User login
Zika knowledge, preparedness low among U.S. pediatricians
BALTIMORE – U.S. pediatricians feel comfortable providing patients with preventive information and travel advice related to Zika, but few feel prepared when it comes to testing and management of infants exposed prenatally to Zika infections, a study found.
“Areas where pediatricians were less likely to report preparedness included recommending testing, providing data to the Centers for Disease Control and Prevention’s Zika Pregnancy Registry, managing infants exposed to Zika prenatally, and informing parents of social services for Zika-infected infants,” senior author Amy J. Houtrow, MD, MPH, PhD, and colleagues reported at the Pediatric Academic Societies annual meeting.
“Results indicate that additional education efforts are needed to grow the overall Zika knowledge of pediatricians and boost preparedness, particularly around recommending Zika testing and providing data to CDC,” they concluded.
But these findings are not surprising given how rare congenital Zika virus syndrome is, explained Dr. Houtrow, an associate professor of physical medicine and rehabilitation and pediatrics at the University of Pittsburgh.
“For most rare conditions, pediatricians report better general than specific knowledge,” Dr. Houtrow said in an interview. “We expect pediatricians have a broad range of knowledge for a multitude of conditions and to be well versed in the care of infants and children with common conditions, coupled with the ability to access knowledge and expertise about rarer conditions such as congenital Zika syndrome.”
Dr. Houtrow and associates drew their findings from the 2018 AAP Periodic Survey of Fellows, which includes both primary care physicians and neonatologists. The survey’s response rate was 42%, with 672 of 1,599 surveys returned, but the researchers limited their analysis to 576 postresidency respondents who were providing direct patient care.
Overall, 39% of physicians reported being knowledgeable about Zika virus, and 47% said they wanted to learn more. More than half of responding doctors (57%) reported feeling moderately or very prepared when it came to informing patients of preventive measures to reduce risk of Zika infection, and nearly half (49%) felt confident about giving patients travel advice.
However, physicians’ preparedness gradually dropped for clinical situations requiring more direct experience with Zika. For example, 37% felt moderately or very prepared to provide clinical referrals for infant patients with an infection, and 33% felt prepared to talk with pregnant women about the risks of birth defects from Zika infection.
Just one in five physicians (22%) felt prepared for recommending Zika virus testing, and 16% felt prepared about providing data to the CDC’s U.S. Zika Pregnancy Registry or managing infants who had been prenatally exposed to Zika infection. Only 15% felt they had the preparedness to tell parents about social services for Zika-affected infants.
Preparedness did not differ by gender, specialty, practice setting, hours worked per week, or population density (urban, rural and suburban). However, differences did appear based on respondents’ age and U.S. region.
Older doctors reported greater knowledge about Zika than younger doctors. Compared with those aged 39 years or younger, those aged 40-49 and 50-59 reported feeling more knowledgeable (adjusted odds ratio, 1.74 and 1.72, respectively; P less than .05). The odds of feeling more knowledgeable was nearly triple among those aged at least 60 years, compared with those under 40 (aOR, 2.92; P less than .001).
Those practicing in the Northeast United States (aOR, 2.19; P less than .01) and in the South (aOR, 1.74; P less than .05) also reported feeling more knowledgeable than those in the West or Midwest.
“This makes sense because infants with a history of prenatal exposure to the Zika Virus are more likely to be seen in practices with more immigrants from the Caribbean and Latin America,” Dr. Houtrow said in an interview.
“ but the urgency of the need for education about Zika virus has diminished because the rates of new congenital Zika syndrome have dropped,” she continued.
Study limitations include the inability to generalize the findings beyond U.S. members of the AAP and the possibility that nonrespondents differed from respondents in terms of Zika knowledge and preparedness.
The research was funded by the AAP and CDC.
BALTIMORE – U.S. pediatricians feel comfortable providing patients with preventive information and travel advice related to Zika, but few feel prepared when it comes to testing and management of infants exposed prenatally to Zika infections, a study found.
“Areas where pediatricians were less likely to report preparedness included recommending testing, providing data to the Centers for Disease Control and Prevention’s Zika Pregnancy Registry, managing infants exposed to Zika prenatally, and informing parents of social services for Zika-infected infants,” senior author Amy J. Houtrow, MD, MPH, PhD, and colleagues reported at the Pediatric Academic Societies annual meeting.
“Results indicate that additional education efforts are needed to grow the overall Zika knowledge of pediatricians and boost preparedness, particularly around recommending Zika testing and providing data to CDC,” they concluded.
But these findings are not surprising given how rare congenital Zika virus syndrome is, explained Dr. Houtrow, an associate professor of physical medicine and rehabilitation and pediatrics at the University of Pittsburgh.
“For most rare conditions, pediatricians report better general than specific knowledge,” Dr. Houtrow said in an interview. “We expect pediatricians have a broad range of knowledge for a multitude of conditions and to be well versed in the care of infants and children with common conditions, coupled with the ability to access knowledge and expertise about rarer conditions such as congenital Zika syndrome.”
Dr. Houtrow and associates drew their findings from the 2018 AAP Periodic Survey of Fellows, which includes both primary care physicians and neonatologists. The survey’s response rate was 42%, with 672 of 1,599 surveys returned, but the researchers limited their analysis to 576 postresidency respondents who were providing direct patient care.
Overall, 39% of physicians reported being knowledgeable about Zika virus, and 47% said they wanted to learn more. More than half of responding doctors (57%) reported feeling moderately or very prepared when it came to informing patients of preventive measures to reduce risk of Zika infection, and nearly half (49%) felt confident about giving patients travel advice.
However, physicians’ preparedness gradually dropped for clinical situations requiring more direct experience with Zika. For example, 37% felt moderately or very prepared to provide clinical referrals for infant patients with an infection, and 33% felt prepared to talk with pregnant women about the risks of birth defects from Zika infection.
Just one in five physicians (22%) felt prepared for recommending Zika virus testing, and 16% felt prepared about providing data to the CDC’s U.S. Zika Pregnancy Registry or managing infants who had been prenatally exposed to Zika infection. Only 15% felt they had the preparedness to tell parents about social services for Zika-affected infants.
Preparedness did not differ by gender, specialty, practice setting, hours worked per week, or population density (urban, rural and suburban). However, differences did appear based on respondents’ age and U.S. region.
Older doctors reported greater knowledge about Zika than younger doctors. Compared with those aged 39 years or younger, those aged 40-49 and 50-59 reported feeling more knowledgeable (adjusted odds ratio, 1.74 and 1.72, respectively; P less than .05). The odds of feeling more knowledgeable was nearly triple among those aged at least 60 years, compared with those under 40 (aOR, 2.92; P less than .001).
Those practicing in the Northeast United States (aOR, 2.19; P less than .01) and in the South (aOR, 1.74; P less than .05) also reported feeling more knowledgeable than those in the West or Midwest.
“This makes sense because infants with a history of prenatal exposure to the Zika Virus are more likely to be seen in practices with more immigrants from the Caribbean and Latin America,” Dr. Houtrow said in an interview.
“ but the urgency of the need for education about Zika virus has diminished because the rates of new congenital Zika syndrome have dropped,” she continued.
Study limitations include the inability to generalize the findings beyond U.S. members of the AAP and the possibility that nonrespondents differed from respondents in terms of Zika knowledge and preparedness.
The research was funded by the AAP and CDC.
BALTIMORE – U.S. pediatricians feel comfortable providing patients with preventive information and travel advice related to Zika, but few feel prepared when it comes to testing and management of infants exposed prenatally to Zika infections, a study found.
“Areas where pediatricians were less likely to report preparedness included recommending testing, providing data to the Centers for Disease Control and Prevention’s Zika Pregnancy Registry, managing infants exposed to Zika prenatally, and informing parents of social services for Zika-infected infants,” senior author Amy J. Houtrow, MD, MPH, PhD, and colleagues reported at the Pediatric Academic Societies annual meeting.
“Results indicate that additional education efforts are needed to grow the overall Zika knowledge of pediatricians and boost preparedness, particularly around recommending Zika testing and providing data to CDC,” they concluded.
But these findings are not surprising given how rare congenital Zika virus syndrome is, explained Dr. Houtrow, an associate professor of physical medicine and rehabilitation and pediatrics at the University of Pittsburgh.
“For most rare conditions, pediatricians report better general than specific knowledge,” Dr. Houtrow said in an interview. “We expect pediatricians have a broad range of knowledge for a multitude of conditions and to be well versed in the care of infants and children with common conditions, coupled with the ability to access knowledge and expertise about rarer conditions such as congenital Zika syndrome.”
Dr. Houtrow and associates drew their findings from the 2018 AAP Periodic Survey of Fellows, which includes both primary care physicians and neonatologists. The survey’s response rate was 42%, with 672 of 1,599 surveys returned, but the researchers limited their analysis to 576 postresidency respondents who were providing direct patient care.
Overall, 39% of physicians reported being knowledgeable about Zika virus, and 47% said they wanted to learn more. More than half of responding doctors (57%) reported feeling moderately or very prepared when it came to informing patients of preventive measures to reduce risk of Zika infection, and nearly half (49%) felt confident about giving patients travel advice.
However, physicians’ preparedness gradually dropped for clinical situations requiring more direct experience with Zika. For example, 37% felt moderately or very prepared to provide clinical referrals for infant patients with an infection, and 33% felt prepared to talk with pregnant women about the risks of birth defects from Zika infection.
Just one in five physicians (22%) felt prepared for recommending Zika virus testing, and 16% felt prepared about providing data to the CDC’s U.S. Zika Pregnancy Registry or managing infants who had been prenatally exposed to Zika infection. Only 15% felt they had the preparedness to tell parents about social services for Zika-affected infants.
Preparedness did not differ by gender, specialty, practice setting, hours worked per week, or population density (urban, rural and suburban). However, differences did appear based on respondents’ age and U.S. region.
Older doctors reported greater knowledge about Zika than younger doctors. Compared with those aged 39 years or younger, those aged 40-49 and 50-59 reported feeling more knowledgeable (adjusted odds ratio, 1.74 and 1.72, respectively; P less than .05). The odds of feeling more knowledgeable was nearly triple among those aged at least 60 years, compared with those under 40 (aOR, 2.92; P less than .001).
Those practicing in the Northeast United States (aOR, 2.19; P less than .01) and in the South (aOR, 1.74; P less than .05) also reported feeling more knowledgeable than those in the West or Midwest.
“This makes sense because infants with a history of prenatal exposure to the Zika Virus are more likely to be seen in practices with more immigrants from the Caribbean and Latin America,” Dr. Houtrow said in an interview.
“ but the urgency of the need for education about Zika virus has diminished because the rates of new congenital Zika syndrome have dropped,” she continued.
Study limitations include the inability to generalize the findings beyond U.S. members of the AAP and the possibility that nonrespondents differed from respondents in terms of Zika knowledge and preparedness.
The research was funded by the AAP and CDC.
REPORTING FROM PAS 2019
Neurodevelopmental concerns may emerge later in Zika-exposed infants
BALTIMORE – Most infants prenatally exposed to Zika showed relatively normal neurodevelopment if their fetal MRI and birth head circumference were normal, but others with similarly initial normal measures appeared to struggle with social cognition and mobility as they got older, according to a new study.
“I think we need to be cautious with saying that these children are normal when these normal-appearing children may not be doing as well as we think,” lead author Sarah Mulkey, MD, of Children’s National Health System and George Washington University, Washington, said in an interview. “While most children are showing fairly normal development, there are some children who are … becoming more abnormal over time.”
Dr. Mulkey shared her findings at the Pediatric Academic Societies annual meeting. She and her colleagues had previously published a prospective study of 82 Zika-exposed infants’ fetal brain MRIs. In their new study, they followed up with the 78 Colombian infants from that study whose fetal neuroimaging and birth head circumstance had been normal.
The researchers used the Alberta Infant Motor Scale (AIMS) and the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) to evaluate 72 of the children, 34 of whom underwent assessment twice. Forty of the children were an average 5.7 months old when evaluated, and 66 were an average 13.5 months old.
As the children got older, their overall WIDEA z-score and their subscores in the social cognition domain and especially in the mobility domain trended downward. Three of the children had AIMS scores two standard deviations below normal, but the rest fell within the normal range.
Their WIDEA communication z-score hovered relatively close to the norm, but self-care also showed a very slight slope downward, albeit not as substantially as in the social cognition and mobility domains.
The younger a child is, the fewer skills they generally show related to neurocognitive development, Dr. Mulkey explained. But as they grow older and are expected to show more skills, it becomes more apparent where gaps and delays might exist.
“We can see that there are a lot of kids doing well, but some of these kids certainly are not,” she said. “Until children have a long time to develop, you really can’t see these changes unless you follow them long-term.”
The researchers also looked separately at a subgroup of 19 children (26%) whose cranial ultrasounds showed mild nonspecific findings. These findings – such as lenticulostriate vasculopathy, choroid plexus cysts, subependymal cysts and calcifications – do not usually indicate any problems, but they appeared in a quarter of this population, considerably more than the approximately 5% typically seen in the general population, Dr. Mulkey said.
Though the findings did not reach significance, infants in this subgroup tended to have a lower WIDEA mobility z-scores (P = .054) and lower AIMS scores (P = .26) than the Zika-exposed infants with normal cranial ultrasounds.
“Mild nonspecific cranial ultrasound findings may represent a mild injury” related to exposure to their mother’s Zika infection during pregnancy, the researchers suggested. “It may be a risk factor for the lower mobility outcome,” Dr. Mulkey said.
The researchers hope to continue later follow-ups as the children age.
The research was funded by the Thrasher Research Fund. Dr. Mulkey had no conflicts of interest.
BALTIMORE – Most infants prenatally exposed to Zika showed relatively normal neurodevelopment if their fetal MRI and birth head circumference were normal, but others with similarly initial normal measures appeared to struggle with social cognition and mobility as they got older, according to a new study.
“I think we need to be cautious with saying that these children are normal when these normal-appearing children may not be doing as well as we think,” lead author Sarah Mulkey, MD, of Children’s National Health System and George Washington University, Washington, said in an interview. “While most children are showing fairly normal development, there are some children who are … becoming more abnormal over time.”
Dr. Mulkey shared her findings at the Pediatric Academic Societies annual meeting. She and her colleagues had previously published a prospective study of 82 Zika-exposed infants’ fetal brain MRIs. In their new study, they followed up with the 78 Colombian infants from that study whose fetal neuroimaging and birth head circumstance had been normal.
The researchers used the Alberta Infant Motor Scale (AIMS) and the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) to evaluate 72 of the children, 34 of whom underwent assessment twice. Forty of the children were an average 5.7 months old when evaluated, and 66 were an average 13.5 months old.
As the children got older, their overall WIDEA z-score and their subscores in the social cognition domain and especially in the mobility domain trended downward. Three of the children had AIMS scores two standard deviations below normal, but the rest fell within the normal range.
Their WIDEA communication z-score hovered relatively close to the norm, but self-care also showed a very slight slope downward, albeit not as substantially as in the social cognition and mobility domains.
The younger a child is, the fewer skills they generally show related to neurocognitive development, Dr. Mulkey explained. But as they grow older and are expected to show more skills, it becomes more apparent where gaps and delays might exist.
“We can see that there are a lot of kids doing well, but some of these kids certainly are not,” she said. “Until children have a long time to develop, you really can’t see these changes unless you follow them long-term.”
The researchers also looked separately at a subgroup of 19 children (26%) whose cranial ultrasounds showed mild nonspecific findings. These findings – such as lenticulostriate vasculopathy, choroid plexus cysts, subependymal cysts and calcifications – do not usually indicate any problems, but they appeared in a quarter of this population, considerably more than the approximately 5% typically seen in the general population, Dr. Mulkey said.
Though the findings did not reach significance, infants in this subgroup tended to have a lower WIDEA mobility z-scores (P = .054) and lower AIMS scores (P = .26) than the Zika-exposed infants with normal cranial ultrasounds.
“Mild nonspecific cranial ultrasound findings may represent a mild injury” related to exposure to their mother’s Zika infection during pregnancy, the researchers suggested. “It may be a risk factor for the lower mobility outcome,” Dr. Mulkey said.
The researchers hope to continue later follow-ups as the children age.
The research was funded by the Thrasher Research Fund. Dr. Mulkey had no conflicts of interest.
BALTIMORE – Most infants prenatally exposed to Zika showed relatively normal neurodevelopment if their fetal MRI and birth head circumference were normal, but others with similarly initial normal measures appeared to struggle with social cognition and mobility as they got older, according to a new study.
“I think we need to be cautious with saying that these children are normal when these normal-appearing children may not be doing as well as we think,” lead author Sarah Mulkey, MD, of Children’s National Health System and George Washington University, Washington, said in an interview. “While most children are showing fairly normal development, there are some children who are … becoming more abnormal over time.”
Dr. Mulkey shared her findings at the Pediatric Academic Societies annual meeting. She and her colleagues had previously published a prospective study of 82 Zika-exposed infants’ fetal brain MRIs. In their new study, they followed up with the 78 Colombian infants from that study whose fetal neuroimaging and birth head circumstance had been normal.
The researchers used the Alberta Infant Motor Scale (AIMS) and the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) to evaluate 72 of the children, 34 of whom underwent assessment twice. Forty of the children were an average 5.7 months old when evaluated, and 66 were an average 13.5 months old.
As the children got older, their overall WIDEA z-score and their subscores in the social cognition domain and especially in the mobility domain trended downward. Three of the children had AIMS scores two standard deviations below normal, but the rest fell within the normal range.
Their WIDEA communication z-score hovered relatively close to the norm, but self-care also showed a very slight slope downward, albeit not as substantially as in the social cognition and mobility domains.
The younger a child is, the fewer skills they generally show related to neurocognitive development, Dr. Mulkey explained. But as they grow older and are expected to show more skills, it becomes more apparent where gaps and delays might exist.
“We can see that there are a lot of kids doing well, but some of these kids certainly are not,” she said. “Until children have a long time to develop, you really can’t see these changes unless you follow them long-term.”
The researchers also looked separately at a subgroup of 19 children (26%) whose cranial ultrasounds showed mild nonspecific findings. These findings – such as lenticulostriate vasculopathy, choroid plexus cysts, subependymal cysts and calcifications – do not usually indicate any problems, but they appeared in a quarter of this population, considerably more than the approximately 5% typically seen in the general population, Dr. Mulkey said.
Though the findings did not reach significance, infants in this subgroup tended to have a lower WIDEA mobility z-scores (P = .054) and lower AIMS scores (P = .26) than the Zika-exposed infants with normal cranial ultrasounds.
“Mild nonspecific cranial ultrasound findings may represent a mild injury” related to exposure to their mother’s Zika infection during pregnancy, the researchers suggested. “It may be a risk factor for the lower mobility outcome,” Dr. Mulkey said.
The researchers hope to continue later follow-ups as the children age.
The research was funded by the Thrasher Research Fund. Dr. Mulkey had no conflicts of interest.
REPORTING FROM PAS 2019
Key clinical point: .
Major finding: Zika-exposed infants with normal fetal MRI neuroimaging showed increasingly lower mobility and social cognition skills as they approached their first birthday.
Study details: The findings are based on neurodevelopmental assessments of 72 Zika-exposed Colombian children at 4-18 months old.
Disclosures: The research was funded by the Thrasher Research Fund. Dr. Mulkey had no conflicts of interest.
FDA committee advises status quo for blood supply Zika testing
Most members of a Food and Drug Administration advisory committee considered that data support maintaining current testing protocols for Zika virus in the blood donor pool. However, committee discussion entertained the idea of revisiting testing strategies after another year or 2 of Zika virus epidemiological data are available.
In its last guidance regarding Zika virus testing, issued in July 2018, the FDA recommended that either minipool nucleic acid testing (MP NAT) or individual donor (ID) NAT be used to screen for Zika virus. Current guidance still requires conversion to all-ID NAT “when certain threshold conditions are met that indicate an increased risk of suspected mosquito-borne transmission in a defined geographic collection area.”
In the first of three separate votes, 11 of 15 voting members of the FDA’s Blood Products Advisory Committee (BPAC) answered in the affirmative to the question of whether available data support continuing the status quo for Zika testing. Committee members then were asked to weigh whether current data support scaling back to a regional testing strategy targeting at-risk areas. Here, six committee members answered in the affirmative, and nine in the negative.
Just one committee member, F. Blaine Hollinger, MD, voted in favor of the third option, elimination of all Zika virus testing without reintroducing donor screening for risk factors in risk-free areas pending another outbreak in the United States. Dr. Hollinger is a professor of virology and microbiology at Baylor College of Medicine, Houston.
The committee as whole wasn’t swayed by a line of questioning put forward by chairman Richard Kaufman, MD. “I will be the devil’s advocate a little bit: We learned that there have been zero confirmed positives from blood donors for the past year. Would anyone be comfortable with just stopping screening of donors?” asked Dr. Kaufman, medical director of the adult transfusion service at Brigham and Women’s Hospital, Boston.
A wide-ranging morning of presentations put data regarding historical trends and current global Zika hot spots in front of the committee. Current upticks in infection rates in northwest Mexico and in some states in India were areas of concern, given North American travel patterns, noted speaker Marc Fisher, MD, of the Center for Disease Control and Prevention’s Arboviral Disease Branch (Fort Collins, Colo.) “We’re going to see sporadic outbreaks; it’s hard to predict the future,” he said. “The new outbreak in India raises concerns.”
Briefing information from the FDA explained that Zika virus local transmission peaked in the United States in late summer of 2016. More than 5,000 cases were reported in the United States and over 36,000 in Puerto Rico. This has plummeted to 220 in 2018, with about two-thirds of these cases occurring in the territories, mostly (97%) from Puerto Rico across all 3 years.
Zika viremic blood donors dropped by an order of magnitude yearly, totaling 363 in 2016, 38 in 2017, and just 3 in 2018. Of the 363 detected in 2016, 96% came from Puerto Rico or Florida, noted Dr. Fisher.
The number of suspected and confirmed cases in the Americas overall has also dropped from over 650,000 in 2016 to under 30,000 in 2018, with most cases in 2018 being suspected rather than laboratory confirmed. In contrast to testing conducted in North America, few cases in much of Central and South America were laboratory confirmed.
Asymptomatic infections have occurred in blood donors, said the FDA, with 1.8% of blood donations in Puerto Rico testing positive for Zika virus during the peak of the outbreak. Transmission by transfusion is thought to have occurred in Brazil.
Although Zika virus infections have plummeted in the United States and worldwide, prevalence and rates of local transmission are unpredictable, said the FDA, which pointed to sporadic increases in autochthonous transmission of viruses such as dengue and chikungunya that are carried by the same mosquito vector as Zika.
Some of the committee’s discussion centered around finding a way to carve out protection for those most harmed by Zika virus – pregnant women and their fetuses. Martin Schreiber, MD, professor of surgery at Oregon Health and Sciences University, Portland, proposed a point-of-care testing strategy in which only blood destined for pregnant women would be tested for Zika virus. Dr. Schreiber, a trauma surgeon, put forward the rationale that Zika virus causes harm almost exclusively to fetuses, except for rare cases of Guillain-Barré syndrome.
In response, Dr. Kaufman pointed out that with rare exceptions for some bacterial testing, all testing is done from samples taken at the point of donation. The supply chain for donor blood is not set up to accommodate point-of-care testing, he said.
Answering questions about another targeted strategy – maintaining a separate, Zika-tested supply of blood for pregnant women – Susan Stramer, PhD, vice president of scientific affairs for the American Red Cross, said, “Most hospitals do not want, and are very adamant against, carrying a dual inventory.”
Ultimately, the committee’s discussion swung toward the realization that it may be too soon after the recent spike in U.S. Zika cases to plot the best course for ongoing testing strategies. “We are at the tail end of a waning epidemic. ... I think it would probably be a pretty easy question for the committee and for the agency if we actually had some way of having a crystal ball and knowing that the current trend was likely to continue,” said Roger Lewis, MD, PhD, professor at the University of California, Los Angeles, and chair of the department of emergency medicine at Harbor-UCLA Medical Center.
“I think that is not the question,” he went on. “I think the question is, What is the optimal strategy if we have no idea if that tail is going to continue in this current trend. ... And that maybe the committee ought to be thinking about what is the right strategy for the next 2 years – with an underlying assumption that this is a question that can be brought back as we learn more about how this disease behaves.”
The FDA usually follows the recommendations of its advisory committees.
Most members of a Food and Drug Administration advisory committee considered that data support maintaining current testing protocols for Zika virus in the blood donor pool. However, committee discussion entertained the idea of revisiting testing strategies after another year or 2 of Zika virus epidemiological data are available.
In its last guidance regarding Zika virus testing, issued in July 2018, the FDA recommended that either minipool nucleic acid testing (MP NAT) or individual donor (ID) NAT be used to screen for Zika virus. Current guidance still requires conversion to all-ID NAT “when certain threshold conditions are met that indicate an increased risk of suspected mosquito-borne transmission in a defined geographic collection area.”
In the first of three separate votes, 11 of 15 voting members of the FDA’s Blood Products Advisory Committee (BPAC) answered in the affirmative to the question of whether available data support continuing the status quo for Zika testing. Committee members then were asked to weigh whether current data support scaling back to a regional testing strategy targeting at-risk areas. Here, six committee members answered in the affirmative, and nine in the negative.
Just one committee member, F. Blaine Hollinger, MD, voted in favor of the third option, elimination of all Zika virus testing without reintroducing donor screening for risk factors in risk-free areas pending another outbreak in the United States. Dr. Hollinger is a professor of virology and microbiology at Baylor College of Medicine, Houston.
The committee as whole wasn’t swayed by a line of questioning put forward by chairman Richard Kaufman, MD. “I will be the devil’s advocate a little bit: We learned that there have been zero confirmed positives from blood donors for the past year. Would anyone be comfortable with just stopping screening of donors?” asked Dr. Kaufman, medical director of the adult transfusion service at Brigham and Women’s Hospital, Boston.
A wide-ranging morning of presentations put data regarding historical trends and current global Zika hot spots in front of the committee. Current upticks in infection rates in northwest Mexico and in some states in India were areas of concern, given North American travel patterns, noted speaker Marc Fisher, MD, of the Center for Disease Control and Prevention’s Arboviral Disease Branch (Fort Collins, Colo.) “We’re going to see sporadic outbreaks; it’s hard to predict the future,” he said. “The new outbreak in India raises concerns.”
Briefing information from the FDA explained that Zika virus local transmission peaked in the United States in late summer of 2016. More than 5,000 cases were reported in the United States and over 36,000 in Puerto Rico. This has plummeted to 220 in 2018, with about two-thirds of these cases occurring in the territories, mostly (97%) from Puerto Rico across all 3 years.
Zika viremic blood donors dropped by an order of magnitude yearly, totaling 363 in 2016, 38 in 2017, and just 3 in 2018. Of the 363 detected in 2016, 96% came from Puerto Rico or Florida, noted Dr. Fisher.
The number of suspected and confirmed cases in the Americas overall has also dropped from over 650,000 in 2016 to under 30,000 in 2018, with most cases in 2018 being suspected rather than laboratory confirmed. In contrast to testing conducted in North America, few cases in much of Central and South America were laboratory confirmed.
Asymptomatic infections have occurred in blood donors, said the FDA, with 1.8% of blood donations in Puerto Rico testing positive for Zika virus during the peak of the outbreak. Transmission by transfusion is thought to have occurred in Brazil.
Although Zika virus infections have plummeted in the United States and worldwide, prevalence and rates of local transmission are unpredictable, said the FDA, which pointed to sporadic increases in autochthonous transmission of viruses such as dengue and chikungunya that are carried by the same mosquito vector as Zika.
Some of the committee’s discussion centered around finding a way to carve out protection for those most harmed by Zika virus – pregnant women and their fetuses. Martin Schreiber, MD, professor of surgery at Oregon Health and Sciences University, Portland, proposed a point-of-care testing strategy in which only blood destined for pregnant women would be tested for Zika virus. Dr. Schreiber, a trauma surgeon, put forward the rationale that Zika virus causes harm almost exclusively to fetuses, except for rare cases of Guillain-Barré syndrome.
In response, Dr. Kaufman pointed out that with rare exceptions for some bacterial testing, all testing is done from samples taken at the point of donation. The supply chain for donor blood is not set up to accommodate point-of-care testing, he said.
Answering questions about another targeted strategy – maintaining a separate, Zika-tested supply of blood for pregnant women – Susan Stramer, PhD, vice president of scientific affairs for the American Red Cross, said, “Most hospitals do not want, and are very adamant against, carrying a dual inventory.”
Ultimately, the committee’s discussion swung toward the realization that it may be too soon after the recent spike in U.S. Zika cases to plot the best course for ongoing testing strategies. “We are at the tail end of a waning epidemic. ... I think it would probably be a pretty easy question for the committee and for the agency if we actually had some way of having a crystal ball and knowing that the current trend was likely to continue,” said Roger Lewis, MD, PhD, professor at the University of California, Los Angeles, and chair of the department of emergency medicine at Harbor-UCLA Medical Center.
“I think that is not the question,” he went on. “I think the question is, What is the optimal strategy if we have no idea if that tail is going to continue in this current trend. ... And that maybe the committee ought to be thinking about what is the right strategy for the next 2 years – with an underlying assumption that this is a question that can be brought back as we learn more about how this disease behaves.”
The FDA usually follows the recommendations of its advisory committees.
Most members of a Food and Drug Administration advisory committee considered that data support maintaining current testing protocols for Zika virus in the blood donor pool. However, committee discussion entertained the idea of revisiting testing strategies after another year or 2 of Zika virus epidemiological data are available.
In its last guidance regarding Zika virus testing, issued in July 2018, the FDA recommended that either minipool nucleic acid testing (MP NAT) or individual donor (ID) NAT be used to screen for Zika virus. Current guidance still requires conversion to all-ID NAT “when certain threshold conditions are met that indicate an increased risk of suspected mosquito-borne transmission in a defined geographic collection area.”
In the first of three separate votes, 11 of 15 voting members of the FDA’s Blood Products Advisory Committee (BPAC) answered in the affirmative to the question of whether available data support continuing the status quo for Zika testing. Committee members then were asked to weigh whether current data support scaling back to a regional testing strategy targeting at-risk areas. Here, six committee members answered in the affirmative, and nine in the negative.
Just one committee member, F. Blaine Hollinger, MD, voted in favor of the third option, elimination of all Zika virus testing without reintroducing donor screening for risk factors in risk-free areas pending another outbreak in the United States. Dr. Hollinger is a professor of virology and microbiology at Baylor College of Medicine, Houston.
The committee as whole wasn’t swayed by a line of questioning put forward by chairman Richard Kaufman, MD. “I will be the devil’s advocate a little bit: We learned that there have been zero confirmed positives from blood donors for the past year. Would anyone be comfortable with just stopping screening of donors?” asked Dr. Kaufman, medical director of the adult transfusion service at Brigham and Women’s Hospital, Boston.
A wide-ranging morning of presentations put data regarding historical trends and current global Zika hot spots in front of the committee. Current upticks in infection rates in northwest Mexico and in some states in India were areas of concern, given North American travel patterns, noted speaker Marc Fisher, MD, of the Center for Disease Control and Prevention’s Arboviral Disease Branch (Fort Collins, Colo.) “We’re going to see sporadic outbreaks; it’s hard to predict the future,” he said. “The new outbreak in India raises concerns.”
Briefing information from the FDA explained that Zika virus local transmission peaked in the United States in late summer of 2016. More than 5,000 cases were reported in the United States and over 36,000 in Puerto Rico. This has plummeted to 220 in 2018, with about two-thirds of these cases occurring in the territories, mostly (97%) from Puerto Rico across all 3 years.
Zika viremic blood donors dropped by an order of magnitude yearly, totaling 363 in 2016, 38 in 2017, and just 3 in 2018. Of the 363 detected in 2016, 96% came from Puerto Rico or Florida, noted Dr. Fisher.
The number of suspected and confirmed cases in the Americas overall has also dropped from over 650,000 in 2016 to under 30,000 in 2018, with most cases in 2018 being suspected rather than laboratory confirmed. In contrast to testing conducted in North America, few cases in much of Central and South America were laboratory confirmed.
Asymptomatic infections have occurred in blood donors, said the FDA, with 1.8% of blood donations in Puerto Rico testing positive for Zika virus during the peak of the outbreak. Transmission by transfusion is thought to have occurred in Brazil.
Although Zika virus infections have plummeted in the United States and worldwide, prevalence and rates of local transmission are unpredictable, said the FDA, which pointed to sporadic increases in autochthonous transmission of viruses such as dengue and chikungunya that are carried by the same mosquito vector as Zika.
Some of the committee’s discussion centered around finding a way to carve out protection for those most harmed by Zika virus – pregnant women and their fetuses. Martin Schreiber, MD, professor of surgery at Oregon Health and Sciences University, Portland, proposed a point-of-care testing strategy in which only blood destined for pregnant women would be tested for Zika virus. Dr. Schreiber, a trauma surgeon, put forward the rationale that Zika virus causes harm almost exclusively to fetuses, except for rare cases of Guillain-Barré syndrome.
In response, Dr. Kaufman pointed out that with rare exceptions for some bacterial testing, all testing is done from samples taken at the point of donation. The supply chain for donor blood is not set up to accommodate point-of-care testing, he said.
Answering questions about another targeted strategy – maintaining a separate, Zika-tested supply of blood for pregnant women – Susan Stramer, PhD, vice president of scientific affairs for the American Red Cross, said, “Most hospitals do not want, and are very adamant against, carrying a dual inventory.”
Ultimately, the committee’s discussion swung toward the realization that it may be too soon after the recent spike in U.S. Zika cases to plot the best course for ongoing testing strategies. “We are at the tail end of a waning epidemic. ... I think it would probably be a pretty easy question for the committee and for the agency if we actually had some way of having a crystal ball and knowing that the current trend was likely to continue,” said Roger Lewis, MD, PhD, professor at the University of California, Los Angeles, and chair of the department of emergency medicine at Harbor-UCLA Medical Center.
“I think that is not the question,” he went on. “I think the question is, What is the optimal strategy if we have no idea if that tail is going to continue in this current trend. ... And that maybe the committee ought to be thinking about what is the right strategy for the next 2 years – with an underlying assumption that this is a question that can be brought back as we learn more about how this disease behaves.”
The FDA usually follows the recommendations of its advisory committees.
Dengue antibodies may reduce Zika infection risk
Previous dengue exposure may confer a protective effect against Zika virus infection, according to a paper published in Science.
In a prospective cohort study, researchers followed 1,453 urban residents in Salvador, Brazil, to assess the impact of the 2015 Zika virus outbreak in the region. Data on dengue immunity was available for 642 of these individuals.
Overall, 73% of the cohort were seropositive for Zika virus. However, the frequency of seropositivity varied significantly by location, from 29% in a valley in the northeastern sector of the study area to 83% in the southeast corner; the authors wrote that this was consistent with some form of acquired immunity “blunting the efficiency of transmission.”
When researchers looked at the relationship between prior immunity to the dengue virus and the risk of Zika infection, they found that each doubling of total IgG titers against dengue NS1 was associated with a 9% reduction in the risk of Zika virus infection.
Individuals in the highest tertile of dengue IgG titers showed a 44% reduction in the odds of Zika seropositivity, compared with individuals with no or low dengue IgG titers, while those in the middle tertile of dengue IgG titer had a 38% reduction.
“These findings provide empirical support for the hypothesis that accumulated immunity drove ZIKV [Zika virus] to local extinction by reducing the efficiency of transmission,” wrote Isabel Rodriguez-Barraquer, MD, PhD, from the department of medicine at the University of California, San Francisco, and her coauthors.
Individuals who were infected with the Zika virus but had high dengue IgG titers were significantly less likely to exhibit fever with viral infection, but had the same risk of developing rash as those with low or no IgG titers.
Researchers also examined the link between a subclass of IgG antibodies that are associated with more recent exposure to dengue virus – within the prior 6 months – and the risk of Zika virus infection. In contrast, they found that the levels of this subclass of antibodies, known as IgG3, were positively associated with an increased risk of Zika virus infection. Each doubling in IgG3 levels was associated with a 23% increase in the odds of being positive for Zika.
“This positive association might reflect an immune profile, in individuals who have experienced a recent DENV [dengue virus] infection, that is associated with having a greater risk of a subsequent ZIKV infection,” the authors wrote. “Alternatively, it is also possible that higher levels of IgG3 are a proxy for frequent DENV exposure and thus greater risk of infection by Aedes aegypti–transmitted viruses.”
The study was supported by Yale University, a number of Brazilian research organizations, the Research Support Foundation for the State of São Paulo, CuraZika Foundation, Wellcome Trust, and the National Institutes of Health. Three authors are listed on a patent application related to the work, and one reported an honoraria from Sanofi-Pasteur.
SOURCE: Rodriguez-Barraquer I et al. Science. 2019;36:607-10.
Previous dengue exposure may confer a protective effect against Zika virus infection, according to a paper published in Science.
In a prospective cohort study, researchers followed 1,453 urban residents in Salvador, Brazil, to assess the impact of the 2015 Zika virus outbreak in the region. Data on dengue immunity was available for 642 of these individuals.
Overall, 73% of the cohort were seropositive for Zika virus. However, the frequency of seropositivity varied significantly by location, from 29% in a valley in the northeastern sector of the study area to 83% in the southeast corner; the authors wrote that this was consistent with some form of acquired immunity “blunting the efficiency of transmission.”
When researchers looked at the relationship between prior immunity to the dengue virus and the risk of Zika infection, they found that each doubling of total IgG titers against dengue NS1 was associated with a 9% reduction in the risk of Zika virus infection.
Individuals in the highest tertile of dengue IgG titers showed a 44% reduction in the odds of Zika seropositivity, compared with individuals with no or low dengue IgG titers, while those in the middle tertile of dengue IgG titer had a 38% reduction.
“These findings provide empirical support for the hypothesis that accumulated immunity drove ZIKV [Zika virus] to local extinction by reducing the efficiency of transmission,” wrote Isabel Rodriguez-Barraquer, MD, PhD, from the department of medicine at the University of California, San Francisco, and her coauthors.
Individuals who were infected with the Zika virus but had high dengue IgG titers were significantly less likely to exhibit fever with viral infection, but had the same risk of developing rash as those with low or no IgG titers.
Researchers also examined the link between a subclass of IgG antibodies that are associated with more recent exposure to dengue virus – within the prior 6 months – and the risk of Zika virus infection. In contrast, they found that the levels of this subclass of antibodies, known as IgG3, were positively associated with an increased risk of Zika virus infection. Each doubling in IgG3 levels was associated with a 23% increase in the odds of being positive for Zika.
“This positive association might reflect an immune profile, in individuals who have experienced a recent DENV [dengue virus] infection, that is associated with having a greater risk of a subsequent ZIKV infection,” the authors wrote. “Alternatively, it is also possible that higher levels of IgG3 are a proxy for frequent DENV exposure and thus greater risk of infection by Aedes aegypti–transmitted viruses.”
The study was supported by Yale University, a number of Brazilian research organizations, the Research Support Foundation for the State of São Paulo, CuraZika Foundation, Wellcome Trust, and the National Institutes of Health. Three authors are listed on a patent application related to the work, and one reported an honoraria from Sanofi-Pasteur.
SOURCE: Rodriguez-Barraquer I et al. Science. 2019;36:607-10.
Previous dengue exposure may confer a protective effect against Zika virus infection, according to a paper published in Science.
In a prospective cohort study, researchers followed 1,453 urban residents in Salvador, Brazil, to assess the impact of the 2015 Zika virus outbreak in the region. Data on dengue immunity was available for 642 of these individuals.
Overall, 73% of the cohort were seropositive for Zika virus. However, the frequency of seropositivity varied significantly by location, from 29% in a valley in the northeastern sector of the study area to 83% in the southeast corner; the authors wrote that this was consistent with some form of acquired immunity “blunting the efficiency of transmission.”
When researchers looked at the relationship between prior immunity to the dengue virus and the risk of Zika infection, they found that each doubling of total IgG titers against dengue NS1 was associated with a 9% reduction in the risk of Zika virus infection.
Individuals in the highest tertile of dengue IgG titers showed a 44% reduction in the odds of Zika seropositivity, compared with individuals with no or low dengue IgG titers, while those in the middle tertile of dengue IgG titer had a 38% reduction.
“These findings provide empirical support for the hypothesis that accumulated immunity drove ZIKV [Zika virus] to local extinction by reducing the efficiency of transmission,” wrote Isabel Rodriguez-Barraquer, MD, PhD, from the department of medicine at the University of California, San Francisco, and her coauthors.
Individuals who were infected with the Zika virus but had high dengue IgG titers were significantly less likely to exhibit fever with viral infection, but had the same risk of developing rash as those with low or no IgG titers.
Researchers also examined the link between a subclass of IgG antibodies that are associated with more recent exposure to dengue virus – within the prior 6 months – and the risk of Zika virus infection. In contrast, they found that the levels of this subclass of antibodies, known as IgG3, were positively associated with an increased risk of Zika virus infection. Each doubling in IgG3 levels was associated with a 23% increase in the odds of being positive for Zika.
“This positive association might reflect an immune profile, in individuals who have experienced a recent DENV [dengue virus] infection, that is associated with having a greater risk of a subsequent ZIKV infection,” the authors wrote. “Alternatively, it is also possible that higher levels of IgG3 are a proxy for frequent DENV exposure and thus greater risk of infection by Aedes aegypti–transmitted viruses.”
The study was supported by Yale University, a number of Brazilian research organizations, the Research Support Foundation for the State of São Paulo, CuraZika Foundation, Wellcome Trust, and the National Institutes of Health. Three authors are listed on a patent application related to the work, and one reported an honoraria from Sanofi-Pasteur.
SOURCE: Rodriguez-Barraquer I et al. Science. 2019;36:607-10.
FROM SCIENCE
Key clinical point: Higher dengue antibody titers are associated with a lower risk of Zika virus infection.
Major finding: The highest tertile of dengue antibody titers was associated with a 44% reduction in the risk of Zika seropositivity.
Study details: A prospective cohort study of 1,453 residents in Salvador, Brazil.
Disclosures: The study was supported by Yale University, a number of Brazilian research organizations, the Research Support Foundation for the State of São Paulo, CuraZika Foundation, Wellcome Trust, and the National Institutes of Health. Three authors are listed on a patent application related to the work, and one reported an honoraria from Sanofi-Pasteur.
Source: Rodriguez-Barraquer I et al. Science. 2019;36:607-10.
Prenatal, postnatal neuroimaging IDs most Zika-related brain injuries
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
FROM JAMA PEDIATRICS
Key clinical point:
Major finding: In 82 pregnant women, prenatal neuroimaging identified fetal abnormalities in 3 cases, while postnatal neuroimaging in 53 of the remaining 79 cases yielded an additional 7 cases with mild abnormalities.
Study details: A prospective longitudinal cohort study of 82 pregnant women with clinical evidence of probable Zika infection in Colombia and the United States.
Disclosures: This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
Source: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26; doi: 10.1001/jamapediatrics.2018.4138.
Zika virus infection: Novel assay extends diagnostic window
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
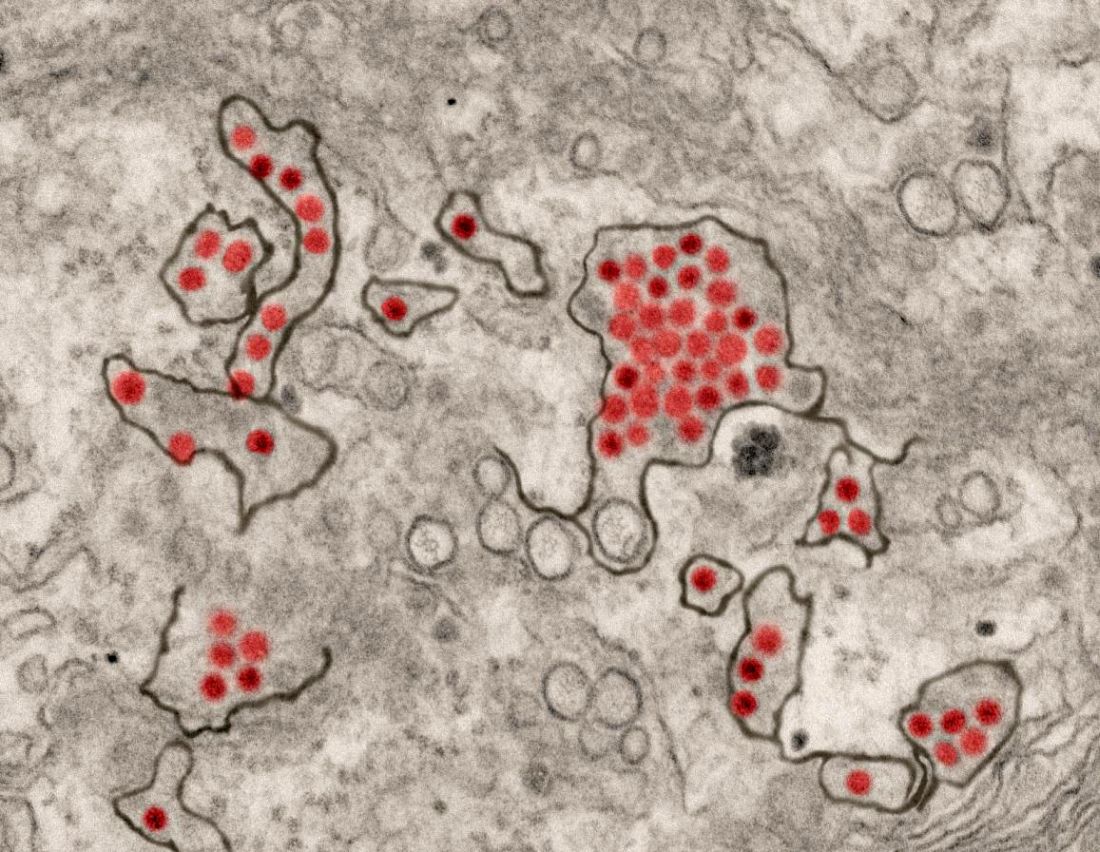
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
REPORTING FROM ICEID 2018
Key clinical point: A novel assay extends the time frame for diagnosing Zika virus infection.
Major finding: The PSQ assay detected and sequence confirmed Zika virus in all 60 samples; 40 negative control samples all tested negative.
Study details: An analysis of 60 tissue samples using a novel assay.
Disclosures: Dr. Bhatnagar reported having no disclosures.
Source: Bhatnagar J et al. ICEID 2018, Abstract O1.
Screen all infants exposed to Zika for eye abnormalities, study suggests
CNS abnormalities associated with antenatal Zika virus infection correlate strongly with opthalmic abnormalities, but there were cases of eye abnormalities in the absence of CNS abnormalities, which suggests a need for universal eye screening in endemic areas, according to a study published in Pediatrics.
Irena Tsui, MD, of the University of California, Los Angeles, and her associates examined 224 infants suspected of antenatal Zika virus infection for eye abnormalities between Jan. 2, 2016, and Feb. 28, 2017. They found that 40% had CNS abnormalities and 25% of all infants had eye abnormalities; of those 90 infants with CNS abnormalities, 54% had eye abnormalities, which makes for an odds ratio of 14.9 (P less than .0001). However, among the 134 infants without CNS abnormalities, 4% had eye abnormalities.
The study also investigated the existence of eye abnormalities among infants did not laboratory-confirmed diagnosis of Zika virus infection. To do so, they performed reverse transcriptase polymerase chain reaction (RT-PCR) testing on 189 infants. They found eye abnormalities among 22% of the 156 RT-PCR–positive infants and 38% of the 68 RT-PCR–unconfirmed infants. Among the 52% of infants with eye abnormalities who were reexamined, there were no signs of worsening, ongoing activity, or regression in their lesions.
The guidelines in Brazil, where the study was performed, recommend eye examinations only for infants with microcephaly, and the United States currently recommends it only at the discretion of the health care provider. The study investigators think that
“The early identification of eye abnormalities enables low-vision interventions to improve visual function with important repercussions for neurocognitive development,” they concluded.
SOURCE: Tsui I et al. Pediatrics. 2018 Oct;142(4):e20181104.
CNS abnormalities associated with antenatal Zika virus infection correlate strongly with opthalmic abnormalities, but there were cases of eye abnormalities in the absence of CNS abnormalities, which suggests a need for universal eye screening in endemic areas, according to a study published in Pediatrics.
Irena Tsui, MD, of the University of California, Los Angeles, and her associates examined 224 infants suspected of antenatal Zika virus infection for eye abnormalities between Jan. 2, 2016, and Feb. 28, 2017. They found that 40% had CNS abnormalities and 25% of all infants had eye abnormalities; of those 90 infants with CNS abnormalities, 54% had eye abnormalities, which makes for an odds ratio of 14.9 (P less than .0001). However, among the 134 infants without CNS abnormalities, 4% had eye abnormalities.
The study also investigated the existence of eye abnormalities among infants did not laboratory-confirmed diagnosis of Zika virus infection. To do so, they performed reverse transcriptase polymerase chain reaction (RT-PCR) testing on 189 infants. They found eye abnormalities among 22% of the 156 RT-PCR–positive infants and 38% of the 68 RT-PCR–unconfirmed infants. Among the 52% of infants with eye abnormalities who were reexamined, there were no signs of worsening, ongoing activity, or regression in their lesions.
The guidelines in Brazil, where the study was performed, recommend eye examinations only for infants with microcephaly, and the United States currently recommends it only at the discretion of the health care provider. The study investigators think that
“The early identification of eye abnormalities enables low-vision interventions to improve visual function with important repercussions for neurocognitive development,” they concluded.
SOURCE: Tsui I et al. Pediatrics. 2018 Oct;142(4):e20181104.
CNS abnormalities associated with antenatal Zika virus infection correlate strongly with opthalmic abnormalities, but there were cases of eye abnormalities in the absence of CNS abnormalities, which suggests a need for universal eye screening in endemic areas, according to a study published in Pediatrics.
Irena Tsui, MD, of the University of California, Los Angeles, and her associates examined 224 infants suspected of antenatal Zika virus infection for eye abnormalities between Jan. 2, 2016, and Feb. 28, 2017. They found that 40% had CNS abnormalities and 25% of all infants had eye abnormalities; of those 90 infants with CNS abnormalities, 54% had eye abnormalities, which makes for an odds ratio of 14.9 (P less than .0001). However, among the 134 infants without CNS abnormalities, 4% had eye abnormalities.
The study also investigated the existence of eye abnormalities among infants did not laboratory-confirmed diagnosis of Zika virus infection. To do so, they performed reverse transcriptase polymerase chain reaction (RT-PCR) testing on 189 infants. They found eye abnormalities among 22% of the 156 RT-PCR–positive infants and 38% of the 68 RT-PCR–unconfirmed infants. Among the 52% of infants with eye abnormalities who were reexamined, there were no signs of worsening, ongoing activity, or regression in their lesions.
The guidelines in Brazil, where the study was performed, recommend eye examinations only for infants with microcephaly, and the United States currently recommends it only at the discretion of the health care provider. The study investigators think that
“The early identification of eye abnormalities enables low-vision interventions to improve visual function with important repercussions for neurocognitive development,” they concluded.
SOURCE: Tsui I et al. Pediatrics. 2018 Oct;142(4):e20181104.
FROM PEDIATRICS
Epilepsy often accompanies congenital Zika infections
Epilepsy occurred in approximately two-thirds of infants with congenital Zika virus infection in a study of 141 children.
“When ZIKV [Zika virus] infection is acquired in utero, it may be associated with epilepsy, and we characterized aspects of this complication in a study performed at our referral center,” wrote Hélio van der Linden Jr., MD, of Dr. Henrique Santillo Rehabilitation and Readaptation Center in Goiânia, Brazil, and colleagues in a letter to the editor published in the New England Journal of Medicine.
The researchers reviewed data from 141 infants aged 1-14 months with a median age of 9 months and Zika virus infection confirmed by laboratory analysis; 55% were girls.
The prevalence of epilepsy was 67%, with a mean age at onset of 4.9 months. Based on data provided by parents, 74% of the children experienced seizures at 6 months of age or younger.
Overall, 77% of the infants experienced a single type of seizure. Epileptic spasms, the most common type, occurred in 72% of infants, followed by focal motor seizure (21%) and tonic seizures (4%).
All 95 epileptic infants were treated with antiepileptic medications and 62 (65%) achieved remission. Of those in remission, 24 (39%) received monotherapy and 38 (61%) received polytherapy. The drugs most associated with seizure control were vigabatrin, levetiracetam, valproate, and phenobarbital.
The prevalence of epilepsy in this study was higher than that seen in previous studies, and most patients had early-onset, drug-resistant epilepsy, the researchers noted. However, burst-suppression patterns and hypsarrhythmia on EEG predicted more severe disease and suggest that epilepsy might complicate cases of congenital Zika infection, they said.
The researchers had no financial conflicts to disclose.
SOURCE: van der Linden H et al. N Engl J Med. 2018 Aug 30. doi: 10.1056/NEJMc1716070.
Epilepsy occurred in approximately two-thirds of infants with congenital Zika virus infection in a study of 141 children.
“When ZIKV [Zika virus] infection is acquired in utero, it may be associated with epilepsy, and we characterized aspects of this complication in a study performed at our referral center,” wrote Hélio van der Linden Jr., MD, of Dr. Henrique Santillo Rehabilitation and Readaptation Center in Goiânia, Brazil, and colleagues in a letter to the editor published in the New England Journal of Medicine.
The researchers reviewed data from 141 infants aged 1-14 months with a median age of 9 months and Zika virus infection confirmed by laboratory analysis; 55% were girls.
The prevalence of epilepsy was 67%, with a mean age at onset of 4.9 months. Based on data provided by parents, 74% of the children experienced seizures at 6 months of age or younger.
Overall, 77% of the infants experienced a single type of seizure. Epileptic spasms, the most common type, occurred in 72% of infants, followed by focal motor seizure (21%) and tonic seizures (4%).
All 95 epileptic infants were treated with antiepileptic medications and 62 (65%) achieved remission. Of those in remission, 24 (39%) received monotherapy and 38 (61%) received polytherapy. The drugs most associated with seizure control were vigabatrin, levetiracetam, valproate, and phenobarbital.
The prevalence of epilepsy in this study was higher than that seen in previous studies, and most patients had early-onset, drug-resistant epilepsy, the researchers noted. However, burst-suppression patterns and hypsarrhythmia on EEG predicted more severe disease and suggest that epilepsy might complicate cases of congenital Zika infection, they said.
The researchers had no financial conflicts to disclose.
SOURCE: van der Linden H et al. N Engl J Med. 2018 Aug 30. doi: 10.1056/NEJMc1716070.
Epilepsy occurred in approximately two-thirds of infants with congenital Zika virus infection in a study of 141 children.
“When ZIKV [Zika virus] infection is acquired in utero, it may be associated with epilepsy, and we characterized aspects of this complication in a study performed at our referral center,” wrote Hélio van der Linden Jr., MD, of Dr. Henrique Santillo Rehabilitation and Readaptation Center in Goiânia, Brazil, and colleagues in a letter to the editor published in the New England Journal of Medicine.
The researchers reviewed data from 141 infants aged 1-14 months with a median age of 9 months and Zika virus infection confirmed by laboratory analysis; 55% were girls.
The prevalence of epilepsy was 67%, with a mean age at onset of 4.9 months. Based on data provided by parents, 74% of the children experienced seizures at 6 months of age or younger.
Overall, 77% of the infants experienced a single type of seizure. Epileptic spasms, the most common type, occurred in 72% of infants, followed by focal motor seizure (21%) and tonic seizures (4%).
All 95 epileptic infants were treated with antiepileptic medications and 62 (65%) achieved remission. Of those in remission, 24 (39%) received monotherapy and 38 (61%) received polytherapy. The drugs most associated with seizure control were vigabatrin, levetiracetam, valproate, and phenobarbital.
The prevalence of epilepsy in this study was higher than that seen in previous studies, and most patients had early-onset, drug-resistant epilepsy, the researchers noted. However, burst-suppression patterns and hypsarrhythmia on EEG predicted more severe disease and suggest that epilepsy might complicate cases of congenital Zika infection, they said.
The researchers had no financial conflicts to disclose.
SOURCE: van der Linden H et al. N Engl J Med. 2018 Aug 30. doi: 10.1056/NEJMc1716070.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Epilepsy occurred in 67% of 141 infants with congenital Zika infections.
Study details: The data come from 141 infants aged 1-14 months with congenital Zika infections.
Disclosures: The researchers had no financial conflicts to disclose.
Source: van der Linden H et al. N Engl J Med. 2018 Aug 30. doi: 10.1056/NEJMc1716070.
Zika virus vaccine trial launches
A first-in-human trial of a live, attenuated Zika virus vaccine has begun, according to an announcement by the National Institutes of Health.
The vaccine, developed by scientists at the National Institute of Allergy and Infectious Diseases will be tested in 28 healthy, nonpregnant adults aged 18-50 years at two centers, the Johns Hopkins Bloomberg School of Public Health Center for Immunization Research in Baltimore, and the Vaccine Testing Center at the University of Vermont in Burlington.
The challenge virus in the vaccine is an attenuated genetic chimera consisting of a dengue virus 4 backbone that expresses Zika virus surface proteins designed to elicit an immune response. The virus was previously tested in rhesus macaque monkeys.
Study participants for the phase 1 trial, Evaluation of the Safety and Immunogenicity of the Live Attenuated Zika Vaccine rZIKV/D4Δ30-713 in Flavivirus-Naive Adults, (NCT03611946) will be assessed based on local and general adverse events to the vaccine and peak neutralizing antibody titer to Zika virus as measured up to 90 days after vaccination. The trial is expected to be reach primary completion by Dec. 31, 2018.
If the phase 1 trial is successful, the goal is to integrate the vaccine with a live, attenuated dengue vaccine candidate called TV003, which is designed to elicit antibodies against all four dengue virus serotypes. The TV003 experimental vaccine is currently under evaluation in a phase 3 clinical trial (NCT02406729) underway in Brazil. Both Zika and dengue viruses frequently are endemic in the same regions and a single vaccine against both diseases would be valued. Stephen Whitehead, PhD of NIAID’s Laboratory of Viral Diseases led the efforts to develop both experimental vaccines.
SOURCE: NIH, August 16, 2018. News Release.
A first-in-human trial of a live, attenuated Zika virus vaccine has begun, according to an announcement by the National Institutes of Health.
The vaccine, developed by scientists at the National Institute of Allergy and Infectious Diseases will be tested in 28 healthy, nonpregnant adults aged 18-50 years at two centers, the Johns Hopkins Bloomberg School of Public Health Center for Immunization Research in Baltimore, and the Vaccine Testing Center at the University of Vermont in Burlington.
The challenge virus in the vaccine is an attenuated genetic chimera consisting of a dengue virus 4 backbone that expresses Zika virus surface proteins designed to elicit an immune response. The virus was previously tested in rhesus macaque monkeys.
Study participants for the phase 1 trial, Evaluation of the Safety and Immunogenicity of the Live Attenuated Zika Vaccine rZIKV/D4Δ30-713 in Flavivirus-Naive Adults, (NCT03611946) will be assessed based on local and general adverse events to the vaccine and peak neutralizing antibody titer to Zika virus as measured up to 90 days after vaccination. The trial is expected to be reach primary completion by Dec. 31, 2018.
If the phase 1 trial is successful, the goal is to integrate the vaccine with a live, attenuated dengue vaccine candidate called TV003, which is designed to elicit antibodies against all four dengue virus serotypes. The TV003 experimental vaccine is currently under evaluation in a phase 3 clinical trial (NCT02406729) underway in Brazil. Both Zika and dengue viruses frequently are endemic in the same regions and a single vaccine against both diseases would be valued. Stephen Whitehead, PhD of NIAID’s Laboratory of Viral Diseases led the efforts to develop both experimental vaccines.
SOURCE: NIH, August 16, 2018. News Release.
A first-in-human trial of a live, attenuated Zika virus vaccine has begun, according to an announcement by the National Institutes of Health.
The vaccine, developed by scientists at the National Institute of Allergy and Infectious Diseases will be tested in 28 healthy, nonpregnant adults aged 18-50 years at two centers, the Johns Hopkins Bloomberg School of Public Health Center for Immunization Research in Baltimore, and the Vaccine Testing Center at the University of Vermont in Burlington.
The challenge virus in the vaccine is an attenuated genetic chimera consisting of a dengue virus 4 backbone that expresses Zika virus surface proteins designed to elicit an immune response. The virus was previously tested in rhesus macaque monkeys.
Study participants for the phase 1 trial, Evaluation of the Safety and Immunogenicity of the Live Attenuated Zika Vaccine rZIKV/D4Δ30-713 in Flavivirus-Naive Adults, (NCT03611946) will be assessed based on local and general adverse events to the vaccine and peak neutralizing antibody titer to Zika virus as measured up to 90 days after vaccination. The trial is expected to be reach primary completion by Dec. 31, 2018.
If the phase 1 trial is successful, the goal is to integrate the vaccine with a live, attenuated dengue vaccine candidate called TV003, which is designed to elicit antibodies against all four dengue virus serotypes. The TV003 experimental vaccine is currently under evaluation in a phase 3 clinical trial (NCT02406729) underway in Brazil. Both Zika and dengue viruses frequently are endemic in the same regions and a single vaccine against both diseases would be valued. Stephen Whitehead, PhD of NIAID’s Laboratory of Viral Diseases led the efforts to develop both experimental vaccines.
SOURCE: NIH, August 16, 2018. News Release.
1 in 7 Zika-exposed babies have at least one health problem related to the virus
About 14% of 1-year-olds with prenatal Zika virus exposure show at least one health problem probably related to the virus, according to a study published in Morbidity and Mortality Weekly Report.
Many of the problems are brain and eye abnormalities, which occurred at 30 times the 0.16% background rate among unexposed babies, Margaret Honein, PhD, and colleagues reported.
In a press briefing, Dr. Honein, chief of the Birth Defects Branch at the National Center on Birth Defects and Developmental Disabilities, described findings from the U.S. Zika Pregnancy and Infant Registry (USZPIR).
“Today’s report is the largest to date with long-term outcomes of babies born to mothers with [lab-confirmed] Zika infections, and the first published data on children 1 year or older from the ongoing surveillance network,” Dr. Honein said. It “clearly shows that the Zika story is not over, especially for the children and families who are affected by it.”
USZPIR is monitoring the outcomes of 7,300 pregnancies with lab-confirmed Zika infection. From these, 4,800 babies were born in the U.S. territories and freely associated states, had reached the age of 1 year by Feb. 1, 2018, and were included in the study.
In addition to clinical outcomes, the investigators looked at how many babies received the recommended evaluations, including neuroimaging, hearing screens, opthalmologic exams, developmental screening, and physical exams.
Almost all (95%) had at least one exam in the first 2 weeks of life; 76% had at least one developmental screening; 60% had postnatal neuroimaging; 48% at least one hearing exam; and 36% at least one eye exam by a specialist, the investigators found.
Findings that many didn’t get all the recommended health screenings are concerning, CDC Director Robert Redfield, MD. said during the briefing. “We are still learning about the full range of long-term health problems these babies could face. We thank clinicians for their continued commitment to conduct all necessary tests and evaluations to ensure appropriate care.”
Zika-associated birth defects occurred 203 babies (14%). Another 136 (9%) had at least one neurodevelopmental abnormality possibly associated with congenital Zika virus infection, and 20 (1%) had both. Most babies (1,386; 96%) did not have microcephaly detected at birth. But there was some “misclassification” of the condition, the investigators found. “Five infants had microcephaly at birth with brain or eye anomalies identified at birth; 59 had microcephaly at birth with no brain or eye anomalies identified at birth; and 20 infants did not have microcephaly identified at birth but had postnatal identification of microcephaly.”
Neurodevelopmental abnormalities possibly associated with Zika occurred in 136 (9%) of the cohort; 116 (8%) had no Zika-associated birth defects. Among these, half (58) had only possible developmental delay.
Zika transmission appears to be slowing, Lyle Peterson, MD, said during the press briefing, with no cases in the continental U.S. since 2017. That year, there were two cases in Florida and five in Texas. However, it is now endemic in many regions. Everyone should continue to take precautions against mosquito bites, he urged.
The MMWR also included updated guidance for men who are planning a pregnancy with a partner and may have been exposed to Zika.
CDC now recommends that these men wait at least 3 months after onset of Zika symptoms or any possible exposure, including travel to or living in a risk area. Past guidance recommended a 6-month waiting period. The new recommendation reflects emerging data suggesting that the risk of infectious Zika in semen declines during the 3 months after symptom onset.
Men who want to avoid passing Zika through sex should abstain for 3 months, or use a condom every time they have sex, the new recommendation said.
“All other Zika guidance remains unchanged,” the guidelines note. “Men with possible Zika virus exposure whose partner is pregnant should use condoms or the couple should not have sex for the entire pregnancy to reduce the risk of transmission.”
SOURCE: Honein, MA et al. MMWR 2018; 67: 1-10.
About 14% of 1-year-olds with prenatal Zika virus exposure show at least one health problem probably related to the virus, according to a study published in Morbidity and Mortality Weekly Report.
Many of the problems are brain and eye abnormalities, which occurred at 30 times the 0.16% background rate among unexposed babies, Margaret Honein, PhD, and colleagues reported.
In a press briefing, Dr. Honein, chief of the Birth Defects Branch at the National Center on Birth Defects and Developmental Disabilities, described findings from the U.S. Zika Pregnancy and Infant Registry (USZPIR).
“Today’s report is the largest to date with long-term outcomes of babies born to mothers with [lab-confirmed] Zika infections, and the first published data on children 1 year or older from the ongoing surveillance network,” Dr. Honein said. It “clearly shows that the Zika story is not over, especially for the children and families who are affected by it.”
USZPIR is monitoring the outcomes of 7,300 pregnancies with lab-confirmed Zika infection. From these, 4,800 babies were born in the U.S. territories and freely associated states, had reached the age of 1 year by Feb. 1, 2018, and were included in the study.
In addition to clinical outcomes, the investigators looked at how many babies received the recommended evaluations, including neuroimaging, hearing screens, opthalmologic exams, developmental screening, and physical exams.
Almost all (95%) had at least one exam in the first 2 weeks of life; 76% had at least one developmental screening; 60% had postnatal neuroimaging; 48% at least one hearing exam; and 36% at least one eye exam by a specialist, the investigators found.
Findings that many didn’t get all the recommended health screenings are concerning, CDC Director Robert Redfield, MD. said during the briefing. “We are still learning about the full range of long-term health problems these babies could face. We thank clinicians for their continued commitment to conduct all necessary tests and evaluations to ensure appropriate care.”
Zika-associated birth defects occurred 203 babies (14%). Another 136 (9%) had at least one neurodevelopmental abnormality possibly associated with congenital Zika virus infection, and 20 (1%) had both. Most babies (1,386; 96%) did not have microcephaly detected at birth. But there was some “misclassification” of the condition, the investigators found. “Five infants had microcephaly at birth with brain or eye anomalies identified at birth; 59 had microcephaly at birth with no brain or eye anomalies identified at birth; and 20 infants did not have microcephaly identified at birth but had postnatal identification of microcephaly.”
Neurodevelopmental abnormalities possibly associated with Zika occurred in 136 (9%) of the cohort; 116 (8%) had no Zika-associated birth defects. Among these, half (58) had only possible developmental delay.
Zika transmission appears to be slowing, Lyle Peterson, MD, said during the press briefing, with no cases in the continental U.S. since 2017. That year, there were two cases in Florida and five in Texas. However, it is now endemic in many regions. Everyone should continue to take precautions against mosquito bites, he urged.
The MMWR also included updated guidance for men who are planning a pregnancy with a partner and may have been exposed to Zika.
CDC now recommends that these men wait at least 3 months after onset of Zika symptoms or any possible exposure, including travel to or living in a risk area. Past guidance recommended a 6-month waiting period. The new recommendation reflects emerging data suggesting that the risk of infectious Zika in semen declines during the 3 months after symptom onset.
Men who want to avoid passing Zika through sex should abstain for 3 months, or use a condom every time they have sex, the new recommendation said.
“All other Zika guidance remains unchanged,” the guidelines note. “Men with possible Zika virus exposure whose partner is pregnant should use condoms or the couple should not have sex for the entire pregnancy to reduce the risk of transmission.”
SOURCE: Honein, MA et al. MMWR 2018; 67: 1-10.
About 14% of 1-year-olds with prenatal Zika virus exposure show at least one health problem probably related to the virus, according to a study published in Morbidity and Mortality Weekly Report.
Many of the problems are brain and eye abnormalities, which occurred at 30 times the 0.16% background rate among unexposed babies, Margaret Honein, PhD, and colleagues reported.
In a press briefing, Dr. Honein, chief of the Birth Defects Branch at the National Center on Birth Defects and Developmental Disabilities, described findings from the U.S. Zika Pregnancy and Infant Registry (USZPIR).
“Today’s report is the largest to date with long-term outcomes of babies born to mothers with [lab-confirmed] Zika infections, and the first published data on children 1 year or older from the ongoing surveillance network,” Dr. Honein said. It “clearly shows that the Zika story is not over, especially for the children and families who are affected by it.”
USZPIR is monitoring the outcomes of 7,300 pregnancies with lab-confirmed Zika infection. From these, 4,800 babies were born in the U.S. territories and freely associated states, had reached the age of 1 year by Feb. 1, 2018, and were included in the study.
In addition to clinical outcomes, the investigators looked at how many babies received the recommended evaluations, including neuroimaging, hearing screens, opthalmologic exams, developmental screening, and physical exams.
Almost all (95%) had at least one exam in the first 2 weeks of life; 76% had at least one developmental screening; 60% had postnatal neuroimaging; 48% at least one hearing exam; and 36% at least one eye exam by a specialist, the investigators found.
Findings that many didn’t get all the recommended health screenings are concerning, CDC Director Robert Redfield, MD. said during the briefing. “We are still learning about the full range of long-term health problems these babies could face. We thank clinicians for their continued commitment to conduct all necessary tests and evaluations to ensure appropriate care.”
Zika-associated birth defects occurred 203 babies (14%). Another 136 (9%) had at least one neurodevelopmental abnormality possibly associated with congenital Zika virus infection, and 20 (1%) had both. Most babies (1,386; 96%) did not have microcephaly detected at birth. But there was some “misclassification” of the condition, the investigators found. “Five infants had microcephaly at birth with brain or eye anomalies identified at birth; 59 had microcephaly at birth with no brain or eye anomalies identified at birth; and 20 infants did not have microcephaly identified at birth but had postnatal identification of microcephaly.”
Neurodevelopmental abnormalities possibly associated with Zika occurred in 136 (9%) of the cohort; 116 (8%) had no Zika-associated birth defects. Among these, half (58) had only possible developmental delay.
Zika transmission appears to be slowing, Lyle Peterson, MD, said during the press briefing, with no cases in the continental U.S. since 2017. That year, there were two cases in Florida and five in Texas. However, it is now endemic in many regions. Everyone should continue to take precautions against mosquito bites, he urged.
The MMWR also included updated guidance for men who are planning a pregnancy with a partner and may have been exposed to Zika.
CDC now recommends that these men wait at least 3 months after onset of Zika symptoms or any possible exposure, including travel to or living in a risk area. Past guidance recommended a 6-month waiting period. The new recommendation reflects emerging data suggesting that the risk of infectious Zika in semen declines during the 3 months after symptom onset.
Men who want to avoid passing Zika through sex should abstain for 3 months, or use a condom every time they have sex, the new recommendation said.
“All other Zika guidance remains unchanged,” the guidelines note. “Men with possible Zika virus exposure whose partner is pregnant should use condoms or the couple should not have sex for the entire pregnancy to reduce the risk of transmission.”
SOURCE: Honein, MA et al. MMWR 2018; 67: 1-10.
FROM MMWR
Key clinical point: Zika-related health problems are present in a substantial number of prenatally exposed babies.
Major finding: Problems occurred in 14% of 4,800 included in a national registry.
Study details: USZPIR is monitoring the outcomes of 7,300 pregnancies with lab-confirmed Zika infection. Disclosures: No relevant conflicts of interest were disclosed.
Source: Honein, MA et al. MMWR 2018; 67: 1-10.