c, and is well tolerated,” Dr. Ebrahimi said in response to a question from the audience.
Dr. Ebrahimi and fellow investigators believe this study will help open the door on unanswered questions related to the cardiovascular safety of this kind of treatment.
“These data will have a clinical impact, especially against the background of the recently published data from the large randomized trial, which has shown that IL-1 antagonism in these patients lead to a significant reduction in cardiovascular mortality,” Dr. Ebrahimi said. “We also still do not know if this treatment is possibly harmful to the patient on cardiovascular outcomes.”
The investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Ebrahimi F. et al. ENDO 2018, Abstract OR15-6.
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The treatment helps patients by targeting testosterone deficiency associated with metabolic syndrome as well as inflammation associated with hypogonadism.
“Antagonism of the interleukin inflammatory pathway led to improved endogenous testosterone production,” said presenter Fahim Ebrahimi, MD, of the University Hospital Basel, Switzerland. “Even with a clinical period so short, only 4 weeks, we have seen reduced blood pressure and increased grip strength.”
A total of 70 men with metabolic syndrome and hypergonadism from the University Hospital in Basel and Kantonsspital Aarau, Switzerland, were included in the randomized, double-blind, placebo-controlled study.
Patients were mostly white, 54-year-old men with an average body mass index of 37 kg/m2.
Testosterone levels at baseline were an average of 9.6 nmol/L in the placebo group and 9.1 nmol/L in the test group.
Dr. Ebrahimi and his colleagues randomly assigned patients to either the IL-1 antagonist treatment anakinra, or a placebo for 4 weeks.
Total testosterone levels in the treatment group rose 11% over 4 weeks, ending the trial with an average level 0.96 nmol/L higher than the placebo group, according to the investigators.
Evidence of the positive effects of the anti-inflammatory were clear when patients were broken into subgroups based on baseline inflammation levels.
Patients who did not have baseline inflammation did not respond to treatment, while patients with a baseline CRP level higher than 2 mg/l had an increase of 2.14 nmol/L, explained Dr. Ebrahimi.
Treatment response also increased with increased body mass index, with patients who had a BMI above 40 kg/m2 seeing testosterone levels improve by 2.64 nmol/L.
Along with higher testosterone, patients in the test group experienced improved grip strength and blood pressure.
Investigators chose targeting IL-1 receptor antagonist specifically because of previous successes with other conditions.
“We chose IL-1 because it has shown previous, very beneficial effects on glucose metabolism, with reductions of A1c, and is well tolerated,” Dr. Ebrahimi said in response to a question from the audience.
Dr. Ebrahimi and fellow investigators believe this study will help open the door on unanswered questions related to the cardiovascular safety of this kind of treatment.
“These data will have a clinical impact, especially against the background of the recently published data from the large randomized trial, which has shown that IL-1 antagonism in these patients lead to a significant reduction in cardiovascular mortality,” Dr. Ebrahimi said. “We also still do not know if this treatment is possibly harmful to the patient on cardiovascular outcomes.”
The investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Ebrahimi F. et al. ENDO 2018, Abstract OR15-6.
REPORTING FROM ENDO 2018
Key clinical point: IL-1 receptor antagonist improved testosterone production for obese hypergonadal men.
Major finding: Total testosterone levels increased by 1.2 nmol/L (95% confidence interval, 0.3-2; P = .012) in treatment group, compared with no change in placebo after 4 weeks.
Study details: Randomized, placebo-controlled trial of 70 male obese patients gathered from the University Hospital Basel and Kantonsspital Aarau, Switzerland.
Disclosures: The investigators reported no relevant financial disclosures.
Source: Ebrahimi F et al. ENDO 2018, Abstract OR15-6.