User login
The 2014-2015 Influenza Season: What You Need to Know
As clinicians and the CDC prepare for the upcoming influenza season, many of the immunization recommendations remain unchanged from last season. Vaccination continues to be recommended for everyone ages 6 months and older. However, for the first time, a specific vaccine is preferred for children ages 2 through 8 years. Here’s what you need to know about this change, as well as how to handle vaccination in patients who are, or might be, allergic to eggs.
USE LAIV FOR KIDS AGES 2 THROUGH 8 (IF AVAILABLE)
For the first time, the CDC’s Advisory Committee on Immunization Practices (ACIP) has stated a preference for a specific influenza vaccine for a specific age-group. It recommends using the live attenuated influenza vaccine (LAIV), which is a nasal spray, for children ages 2 through 8 years.1
A systematic review found evidence of increased efficacy of LAIV compared to inactivated influenza vaccine (IIV) in this age-group; both types of vaccine have similar rates of adverse reactions.2 This increased effectiveness results in 46 fewer cases of confirmed influenza per 1,000 children vaccinated (number needed to treat, 24). Although the evidence of LAIV’s increased effectiveness was found for children ages 2 to 6 years, ACIP extended this recommendation through age 8 because this is the age through which clinicians need to consider two doses of vaccine for a child previously unvaccinated with the influenza vaccine. Children younger than 2 should receive IIV3 or IIV4.3
ACIP realizes that due to programmatic constraints it would be difficult to vaccinate all children with LAIV this year; the committee emphasizes that this recommendation should be implemented when feasible this year but no later than the 2015-2016 influenza season. IIV is effective in children and should be given if LAIV is not available or is contraindicated. Vaccination should not be delayed in the hopes of receiving a supply of LAIV if IIV is available.1
LAIV should not be used in children younger than 2 or adults older than 49. This vaccine is contraindicated in children and adolescents who are taking chronic aspirin therapy, pregnant women, or persons who are immunosuppressed, have a history of egg allergy, or have taken influenza antiviral medications in the past 48 hours.1 LAIV also is not recommended for children ages 2 through 4 years who have asthma or have had a wheezing episode in the past 12 months.1
There are precautions for the use of LAIV in patients with chronic medical conditions that can place them at high risk for complications from influenza. These include chronic lung, heart, renal, neurologic, liver, blood, or metabolic disorders—particularly, asthma and diabetes.1
WHICH VACCINE FOR PATIENTS WHO ARE ALLERGIC TO EGGS?
Two influenza vaccines are now available that are not prepared in embryonated eggs: recombinant influenza vaccine (RIV3) and cell culture–based inactivated influenza vaccine (ccIIV3). Both are trivalent products that contain antigens from two influenza A viruses and one influenza B virus; they were introduced in time for the 2013-2014 flu season. The RIV3 is considered egg-free but ccIIV3 is not, although the amount of egg protein in the latter is miniscule (estimated at 5 × 10-8 mg/0.5 mL dose).1 Neither product is licensed for use in children younger than 18, and RIV3 is licensed only for those ages 18 through 49.
Patients who experience only hives after egg exposure can receive any of the flu vaccines except LAIV—and only because of a lack of data on this product, not because it has been shown to be less safe than the other vaccines. Patients who are unsure if they have an egg allergy or who only get hives when they eat eggs should be observed for at least 30 minutes1 following injection as a precaution. Those ages 18 through 49 who have a history of severe reactions to eggs should receive RIV3. Patients younger than 18 and older than 49 can receive IIV vaccines approved for their specific age-group.
Any patient who is severely allergic but who cannot receive an egg-free vaccine should be vaccinated by a clinician with experience managing severe allergic conditions. Although severe anaphylactic reactions to influenza vaccine are very rare, clinicians should be equipped and prepared to respond to a severe allergic reaction after providing influenza vaccine to anyone with a history of egg allergy.
Continue for additional tips and resources >>
ADDITIONAL TIPS AND RESOURCES
In addition to the LAIV, RIV3, and ccIIV3 vaccines described here, 10 other vaccines are available: five egg-based IIV3 products in standard-dose form, one IIV3 vaccine for intradermal use, one high-dose IIV3 product for patients ages 65 or older, and three standard-dose IIV4 products. More details on each of these vaccines are available on the CDC website (www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?s_cid=rr6207a1_w#Tab1).
Regardless of which type of flu vaccine they receive, children ages 6 months through 8 years should receive two doses, at least four weeks apart, unless they received
• One dose during the 2013-2014 season, or
• Two or more doses of seasonal influenza vaccine since July 2010, or
• Two or more doses of seasonal influenza vaccine before July 2010 and at least one dose of monovalent H1N1 vaccine, or
• At least one dose of seasonal influenza vaccine prior to July 2010 and one or more after.
Vaccine effectiveness. The CDC estimated that vaccine effectiveness during the 2013-2014 flu season was 66%.3 While this degree of effectiveness is important for minimizing morbidity and mortality from influenza each year, it’s important to appreciate the limitations of the vaccine and not rely on it as the only preventive intervention.
Other forms of prevention. We need to advise and practice good respiratory hygiene, frequent hand washing, self-isolation when sick, effective infection control practices at health care facilities, targeted early treatment with antivirals, and targeted pre- and postexposure antiviral chemoprevention. Details on each of these interventions, including recommendations on the use of antiviral medications, can be found on the CDC website (www.cdc.gov/flu).
REFERENCES
1. Grohskopf LA, Olsen SJ, Sokolow LZ, et al; Influenza Division, National Center for Immunization and Respiratory Diseases, CDC. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States 2014-2015 influenza season. MMWR Morb Mortal Wkly Rep. 2014;63: 691-697.
2. Grohskopf L, Olsen S, Sokolow L. Effectiveness of live-attenuated vs inactivated influenza vaccines for healthy children. Presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/05-Flu-Grohskopf.pdf. Accessed October 19, 2014.
3. Flannery B. Interim estimates of 2013-14 seasonal influenza vaccine effectiveness. Presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/04-Flu-Flannery.pdf. Accessed October 19, 2014.
As clinicians and the CDC prepare for the upcoming influenza season, many of the immunization recommendations remain unchanged from last season. Vaccination continues to be recommended for everyone ages 6 months and older. However, for the first time, a specific vaccine is preferred for children ages 2 through 8 years. Here’s what you need to know about this change, as well as how to handle vaccination in patients who are, or might be, allergic to eggs.
USE LAIV FOR KIDS AGES 2 THROUGH 8 (IF AVAILABLE)
For the first time, the CDC’s Advisory Committee on Immunization Practices (ACIP) has stated a preference for a specific influenza vaccine for a specific age-group. It recommends using the live attenuated influenza vaccine (LAIV), which is a nasal spray, for children ages 2 through 8 years.1
A systematic review found evidence of increased efficacy of LAIV compared to inactivated influenza vaccine (IIV) in this age-group; both types of vaccine have similar rates of adverse reactions.2 This increased effectiveness results in 46 fewer cases of confirmed influenza per 1,000 children vaccinated (number needed to treat, 24). Although the evidence of LAIV’s increased effectiveness was found for children ages 2 to 6 years, ACIP extended this recommendation through age 8 because this is the age through which clinicians need to consider two doses of vaccine for a child previously unvaccinated with the influenza vaccine. Children younger than 2 should receive IIV3 or IIV4.3
ACIP realizes that due to programmatic constraints it would be difficult to vaccinate all children with LAIV this year; the committee emphasizes that this recommendation should be implemented when feasible this year but no later than the 2015-2016 influenza season. IIV is effective in children and should be given if LAIV is not available or is contraindicated. Vaccination should not be delayed in the hopes of receiving a supply of LAIV if IIV is available.1
LAIV should not be used in children younger than 2 or adults older than 49. This vaccine is contraindicated in children and adolescents who are taking chronic aspirin therapy, pregnant women, or persons who are immunosuppressed, have a history of egg allergy, or have taken influenza antiviral medications in the past 48 hours.1 LAIV also is not recommended for children ages 2 through 4 years who have asthma or have had a wheezing episode in the past 12 months.1
There are precautions for the use of LAIV in patients with chronic medical conditions that can place them at high risk for complications from influenza. These include chronic lung, heart, renal, neurologic, liver, blood, or metabolic disorders—particularly, asthma and diabetes.1
WHICH VACCINE FOR PATIENTS WHO ARE ALLERGIC TO EGGS?
Two influenza vaccines are now available that are not prepared in embryonated eggs: recombinant influenza vaccine (RIV3) and cell culture–based inactivated influenza vaccine (ccIIV3). Both are trivalent products that contain antigens from two influenza A viruses and one influenza B virus; they were introduced in time for the 2013-2014 flu season. The RIV3 is considered egg-free but ccIIV3 is not, although the amount of egg protein in the latter is miniscule (estimated at 5 × 10-8 mg/0.5 mL dose).1 Neither product is licensed for use in children younger than 18, and RIV3 is licensed only for those ages 18 through 49.
Patients who experience only hives after egg exposure can receive any of the flu vaccines except LAIV—and only because of a lack of data on this product, not because it has been shown to be less safe than the other vaccines. Patients who are unsure if they have an egg allergy or who only get hives when they eat eggs should be observed for at least 30 minutes1 following injection as a precaution. Those ages 18 through 49 who have a history of severe reactions to eggs should receive RIV3. Patients younger than 18 and older than 49 can receive IIV vaccines approved for their specific age-group.
Any patient who is severely allergic but who cannot receive an egg-free vaccine should be vaccinated by a clinician with experience managing severe allergic conditions. Although severe anaphylactic reactions to influenza vaccine are very rare, clinicians should be equipped and prepared to respond to a severe allergic reaction after providing influenza vaccine to anyone with a history of egg allergy.
Continue for additional tips and resources >>
ADDITIONAL TIPS AND RESOURCES
In addition to the LAIV, RIV3, and ccIIV3 vaccines described here, 10 other vaccines are available: five egg-based IIV3 products in standard-dose form, one IIV3 vaccine for intradermal use, one high-dose IIV3 product for patients ages 65 or older, and three standard-dose IIV4 products. More details on each of these vaccines are available on the CDC website (www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?s_cid=rr6207a1_w#Tab1).
Regardless of which type of flu vaccine they receive, children ages 6 months through 8 years should receive two doses, at least four weeks apart, unless they received
• One dose during the 2013-2014 season, or
• Two or more doses of seasonal influenza vaccine since July 2010, or
• Two or more doses of seasonal influenza vaccine before July 2010 and at least one dose of monovalent H1N1 vaccine, or
• At least one dose of seasonal influenza vaccine prior to July 2010 and one or more after.
Vaccine effectiveness. The CDC estimated that vaccine effectiveness during the 2013-2014 flu season was 66%.3 While this degree of effectiveness is important for minimizing morbidity and mortality from influenza each year, it’s important to appreciate the limitations of the vaccine and not rely on it as the only preventive intervention.
Other forms of prevention. We need to advise and practice good respiratory hygiene, frequent hand washing, self-isolation when sick, effective infection control practices at health care facilities, targeted early treatment with antivirals, and targeted pre- and postexposure antiviral chemoprevention. Details on each of these interventions, including recommendations on the use of antiviral medications, can be found on the CDC website (www.cdc.gov/flu).
REFERENCES
1. Grohskopf LA, Olsen SJ, Sokolow LZ, et al; Influenza Division, National Center for Immunization and Respiratory Diseases, CDC. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States 2014-2015 influenza season. MMWR Morb Mortal Wkly Rep. 2014;63: 691-697.
2. Grohskopf L, Olsen S, Sokolow L. Effectiveness of live-attenuated vs inactivated influenza vaccines for healthy children. Presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/05-Flu-Grohskopf.pdf. Accessed October 19, 2014.
3. Flannery B. Interim estimates of 2013-14 seasonal influenza vaccine effectiveness. Presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/04-Flu-Flannery.pdf. Accessed October 19, 2014.
As clinicians and the CDC prepare for the upcoming influenza season, many of the immunization recommendations remain unchanged from last season. Vaccination continues to be recommended for everyone ages 6 months and older. However, for the first time, a specific vaccine is preferred for children ages 2 through 8 years. Here’s what you need to know about this change, as well as how to handle vaccination in patients who are, or might be, allergic to eggs.
USE LAIV FOR KIDS AGES 2 THROUGH 8 (IF AVAILABLE)
For the first time, the CDC’s Advisory Committee on Immunization Practices (ACIP) has stated a preference for a specific influenza vaccine for a specific age-group. It recommends using the live attenuated influenza vaccine (LAIV), which is a nasal spray, for children ages 2 through 8 years.1
A systematic review found evidence of increased efficacy of LAIV compared to inactivated influenza vaccine (IIV) in this age-group; both types of vaccine have similar rates of adverse reactions.2 This increased effectiveness results in 46 fewer cases of confirmed influenza per 1,000 children vaccinated (number needed to treat, 24). Although the evidence of LAIV’s increased effectiveness was found for children ages 2 to 6 years, ACIP extended this recommendation through age 8 because this is the age through which clinicians need to consider two doses of vaccine for a child previously unvaccinated with the influenza vaccine. Children younger than 2 should receive IIV3 or IIV4.3
ACIP realizes that due to programmatic constraints it would be difficult to vaccinate all children with LAIV this year; the committee emphasizes that this recommendation should be implemented when feasible this year but no later than the 2015-2016 influenza season. IIV is effective in children and should be given if LAIV is not available or is contraindicated. Vaccination should not be delayed in the hopes of receiving a supply of LAIV if IIV is available.1
LAIV should not be used in children younger than 2 or adults older than 49. This vaccine is contraindicated in children and adolescents who are taking chronic aspirin therapy, pregnant women, or persons who are immunosuppressed, have a history of egg allergy, or have taken influenza antiviral medications in the past 48 hours.1 LAIV also is not recommended for children ages 2 through 4 years who have asthma or have had a wheezing episode in the past 12 months.1
There are precautions for the use of LAIV in patients with chronic medical conditions that can place them at high risk for complications from influenza. These include chronic lung, heart, renal, neurologic, liver, blood, or metabolic disorders—particularly, asthma and diabetes.1
WHICH VACCINE FOR PATIENTS WHO ARE ALLERGIC TO EGGS?
Two influenza vaccines are now available that are not prepared in embryonated eggs: recombinant influenza vaccine (RIV3) and cell culture–based inactivated influenza vaccine (ccIIV3). Both are trivalent products that contain antigens from two influenza A viruses and one influenza B virus; they were introduced in time for the 2013-2014 flu season. The RIV3 is considered egg-free but ccIIV3 is not, although the amount of egg protein in the latter is miniscule (estimated at 5 × 10-8 mg/0.5 mL dose).1 Neither product is licensed for use in children younger than 18, and RIV3 is licensed only for those ages 18 through 49.
Patients who experience only hives after egg exposure can receive any of the flu vaccines except LAIV—and only because of a lack of data on this product, not because it has been shown to be less safe than the other vaccines. Patients who are unsure if they have an egg allergy or who only get hives when they eat eggs should be observed for at least 30 minutes1 following injection as a precaution. Those ages 18 through 49 who have a history of severe reactions to eggs should receive RIV3. Patients younger than 18 and older than 49 can receive IIV vaccines approved for their specific age-group.
Any patient who is severely allergic but who cannot receive an egg-free vaccine should be vaccinated by a clinician with experience managing severe allergic conditions. Although severe anaphylactic reactions to influenza vaccine are very rare, clinicians should be equipped and prepared to respond to a severe allergic reaction after providing influenza vaccine to anyone with a history of egg allergy.
Continue for additional tips and resources >>
ADDITIONAL TIPS AND RESOURCES
In addition to the LAIV, RIV3, and ccIIV3 vaccines described here, 10 other vaccines are available: five egg-based IIV3 products in standard-dose form, one IIV3 vaccine for intradermal use, one high-dose IIV3 product for patients ages 65 or older, and three standard-dose IIV4 products. More details on each of these vaccines are available on the CDC website (www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?s_cid=rr6207a1_w#Tab1).
Regardless of which type of flu vaccine they receive, children ages 6 months through 8 years should receive two doses, at least four weeks apart, unless they received
• One dose during the 2013-2014 season, or
• Two or more doses of seasonal influenza vaccine since July 2010, or
• Two or more doses of seasonal influenza vaccine before July 2010 and at least one dose of monovalent H1N1 vaccine, or
• At least one dose of seasonal influenza vaccine prior to July 2010 and one or more after.
Vaccine effectiveness. The CDC estimated that vaccine effectiveness during the 2013-2014 flu season was 66%.3 While this degree of effectiveness is important for minimizing morbidity and mortality from influenza each year, it’s important to appreciate the limitations of the vaccine and not rely on it as the only preventive intervention.
Other forms of prevention. We need to advise and practice good respiratory hygiene, frequent hand washing, self-isolation when sick, effective infection control practices at health care facilities, targeted early treatment with antivirals, and targeted pre- and postexposure antiviral chemoprevention. Details on each of these interventions, including recommendations on the use of antiviral medications, can be found on the CDC website (www.cdc.gov/flu).
REFERENCES
1. Grohskopf LA, Olsen SJ, Sokolow LZ, et al; Influenza Division, National Center for Immunization and Respiratory Diseases, CDC. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States 2014-2015 influenza season. MMWR Morb Mortal Wkly Rep. 2014;63: 691-697.
2. Grohskopf L, Olsen S, Sokolow L. Effectiveness of live-attenuated vs inactivated influenza vaccines for healthy children. Presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/05-Flu-Grohskopf.pdf. Accessed October 19, 2014.
3. Flannery B. Interim estimates of 2013-14 seasonal influenza vaccine effectiveness. Presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/04-Flu-Flannery.pdf. Accessed October 19, 2014.
Ebola: The facts FPs need to know
The 2014-2015 influenza season: What you need to know
As physicians and the Centers for Disease Control and Prevention (CDC) prepare for the upcoming influenza season, many of the recommendations remain unchanged from last season. Vaccination continues to be recommended for everyone 6 months of age and older. However, for the first time, a specific vaccine is preferred for children ages 2 through 8 years. Here’s what you need to know about this change, as well as how to handle vaccination in patients who are, or might be, allergic to eggs.
Use LAIV for kids ages 2 through 8 (if available)
For the first time, the CDC’s Advisory Committee on Immunization Practices (ACIP) has stated a preference for a specific influenza vaccine for a specific age group. It recommends using the live attenuated influenza vaccine (LAIV), which is a nasal spray, for children ages 2 through 8 years.1
A systematic review found evidence of increased efficacy of LAIV compared to inactivated influenza vaccine (IIV) in this age group; both types of vaccine have similar rates of adverse reactions.2 This increased effectiveness results in 46 fewer cases of confirmed influenza per 1000 children vaccinated (number needed to treat=24). Although the evidence of LAIV’s increased effectiveness was found for children ages 2 to 6 years, ACIP extended this recommendation through age 8 because this is the age through which physicians need to consider 2 doses of vaccine for a child previously unvaccinated with the influenza vaccine. Children younger than age 2 should receive IIV3 or IIV4.3
ACIP realizes that due to programmatic constraints it would be difficult to vaccinate all children with LAIV this year and is emphasizing that it should be implemented when feasible this year but no later than the 2015 to 2016 influenza season. IIV is effective in children and should be given if LAIV is not available or is contraindicated. Vaccine should not be delayed in the hopes of receiving LAIV if IIV is available.1
LAIV should not be used in children <2 years or adults >49. This vaccine is contraindicated in children and adolescents who are taking chronic aspirin therapy, pregnant women, those who are immunosuppressed, those with a history of egg allergy, or those who have taken influenza antiviral medications in the past 48 hours.1 LAIV also is not recommended for children ages 2 through 4 years who have asthma or had a wheezing episode in the past 12 months.1
There are precautions for the use of LAIV in patients with chronic medical conditions that can place them at high risk for complications from influenza, such as chronic lung, heart, renal, neurologic, liver, blood, or metabolic disorders, including asthma and diabetes.1
Which vaccine for patients who are allergic to eggs?
Two influenza vaccines are now available that are not prepared in embryonated eggs: recombinant influenza vaccine (RIV3) and cell culture-based inactivated influenza vaccine (ccIIV3). Both are trivalent products that contain antigens from 2 influenza A viruses and one influenza B virus and were introduced in time for the 2013 to 2014 flu season. The RIV3 is considered egg-free but ccIIV3 is not, although the amount of egg protein in it is miniscule, estimated at 5 × 10-8 mcg/0.5 mL dose.1 Neither product is licensed for children younger than 18 years and RIV3 is licensed only for those ages 18 through 49 years.
Patients who experience only hives after egg exposure can receive any of the flu vaccines except LAIV, and only because of a lack of data on this product, not because it has been shown to be less safe than the other vaccines. Patients who are unsure if they have an egg allergy or only get hives when they eat eggs should be observed for at least 30 minutes1 following injection as a precaution. Those ages 18 through 49 who have a history of severe reactions to eggs should receive RIV3. Patients younger than 18 years of age and older than 49 years of age can receive IIV vaccines approved for their specific age group. Any patient who is severely allergic and who cannot receive an egg-free vaccine should be vaccinated by a physician with experience managing severe allergic conditions.
Although severe, anaphylactic reactions to influenza vaccine are very rare, physicians should be equipped and prepared to respond to a severe allergic reaction after providing influenza vaccine to anyone with a history of an egg allergy.
Additional tips and resources
In addition to the LAIV, RIV3, and ccIIV3 vaccines described here, 10 other vaccines are available, including 5 egg-based IIV3 products in standard-dose form, 1 IIV3 vaccine for intradermal use, 1 high-dose IIV3 product for patients ages 65 or older, and 3 standard-dose IIV4 products. More details on each of these vaccines are available at http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?_%20cid=rr6207a1_w#Tab1.
Regardless of which type of flu vaccine they receive, children 6 months through 8 years should receive 2 doses, at least 4 weeks apart, unless they received:
- 1 dose in 2013 to 2014, or
- 2 or more doses of seasonal influenza vaccine since July 2010, or
- 2 or more doses of seasonal influenza vaccine before July 2010 and ≥1 dose of monovalent H1N1 vaccine, or
- at least 1 dose of seasonal influenza vaccine prior to July 2010 and ≥1 after.
Vaccine effectiveness. The CDC estimated that vaccine effectiveness during the 2013 to 2014 flu season was 66%.3 While this degree of effectiveness is important for minimizing the morbidity and mortality from influenza each year, it’s important to appreciate the limitations of the vaccine and not rely on it as the only prevention intervention.
Other forms of prevention. We need to advise and practice good respiratory hygiene, frequent hand washing, self-isolation when sick, effective infection control practices at health care facilities, targeted early treatment with antivirals, and targeted pre- and post-exposure antiviral chemoprevention. Details on each of these interventions, including recommendations on the use of antiviral medications, can be found on the CDC Web site at http://www.cdc.gov/flu.
1. Grohskopf LA, Olsen SJ, Sokolow LZ, et al; Influenza Division, National Center for Immunization and Respiratory Diseases, CDC. Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States 2014-2015 influenza season. MMWR Morb Mortal Wkly Rep. 2014;63:691-697.
2. Grohskopf L, Olsen S, Sokolow L. Effectiveness of live-attenuated vs inactivated influenza vaccines for healthy children. PowerPoint presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/05-Flu-Grohskopf.pdf. Accessed August 6, 2014.
3. Flannery B. Interim estimates of 2013-14 seasonal influenza vaccine effectiveness. PowerPoint presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/04-Flu-Flannery.pdf. Accessed August 6, 2014.
As physicians and the Centers for Disease Control and Prevention (CDC) prepare for the upcoming influenza season, many of the recommendations remain unchanged from last season. Vaccination continues to be recommended for everyone 6 months of age and older. However, for the first time, a specific vaccine is preferred for children ages 2 through 8 years. Here’s what you need to know about this change, as well as how to handle vaccination in patients who are, or might be, allergic to eggs.
Use LAIV for kids ages 2 through 8 (if available)
For the first time, the CDC’s Advisory Committee on Immunization Practices (ACIP) has stated a preference for a specific influenza vaccine for a specific age group. It recommends using the live attenuated influenza vaccine (LAIV), which is a nasal spray, for children ages 2 through 8 years.1
A systematic review found evidence of increased efficacy of LAIV compared to inactivated influenza vaccine (IIV) in this age group; both types of vaccine have similar rates of adverse reactions.2 This increased effectiveness results in 46 fewer cases of confirmed influenza per 1000 children vaccinated (number needed to treat=24). Although the evidence of LAIV’s increased effectiveness was found for children ages 2 to 6 years, ACIP extended this recommendation through age 8 because this is the age through which physicians need to consider 2 doses of vaccine for a child previously unvaccinated with the influenza vaccine. Children younger than age 2 should receive IIV3 or IIV4.3
ACIP realizes that due to programmatic constraints it would be difficult to vaccinate all children with LAIV this year and is emphasizing that it should be implemented when feasible this year but no later than the 2015 to 2016 influenza season. IIV is effective in children and should be given if LAIV is not available or is contraindicated. Vaccine should not be delayed in the hopes of receiving LAIV if IIV is available.1
LAIV should not be used in children <2 years or adults >49. This vaccine is contraindicated in children and adolescents who are taking chronic aspirin therapy, pregnant women, those who are immunosuppressed, those with a history of egg allergy, or those who have taken influenza antiviral medications in the past 48 hours.1 LAIV also is not recommended for children ages 2 through 4 years who have asthma or had a wheezing episode in the past 12 months.1
There are precautions for the use of LAIV in patients with chronic medical conditions that can place them at high risk for complications from influenza, such as chronic lung, heart, renal, neurologic, liver, blood, or metabolic disorders, including asthma and diabetes.1
Which vaccine for patients who are allergic to eggs?
Two influenza vaccines are now available that are not prepared in embryonated eggs: recombinant influenza vaccine (RIV3) and cell culture-based inactivated influenza vaccine (ccIIV3). Both are trivalent products that contain antigens from 2 influenza A viruses and one influenza B virus and were introduced in time for the 2013 to 2014 flu season. The RIV3 is considered egg-free but ccIIV3 is not, although the amount of egg protein in it is miniscule, estimated at 5 × 10-8 mcg/0.5 mL dose.1 Neither product is licensed for children younger than 18 years and RIV3 is licensed only for those ages 18 through 49 years.
Patients who experience only hives after egg exposure can receive any of the flu vaccines except LAIV, and only because of a lack of data on this product, not because it has been shown to be less safe than the other vaccines. Patients who are unsure if they have an egg allergy or only get hives when they eat eggs should be observed for at least 30 minutes1 following injection as a precaution. Those ages 18 through 49 who have a history of severe reactions to eggs should receive RIV3. Patients younger than 18 years of age and older than 49 years of age can receive IIV vaccines approved for their specific age group. Any patient who is severely allergic and who cannot receive an egg-free vaccine should be vaccinated by a physician with experience managing severe allergic conditions.
Although severe, anaphylactic reactions to influenza vaccine are very rare, physicians should be equipped and prepared to respond to a severe allergic reaction after providing influenza vaccine to anyone with a history of an egg allergy.
Additional tips and resources
In addition to the LAIV, RIV3, and ccIIV3 vaccines described here, 10 other vaccines are available, including 5 egg-based IIV3 products in standard-dose form, 1 IIV3 vaccine for intradermal use, 1 high-dose IIV3 product for patients ages 65 or older, and 3 standard-dose IIV4 products. More details on each of these vaccines are available at http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?_%20cid=rr6207a1_w#Tab1.
Regardless of which type of flu vaccine they receive, children 6 months through 8 years should receive 2 doses, at least 4 weeks apart, unless they received:
- 1 dose in 2013 to 2014, or
- 2 or more doses of seasonal influenza vaccine since July 2010, or
- 2 or more doses of seasonal influenza vaccine before July 2010 and ≥1 dose of monovalent H1N1 vaccine, or
- at least 1 dose of seasonal influenza vaccine prior to July 2010 and ≥1 after.
Vaccine effectiveness. The CDC estimated that vaccine effectiveness during the 2013 to 2014 flu season was 66%.3 While this degree of effectiveness is important for minimizing the morbidity and mortality from influenza each year, it’s important to appreciate the limitations of the vaccine and not rely on it as the only prevention intervention.
Other forms of prevention. We need to advise and practice good respiratory hygiene, frequent hand washing, self-isolation when sick, effective infection control practices at health care facilities, targeted early treatment with antivirals, and targeted pre- and post-exposure antiviral chemoprevention. Details on each of these interventions, including recommendations on the use of antiviral medications, can be found on the CDC Web site at http://www.cdc.gov/flu.
As physicians and the Centers for Disease Control and Prevention (CDC) prepare for the upcoming influenza season, many of the recommendations remain unchanged from last season. Vaccination continues to be recommended for everyone 6 months of age and older. However, for the first time, a specific vaccine is preferred for children ages 2 through 8 years. Here’s what you need to know about this change, as well as how to handle vaccination in patients who are, or might be, allergic to eggs.
Use LAIV for kids ages 2 through 8 (if available)
For the first time, the CDC’s Advisory Committee on Immunization Practices (ACIP) has stated a preference for a specific influenza vaccine for a specific age group. It recommends using the live attenuated influenza vaccine (LAIV), which is a nasal spray, for children ages 2 through 8 years.1
A systematic review found evidence of increased efficacy of LAIV compared to inactivated influenza vaccine (IIV) in this age group; both types of vaccine have similar rates of adverse reactions.2 This increased effectiveness results in 46 fewer cases of confirmed influenza per 1000 children vaccinated (number needed to treat=24). Although the evidence of LAIV’s increased effectiveness was found for children ages 2 to 6 years, ACIP extended this recommendation through age 8 because this is the age through which physicians need to consider 2 doses of vaccine for a child previously unvaccinated with the influenza vaccine. Children younger than age 2 should receive IIV3 or IIV4.3
ACIP realizes that due to programmatic constraints it would be difficult to vaccinate all children with LAIV this year and is emphasizing that it should be implemented when feasible this year but no later than the 2015 to 2016 influenza season. IIV is effective in children and should be given if LAIV is not available or is contraindicated. Vaccine should not be delayed in the hopes of receiving LAIV if IIV is available.1
LAIV should not be used in children <2 years or adults >49. This vaccine is contraindicated in children and adolescents who are taking chronic aspirin therapy, pregnant women, those who are immunosuppressed, those with a history of egg allergy, or those who have taken influenza antiviral medications in the past 48 hours.1 LAIV also is not recommended for children ages 2 through 4 years who have asthma or had a wheezing episode in the past 12 months.1
There are precautions for the use of LAIV in patients with chronic medical conditions that can place them at high risk for complications from influenza, such as chronic lung, heart, renal, neurologic, liver, blood, or metabolic disorders, including asthma and diabetes.1
Which vaccine for patients who are allergic to eggs?
Two influenza vaccines are now available that are not prepared in embryonated eggs: recombinant influenza vaccine (RIV3) and cell culture-based inactivated influenza vaccine (ccIIV3). Both are trivalent products that contain antigens from 2 influenza A viruses and one influenza B virus and were introduced in time for the 2013 to 2014 flu season. The RIV3 is considered egg-free but ccIIV3 is not, although the amount of egg protein in it is miniscule, estimated at 5 × 10-8 mcg/0.5 mL dose.1 Neither product is licensed for children younger than 18 years and RIV3 is licensed only for those ages 18 through 49 years.
Patients who experience only hives after egg exposure can receive any of the flu vaccines except LAIV, and only because of a lack of data on this product, not because it has been shown to be less safe than the other vaccines. Patients who are unsure if they have an egg allergy or only get hives when they eat eggs should be observed for at least 30 minutes1 following injection as a precaution. Those ages 18 through 49 who have a history of severe reactions to eggs should receive RIV3. Patients younger than 18 years of age and older than 49 years of age can receive IIV vaccines approved for their specific age group. Any patient who is severely allergic and who cannot receive an egg-free vaccine should be vaccinated by a physician with experience managing severe allergic conditions.
Although severe, anaphylactic reactions to influenza vaccine are very rare, physicians should be equipped and prepared to respond to a severe allergic reaction after providing influenza vaccine to anyone with a history of an egg allergy.
Additional tips and resources
In addition to the LAIV, RIV3, and ccIIV3 vaccines described here, 10 other vaccines are available, including 5 egg-based IIV3 products in standard-dose form, 1 IIV3 vaccine for intradermal use, 1 high-dose IIV3 product for patients ages 65 or older, and 3 standard-dose IIV4 products. More details on each of these vaccines are available at http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6207a1.htm?_%20cid=rr6207a1_w#Tab1.
Regardless of which type of flu vaccine they receive, children 6 months through 8 years should receive 2 doses, at least 4 weeks apart, unless they received:
- 1 dose in 2013 to 2014, or
- 2 or more doses of seasonal influenza vaccine since July 2010, or
- 2 or more doses of seasonal influenza vaccine before July 2010 and ≥1 dose of monovalent H1N1 vaccine, or
- at least 1 dose of seasonal influenza vaccine prior to July 2010 and ≥1 after.
Vaccine effectiveness. The CDC estimated that vaccine effectiveness during the 2013 to 2014 flu season was 66%.3 While this degree of effectiveness is important for minimizing the morbidity and mortality from influenza each year, it’s important to appreciate the limitations of the vaccine and not rely on it as the only prevention intervention.
Other forms of prevention. We need to advise and practice good respiratory hygiene, frequent hand washing, self-isolation when sick, effective infection control practices at health care facilities, targeted early treatment with antivirals, and targeted pre- and post-exposure antiviral chemoprevention. Details on each of these interventions, including recommendations on the use of antiviral medications, can be found on the CDC Web site at http://www.cdc.gov/flu.
1. Grohskopf LA, Olsen SJ, Sokolow LZ, et al; Influenza Division, National Center for Immunization and Respiratory Diseases, CDC. Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States 2014-2015 influenza season. MMWR Morb Mortal Wkly Rep. 2014;63:691-697.
2. Grohskopf L, Olsen S, Sokolow L. Effectiveness of live-attenuated vs inactivated influenza vaccines for healthy children. PowerPoint presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/05-Flu-Grohskopf.pdf. Accessed August 6, 2014.
3. Flannery B. Interim estimates of 2013-14 seasonal influenza vaccine effectiveness. PowerPoint presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/04-Flu-Flannery.pdf. Accessed August 6, 2014.
1. Grohskopf LA, Olsen SJ, Sokolow LZ, et al; Influenza Division, National Center for Immunization and Respiratory Diseases, CDC. Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States 2014-2015 influenza season. MMWR Morb Mortal Wkly Rep. 2014;63:691-697.
2. Grohskopf L, Olsen S, Sokolow L. Effectiveness of live-attenuated vs inactivated influenza vaccines for healthy children. PowerPoint presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/05-Flu-Grohskopf.pdf. Accessed August 6, 2014.
3. Flannery B. Interim estimates of 2013-14 seasonal influenza vaccine effectiveness. PowerPoint presented at: Meeting of the Advisory Committee on Immunization Practices; February 26, 2014; Atlanta, GA. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-02/04-Flu-Flannery.pdf. Accessed August 6, 2014.
Diet, exercise, and CVD: When counseling makes the most sense
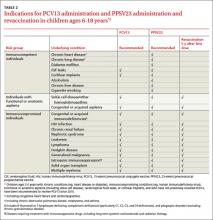
In the past 2 years, the US Preventive Services Task Force (USPSTF) has released 2 recommendations on the primary prevention of cardiovascular disease (CVD). And it is proposing a third. The first recommendation, released in 2012, covered behavioral counseling on diet and physical activity to prevent CVD in individuals without documented CVD risks.1 The second recommendation, released earlier this year, covered the use of vitamins and mineral supplements to prevent CVD.2 A draft of the proposed third recommendation, which was posted for public review until early June, covers behavioral counseling to help adults with known CVD risk factors improve their diet and physical activity (TABLE).1-3
Counseling can influence behavior, but does it affect outcomes?
CVD is the leading cause of death in the United States, accounting for >596,000 deaths per year with an age-adjusted rate of 191.4 per 100,000.4 Age-adjusted CVD mortality has been declining for decades thanks to improved medical care and a reduction in smoking and other risk factors. It is well documented that adults who follow national recommendations for a healthy diet and levels of physical activity have lower rates of CVD and CVD mortality.1 The USPSTF agrees with the American Heart Association (AHA) and the American College of Cardiology (ACC) that everyone would benefit from a healthier diet and more exercise.5 However, the Task Force reviewed the evidence on behavioral counseling in the primary care setting and found that, for adults who do not have known CVD, hypertension, hyperlipidemia, or diabetes, even high-intensity behavioral counseling resulted in only a small benefit in intermediate outcomes, which would translate into very small population-wide improvements.
In the evidence report prepared by the Task Force, the intensity of counseling intervention was defined as low, medium, or high if it lasted, respectively, 1 to 30 minutes, 31 to 360 minutes, or ≥361 minutes. Low-intensity interventions involved brief counseling sessions performed by primary care clinicians or mailing educational materials to patients or both. Medium- and high-intensity interventions usually were conducted by health educators, nutritionists, or other professionals instead of primary care clinicians. These interventions improved patients’ consumption of a healthier diet and participation in physical activity, but yielded only modest reductions in body mass index (BMI), blood pressure (BP), and lipid levels. Moreover, no direct evidence exists for improved CVD outcomes with these interventions.
The recent AHA/ACC guideline on lifestyle modifications recommends that clinicians advise all adults on healthy dietary choices and exercise, based on the known benefits of these behaviors. The guideline developers recognized that the evidence for benefits appears in the highest risk groups, and they did not assess the evidence for effectiveness of behavioral counseling itself.6
The Task Force rationale for recommending counseling
In the draft of its third recommendation addressing those at highest risk for CVD, the Task Force does advise high-intensity behavioral counseling for those who are overweight or obese and who have other CVD risk factors such as hypertension, hyperlipidemia, or impaired fasting glucose levels. This proposed new recommendation replaces one from 2003 that advised intensive dietary counseling for those with CVD risks including hyperlipidemia. The draft focuses attention in primary care on those who are overweight or obese. It complements another Task Force recommendation to provide or to refer patients for intensive multicomponent behavioral interventions if they are obese, defined as a BMI ≥30 kg/m2.7
The Task Force cited 2 examples of behavioral interventions that can improve outcomes in those with CVD risks—the Diabetes Prevention Program and PREMIER, a set of interventions to lower BP.8,9 These programs have improved intermediate outcomes after 12 to 24 months, decreasing total cholesterol by 3 to 6 mg/dL and low-density lipoprotein cholesterol by 1.5 to 5 mg/dL; systolic and diastolic BP by 1 to 3 mm Hg and 1 to 2 mm Hg, respectively; fasting glucose by 1 to 3 mg/dL; and weight by approximately 3 kg. The Task Force felt that while hard evidence is lacking for reducing CVD with counseling, epidemiologic studies demonstrate that, in those at high risk, reductions in CVD rates generally reflect the magnitude of improvement in intermediate measures.
Half of all adults in the United States have at least one documented CVD risk factor. But the potential benefit of behavioral counseling for those without documented CVD risks is relatively small. Rather than expending effort for only modest gain in the lower risk group, the Task Force recommends focusing on those with highest CVD risk. Thus the non-high risk group received a “C” recommendation, while the group of overweight and obese patients with other CVD risks received a “B” recommendation for essentially the same interventions. (For more on the grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.)
In addition to counseling...
The Task Force also recommends other interventions for the primary prevention of CVD:
- screening for and treating hypertension
- selectively screening for hyperlipidemia
- using aspirin to prevent CVD in those at high risk
- intensive counseling on weight management for those who are obese
- advising children and adolescents to avoid tobacco, and using brief interventions for tobacco cessation for smokers.
The recent Task Force recommendation on the use of vitamins, minerals, and multivitamins2 states that, while many adults take vitamin and mineral supplements in the belief that they prevent both heart disease and cancer, there is no evidence to support that belief. And there is good evidence that both β-carotene and vitamin E do not prevent disease. For other vitamins and minerals, singly or in combination, there is insufficient evidence to recommend for or against their use.2
The Community Preventive Services Task Force—a separate expert panel established by the US Department of Health and Human Services to complement the USPSTF—makes recommendations on population-level interventions and has a series of recommendations on ways to improve the population’s nutrition and physical activity.10 These community-based interventions, if widely implemented, would probably yield greater improvements in healthy eating and increased activity levels than resource-intense clinical interventions based on individual patients with low risk.
1. USPSTF. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsphys.htm. Accessed May 21, 2014.
2. USPSTF. Vitamin, mineral, and multivitamin supplements for the primary prevention of cardiovascular disease and cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf14/vitasupp/vitasuppfinalrs.htm. Accessed May 21, 2014.
3. USPSTF. Behavioral counseling to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with known risk factors: US Preventive Services Task Force Recommendation Statement (Draft). US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf13/cvdhighrisk/cvdhighriskdraftrec.htm. Accessed July 22, 2014.
4. Centers for Disease Control and Prevention. Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Report. 2012;61:1-51.
5. Eckel RH, Jakicic JM, Ard, JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
6. Stone NJ, Robinson JG, Lichtenstein AH, et al; 2013 ACC/AHA Cholesterol Guideline Panel. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association cholesterol guideline. Ann Intern Med. 2014;160:339-343.
7. USPSTF. Screening for and management of obesity in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsobes.htm. Accessed May 21, 2014.
8. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
9. Elmer PJ, Obarzanek E, Vollmer WM, et al; PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485-495.
10. USPSTF. The Guide to Community Preventive Services. Community Preventive Services Task Force Web site. Available at: http://www.thecommunityguide.org/index.html. Accessed May 21, 2014.
In the past 2 years, the US Preventive Services Task Force (USPSTF) has released 2 recommendations on the primary prevention of cardiovascular disease (CVD). And it is proposing a third. The first recommendation, released in 2012, covered behavioral counseling on diet and physical activity to prevent CVD in individuals without documented CVD risks.1 The second recommendation, released earlier this year, covered the use of vitamins and mineral supplements to prevent CVD.2 A draft of the proposed third recommendation, which was posted for public review until early June, covers behavioral counseling to help adults with known CVD risk factors improve their diet and physical activity (TABLE).1-3
Counseling can influence behavior, but does it affect outcomes?
CVD is the leading cause of death in the United States, accounting for >596,000 deaths per year with an age-adjusted rate of 191.4 per 100,000.4 Age-adjusted CVD mortality has been declining for decades thanks to improved medical care and a reduction in smoking and other risk factors. It is well documented that adults who follow national recommendations for a healthy diet and levels of physical activity have lower rates of CVD and CVD mortality.1 The USPSTF agrees with the American Heart Association (AHA) and the American College of Cardiology (ACC) that everyone would benefit from a healthier diet and more exercise.5 However, the Task Force reviewed the evidence on behavioral counseling in the primary care setting and found that, for adults who do not have known CVD, hypertension, hyperlipidemia, or diabetes, even high-intensity behavioral counseling resulted in only a small benefit in intermediate outcomes, which would translate into very small population-wide improvements.
In the evidence report prepared by the Task Force, the intensity of counseling intervention was defined as low, medium, or high if it lasted, respectively, 1 to 30 minutes, 31 to 360 minutes, or ≥361 minutes. Low-intensity interventions involved brief counseling sessions performed by primary care clinicians or mailing educational materials to patients or both. Medium- and high-intensity interventions usually were conducted by health educators, nutritionists, or other professionals instead of primary care clinicians. These interventions improved patients’ consumption of a healthier diet and participation in physical activity, but yielded only modest reductions in body mass index (BMI), blood pressure (BP), and lipid levels. Moreover, no direct evidence exists for improved CVD outcomes with these interventions.
The recent AHA/ACC guideline on lifestyle modifications recommends that clinicians advise all adults on healthy dietary choices and exercise, based on the known benefits of these behaviors. The guideline developers recognized that the evidence for benefits appears in the highest risk groups, and they did not assess the evidence for effectiveness of behavioral counseling itself.6
The Task Force rationale for recommending counseling
In the draft of its third recommendation addressing those at highest risk for CVD, the Task Force does advise high-intensity behavioral counseling for those who are overweight or obese and who have other CVD risk factors such as hypertension, hyperlipidemia, or impaired fasting glucose levels. This proposed new recommendation replaces one from 2003 that advised intensive dietary counseling for those with CVD risks including hyperlipidemia. The draft focuses attention in primary care on those who are overweight or obese. It complements another Task Force recommendation to provide or to refer patients for intensive multicomponent behavioral interventions if they are obese, defined as a BMI ≥30 kg/m2.7
The Task Force cited 2 examples of behavioral interventions that can improve outcomes in those with CVD risks—the Diabetes Prevention Program and PREMIER, a set of interventions to lower BP.8,9 These programs have improved intermediate outcomes after 12 to 24 months, decreasing total cholesterol by 3 to 6 mg/dL and low-density lipoprotein cholesterol by 1.5 to 5 mg/dL; systolic and diastolic BP by 1 to 3 mm Hg and 1 to 2 mm Hg, respectively; fasting glucose by 1 to 3 mg/dL; and weight by approximately 3 kg. The Task Force felt that while hard evidence is lacking for reducing CVD with counseling, epidemiologic studies demonstrate that, in those at high risk, reductions in CVD rates generally reflect the magnitude of improvement in intermediate measures.
Half of all adults in the United States have at least one documented CVD risk factor. But the potential benefit of behavioral counseling for those without documented CVD risks is relatively small. Rather than expending effort for only modest gain in the lower risk group, the Task Force recommends focusing on those with highest CVD risk. Thus the non-high risk group received a “C” recommendation, while the group of overweight and obese patients with other CVD risks received a “B” recommendation for essentially the same interventions. (For more on the grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.)
In addition to counseling...
The Task Force also recommends other interventions for the primary prevention of CVD:
- screening for and treating hypertension
- selectively screening for hyperlipidemia
- using aspirin to prevent CVD in those at high risk
- intensive counseling on weight management for those who are obese
- advising children and adolescents to avoid tobacco, and using brief interventions for tobacco cessation for smokers.
The recent Task Force recommendation on the use of vitamins, minerals, and multivitamins2 states that, while many adults take vitamin and mineral supplements in the belief that they prevent both heart disease and cancer, there is no evidence to support that belief. And there is good evidence that both β-carotene and vitamin E do not prevent disease. For other vitamins and minerals, singly or in combination, there is insufficient evidence to recommend for or against their use.2
The Community Preventive Services Task Force—a separate expert panel established by the US Department of Health and Human Services to complement the USPSTF—makes recommendations on population-level interventions and has a series of recommendations on ways to improve the population’s nutrition and physical activity.10 These community-based interventions, if widely implemented, would probably yield greater improvements in healthy eating and increased activity levels than resource-intense clinical interventions based on individual patients with low risk.
In the past 2 years, the US Preventive Services Task Force (USPSTF) has released 2 recommendations on the primary prevention of cardiovascular disease (CVD). And it is proposing a third. The first recommendation, released in 2012, covered behavioral counseling on diet and physical activity to prevent CVD in individuals without documented CVD risks.1 The second recommendation, released earlier this year, covered the use of vitamins and mineral supplements to prevent CVD.2 A draft of the proposed third recommendation, which was posted for public review until early June, covers behavioral counseling to help adults with known CVD risk factors improve their diet and physical activity (TABLE).1-3
Counseling can influence behavior, but does it affect outcomes?
CVD is the leading cause of death in the United States, accounting for >596,000 deaths per year with an age-adjusted rate of 191.4 per 100,000.4 Age-adjusted CVD mortality has been declining for decades thanks to improved medical care and a reduction in smoking and other risk factors. It is well documented that adults who follow national recommendations for a healthy diet and levels of physical activity have lower rates of CVD and CVD mortality.1 The USPSTF agrees with the American Heart Association (AHA) and the American College of Cardiology (ACC) that everyone would benefit from a healthier diet and more exercise.5 However, the Task Force reviewed the evidence on behavioral counseling in the primary care setting and found that, for adults who do not have known CVD, hypertension, hyperlipidemia, or diabetes, even high-intensity behavioral counseling resulted in only a small benefit in intermediate outcomes, which would translate into very small population-wide improvements.
In the evidence report prepared by the Task Force, the intensity of counseling intervention was defined as low, medium, or high if it lasted, respectively, 1 to 30 minutes, 31 to 360 minutes, or ≥361 minutes. Low-intensity interventions involved brief counseling sessions performed by primary care clinicians or mailing educational materials to patients or both. Medium- and high-intensity interventions usually were conducted by health educators, nutritionists, or other professionals instead of primary care clinicians. These interventions improved patients’ consumption of a healthier diet and participation in physical activity, but yielded only modest reductions in body mass index (BMI), blood pressure (BP), and lipid levels. Moreover, no direct evidence exists for improved CVD outcomes with these interventions.
The recent AHA/ACC guideline on lifestyle modifications recommends that clinicians advise all adults on healthy dietary choices and exercise, based on the known benefits of these behaviors. The guideline developers recognized that the evidence for benefits appears in the highest risk groups, and they did not assess the evidence for effectiveness of behavioral counseling itself.6
The Task Force rationale for recommending counseling
In the draft of its third recommendation addressing those at highest risk for CVD, the Task Force does advise high-intensity behavioral counseling for those who are overweight or obese and who have other CVD risk factors such as hypertension, hyperlipidemia, or impaired fasting glucose levels. This proposed new recommendation replaces one from 2003 that advised intensive dietary counseling for those with CVD risks including hyperlipidemia. The draft focuses attention in primary care on those who are overweight or obese. It complements another Task Force recommendation to provide or to refer patients for intensive multicomponent behavioral interventions if they are obese, defined as a BMI ≥30 kg/m2.7
The Task Force cited 2 examples of behavioral interventions that can improve outcomes in those with CVD risks—the Diabetes Prevention Program and PREMIER, a set of interventions to lower BP.8,9 These programs have improved intermediate outcomes after 12 to 24 months, decreasing total cholesterol by 3 to 6 mg/dL and low-density lipoprotein cholesterol by 1.5 to 5 mg/dL; systolic and diastolic BP by 1 to 3 mm Hg and 1 to 2 mm Hg, respectively; fasting glucose by 1 to 3 mg/dL; and weight by approximately 3 kg. The Task Force felt that while hard evidence is lacking for reducing CVD with counseling, epidemiologic studies demonstrate that, in those at high risk, reductions in CVD rates generally reflect the magnitude of improvement in intermediate measures.
Half of all adults in the United States have at least one documented CVD risk factor. But the potential benefit of behavioral counseling for those without documented CVD risks is relatively small. Rather than expending effort for only modest gain in the lower risk group, the Task Force recommends focusing on those with highest CVD risk. Thus the non-high risk group received a “C” recommendation, while the group of overweight and obese patients with other CVD risks received a “B” recommendation for essentially the same interventions. (For more on the grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.)
In addition to counseling...
The Task Force also recommends other interventions for the primary prevention of CVD:
- screening for and treating hypertension
- selectively screening for hyperlipidemia
- using aspirin to prevent CVD in those at high risk
- intensive counseling on weight management for those who are obese
- advising children and adolescents to avoid tobacco, and using brief interventions for tobacco cessation for smokers.
The recent Task Force recommendation on the use of vitamins, minerals, and multivitamins2 states that, while many adults take vitamin and mineral supplements in the belief that they prevent both heart disease and cancer, there is no evidence to support that belief. And there is good evidence that both β-carotene and vitamin E do not prevent disease. For other vitamins and minerals, singly or in combination, there is insufficient evidence to recommend for or against their use.2
The Community Preventive Services Task Force—a separate expert panel established by the US Department of Health and Human Services to complement the USPSTF—makes recommendations on population-level interventions and has a series of recommendations on ways to improve the population’s nutrition and physical activity.10 These community-based interventions, if widely implemented, would probably yield greater improvements in healthy eating and increased activity levels than resource-intense clinical interventions based on individual patients with low risk.
1. USPSTF. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsphys.htm. Accessed May 21, 2014.
2. USPSTF. Vitamin, mineral, and multivitamin supplements for the primary prevention of cardiovascular disease and cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf14/vitasupp/vitasuppfinalrs.htm. Accessed May 21, 2014.
3. USPSTF. Behavioral counseling to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with known risk factors: US Preventive Services Task Force Recommendation Statement (Draft). US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf13/cvdhighrisk/cvdhighriskdraftrec.htm. Accessed July 22, 2014.
4. Centers for Disease Control and Prevention. Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Report. 2012;61:1-51.
5. Eckel RH, Jakicic JM, Ard, JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
6. Stone NJ, Robinson JG, Lichtenstein AH, et al; 2013 ACC/AHA Cholesterol Guideline Panel. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association cholesterol guideline. Ann Intern Med. 2014;160:339-343.
7. USPSTF. Screening for and management of obesity in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsobes.htm. Accessed May 21, 2014.
8. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
9. Elmer PJ, Obarzanek E, Vollmer WM, et al; PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485-495.
10. USPSTF. The Guide to Community Preventive Services. Community Preventive Services Task Force Web site. Available at: http://www.thecommunityguide.org/index.html. Accessed May 21, 2014.
1. USPSTF. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsphys.htm. Accessed May 21, 2014.
2. USPSTF. Vitamin, mineral, and multivitamin supplements for the primary prevention of cardiovascular disease and cancer. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf14/vitasupp/vitasuppfinalrs.htm. Accessed May 21, 2014.
3. USPSTF. Behavioral counseling to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with known risk factors: US Preventive Services Task Force Recommendation Statement (Draft). US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf13/cvdhighrisk/cvdhighriskdraftrec.htm. Accessed July 22, 2014.
4. Centers for Disease Control and Prevention. Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Report. 2012;61:1-51.
5. Eckel RH, Jakicic JM, Ard, JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
6. Stone NJ, Robinson JG, Lichtenstein AH, et al; 2013 ACC/AHA Cholesterol Guideline Panel. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association cholesterol guideline. Ann Intern Med. 2014;160:339-343.
7. USPSTF. Screening for and management of obesity in adults. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsobes.htm. Accessed May 21, 2014.
8. Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
9. Elmer PJ, Obarzanek E, Vollmer WM, et al; PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485-495.
10. USPSTF. The Guide to Community Preventive Services. Community Preventive Services Task Force Web site. Available at: http://www.thecommunityguide.org/index.html. Accessed May 21, 2014.
Measles & pertussis: How best to respond to an outbreak
MERS: What you need to know
USPSTF: What’s recommended, what’s not
The United States Preventive Services Task Force (USPSTF) was busy in 2013, issuing 26 recommendations on 16 topics (TABLES 1-3). We have covered some of these topics previously in Practice Alerts or audiocasts—vitamin D for bone health and fall prevention,1 screening for lung cancer,2 human immunodeficiency virus infection,3 and the use of multivitamins to prevent cancer and cardiovascular disease (CVD).4 Another Practice Alert on chronic hepatitis C virus infection reviewed recommendations of the Centers for Disease Control and Prevention,5 which agree with those of the USPSTF. This Practice Alert discusses the remaining USPSTF recommendations.
Alcohol and tobacco
The Task Force (TF) reports that 30% of adults are affected by alcohol-related problems and that alcohol causes 85,000 deaths per year, making it the third leading cause of preventable death.6 The TF reviewed evidence on screening and counseling and now recommends screening adults ≥18 years for alcohol misuse and providing brief counseling to reduce alcohol use for those who engage in risky or hazardous drinking.6 The TF recommends any of 3 screening tools: using either the Alcohol Use Disorders Identification Test (AUDIT) or the abbreviated AUDIT-Consumption (AUDIT-C), or asking a single-question, such as “How many times in the past year have you had 5 (for men) or 4 (for women and all adults >65 years) or more drinks in a day?”6
Counseling for 5 to 15 minutes during the initial clinical encounter and then at subsequent visits is more effective than very brief (<5 minutes) or single-episode counseling. Counseling can include action plans, drinking diaries, stress management, or problem solving, and it can be done face-to-face or with written self-help materials, computer- or Web-based programs, or telephone support. Despite the importance of alcohol misuse as a health problem, the TF could find no evidence that screening and behavioral counseling is effective for adolescents.
For tobacco use, however, the TF now recommends providing prevention advice to school-age children and adolescents,7 presented in person or through written materials, videos, or other media. Over 8% of middle school children and close to 24% of high school students use tobacco.7 Tobacco is the leading cause of preventable deaths in the United States, and most smokers start before they are adults.7
Cancer screening and prevention
In addition to the recommendation for lung cancer screening, 2 other cancer screening/prevention recommendations were made in 2013. One is a modification of the previous recommendation on the use of BRCA gene testing to detect increased risk of breast and ovarian cancer. The recommendation now states that if a woman has a family member with breast, ovarian, tubal, or peritoneal cancer, her physician should use a screening tool to determine if her family history suggests high risk for having either BRCA1 or BRCA2. With a positive screening result, referral for genetic counseling is warranted. After counseling, the patient may choose to undergo BRCA testing. Screening tools reviewed by the TF are the Ontario Family History Assessment Tool, the Manchester Scoring System, the Referral Screening Tool, the Pedigree Assessment Tool, and the Family History Screening-7 instrument.8
The second recommendation is complex and concerns whether to prescribe tamoxifen or raloxifene to prevent breast cancer in women at high risk—ie, a 5-year risk ≥3%.9 One tool for estimating risk can be found at http://www.cancer.gov/bcrisktool/. It calculates risk based on age, race, genetic profile, age at menopause and menarche, family history of breast cancer, and personal history of breast cancer and biopsies. The TF recommends that physicians share decision making with women who are at high risk of breast cancer and offer medication to those at low risk of complications (those who have had a hysterectomy). Use of tamoxifen or raloxifene can reduce risk of the invasive cancer by 7 to 9 cases per 1000 women over 5 years. However, the risk of venous thromboembolism increases by 4 to 7 cases per 1000 over 5 years, and tamoxifen increases the risk of endometrial cancer by 4 in 1000. Both medications can cause hot flashes.9
Gestational diabetes
For a number of years the TF has assigned an “I” statement (insufficient evidence to assess benefits and harms) to screening for gestational diabetes. It recently changed that to a “B” recommendation for all pregnant women after the 24th week of pregnancy. Screening before 24 weeks is still listed as an I. Possible screening tools include a fasting blood glucose test, a 50-g oral glucose challenge test, or an assessment of risk factors. The TF did not find evidence of superiority with any of these methods. The TF found that diet modifications, glucose monitoring, and use of insulin can, in some cases, moderately reduce the incidence of preeclampsia, macrosomia, and shoulder dystocia.10
Intimate partner violence
Another change from a previous “I” statement pertains to intimate partner violence (IPV). The TF now recommends screening women of childbearing age for IPV and either providing intervention services for those who screen positive for IPV or referring for services. Reproductive age is defined as 14 to 46 years, although the TF admits that most studies have looked at women ≥18 years.11 Most of the benefits from screening and counseling have been demonstrated in pregnant women.
IPV can include physical, sexual, or psychological harm by a current or former partner or spouse, and it is not limited to opposite sex couples.11 Screening tools with the highest sensitivity and specificity include the Hurt, Insult, Threaten, and Scream (HITS) scale. Potential interventions include counseling, home visits, information cards, referrals to community services, and mentoring support.
While the TF acknowledges that both child abuse and elder abuse are prominent problems, there is not enough evidence to assess and recommend interventions.11,12
D recommendations
There were 4 “D” recommendations (recommend against) in 2013: testing for BRCA or using tamoxifen or raloxifene in women at low risk of breast cancer; using β-carotene or vitamin E to prevent CVD and cancer; and using low doses of vitamin D and calcium to prevent fractures in noninstitutionalized postmenopausal women (TABLE 2). In each instance the harms of the intervention were deemed to exceed potential benefits.
I statements
The TF still finds little evidence to support some common practices (TABLE 3). Physicians who use these interventions should realize that the TF, after thorough systematic reviews of the available evidence, does not find enough evidence to assess their relative benefits and harms. A description of the evidence on each condition can be found in the recommendations section of the USPSTF Web site (http://www.uspreventiveservicestaskforce.org/uspstopics.htm).
1. Campos-Outcalt D. Vitamin D: when it helps, when it harms. J Fam Pract. 2013;62:368-370.
2. Campos-Outcalt D. Lung cancer screening: USPSTF revises its recommendation. J Fam Pract. 2013;62:733-740.
3. Campos-Outcalt D. HIV screening: what the USPSTF says now. [Audiocast]. Parsippany, NJ; The Journal of Family Practice: 2013. Available at: http://www.jfponline.com/multimedia/audio/article/hiv-screening-what-the-uspstf-says-now/a1c4bc0fc9405f18820bb19fe971f743.html. Accessed March 14, 2014.
4. Campos-Outcalt D. Does your patient really need a supplement? [Audiocast]. Parsippany, NJ: The Journal of Family Practice; 2013. Available at: http://www.jfponline.com/index.php?id=21643&cHash=071010&tx_ttnews[tt_news]=226385. Accessed March 14, 2014.
5. Campos-Outcalt D. Hepatitis C: new CDC screening recommendations. J Fam Pract. 2012;61:744-746.
6. US Preventive Services Task Force Web site. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrin.htm. Accessed March 14, 2014.
7. US Preventive Services Task Force Web site. Primary care interventions to prevent tobacco use in children and adolescents. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstbac.htm. Accessed March 14, 2014.
8. US Preventive Services Task Force Web site. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrgen.htm. Accessed March 14, 2014.
9. US Preventive Services Task Force Web site. Medication for risk reduction of primary breast cancer in women. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrpv.htm. Accessed March 14, 2014.
10. US Preventive Services Task Force Web site. Screening for gestational diabetes mellitius. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgdm.htm. Accessed March 14, 2014.
11. US Preventive Services Task Force Web site. Screening for intimate partner violence and abuse of elderly and vulnerable adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsipv.htm. Accessed March 14, 2014.
12. US Preventive Services Task Force Web site. Primary interventions to prevent child maltreatment. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsfamv.htm. Accessed March 14, 2014.
The United States Preventive Services Task Force (USPSTF) was busy in 2013, issuing 26 recommendations on 16 topics (TABLES 1-3). We have covered some of these topics previously in Practice Alerts or audiocasts—vitamin D for bone health and fall prevention,1 screening for lung cancer,2 human immunodeficiency virus infection,3 and the use of multivitamins to prevent cancer and cardiovascular disease (CVD).4 Another Practice Alert on chronic hepatitis C virus infection reviewed recommendations of the Centers for Disease Control and Prevention,5 which agree with those of the USPSTF. This Practice Alert discusses the remaining USPSTF recommendations.
Alcohol and tobacco
The Task Force (TF) reports that 30% of adults are affected by alcohol-related problems and that alcohol causes 85,000 deaths per year, making it the third leading cause of preventable death.6 The TF reviewed evidence on screening and counseling and now recommends screening adults ≥18 years for alcohol misuse and providing brief counseling to reduce alcohol use for those who engage in risky or hazardous drinking.6 The TF recommends any of 3 screening tools: using either the Alcohol Use Disorders Identification Test (AUDIT) or the abbreviated AUDIT-Consumption (AUDIT-C), or asking a single-question, such as “How many times in the past year have you had 5 (for men) or 4 (for women and all adults >65 years) or more drinks in a day?”6
Counseling for 5 to 15 minutes during the initial clinical encounter and then at subsequent visits is more effective than very brief (<5 minutes) or single-episode counseling. Counseling can include action plans, drinking diaries, stress management, or problem solving, and it can be done face-to-face or with written self-help materials, computer- or Web-based programs, or telephone support. Despite the importance of alcohol misuse as a health problem, the TF could find no evidence that screening and behavioral counseling is effective for adolescents.
For tobacco use, however, the TF now recommends providing prevention advice to school-age children and adolescents,7 presented in person or through written materials, videos, or other media. Over 8% of middle school children and close to 24% of high school students use tobacco.7 Tobacco is the leading cause of preventable deaths in the United States, and most smokers start before they are adults.7
Cancer screening and prevention
In addition to the recommendation for lung cancer screening, 2 other cancer screening/prevention recommendations were made in 2013. One is a modification of the previous recommendation on the use of BRCA gene testing to detect increased risk of breast and ovarian cancer. The recommendation now states that if a woman has a family member with breast, ovarian, tubal, or peritoneal cancer, her physician should use a screening tool to determine if her family history suggests high risk for having either BRCA1 or BRCA2. With a positive screening result, referral for genetic counseling is warranted. After counseling, the patient may choose to undergo BRCA testing. Screening tools reviewed by the TF are the Ontario Family History Assessment Tool, the Manchester Scoring System, the Referral Screening Tool, the Pedigree Assessment Tool, and the Family History Screening-7 instrument.8
The second recommendation is complex and concerns whether to prescribe tamoxifen or raloxifene to prevent breast cancer in women at high risk—ie, a 5-year risk ≥3%.9 One tool for estimating risk can be found at http://www.cancer.gov/bcrisktool/. It calculates risk based on age, race, genetic profile, age at menopause and menarche, family history of breast cancer, and personal history of breast cancer and biopsies. The TF recommends that physicians share decision making with women who are at high risk of breast cancer and offer medication to those at low risk of complications (those who have had a hysterectomy). Use of tamoxifen or raloxifene can reduce risk of the invasive cancer by 7 to 9 cases per 1000 women over 5 years. However, the risk of venous thromboembolism increases by 4 to 7 cases per 1000 over 5 years, and tamoxifen increases the risk of endometrial cancer by 4 in 1000. Both medications can cause hot flashes.9
Gestational diabetes
For a number of years the TF has assigned an “I” statement (insufficient evidence to assess benefits and harms) to screening for gestational diabetes. It recently changed that to a “B” recommendation for all pregnant women after the 24th week of pregnancy. Screening before 24 weeks is still listed as an I. Possible screening tools include a fasting blood glucose test, a 50-g oral glucose challenge test, or an assessment of risk factors. The TF did not find evidence of superiority with any of these methods. The TF found that diet modifications, glucose monitoring, and use of insulin can, in some cases, moderately reduce the incidence of preeclampsia, macrosomia, and shoulder dystocia.10
Intimate partner violence
Another change from a previous “I” statement pertains to intimate partner violence (IPV). The TF now recommends screening women of childbearing age for IPV and either providing intervention services for those who screen positive for IPV or referring for services. Reproductive age is defined as 14 to 46 years, although the TF admits that most studies have looked at women ≥18 years.11 Most of the benefits from screening and counseling have been demonstrated in pregnant women.
IPV can include physical, sexual, or psychological harm by a current or former partner or spouse, and it is not limited to opposite sex couples.11 Screening tools with the highest sensitivity and specificity include the Hurt, Insult, Threaten, and Scream (HITS) scale. Potential interventions include counseling, home visits, information cards, referrals to community services, and mentoring support.
While the TF acknowledges that both child abuse and elder abuse are prominent problems, there is not enough evidence to assess and recommend interventions.11,12
D recommendations
There were 4 “D” recommendations (recommend against) in 2013: testing for BRCA or using tamoxifen or raloxifene in women at low risk of breast cancer; using β-carotene or vitamin E to prevent CVD and cancer; and using low doses of vitamin D and calcium to prevent fractures in noninstitutionalized postmenopausal women (TABLE 2). In each instance the harms of the intervention were deemed to exceed potential benefits.
I statements
The TF still finds little evidence to support some common practices (TABLE 3). Physicians who use these interventions should realize that the TF, after thorough systematic reviews of the available evidence, does not find enough evidence to assess their relative benefits and harms. A description of the evidence on each condition can be found in the recommendations section of the USPSTF Web site (http://www.uspreventiveservicestaskforce.org/uspstopics.htm).
The United States Preventive Services Task Force (USPSTF) was busy in 2013, issuing 26 recommendations on 16 topics (TABLES 1-3). We have covered some of these topics previously in Practice Alerts or audiocasts—vitamin D for bone health and fall prevention,1 screening for lung cancer,2 human immunodeficiency virus infection,3 and the use of multivitamins to prevent cancer and cardiovascular disease (CVD).4 Another Practice Alert on chronic hepatitis C virus infection reviewed recommendations of the Centers for Disease Control and Prevention,5 which agree with those of the USPSTF. This Practice Alert discusses the remaining USPSTF recommendations.
Alcohol and tobacco
The Task Force (TF) reports that 30% of adults are affected by alcohol-related problems and that alcohol causes 85,000 deaths per year, making it the third leading cause of preventable death.6 The TF reviewed evidence on screening and counseling and now recommends screening adults ≥18 years for alcohol misuse and providing brief counseling to reduce alcohol use for those who engage in risky or hazardous drinking.6 The TF recommends any of 3 screening tools: using either the Alcohol Use Disorders Identification Test (AUDIT) or the abbreviated AUDIT-Consumption (AUDIT-C), or asking a single-question, such as “How many times in the past year have you had 5 (for men) or 4 (for women and all adults >65 years) or more drinks in a day?”6
Counseling for 5 to 15 minutes during the initial clinical encounter and then at subsequent visits is more effective than very brief (<5 minutes) or single-episode counseling. Counseling can include action plans, drinking diaries, stress management, or problem solving, and it can be done face-to-face or with written self-help materials, computer- or Web-based programs, or telephone support. Despite the importance of alcohol misuse as a health problem, the TF could find no evidence that screening and behavioral counseling is effective for adolescents.
For tobacco use, however, the TF now recommends providing prevention advice to school-age children and adolescents,7 presented in person or through written materials, videos, or other media. Over 8% of middle school children and close to 24% of high school students use tobacco.7 Tobacco is the leading cause of preventable deaths in the United States, and most smokers start before they are adults.7
Cancer screening and prevention
In addition to the recommendation for lung cancer screening, 2 other cancer screening/prevention recommendations were made in 2013. One is a modification of the previous recommendation on the use of BRCA gene testing to detect increased risk of breast and ovarian cancer. The recommendation now states that if a woman has a family member with breast, ovarian, tubal, or peritoneal cancer, her physician should use a screening tool to determine if her family history suggests high risk for having either BRCA1 or BRCA2. With a positive screening result, referral for genetic counseling is warranted. After counseling, the patient may choose to undergo BRCA testing. Screening tools reviewed by the TF are the Ontario Family History Assessment Tool, the Manchester Scoring System, the Referral Screening Tool, the Pedigree Assessment Tool, and the Family History Screening-7 instrument.8
The second recommendation is complex and concerns whether to prescribe tamoxifen or raloxifene to prevent breast cancer in women at high risk—ie, a 5-year risk ≥3%.9 One tool for estimating risk can be found at http://www.cancer.gov/bcrisktool/. It calculates risk based on age, race, genetic profile, age at menopause and menarche, family history of breast cancer, and personal history of breast cancer and biopsies. The TF recommends that physicians share decision making with women who are at high risk of breast cancer and offer medication to those at low risk of complications (those who have had a hysterectomy). Use of tamoxifen or raloxifene can reduce risk of the invasive cancer by 7 to 9 cases per 1000 women over 5 years. However, the risk of venous thromboembolism increases by 4 to 7 cases per 1000 over 5 years, and tamoxifen increases the risk of endometrial cancer by 4 in 1000. Both medications can cause hot flashes.9
Gestational diabetes
For a number of years the TF has assigned an “I” statement (insufficient evidence to assess benefits and harms) to screening for gestational diabetes. It recently changed that to a “B” recommendation for all pregnant women after the 24th week of pregnancy. Screening before 24 weeks is still listed as an I. Possible screening tools include a fasting blood glucose test, a 50-g oral glucose challenge test, or an assessment of risk factors. The TF did not find evidence of superiority with any of these methods. The TF found that diet modifications, glucose monitoring, and use of insulin can, in some cases, moderately reduce the incidence of preeclampsia, macrosomia, and shoulder dystocia.10
Intimate partner violence
Another change from a previous “I” statement pertains to intimate partner violence (IPV). The TF now recommends screening women of childbearing age for IPV and either providing intervention services for those who screen positive for IPV or referring for services. Reproductive age is defined as 14 to 46 years, although the TF admits that most studies have looked at women ≥18 years.11 Most of the benefits from screening and counseling have been demonstrated in pregnant women.
IPV can include physical, sexual, or psychological harm by a current or former partner or spouse, and it is not limited to opposite sex couples.11 Screening tools with the highest sensitivity and specificity include the Hurt, Insult, Threaten, and Scream (HITS) scale. Potential interventions include counseling, home visits, information cards, referrals to community services, and mentoring support.
While the TF acknowledges that both child abuse and elder abuse are prominent problems, there is not enough evidence to assess and recommend interventions.11,12
D recommendations
There were 4 “D” recommendations (recommend against) in 2013: testing for BRCA or using tamoxifen or raloxifene in women at low risk of breast cancer; using β-carotene or vitamin E to prevent CVD and cancer; and using low doses of vitamin D and calcium to prevent fractures in noninstitutionalized postmenopausal women (TABLE 2). In each instance the harms of the intervention were deemed to exceed potential benefits.
I statements
The TF still finds little evidence to support some common practices (TABLE 3). Physicians who use these interventions should realize that the TF, after thorough systematic reviews of the available evidence, does not find enough evidence to assess their relative benefits and harms. A description of the evidence on each condition can be found in the recommendations section of the USPSTF Web site (http://www.uspreventiveservicestaskforce.org/uspstopics.htm).
1. Campos-Outcalt D. Vitamin D: when it helps, when it harms. J Fam Pract. 2013;62:368-370.
2. Campos-Outcalt D. Lung cancer screening: USPSTF revises its recommendation. J Fam Pract. 2013;62:733-740.
3. Campos-Outcalt D. HIV screening: what the USPSTF says now. [Audiocast]. Parsippany, NJ; The Journal of Family Practice: 2013. Available at: http://www.jfponline.com/multimedia/audio/article/hiv-screening-what-the-uspstf-says-now/a1c4bc0fc9405f18820bb19fe971f743.html. Accessed March 14, 2014.
4. Campos-Outcalt D. Does your patient really need a supplement? [Audiocast]. Parsippany, NJ: The Journal of Family Practice; 2013. Available at: http://www.jfponline.com/index.php?id=21643&cHash=071010&tx_ttnews[tt_news]=226385. Accessed March 14, 2014.
5. Campos-Outcalt D. Hepatitis C: new CDC screening recommendations. J Fam Pract. 2012;61:744-746.
6. US Preventive Services Task Force Web site. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrin.htm. Accessed March 14, 2014.
7. US Preventive Services Task Force Web site. Primary care interventions to prevent tobacco use in children and adolescents. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstbac.htm. Accessed March 14, 2014.
8. US Preventive Services Task Force Web site. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrgen.htm. Accessed March 14, 2014.
9. US Preventive Services Task Force Web site. Medication for risk reduction of primary breast cancer in women. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrpv.htm. Accessed March 14, 2014.
10. US Preventive Services Task Force Web site. Screening for gestational diabetes mellitius. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgdm.htm. Accessed March 14, 2014.
11. US Preventive Services Task Force Web site. Screening for intimate partner violence and abuse of elderly and vulnerable adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsipv.htm. Accessed March 14, 2014.
12. US Preventive Services Task Force Web site. Primary interventions to prevent child maltreatment. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsfamv.htm. Accessed March 14, 2014.
1. Campos-Outcalt D. Vitamin D: when it helps, when it harms. J Fam Pract. 2013;62:368-370.
2. Campos-Outcalt D. Lung cancer screening: USPSTF revises its recommendation. J Fam Pract. 2013;62:733-740.
3. Campos-Outcalt D. HIV screening: what the USPSTF says now. [Audiocast]. Parsippany, NJ; The Journal of Family Practice: 2013. Available at: http://www.jfponline.com/multimedia/audio/article/hiv-screening-what-the-uspstf-says-now/a1c4bc0fc9405f18820bb19fe971f743.html. Accessed March 14, 2014.
4. Campos-Outcalt D. Does your patient really need a supplement? [Audiocast]. Parsippany, NJ: The Journal of Family Practice; 2013. Available at: http://www.jfponline.com/index.php?id=21643&cHash=071010&tx_ttnews[tt_news]=226385. Accessed March 14, 2014.
5. Campos-Outcalt D. Hepatitis C: new CDC screening recommendations. J Fam Pract. 2012;61:744-746.
6. US Preventive Services Task Force Web site. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrin.htm. Accessed March 14, 2014.
7. US Preventive Services Task Force Web site. Primary care interventions to prevent tobacco use in children and adolescents. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstbac.htm. Accessed March 14, 2014.
8. US Preventive Services Task Force Web site. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrgen.htm. Accessed March 14, 2014.
9. US Preventive Services Task Force Web site. Medication for risk reduction of primary breast cancer in women. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrpv.htm. Accessed March 14, 2014.
10. US Preventive Services Task Force Web site. Screening for gestational diabetes mellitius. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgdm.htm. Accessed March 14, 2014.
11. US Preventive Services Task Force Web site. Screening for intimate partner violence and abuse of elderly and vulnerable adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsipv.htm. Accessed March 14, 2014.
12. US Preventive Services Task Force Web site. Primary interventions to prevent child maltreatment. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsfamv.htm. Accessed March 14, 2014.
Immunization update: The latest ACIP recommendations
The Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC) released several new immunization recommendations in 2013, and they pertain to special populations: infants at high risk for meningococcal disease who could benefit from a new vaccine; children ages 2 to 16 years who may now receive the Japanese encephalitis (JE) vaccine if traveling to Asia; and children and adolescents at high risk for Streptococcus pneumoniae infections who should receive the 13-valent pneumococcal conjugate vaccine (PCV13).
New meningococcal vaccine for high-risk infants
A third vaccine against meningococcal disease, Menveo (Novartis), has been approved for use in high-risk infants ages 2 to 23 months—those with complement deficiencies or functional or anatomic asplenia, those involved in an institutional or community outbreak of meningococcal disease, and those traveling to a meningococcal-endemic area (eg, the meningitis belt of Africa). The 3 vaccines approved for use in infants (TABLE 1) vary in indications and use for travel.1 Keep in mind that vaccination against meningococcal disease is not recommended for routine use in infants because of the low prevalence of disease and a predominance of meningococcal type B, which is not prevented by any of the current vaccines.2
Japanese encephalitis vaccine approved for children, adolescents
Since 2009, a vaccine of inactivated JE virus derived from Vero cell culture (Ixiaro, manufactured by Intercell Biomedical and distributed by Norvartis) has been available in the United States for adults ≥17 years who travel during JE virus transmission season to parts of Asia where the virus is endemic. In May 2013, the US Food and Drug Administration licensed the JE vaccine for use in children ages 2 to 16 years, and in June 2013, ACIP recommended it for those in this age group for the same indications as adults.3
Individuals at high risk are those likely to visit rural areas where the virus is prevalent. The vaccine is not recommended for short-term travelers who will confine their visit to urban areas or who will refrain from traveling during the JE transmission season. The CDC travel Web site describes the geographic areas where the JE virus can be found and the timing of the JE season (http://wwwnc.cdc.gov/travel/diseases/japanese-encephalitis; see “Who is at risk?”). Use of the vaccine will be uncommon, and most of those who will receive it will need to visit a travel clinic or local health department. A primary series is 2 doses, given 28 days apart.
Pneumococcal vaccine for high-risk children up to age 18
ACIP now recommends the use of both PCV13 and 23-valent pneumococcal polysaccharide vaccine (PPSV23) in children ages 6 to 18 years who have not been vaccinated with these products and who have certain immunocompromising conditions, functional or anatomic asplenia (including those with sickle cell disease), cerebrospinal fluid leaks, or cochlear implants (TABLE 2).4 PPSV23 alone is recommended for those in this age group with chronic heart, lung, or liver disease or diabetes, and for those who smoke. The recommendation is complicated because those with asplenia or immunocompromising conditions should receive 2 doses of PPSV23 at least 5 years apart (TABLE 2). PCV13 is indicated even if the patient was previously fully immunized with 7-valent pneumococcal conjugate vaccine.
Ideally, all children for whom PCV13 is indicated would receive a full vaccine series as infants, and at 2, 4, 6, and 12 to 15 months of age. Those with chronic medical conditions and immunocompromising conditions should additionally receive PPSV23 at age 2 years, and again 5 years later if they have asplenia or an immunocompromising condition.5 However, some of these children will remain unimmunized; others can become underimmunized if they acquire a condition that heightens their risk for pneumococcal disease. Both situations make necessary the new recommendation for those ages 6 to 18 years. For those who have received neither vaccine, the recommended sequence is to receive PCV13 first, followed by PPSV23 at least 8 weeks later.
Pneumococcal vaccine recommendations are now uniform for those ages 6 to 64 years with chronic medical conditions and immunocompromising conditions.2,6 All those ≥65 should receive PPSV23, even if they have received 2 previous doses. At least 5 years should have passed from a previous PPSV23 dose. This is the only scenario in which a third dose of PPSV23 is recommended.
Universal use of pneumococcal vaccines has markedly reduced invasive pneumococcal disease nationally in vaccinated and unvaccinated individuals.5 While invasive pneumococcal disease rates have fallen overall, patients with high-risk conditions still have a high relative risk. The incidence rates (cases per 100,000) for children with hematologic malignancies were estimated at 1282 (rate ratio [RR], compared with children without this condition, of 822); 197 for those with HIV infection (RR=122), and 56 for those with sickle cell disease (RR=27).4
As the incidence of antibiotic resistance increases, the primary prevention of bacterial infections becomes more significant. It is of both public health and individual importance that those who develop conditions placing them at increased risk for pneumococcal disease or complications from pneumococcal infection receive recommended pneumococcal vaccines.
1. MacNeil J. Recommendations for use of MenACWY-CRM (Menveo) in infants at increased risk for meningococcal disease. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 23, 2013; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2013/04-MCV-MacNeil.pdf. Accessed February 12, 2014.
2. Centers for Disease Control and Prevention (CDC). Infant meningococcal vaccination: Advisory Committee on Immunization Practices (ACIP) recommendations and rationale. MMWR Morb Mortal Wkly Rep. 2013;62:52-54.
3. Centers for Disease Control and Prevention (CDC). Use of Japanese encephalitis vaccine in children: recommendations of the advisory committee on immunization practices, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:898-900.
4. Centers for Disease Control and Prevention (CDC). Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among children aged 6-18 years with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2013;62:521-524.
5. Nuorti JP, Whitney CG; Centers for Disease Control and Prevention (CDC). Prevention of pneumococcal disease among infants and children - use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine - recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010;59(RR-11):1-18.
6. Centers for Disease Control and Prevention (CDC). Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2012;61:816-819.
The Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC) released several new immunization recommendations in 2013, and they pertain to special populations: infants at high risk for meningococcal disease who could benefit from a new vaccine; children ages 2 to 16 years who may now receive the Japanese encephalitis (JE) vaccine if traveling to Asia; and children and adolescents at high risk for Streptococcus pneumoniae infections who should receive the 13-valent pneumococcal conjugate vaccine (PCV13).
New meningococcal vaccine for high-risk infants
A third vaccine against meningococcal disease, Menveo (Novartis), has been approved for use in high-risk infants ages 2 to 23 months—those with complement deficiencies or functional or anatomic asplenia, those involved in an institutional or community outbreak of meningococcal disease, and those traveling to a meningococcal-endemic area (eg, the meningitis belt of Africa). The 3 vaccines approved for use in infants (TABLE 1) vary in indications and use for travel.1 Keep in mind that vaccination against meningococcal disease is not recommended for routine use in infants because of the low prevalence of disease and a predominance of meningococcal type B, which is not prevented by any of the current vaccines.2
Japanese encephalitis vaccine approved for children, adolescents
Since 2009, a vaccine of inactivated JE virus derived from Vero cell culture (Ixiaro, manufactured by Intercell Biomedical and distributed by Norvartis) has been available in the United States for adults ≥17 years who travel during JE virus transmission season to parts of Asia where the virus is endemic. In May 2013, the US Food and Drug Administration licensed the JE vaccine for use in children ages 2 to 16 years, and in June 2013, ACIP recommended it for those in this age group for the same indications as adults.3
Individuals at high risk are those likely to visit rural areas where the virus is prevalent. The vaccine is not recommended for short-term travelers who will confine their visit to urban areas or who will refrain from traveling during the JE transmission season. The CDC travel Web site describes the geographic areas where the JE virus can be found and the timing of the JE season (http://wwwnc.cdc.gov/travel/diseases/japanese-encephalitis; see “Who is at risk?”). Use of the vaccine will be uncommon, and most of those who will receive it will need to visit a travel clinic or local health department. A primary series is 2 doses, given 28 days apart.
Pneumococcal vaccine for high-risk children up to age 18
ACIP now recommends the use of both PCV13 and 23-valent pneumococcal polysaccharide vaccine (PPSV23) in children ages 6 to 18 years who have not been vaccinated with these products and who have certain immunocompromising conditions, functional or anatomic asplenia (including those with sickle cell disease), cerebrospinal fluid leaks, or cochlear implants (TABLE 2).4 PPSV23 alone is recommended for those in this age group with chronic heart, lung, or liver disease or diabetes, and for those who smoke. The recommendation is complicated because those with asplenia or immunocompromising conditions should receive 2 doses of PPSV23 at least 5 years apart (TABLE 2). PCV13 is indicated even if the patient was previously fully immunized with 7-valent pneumococcal conjugate vaccine.
Ideally, all children for whom PCV13 is indicated would receive a full vaccine series as infants, and at 2, 4, 6, and 12 to 15 months of age. Those with chronic medical conditions and immunocompromising conditions should additionally receive PPSV23 at age 2 years, and again 5 years later if they have asplenia or an immunocompromising condition.5 However, some of these children will remain unimmunized; others can become underimmunized if they acquire a condition that heightens their risk for pneumococcal disease. Both situations make necessary the new recommendation for those ages 6 to 18 years. For those who have received neither vaccine, the recommended sequence is to receive PCV13 first, followed by PPSV23 at least 8 weeks later.
Pneumococcal vaccine recommendations are now uniform for those ages 6 to 64 years with chronic medical conditions and immunocompromising conditions.2,6 All those ≥65 should receive PPSV23, even if they have received 2 previous doses. At least 5 years should have passed from a previous PPSV23 dose. This is the only scenario in which a third dose of PPSV23 is recommended.
Universal use of pneumococcal vaccines has markedly reduced invasive pneumococcal disease nationally in vaccinated and unvaccinated individuals.5 While invasive pneumococcal disease rates have fallen overall, patients with high-risk conditions still have a high relative risk. The incidence rates (cases per 100,000) for children with hematologic malignancies were estimated at 1282 (rate ratio [RR], compared with children without this condition, of 822); 197 for those with HIV infection (RR=122), and 56 for those with sickle cell disease (RR=27).4
As the incidence of antibiotic resistance increases, the primary prevention of bacterial infections becomes more significant. It is of both public health and individual importance that those who develop conditions placing them at increased risk for pneumococcal disease or complications from pneumococcal infection receive recommended pneumococcal vaccines.
The Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC) released several new immunization recommendations in 2013, and they pertain to special populations: infants at high risk for meningococcal disease who could benefit from a new vaccine; children ages 2 to 16 years who may now receive the Japanese encephalitis (JE) vaccine if traveling to Asia; and children and adolescents at high risk for Streptococcus pneumoniae infections who should receive the 13-valent pneumococcal conjugate vaccine (PCV13).
New meningococcal vaccine for high-risk infants
A third vaccine against meningococcal disease, Menveo (Novartis), has been approved for use in high-risk infants ages 2 to 23 months—those with complement deficiencies or functional or anatomic asplenia, those involved in an institutional or community outbreak of meningococcal disease, and those traveling to a meningococcal-endemic area (eg, the meningitis belt of Africa). The 3 vaccines approved for use in infants (TABLE 1) vary in indications and use for travel.1 Keep in mind that vaccination against meningococcal disease is not recommended for routine use in infants because of the low prevalence of disease and a predominance of meningococcal type B, which is not prevented by any of the current vaccines.2
Japanese encephalitis vaccine approved for children, adolescents
Since 2009, a vaccine of inactivated JE virus derived from Vero cell culture (Ixiaro, manufactured by Intercell Biomedical and distributed by Norvartis) has been available in the United States for adults ≥17 years who travel during JE virus transmission season to parts of Asia where the virus is endemic. In May 2013, the US Food and Drug Administration licensed the JE vaccine for use in children ages 2 to 16 years, and in June 2013, ACIP recommended it for those in this age group for the same indications as adults.3
Individuals at high risk are those likely to visit rural areas where the virus is prevalent. The vaccine is not recommended for short-term travelers who will confine their visit to urban areas or who will refrain from traveling during the JE transmission season. The CDC travel Web site describes the geographic areas where the JE virus can be found and the timing of the JE season (http://wwwnc.cdc.gov/travel/diseases/japanese-encephalitis; see “Who is at risk?”). Use of the vaccine will be uncommon, and most of those who will receive it will need to visit a travel clinic or local health department. A primary series is 2 doses, given 28 days apart.
Pneumococcal vaccine for high-risk children up to age 18
ACIP now recommends the use of both PCV13 and 23-valent pneumococcal polysaccharide vaccine (PPSV23) in children ages 6 to 18 years who have not been vaccinated with these products and who have certain immunocompromising conditions, functional or anatomic asplenia (including those with sickle cell disease), cerebrospinal fluid leaks, or cochlear implants (TABLE 2).4 PPSV23 alone is recommended for those in this age group with chronic heart, lung, or liver disease or diabetes, and for those who smoke. The recommendation is complicated because those with asplenia or immunocompromising conditions should receive 2 doses of PPSV23 at least 5 years apart (TABLE 2). PCV13 is indicated even if the patient was previously fully immunized with 7-valent pneumococcal conjugate vaccine.
Ideally, all children for whom PCV13 is indicated would receive a full vaccine series as infants, and at 2, 4, 6, and 12 to 15 months of age. Those with chronic medical conditions and immunocompromising conditions should additionally receive PPSV23 at age 2 years, and again 5 years later if they have asplenia or an immunocompromising condition.5 However, some of these children will remain unimmunized; others can become underimmunized if they acquire a condition that heightens their risk for pneumococcal disease. Both situations make necessary the new recommendation for those ages 6 to 18 years. For those who have received neither vaccine, the recommended sequence is to receive PCV13 first, followed by PPSV23 at least 8 weeks later.
Pneumococcal vaccine recommendations are now uniform for those ages 6 to 64 years with chronic medical conditions and immunocompromising conditions.2,6 All those ≥65 should receive PPSV23, even if they have received 2 previous doses. At least 5 years should have passed from a previous PPSV23 dose. This is the only scenario in which a third dose of PPSV23 is recommended.
Universal use of pneumococcal vaccines has markedly reduced invasive pneumococcal disease nationally in vaccinated and unvaccinated individuals.5 While invasive pneumococcal disease rates have fallen overall, patients with high-risk conditions still have a high relative risk. The incidence rates (cases per 100,000) for children with hematologic malignancies were estimated at 1282 (rate ratio [RR], compared with children without this condition, of 822); 197 for those with HIV infection (RR=122), and 56 for those with sickle cell disease (RR=27).4
As the incidence of antibiotic resistance increases, the primary prevention of bacterial infections becomes more significant. It is of both public health and individual importance that those who develop conditions placing them at increased risk for pneumococcal disease or complications from pneumococcal infection receive recommended pneumococcal vaccines.
1. MacNeil J. Recommendations for use of MenACWY-CRM (Menveo) in infants at increased risk for meningococcal disease. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 23, 2013; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2013/04-MCV-MacNeil.pdf. Accessed February 12, 2014.
2. Centers for Disease Control and Prevention (CDC). Infant meningococcal vaccination: Advisory Committee on Immunization Practices (ACIP) recommendations and rationale. MMWR Morb Mortal Wkly Rep. 2013;62:52-54.
3. Centers for Disease Control and Prevention (CDC). Use of Japanese encephalitis vaccine in children: recommendations of the advisory committee on immunization practices, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:898-900.
4. Centers for Disease Control and Prevention (CDC). Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among children aged 6-18 years with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2013;62:521-524.
5. Nuorti JP, Whitney CG; Centers for Disease Control and Prevention (CDC). Prevention of pneumococcal disease among infants and children - use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine - recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010;59(RR-11):1-18.
6. Centers for Disease Control and Prevention (CDC). Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2012;61:816-819.
1. MacNeil J. Recommendations for use of MenACWY-CRM (Menveo) in infants at increased risk for meningococcal disease. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 23, 2013; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2013/04-MCV-MacNeil.pdf. Accessed February 12, 2014.
2. Centers for Disease Control and Prevention (CDC). Infant meningococcal vaccination: Advisory Committee on Immunization Practices (ACIP) recommendations and rationale. MMWR Morb Mortal Wkly Rep. 2013;62:52-54.
3. Centers for Disease Control and Prevention (CDC). Use of Japanese encephalitis vaccine in children: recommendations of the advisory committee on immunization practices, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:898-900.
4. Centers for Disease Control and Prevention (CDC). Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among children aged 6-18 years with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2013;62:521-524.
5. Nuorti JP, Whitney CG; Centers for Disease Control and Prevention (CDC). Prevention of pneumococcal disease among infants and children - use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine - recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010;59(RR-11):1-18.
6. Centers for Disease Control and Prevention (CDC). Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2012;61:816-819.
The new cardiovascular disease prevention guidelines: What you need to know
A significant milestone in evidence-based practice was reached in November 2013, when the American Heart Association and American College of Cardiology (AHA/ACC) published 4 clinical practice guidelines on the prevention of cardiovascular disease.1-4 These guidelines—on obesity, lifestyle management, cardiovascular disease (CVD) risk assessment, and cholesterol—were developed under the auspices of the National Heart, Lung, and Blood Institute (NHLBI) to update its prior guidelines on the treatment of hypertension, high cholesterol, and obesity that were published more than a decade ago.5-7 After the NHLBI had organized the respective guideline panels and progressed through most of the guideline development process (which lasted several years each), it arranged for the AHA/ACC to assume sponsorship and publication of the guidelines. The NHLBI decided its role should be to develop evidence reports, leaving the development of guidelines to professional organizations.
While the prior guidelines on hypertension and hypercholesterolemia were influential and widely cited as the standard of care, they were heavily influenced by expert opinion and were not strictly evidence based. The NHLBI sought to develop the new guidelines using more contemporary and rigorous evidence-based processes to meet standards set by the Institute of Medicine (IOM). The group started with key clinical questions, conducted comprehensive systematic reviews of the evidence, and then rated the quality of the evidence and assigned strength of recommendation ratings.8 The guidelines and evidence reports are lengthy, and are summarized below.
In December 2013, the Eighth Joint National Committee (the 5th panel organized by the NHLBI to address CVD prevention) published its updated guideline on the treatment of hypertension, which has also generated controversy. Visit www.jfponline.com to listen to an audiocast summary of these recommendations.9
Obesity and overweight
The guideline on managing obesity and overweight adults has 17 recommendations, only 3 of which are based on expert opinion.1 (TABLE 1 summarizes the strong [A] and moderate [B] recommendations.) The recommendations stress screening, diagnosis, and treatment using diet, exercise, and lifestyle modification. They also address bariatric surgery for those with a body mass index (BMI) ≥40 or a persisting BMI ≥35 despite weight loss interventions. This set of recommendations, like those of the United States Preventive Services Task Force, advises intensive interventions for weight management and additionally offers much more detail on recommended diet and exercise.
Lifestyle management
The 10 recommendations on lifestyle management to reduce cardiovascular risk, all evidence based, are limited to diet and exercise as a means to control hypertension and hypercholesterolemia.2 They do not cover other important lifestyle modifications for preventing CVD, such as smoking cessation. The guideline panel acknowledged that the interventions are aimed at those with high blood pressure and elevated cholesterol, but they encourage all adults to follow them. Although these recommendations are not particularly controversial, the 2 recommendations to reduce sodium intake are said to be based on strong or moderate strength evidence, in contrast to a recent IOM report that concluded evidence for the health benefits of salt intake <2.3 g/d is weak.10 This illustrates how separate authoritative groups can rate the strength of the same evidence differently.
Summary highlights:
• Encourage adults who would benefit from lowering either blood pressure (BP) or low-density lipoprotein cholesterol (LDL-C) to eat a diet that emphasizes vegetables, fruits, whole grains, low-fat dairy products, and other notably healthful foods, and to cut down on products high in sugar content and on red meats.
• Review, as appropriate, such options as the DASH (dietary approaches to stop hypertension) eating plan, US Department of Agriculture Food Patterns, or the American Heart Association’s diet.
• Establish a dietary plan that also incorporates nutritional requirements for an existing comorbidity, such as type 2 diabetes mellitus (T2DM).
• Lower saturated-fat intake to 5% to 6% of total calories, and reduce trans fats.
• Advise patients with high BP to reduce sodium consumption to ≤2400 mg/d; or, at the very least, to reduce daily consumption by 1000 mg.
• Promote aerobic activity to reduce either LDL-C or BP, at moderate or vigorous intensity 3 to 4 times a week with 40-minute sessions.
CVD risk assessment
The CVD risk assessment guideline3 has generated a lot of controversy. It proposes a new tool for assessing an individual’s 10-year risk of developing an atherosclerotic cardiovascular disease (ASCVD) event, defined as a fatal or nonfatal heart attack or stroke. While the tool is new, the risk factor categories it uses have been known for decades: age, gender, race, lipid levels, diabetes, smoking status, and BP. It has not performed better in validation studies than other existing tools (all of which are suboptimal), and it may be worse.11,12 Moreover, this new tool has been tested only in African Americans and non-Hispanic whites. Using it could classify 33 million adults age 40 to 79 years as having a 10-year risk of 7.5%, and 13 million a risk between 5% and 7.5%.12 The significance of this is discussed in the next section on the management of high cholesterol levels.
Summary highlights:
• Use race- and sex-specific Pooled Cohort Equations to predict 10-year risk for a first hard ASCVD event (nonfatalmyocardial infarction, coronary death, or nonfatal or fatal stroke) in non-Hispanic African Americans and non-Hispanic Whites, 40 to 79 years of age.
• Consider assessing a patient’s family history, high-sensitivity C-reactive protein, coronary artery calcium, or anklebrachial index to help guide treatment decisions if quantitative risk assessment has led to uncertainty. (This recommendation is based on expert opinion.)
• Consider evaluating ASCVD risk factors every 4 to 6 years in individuals 20 to 79 years of age who do not have ASCVD, and calculating the 10-year risk of an ASCVD event in those 40 to 79 years of age.
• Consider evaluating 30-year or lifetime ASCVD risk using traditional risk factors in individuals 20 to 59 years of age who do not have ASCVD and have no high short-term risk. (This is based on low-level evidence.)
Cholesterol management
The guideline on lowering blood cholesterol4 is a significant departure from the previous one.6 It contains 54 recommendations, 21 based on expert opinion. Using an unusual methodology that considered only randomized controlled trials in the evidence report, the guideline panel stated that the evidence demonstrates that 4 groups will benefit from treatment with statins:
• patients with established ASCVD
• individuals whose LDL-C is ≥190 mg/dL
• patients with diabetes and no established ASCVD who are 40 to 75 years of age and have an LDL-C between 70 and 189 mg/dL
• anyone with an estimated 10-year ASCVD risk of ≥7.5% (based on the new risk-assessment tool) and an LDL-C of 70 to 189 mg/dL.
The major departure from the old guideline is an abandonment of “treating to target” that attempts to lower LDL-C to a specified level. The panel concluded that the evidence does not show any benefit in achieving a specified level of LDL-C and that this approach can lead to either over- or under-treatment. The proposed new approach is to use high-, moderate-, or low-intensity statin treatment based on a patient’s age and reason for treatment, and the dose that they can tolerate (TABLE 2).4
Absent any contraindications, high-intensity treatment is indicated for:
• patients ≤75 years old with established ASCVD
• patients with an LDL-C level ≥190mg/dL
• patients 40 to 75 years old with diabetes and a ≥7.5% 10-year risk of ASCVD. z
Moderate-intensity treatment is indicated for those who cannot tolerate a high-intensity regimen, and for those ages 40 to 75 with diabetes and <7.5% 10-year ASCVD risk.
Low-intensity treatment is recommended for those who should receive moderate-intensity treatment but cannot tolerate it.
For those >75 years of age, the guideline makes only 2 recommendations:
• Prescribe a statin at the highest tolerable intensity for an LDL-C ≥190mg/dL.
• Assess those with established ASCVD for potential benefits and risks of moderate to high-intensity statin treatment. (It is reasonable to continue statin therapy for those already on it and tolerating it.)
Value of nonstatin drugs is questionable. In another significant departure from the previous guideline, the panel said that other cholesterol-lowering drugs can be considered when LDL-C remains high after statin treatment, but the benefit of these agents in preventing ASCVD is not proven.
Several objections to the new guideline have been raised in the short time since its release. Criticisms center on the large number of adults who would now qualify for statin treatment based on the new risk-assessment tool. Using the 7.5% 10-year risk cutoff, the number needed to treat to prevent one ASCVD event over 10 years would be 67. Also of concern to many is the fact that 7 out of 16 members of the guideline panel had financial ties to the pharmaceutical industry.12
Commentary
The new guidelines reflect a more rigorous evidence-based approach than those of the past. That some of them diverge significantly from previous recommendations that relied heavily on expert opinion reveals the pitfalls of making authoritative recommendations based on weak evidence. Such recommendations, especially those emerging from the National Institutes of Health, are used as national and international standards and serve as the basis of performance measures. When they do not stand the test of time because of a weak evidence base, medicine’s reputation is damaged. Notably, the new set of cholesterol recommendations, while an improvement from an evidentiary perspective, is founded partly on a questionable risk-assessment tool, and it is possible it will suffer the same long-term fate as its predecessor. (For more on these guidelines, see “The new cholesterol guideline: Beyond the headlines,” [J Fam Pract. 2013;62:730.])
1. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2013 Nov 12. [Epub ahead of print].
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC Guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
3. Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA Guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
4. Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421.
6. Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560-2572.
7. Clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S-209S.
8. Institute of Medicine. Clinical Practice Guidelines we can trust. Washington, DC: National Academy of Sciences; 2011.
9. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2013 Dec 18. [Epub ahead of print].
10. Institute of Medicine. Sodium intake in populations: assessment of evidence. Washington, DC: National Academy of Sciences; 2013.
11. Siontis GC, Tzoulaki I, Siontis KC, et al. Comparisons of established risk prediction models for cardiovascular disease: systematic review. BMJ. 2012;344:e3318.
12. Ioannidis JP. More than a billion people taking statins? Potential political implications of the new cardiovascular guidelines. JAMA. 2013 Dec 2. [Epub ahead of print].
A significant milestone in evidence-based practice was reached in November 2013, when the American Heart Association and American College of Cardiology (AHA/ACC) published 4 clinical practice guidelines on the prevention of cardiovascular disease.1-4 These guidelines—on obesity, lifestyle management, cardiovascular disease (CVD) risk assessment, and cholesterol—were developed under the auspices of the National Heart, Lung, and Blood Institute (NHLBI) to update its prior guidelines on the treatment of hypertension, high cholesterol, and obesity that were published more than a decade ago.5-7 After the NHLBI had organized the respective guideline panels and progressed through most of the guideline development process (which lasted several years each), it arranged for the AHA/ACC to assume sponsorship and publication of the guidelines. The NHLBI decided its role should be to develop evidence reports, leaving the development of guidelines to professional organizations.
While the prior guidelines on hypertension and hypercholesterolemia were influential and widely cited as the standard of care, they were heavily influenced by expert opinion and were not strictly evidence based. The NHLBI sought to develop the new guidelines using more contemporary and rigorous evidence-based processes to meet standards set by the Institute of Medicine (IOM). The group started with key clinical questions, conducted comprehensive systematic reviews of the evidence, and then rated the quality of the evidence and assigned strength of recommendation ratings.8 The guidelines and evidence reports are lengthy, and are summarized below.
In December 2013, the Eighth Joint National Committee (the 5th panel organized by the NHLBI to address CVD prevention) published its updated guideline on the treatment of hypertension, which has also generated controversy. Visit www.jfponline.com to listen to an audiocast summary of these recommendations.9
Obesity and overweight
The guideline on managing obesity and overweight adults has 17 recommendations, only 3 of which are based on expert opinion.1 (TABLE 1 summarizes the strong [A] and moderate [B] recommendations.) The recommendations stress screening, diagnosis, and treatment using diet, exercise, and lifestyle modification. They also address bariatric surgery for those with a body mass index (BMI) ≥40 or a persisting BMI ≥35 despite weight loss interventions. This set of recommendations, like those of the United States Preventive Services Task Force, advises intensive interventions for weight management and additionally offers much more detail on recommended diet and exercise.
Lifestyle management
The 10 recommendations on lifestyle management to reduce cardiovascular risk, all evidence based, are limited to diet and exercise as a means to control hypertension and hypercholesterolemia.2 They do not cover other important lifestyle modifications for preventing CVD, such as smoking cessation. The guideline panel acknowledged that the interventions are aimed at those with high blood pressure and elevated cholesterol, but they encourage all adults to follow them. Although these recommendations are not particularly controversial, the 2 recommendations to reduce sodium intake are said to be based on strong or moderate strength evidence, in contrast to a recent IOM report that concluded evidence for the health benefits of salt intake <2.3 g/d is weak.10 This illustrates how separate authoritative groups can rate the strength of the same evidence differently.
Summary highlights:
• Encourage adults who would benefit from lowering either blood pressure (BP) or low-density lipoprotein cholesterol (LDL-C) to eat a diet that emphasizes vegetables, fruits, whole grains, low-fat dairy products, and other notably healthful foods, and to cut down on products high in sugar content and on red meats.
• Review, as appropriate, such options as the DASH (dietary approaches to stop hypertension) eating plan, US Department of Agriculture Food Patterns, or the American Heart Association’s diet.
• Establish a dietary plan that also incorporates nutritional requirements for an existing comorbidity, such as type 2 diabetes mellitus (T2DM).
• Lower saturated-fat intake to 5% to 6% of total calories, and reduce trans fats.
• Advise patients with high BP to reduce sodium consumption to ≤2400 mg/d; or, at the very least, to reduce daily consumption by 1000 mg.
• Promote aerobic activity to reduce either LDL-C or BP, at moderate or vigorous intensity 3 to 4 times a week with 40-minute sessions.
CVD risk assessment
The CVD risk assessment guideline3 has generated a lot of controversy. It proposes a new tool for assessing an individual’s 10-year risk of developing an atherosclerotic cardiovascular disease (ASCVD) event, defined as a fatal or nonfatal heart attack or stroke. While the tool is new, the risk factor categories it uses have been known for decades: age, gender, race, lipid levels, diabetes, smoking status, and BP. It has not performed better in validation studies than other existing tools (all of which are suboptimal), and it may be worse.11,12 Moreover, this new tool has been tested only in African Americans and non-Hispanic whites. Using it could classify 33 million adults age 40 to 79 years as having a 10-year risk of 7.5%, and 13 million a risk between 5% and 7.5%.12 The significance of this is discussed in the next section on the management of high cholesterol levels.
Summary highlights:
• Use race- and sex-specific Pooled Cohort Equations to predict 10-year risk for a first hard ASCVD event (nonfatalmyocardial infarction, coronary death, or nonfatal or fatal stroke) in non-Hispanic African Americans and non-Hispanic Whites, 40 to 79 years of age.
• Consider assessing a patient’s family history, high-sensitivity C-reactive protein, coronary artery calcium, or anklebrachial index to help guide treatment decisions if quantitative risk assessment has led to uncertainty. (This recommendation is based on expert opinion.)
• Consider evaluating ASCVD risk factors every 4 to 6 years in individuals 20 to 79 years of age who do not have ASCVD, and calculating the 10-year risk of an ASCVD event in those 40 to 79 years of age.
• Consider evaluating 30-year or lifetime ASCVD risk using traditional risk factors in individuals 20 to 59 years of age who do not have ASCVD and have no high short-term risk. (This is based on low-level evidence.)
Cholesterol management
The guideline on lowering blood cholesterol4 is a significant departure from the previous one.6 It contains 54 recommendations, 21 based on expert opinion. Using an unusual methodology that considered only randomized controlled trials in the evidence report, the guideline panel stated that the evidence demonstrates that 4 groups will benefit from treatment with statins:
• patients with established ASCVD
• individuals whose LDL-C is ≥190 mg/dL
• patients with diabetes and no established ASCVD who are 40 to 75 years of age and have an LDL-C between 70 and 189 mg/dL
• anyone with an estimated 10-year ASCVD risk of ≥7.5% (based on the new risk-assessment tool) and an LDL-C of 70 to 189 mg/dL.
The major departure from the old guideline is an abandonment of “treating to target” that attempts to lower LDL-C to a specified level. The panel concluded that the evidence does not show any benefit in achieving a specified level of LDL-C and that this approach can lead to either over- or under-treatment. The proposed new approach is to use high-, moderate-, or low-intensity statin treatment based on a patient’s age and reason for treatment, and the dose that they can tolerate (TABLE 2).4
Absent any contraindications, high-intensity treatment is indicated for:
• patients ≤75 years old with established ASCVD
• patients with an LDL-C level ≥190mg/dL
• patients 40 to 75 years old with diabetes and a ≥7.5% 10-year risk of ASCVD. z
Moderate-intensity treatment is indicated for those who cannot tolerate a high-intensity regimen, and for those ages 40 to 75 with diabetes and <7.5% 10-year ASCVD risk.
Low-intensity treatment is recommended for those who should receive moderate-intensity treatment but cannot tolerate it.
For those >75 years of age, the guideline makes only 2 recommendations:
• Prescribe a statin at the highest tolerable intensity for an LDL-C ≥190mg/dL.
• Assess those with established ASCVD for potential benefits and risks of moderate to high-intensity statin treatment. (It is reasonable to continue statin therapy for those already on it and tolerating it.)
Value of nonstatin drugs is questionable. In another significant departure from the previous guideline, the panel said that other cholesterol-lowering drugs can be considered when LDL-C remains high after statin treatment, but the benefit of these agents in preventing ASCVD is not proven.
Several objections to the new guideline have been raised in the short time since its release. Criticisms center on the large number of adults who would now qualify for statin treatment based on the new risk-assessment tool. Using the 7.5% 10-year risk cutoff, the number needed to treat to prevent one ASCVD event over 10 years would be 67. Also of concern to many is the fact that 7 out of 16 members of the guideline panel had financial ties to the pharmaceutical industry.12
Commentary
The new guidelines reflect a more rigorous evidence-based approach than those of the past. That some of them diverge significantly from previous recommendations that relied heavily on expert opinion reveals the pitfalls of making authoritative recommendations based on weak evidence. Such recommendations, especially those emerging from the National Institutes of Health, are used as national and international standards and serve as the basis of performance measures. When they do not stand the test of time because of a weak evidence base, medicine’s reputation is damaged. Notably, the new set of cholesterol recommendations, while an improvement from an evidentiary perspective, is founded partly on a questionable risk-assessment tool, and it is possible it will suffer the same long-term fate as its predecessor. (For more on these guidelines, see “The new cholesterol guideline: Beyond the headlines,” [J Fam Pract. 2013;62:730.])
A significant milestone in evidence-based practice was reached in November 2013, when the American Heart Association and American College of Cardiology (AHA/ACC) published 4 clinical practice guidelines on the prevention of cardiovascular disease.1-4 These guidelines—on obesity, lifestyle management, cardiovascular disease (CVD) risk assessment, and cholesterol—were developed under the auspices of the National Heart, Lung, and Blood Institute (NHLBI) to update its prior guidelines on the treatment of hypertension, high cholesterol, and obesity that were published more than a decade ago.5-7 After the NHLBI had organized the respective guideline panels and progressed through most of the guideline development process (which lasted several years each), it arranged for the AHA/ACC to assume sponsorship and publication of the guidelines. The NHLBI decided its role should be to develop evidence reports, leaving the development of guidelines to professional organizations.
While the prior guidelines on hypertension and hypercholesterolemia were influential and widely cited as the standard of care, they were heavily influenced by expert opinion and were not strictly evidence based. The NHLBI sought to develop the new guidelines using more contemporary and rigorous evidence-based processes to meet standards set by the Institute of Medicine (IOM). The group started with key clinical questions, conducted comprehensive systematic reviews of the evidence, and then rated the quality of the evidence and assigned strength of recommendation ratings.8 The guidelines and evidence reports are lengthy, and are summarized below.
In December 2013, the Eighth Joint National Committee (the 5th panel organized by the NHLBI to address CVD prevention) published its updated guideline on the treatment of hypertension, which has also generated controversy. Visit www.jfponline.com to listen to an audiocast summary of these recommendations.9
Obesity and overweight
The guideline on managing obesity and overweight adults has 17 recommendations, only 3 of which are based on expert opinion.1 (TABLE 1 summarizes the strong [A] and moderate [B] recommendations.) The recommendations stress screening, diagnosis, and treatment using diet, exercise, and lifestyle modification. They also address bariatric surgery for those with a body mass index (BMI) ≥40 or a persisting BMI ≥35 despite weight loss interventions. This set of recommendations, like those of the United States Preventive Services Task Force, advises intensive interventions for weight management and additionally offers much more detail on recommended diet and exercise.
Lifestyle management
The 10 recommendations on lifestyle management to reduce cardiovascular risk, all evidence based, are limited to diet and exercise as a means to control hypertension and hypercholesterolemia.2 They do not cover other important lifestyle modifications for preventing CVD, such as smoking cessation. The guideline panel acknowledged that the interventions are aimed at those with high blood pressure and elevated cholesterol, but they encourage all adults to follow them. Although these recommendations are not particularly controversial, the 2 recommendations to reduce sodium intake are said to be based on strong or moderate strength evidence, in contrast to a recent IOM report that concluded evidence for the health benefits of salt intake <2.3 g/d is weak.10 This illustrates how separate authoritative groups can rate the strength of the same evidence differently.
Summary highlights:
• Encourage adults who would benefit from lowering either blood pressure (BP) or low-density lipoprotein cholesterol (LDL-C) to eat a diet that emphasizes vegetables, fruits, whole grains, low-fat dairy products, and other notably healthful foods, and to cut down on products high in sugar content and on red meats.
• Review, as appropriate, such options as the DASH (dietary approaches to stop hypertension) eating plan, US Department of Agriculture Food Patterns, or the American Heart Association’s diet.
• Establish a dietary plan that also incorporates nutritional requirements for an existing comorbidity, such as type 2 diabetes mellitus (T2DM).
• Lower saturated-fat intake to 5% to 6% of total calories, and reduce trans fats.
• Advise patients with high BP to reduce sodium consumption to ≤2400 mg/d; or, at the very least, to reduce daily consumption by 1000 mg.
• Promote aerobic activity to reduce either LDL-C or BP, at moderate or vigorous intensity 3 to 4 times a week with 40-minute sessions.
CVD risk assessment
The CVD risk assessment guideline3 has generated a lot of controversy. It proposes a new tool for assessing an individual’s 10-year risk of developing an atherosclerotic cardiovascular disease (ASCVD) event, defined as a fatal or nonfatal heart attack or stroke. While the tool is new, the risk factor categories it uses have been known for decades: age, gender, race, lipid levels, diabetes, smoking status, and BP. It has not performed better in validation studies than other existing tools (all of which are suboptimal), and it may be worse.11,12 Moreover, this new tool has been tested only in African Americans and non-Hispanic whites. Using it could classify 33 million adults age 40 to 79 years as having a 10-year risk of 7.5%, and 13 million a risk between 5% and 7.5%.12 The significance of this is discussed in the next section on the management of high cholesterol levels.
Summary highlights:
• Use race- and sex-specific Pooled Cohort Equations to predict 10-year risk for a first hard ASCVD event (nonfatalmyocardial infarction, coronary death, or nonfatal or fatal stroke) in non-Hispanic African Americans and non-Hispanic Whites, 40 to 79 years of age.
• Consider assessing a patient’s family history, high-sensitivity C-reactive protein, coronary artery calcium, or anklebrachial index to help guide treatment decisions if quantitative risk assessment has led to uncertainty. (This recommendation is based on expert opinion.)
• Consider evaluating ASCVD risk factors every 4 to 6 years in individuals 20 to 79 years of age who do not have ASCVD, and calculating the 10-year risk of an ASCVD event in those 40 to 79 years of age.
• Consider evaluating 30-year or lifetime ASCVD risk using traditional risk factors in individuals 20 to 59 years of age who do not have ASCVD and have no high short-term risk. (This is based on low-level evidence.)
Cholesterol management
The guideline on lowering blood cholesterol4 is a significant departure from the previous one.6 It contains 54 recommendations, 21 based on expert opinion. Using an unusual methodology that considered only randomized controlled trials in the evidence report, the guideline panel stated that the evidence demonstrates that 4 groups will benefit from treatment with statins:
• patients with established ASCVD
• individuals whose LDL-C is ≥190 mg/dL
• patients with diabetes and no established ASCVD who are 40 to 75 years of age and have an LDL-C between 70 and 189 mg/dL
• anyone with an estimated 10-year ASCVD risk of ≥7.5% (based on the new risk-assessment tool) and an LDL-C of 70 to 189 mg/dL.
The major departure from the old guideline is an abandonment of “treating to target” that attempts to lower LDL-C to a specified level. The panel concluded that the evidence does not show any benefit in achieving a specified level of LDL-C and that this approach can lead to either over- or under-treatment. The proposed new approach is to use high-, moderate-, or low-intensity statin treatment based on a patient’s age and reason for treatment, and the dose that they can tolerate (TABLE 2).4
Absent any contraindications, high-intensity treatment is indicated for:
• patients ≤75 years old with established ASCVD
• patients with an LDL-C level ≥190mg/dL
• patients 40 to 75 years old with diabetes and a ≥7.5% 10-year risk of ASCVD. z
Moderate-intensity treatment is indicated for those who cannot tolerate a high-intensity regimen, and for those ages 40 to 75 with diabetes and <7.5% 10-year ASCVD risk.
Low-intensity treatment is recommended for those who should receive moderate-intensity treatment but cannot tolerate it.
For those >75 years of age, the guideline makes only 2 recommendations:
• Prescribe a statin at the highest tolerable intensity for an LDL-C ≥190mg/dL.
• Assess those with established ASCVD for potential benefits and risks of moderate to high-intensity statin treatment. (It is reasonable to continue statin therapy for those already on it and tolerating it.)
Value of nonstatin drugs is questionable. In another significant departure from the previous guideline, the panel said that other cholesterol-lowering drugs can be considered when LDL-C remains high after statin treatment, but the benefit of these agents in preventing ASCVD is not proven.
Several objections to the new guideline have been raised in the short time since its release. Criticisms center on the large number of adults who would now qualify for statin treatment based on the new risk-assessment tool. Using the 7.5% 10-year risk cutoff, the number needed to treat to prevent one ASCVD event over 10 years would be 67. Also of concern to many is the fact that 7 out of 16 members of the guideline panel had financial ties to the pharmaceutical industry.12
Commentary
The new guidelines reflect a more rigorous evidence-based approach than those of the past. That some of them diverge significantly from previous recommendations that relied heavily on expert opinion reveals the pitfalls of making authoritative recommendations based on weak evidence. Such recommendations, especially those emerging from the National Institutes of Health, are used as national and international standards and serve as the basis of performance measures. When they do not stand the test of time because of a weak evidence base, medicine’s reputation is damaged. Notably, the new set of cholesterol recommendations, while an improvement from an evidentiary perspective, is founded partly on a questionable risk-assessment tool, and it is possible it will suffer the same long-term fate as its predecessor. (For more on these guidelines, see “The new cholesterol guideline: Beyond the headlines,” [J Fam Pract. 2013;62:730.])
1. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2013 Nov 12. [Epub ahead of print].
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC Guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
3. Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA Guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
4. Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421.
6. Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560-2572.
7. Clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S-209S.
8. Institute of Medicine. Clinical Practice Guidelines we can trust. Washington, DC: National Academy of Sciences; 2011.
9. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2013 Dec 18. [Epub ahead of print].
10. Institute of Medicine. Sodium intake in populations: assessment of evidence. Washington, DC: National Academy of Sciences; 2013.
11. Siontis GC, Tzoulaki I, Siontis KC, et al. Comparisons of established risk prediction models for cardiovascular disease: systematic review. BMJ. 2012;344:e3318.
12. Ioannidis JP. More than a billion people taking statins? Potential political implications of the new cardiovascular guidelines. JAMA. 2013 Dec 2. [Epub ahead of print].
1. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2013 Nov 12. [Epub ahead of print].
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC Guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
3. Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA Guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
4. Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Nov 12. [Epub ahead of print].
5. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421.
6. Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560-2572.
7. Clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S-209S.
8. Institute of Medicine. Clinical Practice Guidelines we can trust. Washington, DC: National Academy of Sciences; 2011.
9. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2013 Dec 18. [Epub ahead of print].
10. Institute of Medicine. Sodium intake in populations: assessment of evidence. Washington, DC: National Academy of Sciences; 2013.
11. Siontis GC, Tzoulaki I, Siontis KC, et al. Comparisons of established risk prediction models for cardiovascular disease: systematic review. BMJ. 2012;344:e3318.
12. Ioannidis JP. More than a billion people taking statins? Potential political implications of the new cardiovascular guidelines. JAMA. 2013 Dec 2. [Epub ahead of print].