User login
Pregnancy and safety rates evaluated for Liletta at 5 years of use
Liletta, a levonorgestrel 52 mg contraceptive intrauterine system (IUS) (Allergan), is currently approved by the US Food and Drug Administration for up to 4 years of use. A multicenter trial is continuing to measure Liletta’s efficacy and safety for a total of 8 years of use.1
Meanwhile, investigators led by Stephanie B. Teal, MD, from the University of Colorado, Aurora, have evaluated the 5-year data for Liletta. Resea
Study details
A total of 1,714 women aged 16−45 years were enrolled in the multicenter study for 5 years after successful IUS placement. This included 146 women aged 36−45 years who received the IUS for safety evaluation only, and 1,568 women aged 16−35 years who were evaluated for both safety and efficacy.1
Results of the study
The 16−35-year-old participants included 1,011 (57.7%) nulliparous and 438 (25.1%) obese women. Among these participants, 9 pregnancies occurred, including 4 in nulliparous women and 1 in an obese woman. In this age group, 1 pregnancy occurred after perforation and 1 following expulsion. Six (67%) of the pregnancies were ectopic.1
The Pearl Index in the first year was .15 (95% confidence interval [CI], .02−.55). Cumulative life-table pregnancy rates at the end of years 3 and 5 were .59 (95% CI, .28−1.25) and .92 (95% CI, .46–1.82), respectively.1
Of the total participants, perforation occurred in 2 (0.1%) women, both within the first year. Expulsion occurred in 63 participants (3.7%), most (50 [80.6%]) during the first year. Eleven patients (0.6%) were found to have a pelvic infection. Thirty-nine women (2.3%) discontinued use of Liletta due to bleeding complaints, primarily (n = 29 [74.3%]) in the first year.1
Conclusion
The researchers concluded that Liletta is highly effective and has an excellent safety profile over 5 years of use. Most adverse effects, including expulsion and discontinuation for bleeding, occurred during the first year.1
- Teal SB, Turok DK, Jensen JT, Chen BA, Kimble TD, Creinin MD. Five-year efficacy and safety of the Liletta® Levonorgestrel Intrauterine System. Obstet Gynecol. 2018;131(5 suppl):66S−67S.
Liletta, a levonorgestrel 52 mg contraceptive intrauterine system (IUS) (Allergan), is currently approved by the US Food and Drug Administration for up to 4 years of use. A multicenter trial is continuing to measure Liletta’s efficacy and safety for a total of 8 years of use.1
Meanwhile, investigators led by Stephanie B. Teal, MD, from the University of Colorado, Aurora, have evaluated the 5-year data for Liletta. Resea
Study details
A total of 1,714 women aged 16−45 years were enrolled in the multicenter study for 5 years after successful IUS placement. This included 146 women aged 36−45 years who received the IUS for safety evaluation only, and 1,568 women aged 16−35 years who were evaluated for both safety and efficacy.1
Results of the study
The 16−35-year-old participants included 1,011 (57.7%) nulliparous and 438 (25.1%) obese women. Among these participants, 9 pregnancies occurred, including 4 in nulliparous women and 1 in an obese woman. In this age group, 1 pregnancy occurred after perforation and 1 following expulsion. Six (67%) of the pregnancies were ectopic.1
The Pearl Index in the first year was .15 (95% confidence interval [CI], .02−.55). Cumulative life-table pregnancy rates at the end of years 3 and 5 were .59 (95% CI, .28−1.25) and .92 (95% CI, .46–1.82), respectively.1
Of the total participants, perforation occurred in 2 (0.1%) women, both within the first year. Expulsion occurred in 63 participants (3.7%), most (50 [80.6%]) during the first year. Eleven patients (0.6%) were found to have a pelvic infection. Thirty-nine women (2.3%) discontinued use of Liletta due to bleeding complaints, primarily (n = 29 [74.3%]) in the first year.1
Conclusion
The researchers concluded that Liletta is highly effective and has an excellent safety profile over 5 years of use. Most adverse effects, including expulsion and discontinuation for bleeding, occurred during the first year.1
Liletta, a levonorgestrel 52 mg contraceptive intrauterine system (IUS) (Allergan), is currently approved by the US Food and Drug Administration for up to 4 years of use. A multicenter trial is continuing to measure Liletta’s efficacy and safety for a total of 8 years of use.1
Meanwhile, investigators led by Stephanie B. Teal, MD, from the University of Colorado, Aurora, have evaluated the 5-year data for Liletta. Resea
Study details
A total of 1,714 women aged 16−45 years were enrolled in the multicenter study for 5 years after successful IUS placement. This included 146 women aged 36−45 years who received the IUS for safety evaluation only, and 1,568 women aged 16−35 years who were evaluated for both safety and efficacy.1
Results of the study
The 16−35-year-old participants included 1,011 (57.7%) nulliparous and 438 (25.1%) obese women. Among these participants, 9 pregnancies occurred, including 4 in nulliparous women and 1 in an obese woman. In this age group, 1 pregnancy occurred after perforation and 1 following expulsion. Six (67%) of the pregnancies were ectopic.1
The Pearl Index in the first year was .15 (95% confidence interval [CI], .02−.55). Cumulative life-table pregnancy rates at the end of years 3 and 5 were .59 (95% CI, .28−1.25) and .92 (95% CI, .46–1.82), respectively.1
Of the total participants, perforation occurred in 2 (0.1%) women, both within the first year. Expulsion occurred in 63 participants (3.7%), most (50 [80.6%]) during the first year. Eleven patients (0.6%) were found to have a pelvic infection. Thirty-nine women (2.3%) discontinued use of Liletta due to bleeding complaints, primarily (n = 29 [74.3%]) in the first year.1
Conclusion
The researchers concluded that Liletta is highly effective and has an excellent safety profile over 5 years of use. Most adverse effects, including expulsion and discontinuation for bleeding, occurred during the first year.1
- Teal SB, Turok DK, Jensen JT, Chen BA, Kimble TD, Creinin MD. Five-year efficacy and safety of the Liletta® Levonorgestrel Intrauterine System. Obstet Gynecol. 2018;131(5 suppl):66S−67S.
- Teal SB, Turok DK, Jensen JT, Chen BA, Kimble TD, Creinin MD. Five-year efficacy and safety of the Liletta® Levonorgestrel Intrauterine System. Obstet Gynecol. 2018;131(5 suppl):66S−67S.
FDA issues safety measures for all gadolinium-based contrast agents for MRI
A US Food & Drug Administration (FDA) Drug Safety Communication concerning a New Class Warning for all gadolinium-based contrast agents (GBCAs) for magnetic resonance imaging (MRI) has been released. Gadolinium has been found to remain in patients’ bodies, including the brain, for months to years.1
The FDA concluded that the benefit of all approved GBCAs outweighs any potential risks because gadolinium retention has not been directly linked to adverse health effects in patients with normal kidney function. To date, the only known adverse health effect related to gadolinium retention is a rare condition called nephrogenic systemic fibrosis that occurs in a small subgroup of patients with preexisting kidney failure. However, the FDA has recently received reports of adverse events involving multiple organ systems in patients with normal kidney function.1
After a review by the Medical Imaging Drugs Advisory Committee, the FDA is requiring several actions1:
- the development of a new Patient Medication Guide for GBCAs
- a requirement that every patient must read educational information before receiving a GBCA
- manufacturers of GBCAs must conduct human and animal studies to further assess the safety of these contrast agents.
FDA recommendations for your practice
The FDA advises that health care professionals should consider the retention characteristics of each agent when choosing a GBCA for patients who might be of higher risk for gadolinium retention.1,2 These patients include1:
- those requiring multiple lifetime doses
- pregnant women
- children
- patients with inflammatory conditions.
There are 2 types of GBCAs based on chemical structure: linear and macrocyclic. Linear GBCAs result in more retention and retention for a longer time than macrocyclic GBCAs.2 A list of FDA-approved GBCAs with their chemical structures is found here: https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm.2
Recommendations also state that repeated GBCA imaging studies be minimized when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be avoided or deferred.1
Report adverse effects
Health care professionals and patients are encouraged to report adverse effects or side effects related to the use of GBCAs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program found here: https://www.accessdata.fda.gov/scripts/medwatch/index.cfm?action=reporting.home.
- US Food & Drug Administration. Safety: Gadolinium-based Contrast Agents (GBCAs): Drug Safety Communication - Retained in Body; New Class Warnings. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm589580.htm. Published December 19, 2017. Accessed January 10, 2018.
- US Food & Drug Administration. Drugs: FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warning. https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm. Published December 19, 2017. Accessed January 10, 2018.
A US Food & Drug Administration (FDA) Drug Safety Communication concerning a New Class Warning for all gadolinium-based contrast agents (GBCAs) for magnetic resonance imaging (MRI) has been released. Gadolinium has been found to remain in patients’ bodies, including the brain, for months to years.1
The FDA concluded that the benefit of all approved GBCAs outweighs any potential risks because gadolinium retention has not been directly linked to adverse health effects in patients with normal kidney function. To date, the only known adverse health effect related to gadolinium retention is a rare condition called nephrogenic systemic fibrosis that occurs in a small subgroup of patients with preexisting kidney failure. However, the FDA has recently received reports of adverse events involving multiple organ systems in patients with normal kidney function.1
After a review by the Medical Imaging Drugs Advisory Committee, the FDA is requiring several actions1:
- the development of a new Patient Medication Guide for GBCAs
- a requirement that every patient must read educational information before receiving a GBCA
- manufacturers of GBCAs must conduct human and animal studies to further assess the safety of these contrast agents.
FDA recommendations for your practice
The FDA advises that health care professionals should consider the retention characteristics of each agent when choosing a GBCA for patients who might be of higher risk for gadolinium retention.1,2 These patients include1:
- those requiring multiple lifetime doses
- pregnant women
- children
- patients with inflammatory conditions.
There are 2 types of GBCAs based on chemical structure: linear and macrocyclic. Linear GBCAs result in more retention and retention for a longer time than macrocyclic GBCAs.2 A list of FDA-approved GBCAs with their chemical structures is found here: https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm.2
Recommendations also state that repeated GBCA imaging studies be minimized when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be avoided or deferred.1
Report adverse effects
Health care professionals and patients are encouraged to report adverse effects or side effects related to the use of GBCAs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program found here: https://www.accessdata.fda.gov/scripts/medwatch/index.cfm?action=reporting.home.
A US Food & Drug Administration (FDA) Drug Safety Communication concerning a New Class Warning for all gadolinium-based contrast agents (GBCAs) for magnetic resonance imaging (MRI) has been released. Gadolinium has been found to remain in patients’ bodies, including the brain, for months to years.1
The FDA concluded that the benefit of all approved GBCAs outweighs any potential risks because gadolinium retention has not been directly linked to adverse health effects in patients with normal kidney function. To date, the only known adverse health effect related to gadolinium retention is a rare condition called nephrogenic systemic fibrosis that occurs in a small subgroup of patients with preexisting kidney failure. However, the FDA has recently received reports of adverse events involving multiple organ systems in patients with normal kidney function.1
After a review by the Medical Imaging Drugs Advisory Committee, the FDA is requiring several actions1:
- the development of a new Patient Medication Guide for GBCAs
- a requirement that every patient must read educational information before receiving a GBCA
- manufacturers of GBCAs must conduct human and animal studies to further assess the safety of these contrast agents.
FDA recommendations for your practice
The FDA advises that health care professionals should consider the retention characteristics of each agent when choosing a GBCA for patients who might be of higher risk for gadolinium retention.1,2 These patients include1:
- those requiring multiple lifetime doses
- pregnant women
- children
- patients with inflammatory conditions.
There are 2 types of GBCAs based on chemical structure: linear and macrocyclic. Linear GBCAs result in more retention and retention for a longer time than macrocyclic GBCAs.2 A list of FDA-approved GBCAs with their chemical structures is found here: https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm.2
Recommendations also state that repeated GBCA imaging studies be minimized when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be avoided or deferred.1
Report adverse effects
Health care professionals and patients are encouraged to report adverse effects or side effects related to the use of GBCAs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program found here: https://www.accessdata.fda.gov/scripts/medwatch/index.cfm?action=reporting.home.
- US Food & Drug Administration. Safety: Gadolinium-based Contrast Agents (GBCAs): Drug Safety Communication - Retained in Body; New Class Warnings. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm589580.htm. Published December 19, 2017. Accessed January 10, 2018.
- US Food & Drug Administration. Drugs: FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warning. https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm. Published December 19, 2017. Accessed January 10, 2018.
- US Food & Drug Administration. Safety: Gadolinium-based Contrast Agents (GBCAs): Drug Safety Communication - Retained in Body; New Class Warnings. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm589580.htm. Published December 19, 2017. Accessed January 10, 2018.
- US Food & Drug Administration. Drugs: FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warning. https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm. Published December 19, 2017. Accessed January 10, 2018.
Clinical implications of cesarean-induced isthmoceles
In a presentation of the Golden Hysteroscope Award Best Paper on Hysteroscopy at the 46th AAGL Global Congress on Minimally Invasive Surgery in National Harbor, Maryland, James Coad, MD, described a study that he and colleagues from West Virginia University School of Medicine in Morgantown, and Universidad Autónoma de Nuevo León in Monterrey, Mexico, conducted concerning the healing differences of cesarean incisions and the development of isthmoceles (cesarean scar defects).1
Detecting isthmoceles
Isthmoceles are variably sized evaginations into the anterior lower uterine segment at a previous cesarean delivery incision due to suboptimal myometrium healing. This leads to thinning of the anterior uterine wall, which creates an indentation and fluid-filled pouch at the cesarean scar site.1,2
Recent findings, say Coad and colleagues, associate isthmoceles with adverse reproductive and gynecologic conditions such as infertility, postmenstrual spotting, dysmenorrhea, and chronic pelvic pain. Patients who have undergone multiple cesarean deliveries tend to have larger isthmoceles with widths correlating to increased symptoms.1
While the presence of inner nonunion healing can be hysteroscopically visualized, it is difficult to detect outer nonunion healing. The reported incidence of isthmoceles differs by imaging technique used: up to 70% are found with transvaginal ultrasound, and up to 84% are detected by sonohysterography.3,4 This study found that 98% of isthomoceles can be detected by gross examination.1
Related article:
Cesarean scar defect: What is it and how should it be treated?
Study details
Researchers designed a prospective de-identified anatomic pathology study to evaluate the anatomy of uteri from 204 premenopausal women who underwent hysterectomy for benign disease due to abnormal uterine bleeding, fibroids, and/or adenomyosis. Uteri were midline sagittally sectioned and the area of cesarean section anatomy was documented, including the presence of inner and outer nonunion healing.1
Of the 204 uteri, 134 (66%) had at least 1 identifiable cesarean scar (22% had 1 scar, 19% had 2 scars, and 25% had 3 or more scars). Of these, 2 uteri (1.5%) had intact incisional healing with minimal wall narrowing showing complete union healing. Isolated inner nonunion healing with the formation of prominent isthmoceles was found in 111 uteri (82.8%). Five uteri (3.7%) showed isolated outer nonunion healing without the formation of isthmoceles. Fourteen uteri (10.5%) had both inner and outer nonunion healing. Two uteri (1.5%) had complete transmural union healing with localized loss of anterior lower segment wall integrity. No isthmoceles were detected in women who had not undergone cesarean delivery.1
Study results
When present, inner nonunion healing involved a mean (SD) 39% (23%; range, 5% – 90%) of the wall thickness and outer nonunion healing involved a mean (SD) 27% (17%; range, 10% – 60%). Due to nonunion healing, the resultant wall thicknesses at cesarean scar site were a mean (SD) 5.6 mm ( 2.60 mm; range, 0.0 mm – 14.2 mm). When compared with the adjacent uterine wall, the nonunion healing resulted in an approximate mean (SD) of 70% (16%) thinner wall. 1
Conclusions and a warning
The authors concluded that, following cesarean delivery, there is a high incidence of architectural healing–related change, including significant inner and outer wall thinning. While inner nonunion healing can be hysteroscopically visualized, outer-wall healing cannot be visualized and may result in finding a thinner wall than expected during procedures in this region, including isthmocele repairs.1
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Coad JE, Fugett II JH, Wolfe T, et al. Anatomy of cesarean-induced isthmoceles: Clinical implications [abstract 159]. In: Abstracts of the 46th AAGL Global Congress on Minimally Invasive Surgery. JMIG. 2017;24(7 suppl):S64.
- Nezhat C, Grace L, Soliemannjad R, Razavi GM, Nezhat A. Cesarean scar defect: What is it and how should it be treated? OBG Manag. 2016;28(4):32,34,36,38–39,53.
- Bij de Vaate AJ, van der Voet LF, Naji O, et al. Prevalenc, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: systematic review. Ultrasound Obstet Gynecol. 2014;43(4):372–382.
- Osser OV, Jokubkiene L, Valentin L. High prevalence of defects in Cesarean section scars at transvaginal ultrasound examination. Ultrasound Obstet Gynecol. 2009;34(1):90–97.
In a presentation of the Golden Hysteroscope Award Best Paper on Hysteroscopy at the 46th AAGL Global Congress on Minimally Invasive Surgery in National Harbor, Maryland, James Coad, MD, described a study that he and colleagues from West Virginia University School of Medicine in Morgantown, and Universidad Autónoma de Nuevo León in Monterrey, Mexico, conducted concerning the healing differences of cesarean incisions and the development of isthmoceles (cesarean scar defects).1
Detecting isthmoceles
Isthmoceles are variably sized evaginations into the anterior lower uterine segment at a previous cesarean delivery incision due to suboptimal myometrium healing. This leads to thinning of the anterior uterine wall, which creates an indentation and fluid-filled pouch at the cesarean scar site.1,2
Recent findings, say Coad and colleagues, associate isthmoceles with adverse reproductive and gynecologic conditions such as infertility, postmenstrual spotting, dysmenorrhea, and chronic pelvic pain. Patients who have undergone multiple cesarean deliveries tend to have larger isthmoceles with widths correlating to increased symptoms.1
While the presence of inner nonunion healing can be hysteroscopically visualized, it is difficult to detect outer nonunion healing. The reported incidence of isthmoceles differs by imaging technique used: up to 70% are found with transvaginal ultrasound, and up to 84% are detected by sonohysterography.3,4 This study found that 98% of isthomoceles can be detected by gross examination.1
Related article:
Cesarean scar defect: What is it and how should it be treated?
Study details
Researchers designed a prospective de-identified anatomic pathology study to evaluate the anatomy of uteri from 204 premenopausal women who underwent hysterectomy for benign disease due to abnormal uterine bleeding, fibroids, and/or adenomyosis. Uteri were midline sagittally sectioned and the area of cesarean section anatomy was documented, including the presence of inner and outer nonunion healing.1
Of the 204 uteri, 134 (66%) had at least 1 identifiable cesarean scar (22% had 1 scar, 19% had 2 scars, and 25% had 3 or more scars). Of these, 2 uteri (1.5%) had intact incisional healing with minimal wall narrowing showing complete union healing. Isolated inner nonunion healing with the formation of prominent isthmoceles was found in 111 uteri (82.8%). Five uteri (3.7%) showed isolated outer nonunion healing without the formation of isthmoceles. Fourteen uteri (10.5%) had both inner and outer nonunion healing. Two uteri (1.5%) had complete transmural union healing with localized loss of anterior lower segment wall integrity. No isthmoceles were detected in women who had not undergone cesarean delivery.1
Study results
When present, inner nonunion healing involved a mean (SD) 39% (23%; range, 5% – 90%) of the wall thickness and outer nonunion healing involved a mean (SD) 27% (17%; range, 10% – 60%). Due to nonunion healing, the resultant wall thicknesses at cesarean scar site were a mean (SD) 5.6 mm ( 2.60 mm; range, 0.0 mm – 14.2 mm). When compared with the adjacent uterine wall, the nonunion healing resulted in an approximate mean (SD) of 70% (16%) thinner wall. 1
Conclusions and a warning
The authors concluded that, following cesarean delivery, there is a high incidence of architectural healing–related change, including significant inner and outer wall thinning. While inner nonunion healing can be hysteroscopically visualized, outer-wall healing cannot be visualized and may result in finding a thinner wall than expected during procedures in this region, including isthmocele repairs.1
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In a presentation of the Golden Hysteroscope Award Best Paper on Hysteroscopy at the 46th AAGL Global Congress on Minimally Invasive Surgery in National Harbor, Maryland, James Coad, MD, described a study that he and colleagues from West Virginia University School of Medicine in Morgantown, and Universidad Autónoma de Nuevo León in Monterrey, Mexico, conducted concerning the healing differences of cesarean incisions and the development of isthmoceles (cesarean scar defects).1
Detecting isthmoceles
Isthmoceles are variably sized evaginations into the anterior lower uterine segment at a previous cesarean delivery incision due to suboptimal myometrium healing. This leads to thinning of the anterior uterine wall, which creates an indentation and fluid-filled pouch at the cesarean scar site.1,2
Recent findings, say Coad and colleagues, associate isthmoceles with adverse reproductive and gynecologic conditions such as infertility, postmenstrual spotting, dysmenorrhea, and chronic pelvic pain. Patients who have undergone multiple cesarean deliveries tend to have larger isthmoceles with widths correlating to increased symptoms.1
While the presence of inner nonunion healing can be hysteroscopically visualized, it is difficult to detect outer nonunion healing. The reported incidence of isthmoceles differs by imaging technique used: up to 70% are found with transvaginal ultrasound, and up to 84% are detected by sonohysterography.3,4 This study found that 98% of isthomoceles can be detected by gross examination.1
Related article:
Cesarean scar defect: What is it and how should it be treated?
Study details
Researchers designed a prospective de-identified anatomic pathology study to evaluate the anatomy of uteri from 204 premenopausal women who underwent hysterectomy for benign disease due to abnormal uterine bleeding, fibroids, and/or adenomyosis. Uteri were midline sagittally sectioned and the area of cesarean section anatomy was documented, including the presence of inner and outer nonunion healing.1
Of the 204 uteri, 134 (66%) had at least 1 identifiable cesarean scar (22% had 1 scar, 19% had 2 scars, and 25% had 3 or more scars). Of these, 2 uteri (1.5%) had intact incisional healing with minimal wall narrowing showing complete union healing. Isolated inner nonunion healing with the formation of prominent isthmoceles was found in 111 uteri (82.8%). Five uteri (3.7%) showed isolated outer nonunion healing without the formation of isthmoceles. Fourteen uteri (10.5%) had both inner and outer nonunion healing. Two uteri (1.5%) had complete transmural union healing with localized loss of anterior lower segment wall integrity. No isthmoceles were detected in women who had not undergone cesarean delivery.1
Study results
When present, inner nonunion healing involved a mean (SD) 39% (23%; range, 5% – 90%) of the wall thickness and outer nonunion healing involved a mean (SD) 27% (17%; range, 10% – 60%). Due to nonunion healing, the resultant wall thicknesses at cesarean scar site were a mean (SD) 5.6 mm ( 2.60 mm; range, 0.0 mm – 14.2 mm). When compared with the adjacent uterine wall, the nonunion healing resulted in an approximate mean (SD) of 70% (16%) thinner wall. 1
Conclusions and a warning
The authors concluded that, following cesarean delivery, there is a high incidence of architectural healing–related change, including significant inner and outer wall thinning. While inner nonunion healing can be hysteroscopically visualized, outer-wall healing cannot be visualized and may result in finding a thinner wall than expected during procedures in this region, including isthmocele repairs.1
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Coad JE, Fugett II JH, Wolfe T, et al. Anatomy of cesarean-induced isthmoceles: Clinical implications [abstract 159]. In: Abstracts of the 46th AAGL Global Congress on Minimally Invasive Surgery. JMIG. 2017;24(7 suppl):S64.
- Nezhat C, Grace L, Soliemannjad R, Razavi GM, Nezhat A. Cesarean scar defect: What is it and how should it be treated? OBG Manag. 2016;28(4):32,34,36,38–39,53.
- Bij de Vaate AJ, van der Voet LF, Naji O, et al. Prevalenc, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: systematic review. Ultrasound Obstet Gynecol. 2014;43(4):372–382.
- Osser OV, Jokubkiene L, Valentin L. High prevalence of defects in Cesarean section scars at transvaginal ultrasound examination. Ultrasound Obstet Gynecol. 2009;34(1):90–97.
- Coad JE, Fugett II JH, Wolfe T, et al. Anatomy of cesarean-induced isthmoceles: Clinical implications [abstract 159]. In: Abstracts of the 46th AAGL Global Congress on Minimally Invasive Surgery. JMIG. 2017;24(7 suppl):S64.
- Nezhat C, Grace L, Soliemannjad R, Razavi GM, Nezhat A. Cesarean scar defect: What is it and how should it be treated? OBG Manag. 2016;28(4):32,34,36,38–39,53.
- Bij de Vaate AJ, van der Voet LF, Naji O, et al. Prevalenc, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: systematic review. Ultrasound Obstet Gynecol. 2014;43(4):372–382.
- Osser OV, Jokubkiene L, Valentin L. High prevalence of defects in Cesarean section scars at transvaginal ultrasound examination. Ultrasound Obstet Gynecol. 2009;34(1):90–97.
ObGyns’ choice of practice environment is a big deal
ObGyns are mindfully choosing their practice environments. The trend, as reported by the American College of Obstetricians and Gynecologists (ACOG),1 shows movement from private practice to employment: an increasing number of ObGyns have joined large practices and are employed. Overall, fewer than half of US physicians owned their medical practice in 2016, reported the American Medical Association (AMA).2 This is the first time that the majority of physicians are not practice owners.
Although employed ObGyns earn 9% less than self-employed ObGyns, ($276,000 vs $300,000, respectively), trading a higher salary for less time spent on administrative tasks seems to be worth the pay cut, reports Medscape. Employed ObGyns reported receiving additional benefits that might not have been available to self-employed ObGyns: professional liability coverage, employer-subsidized health and dental insurance, paid time off, and a retirement plan with employer match.3
What matters to ObGyns when choosing a practice setting?
Several decisions about practice setting need to be made at the beginning and throughout a career, among them the type of practice, desired salary, work-life balance, (the latter 2 may be influenced by practice type), and location.
Type of practice
“Patients benefit when physicians practice in settings they find professionally and personally rewarding,” said AMA President Andrew W. Gurman, MD. “The AMA is committed to helping physicians navigate their practice options and offers innovative strategies and resources to ensure physicians in all practice sizes and setting can thrive in the changing health environment.”2
More and more, that environment is a practice wholly owned by physicians. The AMA reports that in 2016, 55.8% of physicians worked in such a practice (including physicians who have an ownership stake in the practice, those who are employed by the practice, and those who are independent contractors).2 An approximate 13.8% of physicians worked at practices with more than 50 physicians in 2016. The majority (57.8%), however, practiced in groups with 10 or fewer physicians. The most common practice type was the single-specialty group (42.8%), followed by the multispecialty group practice (24.6%).2
Paying physicians a salary instead of compensating them based on volume may improve physician satisfaction—it removes the need to deal with complex fee-for-service systems, say Ian Larkin, PhD, and George Loewenstein, PhD. In fee-for-service payment arrangements, physicians may be encouraged to order more tests and procedures because doing so may increase income. A better strategy, say Larkin and Loewenstein, is to switch to a straight salary system. Known for their quality of care and comparatively low costs, the Mayo Clinic, Cleveland Clinic, and Kaiser Permanente have successfully implemented this payment system.4
Related article:
ObGyn salaries jumped in the last year
Desired salary
The mean income for ObGyns rose by 3% in 2016 over 2015 ($286,000 compared with $277,000), according to Medscape.5 This jump follows a gradual increase over the last few years ($249,000 in 2014; $243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1,5,6
The highest earnings among all physicians were orthopedists ($489,000), plastic surgeons ($440,000), and cardiologists ($410,000). Pediatricians were the lowest paid physicians at $202,000.3
Fair compensation. Fewer than half (48%) of ObGyns who completed the Medscape survey felt they were fairly compensated in 2016, and 41% of those who were dissatisfied with their compensation believed they deserved to be earning between 11% and 25% more. When asked if they would still choose medicine, 72% of ObGyns answered affirmatively. Of those who would choose medicine again, 76% would choose obstetrics and gynecology once more.3
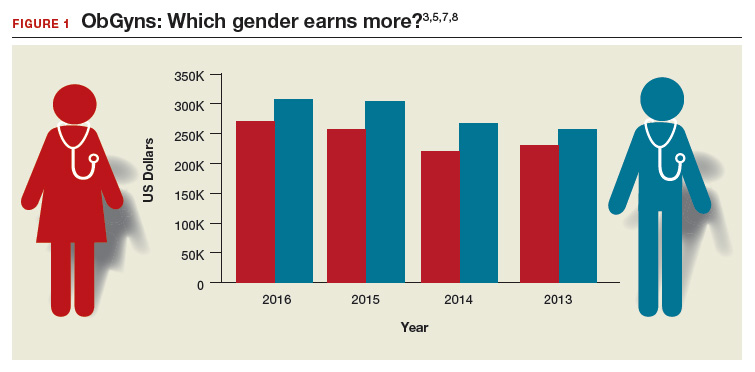
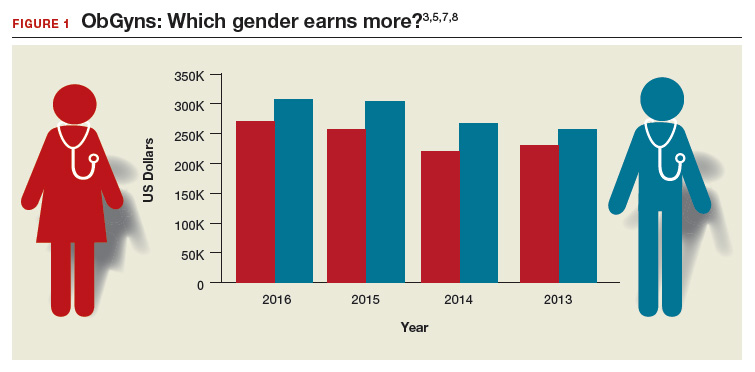
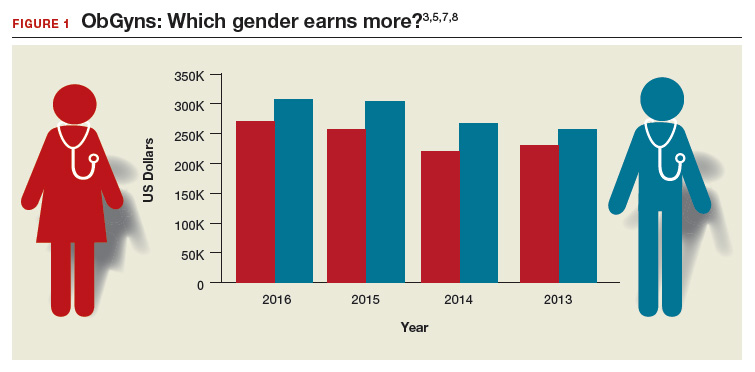
Gender differences. As in years past, full-time male ObGyns reported higher earnings (13%) than female ObGyns ($306,000 vs $270,000, respectively; (FIGURE 1).3,5,7,8
Among ObGyns who responded to the 2017 Medscape survey, 14% of women and 10% of men indicated that they work part-time.3 Last year, 13% of female ObGyns reported part-time employment versus 16% of male ObGyns.6
Among the ObGyns who answered the 2017 survey, there was a gender gap in participation related to race. Although more men than women responded to the survey, more women than men ObGyns among black/African American (women, 78%), Asian (women, 69%), and white/Caucasian (women, 53%) groups responded. Men outweighed women only among Hispanic/Latino ObGyns (60%) who answered the survey.3
Read about work-life balance, job satisfaction, and burnout
Work-life balance
ACOG predicts that mid-career and younger ObGyns will focus on work-life balance issues. Practice sites (ambulatory, hospital, or a combination) that offer part-time schedules or extra time for nonprofessional matters are becoming the most desirable to these practitioners.1
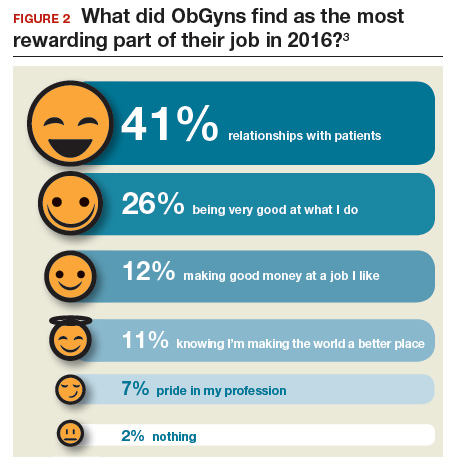
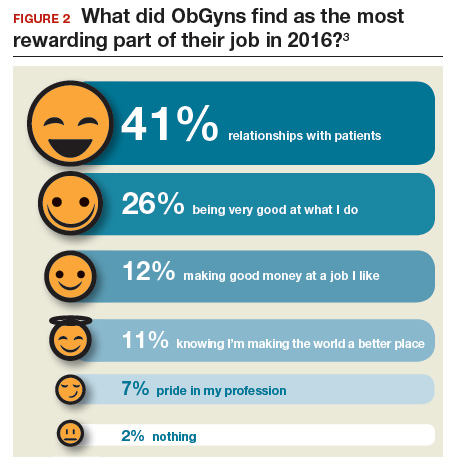
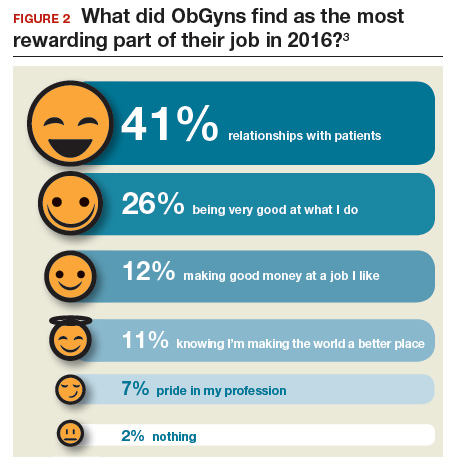
What satisfies and dissatisfies ObGyns? ObGyns reported to Medscape that their relationships with patients (41% of respondents) was the most rewarding part of their job (FIGURE 2).3
There are many job aspects that dissatisfy ObGyns, including1,3,9:
- too many bureaucratic tasks
- the short time allotted for each patient office visit
- electronic health records (EHR) and increased computerization
- not feeling appreciated or properly compensated
- spending too many hours at work
- the impact of regulatory changes on clinical practice.
Bureaucratic tasks remain a primary cause for burnout among all physicians.10 This year, 56% of all physicians reported spending 10 hours or more per week on paperwork and administrative tasks, up from 35% in the 2014 report. More than half (54%) of ObGyns reported spending 10 hours or more on paperwork.3 For every hour of face-to-face patient time, physicians spent nearly 2 additional hours on their EHR and administration tasks.9
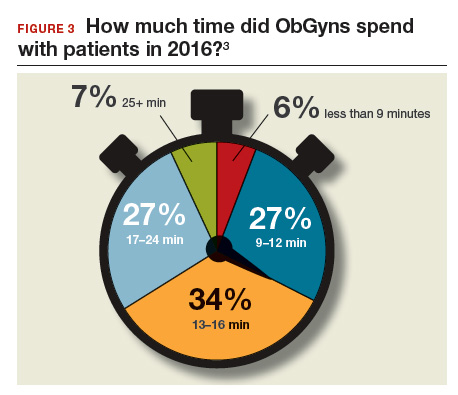
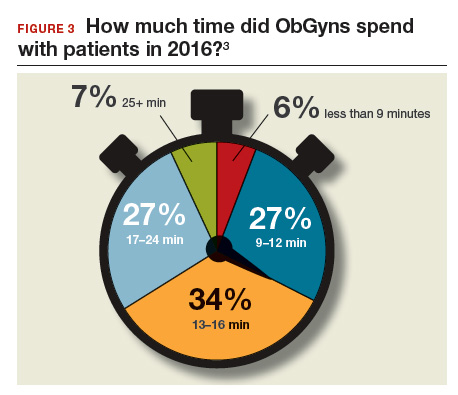
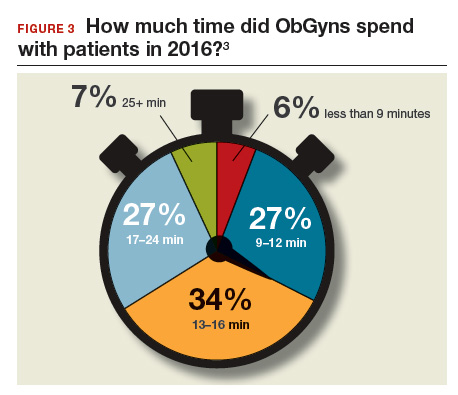
Time with patients. Medscape reported that 38% of ObGyns spent more than 45 hours per week with patients (FIGURE 3).
ACOG notes that ObGyns are increasingly referring patients to subspecialists, which frustrates patients and increases their costs.1
ObGyns rank high in burnout rates. Burnout rates for physicians are twice that of other working adults.1 ObGyns rank second (56%) in burn out (Emergency Medicine, 59%).10 When Medscape survey respondents were asked to grade their burnout level from 1 to 7 (1 = “It does not interfere with my life;” 7 = “It is so severe that I am thinking of leaving medicine altogether”), ObGyns ranked their burnout level at 4.3.10 Female physicians reported a higher percentage of burnout than their male colleagues (55% vs 45%, respectively).10 An estimated 40% to 75% of ObGyns experienced some level of burnout.1
According to ACOG, the specialty is included among the “noncontrollable” lifestyle specialties, especially for those aged 50 years or younger. Many Millennials (born 1980 to 2000) do not view their work and professional achievement as central to their lives; ObGyns aged younger than 35 years want to work fewer hours per week compared with their older colleagues, says ACOG. However, when this option is unavailable, an increasing number of Millennials report lowered job satisfaction.1
Related article:
What can administrators and ObGyns do together to reduce physician burnout?
Mindfulness about quality of life. The relationship of burnout to quality of life issues is gaining in awareness. In a recent
“We need to stop blaming individuals and treat physician burnout as a system issue…If it affects half our physicians, it is indirectly affecting half our patients,” notes Tait Shanafelt, MD, a hematologist and physician-burnout researcher at the Mayo Clinic.9 He says that burnout relates to a physician’s “professional spirit of life, and it primarily affects individuals whose work involves an intense interaction with people.”9
The Mayo Clinic in Minneapolis, Minnesota, has taken a lead in developing a space for their physicians to “reset” by offering a room where health professionals can retreat if they need a moment to recover from a traumatic event.9
Read about what factors attract ObGyns to specific locations
Location, location, location
Specific areas of the country are more attractive for their higher compensation rates. The highest average compensation was reported by ObGyns in the North Central area ($339,000), West ($301,000), and Great Lakes ($297,000) regions, while the lowest compensation rates were found in the Northwest ($260,000), Southwest ($268,000), and South Central ($275,000) areas.3
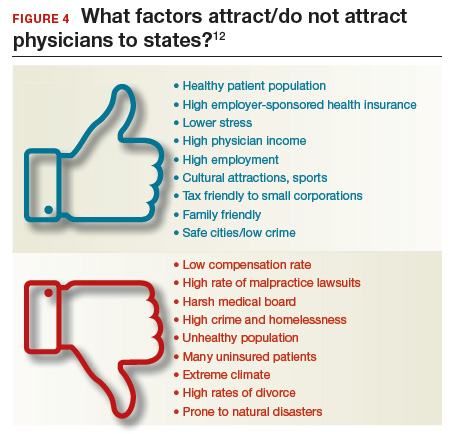
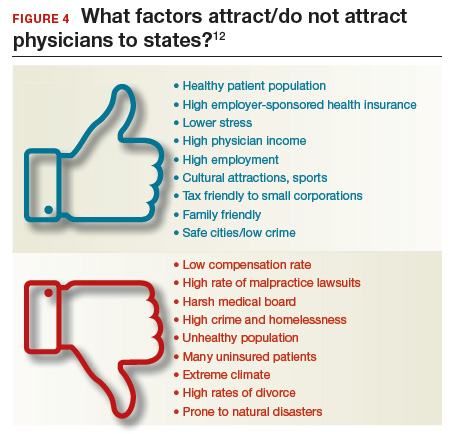
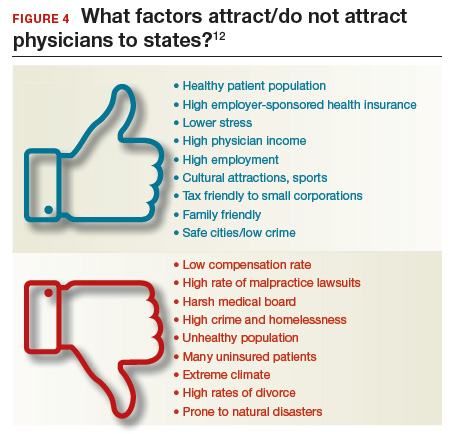
Key factors, such as healthy patient populations, higher rates of health insurance coverage, and lower stress levels attract physicians (FIGURE 4). Minnesota ranked the #1 best place to practice because it has the 4th healthiest population, 2nd highest rate of employer-sponsored health insurance, the 17th lowest number of malpractice lawsuits, and a medical board that is the 3rd least harsh in the nation.12 Unfortunate situations such as the highest malpractice rates per capita, least healthy population, 8th lowest rate of employer-sponsored health insurance, and the 9th lowest compensation rate for physicians make Louisiana the worst place to practice in 2017.12
Supply and demand creates substantial geographic imbalances in the number of ObGyns in the United States. ACOG pro-jects that the need for ObGyns will increase nationally by 6% in the next 10 years, although demand will vary geographically from a 27% increase in Nevada to an 11% decrease in West Virginia.1 Especially vulnerable states (Arizona, Washington, Utah, Idaho) currently have an insufficient supply of ObGyns and are projected to see an increased future demand. Florida, Texas, North Carolina, and Nevada will be at risk, according to ACOG, because the adult female population is expected to increase.1
2017 Medscape survey demographics
The Medscape Compensation Report 2017 is a based on the responses of 19,270 physicians across 27+ specialties, 5% of whom were ObGyns. Data were collected in an online survey conducted from December 20, 2016, to March 7, 2017.3
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- American Congress of Obstetricians and Gynecologists. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. https://www.acog.org/Resources-And-Publications/The-Ob-Gyn-Workforce/The-Obstetrician-Gynecologist-Workforce-in-the-United-States. Accessed June 7, 2017.
- Murphy B. For the first time, physician practice owners are not the majority. AMA Wire. https://wire.ama-assn.org/practice-management/first-time-physician-practice-owners-are-not-majority?utm_source=BulletinHealthCare&utm_medium=email&utm_term=060117&utm_content=general&utm_campaign=article_alert-morning_rounds_daily. Published May 31, 2017. Accessed June 7, 2017.
- Grisham S. Medscape Ob/Gyn Compensation Report 2017. Medscape Website. http://www.medscape.com/slideshow/compensation-2017-ob-gyn-6008576. Published April 12, 2017. Accessed June 7, 2017.
- Larkin I, Loewenstein G. Business model—Related conflict of interests in medicine: Problems and potential solutions. JAMA. 2017;317(17):1745–1746.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 7, 2017.
- Reale D, Christie K. ObGyn salaries jumped in the last year. OBG Manag. 2016;28(7):25–27, 30, 37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2015. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed July 24, 2017.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed July 24, 2017.
- Parks T. AMA burnout by specialty. AMA Wire. https://wire.ama-assn.org/life-career/report-reveals-severity-burnout-specialty. Published January 31, 2017. Accessed June 7, 2017.
- Peckham C. Medscape Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout. Medscape Website. http://www.medscape.com/features/slideshow/lifestyle/2017/overview#page=1. Published January 11, 2017. Accessed June 7, 2017.
- DiVenere L. ObGyn burnout: ACOG takes aim. OBG Manag. 2016;28(9):25,30,32,33.
- Page L. Best and Worst Places to Practice 2017. Medscape Website. http://www.medscape.com/slideshow/best-places-to-practice-2017-6008688?src=wnl_physrep_170510_mscpmrk_bestplaces2017&impID=1345406&faf. Published May 10, 2017. Accessed June 7, 2017.
ObGyns are mindfully choosing their practice environments. The trend, as reported by the American College of Obstetricians and Gynecologists (ACOG),1 shows movement from private practice to employment: an increasing number of ObGyns have joined large practices and are employed. Overall, fewer than half of US physicians owned their medical practice in 2016, reported the American Medical Association (AMA).2 This is the first time that the majority of physicians are not practice owners.
Although employed ObGyns earn 9% less than self-employed ObGyns, ($276,000 vs $300,000, respectively), trading a higher salary for less time spent on administrative tasks seems to be worth the pay cut, reports Medscape. Employed ObGyns reported receiving additional benefits that might not have been available to self-employed ObGyns: professional liability coverage, employer-subsidized health and dental insurance, paid time off, and a retirement plan with employer match.3
What matters to ObGyns when choosing a practice setting?
Several decisions about practice setting need to be made at the beginning and throughout a career, among them the type of practice, desired salary, work-life balance, (the latter 2 may be influenced by practice type), and location.
Type of practice
“Patients benefit when physicians practice in settings they find professionally and personally rewarding,” said AMA President Andrew W. Gurman, MD. “The AMA is committed to helping physicians navigate their practice options and offers innovative strategies and resources to ensure physicians in all practice sizes and setting can thrive in the changing health environment.”2
More and more, that environment is a practice wholly owned by physicians. The AMA reports that in 2016, 55.8% of physicians worked in such a practice (including physicians who have an ownership stake in the practice, those who are employed by the practice, and those who are independent contractors).2 An approximate 13.8% of physicians worked at practices with more than 50 physicians in 2016. The majority (57.8%), however, practiced in groups with 10 or fewer physicians. The most common practice type was the single-specialty group (42.8%), followed by the multispecialty group practice (24.6%).2
Paying physicians a salary instead of compensating them based on volume may improve physician satisfaction—it removes the need to deal with complex fee-for-service systems, say Ian Larkin, PhD, and George Loewenstein, PhD. In fee-for-service payment arrangements, physicians may be encouraged to order more tests and procedures because doing so may increase income. A better strategy, say Larkin and Loewenstein, is to switch to a straight salary system. Known for their quality of care and comparatively low costs, the Mayo Clinic, Cleveland Clinic, and Kaiser Permanente have successfully implemented this payment system.4
Related article:
ObGyn salaries jumped in the last year
Desired salary
The mean income for ObGyns rose by 3% in 2016 over 2015 ($286,000 compared with $277,000), according to Medscape.5 This jump follows a gradual increase over the last few years ($249,000 in 2014; $243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1,5,6
The highest earnings among all physicians were orthopedists ($489,000), plastic surgeons ($440,000), and cardiologists ($410,000). Pediatricians were the lowest paid physicians at $202,000.3
Fair compensation. Fewer than half (48%) of ObGyns who completed the Medscape survey felt they were fairly compensated in 2016, and 41% of those who were dissatisfied with their compensation believed they deserved to be earning between 11% and 25% more. When asked if they would still choose medicine, 72% of ObGyns answered affirmatively. Of those who would choose medicine again, 76% would choose obstetrics and gynecology once more.3
Gender differences. As in years past, full-time male ObGyns reported higher earnings (13%) than female ObGyns ($306,000 vs $270,000, respectively; (FIGURE 1).3,5,7,8
Among ObGyns who responded to the 2017 Medscape survey, 14% of women and 10% of men indicated that they work part-time.3 Last year, 13% of female ObGyns reported part-time employment versus 16% of male ObGyns.6
Among the ObGyns who answered the 2017 survey, there was a gender gap in participation related to race. Although more men than women responded to the survey, more women than men ObGyns among black/African American (women, 78%), Asian (women, 69%), and white/Caucasian (women, 53%) groups responded. Men outweighed women only among Hispanic/Latino ObGyns (60%) who answered the survey.3
Read about work-life balance, job satisfaction, and burnout
Work-life balance
ACOG predicts that mid-career and younger ObGyns will focus on work-life balance issues. Practice sites (ambulatory, hospital, or a combination) that offer part-time schedules or extra time for nonprofessional matters are becoming the most desirable to these practitioners.1
What satisfies and dissatisfies ObGyns? ObGyns reported to Medscape that their relationships with patients (41% of respondents) was the most rewarding part of their job (FIGURE 2).3
There are many job aspects that dissatisfy ObGyns, including1,3,9:
- too many bureaucratic tasks
- the short time allotted for each patient office visit
- electronic health records (EHR) and increased computerization
- not feeling appreciated or properly compensated
- spending too many hours at work
- the impact of regulatory changes on clinical practice.
Bureaucratic tasks remain a primary cause for burnout among all physicians.10 This year, 56% of all physicians reported spending 10 hours or more per week on paperwork and administrative tasks, up from 35% in the 2014 report. More than half (54%) of ObGyns reported spending 10 hours or more on paperwork.3 For every hour of face-to-face patient time, physicians spent nearly 2 additional hours on their EHR and administration tasks.9
Time with patients. Medscape reported that 38% of ObGyns spent more than 45 hours per week with patients (FIGURE 3).
ACOG notes that ObGyns are increasingly referring patients to subspecialists, which frustrates patients and increases their costs.1
ObGyns rank high in burnout rates. Burnout rates for physicians are twice that of other working adults.1 ObGyns rank second (56%) in burn out (Emergency Medicine, 59%).10 When Medscape survey respondents were asked to grade their burnout level from 1 to 7 (1 = “It does not interfere with my life;” 7 = “It is so severe that I am thinking of leaving medicine altogether”), ObGyns ranked their burnout level at 4.3.10 Female physicians reported a higher percentage of burnout than their male colleagues (55% vs 45%, respectively).10 An estimated 40% to 75% of ObGyns experienced some level of burnout.1
According to ACOG, the specialty is included among the “noncontrollable” lifestyle specialties, especially for those aged 50 years or younger. Many Millennials (born 1980 to 2000) do not view their work and professional achievement as central to their lives; ObGyns aged younger than 35 years want to work fewer hours per week compared with their older colleagues, says ACOG. However, when this option is unavailable, an increasing number of Millennials report lowered job satisfaction.1
Related article:
What can administrators and ObGyns do together to reduce physician burnout?
Mindfulness about quality of life. The relationship of burnout to quality of life issues is gaining in awareness. In a recent
“We need to stop blaming individuals and treat physician burnout as a system issue…If it affects half our physicians, it is indirectly affecting half our patients,” notes Tait Shanafelt, MD, a hematologist and physician-burnout researcher at the Mayo Clinic.9 He says that burnout relates to a physician’s “professional spirit of life, and it primarily affects individuals whose work involves an intense interaction with people.”9
The Mayo Clinic in Minneapolis, Minnesota, has taken a lead in developing a space for their physicians to “reset” by offering a room where health professionals can retreat if they need a moment to recover from a traumatic event.9
Read about what factors attract ObGyns to specific locations
Location, location, location
Specific areas of the country are more attractive for their higher compensation rates. The highest average compensation was reported by ObGyns in the North Central area ($339,000), West ($301,000), and Great Lakes ($297,000) regions, while the lowest compensation rates were found in the Northwest ($260,000), Southwest ($268,000), and South Central ($275,000) areas.3
Key factors, such as healthy patient populations, higher rates of health insurance coverage, and lower stress levels attract physicians (FIGURE 4). Minnesota ranked the #1 best place to practice because it has the 4th healthiest population, 2nd highest rate of employer-sponsored health insurance, the 17th lowest number of malpractice lawsuits, and a medical board that is the 3rd least harsh in the nation.12 Unfortunate situations such as the highest malpractice rates per capita, least healthy population, 8th lowest rate of employer-sponsored health insurance, and the 9th lowest compensation rate for physicians make Louisiana the worst place to practice in 2017.12
Supply and demand creates substantial geographic imbalances in the number of ObGyns in the United States. ACOG pro-jects that the need for ObGyns will increase nationally by 6% in the next 10 years, although demand will vary geographically from a 27% increase in Nevada to an 11% decrease in West Virginia.1 Especially vulnerable states (Arizona, Washington, Utah, Idaho) currently have an insufficient supply of ObGyns and are projected to see an increased future demand. Florida, Texas, North Carolina, and Nevada will be at risk, according to ACOG, because the adult female population is expected to increase.1
2017 Medscape survey demographics
The Medscape Compensation Report 2017 is a based on the responses of 19,270 physicians across 27+ specialties, 5% of whom were ObGyns. Data were collected in an online survey conducted from December 20, 2016, to March 7, 2017.3
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
ObGyns are mindfully choosing their practice environments. The trend, as reported by the American College of Obstetricians and Gynecologists (ACOG),1 shows movement from private practice to employment: an increasing number of ObGyns have joined large practices and are employed. Overall, fewer than half of US physicians owned their medical practice in 2016, reported the American Medical Association (AMA).2 This is the first time that the majority of physicians are not practice owners.
Although employed ObGyns earn 9% less than self-employed ObGyns, ($276,000 vs $300,000, respectively), trading a higher salary for less time spent on administrative tasks seems to be worth the pay cut, reports Medscape. Employed ObGyns reported receiving additional benefits that might not have been available to self-employed ObGyns: professional liability coverage, employer-subsidized health and dental insurance, paid time off, and a retirement plan with employer match.3
What matters to ObGyns when choosing a practice setting?
Several decisions about practice setting need to be made at the beginning and throughout a career, among them the type of practice, desired salary, work-life balance, (the latter 2 may be influenced by practice type), and location.
Type of practice
“Patients benefit when physicians practice in settings they find professionally and personally rewarding,” said AMA President Andrew W. Gurman, MD. “The AMA is committed to helping physicians navigate their practice options and offers innovative strategies and resources to ensure physicians in all practice sizes and setting can thrive in the changing health environment.”2
More and more, that environment is a practice wholly owned by physicians. The AMA reports that in 2016, 55.8% of physicians worked in such a practice (including physicians who have an ownership stake in the practice, those who are employed by the practice, and those who are independent contractors).2 An approximate 13.8% of physicians worked at practices with more than 50 physicians in 2016. The majority (57.8%), however, practiced in groups with 10 or fewer physicians. The most common practice type was the single-specialty group (42.8%), followed by the multispecialty group practice (24.6%).2
Paying physicians a salary instead of compensating them based on volume may improve physician satisfaction—it removes the need to deal with complex fee-for-service systems, say Ian Larkin, PhD, and George Loewenstein, PhD. In fee-for-service payment arrangements, physicians may be encouraged to order more tests and procedures because doing so may increase income. A better strategy, say Larkin and Loewenstein, is to switch to a straight salary system. Known for their quality of care and comparatively low costs, the Mayo Clinic, Cleveland Clinic, and Kaiser Permanente have successfully implemented this payment system.4
Related article:
ObGyn salaries jumped in the last year
Desired salary
The mean income for ObGyns rose by 3% in 2016 over 2015 ($286,000 compared with $277,000), according to Medscape.5 This jump follows a gradual increase over the last few years ($249,000 in 2014; $243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1,5,6
The highest earnings among all physicians were orthopedists ($489,000), plastic surgeons ($440,000), and cardiologists ($410,000). Pediatricians were the lowest paid physicians at $202,000.3
Fair compensation. Fewer than half (48%) of ObGyns who completed the Medscape survey felt they were fairly compensated in 2016, and 41% of those who were dissatisfied with their compensation believed they deserved to be earning between 11% and 25% more. When asked if they would still choose medicine, 72% of ObGyns answered affirmatively. Of those who would choose medicine again, 76% would choose obstetrics and gynecology once more.3
Gender differences. As in years past, full-time male ObGyns reported higher earnings (13%) than female ObGyns ($306,000 vs $270,000, respectively; (FIGURE 1).3,5,7,8
Among ObGyns who responded to the 2017 Medscape survey, 14% of women and 10% of men indicated that they work part-time.3 Last year, 13% of female ObGyns reported part-time employment versus 16% of male ObGyns.6
Among the ObGyns who answered the 2017 survey, there was a gender gap in participation related to race. Although more men than women responded to the survey, more women than men ObGyns among black/African American (women, 78%), Asian (women, 69%), and white/Caucasian (women, 53%) groups responded. Men outweighed women only among Hispanic/Latino ObGyns (60%) who answered the survey.3
Read about work-life balance, job satisfaction, and burnout
Work-life balance
ACOG predicts that mid-career and younger ObGyns will focus on work-life balance issues. Practice sites (ambulatory, hospital, or a combination) that offer part-time schedules or extra time for nonprofessional matters are becoming the most desirable to these practitioners.1
What satisfies and dissatisfies ObGyns? ObGyns reported to Medscape that their relationships with patients (41% of respondents) was the most rewarding part of their job (FIGURE 2).3
There are many job aspects that dissatisfy ObGyns, including1,3,9:
- too many bureaucratic tasks
- the short time allotted for each patient office visit
- electronic health records (EHR) and increased computerization
- not feeling appreciated or properly compensated
- spending too many hours at work
- the impact of regulatory changes on clinical practice.
Bureaucratic tasks remain a primary cause for burnout among all physicians.10 This year, 56% of all physicians reported spending 10 hours or more per week on paperwork and administrative tasks, up from 35% in the 2014 report. More than half (54%) of ObGyns reported spending 10 hours or more on paperwork.3 For every hour of face-to-face patient time, physicians spent nearly 2 additional hours on their EHR and administration tasks.9
Time with patients. Medscape reported that 38% of ObGyns spent more than 45 hours per week with patients (FIGURE 3).
ACOG notes that ObGyns are increasingly referring patients to subspecialists, which frustrates patients and increases their costs.1
ObGyns rank high in burnout rates. Burnout rates for physicians are twice that of other working adults.1 ObGyns rank second (56%) in burn out (Emergency Medicine, 59%).10 When Medscape survey respondents were asked to grade their burnout level from 1 to 7 (1 = “It does not interfere with my life;” 7 = “It is so severe that I am thinking of leaving medicine altogether”), ObGyns ranked their burnout level at 4.3.10 Female physicians reported a higher percentage of burnout than their male colleagues (55% vs 45%, respectively).10 An estimated 40% to 75% of ObGyns experienced some level of burnout.1
According to ACOG, the specialty is included among the “noncontrollable” lifestyle specialties, especially for those aged 50 years or younger. Many Millennials (born 1980 to 2000) do not view their work and professional achievement as central to their lives; ObGyns aged younger than 35 years want to work fewer hours per week compared with their older colleagues, says ACOG. However, when this option is unavailable, an increasing number of Millennials report lowered job satisfaction.1
Related article:
What can administrators and ObGyns do together to reduce physician burnout?
Mindfulness about quality of life. The relationship of burnout to quality of life issues is gaining in awareness. In a recent
“We need to stop blaming individuals and treat physician burnout as a system issue…If it affects half our physicians, it is indirectly affecting half our patients,” notes Tait Shanafelt, MD, a hematologist and physician-burnout researcher at the Mayo Clinic.9 He says that burnout relates to a physician’s “professional spirit of life, and it primarily affects individuals whose work involves an intense interaction with people.”9
The Mayo Clinic in Minneapolis, Minnesota, has taken a lead in developing a space for their physicians to “reset” by offering a room where health professionals can retreat if they need a moment to recover from a traumatic event.9
Read about what factors attract ObGyns to specific locations
Location, location, location
Specific areas of the country are more attractive for their higher compensation rates. The highest average compensation was reported by ObGyns in the North Central area ($339,000), West ($301,000), and Great Lakes ($297,000) regions, while the lowest compensation rates were found in the Northwest ($260,000), Southwest ($268,000), and South Central ($275,000) areas.3
Key factors, such as healthy patient populations, higher rates of health insurance coverage, and lower stress levels attract physicians (FIGURE 4). Minnesota ranked the #1 best place to practice because it has the 4th healthiest population, 2nd highest rate of employer-sponsored health insurance, the 17th lowest number of malpractice lawsuits, and a medical board that is the 3rd least harsh in the nation.12 Unfortunate situations such as the highest malpractice rates per capita, least healthy population, 8th lowest rate of employer-sponsored health insurance, and the 9th lowest compensation rate for physicians make Louisiana the worst place to practice in 2017.12
Supply and demand creates substantial geographic imbalances in the number of ObGyns in the United States. ACOG pro-jects that the need for ObGyns will increase nationally by 6% in the next 10 years, although demand will vary geographically from a 27% increase in Nevada to an 11% decrease in West Virginia.1 Especially vulnerable states (Arizona, Washington, Utah, Idaho) currently have an insufficient supply of ObGyns and are projected to see an increased future demand. Florida, Texas, North Carolina, and Nevada will be at risk, according to ACOG, because the adult female population is expected to increase.1
2017 Medscape survey demographics
The Medscape Compensation Report 2017 is a based on the responses of 19,270 physicians across 27+ specialties, 5% of whom were ObGyns. Data were collected in an online survey conducted from December 20, 2016, to March 7, 2017.3
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- American Congress of Obstetricians and Gynecologists. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. https://www.acog.org/Resources-And-Publications/The-Ob-Gyn-Workforce/The-Obstetrician-Gynecologist-Workforce-in-the-United-States. Accessed June 7, 2017.
- Murphy B. For the first time, physician practice owners are not the majority. AMA Wire. https://wire.ama-assn.org/practice-management/first-time-physician-practice-owners-are-not-majority?utm_source=BulletinHealthCare&utm_medium=email&utm_term=060117&utm_content=general&utm_campaign=article_alert-morning_rounds_daily. Published May 31, 2017. Accessed June 7, 2017.
- Grisham S. Medscape Ob/Gyn Compensation Report 2017. Medscape Website. http://www.medscape.com/slideshow/compensation-2017-ob-gyn-6008576. Published April 12, 2017. Accessed June 7, 2017.
- Larkin I, Loewenstein G. Business model—Related conflict of interests in medicine: Problems and potential solutions. JAMA. 2017;317(17):1745–1746.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 7, 2017.
- Reale D, Christie K. ObGyn salaries jumped in the last year. OBG Manag. 2016;28(7):25–27, 30, 37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2015. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed July 24, 2017.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed July 24, 2017.
- Parks T. AMA burnout by specialty. AMA Wire. https://wire.ama-assn.org/life-career/report-reveals-severity-burnout-specialty. Published January 31, 2017. Accessed June 7, 2017.
- Peckham C. Medscape Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout. Medscape Website. http://www.medscape.com/features/slideshow/lifestyle/2017/overview#page=1. Published January 11, 2017. Accessed June 7, 2017.
- DiVenere L. ObGyn burnout: ACOG takes aim. OBG Manag. 2016;28(9):25,30,32,33.
- Page L. Best and Worst Places to Practice 2017. Medscape Website. http://www.medscape.com/slideshow/best-places-to-practice-2017-6008688?src=wnl_physrep_170510_mscpmrk_bestplaces2017&impID=1345406&faf. Published May 10, 2017. Accessed June 7, 2017.
- American Congress of Obstetricians and Gynecologists. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. https://www.acog.org/Resources-And-Publications/The-Ob-Gyn-Workforce/The-Obstetrician-Gynecologist-Workforce-in-the-United-States. Accessed June 7, 2017.
- Murphy B. For the first time, physician practice owners are not the majority. AMA Wire. https://wire.ama-assn.org/practice-management/first-time-physician-practice-owners-are-not-majority?utm_source=BulletinHealthCare&utm_medium=email&utm_term=060117&utm_content=general&utm_campaign=article_alert-morning_rounds_daily. Published May 31, 2017. Accessed June 7, 2017.
- Grisham S. Medscape Ob/Gyn Compensation Report 2017. Medscape Website. http://www.medscape.com/slideshow/compensation-2017-ob-gyn-6008576. Published April 12, 2017. Accessed June 7, 2017.
- Larkin I, Loewenstein G. Business model—Related conflict of interests in medicine: Problems and potential solutions. JAMA. 2017;317(17):1745–1746.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 7, 2017.
- Reale D, Christie K. ObGyn salaries jumped in the last year. OBG Manag. 2016;28(7):25–27, 30, 37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2015. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed July 24, 2017.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed July 24, 2017.
- Parks T. AMA burnout by specialty. AMA Wire. https://wire.ama-assn.org/life-career/report-reveals-severity-burnout-specialty. Published January 31, 2017. Accessed June 7, 2017.
- Peckham C. Medscape Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout. Medscape Website. http://www.medscape.com/features/slideshow/lifestyle/2017/overview#page=1. Published January 11, 2017. Accessed June 7, 2017.
- DiVenere L. ObGyn burnout: ACOG takes aim. OBG Manag. 2016;28(9):25,30,32,33.
- Page L. Best and Worst Places to Practice 2017. Medscape Website. http://www.medscape.com/slideshow/best-places-to-practice-2017-6008688?src=wnl_physrep_170510_mscpmrk_bestplaces2017&impID=1345406&faf. Published May 10, 2017. Accessed June 7, 2017.
Los Angeles County encourages LARC use to decrease Zika cases
Los Angeles County, California, has been identified as one of 7 areas in the nation with the highest risk of local Zika transmission by the Centers for Disease Control and Prevention (CDC), advise Adriana Ramos and colleagues from Los Angeles County Department of Public Health (DPH), Maternal, Child & Adolescent Health Programs.1 One factor for this classification is the county’s high birth rate. According to Ramos at el the CDC recommends that, before a Zika outbreak occurs, health departments in areas with Aedes species mosquitos increase access to and use of effective contraception.1 Long-acting reversible contraceptives (LARCs), including the intrauterine device (IUD) and the implant, are proven most effective methods.1
In a poster presented at the American College of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting in San Diego, California, Ramos and colleagues summarized contraceptive use within LA County using data from the Los Angeles Mommy and Baby (LAMB) project, conducted by the Maternal, Child, and Adolescent Health (MCAH) Programs of the LA County DPH, which surveyed mothers who recently delivered a live baby about their preconception and perinatal experiences. In 2012, 6,893 mothers participated. In 2014, MCAH re-interviewed the 2012 LAMB respondents, excluding those with a subsequent pregnancy after the 2012 survey or who had not originally answered questions about family planning, leaving 3,175 respondents. Findings, weighted to the 2012 live-birth cohort, estimated the weighted population at 115,284 live births.1
The study defined contraception use by efficacy, identifying no contraception use, condoms, withdrawal, and the rhythm method as less effective; oral contraceptive pills and vaginal ring as moderately effective; and LARCs and sterilization as highly effective. Unintended births account for 47% of births in LAC and more than 59% of women report using less effective contraceptive methods.1
Results of the study
As a result of their study, MCAH researchers Adriana Ramos, Shin Chao, MD, MPH, and Diana E. Ramos, MD, MPH, conclude that educating providers to place LARC contraceptives and educating the public on the most effective contraceptive methods can decrease the neonatal Zika complication rates by preventing unplanned pregnancy. LAC is undertaking these activities to decrease the number of neonatal Zika cases.1
- Ramos A, Chao S, Ramos DE. Zika: Preconception & perinatal opportunities in Los Angeles County. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 6, 2017; San Diego, California.
Los Angeles County, California, has been identified as one of 7 areas in the nation with the highest risk of local Zika transmission by the Centers for Disease Control and Prevention (CDC), advise Adriana Ramos and colleagues from Los Angeles County Department of Public Health (DPH), Maternal, Child & Adolescent Health Programs.1 One factor for this classification is the county’s high birth rate. According to Ramos at el the CDC recommends that, before a Zika outbreak occurs, health departments in areas with Aedes species mosquitos increase access to and use of effective contraception.1 Long-acting reversible contraceptives (LARCs), including the intrauterine device (IUD) and the implant, are proven most effective methods.1
In a poster presented at the American College of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting in San Diego, California, Ramos and colleagues summarized contraceptive use within LA County using data from the Los Angeles Mommy and Baby (LAMB) project, conducted by the Maternal, Child, and Adolescent Health (MCAH) Programs of the LA County DPH, which surveyed mothers who recently delivered a live baby about their preconception and perinatal experiences. In 2012, 6,893 mothers participated. In 2014, MCAH re-interviewed the 2012 LAMB respondents, excluding those with a subsequent pregnancy after the 2012 survey or who had not originally answered questions about family planning, leaving 3,175 respondents. Findings, weighted to the 2012 live-birth cohort, estimated the weighted population at 115,284 live births.1
The study defined contraception use by efficacy, identifying no contraception use, condoms, withdrawal, and the rhythm method as less effective; oral contraceptive pills and vaginal ring as moderately effective; and LARCs and sterilization as highly effective. Unintended births account for 47% of births in LAC and more than 59% of women report using less effective contraceptive methods.1
Results of the study
As a result of their study, MCAH researchers Adriana Ramos, Shin Chao, MD, MPH, and Diana E. Ramos, MD, MPH, conclude that educating providers to place LARC contraceptives and educating the public on the most effective contraceptive methods can decrease the neonatal Zika complication rates by preventing unplanned pregnancy. LAC is undertaking these activities to decrease the number of neonatal Zika cases.1
Los Angeles County, California, has been identified as one of 7 areas in the nation with the highest risk of local Zika transmission by the Centers for Disease Control and Prevention (CDC), advise Adriana Ramos and colleagues from Los Angeles County Department of Public Health (DPH), Maternal, Child & Adolescent Health Programs.1 One factor for this classification is the county’s high birth rate. According to Ramos at el the CDC recommends that, before a Zika outbreak occurs, health departments in areas with Aedes species mosquitos increase access to and use of effective contraception.1 Long-acting reversible contraceptives (LARCs), including the intrauterine device (IUD) and the implant, are proven most effective methods.1
In a poster presented at the American College of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting in San Diego, California, Ramos and colleagues summarized contraceptive use within LA County using data from the Los Angeles Mommy and Baby (LAMB) project, conducted by the Maternal, Child, and Adolescent Health (MCAH) Programs of the LA County DPH, which surveyed mothers who recently delivered a live baby about their preconception and perinatal experiences. In 2012, 6,893 mothers participated. In 2014, MCAH re-interviewed the 2012 LAMB respondents, excluding those with a subsequent pregnancy after the 2012 survey or who had not originally answered questions about family planning, leaving 3,175 respondents. Findings, weighted to the 2012 live-birth cohort, estimated the weighted population at 115,284 live births.1
The study defined contraception use by efficacy, identifying no contraception use, condoms, withdrawal, and the rhythm method as less effective; oral contraceptive pills and vaginal ring as moderately effective; and LARCs and sterilization as highly effective. Unintended births account for 47% of births in LAC and more than 59% of women report using less effective contraceptive methods.1
Results of the study
As a result of their study, MCAH researchers Adriana Ramos, Shin Chao, MD, MPH, and Diana E. Ramos, MD, MPH, conclude that educating providers to place LARC contraceptives and educating the public on the most effective contraceptive methods can decrease the neonatal Zika complication rates by preventing unplanned pregnancy. LAC is undertaking these activities to decrease the number of neonatal Zika cases.1
- Ramos A, Chao S, Ramos DE. Zika: Preconception & perinatal opportunities in Los Angeles County. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 6, 2017; San Diego, California.
- Ramos A, Chao S, Ramos DE. Zika: Preconception & perinatal opportunities in Los Angeles County. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 6, 2017; San Diego, California.
Risk-reducing salpingectomy at benign hysterectomy: Have surgeons embraced this practice?
According to its January 2015 Committee Opinion, the American College of Obstetricians and Gynecologists supported the following recommendations and conclusions regarding salpingectomy for ovarian cancer prevention1:
- The surgeon and patient should discuss the potential benefits of the removal of the fallopian tubes during a hysterectomy in women at population risk of ovarian cancer who are not having an oophorectomy.
- When counseling women about laparoscopic sterilization methods, clinicians can communicate that bilateral salpingectomy can be considered a method that provides effective contraception.
- Prophylactic salpingectomy may offer clinicians the opportunity to prevent ovarian cancer in their patients.
- Randomized controlled trials are needed to support the validity of this approach to reduce the incidence of ovarian cancer.
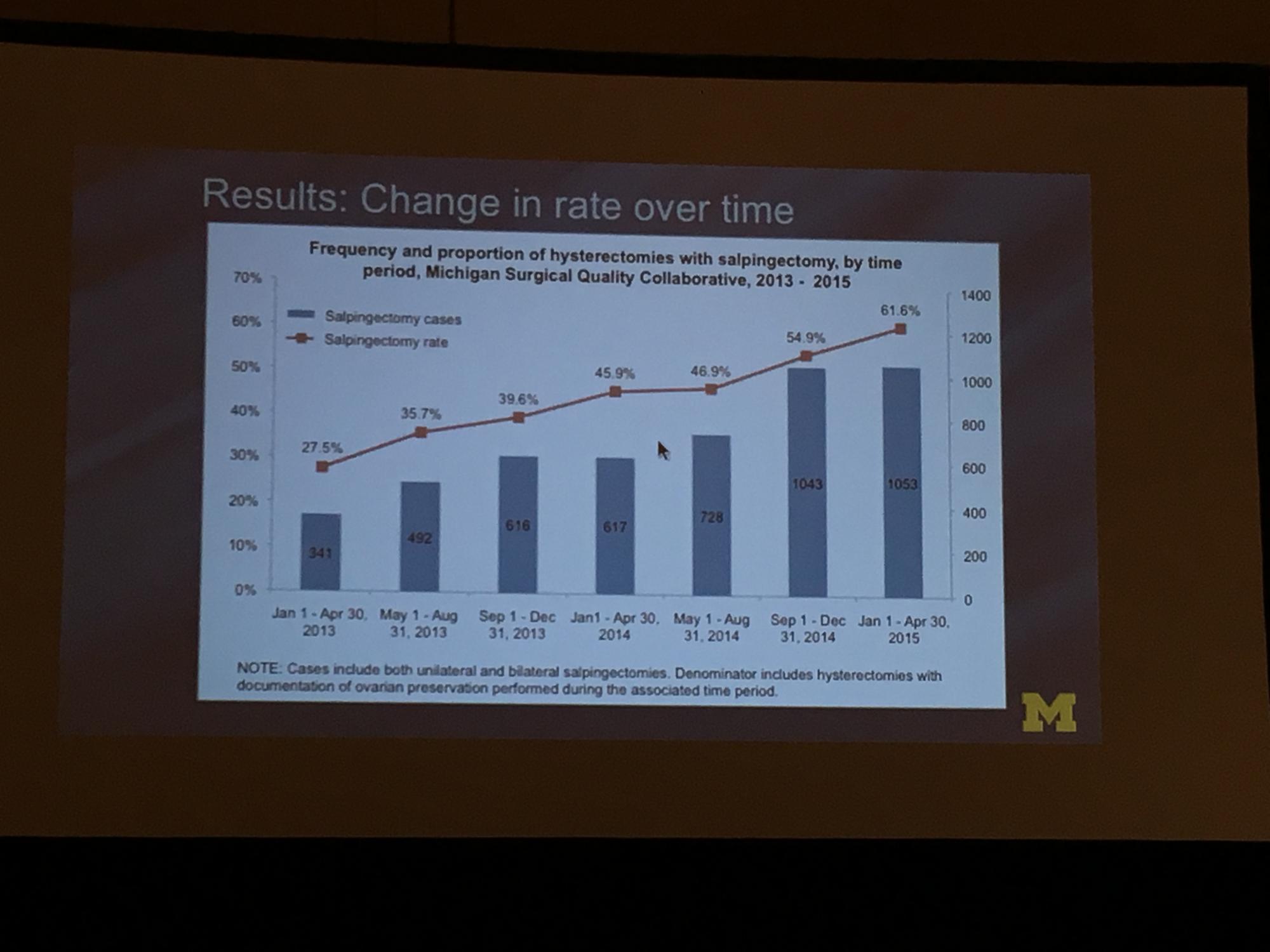
To determine the change in rate of salpingectomy performed at benign hysterectomy at Michigan hospitals, Sara Till, MD, MPH, and colleagues from the University of Michigan Health System performed a retrospective cross-sectioned study of data from the Michigan Surgical Quality Collaborative. They examined hysterectomies performed for all surgical routes between January 2013 and April 2015. Exclusion criteria included malignancy and obstetric indication. The primary objective was to measure salpingectomy at the time of hysterectomy with ovarian preservation. Measures studied included demographics; comorbidities; perioperative and postoperative results; and hospital/surgeon-related data; including surgeon volume, hospital type (ie, teaching), and hospital size.2
During the study period (January 1, 2013, to April 30, 2015), 18,642 hysterectomies were performed for benign indications, of which 55.7% (n = 10,382) were ovarian conserving. Among patients who underwent ovarian conserving hysterectomy, 44.9% (n = 4,668) had salpingectomy, with rates increasing steadily from 26.4% to 61.1% across the study period (P<.001). Salpingectomy was more likely with a laparoscopic approach (odds ratio [OR], 2.93; 95% confidence interval [CI], 2.69–3.20) and among women aged <60 years (OR, 2.60; 95% CI, 1.42–1.98), but did not vary with surgeon volume. After adjustments for age, body mass index, and surgical approach using a mixed model, the researchers found substantial variation in rates of salpingectomy across hospital sites, ranging from 3.7% to 88.3%. Variation in adjusted salpingectomy rates was not associated with academic affiliation or hospital size.2
Dr. Till and colleagues concluded that there was a substantial rise in risk-reducing salpingectomy from January 1, 2013, to April 30, 2015, and that there is substantial variation in the practice of salpingectomy, which is not accounted for by patient, surgeon, or hospital characteristics.2
- American College of Obstetricians and Gynecologists, Committee on Gynecologic Practice. Salpingectomy for ovarian cancer prevention. Committee Opinion No. 620 [published correction appears in: Obstet Gynecol. 2016;127(2):405]. Obstet Gynecol. 2015;125(1):279–281.
- Till SR, Edwards MG, Kobernik EK, Kamdar NS, As-Sanie S, Morgan DM. Implementation rate of risk-reducing salpingectomy at time of benign hysterectomy. Poster presented at: AAGL Global Congress of Minimally Invasive Gynecology; November 16, 2016; Orlando, Florida. J Minim Invasiv Gynecol. 2016;23(7 suppl):S1.
According to its January 2015 Committee Opinion, the American College of Obstetricians and Gynecologists supported the following recommendations and conclusions regarding salpingectomy for ovarian cancer prevention1:
- The surgeon and patient should discuss the potential benefits of the removal of the fallopian tubes during a hysterectomy in women at population risk of ovarian cancer who are not having an oophorectomy.
- When counseling women about laparoscopic sterilization methods, clinicians can communicate that bilateral salpingectomy can be considered a method that provides effective contraception.
- Prophylactic salpingectomy may offer clinicians the opportunity to prevent ovarian cancer in their patients.
- Randomized controlled trials are needed to support the validity of this approach to reduce the incidence of ovarian cancer.
To determine the change in rate of salpingectomy performed at benign hysterectomy at Michigan hospitals, Sara Till, MD, MPH, and colleagues from the University of Michigan Health System performed a retrospective cross-sectioned study of data from the Michigan Surgical Quality Collaborative. They examined hysterectomies performed for all surgical routes between January 2013 and April 2015. Exclusion criteria included malignancy and obstetric indication. The primary objective was to measure salpingectomy at the time of hysterectomy with ovarian preservation. Measures studied included demographics; comorbidities; perioperative and postoperative results; and hospital/surgeon-related data; including surgeon volume, hospital type (ie, teaching), and hospital size.2
During the study period (January 1, 2013, to April 30, 2015), 18,642 hysterectomies were performed for benign indications, of which 55.7% (n = 10,382) were ovarian conserving. Among patients who underwent ovarian conserving hysterectomy, 44.9% (n = 4,668) had salpingectomy, with rates increasing steadily from 26.4% to 61.1% across the study period (P<.001). Salpingectomy was more likely with a laparoscopic approach (odds ratio [OR], 2.93; 95% confidence interval [CI], 2.69–3.20) and among women aged <60 years (OR, 2.60; 95% CI, 1.42–1.98), but did not vary with surgeon volume. After adjustments for age, body mass index, and surgical approach using a mixed model, the researchers found substantial variation in rates of salpingectomy across hospital sites, ranging from 3.7% to 88.3%. Variation in adjusted salpingectomy rates was not associated with academic affiliation or hospital size.2
Dr. Till and colleagues concluded that there was a substantial rise in risk-reducing salpingectomy from January 1, 2013, to April 30, 2015, and that there is substantial variation in the practice of salpingectomy, which is not accounted for by patient, surgeon, or hospital characteristics.2
According to its January 2015 Committee Opinion, the American College of Obstetricians and Gynecologists supported the following recommendations and conclusions regarding salpingectomy for ovarian cancer prevention1:
- The surgeon and patient should discuss the potential benefits of the removal of the fallopian tubes during a hysterectomy in women at population risk of ovarian cancer who are not having an oophorectomy.
- When counseling women about laparoscopic sterilization methods, clinicians can communicate that bilateral salpingectomy can be considered a method that provides effective contraception.
- Prophylactic salpingectomy may offer clinicians the opportunity to prevent ovarian cancer in their patients.
- Randomized controlled trials are needed to support the validity of this approach to reduce the incidence of ovarian cancer.
To determine the change in rate of salpingectomy performed at benign hysterectomy at Michigan hospitals, Sara Till, MD, MPH, and colleagues from the University of Michigan Health System performed a retrospective cross-sectioned study of data from the Michigan Surgical Quality Collaborative. They examined hysterectomies performed for all surgical routes between January 2013 and April 2015. Exclusion criteria included malignancy and obstetric indication. The primary objective was to measure salpingectomy at the time of hysterectomy with ovarian preservation. Measures studied included demographics; comorbidities; perioperative and postoperative results; and hospital/surgeon-related data; including surgeon volume, hospital type (ie, teaching), and hospital size.2
During the study period (January 1, 2013, to April 30, 2015), 18,642 hysterectomies were performed for benign indications, of which 55.7% (n = 10,382) were ovarian conserving. Among patients who underwent ovarian conserving hysterectomy, 44.9% (n = 4,668) had salpingectomy, with rates increasing steadily from 26.4% to 61.1% across the study period (P<.001). Salpingectomy was more likely with a laparoscopic approach (odds ratio [OR], 2.93; 95% confidence interval [CI], 2.69–3.20) and among women aged <60 years (OR, 2.60; 95% CI, 1.42–1.98), but did not vary with surgeon volume. After adjustments for age, body mass index, and surgical approach using a mixed model, the researchers found substantial variation in rates of salpingectomy across hospital sites, ranging from 3.7% to 88.3%. Variation in adjusted salpingectomy rates was not associated with academic affiliation or hospital size.2
Dr. Till and colleagues concluded that there was a substantial rise in risk-reducing salpingectomy from January 1, 2013, to April 30, 2015, and that there is substantial variation in the practice of salpingectomy, which is not accounted for by patient, surgeon, or hospital characteristics.2
- American College of Obstetricians and Gynecologists, Committee on Gynecologic Practice. Salpingectomy for ovarian cancer prevention. Committee Opinion No. 620 [published correction appears in: Obstet Gynecol. 2016;127(2):405]. Obstet Gynecol. 2015;125(1):279–281.
- Till SR, Edwards MG, Kobernik EK, Kamdar NS, As-Sanie S, Morgan DM. Implementation rate of risk-reducing salpingectomy at time of benign hysterectomy. Poster presented at: AAGL Global Congress of Minimally Invasive Gynecology; November 16, 2016; Orlando, Florida. J Minim Invasiv Gynecol. 2016;23(7 suppl):S1.
- American College of Obstetricians and Gynecologists, Committee on Gynecologic Practice. Salpingectomy for ovarian cancer prevention. Committee Opinion No. 620 [published correction appears in: Obstet Gynecol. 2016;127(2):405]. Obstet Gynecol. 2015;125(1):279–281.
- Till SR, Edwards MG, Kobernik EK, Kamdar NS, As-Sanie S, Morgan DM. Implementation rate of risk-reducing salpingectomy at time of benign hysterectomy. Poster presented at: AAGL Global Congress of Minimally Invasive Gynecology; November 16, 2016; Orlando, Florida. J Minim Invasiv Gynecol. 2016;23(7 suppl):S1.