User login
Amniotic fluid embolism: Management using a checklist
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
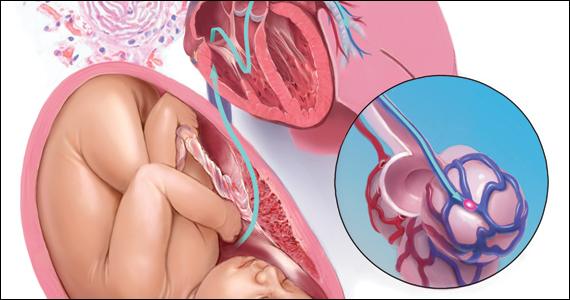
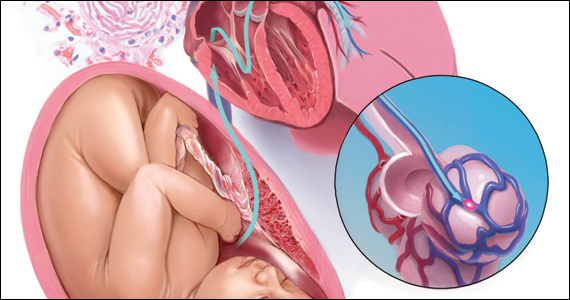
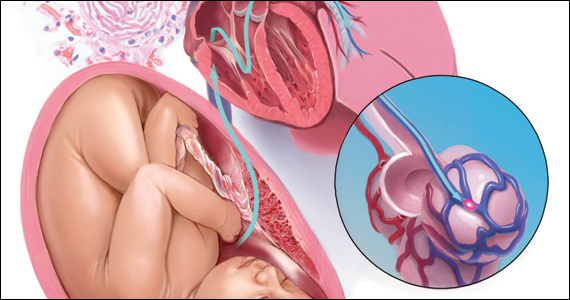
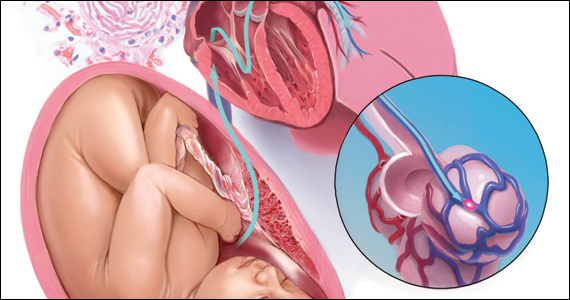
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
Point/Counterpoint: Glucose Sensors and Insulin Pumps for Diabetic Pregnancies?
Yes – Continuous Glucose Monitoring and Insulin Pumps Improve Glycemic Control
Consider the case of a 33-year-old teacher who has a toddler in preschool, regularly attends Pilates classes, and is in her second pregnancy. Her privacy is limited, and her lunchtime varies by at least 30 minutes. In her first pregnancy, when she used multiple daily injections (MDI) for insulin injection, her hemoglobin A1c at 36 weeks’ gestation was 7.2%, and her baby’s birth weight was 4,200 g. This time around, she cannot get her fasting blood glucose under 110 mg/dL without experiencing marked hypoglycemia around 3:30 a.m.
In her case, the demonstrated benefits of continuous glucose monitoring (CGM) and an insulin pump (for continuous subcutaneous insulin infusion, or CSII) make this method of insulin administration a compelling – and even obvious – choice over MDI. A glucose sensor and insulin pump would improve her glucose control, bring down her HbA1c, and lessen the frequency and severity of hypoglycemic episodes, while better meshing with her lifestyle.
She is far from the only type of patient who would benefit, however. Modern CSII pumps (with Bolus Wizard calculators) have been around for a decade, yet we significantly underutilize them. Many, if not most, insulin-requiring pregnant women are good candidates for glucose sensors and insulin pumps.
CSII improves glucose control by providing "background" changes in insulin dosing to match the complexities of metabolism in pregnancy, and CGM (as opposed to self–blood glucose monitoring) improves glucose control by removing the fear of unexpected lows, which is a big issue in my patients, and by warning of impending highs.
Together, today’s equipment also improves patients’ ability to administer insulin in social and business settings. The equipment is also easily programmable and understandable to women who routinely use electronic devices.
A Cochrane systematic review of CSII vs. MDI in pregnancy, published in 2007, unfortunately was not that telling for obstetrics, as only two of the seven available randomized trials were deemed appropriate for meta-analysis. While the mean birth weight was higher in the CSII group, there were no significant differences in macrosomia or any other outcomes, and the reviewers warned they could not draw any conclusions because of the dearth of data. It is important to note, too, that the studies involved ’90s-style pumps (Cochrane Database Syst. Rev. 2007 [doi:10.1002/14651858.CD005542.pub2]).
Fortunately, outside of pregnant populations, we see quite a bit of data on CSII v. MDI. For instance, a 2010 Cochrane systematic review of CSII v. MDI covering 23 randomized controlled trials of 976 nonpregnant patients with type 1 diabetes found a statistically significant difference in HbA1c favoring CSII (–0.3%), as well as a reduction in severe hypoglycemia and higher quality of life scores (Cochrane Database Syst. Rev. 2010 [doi:10.1002/14651858.CD005103.pub2]).
A randomized, controlled, crossover trial published in 2006 called the 5-Nations Trial similarly showed that CSII treatment in individuals with type 1 diabetes resulted in lower HbA1c, lower mean blood glucose level, less fluctuation in glucose levels, and higher quality of life than MDI (Diabet. Med. 2006;23:141-7).
CGM technology is rapidly evolving. A randomized controlled trial published this year found that patients receiving CGM spent significantly less time in hypoglycemia each day and had a concomitant decrease in HbA1c (again –0.3%, approximately). Normoglycemia was significantly longer (mean of 17.6 v. 16 hours per day). The 120 type 1 patients in the study had been randomly assigned to either receive real-time CGM or perform conventional self-monitoring (while wearing a masked CGM device) (Diabetes Care 2011;34:795-800).
Another smaller study of patients with type 1 diabetes or gestational diabetes mellitus being treated with MDI found that nocturnal hypoglycemic events dropped significantly when the patients switched to CGM.
Granted, the false alarms that occur with glucose sensors can be disconcerting, the equipment is expensive, and patients have to enter a series of finger-stick blood sugar readings into the monitor for calibration. Still, most patients place a value on being able to get real-time blood glucose readings at any time, even when asleep, busy, or distracted. And they can always temporarily suspend their system – to get ready for bed, for example, or to go to Pilates classes.
Dr. Moore is professor and chair of reproductive medicine at the University of California, San Diego. He said he had no relevant financial disclosures.
No – There Is Little Data Showing Improved Outcomes
I use these tools in less than one-third of my patients with type 1 diabetes, and only rarely in patients with type 2 diabetes or gestational diabetes. There is very little evidence about the efficacy and implications of monitoring. Because of this, and because it is expensive, many payers do not reimburse for continuous glucose monitoring (CGM).
The goals of monitoring and treatment are very different. We monitor in order to guide treatment, to guide further diagnostic testing, to predict outcome, and to understand pathophysiology. But when we consider the value of glucose sensors and insulin pumps, we really need to consider the goals of treatment, which include reducing hyperglycemia without tripping over the threshold into hypoglycemia, and reducing short- and long-term neonatal and maternal complications of diabetes.
We have little data to guide us. A 2007 meta-analysis of randomized controlled trials comparing continuous subcutaneous insulin infusion (CSII) to multiple daily injections (MDI) in pregnant patients – an analysis separate from the Cochrane systematic review of 2007 that Dr. Moore mentions – found no significant differences in glycemic control or pregnancy outcomes. The studies included were published between 1986 and 1993, and since then, there have been no randomized trials comparing CSII and MDI in pregnant women (Am. J. Obstet. Gynecol. 2007;197:447-56).
With respect to CGM, a study reported by Dr. Y. Yogev and his associates in 2003 showed some promise: It compared the daily glycemic profiles reflected by continuous and intermittent blood glucose monitoring in pregnant women with type 1 diabetes, and found that CGM recorded high postprandial blood glucose levels and nocturnal hypoglycemic events that were unrecognized by intermittent monitoring. The question remains, however, whether such information leads to clinical interventions that can improve outcomes (Obstet. Gynecol. 2003;101:633-8).
A study published a year later, also by Dr. Yogev, showed that asymptomatic hypoglycemic events were surprisingly common in insulin- and glyburide-treated patients with gestational diabetes mellitus. The findings were eye-opening, but we really don’t know the significance of such hypoglycemic events.
We take it as a matter of faith that it’s bad to be hypoglycemic. In reality we know very little about what’s "normal" and "abnormal" in diabetic pregnant women and nondiabetic pregnant women.
In the only randomized controlled trial of CGM during pregnancy, women with type 1 and type 2 diabetes who were early in their pregnancies were assigned to perform self–blood glucose monitoring seven times a day or to have professional CGM for 1-week periods every 4-6 weeks. Findings in both groups were used to adjust therapy. By 36 weeks’ gestation, the CGM group had significantly lower HbA1c. Birth weights and the rate of macrosomia also were reduced (BMJ 2008;337:a1680).
The findings were impressive, but some of the data are unusual. For instance, the incidence of large-for-gestational-age (LGA) infants was reduced from 60% to 35%; both of these rates are high compared with rates at other centers. Data from the California Sweet Success program – a statewide effort to collect and share data on diabetes in pregnancy – show LGA in patients with type 1, type 2, and gestational diabetes to be 22.5%, 20%, and 11.4%, respectively – 27% of the type 1 patients were on CSII.
The American Association of Clinical Endocrinologists last year published a consensus statement recommending CGM for patients with type 1 diabetes who have certain risk factors, like frequent hypoglycemia or HbA1c over target. The AACE statement also includes those who are pregnant or about to become pregnant as ideal candidates for CGM, but curiously it provides no data to support this.
We have much more to learn. It is telling that in a recently published evaluation of a closed-loop insulin delivery model (an "artificial pancreas") in pregnant women with type 1 diabetes, investigators concluded that "before outpatient closed-loop studies proceed, they must be supported by scientifically rigorous data on safety and efficacy of real-time CGM," as well as more data on the algorithm for adjusting insulin infusion rates based on glycemic levels seen in pregnancy.
Dr. Combs is with Obstetrix Medical Group in San Jose, Calif. He said he had no relevant financial disclosures.
This feature is based on presentations given by Dr. Moore and Dr. Combs at the annual meeting of the Diabetes in Pregnancy Study Group of North America in Washington, D.C.
Yes – Continuous Glucose Monitoring and Insulin Pumps Improve Glycemic Control
Consider the case of a 33-year-old teacher who has a toddler in preschool, regularly attends Pilates classes, and is in her second pregnancy. Her privacy is limited, and her lunchtime varies by at least 30 minutes. In her first pregnancy, when she used multiple daily injections (MDI) for insulin injection, her hemoglobin A1c at 36 weeks’ gestation was 7.2%, and her baby’s birth weight was 4,200 g. This time around, she cannot get her fasting blood glucose under 110 mg/dL without experiencing marked hypoglycemia around 3:30 a.m.
In her case, the demonstrated benefits of continuous glucose monitoring (CGM) and an insulin pump (for continuous subcutaneous insulin infusion, or CSII) make this method of insulin administration a compelling – and even obvious – choice over MDI. A glucose sensor and insulin pump would improve her glucose control, bring down her HbA1c, and lessen the frequency and severity of hypoglycemic episodes, while better meshing with her lifestyle.
She is far from the only type of patient who would benefit, however. Modern CSII pumps (with Bolus Wizard calculators) have been around for a decade, yet we significantly underutilize them. Many, if not most, insulin-requiring pregnant women are good candidates for glucose sensors and insulin pumps.
CSII improves glucose control by providing "background" changes in insulin dosing to match the complexities of metabolism in pregnancy, and CGM (as opposed to self–blood glucose monitoring) improves glucose control by removing the fear of unexpected lows, which is a big issue in my patients, and by warning of impending highs.
Together, today’s equipment also improves patients’ ability to administer insulin in social and business settings. The equipment is also easily programmable and understandable to women who routinely use electronic devices.
A Cochrane systematic review of CSII vs. MDI in pregnancy, published in 2007, unfortunately was not that telling for obstetrics, as only two of the seven available randomized trials were deemed appropriate for meta-analysis. While the mean birth weight was higher in the CSII group, there were no significant differences in macrosomia or any other outcomes, and the reviewers warned they could not draw any conclusions because of the dearth of data. It is important to note, too, that the studies involved ’90s-style pumps (Cochrane Database Syst. Rev. 2007 [doi:10.1002/14651858.CD005542.pub2]).
Fortunately, outside of pregnant populations, we see quite a bit of data on CSII v. MDI. For instance, a 2010 Cochrane systematic review of CSII v. MDI covering 23 randomized controlled trials of 976 nonpregnant patients with type 1 diabetes found a statistically significant difference in HbA1c favoring CSII (–0.3%), as well as a reduction in severe hypoglycemia and higher quality of life scores (Cochrane Database Syst. Rev. 2010 [doi:10.1002/14651858.CD005103.pub2]).
A randomized, controlled, crossover trial published in 2006 called the 5-Nations Trial similarly showed that CSII treatment in individuals with type 1 diabetes resulted in lower HbA1c, lower mean blood glucose level, less fluctuation in glucose levels, and higher quality of life than MDI (Diabet. Med. 2006;23:141-7).
CGM technology is rapidly evolving. A randomized controlled trial published this year found that patients receiving CGM spent significantly less time in hypoglycemia each day and had a concomitant decrease in HbA1c (again –0.3%, approximately). Normoglycemia was significantly longer (mean of 17.6 v. 16 hours per day). The 120 type 1 patients in the study had been randomly assigned to either receive real-time CGM or perform conventional self-monitoring (while wearing a masked CGM device) (Diabetes Care 2011;34:795-800).
Another smaller study of patients with type 1 diabetes or gestational diabetes mellitus being treated with MDI found that nocturnal hypoglycemic events dropped significantly when the patients switched to CGM.
Granted, the false alarms that occur with glucose sensors can be disconcerting, the equipment is expensive, and patients have to enter a series of finger-stick blood sugar readings into the monitor for calibration. Still, most patients place a value on being able to get real-time blood glucose readings at any time, even when asleep, busy, or distracted. And they can always temporarily suspend their system – to get ready for bed, for example, or to go to Pilates classes.
Dr. Moore is professor and chair of reproductive medicine at the University of California, San Diego. He said he had no relevant financial disclosures.
No – There Is Little Data Showing Improved Outcomes
I use these tools in less than one-third of my patients with type 1 diabetes, and only rarely in patients with type 2 diabetes or gestational diabetes. There is very little evidence about the efficacy and implications of monitoring. Because of this, and because it is expensive, many payers do not reimburse for continuous glucose monitoring (CGM).
The goals of monitoring and treatment are very different. We monitor in order to guide treatment, to guide further diagnostic testing, to predict outcome, and to understand pathophysiology. But when we consider the value of glucose sensors and insulin pumps, we really need to consider the goals of treatment, which include reducing hyperglycemia without tripping over the threshold into hypoglycemia, and reducing short- and long-term neonatal and maternal complications of diabetes.
We have little data to guide us. A 2007 meta-analysis of randomized controlled trials comparing continuous subcutaneous insulin infusion (CSII) to multiple daily injections (MDI) in pregnant patients – an analysis separate from the Cochrane systematic review of 2007 that Dr. Moore mentions – found no significant differences in glycemic control or pregnancy outcomes. The studies included were published between 1986 and 1993, and since then, there have been no randomized trials comparing CSII and MDI in pregnant women (Am. J. Obstet. Gynecol. 2007;197:447-56).
With respect to CGM, a study reported by Dr. Y. Yogev and his associates in 2003 showed some promise: It compared the daily glycemic profiles reflected by continuous and intermittent blood glucose monitoring in pregnant women with type 1 diabetes, and found that CGM recorded high postprandial blood glucose levels and nocturnal hypoglycemic events that were unrecognized by intermittent monitoring. The question remains, however, whether such information leads to clinical interventions that can improve outcomes (Obstet. Gynecol. 2003;101:633-8).
A study published a year later, also by Dr. Yogev, showed that asymptomatic hypoglycemic events were surprisingly common in insulin- and glyburide-treated patients with gestational diabetes mellitus. The findings were eye-opening, but we really don’t know the significance of such hypoglycemic events.
We take it as a matter of faith that it’s bad to be hypoglycemic. In reality we know very little about what’s "normal" and "abnormal" in diabetic pregnant women and nondiabetic pregnant women.
In the only randomized controlled trial of CGM during pregnancy, women with type 1 and type 2 diabetes who were early in their pregnancies were assigned to perform self–blood glucose monitoring seven times a day or to have professional CGM for 1-week periods every 4-6 weeks. Findings in both groups were used to adjust therapy. By 36 weeks’ gestation, the CGM group had significantly lower HbA1c. Birth weights and the rate of macrosomia also were reduced (BMJ 2008;337:a1680).
The findings were impressive, but some of the data are unusual. For instance, the incidence of large-for-gestational-age (LGA) infants was reduced from 60% to 35%; both of these rates are high compared with rates at other centers. Data from the California Sweet Success program – a statewide effort to collect and share data on diabetes in pregnancy – show LGA in patients with type 1, type 2, and gestational diabetes to be 22.5%, 20%, and 11.4%, respectively – 27% of the type 1 patients were on CSII.
The American Association of Clinical Endocrinologists last year published a consensus statement recommending CGM for patients with type 1 diabetes who have certain risk factors, like frequent hypoglycemia or HbA1c over target. The AACE statement also includes those who are pregnant or about to become pregnant as ideal candidates for CGM, but curiously it provides no data to support this.
We have much more to learn. It is telling that in a recently published evaluation of a closed-loop insulin delivery model (an "artificial pancreas") in pregnant women with type 1 diabetes, investigators concluded that "before outpatient closed-loop studies proceed, they must be supported by scientifically rigorous data on safety and efficacy of real-time CGM," as well as more data on the algorithm for adjusting insulin infusion rates based on glycemic levels seen in pregnancy.
Dr. Combs is with Obstetrix Medical Group in San Jose, Calif. He said he had no relevant financial disclosures.
This feature is based on presentations given by Dr. Moore and Dr. Combs at the annual meeting of the Diabetes in Pregnancy Study Group of North America in Washington, D.C.
Yes – Continuous Glucose Monitoring and Insulin Pumps Improve Glycemic Control
Consider the case of a 33-year-old teacher who has a toddler in preschool, regularly attends Pilates classes, and is in her second pregnancy. Her privacy is limited, and her lunchtime varies by at least 30 minutes. In her first pregnancy, when she used multiple daily injections (MDI) for insulin injection, her hemoglobin A1c at 36 weeks’ gestation was 7.2%, and her baby’s birth weight was 4,200 g. This time around, she cannot get her fasting blood glucose under 110 mg/dL without experiencing marked hypoglycemia around 3:30 a.m.
In her case, the demonstrated benefits of continuous glucose monitoring (CGM) and an insulin pump (for continuous subcutaneous insulin infusion, or CSII) make this method of insulin administration a compelling – and even obvious – choice over MDI. A glucose sensor and insulin pump would improve her glucose control, bring down her HbA1c, and lessen the frequency and severity of hypoglycemic episodes, while better meshing with her lifestyle.
She is far from the only type of patient who would benefit, however. Modern CSII pumps (with Bolus Wizard calculators) have been around for a decade, yet we significantly underutilize them. Many, if not most, insulin-requiring pregnant women are good candidates for glucose sensors and insulin pumps.
CSII improves glucose control by providing "background" changes in insulin dosing to match the complexities of metabolism in pregnancy, and CGM (as opposed to self–blood glucose monitoring) improves glucose control by removing the fear of unexpected lows, which is a big issue in my patients, and by warning of impending highs.
Together, today’s equipment also improves patients’ ability to administer insulin in social and business settings. The equipment is also easily programmable and understandable to women who routinely use electronic devices.
A Cochrane systematic review of CSII vs. MDI in pregnancy, published in 2007, unfortunately was not that telling for obstetrics, as only two of the seven available randomized trials were deemed appropriate for meta-analysis. While the mean birth weight was higher in the CSII group, there were no significant differences in macrosomia or any other outcomes, and the reviewers warned they could not draw any conclusions because of the dearth of data. It is important to note, too, that the studies involved ’90s-style pumps (Cochrane Database Syst. Rev. 2007 [doi:10.1002/14651858.CD005542.pub2]).
Fortunately, outside of pregnant populations, we see quite a bit of data on CSII v. MDI. For instance, a 2010 Cochrane systematic review of CSII v. MDI covering 23 randomized controlled trials of 976 nonpregnant patients with type 1 diabetes found a statistically significant difference in HbA1c favoring CSII (–0.3%), as well as a reduction in severe hypoglycemia and higher quality of life scores (Cochrane Database Syst. Rev. 2010 [doi:10.1002/14651858.CD005103.pub2]).
A randomized, controlled, crossover trial published in 2006 called the 5-Nations Trial similarly showed that CSII treatment in individuals with type 1 diabetes resulted in lower HbA1c, lower mean blood glucose level, less fluctuation in glucose levels, and higher quality of life than MDI (Diabet. Med. 2006;23:141-7).
CGM technology is rapidly evolving. A randomized controlled trial published this year found that patients receiving CGM spent significantly less time in hypoglycemia each day and had a concomitant decrease in HbA1c (again –0.3%, approximately). Normoglycemia was significantly longer (mean of 17.6 v. 16 hours per day). The 120 type 1 patients in the study had been randomly assigned to either receive real-time CGM or perform conventional self-monitoring (while wearing a masked CGM device) (Diabetes Care 2011;34:795-800).
Another smaller study of patients with type 1 diabetes or gestational diabetes mellitus being treated with MDI found that nocturnal hypoglycemic events dropped significantly when the patients switched to CGM.
Granted, the false alarms that occur with glucose sensors can be disconcerting, the equipment is expensive, and patients have to enter a series of finger-stick blood sugar readings into the monitor for calibration. Still, most patients place a value on being able to get real-time blood glucose readings at any time, even when asleep, busy, or distracted. And they can always temporarily suspend their system – to get ready for bed, for example, or to go to Pilates classes.
Dr. Moore is professor and chair of reproductive medicine at the University of California, San Diego. He said he had no relevant financial disclosures.
No – There Is Little Data Showing Improved Outcomes
I use these tools in less than one-third of my patients with type 1 diabetes, and only rarely in patients with type 2 diabetes or gestational diabetes. There is very little evidence about the efficacy and implications of monitoring. Because of this, and because it is expensive, many payers do not reimburse for continuous glucose monitoring (CGM).
The goals of monitoring and treatment are very different. We monitor in order to guide treatment, to guide further diagnostic testing, to predict outcome, and to understand pathophysiology. But when we consider the value of glucose sensors and insulin pumps, we really need to consider the goals of treatment, which include reducing hyperglycemia without tripping over the threshold into hypoglycemia, and reducing short- and long-term neonatal and maternal complications of diabetes.
We have little data to guide us. A 2007 meta-analysis of randomized controlled trials comparing continuous subcutaneous insulin infusion (CSII) to multiple daily injections (MDI) in pregnant patients – an analysis separate from the Cochrane systematic review of 2007 that Dr. Moore mentions – found no significant differences in glycemic control or pregnancy outcomes. The studies included were published between 1986 and 1993, and since then, there have been no randomized trials comparing CSII and MDI in pregnant women (Am. J. Obstet. Gynecol. 2007;197:447-56).
With respect to CGM, a study reported by Dr. Y. Yogev and his associates in 2003 showed some promise: It compared the daily glycemic profiles reflected by continuous and intermittent blood glucose monitoring in pregnant women with type 1 diabetes, and found that CGM recorded high postprandial blood glucose levels and nocturnal hypoglycemic events that were unrecognized by intermittent monitoring. The question remains, however, whether such information leads to clinical interventions that can improve outcomes (Obstet. Gynecol. 2003;101:633-8).
A study published a year later, also by Dr. Yogev, showed that asymptomatic hypoglycemic events were surprisingly common in insulin- and glyburide-treated patients with gestational diabetes mellitus. The findings were eye-opening, but we really don’t know the significance of such hypoglycemic events.
We take it as a matter of faith that it’s bad to be hypoglycemic. In reality we know very little about what’s "normal" and "abnormal" in diabetic pregnant women and nondiabetic pregnant women.
In the only randomized controlled trial of CGM during pregnancy, women with type 1 and type 2 diabetes who were early in their pregnancies were assigned to perform self–blood glucose monitoring seven times a day or to have professional CGM for 1-week periods every 4-6 weeks. Findings in both groups were used to adjust therapy. By 36 weeks’ gestation, the CGM group had significantly lower HbA1c. Birth weights and the rate of macrosomia also were reduced (BMJ 2008;337:a1680).
The findings were impressive, but some of the data are unusual. For instance, the incidence of large-for-gestational-age (LGA) infants was reduced from 60% to 35%; both of these rates are high compared with rates at other centers. Data from the California Sweet Success program – a statewide effort to collect and share data on diabetes in pregnancy – show LGA in patients with type 1, type 2, and gestational diabetes to be 22.5%, 20%, and 11.4%, respectively – 27% of the type 1 patients were on CSII.
The American Association of Clinical Endocrinologists last year published a consensus statement recommending CGM for patients with type 1 diabetes who have certain risk factors, like frequent hypoglycemia or HbA1c over target. The AACE statement also includes those who are pregnant or about to become pregnant as ideal candidates for CGM, but curiously it provides no data to support this.
We have much more to learn. It is telling that in a recently published evaluation of a closed-loop insulin delivery model (an "artificial pancreas") in pregnant women with type 1 diabetes, investigators concluded that "before outpatient closed-loop studies proceed, they must be supported by scientifically rigorous data on safety and efficacy of real-time CGM," as well as more data on the algorithm for adjusting insulin infusion rates based on glycemic levels seen in pregnancy.
Dr. Combs is with Obstetrix Medical Group in San Jose, Calif. He said he had no relevant financial disclosures.
This feature is based on presentations given by Dr. Moore and Dr. Combs at the annual meeting of the Diabetes in Pregnancy Study Group of North America in Washington, D.C.