User login
Top DEI Topics to Incorporate Into Dermatology Residency Training: An Electronic Delphi Consensus Study
Diversity, equity, and inclusion (DEI) programs seek to improve dermatologic education and clinical care for an increasingly diverse patient population as well as to recruit and sustain a physician workforce that reflects the diversity of the patients they serve.1,2 In dermatology, only 4.2% and 3.0% of practicing dermatologists self-identify as being of Hispanic and African American ethnicity, respectively, compared with 18.5% and 13.4% of the general population, respectively.3 Creating an educational system that works to meet the goals of DEI is essential to improve health outcomes and address disparities. The lack of robust DEI-related curricula during residency training may limit the ability of practicing dermatologists to provide comprehensive and culturally sensitive care. It has been shown that racial concordance between patients and physicians has a positive impact on patient satisfaction by fostering a trusting patient-physician relationship.4
It is the responsibility of all dermatologists to create an environment where patients from any background can feel comfortable, which can be cultivated by establishing patient-centered communication and cultural humility.5 These skills can be strengthened via the implementation of DEI-related curricula during residency training. Augmenting exposure of these topics during training can optimize the delivery of dermatologic care by providing residents with the tools and confidence needed to care for patients of culturally diverse backgrounds. Enhancing DEI education is crucial to not only improve the recognition and treatment of dermatologic conditions in all skin and hair types but also to minimize misconceptions, stigma, health disparities, and discrimination faced by historically marginalized communities. Creating a culture of inclusion is of paramount importance to build successful relationships with patients and colleagues of culturally diverse backgrounds.6
There are multiple efforts underway to increase DEI education across the field of dermatology, including the development of DEI task forces in professional organizations and societies that serve to expand DEI-related research, mentorship, and education. The American Academy of Dermatology has been leading efforts to create a curriculum focused on skin of color, particularly addressing inadequate educational training on how dermatologic conditions manifest in this population.7 The Skin of Color Society has similar efforts underway and is developing a speakers bureau to give leading experts a platform to lecture dermatology trainees as well as patient and community audiences on various topics in skin of color.8 These are just 2 of many professional dermatology organizations that are advocating for expanded education on DEI; however, consistently integrating DEI-related topics into dermatology residency training curricula remains a gap in pedagogy. To identify the DEI-related topics of greatest relevance to the dermatology resident curricula, we implemented a modified electronic Delphi (e-Delphi) consensus process to provide standardized recommendations.
Methods
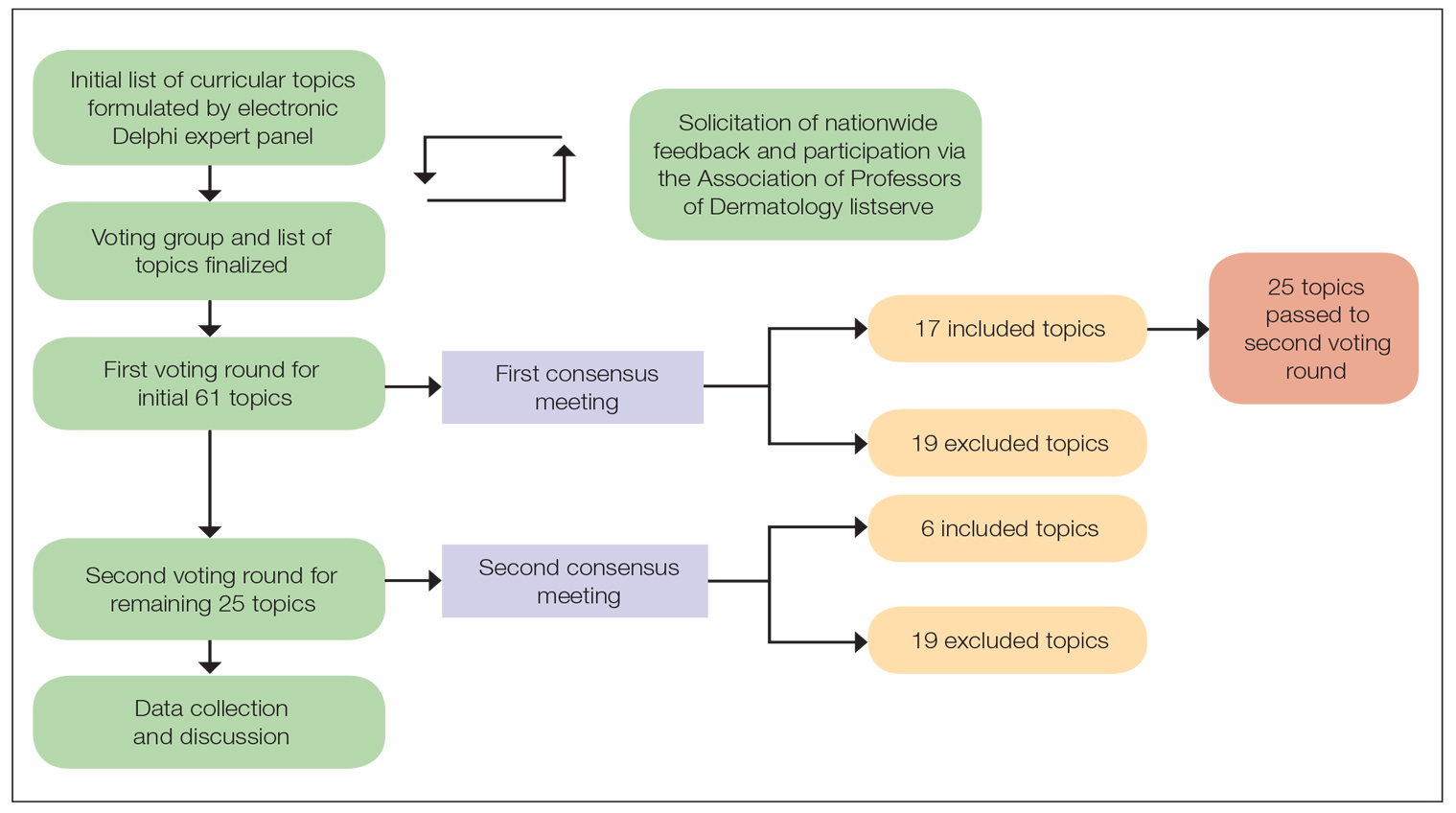
A 2-round modified e-Delphi method was utilized (Figure). An initial list of potential curricular topics was formulated by an expert panel consisting of 5 dermatologists from the Association of Professors of Dermatology DEI subcommittee and the American Academy of Dermatology Diversity Task Force (A.M.A., S.B., R.V., S.D.W., J.I.S.). Initial topics were selected via several meetings among the panel members to discuss existing DEI concerns and issues that were deemed relevant due to education gaps in residency training. The list of topics was further expanded with recommendations obtained via an email sent to dermatology program directors on the Association of Professors of Dermatology listserve, which solicited voluntary participation of academic dermatologists, including program directors and dermatology residents.
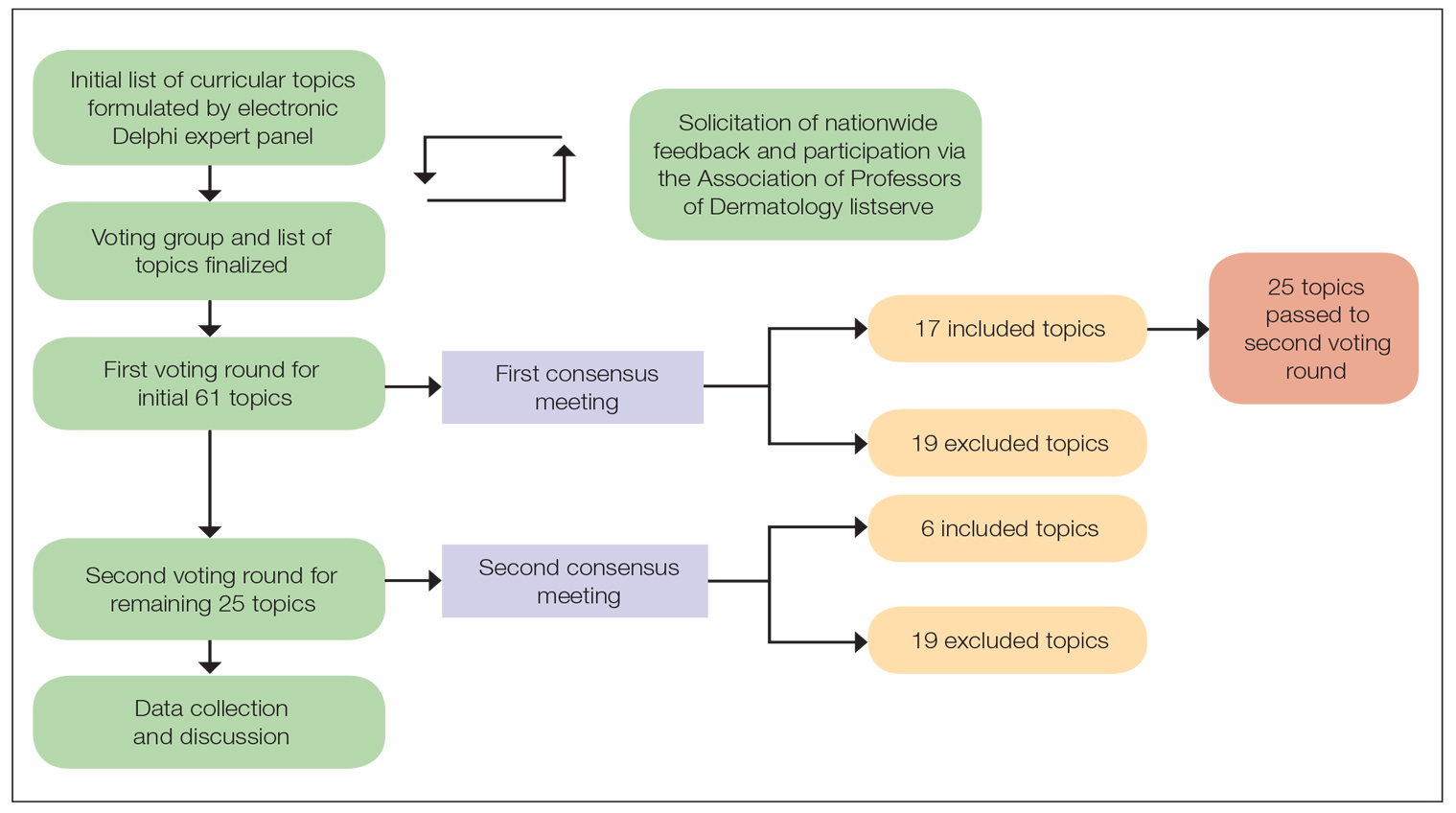
There were 2 voting rounds, with each round consisting of questions scored on a Likert scale ranging from 1 to 5 (1=not essential, 2=probably not essential, 3=neutral, 4=probably essential, 5=definitely essential). The inclusion criteria to classify a topic as necessary for integration into the dermatology residency curriculum included 95% (18/19) or more of respondents rating the topic as probably essential or definitely essential; if more than 90% (17/19) of respondents rated the topic as probably essential or definitely essential and less than 10% (2/19) rated it as not essential or probably not essential, the topic was still included as part of the suggested curriculum. Topics that received ratings of probably essential or definitely essential by less than 80% (15/19) of respondents were removed from consideration. The topics that did not meet inclusion or exclusion criteria during the first round of voting were refined by the e-Delphi steering committee (V.S.E-C. and F-A.R.) based on open-ended feedback from the voting group provided at the end of the survey and subsequently passed to the second round of voting.
Results
Participants—A total of 19 respondents participated in both voting rounds, the majority (80% [15/19]) of whom were program directors or dermatologists affiliated with academia or development of DEI education; the remaining 20% [4/19]) were dermatology residents.
Open-Ended Feedback—Voting group members were able to provide open-ended feedback for each of the sets of topics after the survey, which the steering committee utilized to modify the topics as needed for the final voting round. For example, “structural racism/discrimination” was originally mentioned as a topic, but several participants suggested including specific types of racism; therefore, the wording was changed to “racism: types, definitions” to encompass broader definitions and types of racism.
Survey Results—Two genres of topics were surveyed in each voting round: clinical and nonclinical. Participants voted on a total of 61 topics, with 23 ultimately selected in the final list of consensus curricular topics. Of those, 9 were clinical and 14 nonclinical. All topics deemed necessary for inclusion in residency curricula are presented in eTables 1 and 2.
During the first round of voting, the e-Delphi panel reached a consensus to include the following 17 topics as essential to dermatology residency training (along with the percentage of voters who classified them as probably essential or definitely essential): how to mitigate bias in clinical and workplace settings (100% [40/40]); social determinants of health-related disparities in dermatology (100% [40/40]); hairstyling practices across different hair textures (100% [40/40]); definitions and examples of microaggressions (97.50% [39/40]); definition, background, and types of bias (97.50% [39/40]); manifestations of bias in the clinical setting (97.44% [38/39]); racial and ethnic disparities in dermatology (97.44% [38/39]); keloids (97.37% [37/38]); differences in dermoscopic presentations in skin of color (97.30% [36/37]); skin cancer in patients with skin of color (97.30% [36/37]); disparities due to bias (95.00% [38/40]); how to apply cultural humility and safety to patients of different cultural backgrounds (94.87% [37/40]); best practices in providing care to patients with limited English proficiency (94.87% [37/40]); hair loss in patients with textured hair (94.74% [36/38]); pseudofolliculitis barbae and acne keloidalis nuchae (94.60% [35/37]); disparities regarding people experiencing homelessness (92.31% [36/39]); and definitions and types of racism and other forms of discrimination (92.31% [36/39]). eTable 1 provides a list of suggested resources to incorporate these topics into the educational components of residency curricula. The resources provided were not part of the voting process, and they were not considered in the consensus analysis; they are included here as suggested educational catalysts.
During the second round of voting, 25 topics were evaluated. Of those, the following 6 topics were proposed to be included as essential in residency training: differences in prevalence and presentation of common inflammatory disorders (100% [29/29]); manifestations of bias in the learning environment (96.55%); antiracist action and how to decrease the effects of structural racism in clinical and educational settings (96.55% [28/29]); diversity of images in dermatology education (96.55% [28/29]); pigmentary disorders and their psychological effects (96.55% [28/29]); and LGBTQ (lesbian, gay, bisexual, transgender, and queer) dermatologic health care (96.55% [28/29]). eTable 2 includes these topics as well as suggested resources to help incorporate them into training.
Comment
This study utilized a modified e-Delphi technique to identify relevant clinical and nonclinical DEI topics that should be incorporated into dermatology residency curricula. The panel members reached a consensus for 9 clinical DEI-related topics. The respondents agreed that the topics related to skin and hair conditions in patients with skin of color as well as textured hair were crucial to residency education. Skin cancer, hair loss, pseudofolliculitis barbae, acne keloidalis nuchae, keloids, pigmentary disorders, and their varying presentations in patients with skin of color were among the recommended topics. The panel also recommended educating residents on the variable visual presentations of inflammatory conditions in skin of color. Addressing the needs of diverse patients—for example, those belonging to the LGBTQ community—also was deemed important for inclusion.
The remaining 14 chosen topics were nonclinical items addressing concepts such as bias and health care disparities as well as cultural humility and safety.9 Cultural humility and safety focus on developing cultural awareness by creating a safe setting for patients rather than encouraging power relationships between them and their physicians. Various topics related to racism also were recommended to be included in residency curricula, including education on implementation of antiracist action in the workplace.
Many of the nonclinical topics are intertwined; for instance, learning about health care disparities in patients with limited English proficiency allows for improved best practices in delivering care to patients from this population. The first step in overcoming bias and subsequent disparities is acknowledging how the perpetuation of bias leads to disparities after being taught tools to recognize it.
Our group’s guidance on DEI topics should help dermatology residency program leaders as they design and refine program curricula. There are multiple avenues for incorporating education on these topics, including lectures, interactive workshops, role-playing sessions, book or journal clubs, and discussion circles. Many of these topics/programs may already be included in programs’ didactic curricula, which would minimize the burden of finding space to educate on these topics. Institutional cultural change is key to ensuring truly diverse, equitable, and inclusive workplaces. Educating tomorrow’s dermatologists on these topics is a first step toward achieving that cultural change.
Limitations—A limitation of this e-Delphi survey is that only a selection of experts in this field was included. Additionally, we were concerned that the Likert scale format and the bar we set for inclusion and exclusion may have failed to adequately capture participants’ nuanced opinions. As such, participants were able to provide open-ended feedback, and suggestions for alternate wording or other changes were considered by the steering committee. Finally, inclusion recommendations identified in this survey were developed specifically for US dermatology residents.
Conclusion
In this e-Delphi consensus assessment of DEI-related topics, we recommend the inclusion of 23 topics into dermatology residency program curricula to improve medical training and the patient-physician relationship as well as to create better health outcomes. We also provide specific sample resource recommendations in eTables 1 and 2 to facilitate inclusion of these topics into residency curricula across the country.
- US Census Bureau projections show a slower growing, older, more diverse nation a half century from now. News release. US Census Bureau. December 12, 2012. Accessed August 14, 2024. https://www.census.gov/newsroom/releases/archives/population/cb12243.html#:~:text=12%2C%202012,U.S.%20Census%20Bureau%20Projections%20Show%20a%20Slower%20Growing%2C%20Older%2C%20More,by%20the%20U.S.%20Census%20Bureau
- Lopez S, Lourido JO, Lim HW, et al. The call to action to increase racial and ethnic diversity in dermatology: a retrospective, cross-sectional study to monitor progress. J Am Acad Dermatol. 2020;86:E121-E123. doi:10.1016/j.jaad.2021.10.011
- El-Kashlan N, Alexis A. Disparities in dermatology: a reflection. J Clin Aesthet Dermatol. 2022;15:27-29.
- Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43:296-306.
- Street RL Jr, O’Malley KJ, Cooper LA, et al. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6:198-205. doi:10.1370/afm.821
- Dadrass F, Bowers S, Shinkai K, et al. Diversity, equity, and inclusion in dermatology residency. Dermatol Clin. 2023;41:257-263. doi:10.1016/j.det.2022.10.006
- Diversity and the Academy. American Academy of Dermatology website. Accessed August 22, 2024. https://www.aad.org/member/career/diversity
- SOCS speaks. Skin of Color Society website. Accessed August 22, 2024. https://skinofcolorsociety.org/news-media/socs-speaks
- Solchanyk D, Ekeh O, Saffran L, et al. Integrating cultural humility into the medical education curriculum: strategies for educators. Teach Learn Med. 2021;33:554-560. doi:10.1080/10401334.2021.1877711
Diversity, equity, and inclusion (DEI) programs seek to improve dermatologic education and clinical care for an increasingly diverse patient population as well as to recruit and sustain a physician workforce that reflects the diversity of the patients they serve.1,2 In dermatology, only 4.2% and 3.0% of practicing dermatologists self-identify as being of Hispanic and African American ethnicity, respectively, compared with 18.5% and 13.4% of the general population, respectively.3 Creating an educational system that works to meet the goals of DEI is essential to improve health outcomes and address disparities. The lack of robust DEI-related curricula during residency training may limit the ability of practicing dermatologists to provide comprehensive and culturally sensitive care. It has been shown that racial concordance between patients and physicians has a positive impact on patient satisfaction by fostering a trusting patient-physician relationship.4
It is the responsibility of all dermatologists to create an environment where patients from any background can feel comfortable, which can be cultivated by establishing patient-centered communication and cultural humility.5 These skills can be strengthened via the implementation of DEI-related curricula during residency training. Augmenting exposure of these topics during training can optimize the delivery of dermatologic care by providing residents with the tools and confidence needed to care for patients of culturally diverse backgrounds. Enhancing DEI education is crucial to not only improve the recognition and treatment of dermatologic conditions in all skin and hair types but also to minimize misconceptions, stigma, health disparities, and discrimination faced by historically marginalized communities. Creating a culture of inclusion is of paramount importance to build successful relationships with patients and colleagues of culturally diverse backgrounds.6
There are multiple efforts underway to increase DEI education across the field of dermatology, including the development of DEI task forces in professional organizations and societies that serve to expand DEI-related research, mentorship, and education. The American Academy of Dermatology has been leading efforts to create a curriculum focused on skin of color, particularly addressing inadequate educational training on how dermatologic conditions manifest in this population.7 The Skin of Color Society has similar efforts underway and is developing a speakers bureau to give leading experts a platform to lecture dermatology trainees as well as patient and community audiences on various topics in skin of color.8 These are just 2 of many professional dermatology organizations that are advocating for expanded education on DEI; however, consistently integrating DEI-related topics into dermatology residency training curricula remains a gap in pedagogy. To identify the DEI-related topics of greatest relevance to the dermatology resident curricula, we implemented a modified electronic Delphi (e-Delphi) consensus process to provide standardized recommendations.
Methods
A 2-round modified e-Delphi method was utilized (Figure). An initial list of potential curricular topics was formulated by an expert panel consisting of 5 dermatologists from the Association of Professors of Dermatology DEI subcommittee and the American Academy of Dermatology Diversity Task Force (A.M.A., S.B., R.V., S.D.W., J.I.S.). Initial topics were selected via several meetings among the panel members to discuss existing DEI concerns and issues that were deemed relevant due to education gaps in residency training. The list of topics was further expanded with recommendations obtained via an email sent to dermatology program directors on the Association of Professors of Dermatology listserve, which solicited voluntary participation of academic dermatologists, including program directors and dermatology residents.
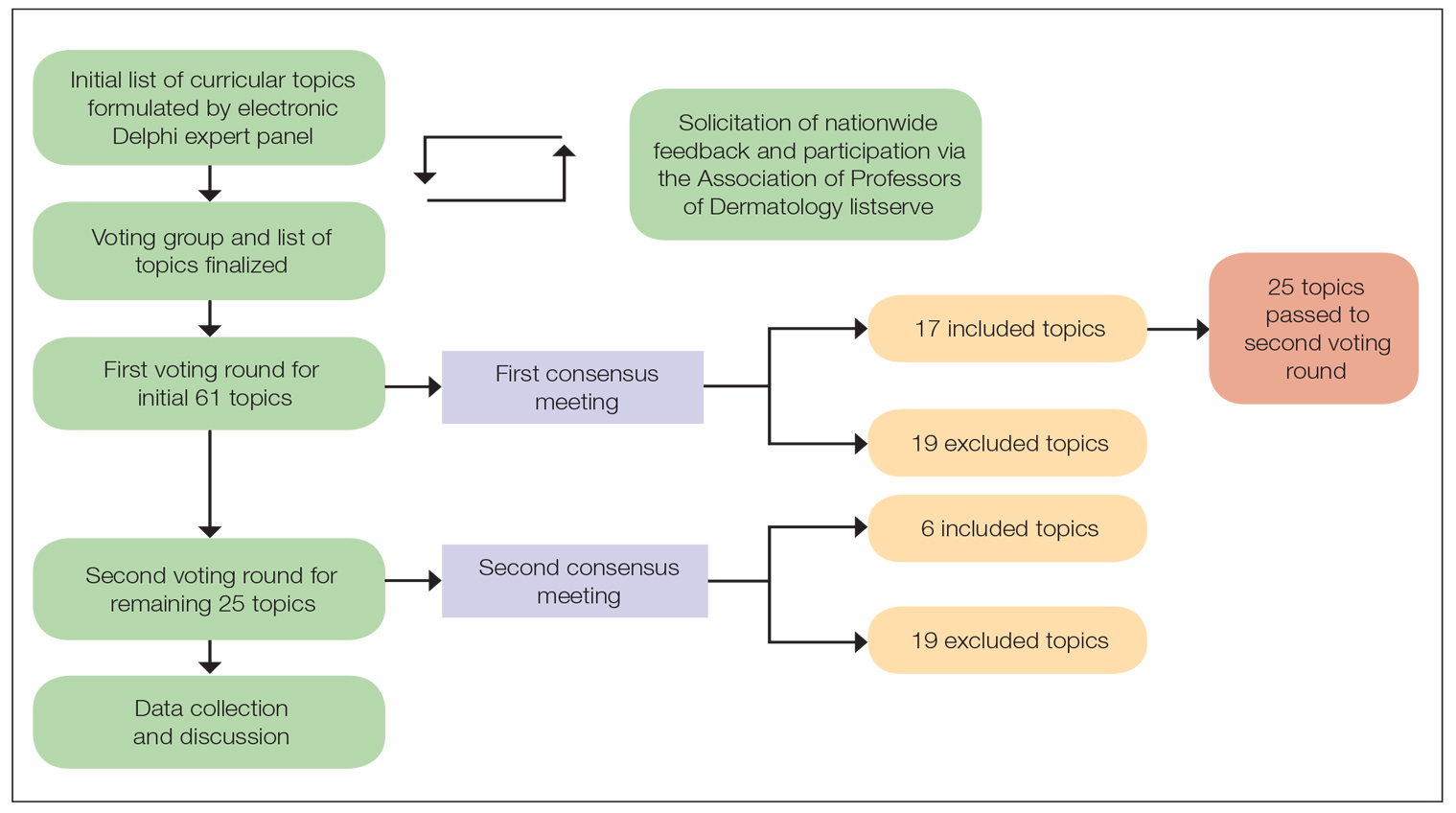
There were 2 voting rounds, with each round consisting of questions scored on a Likert scale ranging from 1 to 5 (1=not essential, 2=probably not essential, 3=neutral, 4=probably essential, 5=definitely essential). The inclusion criteria to classify a topic as necessary for integration into the dermatology residency curriculum included 95% (18/19) or more of respondents rating the topic as probably essential or definitely essential; if more than 90% (17/19) of respondents rated the topic as probably essential or definitely essential and less than 10% (2/19) rated it as not essential or probably not essential, the topic was still included as part of the suggested curriculum. Topics that received ratings of probably essential or definitely essential by less than 80% (15/19) of respondents were removed from consideration. The topics that did not meet inclusion or exclusion criteria during the first round of voting were refined by the e-Delphi steering committee (V.S.E-C. and F-A.R.) based on open-ended feedback from the voting group provided at the end of the survey and subsequently passed to the second round of voting.
Results
Participants—A total of 19 respondents participated in both voting rounds, the majority (80% [15/19]) of whom were program directors or dermatologists affiliated with academia or development of DEI education; the remaining 20% [4/19]) were dermatology residents.
Open-Ended Feedback—Voting group members were able to provide open-ended feedback for each of the sets of topics after the survey, which the steering committee utilized to modify the topics as needed for the final voting round. For example, “structural racism/discrimination” was originally mentioned as a topic, but several participants suggested including specific types of racism; therefore, the wording was changed to “racism: types, definitions” to encompass broader definitions and types of racism.
Survey Results—Two genres of topics were surveyed in each voting round: clinical and nonclinical. Participants voted on a total of 61 topics, with 23 ultimately selected in the final list of consensus curricular topics. Of those, 9 were clinical and 14 nonclinical. All topics deemed necessary for inclusion in residency curricula are presented in eTables 1 and 2.
During the first round of voting, the e-Delphi panel reached a consensus to include the following 17 topics as essential to dermatology residency training (along with the percentage of voters who classified them as probably essential or definitely essential): how to mitigate bias in clinical and workplace settings (100% [40/40]); social determinants of health-related disparities in dermatology (100% [40/40]); hairstyling practices across different hair textures (100% [40/40]); definitions and examples of microaggressions (97.50% [39/40]); definition, background, and types of bias (97.50% [39/40]); manifestations of bias in the clinical setting (97.44% [38/39]); racial and ethnic disparities in dermatology (97.44% [38/39]); keloids (97.37% [37/38]); differences in dermoscopic presentations in skin of color (97.30% [36/37]); skin cancer in patients with skin of color (97.30% [36/37]); disparities due to bias (95.00% [38/40]); how to apply cultural humility and safety to patients of different cultural backgrounds (94.87% [37/40]); best practices in providing care to patients with limited English proficiency (94.87% [37/40]); hair loss in patients with textured hair (94.74% [36/38]); pseudofolliculitis barbae and acne keloidalis nuchae (94.60% [35/37]); disparities regarding people experiencing homelessness (92.31% [36/39]); and definitions and types of racism and other forms of discrimination (92.31% [36/39]). eTable 1 provides a list of suggested resources to incorporate these topics into the educational components of residency curricula. The resources provided were not part of the voting process, and they were not considered in the consensus analysis; they are included here as suggested educational catalysts.
During the second round of voting, 25 topics were evaluated. Of those, the following 6 topics were proposed to be included as essential in residency training: differences in prevalence and presentation of common inflammatory disorders (100% [29/29]); manifestations of bias in the learning environment (96.55%); antiracist action and how to decrease the effects of structural racism in clinical and educational settings (96.55% [28/29]); diversity of images in dermatology education (96.55% [28/29]); pigmentary disorders and their psychological effects (96.55% [28/29]); and LGBTQ (lesbian, gay, bisexual, transgender, and queer) dermatologic health care (96.55% [28/29]). eTable 2 includes these topics as well as suggested resources to help incorporate them into training.
Comment
This study utilized a modified e-Delphi technique to identify relevant clinical and nonclinical DEI topics that should be incorporated into dermatology residency curricula. The panel members reached a consensus for 9 clinical DEI-related topics. The respondents agreed that the topics related to skin and hair conditions in patients with skin of color as well as textured hair were crucial to residency education. Skin cancer, hair loss, pseudofolliculitis barbae, acne keloidalis nuchae, keloids, pigmentary disorders, and their varying presentations in patients with skin of color were among the recommended topics. The panel also recommended educating residents on the variable visual presentations of inflammatory conditions in skin of color. Addressing the needs of diverse patients—for example, those belonging to the LGBTQ community—also was deemed important for inclusion.
The remaining 14 chosen topics were nonclinical items addressing concepts such as bias and health care disparities as well as cultural humility and safety.9 Cultural humility and safety focus on developing cultural awareness by creating a safe setting for patients rather than encouraging power relationships between them and their physicians. Various topics related to racism also were recommended to be included in residency curricula, including education on implementation of antiracist action in the workplace.
Many of the nonclinical topics are intertwined; for instance, learning about health care disparities in patients with limited English proficiency allows for improved best practices in delivering care to patients from this population. The first step in overcoming bias and subsequent disparities is acknowledging how the perpetuation of bias leads to disparities after being taught tools to recognize it.
Our group’s guidance on DEI topics should help dermatology residency program leaders as they design and refine program curricula. There are multiple avenues for incorporating education on these topics, including lectures, interactive workshops, role-playing sessions, book or journal clubs, and discussion circles. Many of these topics/programs may already be included in programs’ didactic curricula, which would minimize the burden of finding space to educate on these topics. Institutional cultural change is key to ensuring truly diverse, equitable, and inclusive workplaces. Educating tomorrow’s dermatologists on these topics is a first step toward achieving that cultural change.
Limitations—A limitation of this e-Delphi survey is that only a selection of experts in this field was included. Additionally, we were concerned that the Likert scale format and the bar we set for inclusion and exclusion may have failed to adequately capture participants’ nuanced opinions. As such, participants were able to provide open-ended feedback, and suggestions for alternate wording or other changes were considered by the steering committee. Finally, inclusion recommendations identified in this survey were developed specifically for US dermatology residents.
Conclusion
In this e-Delphi consensus assessment of DEI-related topics, we recommend the inclusion of 23 topics into dermatology residency program curricula to improve medical training and the patient-physician relationship as well as to create better health outcomes. We also provide specific sample resource recommendations in eTables 1 and 2 to facilitate inclusion of these topics into residency curricula across the country.
Diversity, equity, and inclusion (DEI) programs seek to improve dermatologic education and clinical care for an increasingly diverse patient population as well as to recruit and sustain a physician workforce that reflects the diversity of the patients they serve.1,2 In dermatology, only 4.2% and 3.0% of practicing dermatologists self-identify as being of Hispanic and African American ethnicity, respectively, compared with 18.5% and 13.4% of the general population, respectively.3 Creating an educational system that works to meet the goals of DEI is essential to improve health outcomes and address disparities. The lack of robust DEI-related curricula during residency training may limit the ability of practicing dermatologists to provide comprehensive and culturally sensitive care. It has been shown that racial concordance between patients and physicians has a positive impact on patient satisfaction by fostering a trusting patient-physician relationship.4
It is the responsibility of all dermatologists to create an environment where patients from any background can feel comfortable, which can be cultivated by establishing patient-centered communication and cultural humility.5 These skills can be strengthened via the implementation of DEI-related curricula during residency training. Augmenting exposure of these topics during training can optimize the delivery of dermatologic care by providing residents with the tools and confidence needed to care for patients of culturally diverse backgrounds. Enhancing DEI education is crucial to not only improve the recognition and treatment of dermatologic conditions in all skin and hair types but also to minimize misconceptions, stigma, health disparities, and discrimination faced by historically marginalized communities. Creating a culture of inclusion is of paramount importance to build successful relationships with patients and colleagues of culturally diverse backgrounds.6
There are multiple efforts underway to increase DEI education across the field of dermatology, including the development of DEI task forces in professional organizations and societies that serve to expand DEI-related research, mentorship, and education. The American Academy of Dermatology has been leading efforts to create a curriculum focused on skin of color, particularly addressing inadequate educational training on how dermatologic conditions manifest in this population.7 The Skin of Color Society has similar efforts underway and is developing a speakers bureau to give leading experts a platform to lecture dermatology trainees as well as patient and community audiences on various topics in skin of color.8 These are just 2 of many professional dermatology organizations that are advocating for expanded education on DEI; however, consistently integrating DEI-related topics into dermatology residency training curricula remains a gap in pedagogy. To identify the DEI-related topics of greatest relevance to the dermatology resident curricula, we implemented a modified electronic Delphi (e-Delphi) consensus process to provide standardized recommendations.
Methods
A 2-round modified e-Delphi method was utilized (Figure). An initial list of potential curricular topics was formulated by an expert panel consisting of 5 dermatologists from the Association of Professors of Dermatology DEI subcommittee and the American Academy of Dermatology Diversity Task Force (A.M.A., S.B., R.V., S.D.W., J.I.S.). Initial topics were selected via several meetings among the panel members to discuss existing DEI concerns and issues that were deemed relevant due to education gaps in residency training. The list of topics was further expanded with recommendations obtained via an email sent to dermatology program directors on the Association of Professors of Dermatology listserve, which solicited voluntary participation of academic dermatologists, including program directors and dermatology residents.
There were 2 voting rounds, with each round consisting of questions scored on a Likert scale ranging from 1 to 5 (1=not essential, 2=probably not essential, 3=neutral, 4=probably essential, 5=definitely essential). The inclusion criteria to classify a topic as necessary for integration into the dermatology residency curriculum included 95% (18/19) or more of respondents rating the topic as probably essential or definitely essential; if more than 90% (17/19) of respondents rated the topic as probably essential or definitely essential and less than 10% (2/19) rated it as not essential or probably not essential, the topic was still included as part of the suggested curriculum. Topics that received ratings of probably essential or definitely essential by less than 80% (15/19) of respondents were removed from consideration. The topics that did not meet inclusion or exclusion criteria during the first round of voting were refined by the e-Delphi steering committee (V.S.E-C. and F-A.R.) based on open-ended feedback from the voting group provided at the end of the survey and subsequently passed to the second round of voting.
Results
Participants—A total of 19 respondents participated in both voting rounds, the majority (80% [15/19]) of whom were program directors or dermatologists affiliated with academia or development of DEI education; the remaining 20% [4/19]) were dermatology residents.
Open-Ended Feedback—Voting group members were able to provide open-ended feedback for each of the sets of topics after the survey, which the steering committee utilized to modify the topics as needed for the final voting round. For example, “structural racism/discrimination” was originally mentioned as a topic, but several participants suggested including specific types of racism; therefore, the wording was changed to “racism: types, definitions” to encompass broader definitions and types of racism.
Survey Results—Two genres of topics were surveyed in each voting round: clinical and nonclinical. Participants voted on a total of 61 topics, with 23 ultimately selected in the final list of consensus curricular topics. Of those, 9 were clinical and 14 nonclinical. All topics deemed necessary for inclusion in residency curricula are presented in eTables 1 and 2.
During the first round of voting, the e-Delphi panel reached a consensus to include the following 17 topics as essential to dermatology residency training (along with the percentage of voters who classified them as probably essential or definitely essential): how to mitigate bias in clinical and workplace settings (100% [40/40]); social determinants of health-related disparities in dermatology (100% [40/40]); hairstyling practices across different hair textures (100% [40/40]); definitions and examples of microaggressions (97.50% [39/40]); definition, background, and types of bias (97.50% [39/40]); manifestations of bias in the clinical setting (97.44% [38/39]); racial and ethnic disparities in dermatology (97.44% [38/39]); keloids (97.37% [37/38]); differences in dermoscopic presentations in skin of color (97.30% [36/37]); skin cancer in patients with skin of color (97.30% [36/37]); disparities due to bias (95.00% [38/40]); how to apply cultural humility and safety to patients of different cultural backgrounds (94.87% [37/40]); best practices in providing care to patients with limited English proficiency (94.87% [37/40]); hair loss in patients with textured hair (94.74% [36/38]); pseudofolliculitis barbae and acne keloidalis nuchae (94.60% [35/37]); disparities regarding people experiencing homelessness (92.31% [36/39]); and definitions and types of racism and other forms of discrimination (92.31% [36/39]). eTable 1 provides a list of suggested resources to incorporate these topics into the educational components of residency curricula. The resources provided were not part of the voting process, and they were not considered in the consensus analysis; they are included here as suggested educational catalysts.
During the second round of voting, 25 topics were evaluated. Of those, the following 6 topics were proposed to be included as essential in residency training: differences in prevalence and presentation of common inflammatory disorders (100% [29/29]); manifestations of bias in the learning environment (96.55%); antiracist action and how to decrease the effects of structural racism in clinical and educational settings (96.55% [28/29]); diversity of images in dermatology education (96.55% [28/29]); pigmentary disorders and their psychological effects (96.55% [28/29]); and LGBTQ (lesbian, gay, bisexual, transgender, and queer) dermatologic health care (96.55% [28/29]). eTable 2 includes these topics as well as suggested resources to help incorporate them into training.
Comment
This study utilized a modified e-Delphi technique to identify relevant clinical and nonclinical DEI topics that should be incorporated into dermatology residency curricula. The panel members reached a consensus for 9 clinical DEI-related topics. The respondents agreed that the topics related to skin and hair conditions in patients with skin of color as well as textured hair were crucial to residency education. Skin cancer, hair loss, pseudofolliculitis barbae, acne keloidalis nuchae, keloids, pigmentary disorders, and their varying presentations in patients with skin of color were among the recommended topics. The panel also recommended educating residents on the variable visual presentations of inflammatory conditions in skin of color. Addressing the needs of diverse patients—for example, those belonging to the LGBTQ community—also was deemed important for inclusion.
The remaining 14 chosen topics were nonclinical items addressing concepts such as bias and health care disparities as well as cultural humility and safety.9 Cultural humility and safety focus on developing cultural awareness by creating a safe setting for patients rather than encouraging power relationships between them and their physicians. Various topics related to racism also were recommended to be included in residency curricula, including education on implementation of antiracist action in the workplace.
Many of the nonclinical topics are intertwined; for instance, learning about health care disparities in patients with limited English proficiency allows for improved best practices in delivering care to patients from this population. The first step in overcoming bias and subsequent disparities is acknowledging how the perpetuation of bias leads to disparities after being taught tools to recognize it.
Our group’s guidance on DEI topics should help dermatology residency program leaders as they design and refine program curricula. There are multiple avenues for incorporating education on these topics, including lectures, interactive workshops, role-playing sessions, book or journal clubs, and discussion circles. Many of these topics/programs may already be included in programs’ didactic curricula, which would minimize the burden of finding space to educate on these topics. Institutional cultural change is key to ensuring truly diverse, equitable, and inclusive workplaces. Educating tomorrow’s dermatologists on these topics is a first step toward achieving that cultural change.
Limitations—A limitation of this e-Delphi survey is that only a selection of experts in this field was included. Additionally, we were concerned that the Likert scale format and the bar we set for inclusion and exclusion may have failed to adequately capture participants’ nuanced opinions. As such, participants were able to provide open-ended feedback, and suggestions for alternate wording or other changes were considered by the steering committee. Finally, inclusion recommendations identified in this survey were developed specifically for US dermatology residents.
Conclusion
In this e-Delphi consensus assessment of DEI-related topics, we recommend the inclusion of 23 topics into dermatology residency program curricula to improve medical training and the patient-physician relationship as well as to create better health outcomes. We also provide specific sample resource recommendations in eTables 1 and 2 to facilitate inclusion of these topics into residency curricula across the country.
- US Census Bureau projections show a slower growing, older, more diverse nation a half century from now. News release. US Census Bureau. December 12, 2012. Accessed August 14, 2024. https://www.census.gov/newsroom/releases/archives/population/cb12243.html#:~:text=12%2C%202012,U.S.%20Census%20Bureau%20Projections%20Show%20a%20Slower%20Growing%2C%20Older%2C%20More,by%20the%20U.S.%20Census%20Bureau
- Lopez S, Lourido JO, Lim HW, et al. The call to action to increase racial and ethnic diversity in dermatology: a retrospective, cross-sectional study to monitor progress. J Am Acad Dermatol. 2020;86:E121-E123. doi:10.1016/j.jaad.2021.10.011
- El-Kashlan N, Alexis A. Disparities in dermatology: a reflection. J Clin Aesthet Dermatol. 2022;15:27-29.
- Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43:296-306.
- Street RL Jr, O’Malley KJ, Cooper LA, et al. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6:198-205. doi:10.1370/afm.821
- Dadrass F, Bowers S, Shinkai K, et al. Diversity, equity, and inclusion in dermatology residency. Dermatol Clin. 2023;41:257-263. doi:10.1016/j.det.2022.10.006
- Diversity and the Academy. American Academy of Dermatology website. Accessed August 22, 2024. https://www.aad.org/member/career/diversity
- SOCS speaks. Skin of Color Society website. Accessed August 22, 2024. https://skinofcolorsociety.org/news-media/socs-speaks
- Solchanyk D, Ekeh O, Saffran L, et al. Integrating cultural humility into the medical education curriculum: strategies for educators. Teach Learn Med. 2021;33:554-560. doi:10.1080/10401334.2021.1877711
- US Census Bureau projections show a slower growing, older, more diverse nation a half century from now. News release. US Census Bureau. December 12, 2012. Accessed August 14, 2024. https://www.census.gov/newsroom/releases/archives/population/cb12243.html#:~:text=12%2C%202012,U.S.%20Census%20Bureau%20Projections%20Show%20a%20Slower%20Growing%2C%20Older%2C%20More,by%20the%20U.S.%20Census%20Bureau
- Lopez S, Lourido JO, Lim HW, et al. The call to action to increase racial and ethnic diversity in dermatology: a retrospective, cross-sectional study to monitor progress. J Am Acad Dermatol. 2020;86:E121-E123. doi:10.1016/j.jaad.2021.10.011
- El-Kashlan N, Alexis A. Disparities in dermatology: a reflection. J Clin Aesthet Dermatol. 2022;15:27-29.
- Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43:296-306.
- Street RL Jr, O’Malley KJ, Cooper LA, et al. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6:198-205. doi:10.1370/afm.821
- Dadrass F, Bowers S, Shinkai K, et al. Diversity, equity, and inclusion in dermatology residency. Dermatol Clin. 2023;41:257-263. doi:10.1016/j.det.2022.10.006
- Diversity and the Academy. American Academy of Dermatology website. Accessed August 22, 2024. https://www.aad.org/member/career/diversity
- SOCS speaks. Skin of Color Society website. Accessed August 22, 2024. https://skinofcolorsociety.org/news-media/socs-speaks
- Solchanyk D, Ekeh O, Saffran L, et al. Integrating cultural humility into the medical education curriculum: strategies for educators. Teach Learn Med. 2021;33:554-560. doi:10.1080/10401334.2021.1877711
PRACTICE POINTS
- Advancing curricula related to diversity, equity, and inclusion in dermatology training can improve health outcomes, address health care workforce disparities, and enhance clinical care for diverse patient populations.
- Education on patient-centered communication, cultural humility, and the impact of social determinants of health results in dermatology residents who are better equipped with the necessary tools to effectively care for patients from diverse backgrounds.
Improving Diagnostic Accuracy in Skin of Color Using an Educational Module
Dermatologic disparities disproportionately affect patients with skin of color (SOC). Two studies assessing the diagnostic accuracy of medical students have shown disparities in diagnosing common skin conditions presenting in darker skin compared to lighter skin at early stages of training.1,2 This knowledge gap could be attributed to the underrepresentation of SOC in dermatologic textbooks, journals, and educational curricula.3-6 It is important for dermatologists as well as physicians in other specialties and ancillary health care workers involved in treating or triaging dermatologic diseases to recognize common skin conditions presenting in SOC. We sought to evaluate the effectiveness of a focused educational module for improving diagnostic accuracy and confidence in treating SOC among interprofessional health care providers.
Methods
Interprofessional health care providers—medical students, residents/fellows, attending physicians, advanced practice providers (APPs), and nurses practicing across various medical specialties—at The University of Texas at Austin Dell Medical School and Ascension Medical Group (both in Austin, Texas) were invited to participate in an institutional review board–exempt study involving a virtual SOC educational module from February through May 2021. The 1-hour module involved a pretest, a 15-minute lecture, an immediate posttest, and a 3-month posttest. All tests included the same 40 multiple-choice questions of 20 dermatologic conditions portrayed in lighter and darker skin types from VisualDx.com, and participants were asked to identify the condition in each photograph. Questions appeared one at a time in a randomized order, and answers could not be changed once submitted.
For analysis, the dermatologic conditions were categorized into 4 groups: cancerous, infectious, inflammatory, and SOC-associated conditions. Cancerous conditions included basal cell carcinoma, squamous cell carcinoma, and melanoma. Infectious conditions included herpes zoster, tinea corporis, tinea versicolor, staphylococcal scalded skin syndrome, and verruca vulgaris. Inflammatory conditions included acne, atopic dermatitis, pityriasis rosea, psoriasis, seborrheic dermatitis, contact dermatitis, lichen planus, and urticaria. Skin of color–associated conditions included hidradenitis suppurativa, acanthosis nigricans, keloid, and melasma. Two questions utilizing a 5-point Likert scale assessing confidence in diagnosing light and dark skin also were included.
The pre-recorded 15-minute video lecture was given by 2 dermatology residents (P.L.K. and C.P.), and the learning objectives covered morphologic differences in lighter skin and darker skin, comparisons of common dermatologic diseases in lighter skin and darker skin, diseases more commonly affecting patients with SOC, and treatment considerations for conditions affecting skin and hair in patients with SOC. Photographs from the diagnostic accuracy assessment were not reused in the lecture. Detailed explanations on morphology, diagnostic pearls, and treatment options for all conditions tested were provided to participants upon completion of the 3-month posttest.
Statistical Analysis—Test scores were compared between conditions shown in lighter and darker skin types and from the pretest to the immediate posttest and 3-month posttest. Multiple linear regression was used to assess for intervention effects on lighter and darker skin scores controlling for provider type and specialty. All tests were 2-sided with significance at P<.05. Analyses were conducted using Stata 17.
Results
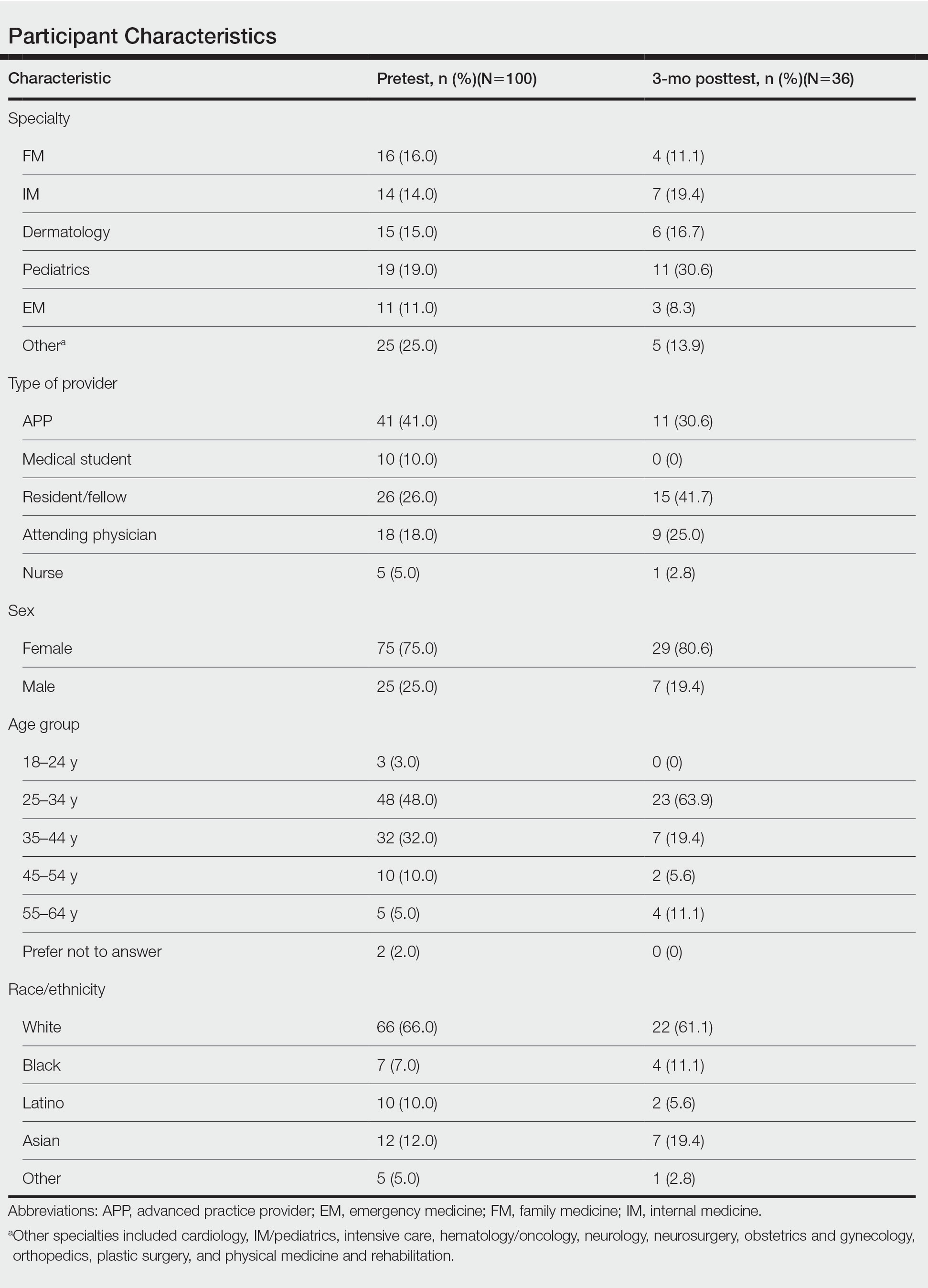
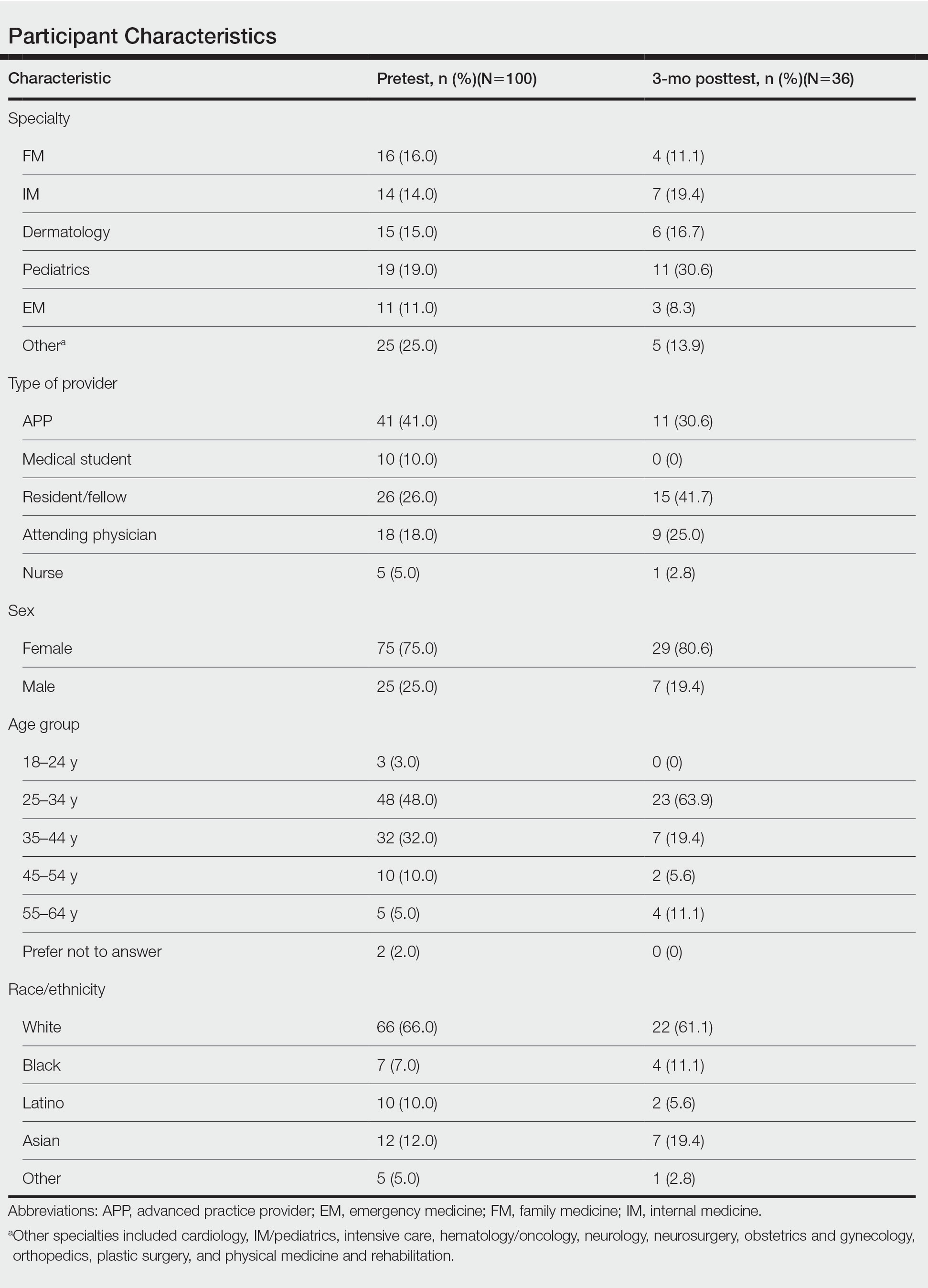
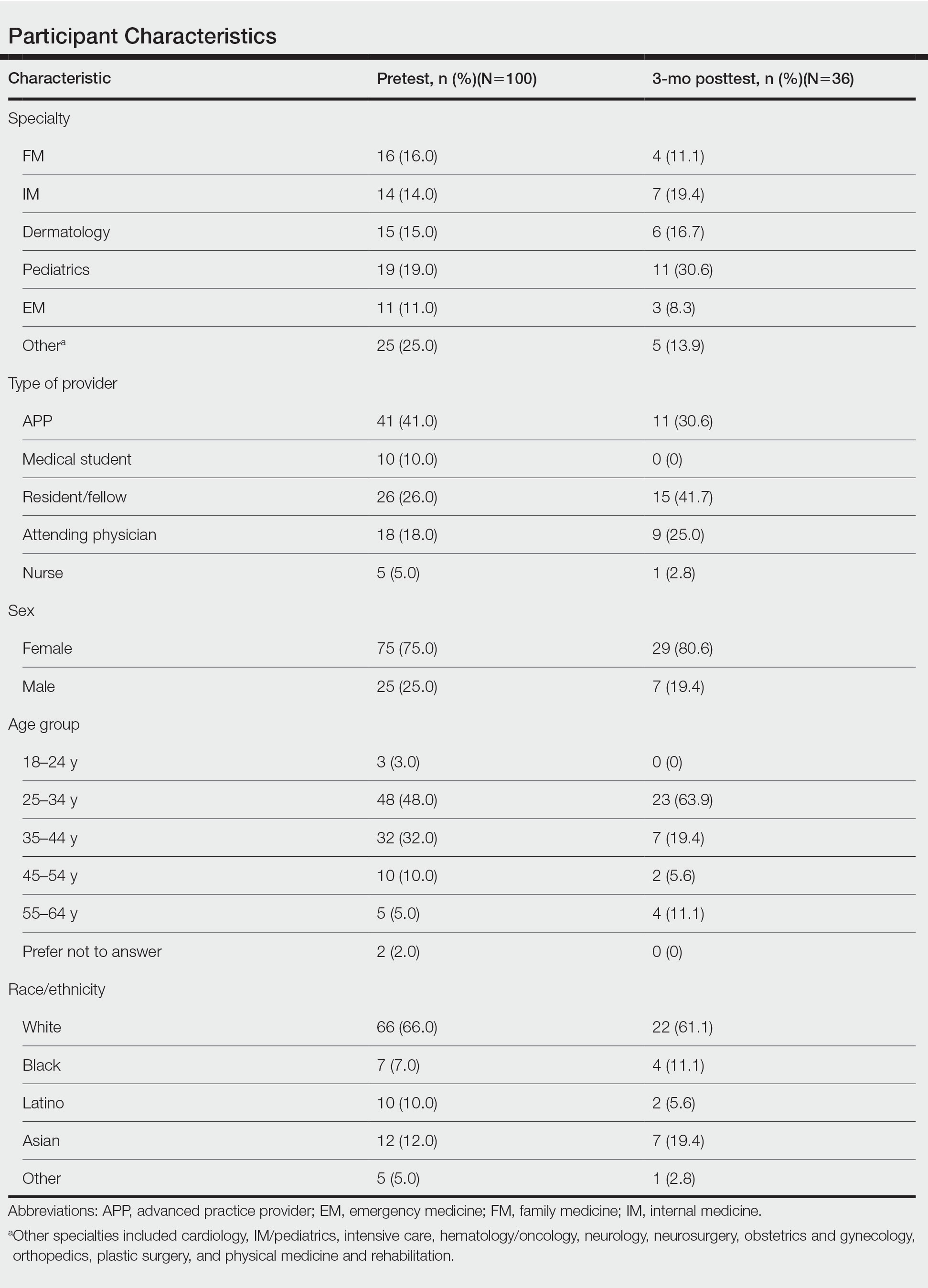
One hundred participants completed the pretest and immediate posttest, 36 of whom also completed the 3-month posttest (Table). There was no significant difference in baseline characteristics between the pretest and 3-month posttest groups.
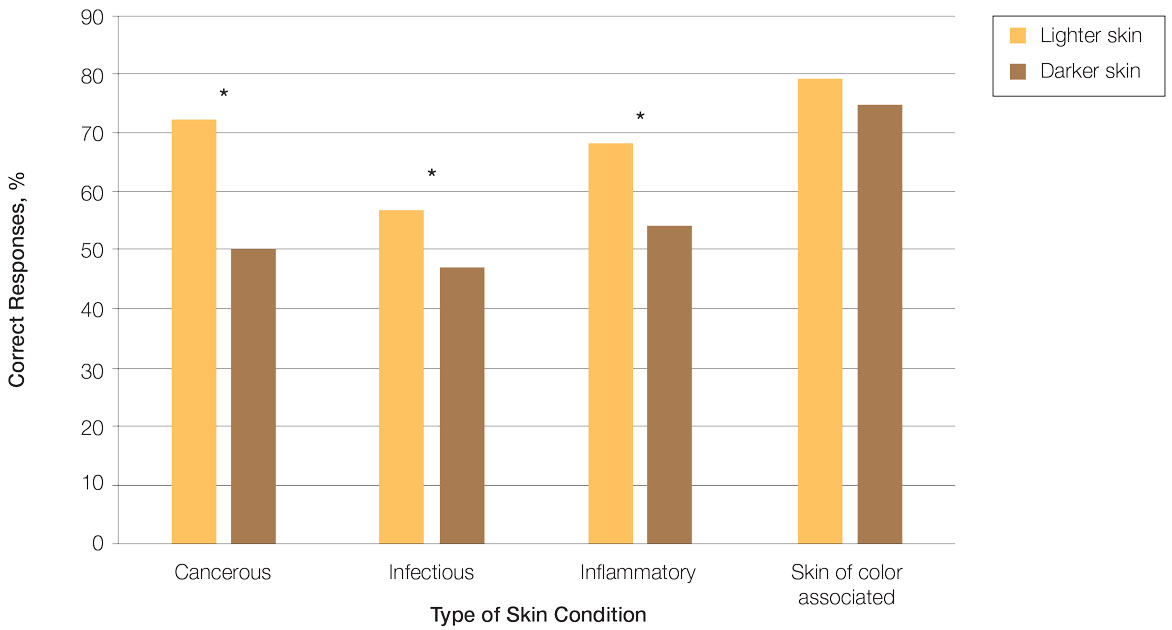
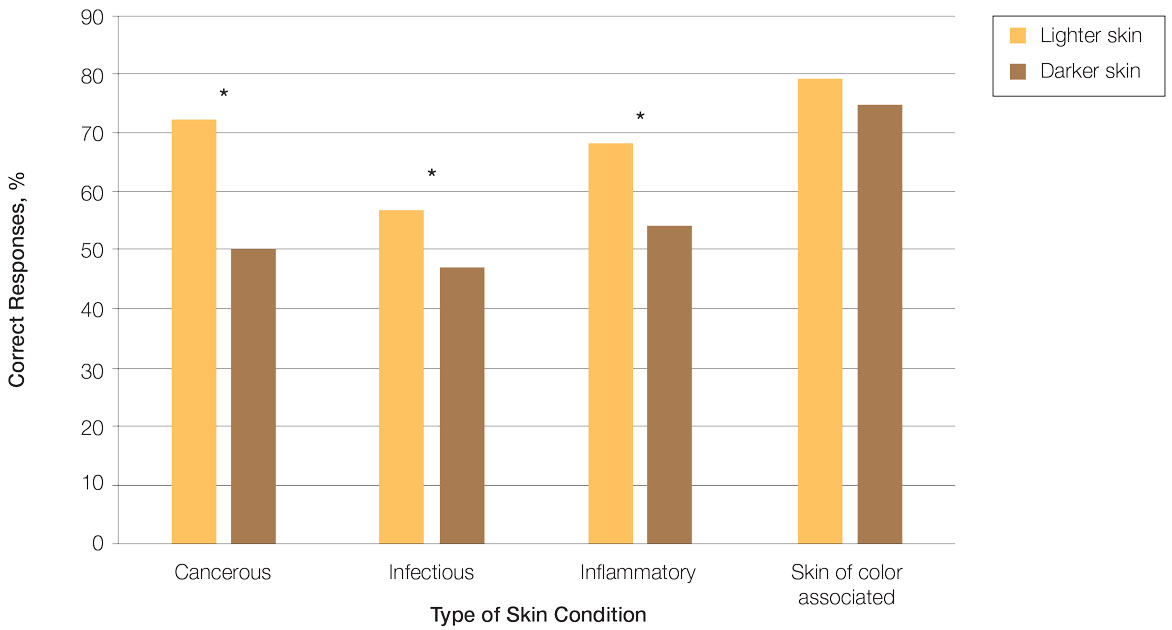
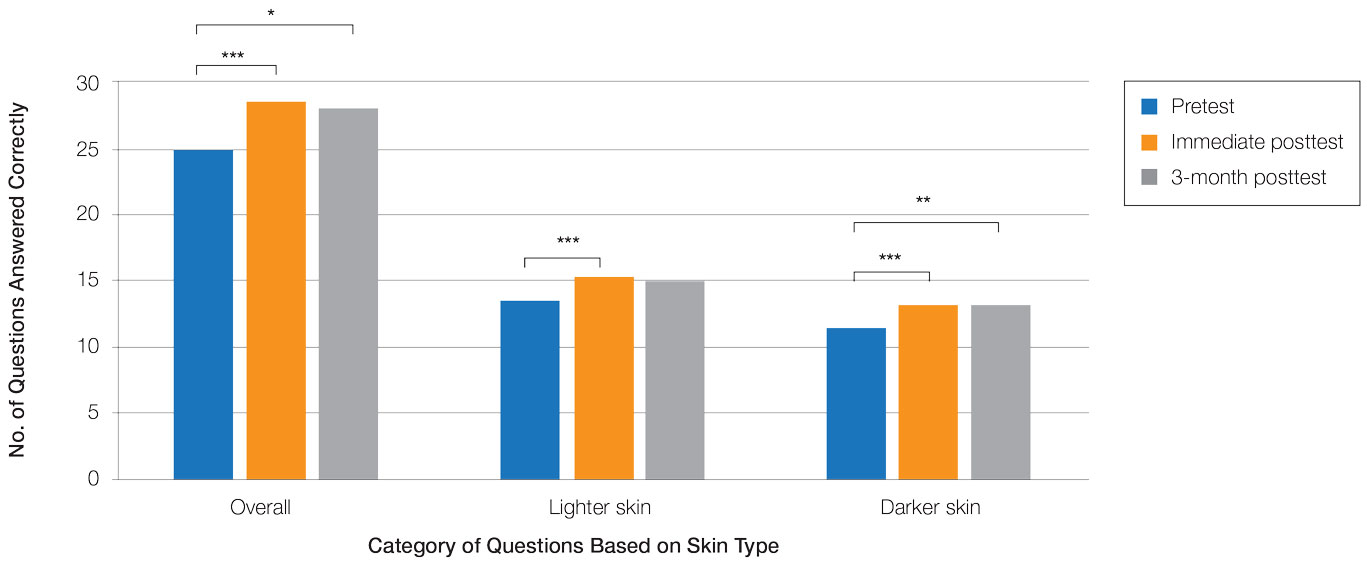
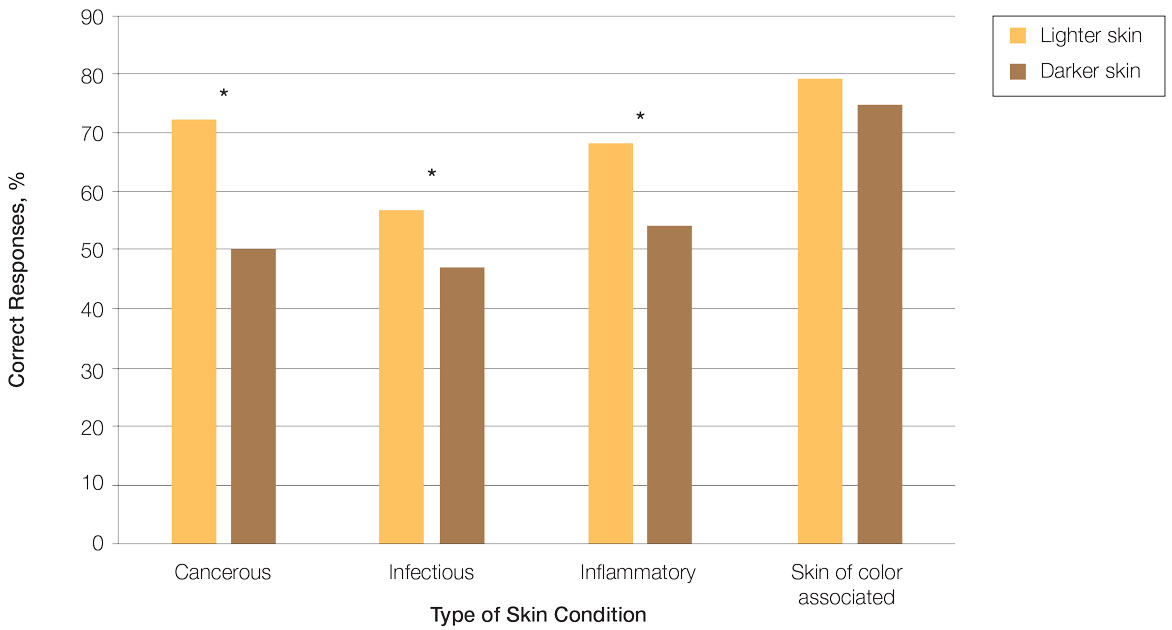
Test scores were correlated with provider type and specialty but not age, sex, or race/ethnicity. Specializing in dermatology and being a resident or attending physician were independently associated with higher test scores. Mean pretest diagnostic accuracy and confidence scores were higher for skin conditions shown in lighter skin compared with those shown in darker skin (13.6 vs 11.3 and 2.7 vs 1.9, respectively; both P<.001). Pretest diagnostic accuracy was significantly higher for skin conditions shown in lighter skin compared with darker skin for cancerous, inflammatory, and infectious conditions (72% vs 50%, 68% vs 55%, and 57% vs 47%, respectively; P<.001 for all)(Figure 1). Skin of color–associated conditions were not associated with significantly different scores for lighter skin compared with darker skin (79% vs 75%; P=.059).
Controlling for provider type and specialty, significantly improved diagnostic accuracy was seen in immediate posttest scores compared with pretest scores for conditions shown in both lighter and darker skin types (lighter: 15.2 vs 13.6; darker: 13.3 vs 11.3; both P<.001)(Figure 2). The immediate posttest demonstrated higher mean diagnostic accuracy and confidence scores for skin conditions shown in lighter skin compared with darker skin (diagnostic accuracy: 15.2 vs 13.3; confidence: 3.0 vs 2.6; both P<.001), but the disparity between scores was less than in the pretest.
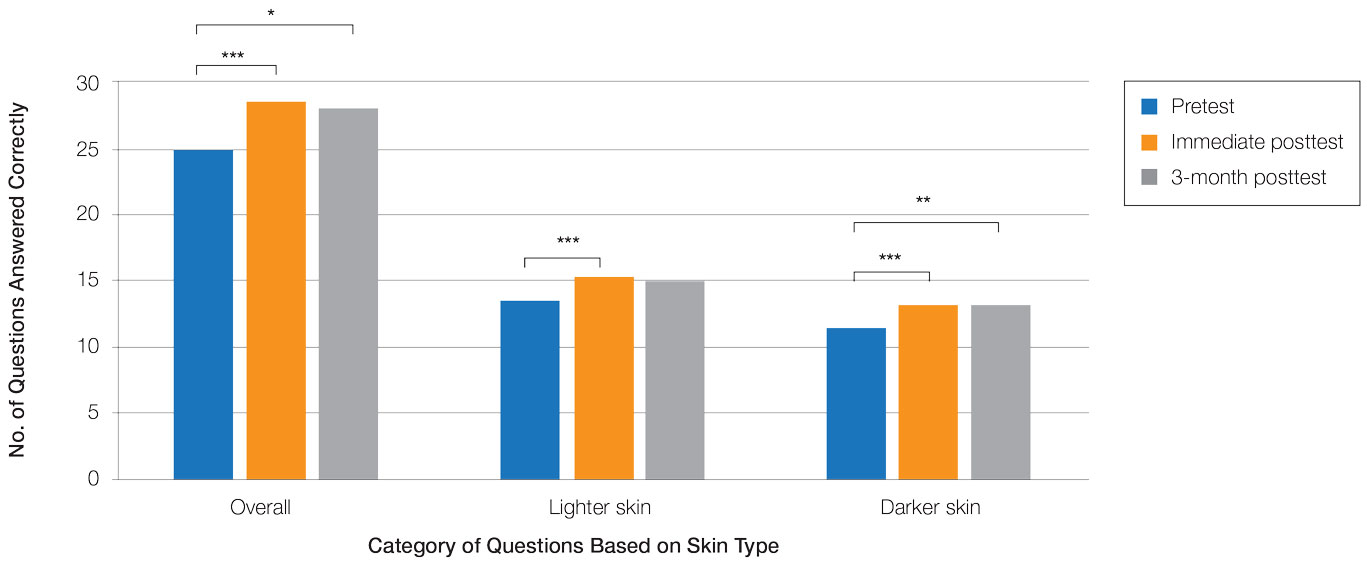
Following the 3-month posttest, improvement in diagnostic accuracy was noted among both lighter and darker skin types compared with the pretest, but the difference remained significant only for conditions shown in darker skin (mean scores, 11.3 vs 13.3; P<.01). Similarly, confidence in diagnosing conditions in both lighter and darker skin improved following the immediate posttest (mean scores, 2.7 vs 3.0 and 1.9 vs 2.6; both P<.001), and this improvement remained significant for only darker skin following the 3-month posttest (mean scores, 1.9 vs 2.3; P<.001). Despite these improvements, diagnostic accuracy and confidence remained higher for skin conditions shown in lighter skin compared with darker skin (diagnostic accuracy: 14.7 vs 13.3; P<.01; confidence: 2.8 vs 2.3; P<.001), though the disparity between scores was again less than in the pretest.
Comment
Our study showed that there are diagnostic disparities between lighter and darker skin types among interprofessional health care providers. Education on SOC should extend to interprofessional health care providers and other medical specialties involved in treating or triaging dermatologic diseases. A focused educational module may provide long-term improvements in diagnostic accuracy and confidence for conditions presenting in SOC. Differences in diagnostic accuracy between conditions shown in lighter and darker skin types were noted for the disease categories of infectious, cancerous, and inflammatory conditions, with the exception of conditions more frequently seen in patients with SOC. Learning resources for SOC-associated conditions are more likely to have greater representation of images depicting darker skin types.7 Future educational interventions may need to focus on dermatologic conditions that are not preferentially seen in patients with SOC. In our study, the pretest scores for conditions shown in darker skin were lowest among infectious and cancerous conditions. For infections, certain morphologic clues such as erythema are important for diagnosis but may be more subtle or difficult to discern in darker skin. It also is possible that providers may be less likely to suspect skin cancer in patients with SOC given that the morphologic presentation and/or anatomic site of involvement for skin cancers in SOC differs from those in lighter skin. Future educational interventions targeting disparities in diagnostic accuracy should focus on conditions that are not specifically associated with SOC.
Limitations of our study included the small number of participants, the study population came from a single institution, and a possible selection bias for providers interested in dermatology.
Conclusion
Disparities exist among interprofessional health care providers when treating conditions in patients with lighter skin compared to darker skin. An educational module for health care providers may provide long-term improvements in diagnostic accuracy and confidence for conditions presenting in patients with SOC.
- Fenton A, Elliott E, Shahbandi A, et al. Medical students’ ability to diagnose common dermatologic conditions in skin of color. J Am Acad Dermatol. 2020;83:957-958. doi:10.1016/j.jaad.2019.12.078
- Mamo A, Szeto MD, Rietcheck H, et al. Evaluating medical student assessment of common dermatologic conditions across Fitzpatrick phototypes and skin of color. J Am Acad Dermatol. 2022;87:167-169. doi:10.1016/j.jaad.2021.06.868
- Guda VA, Paek SY. Skin of color representation in commonly utilized medical student dermatology resources. J Drugs Dermatol. 2021;20:799. doi:10.36849/JDD.5726
- Wilson BN, Sun M, Ashbaugh AG, et al. Assessment of skin of color and diversity and inclusion content of dermatologic published literature: an analysis and call to action. Int J Womens Dermatol. 2021;7:391-397. doi:10.1016/j.ijwd.2021.04.001
- Ibraheim MK, Gupta R, Dao H, et al. Evaluating skin of color education in dermatology residency programs: data from a national survey. Clin Dermatol. 2022;40:228-233. doi:10.1016/j.clindermatol.2021.11.015
- Gupta R, Ibraheim MK, Dao H Jr, et al. Assessing dermatology resident confidence in caring for patients with skin of color. Clin Dermatol. 2021;39:873-878. doi:10.1016/j.clindermatol.2021.08.019
- Chang MJ, Lipner SR. Analysis of skin color on the American Academy of Dermatology public education website. J Drugs Dermatol. 2020;19:1236-1237. doi:10.36849/JDD.2020.5545
Dermatologic disparities disproportionately affect patients with skin of color (SOC). Two studies assessing the diagnostic accuracy of medical students have shown disparities in diagnosing common skin conditions presenting in darker skin compared to lighter skin at early stages of training.1,2 This knowledge gap could be attributed to the underrepresentation of SOC in dermatologic textbooks, journals, and educational curricula.3-6 It is important for dermatologists as well as physicians in other specialties and ancillary health care workers involved in treating or triaging dermatologic diseases to recognize common skin conditions presenting in SOC. We sought to evaluate the effectiveness of a focused educational module for improving diagnostic accuracy and confidence in treating SOC among interprofessional health care providers.
Methods
Interprofessional health care providers—medical students, residents/fellows, attending physicians, advanced practice providers (APPs), and nurses practicing across various medical specialties—at The University of Texas at Austin Dell Medical School and Ascension Medical Group (both in Austin, Texas) were invited to participate in an institutional review board–exempt study involving a virtual SOC educational module from February through May 2021. The 1-hour module involved a pretest, a 15-minute lecture, an immediate posttest, and a 3-month posttest. All tests included the same 40 multiple-choice questions of 20 dermatologic conditions portrayed in lighter and darker skin types from VisualDx.com, and participants were asked to identify the condition in each photograph. Questions appeared one at a time in a randomized order, and answers could not be changed once submitted.
For analysis, the dermatologic conditions were categorized into 4 groups: cancerous, infectious, inflammatory, and SOC-associated conditions. Cancerous conditions included basal cell carcinoma, squamous cell carcinoma, and melanoma. Infectious conditions included herpes zoster, tinea corporis, tinea versicolor, staphylococcal scalded skin syndrome, and verruca vulgaris. Inflammatory conditions included acne, atopic dermatitis, pityriasis rosea, psoriasis, seborrheic dermatitis, contact dermatitis, lichen planus, and urticaria. Skin of color–associated conditions included hidradenitis suppurativa, acanthosis nigricans, keloid, and melasma. Two questions utilizing a 5-point Likert scale assessing confidence in diagnosing light and dark skin also were included.
The pre-recorded 15-minute video lecture was given by 2 dermatology residents (P.L.K. and C.P.), and the learning objectives covered morphologic differences in lighter skin and darker skin, comparisons of common dermatologic diseases in lighter skin and darker skin, diseases more commonly affecting patients with SOC, and treatment considerations for conditions affecting skin and hair in patients with SOC. Photographs from the diagnostic accuracy assessment were not reused in the lecture. Detailed explanations on morphology, diagnostic pearls, and treatment options for all conditions tested were provided to participants upon completion of the 3-month posttest.
Statistical Analysis—Test scores were compared between conditions shown in lighter and darker skin types and from the pretest to the immediate posttest and 3-month posttest. Multiple linear regression was used to assess for intervention effects on lighter and darker skin scores controlling for provider type and specialty. All tests were 2-sided with significance at P<.05. Analyses were conducted using Stata 17.
Results
One hundred participants completed the pretest and immediate posttest, 36 of whom also completed the 3-month posttest (Table). There was no significant difference in baseline characteristics between the pretest and 3-month posttest groups.
Test scores were correlated with provider type and specialty but not age, sex, or race/ethnicity. Specializing in dermatology and being a resident or attending physician were independently associated with higher test scores. Mean pretest diagnostic accuracy and confidence scores were higher for skin conditions shown in lighter skin compared with those shown in darker skin (13.6 vs 11.3 and 2.7 vs 1.9, respectively; both P<.001). Pretest diagnostic accuracy was significantly higher for skin conditions shown in lighter skin compared with darker skin for cancerous, inflammatory, and infectious conditions (72% vs 50%, 68% vs 55%, and 57% vs 47%, respectively; P<.001 for all)(Figure 1). Skin of color–associated conditions were not associated with significantly different scores for lighter skin compared with darker skin (79% vs 75%; P=.059).
Controlling for provider type and specialty, significantly improved diagnostic accuracy was seen in immediate posttest scores compared with pretest scores for conditions shown in both lighter and darker skin types (lighter: 15.2 vs 13.6; darker: 13.3 vs 11.3; both P<.001)(Figure 2). The immediate posttest demonstrated higher mean diagnostic accuracy and confidence scores for skin conditions shown in lighter skin compared with darker skin (diagnostic accuracy: 15.2 vs 13.3; confidence: 3.0 vs 2.6; both P<.001), but the disparity between scores was less than in the pretest.
Following the 3-month posttest, improvement in diagnostic accuracy was noted among both lighter and darker skin types compared with the pretest, but the difference remained significant only for conditions shown in darker skin (mean scores, 11.3 vs 13.3; P<.01). Similarly, confidence in diagnosing conditions in both lighter and darker skin improved following the immediate posttest (mean scores, 2.7 vs 3.0 and 1.9 vs 2.6; both P<.001), and this improvement remained significant for only darker skin following the 3-month posttest (mean scores, 1.9 vs 2.3; P<.001). Despite these improvements, diagnostic accuracy and confidence remained higher for skin conditions shown in lighter skin compared with darker skin (diagnostic accuracy: 14.7 vs 13.3; P<.01; confidence: 2.8 vs 2.3; P<.001), though the disparity between scores was again less than in the pretest.
Comment
Our study showed that there are diagnostic disparities between lighter and darker skin types among interprofessional health care providers. Education on SOC should extend to interprofessional health care providers and other medical specialties involved in treating or triaging dermatologic diseases. A focused educational module may provide long-term improvements in diagnostic accuracy and confidence for conditions presenting in SOC. Differences in diagnostic accuracy between conditions shown in lighter and darker skin types were noted for the disease categories of infectious, cancerous, and inflammatory conditions, with the exception of conditions more frequently seen in patients with SOC. Learning resources for SOC-associated conditions are more likely to have greater representation of images depicting darker skin types.7 Future educational interventions may need to focus on dermatologic conditions that are not preferentially seen in patients with SOC. In our study, the pretest scores for conditions shown in darker skin were lowest among infectious and cancerous conditions. For infections, certain morphologic clues such as erythema are important for diagnosis but may be more subtle or difficult to discern in darker skin. It also is possible that providers may be less likely to suspect skin cancer in patients with SOC given that the morphologic presentation and/or anatomic site of involvement for skin cancers in SOC differs from those in lighter skin. Future educational interventions targeting disparities in diagnostic accuracy should focus on conditions that are not specifically associated with SOC.
Limitations of our study included the small number of participants, the study population came from a single institution, and a possible selection bias for providers interested in dermatology.
Conclusion
Disparities exist among interprofessional health care providers when treating conditions in patients with lighter skin compared to darker skin. An educational module for health care providers may provide long-term improvements in diagnostic accuracy and confidence for conditions presenting in patients with SOC.
Dermatologic disparities disproportionately affect patients with skin of color (SOC). Two studies assessing the diagnostic accuracy of medical students have shown disparities in diagnosing common skin conditions presenting in darker skin compared to lighter skin at early stages of training.1,2 This knowledge gap could be attributed to the underrepresentation of SOC in dermatologic textbooks, journals, and educational curricula.3-6 It is important for dermatologists as well as physicians in other specialties and ancillary health care workers involved in treating or triaging dermatologic diseases to recognize common skin conditions presenting in SOC. We sought to evaluate the effectiveness of a focused educational module for improving diagnostic accuracy and confidence in treating SOC among interprofessional health care providers.
Methods
Interprofessional health care providers—medical students, residents/fellows, attending physicians, advanced practice providers (APPs), and nurses practicing across various medical specialties—at The University of Texas at Austin Dell Medical School and Ascension Medical Group (both in Austin, Texas) were invited to participate in an institutional review board–exempt study involving a virtual SOC educational module from February through May 2021. The 1-hour module involved a pretest, a 15-minute lecture, an immediate posttest, and a 3-month posttest. All tests included the same 40 multiple-choice questions of 20 dermatologic conditions portrayed in lighter and darker skin types from VisualDx.com, and participants were asked to identify the condition in each photograph. Questions appeared one at a time in a randomized order, and answers could not be changed once submitted.
For analysis, the dermatologic conditions were categorized into 4 groups: cancerous, infectious, inflammatory, and SOC-associated conditions. Cancerous conditions included basal cell carcinoma, squamous cell carcinoma, and melanoma. Infectious conditions included herpes zoster, tinea corporis, tinea versicolor, staphylococcal scalded skin syndrome, and verruca vulgaris. Inflammatory conditions included acne, atopic dermatitis, pityriasis rosea, psoriasis, seborrheic dermatitis, contact dermatitis, lichen planus, and urticaria. Skin of color–associated conditions included hidradenitis suppurativa, acanthosis nigricans, keloid, and melasma. Two questions utilizing a 5-point Likert scale assessing confidence in diagnosing light and dark skin also were included.
The pre-recorded 15-minute video lecture was given by 2 dermatology residents (P.L.K. and C.P.), and the learning objectives covered morphologic differences in lighter skin and darker skin, comparisons of common dermatologic diseases in lighter skin and darker skin, diseases more commonly affecting patients with SOC, and treatment considerations for conditions affecting skin and hair in patients with SOC. Photographs from the diagnostic accuracy assessment were not reused in the lecture. Detailed explanations on morphology, diagnostic pearls, and treatment options for all conditions tested were provided to participants upon completion of the 3-month posttest.
Statistical Analysis—Test scores were compared between conditions shown in lighter and darker skin types and from the pretest to the immediate posttest and 3-month posttest. Multiple linear regression was used to assess for intervention effects on lighter and darker skin scores controlling for provider type and specialty. All tests were 2-sided with significance at P<.05. Analyses were conducted using Stata 17.
Results
One hundred participants completed the pretest and immediate posttest, 36 of whom also completed the 3-month posttest (Table). There was no significant difference in baseline characteristics between the pretest and 3-month posttest groups.
Test scores were correlated with provider type and specialty but not age, sex, or race/ethnicity. Specializing in dermatology and being a resident or attending physician were independently associated with higher test scores. Mean pretest diagnostic accuracy and confidence scores were higher for skin conditions shown in lighter skin compared with those shown in darker skin (13.6 vs 11.3 and 2.7 vs 1.9, respectively; both P<.001). Pretest diagnostic accuracy was significantly higher for skin conditions shown in lighter skin compared with darker skin for cancerous, inflammatory, and infectious conditions (72% vs 50%, 68% vs 55%, and 57% vs 47%, respectively; P<.001 for all)(Figure 1). Skin of color–associated conditions were not associated with significantly different scores for lighter skin compared with darker skin (79% vs 75%; P=.059).
Controlling for provider type and specialty, significantly improved diagnostic accuracy was seen in immediate posttest scores compared with pretest scores for conditions shown in both lighter and darker skin types (lighter: 15.2 vs 13.6; darker: 13.3 vs 11.3; both P<.001)(Figure 2). The immediate posttest demonstrated higher mean diagnostic accuracy and confidence scores for skin conditions shown in lighter skin compared with darker skin (diagnostic accuracy: 15.2 vs 13.3; confidence: 3.0 vs 2.6; both P<.001), but the disparity between scores was less than in the pretest.
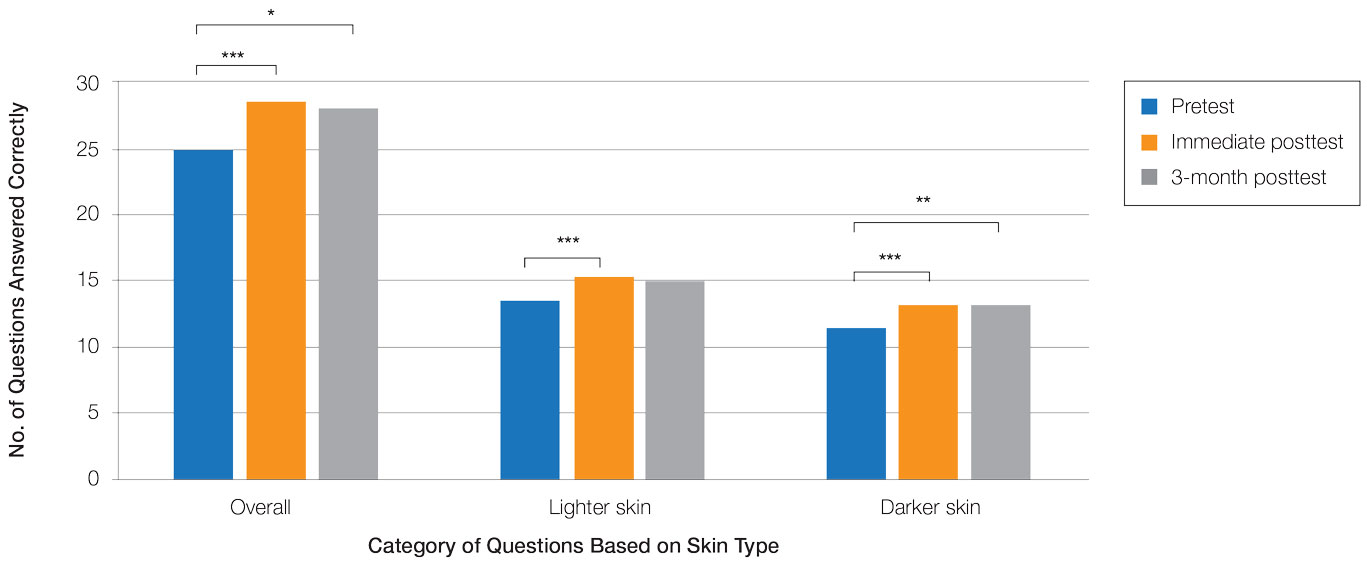
Following the 3-month posttest, improvement in diagnostic accuracy was noted among both lighter and darker skin types compared with the pretest, but the difference remained significant only for conditions shown in darker skin (mean scores, 11.3 vs 13.3; P<.01). Similarly, confidence in diagnosing conditions in both lighter and darker skin improved following the immediate posttest (mean scores, 2.7 vs 3.0 and 1.9 vs 2.6; both P<.001), and this improvement remained significant for only darker skin following the 3-month posttest (mean scores, 1.9 vs 2.3; P<.001). Despite these improvements, diagnostic accuracy and confidence remained higher for skin conditions shown in lighter skin compared with darker skin (diagnostic accuracy: 14.7 vs 13.3; P<.01; confidence: 2.8 vs 2.3; P<.001), though the disparity between scores was again less than in the pretest.
Comment
Our study showed that there are diagnostic disparities between lighter and darker skin types among interprofessional health care providers. Education on SOC should extend to interprofessional health care providers and other medical specialties involved in treating or triaging dermatologic diseases. A focused educational module may provide long-term improvements in diagnostic accuracy and confidence for conditions presenting in SOC. Differences in diagnostic accuracy between conditions shown in lighter and darker skin types were noted for the disease categories of infectious, cancerous, and inflammatory conditions, with the exception of conditions more frequently seen in patients with SOC. Learning resources for SOC-associated conditions are more likely to have greater representation of images depicting darker skin types.7 Future educational interventions may need to focus on dermatologic conditions that are not preferentially seen in patients with SOC. In our study, the pretest scores for conditions shown in darker skin were lowest among infectious and cancerous conditions. For infections, certain morphologic clues such as erythema are important for diagnosis but may be more subtle or difficult to discern in darker skin. It also is possible that providers may be less likely to suspect skin cancer in patients with SOC given that the morphologic presentation and/or anatomic site of involvement for skin cancers in SOC differs from those in lighter skin. Future educational interventions targeting disparities in diagnostic accuracy should focus on conditions that are not specifically associated with SOC.
Limitations of our study included the small number of participants, the study population came from a single institution, and a possible selection bias for providers interested in dermatology.
Conclusion
Disparities exist among interprofessional health care providers when treating conditions in patients with lighter skin compared to darker skin. An educational module for health care providers may provide long-term improvements in diagnostic accuracy and confidence for conditions presenting in patients with SOC.
- Fenton A, Elliott E, Shahbandi A, et al. Medical students’ ability to diagnose common dermatologic conditions in skin of color. J Am Acad Dermatol. 2020;83:957-958. doi:10.1016/j.jaad.2019.12.078
- Mamo A, Szeto MD, Rietcheck H, et al. Evaluating medical student assessment of common dermatologic conditions across Fitzpatrick phototypes and skin of color. J Am Acad Dermatol. 2022;87:167-169. doi:10.1016/j.jaad.2021.06.868
- Guda VA, Paek SY. Skin of color representation in commonly utilized medical student dermatology resources. J Drugs Dermatol. 2021;20:799. doi:10.36849/JDD.5726
- Wilson BN, Sun M, Ashbaugh AG, et al. Assessment of skin of color and diversity and inclusion content of dermatologic published literature: an analysis and call to action. Int J Womens Dermatol. 2021;7:391-397. doi:10.1016/j.ijwd.2021.04.001
- Ibraheim MK, Gupta R, Dao H, et al. Evaluating skin of color education in dermatology residency programs: data from a national survey. Clin Dermatol. 2022;40:228-233. doi:10.1016/j.clindermatol.2021.11.015
- Gupta R, Ibraheim MK, Dao H Jr, et al. Assessing dermatology resident confidence in caring for patients with skin of color. Clin Dermatol. 2021;39:873-878. doi:10.1016/j.clindermatol.2021.08.019
- Chang MJ, Lipner SR. Analysis of skin color on the American Academy of Dermatology public education website. J Drugs Dermatol. 2020;19:1236-1237. doi:10.36849/JDD.2020.5545
- Fenton A, Elliott E, Shahbandi A, et al. Medical students’ ability to diagnose common dermatologic conditions in skin of color. J Am Acad Dermatol. 2020;83:957-958. doi:10.1016/j.jaad.2019.12.078
- Mamo A, Szeto MD, Rietcheck H, et al. Evaluating medical student assessment of common dermatologic conditions across Fitzpatrick phototypes and skin of color. J Am Acad Dermatol. 2022;87:167-169. doi:10.1016/j.jaad.2021.06.868
- Guda VA, Paek SY. Skin of color representation in commonly utilized medical student dermatology resources. J Drugs Dermatol. 2021;20:799. doi:10.36849/JDD.5726
- Wilson BN, Sun M, Ashbaugh AG, et al. Assessment of skin of color and diversity and inclusion content of dermatologic published literature: an analysis and call to action. Int J Womens Dermatol. 2021;7:391-397. doi:10.1016/j.ijwd.2021.04.001
- Ibraheim MK, Gupta R, Dao H, et al. Evaluating skin of color education in dermatology residency programs: data from a national survey. Clin Dermatol. 2022;40:228-233. doi:10.1016/j.clindermatol.2021.11.015
- Gupta R, Ibraheim MK, Dao H Jr, et al. Assessing dermatology resident confidence in caring for patients with skin of color. Clin Dermatol. 2021;39:873-878. doi:10.1016/j.clindermatol.2021.08.019
- Chang MJ, Lipner SR. Analysis of skin color on the American Academy of Dermatology public education website. J Drugs Dermatol. 2020;19:1236-1237. doi:10.36849/JDD.2020.5545
Practice Points
- Disparities exist among interprofessional health care providers when diagnosing conditions in patients with lighter and darker skin, specifically for infectious, cancerous, or inflammatory conditions vs conditions that are preferentially seen in patients with skin of color (SOC).
- A focused educational module for health care providers may provide long-term improvements in diagnostic accuracy and confidence for conditions presenting in patients with SOC.
How to Advise Medical Students Interested in Dermatology: A Survey of Academic Dermatology Mentors
Dermatology remains one of the most competitive specialties in medicine. In 2022, there were 851 applicants (613 doctor of medicine seniors, 85 doctor of osteopathic medicine seniors) for 492 postgraduate year (PGY) 2 positions.1 During the 2022 application season, the average matched dermatology candidate had 7.2 research experiences; 20.9 abstracts, presentations, or publications; 11 volunteer experiences; and a US Medical Licensing Examination (USMLE) Step 2 Clinical Knowledge score of 257.1 With hopes of matching into such a competitive field, students often seek advice from academic dermatology mentors. Such advice may substantially differ based on each mentor and may or may not be evidence based.
We sought to analyze the range of advice given to medical students applying to dermatology residency programs via a survey to members of the Association of Professors of Dermatology (APD) with the intent to help applicants and mentors understand how letters of intent, letters of recommendation (LORs), and Electronic Residency Application Service (ERAS) supplemental applications are used by dermatology programs nationwide.
Methods
The study was reviewed by The Ohio State University institutional review board and was deemed exempt. A branching-logic survey with common questions from medical students while applying to dermatology residency programs (Table) was sent to all members of APD through the email listserve. Study data were collected and managed using REDCap electronic data capture tools hosted at The Ohio State University (Columbus, Ohio) to ensure data security.
The survey was distributed from August 28, 2022, to September 12, 2022. A total of 101 surveys were returned from 646 listserve members (15.6%). Given the branching-logic questions, differing numbers of responses were collected for each question. Descriptive statistics were utilized to analyze and report the results.
Results
Residency Program Number—Members of the APD were asked if they recommend students apply to a certain number of programs, and if so, how many programs. Of members who responded, 62.2% (61/98) either always (22.4% [22/98]) or sometimes (40.2% [39/97]) suggested students apply to a certain number of programs. When mentors made a recommendation, 54.1% (33/61) recommended applying to 59 or fewer programs, with only 9.8% (6/61) recommending students apply to 80 or more programs.
Gap Year—We queried mentors about their recommendations for a research gap year and asked which applicants should pursue this extra year. Our survey found that 74.5% of mentors (73/98) almost always (4.1% [4/98]) or sometimes (70.4% [69/98]) recommended a research gap year, most commonly for those applicants with a strong research interest (71.8% [51/71]). Other reasons mentors recommended a dedicated research year during medical school included low USMLE Step scores (50.7% [36/71]), low grades (45.1% [32/71]), little research (46.5% [33/71]), and no home program (43.7% [31/71]).
Internship Choices—Our survey results indicated that nearly two-thirds (63.3% [62/98]) of mentors did not give applicants a recommendation on type of internship (PGY-1). If a recommendation was given, academic dermatologists more commonly recommended an internal medicine preliminary year (29.6% [29/98]) over a transitional year (7.1% [7/98]).
Communication of Interest Via a Letter of Intent—We asked mentors if they recommended applicants send a letter of intent and conversely if receiving a letter of intent impacted their rank list. Nearly half (48.5% [47/97]) of mentors indicated they did not recommend sending a letter of intent, with only 15.5% (15/97) of mentors regularly recommending this practice. Additionally, 75.8% of mentors indicated that a letter of intent never (42.1% [40/95]) or rarely (33.7% [32/95]) impacted their rank list.
Rotation Choices—We queried mentors if they recommended students complete away rotations, and if so, how many rotations did they recommend. We found that 85.9% (85/99) of mentors recommended students complete an away rotation; 63.1% (53/84) of them recommended performing 2 away rotations, and 14.3% (12/84) of respondents recommended students complete 3 away rotations. More than a quarter of mentors (27.1% [23/85]) indicated their home medical schools limited the number of away rotations a medical student could complete in any 1 specialty, and 42.4% (36/85) of respondents were unsure if such a limitation existed.
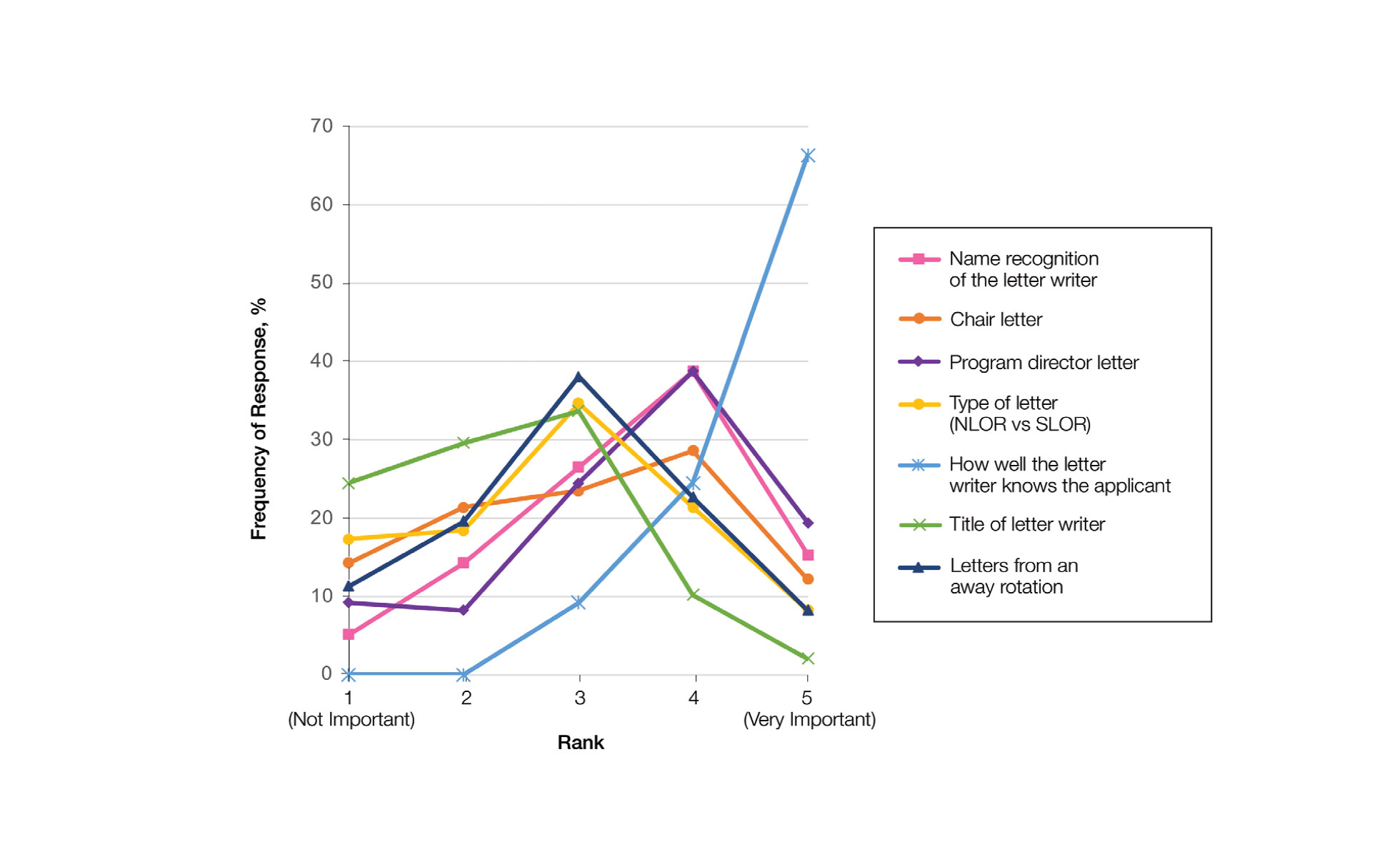
Letters of Recommendation—Our survey asked respondents to rank various factors on a 5-point scale (1=not important; 5=very important) when deciding who should write the students’ LORs. Mentors indicated that the most important factor for letter-writer selection was how well the letter writer knows the applicant, with 90.8% (89/98) of mentors rating the importance of this quality as a 4 or 5 (Figure). More than half of respondents rated the name recognition of the letter writer and program director letter as a 4 or 5 in importance (54.1% [53/98] and 58.2% [57/98], respectively). Type of letter (standardized vs nonstandardized), title of letter writer, letters from an away rotation, and chair letter scored lower, with fewer than half of mentors rating these as a 4 or 5 in importance.
Supplemental Application—When asked about the 2022 application cycle, respondents of our survey reported that the supplemental application was overall more important in deciding which applicants to interview vs which to rank highly. Prior experiences were important (ranked 4 or 5) for 58.8% (57/97) of respondents in choosing applicants to interview, and 49.4% (48/97) of respondents thought prior experiences were important for ranking. Similarly, 34.0% (33/97) of mentors indicated geographic preference was important (ranked 4 or 5) for interview compared with only 23.8% (23/97) for ranking. Finally, 57.7% (56/97) of our survey respondents denoted that program signals were important or very important in choosing which applicants to interview, while 32.0% (31/97) indicated that program signals were important in ranking applicants.
Comment
Residency Programs: Which Ones, and How Many?—The number of applications for dermatology residency programs has increased 33.9% from 2010 to 2019.2 The American Association of Medical Colleges Apply Smart data from 2013 to 2017 indicate that dermatology applicants arrive at a point of diminishing return between 37 and 62 applications, with variation within that range based on USMLE Step 1 score,3 and our data support this with nearly two-thirds of dermatology advisors recommending students apply within this range. Despite this data, dermatology residency applicants applied to more programs over the last decade (64.8 vs 77.0),2 likely to maximize their chance of matching.
Research Gap Years During Medical School—Prior research has shown that nearly half of faculty indicated that a research year during medical school can distinguish similar applicants, and close to 25% of applicants completed a research gap year.4,5 However, available data indicate that taking a research gap year has no effect on match rate or number of interview invites but does correlate with match rates at the highest ranked dermatology residency programs.6-8
Our data indicate that the most commonly recommended reason for a research gap year was an applicants’ strong interest in research. However, nearly half of dermatology mentors recommended research years during medical school for reasons other than an interest in research. As research gap years increase in popularity, future research is needed to confirm the consequence of this additional year and which applicants, if any, will benefit from such a year.
Preferences for Intern Year—Prior research suggests that dermatology residency program directors favor PGY-1 preliminary medicine internships because of the rigor of training.9,10 Our data continue to show a preference for internal medicine preliminary years over transitional years. However, given nearly two-thirds of dermatology mentors do not give applicants any recommendations on PGY-1 year, this preference may be fading.
Letters of Intent Not Recommended—Research in 2022 found that 78.8% of dermatology applicants sent a letter of intent communicating a plan to rank that program number 1, with nearly 13% sending such a letter to more than 1 program.11 With nearly half of mentors in our survey actively discouraging this process and more than 75% of mentors not utilizing this letter, the APD issued a brief statement on the 2022-2023 application cycle stating, “Post-interview communication of preference—including ‘letters of intent’ and thank you letters—should not be sent to programs. These types of communication are typically not used by residency programs in decision-making and lead to downstream pressures on applicants.”12
Away Rotations—Prior to the COVID-19 pandemic, data demonstrated that nearly one-third of dermatology applicants (29%) matched at their home institution, and nearly one-fifth (18%) matched where they completed an away rotation.13 In-person away rotations were eliminated in 2020 and restricted to 1 away rotation in 2021. Restrictions regarding away rotations were removed in 2022. Our data indicate that dermatology mentors strongly supported an away rotation, with more than half of them recommending at least 2 away rotations.
Further research is needed to determine the effect numerous away rotations have on minimizing students’ exposure to other specialties outside their chosen field. Additionally, further studies are needed to determine the impact away rotations have on economically disadvantaged students, students without home programs, and students with families. In an effort to standardize the number of away rotations, the APD issued a statement for the 2023-2024 application cycle indicating that dermatology applicants should limit away rotations to 2 in-person electives. Students without a home dermatology program could consider completing up to 3 electives.14
Who Should Write LORs?—Research in 2014 demonstrated that LORs were very important in determining applicants to interview, with a strong preference for LORs from academic dermatologists and colleagues.15 Our data strongly indicated applicants should predominantly ask for letters from writers who know them well. The majority of mentors did not give value to the rank of the letter writer (eg, assistant professor, associate professor, professor), type of letter, chair letters, or letters from an away rotation. These data may help alleviate stress many students feel as they search for letter writers.
How is the Supplemental Application Used?—In 2022, the ERAS supplemental application was introduced, which allowed applicants to detail 5 meaningful experiences, describe impactful life challenges, and indicate preferences for geographic region. Dermatology residency applicants also were able to choose 3 residency programs to signal interest in that program. Our data found that the supplemental application was utilized predominantly to select applicants to interview, which is in line with the Association of American Medical Colleges’ and APD guidelines indicating that this tool is solely meant to assist with application review.16 Further research and data will hopefully inform approaches to best utilize the ERAS supplemental application data.
Limitations—Our data were limited by response rate and sample size, as only academic dermatologists belonging to the APD were queried. Additionally, we did not track personal information of the mentors, so more than 1 mentor may have responded from a single institution, making it possible that our data may not be broadly applicable to all institutions.
Conclusion
Although there is no algorithmic method of advising medical students who are interested in dermatology, our survey data help to describe the range of advice currently given to students, which can improve and guide future recommendations. Additionally, some of our data demonstrate a discrepancy between mentor advice and current medical student practice for the number of applications and use of a letter of intent. We hope our data will assist academic dermatology mentors in the provision of advice to mentees as well as inform organizations seeking to create standards and official recommendations regarding aspects of the application process.
- National Resident Matching Program. Results and Data: 2022 Main Residency Match. May 2022. Accessed February 21, 2023. https://www.nrmp.org/wp-content/uploads/2022/05/2022-Main-Match-Results-and-Data_Final.pdf
- Secrest AM, Coman GC, Swink JM, et al. Limiting residency applications to dermatology benefits nearly everyone. J Clin Aesthet Dermatol. 2021;14:30-32.
- Apply smart for residency. Association of American Medical Colleges website. Accessed February 21, 2023. https://students-residents.aamc.org/apply-smart-residency
- Shamloul N, Grandhi R, Hossler E. Perceived importance of dermatology research fellowships. Presented at: Dermatology Teachers Exchange Group; October 3, 2020.
- Runge M, Jairath NK, Renati S, et al. Pursuit of a research year or dual degree by dermatology residency applicants: a cross-sectional study. Cutis. 2022;109:E12-E13.
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role of race and ethnicity in the dermatology applicant match process. J Natl Med Assoc. 2022;113:666-670.
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role research gap years play in a successful dermatology match. Int J Dermatol. 2022;61:226-230.
- Ramachandran V, Nguyen HY, Dao H Jr. Does it match? analyzing self-reported online dermatology match data to charting outcomes in the Match. Dermatol Online J. 2020;26:13030/qt4604h1w4.
- Hopkins C, Jalali O, Guffey D, et al. A survey of dermatology residents and program directors assessing the transition to dermatology residency. Proc (Bayl Univ Med Center). 2021;34:59-62.
- Stratman EJ, Ness RM. Factors associated with successful matching to dermatology residency programs by reapplicants and other applicants who previously graduated from medical school. Arch Dermatol. 2011;147:196-202.
- Brumfiel CM, Jefferson IS, Rinderknecht FA, et al. Current perspectives of and potential reforms to the dermatology residency application process: a nationwide survey of program directors and applicants. Clin Dermatol. 2022;40:595-601.
- Association of Professors of Dermatology. Residency Program Directors Section. Updated Information Regarding the 2022-2023 Application Cycle. Updated October 18, 2022. Accessed February 24, 2023. https://www.dermatologyprofessors.org/files/APD%20statement%20on%202022-2023%20application%20cycle_updated%20Oct.pdf
- Narang J, Morgan F, Eversman A, et al. Trends in geographic and home program preferences in the dermatology residency match: a retrospective cohort analysis. J Am Acad Dermatol. 2022;86:645-647.
- Association of Professors of Dermatology Residency Program Directors Section. Recommendations Regarding Away Electives. Updated December 14, 2022. Accessed February 24, 2022. https://www.dermatologyprofessors.org/files/APD%20recommendations%20on%20away%20rotations%202023-2024.pdf
- Kaffenberger BH, Kaffenberger JA, Zirwas MJ. Academic dermatologists’ views on the value of residency letters of recommendation. J Am Acad Dermatol. 2014;71:395-396.
- Supplemental ERAS Application: Guide for Residency Program. Association of American Medical Colleges; June 2022.
Dermatology remains one of the most competitive specialties in medicine. In 2022, there were 851 applicants (613 doctor of medicine seniors, 85 doctor of osteopathic medicine seniors) for 492 postgraduate year (PGY) 2 positions.1 During the 2022 application season, the average matched dermatology candidate had 7.2 research experiences; 20.9 abstracts, presentations, or publications; 11 volunteer experiences; and a US Medical Licensing Examination (USMLE) Step 2 Clinical Knowledge score of 257.1 With hopes of matching into such a competitive field, students often seek advice from academic dermatology mentors. Such advice may substantially differ based on each mentor and may or may not be evidence based.
We sought to analyze the range of advice given to medical students applying to dermatology residency programs via a survey to members of the Association of Professors of Dermatology (APD) with the intent to help applicants and mentors understand how letters of intent, letters of recommendation (LORs), and Electronic Residency Application Service (ERAS) supplemental applications are used by dermatology programs nationwide.
Methods
The study was reviewed by The Ohio State University institutional review board and was deemed exempt. A branching-logic survey with common questions from medical students while applying to dermatology residency programs (Table) was sent to all members of APD through the email listserve. Study data were collected and managed using REDCap electronic data capture tools hosted at The Ohio State University (Columbus, Ohio) to ensure data security.
The survey was distributed from August 28, 2022, to September 12, 2022. A total of 101 surveys were returned from 646 listserve members (15.6%). Given the branching-logic questions, differing numbers of responses were collected for each question. Descriptive statistics were utilized to analyze and report the results.
Results
Residency Program Number—Members of the APD were asked if they recommend students apply to a certain number of programs, and if so, how many programs. Of members who responded, 62.2% (61/98) either always (22.4% [22/98]) or sometimes (40.2% [39/97]) suggested students apply to a certain number of programs. When mentors made a recommendation, 54.1% (33/61) recommended applying to 59 or fewer programs, with only 9.8% (6/61) recommending students apply to 80 or more programs.
Gap Year—We queried mentors about their recommendations for a research gap year and asked which applicants should pursue this extra year. Our survey found that 74.5% of mentors (73/98) almost always (4.1% [4/98]) or sometimes (70.4% [69/98]) recommended a research gap year, most commonly for those applicants with a strong research interest (71.8% [51/71]). Other reasons mentors recommended a dedicated research year during medical school included low USMLE Step scores (50.7% [36/71]), low grades (45.1% [32/71]), little research (46.5% [33/71]), and no home program (43.7% [31/71]).
Internship Choices—Our survey results indicated that nearly two-thirds (63.3% [62/98]) of mentors did not give applicants a recommendation on type of internship (PGY-1). If a recommendation was given, academic dermatologists more commonly recommended an internal medicine preliminary year (29.6% [29/98]) over a transitional year (7.1% [7/98]).
Communication of Interest Via a Letter of Intent—We asked mentors if they recommended applicants send a letter of intent and conversely if receiving a letter of intent impacted their rank list. Nearly half (48.5% [47/97]) of mentors indicated they did not recommend sending a letter of intent, with only 15.5% (15/97) of mentors regularly recommending this practice. Additionally, 75.8% of mentors indicated that a letter of intent never (42.1% [40/95]) or rarely (33.7% [32/95]) impacted their rank list.
Rotation Choices—We queried mentors if they recommended students complete away rotations, and if so, how many rotations did they recommend. We found that 85.9% (85/99) of mentors recommended students complete an away rotation; 63.1% (53/84) of them recommended performing 2 away rotations, and 14.3% (12/84) of respondents recommended students complete 3 away rotations. More than a quarter of mentors (27.1% [23/85]) indicated their home medical schools limited the number of away rotations a medical student could complete in any 1 specialty, and 42.4% (36/85) of respondents were unsure if such a limitation existed.
Letters of Recommendation—Our survey asked respondents to rank various factors on a 5-point scale (1=not important; 5=very important) when deciding who should write the students’ LORs. Mentors indicated that the most important factor for letter-writer selection was how well the letter writer knows the applicant, with 90.8% (89/98) of mentors rating the importance of this quality as a 4 or 5 (Figure). More than half of respondents rated the name recognition of the letter writer and program director letter as a 4 or 5 in importance (54.1% [53/98] and 58.2% [57/98], respectively). Type of letter (standardized vs nonstandardized), title of letter writer, letters from an away rotation, and chair letter scored lower, with fewer than half of mentors rating these as a 4 or 5 in importance.
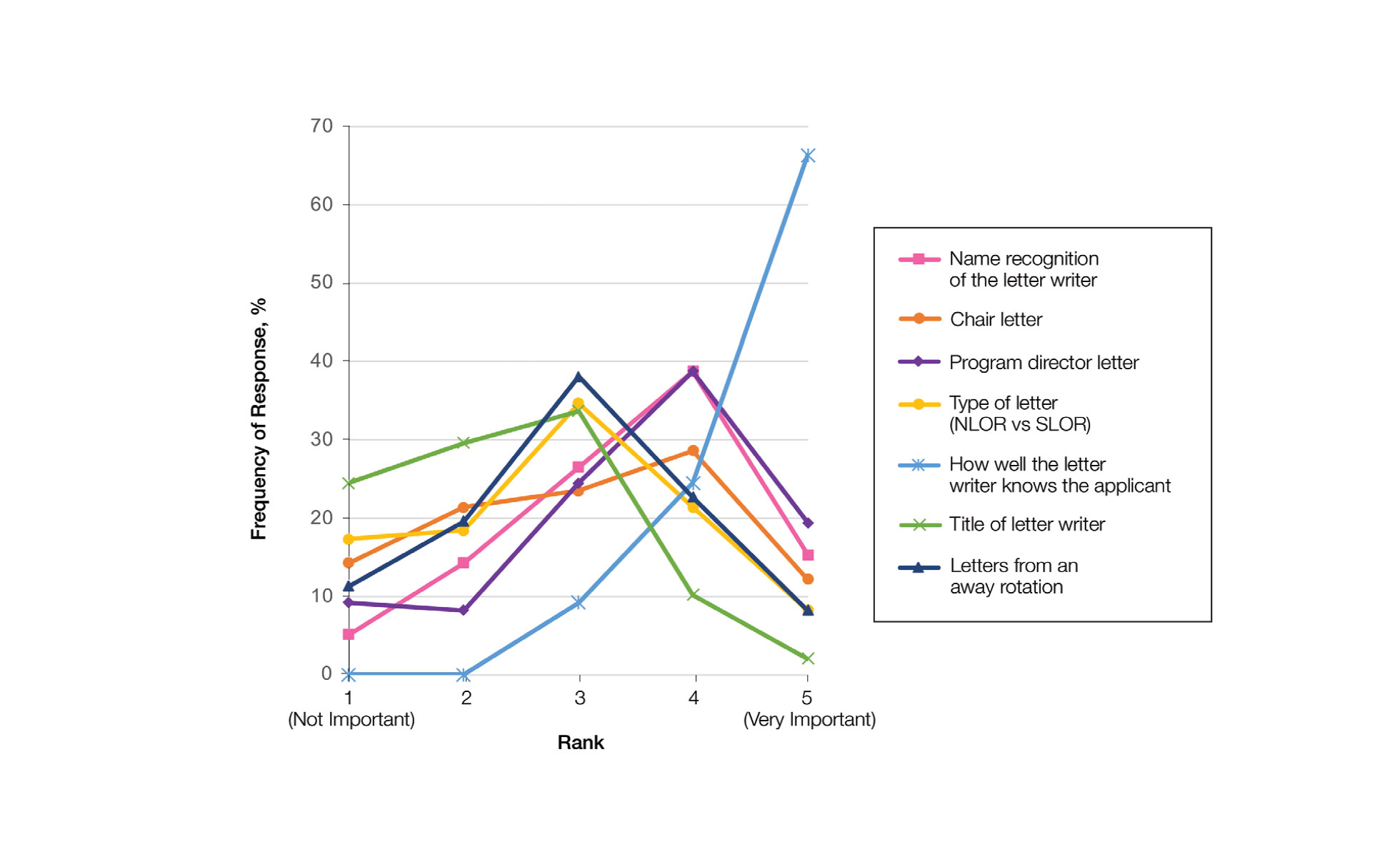
Supplemental Application—When asked about the 2022 application cycle, respondents of our survey reported that the supplemental application was overall more important in deciding which applicants to interview vs which to rank highly. Prior experiences were important (ranked 4 or 5) for 58.8% (57/97) of respondents in choosing applicants to interview, and 49.4% (48/97) of respondents thought prior experiences were important for ranking. Similarly, 34.0% (33/97) of mentors indicated geographic preference was important (ranked 4 or 5) for interview compared with only 23.8% (23/97) for ranking. Finally, 57.7% (56/97) of our survey respondents denoted that program signals were important or very important in choosing which applicants to interview, while 32.0% (31/97) indicated that program signals were important in ranking applicants.
Comment
Residency Programs: Which Ones, and How Many?—The number of applications for dermatology residency programs has increased 33.9% from 2010 to 2019.2 The American Association of Medical Colleges Apply Smart data from 2013 to 2017 indicate that dermatology applicants arrive at a point of diminishing return between 37 and 62 applications, with variation within that range based on USMLE Step 1 score,3 and our data support this with nearly two-thirds of dermatology advisors recommending students apply within this range. Despite this data, dermatology residency applicants applied to more programs over the last decade (64.8 vs 77.0),2 likely to maximize their chance of matching.
Research Gap Years During Medical School—Prior research has shown that nearly half of faculty indicated that a research year during medical school can distinguish similar applicants, and close to 25% of applicants completed a research gap year.4,5 However, available data indicate that taking a research gap year has no effect on match rate or number of interview invites but does correlate with match rates at the highest ranked dermatology residency programs.6-8
Our data indicate that the most commonly recommended reason for a research gap year was an applicants’ strong interest in research. However, nearly half of dermatology mentors recommended research years during medical school for reasons other than an interest in research. As research gap years increase in popularity, future research is needed to confirm the consequence of this additional year and which applicants, if any, will benefit from such a year.
Preferences for Intern Year—Prior research suggests that dermatology residency program directors favor PGY-1 preliminary medicine internships because of the rigor of training.9,10 Our data continue to show a preference for internal medicine preliminary years over transitional years. However, given nearly two-thirds of dermatology mentors do not give applicants any recommendations on PGY-1 year, this preference may be fading.
Letters of Intent Not Recommended—Research in 2022 found that 78.8% of dermatology applicants sent a letter of intent communicating a plan to rank that program number 1, with nearly 13% sending such a letter to more than 1 program.11 With nearly half of mentors in our survey actively discouraging this process and more than 75% of mentors not utilizing this letter, the APD issued a brief statement on the 2022-2023 application cycle stating, “Post-interview communication of preference—including ‘letters of intent’ and thank you letters—should not be sent to programs. These types of communication are typically not used by residency programs in decision-making and lead to downstream pressures on applicants.”12
Away Rotations—Prior to the COVID-19 pandemic, data demonstrated that nearly one-third of dermatology applicants (29%) matched at their home institution, and nearly one-fifth (18%) matched where they completed an away rotation.13 In-person away rotations were eliminated in 2020 and restricted to 1 away rotation in 2021. Restrictions regarding away rotations were removed in 2022. Our data indicate that dermatology mentors strongly supported an away rotation, with more than half of them recommending at least 2 away rotations.
Further research is needed to determine the effect numerous away rotations have on minimizing students’ exposure to other specialties outside their chosen field. Additionally, further studies are needed to determine the impact away rotations have on economically disadvantaged students, students without home programs, and students with families. In an effort to standardize the number of away rotations, the APD issued a statement for the 2023-2024 application cycle indicating that dermatology applicants should limit away rotations to 2 in-person electives. Students without a home dermatology program could consider completing up to 3 electives.14
Who Should Write LORs?—Research in 2014 demonstrated that LORs were very important in determining applicants to interview, with a strong preference for LORs from academic dermatologists and colleagues.15 Our data strongly indicated applicants should predominantly ask for letters from writers who know them well. The majority of mentors did not give value to the rank of the letter writer (eg, assistant professor, associate professor, professor), type of letter, chair letters, or letters from an away rotation. These data may help alleviate stress many students feel as they search for letter writers.
How is the Supplemental Application Used?—In 2022, the ERAS supplemental application was introduced, which allowed applicants to detail 5 meaningful experiences, describe impactful life challenges, and indicate preferences for geographic region. Dermatology residency applicants also were able to choose 3 residency programs to signal interest in that program. Our data found that the supplemental application was utilized predominantly to select applicants to interview, which is in line with the Association of American Medical Colleges’ and APD guidelines indicating that this tool is solely meant to assist with application review.16 Further research and data will hopefully inform approaches to best utilize the ERAS supplemental application data.
Limitations—Our data were limited by response rate and sample size, as only academic dermatologists belonging to the APD were queried. Additionally, we did not track personal information of the mentors, so more than 1 mentor may have responded from a single institution, making it possible that our data may not be broadly applicable to all institutions.
Conclusion
Although there is no algorithmic method of advising medical students who are interested in dermatology, our survey data help to describe the range of advice currently given to students, which can improve and guide future recommendations. Additionally, some of our data demonstrate a discrepancy between mentor advice and current medical student practice for the number of applications and use of a letter of intent. We hope our data will assist academic dermatology mentors in the provision of advice to mentees as well as inform organizations seeking to create standards and official recommendations regarding aspects of the application process.
Dermatology remains one of the most competitive specialties in medicine. In 2022, there were 851 applicants (613 doctor of medicine seniors, 85 doctor of osteopathic medicine seniors) for 492 postgraduate year (PGY) 2 positions.1 During the 2022 application season, the average matched dermatology candidate had 7.2 research experiences; 20.9 abstracts, presentations, or publications; 11 volunteer experiences; and a US Medical Licensing Examination (USMLE) Step 2 Clinical Knowledge score of 257.1 With hopes of matching into such a competitive field, students often seek advice from academic dermatology mentors. Such advice may substantially differ based on each mentor and may or may not be evidence based.
We sought to analyze the range of advice given to medical students applying to dermatology residency programs via a survey to members of the Association of Professors of Dermatology (APD) with the intent to help applicants and mentors understand how letters of intent, letters of recommendation (LORs), and Electronic Residency Application Service (ERAS) supplemental applications are used by dermatology programs nationwide.
Methods
The study was reviewed by The Ohio State University institutional review board and was deemed exempt. A branching-logic survey with common questions from medical students while applying to dermatology residency programs (Table) was sent to all members of APD through the email listserve. Study data were collected and managed using REDCap electronic data capture tools hosted at The Ohio State University (Columbus, Ohio) to ensure data security.
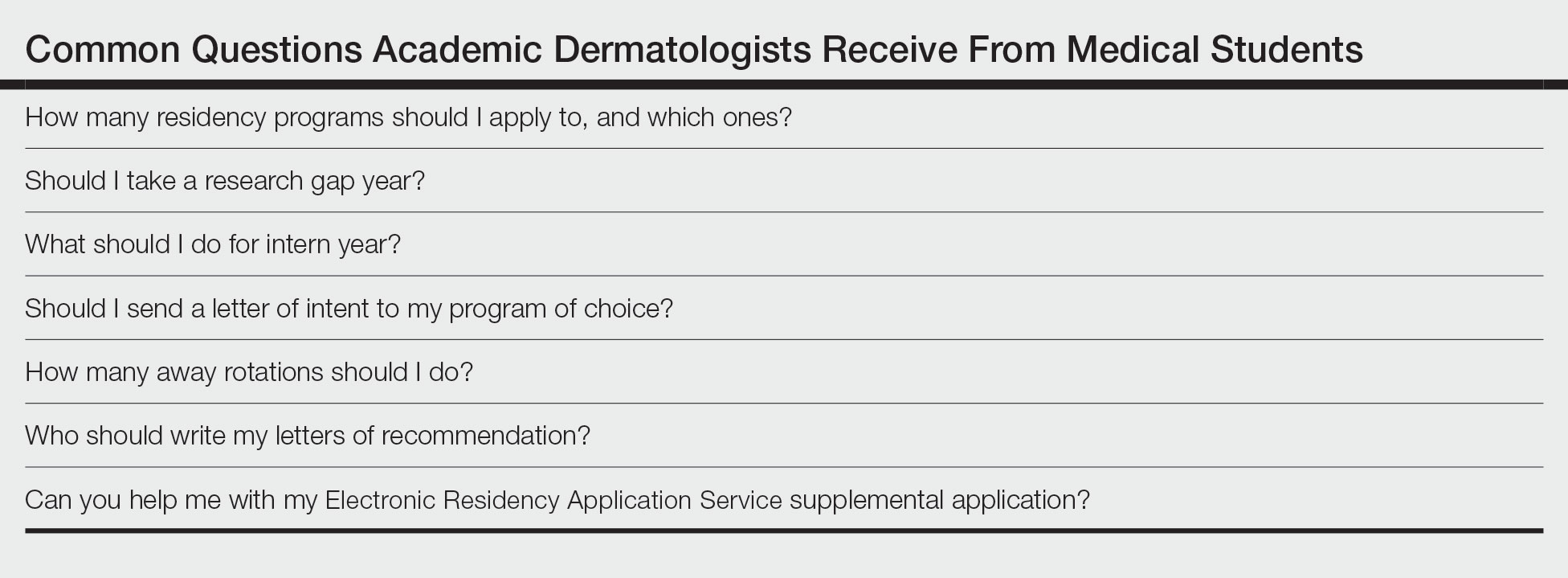
The survey was distributed from August 28, 2022, to September 12, 2022. A total of 101 surveys were returned from 646 listserve members (15.6%). Given the branching-logic questions, differing numbers of responses were collected for each question. Descriptive statistics were utilized to analyze and report the results.
Results
Residency Program Number—Members of the APD were asked if they recommend students apply to a certain number of programs, and if so, how many programs. Of members who responded, 62.2% (61/98) either always (22.4% [22/98]) or sometimes (40.2% [39/97]) suggested students apply to a certain number of programs. When mentors made a recommendation, 54.1% (33/61) recommended applying to 59 or fewer programs, with only 9.8% (6/61) recommending students apply to 80 or more programs.
Gap Year—We queried mentors about their recommendations for a research gap year and asked which applicants should pursue this extra year. Our survey found that 74.5% of mentors (73/98) almost always (4.1% [4/98]) or sometimes (70.4% [69/98]) recommended a research gap year, most commonly for those applicants with a strong research interest (71.8% [51/71]). Other reasons mentors recommended a dedicated research year during medical school included low USMLE Step scores (50.7% [36/71]), low grades (45.1% [32/71]), little research (46.5% [33/71]), and no home program (43.7% [31/71]).
Internship Choices—Our survey results indicated that nearly two-thirds (63.3% [62/98]) of mentors did not give applicants a recommendation on type of internship (PGY-1). If a recommendation was given, academic dermatologists more commonly recommended an internal medicine preliminary year (29.6% [29/98]) over a transitional year (7.1% [7/98]).
Communication of Interest Via a Letter of Intent—We asked mentors if they recommended applicants send a letter of intent and conversely if receiving a letter of intent impacted their rank list. Nearly half (48.5% [47/97]) of mentors indicated they did not recommend sending a letter of intent, with only 15.5% (15/97) of mentors regularly recommending this practice. Additionally, 75.8% of mentors indicated that a letter of intent never (42.1% [40/95]) or rarely (33.7% [32/95]) impacted their rank list.
Rotation Choices—We queried mentors if they recommended students complete away rotations, and if so, how many rotations did they recommend. We found that 85.9% (85/99) of mentors recommended students complete an away rotation; 63.1% (53/84) of them recommended performing 2 away rotations, and 14.3% (12/84) of respondents recommended students complete 3 away rotations. More than a quarter of mentors (27.1% [23/85]) indicated their home medical schools limited the number of away rotations a medical student could complete in any 1 specialty, and 42.4% (36/85) of respondents were unsure if such a limitation existed.
Letters of Recommendation—Our survey asked respondents to rank various factors on a 5-point scale (1=not important; 5=very important) when deciding who should write the students’ LORs. Mentors indicated that the most important factor for letter-writer selection was how well the letter writer knows the applicant, with 90.8% (89/98) of mentors rating the importance of this quality as a 4 or 5 (Figure). More than half of respondents rated the name recognition of the letter writer and program director letter as a 4 or 5 in importance (54.1% [53/98] and 58.2% [57/98], respectively). Type of letter (standardized vs nonstandardized), title of letter writer, letters from an away rotation, and chair letter scored lower, with fewer than half of mentors rating these as a 4 or 5 in importance.
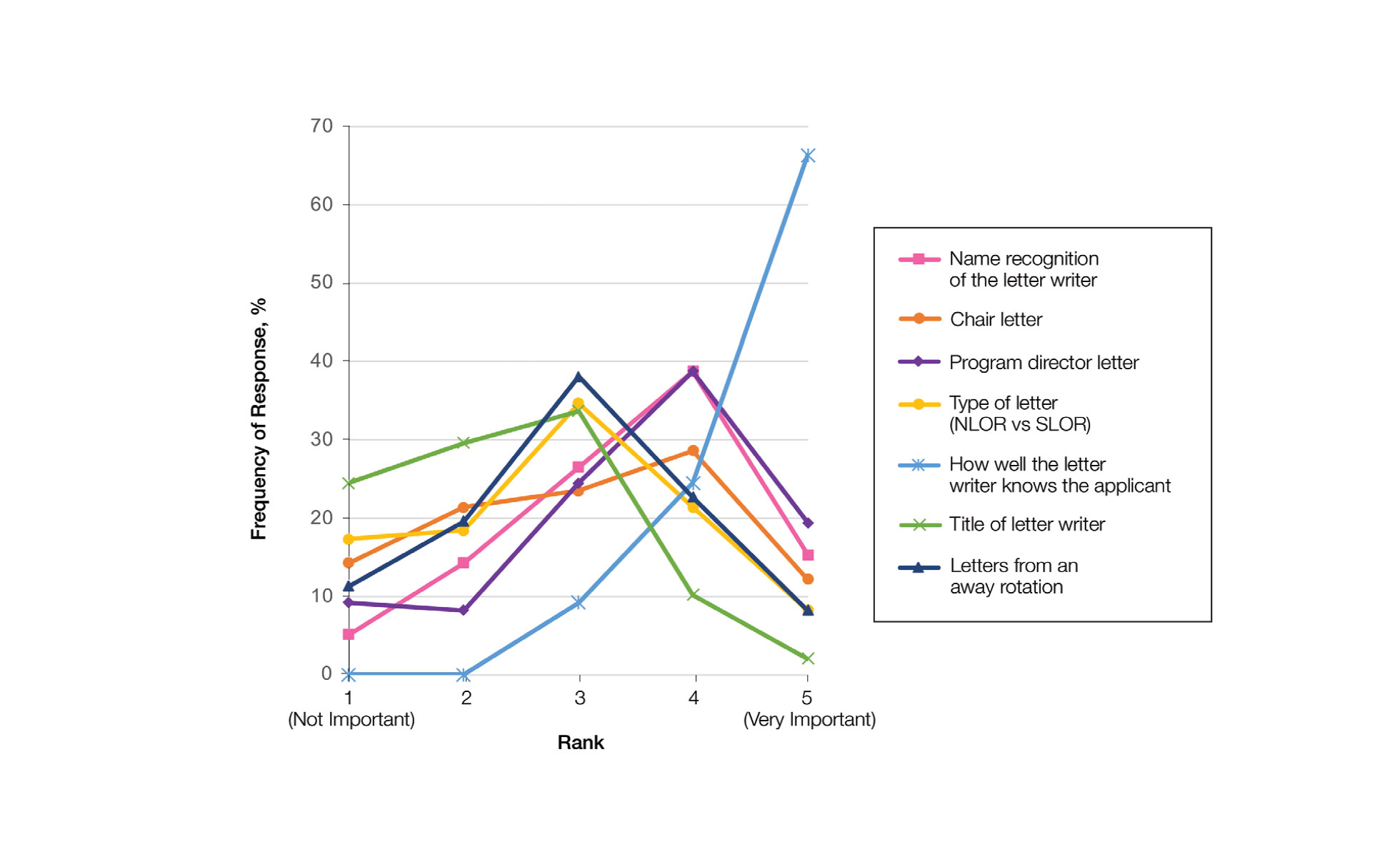
Supplemental Application—When asked about the 2022 application cycle, respondents of our survey reported that the supplemental application was overall more important in deciding which applicants to interview vs which to rank highly. Prior experiences were important (ranked 4 or 5) for 58.8% (57/97) of respondents in choosing applicants to interview, and 49.4% (48/97) of respondents thought prior experiences were important for ranking. Similarly, 34.0% (33/97) of mentors indicated geographic preference was important (ranked 4 or 5) for interview compared with only 23.8% (23/97) for ranking. Finally, 57.7% (56/97) of our survey respondents denoted that program signals were important or very important in choosing which applicants to interview, while 32.0% (31/97) indicated that program signals were important in ranking applicants.
Comment
Residency Programs: Which Ones, and How Many?—The number of applications for dermatology residency programs has increased 33.9% from 2010 to 2019.2 The American Association of Medical Colleges Apply Smart data from 2013 to 2017 indicate that dermatology applicants arrive at a point of diminishing return between 37 and 62 applications, with variation within that range based on USMLE Step 1 score,3 and our data support this with nearly two-thirds of dermatology advisors recommending students apply within this range. Despite this data, dermatology residency applicants applied to more programs over the last decade (64.8 vs 77.0),2 likely to maximize their chance of matching.
Research Gap Years During Medical School—Prior research has shown that nearly half of faculty indicated that a research year during medical school can distinguish similar applicants, and close to 25% of applicants completed a research gap year.4,5 However, available data indicate that taking a research gap year has no effect on match rate or number of interview invites but does correlate with match rates at the highest ranked dermatology residency programs.6-8
Our data indicate that the most commonly recommended reason for a research gap year was an applicants’ strong interest in research. However, nearly half of dermatology mentors recommended research years during medical school for reasons other than an interest in research. As research gap years increase in popularity, future research is needed to confirm the consequence of this additional year and which applicants, if any, will benefit from such a year.
Preferences for Intern Year—Prior research suggests that dermatology residency program directors favor PGY-1 preliminary medicine internships because of the rigor of training.9,10 Our data continue to show a preference for internal medicine preliminary years over transitional years. However, given nearly two-thirds of dermatology mentors do not give applicants any recommendations on PGY-1 year, this preference may be fading.
Letters of Intent Not Recommended—Research in 2022 found that 78.8% of dermatology applicants sent a letter of intent communicating a plan to rank that program number 1, with nearly 13% sending such a letter to more than 1 program.11 With nearly half of mentors in our survey actively discouraging this process and more than 75% of mentors not utilizing this letter, the APD issued a brief statement on the 2022-2023 application cycle stating, “Post-interview communication of preference—including ‘letters of intent’ and thank you letters—should not be sent to programs. These types of communication are typically not used by residency programs in decision-making and lead to downstream pressures on applicants.”12
Away Rotations—Prior to the COVID-19 pandemic, data demonstrated that nearly one-third of dermatology applicants (29%) matched at their home institution, and nearly one-fifth (18%) matched where they completed an away rotation.13 In-person away rotations were eliminated in 2020 and restricted to 1 away rotation in 2021. Restrictions regarding away rotations were removed in 2022. Our data indicate that dermatology mentors strongly supported an away rotation, with more than half of them recommending at least 2 away rotations.
Further research is needed to determine the effect numerous away rotations have on minimizing students’ exposure to other specialties outside their chosen field. Additionally, further studies are needed to determine the impact away rotations have on economically disadvantaged students, students without home programs, and students with families. In an effort to standardize the number of away rotations, the APD issued a statement for the 2023-2024 application cycle indicating that dermatology applicants should limit away rotations to 2 in-person electives. Students without a home dermatology program could consider completing up to 3 electives.14
Who Should Write LORs?—Research in 2014 demonstrated that LORs were very important in determining applicants to interview, with a strong preference for LORs from academic dermatologists and colleagues.15 Our data strongly indicated applicants should predominantly ask for letters from writers who know them well. The majority of mentors did not give value to the rank of the letter writer (eg, assistant professor, associate professor, professor), type of letter, chair letters, or letters from an away rotation. These data may help alleviate stress many students feel as they search for letter writers.
How is the Supplemental Application Used?—In 2022, the ERAS supplemental application was introduced, which allowed applicants to detail 5 meaningful experiences, describe impactful life challenges, and indicate preferences for geographic region. Dermatology residency applicants also were able to choose 3 residency programs to signal interest in that program. Our data found that the supplemental application was utilized predominantly to select applicants to interview, which is in line with the Association of American Medical Colleges’ and APD guidelines indicating that this tool is solely meant to assist with application review.16 Further research and data will hopefully inform approaches to best utilize the ERAS supplemental application data.
Limitations—Our data were limited by response rate and sample size, as only academic dermatologists belonging to the APD were queried. Additionally, we did not track personal information of the mentors, so more than 1 mentor may have responded from a single institution, making it possible that our data may not be broadly applicable to all institutions.
Conclusion
Although there is no algorithmic method of advising medical students who are interested in dermatology, our survey data help to describe the range of advice currently given to students, which can improve and guide future recommendations. Additionally, some of our data demonstrate a discrepancy between mentor advice and current medical student practice for the number of applications and use of a letter of intent. We hope our data will assist academic dermatology mentors in the provision of advice to mentees as well as inform organizations seeking to create standards and official recommendations regarding aspects of the application process.
- National Resident Matching Program. Results and Data: 2022 Main Residency Match. May 2022. Accessed February 21, 2023. https://www.nrmp.org/wp-content/uploads/2022/05/2022-Main-Match-Results-and-Data_Final.pdf
- Secrest AM, Coman GC, Swink JM, et al. Limiting residency applications to dermatology benefits nearly everyone. J Clin Aesthet Dermatol. 2021;14:30-32.
- Apply smart for residency. Association of American Medical Colleges website. Accessed February 21, 2023. https://students-residents.aamc.org/apply-smart-residency
- Shamloul N, Grandhi R, Hossler E. Perceived importance of dermatology research fellowships. Presented at: Dermatology Teachers Exchange Group; October 3, 2020.
- Runge M, Jairath NK, Renati S, et al. Pursuit of a research year or dual degree by dermatology residency applicants: a cross-sectional study. Cutis. 2022;109:E12-E13.
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role of race and ethnicity in the dermatology applicant match process. J Natl Med Assoc. 2022;113:666-670.
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role research gap years play in a successful dermatology match. Int J Dermatol. 2022;61:226-230.
- Ramachandran V, Nguyen HY, Dao H Jr. Does it match? analyzing self-reported online dermatology match data to charting outcomes in the Match. Dermatol Online J. 2020;26:13030/qt4604h1w4.
- Hopkins C, Jalali O, Guffey D, et al. A survey of dermatology residents and program directors assessing the transition to dermatology residency. Proc (Bayl Univ Med Center). 2021;34:59-62.
- Stratman EJ, Ness RM. Factors associated with successful matching to dermatology residency programs by reapplicants and other applicants who previously graduated from medical school. Arch Dermatol. 2011;147:196-202.
- Brumfiel CM, Jefferson IS, Rinderknecht FA, et al. Current perspectives of and potential reforms to the dermatology residency application process: a nationwide survey of program directors and applicants. Clin Dermatol. 2022;40:595-601.
- Association of Professors of Dermatology. Residency Program Directors Section. Updated Information Regarding the 2022-2023 Application Cycle. Updated October 18, 2022. Accessed February 24, 2023. https://www.dermatologyprofessors.org/files/APD%20statement%20on%202022-2023%20application%20cycle_updated%20Oct.pdf
- Narang J, Morgan F, Eversman A, et al. Trends in geographic and home program preferences in the dermatology residency match: a retrospective cohort analysis. J Am Acad Dermatol. 2022;86:645-647.
- Association of Professors of Dermatology Residency Program Directors Section. Recommendations Regarding Away Electives. Updated December 14, 2022. Accessed February 24, 2022. https://www.dermatologyprofessors.org/files/APD%20recommendations%20on%20away%20rotations%202023-2024.pdf
- Kaffenberger BH, Kaffenberger JA, Zirwas MJ. Academic dermatologists’ views on the value of residency letters of recommendation. J Am Acad Dermatol. 2014;71:395-396.
- Supplemental ERAS Application: Guide for Residency Program. Association of American Medical Colleges; June 2022.
- National Resident Matching Program. Results and Data: 2022 Main Residency Match. May 2022. Accessed February 21, 2023. https://www.nrmp.org/wp-content/uploads/2022/05/2022-Main-Match-Results-and-Data_Final.pdf
- Secrest AM, Coman GC, Swink JM, et al. Limiting residency applications to dermatology benefits nearly everyone. J Clin Aesthet Dermatol. 2021;14:30-32.
- Apply smart for residency. Association of American Medical Colleges website. Accessed February 21, 2023. https://students-residents.aamc.org/apply-smart-residency
- Shamloul N, Grandhi R, Hossler E. Perceived importance of dermatology research fellowships. Presented at: Dermatology Teachers Exchange Group; October 3, 2020.
- Runge M, Jairath NK, Renati S, et al. Pursuit of a research year or dual degree by dermatology residency applicants: a cross-sectional study. Cutis. 2022;109:E12-E13.
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role of race and ethnicity in the dermatology applicant match process. J Natl Med Assoc. 2022;113:666-670.
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role research gap years play in a successful dermatology match. Int J Dermatol. 2022;61:226-230.
- Ramachandran V, Nguyen HY, Dao H Jr. Does it match? analyzing self-reported online dermatology match data to charting outcomes in the Match. Dermatol Online J. 2020;26:13030/qt4604h1w4.
- Hopkins C, Jalali O, Guffey D, et al. A survey of dermatology residents and program directors assessing the transition to dermatology residency. Proc (Bayl Univ Med Center). 2021;34:59-62.
- Stratman EJ, Ness RM. Factors associated with successful matching to dermatology residency programs by reapplicants and other applicants who previously graduated from medical school. Arch Dermatol. 2011;147:196-202.
- Brumfiel CM, Jefferson IS, Rinderknecht FA, et al. Current perspectives of and potential reforms to the dermatology residency application process: a nationwide survey of program directors and applicants. Clin Dermatol. 2022;40:595-601.
- Association of Professors of Dermatology. Residency Program Directors Section. Updated Information Regarding the 2022-2023 Application Cycle. Updated October 18, 2022. Accessed February 24, 2023. https://www.dermatologyprofessors.org/files/APD%20statement%20on%202022-2023%20application%20cycle_updated%20Oct.pdf
- Narang J, Morgan F, Eversman A, et al. Trends in geographic and home program preferences in the dermatology residency match: a retrospective cohort analysis. J Am Acad Dermatol. 2022;86:645-647.
- Association of Professors of Dermatology Residency Program Directors Section. Recommendations Regarding Away Electives. Updated December 14, 2022. Accessed February 24, 2022. https://www.dermatologyprofessors.org/files/APD%20recommendations%20on%20away%20rotations%202023-2024.pdf
- Kaffenberger BH, Kaffenberger JA, Zirwas MJ. Academic dermatologists’ views on the value of residency letters of recommendation. J Am Acad Dermatol. 2014;71:395-396.
- Supplemental ERAS Application: Guide for Residency Program. Association of American Medical Colleges; June 2022.
Practice Points
- Dermatology mentors recommend students apply to 60 or fewer programs, with only a small percentage of faculty routinely recommending students apply to more than 80 programs.
- Dermatology mentors strongly recommend that students should not send a letter of intent to programs, as it rarely is used in the ranking process.
- Dermatology mentors encourage students to ask for letters of recommendation from writers who know them the best, irrespective of the letter writer’s rank or title. The type of letter (standardized vs nonstandardized), chair letter, or letters from an away rotation do not hold as much importance.
Assessing Treatment Delays for Vitiligo Patients: A Retrospective Chart Review
Similar to other dermatologic conditions, barriers to early care in patients with vitiligo can exacerbate health disparities.1 Delayed treatment of vitiligo is known to hamper successful disease stabilization and repigmentation, as therapies tend to work more effectively in early stages of the disease.2
To investigate the factors associated with treatment delays for patients with vitiligo, we conducted a retrospective chart review of 102 consecutive patients with vitiligo attending an academic outpatient clinic in Austin, Texas, over 36 months.
Methods
Our sample included 102 consecutive patients with vitiligo who attended an academic outpatient clinic in Austin, Texas, from January 2017 to January 2020. Demographic information, clinical characteristics of vitiligo, and treatment data were self-reported via a standardized questionnaire given to all patients with vitiligo and gathered from medical chart review. Patient characteristics are outlined in the Table. The delay to treatment was the time (in months) from the date the patient first noticed the lesion to the start date of first treatment. This retrospective chart review was reviewed by the University of Texas at Austin institutional review board and was determined to be exempt.
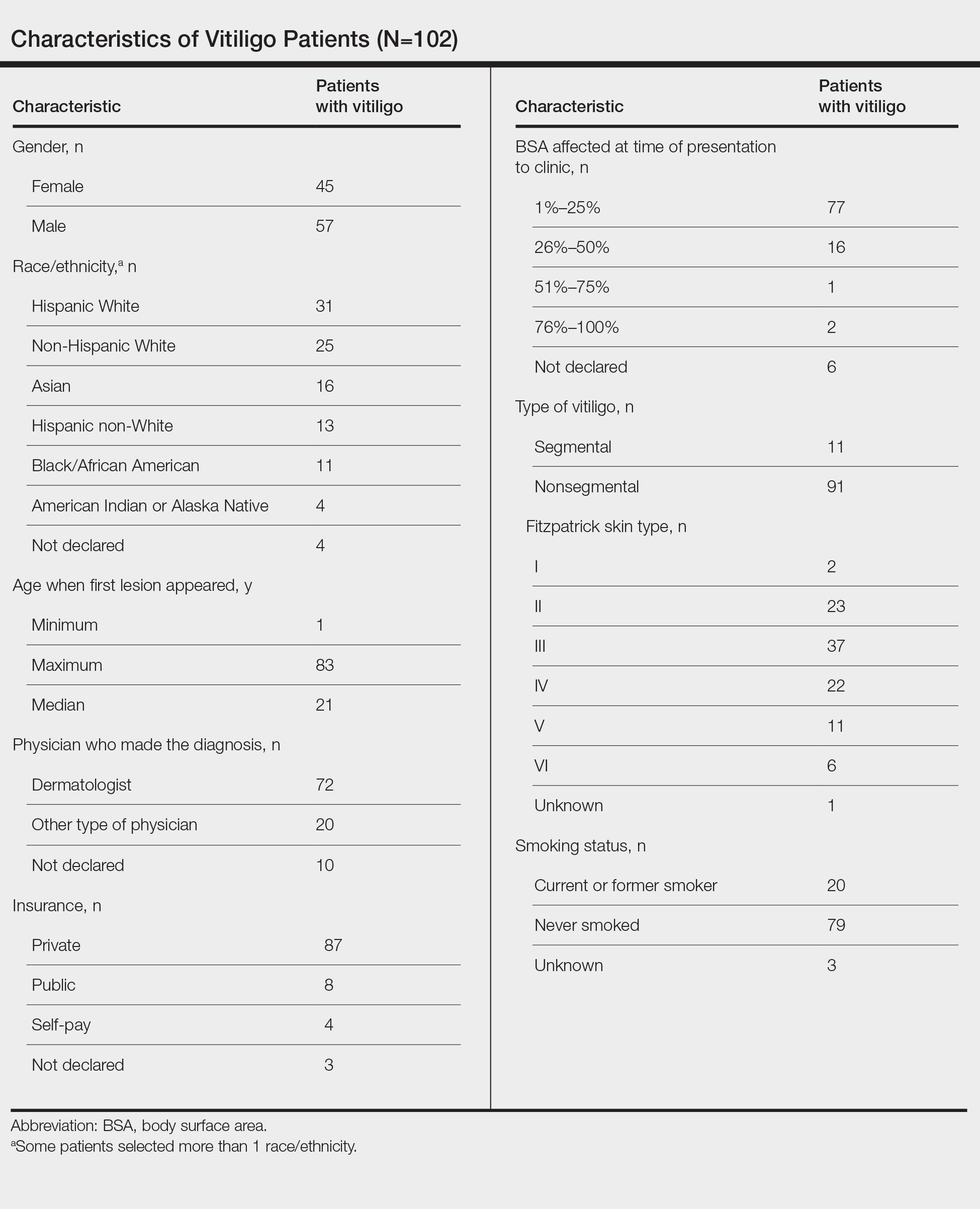
Statistical Analysis—The data were analyzed descriptively with a Wilcoxon rank sum test (type I error rate of .05).
Results
Of the 102 charts that were analyzed, 45 were females and 57 were males. More than half of the patients (54.9% [56/102]) were White. Sixteen were Asian, 13 were Hispanic non-White, 11 were Black/African American, and 4 were American Indian/Alaska Native. The median age of disease onset was 21 years, minimum age was 1 year, and maximum age was 83 years. The diagnosis of vitiligo was made by a dermatologist for 72 patients and by a physician of another specialty for 20 patients. Ten patients did not declare the specialty of the diagnosing physician.
Individuals older than 21 years when their disease started had a shorter delay to treatment than individuals who noticed their first lesion at an age younger than 21 years (median, 75 months vs 13 months; P<.01). Individuals diagnosed by a dermatologist had a shorter delay to treatment than individuals diagnosed by a physician of another specialty (median, 13 months vs 58 months; P<.05). White individuals had a shorter delay to treatment than individuals with skin of color (median, 13 months vs 31 months; P=.08), though this trend did not reach statistical significance. Individuals with 1% to 25% of body surface area (BSA) affected at time of presentation to clinic also had a shorter delay to treatment than those with a greater BSA affected (median, 13 months vs 74 months; P<.06), though this trend did not reach statistical significance. Type of vitiligo (P<.8), Fitzpatrick skin type (P<.6), and smoking status (P<.7) were not associated with differential delays.
Comment
Impact of Age on Vitiligo Treatment—Our data suggest that individuals who develop vitiligo at a younger age experience longer treatment delays compared to older individuals. Reasons for this are uncertain but could include access issues, medical decision-making agency, and younger patients not remembering being treated during their youth. Our data also could be influenced by some of the adult patients in our study first noticing their lesions many years ago when treatments for vitiligo were more limited. Nevertheless, detrimental effects on quality of life in children and adolescents with vitiligo suggest that motivating younger individuals with vitiligo to seek treatment or proactively making them aware of treatment opportunities may be beneficial.3
Diagnosis of Vitiligo by Nondermatologists—The increase in delay to treatment when a nondermatologist diagnoses vitiligo suggests that prompt initiation of treatment or referrals to dermatology by primary care providers may not routinely be occurring.4 Our data indicate the need to educate primary care providers on treatment opportunities for individuals with vitiligo and that early treatment generally is more effective.5
Impact of Race/Ethnicity on Vitiligo Treatment—Our data also show trends for longer treatment delays for individuals with skin of color. Although this did not reach statistical significance, we hope future studies will investigate this issue, especially because patients with skin of color experience more stigmatization and quality-of-life impacts by vitiligo than White patients.5
Impact of BSA on Vitiligo Treatment—Our data show that patients with a smaller BSA had a shorter delay to treatment than those with a greater BSA affected. This was a unique finding given it initially was hypothesized that patients with greater BSA would seek treatment earlier because of the associated increase in quality of life impact. This trend was not statistically significant, but further investigation would be helpful to analyze the reason behind treatment delays in patients with greater BSA affected.
Conclusion
The delay to treatment in our study population was correlated with the diagnosing physician’s specialty and patient age at disease onset, with trends also observed for race and BSA affected. These findings emphasize the need to investigate specific causes of barriers to early care to promote health equity among individuals with vitiligo.
- Tripathi R, Archibald LK, Mazmudar RS, et al. Racial differences in time to treatment for melanoma. J Am Acad Dermatol. 2020;83:854-859.
- Boniface K, Seneschal J. Vitiligo as a skin memory disease: the need for early intervention with immunomodulating agents and a maintenance therapy to target resident memory T cells. Exp Dermatol. 2019;28:656-661.
- Silverberg JI, Silverberg NB. Quality of life impairment in children and adolescents with vitiligo. Pediatr Dermatol. 2014;31:309-318.
- Amer AA, Gao XH. Quality of life in patients with vitiligo: an analysis of the dermatology life quality index outcome over the past two decades. Int J Dermatol. 2016;55:608-614.
- Weibel L, Laguda B, Atherton D, et al. Misdiagnosis and delay in referral of children with localized scleroderma. Br J Dermatol. 2011;165:1308-1313.
Similar to other dermatologic conditions, barriers to early care in patients with vitiligo can exacerbate health disparities.1 Delayed treatment of vitiligo is known to hamper successful disease stabilization and repigmentation, as therapies tend to work more effectively in early stages of the disease.2
To investigate the factors associated with treatment delays for patients with vitiligo, we conducted a retrospective chart review of 102 consecutive patients with vitiligo attending an academic outpatient clinic in Austin, Texas, over 36 months.
Methods
Our sample included 102 consecutive patients with vitiligo who attended an academic outpatient clinic in Austin, Texas, from January 2017 to January 2020. Demographic information, clinical characteristics of vitiligo, and treatment data were self-reported via a standardized questionnaire given to all patients with vitiligo and gathered from medical chart review. Patient characteristics are outlined in the Table. The delay to treatment was the time (in months) from the date the patient first noticed the lesion to the start date of first treatment. This retrospective chart review was reviewed by the University of Texas at Austin institutional review board and was determined to be exempt.
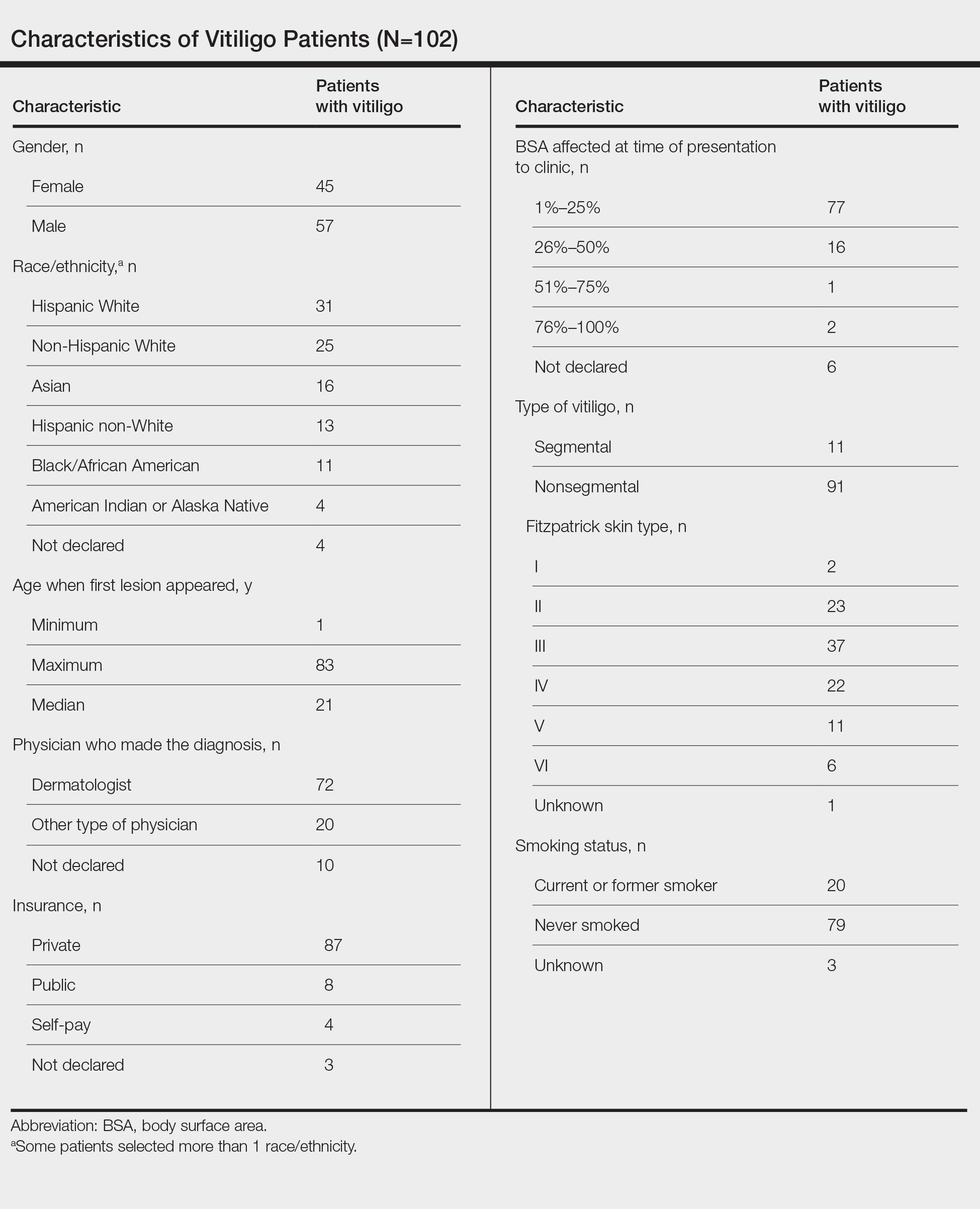
Statistical Analysis—The data were analyzed descriptively with a Wilcoxon rank sum test (type I error rate of .05).
Results
Of the 102 charts that were analyzed, 45 were females and 57 were males. More than half of the patients (54.9% [56/102]) were White. Sixteen were Asian, 13 were Hispanic non-White, 11 were Black/African American, and 4 were American Indian/Alaska Native. The median age of disease onset was 21 years, minimum age was 1 year, and maximum age was 83 years. The diagnosis of vitiligo was made by a dermatologist for 72 patients and by a physician of another specialty for 20 patients. Ten patients did not declare the specialty of the diagnosing physician.
Individuals older than 21 years when their disease started had a shorter delay to treatment than individuals who noticed their first lesion at an age younger than 21 years (median, 75 months vs 13 months; P<.01). Individuals diagnosed by a dermatologist had a shorter delay to treatment than individuals diagnosed by a physician of another specialty (median, 13 months vs 58 months; P<.05). White individuals had a shorter delay to treatment than individuals with skin of color (median, 13 months vs 31 months; P=.08), though this trend did not reach statistical significance. Individuals with 1% to 25% of body surface area (BSA) affected at time of presentation to clinic also had a shorter delay to treatment than those with a greater BSA affected (median, 13 months vs 74 months; P<.06), though this trend did not reach statistical significance. Type of vitiligo (P<.8), Fitzpatrick skin type (P<.6), and smoking status (P<.7) were not associated with differential delays.
Comment
Impact of Age on Vitiligo Treatment—Our data suggest that individuals who develop vitiligo at a younger age experience longer treatment delays compared to older individuals. Reasons for this are uncertain but could include access issues, medical decision-making agency, and younger patients not remembering being treated during their youth. Our data also could be influenced by some of the adult patients in our study first noticing their lesions many years ago when treatments for vitiligo were more limited. Nevertheless, detrimental effects on quality of life in children and adolescents with vitiligo suggest that motivating younger individuals with vitiligo to seek treatment or proactively making them aware of treatment opportunities may be beneficial.3
Diagnosis of Vitiligo by Nondermatologists—The increase in delay to treatment when a nondermatologist diagnoses vitiligo suggests that prompt initiation of treatment or referrals to dermatology by primary care providers may not routinely be occurring.4 Our data indicate the need to educate primary care providers on treatment opportunities for individuals with vitiligo and that early treatment generally is more effective.5
Impact of Race/Ethnicity on Vitiligo Treatment—Our data also show trends for longer treatment delays for individuals with skin of color. Although this did not reach statistical significance, we hope future studies will investigate this issue, especially because patients with skin of color experience more stigmatization and quality-of-life impacts by vitiligo than White patients.5
Impact of BSA on Vitiligo Treatment—Our data show that patients with a smaller BSA had a shorter delay to treatment than those with a greater BSA affected. This was a unique finding given it initially was hypothesized that patients with greater BSA would seek treatment earlier because of the associated increase in quality of life impact. This trend was not statistically significant, but further investigation would be helpful to analyze the reason behind treatment delays in patients with greater BSA affected.
Conclusion
The delay to treatment in our study population was correlated with the diagnosing physician’s specialty and patient age at disease onset, with trends also observed for race and BSA affected. These findings emphasize the need to investigate specific causes of barriers to early care to promote health equity among individuals with vitiligo.
Similar to other dermatologic conditions, barriers to early care in patients with vitiligo can exacerbate health disparities.1 Delayed treatment of vitiligo is known to hamper successful disease stabilization and repigmentation, as therapies tend to work more effectively in early stages of the disease.2
To investigate the factors associated with treatment delays for patients with vitiligo, we conducted a retrospective chart review of 102 consecutive patients with vitiligo attending an academic outpatient clinic in Austin, Texas, over 36 months.
Methods
Our sample included 102 consecutive patients with vitiligo who attended an academic outpatient clinic in Austin, Texas, from January 2017 to January 2020. Demographic information, clinical characteristics of vitiligo, and treatment data were self-reported via a standardized questionnaire given to all patients with vitiligo and gathered from medical chart review. Patient characteristics are outlined in the Table. The delay to treatment was the time (in months) from the date the patient first noticed the lesion to the start date of first treatment. This retrospective chart review was reviewed by the University of Texas at Austin institutional review board and was determined to be exempt.
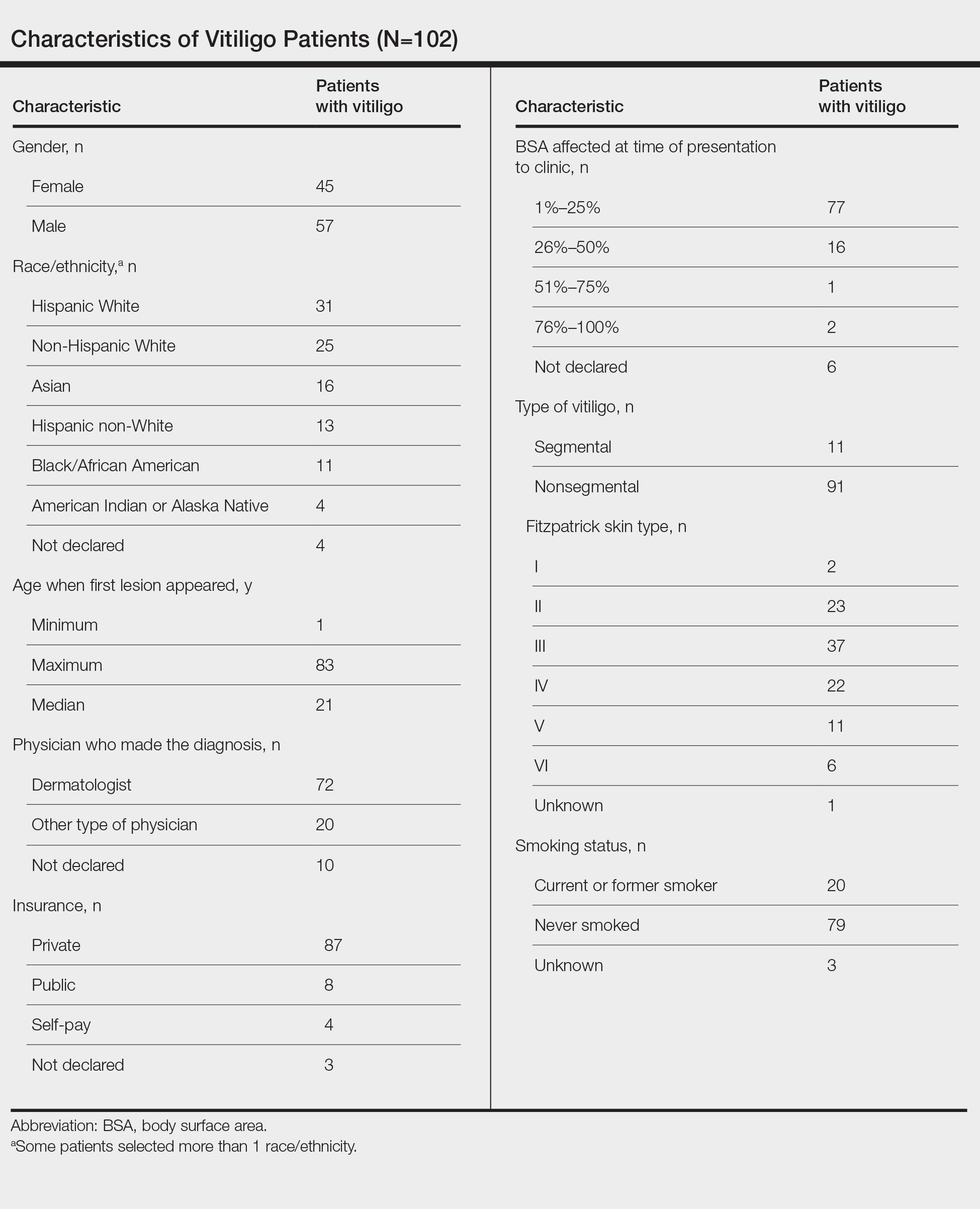
Statistical Analysis—The data were analyzed descriptively with a Wilcoxon rank sum test (type I error rate of .05).
Results
Of the 102 charts that were analyzed, 45 were females and 57 were males. More than half of the patients (54.9% [56/102]) were White. Sixteen were Asian, 13 were Hispanic non-White, 11 were Black/African American, and 4 were American Indian/Alaska Native. The median age of disease onset was 21 years, minimum age was 1 year, and maximum age was 83 years. The diagnosis of vitiligo was made by a dermatologist for 72 patients and by a physician of another specialty for 20 patients. Ten patients did not declare the specialty of the diagnosing physician.
Individuals older than 21 years when their disease started had a shorter delay to treatment than individuals who noticed their first lesion at an age younger than 21 years (median, 75 months vs 13 months; P<.01). Individuals diagnosed by a dermatologist had a shorter delay to treatment than individuals diagnosed by a physician of another specialty (median, 13 months vs 58 months; P<.05). White individuals had a shorter delay to treatment than individuals with skin of color (median, 13 months vs 31 months; P=.08), though this trend did not reach statistical significance. Individuals with 1% to 25% of body surface area (BSA) affected at time of presentation to clinic also had a shorter delay to treatment than those with a greater BSA affected (median, 13 months vs 74 months; P<.06), though this trend did not reach statistical significance. Type of vitiligo (P<.8), Fitzpatrick skin type (P<.6), and smoking status (P<.7) were not associated with differential delays.
Comment
Impact of Age on Vitiligo Treatment—Our data suggest that individuals who develop vitiligo at a younger age experience longer treatment delays compared to older individuals. Reasons for this are uncertain but could include access issues, medical decision-making agency, and younger patients not remembering being treated during their youth. Our data also could be influenced by some of the adult patients in our study first noticing their lesions many years ago when treatments for vitiligo were more limited. Nevertheless, detrimental effects on quality of life in children and adolescents with vitiligo suggest that motivating younger individuals with vitiligo to seek treatment or proactively making them aware of treatment opportunities may be beneficial.3
Diagnosis of Vitiligo by Nondermatologists—The increase in delay to treatment when a nondermatologist diagnoses vitiligo suggests that prompt initiation of treatment or referrals to dermatology by primary care providers may not routinely be occurring.4 Our data indicate the need to educate primary care providers on treatment opportunities for individuals with vitiligo and that early treatment generally is more effective.5
Impact of Race/Ethnicity on Vitiligo Treatment—Our data also show trends for longer treatment delays for individuals with skin of color. Although this did not reach statistical significance, we hope future studies will investigate this issue, especially because patients with skin of color experience more stigmatization and quality-of-life impacts by vitiligo than White patients.5
Impact of BSA on Vitiligo Treatment—Our data show that patients with a smaller BSA had a shorter delay to treatment than those with a greater BSA affected. This was a unique finding given it initially was hypothesized that patients with greater BSA would seek treatment earlier because of the associated increase in quality of life impact. This trend was not statistically significant, but further investigation would be helpful to analyze the reason behind treatment delays in patients with greater BSA affected.
Conclusion
The delay to treatment in our study population was correlated with the diagnosing physician’s specialty and patient age at disease onset, with trends also observed for race and BSA affected. These findings emphasize the need to investigate specific causes of barriers to early care to promote health equity among individuals with vitiligo.
- Tripathi R, Archibald LK, Mazmudar RS, et al. Racial differences in time to treatment for melanoma. J Am Acad Dermatol. 2020;83:854-859.
- Boniface K, Seneschal J. Vitiligo as a skin memory disease: the need for early intervention with immunomodulating agents and a maintenance therapy to target resident memory T cells. Exp Dermatol. 2019;28:656-661.
- Silverberg JI, Silverberg NB. Quality of life impairment in children and adolescents with vitiligo. Pediatr Dermatol. 2014;31:309-318.
- Amer AA, Gao XH. Quality of life in patients with vitiligo: an analysis of the dermatology life quality index outcome over the past two decades. Int J Dermatol. 2016;55:608-614.
- Weibel L, Laguda B, Atherton D, et al. Misdiagnosis and delay in referral of children with localized scleroderma. Br J Dermatol. 2011;165:1308-1313.
- Tripathi R, Archibald LK, Mazmudar RS, et al. Racial differences in time to treatment for melanoma. J Am Acad Dermatol. 2020;83:854-859.
- Boniface K, Seneschal J. Vitiligo as a skin memory disease: the need for early intervention with immunomodulating agents and a maintenance therapy to target resident memory T cells. Exp Dermatol. 2019;28:656-661.
- Silverberg JI, Silverberg NB. Quality of life impairment in children and adolescents with vitiligo. Pediatr Dermatol. 2014;31:309-318.
- Amer AA, Gao XH. Quality of life in patients with vitiligo: an analysis of the dermatology life quality index outcome over the past two decades. Int J Dermatol. 2016;55:608-614.
- Weibel L, Laguda B, Atherton D, et al. Misdiagnosis and delay in referral of children with localized scleroderma. Br J Dermatol. 2011;165:1308-1313.
Practice Points
- The medical community should be aware of factors associated with delay to treatment in patients with vitiligo, such as the diagnosing physician’s specialty and patient age at disease onset.
- Race and percentage of body surface area affected at time of presentation also demonstrate trends regarding treatment delays in patients with vitiligo.
The ERAS Supplemental Application: Current Status and Recommendations for Dermatology Applicants and Programs
In the 2021-2022 residency application cycle, the Association of American Medical Colleges (AAMC) piloted a supplemental application to accompany the standard residency application submitted via the AAMC’s Electronic Residency Application Service (ERAS).1 Dermatology was 1 of 3 specialties to participate in the pilot alongside internal medicine and general surgery. The goal was to develop a tool that could align applicants with programs that best matched their career goals as well as program and geographic preferences. The Association of Professors of Dermatology Residency Program Directors Section was an early advocate for the supplemental application, and members of our leadership were involved in the design, implementation, and evaluation of the pilot supplemental application.
Participating in the supplemental application was optional for both applicants and programs. The supplemental application included a Past Experiences section, which allowed applicants to highlight their 5 most meaningful research, work, and/or volunteer experiences and to describe a challenging life event that might not otherwise be included with their application. The geographic preferences section permitted applicants to select up to 3 regions of interest as well as to indicate an urban vs rural preference. Lastly, a preference-signaling section allowed dermatology applicants to send signals to up to 3 programs of particular interest.
With the close of another application cycle, applicants and programs will begin preparing for the 2022-2023 recruitment season. In this column, we present dermatology-specific data regarding the supplemental application, highlight tentative changes for the upcoming application cycle, and offer tips for applicants and programs as we approach year 2 of the supplemental application.
Results of Supplemental Application Evaluation Surveys
During the 2021-2022 recruitment season, 93% (950/1019) of dermatology applicants submitted the supplemental application, and 87% (117/135) of dermatology residency programs participated in the pilot.2 Surveys conducted by the AAMC between October 2021 and January 2022 showed that a large majority of dermatology programs used supplemental application data during initial application review when deciding who to interview. Eighty-three percent (40/48) of program directors felt that preference signals in particular helped them identify applicants they would have otherwise overlooked. Fifty-seven percent (4288/7516) of applicants across all specialties that participated in the pilot felt that preference signals would help them be noticed by their preferred programs.2 Preference signals were not evenly distributed among dermatology programs. Programs received an average of 23 signals, with a range of 2 to 87 (AAMC, unpublished data, February 2022).
Additional questions remain to be answered: How does the number of signals received affect application review? How often do geographic and program signals convert to interview offers and matches? Regardless, enthusiasm among dermatology programs for the supplemental application remains. In a recent survey of Association of Professors of Dermatology program directors, all 43 respondents planned to participate in the supplemental application again in the upcoming year (Ilana Rosman, MD; unpublished data; February 2022). The pilot will be expanded to include at least 12 other specialties.1As many who reviewed residency applications in 2021-2022 will attest, there was difficulty accessing the supplemental application data because it was not integrated into the Program Directors’ Work Station, the ERAS platform for programs to access applications, which will be remedied for the 2022-2023 iteration. Other tentative changes include modifications to the past experiences sections and timeline of the application.2
Utilizing the Supplemental Application: Recommendations to Applicants
Format of the Application—Applicants should familiarize themselves with the format of the supplemental application in advance and give themselves sufficient time to complete the application. In general, 3 to 4 hours of focused work should be enough time. Applicants should proofread for grammar and spelling before submitting.
Past Experiences—The past experiences section is intended to provide a focused snapshot of an applicant’s most meaningful activities and unique path to residency. Applicants should answer honestly based on their interests. If a student’s focus has been on volunteerism, the bulk of their 5 experiences listed may be related to service. Similarly, a student who has focused on research may preferentially highlight those experiences. In place of the long list of research, volunteer, and work experiences in the traditional ERAS application, applicants can highlight those activities in which they have been most invested. Applicants are encouraged to reflect on all genres of activities at any stage of their careers, even those not medical in nature, including work experience, military service, college athletics, or sustained musical or artistic achievement. Applicants should explain why each experience is meaningful rather than simply describing the activity.
Applicants also have the option to share a notable challenge they have overcome. It is not expected that each applicant will complete this question; in general, applicants who have not faced notable personal or professional obstacles should avoid answering. Additionally, if these challenges have been discussed in other areas of the application—for example, in the personal statement or medical student performance evaluation—it is not necessary to restate them here, though applicants can choose to do so. Examples of topics a student might discuss include being a first-generation college or medical student, growing up in poverty, facing notable personal or family health challenges, or having limited educational opportunities. It is important to share how this experience impacted an applicant’s journey to dermatology residency.
Geographic Preferences—The geographic preferences section can be difficult for applicants to navigate, as it may involve balancing a desire to attend a residency program in a particular region vs a greater desire to simply match in dermatology. In the past, programs may have made assumptions about geographic preferences based on an applicant’s birthplace, hometown, or medical school. In the supplemental application, applicants have the opportunity to directly reveal their preferences. We encourage applicants to be candid. Selecting a geographic region will not necessarily exclude applicants from consideration at other programs. For some applicants, program qualities may be more important than geography, or there may be no regional preferences. Those applicants can choose “no geographic preference.” There is considerable variability in how programs use geographic preferences. For this reason, it is in the best interest of applicants to simply respond honestly.
Preference Signaling—Preference signaling allows applicants to signal up to 3 preferred programs. Dermatology program directors agree that applicants should not signal their home program or programs at which they did in-person away rotations, as those programs would already be aware of the applicant’s interest. Although a signal increases the chances that the application will be reviewed holistically, it does not guarantee an interview offer. Programs may differentially utilize signals depending on multiple factors, including the number of signals received. We encourage applicants to discuss preference signaling strategies with advisors and focus on signaling programs in which they have genuine interest.
Recommendations to Selection Committees and Program Directors
The intent of the supplemental application is to provide a more meaningful picture of applicants and their experiences and preferences, with the goal of optimizing applicant-program fit. Programs should explicitly define for themselves the applicant characteristics and experiences they prioritize as well as their program goals. The supplemental application offers the potential to streamline holistic application review based on these elements. The short essay answers in the past experiences section permit reviewers to quickly scan for important experiences that align with the program’s recruitment goals. Importantly, reviewers should not penalize applicants who have not completed the question regarding other impactful life experiences, as not all applicants will have relevant information to share.
Some programs may find the geographic preferences section more valuable than others. Multiple factors affect how much weight will be given to geographic preferences, including program location and other characteristics that affect the desirability of the program to applicants. The competitiveness of the field, relatively low match rate, and limited number of programs may lead to less emphasis on geographic preferences in dermatology compared to other specialties. The purpose of this section is not to exclude applicants but to give programs more information that may help with alignment.
Anecdotally, many dermatology program directors were most interested in the preference signaling section of the supplemental application. Programs should consider signals to be evidence of strong preliminary interest. Programs may utilize signals differently depending on many factors such as the overall competitiveness of the program, program location, and the total number of signals the program receives. We recommend that programs holistically review all applications accompanied by a signal. Programs that utilize a points system may choose to award a certain number of points for a signal to their program. A signal might have a higher value at a program that receives only a few signals; conversely, a program that receives a large number of signals might not place tremendous value on the signal but may use it as a tiebreaker between similarly qualified applicants. Preference signaling is solely a tool for application review; because applicants’ preferences may change after the interview process, signals should not be utilized during ranking.
Next Steps
For program directors who have excitedly awaited residency application reform, the supplemental ERAS application is an important first step. Ultimately, we hope the supplemental application supplants much of the current residency application, serving as an efficient high-yield tool for holistically evaluating applicants’ academic and service records, accomplishments, and training preferences. Arriving at a new application will undoubtedly take time and discussion among the various stakeholders. Please continue to complete surveys from the AAMC, as feedback is the best method for refining the tool to serve its intended purpose.
Optimization of the application content is only one component of the reforms needed to improve the application process. Even with a revamped application tool, holistic review is challenging when programs are inundated with an ever-increasing number of applications. As such, we encourage stakeholders to simultaneously consider other potential reforms, such as caps on the number of applications, to allow programs and applicants the best opportunity for a mutually successful match.
- Supplemental ERAS application. Association of American Medical Colleges website. Accessed May 9, 2022. https://students-residents.aamc.org/applying-residencies-eras/supplemental-eras-application-eras-2023-cycle
- Association of American Medical Colleges. Supplemental application data and reports. Accessed May 9, 2022. https://www.aamc.org/data-reports/students-residents/report/supplemental-eras-application-data-and-reports
In the 2021-2022 residency application cycle, the Association of American Medical Colleges (AAMC) piloted a supplemental application to accompany the standard residency application submitted via the AAMC’s Electronic Residency Application Service (ERAS).1 Dermatology was 1 of 3 specialties to participate in the pilot alongside internal medicine and general surgery. The goal was to develop a tool that could align applicants with programs that best matched their career goals as well as program and geographic preferences. The Association of Professors of Dermatology Residency Program Directors Section was an early advocate for the supplemental application, and members of our leadership were involved in the design, implementation, and evaluation of the pilot supplemental application.
Participating in the supplemental application was optional for both applicants and programs. The supplemental application included a Past Experiences section, which allowed applicants to highlight their 5 most meaningful research, work, and/or volunteer experiences and to describe a challenging life event that might not otherwise be included with their application. The geographic preferences section permitted applicants to select up to 3 regions of interest as well as to indicate an urban vs rural preference. Lastly, a preference-signaling section allowed dermatology applicants to send signals to up to 3 programs of particular interest.
With the close of another application cycle, applicants and programs will begin preparing for the 2022-2023 recruitment season. In this column, we present dermatology-specific data regarding the supplemental application, highlight tentative changes for the upcoming application cycle, and offer tips for applicants and programs as we approach year 2 of the supplemental application.
Results of Supplemental Application Evaluation Surveys
During the 2021-2022 recruitment season, 93% (950/1019) of dermatology applicants submitted the supplemental application, and 87% (117/135) of dermatology residency programs participated in the pilot.2 Surveys conducted by the AAMC between October 2021 and January 2022 showed that a large majority of dermatology programs used supplemental application data during initial application review when deciding who to interview. Eighty-three percent (40/48) of program directors felt that preference signals in particular helped them identify applicants they would have otherwise overlooked. Fifty-seven percent (4288/7516) of applicants across all specialties that participated in the pilot felt that preference signals would help them be noticed by their preferred programs.2 Preference signals were not evenly distributed among dermatology programs. Programs received an average of 23 signals, with a range of 2 to 87 (AAMC, unpublished data, February 2022).
Additional questions remain to be answered: How does the number of signals received affect application review? How often do geographic and program signals convert to interview offers and matches? Regardless, enthusiasm among dermatology programs for the supplemental application remains. In a recent survey of Association of Professors of Dermatology program directors, all 43 respondents planned to participate in the supplemental application again in the upcoming year (Ilana Rosman, MD; unpublished data; February 2022). The pilot will be expanded to include at least 12 other specialties.1As many who reviewed residency applications in 2021-2022 will attest, there was difficulty accessing the supplemental application data because it was not integrated into the Program Directors’ Work Station, the ERAS platform for programs to access applications, which will be remedied for the 2022-2023 iteration. Other tentative changes include modifications to the past experiences sections and timeline of the application.2
Utilizing the Supplemental Application: Recommendations to Applicants
Format of the Application—Applicants should familiarize themselves with the format of the supplemental application in advance and give themselves sufficient time to complete the application. In general, 3 to 4 hours of focused work should be enough time. Applicants should proofread for grammar and spelling before submitting.
Past Experiences—The past experiences section is intended to provide a focused snapshot of an applicant’s most meaningful activities and unique path to residency. Applicants should answer honestly based on their interests. If a student’s focus has been on volunteerism, the bulk of their 5 experiences listed may be related to service. Similarly, a student who has focused on research may preferentially highlight those experiences. In place of the long list of research, volunteer, and work experiences in the traditional ERAS application, applicants can highlight those activities in which they have been most invested. Applicants are encouraged to reflect on all genres of activities at any stage of their careers, even those not medical in nature, including work experience, military service, college athletics, or sustained musical or artistic achievement. Applicants should explain why each experience is meaningful rather than simply describing the activity.
Applicants also have the option to share a notable challenge they have overcome. It is not expected that each applicant will complete this question; in general, applicants who have not faced notable personal or professional obstacles should avoid answering. Additionally, if these challenges have been discussed in other areas of the application—for example, in the personal statement or medical student performance evaluation—it is not necessary to restate them here, though applicants can choose to do so. Examples of topics a student might discuss include being a first-generation college or medical student, growing up in poverty, facing notable personal or family health challenges, or having limited educational opportunities. It is important to share how this experience impacted an applicant’s journey to dermatology residency.
Geographic Preferences—The geographic preferences section can be difficult for applicants to navigate, as it may involve balancing a desire to attend a residency program in a particular region vs a greater desire to simply match in dermatology. In the past, programs may have made assumptions about geographic preferences based on an applicant’s birthplace, hometown, or medical school. In the supplemental application, applicants have the opportunity to directly reveal their preferences. We encourage applicants to be candid. Selecting a geographic region will not necessarily exclude applicants from consideration at other programs. For some applicants, program qualities may be more important than geography, or there may be no regional preferences. Those applicants can choose “no geographic preference.” There is considerable variability in how programs use geographic preferences. For this reason, it is in the best interest of applicants to simply respond honestly.
Preference Signaling—Preference signaling allows applicants to signal up to 3 preferred programs. Dermatology program directors agree that applicants should not signal their home program or programs at which they did in-person away rotations, as those programs would already be aware of the applicant’s interest. Although a signal increases the chances that the application will be reviewed holistically, it does not guarantee an interview offer. Programs may differentially utilize signals depending on multiple factors, including the number of signals received. We encourage applicants to discuss preference signaling strategies with advisors and focus on signaling programs in which they have genuine interest.
Recommendations to Selection Committees and Program Directors
The intent of the supplemental application is to provide a more meaningful picture of applicants and their experiences and preferences, with the goal of optimizing applicant-program fit. Programs should explicitly define for themselves the applicant characteristics and experiences they prioritize as well as their program goals. The supplemental application offers the potential to streamline holistic application review based on these elements. The short essay answers in the past experiences section permit reviewers to quickly scan for important experiences that align with the program’s recruitment goals. Importantly, reviewers should not penalize applicants who have not completed the question regarding other impactful life experiences, as not all applicants will have relevant information to share.
Some programs may find the geographic preferences section more valuable than others. Multiple factors affect how much weight will be given to geographic preferences, including program location and other characteristics that affect the desirability of the program to applicants. The competitiveness of the field, relatively low match rate, and limited number of programs may lead to less emphasis on geographic preferences in dermatology compared to other specialties. The purpose of this section is not to exclude applicants but to give programs more information that may help with alignment.
Anecdotally, many dermatology program directors were most interested in the preference signaling section of the supplemental application. Programs should consider signals to be evidence of strong preliminary interest. Programs may utilize signals differently depending on many factors such as the overall competitiveness of the program, program location, and the total number of signals the program receives. We recommend that programs holistically review all applications accompanied by a signal. Programs that utilize a points system may choose to award a certain number of points for a signal to their program. A signal might have a higher value at a program that receives only a few signals; conversely, a program that receives a large number of signals might not place tremendous value on the signal but may use it as a tiebreaker between similarly qualified applicants. Preference signaling is solely a tool for application review; because applicants’ preferences may change after the interview process, signals should not be utilized during ranking.
Next Steps
For program directors who have excitedly awaited residency application reform, the supplemental ERAS application is an important first step. Ultimately, we hope the supplemental application supplants much of the current residency application, serving as an efficient high-yield tool for holistically evaluating applicants’ academic and service records, accomplishments, and training preferences. Arriving at a new application will undoubtedly take time and discussion among the various stakeholders. Please continue to complete surveys from the AAMC, as feedback is the best method for refining the tool to serve its intended purpose.
Optimization of the application content is only one component of the reforms needed to improve the application process. Even with a revamped application tool, holistic review is challenging when programs are inundated with an ever-increasing number of applications. As such, we encourage stakeholders to simultaneously consider other potential reforms, such as caps on the number of applications, to allow programs and applicants the best opportunity for a mutually successful match.
In the 2021-2022 residency application cycle, the Association of American Medical Colleges (AAMC) piloted a supplemental application to accompany the standard residency application submitted via the AAMC’s Electronic Residency Application Service (ERAS).1 Dermatology was 1 of 3 specialties to participate in the pilot alongside internal medicine and general surgery. The goal was to develop a tool that could align applicants with programs that best matched their career goals as well as program and geographic preferences. The Association of Professors of Dermatology Residency Program Directors Section was an early advocate for the supplemental application, and members of our leadership were involved in the design, implementation, and evaluation of the pilot supplemental application.
Participating in the supplemental application was optional for both applicants and programs. The supplemental application included a Past Experiences section, which allowed applicants to highlight their 5 most meaningful research, work, and/or volunteer experiences and to describe a challenging life event that might not otherwise be included with their application. The geographic preferences section permitted applicants to select up to 3 regions of interest as well as to indicate an urban vs rural preference. Lastly, a preference-signaling section allowed dermatology applicants to send signals to up to 3 programs of particular interest.
With the close of another application cycle, applicants and programs will begin preparing for the 2022-2023 recruitment season. In this column, we present dermatology-specific data regarding the supplemental application, highlight tentative changes for the upcoming application cycle, and offer tips for applicants and programs as we approach year 2 of the supplemental application.
Results of Supplemental Application Evaluation Surveys
During the 2021-2022 recruitment season, 93% (950/1019) of dermatology applicants submitted the supplemental application, and 87% (117/135) of dermatology residency programs participated in the pilot.2 Surveys conducted by the AAMC between October 2021 and January 2022 showed that a large majority of dermatology programs used supplemental application data during initial application review when deciding who to interview. Eighty-three percent (40/48) of program directors felt that preference signals in particular helped them identify applicants they would have otherwise overlooked. Fifty-seven percent (4288/7516) of applicants across all specialties that participated in the pilot felt that preference signals would help them be noticed by their preferred programs.2 Preference signals were not evenly distributed among dermatology programs. Programs received an average of 23 signals, with a range of 2 to 87 (AAMC, unpublished data, February 2022).
Additional questions remain to be answered: How does the number of signals received affect application review? How often do geographic and program signals convert to interview offers and matches? Regardless, enthusiasm among dermatology programs for the supplemental application remains. In a recent survey of Association of Professors of Dermatology program directors, all 43 respondents planned to participate in the supplemental application again in the upcoming year (Ilana Rosman, MD; unpublished data; February 2022). The pilot will be expanded to include at least 12 other specialties.1As many who reviewed residency applications in 2021-2022 will attest, there was difficulty accessing the supplemental application data because it was not integrated into the Program Directors’ Work Station, the ERAS platform for programs to access applications, which will be remedied for the 2022-2023 iteration. Other tentative changes include modifications to the past experiences sections and timeline of the application.2
Utilizing the Supplemental Application: Recommendations to Applicants
Format of the Application—Applicants should familiarize themselves with the format of the supplemental application in advance and give themselves sufficient time to complete the application. In general, 3 to 4 hours of focused work should be enough time. Applicants should proofread for grammar and spelling before submitting.
Past Experiences—The past experiences section is intended to provide a focused snapshot of an applicant’s most meaningful activities and unique path to residency. Applicants should answer honestly based on their interests. If a student’s focus has been on volunteerism, the bulk of their 5 experiences listed may be related to service. Similarly, a student who has focused on research may preferentially highlight those experiences. In place of the long list of research, volunteer, and work experiences in the traditional ERAS application, applicants can highlight those activities in which they have been most invested. Applicants are encouraged to reflect on all genres of activities at any stage of their careers, even those not medical in nature, including work experience, military service, college athletics, or sustained musical or artistic achievement. Applicants should explain why each experience is meaningful rather than simply describing the activity.
Applicants also have the option to share a notable challenge they have overcome. It is not expected that each applicant will complete this question; in general, applicants who have not faced notable personal or professional obstacles should avoid answering. Additionally, if these challenges have been discussed in other areas of the application—for example, in the personal statement or medical student performance evaluation—it is not necessary to restate them here, though applicants can choose to do so. Examples of topics a student might discuss include being a first-generation college or medical student, growing up in poverty, facing notable personal or family health challenges, or having limited educational opportunities. It is important to share how this experience impacted an applicant’s journey to dermatology residency.
Geographic Preferences—The geographic preferences section can be difficult for applicants to navigate, as it may involve balancing a desire to attend a residency program in a particular region vs a greater desire to simply match in dermatology. In the past, programs may have made assumptions about geographic preferences based on an applicant’s birthplace, hometown, or medical school. In the supplemental application, applicants have the opportunity to directly reveal their preferences. We encourage applicants to be candid. Selecting a geographic region will not necessarily exclude applicants from consideration at other programs. For some applicants, program qualities may be more important than geography, or there may be no regional preferences. Those applicants can choose “no geographic preference.” There is considerable variability in how programs use geographic preferences. For this reason, it is in the best interest of applicants to simply respond honestly.
Preference Signaling—Preference signaling allows applicants to signal up to 3 preferred programs. Dermatology program directors agree that applicants should not signal their home program or programs at which they did in-person away rotations, as those programs would already be aware of the applicant’s interest. Although a signal increases the chances that the application will be reviewed holistically, it does not guarantee an interview offer. Programs may differentially utilize signals depending on multiple factors, including the number of signals received. We encourage applicants to discuss preference signaling strategies with advisors and focus on signaling programs in which they have genuine interest.
Recommendations to Selection Committees and Program Directors
The intent of the supplemental application is to provide a more meaningful picture of applicants and their experiences and preferences, with the goal of optimizing applicant-program fit. Programs should explicitly define for themselves the applicant characteristics and experiences they prioritize as well as their program goals. The supplemental application offers the potential to streamline holistic application review based on these elements. The short essay answers in the past experiences section permit reviewers to quickly scan for important experiences that align with the program’s recruitment goals. Importantly, reviewers should not penalize applicants who have not completed the question regarding other impactful life experiences, as not all applicants will have relevant information to share.
Some programs may find the geographic preferences section more valuable than others. Multiple factors affect how much weight will be given to geographic preferences, including program location and other characteristics that affect the desirability of the program to applicants. The competitiveness of the field, relatively low match rate, and limited number of programs may lead to less emphasis on geographic preferences in dermatology compared to other specialties. The purpose of this section is not to exclude applicants but to give programs more information that may help with alignment.
Anecdotally, many dermatology program directors were most interested in the preference signaling section of the supplemental application. Programs should consider signals to be evidence of strong preliminary interest. Programs may utilize signals differently depending on many factors such as the overall competitiveness of the program, program location, and the total number of signals the program receives. We recommend that programs holistically review all applications accompanied by a signal. Programs that utilize a points system may choose to award a certain number of points for a signal to their program. A signal might have a higher value at a program that receives only a few signals; conversely, a program that receives a large number of signals might not place tremendous value on the signal but may use it as a tiebreaker between similarly qualified applicants. Preference signaling is solely a tool for application review; because applicants’ preferences may change after the interview process, signals should not be utilized during ranking.
Next Steps
For program directors who have excitedly awaited residency application reform, the supplemental ERAS application is an important first step. Ultimately, we hope the supplemental application supplants much of the current residency application, serving as an efficient high-yield tool for holistically evaluating applicants’ academic and service records, accomplishments, and training preferences. Arriving at a new application will undoubtedly take time and discussion among the various stakeholders. Please continue to complete surveys from the AAMC, as feedback is the best method for refining the tool to serve its intended purpose.
Optimization of the application content is only one component of the reforms needed to improve the application process. Even with a revamped application tool, holistic review is challenging when programs are inundated with an ever-increasing number of applications. As such, we encourage stakeholders to simultaneously consider other potential reforms, such as caps on the number of applications, to allow programs and applicants the best opportunity for a mutually successful match.
- Supplemental ERAS application. Association of American Medical Colleges website. Accessed May 9, 2022. https://students-residents.aamc.org/applying-residencies-eras/supplemental-eras-application-eras-2023-cycle
- Association of American Medical Colleges. Supplemental application data and reports. Accessed May 9, 2022. https://www.aamc.org/data-reports/students-residents/report/supplemental-eras-application-data-and-reports
- Supplemental ERAS application. Association of American Medical Colleges website. Accessed May 9, 2022. https://students-residents.aamc.org/applying-residencies-eras/supplemental-eras-application-eras-2023-cycle
- Association of American Medical Colleges. Supplemental application data and reports. Accessed May 9, 2022. https://www.aamc.org/data-reports/students-residents/report/supplemental-eras-application-data-and-reports
Practice Points
- The Electronic Residency Application Service (ERAS) Supplemental Application was piloted in the 2021-2022 residency application cycle and was utilized by the vast majority of dermatology applicants and programs.
- Survey data suggested that both applicants and programs found the supplemental application useful, particularly the preference signaling portion.
- The supplemental application will return for the 2022-2023 application cycle and will be integrated into the MyERAS workstation platform for easier access by programs.
Erythematous Papules and Pustules on the Nose
The Diagnosis: Granulosis Rubra Nasi
A history of prominent nasal sweating was later elicited and the patient was subsequently diagnosed with granulosis rubra nasi. She was instructed to continue daily use of topical pimecrolimus with the addition of topical atropine, resulting in complete resolution of the eruption at 6-week follow-up (Figure, A). She was then maintained on topical atropine monotherapy, only noting recurrence with cessation of the atropine (Figure, B).
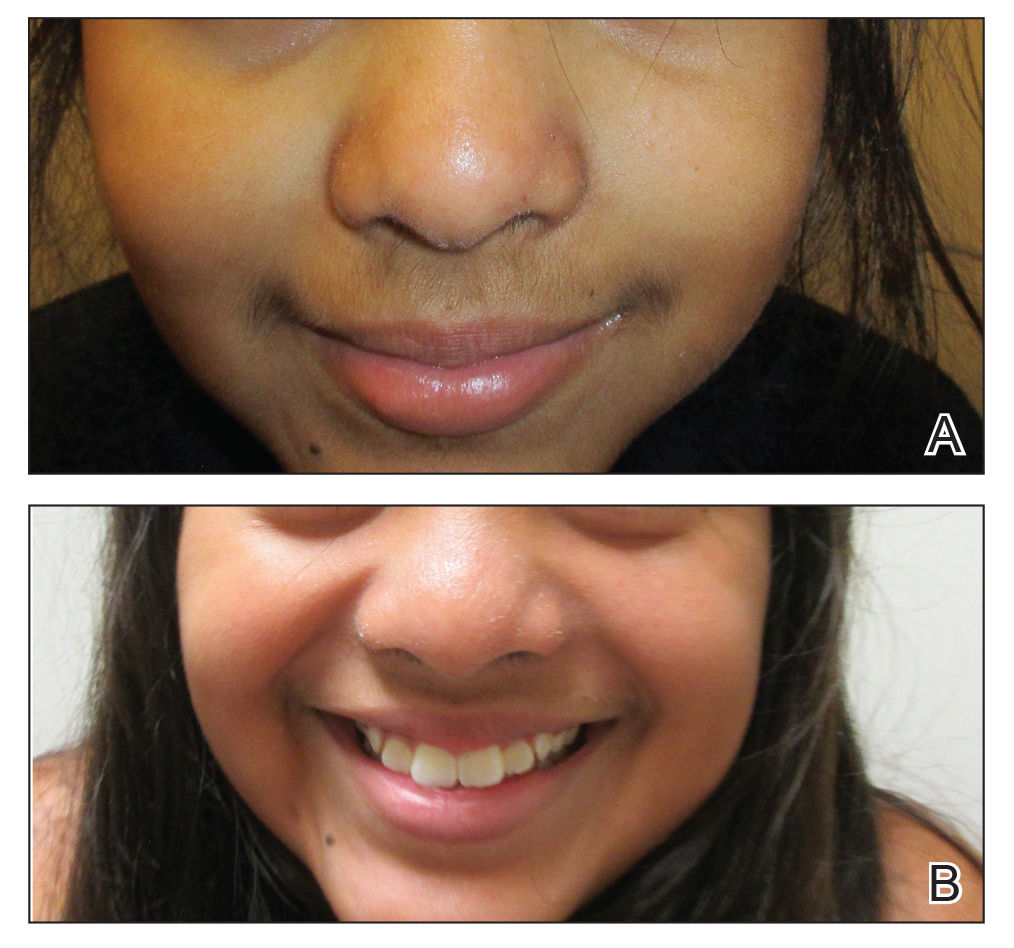
Other successful treatment regimens of granulosis rubra nasi include injection of botulinum toxin into the nose,1 monotherapy with topical tacrolimus,2 topical indomethacin, steroids, and cryotherapy, among other modalities.1 Topical atropine and pimecrolimus were selected as first-line agents for treating our pediatric patient due to tolerability and their anti-inflammatory and anticholinergic properties.
Granulosis rubra nasi is a form of focal hyperhidrosis that presents as erythematous papules, pustules, and vesicles of the midface, especially the nose.3 It is a fairly rare condition that can mimic many other common clinical entities, including comedonal acne, nevus comedonicus, periorificial dermatitis, and tinea faciei, but is resistant to treatments aimed at these disorders. It was first described as a "peculiar disease of the skin of the nose in children" in a case report by Jadassohn4 in 1901. It is most common in children aged 7 to 12 years and typically resolves at puberty; adults rarely are affected. Although the etiology has not yet been elucidated, autosomal-dominant transmission has been described, and the cutaneous changes are hypothesized to be secondary to hyperhidrosis.5 This postulation is further corroborated by a case report of a pheochromocytoma-associated granulosis rubra nasi that resolved with surgical excision of the pheochromocytoma.6 It is not uncommon for patients to have concomitant palmoplantar hyperhidrosis and acrocyanosis.5 Histopathologic examination is not necessary for diagnosis, but when performed, it discloses a mononuclear cellular infiltrate surrounding eccrine sweat ducts, blood vessels, and lymphatics without other abnormalities of the epidermis or pilosebaceous unit.1-3,7
- Grazziotin TC, Buffon RB, Da Silva Manzoni AP, et al. Treatment of granulosis rubra nasi with botulinum toxin. Dermatol Surg. 2009;35:1298-1299.
- Kumar P, Gosai A, Mondal AK, et al. Granulosis rubra nasi: a rare condition treated successfully with topical tacrolimus. Dermatol Reports. 2012;4:E5.
- Sargunam C, Thomas J, Ahmed NA. Granulosis rubra nasi. Indian Dermatol Online J. 2013;4:208-209.
- Jadassohn J. Ueber eine eigenartige erkrankung der nasenhaut bei kindern. Arch Derm Syph. 1901;58:145-158.
- Hellier FF. Granulosis rubra nasi in a mother and daughter. Br Med J. 1937;2:1068.
- Heid E, Samain F, Jelen G, et al. Granulosis rubra nasi and pheochromocytoma. Ann Dermatol Venereol. 1996;123:106-108.
- Akhdari N. Granulosis rubra nasi. Int J Dermatol. 2007;46:396.
The Diagnosis: Granulosis Rubra Nasi
A history of prominent nasal sweating was later elicited and the patient was subsequently diagnosed with granulosis rubra nasi. She was instructed to continue daily use of topical pimecrolimus with the addition of topical atropine, resulting in complete resolution of the eruption at 6-week follow-up (Figure, A). She was then maintained on topical atropine monotherapy, only noting recurrence with cessation of the atropine (Figure, B).
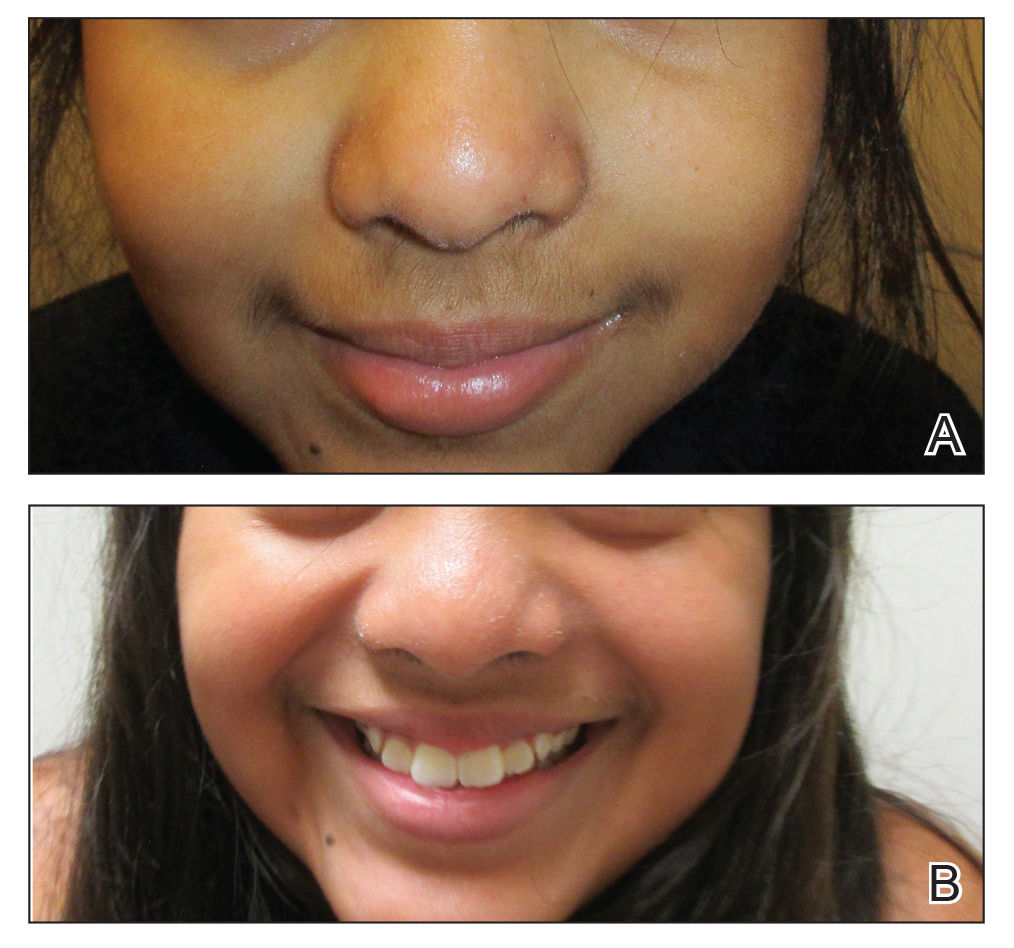
Other successful treatment regimens of granulosis rubra nasi include injection of botulinum toxin into the nose,1 monotherapy with topical tacrolimus,2 topical indomethacin, steroids, and cryotherapy, among other modalities.1 Topical atropine and pimecrolimus were selected as first-line agents for treating our pediatric patient due to tolerability and their anti-inflammatory and anticholinergic properties.
Granulosis rubra nasi is a form of focal hyperhidrosis that presents as erythematous papules, pustules, and vesicles of the midface, especially the nose.3 It is a fairly rare condition that can mimic many other common clinical entities, including comedonal acne, nevus comedonicus, periorificial dermatitis, and tinea faciei, but is resistant to treatments aimed at these disorders. It was first described as a "peculiar disease of the skin of the nose in children" in a case report by Jadassohn4 in 1901. It is most common in children aged 7 to 12 years and typically resolves at puberty; adults rarely are affected. Although the etiology has not yet been elucidated, autosomal-dominant transmission has been described, and the cutaneous changes are hypothesized to be secondary to hyperhidrosis.5 This postulation is further corroborated by a case report of a pheochromocytoma-associated granulosis rubra nasi that resolved with surgical excision of the pheochromocytoma.6 It is not uncommon for patients to have concomitant palmoplantar hyperhidrosis and acrocyanosis.5 Histopathologic examination is not necessary for diagnosis, but when performed, it discloses a mononuclear cellular infiltrate surrounding eccrine sweat ducts, blood vessels, and lymphatics without other abnormalities of the epidermis or pilosebaceous unit.1-3,7
The Diagnosis: Granulosis Rubra Nasi
A history of prominent nasal sweating was later elicited and the patient was subsequently diagnosed with granulosis rubra nasi. She was instructed to continue daily use of topical pimecrolimus with the addition of topical atropine, resulting in complete resolution of the eruption at 6-week follow-up (Figure, A). She was then maintained on topical atropine monotherapy, only noting recurrence with cessation of the atropine (Figure, B).
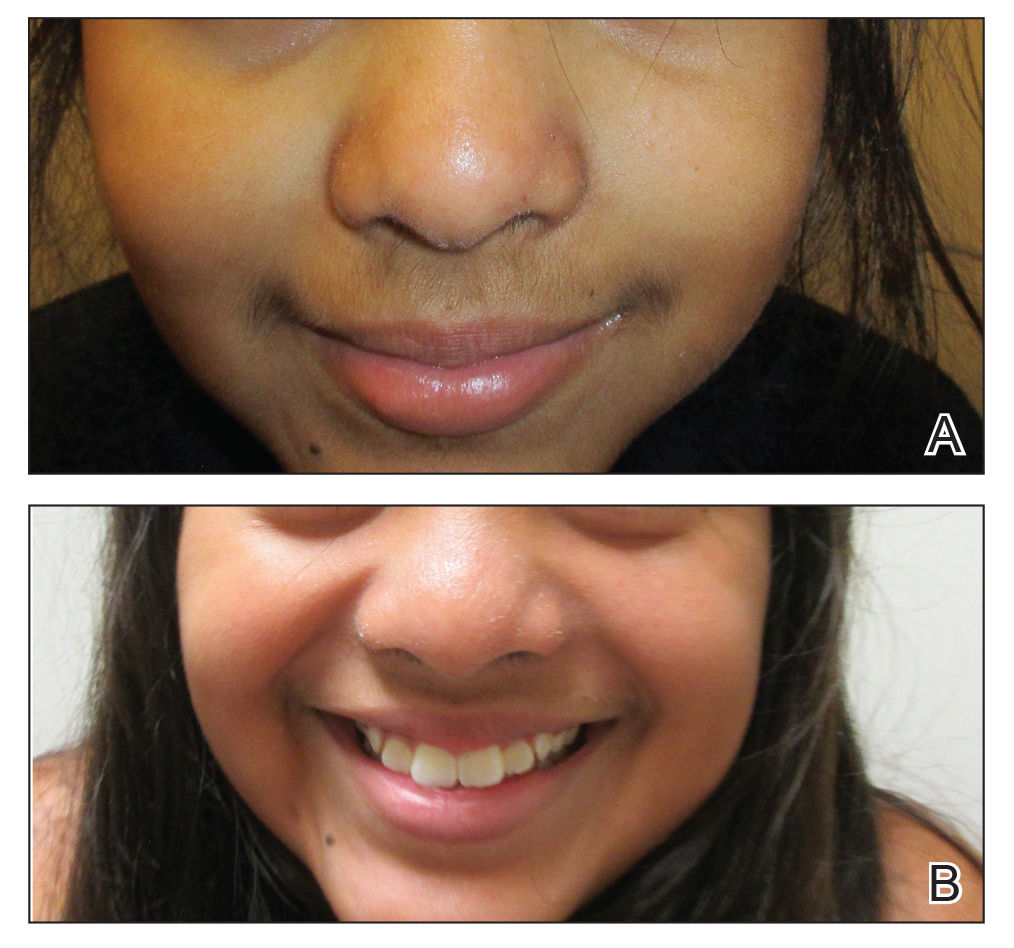
Other successful treatment regimens of granulosis rubra nasi include injection of botulinum toxin into the nose,1 monotherapy with topical tacrolimus,2 topical indomethacin, steroids, and cryotherapy, among other modalities.1 Topical atropine and pimecrolimus were selected as first-line agents for treating our pediatric patient due to tolerability and their anti-inflammatory and anticholinergic properties.
Granulosis rubra nasi is a form of focal hyperhidrosis that presents as erythematous papules, pustules, and vesicles of the midface, especially the nose.3 It is a fairly rare condition that can mimic many other common clinical entities, including comedonal acne, nevus comedonicus, periorificial dermatitis, and tinea faciei, but is resistant to treatments aimed at these disorders. It was first described as a "peculiar disease of the skin of the nose in children" in a case report by Jadassohn4 in 1901. It is most common in children aged 7 to 12 years and typically resolves at puberty; adults rarely are affected. Although the etiology has not yet been elucidated, autosomal-dominant transmission has been described, and the cutaneous changes are hypothesized to be secondary to hyperhidrosis.5 This postulation is further corroborated by a case report of a pheochromocytoma-associated granulosis rubra nasi that resolved with surgical excision of the pheochromocytoma.6 It is not uncommon for patients to have concomitant palmoplantar hyperhidrosis and acrocyanosis.5 Histopathologic examination is not necessary for diagnosis, but when performed, it discloses a mononuclear cellular infiltrate surrounding eccrine sweat ducts, blood vessels, and lymphatics without other abnormalities of the epidermis or pilosebaceous unit.1-3,7
- Grazziotin TC, Buffon RB, Da Silva Manzoni AP, et al. Treatment of granulosis rubra nasi with botulinum toxin. Dermatol Surg. 2009;35:1298-1299.
- Kumar P, Gosai A, Mondal AK, et al. Granulosis rubra nasi: a rare condition treated successfully with topical tacrolimus. Dermatol Reports. 2012;4:E5.
- Sargunam C, Thomas J, Ahmed NA. Granulosis rubra nasi. Indian Dermatol Online J. 2013;4:208-209.
- Jadassohn J. Ueber eine eigenartige erkrankung der nasenhaut bei kindern. Arch Derm Syph. 1901;58:145-158.
- Hellier FF. Granulosis rubra nasi in a mother and daughter. Br Med J. 1937;2:1068.
- Heid E, Samain F, Jelen G, et al. Granulosis rubra nasi and pheochromocytoma. Ann Dermatol Venereol. 1996;123:106-108.
- Akhdari N. Granulosis rubra nasi. Int J Dermatol. 2007;46:396.
- Grazziotin TC, Buffon RB, Da Silva Manzoni AP, et al. Treatment of granulosis rubra nasi with botulinum toxin. Dermatol Surg. 2009;35:1298-1299.
- Kumar P, Gosai A, Mondal AK, et al. Granulosis rubra nasi: a rare condition treated successfully with topical tacrolimus. Dermatol Reports. 2012;4:E5.
- Sargunam C, Thomas J, Ahmed NA. Granulosis rubra nasi. Indian Dermatol Online J. 2013;4:208-209.
- Jadassohn J. Ueber eine eigenartige erkrankung der nasenhaut bei kindern. Arch Derm Syph. 1901;58:145-158.
- Hellier FF. Granulosis rubra nasi in a mother and daughter. Br Med J. 1937;2:1068.
- Heid E, Samain F, Jelen G, et al. Granulosis rubra nasi and pheochromocytoma. Ann Dermatol Venereol. 1996;123:106-108.
- Akhdari N. Granulosis rubra nasi. Int J Dermatol. 2007;46:396.

A healthy 9-year-old girl presented with a 2-year history of erythematous papules and pustules on the nose. There was no involvement of the rest of the face or body. At the time of presentation, she had been treated with several topical therapies including steroids, calcineurin inhibitors, antibiotics, and retinoids without improvement. A potassium hydroxide preparation from a pustule was performed and revealed only normal keratinocytes.

