User login
Ferric citrate effective for anemia in non–dialysis-dependent CKD
CHICAGO – Ferric citrate was safe and effective for treatment of iron-deficiency anemia in patients who had non–dialysis-dependent chronic kidney disease (NDD-CKD), based on data from a phase III, randomized, double-blind study.
The responses were durable, and none of the patients received erythropoiesis-stimulating agents (ESAs), presenter Pablo Pergola, MD, PhD, of Renal Associates, San Antonio, said in an interview at a meeting sponsored by the American Society of Nephrology.
The trial involved 234 anemic adults who had NDD-CKD and had not responded to oral iron supplements. The subjects were randomized to receive oral ferric citrate (n = 117) or placebo (n = 115) with meals (one patient did not receive placebo and laboratory data were lacking for one patient). The mean dose in the treatment arm was 5 pills per day.
The primary endpoint was the proportion of patients with hemoglobin (Hgb) greater than or equal to 1.0 g/dL anytime from baseline through week 16. Secondary endpoints included mean changes from baseline in Hgb, transferrin saturation, ferritin, and serum phosphate and evidence of sustained treatment effect based on target changes in Hgb with time.
Both arms were comparable at baseline for demographic and clinical characteristics, including phosphorus and hemoglobin levels and estimated glomerular filtration rate.
The primary endpoint was met by 51.2% of patients receiving ferric citrate and 19.1% of patients receiving placebo (P less than .001). All secondary efficacy endpoints were met, with statistically significant differences between the treatment and placebo arms, Dr. Pergola reported.
Serum phosphate level was significantly reduced from baseline at week 16 (–0.21 mg/dL; 95% confidence interval, –0.39 to –0.03 mg/dL; P equal to .02) in the active treatment group, and the levels remained in the normal range, he said.
During the 16-week treatment period and subsequent 8-week, open-label safety extension period, ferric citrate was well tolerated. Treatment-emergent adverse events (AEs), most commonly diarrhea, occurred in 93 (79.5%) and 75 (64.7%) patients in the treatment and placebo arms, respectively. Serious AEs developed in 14 (12.0%) and 13 (11.2%) of patients in the same respective order. Two deaths occurred, both in the treatment group. The deaths and serious AEs were not considered drug related.
Ferric citrate binds with dietary phosphate in the gastrointestinal tract. The resulting ferric phosphate is insoluble and is excreted. The remaining unbound ferric citrate increases serum iron parameters, including ferritin and transferrin saturation.
The findings potentially extend the therapeutic reach of the drug beyond its Food and Drug Administration–approved use for control of phosphorus levels in CKD patients on dialysis, Dr. Pergola said. The trial data will be used to seek approval for the oral iron medication as a treatment for iron-deficiency anemia in adults with NDD-CKD.
The study was sponsored by Keryx Biopharmaceuticals. Dr. Pergola is supported by honoraria and lecture fees from Akebia Therapeutics, Keryx, Relypsa, Vifor/Fresenius Pharma, and ZS Pharma.
CHICAGO – Ferric citrate was safe and effective for treatment of iron-deficiency anemia in patients who had non–dialysis-dependent chronic kidney disease (NDD-CKD), based on data from a phase III, randomized, double-blind study.
The responses were durable, and none of the patients received erythropoiesis-stimulating agents (ESAs), presenter Pablo Pergola, MD, PhD, of Renal Associates, San Antonio, said in an interview at a meeting sponsored by the American Society of Nephrology.
The trial involved 234 anemic adults who had NDD-CKD and had not responded to oral iron supplements. The subjects were randomized to receive oral ferric citrate (n = 117) or placebo (n = 115) with meals (one patient did not receive placebo and laboratory data were lacking for one patient). The mean dose in the treatment arm was 5 pills per day.
The primary endpoint was the proportion of patients with hemoglobin (Hgb) greater than or equal to 1.0 g/dL anytime from baseline through week 16. Secondary endpoints included mean changes from baseline in Hgb, transferrin saturation, ferritin, and serum phosphate and evidence of sustained treatment effect based on target changes in Hgb with time.
Both arms were comparable at baseline for demographic and clinical characteristics, including phosphorus and hemoglobin levels and estimated glomerular filtration rate.
The primary endpoint was met by 51.2% of patients receiving ferric citrate and 19.1% of patients receiving placebo (P less than .001). All secondary efficacy endpoints were met, with statistically significant differences between the treatment and placebo arms, Dr. Pergola reported.
Serum phosphate level was significantly reduced from baseline at week 16 (–0.21 mg/dL; 95% confidence interval, –0.39 to –0.03 mg/dL; P equal to .02) in the active treatment group, and the levels remained in the normal range, he said.
During the 16-week treatment period and subsequent 8-week, open-label safety extension period, ferric citrate was well tolerated. Treatment-emergent adverse events (AEs), most commonly diarrhea, occurred in 93 (79.5%) and 75 (64.7%) patients in the treatment and placebo arms, respectively. Serious AEs developed in 14 (12.0%) and 13 (11.2%) of patients in the same respective order. Two deaths occurred, both in the treatment group. The deaths and serious AEs were not considered drug related.
Ferric citrate binds with dietary phosphate in the gastrointestinal tract. The resulting ferric phosphate is insoluble and is excreted. The remaining unbound ferric citrate increases serum iron parameters, including ferritin and transferrin saturation.
The findings potentially extend the therapeutic reach of the drug beyond its Food and Drug Administration–approved use for control of phosphorus levels in CKD patients on dialysis, Dr. Pergola said. The trial data will be used to seek approval for the oral iron medication as a treatment for iron-deficiency anemia in adults with NDD-CKD.
The study was sponsored by Keryx Biopharmaceuticals. Dr. Pergola is supported by honoraria and lecture fees from Akebia Therapeutics, Keryx, Relypsa, Vifor/Fresenius Pharma, and ZS Pharma.
CHICAGO – Ferric citrate was safe and effective for treatment of iron-deficiency anemia in patients who had non–dialysis-dependent chronic kidney disease (NDD-CKD), based on data from a phase III, randomized, double-blind study.
The responses were durable, and none of the patients received erythropoiesis-stimulating agents (ESAs), presenter Pablo Pergola, MD, PhD, of Renal Associates, San Antonio, said in an interview at a meeting sponsored by the American Society of Nephrology.
The trial involved 234 anemic adults who had NDD-CKD and had not responded to oral iron supplements. The subjects were randomized to receive oral ferric citrate (n = 117) or placebo (n = 115) with meals (one patient did not receive placebo and laboratory data were lacking for one patient). The mean dose in the treatment arm was 5 pills per day.
The primary endpoint was the proportion of patients with hemoglobin (Hgb) greater than or equal to 1.0 g/dL anytime from baseline through week 16. Secondary endpoints included mean changes from baseline in Hgb, transferrin saturation, ferritin, and serum phosphate and evidence of sustained treatment effect based on target changes in Hgb with time.
Both arms were comparable at baseline for demographic and clinical characteristics, including phosphorus and hemoglobin levels and estimated glomerular filtration rate.
The primary endpoint was met by 51.2% of patients receiving ferric citrate and 19.1% of patients receiving placebo (P less than .001). All secondary efficacy endpoints were met, with statistically significant differences between the treatment and placebo arms, Dr. Pergola reported.
Serum phosphate level was significantly reduced from baseline at week 16 (–0.21 mg/dL; 95% confidence interval, –0.39 to –0.03 mg/dL; P equal to .02) in the active treatment group, and the levels remained in the normal range, he said.
During the 16-week treatment period and subsequent 8-week, open-label safety extension period, ferric citrate was well tolerated. Treatment-emergent adverse events (AEs), most commonly diarrhea, occurred in 93 (79.5%) and 75 (64.7%) patients in the treatment and placebo arms, respectively. Serious AEs developed in 14 (12.0%) and 13 (11.2%) of patients in the same respective order. Two deaths occurred, both in the treatment group. The deaths and serious AEs were not considered drug related.
Ferric citrate binds with dietary phosphate in the gastrointestinal tract. The resulting ferric phosphate is insoluble and is excreted. The remaining unbound ferric citrate increases serum iron parameters, including ferritin and transferrin saturation.
The findings potentially extend the therapeutic reach of the drug beyond its Food and Drug Administration–approved use for control of phosphorus levels in CKD patients on dialysis, Dr. Pergola said. The trial data will be used to seek approval for the oral iron medication as a treatment for iron-deficiency anemia in adults with NDD-CKD.
The study was sponsored by Keryx Biopharmaceuticals. Dr. Pergola is supported by honoraria and lecture fees from Akebia Therapeutics, Keryx, Relypsa, Vifor/Fresenius Pharma, and ZS Pharma.
AT KIDNEY WEEK 2016
Key clinical point: Ferric citrate appears to be safe and effective for treating anemia in non–dialysis-dependent CKD patients.
Major finding: Prevalence of increased hemoglobin was 52.1% in patients receiving the active drug and 19.1% in those given placebo.
Data source: Randomized, double-blind, placebo-controlled, phase III trial with 234 patients.
Disclosures: The study was sponsored by Keryx Biopharmaceuticals. Dr. Pergola is supported by honoraria and lecture fees from Akebia Therapeutics, Keryx, Relypsa, Vifor/Fresenius Pharma, and ZS Pharma.
Smoking might affect response to ACE inhibitor in chronic kidney disease
CHICAGO – Smoking appears to be a modifiable risk factor for progression of chronic kidney disease associated with primary hypertension in patients treated with ACE inhibitors, Bethany Roehm, MD, reported at a meeting sponsored by the American Society of Nephrology.
Significantly increased albuminuria was noted in patients with chronic kidney disease who continued to smoke after initiating ACE inhibitor therapy, based on results from a 5-year follow-up study of 108 patients who smoked cigarettes at study entry – 25 of whom quit smoking within the first year of the study – and 108 patients who never smoked.
Further, smokers who were able to quit had improvements in measures of kidney function, said Dr. Roehm, of Tufts Medical Center, Boston, who presented the study findings.
It’s important that “we motivate our patients to stop smoking even though this can be challenging in the outpatient setting, she said. “More studies are needed to further investigate the relationship between the kidney protective effects of ACE inhibitors and the impact cigarette smoking may have on these effects.”
In addition to primary hypertension, study subjects had an estimated glomerular filtration ratio (eGFR) of 60 to 89 mL/min per 1.73 m2, and a urine albumin–to-creatinine ratio (UACR) greater than 200 mg/g. At baseline, the 108 smokers had at least a 1-year history of smoking more than a pack of cigarettes daily. They were matched with 108 people who had never smoked.
The smokers received smoking cessation information and guidance; 25 quit smoking. The nonsmokers, continued smokers, and quitters were comparable at baseline. The three groups were followed for 5 years after starting treatment with an ACE inhibitor, usually enalapril.
At 5 years, average eGFR was lower (P less than .01) in continued smokers (54.9 mL/min) than in nonsmokers (66.8 mL/min) and quitters (64.1 mL/min).
Baseline levels of urine (mcg)-to-creatinine (g) isoprostane 8-isoprostaglandin F2-alpha (8-iso/cr), an indicator of lipid peroxidation, were higher in smokers than in nonsmokers. In those who quit smoking, the level had declined at 1 year and remained at a level almost identical to that seen in the nonsmokers. One-year mean urine 8-iso/cr was higher in continued smokers (3.6) than in nonsmokers (1.6, P less than .01) and quitters (1.6, P less than .01).
Systolic blood pressure declined similarly in all three groups over the follow-up.
“The smokers had a faster decline in kidney function over time than the nonsmokers and the subjects who quit smoking ... [and] our continued smokers actually had an increase in albuminuria despite being placed on an ACE inhibitor,” Dr. Roehm said in an interview. Continued smoking appeared to interfere with the decrease in urinary protein excretion that typically accompanies ACE inhibitor therapy. “Higher urine 8-iso excretion, consistent with higher oxidative stress, was present in continued smokers, suggesting oxidative stress as a factor.”
The findings need to be confirmed in larger studies and in patients with CKD due to a wider variety of causes, Dr. Roehm said. Funding for the study was provided by pharmaceutical company support to Texas Tech University, Lubbock, and the Larry and Jane Woirhaye Memorial Endowment in Renal Research. Dr. Roehm reported having no financial disclosures.
CHICAGO – Smoking appears to be a modifiable risk factor for progression of chronic kidney disease associated with primary hypertension in patients treated with ACE inhibitors, Bethany Roehm, MD, reported at a meeting sponsored by the American Society of Nephrology.
Significantly increased albuminuria was noted in patients with chronic kidney disease who continued to smoke after initiating ACE inhibitor therapy, based on results from a 5-year follow-up study of 108 patients who smoked cigarettes at study entry – 25 of whom quit smoking within the first year of the study – and 108 patients who never smoked.
Further, smokers who were able to quit had improvements in measures of kidney function, said Dr. Roehm, of Tufts Medical Center, Boston, who presented the study findings.
It’s important that “we motivate our patients to stop smoking even though this can be challenging in the outpatient setting, she said. “More studies are needed to further investigate the relationship between the kidney protective effects of ACE inhibitors and the impact cigarette smoking may have on these effects.”
In addition to primary hypertension, study subjects had an estimated glomerular filtration ratio (eGFR) of 60 to 89 mL/min per 1.73 m2, and a urine albumin–to-creatinine ratio (UACR) greater than 200 mg/g. At baseline, the 108 smokers had at least a 1-year history of smoking more than a pack of cigarettes daily. They were matched with 108 people who had never smoked.
The smokers received smoking cessation information and guidance; 25 quit smoking. The nonsmokers, continued smokers, and quitters were comparable at baseline. The three groups were followed for 5 years after starting treatment with an ACE inhibitor, usually enalapril.
At 5 years, average eGFR was lower (P less than .01) in continued smokers (54.9 mL/min) than in nonsmokers (66.8 mL/min) and quitters (64.1 mL/min).
Baseline levels of urine (mcg)-to-creatinine (g) isoprostane 8-isoprostaglandin F2-alpha (8-iso/cr), an indicator of lipid peroxidation, were higher in smokers than in nonsmokers. In those who quit smoking, the level had declined at 1 year and remained at a level almost identical to that seen in the nonsmokers. One-year mean urine 8-iso/cr was higher in continued smokers (3.6) than in nonsmokers (1.6, P less than .01) and quitters (1.6, P less than .01).
Systolic blood pressure declined similarly in all three groups over the follow-up.
“The smokers had a faster decline in kidney function over time than the nonsmokers and the subjects who quit smoking ... [and] our continued smokers actually had an increase in albuminuria despite being placed on an ACE inhibitor,” Dr. Roehm said in an interview. Continued smoking appeared to interfere with the decrease in urinary protein excretion that typically accompanies ACE inhibitor therapy. “Higher urine 8-iso excretion, consistent with higher oxidative stress, was present in continued smokers, suggesting oxidative stress as a factor.”
The findings need to be confirmed in larger studies and in patients with CKD due to a wider variety of causes, Dr. Roehm said. Funding for the study was provided by pharmaceutical company support to Texas Tech University, Lubbock, and the Larry and Jane Woirhaye Memorial Endowment in Renal Research. Dr. Roehm reported having no financial disclosures.
CHICAGO – Smoking appears to be a modifiable risk factor for progression of chronic kidney disease associated with primary hypertension in patients treated with ACE inhibitors, Bethany Roehm, MD, reported at a meeting sponsored by the American Society of Nephrology.
Significantly increased albuminuria was noted in patients with chronic kidney disease who continued to smoke after initiating ACE inhibitor therapy, based on results from a 5-year follow-up study of 108 patients who smoked cigarettes at study entry – 25 of whom quit smoking within the first year of the study – and 108 patients who never smoked.
Further, smokers who were able to quit had improvements in measures of kidney function, said Dr. Roehm, of Tufts Medical Center, Boston, who presented the study findings.
It’s important that “we motivate our patients to stop smoking even though this can be challenging in the outpatient setting, she said. “More studies are needed to further investigate the relationship between the kidney protective effects of ACE inhibitors and the impact cigarette smoking may have on these effects.”
In addition to primary hypertension, study subjects had an estimated glomerular filtration ratio (eGFR) of 60 to 89 mL/min per 1.73 m2, and a urine albumin–to-creatinine ratio (UACR) greater than 200 mg/g. At baseline, the 108 smokers had at least a 1-year history of smoking more than a pack of cigarettes daily. They were matched with 108 people who had never smoked.
The smokers received smoking cessation information and guidance; 25 quit smoking. The nonsmokers, continued smokers, and quitters were comparable at baseline. The three groups were followed for 5 years after starting treatment with an ACE inhibitor, usually enalapril.
At 5 years, average eGFR was lower (P less than .01) in continued smokers (54.9 mL/min) than in nonsmokers (66.8 mL/min) and quitters (64.1 mL/min).
Baseline levels of urine (mcg)-to-creatinine (g) isoprostane 8-isoprostaglandin F2-alpha (8-iso/cr), an indicator of lipid peroxidation, were higher in smokers than in nonsmokers. In those who quit smoking, the level had declined at 1 year and remained at a level almost identical to that seen in the nonsmokers. One-year mean urine 8-iso/cr was higher in continued smokers (3.6) than in nonsmokers (1.6, P less than .01) and quitters (1.6, P less than .01).
Systolic blood pressure declined similarly in all three groups over the follow-up.
“The smokers had a faster decline in kidney function over time than the nonsmokers and the subjects who quit smoking ... [and] our continued smokers actually had an increase in albuminuria despite being placed on an ACE inhibitor,” Dr. Roehm said in an interview. Continued smoking appeared to interfere with the decrease in urinary protein excretion that typically accompanies ACE inhibitor therapy. “Higher urine 8-iso excretion, consistent with higher oxidative stress, was present in continued smokers, suggesting oxidative stress as a factor.”
The findings need to be confirmed in larger studies and in patients with CKD due to a wider variety of causes, Dr. Roehm said. Funding for the study was provided by pharmaceutical company support to Texas Tech University, Lubbock, and the Larry and Jane Woirhaye Memorial Endowment in Renal Research. Dr. Roehm reported having no financial disclosures.
AT KIDNEY WEEK 2016
Key clinical point: Smoking cessation could improve therapeutic response in patients who have chronic kidney disease and are treated with ACE inhibitors.
Major finding: At 5 years, eGFR was lower (P less than .01) in continued smokers (54.9 mL/min) than in nonsmokers (66.8 mL/min) and quitters (64.1 mL/min).
Data source: Prospective case-control study involving 216 subjects.
Disclosures: Funding for the study was provided by pharmaceutical company support to Texas Tech University, Lubbock, and the Larry and Jane Woirhaye Memorial Endowment in Renal Research. Dr. Roehm reported having no financial disclosures.
Tinzaparin is a safe, effective anticoagulant in patients on dialysis
CHICAGO – Tinzaparin was safe and effective as an anticoagulant for hemodialysis patients based on results from the Intermittent Hemodialysis Anticoagulation with Tinzaparin (HEMO-TIN) trial presented at the annual meeting sponsored by the American Society for Nephrology.
In the multicenter randomized controlled trial of 192 adults on hemodialysis, tinzaparin, a low molecular weight heparin with antithrombotic properties, was compared with unfractionated heparin. Tinzaparin has been considered for hemodialysis patients because it is thought to be less dependent on renal clearance than are other low molecular weight heparins, Christine Ribic, MD, MSc, of McMaster University, Hamilton, Ont., said in reporting the results.
After 3 months, the 78 patients remaining in the tinzaparin group crossed over to receive unfractionated heparin for 3 months. The 79 patients remaining in the unfractionated heparin group crossed over to receive tinzaparin for 3 months. Of these 156 patients, 125 completed the 3-month crossover phase.
There were 421 bleeding events in the 12,125 hemodialysis sessions studied. They were evenly distributed in the groups, with 212 (50.4%) in those receiving unfractionated heparin and 209 (49.6%) in those receiving tinzaparin. The prevalence of major bleeds (2.1 vs 1.6%), clinically important nonmajor bleeds (1.2% vs 0.2%), and minor bleeds (47.0% vs 47.7%) was also similar between the unfractionated heparin and tinzaparin groups.
Anti-Xa heparin levels were used as a surrogate measure of low molecular weight heparin activity levels and bleeding risk due to bioaccumulation. In tinzaparin-treated patients, anti-Xa heparin levels never exceeded a value of 0.2 either before or after dialysis. This value was considered the threshold between safety and increased risk for bleeding. This threshold level was routinely exceeded pre- and post-dialysis in patients receiving unfractionated heparin at baseline and both before and after crossover.
Grade 4 clotting was similar for tinzaparin and unfractionated heparin, occurring in 23 of 6,095 (0.4%) unfractionated heparin hemodialysis sessions and 41 of 6030 (0.7%) tinzaparin hemodialysis sessions. Mean dialyzer clotting scores and mean air trap clotting scores were also comparable.
The trial was supported by Leo Pharma, the maker of tinzaparin (innohep), in collaboration with McMaster University. Dr. Ribic is the sponsor of the trial.
CHICAGO – Tinzaparin was safe and effective as an anticoagulant for hemodialysis patients based on results from the Intermittent Hemodialysis Anticoagulation with Tinzaparin (HEMO-TIN) trial presented at the annual meeting sponsored by the American Society for Nephrology.
In the multicenter randomized controlled trial of 192 adults on hemodialysis, tinzaparin, a low molecular weight heparin with antithrombotic properties, was compared with unfractionated heparin. Tinzaparin has been considered for hemodialysis patients because it is thought to be less dependent on renal clearance than are other low molecular weight heparins, Christine Ribic, MD, MSc, of McMaster University, Hamilton, Ont., said in reporting the results.
After 3 months, the 78 patients remaining in the tinzaparin group crossed over to receive unfractionated heparin for 3 months. The 79 patients remaining in the unfractionated heparin group crossed over to receive tinzaparin for 3 months. Of these 156 patients, 125 completed the 3-month crossover phase.
There were 421 bleeding events in the 12,125 hemodialysis sessions studied. They were evenly distributed in the groups, with 212 (50.4%) in those receiving unfractionated heparin and 209 (49.6%) in those receiving tinzaparin. The prevalence of major bleeds (2.1 vs 1.6%), clinically important nonmajor bleeds (1.2% vs 0.2%), and minor bleeds (47.0% vs 47.7%) was also similar between the unfractionated heparin and tinzaparin groups.
Anti-Xa heparin levels were used as a surrogate measure of low molecular weight heparin activity levels and bleeding risk due to bioaccumulation. In tinzaparin-treated patients, anti-Xa heparin levels never exceeded a value of 0.2 either before or after dialysis. This value was considered the threshold between safety and increased risk for bleeding. This threshold level was routinely exceeded pre- and post-dialysis in patients receiving unfractionated heparin at baseline and both before and after crossover.
Grade 4 clotting was similar for tinzaparin and unfractionated heparin, occurring in 23 of 6,095 (0.4%) unfractionated heparin hemodialysis sessions and 41 of 6030 (0.7%) tinzaparin hemodialysis sessions. Mean dialyzer clotting scores and mean air trap clotting scores were also comparable.
The trial was supported by Leo Pharma, the maker of tinzaparin (innohep), in collaboration with McMaster University. Dr. Ribic is the sponsor of the trial.
CHICAGO – Tinzaparin was safe and effective as an anticoagulant for hemodialysis patients based on results from the Intermittent Hemodialysis Anticoagulation with Tinzaparin (HEMO-TIN) trial presented at the annual meeting sponsored by the American Society for Nephrology.
In the multicenter randomized controlled trial of 192 adults on hemodialysis, tinzaparin, a low molecular weight heparin with antithrombotic properties, was compared with unfractionated heparin. Tinzaparin has been considered for hemodialysis patients because it is thought to be less dependent on renal clearance than are other low molecular weight heparins, Christine Ribic, MD, MSc, of McMaster University, Hamilton, Ont., said in reporting the results.
After 3 months, the 78 patients remaining in the tinzaparin group crossed over to receive unfractionated heparin for 3 months. The 79 patients remaining in the unfractionated heparin group crossed over to receive tinzaparin for 3 months. Of these 156 patients, 125 completed the 3-month crossover phase.
There were 421 bleeding events in the 12,125 hemodialysis sessions studied. They were evenly distributed in the groups, with 212 (50.4%) in those receiving unfractionated heparin and 209 (49.6%) in those receiving tinzaparin. The prevalence of major bleeds (2.1 vs 1.6%), clinically important nonmajor bleeds (1.2% vs 0.2%), and minor bleeds (47.0% vs 47.7%) was also similar between the unfractionated heparin and tinzaparin groups.
Anti-Xa heparin levels were used as a surrogate measure of low molecular weight heparin activity levels and bleeding risk due to bioaccumulation. In tinzaparin-treated patients, anti-Xa heparin levels never exceeded a value of 0.2 either before or after dialysis. This value was considered the threshold between safety and increased risk for bleeding. This threshold level was routinely exceeded pre- and post-dialysis in patients receiving unfractionated heparin at baseline and both before and after crossover.
Grade 4 clotting was similar for tinzaparin and unfractionated heparin, occurring in 23 of 6,095 (0.4%) unfractionated heparin hemodialysis sessions and 41 of 6030 (0.7%) tinzaparin hemodialysis sessions. Mean dialyzer clotting scores and mean air trap clotting scores were also comparable.
The trial was supported by Leo Pharma, the maker of tinzaparin (innohep), in collaboration with McMaster University. Dr. Ribic is the sponsor of the trial.
AT KIDNEY WEEK 2016
Key clinical point: Tinzaparin outcomes compare to those with low molecular weight heparin, and tinzaparin may be safer because it is less dependent on renal clearance than are low molecular weight heparins.
Major finding: Mean anti-Xa levels post-hemodialysis did not exceed 0.2 for tinzaparin, indicating no residual anticoagulant effect.
Data source: Randomized, double-dummy, blinded crossover controlled trial involving 192 patients.
Disclosures: Study sponsor was McMaster University, Hamilton, Ont. The study was funded by Leo Pharma. Dr. Ribic reported having no financial disclosures.
Liraglutide lessens risk of kidney disease progression in type 2 diabetes
CHICAGO – Liraglutide reduced the risk of kidney disease progression in patients with type 2 diabetes, a study showed.
The latest results from the LEADER (Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results) trial build on the previously reported success of liraglutide in reducing the risk of adverse cardiovascular events in people with type 2 diabetes.
“We now have drugs that not only lower blood sugar but also have an impact on new development of diabetic kidney disease and cardiovascular disease,” said Johannes Mann, MD, of the University of Erlangen-Nürnberg, Erlangen, Germany, in a plenary presentation at the meeting sponsored by the American Society of Nephrology.
The LEADER trial involved people with type 2 diabetes mellitus (mean duration, about 13 years) with a baseline hemoglobin A1c level greater than or equal to 7%. Some had never taken antidiabetic drugs, and some were taking oral antidiabetic drugs and/or basal/premixed insulin. They were either 50 years of age or older with established cardiovascular disease and chronic kidney disease, or 60 years and older with risk factors for cardiovascular disease.
Exclusion criteria included type 1 diabetes; a history of medication with glucagonlike peptide–1 receptor agonists, dipeptidyl peptidase–4 inhibitors, pramlintide, or rapid-acting insulin; and a family/personal history of multiple endocrine neoplasia type 2 or medullary thyroid cancer.
The 9,340 subjects were randomized in a double-blind fashion to daily subcutaneous injection with 0.6-1.8 mg of liraglutide (4,668) or placebo (4,672) for at least 3.5 years to a maximum treatment time of 5 years. The mean follow-up was 3.8 years.
At baseline, microalbuminuria had been diagnosed in 26.4% and 26.6% of those randomized to liraglutide or placebo, respectively. The respective baseline rates of macroalbuminuria were 10% and 11%. An estimated glomerular filtration rate (eGFR) less than 60 mL/min per 1.73 m2 was present in 23.9% of the liraglutide group and 22.3% of the control group.
In this analysis of the LEADER results, the primary renal outcome was a composite of the development of macroalbuminuria, doubling of serum creatinine, end-stage renal disease, or renal death. Liraglutide was superior to placebo in delaying the time to the primary outcome (hazard ratio, 0.78; 95% confidence interval, 0.67-0.92; P equal to .003). The outcome was driven by the reduction in development of macroalbuminuria (HR, 0.74; 95% CI, 0.60-0.91; P = .004), with treatment not being significantly effective for doubling of serum creatinine (HR, 0.89; 95% CI, 0.67-1.19) or the need for dialysis (HR, 0.87; 95% CI, 0.61-1.24).
The eGFR declined less in the liraglutide arm. The renal protection of the drug was restricted to subjects with a baseline eGFR of 30-59 mL/min per 1.73 m2. Liragutide was not associated with an increased risk of adverse renal events.
The latest results extend the potential indications of the therapeutic prowess of liraglutide in type 2 diabetes patients with chronic kidney disease, with the caveat that the significance of the primary outcome was due to macroalbuminuria rather than the arguably more important outcomes of doubling of serum creatinine and development of end-stage renal disease.
The trial was sponsored and funded by Novo Nordisk, the maker of liraglutide (Victoza) and the National Institutes of Health. Dr. Mann disclosed financial relationships with various drug companies, including Novo Nordisk.
CHICAGO – Liraglutide reduced the risk of kidney disease progression in patients with type 2 diabetes, a study showed.
The latest results from the LEADER (Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results) trial build on the previously reported success of liraglutide in reducing the risk of adverse cardiovascular events in people with type 2 diabetes.
“We now have drugs that not only lower blood sugar but also have an impact on new development of diabetic kidney disease and cardiovascular disease,” said Johannes Mann, MD, of the University of Erlangen-Nürnberg, Erlangen, Germany, in a plenary presentation at the meeting sponsored by the American Society of Nephrology.
The LEADER trial involved people with type 2 diabetes mellitus (mean duration, about 13 years) with a baseline hemoglobin A1c level greater than or equal to 7%. Some had never taken antidiabetic drugs, and some were taking oral antidiabetic drugs and/or basal/premixed insulin. They were either 50 years of age or older with established cardiovascular disease and chronic kidney disease, or 60 years and older with risk factors for cardiovascular disease.
Exclusion criteria included type 1 diabetes; a history of medication with glucagonlike peptide–1 receptor agonists, dipeptidyl peptidase–4 inhibitors, pramlintide, or rapid-acting insulin; and a family/personal history of multiple endocrine neoplasia type 2 or medullary thyroid cancer.
The 9,340 subjects were randomized in a double-blind fashion to daily subcutaneous injection with 0.6-1.8 mg of liraglutide (4,668) or placebo (4,672) for at least 3.5 years to a maximum treatment time of 5 years. The mean follow-up was 3.8 years.
At baseline, microalbuminuria had been diagnosed in 26.4% and 26.6% of those randomized to liraglutide or placebo, respectively. The respective baseline rates of macroalbuminuria were 10% and 11%. An estimated glomerular filtration rate (eGFR) less than 60 mL/min per 1.73 m2 was present in 23.9% of the liraglutide group and 22.3% of the control group.
In this analysis of the LEADER results, the primary renal outcome was a composite of the development of macroalbuminuria, doubling of serum creatinine, end-stage renal disease, or renal death. Liraglutide was superior to placebo in delaying the time to the primary outcome (hazard ratio, 0.78; 95% confidence interval, 0.67-0.92; P equal to .003). The outcome was driven by the reduction in development of macroalbuminuria (HR, 0.74; 95% CI, 0.60-0.91; P = .004), with treatment not being significantly effective for doubling of serum creatinine (HR, 0.89; 95% CI, 0.67-1.19) or the need for dialysis (HR, 0.87; 95% CI, 0.61-1.24).
The eGFR declined less in the liraglutide arm. The renal protection of the drug was restricted to subjects with a baseline eGFR of 30-59 mL/min per 1.73 m2. Liragutide was not associated with an increased risk of adverse renal events.
The latest results extend the potential indications of the therapeutic prowess of liraglutide in type 2 diabetes patients with chronic kidney disease, with the caveat that the significance of the primary outcome was due to macroalbuminuria rather than the arguably more important outcomes of doubling of serum creatinine and development of end-stage renal disease.
The trial was sponsored and funded by Novo Nordisk, the maker of liraglutide (Victoza) and the National Institutes of Health. Dr. Mann disclosed financial relationships with various drug companies, including Novo Nordisk.
CHICAGO – Liraglutide reduced the risk of kidney disease progression in patients with type 2 diabetes, a study showed.
The latest results from the LEADER (Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results) trial build on the previously reported success of liraglutide in reducing the risk of adverse cardiovascular events in people with type 2 diabetes.
“We now have drugs that not only lower blood sugar but also have an impact on new development of diabetic kidney disease and cardiovascular disease,” said Johannes Mann, MD, of the University of Erlangen-Nürnberg, Erlangen, Germany, in a plenary presentation at the meeting sponsored by the American Society of Nephrology.
The LEADER trial involved people with type 2 diabetes mellitus (mean duration, about 13 years) with a baseline hemoglobin A1c level greater than or equal to 7%. Some had never taken antidiabetic drugs, and some were taking oral antidiabetic drugs and/or basal/premixed insulin. They were either 50 years of age or older with established cardiovascular disease and chronic kidney disease, or 60 years and older with risk factors for cardiovascular disease.
Exclusion criteria included type 1 diabetes; a history of medication with glucagonlike peptide–1 receptor agonists, dipeptidyl peptidase–4 inhibitors, pramlintide, or rapid-acting insulin; and a family/personal history of multiple endocrine neoplasia type 2 or medullary thyroid cancer.
The 9,340 subjects were randomized in a double-blind fashion to daily subcutaneous injection with 0.6-1.8 mg of liraglutide (4,668) or placebo (4,672) for at least 3.5 years to a maximum treatment time of 5 years. The mean follow-up was 3.8 years.
At baseline, microalbuminuria had been diagnosed in 26.4% and 26.6% of those randomized to liraglutide or placebo, respectively. The respective baseline rates of macroalbuminuria were 10% and 11%. An estimated glomerular filtration rate (eGFR) less than 60 mL/min per 1.73 m2 was present in 23.9% of the liraglutide group and 22.3% of the control group.
In this analysis of the LEADER results, the primary renal outcome was a composite of the development of macroalbuminuria, doubling of serum creatinine, end-stage renal disease, or renal death. Liraglutide was superior to placebo in delaying the time to the primary outcome (hazard ratio, 0.78; 95% confidence interval, 0.67-0.92; P equal to .003). The outcome was driven by the reduction in development of macroalbuminuria (HR, 0.74; 95% CI, 0.60-0.91; P = .004), with treatment not being significantly effective for doubling of serum creatinine (HR, 0.89; 95% CI, 0.67-1.19) or the need for dialysis (HR, 0.87; 95% CI, 0.61-1.24).
The eGFR declined less in the liraglutide arm. The renal protection of the drug was restricted to subjects with a baseline eGFR of 30-59 mL/min per 1.73 m2. Liragutide was not associated with an increased risk of adverse renal events.
The latest results extend the potential indications of the therapeutic prowess of liraglutide in type 2 diabetes patients with chronic kidney disease, with the caveat that the significance of the primary outcome was due to macroalbuminuria rather than the arguably more important outcomes of doubling of serum creatinine and development of end-stage renal disease.
The trial was sponsored and funded by Novo Nordisk, the maker of liraglutide (Victoza) and the National Institutes of Health. Dr. Mann disclosed financial relationships with various drug companies, including Novo Nordisk.
AT KIDNEY WEEK 2016
Key clinical point:
Major finding: Liraglutide significantly lessened all-cause death, compared with placebo.
Data source: LEADER, a multicenter, randomized, double-blind placebo-controlled trial involving 9,340 patients.
Disclosures: The trial was sponsored and funded by Novo Nordisk, the maker of liraglutide (Victoza) and the National Institutes of Health. Dr. Mann disclosed financial relationships with various drug companies, including Novo Nordisk.
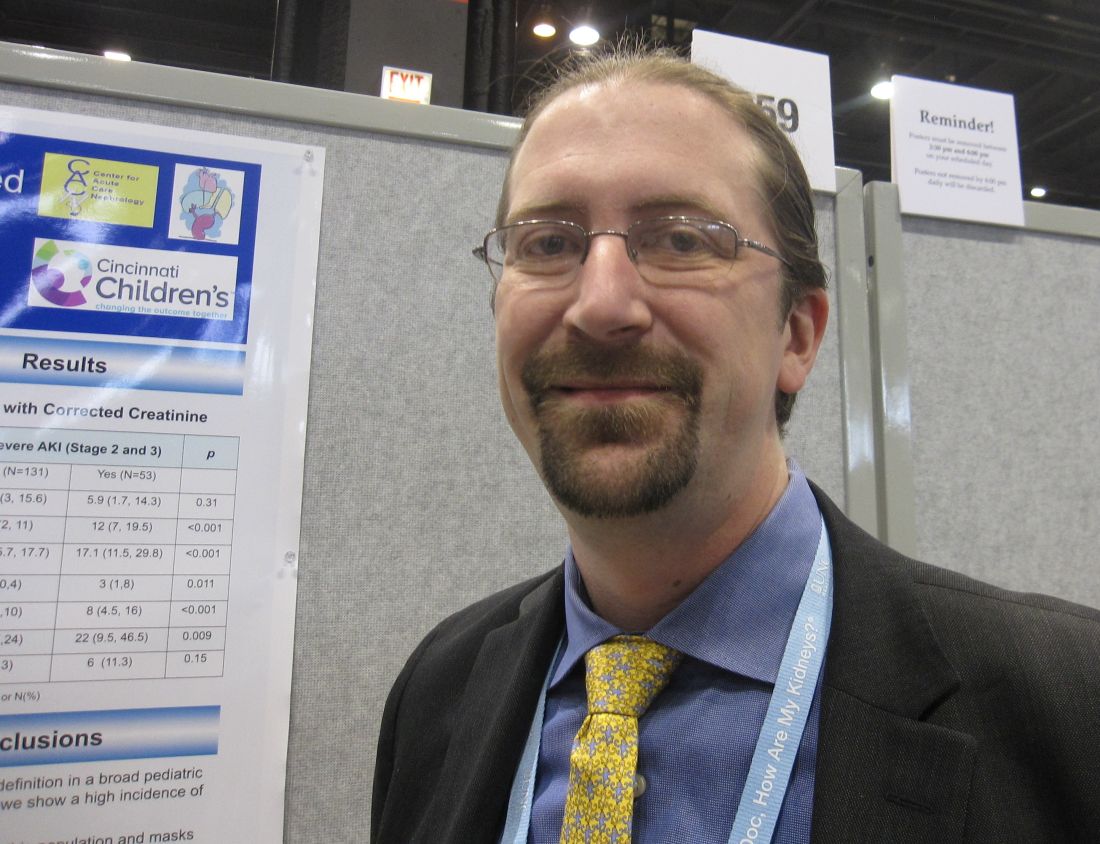
Adjustment for fluid balance improved detection of AKI in critically ill children
CHICAGO – Adjustment for fluid balance increased the detection rate of acute kidney injury, more accurately staged the kidney damage, and distinguished false-positive cases in critically ill children, based on a secondary analysis of the Study of the Prediction of Acute Kidney Injury in Children Using Risk Stratification and Biomarkers (AKI-CHERUB).
Fluid overload can mask acute kidney injury (AKI) in critically ill children. “The failure to correct serum creatinine measure for fluid overload dilutes the impact of AKI on outcomes,” David T. Selewski, MD, of the University of Michigan, Ann Arbor, said at the annual meeting sponsored by the American Society for Nephrology.
The primary outcome was ICU mortality. Secondary outcomes were length of mechanical ventilation, and length of stay in the ICU and the hospital.
The original study documented an ICU mortality rate of 7.1%. AKI was identified in 77 (41.8%) of the 184 patients. The median peak fluid overload during ICU admission was 12.9 (interquartile range, 7.4-20.8).
The serum creatinine data were corrected for fluid balance and these rates were reassessed. Following the adjustment, the rate of AKI increased from 41.8% to 53.4%, with 30 new cases identified according to standard defined criteria. The mean fluid overload was now 11.2 (interquartile range, 5.7-17.7).
In the original cohort, there were 40 cases of severe AKI (stage 2 and 3). Following the creatinine correction, 13 more cases were judged to be severe. Of these, five cases were associated with a worse outcome in terms of ICU mortality. Additionally, 10 cases that had been diagnosed as AKI were found to be false positives.
The results need to be studied in larger studies and in other populations, such as neonates, Dr. Selewski said.
CHICAGO – Adjustment for fluid balance increased the detection rate of acute kidney injury, more accurately staged the kidney damage, and distinguished false-positive cases in critically ill children, based on a secondary analysis of the Study of the Prediction of Acute Kidney Injury in Children Using Risk Stratification and Biomarkers (AKI-CHERUB).
Fluid overload can mask acute kidney injury (AKI) in critically ill children. “The failure to correct serum creatinine measure for fluid overload dilutes the impact of AKI on outcomes,” David T. Selewski, MD, of the University of Michigan, Ann Arbor, said at the annual meeting sponsored by the American Society for Nephrology.
The primary outcome was ICU mortality. Secondary outcomes were length of mechanical ventilation, and length of stay in the ICU and the hospital.
The original study documented an ICU mortality rate of 7.1%. AKI was identified in 77 (41.8%) of the 184 patients. The median peak fluid overload during ICU admission was 12.9 (interquartile range, 7.4-20.8).
The serum creatinine data were corrected for fluid balance and these rates were reassessed. Following the adjustment, the rate of AKI increased from 41.8% to 53.4%, with 30 new cases identified according to standard defined criteria. The mean fluid overload was now 11.2 (interquartile range, 5.7-17.7).
In the original cohort, there were 40 cases of severe AKI (stage 2 and 3). Following the creatinine correction, 13 more cases were judged to be severe. Of these, five cases were associated with a worse outcome in terms of ICU mortality. Additionally, 10 cases that had been diagnosed as AKI were found to be false positives.
The results need to be studied in larger studies and in other populations, such as neonates, Dr. Selewski said.
CHICAGO – Adjustment for fluid balance increased the detection rate of acute kidney injury, more accurately staged the kidney damage, and distinguished false-positive cases in critically ill children, based on a secondary analysis of the Study of the Prediction of Acute Kidney Injury in Children Using Risk Stratification and Biomarkers (AKI-CHERUB).
Fluid overload can mask acute kidney injury (AKI) in critically ill children. “The failure to correct serum creatinine measure for fluid overload dilutes the impact of AKI on outcomes,” David T. Selewski, MD, of the University of Michigan, Ann Arbor, said at the annual meeting sponsored by the American Society for Nephrology.
The primary outcome was ICU mortality. Secondary outcomes were length of mechanical ventilation, and length of stay in the ICU and the hospital.
The original study documented an ICU mortality rate of 7.1%. AKI was identified in 77 (41.8%) of the 184 patients. The median peak fluid overload during ICU admission was 12.9 (interquartile range, 7.4-20.8).
The serum creatinine data were corrected for fluid balance and these rates were reassessed. Following the adjustment, the rate of AKI increased from 41.8% to 53.4%, with 30 new cases identified according to standard defined criteria. The mean fluid overload was now 11.2 (interquartile range, 5.7-17.7).
In the original cohort, there were 40 cases of severe AKI (stage 2 and 3). Following the creatinine correction, 13 more cases were judged to be severe. Of these, five cases were associated with a worse outcome in terms of ICU mortality. Additionally, 10 cases that had been diagnosed as AKI were found to be false positives.
The results need to be studied in larger studies and in other populations, such as neonates, Dr. Selewski said.
AT KIDNEY WEEK 2016
Key clinical point: Acute kidney injury can be detected more accurately in critically ill children by correcting for fluid overload.
Major finding: Fluid overload masked diagnosis of over 40% of patients with acute kidney injury in an observational study.
Data source: Secondary analysis of AKI-CHERUB single-center observational study involving 181 critically ill children.
Disclosures: The AKI-CHERUB study was funded by NIH. Dr. Selewski reported having no financial disclosures.
Blood pressure changes and persistent hypertension elevate dementia risk
BALTIMORE – The impact of blood pressure on the risk of dementia in late life follows a U-shaped curve in which elevated mid-life and late-life blood pressure, as well as late-life decline in blood pressure, all independently raise the risk of dementia, according to findings from a longitudinal study of the Framingham Offspring cohort of the Framingham Heart Study.
The findings highlight the benefits of establishing and maintaining lower blood pressure in midlife in preventing or lowering the risk of dementia, Emer McGrath, MD, said at the annual meeting of the American Neurological Association.
The researchers explored the issue using data from the Framingham Offspring cohort of the Framingham Heart Study. The cohort comprises 5,124 children, and spouses of children, of the original Framingham cohort. They have been examined clinically at regular intervals since 1971. The present study focused on 1,440 individuals who had five consecutive examinations during a 15-year period anytime between 1983 and 2001 and who had not been diagnosed with dementia at the time of the final blood pressure determination.
The 1,440 participants had a mean age of 69 years at their fifth examination. Just over half were female, 20% had been diagnosed with cardiovascular disease, and slightly less than 20% had been diagnosed with diabetes. Half were using antihypertensive medications.
During a mean 8-year follow-up period, 107 individuals developed dementia. Dementia was independently associated with midlife hypertension (140/90 mm Hg or higher), with a stronger association for systolic hypertension (hazard ratio, 1.57; 95% confidence interval, 1.05-2.35). Persistence of hypertension into late life, particularly systolic hypertension (HR, 1.96; 95% CI, 1.25-3.09), was another independent risk factor for dementia.
Among individuals who did not have hypertension at midlife, a decline in systolic blood pressure to less than 100/70 mm Hg in the ensuing years increased the risk of dementia (HR, 1.63; 95% CI, 1.08-2.46).
According to the researchers, the findings support the hypothesis of the U-shaped relationship between blood pressure and dementia. “Our data also highlight the potential sustained cognitive benefits of lower midlife blood pressure,” Dr. McGrath said.
The study was funded by the Framingham Heart Study, the National Institute on Aging, and the National Institute for Neurological Diseases and Stroke. Dr. McGrath had no disclosures.
BALTIMORE – The impact of blood pressure on the risk of dementia in late life follows a U-shaped curve in which elevated mid-life and late-life blood pressure, as well as late-life decline in blood pressure, all independently raise the risk of dementia, according to findings from a longitudinal study of the Framingham Offspring cohort of the Framingham Heart Study.
The findings highlight the benefits of establishing and maintaining lower blood pressure in midlife in preventing or lowering the risk of dementia, Emer McGrath, MD, said at the annual meeting of the American Neurological Association.
The researchers explored the issue using data from the Framingham Offspring cohort of the Framingham Heart Study. The cohort comprises 5,124 children, and spouses of children, of the original Framingham cohort. They have been examined clinically at regular intervals since 1971. The present study focused on 1,440 individuals who had five consecutive examinations during a 15-year period anytime between 1983 and 2001 and who had not been diagnosed with dementia at the time of the final blood pressure determination.
The 1,440 participants had a mean age of 69 years at their fifth examination. Just over half were female, 20% had been diagnosed with cardiovascular disease, and slightly less than 20% had been diagnosed with diabetes. Half were using antihypertensive medications.
During a mean 8-year follow-up period, 107 individuals developed dementia. Dementia was independently associated with midlife hypertension (140/90 mm Hg or higher), with a stronger association for systolic hypertension (hazard ratio, 1.57; 95% confidence interval, 1.05-2.35). Persistence of hypertension into late life, particularly systolic hypertension (HR, 1.96; 95% CI, 1.25-3.09), was another independent risk factor for dementia.
Among individuals who did not have hypertension at midlife, a decline in systolic blood pressure to less than 100/70 mm Hg in the ensuing years increased the risk of dementia (HR, 1.63; 95% CI, 1.08-2.46).
According to the researchers, the findings support the hypothesis of the U-shaped relationship between blood pressure and dementia. “Our data also highlight the potential sustained cognitive benefits of lower midlife blood pressure,” Dr. McGrath said.
The study was funded by the Framingham Heart Study, the National Institute on Aging, and the National Institute for Neurological Diseases and Stroke. Dr. McGrath had no disclosures.
BALTIMORE – The impact of blood pressure on the risk of dementia in late life follows a U-shaped curve in which elevated mid-life and late-life blood pressure, as well as late-life decline in blood pressure, all independently raise the risk of dementia, according to findings from a longitudinal study of the Framingham Offspring cohort of the Framingham Heart Study.
The findings highlight the benefits of establishing and maintaining lower blood pressure in midlife in preventing or lowering the risk of dementia, Emer McGrath, MD, said at the annual meeting of the American Neurological Association.
The researchers explored the issue using data from the Framingham Offspring cohort of the Framingham Heart Study. The cohort comprises 5,124 children, and spouses of children, of the original Framingham cohort. They have been examined clinically at regular intervals since 1971. The present study focused on 1,440 individuals who had five consecutive examinations during a 15-year period anytime between 1983 and 2001 and who had not been diagnosed with dementia at the time of the final blood pressure determination.
The 1,440 participants had a mean age of 69 years at their fifth examination. Just over half were female, 20% had been diagnosed with cardiovascular disease, and slightly less than 20% had been diagnosed with diabetes. Half were using antihypertensive medications.
During a mean 8-year follow-up period, 107 individuals developed dementia. Dementia was independently associated with midlife hypertension (140/90 mm Hg or higher), with a stronger association for systolic hypertension (hazard ratio, 1.57; 95% confidence interval, 1.05-2.35). Persistence of hypertension into late life, particularly systolic hypertension (HR, 1.96; 95% CI, 1.25-3.09), was another independent risk factor for dementia.
Among individuals who did not have hypertension at midlife, a decline in systolic blood pressure to less than 100/70 mm Hg in the ensuing years increased the risk of dementia (HR, 1.63; 95% CI, 1.08-2.46).
According to the researchers, the findings support the hypothesis of the U-shaped relationship between blood pressure and dementia. “Our data also highlight the potential sustained cognitive benefits of lower midlife blood pressure,” Dr. McGrath said.
The study was funded by the Framingham Heart Study, the National Institute on Aging, and the National Institute for Neurological Diseases and Stroke. Dr. McGrath had no disclosures.
AT ANA 2016
Key clinical point:
Major finding: Persistence of hypertension into late life, particularly systolic hypertension (HR, 1.96; 95% CI, 1.25-3.09), was another independent risk factor for dementia.
Data source: Offspring cohort of the Framingham Heart Study.
Disclosures: The study was funded by the Framingham Heart Study, the National Institute on Aging, and the National Institute for Neurological Diseases and Stroke. Dr. McGrath had no disclosures.
Deep brain stimulation for early Parkinson’s disease has long-term benefit
BALTIMORE – The use of subthalamic nucleus deep brain stimulation (DBS) along with optimal drug therapy in patients with early stage Parkinson’s disease produced clinically meaningful improvements in clinician-assessed motor control that lasted at least 5 years in a prospective pilot study.
If the findings bear out a phase III trial that has been approved, DBS may become a valuable method to achieve long-term improvement in motor skills in patients with Parkinson’s disease.
The pilot trial involved 30 patients with Parkinson’s disease, aged 50-75 years, and demonstrated the safety and benefit of DBS in conjunction with optimal drug therapy (ODT) – involving drugs such as carbidopa/levodopa, pramipexole, ropinirole, and selegiline – compared with ODT alone in improving motor scores of the patients through 2 years (Parkinsonism Relat Disord. 2014. 20[7]:731-7). The latest subanalysis of the trial data took a longer look, examining the effect of DBS through 5 years.
The subanalysis involved 28 patients; 14 in the DBS plus ODT group and 14 in the ODT-only group. Both groups were predominantly male and were similar in age at baseline (about 61 years). Motor control was assessed during the periods when DBS was applied and not applied by using the Unified Parkinson’s Disease Rating Scale (UPDRS) Part III (clinician assessed) and the Hoehn and Yahr scale.
Over the 5-year period, mean UPDRS motor scores progressively worsened for the ODT group but improved for patients receiving DBS. Patients who received DBS plus ODT had improvements relative to the ODT-only patients of 4.6 points at 1.5 years, 5.8 points at 2 years, 8.9 points at 4 years, and 10.1 points at 5 years.
“These results demonstrate that subthalamic nucleus deep brain stimulation applied in early-stage Parkinson’s disease may provide long-term, clinically meaningful improvement in motor function over standard clinical therapy,” Dr. Hacker said.
The exact mechanism of DBS is still unknown. But, there is evidence that synaptic plasticity is involved. Dr. Hacker speculated that in early Parkinson’s, the DBS intervention comes at a time of relative neuronal stability, which is then maintained.
The results of the pilot trial led to Food and Drug Administration approval of a large-scale, multicenter clinical trial. All participants will be implanted with a DBS device and will receive ODT. Some of the subjects will be randomized to receive DBS during the first 2 years, along with ODT, with the remainder receiving ODT only. In the next 2 years, all subjects will receive DBS and ODT.
Funding was provided by the National Center for Advancing Translational Science, the National Institutes of Health, Medtronic, and the Michael J. Fox Foundation for Parkinson’s Research. Dr. Hacker had no disclosures.
BALTIMORE – The use of subthalamic nucleus deep brain stimulation (DBS) along with optimal drug therapy in patients with early stage Parkinson’s disease produced clinically meaningful improvements in clinician-assessed motor control that lasted at least 5 years in a prospective pilot study.
If the findings bear out a phase III trial that has been approved, DBS may become a valuable method to achieve long-term improvement in motor skills in patients with Parkinson’s disease.
The pilot trial involved 30 patients with Parkinson’s disease, aged 50-75 years, and demonstrated the safety and benefit of DBS in conjunction with optimal drug therapy (ODT) – involving drugs such as carbidopa/levodopa, pramipexole, ropinirole, and selegiline – compared with ODT alone in improving motor scores of the patients through 2 years (Parkinsonism Relat Disord. 2014. 20[7]:731-7). The latest subanalysis of the trial data took a longer look, examining the effect of DBS through 5 years.
The subanalysis involved 28 patients; 14 in the DBS plus ODT group and 14 in the ODT-only group. Both groups were predominantly male and were similar in age at baseline (about 61 years). Motor control was assessed during the periods when DBS was applied and not applied by using the Unified Parkinson’s Disease Rating Scale (UPDRS) Part III (clinician assessed) and the Hoehn and Yahr scale.
Over the 5-year period, mean UPDRS motor scores progressively worsened for the ODT group but improved for patients receiving DBS. Patients who received DBS plus ODT had improvements relative to the ODT-only patients of 4.6 points at 1.5 years, 5.8 points at 2 years, 8.9 points at 4 years, and 10.1 points at 5 years.
“These results demonstrate that subthalamic nucleus deep brain stimulation applied in early-stage Parkinson’s disease may provide long-term, clinically meaningful improvement in motor function over standard clinical therapy,” Dr. Hacker said.
The exact mechanism of DBS is still unknown. But, there is evidence that synaptic plasticity is involved. Dr. Hacker speculated that in early Parkinson’s, the DBS intervention comes at a time of relative neuronal stability, which is then maintained.
The results of the pilot trial led to Food and Drug Administration approval of a large-scale, multicenter clinical trial. All participants will be implanted with a DBS device and will receive ODT. Some of the subjects will be randomized to receive DBS during the first 2 years, along with ODT, with the remainder receiving ODT only. In the next 2 years, all subjects will receive DBS and ODT.
Funding was provided by the National Center for Advancing Translational Science, the National Institutes of Health, Medtronic, and the Michael J. Fox Foundation for Parkinson’s Research. Dr. Hacker had no disclosures.
BALTIMORE – The use of subthalamic nucleus deep brain stimulation (DBS) along with optimal drug therapy in patients with early stage Parkinson’s disease produced clinically meaningful improvements in clinician-assessed motor control that lasted at least 5 years in a prospective pilot study.
If the findings bear out a phase III trial that has been approved, DBS may become a valuable method to achieve long-term improvement in motor skills in patients with Parkinson’s disease.
The pilot trial involved 30 patients with Parkinson’s disease, aged 50-75 years, and demonstrated the safety and benefit of DBS in conjunction with optimal drug therapy (ODT) – involving drugs such as carbidopa/levodopa, pramipexole, ropinirole, and selegiline – compared with ODT alone in improving motor scores of the patients through 2 years (Parkinsonism Relat Disord. 2014. 20[7]:731-7). The latest subanalysis of the trial data took a longer look, examining the effect of DBS through 5 years.
The subanalysis involved 28 patients; 14 in the DBS plus ODT group and 14 in the ODT-only group. Both groups were predominantly male and were similar in age at baseline (about 61 years). Motor control was assessed during the periods when DBS was applied and not applied by using the Unified Parkinson’s Disease Rating Scale (UPDRS) Part III (clinician assessed) and the Hoehn and Yahr scale.
Over the 5-year period, mean UPDRS motor scores progressively worsened for the ODT group but improved for patients receiving DBS. Patients who received DBS plus ODT had improvements relative to the ODT-only patients of 4.6 points at 1.5 years, 5.8 points at 2 years, 8.9 points at 4 years, and 10.1 points at 5 years.
“These results demonstrate that subthalamic nucleus deep brain stimulation applied in early-stage Parkinson’s disease may provide long-term, clinically meaningful improvement in motor function over standard clinical therapy,” Dr. Hacker said.
The exact mechanism of DBS is still unknown. But, there is evidence that synaptic plasticity is involved. Dr. Hacker speculated that in early Parkinson’s, the DBS intervention comes at a time of relative neuronal stability, which is then maintained.
The results of the pilot trial led to Food and Drug Administration approval of a large-scale, multicenter clinical trial. All participants will be implanted with a DBS device and will receive ODT. Some of the subjects will be randomized to receive DBS during the first 2 years, along with ODT, with the remainder receiving ODT only. In the next 2 years, all subjects will receive DBS and ODT.
Funding was provided by the National Center for Advancing Translational Science, the National Institutes of Health, Medtronic, and the Michael J. Fox Foundation for Parkinson’s Research. Dr. Hacker had no disclosures.
Key clinical point:
Major finding: Patients who received DBS plus ODT had UPDRS motor score improvements relative to the ODT-only patients of 4.6 points at 1.5 years, 5.8 points at 2 years, 8.9 points at 4 years, and 10.1 points at 5 years.
Data source: Secondary analysis of a pilot, prospective, randomized, controlled, single-blind clinical trial involving 30 patients with early Parkinson’s disease.
Disclosures: Dr. Hacker had no disclosures. Funding was provided by the National Center for Advancing Translational Science, the National Institutes of Health, Medtronic, and the Michael J. Fox Foundation for Parkinson’s Research.
New trials address unresolved issues in endovascular therapy for acute ischemic stroke
BALTIMORE – Endovascular therapy is a bedrock of acute ischemic stroke treatment, but some vexing issues remain unresolved, according to Joseph Broderick, MD, of the University of Cincinnati.
“We have learned a tremendous amount the last few years. We know that thrombectomy can work if initiated in patients within 6 hours of stroke onset with or without TPA [tissue plasminogen activator]. The question is what we don’t know,” Dr. Broderick said.
The good news is that clinical trials are underway or planned to address several of these issues, he said at the annual meeting of the American Neurological Association.
Mechanical thrombectomy beyond 6 hours
Whether the treatment window for thrombectomy can be safely extended in appropriately selected patients beyond 6 hours from onset is “one of the most important issues we face,” Dr. Broderick said.
Along with DEFUSE 3, the DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention (DAWN) trial will examine whether medical management that includes thrombectomy delivered up to 24 hours after AIS symptoms first appear will yield better clinical outcomes than medical management alone in appropriate patients.
The use of mechanical thrombectomy up to 12 hours after symptom development in AIS patients for whom intravenous TPA can’t be used or doesn’t work will be assessed in the Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy (POSITIVE) trial. The primary objective is to show less stroke-related disability and improved good functional outcomes, compared with those who receive best medical therapy.
The first Multicenter Randomized Clinical Trial of Endovascular Treatment in the Netherlands (MR CLEAN) trial, which used stent retrievers in almost all cases, demonstrated the benefit of endovascular therapy up to 6 hours after stroke onset in the proximal anterior circulation when used along with best medical therapy (N Engl J Med. 2015;372:11-20). The MR CLEAN LATE trial involving 500 patients will expand the time window up to 12 hours.
Triage of acute stroke patients
The triage of AIS patients before their arrival at the hospital also is an evolving emergency medical service issue. While the classic triage involving CT takes time, the use of scoring systems like the National Institutes of Health Stroke Scale and the Cincinnati Stroke Triage Assessment Tool, or telemedicine-based consultation, can be done faster and with less training.
Where the patient is taken first could be important. The RACECAT trial being conducted in the Catalan territory will compare transfer of acute stroke patients with suspected large-vessel occlusion to the closest local stroke center versus direct transfer to an endovascular stroke center.
Conscious sedation or general anesthesia
Some patients undergoing thrombectomy may be able to tolerate conscious sedation in place of general anesthesia. For these patients, cost-effectiveness becomes a dominant consideration. Several anesthesia trials are addressing the issue. The Sedation Versus Intubation for Endovascular Stroke Treatment (SIESTA) trial involving 150 German patients has been completed, but the findings have not been reported. The General or Local Anaesthesia in Intra-arterial Therapy (GOLIATH) trial is recruiting patients in the Netherlands, with a target enrollment of 128. Other trials are planned in China and Sweden, but recruitment has not started.
Thrombectomy alone
For patients with AIS caused by basilar artery occlusion, stroke specialists have wondered whether intra-arterial treatment, including thrombolysis and potentially thrombectomy, could be more effective than best medical therapy, including intravenous thrombolysis. The Basilar Artery International Cooperation Study (BASICS) in Europe and the BEST trial in China are two trials in the early stages of assessing this question.
A related issue is whether thrombectomy alone is better than intravenous TPA followed by thrombectomy. This issue is being addressed in another MR CLEAN trial that is designed to compare the two approaches in 500 patients randomized to one or the other treatment.
Other intravenous antithrombotic drugs
Another unresolved issue relates to the use of other antithrombotic medications delivered intravenously in combination with TPA. This could be the sole treatment strategy, or could be used in patients who also undergo endovascular thrombectomy. The Multi-Arm Optimization of Stroke Thrombolysis (MOST) trial will randomize patients to receive argatroban or eptifibatide along with TPA, or TPA alone, within 3 hours of stroke symptom onset. Endovascular therapy will be done as indicated.
Heparin use in endovascular therapy
The proper use of antithrombotics like heparin in patients treated with endovascular therapy is unclear. The MR CLEAN MED trial will assess the benefits of two doses of unfractionated heparin and aspirin alone or in combination in 1,500 patients with AIS who receive intra-arterial treatment for confirmed anterior circulation occlusion.
On the horizon
Whether neuroprotection can improve the outcome in patients who undergo embolectomy is unclear, and will be the subject of a trial in Canada that is not yet recruiting patients. Finally, the best way to manage blood pressure following embolectomy and reperfusion is also unclear.
Dr. Broderick had no relevant financial disclosures.
BALTIMORE – Endovascular therapy is a bedrock of acute ischemic stroke treatment, but some vexing issues remain unresolved, according to Joseph Broderick, MD, of the University of Cincinnati.
“We have learned a tremendous amount the last few years. We know that thrombectomy can work if initiated in patients within 6 hours of stroke onset with or without TPA [tissue plasminogen activator]. The question is what we don’t know,” Dr. Broderick said.
The good news is that clinical trials are underway or planned to address several of these issues, he said at the annual meeting of the American Neurological Association.
Mechanical thrombectomy beyond 6 hours
Whether the treatment window for thrombectomy can be safely extended in appropriately selected patients beyond 6 hours from onset is “one of the most important issues we face,” Dr. Broderick said.
Along with DEFUSE 3, the DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention (DAWN) trial will examine whether medical management that includes thrombectomy delivered up to 24 hours after AIS symptoms first appear will yield better clinical outcomes than medical management alone in appropriate patients.
The use of mechanical thrombectomy up to 12 hours after symptom development in AIS patients for whom intravenous TPA can’t be used or doesn’t work will be assessed in the Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy (POSITIVE) trial. The primary objective is to show less stroke-related disability and improved good functional outcomes, compared with those who receive best medical therapy.
The first Multicenter Randomized Clinical Trial of Endovascular Treatment in the Netherlands (MR CLEAN) trial, which used stent retrievers in almost all cases, demonstrated the benefit of endovascular therapy up to 6 hours after stroke onset in the proximal anterior circulation when used along with best medical therapy (N Engl J Med. 2015;372:11-20). The MR CLEAN LATE trial involving 500 patients will expand the time window up to 12 hours.
Triage of acute stroke patients
The triage of AIS patients before their arrival at the hospital also is an evolving emergency medical service issue. While the classic triage involving CT takes time, the use of scoring systems like the National Institutes of Health Stroke Scale and the Cincinnati Stroke Triage Assessment Tool, or telemedicine-based consultation, can be done faster and with less training.
Where the patient is taken first could be important. The RACECAT trial being conducted in the Catalan territory will compare transfer of acute stroke patients with suspected large-vessel occlusion to the closest local stroke center versus direct transfer to an endovascular stroke center.
Conscious sedation or general anesthesia
Some patients undergoing thrombectomy may be able to tolerate conscious sedation in place of general anesthesia. For these patients, cost-effectiveness becomes a dominant consideration. Several anesthesia trials are addressing the issue. The Sedation Versus Intubation for Endovascular Stroke Treatment (SIESTA) trial involving 150 German patients has been completed, but the findings have not been reported. The General or Local Anaesthesia in Intra-arterial Therapy (GOLIATH) trial is recruiting patients in the Netherlands, with a target enrollment of 128. Other trials are planned in China and Sweden, but recruitment has not started.
Thrombectomy alone
For patients with AIS caused by basilar artery occlusion, stroke specialists have wondered whether intra-arterial treatment, including thrombolysis and potentially thrombectomy, could be more effective than best medical therapy, including intravenous thrombolysis. The Basilar Artery International Cooperation Study (BASICS) in Europe and the BEST trial in China are two trials in the early stages of assessing this question.
A related issue is whether thrombectomy alone is better than intravenous TPA followed by thrombectomy. This issue is being addressed in another MR CLEAN trial that is designed to compare the two approaches in 500 patients randomized to one or the other treatment.
Other intravenous antithrombotic drugs
Another unresolved issue relates to the use of other antithrombotic medications delivered intravenously in combination with TPA. This could be the sole treatment strategy, or could be used in patients who also undergo endovascular thrombectomy. The Multi-Arm Optimization of Stroke Thrombolysis (MOST) trial will randomize patients to receive argatroban or eptifibatide along with TPA, or TPA alone, within 3 hours of stroke symptom onset. Endovascular therapy will be done as indicated.
Heparin use in endovascular therapy
The proper use of antithrombotics like heparin in patients treated with endovascular therapy is unclear. The MR CLEAN MED trial will assess the benefits of two doses of unfractionated heparin and aspirin alone or in combination in 1,500 patients with AIS who receive intra-arterial treatment for confirmed anterior circulation occlusion.
On the horizon
Whether neuroprotection can improve the outcome in patients who undergo embolectomy is unclear, and will be the subject of a trial in Canada that is not yet recruiting patients. Finally, the best way to manage blood pressure following embolectomy and reperfusion is also unclear.
Dr. Broderick had no relevant financial disclosures.
BALTIMORE – Endovascular therapy is a bedrock of acute ischemic stroke treatment, but some vexing issues remain unresolved, according to Joseph Broderick, MD, of the University of Cincinnati.
“We have learned a tremendous amount the last few years. We know that thrombectomy can work if initiated in patients within 6 hours of stroke onset with or without TPA [tissue plasminogen activator]. The question is what we don’t know,” Dr. Broderick said.
The good news is that clinical trials are underway or planned to address several of these issues, he said at the annual meeting of the American Neurological Association.
Mechanical thrombectomy beyond 6 hours
Whether the treatment window for thrombectomy can be safely extended in appropriately selected patients beyond 6 hours from onset is “one of the most important issues we face,” Dr. Broderick said.
Along with DEFUSE 3, the DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention (DAWN) trial will examine whether medical management that includes thrombectomy delivered up to 24 hours after AIS symptoms first appear will yield better clinical outcomes than medical management alone in appropriate patients.
The use of mechanical thrombectomy up to 12 hours after symptom development in AIS patients for whom intravenous TPA can’t be used or doesn’t work will be assessed in the Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy (POSITIVE) trial. The primary objective is to show less stroke-related disability and improved good functional outcomes, compared with those who receive best medical therapy.
The first Multicenter Randomized Clinical Trial of Endovascular Treatment in the Netherlands (MR CLEAN) trial, which used stent retrievers in almost all cases, demonstrated the benefit of endovascular therapy up to 6 hours after stroke onset in the proximal anterior circulation when used along with best medical therapy (N Engl J Med. 2015;372:11-20). The MR CLEAN LATE trial involving 500 patients will expand the time window up to 12 hours.
Triage of acute stroke patients
The triage of AIS patients before their arrival at the hospital also is an evolving emergency medical service issue. While the classic triage involving CT takes time, the use of scoring systems like the National Institutes of Health Stroke Scale and the Cincinnati Stroke Triage Assessment Tool, or telemedicine-based consultation, can be done faster and with less training.
Where the patient is taken first could be important. The RACECAT trial being conducted in the Catalan territory will compare transfer of acute stroke patients with suspected large-vessel occlusion to the closest local stroke center versus direct transfer to an endovascular stroke center.
Conscious sedation or general anesthesia
Some patients undergoing thrombectomy may be able to tolerate conscious sedation in place of general anesthesia. For these patients, cost-effectiveness becomes a dominant consideration. Several anesthesia trials are addressing the issue. The Sedation Versus Intubation for Endovascular Stroke Treatment (SIESTA) trial involving 150 German patients has been completed, but the findings have not been reported. The General or Local Anaesthesia in Intra-arterial Therapy (GOLIATH) trial is recruiting patients in the Netherlands, with a target enrollment of 128. Other trials are planned in China and Sweden, but recruitment has not started.
Thrombectomy alone
For patients with AIS caused by basilar artery occlusion, stroke specialists have wondered whether intra-arterial treatment, including thrombolysis and potentially thrombectomy, could be more effective than best medical therapy, including intravenous thrombolysis. The Basilar Artery International Cooperation Study (BASICS) in Europe and the BEST trial in China are two trials in the early stages of assessing this question.
A related issue is whether thrombectomy alone is better than intravenous TPA followed by thrombectomy. This issue is being addressed in another MR CLEAN trial that is designed to compare the two approaches in 500 patients randomized to one or the other treatment.
Other intravenous antithrombotic drugs
Another unresolved issue relates to the use of other antithrombotic medications delivered intravenously in combination with TPA. This could be the sole treatment strategy, or could be used in patients who also undergo endovascular thrombectomy. The Multi-Arm Optimization of Stroke Thrombolysis (MOST) trial will randomize patients to receive argatroban or eptifibatide along with TPA, or TPA alone, within 3 hours of stroke symptom onset. Endovascular therapy will be done as indicated.
Heparin use in endovascular therapy
The proper use of antithrombotics like heparin in patients treated with endovascular therapy is unclear. The MR CLEAN MED trial will assess the benefits of two doses of unfractionated heparin and aspirin alone or in combination in 1,500 patients with AIS who receive intra-arterial treatment for confirmed anterior circulation occlusion.
On the horizon
Whether neuroprotection can improve the outcome in patients who undergo embolectomy is unclear, and will be the subject of a trial in Canada that is not yet recruiting patients. Finally, the best way to manage blood pressure following embolectomy and reperfusion is also unclear.
Dr. Broderick had no relevant financial disclosures.
Telehealth has value in Parkinson’s and poststroke care
BALTIMORE – The broadening of access to medical care through telemedicine that’s been occurring for acute neurologic conditions such as stroke has begun to expand to care for more chronic conditions such as Parkinson’s disease and poststroke recovery, according to presentations given at the annual meeting of the American Neurological Association.
Telemedicine care for patients with Parkinson’s appears feasible and acceptable to both patients and clinicians alike, based on recent findings. Ray Dorsey, MD, of the University of Rochester (N.Y.) initiated the Connect.Parkinson study with his colleagues in 2014 to compare usual care enhanced with educational materials against others who received usual care, educational materials, and four virtual sessions with a Parkinson’s disease specialist from 1 of 18 neurology centers nationwide. Some of the participants who lived far away from one of these centers would not otherwise have received such specialized care (Telemed J E Health. 2016;22[7]:590-8).
The participating physicians had concerns about the quality of the video connection, but otherwise were satisfied with the care delivered to the patients. Surveys of participants revealed no differences between the two groups in quality of life and quality of care. About 80% of those who received virtual calls preferred this contact to the regular office visits.
The development of smartphone apps that allow aspects of diseases like Parkinson’s to be monitored are also enabling high-quality, diagnostic telecare. A pilot study of an Android smartphone Parkinson’s disease app by Dr. Dorsey and his colleagues demonstrated its utility in tests of voice, postural sway, gait, finger tapping, and reaction time (Parkinsonism Relat Disord. 2015;21[6]:650-3).
Since that study was completed, an iOS smartphone version of the app, called mPower, has been developed and has enrolled many Parkinson’s disease patients. The technology is being tested to virtually gauge Parkinson’s disease symptoms and the effects of medications on them. This has opened the door to the world of virtual clinical trials and longitudinal studies targeting genetic subpopulations, Dr. Dorsey said at the meeting.
The telehealth portion of COMPASS – in the form of regular phone calls and web-based feedback – enables better stroke care following hospital discharge by keeping track of common complications that are partly responsible for a readmittance rate of around 25% within 90 days of hospital discharge and tracking physiological aspects like blood pressure, diabetes, diet, exercise, and smoking.
The pilot demonstration of the potential of the program was pivotal in securing funding for a cluster-randomized pragmatic trial. The trial will randomize hospitals to normal discharge or discharge followed by regular poststroke contact. Patient functional status at 90 days post stroke will be assessed for 1 year. After the year, the hospitals randomized to COMPASS care delivery will continue this care, and the hospitals offering normal discharge will also adopt this poststroke service care. Patient outcome will be followed for another year.
The anticipated patient enrollment is 5,400. Results from the first year of the 2-year study are expected in Spring 2018. “COMPASS will have an impact on the post-acute stroke care pathway. After evaluating the effectiveness, the goal is to disseminate and scale to other settings,” Dr. Bushnell said at the meeting.
Dr. Dorsey receives research support from Excellus BlueCross BlueShield, Google, and the Verizon Foundation. He has received compensation for consulting services for Medtronic and owns stock options in ConsultingMD. Dr. Bushnell acknowledged salary support from the COMPASS program, which receives funding from the Patient-Centered Outcomes Research Institute.
BALTIMORE – The broadening of access to medical care through telemedicine that’s been occurring for acute neurologic conditions such as stroke has begun to expand to care for more chronic conditions such as Parkinson’s disease and poststroke recovery, according to presentations given at the annual meeting of the American Neurological Association.
Telemedicine care for patients with Parkinson’s appears feasible and acceptable to both patients and clinicians alike, based on recent findings. Ray Dorsey, MD, of the University of Rochester (N.Y.) initiated the Connect.Parkinson study with his colleagues in 2014 to compare usual care enhanced with educational materials against others who received usual care, educational materials, and four virtual sessions with a Parkinson’s disease specialist from 1 of 18 neurology centers nationwide. Some of the participants who lived far away from one of these centers would not otherwise have received such specialized care (Telemed J E Health. 2016;22[7]:590-8).
The participating physicians had concerns about the quality of the video connection, but otherwise were satisfied with the care delivered to the patients. Surveys of participants revealed no differences between the two groups in quality of life and quality of care. About 80% of those who received virtual calls preferred this contact to the regular office visits.
The development of smartphone apps that allow aspects of diseases like Parkinson’s to be monitored are also enabling high-quality, diagnostic telecare. A pilot study of an Android smartphone Parkinson’s disease app by Dr. Dorsey and his colleagues demonstrated its utility in tests of voice, postural sway, gait, finger tapping, and reaction time (Parkinsonism Relat Disord. 2015;21[6]:650-3).
Since that study was completed, an iOS smartphone version of the app, called mPower, has been developed and has enrolled many Parkinson’s disease patients. The technology is being tested to virtually gauge Parkinson’s disease symptoms and the effects of medications on them. This has opened the door to the world of virtual clinical trials and longitudinal studies targeting genetic subpopulations, Dr. Dorsey said at the meeting.
The telehealth portion of COMPASS – in the form of regular phone calls and web-based feedback – enables better stroke care following hospital discharge by keeping track of common complications that are partly responsible for a readmittance rate of around 25% within 90 days of hospital discharge and tracking physiological aspects like blood pressure, diabetes, diet, exercise, and smoking.
The pilot demonstration of the potential of the program was pivotal in securing funding for a cluster-randomized pragmatic trial. The trial will randomize hospitals to normal discharge or discharge followed by regular poststroke contact. Patient functional status at 90 days post stroke will be assessed for 1 year. After the year, the hospitals randomized to COMPASS care delivery will continue this care, and the hospitals offering normal discharge will also adopt this poststroke service care. Patient outcome will be followed for another year.
The anticipated patient enrollment is 5,400. Results from the first year of the 2-year study are expected in Spring 2018. “COMPASS will have an impact on the post-acute stroke care pathway. After evaluating the effectiveness, the goal is to disseminate and scale to other settings,” Dr. Bushnell said at the meeting.
Dr. Dorsey receives research support from Excellus BlueCross BlueShield, Google, and the Verizon Foundation. He has received compensation for consulting services for Medtronic and owns stock options in ConsultingMD. Dr. Bushnell acknowledged salary support from the COMPASS program, which receives funding from the Patient-Centered Outcomes Research Institute.
BALTIMORE – The broadening of access to medical care through telemedicine that’s been occurring for acute neurologic conditions such as stroke has begun to expand to care for more chronic conditions such as Parkinson’s disease and poststroke recovery, according to presentations given at the annual meeting of the American Neurological Association.
Telemedicine care for patients with Parkinson’s appears feasible and acceptable to both patients and clinicians alike, based on recent findings. Ray Dorsey, MD, of the University of Rochester (N.Y.) initiated the Connect.Parkinson study with his colleagues in 2014 to compare usual care enhanced with educational materials against others who received usual care, educational materials, and four virtual sessions with a Parkinson’s disease specialist from 1 of 18 neurology centers nationwide. Some of the participants who lived far away from one of these centers would not otherwise have received such specialized care (Telemed J E Health. 2016;22[7]:590-8).
The participating physicians had concerns about the quality of the video connection, but otherwise were satisfied with the care delivered to the patients. Surveys of participants revealed no differences between the two groups in quality of life and quality of care. About 80% of those who received virtual calls preferred this contact to the regular office visits.
The development of smartphone apps that allow aspects of diseases like Parkinson’s to be monitored are also enabling high-quality, diagnostic telecare. A pilot study of an Android smartphone Parkinson’s disease app by Dr. Dorsey and his colleagues demonstrated its utility in tests of voice, postural sway, gait, finger tapping, and reaction time (Parkinsonism Relat Disord. 2015;21[6]:650-3).
Since that study was completed, an iOS smartphone version of the app, called mPower, has been developed and has enrolled many Parkinson’s disease patients. The technology is being tested to virtually gauge Parkinson’s disease symptoms and the effects of medications on them. This has opened the door to the world of virtual clinical trials and longitudinal studies targeting genetic subpopulations, Dr. Dorsey said at the meeting.
The telehealth portion of COMPASS – in the form of regular phone calls and web-based feedback – enables better stroke care following hospital discharge by keeping track of common complications that are partly responsible for a readmittance rate of around 25% within 90 days of hospital discharge and tracking physiological aspects like blood pressure, diabetes, diet, exercise, and smoking.
The pilot demonstration of the potential of the program was pivotal in securing funding for a cluster-randomized pragmatic trial. The trial will randomize hospitals to normal discharge or discharge followed by regular poststroke contact. Patient functional status at 90 days post stroke will be assessed for 1 year. After the year, the hospitals randomized to COMPASS care delivery will continue this care, and the hospitals offering normal discharge will also adopt this poststroke service care. Patient outcome will be followed for another year.
The anticipated patient enrollment is 5,400. Results from the first year of the 2-year study are expected in Spring 2018. “COMPASS will have an impact on the post-acute stroke care pathway. After evaluating the effectiveness, the goal is to disseminate and scale to other settings,” Dr. Bushnell said at the meeting.
Dr. Dorsey receives research support from Excellus BlueCross BlueShield, Google, and the Verizon Foundation. He has received compensation for consulting services for Medtronic and owns stock options in ConsultingMD. Dr. Bushnell acknowledged salary support from the COMPASS program, which receives funding from the Patient-Centered Outcomes Research Institute.
EXPERT ANALYSIS FROM ANA 2016
Computed tomography angiography after NCCT delays thrombectomy
BALTIMORE – Performing computed tomography angiography (CTA) following noncontrast computed tomography (NCCT) to obtain a high-resolution image of the large-vessel occlusion significantly delays the time to thrombectomy.
In clinical practice, omitting CTA in patients whose middle cerebral artery visualized on NCCT reveals the hyperdense sign may speed the time to thrombectomy and improve outcome. The findings of a retrospective cohort study of prospectively collected data were presented by Kunakorn Atchaneeyasakul, MD, of the University of Miami, as a poster and a brief oral presentation at the annual meeting of the American Neurological Association.
This study retrospectively compared the time from imaging to groin puncture, which is the first step in thrombectomy, in patients who received NCCT followed by CTA with those who received just NCCT for anterior circulation occlusion at the tertiary care University of Miami medical center. Of the 289 patients who received thrombectomy, 255 were excluded because of transfer from another hospital, occurrence of stroke while hospitalized, or use of other imaging prior to thrombectomy.
The remaining 34 patients were all evaluated with thin (0.625-mm) NCCT with automated image reconstruction. Fourteen received NCCT only, and 20 received CTA in addition to NCCT. The two groups were similar in mean age (64-71 years), gender (50% were female in each group), prevalence of hypertension (64% and 70% in the NCCT and NCCT + CTA group, respectively), and prevalence of diabetes, hyperlipidemia, atrial fibrillation, smoking, occlusion site, modified Rankin Scale score at discharge, and National Institutes of Health Stroke Scale scores at presentation and discharge. All 14 NCCT patients received intravenous tPA in contrast to 11 of the 20 (55%) NCCT + CTA patients (P = .003).
The middle cerebral artery was visualized on NCCT in about 85% of patients in each treatment group. Reperfusion was successful in 64% and 80% of patients receiving NCCT and NCCT + CTA, respectively (P = .31).
The total duration of imaging was 2 minutes (range, 1-6) in the NCCT group. The duration was significantly longer in the NCCT + CTA group (28 minutes; range, 23-65; P less than .001). The time from imaging to groin puncture was 68 minutes (range, 32-99) in the NCCT group. This was more than 30 minutes shorter than the NCCT + CTA group (104 minutes; range, 79-128; P = .030).
The times from emergency department admission to NCCT and from admission to groin puncture were similar in both groups.
“Avoiding advanced imaging in patients with anterior circulation large-vessel occlusion in whom thin-section NCCT with maximum-intensity projections reveals a hyperdense sign significantly shortens the imaging to groin puncture time,” concluded Dr. Atchaneeyasakul.
In the scenario, the detection of hyperdense middle cerebral artery would fast track the patient to the angiography suite, forgoing CTA. The result, according to Dr. Atchaneeyasakul, could alleviate a delay in thrombectomy, which could better preserve brain function.
Funding information was not provided.
BALTIMORE – Performing computed tomography angiography (CTA) following noncontrast computed tomography (NCCT) to obtain a high-resolution image of the large-vessel occlusion significantly delays the time to thrombectomy.
In clinical practice, omitting CTA in patients whose middle cerebral artery visualized on NCCT reveals the hyperdense sign may speed the time to thrombectomy and improve outcome. The findings of a retrospective cohort study of prospectively collected data were presented by Kunakorn Atchaneeyasakul, MD, of the University of Miami, as a poster and a brief oral presentation at the annual meeting of the American Neurological Association.
This study retrospectively compared the time from imaging to groin puncture, which is the first step in thrombectomy, in patients who received NCCT followed by CTA with those who received just NCCT for anterior circulation occlusion at the tertiary care University of Miami medical center. Of the 289 patients who received thrombectomy, 255 were excluded because of transfer from another hospital, occurrence of stroke while hospitalized, or use of other imaging prior to thrombectomy.
The remaining 34 patients were all evaluated with thin (0.625-mm) NCCT with automated image reconstruction. Fourteen received NCCT only, and 20 received CTA in addition to NCCT. The two groups were similar in mean age (64-71 years), gender (50% were female in each group), prevalence of hypertension (64% and 70% in the NCCT and NCCT + CTA group, respectively), and prevalence of diabetes, hyperlipidemia, atrial fibrillation, smoking, occlusion site, modified Rankin Scale score at discharge, and National Institutes of Health Stroke Scale scores at presentation and discharge. All 14 NCCT patients received intravenous tPA in contrast to 11 of the 20 (55%) NCCT + CTA patients (P = .003).
The middle cerebral artery was visualized on NCCT in about 85% of patients in each treatment group. Reperfusion was successful in 64% and 80% of patients receiving NCCT and NCCT + CTA, respectively (P = .31).
The total duration of imaging was 2 minutes (range, 1-6) in the NCCT group. The duration was significantly longer in the NCCT + CTA group (28 minutes; range, 23-65; P less than .001). The time from imaging to groin puncture was 68 minutes (range, 32-99) in the NCCT group. This was more than 30 minutes shorter than the NCCT + CTA group (104 minutes; range, 79-128; P = .030).
The times from emergency department admission to NCCT and from admission to groin puncture were similar in both groups.
“Avoiding advanced imaging in patients with anterior circulation large-vessel occlusion in whom thin-section NCCT with maximum-intensity projections reveals a hyperdense sign significantly shortens the imaging to groin puncture time,” concluded Dr. Atchaneeyasakul.
In the scenario, the detection of hyperdense middle cerebral artery would fast track the patient to the angiography suite, forgoing CTA. The result, according to Dr. Atchaneeyasakul, could alleviate a delay in thrombectomy, which could better preserve brain function.
Funding information was not provided.
BALTIMORE – Performing computed tomography angiography (CTA) following noncontrast computed tomography (NCCT) to obtain a high-resolution image of the large-vessel occlusion significantly delays the time to thrombectomy.
In clinical practice, omitting CTA in patients whose middle cerebral artery visualized on NCCT reveals the hyperdense sign may speed the time to thrombectomy and improve outcome. The findings of a retrospective cohort study of prospectively collected data were presented by Kunakorn Atchaneeyasakul, MD, of the University of Miami, as a poster and a brief oral presentation at the annual meeting of the American Neurological Association.
This study retrospectively compared the time from imaging to groin puncture, which is the first step in thrombectomy, in patients who received NCCT followed by CTA with those who received just NCCT for anterior circulation occlusion at the tertiary care University of Miami medical center. Of the 289 patients who received thrombectomy, 255 were excluded because of transfer from another hospital, occurrence of stroke while hospitalized, or use of other imaging prior to thrombectomy.
The remaining 34 patients were all evaluated with thin (0.625-mm) NCCT with automated image reconstruction. Fourteen received NCCT only, and 20 received CTA in addition to NCCT. The two groups were similar in mean age (64-71 years), gender (50% were female in each group), prevalence of hypertension (64% and 70% in the NCCT and NCCT + CTA group, respectively), and prevalence of diabetes, hyperlipidemia, atrial fibrillation, smoking, occlusion site, modified Rankin Scale score at discharge, and National Institutes of Health Stroke Scale scores at presentation and discharge. All 14 NCCT patients received intravenous tPA in contrast to 11 of the 20 (55%) NCCT + CTA patients (P = .003).
The middle cerebral artery was visualized on NCCT in about 85% of patients in each treatment group. Reperfusion was successful in 64% and 80% of patients receiving NCCT and NCCT + CTA, respectively (P = .31).
The total duration of imaging was 2 minutes (range, 1-6) in the NCCT group. The duration was significantly longer in the NCCT + CTA group (28 minutes; range, 23-65; P less than .001). The time from imaging to groin puncture was 68 minutes (range, 32-99) in the NCCT group. This was more than 30 minutes shorter than the NCCT + CTA group (104 minutes; range, 79-128; P = .030).
The times from emergency department admission to NCCT and from admission to groin puncture were similar in both groups.
“Avoiding advanced imaging in patients with anterior circulation large-vessel occlusion in whom thin-section NCCT with maximum-intensity projections reveals a hyperdense sign significantly shortens the imaging to groin puncture time,” concluded Dr. Atchaneeyasakul.
In the scenario, the detection of hyperdense middle cerebral artery would fast track the patient to the angiography suite, forgoing CTA. The result, according to Dr. Atchaneeyasakul, could alleviate a delay in thrombectomy, which could better preserve brain function.
Funding information was not provided.
AT ANA 2016
Key clinical point:
Major finding: Time from imaging to groin puncture was 68 minutes for NCCT vs. 104 minutes for NCCT + CTA.
Data source: Retrospective cohort study of prospectively collected data.
Disclosures: Dr. Atchaneeyasakul had no disclosures.