User login
Our EHRs have a drug problem
The “opioid epidemic” has become, perhaps, the most talked-about health crisis of the 21st century. It is a pervasive topic of discussion in the health literature and beyond, written about on the front pages of national newspapers and even mentioned in presidential state-of-the-union addresses.
As practicing physicians, we are all too familiar with the ills of chronic opioid use and have dealt with the implications of the crisis long before the issue attracted the public’s attention. In many ways, we have felt alone in bearing the burdens of caring for patients on chronic controlled substances. Until this point it has been our sacred duty to determine which patients are truly in need of those medications, and which are merely dependent on or – even worse – abusing them.
Health care providers have been largely blamed for the creation of this crisis, but we are not alone. Responsibility must also be shared by the pharmaceutical industry, health insurers, and even the government. Marketing practices, inadequate coverage of pain-relieving procedures and rehabilitation, and poorly-conceived drug policies have created an environment where it has been far too difficult to provide appropriate care for patients with chronic pain. As a result, patients who may have had an alternative to opioids were still started on these medications, and we – their physicians – have been left alone to manage the outcome.
Recently, however, health policy and public awareness have signaled a dramatic shift in the management of long-term pain medication. Significant legislation has been enacted on national, state, and local levels, and parties who are perceived to be responsible for the crisis are being held to task. For example, in August a landmark legal case was decided in an Oklahoma district court. Johnson & Johnson Pharmaceuticals was found guilty of promoting drug addiction through false and misleading marketing and was thus ordered to pay $572 million to the state to fund drug rehabilitation programs. This is likely a harbinger of many more such decisions to come, and the industry as a whole is bracing for the worst.
Physician prescribing practices are also being carefully scrutinized by the DEA, and a significant number of new “checks and balances” have been put in place to address dependence and addiction concerns. Unfortunately, as with all sweeping reform programs, there are good – and not-so-good – aspects to these changes. In many ways, the new tools at our disposal are a powerful way of mitigating drug dependence and diversion while protecting the sanctity of our “prescription pads.” Yet, as with so many other government mandates, we are burdened with the onus of complying with the new mandates for each and every opioid prescription, while our EHRs provide little help. This means more “clicks” for us, which can feel quite burdensome. It doesn’t need to be this way. Below are two straightforward things that can and should occur in order for providers to feel unburdened and to fully embrace the changes.
PDMP integration
One of the major ways of controlling prescription opioid abuse is through effective monitoring. Forty-nine of the 50 U.S. states have developed Prescription Drug Monitoring Programs (PDMPs), with Missouri being the only holdout (due to the politics of individual privacy concerns and conflation with gun control legislation). Most – though not all – of the states with a PDMP also mandate that physicians query a database prior to prescribing controlled substances. While noble and helpful in principle, querying a PDMP can be cumbersome, and the process is rarely integrated into the EHR workflow. Instead, physicians typically need to login to a separate website and manually transpose patient data to search the database. While most states have offered to subsidize PDMP integration with electronic records, EHR vendors have been very slow to develop the capability, leaving most physicians with no choice but to continue the aforementioned workflow. That is, if they comply at all; many well-meaning physicians have told us that they find themselves too harried to use the PDMP consistently. This reduces the value of these databases and places the physicians at significant risk. In some states, failure to query the database can lead to loss of a doctor’s medical license. It is high time that EHR vendors step up and integrate with every state’s prescription drug database.
Electronic prescribing of controlled substances
The other major milestone in prescription opioid management is the electronic prescribing of controlled substances (EPCS). This received national priority when the SUPPORT for Patients and Communities Act was signed into federal law in October of 2018. Included in this act is a requirement that, by January of 2021, all controlled substance prescriptions covered under Medicare Part D be sent electronically. Taking this as inspiration, many states and private companies have adopted more aggressive policies, choosing to implement electronic prescription requirements prior to the 2021 deadline. In Pennsylvania, where we practice, an EPCS requirement goes into effect in October of this year (2019). National pharmacy chains have also taken a more proactive approach. Walmart, for example, has decided that it will require EPCS nationwide in all of its stores beginning in January of 2020.
Essentially physicians have no choice – if they plan to continue to prescribe controlled substances, they will need to begin doing so electronically. Unfortunately, this may not be a straightforward process. While most EHRs offer some sort of EPCS solution, it is typically far from user friendly. Setting up EPCS can be costly and incredibly time consuming, and the procedure of actually submitting controlled prescriptions can be onerous and add many extra clicks. If vendors are serious about assisting in solving the opioid crisis, they need to make streamlining the steps of EPCS a high priority.
A prescription for success
As with so many other topics we’ve written about, we face an ever-increasing burden to provide quality patient care while complying with cumbersome and often unfunded external mandates. In the case of the opioid crisis, we believe we can do better. Our prescription for success? Streamlined workflow, smarter EHRs, and fewer clicks. There is no question that physicians and patients will benefit from effective implementation of the new tools at our disposal, but we need EHR vendors to step up and help carry the load.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter @doctornotte. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
The “opioid epidemic” has become, perhaps, the most talked-about health crisis of the 21st century. It is a pervasive topic of discussion in the health literature and beyond, written about on the front pages of national newspapers and even mentioned in presidential state-of-the-union addresses.
As practicing physicians, we are all too familiar with the ills of chronic opioid use and have dealt with the implications of the crisis long before the issue attracted the public’s attention. In many ways, we have felt alone in bearing the burdens of caring for patients on chronic controlled substances. Until this point it has been our sacred duty to determine which patients are truly in need of those medications, and which are merely dependent on or – even worse – abusing them.
Health care providers have been largely blamed for the creation of this crisis, but we are not alone. Responsibility must also be shared by the pharmaceutical industry, health insurers, and even the government. Marketing practices, inadequate coverage of pain-relieving procedures and rehabilitation, and poorly-conceived drug policies have created an environment where it has been far too difficult to provide appropriate care for patients with chronic pain. As a result, patients who may have had an alternative to opioids were still started on these medications, and we – their physicians – have been left alone to manage the outcome.
Recently, however, health policy and public awareness have signaled a dramatic shift in the management of long-term pain medication. Significant legislation has been enacted on national, state, and local levels, and parties who are perceived to be responsible for the crisis are being held to task. For example, in August a landmark legal case was decided in an Oklahoma district court. Johnson & Johnson Pharmaceuticals was found guilty of promoting drug addiction through false and misleading marketing and was thus ordered to pay $572 million to the state to fund drug rehabilitation programs. This is likely a harbinger of many more such decisions to come, and the industry as a whole is bracing for the worst.
Physician prescribing practices are also being carefully scrutinized by the DEA, and a significant number of new “checks and balances” have been put in place to address dependence and addiction concerns. Unfortunately, as with all sweeping reform programs, there are good – and not-so-good – aspects to these changes. In many ways, the new tools at our disposal are a powerful way of mitigating drug dependence and diversion while protecting the sanctity of our “prescription pads.” Yet, as with so many other government mandates, we are burdened with the onus of complying with the new mandates for each and every opioid prescription, while our EHRs provide little help. This means more “clicks” for us, which can feel quite burdensome. It doesn’t need to be this way. Below are two straightforward things that can and should occur in order for providers to feel unburdened and to fully embrace the changes.
PDMP integration
One of the major ways of controlling prescription opioid abuse is through effective monitoring. Forty-nine of the 50 U.S. states have developed Prescription Drug Monitoring Programs (PDMPs), with Missouri being the only holdout (due to the politics of individual privacy concerns and conflation with gun control legislation). Most – though not all – of the states with a PDMP also mandate that physicians query a database prior to prescribing controlled substances. While noble and helpful in principle, querying a PDMP can be cumbersome, and the process is rarely integrated into the EHR workflow. Instead, physicians typically need to login to a separate website and manually transpose patient data to search the database. While most states have offered to subsidize PDMP integration with electronic records, EHR vendors have been very slow to develop the capability, leaving most physicians with no choice but to continue the aforementioned workflow. That is, if they comply at all; many well-meaning physicians have told us that they find themselves too harried to use the PDMP consistently. This reduces the value of these databases and places the physicians at significant risk. In some states, failure to query the database can lead to loss of a doctor’s medical license. It is high time that EHR vendors step up and integrate with every state’s prescription drug database.
Electronic prescribing of controlled substances
The other major milestone in prescription opioid management is the electronic prescribing of controlled substances (EPCS). This received national priority when the SUPPORT for Patients and Communities Act was signed into federal law in October of 2018. Included in this act is a requirement that, by January of 2021, all controlled substance prescriptions covered under Medicare Part D be sent electronically. Taking this as inspiration, many states and private companies have adopted more aggressive policies, choosing to implement electronic prescription requirements prior to the 2021 deadline. In Pennsylvania, where we practice, an EPCS requirement goes into effect in October of this year (2019). National pharmacy chains have also taken a more proactive approach. Walmart, for example, has decided that it will require EPCS nationwide in all of its stores beginning in January of 2020.
Essentially physicians have no choice – if they plan to continue to prescribe controlled substances, they will need to begin doing so electronically. Unfortunately, this may not be a straightforward process. While most EHRs offer some sort of EPCS solution, it is typically far from user friendly. Setting up EPCS can be costly and incredibly time consuming, and the procedure of actually submitting controlled prescriptions can be onerous and add many extra clicks. If vendors are serious about assisting in solving the opioid crisis, they need to make streamlining the steps of EPCS a high priority.
A prescription for success
As with so many other topics we’ve written about, we face an ever-increasing burden to provide quality patient care while complying with cumbersome and often unfunded external mandates. In the case of the opioid crisis, we believe we can do better. Our prescription for success? Streamlined workflow, smarter EHRs, and fewer clicks. There is no question that physicians and patients will benefit from effective implementation of the new tools at our disposal, but we need EHR vendors to step up and help carry the load.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter @doctornotte. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
The “opioid epidemic” has become, perhaps, the most talked-about health crisis of the 21st century. It is a pervasive topic of discussion in the health literature and beyond, written about on the front pages of national newspapers and even mentioned in presidential state-of-the-union addresses.
As practicing physicians, we are all too familiar with the ills of chronic opioid use and have dealt with the implications of the crisis long before the issue attracted the public’s attention. In many ways, we have felt alone in bearing the burdens of caring for patients on chronic controlled substances. Until this point it has been our sacred duty to determine which patients are truly in need of those medications, and which are merely dependent on or – even worse – abusing them.
Health care providers have been largely blamed for the creation of this crisis, but we are not alone. Responsibility must also be shared by the pharmaceutical industry, health insurers, and even the government. Marketing practices, inadequate coverage of pain-relieving procedures and rehabilitation, and poorly-conceived drug policies have created an environment where it has been far too difficult to provide appropriate care for patients with chronic pain. As a result, patients who may have had an alternative to opioids were still started on these medications, and we – their physicians – have been left alone to manage the outcome.
Recently, however, health policy and public awareness have signaled a dramatic shift in the management of long-term pain medication. Significant legislation has been enacted on national, state, and local levels, and parties who are perceived to be responsible for the crisis are being held to task. For example, in August a landmark legal case was decided in an Oklahoma district court. Johnson & Johnson Pharmaceuticals was found guilty of promoting drug addiction through false and misleading marketing and was thus ordered to pay $572 million to the state to fund drug rehabilitation programs. This is likely a harbinger of many more such decisions to come, and the industry as a whole is bracing for the worst.
Physician prescribing practices are also being carefully scrutinized by the DEA, and a significant number of new “checks and balances” have been put in place to address dependence and addiction concerns. Unfortunately, as with all sweeping reform programs, there are good – and not-so-good – aspects to these changes. In many ways, the new tools at our disposal are a powerful way of mitigating drug dependence and diversion while protecting the sanctity of our “prescription pads.” Yet, as with so many other government mandates, we are burdened with the onus of complying with the new mandates for each and every opioid prescription, while our EHRs provide little help. This means more “clicks” for us, which can feel quite burdensome. It doesn’t need to be this way. Below are two straightforward things that can and should occur in order for providers to feel unburdened and to fully embrace the changes.
PDMP integration
One of the major ways of controlling prescription opioid abuse is through effective monitoring. Forty-nine of the 50 U.S. states have developed Prescription Drug Monitoring Programs (PDMPs), with Missouri being the only holdout (due to the politics of individual privacy concerns and conflation with gun control legislation). Most – though not all – of the states with a PDMP also mandate that physicians query a database prior to prescribing controlled substances. While noble and helpful in principle, querying a PDMP can be cumbersome, and the process is rarely integrated into the EHR workflow. Instead, physicians typically need to login to a separate website and manually transpose patient data to search the database. While most states have offered to subsidize PDMP integration with electronic records, EHR vendors have been very slow to develop the capability, leaving most physicians with no choice but to continue the aforementioned workflow. That is, if they comply at all; many well-meaning physicians have told us that they find themselves too harried to use the PDMP consistently. This reduces the value of these databases and places the physicians at significant risk. In some states, failure to query the database can lead to loss of a doctor’s medical license. It is high time that EHR vendors step up and integrate with every state’s prescription drug database.
Electronic prescribing of controlled substances
The other major milestone in prescription opioid management is the electronic prescribing of controlled substances (EPCS). This received national priority when the SUPPORT for Patients and Communities Act was signed into federal law in October of 2018. Included in this act is a requirement that, by January of 2021, all controlled substance prescriptions covered under Medicare Part D be sent electronically. Taking this as inspiration, many states and private companies have adopted more aggressive policies, choosing to implement electronic prescription requirements prior to the 2021 deadline. In Pennsylvania, where we practice, an EPCS requirement goes into effect in October of this year (2019). National pharmacy chains have also taken a more proactive approach. Walmart, for example, has decided that it will require EPCS nationwide in all of its stores beginning in January of 2020.
Essentially physicians have no choice – if they plan to continue to prescribe controlled substances, they will need to begin doing so electronically. Unfortunately, this may not be a straightforward process. While most EHRs offer some sort of EPCS solution, it is typically far from user friendly. Setting up EPCS can be costly and incredibly time consuming, and the procedure of actually submitting controlled prescriptions can be onerous and add many extra clicks. If vendors are serious about assisting in solving the opioid crisis, they need to make streamlining the steps of EPCS a high priority.
A prescription for success
As with so many other topics we’ve written about, we face an ever-increasing burden to provide quality patient care while complying with cumbersome and often unfunded external mandates. In the case of the opioid crisis, we believe we can do better. Our prescription for success? Streamlined workflow, smarter EHRs, and fewer clicks. There is no question that physicians and patients will benefit from effective implementation of the new tools at our disposal, but we need EHR vendors to step up and help carry the load.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter @doctornotte. Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
The 21st Century Cures Act: Tearing down fortresses to put patients first
"A fortress not only protects those inside of it, but it also enslaves them to work.”
– Anthony T. Hincks
As physicians, we spend a great deal of time intending to do our best for the people we serve. We believe fundamentally in the idea that our patients come first, and we toil daily to exercise that belief. We also want our patients to feel they are driving their care as active participants along the journey. Yet time and time again, despite our greatest attempts, those efforts are stymied by the state of modern medicine;
Over the past 10 years, we have done a tremendous job of constructing expensive fortresses around patient information known as electronic health records (EHRs). Billions of dollars have been spent implementing, upgrading, and optimizing. In spite of this, physicians are increasingly frustrated by EHRs (and in many cases, long to return to the days of paper). It isn’t surprising, then, that patients are frustrated as well. We use terms such as “patient-centered care,” but patients feel like they are not in the center at all. Instead, they can find themselves feeling like complete outsiders, at the mercy of the medical juggernaut to make sure they have the appropriate information when they need it. There are several issues that contribute to the frustrations of physicians and patients, but two in particular warrant attention. The first is the diversity of Health IT systems and ongoing issues with EHR interoperability. The second is a provincial attitude surrounding transparency and medical record ownership. We will discuss both of these here, as well as recent legislation designed to advance both concerns.
We have written in previous columns about the many challenges of interoperability. Electronic health records, sold by different vendors, typically won’t “talk” to each other. In spite of years of maturation, issues of compatibility remain. Patient data locked inside of one EHR is not easily accessible by a physician using a different EHR. While efforts have been made to streamline information sharing, there are still many fortresses that cannot be breached.
Bridging the moat
The 21st Century Cures Act, enacted by Congress in December of 2016, seeks to define and require interoperability while addressing many other significant problems in health care. According to the legislation, true interoperability means that health IT should enable the secure exchange of electronic health information with other electronic record systems without special effort on the part of the user; the process should be seamless and shouldn’t be cumbersome for physicians or patients. It also must be fully supported by EHR vendors, but those vendors have been expressing significant concerns with the ways in which the act is being interpreted.
In a recent blog post, the HIMSS Electronic Health Record Association – a consortium of vendors including Epic, Allscripts, eClinicalWorks, as well as several others – expressed “significant concerns regarding timelines, ambiguous language, disincentives for innovation, and definitions related to information blocking.”1 This is not surprising, as the onus for improving interoperability falls squarely on their shoulders, and the work to get there is arduous. Regardless of one’s interpretation, the goal of the Cures act is clear: Arrive at true interoperability in the shortest period of time, while eliminating barriers that prevent patients from accessing their health records. In other words, it asks for the avoidance of “information blocking.”
Breaching the gate
Information blocking, as defined by the Cures Act, is “a practice by a health care provider, health IT developer, health information exchange, or health information network that … is likely to interfere with, prevent, or materially discourage access, exchange, or use of electronic health information.”2 This practice is explicitly prohibited by the legislation – and is ethically wrong – yet it continues to occur implicitly every day as it has for many years. Even if unintentional and solely because of the growing complexity of our information systems, it makes accessing health information incredibly cumbersome for patients. Even worse, attempts to improve patients’ ability to access their health records have only created additional obstacles.
HIPAA (the Health Insurance Portability and Accountability Act of 1996) was designed to protect patient confidentiality and create security around protected health information. While noble in purpose, many have found it burdensome to work within the parameters set forth in the law. Physicians and patients needing legitimate access to clinical data discover endless release forms and convoluted processes standing in their way. Access to the information eventually comes in the form of reams of printed paper or faxed notes that cannot be easily consumed by or integrated into other systems.
The Meaningful Use initiative, while envisioned to improve data exchange and enhance population health, did little to help. Instead of enabling documentation efficiency and improving patient access, it promoted the proliferation of incompatible EHRs and poorly conceived patient portals. It also created heavy costs for both the federal government and physicians and was largely ineffective at producing systems whose use could be considered meaningful. The federal government paid out as much as $44,000 per physician to incentivize them to purchase medical records, while physicians often spent more than the $44,000 and, in many cases, wound up with EHRs that didn’t work well and had to be replaced.
Authors and supporters of the 21st Century Cures Act are hoping to avoid the shortcomings of prior legislation by attaching financial penalties to health care providers or IT vendors who engage in information blocking. While allowing for exceptions in appropriate cases, the law is clear: Patients deserve complete access to their medical records. While this goes against tradition, it has been proven to result in better outcomes.
Initiatives such as the OpenNotes movement have been pushing the value of full transparency for some time, and their website includes a long list of numerous examples to prove it. Indeed, several studies have demonstrated increased physician and patient satisfaction when both parties have ready access to health information. We believe that we, as physicians, should fully support the idea and lobby our EHR vendors to do the same.
It is time to tear down the impenetrable fortresses of traditional medicine, then work diligently to rebuild them with our patients safely inside.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. The Electronic Health Record Association blog
"A fortress not only protects those inside of it, but it also enslaves them to work.”
– Anthony T. Hincks
As physicians, we spend a great deal of time intending to do our best for the people we serve. We believe fundamentally in the idea that our patients come first, and we toil daily to exercise that belief. We also want our patients to feel they are driving their care as active participants along the journey. Yet time and time again, despite our greatest attempts, those efforts are stymied by the state of modern medicine;
Over the past 10 years, we have done a tremendous job of constructing expensive fortresses around patient information known as electronic health records (EHRs). Billions of dollars have been spent implementing, upgrading, and optimizing. In spite of this, physicians are increasingly frustrated by EHRs (and in many cases, long to return to the days of paper). It isn’t surprising, then, that patients are frustrated as well. We use terms such as “patient-centered care,” but patients feel like they are not in the center at all. Instead, they can find themselves feeling like complete outsiders, at the mercy of the medical juggernaut to make sure they have the appropriate information when they need it. There are several issues that contribute to the frustrations of physicians and patients, but two in particular warrant attention. The first is the diversity of Health IT systems and ongoing issues with EHR interoperability. The second is a provincial attitude surrounding transparency and medical record ownership. We will discuss both of these here, as well as recent legislation designed to advance both concerns.
We have written in previous columns about the many challenges of interoperability. Electronic health records, sold by different vendors, typically won’t “talk” to each other. In spite of years of maturation, issues of compatibility remain. Patient data locked inside of one EHR is not easily accessible by a physician using a different EHR. While efforts have been made to streamline information sharing, there are still many fortresses that cannot be breached.
Bridging the moat
The 21st Century Cures Act, enacted by Congress in December of 2016, seeks to define and require interoperability while addressing many other significant problems in health care. According to the legislation, true interoperability means that health IT should enable the secure exchange of electronic health information with other electronic record systems without special effort on the part of the user; the process should be seamless and shouldn’t be cumbersome for physicians or patients. It also must be fully supported by EHR vendors, but those vendors have been expressing significant concerns with the ways in which the act is being interpreted.
In a recent blog post, the HIMSS Electronic Health Record Association – a consortium of vendors including Epic, Allscripts, eClinicalWorks, as well as several others – expressed “significant concerns regarding timelines, ambiguous language, disincentives for innovation, and definitions related to information blocking.”1 This is not surprising, as the onus for improving interoperability falls squarely on their shoulders, and the work to get there is arduous. Regardless of one’s interpretation, the goal of the Cures act is clear: Arrive at true interoperability in the shortest period of time, while eliminating barriers that prevent patients from accessing their health records. In other words, it asks for the avoidance of “information blocking.”
Breaching the gate
Information blocking, as defined by the Cures Act, is “a practice by a health care provider, health IT developer, health information exchange, or health information network that … is likely to interfere with, prevent, or materially discourage access, exchange, or use of electronic health information.”2 This practice is explicitly prohibited by the legislation – and is ethically wrong – yet it continues to occur implicitly every day as it has for many years. Even if unintentional and solely because of the growing complexity of our information systems, it makes accessing health information incredibly cumbersome for patients. Even worse, attempts to improve patients’ ability to access their health records have only created additional obstacles.
HIPAA (the Health Insurance Portability and Accountability Act of 1996) was designed to protect patient confidentiality and create security around protected health information. While noble in purpose, many have found it burdensome to work within the parameters set forth in the law. Physicians and patients needing legitimate access to clinical data discover endless release forms and convoluted processes standing in their way. Access to the information eventually comes in the form of reams of printed paper or faxed notes that cannot be easily consumed by or integrated into other systems.
The Meaningful Use initiative, while envisioned to improve data exchange and enhance population health, did little to help. Instead of enabling documentation efficiency and improving patient access, it promoted the proliferation of incompatible EHRs and poorly conceived patient portals. It also created heavy costs for both the federal government and physicians and was largely ineffective at producing systems whose use could be considered meaningful. The federal government paid out as much as $44,000 per physician to incentivize them to purchase medical records, while physicians often spent more than the $44,000 and, in many cases, wound up with EHRs that didn’t work well and had to be replaced.
Authors and supporters of the 21st Century Cures Act are hoping to avoid the shortcomings of prior legislation by attaching financial penalties to health care providers or IT vendors who engage in information blocking. While allowing for exceptions in appropriate cases, the law is clear: Patients deserve complete access to their medical records. While this goes against tradition, it has been proven to result in better outcomes.
Initiatives such as the OpenNotes movement have been pushing the value of full transparency for some time, and their website includes a long list of numerous examples to prove it. Indeed, several studies have demonstrated increased physician and patient satisfaction when both parties have ready access to health information. We believe that we, as physicians, should fully support the idea and lobby our EHR vendors to do the same.
It is time to tear down the impenetrable fortresses of traditional medicine, then work diligently to rebuild them with our patients safely inside.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. The Electronic Health Record Association blog
"A fortress not only protects those inside of it, but it also enslaves them to work.”
– Anthony T. Hincks
As physicians, we spend a great deal of time intending to do our best for the people we serve. We believe fundamentally in the idea that our patients come first, and we toil daily to exercise that belief. We also want our patients to feel they are driving their care as active participants along the journey. Yet time and time again, despite our greatest attempts, those efforts are stymied by the state of modern medicine;
Over the past 10 years, we have done a tremendous job of constructing expensive fortresses around patient information known as electronic health records (EHRs). Billions of dollars have been spent implementing, upgrading, and optimizing. In spite of this, physicians are increasingly frustrated by EHRs (and in many cases, long to return to the days of paper). It isn’t surprising, then, that patients are frustrated as well. We use terms such as “patient-centered care,” but patients feel like they are not in the center at all. Instead, they can find themselves feeling like complete outsiders, at the mercy of the medical juggernaut to make sure they have the appropriate information when they need it. There are several issues that contribute to the frustrations of physicians and patients, but two in particular warrant attention. The first is the diversity of Health IT systems and ongoing issues with EHR interoperability. The second is a provincial attitude surrounding transparency and medical record ownership. We will discuss both of these here, as well as recent legislation designed to advance both concerns.
We have written in previous columns about the many challenges of interoperability. Electronic health records, sold by different vendors, typically won’t “talk” to each other. In spite of years of maturation, issues of compatibility remain. Patient data locked inside of one EHR is not easily accessible by a physician using a different EHR. While efforts have been made to streamline information sharing, there are still many fortresses that cannot be breached.
Bridging the moat
The 21st Century Cures Act, enacted by Congress in December of 2016, seeks to define and require interoperability while addressing many other significant problems in health care. According to the legislation, true interoperability means that health IT should enable the secure exchange of electronic health information with other electronic record systems without special effort on the part of the user; the process should be seamless and shouldn’t be cumbersome for physicians or patients. It also must be fully supported by EHR vendors, but those vendors have been expressing significant concerns with the ways in which the act is being interpreted.
In a recent blog post, the HIMSS Electronic Health Record Association – a consortium of vendors including Epic, Allscripts, eClinicalWorks, as well as several others – expressed “significant concerns regarding timelines, ambiguous language, disincentives for innovation, and definitions related to information blocking.”1 This is not surprising, as the onus for improving interoperability falls squarely on their shoulders, and the work to get there is arduous. Regardless of one’s interpretation, the goal of the Cures act is clear: Arrive at true interoperability in the shortest period of time, while eliminating barriers that prevent patients from accessing their health records. In other words, it asks for the avoidance of “information blocking.”
Breaching the gate
Information blocking, as defined by the Cures Act, is “a practice by a health care provider, health IT developer, health information exchange, or health information network that … is likely to interfere with, prevent, or materially discourage access, exchange, or use of electronic health information.”2 This practice is explicitly prohibited by the legislation – and is ethically wrong – yet it continues to occur implicitly every day as it has for many years. Even if unintentional and solely because of the growing complexity of our information systems, it makes accessing health information incredibly cumbersome for patients. Even worse, attempts to improve patients’ ability to access their health records have only created additional obstacles.
HIPAA (the Health Insurance Portability and Accountability Act of 1996) was designed to protect patient confidentiality and create security around protected health information. While noble in purpose, many have found it burdensome to work within the parameters set forth in the law. Physicians and patients needing legitimate access to clinical data discover endless release forms and convoluted processes standing in their way. Access to the information eventually comes in the form of reams of printed paper or faxed notes that cannot be easily consumed by or integrated into other systems.
The Meaningful Use initiative, while envisioned to improve data exchange and enhance population health, did little to help. Instead of enabling documentation efficiency and improving patient access, it promoted the proliferation of incompatible EHRs and poorly conceived patient portals. It also created heavy costs for both the federal government and physicians and was largely ineffective at producing systems whose use could be considered meaningful. The federal government paid out as much as $44,000 per physician to incentivize them to purchase medical records, while physicians often spent more than the $44,000 and, in many cases, wound up with EHRs that didn’t work well and had to be replaced.
Authors and supporters of the 21st Century Cures Act are hoping to avoid the shortcomings of prior legislation by attaching financial penalties to health care providers or IT vendors who engage in information blocking. While allowing for exceptions in appropriate cases, the law is clear: Patients deserve complete access to their medical records. While this goes against tradition, it has been proven to result in better outcomes.
Initiatives such as the OpenNotes movement have been pushing the value of full transparency for some time, and their website includes a long list of numerous examples to prove it. Indeed, several studies have demonstrated increased physician and patient satisfaction when both parties have ready access to health information. We believe that we, as physicians, should fully support the idea and lobby our EHR vendors to do the same.
It is time to tear down the impenetrable fortresses of traditional medicine, then work diligently to rebuild them with our patients safely inside.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. The Electronic Health Record Association blog
Electronic health records and the lost power of prose
“Don’t tell me the moon is shining; show me the glint of light on broken glass,” Anton Chekhov
In March 2006, four programmers turned entrepreneurs launched Twitter. This revolutionary tool experienced a monumental growth in scale over the next 10 years from a handful of users sharing a few thousand messages (known as “tweets”) each day to a global social network of over 300 million users valued at over $25 billion dollars. In fact, on Election Day 2016, Twitter was the No. 1 source of breaking news1, and it has been used as a launchpad for everything from social activism to national revolutions.
When Twitter was first conceived, it was designed to operate through wireless phone carriers’ SMS messaging functionality (aka “via text message”). SMS messages are limited to just 160 characters, so Twitter’s creators decided to restrict tweets to 140 characters, allowing 20 characters for a username. This decision created a necessity for communication efficiency that harks back to the days of the telegraph. From the liberal use of contractions and abbreviations to the tireless search for the shortest synonyms possible, Twitter users have employed countless techniques to enable them to say more with less. While clever and creative, this extreme verbal austerity has pervaded other media as well, becoming the hallmark literary style of the current generation.
Contemporaneous with the Twitter revolution, the medical field has allowed technology to dramatically change its style of communication as well, but in the opposite way. We have become far less efficient in our use of words, yet we seem to be doing a really poor job of expressing ourselves.
Saying less with more
I was once asked to provide expert testimony in a medical malpractice lawsuit. Working in support of the defense, I endured question after question from the plaintiff’s legal team as they picked apart every aspect of the case. Of particular interest was the physician’s documentation. Sadly – yet perhaps unsurprisingly – it was poor. The defendant had clearly used an EHR template and clicked checkboxes to create his note, documenting history, physical exam, assessment, and plan without having typed a single word. While adequate for billing purposes, the note was missing any narrative that could communicate the story of what had transpired during the patient’s visit. Sure, the presenting symptoms and vital signs were there, but the no description of the patient’s appearance had been recorded? What had the physician been thinking? What unspoken messages had led the physician to make the decisions he had made?
Like Twitter, the dawn of EHRs created an entirely new form of communication, but instead of limiting the content of physicians’ notes it expanded it. Objectively, this has made for more complete notes. Subjectively, this has led to notes packed with data, yet devoid of meaningful narrative. While handwritten notes from the previous generation were brief, they included the most important elements of the patient’s history and often the physician’s thought process in forming the differential. The electronically generated notes of today are quite the opposite; they are dense, yet far from illuminating. A clinician referring back to the record might have tremendous difficulty discerning salient features amidst all of the “note bloat.”This puts the patient (and the provider, as in the case above) at risk. Details may be present, but the diagnosis will be missed without the story that ties them all together.
Writing a new chapter
Physicians hoping to create meaningful notes are often stymied by the technology at their disposal or the demands placed on their time. These issues, combined with an ever-growing number of regulatory requirements, are what led to the decay of narrative in the first place. As a result, doctors are looking for alternative ways to buck the trend and bring patients’ stories back to their medical records. These methods are often expensive or involved, but in many cases they dramatically improve quality and efficiency.
An example of a tool that allows doctors to achieve these goals is speech recognition technology. Instead of typing or clicking, physicians dictate into the EHR, creating notes that are typically richer and more akin to a story than a list of symptoms or data points. When voice-to-text is properly deployed and utilized, documentation improves along with efficiency. Alternately, many providers are now employing scribes to accompany them in the exam room and complete the medical record. Taking this step leads to more descriptive notes, better productivity, and happier providers. The use of scribes also seems to result in happier patients, who report better therapeutic interactions when their doctors aren’t typing or staring at a computer screen.
The above-mentioned methods for recording information about a patient during a visit may be too expensive or complicated for some providers, but there are other simple techniques that can be used without incurring additional cost or resources. Previsit planning is one such possibility. By reviewing patient charts in advance of appointments, physicians can look over results, identify preventive health gaps, and anticipate follow-up needs and medication refills. They can then create skeleton notes and prepopulate orders to reduce the documentation burden during the visit. While time consuming at first, physicians have reported this practice actually saves time in the long run and allows them to focus on recording the patient narrative during the visit.
Another strategy is even more simple in concept, though may seem counter-intuitive at first: get better acquainted with the electronic records system. That is, take the time to really learn and understand the tools designed to improve productivity that are available in your EHR, then use them judiciously; take advantage of templates and macros when they’ll make you more efficient yet won’t inhibit your ability to tell the patient’s story; embrace optimization but don’t compromise on narrative. By carefully choosing your words, you’ll paint a clearer picture of every patient and enable safer and more personalized care.
Reference
1. “For Election Day Influence, Twitter Ruled Social Media” New York Times. Nov. 8, 2016.
“Don’t tell me the moon is shining; show me the glint of light on broken glass,” Anton Chekhov
In March 2006, four programmers turned entrepreneurs launched Twitter. This revolutionary tool experienced a monumental growth in scale over the next 10 years from a handful of users sharing a few thousand messages (known as “tweets”) each day to a global social network of over 300 million users valued at over $25 billion dollars. In fact, on Election Day 2016, Twitter was the No. 1 source of breaking news1, and it has been used as a launchpad for everything from social activism to national revolutions.
When Twitter was first conceived, it was designed to operate through wireless phone carriers’ SMS messaging functionality (aka “via text message”). SMS messages are limited to just 160 characters, so Twitter’s creators decided to restrict tweets to 140 characters, allowing 20 characters for a username. This decision created a necessity for communication efficiency that harks back to the days of the telegraph. From the liberal use of contractions and abbreviations to the tireless search for the shortest synonyms possible, Twitter users have employed countless techniques to enable them to say more with less. While clever and creative, this extreme verbal austerity has pervaded other media as well, becoming the hallmark literary style of the current generation.
Contemporaneous with the Twitter revolution, the medical field has allowed technology to dramatically change its style of communication as well, but in the opposite way. We have become far less efficient in our use of words, yet we seem to be doing a really poor job of expressing ourselves.
Saying less with more
I was once asked to provide expert testimony in a medical malpractice lawsuit. Working in support of the defense, I endured question after question from the plaintiff’s legal team as they picked apart every aspect of the case. Of particular interest was the physician’s documentation. Sadly – yet perhaps unsurprisingly – it was poor. The defendant had clearly used an EHR template and clicked checkboxes to create his note, documenting history, physical exam, assessment, and plan without having typed a single word. While adequate for billing purposes, the note was missing any narrative that could communicate the story of what had transpired during the patient’s visit. Sure, the presenting symptoms and vital signs were there, but the no description of the patient’s appearance had been recorded? What had the physician been thinking? What unspoken messages had led the physician to make the decisions he had made?
Like Twitter, the dawn of EHRs created an entirely new form of communication, but instead of limiting the content of physicians’ notes it expanded it. Objectively, this has made for more complete notes. Subjectively, this has led to notes packed with data, yet devoid of meaningful narrative. While handwritten notes from the previous generation were brief, they included the most important elements of the patient’s history and often the physician’s thought process in forming the differential. The electronically generated notes of today are quite the opposite; they are dense, yet far from illuminating. A clinician referring back to the record might have tremendous difficulty discerning salient features amidst all of the “note bloat.”This puts the patient (and the provider, as in the case above) at risk. Details may be present, but the diagnosis will be missed without the story that ties them all together.
Writing a new chapter
Physicians hoping to create meaningful notes are often stymied by the technology at their disposal or the demands placed on their time. These issues, combined with an ever-growing number of regulatory requirements, are what led to the decay of narrative in the first place. As a result, doctors are looking for alternative ways to buck the trend and bring patients’ stories back to their medical records. These methods are often expensive or involved, but in many cases they dramatically improve quality and efficiency.
An example of a tool that allows doctors to achieve these goals is speech recognition technology. Instead of typing or clicking, physicians dictate into the EHR, creating notes that are typically richer and more akin to a story than a list of symptoms or data points. When voice-to-text is properly deployed and utilized, documentation improves along with efficiency. Alternately, many providers are now employing scribes to accompany them in the exam room and complete the medical record. Taking this step leads to more descriptive notes, better productivity, and happier providers. The use of scribes also seems to result in happier patients, who report better therapeutic interactions when their doctors aren’t typing or staring at a computer screen.
The above-mentioned methods for recording information about a patient during a visit may be too expensive or complicated for some providers, but there are other simple techniques that can be used without incurring additional cost or resources. Previsit planning is one such possibility. By reviewing patient charts in advance of appointments, physicians can look over results, identify preventive health gaps, and anticipate follow-up needs and medication refills. They can then create skeleton notes and prepopulate orders to reduce the documentation burden during the visit. While time consuming at first, physicians have reported this practice actually saves time in the long run and allows them to focus on recording the patient narrative during the visit.
Another strategy is even more simple in concept, though may seem counter-intuitive at first: get better acquainted with the electronic records system. That is, take the time to really learn and understand the tools designed to improve productivity that are available in your EHR, then use them judiciously; take advantage of templates and macros when they’ll make you more efficient yet won’t inhibit your ability to tell the patient’s story; embrace optimization but don’t compromise on narrative. By carefully choosing your words, you’ll paint a clearer picture of every patient and enable safer and more personalized care.
Reference
1. “For Election Day Influence, Twitter Ruled Social Media” New York Times. Nov. 8, 2016.
“Don’t tell me the moon is shining; show me the glint of light on broken glass,” Anton Chekhov
In March 2006, four programmers turned entrepreneurs launched Twitter. This revolutionary tool experienced a monumental growth in scale over the next 10 years from a handful of users sharing a few thousand messages (known as “tweets”) each day to a global social network of over 300 million users valued at over $25 billion dollars. In fact, on Election Day 2016, Twitter was the No. 1 source of breaking news1, and it has been used as a launchpad for everything from social activism to national revolutions.
When Twitter was first conceived, it was designed to operate through wireless phone carriers’ SMS messaging functionality (aka “via text message”). SMS messages are limited to just 160 characters, so Twitter’s creators decided to restrict tweets to 140 characters, allowing 20 characters for a username. This decision created a necessity for communication efficiency that harks back to the days of the telegraph. From the liberal use of contractions and abbreviations to the tireless search for the shortest synonyms possible, Twitter users have employed countless techniques to enable them to say more with less. While clever and creative, this extreme verbal austerity has pervaded other media as well, becoming the hallmark literary style of the current generation.
Contemporaneous with the Twitter revolution, the medical field has allowed technology to dramatically change its style of communication as well, but in the opposite way. We have become far less efficient in our use of words, yet we seem to be doing a really poor job of expressing ourselves.
Saying less with more
I was once asked to provide expert testimony in a medical malpractice lawsuit. Working in support of the defense, I endured question after question from the plaintiff’s legal team as they picked apart every aspect of the case. Of particular interest was the physician’s documentation. Sadly – yet perhaps unsurprisingly – it was poor. The defendant had clearly used an EHR template and clicked checkboxes to create his note, documenting history, physical exam, assessment, and plan without having typed a single word. While adequate for billing purposes, the note was missing any narrative that could communicate the story of what had transpired during the patient’s visit. Sure, the presenting symptoms and vital signs were there, but the no description of the patient’s appearance had been recorded? What had the physician been thinking? What unspoken messages had led the physician to make the decisions he had made?
Like Twitter, the dawn of EHRs created an entirely new form of communication, but instead of limiting the content of physicians’ notes it expanded it. Objectively, this has made for more complete notes. Subjectively, this has led to notes packed with data, yet devoid of meaningful narrative. While handwritten notes from the previous generation were brief, they included the most important elements of the patient’s history and often the physician’s thought process in forming the differential. The electronically generated notes of today are quite the opposite; they are dense, yet far from illuminating. A clinician referring back to the record might have tremendous difficulty discerning salient features amidst all of the “note bloat.”This puts the patient (and the provider, as in the case above) at risk. Details may be present, but the diagnosis will be missed without the story that ties them all together.
Writing a new chapter
Physicians hoping to create meaningful notes are often stymied by the technology at their disposal or the demands placed on their time. These issues, combined with an ever-growing number of regulatory requirements, are what led to the decay of narrative in the first place. As a result, doctors are looking for alternative ways to buck the trend and bring patients’ stories back to their medical records. These methods are often expensive or involved, but in many cases they dramatically improve quality and efficiency.
An example of a tool that allows doctors to achieve these goals is speech recognition technology. Instead of typing or clicking, physicians dictate into the EHR, creating notes that are typically richer and more akin to a story than a list of symptoms or data points. When voice-to-text is properly deployed and utilized, documentation improves along with efficiency. Alternately, many providers are now employing scribes to accompany them in the exam room and complete the medical record. Taking this step leads to more descriptive notes, better productivity, and happier providers. The use of scribes also seems to result in happier patients, who report better therapeutic interactions when their doctors aren’t typing or staring at a computer screen.
The above-mentioned methods for recording information about a patient during a visit may be too expensive or complicated for some providers, but there are other simple techniques that can be used without incurring additional cost or resources. Previsit planning is one such possibility. By reviewing patient charts in advance of appointments, physicians can look over results, identify preventive health gaps, and anticipate follow-up needs and medication refills. They can then create skeleton notes and prepopulate orders to reduce the documentation burden during the visit. While time consuming at first, physicians have reported this practice actually saves time in the long run and allows them to focus on recording the patient narrative during the visit.
Another strategy is even more simple in concept, though may seem counter-intuitive at first: get better acquainted with the electronic records system. That is, take the time to really learn and understand the tools designed to improve productivity that are available in your EHR, then use them judiciously; take advantage of templates and macros when they’ll make you more efficient yet won’t inhibit your ability to tell the patient’s story; embrace optimization but don’t compromise on narrative. By carefully choosing your words, you’ll paint a clearer picture of every patient and enable safer and more personalized care.
Reference
1. “For Election Day Influence, Twitter Ruled Social Media” New York Times. Nov. 8, 2016.
Breaking down blockchain: How this novel technology will unfetter health care
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
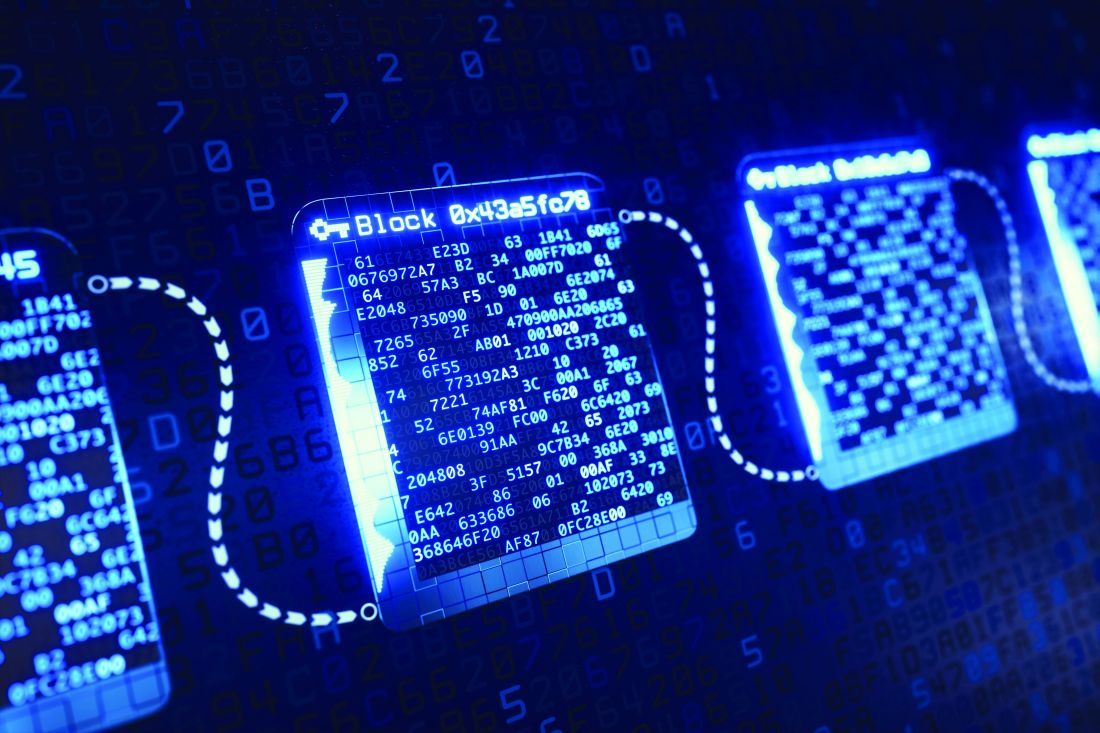
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
Where to go with wearables
On Sept. 14 of this year, Apple executives took to the stage to tout the incredible benefits of their new Apple Watch Series 4. While impressively presented in typical Apple fashion, the watch appeared to be only an evolution – not a revolution – in wearable technology. Still, there were a few noteworthy aspects of the new model that seemed to shine a light on the direction of the industry as a whole, and these were all focused on health care.
Like products from FitBit, Garmin, and others, the new Apple Watch can monitor a user’s heart rate and notify if it goes too high or too low. In addition, the watch now includes “fall detection,” and can automatically call for help if its wearer has taken a spill and become unresponsive. Soon it will even be capable of recording a single-lead ECG and detecting atrial fibrillation. While this all sounds fantastic, it also raises an important question in the minds of many physicians (including us): What do we do with all of these new data?
Findings from a Digital Health Study published by the American Medical Association in 20161 reveal that most doctors are aware of growing advances in Mobile Health (mHealth). Interestingly, however, while 85% see potential advantages in mHealth, less than 30% have begun employing it in their practices. This speaks to an adoption divide and highlights the many barriers to overcome before we can bridge it.
First and foremost, providers need confidence in the accuracy of the monitoring equipment, and, thus far, that accuracy has been questionable. Heart rate measurement, for example, is a staple of all currently available fitness wearables, yet is replete with technological pitfalls. This is because most consumer devices rely on optical sensors to measure heart rate. While inexpensive and noninvasive, the accuracy of these sensors can be affected by the interference of sweat, movement, and even the patient’s skin conditions – so much so that FitBit is currently embroiled in a class action lawsuit2 over the issue, in spite of providing disclaimers that a FitBit is “not a medical device.” To improve heart-monitoring capability, Apple has changed to a new sensor technology for this latest generation of Apple Watch. So far its accuracy has yet to be proven, and Apple’s delay in releasing the ECG features until “later this year” suggests there may still be bugs to work out.
Another significant concern raised by the onslaught of wearable health data is how to incorporate it into the electronic health record. Physicians care about efficient data integration, and, when asked in the aforementioned AMA study, physicians named this as their No. 1 functional requirement. EHR vendors have made some strides to allow patients to upload monitoring data directly through an online portal, but the large variety of available consumer devices has made standardizing this process difficult. Doctors have also made it clear that they want it to be straightforward to access and use the information provided by patients, and don’t want it to require special training. These are considerable challenges that will require collaboration between EHR vendors and wearable manufacturers to solve.
The introduction of additional players into the health care space also evokes questions of who owns this new health data set, and who is accountable for its integrity. If history is any indicator, device manufacturers will try their best to eschew any liability, and shift culpability onto patients and physicians. This is causing malpractice insurers to rethink policy coverage and forcing doctors to face a new reality of having “too much information.” While we are excited about the potential for better access to patient monitoring data, we agree that physicians need to understand where their responsibility for these data begins and ends.
Likewise, patients need to understand who has access to their personal health information, and how it’s being used. Privacy concerns will only become more evident as our society becomes ever more connected and as technologies become more invasive. The term “wearable” may soon become antiquated, as more products are coming to market that cross the skin barrier to collect samples directly from the blood or interstitial fluid. Devices such as Abbott’s new FreeStyle Libre continuous blood glucose monitor can be worn for weeks at a time, with its tiny sensor placed just under the skin. It constantly monitors trends in blood sugar and produces enough data points to determine the eating, sleeping, and activity habits of its wearer. This is all uploadable to Abbott’s servers, allowing patients and their providers to review it, thereby further expanding their personal health information footprint.
One encouraging aspect of the expansion mobile health technology is its organic, patient-led adoption. This is quite different from the epoch of electronic health records, which was motivated largely by government financial incentives and resulted in expensive, inefficient software. Patients are expressing a greater desire to take ownership of their health and have a growing interest in personal fitness. Also, the size of the consumer marketplace is forcing vendors to create competitive, high-value, and user-friendly mHealth devices. These products may seem to offer endless possibilities, but patients, vendors, and providers must fully acknowledge existing limitations in order to truly spark a revolution in wearable technology and actually improve patient care.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. Digital Health Study: Physicians’ motivations and requirements for adopting digital clinical tools. (2016) American Medical Association.
2. Kate Mclellan et al. v. Fitbit Inc. Fitbit Heart Rate Monitors Fraud & Defects Lawsuit.
On Sept. 14 of this year, Apple executives took to the stage to tout the incredible benefits of their new Apple Watch Series 4. While impressively presented in typical Apple fashion, the watch appeared to be only an evolution – not a revolution – in wearable technology. Still, there were a few noteworthy aspects of the new model that seemed to shine a light on the direction of the industry as a whole, and these were all focused on health care.
Like products from FitBit, Garmin, and others, the new Apple Watch can monitor a user’s heart rate and notify if it goes too high or too low. In addition, the watch now includes “fall detection,” and can automatically call for help if its wearer has taken a spill and become unresponsive. Soon it will even be capable of recording a single-lead ECG and detecting atrial fibrillation. While this all sounds fantastic, it also raises an important question in the minds of many physicians (including us): What do we do with all of these new data?
Findings from a Digital Health Study published by the American Medical Association in 20161 reveal that most doctors are aware of growing advances in Mobile Health (mHealth). Interestingly, however, while 85% see potential advantages in mHealth, less than 30% have begun employing it in their practices. This speaks to an adoption divide and highlights the many barriers to overcome before we can bridge it.
First and foremost, providers need confidence in the accuracy of the monitoring equipment, and, thus far, that accuracy has been questionable. Heart rate measurement, for example, is a staple of all currently available fitness wearables, yet is replete with technological pitfalls. This is because most consumer devices rely on optical sensors to measure heart rate. While inexpensive and noninvasive, the accuracy of these sensors can be affected by the interference of sweat, movement, and even the patient’s skin conditions – so much so that FitBit is currently embroiled in a class action lawsuit2 over the issue, in spite of providing disclaimers that a FitBit is “not a medical device.” To improve heart-monitoring capability, Apple has changed to a new sensor technology for this latest generation of Apple Watch. So far its accuracy has yet to be proven, and Apple’s delay in releasing the ECG features until “later this year” suggests there may still be bugs to work out.
Another significant concern raised by the onslaught of wearable health data is how to incorporate it into the electronic health record. Physicians care about efficient data integration, and, when asked in the aforementioned AMA study, physicians named this as their No. 1 functional requirement. EHR vendors have made some strides to allow patients to upload monitoring data directly through an online portal, but the large variety of available consumer devices has made standardizing this process difficult. Doctors have also made it clear that they want it to be straightforward to access and use the information provided by patients, and don’t want it to require special training. These are considerable challenges that will require collaboration between EHR vendors and wearable manufacturers to solve.
The introduction of additional players into the health care space also evokes questions of who owns this new health data set, and who is accountable for its integrity. If history is any indicator, device manufacturers will try their best to eschew any liability, and shift culpability onto patients and physicians. This is causing malpractice insurers to rethink policy coverage and forcing doctors to face a new reality of having “too much information.” While we are excited about the potential for better access to patient monitoring data, we agree that physicians need to understand where their responsibility for these data begins and ends.
Likewise, patients need to understand who has access to their personal health information, and how it’s being used. Privacy concerns will only become more evident as our society becomes ever more connected and as technologies become more invasive. The term “wearable” may soon become antiquated, as more products are coming to market that cross the skin barrier to collect samples directly from the blood or interstitial fluid. Devices such as Abbott’s new FreeStyle Libre continuous blood glucose monitor can be worn for weeks at a time, with its tiny sensor placed just under the skin. It constantly monitors trends in blood sugar and produces enough data points to determine the eating, sleeping, and activity habits of its wearer. This is all uploadable to Abbott’s servers, allowing patients and their providers to review it, thereby further expanding their personal health information footprint.
One encouraging aspect of the expansion mobile health technology is its organic, patient-led adoption. This is quite different from the epoch of electronic health records, which was motivated largely by government financial incentives and resulted in expensive, inefficient software. Patients are expressing a greater desire to take ownership of their health and have a growing interest in personal fitness. Also, the size of the consumer marketplace is forcing vendors to create competitive, high-value, and user-friendly mHealth devices. These products may seem to offer endless possibilities, but patients, vendors, and providers must fully acknowledge existing limitations in order to truly spark a revolution in wearable technology and actually improve patient care.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. Digital Health Study: Physicians’ motivations and requirements for adopting digital clinical tools. (2016) American Medical Association.
2. Kate Mclellan et al. v. Fitbit Inc. Fitbit Heart Rate Monitors Fraud & Defects Lawsuit.
On Sept. 14 of this year, Apple executives took to the stage to tout the incredible benefits of their new Apple Watch Series 4. While impressively presented in typical Apple fashion, the watch appeared to be only an evolution – not a revolution – in wearable technology. Still, there were a few noteworthy aspects of the new model that seemed to shine a light on the direction of the industry as a whole, and these were all focused on health care.
Like products from FitBit, Garmin, and others, the new Apple Watch can monitor a user’s heart rate and notify if it goes too high or too low. In addition, the watch now includes “fall detection,” and can automatically call for help if its wearer has taken a spill and become unresponsive. Soon it will even be capable of recording a single-lead ECG and detecting atrial fibrillation. While this all sounds fantastic, it also raises an important question in the minds of many physicians (including us): What do we do with all of these new data?
Findings from a Digital Health Study published by the American Medical Association in 20161 reveal that most doctors are aware of growing advances in Mobile Health (mHealth). Interestingly, however, while 85% see potential advantages in mHealth, less than 30% have begun employing it in their practices. This speaks to an adoption divide and highlights the many barriers to overcome before we can bridge it.
First and foremost, providers need confidence in the accuracy of the monitoring equipment, and, thus far, that accuracy has been questionable. Heart rate measurement, for example, is a staple of all currently available fitness wearables, yet is replete with technological pitfalls. This is because most consumer devices rely on optical sensors to measure heart rate. While inexpensive and noninvasive, the accuracy of these sensors can be affected by the interference of sweat, movement, and even the patient’s skin conditions – so much so that FitBit is currently embroiled in a class action lawsuit2 over the issue, in spite of providing disclaimers that a FitBit is “not a medical device.” To improve heart-monitoring capability, Apple has changed to a new sensor technology for this latest generation of Apple Watch. So far its accuracy has yet to be proven, and Apple’s delay in releasing the ECG features until “later this year” suggests there may still be bugs to work out.
Another significant concern raised by the onslaught of wearable health data is how to incorporate it into the electronic health record. Physicians care about efficient data integration, and, when asked in the aforementioned AMA study, physicians named this as their No. 1 functional requirement. EHR vendors have made some strides to allow patients to upload monitoring data directly through an online portal, but the large variety of available consumer devices has made standardizing this process difficult. Doctors have also made it clear that they want it to be straightforward to access and use the information provided by patients, and don’t want it to require special training. These are considerable challenges that will require collaboration between EHR vendors and wearable manufacturers to solve.
The introduction of additional players into the health care space also evokes questions of who owns this new health data set, and who is accountable for its integrity. If history is any indicator, device manufacturers will try their best to eschew any liability, and shift culpability onto patients and physicians. This is causing malpractice insurers to rethink policy coverage and forcing doctors to face a new reality of having “too much information.” While we are excited about the potential for better access to patient monitoring data, we agree that physicians need to understand where their responsibility for these data begins and ends.
Likewise, patients need to understand who has access to their personal health information, and how it’s being used. Privacy concerns will only become more evident as our society becomes ever more connected and as technologies become more invasive. The term “wearable” may soon become antiquated, as more products are coming to market that cross the skin barrier to collect samples directly from the blood or interstitial fluid. Devices such as Abbott’s new FreeStyle Libre continuous blood glucose monitor can be worn for weeks at a time, with its tiny sensor placed just under the skin. It constantly monitors trends in blood sugar and produces enough data points to determine the eating, sleeping, and activity habits of its wearer. This is all uploadable to Abbott’s servers, allowing patients and their providers to review it, thereby further expanding their personal health information footprint.
One encouraging aspect of the expansion mobile health technology is its organic, patient-led adoption. This is quite different from the epoch of electronic health records, which was motivated largely by government financial incentives and resulted in expensive, inefficient software. Patients are expressing a greater desire to take ownership of their health and have a growing interest in personal fitness. Also, the size of the consumer marketplace is forcing vendors to create competitive, high-value, and user-friendly mHealth devices. These products may seem to offer endless possibilities, but patients, vendors, and providers must fully acknowledge existing limitations in order to truly spark a revolution in wearable technology and actually improve patient care.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. Digital Health Study: Physicians’ motivations and requirements for adopting digital clinical tools. (2016) American Medical Association.
2. Kate Mclellan et al. v. Fitbit Inc. Fitbit Heart Rate Monitors Fraud & Defects Lawsuit.
Countdown to launch: Health care IT primed for disruption
On Friday, June 29, at 5:42 a.m., I stood with my family on a Florida shore overlooking Kennedy Space Center. We had gathered with about a hundred other people to watch a rocket launch and were overwhelmed with excitement as the coastline erupted in fire, and the spacecraft lifted off toward the heavens. Standing there watching the spectacle, I couldn’t help but be caught up in the irony of the moment. Here we were, at the place where NASA sent the first Americans into space – on the very shores where the Apollo astronauts set off for the moon to plant our nation’s flag in the lunar dust in July of 1969. Yet now, almost 50 years later, this launch was profoundly different. The rocket wasn’t built by NASA, and the intention of its builders wasn’t exploration. This was a Falcon 9, built by SpaceX, a for-profit company founded by an enterprising billionaire. Most surprisingly, this relatively routine launch was intended to accomplish something that NASA – the United States’ own space agency – currently can’t do on its own: Launch rockets.
Since retiring the Space Shuttle in 2011, the United States has had to rely on others – including even Roscosmos (the Russian space agency) – to ferry passengers, satellites, and cargo into space. Seeing this opportunity in a multibillion-dollar industry, private enterprise has risen to the challenge, innovating more quickly and at a lower cost than “the establishment” has ever been capable of. As a result, space travel has been disrupted by corporations competing in a new “space race.” Instead of national pride or scientific dominance, this race has been fueled by profit and is quite similar to one being run in another industry: health care.
Just 1 day prior to watching the launch – on June 28 – we learned that Amazon had purchased PillPack, a prescription drug home delivery service. The stock market responded to the news, and the establishment (in this case CVS, Walgreen’s, and WalMart, among others) collectively lost $17.5 billion in one day. This isn’t the first time Amazon has disrupted the health care world; in January of this year, they, along with Berkshire Hathaway and JPMorgan Chase, announced a health care partnership to cut costs and improve care delivery for their employees. This move also sent shivers through the market, as health insurers and providers such as Aetna and United Health lost big on expectations that Amazon et al. wouldn’t stop with their own employees. Those of us watching this play out from the sidelines realized we were witnessing a revolution that would mean the end of health care delivery as we know it – and that’s not necessarily a bad thing, especially in the world of Electronic Health Records.
As you’ve probably noticed, it is quite rare to find physicians nowadays who love computers. Once an exciting novelty in health care, PCs have become a burdensome necessity and providers often feel enslaved to the EHRs that run on them. There are numerous reasons for this, but one primary cause is that the hundreds of disparate EHRs currently available sprouted out of health care – a centuries-old and very provincial industry – prior to the development of technical and regulatory standards to govern them. As they’ve grown larger and larger from their primitive underpinnings, these EHRs have become more cumbersome to navigate, and vendors have simply “bolted-on” additional features without significant changes to their near-obsolete software architecture.
It’s worth noting that a few EHR companies purport to be true innovators in platform usability, such as industry giant, Epic. According to CEO Judy Faulkner, Epic pours 50% of their revenue back into research and development (though, as Epic is a privately held company, this number can’t be verified). If accurate, Epic is truly an exception, as most electronic record companies spend about 10%-30% on improving their products – far less than they spend on recruiting new customers. Regardless, the outcome is this: Physician expectations for user interface and user experience have far outpaced the current state of the art of EHRs, and this has left a gap that new players outside the health care establishment are apt to fill.
Like Amazon, other software giants have made significant investments in health care over the past several years. According to their website, Apple has been working with hospitals, scientists, and developers to “help health care providers streamline their work, deliver better care, and conduct medical research.” Similarly, Google claims to be “making a number of big bets in health care and life sciences,” by leveraging their artificial intelligence technology to assist in clinical diagnosis and scientific discovery. In spite of a few false starts in the past, these companies are poised to do more than simply disrupt health care. As experts in user interface and design, they could truly change the way physicians interact with health care technology, and it seems like it’s no longer a question of if, but when we’ll see that happen.
The effort of SpaceX and others to change the way we launch rockets tells a story that transcends space travel – It’s a story of how new thinking, more efficient processes, and better design can disrupt the establishment. It’s worth pointing out that NASA hasn’t given up – they are continuing to develop the Space Launch System, which, when completed, will be the most powerful rocket in the world and be capable of carrying astronauts into deep space. In the meantime, however, NASA is embracing the efforts of private industry to help pave a better way forward and make space travel safer and more accessible for everyone. We are hopeful that EHR vendors and other establishment health care institutions are taking note, adapting to meet the needs of the current generation of physicians and patients, and innovating a better way to launch health care into the future.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
On Friday, June 29, at 5:42 a.m., I stood with my family on a Florida shore overlooking Kennedy Space Center. We had gathered with about a hundred other people to watch a rocket launch and were overwhelmed with excitement as the coastline erupted in fire, and the spacecraft lifted off toward the heavens. Standing there watching the spectacle, I couldn’t help but be caught up in the irony of the moment. Here we were, at the place where NASA sent the first Americans into space – on the very shores where the Apollo astronauts set off for the moon to plant our nation’s flag in the lunar dust in July of 1969. Yet now, almost 50 years later, this launch was profoundly different. The rocket wasn’t built by NASA, and the intention of its builders wasn’t exploration. This was a Falcon 9, built by SpaceX, a for-profit company founded by an enterprising billionaire. Most surprisingly, this relatively routine launch was intended to accomplish something that NASA – the United States’ own space agency – currently can’t do on its own: Launch rockets.
Since retiring the Space Shuttle in 2011, the United States has had to rely on others – including even Roscosmos (the Russian space agency) – to ferry passengers, satellites, and cargo into space. Seeing this opportunity in a multibillion-dollar industry, private enterprise has risen to the challenge, innovating more quickly and at a lower cost than “the establishment” has ever been capable of. As a result, space travel has been disrupted by corporations competing in a new “space race.” Instead of national pride or scientific dominance, this race has been fueled by profit and is quite similar to one being run in another industry: health care.
Just 1 day prior to watching the launch – on June 28 – we learned that Amazon had purchased PillPack, a prescription drug home delivery service. The stock market responded to the news, and the establishment (in this case CVS, Walgreen’s, and WalMart, among others) collectively lost $17.5 billion in one day. This isn’t the first time Amazon has disrupted the health care world; in January of this year, they, along with Berkshire Hathaway and JPMorgan Chase, announced a health care partnership to cut costs and improve care delivery for their employees. This move also sent shivers through the market, as health insurers and providers such as Aetna and United Health lost big on expectations that Amazon et al. wouldn’t stop with their own employees. Those of us watching this play out from the sidelines realized we were witnessing a revolution that would mean the end of health care delivery as we know it – and that’s not necessarily a bad thing, especially in the world of Electronic Health Records.
As you’ve probably noticed, it is quite rare to find physicians nowadays who love computers. Once an exciting novelty in health care, PCs have become a burdensome necessity and providers often feel enslaved to the EHRs that run on them. There are numerous reasons for this, but one primary cause is that the hundreds of disparate EHRs currently available sprouted out of health care – a centuries-old and very provincial industry – prior to the development of technical and regulatory standards to govern them. As they’ve grown larger and larger from their primitive underpinnings, these EHRs have become more cumbersome to navigate, and vendors have simply “bolted-on” additional features without significant changes to their near-obsolete software architecture.
It’s worth noting that a few EHR companies purport to be true innovators in platform usability, such as industry giant, Epic. According to CEO Judy Faulkner, Epic pours 50% of their revenue back into research and development (though, as Epic is a privately held company, this number can’t be verified). If accurate, Epic is truly an exception, as most electronic record companies spend about 10%-30% on improving their products – far less than they spend on recruiting new customers. Regardless, the outcome is this: Physician expectations for user interface and user experience have far outpaced the current state of the art of EHRs, and this has left a gap that new players outside the health care establishment are apt to fill.
Like Amazon, other software giants have made significant investments in health care over the past several years. According to their website, Apple has been working with hospitals, scientists, and developers to “help health care providers streamline their work, deliver better care, and conduct medical research.” Similarly, Google claims to be “making a number of big bets in health care and life sciences,” by leveraging their artificial intelligence technology to assist in clinical diagnosis and scientific discovery. In spite of a few false starts in the past, these companies are poised to do more than simply disrupt health care. As experts in user interface and design, they could truly change the way physicians interact with health care technology, and it seems like it’s no longer a question of if, but when we’ll see that happen.
The effort of SpaceX and others to change the way we launch rockets tells a story that transcends space travel – It’s a story of how new thinking, more efficient processes, and better design can disrupt the establishment. It’s worth pointing out that NASA hasn’t given up – they are continuing to develop the Space Launch System, which, when completed, will be the most powerful rocket in the world and be capable of carrying astronauts into deep space. In the meantime, however, NASA is embracing the efforts of private industry to help pave a better way forward and make space travel safer and more accessible for everyone. We are hopeful that EHR vendors and other establishment health care institutions are taking note, adapting to meet the needs of the current generation of physicians and patients, and innovating a better way to launch health care into the future.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
On Friday, June 29, at 5:42 a.m., I stood with my family on a Florida shore overlooking Kennedy Space Center. We had gathered with about a hundred other people to watch a rocket launch and were overwhelmed with excitement as the coastline erupted in fire, and the spacecraft lifted off toward the heavens. Standing there watching the spectacle, I couldn’t help but be caught up in the irony of the moment. Here we were, at the place where NASA sent the first Americans into space – on the very shores where the Apollo astronauts set off for the moon to plant our nation’s flag in the lunar dust in July of 1969. Yet now, almost 50 years later, this launch was profoundly different. The rocket wasn’t built by NASA, and the intention of its builders wasn’t exploration. This was a Falcon 9, built by SpaceX, a for-profit company founded by an enterprising billionaire. Most surprisingly, this relatively routine launch was intended to accomplish something that NASA – the United States’ own space agency – currently can’t do on its own: Launch rockets.
Since retiring the Space Shuttle in 2011, the United States has had to rely on others – including even Roscosmos (the Russian space agency) – to ferry passengers, satellites, and cargo into space. Seeing this opportunity in a multibillion-dollar industry, private enterprise has risen to the challenge, innovating more quickly and at a lower cost than “the establishment” has ever been capable of. As a result, space travel has been disrupted by corporations competing in a new “space race.” Instead of national pride or scientific dominance, this race has been fueled by profit and is quite similar to one being run in another industry: health care.
Just 1 day prior to watching the launch – on June 28 – we learned that Amazon had purchased PillPack, a prescription drug home delivery service. The stock market responded to the news, and the establishment (in this case CVS, Walgreen’s, and WalMart, among others) collectively lost $17.5 billion in one day. This isn’t the first time Amazon has disrupted the health care world; in January of this year, they, along with Berkshire Hathaway and JPMorgan Chase, announced a health care partnership to cut costs and improve care delivery for their employees. This move also sent shivers through the market, as health insurers and providers such as Aetna and United Health lost big on expectations that Amazon et al. wouldn’t stop with their own employees. Those of us watching this play out from the sidelines realized we were witnessing a revolution that would mean the end of health care delivery as we know it – and that’s not necessarily a bad thing, especially in the world of Electronic Health Records.
As you’ve probably noticed, it is quite rare to find physicians nowadays who love computers. Once an exciting novelty in health care, PCs have become a burdensome necessity and providers often feel enslaved to the EHRs that run on them. There are numerous reasons for this, but one primary cause is that the hundreds of disparate EHRs currently available sprouted out of health care – a centuries-old and very provincial industry – prior to the development of technical and regulatory standards to govern them. As they’ve grown larger and larger from their primitive underpinnings, these EHRs have become more cumbersome to navigate, and vendors have simply “bolted-on” additional features without significant changes to their near-obsolete software architecture.
It’s worth noting that a few EHR companies purport to be true innovators in platform usability, such as industry giant, Epic. According to CEO Judy Faulkner, Epic pours 50% of their revenue back into research and development (though, as Epic is a privately held company, this number can’t be verified). If accurate, Epic is truly an exception, as most electronic record companies spend about 10%-30% on improving their products – far less than they spend on recruiting new customers. Regardless, the outcome is this: Physician expectations for user interface and user experience have far outpaced the current state of the art of EHRs, and this has left a gap that new players outside the health care establishment are apt to fill.
Like Amazon, other software giants have made significant investments in health care over the past several years. According to their website, Apple has been working with hospitals, scientists, and developers to “help health care providers streamline their work, deliver better care, and conduct medical research.” Similarly, Google claims to be “making a number of big bets in health care and life sciences,” by leveraging their artificial intelligence technology to assist in clinical diagnosis and scientific discovery. In spite of a few false starts in the past, these companies are poised to do more than simply disrupt health care. As experts in user interface and design, they could truly change the way physicians interact with health care technology, and it seems like it’s no longer a question of if, but when we’ll see that happen.
The effort of SpaceX and others to change the way we launch rockets tells a story that transcends space travel – It’s a story of how new thinking, more efficient processes, and better design can disrupt the establishment. It’s worth pointing out that NASA hasn’t given up – they are continuing to develop the Space Launch System, which, when completed, will be the most powerful rocket in the world and be capable of carrying astronauts into deep space. In the meantime, however, NASA is embracing the efforts of private industry to help pave a better way forward and make space travel safer and more accessible for everyone. We are hopeful that EHR vendors and other establishment health care institutions are taking note, adapting to meet the needs of the current generation of physicians and patients, and innovating a better way to launch health care into the future.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
“I’m sorry, doctor, I’m afraid I can’t do that”
In “2001: A Space Odyssey,” the epic 1968 film by Stanley Kubrick and Arthur C. Clarke, humanity makes first contact with an alien intelligence, and the course of history is irreversibly altered. Hailed as a watershed moment in science fiction, “2001” was considered way ahead of its time and raised a number of philosophical questions about what would happen if we ever encountered another form of life. Interestingly, the most noteworthy character in the film isn’t human or alien, but instead a new form of life altogether: an artificial intelligence (AI) known as the Heuristically programmed ALgorithmic computer 9000. HAL (as he is known colloquially) operates the Discovery One spacecraft, ferrying several scientists bound for Jupiter on a mission of exploration. Stating that he is “foolproof and incapable of error,” HAL’s superiority complex leads him to become the film’s antagonist, as he believes that human error is the cause of the difficulties they encounter. He eventually concludes that the best way to complete the mission is to eliminate human interference. When asked by scientist Dr. David Bowman to perform a simple function essential to the survival of the crew, HAL simply states “I’m sorry, Dave, I’m afraid I can’t do that.” Bowman is forced to disconnect HAL’s higher intellectual capabilities, reverting the computer to its most basic functions to ensure human survival.
Kubrick and Clarke may have been overly ambitious in predicting the progress of human space flight, but their call for concern over the risks of artificial intelligence seems quite prescient. Recently, billionaire entrepreneur Elon Musk (CEO of Tesla Motors and SpaceX) raised his concerns about AI, warning that, left unchecked, AI could be mankind’s final invention – one that could eventually destroy us. Other giants of the tech industry, including Bill Gates and Mark Zuckerberg, disagree. They believe AI represents tremendous promise for humanity and could usher in innovations unlike any we have ever seen.
A few weeks ago, we attended a national electronic health records conference where a well-known EHR vendor unveiled the new features in the upcoming release of their software. One of the most noteworthy additions was an intelligent virtual assistant, designed to help providers care for patients. While this is not the first time AI has ventured into health care (see IBM’s “Watson”), it is the first time the idea has become mainstream and fully integrated into physician workflow. Much like the virtual assistants mentioned above, this one can use voice or mouse/keyboard interaction to find clinical information, simplify common tasks, and help with medical decision-making.
While exciting at first, the idea of artificially intelligent EHRs may sound terrifying to some who aren’t yet ready to trust any patient care to machines. Reassuringly, while the integrated virtual assistant mentioned above can make suggestions to guide physicians to the right data or offer decision support when available, it is primarily focused on interface enhancement to improve work flow. It is not yet capable of making true clinical decisions that remove the physician from care delivery, but computers that do the diagnostic work of physicians may be closer than you think.
Research done at Jefferson University in Philadelphia and published in the August 2017 edition of Radiology1 investigated the ability of deep-learning algorithms to interpret chest radiographs for the diagnosis of tuberculosis. The computers achieved an impressive reliability of 99%. While at first radiograph interpretation seems quite different than the diagnostic decision-making done in primary care, the fundamental skill required for both is similar: pattern recognition. To build those patterns, artificial intelligence requires an enormous number of data points, but that’s hardly a problem thanks to the continual collection of patient data through electronic health records. The amount of raw information available to these algorithms is growing exponentially by the day, and with time their predictive ability will be unmatched. So where will that leave us, the physicians, entrusted for generations with the responsibility of diagnosis? Possibly more satisfied than we are today.
There was a time – not long ago – when the body of available medical knowledge was incredibly limited. Diagnostic testing was primitive and often inaccurate, and the treatment provided by physicians was focused on supporting, communicating, and genuinely caring for patients and their families. In the past 50 years, medical knowledge has exploded, and diagnostic testing has become incredibly advanced. Sadly, at the same time physicians have begun to feel more like clerical workers: entering data, writing prescriptions, and filling out forms. As artificial intelligence assumes some of this busywork and takes much of the guesswork out of diagnosis, physicians may find greater job satisfaction as they provide the skills a computer never can: a human touch, a personal and reflective interpretation of a patient’s diagnosis, and a true emotional connection. Ask this of a computer, and the response will always be the same: “I’m sorry, doctor, I’m afraid I can’t do that.”
Reference
1. Lakhani, Paras & Sundaram, Baskaran, “Deep Learning at Chest Radiography: Automated Classification of Pulmonary Tuberculosis by Using Convolutional Neural Networks,” Radiology. 2017 Aug;284:574-82.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
In “2001: A Space Odyssey,” the epic 1968 film by Stanley Kubrick and Arthur C. Clarke, humanity makes first contact with an alien intelligence, and the course of history is irreversibly altered. Hailed as a watershed moment in science fiction, “2001” was considered way ahead of its time and raised a number of philosophical questions about what would happen if we ever encountered another form of life. Interestingly, the most noteworthy character in the film isn’t human or alien, but instead a new form of life altogether: an artificial intelligence (AI) known as the Heuristically programmed ALgorithmic computer 9000. HAL (as he is known colloquially) operates the Discovery One spacecraft, ferrying several scientists bound for Jupiter on a mission of exploration. Stating that he is “foolproof and incapable of error,” HAL’s superiority complex leads him to become the film’s antagonist, as he believes that human error is the cause of the difficulties they encounter. He eventually concludes that the best way to complete the mission is to eliminate human interference. When asked by scientist Dr. David Bowman to perform a simple function essential to the survival of the crew, HAL simply states “I’m sorry, Dave, I’m afraid I can’t do that.” Bowman is forced to disconnect HAL’s higher intellectual capabilities, reverting the computer to its most basic functions to ensure human survival.
Kubrick and Clarke may have been overly ambitious in predicting the progress of human space flight, but their call for concern over the risks of artificial intelligence seems quite prescient. Recently, billionaire entrepreneur Elon Musk (CEO of Tesla Motors and SpaceX) raised his concerns about AI, warning that, left unchecked, AI could be mankind’s final invention – one that could eventually destroy us. Other giants of the tech industry, including Bill Gates and Mark Zuckerberg, disagree. They believe AI represents tremendous promise for humanity and could usher in innovations unlike any we have ever seen.
A few weeks ago, we attended a national electronic health records conference where a well-known EHR vendor unveiled the new features in the upcoming release of their software. One of the most noteworthy additions was an intelligent virtual assistant, designed to help providers care for patients. While this is not the first time AI has ventured into health care (see IBM’s “Watson”), it is the first time the idea has become mainstream and fully integrated into physician workflow. Much like the virtual assistants mentioned above, this one can use voice or mouse/keyboard interaction to find clinical information, simplify common tasks, and help with medical decision-making.
While exciting at first, the idea of artificially intelligent EHRs may sound terrifying to some who aren’t yet ready to trust any patient care to machines. Reassuringly, while the integrated virtual assistant mentioned above can make suggestions to guide physicians to the right data or offer decision support when available, it is primarily focused on interface enhancement to improve work flow. It is not yet capable of making true clinical decisions that remove the physician from care delivery, but computers that do the diagnostic work of physicians may be closer than you think.
Research done at Jefferson University in Philadelphia and published in the August 2017 edition of Radiology1 investigated the ability of deep-learning algorithms to interpret chest radiographs for the diagnosis of tuberculosis. The computers achieved an impressive reliability of 99%. While at first radiograph interpretation seems quite different than the diagnostic decision-making done in primary care, the fundamental skill required for both is similar: pattern recognition. To build those patterns, artificial intelligence requires an enormous number of data points, but that’s hardly a problem thanks to the continual collection of patient data through electronic health records. The amount of raw information available to these algorithms is growing exponentially by the day, and with time their predictive ability will be unmatched. So where will that leave us, the physicians, entrusted for generations with the responsibility of diagnosis? Possibly more satisfied than we are today.
There was a time – not long ago – when the body of available medical knowledge was incredibly limited. Diagnostic testing was primitive and often inaccurate, and the treatment provided by physicians was focused on supporting, communicating, and genuinely caring for patients and their families. In the past 50 years, medical knowledge has exploded, and diagnostic testing has become incredibly advanced. Sadly, at the same time physicians have begun to feel more like clerical workers: entering data, writing prescriptions, and filling out forms. As artificial intelligence assumes some of this busywork and takes much of the guesswork out of diagnosis, physicians may find greater job satisfaction as they provide the skills a computer never can: a human touch, a personal and reflective interpretation of a patient’s diagnosis, and a true emotional connection. Ask this of a computer, and the response will always be the same: “I’m sorry, doctor, I’m afraid I can’t do that.”
Reference
1. Lakhani, Paras & Sundaram, Baskaran, “Deep Learning at Chest Radiography: Automated Classification of Pulmonary Tuberculosis by Using Convolutional Neural Networks,” Radiology. 2017 Aug;284:574-82.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
In “2001: A Space Odyssey,” the epic 1968 film by Stanley Kubrick and Arthur C. Clarke, humanity makes first contact with an alien intelligence, and the course of history is irreversibly altered. Hailed as a watershed moment in science fiction, “2001” was considered way ahead of its time and raised a number of philosophical questions about what would happen if we ever encountered another form of life. Interestingly, the most noteworthy character in the film isn’t human or alien, but instead a new form of life altogether: an artificial intelligence (AI) known as the Heuristically programmed ALgorithmic computer 9000. HAL (as he is known colloquially) operates the Discovery One spacecraft, ferrying several scientists bound for Jupiter on a mission of exploration. Stating that he is “foolproof and incapable of error,” HAL’s superiority complex leads him to become the film’s antagonist, as he believes that human error is the cause of the difficulties they encounter. He eventually concludes that the best way to complete the mission is to eliminate human interference. When asked by scientist Dr. David Bowman to perform a simple function essential to the survival of the crew, HAL simply states “I’m sorry, Dave, I’m afraid I can’t do that.” Bowman is forced to disconnect HAL’s higher intellectual capabilities, reverting the computer to its most basic functions to ensure human survival.
Kubrick and Clarke may have been overly ambitious in predicting the progress of human space flight, but their call for concern over the risks of artificial intelligence seems quite prescient. Recently, billionaire entrepreneur Elon Musk (CEO of Tesla Motors and SpaceX) raised his concerns about AI, warning that, left unchecked, AI could be mankind’s final invention – one that could eventually destroy us. Other giants of the tech industry, including Bill Gates and Mark Zuckerberg, disagree. They believe AI represents tremendous promise for humanity and could usher in innovations unlike any we have ever seen.
A few weeks ago, we attended a national electronic health records conference where a well-known EHR vendor unveiled the new features in the upcoming release of their software. One of the most noteworthy additions was an intelligent virtual assistant, designed to help providers care for patients. While this is not the first time AI has ventured into health care (see IBM’s “Watson”), it is the first time the idea has become mainstream and fully integrated into physician workflow. Much like the virtual assistants mentioned above, this one can use voice or mouse/keyboard interaction to find clinical information, simplify common tasks, and help with medical decision-making.
While exciting at first, the idea of artificially intelligent EHRs may sound terrifying to some who aren’t yet ready to trust any patient care to machines. Reassuringly, while the integrated virtual assistant mentioned above can make suggestions to guide physicians to the right data or offer decision support when available, it is primarily focused on interface enhancement to improve work flow. It is not yet capable of making true clinical decisions that remove the physician from care delivery, but computers that do the diagnostic work of physicians may be closer than you think.
Research done at Jefferson University in Philadelphia and published in the August 2017 edition of Radiology1 investigated the ability of deep-learning algorithms to interpret chest radiographs for the diagnosis of tuberculosis. The computers achieved an impressive reliability of 99%. While at first radiograph interpretation seems quite different than the diagnostic decision-making done in primary care, the fundamental skill required for both is similar: pattern recognition. To build those patterns, artificial intelligence requires an enormous number of data points, but that’s hardly a problem thanks to the continual collection of patient data through electronic health records. The amount of raw information available to these algorithms is growing exponentially by the day, and with time their predictive ability will be unmatched. So where will that leave us, the physicians, entrusted for generations with the responsibility of diagnosis? Possibly more satisfied than we are today.
There was a time – not long ago – when the body of available medical knowledge was incredibly limited. Diagnostic testing was primitive and often inaccurate, and the treatment provided by physicians was focused on supporting, communicating, and genuinely caring for patients and their families. In the past 50 years, medical knowledge has exploded, and diagnostic testing has become incredibly advanced. Sadly, at the same time physicians have begun to feel more like clerical workers: entering data, writing prescriptions, and filling out forms. As artificial intelligence assumes some of this busywork and takes much of the guesswork out of diagnosis, physicians may find greater job satisfaction as they provide the skills a computer never can: a human touch, a personal and reflective interpretation of a patient’s diagnosis, and a true emotional connection. Ask this of a computer, and the response will always be the same: “I’m sorry, doctor, I’m afraid I can’t do that.”
Reference
1. Lakhani, Paras & Sundaram, Baskaran, “Deep Learning at Chest Radiography: Automated Classification of Pulmonary Tuberculosis by Using Convolutional Neural Networks,” Radiology. 2017 Aug;284:574-82.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
Now boarding: How we can skip coach and bump our patients up to first class
Cruising above the earth at 37,000 feet on the way back from vacation, my mind starts wandering. The impending reality of returning to work is setting in, and I can’t help but reflect on how the experience of a weary traveler trying to get home is like that of a weary patient trying to navigate modern health care. As it turns out, there are more than a few similarities, and that is not necessarily a good thing.
The modern airline industry is often cited by experts as a model for safety, efficiency, and innovation, though just a few decades ago this wasn’t the case. Several factors (for example, catastrophic crashes; the events of September 11th, 2001; the economic downturn) forced airlines to make radical improvements in how they operated – many of which I am quite thankful for as I gaze down upon America’s heartland from my window seat. Still, there are many who would say that in spite of (and sometimes because of) these improvements, air travel is the worst it’s ever been; airport lines are longer than ever, costs have steadily increased, and customer service has become little more than a quaint idea from a bygone era.
Most people deride the frustrations of air travel yet accept them as normal. The same expectations have unfortunately been set in health care. Patients wait, though waiting only contributes to anxiety and leads them to question the quality of their care. They also expect their journey to have many layover stops, though these involve even more waiting and often unnecessary redundancy. We need to streamline the care delivery process, and this is where technology can help.
First of all, we need to address the waiting. In health care, we tend to call this “access,” an ever-present problem for patients and providers. Thankfully, some recent innovations have helped significantly. The first of these innovations is online scheduling, which allows patients to find openings and schedule visits without the need to pick up the phone. Much like the ability to book a dinner reservation online, this is becoming an expectation for health care consumers. Participating practices and health systems can also use it as a marketing advantage; it is a fantastic way to recruit new patients as they search for a new provider online (that is, seeing that a physician has immediate openings may make the decision easier).
There are several companies providing third-party online scheduling services, and many of these can interface directly with electronic health records. EHR vendors themselves also provide this functionality to existing patients through an online web portal or mobile app. Either way, if you haven’t considered it yet, you should. It’s a great way to fill last-minute schedule openings and increase your patient base, all while improving access and patient satisfaction.
Another way to improve access is through telemedicine. We’ve written about this in prior columns, but it has certainly become more prevalent and available since then. Now more insurers are reimbursing for telemedicine services, and consumers are starting to embrace it as well. Consider some advantages: it’s more convenient for patients and often less expensive for those without insurance – cash prices tend to be in the $50-$75 range. It can also be more convenient for providers, as the typical telemedicine visit lasts only about 10 minutes and can be easily fit in last-minute. Better still, telemedicine can be a way for providers to now be paid for services they might have previously provided for free by telephone. It is critical to choose patients and conditions appropriate for these “virtual visits.” Medication checks, lab follow-ups, or rash evaluations are just a few examples, but with a little bit of thought it is easy to find dozens of other opportunities to use telemedicine to improve access.
In addition to access, we need to look for ways to improve efficiency and decrease redundancy when sending patients for testing and consultations. Recently, I had the experience of visiting a specialist for a minor medical issue. In spite of the fact that the specialist was a member of the same health system as my PCP, I still spent the first 15 minutes of my visit filling out paperwork that requested information easily available from my health record. There must be a better way.
Patients are beginning to question why, in the world of ubiquitous social media and connectivity, our computerized medical records can’t communicate. This is especially true when they are seeing physicians who are part of the same health system (as in my case). Thankfully, vendors have gotten the message and have begun allowing providers to collaborate, not only with physicians using the same software, but also with those using other EHRs through Health Information Exchanges (HIEs). Unfortunately, this alone won’t be enough. We must continue to promote the notion of patient-owned medical records, as that will be the only way to ensure true patient-centered care. In a future column, we’ll explore this concept in greater detail, but for now we’ll confirm our belief that universal interoperability is reasonable and possible.
As we are getting ready to land, I reflect on the wonderful vacation I just had and the tasks ahead at home, most of which I enjoy. Patients aren’t always as lucky; they are accessing medical care because they have to, not because they want to. Their “destination” is all too often an unfortunate diagnosis, unexpected surgical procedure, or lifetime of chronic discomfort. It is therefore incumbent on us, their care providers, to use the tools at our disposal to offer them the most efficient, most comfortable, and most connected journey possible.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
Cruising above the earth at 37,000 feet on the way back from vacation, my mind starts wandering. The impending reality of returning to work is setting in, and I can’t help but reflect on how the experience of a weary traveler trying to get home is like that of a weary patient trying to navigate modern health care. As it turns out, there are more than a few similarities, and that is not necessarily a good thing.
The modern airline industry is often cited by experts as a model for safety, efficiency, and innovation, though just a few decades ago this wasn’t the case. Several factors (for example, catastrophic crashes; the events of September 11th, 2001; the economic downturn) forced airlines to make radical improvements in how they operated – many of which I am quite thankful for as I gaze down upon America’s heartland from my window seat. Still, there are many who would say that in spite of (and sometimes because of) these improvements, air travel is the worst it’s ever been; airport lines are longer than ever, costs have steadily increased, and customer service has become little more than a quaint idea from a bygone era.
Most people deride the frustrations of air travel yet accept them as normal. The same expectations have unfortunately been set in health care. Patients wait, though waiting only contributes to anxiety and leads them to question the quality of their care. They also expect their journey to have many layover stops, though these involve even more waiting and often unnecessary redundancy. We need to streamline the care delivery process, and this is where technology can help.
First of all, we need to address the waiting. In health care, we tend to call this “access,” an ever-present problem for patients and providers. Thankfully, some recent innovations have helped significantly. The first of these innovations is online scheduling, which allows patients to find openings and schedule visits without the need to pick up the phone. Much like the ability to book a dinner reservation online, this is becoming an expectation for health care consumers. Participating practices and health systems can also use it as a marketing advantage; it is a fantastic way to recruit new patients as they search for a new provider online (that is, seeing that a physician has immediate openings may make the decision easier).
There are several companies providing third-party online scheduling services, and many of these can interface directly with electronic health records. EHR vendors themselves also provide this functionality to existing patients through an online web portal or mobile app. Either way, if you haven’t considered it yet, you should. It’s a great way to fill last-minute schedule openings and increase your patient base, all while improving access and patient satisfaction.
Another way to improve access is through telemedicine. We’ve written about this in prior columns, but it has certainly become more prevalent and available since then. Now more insurers are reimbursing for telemedicine services, and consumers are starting to embrace it as well. Consider some advantages: it’s more convenient for patients and often less expensive for those without insurance – cash prices tend to be in the $50-$75 range. It can also be more convenient for providers, as the typical telemedicine visit lasts only about 10 minutes and can be easily fit in last-minute. Better still, telemedicine can be a way for providers to now be paid for services they might have previously provided for free by telephone. It is critical to choose patients and conditions appropriate for these “virtual visits.” Medication checks, lab follow-ups, or rash evaluations are just a few examples, but with a little bit of thought it is easy to find dozens of other opportunities to use telemedicine to improve access.
In addition to access, we need to look for ways to improve efficiency and decrease redundancy when sending patients for testing and consultations. Recently, I had the experience of visiting a specialist for a minor medical issue. In spite of the fact that the specialist was a member of the same health system as my PCP, I still spent the first 15 minutes of my visit filling out paperwork that requested information easily available from my health record. There must be a better way.
Patients are beginning to question why, in the world of ubiquitous social media and connectivity, our computerized medical records can’t communicate. This is especially true when they are seeing physicians who are part of the same health system (as in my case). Thankfully, vendors have gotten the message and have begun allowing providers to collaborate, not only with physicians using the same software, but also with those using other EHRs through Health Information Exchanges (HIEs). Unfortunately, this alone won’t be enough. We must continue to promote the notion of patient-owned medical records, as that will be the only way to ensure true patient-centered care. In a future column, we’ll explore this concept in greater detail, but for now we’ll confirm our belief that universal interoperability is reasonable and possible.
As we are getting ready to land, I reflect on the wonderful vacation I just had and the tasks ahead at home, most of which I enjoy. Patients aren’t always as lucky; they are accessing medical care because they have to, not because they want to. Their “destination” is all too often an unfortunate diagnosis, unexpected surgical procedure, or lifetime of chronic discomfort. It is therefore incumbent on us, their care providers, to use the tools at our disposal to offer them the most efficient, most comfortable, and most connected journey possible.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
Cruising above the earth at 37,000 feet on the way back from vacation, my mind starts wandering. The impending reality of returning to work is setting in, and I can’t help but reflect on how the experience of a weary traveler trying to get home is like that of a weary patient trying to navigate modern health care. As it turns out, there are more than a few similarities, and that is not necessarily a good thing.
The modern airline industry is often cited by experts as a model for safety, efficiency, and innovation, though just a few decades ago this wasn’t the case. Several factors (for example, catastrophic crashes; the events of September 11th, 2001; the economic downturn) forced airlines to make radical improvements in how they operated – many of which I am quite thankful for as I gaze down upon America’s heartland from my window seat. Still, there are many who would say that in spite of (and sometimes because of) these improvements, air travel is the worst it’s ever been; airport lines are longer than ever, costs have steadily increased, and customer service has become little more than a quaint idea from a bygone era.
Most people deride the frustrations of air travel yet accept them as normal. The same expectations have unfortunately been set in health care. Patients wait, though waiting only contributes to anxiety and leads them to question the quality of their care. They also expect their journey to have many layover stops, though these involve even more waiting and often unnecessary redundancy. We need to streamline the care delivery process, and this is where technology can help.
First of all, we need to address the waiting. In health care, we tend to call this “access,” an ever-present problem for patients and providers. Thankfully, some recent innovations have helped significantly. The first of these innovations is online scheduling, which allows patients to find openings and schedule visits without the need to pick up the phone. Much like the ability to book a dinner reservation online, this is becoming an expectation for health care consumers. Participating practices and health systems can also use it as a marketing advantage; it is a fantastic way to recruit new patients as they search for a new provider online (that is, seeing that a physician has immediate openings may make the decision easier).
There are several companies providing third-party online scheduling services, and many of these can interface directly with electronic health records. EHR vendors themselves also provide this functionality to existing patients through an online web portal or mobile app. Either way, if you haven’t considered it yet, you should. It’s a great way to fill last-minute schedule openings and increase your patient base, all while improving access and patient satisfaction.
Another way to improve access is through telemedicine. We’ve written about this in prior columns, but it has certainly become more prevalent and available since then. Now more insurers are reimbursing for telemedicine services, and consumers are starting to embrace it as well. Consider some advantages: it’s more convenient for patients and often less expensive for those without insurance – cash prices tend to be in the $50-$75 range. It can also be more convenient for providers, as the typical telemedicine visit lasts only about 10 minutes and can be easily fit in last-minute. Better still, telemedicine can be a way for providers to now be paid for services they might have previously provided for free by telephone. It is critical to choose patients and conditions appropriate for these “virtual visits.” Medication checks, lab follow-ups, or rash evaluations are just a few examples, but with a little bit of thought it is easy to find dozens of other opportunities to use telemedicine to improve access.
In addition to access, we need to look for ways to improve efficiency and decrease redundancy when sending patients for testing and consultations. Recently, I had the experience of visiting a specialist for a minor medical issue. In spite of the fact that the specialist was a member of the same health system as my PCP, I still spent the first 15 minutes of my visit filling out paperwork that requested information easily available from my health record. There must be a better way.
Patients are beginning to question why, in the world of ubiquitous social media and connectivity, our computerized medical records can’t communicate. This is especially true when they are seeing physicians who are part of the same health system (as in my case). Thankfully, vendors have gotten the message and have begun allowing providers to collaborate, not only with physicians using the same software, but also with those using other EHRs through Health Information Exchanges (HIEs). Unfortunately, this alone won’t be enough. We must continue to promote the notion of patient-owned medical records, as that will be the only way to ensure true patient-centered care. In a future column, we’ll explore this concept in greater detail, but for now we’ll confirm our belief that universal interoperability is reasonable and possible.
As we are getting ready to land, I reflect on the wonderful vacation I just had and the tasks ahead at home, most of which I enjoy. Patients aren’t always as lucky; they are accessing medical care because they have to, not because they want to. Their “destination” is all too often an unfortunate diagnosis, unexpected surgical procedure, or lifetime of chronic discomfort. It is therefore incumbent on us, their care providers, to use the tools at our disposal to offer them the most efficient, most comfortable, and most connected journey possible.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
EHR Report: Don’t let the electronic health record do the driving
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
Restoring the promise of (really) meaningful use
When we started publishing the EHR Report several years ago, our very first column was a brief overview of a new federal incentive program known as Meaningful Use. At that time, the prospect of receiving thousands of dollars to adopt an electronic health record seemed exciting, and our dream of health care’s digital future appeared to be coming true.
Best of all, we as physicians would be paid to simply embrace it!
Unfortunately, it wasn’t long before that dream (for many at least) devolved into a nightmare. Electronic health records hadn’t been designed to fit into physicians’ long-established work flows, and just weren’t up to the challenge of increasing efficiency. In fact, EHRs quickly became virtual taskmasters, leaving physicians mired in a sea of clicks and slow-moving screens.
Frankly speaking, Meaningful Use hasn’t lived up to its promises. With measures obligating users to fill in a myriad of check-boxes and document often irrelevant information, the program has seemed less like an incentive and more like a penance.
To top it off, the all-or-nothing requirement has meant that – after a year of hard work – providers missing even one goal receive no payments at all, and instead are assessed financial penalties!
All of this has appropriately led physicians to become jaded – not excited – about the digital future.
Thankfully, there is reason for hope: 2017 marks the end of Meaningful Use under Medicare.
What’s new for 2017?
MACRA has a much grander scope and sets an even loftier goal: transforming care delivery to achieve better value and ultimately healthier patients.
Now, in case you’re not already confused by the number of programs cited above, there is one more we need to mention to explain the future of EHR incentives: the Merit-based Incentive Payment System, or MIPS, one of two tracks in the Quality Payment Program.
The majority of Medicare providers will choose this track, which focuses on four major components to determine reimbursement incentives: quality, improvement activities, advancing care information, and cost.
Depending on performance in each of these areas, participants will see a variable payment adjustment (upward or downward) in subsequent years (this is a percentage of Medicare payments that increases annually, beginning with a possible +/– 4% in 2019, to a maximum of +/– 9% in 2022).
Providers under MIPS who choose to attest for this year can select from three levels of participation:
1. Test: submission of only a minimal amount of 2017 data (such as one or two measures) to avoid penalty.
2. Partial: submission of 90 days’ worth of data, which may result in a neutral or positive payment adjustment (and may even earn the max adjustment).
3. Full: submission of a full year of data.
Here’s an example of how this will work: A provider who attests in March 2018 for the full 2017 year and does really well could see up to a 4% incentive bonus on Medicare payments in 2019. A provider who chooses not to attest would receive a penalty of 4%.
It’s worth noting here that MIPS expands upon the inclusion criteria set for Meaningful Use under Medicare. Medicare Part B clinicians are eligible to participate if they bill $30,000 in charges and see at least 100 Medicare patients annually. MIPS also broadens the list of eligible provider types. Physicians, nurse practitioners, physician assistants, clinical nurse specialists, and certified registered nurse anesthetists are all able to attest.
Advancing Care Information
Under MIPS, Meaningful Use is replaced by an initiative called Advancing Care Information, or ACI. In this new incarnation, there are fewer required measures, and they are much less onerous than they were under the former program.
Also, there are a number of optional measures. A provider may choose to attest to these nonrequired metrics to improve his or her chances of achieving the maximum incentive, but it isn’t necessary. There are also bonus measures involving public health registry reporting. These are optional but a sure bet to increase incentives. In all, the ACI component composes 25% of a provider’s final MIPS score.
For 2017, participants are able to choose one of two tracks in the ACI program, depending on their EHR’s certification year. (If you are confused by this or don’t know the status of your product, check with your vendor or go to https://chpl.healthit.gov to figure it out).
Providers with technology certified to the 2015 edition (or a combination of technologies from the 2014 and 2015 editions) can fully attest to the ACI objectives and measures or elect to use the transition objectives and measures. Those with 2014 edition software must choose the transition measures.
We will cover the specific measures in a future column, but for now we’ll note that both tracks are very similar and focus on protecting patient data, encouraging patient access to their own records, and sharing information electronically with other providers.
Rekindling the dream
We are certain that changing legislation won’t solve all of the problems inherent in current EHR systems, but we are always encouraged by any attempt to reduce the documentation burden on physicians. By eschewing thresholds, eliminating the all-or-nothing requirement, and reducing the number of required measures, the ACI program does seem to shift the focus away from volume and toward value.
That alone has the potential to restore our hope of a brighter future, and make our use of electronic health records significantly more meaningful.
Note: To learn more about Quality Payment Program and MIPS, we highly recommend an online resource published by the Centers for Medicare & Medicaid Services that is easy to follow and is full of useful information. It can be found at https://qpp.cms.gov.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
When we started publishing the EHR Report several years ago, our very first column was a brief overview of a new federal incentive program known as Meaningful Use. At that time, the prospect of receiving thousands of dollars to adopt an electronic health record seemed exciting, and our dream of health care’s digital future appeared to be coming true.
Best of all, we as physicians would be paid to simply embrace it!
Unfortunately, it wasn’t long before that dream (for many at least) devolved into a nightmare. Electronic health records hadn’t been designed to fit into physicians’ long-established work flows, and just weren’t up to the challenge of increasing efficiency. In fact, EHRs quickly became virtual taskmasters, leaving physicians mired in a sea of clicks and slow-moving screens.
Frankly speaking, Meaningful Use hasn’t lived up to its promises. With measures obligating users to fill in a myriad of check-boxes and document often irrelevant information, the program has seemed less like an incentive and more like a penance.
To top it off, the all-or-nothing requirement has meant that – after a year of hard work – providers missing even one goal receive no payments at all, and instead are assessed financial penalties!
All of this has appropriately led physicians to become jaded – not excited – about the digital future.
Thankfully, there is reason for hope: 2017 marks the end of Meaningful Use under Medicare.
What’s new for 2017?
MACRA has a much grander scope and sets an even loftier goal: transforming care delivery to achieve better value and ultimately healthier patients.
Now, in case you’re not already confused by the number of programs cited above, there is one more we need to mention to explain the future of EHR incentives: the Merit-based Incentive Payment System, or MIPS, one of two tracks in the Quality Payment Program.
The majority of Medicare providers will choose this track, which focuses on four major components to determine reimbursement incentives: quality, improvement activities, advancing care information, and cost.
Depending on performance in each of these areas, participants will see a variable payment adjustment (upward or downward) in subsequent years (this is a percentage of Medicare payments that increases annually, beginning with a possible +/– 4% in 2019, to a maximum of +/– 9% in 2022).
Providers under MIPS who choose to attest for this year can select from three levels of participation:
1. Test: submission of only a minimal amount of 2017 data (such as one or two measures) to avoid penalty.
2. Partial: submission of 90 days’ worth of data, which may result in a neutral or positive payment adjustment (and may even earn the max adjustment).
3. Full: submission of a full year of data.
Here’s an example of how this will work: A provider who attests in March 2018 for the full 2017 year and does really well could see up to a 4% incentive bonus on Medicare payments in 2019. A provider who chooses not to attest would receive a penalty of 4%.
It’s worth noting here that MIPS expands upon the inclusion criteria set for Meaningful Use under Medicare. Medicare Part B clinicians are eligible to participate if they bill $30,000 in charges and see at least 100 Medicare patients annually. MIPS also broadens the list of eligible provider types. Physicians, nurse practitioners, physician assistants, clinical nurse specialists, and certified registered nurse anesthetists are all able to attest.
Advancing Care Information
Under MIPS, Meaningful Use is replaced by an initiative called Advancing Care Information, or ACI. In this new incarnation, there are fewer required measures, and they are much less onerous than they were under the former program.
Also, there are a number of optional measures. A provider may choose to attest to these nonrequired metrics to improve his or her chances of achieving the maximum incentive, but it isn’t necessary. There are also bonus measures involving public health registry reporting. These are optional but a sure bet to increase incentives. In all, the ACI component composes 25% of a provider’s final MIPS score.
For 2017, participants are able to choose one of two tracks in the ACI program, depending on their EHR’s certification year. (If you are confused by this or don’t know the status of your product, check with your vendor or go to https://chpl.healthit.gov to figure it out).
Providers with technology certified to the 2015 edition (or a combination of technologies from the 2014 and 2015 editions) can fully attest to the ACI objectives and measures or elect to use the transition objectives and measures. Those with 2014 edition software must choose the transition measures.
We will cover the specific measures in a future column, but for now we’ll note that both tracks are very similar and focus on protecting patient data, encouraging patient access to their own records, and sharing information electronically with other providers.
Rekindling the dream
We are certain that changing legislation won’t solve all of the problems inherent in current EHR systems, but we are always encouraged by any attempt to reduce the documentation burden on physicians. By eschewing thresholds, eliminating the all-or-nothing requirement, and reducing the number of required measures, the ACI program does seem to shift the focus away from volume and toward value.
That alone has the potential to restore our hope of a brighter future, and make our use of electronic health records significantly more meaningful.
Note: To learn more about Quality Payment Program and MIPS, we highly recommend an online resource published by the Centers for Medicare & Medicaid Services that is easy to follow and is full of useful information. It can be found at https://qpp.cms.gov.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
When we started publishing the EHR Report several years ago, our very first column was a brief overview of a new federal incentive program known as Meaningful Use. At that time, the prospect of receiving thousands of dollars to adopt an electronic health record seemed exciting, and our dream of health care’s digital future appeared to be coming true.
Best of all, we as physicians would be paid to simply embrace it!
Unfortunately, it wasn’t long before that dream (for many at least) devolved into a nightmare. Electronic health records hadn’t been designed to fit into physicians’ long-established work flows, and just weren’t up to the challenge of increasing efficiency. In fact, EHRs quickly became virtual taskmasters, leaving physicians mired in a sea of clicks and slow-moving screens.
Frankly speaking, Meaningful Use hasn’t lived up to its promises. With measures obligating users to fill in a myriad of check-boxes and document often irrelevant information, the program has seemed less like an incentive and more like a penance.
To top it off, the all-or-nothing requirement has meant that – after a year of hard work – providers missing even one goal receive no payments at all, and instead are assessed financial penalties!
All of this has appropriately led physicians to become jaded – not excited – about the digital future.
Thankfully, there is reason for hope: 2017 marks the end of Meaningful Use under Medicare.
What’s new for 2017?
MACRA has a much grander scope and sets an even loftier goal: transforming care delivery to achieve better value and ultimately healthier patients.
Now, in case you’re not already confused by the number of programs cited above, there is one more we need to mention to explain the future of EHR incentives: the Merit-based Incentive Payment System, or MIPS, one of two tracks in the Quality Payment Program.
The majority of Medicare providers will choose this track, which focuses on four major components to determine reimbursement incentives: quality, improvement activities, advancing care information, and cost.
Depending on performance in each of these areas, participants will see a variable payment adjustment (upward or downward) in subsequent years (this is a percentage of Medicare payments that increases annually, beginning with a possible +/– 4% in 2019, to a maximum of +/– 9% in 2022).
Providers under MIPS who choose to attest for this year can select from three levels of participation:
1. Test: submission of only a minimal amount of 2017 data (such as one or two measures) to avoid penalty.
2. Partial: submission of 90 days’ worth of data, which may result in a neutral or positive payment adjustment (and may even earn the max adjustment).
3. Full: submission of a full year of data.
Here’s an example of how this will work: A provider who attests in March 2018 for the full 2017 year and does really well could see up to a 4% incentive bonus on Medicare payments in 2019. A provider who chooses not to attest would receive a penalty of 4%.
It’s worth noting here that MIPS expands upon the inclusion criteria set for Meaningful Use under Medicare. Medicare Part B clinicians are eligible to participate if they bill $30,000 in charges and see at least 100 Medicare patients annually. MIPS also broadens the list of eligible provider types. Physicians, nurse practitioners, physician assistants, clinical nurse specialists, and certified registered nurse anesthetists are all able to attest.
Advancing Care Information
Under MIPS, Meaningful Use is replaced by an initiative called Advancing Care Information, or ACI. In this new incarnation, there are fewer required measures, and they are much less onerous than they were under the former program.
Also, there are a number of optional measures. A provider may choose to attest to these nonrequired metrics to improve his or her chances of achieving the maximum incentive, but it isn’t necessary. There are also bonus measures involving public health registry reporting. These are optional but a sure bet to increase incentives. In all, the ACI component composes 25% of a provider’s final MIPS score.
For 2017, participants are able to choose one of two tracks in the ACI program, depending on their EHR’s certification year. (If you are confused by this or don’t know the status of your product, check with your vendor or go to https://chpl.healthit.gov to figure it out).
Providers with technology certified to the 2015 edition (or a combination of technologies from the 2014 and 2015 editions) can fully attest to the ACI objectives and measures or elect to use the transition objectives and measures. Those with 2014 edition software must choose the transition measures.
We will cover the specific measures in a future column, but for now we’ll note that both tracks are very similar and focus on protecting patient data, encouraging patient access to their own records, and sharing information electronically with other providers.
Rekindling the dream
We are certain that changing legislation won’t solve all of the problems inherent in current EHR systems, but we are always encouraged by any attempt to reduce the documentation burden on physicians. By eschewing thresholds, eliminating the all-or-nothing requirement, and reducing the number of required measures, the ACI program does seem to shift the focus away from volume and toward value.
That alone has the potential to restore our hope of a brighter future, and make our use of electronic health records significantly more meaningful.
Note: To learn more about Quality Payment Program and MIPS, we highly recommend an online resource published by the Centers for Medicare & Medicaid Services that is easy to follow and is full of useful information. It can be found at https://qpp.cms.gov.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.