User login
Service Connection Expanded to Additional Cancers
The US Department of Veterans Affairs (VA) is "lowering the burden of proof" for thousands, making acute and chronic leukemias, multiple myelomas, myelodysplastic syndromes, myelofibrosis, urinary bladder, ureter, and related genitourinary cancers presumptive for service connection.
The Jan. 8 decision included Gulf War veterans, those who served in Somalia or the Southwest Asia theater of operations during the Persian Gulf War on or after Aug. 2, 1990; and post-9/11 veterans, those who served in Afghanistan, Iraq, Djibouti, Egypt, Jordan, Lebanon, Syria, Yemen, or Uzbekistan and the airspace above these locations during the Gulf War on or after Sept. 11, 2001. It also includes veterans who served at the Karshi-Khanabad (K2) base in Uzbekistan after Sept. 11, 2001.
Veterans no longer must prove their service caused their condition to receive benefits. This landmark decision allows them access to free health care for that condition.
According to the VA, these steps are also part of a comprehensive effort to ensure that K2 veterans—and their survivors—receive the care and benefits they deserve. K2 veterans have higher claim and approval rates than any other cohort of veterans: 13,002 are enrolled in VA health care, and the average K2 veteran is service connected for 14.6 conditions.
The 2022 PACT Act was the largest expansion of veteran benefits in generations. The VA then made millions of veterans eligible for health care and benefits years earlier than called for by the law. It also launched the largest outreach campaign in the history of the VA to encourage veterans to apply.
Nearly 890,000 veterans have signed up for VA health care since the bill was signed into law, a nearly 40% increase over the previous equivalent period, and veterans have submitted > 4.8 million applications for VA benefits (a 42% increase over the previous equivalent period and an all-time record). The VA has delivered > $600 billion in earned benefits directly to veterans, their families, and survivors during that time.
The VA encourages all eligible veterans—including those with previously denied claims—to apply for benefits. To apply for benefits, veterans and survivors may visit VA.gov or call 1-800-MYVA411.
The US Department of Veterans Affairs (VA) is "lowering the burden of proof" for thousands, making acute and chronic leukemias, multiple myelomas, myelodysplastic syndromes, myelofibrosis, urinary bladder, ureter, and related genitourinary cancers presumptive for service connection.
The Jan. 8 decision included Gulf War veterans, those who served in Somalia or the Southwest Asia theater of operations during the Persian Gulf War on or after Aug. 2, 1990; and post-9/11 veterans, those who served in Afghanistan, Iraq, Djibouti, Egypt, Jordan, Lebanon, Syria, Yemen, or Uzbekistan and the airspace above these locations during the Gulf War on or after Sept. 11, 2001. It also includes veterans who served at the Karshi-Khanabad (K2) base in Uzbekistan after Sept. 11, 2001.
Veterans no longer must prove their service caused their condition to receive benefits. This landmark decision allows them access to free health care for that condition.
According to the VA, these steps are also part of a comprehensive effort to ensure that K2 veterans—and their survivors—receive the care and benefits they deserve. K2 veterans have higher claim and approval rates than any other cohort of veterans: 13,002 are enrolled in VA health care, and the average K2 veteran is service connected for 14.6 conditions.
The 2022 PACT Act was the largest expansion of veteran benefits in generations. The VA then made millions of veterans eligible for health care and benefits years earlier than called for by the law. It also launched the largest outreach campaign in the history of the VA to encourage veterans to apply.
Nearly 890,000 veterans have signed up for VA health care since the bill was signed into law, a nearly 40% increase over the previous equivalent period, and veterans have submitted > 4.8 million applications for VA benefits (a 42% increase over the previous equivalent period and an all-time record). The VA has delivered > $600 billion in earned benefits directly to veterans, their families, and survivors during that time.
The VA encourages all eligible veterans—including those with previously denied claims—to apply for benefits. To apply for benefits, veterans and survivors may visit VA.gov or call 1-800-MYVA411.
The US Department of Veterans Affairs (VA) is "lowering the burden of proof" for thousands, making acute and chronic leukemias, multiple myelomas, myelodysplastic syndromes, myelofibrosis, urinary bladder, ureter, and related genitourinary cancers presumptive for service connection.
The Jan. 8 decision included Gulf War veterans, those who served in Somalia or the Southwest Asia theater of operations during the Persian Gulf War on or after Aug. 2, 1990; and post-9/11 veterans, those who served in Afghanistan, Iraq, Djibouti, Egypt, Jordan, Lebanon, Syria, Yemen, or Uzbekistan and the airspace above these locations during the Gulf War on or after Sept. 11, 2001. It also includes veterans who served at the Karshi-Khanabad (K2) base in Uzbekistan after Sept. 11, 2001.
Veterans no longer must prove their service caused their condition to receive benefits. This landmark decision allows them access to free health care for that condition.
According to the VA, these steps are also part of a comprehensive effort to ensure that K2 veterans—and their survivors—receive the care and benefits they deserve. K2 veterans have higher claim and approval rates than any other cohort of veterans: 13,002 are enrolled in VA health care, and the average K2 veteran is service connected for 14.6 conditions.
The 2022 PACT Act was the largest expansion of veteran benefits in generations. The VA then made millions of veterans eligible for health care and benefits years earlier than called for by the law. It also launched the largest outreach campaign in the history of the VA to encourage veterans to apply.
Nearly 890,000 veterans have signed up for VA health care since the bill was signed into law, a nearly 40% increase over the previous equivalent period, and veterans have submitted > 4.8 million applications for VA benefits (a 42% increase over the previous equivalent period and an all-time record). The VA has delivered > $600 billion in earned benefits directly to veterans, their families, and survivors during that time.
The VA encourages all eligible veterans—including those with previously denied claims—to apply for benefits. To apply for benefits, veterans and survivors may visit VA.gov or call 1-800-MYVA411.
VA Performs Its First ‘Bloodless’ Stem Cell Transplant
PHOENIX ‑ A US Department of Veterans Affairs (VA) hospital in Tennessee has performed the first “bloodless” autologous stem cell transplant within the Veterans Health Administration, treating a 61-year-old Jehovah’s Witness patient with multiple myeloma who traveled from California for the procedure.
The case, presented at the annual meeting of the Association of VA Hematology/Oncology, stated that “we should not withhold any therapies for patients who are Jehovah’s Witnesses out of fear of them bleeding out or having complications from anemia,” said Bhagirathbhai Dholaria, MBBS, an associate professor of medicine at Vanderbilt University Medical Center who worked with the VA Tennessee Valley Healthcare System in Nashville.
While Jehovah’s Witnesses accept medical treatment, their faith forbids blood transfusions, including of preoperative autologous blood, due to its interpretation of the Bible. The faith allows individuals to decide whether to accept stem cells collected from their blood or someone else’s “provided that blood components are not intentionally collected, stored, and reinfused along with the stem cells.”
There are an estimated 1.2 million Jehovah’s Witnesses in the US.
Traditional Stem Cell Transplants Require Blood Support
In conventional autologous stem cell transplants for multiple myeloma, high-dose chemotherapy temporarily wipes out the patient’s bone marrow for about 2 to 3 weeks, Dholaria explained. During this period, patients typically receive 2 units of packed red blood cells and platelet transfusions to prevent severe complications from anemia and low platelet counts.
“Because of this reason, Jehovah’s Witnesses have been traditionally denied these therapies,” Dholaria said.
However, bloodless autologous transplants have been performed for about 2 decades, and Vanderbilt University has been offering the procedures for about 3 years, according to Dholaria.
For the first bloodless procedure in the VA, the patient–who had an aggressive, newly diagnosed IgG kappa multiple myeloma–was evaluated.
“He had been treated by local doctors in California. Otherwise, he was actually in really good shape. Physically, he didn’t have any major issues,” Dholaria said. “So, he met the criteria for our bloodless protocol, and we decided to offer him the procedure.”
The team consulted ethics and legal departments and noted the patient’s blood product preferences in his electronic health record. The patient then underwent a preoptimization protocol that included erythropoiesis-stimulating agents, intravenous iron, and vitamin B12 supplementation to boost blood counts before the transplant, according to the case presentation.
Special Protocol Required in ‘Bloodless’ Procedures
After stem cell collection and chemotherapy, patients undergoing bloodless procedures receive aggressive growth factor support to minimize the duration and severity of cytopenia, Dholaria said. As part of the protocol, the care team uses pediatric tubes for blood draws to minimize blood loss and monitors patients closely on cardiac monitors, he added. In addition, blood draws are only performed every 3 days.
“We watch for any cardiac decompensation because these patients have severe anemia for a brief period of time. We make sure they don’t [have a] heart attack or arrhythmias,” Dholaria said. “Or if the platelets are too low, and they start oozing blood from the nose, gums, or gut, that needs to be dealt with accordingly.”
For bleeding complications, the team uses clotting factors and intravenous and oral medications to support remaining platelet function rather than platelet transfusions.
The patient in this case tolerated the transplant “exceptionally well with minimal complications,” according to the case presentation. He achieved full engraftment on day 14 after transplant and was discharged from inpatient care with continued monitoring through day 30.
“The patient was very compliant,” said Salyka Sengsayadeth, MD, medical director of the VA Tennessee Valley Healthcare System Stem Cell Transplant and Cellular Therapy Program and associate professor of medicine at Vanderbilt.
“He tolerated everything that we needed to do,” she said. “He called us when he needed to call us and did everything that we asked and recommended for him.”
The patient’s roughly 30-day hospital stay matched that of typical transplant patients, Sengsayadeth noted. His myeloma responded to treatment, and he returned to California, Dholaria said.
‘Bloodless’ Procedures Not for All Stem Cell Transplants
The case highlights the availability of stem cell transplants in the VA–they are only performed in Seattle and Nashville–and opportunities for patients who wish to avoid blood transfusions. Sengsayadeth said the bloodless protocol is available for patients without religious objections who simply prefer to avoid blood products.
Dholaria cautioned that bloodless protocol applies specifically to autologous transplants, where patients receive their own stem cells. The team does not plan to offer bloodless allogeneic transplants, which use donor stem cells for conditions like leukemia, due to higher risks. In addition, most Jehovah’s Witnesses decline allogeneic transplants because they do not accept stem cells from another person, Dholaria said.
Beyond multiple myeloma, the Tennessee Valley Healthcare System offers bloodless autologous transplants for various blood cancers, including non-Hodgkin lymphomas such as large B-cell lymphoma, follicular lymphoma, and mantle cell lymphoma, as well as lymphomas affecting the brain, Dholaria said.
Clinicians “should start thinking about this early on, as soon as the cancer diagnosis is made, to make the referral and get the patient on our radar,” Dholaria said.
Sengsayadeth said physicians within the VA typically know how to refer appropriate patients to her team. “They just send us an email or give us a call or a message to say ‘I have this patient. Do you think they’re someone I should send to you?’ We usually answer right back, and then we can proceed with the full evaluation if we think that’s a reasonable thing to do.”
‘Treated Like Family’
The patient, a Marine Corps veteran named Keith Cody, spoke about the procedure in a video interview. Cody said he was reluctant at first to undergo the procedure because he didn’t understand what it would accomplish.
“As I was doing the massive chemo every week, and then suffering with the side effects, I decided to ask again about this procedure and how it improves my quality of life,” he said.
At the time of the taping of the video, Cody was getting ready to go home to California. “They’ve told me that I’ll still need more time to get my energy back, but I do feel much better already,” he said.
He also praised the staff. “Everybody that we came across, I enjoyed the interactions. It’s actually sad to leave people behind that you really felt treated you like family.”
Dholaria discloses relationships with Janssen, Angiocrine, Pfizer, Poseida, MEI, Orcabio, Wugen, Allovir, Adicet, BMS, Molecular Templates, Atara, MJH, Arvinas, Janssen, ADC, Gilead, GSK, Caribou, F. Hoffmann-La Roche AG, Autolus, and Pierre Fabre.
Sengsayadeth has no disclosures.
PHOENIX ‑ A US Department of Veterans Affairs (VA) hospital in Tennessee has performed the first “bloodless” autologous stem cell transplant within the Veterans Health Administration, treating a 61-year-old Jehovah’s Witness patient with multiple myeloma who traveled from California for the procedure.
The case, presented at the annual meeting of the Association of VA Hematology/Oncology, stated that “we should not withhold any therapies for patients who are Jehovah’s Witnesses out of fear of them bleeding out or having complications from anemia,” said Bhagirathbhai Dholaria, MBBS, an associate professor of medicine at Vanderbilt University Medical Center who worked with the VA Tennessee Valley Healthcare System in Nashville.
While Jehovah’s Witnesses accept medical treatment, their faith forbids blood transfusions, including of preoperative autologous blood, due to its interpretation of the Bible. The faith allows individuals to decide whether to accept stem cells collected from their blood or someone else’s “provided that blood components are not intentionally collected, stored, and reinfused along with the stem cells.”
There are an estimated 1.2 million Jehovah’s Witnesses in the US.
Traditional Stem Cell Transplants Require Blood Support
In conventional autologous stem cell transplants for multiple myeloma, high-dose chemotherapy temporarily wipes out the patient’s bone marrow for about 2 to 3 weeks, Dholaria explained. During this period, patients typically receive 2 units of packed red blood cells and platelet transfusions to prevent severe complications from anemia and low platelet counts.
“Because of this reason, Jehovah’s Witnesses have been traditionally denied these therapies,” Dholaria said.
However, bloodless autologous transplants have been performed for about 2 decades, and Vanderbilt University has been offering the procedures for about 3 years, according to Dholaria.
For the first bloodless procedure in the VA, the patient–who had an aggressive, newly diagnosed IgG kappa multiple myeloma–was evaluated.
“He had been treated by local doctors in California. Otherwise, he was actually in really good shape. Physically, he didn’t have any major issues,” Dholaria said. “So, he met the criteria for our bloodless protocol, and we decided to offer him the procedure.”
The team consulted ethics and legal departments and noted the patient’s blood product preferences in his electronic health record. The patient then underwent a preoptimization protocol that included erythropoiesis-stimulating agents, intravenous iron, and vitamin B12 supplementation to boost blood counts before the transplant, according to the case presentation.
Special Protocol Required in ‘Bloodless’ Procedures
After stem cell collection and chemotherapy, patients undergoing bloodless procedures receive aggressive growth factor support to minimize the duration and severity of cytopenia, Dholaria said. As part of the protocol, the care team uses pediatric tubes for blood draws to minimize blood loss and monitors patients closely on cardiac monitors, he added. In addition, blood draws are only performed every 3 days.
“We watch for any cardiac decompensation because these patients have severe anemia for a brief period of time. We make sure they don’t [have a] heart attack or arrhythmias,” Dholaria said. “Or if the platelets are too low, and they start oozing blood from the nose, gums, or gut, that needs to be dealt with accordingly.”
For bleeding complications, the team uses clotting factors and intravenous and oral medications to support remaining platelet function rather than platelet transfusions.
The patient in this case tolerated the transplant “exceptionally well with minimal complications,” according to the case presentation. He achieved full engraftment on day 14 after transplant and was discharged from inpatient care with continued monitoring through day 30.
“The patient was very compliant,” said Salyka Sengsayadeth, MD, medical director of the VA Tennessee Valley Healthcare System Stem Cell Transplant and Cellular Therapy Program and associate professor of medicine at Vanderbilt.
“He tolerated everything that we needed to do,” she said. “He called us when he needed to call us and did everything that we asked and recommended for him.”
The patient’s roughly 30-day hospital stay matched that of typical transplant patients, Sengsayadeth noted. His myeloma responded to treatment, and he returned to California, Dholaria said.
‘Bloodless’ Procedures Not for All Stem Cell Transplants
The case highlights the availability of stem cell transplants in the VA–they are only performed in Seattle and Nashville–and opportunities for patients who wish to avoid blood transfusions. Sengsayadeth said the bloodless protocol is available for patients without religious objections who simply prefer to avoid blood products.
Dholaria cautioned that bloodless protocol applies specifically to autologous transplants, where patients receive their own stem cells. The team does not plan to offer bloodless allogeneic transplants, which use donor stem cells for conditions like leukemia, due to higher risks. In addition, most Jehovah’s Witnesses decline allogeneic transplants because they do not accept stem cells from another person, Dholaria said.
Beyond multiple myeloma, the Tennessee Valley Healthcare System offers bloodless autologous transplants for various blood cancers, including non-Hodgkin lymphomas such as large B-cell lymphoma, follicular lymphoma, and mantle cell lymphoma, as well as lymphomas affecting the brain, Dholaria said.
Clinicians “should start thinking about this early on, as soon as the cancer diagnosis is made, to make the referral and get the patient on our radar,” Dholaria said.
Sengsayadeth said physicians within the VA typically know how to refer appropriate patients to her team. “They just send us an email or give us a call or a message to say ‘I have this patient. Do you think they’re someone I should send to you?’ We usually answer right back, and then we can proceed with the full evaluation if we think that’s a reasonable thing to do.”
‘Treated Like Family’
The patient, a Marine Corps veteran named Keith Cody, spoke about the procedure in a video interview. Cody said he was reluctant at first to undergo the procedure because he didn’t understand what it would accomplish.
“As I was doing the massive chemo every week, and then suffering with the side effects, I decided to ask again about this procedure and how it improves my quality of life,” he said.
At the time of the taping of the video, Cody was getting ready to go home to California. “They’ve told me that I’ll still need more time to get my energy back, but I do feel much better already,” he said.
He also praised the staff. “Everybody that we came across, I enjoyed the interactions. It’s actually sad to leave people behind that you really felt treated you like family.”
Dholaria discloses relationships with Janssen, Angiocrine, Pfizer, Poseida, MEI, Orcabio, Wugen, Allovir, Adicet, BMS, Molecular Templates, Atara, MJH, Arvinas, Janssen, ADC, Gilead, GSK, Caribou, F. Hoffmann-La Roche AG, Autolus, and Pierre Fabre.
Sengsayadeth has no disclosures.
PHOENIX ‑ A US Department of Veterans Affairs (VA) hospital in Tennessee has performed the first “bloodless” autologous stem cell transplant within the Veterans Health Administration, treating a 61-year-old Jehovah’s Witness patient with multiple myeloma who traveled from California for the procedure.
The case, presented at the annual meeting of the Association of VA Hematology/Oncology, stated that “we should not withhold any therapies for patients who are Jehovah’s Witnesses out of fear of them bleeding out or having complications from anemia,” said Bhagirathbhai Dholaria, MBBS, an associate professor of medicine at Vanderbilt University Medical Center who worked with the VA Tennessee Valley Healthcare System in Nashville.
While Jehovah’s Witnesses accept medical treatment, their faith forbids blood transfusions, including of preoperative autologous blood, due to its interpretation of the Bible. The faith allows individuals to decide whether to accept stem cells collected from their blood or someone else’s “provided that blood components are not intentionally collected, stored, and reinfused along with the stem cells.”
There are an estimated 1.2 million Jehovah’s Witnesses in the US.
Traditional Stem Cell Transplants Require Blood Support
In conventional autologous stem cell transplants for multiple myeloma, high-dose chemotherapy temporarily wipes out the patient’s bone marrow for about 2 to 3 weeks, Dholaria explained. During this period, patients typically receive 2 units of packed red blood cells and platelet transfusions to prevent severe complications from anemia and low platelet counts.
“Because of this reason, Jehovah’s Witnesses have been traditionally denied these therapies,” Dholaria said.
However, bloodless autologous transplants have been performed for about 2 decades, and Vanderbilt University has been offering the procedures for about 3 years, according to Dholaria.
For the first bloodless procedure in the VA, the patient–who had an aggressive, newly diagnosed IgG kappa multiple myeloma–was evaluated.
“He had been treated by local doctors in California. Otherwise, he was actually in really good shape. Physically, he didn’t have any major issues,” Dholaria said. “So, he met the criteria for our bloodless protocol, and we decided to offer him the procedure.”
The team consulted ethics and legal departments and noted the patient’s blood product preferences in his electronic health record. The patient then underwent a preoptimization protocol that included erythropoiesis-stimulating agents, intravenous iron, and vitamin B12 supplementation to boost blood counts before the transplant, according to the case presentation.
Special Protocol Required in ‘Bloodless’ Procedures
After stem cell collection and chemotherapy, patients undergoing bloodless procedures receive aggressive growth factor support to minimize the duration and severity of cytopenia, Dholaria said. As part of the protocol, the care team uses pediatric tubes for blood draws to minimize blood loss and monitors patients closely on cardiac monitors, he added. In addition, blood draws are only performed every 3 days.
“We watch for any cardiac decompensation because these patients have severe anemia for a brief period of time. We make sure they don’t [have a] heart attack or arrhythmias,” Dholaria said. “Or if the platelets are too low, and they start oozing blood from the nose, gums, or gut, that needs to be dealt with accordingly.”
For bleeding complications, the team uses clotting factors and intravenous and oral medications to support remaining platelet function rather than platelet transfusions.
The patient in this case tolerated the transplant “exceptionally well with minimal complications,” according to the case presentation. He achieved full engraftment on day 14 after transplant and was discharged from inpatient care with continued monitoring through day 30.
“The patient was very compliant,” said Salyka Sengsayadeth, MD, medical director of the VA Tennessee Valley Healthcare System Stem Cell Transplant and Cellular Therapy Program and associate professor of medicine at Vanderbilt.
“He tolerated everything that we needed to do,” she said. “He called us when he needed to call us and did everything that we asked and recommended for him.”
The patient’s roughly 30-day hospital stay matched that of typical transplant patients, Sengsayadeth noted. His myeloma responded to treatment, and he returned to California, Dholaria said.
‘Bloodless’ Procedures Not for All Stem Cell Transplants
The case highlights the availability of stem cell transplants in the VA–they are only performed in Seattle and Nashville–and opportunities for patients who wish to avoid blood transfusions. Sengsayadeth said the bloodless protocol is available for patients without religious objections who simply prefer to avoid blood products.
Dholaria cautioned that bloodless protocol applies specifically to autologous transplants, where patients receive their own stem cells. The team does not plan to offer bloodless allogeneic transplants, which use donor stem cells for conditions like leukemia, due to higher risks. In addition, most Jehovah’s Witnesses decline allogeneic transplants because they do not accept stem cells from another person, Dholaria said.
Beyond multiple myeloma, the Tennessee Valley Healthcare System offers bloodless autologous transplants for various blood cancers, including non-Hodgkin lymphomas such as large B-cell lymphoma, follicular lymphoma, and mantle cell lymphoma, as well as lymphomas affecting the brain, Dholaria said.
Clinicians “should start thinking about this early on, as soon as the cancer diagnosis is made, to make the referral and get the patient on our radar,” Dholaria said.
Sengsayadeth said physicians within the VA typically know how to refer appropriate patients to her team. “They just send us an email or give us a call or a message to say ‘I have this patient. Do you think they’re someone I should send to you?’ We usually answer right back, and then we can proceed with the full evaluation if we think that’s a reasonable thing to do.”
‘Treated Like Family’
The patient, a Marine Corps veteran named Keith Cody, spoke about the procedure in a video interview. Cody said he was reluctant at first to undergo the procedure because he didn’t understand what it would accomplish.
“As I was doing the massive chemo every week, and then suffering with the side effects, I decided to ask again about this procedure and how it improves my quality of life,” he said.
At the time of the taping of the video, Cody was getting ready to go home to California. “They’ve told me that I’ll still need more time to get my energy back, but I do feel much better already,” he said.
He also praised the staff. “Everybody that we came across, I enjoyed the interactions. It’s actually sad to leave people behind that you really felt treated you like family.”
Dholaria discloses relationships with Janssen, Angiocrine, Pfizer, Poseida, MEI, Orcabio, Wugen, Allovir, Adicet, BMS, Molecular Templates, Atara, MJH, Arvinas, Janssen, ADC, Gilead, GSK, Caribou, F. Hoffmann-La Roche AG, Autolus, and Pierre Fabre.
Sengsayadeth has no disclosures.
A Case Report on Bortezomib-Induced Hypotension: Rare Adverse Effect in Proteasome Inhibitor Therapy
Case Presentation
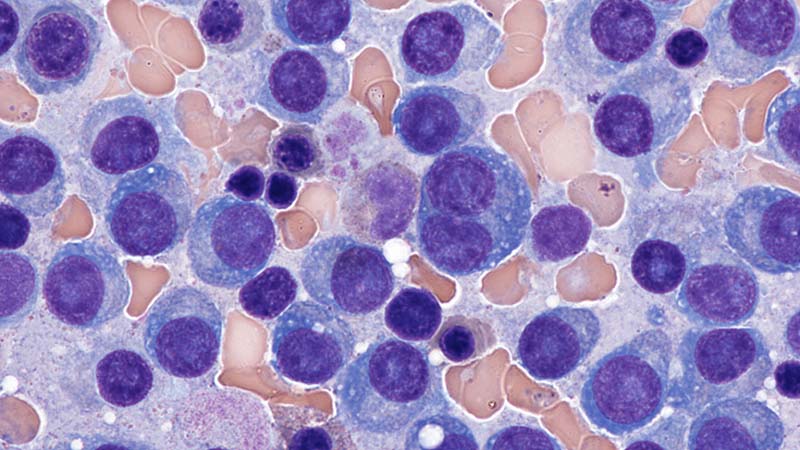
A 75-year-old man with chronic kidney disease, hypertension and diabetes mellitus presented with acute kidney injury (creatinine 5.2 from baseline 4.2) and a two-week history of increased urinary frequency. Labs revealed high anion gap metabolic acidosis, proteinuria, hematuria, pyuria, and acute on chronic anemia. He was diagnosed with kappa light chain nephropathy and multiple myeloma with 32% plasma cells on bone marrow biopsy. He began treatment with bortezomib, cyclophosphamide, and dexamethasone (Cy- BorD). Three days after cyclophosphamide and five days after bortezomib, the patient developed persistent hypotension with systolic BP in the 50s, unresponsive to fluids and Trendelenburg position. Due to end-stage renal disease with anuria, fluid resuscitation was limited. He required norepinephrine and was transferred to the ICU. Given instability, hemodialysis was deferred, and continuous renal replacement therapy was initiated. Shock evaluation included a CT abdomen showing enteritis versus ileus; however, infectious workup was negative. Cardiogenic shock was ruled out with a serial echocardiogram showing normal ejection fractions of 59-67% without significant valvular disease. The workup for adrenal insufficiency was negative. After the exclusion of other potential causes of shock, severe refractory hypotension was attributed to bortezomib toxicity.Hypotension is a known adverse effect of bortezomib. Orthostatic hypotension may occur in 8 to 9% of patients, and rarely, patients may experience heart failure, conduction disorders and arrhythmias, or cardiogenic shock. The pathologic mechanism of this toxicity is still poorly understood. Proposed mechanisms include direct endothelial toxicity as evidenced by thrombotic microangiopathy or impairment of sympathetic and parasympathetic nerve fibres. Most commonly, patients experience neurotoxicity, which may manifest as autonomic dysfunction or peripheral neuropathy. Cardiovascular complications are typically reversible. Our patient’s cardiac function remained within normal limits; therefore, his persistent hypotension was felt to be the result of direct toxicity from bortezomib rather than cardiogenic shock. Ultimately, blood pressure did improve, and vasopressors were discontinued. However, he continued to have orthostatic hypotension and continued to require supportive fludrocortisone, midodrine, and pyridostigmine. Goals of care have been discussed, and he wished to continue pursuing restorative care, with a plan for transition to carfilzomib versus daratumumab outpatient.
Case Presentation
A 75-year-old man with chronic kidney disease, hypertension and diabetes mellitus presented with acute kidney injury (creatinine 5.2 from baseline 4.2) and a two-week history of increased urinary frequency. Labs revealed high anion gap metabolic acidosis, proteinuria, hematuria, pyuria, and acute on chronic anemia. He was diagnosed with kappa light chain nephropathy and multiple myeloma with 32% plasma cells on bone marrow biopsy. He began treatment with bortezomib, cyclophosphamide, and dexamethasone (Cy- BorD). Three days after cyclophosphamide and five days after bortezomib, the patient developed persistent hypotension with systolic BP in the 50s, unresponsive to fluids and Trendelenburg position. Due to end-stage renal disease with anuria, fluid resuscitation was limited. He required norepinephrine and was transferred to the ICU. Given instability, hemodialysis was deferred, and continuous renal replacement therapy was initiated. Shock evaluation included a CT abdomen showing enteritis versus ileus; however, infectious workup was negative. Cardiogenic shock was ruled out with a serial echocardiogram showing normal ejection fractions of 59-67% without significant valvular disease. The workup for adrenal insufficiency was negative. After the exclusion of other potential causes of shock, severe refractory hypotension was attributed to bortezomib toxicity.Hypotension is a known adverse effect of bortezomib. Orthostatic hypotension may occur in 8 to 9% of patients, and rarely, patients may experience heart failure, conduction disorders and arrhythmias, or cardiogenic shock. The pathologic mechanism of this toxicity is still poorly understood. Proposed mechanisms include direct endothelial toxicity as evidenced by thrombotic microangiopathy or impairment of sympathetic and parasympathetic nerve fibres. Most commonly, patients experience neurotoxicity, which may manifest as autonomic dysfunction or peripheral neuropathy. Cardiovascular complications are typically reversible. Our patient’s cardiac function remained within normal limits; therefore, his persistent hypotension was felt to be the result of direct toxicity from bortezomib rather than cardiogenic shock. Ultimately, blood pressure did improve, and vasopressors were discontinued. However, he continued to have orthostatic hypotension and continued to require supportive fludrocortisone, midodrine, and pyridostigmine. Goals of care have been discussed, and he wished to continue pursuing restorative care, with a plan for transition to carfilzomib versus daratumumab outpatient.
Case Presentation
A 75-year-old man with chronic kidney disease, hypertension and diabetes mellitus presented with acute kidney injury (creatinine 5.2 from baseline 4.2) and a two-week history of increased urinary frequency. Labs revealed high anion gap metabolic acidosis, proteinuria, hematuria, pyuria, and acute on chronic anemia. He was diagnosed with kappa light chain nephropathy and multiple myeloma with 32% plasma cells on bone marrow biopsy. He began treatment with bortezomib, cyclophosphamide, and dexamethasone (Cy- BorD). Three days after cyclophosphamide and five days after bortezomib, the patient developed persistent hypotension with systolic BP in the 50s, unresponsive to fluids and Trendelenburg position. Due to end-stage renal disease with anuria, fluid resuscitation was limited. He required norepinephrine and was transferred to the ICU. Given instability, hemodialysis was deferred, and continuous renal replacement therapy was initiated. Shock evaluation included a CT abdomen showing enteritis versus ileus; however, infectious workup was negative. Cardiogenic shock was ruled out with a serial echocardiogram showing normal ejection fractions of 59-67% without significant valvular disease. The workup for adrenal insufficiency was negative. After the exclusion of other potential causes of shock, severe refractory hypotension was attributed to bortezomib toxicity.Hypotension is a known adverse effect of bortezomib. Orthostatic hypotension may occur in 8 to 9% of patients, and rarely, patients may experience heart failure, conduction disorders and arrhythmias, or cardiogenic shock. The pathologic mechanism of this toxicity is still poorly understood. Proposed mechanisms include direct endothelial toxicity as evidenced by thrombotic microangiopathy or impairment of sympathetic and parasympathetic nerve fibres. Most commonly, patients experience neurotoxicity, which may manifest as autonomic dysfunction or peripheral neuropathy. Cardiovascular complications are typically reversible. Our patient’s cardiac function remained within normal limits; therefore, his persistent hypotension was felt to be the result of direct toxicity from bortezomib rather than cardiogenic shock. Ultimately, blood pressure did improve, and vasopressors were discontinued. However, he continued to have orthostatic hypotension and continued to require supportive fludrocortisone, midodrine, and pyridostigmine. Goals of care have been discussed, and he wished to continue pursuing restorative care, with a plan for transition to carfilzomib versus daratumumab outpatient.
Case Presentation: First Ever VA "Bloodless" Autologous Stem Cell Transplant Was a Success
Background
Autologous stem cell transplant (ASCT) is an important part of the treatment paradigm for patients with multiple myeloma (MM) and remains the standard of care for newly diagnosed patients. Blood product transfusion support in the form of platelets and packed red blood cells (pRBCs) is part of the standard of practice as supportive measures during the severely pancytopenic period. Some MM patients, such as those of Jehovah’s Witness (JW) faith, may have religious beliefs or preferences that preclude acceptance of such blood products. Some transplant centers have developed protocols to allow safe “bloodless” ASCT that allows these patients to receive this important treatment while adhering to their beliefs or preferences.
Case Presentation
A 61-year-old veteran of JW faith with newly diagnosed IgG Kappa Multiple Myeloma was referred to the Tennessee Valley Healthcare System (TVHS) Stem Cell Transplant program for consideration of “bloodless” ASCT. With the assistance and expertise of the academic affiliate, Vanderbilt University Medical Center’s established bloodless ASCT protocol, this same protocol was established at TVHS to optimize the patient’s care pretransplant (use of erythropoiesis stimulating agents, intravenous iron, B12 supplementation) as well as post-transplant (use of antifibrinolytics, close inpatient monitoring). Both Ethics and Legal consultation was obtained, and guidance was provided to create a life sustaining treatment (LST) note in the veteran’s electronic health record that captured the veteran’s blood product preference. Once all protocols and guidance were in place, the TVHS SCT/CT program proceeded to treat the veteran with a myeloablative melphalan ASCT. The patient tolerated the procedure exceptionally well with minimal complications. He achieved full engraftment on day +14 after ASCT as expected and was discharged from the inpatient setting. He was monitored in the outpatient setting until day +30 without further complications.
Conclusions
The TVHS SCT/CT performed the first ever bloodless autologous stem cell transplant within the VA. This pioneering effort to establish such protocols to provide care to all veterans whatever their personal or religious preferences is a testament to commitment of VA to provide care for all veterans and the willingness to innovate to do so.
Background
Autologous stem cell transplant (ASCT) is an important part of the treatment paradigm for patients with multiple myeloma (MM) and remains the standard of care for newly diagnosed patients. Blood product transfusion support in the form of platelets and packed red blood cells (pRBCs) is part of the standard of practice as supportive measures during the severely pancytopenic period. Some MM patients, such as those of Jehovah’s Witness (JW) faith, may have religious beliefs or preferences that preclude acceptance of such blood products. Some transplant centers have developed protocols to allow safe “bloodless” ASCT that allows these patients to receive this important treatment while adhering to their beliefs or preferences.
Case Presentation
A 61-year-old veteran of JW faith with newly diagnosed IgG Kappa Multiple Myeloma was referred to the Tennessee Valley Healthcare System (TVHS) Stem Cell Transplant program for consideration of “bloodless” ASCT. With the assistance and expertise of the academic affiliate, Vanderbilt University Medical Center’s established bloodless ASCT protocol, this same protocol was established at TVHS to optimize the patient’s care pretransplant (use of erythropoiesis stimulating agents, intravenous iron, B12 supplementation) as well as post-transplant (use of antifibrinolytics, close inpatient monitoring). Both Ethics and Legal consultation was obtained, and guidance was provided to create a life sustaining treatment (LST) note in the veteran’s electronic health record that captured the veteran’s blood product preference. Once all protocols and guidance were in place, the TVHS SCT/CT program proceeded to treat the veteran with a myeloablative melphalan ASCT. The patient tolerated the procedure exceptionally well with minimal complications. He achieved full engraftment on day +14 after ASCT as expected and was discharged from the inpatient setting. He was monitored in the outpatient setting until day +30 without further complications.
Conclusions
The TVHS SCT/CT performed the first ever bloodless autologous stem cell transplant within the VA. This pioneering effort to establish such protocols to provide care to all veterans whatever their personal or religious preferences is a testament to commitment of VA to provide care for all veterans and the willingness to innovate to do so.
Background
Autologous stem cell transplant (ASCT) is an important part of the treatment paradigm for patients with multiple myeloma (MM) and remains the standard of care for newly diagnosed patients. Blood product transfusion support in the form of platelets and packed red blood cells (pRBCs) is part of the standard of practice as supportive measures during the severely pancytopenic period. Some MM patients, such as those of Jehovah’s Witness (JW) faith, may have religious beliefs or preferences that preclude acceptance of such blood products. Some transplant centers have developed protocols to allow safe “bloodless” ASCT that allows these patients to receive this important treatment while adhering to their beliefs or preferences.
Case Presentation
A 61-year-old veteran of JW faith with newly diagnosed IgG Kappa Multiple Myeloma was referred to the Tennessee Valley Healthcare System (TVHS) Stem Cell Transplant program for consideration of “bloodless” ASCT. With the assistance and expertise of the academic affiliate, Vanderbilt University Medical Center’s established bloodless ASCT protocol, this same protocol was established at TVHS to optimize the patient’s care pretransplant (use of erythropoiesis stimulating agents, intravenous iron, B12 supplementation) as well as post-transplant (use of antifibrinolytics, close inpatient monitoring). Both Ethics and Legal consultation was obtained, and guidance was provided to create a life sustaining treatment (LST) note in the veteran’s electronic health record that captured the veteran’s blood product preference. Once all protocols and guidance were in place, the TVHS SCT/CT program proceeded to treat the veteran with a myeloablative melphalan ASCT. The patient tolerated the procedure exceptionally well with minimal complications. He achieved full engraftment on day +14 after ASCT as expected and was discharged from the inpatient setting. He was monitored in the outpatient setting until day +30 without further complications.
Conclusions
The TVHS SCT/CT performed the first ever bloodless autologous stem cell transplant within the VA. This pioneering effort to establish such protocols to provide care to all veterans whatever their personal or religious preferences is a testament to commitment of VA to provide care for all veterans and the willingness to innovate to do so.
FDA Advisory Panel Votes NO on Belantamab for Myeloma
A bid by GlaxoSmithKline (GSK) to bring its multiple myeloma drug belantamab mafodotin (Blenrep) back to the market hit a stumbling block during an FDA panel meeting held on July 17.
The FDA’s Oncologic Drugs Advisory Committee (ODAC) voted 5-3 against belantamab in combination with bortezomib and dexamethasone and 7-1 against belantamab in combination with pomalidamide and dexamethasone on the specific questions of whether the benefits of each treatment regimen at the proposed doses outweigh the risks for patients with relapsed or refractory disease after at least one prior line of therapy.
ODAC members voting no cited concerns about the lack of exploration of optimal dosing, as well as high rates of ocular toxicity and a lack of diversity among trial participants.
“This was a challenging decision because the efficacy data were strong, but the toxicity data were also very strong,” said Neil Vasan, MD, PhD, of New York University Langone Health in New York City.
Regarding optimal dosing, Vasan, who voted no on both questions, cited “a missed opportunity over the course of many years during the development of this drug to explore these different dosages,” but he also noted that “the building blocks are here to explore this question in the future.”
Belantamab, an antibody-drug conjugate targeting B-cell maturation antigen, was granted accelerated approval as a late-line therapy for relapsed or refractory multiple myeloma in August 2020 based on findings from the DREAMM-2 trial. However, GSK voluntarily withdrew the drug from the US market in 2023 after the confirmatory DREAMM-3 trial did not meet its primary endpoint of improved progression-free survival (PFS).
The company continued to explore belantamab in combination with other agents and in earlier lines of therapy. Based on findings from the DREAMM-7 and DREAMM-8 trials, which both showed improved PFS vs standard-of-care triplet therapies, the company submitted a new Biologics License Application in November 2024 seeking approval of the belantamab-based regimens.
Findings from DREAMM-7 and DREAMM-8 were reported at the 2025 American Society of Clinical Oncology conference in Chicago in June.
Both studies met their primary PFS endpoints, but the FDA expressed concerns about adverse events, dosing, and the relevance of the data for US patients and therefore sought input from ODAC members on the proposed dosages of 2.5 mg/kg every 3 weeks for the belantamab plus bortezomib and dexamethasone combination and 2.5 mg/kg in cycle 1, followed by 1.0 mg/kg every 4 weeks for the belantamab plus pomalidamide and dexamethasone combination.
Although GSK and several patients with multiple myeloma touted life-saving benefits of belantamab and argued that ocular toxicity associated with treatment is manageable and transient, most — but not all — ODAC members were unconvinced, at least as to the immediate questions regarding the benefit-risk profile.
“This is probably one of the most difficult votes I’ve done as a member of this committee,” said Grzegorz S. Nowakowski, MD, of the Mayo Clinic, Rochester, Minnesota, who voted yes on belantamab plus bortezomib and dexamethasone.
Nowakowski noted mistakes made from a regulatory perspective, including a lack of appropriate US patient representation in the trials and attention to dose optimization, but ultimately said that, as a practicing hematologist, he couldn’t ignore the drug’s clear activity, including a possible overall survival benefit, and the potential for mitigating toxicity with careful follow-up and dose reductions.
John DeFlice, MD, of Cedars-Sinai Samuel Oschin Cancer Center in Los Angeles — a multiple myeloma survivor and patient representative on the committee — voted yes on both questions, noting that, based on the testimony of patients and the clinical experience of the investigators, belantamab is “an amazing drug for an incurable disease.”
“I think [these] are the wrong issues to be evaluated,” DeFlice said of the specific questions posed by the FDA at the hearing.
The FDA considers the recommendations of its advisory panels in making final approval decisions but is not bound by them.
A version of this article first appeared on Medscape.com.
A bid by GlaxoSmithKline (GSK) to bring its multiple myeloma drug belantamab mafodotin (Blenrep) back to the market hit a stumbling block during an FDA panel meeting held on July 17.
The FDA’s Oncologic Drugs Advisory Committee (ODAC) voted 5-3 against belantamab in combination with bortezomib and dexamethasone and 7-1 against belantamab in combination with pomalidamide and dexamethasone on the specific questions of whether the benefits of each treatment regimen at the proposed doses outweigh the risks for patients with relapsed or refractory disease after at least one prior line of therapy.
ODAC members voting no cited concerns about the lack of exploration of optimal dosing, as well as high rates of ocular toxicity and a lack of diversity among trial participants.
“This was a challenging decision because the efficacy data were strong, but the toxicity data were also very strong,” said Neil Vasan, MD, PhD, of New York University Langone Health in New York City.
Regarding optimal dosing, Vasan, who voted no on both questions, cited “a missed opportunity over the course of many years during the development of this drug to explore these different dosages,” but he also noted that “the building blocks are here to explore this question in the future.”
Belantamab, an antibody-drug conjugate targeting B-cell maturation antigen, was granted accelerated approval as a late-line therapy for relapsed or refractory multiple myeloma in August 2020 based on findings from the DREAMM-2 trial. However, GSK voluntarily withdrew the drug from the US market in 2023 after the confirmatory DREAMM-3 trial did not meet its primary endpoint of improved progression-free survival (PFS).
The company continued to explore belantamab in combination with other agents and in earlier lines of therapy. Based on findings from the DREAMM-7 and DREAMM-8 trials, which both showed improved PFS vs standard-of-care triplet therapies, the company submitted a new Biologics License Application in November 2024 seeking approval of the belantamab-based regimens.
Findings from DREAMM-7 and DREAMM-8 were reported at the 2025 American Society of Clinical Oncology conference in Chicago in June.
Both studies met their primary PFS endpoints, but the FDA expressed concerns about adverse events, dosing, and the relevance of the data for US patients and therefore sought input from ODAC members on the proposed dosages of 2.5 mg/kg every 3 weeks for the belantamab plus bortezomib and dexamethasone combination and 2.5 mg/kg in cycle 1, followed by 1.0 mg/kg every 4 weeks for the belantamab plus pomalidamide and dexamethasone combination.
Although GSK and several patients with multiple myeloma touted life-saving benefits of belantamab and argued that ocular toxicity associated with treatment is manageable and transient, most — but not all — ODAC members were unconvinced, at least as to the immediate questions regarding the benefit-risk profile.
“This is probably one of the most difficult votes I’ve done as a member of this committee,” said Grzegorz S. Nowakowski, MD, of the Mayo Clinic, Rochester, Minnesota, who voted yes on belantamab plus bortezomib and dexamethasone.
Nowakowski noted mistakes made from a regulatory perspective, including a lack of appropriate US patient representation in the trials and attention to dose optimization, but ultimately said that, as a practicing hematologist, he couldn’t ignore the drug’s clear activity, including a possible overall survival benefit, and the potential for mitigating toxicity with careful follow-up and dose reductions.
John DeFlice, MD, of Cedars-Sinai Samuel Oschin Cancer Center in Los Angeles — a multiple myeloma survivor and patient representative on the committee — voted yes on both questions, noting that, based on the testimony of patients and the clinical experience of the investigators, belantamab is “an amazing drug for an incurable disease.”
“I think [these] are the wrong issues to be evaluated,” DeFlice said of the specific questions posed by the FDA at the hearing.
The FDA considers the recommendations of its advisory panels in making final approval decisions but is not bound by them.
A version of this article first appeared on Medscape.com.
A bid by GlaxoSmithKline (GSK) to bring its multiple myeloma drug belantamab mafodotin (Blenrep) back to the market hit a stumbling block during an FDA panel meeting held on July 17.
The FDA’s Oncologic Drugs Advisory Committee (ODAC) voted 5-3 against belantamab in combination with bortezomib and dexamethasone and 7-1 against belantamab in combination with pomalidamide and dexamethasone on the specific questions of whether the benefits of each treatment regimen at the proposed doses outweigh the risks for patients with relapsed or refractory disease after at least one prior line of therapy.
ODAC members voting no cited concerns about the lack of exploration of optimal dosing, as well as high rates of ocular toxicity and a lack of diversity among trial participants.
“This was a challenging decision because the efficacy data were strong, but the toxicity data were also very strong,” said Neil Vasan, MD, PhD, of New York University Langone Health in New York City.
Regarding optimal dosing, Vasan, who voted no on both questions, cited “a missed opportunity over the course of many years during the development of this drug to explore these different dosages,” but he also noted that “the building blocks are here to explore this question in the future.”
Belantamab, an antibody-drug conjugate targeting B-cell maturation antigen, was granted accelerated approval as a late-line therapy for relapsed or refractory multiple myeloma in August 2020 based on findings from the DREAMM-2 trial. However, GSK voluntarily withdrew the drug from the US market in 2023 after the confirmatory DREAMM-3 trial did not meet its primary endpoint of improved progression-free survival (PFS).
The company continued to explore belantamab in combination with other agents and in earlier lines of therapy. Based on findings from the DREAMM-7 and DREAMM-8 trials, which both showed improved PFS vs standard-of-care triplet therapies, the company submitted a new Biologics License Application in November 2024 seeking approval of the belantamab-based regimens.
Findings from DREAMM-7 and DREAMM-8 were reported at the 2025 American Society of Clinical Oncology conference in Chicago in June.
Both studies met their primary PFS endpoints, but the FDA expressed concerns about adverse events, dosing, and the relevance of the data for US patients and therefore sought input from ODAC members on the proposed dosages of 2.5 mg/kg every 3 weeks for the belantamab plus bortezomib and dexamethasone combination and 2.5 mg/kg in cycle 1, followed by 1.0 mg/kg every 4 weeks for the belantamab plus pomalidamide and dexamethasone combination.
Although GSK and several patients with multiple myeloma touted life-saving benefits of belantamab and argued that ocular toxicity associated with treatment is manageable and transient, most — but not all — ODAC members were unconvinced, at least as to the immediate questions regarding the benefit-risk profile.
“This is probably one of the most difficult votes I’ve done as a member of this committee,” said Grzegorz S. Nowakowski, MD, of the Mayo Clinic, Rochester, Minnesota, who voted yes on belantamab plus bortezomib and dexamethasone.
Nowakowski noted mistakes made from a regulatory perspective, including a lack of appropriate US patient representation in the trials and attention to dose optimization, but ultimately said that, as a practicing hematologist, he couldn’t ignore the drug’s clear activity, including a possible overall survival benefit, and the potential for mitigating toxicity with careful follow-up and dose reductions.
John DeFlice, MD, of Cedars-Sinai Samuel Oschin Cancer Center in Los Angeles — a multiple myeloma survivor and patient representative on the committee — voted yes on both questions, noting that, based on the testimony of patients and the clinical experience of the investigators, belantamab is “an amazing drug for an incurable disease.”
“I think [these] are the wrong issues to be evaluated,” DeFlice said of the specific questions posed by the FDA at the hearing.
The FDA considers the recommendations of its advisory panels in making final approval decisions but is not bound by them.
A version of this article first appeared on Medscape.com.
Myeloma: Can Lymphopenia Help Predict Patient Outcomes?
TOPLINE:
The analysis of 11,427 US Deparment of Veterans Affairs (VA) hospital patients with multiple myeloma (MM) reveals that lymphopenia affects 53% of patients at diagnosis. The median overall survival was 2.7 years in patients with severely low absolute lymphocyte count vs 4.2 years in those with normal counts.
METHODOLOGY:
- Researchers evaluated 11,427 patients diagnosed with MM between 2000 and 2019 at VA medical centers using absolute lymphocyte count obtained closest to diagnosis and up to 2.5 years thereafter.
- Patients were stratified into three absolute lymphocyte count categories: Severely low (less than 1 × 10⁹/μL), low (1 × 10⁹/μL to 1.5 × 10⁹/μL), and normal (> 1.5 × 10⁹/μL).
- Analysis excluded patients with acute and chronic leukemias, aplastic anemia, myelodysplastic syndrome, hairy cell leukemia, or myeloproliferative neoplasms before MM diagnosis.
- Follow-up duration extended from diagnosis until development of another hematologic malignancy, death, truncation date (15 years after diagnosis), or study end date.
TAKEAWAY:
- Lymphopenia was present in 53% of patients at MM diagnosis and was associated with inferior overall survival.
- Median overall survival for patients with severely low, low, and normal absolute lymphocyte count at diagnosis was 2.7 years, 3.3 years, and 4.2 years, respectively (P < .001).
- Persistent or new development of lymphopenia during treatment and follow-up was linked to inferior overall survival.
- Standard induction therapy with lenalidomide, bortezomib, and dexamethasone did not overcome inferior outcomes in patients with lymphopenia, showing median overall survival of 3.6 years, 4.6 years, and 5.7 years among patients with severely low, low, and normal baseline absolute lymphocyte count, respectively (P less than .001).
IN PRACTICE:
“Because immune dysregulation and immunosenescence in the bone marrow microenvironment are reflected in the peripheral blood lymphocyte count and peripheral blood markers may, in turn, correlate with clinical features and outcome in MM, we sought to identify clinical features correlating with peripheral blood lymphopenia and evaluate absolute lymphocyte count at diagnosis as a predictor of outcome in MM and in the context of standard induction treatment,” the authors wrote.
SOURCE:
This study was led by Grace M. Ferri and Cenk Yildirim, Boston Medical Center in Boston. It was published online in Blood Advances.
LIMITATIONS:
This study population consisted predominantly of male participants due to being conducted in the VA system. Additionally, researchers acknowledged that lymphopenia could not be exclusively attributed to MM, as other treatments common in older populations might contribute. The use of alkylating agents like cyclophosphamide and melphalan during treatment could also influence lymphopenia levels.
DISCLOSURES:
Individual-level data underlying this study are available to researchers with VA regulatory approval, consistent with VA policy.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
The analysis of 11,427 US Deparment of Veterans Affairs (VA) hospital patients with multiple myeloma (MM) reveals that lymphopenia affects 53% of patients at diagnosis. The median overall survival was 2.7 years in patients with severely low absolute lymphocyte count vs 4.2 years in those with normal counts.
METHODOLOGY:
- Researchers evaluated 11,427 patients diagnosed with MM between 2000 and 2019 at VA medical centers using absolute lymphocyte count obtained closest to diagnosis and up to 2.5 years thereafter.
- Patients were stratified into three absolute lymphocyte count categories: Severely low (less than 1 × 10⁹/μL), low (1 × 10⁹/μL to 1.5 × 10⁹/μL), and normal (> 1.5 × 10⁹/μL).
- Analysis excluded patients with acute and chronic leukemias, aplastic anemia, myelodysplastic syndrome, hairy cell leukemia, or myeloproliferative neoplasms before MM diagnosis.
- Follow-up duration extended from diagnosis until development of another hematologic malignancy, death, truncation date (15 years after diagnosis), or study end date.
TAKEAWAY:
- Lymphopenia was present in 53% of patients at MM diagnosis and was associated with inferior overall survival.
- Median overall survival for patients with severely low, low, and normal absolute lymphocyte count at diagnosis was 2.7 years, 3.3 years, and 4.2 years, respectively (P < .001).
- Persistent or new development of lymphopenia during treatment and follow-up was linked to inferior overall survival.
- Standard induction therapy with lenalidomide, bortezomib, and dexamethasone did not overcome inferior outcomes in patients with lymphopenia, showing median overall survival of 3.6 years, 4.6 years, and 5.7 years among patients with severely low, low, and normal baseline absolute lymphocyte count, respectively (P less than .001).
IN PRACTICE:
“Because immune dysregulation and immunosenescence in the bone marrow microenvironment are reflected in the peripheral blood lymphocyte count and peripheral blood markers may, in turn, correlate with clinical features and outcome in MM, we sought to identify clinical features correlating with peripheral blood lymphopenia and evaluate absolute lymphocyte count at diagnosis as a predictor of outcome in MM and in the context of standard induction treatment,” the authors wrote.
SOURCE:
This study was led by Grace M. Ferri and Cenk Yildirim, Boston Medical Center in Boston. It was published online in Blood Advances.
LIMITATIONS:
This study population consisted predominantly of male participants due to being conducted in the VA system. Additionally, researchers acknowledged that lymphopenia could not be exclusively attributed to MM, as other treatments common in older populations might contribute. The use of alkylating agents like cyclophosphamide and melphalan during treatment could also influence lymphopenia levels.
DISCLOSURES:
Individual-level data underlying this study are available to researchers with VA regulatory approval, consistent with VA policy.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
The analysis of 11,427 US Deparment of Veterans Affairs (VA) hospital patients with multiple myeloma (MM) reveals that lymphopenia affects 53% of patients at diagnosis. The median overall survival was 2.7 years in patients with severely low absolute lymphocyte count vs 4.2 years in those with normal counts.
METHODOLOGY:
- Researchers evaluated 11,427 patients diagnosed with MM between 2000 and 2019 at VA medical centers using absolute lymphocyte count obtained closest to diagnosis and up to 2.5 years thereafter.
- Patients were stratified into three absolute lymphocyte count categories: Severely low (less than 1 × 10⁹/μL), low (1 × 10⁹/μL to 1.5 × 10⁹/μL), and normal (> 1.5 × 10⁹/μL).
- Analysis excluded patients with acute and chronic leukemias, aplastic anemia, myelodysplastic syndrome, hairy cell leukemia, or myeloproliferative neoplasms before MM diagnosis.
- Follow-up duration extended from diagnosis until development of another hematologic malignancy, death, truncation date (15 years after diagnosis), or study end date.
TAKEAWAY:
- Lymphopenia was present in 53% of patients at MM diagnosis and was associated with inferior overall survival.
- Median overall survival for patients with severely low, low, and normal absolute lymphocyte count at diagnosis was 2.7 years, 3.3 years, and 4.2 years, respectively (P < .001).
- Persistent or new development of lymphopenia during treatment and follow-up was linked to inferior overall survival.
- Standard induction therapy with lenalidomide, bortezomib, and dexamethasone did not overcome inferior outcomes in patients with lymphopenia, showing median overall survival of 3.6 years, 4.6 years, and 5.7 years among patients with severely low, low, and normal baseline absolute lymphocyte count, respectively (P less than .001).
IN PRACTICE:
“Because immune dysregulation and immunosenescence in the bone marrow microenvironment are reflected in the peripheral blood lymphocyte count and peripheral blood markers may, in turn, correlate with clinical features and outcome in MM, we sought to identify clinical features correlating with peripheral blood lymphopenia and evaluate absolute lymphocyte count at diagnosis as a predictor of outcome in MM and in the context of standard induction treatment,” the authors wrote.
SOURCE:
This study was led by Grace M. Ferri and Cenk Yildirim, Boston Medical Center in Boston. It was published online in Blood Advances.
LIMITATIONS:
This study population consisted predominantly of male participants due to being conducted in the VA system. Additionally, researchers acknowledged that lymphopenia could not be exclusively attributed to MM, as other treatments common in older populations might contribute. The use of alkylating agents like cyclophosphamide and melphalan during treatment could also influence lymphopenia levels.
DISCLOSURES:
Individual-level data underlying this study are available to researchers with VA regulatory approval, consistent with VA policy.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
Myeloma: Can Failed Drugs Work Again?
TOPLINE:
METHODOLOGY:
- Researchers retrospectively reviewed patients with relapsed/refractory multiple myeloma who started new systemic therapy for disease progression between January 2015 and April 2022 at their institution.
- Analysis included 315 patients treated with a drug that their disease had previously been refractory to, defined as disease progression while receiving the drug or within 60 days of the last dose.
- Patient characteristics collected at diagnosis included age, sex, International Staging System stage, revised International Staging System stage, and interphase fluorescence in situ hybridization abnormalities.
- Investigators considered the first relapse after January 2015 requiring new systemic therapy as the index relapse and study start time.
TAKEAWAY:
- Analysis revealed an overall response rate of 56.2% and median progression-free survival of 11 months with retreatment.
- Patients with longer initial therapy duration with index drug (> 28.4 months) demonstrated superior progression-free survival (median, 16.9 vs 8.1 months; P < .001).
- Researchers found that patients with longer time gap between initial therapy and retreatment (> 46.1 months) showed better progression-free survival (median, 28.2 vs 8.9 months; P = .016).
- Among the 285 evaluable patients, 26% achieved partial response and 30.2% achieved very good partial response or better with retreatment.
IN PRACTICE:
“Retreatment with previously refractory drugs is a viable option for late-line [relapsed/refractory multiple myeloma]. Patients with a longer gap between initial line of therapy with index drug and retreatment had superior outcomes with retreatment,” wrote the authors of the study.
SOURCE:
The study was led by Utkarsh Goel, Division of Hematology, Mayo Clinic in Rochester, Minnesota. It was published online on December 24, 2024, in Blood Advances.
LIMITATIONS:
The retrospective nature and single-institution design of the study may introduce bias in terms of patient population and practice patterns. The favorable outcomes observed in patients with longer initial therapy duration and greater time between treatments could reflect selection bias toward more indolent disease biology. Despite adjusting for nonrefractory partner drugs during index relapse, residual bias may limit the ability to attribute outcomes solely to retreatment. The heterogeneous nature of treatments received during index relapse may limit comparisons across different groups.
DISCLOSURES:
Nelson Leung reported ties with AbbVie, Senseonics, Verrica Pharmaceuticals, and Omeros. Yi Lin disclosed relationships with multiple institutions, including Bristol Myers Squibb, Caribou Biosciences, and Janssen Oncology. Shaji Kumar reported ties with AbbVie, Bristol-Myers Squibb/Celgene, and Janssen Oncology. Additional disclosures were noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers retrospectively reviewed patients with relapsed/refractory multiple myeloma who started new systemic therapy for disease progression between January 2015 and April 2022 at their institution.
- Analysis included 315 patients treated with a drug that their disease had previously been refractory to, defined as disease progression while receiving the drug or within 60 days of the last dose.
- Patient characteristics collected at diagnosis included age, sex, International Staging System stage, revised International Staging System stage, and interphase fluorescence in situ hybridization abnormalities.
- Investigators considered the first relapse after January 2015 requiring new systemic therapy as the index relapse and study start time.
TAKEAWAY:
- Analysis revealed an overall response rate of 56.2% and median progression-free survival of 11 months with retreatment.
- Patients with longer initial therapy duration with index drug (> 28.4 months) demonstrated superior progression-free survival (median, 16.9 vs 8.1 months; P < .001).
- Researchers found that patients with longer time gap between initial therapy and retreatment (> 46.1 months) showed better progression-free survival (median, 28.2 vs 8.9 months; P = .016).
- Among the 285 evaluable patients, 26% achieved partial response and 30.2% achieved very good partial response or better with retreatment.
IN PRACTICE:
“Retreatment with previously refractory drugs is a viable option for late-line [relapsed/refractory multiple myeloma]. Patients with a longer gap between initial line of therapy with index drug and retreatment had superior outcomes with retreatment,” wrote the authors of the study.
SOURCE:
The study was led by Utkarsh Goel, Division of Hematology, Mayo Clinic in Rochester, Minnesota. It was published online on December 24, 2024, in Blood Advances.
LIMITATIONS:
The retrospective nature and single-institution design of the study may introduce bias in terms of patient population and practice patterns. The favorable outcomes observed in patients with longer initial therapy duration and greater time between treatments could reflect selection bias toward more indolent disease biology. Despite adjusting for nonrefractory partner drugs during index relapse, residual bias may limit the ability to attribute outcomes solely to retreatment. The heterogeneous nature of treatments received during index relapse may limit comparisons across different groups.
DISCLOSURES:
Nelson Leung reported ties with AbbVie, Senseonics, Verrica Pharmaceuticals, and Omeros. Yi Lin disclosed relationships with multiple institutions, including Bristol Myers Squibb, Caribou Biosciences, and Janssen Oncology. Shaji Kumar reported ties with AbbVie, Bristol-Myers Squibb/Celgene, and Janssen Oncology. Additional disclosures were noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers retrospectively reviewed patients with relapsed/refractory multiple myeloma who started new systemic therapy for disease progression between January 2015 and April 2022 at their institution.
- Analysis included 315 patients treated with a drug that their disease had previously been refractory to, defined as disease progression while receiving the drug or within 60 days of the last dose.
- Patient characteristics collected at diagnosis included age, sex, International Staging System stage, revised International Staging System stage, and interphase fluorescence in situ hybridization abnormalities.
- Investigators considered the first relapse after January 2015 requiring new systemic therapy as the index relapse and study start time.
TAKEAWAY:
- Analysis revealed an overall response rate of 56.2% and median progression-free survival of 11 months with retreatment.
- Patients with longer initial therapy duration with index drug (> 28.4 months) demonstrated superior progression-free survival (median, 16.9 vs 8.1 months; P < .001).
- Researchers found that patients with longer time gap between initial therapy and retreatment (> 46.1 months) showed better progression-free survival (median, 28.2 vs 8.9 months; P = .016).
- Among the 285 evaluable patients, 26% achieved partial response and 30.2% achieved very good partial response or better with retreatment.
IN PRACTICE:
“Retreatment with previously refractory drugs is a viable option for late-line [relapsed/refractory multiple myeloma]. Patients with a longer gap between initial line of therapy with index drug and retreatment had superior outcomes with retreatment,” wrote the authors of the study.
SOURCE:
The study was led by Utkarsh Goel, Division of Hematology, Mayo Clinic in Rochester, Minnesota. It was published online on December 24, 2024, in Blood Advances.
LIMITATIONS:
The retrospective nature and single-institution design of the study may introduce bias in terms of patient population and practice patterns. The favorable outcomes observed in patients with longer initial therapy duration and greater time between treatments could reflect selection bias toward more indolent disease biology. Despite adjusting for nonrefractory partner drugs during index relapse, residual bias may limit the ability to attribute outcomes solely to retreatment. The heterogeneous nature of treatments received during index relapse may limit comparisons across different groups.
DISCLOSURES:
Nelson Leung reported ties with AbbVie, Senseonics, Verrica Pharmaceuticals, and Omeros. Yi Lin disclosed relationships with multiple institutions, including Bristol Myers Squibb, Caribou Biosciences, and Janssen Oncology. Shaji Kumar reported ties with AbbVie, Bristol-Myers Squibb/Celgene, and Janssen Oncology. Additional disclosures were noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Daratumumab Confirmed as SOC for AL Amyloidosis
Adding DARA to VCd (D-VCd; Darzalex Faspro; Janssen Biotech) provided deeper and more rapid hematologic response and clinically meaningful and statistically significant improvement in overall survival (OS) and major organ deterioration progression-free survival (MOD-PFS), combined with 40.7% cardiac complete response (CR), first author Efstathios Kastritis, MD, said during presentation of an oral abstract at the American Society of Hematology (ASH) 2024 Annual Meeting.
“The Andromeda study is the first comparing two contemporary regimens that shows a significant survival improvement for patients with AL amyloidosis,” said Kastritis, an associate professor at the National and Kapodistrian University of Athens in Greece. “These findings reaffirm frontline D-VCd as the standard of care in this difficult-to-treat disease.”
The regimen was approved for this indication in 2021 based on prior earlier findings from the Andromeda trial. The current results are from a preplanned analysis for MOD-PFS and OS.
At a median follow-up of 61.4 months, the overall hematologic CR rates were 59.5% and 19.2% among 388 patients randomized to receive D-VCd or VCd, respectively (odds ratio, 6.03), which showed continued improvement with additional DARA vs the 53.3% and 18.1% rates observed at the primary analysis, Kastritis reported.
Time to hematologic CR was 67.5 days and 85.0 days in the treatment groups, respectively, and median duration of hematologic CR was not reached in either group.
A significant 56% improvement was also observed in MOD-PFS (hazard ratio [HR], 0.44). Median MOD-PFS was not reached in the D-VCd group and was 30.3 months in the VCd group.
A significant 38% improvement was observed in OS (HR, 0.62), 5-year OS was 76.1% vs 64.7% in the D-VCd and VCd groups, respectively, he said.
“[The OS] benefit occurred even though more than 70% of the patients in the VCd arm who received a subsequent therapy were treated with a DARA-based regimen,” he stressed. “This further emphasizes the importance of using DSTS in the frontline setting.”
Trial participants had newly diagnosed AL amyloidosis with measurable hematologic disease, one or more involved organs, cardiac stage I-IIIA, estimated glomerular filtration rate of at least 20 mL/min, and absence of symptomatic multiple myeloma. They were randomized 1:1 to the two treatment groups. All patients received 1.3 mg/m2 of bortezomib by weekly injection, 300 mg/m2 of cyclophosphamide either by weekly oral or intravenous administration, and 20-40 mg of dexamethasone by weekly oral or intravenous administration for six 28-day cycles.
Those in the D-VCd group also received 1800 mg of DARA coformulated with rHuPH20 as a weekly injection in cycles 1-2, as a biweekly injection in cycles 3-6, and by injection every 4 weeks thereafter for up to 24 28-day cycles.
The median duration of treatment was 21.3 months for D-VCd and 5.3 months for VCd, and of 122 patients who received subsequent therapy, 82 (67%) received subsequent DARA.
Patients who achieved hematologic CR had better MOD-PFS and OS (HR, 0.30 and 0.41, respectively), regardless of the treatment received, he noted, adding that “this further supports that complete hematologic response is a valid early endpoint for the evaluation of anti-monoclonal therapies in AL amyloidosis.”
“I think this is very important for the further development of new treatments in this disease,” he said.
Of note, cardiac and renal response rates in the D-VCd group were about two to three times greater than those in the VCd group at 6, 12, 24, 36, and 48 months, Kastritis said.
Among 235 patients with an evaluable cardiac response, 113 achieved a very good partial response or better, including 76 of 118 (64.4%) in the D-VCd group and 37 of 117 (31.6%) in the VCd group. Of these, 48 (40.7%) and 16 (13.7%) achieved a cardiac CR.
Grade 3 or 4 treatment-emergent adverse events (TEAEs) occurring in at least 5% of patients in the D-VCd and VCd groups, respectively, were lymphopenia (13% and 10%), pneumonia (8% and 4%), hypokalemia (2% and 5%), and peripheral edema (3% and 6%), he noted, adding that systemic administration-related reactions occurred in 14 (7%) of patients receiving D-VCd; all were grade 1 or 2 and most (86%) occurred after the first injection. TEAEs led to treatment discontinuation in 5% and 4% of patients in the groups, respectively.
No new safety signals were observed during the extended follow-up, he said.
Kastritis reported relationships with Pfizer, Genesis Pharma, Sanofi, AbbVie, GSK, Prothena, Janssen, and Amgen.
A version of this article first appeared on Medscape.com.
Adding DARA to VCd (D-VCd; Darzalex Faspro; Janssen Biotech) provided deeper and more rapid hematologic response and clinically meaningful and statistically significant improvement in overall survival (OS) and major organ deterioration progression-free survival (MOD-PFS), combined with 40.7% cardiac complete response (CR), first author Efstathios Kastritis, MD, said during presentation of an oral abstract at the American Society of Hematology (ASH) 2024 Annual Meeting.
“The Andromeda study is the first comparing two contemporary regimens that shows a significant survival improvement for patients with AL amyloidosis,” said Kastritis, an associate professor at the National and Kapodistrian University of Athens in Greece. “These findings reaffirm frontline D-VCd as the standard of care in this difficult-to-treat disease.”
The regimen was approved for this indication in 2021 based on prior earlier findings from the Andromeda trial. The current results are from a preplanned analysis for MOD-PFS and OS.
At a median follow-up of 61.4 months, the overall hematologic CR rates were 59.5% and 19.2% among 388 patients randomized to receive D-VCd or VCd, respectively (odds ratio, 6.03), which showed continued improvement with additional DARA vs the 53.3% and 18.1% rates observed at the primary analysis, Kastritis reported.
Time to hematologic CR was 67.5 days and 85.0 days in the treatment groups, respectively, and median duration of hematologic CR was not reached in either group.
A significant 56% improvement was also observed in MOD-PFS (hazard ratio [HR], 0.44). Median MOD-PFS was not reached in the D-VCd group and was 30.3 months in the VCd group.
A significant 38% improvement was observed in OS (HR, 0.62), 5-year OS was 76.1% vs 64.7% in the D-VCd and VCd groups, respectively, he said.
“[The OS] benefit occurred even though more than 70% of the patients in the VCd arm who received a subsequent therapy were treated with a DARA-based regimen,” he stressed. “This further emphasizes the importance of using DSTS in the frontline setting.”
Trial participants had newly diagnosed AL amyloidosis with measurable hematologic disease, one or more involved organs, cardiac stage I-IIIA, estimated glomerular filtration rate of at least 20 mL/min, and absence of symptomatic multiple myeloma. They were randomized 1:1 to the two treatment groups. All patients received 1.3 mg/m2 of bortezomib by weekly injection, 300 mg/m2 of cyclophosphamide either by weekly oral or intravenous administration, and 20-40 mg of dexamethasone by weekly oral or intravenous administration for six 28-day cycles.
Those in the D-VCd group also received 1800 mg of DARA coformulated with rHuPH20 as a weekly injection in cycles 1-2, as a biweekly injection in cycles 3-6, and by injection every 4 weeks thereafter for up to 24 28-day cycles.
The median duration of treatment was 21.3 months for D-VCd and 5.3 months for VCd, and of 122 patients who received subsequent therapy, 82 (67%) received subsequent DARA.
Patients who achieved hematologic CR had better MOD-PFS and OS (HR, 0.30 and 0.41, respectively), regardless of the treatment received, he noted, adding that “this further supports that complete hematologic response is a valid early endpoint for the evaluation of anti-monoclonal therapies in AL amyloidosis.”
“I think this is very important for the further development of new treatments in this disease,” he said.
Of note, cardiac and renal response rates in the D-VCd group were about two to three times greater than those in the VCd group at 6, 12, 24, 36, and 48 months, Kastritis said.
Among 235 patients with an evaluable cardiac response, 113 achieved a very good partial response or better, including 76 of 118 (64.4%) in the D-VCd group and 37 of 117 (31.6%) in the VCd group. Of these, 48 (40.7%) and 16 (13.7%) achieved a cardiac CR.
Grade 3 or 4 treatment-emergent adverse events (TEAEs) occurring in at least 5% of patients in the D-VCd and VCd groups, respectively, were lymphopenia (13% and 10%), pneumonia (8% and 4%), hypokalemia (2% and 5%), and peripheral edema (3% and 6%), he noted, adding that systemic administration-related reactions occurred in 14 (7%) of patients receiving D-VCd; all were grade 1 or 2 and most (86%) occurred after the first injection. TEAEs led to treatment discontinuation in 5% and 4% of patients in the groups, respectively.
No new safety signals were observed during the extended follow-up, he said.
Kastritis reported relationships with Pfizer, Genesis Pharma, Sanofi, AbbVie, GSK, Prothena, Janssen, and Amgen.
A version of this article first appeared on Medscape.com.
Adding DARA to VCd (D-VCd; Darzalex Faspro; Janssen Biotech) provided deeper and more rapid hematologic response and clinically meaningful and statistically significant improvement in overall survival (OS) and major organ deterioration progression-free survival (MOD-PFS), combined with 40.7% cardiac complete response (CR), first author Efstathios Kastritis, MD, said during presentation of an oral abstract at the American Society of Hematology (ASH) 2024 Annual Meeting.
“The Andromeda study is the first comparing two contemporary regimens that shows a significant survival improvement for patients with AL amyloidosis,” said Kastritis, an associate professor at the National and Kapodistrian University of Athens in Greece. “These findings reaffirm frontline D-VCd as the standard of care in this difficult-to-treat disease.”
The regimen was approved for this indication in 2021 based on prior earlier findings from the Andromeda trial. The current results are from a preplanned analysis for MOD-PFS and OS.
At a median follow-up of 61.4 months, the overall hematologic CR rates were 59.5% and 19.2% among 388 patients randomized to receive D-VCd or VCd, respectively (odds ratio, 6.03), which showed continued improvement with additional DARA vs the 53.3% and 18.1% rates observed at the primary analysis, Kastritis reported.
Time to hematologic CR was 67.5 days and 85.0 days in the treatment groups, respectively, and median duration of hematologic CR was not reached in either group.
A significant 56% improvement was also observed in MOD-PFS (hazard ratio [HR], 0.44). Median MOD-PFS was not reached in the D-VCd group and was 30.3 months in the VCd group.
A significant 38% improvement was observed in OS (HR, 0.62), 5-year OS was 76.1% vs 64.7% in the D-VCd and VCd groups, respectively, he said.
“[The OS] benefit occurred even though more than 70% of the patients in the VCd arm who received a subsequent therapy were treated with a DARA-based regimen,” he stressed. “This further emphasizes the importance of using DSTS in the frontline setting.”
Trial participants had newly diagnosed AL amyloidosis with measurable hematologic disease, one or more involved organs, cardiac stage I-IIIA, estimated glomerular filtration rate of at least 20 mL/min, and absence of symptomatic multiple myeloma. They were randomized 1:1 to the two treatment groups. All patients received 1.3 mg/m2 of bortezomib by weekly injection, 300 mg/m2 of cyclophosphamide either by weekly oral or intravenous administration, and 20-40 mg of dexamethasone by weekly oral or intravenous administration for six 28-day cycles.
Those in the D-VCd group also received 1800 mg of DARA coformulated with rHuPH20 as a weekly injection in cycles 1-2, as a biweekly injection in cycles 3-6, and by injection every 4 weeks thereafter for up to 24 28-day cycles.
The median duration of treatment was 21.3 months for D-VCd and 5.3 months for VCd, and of 122 patients who received subsequent therapy, 82 (67%) received subsequent DARA.
Patients who achieved hematologic CR had better MOD-PFS and OS (HR, 0.30 and 0.41, respectively), regardless of the treatment received, he noted, adding that “this further supports that complete hematologic response is a valid early endpoint for the evaluation of anti-monoclonal therapies in AL amyloidosis.”
“I think this is very important for the further development of new treatments in this disease,” he said.
Of note, cardiac and renal response rates in the D-VCd group were about two to three times greater than those in the VCd group at 6, 12, 24, 36, and 48 months, Kastritis said.
Among 235 patients with an evaluable cardiac response, 113 achieved a very good partial response or better, including 76 of 118 (64.4%) in the D-VCd group and 37 of 117 (31.6%) in the VCd group. Of these, 48 (40.7%) and 16 (13.7%) achieved a cardiac CR.
Grade 3 or 4 treatment-emergent adverse events (TEAEs) occurring in at least 5% of patients in the D-VCd and VCd groups, respectively, were lymphopenia (13% and 10%), pneumonia (8% and 4%), hypokalemia (2% and 5%), and peripheral edema (3% and 6%), he noted, adding that systemic administration-related reactions occurred in 14 (7%) of patients receiving D-VCd; all were grade 1 or 2 and most (86%) occurred after the first injection. TEAEs led to treatment discontinuation in 5% and 4% of patients in the groups, respectively.
No new safety signals were observed during the extended follow-up, he said.
Kastritis reported relationships with Pfizer, Genesis Pharma, Sanofi, AbbVie, GSK, Prothena, Janssen, and Amgen.
A version of this article first appeared on Medscape.com.
FROM ASH 2024
Smoldering MM: Big Prevention Benefits With Daratumumab?
Among 390 patients with SMM (194 assigned to daratumumab and 196 to active monitoring), progression to active MM or death over a follow-up of 65.2 (0-76.6) months was 51% lower in the daratumumab group vs active monitoring (34.5% vs 50.5%, hazard ratio [HR], 0.49; 95% CI, 0.36-0.67; P < .0001), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting and in a simultaneous publication in the New England Journal of Medicine.
Rahul Banerjee, MD, an assistant professor with the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, who wasn’t involved with the research, said the study “is a big deal, and I suspect this will ultimately lead to an FDA [Food and Drug Administration] approval for daratumumab in this setting. If using daratumumab up-front can prevent further myeloma and therefore make patients live longer, this would be immediately adopted at many practices.”
As study first author Meletios Athanasios Dimopoulos, MD, of National and Kapodistrian University of Athens and Alexandra General Hospital in Greece, noted at a news briefing, SMM is common, affecting 0.5% of the population aged over 40, per a 2023 Iceland study.
“Standard practice is close follow-up without immediate intervention. However, this oftentimes ends in organ tissue damage, and hypercalcemia, bone lesions, renal impairment, and anemia,” Dimopoulos said.
According to him, researchers launched the AQUILA study in light of indications that daratumumab may benefit patients with intermediate- and high-risk SMM.
For the study, researchers recruited patients from 2017 to 2019 in 23 countries with confirmed high-risk SMM for ≤ 5 years (median age, 64 [31-86] years; 47%-49% men; 83% White).
In the daratumumab group, the drug was administered in 28-day cycles until cycle 39, 36 months, or disease progression, whichever came first (median treatment duration, 38 months [35 months]).
At 5 years, progression-free survival (PFS) — the primary endpoint — was 63.1% (daratumumab) and 40.8% (active monitoring). Researchers estimated 60-month PFS rates at 63.1% and 40.8%, respectively, and overall response rates were 63.4% vs 2.0% (P < .0001), respectively.
The 60-month overall survival rates were 93.0% and 86.9% (HR, 0.52; 95% CI, 0.27-0.98) with 15 deaths in the daratumumab and 26 in the active monitoring group.
“During the follow-up period, there was continuous improvement in favor of the daratumumab arm,” Dimopoulos said. “Even after treatment was discontinued at 3 years, or even at 5 or 6 years, there was a continuous benefit from treatment with daratumumab.”
By clinical cutoff in May 2024, 65% of patients taking daratumumab had finished 39 cycles/3 years of treatment vs 40.8% in the active monitoring group. Progressive disease was the most common reason that patients stopped treatment (21.8% and 41.8% of patients in the groups, respectively).
Grade 3/4 treatment-emergent adverse events (TEAEs) occurred in 40.4% (daratumumab) and 30.1% (active monitoring) of patients. The most common was hypertension (5.7% and 4.6%, respectively).
In the daratumumab group, 5.7% discontinued therapy because of TEAEs, which the researchers described as a “low” number, and fatal TEAEs were similar in both groups (1.0% and 2.0%, respectively).
Banerjee said that “one theoretical risk of using daratumumab monotherapy to treat perceived high-risk SMM is that if the patient actually has active multiple myeloma, you are undertreating them. For anyone with HR-SMM, active multiple myeloma must be completely ruled out. I always insist on both a PET-CT and a whole-body MRI to evaluate the bone marrow comprehensively.”
For now, Banerjee said, clinicians should wait for the US Food and Drug Administration approval before prescribing daratumumab for high-risk SMM.
Are there alternatives to reduce the risk for SMM turning into MM? “Generally, I advise close observation in most cases, but we do have clinical trials in this space,” Banerjee said. “Technically, it is possible to consider lenalidomide monotherapy in SMM based on the results of a large phase 3 study. But lenalidomide is expensive and has many side effects. Insurance companies often won’t cover it fully, and patients almost always have at least one side effect.”
Also, he added, “only half of patients saw their high-risk SMM disease burden drop. Lenalidomide also has a clear link to rare, delayed toxicities such as second primary malignancies, which makes us nervous.”
Janssen Pharmaceuticals, the maker of daratumumab, funded the study. Dimopoulos disclosed ties with Sanofi, Regeneron, Menarini, Takeda, GSK, BMS, Janssen Pharmaceuticals, BeiGene, Swixx, AstraZeneca, and Amgen. Banerjee disclosed ties with AbbVie, Adaptive, BMS, Caribou, Genentech/Roche, GSK, Karyopharm Therapeutics, Legend, Johnson & Johnson, Novartis, Pack, Pfizer, Prothena, Sanofi Pasteur, and SparkCures. Some other authors reported various and multiple disclosures, including ties with Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Among 390 patients with SMM (194 assigned to daratumumab and 196 to active monitoring), progression to active MM or death over a follow-up of 65.2 (0-76.6) months was 51% lower in the daratumumab group vs active monitoring (34.5% vs 50.5%, hazard ratio [HR], 0.49; 95% CI, 0.36-0.67; P < .0001), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting and in a simultaneous publication in the New England Journal of Medicine.
Rahul Banerjee, MD, an assistant professor with the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, who wasn’t involved with the research, said the study “is a big deal, and I suspect this will ultimately lead to an FDA [Food and Drug Administration] approval for daratumumab in this setting. If using daratumumab up-front can prevent further myeloma and therefore make patients live longer, this would be immediately adopted at many practices.”
As study first author Meletios Athanasios Dimopoulos, MD, of National and Kapodistrian University of Athens and Alexandra General Hospital in Greece, noted at a news briefing, SMM is common, affecting 0.5% of the population aged over 40, per a 2023 Iceland study.
“Standard practice is close follow-up without immediate intervention. However, this oftentimes ends in organ tissue damage, and hypercalcemia, bone lesions, renal impairment, and anemia,” Dimopoulos said.
According to him, researchers launched the AQUILA study in light of indications that daratumumab may benefit patients with intermediate- and high-risk SMM.
For the study, researchers recruited patients from 2017 to 2019 in 23 countries with confirmed high-risk SMM for ≤ 5 years (median age, 64 [31-86] years; 47%-49% men; 83% White).
In the daratumumab group, the drug was administered in 28-day cycles until cycle 39, 36 months, or disease progression, whichever came first (median treatment duration, 38 months [35 months]).
At 5 years, progression-free survival (PFS) — the primary endpoint — was 63.1% (daratumumab) and 40.8% (active monitoring). Researchers estimated 60-month PFS rates at 63.1% and 40.8%, respectively, and overall response rates were 63.4% vs 2.0% (P < .0001), respectively.
The 60-month overall survival rates were 93.0% and 86.9% (HR, 0.52; 95% CI, 0.27-0.98) with 15 deaths in the daratumumab and 26 in the active monitoring group.
“During the follow-up period, there was continuous improvement in favor of the daratumumab arm,” Dimopoulos said. “Even after treatment was discontinued at 3 years, or even at 5 or 6 years, there was a continuous benefit from treatment with daratumumab.”
By clinical cutoff in May 2024, 65% of patients taking daratumumab had finished 39 cycles/3 years of treatment vs 40.8% in the active monitoring group. Progressive disease was the most common reason that patients stopped treatment (21.8% and 41.8% of patients in the groups, respectively).
Grade 3/4 treatment-emergent adverse events (TEAEs) occurred in 40.4% (daratumumab) and 30.1% (active monitoring) of patients. The most common was hypertension (5.7% and 4.6%, respectively).
In the daratumumab group, 5.7% discontinued therapy because of TEAEs, which the researchers described as a “low” number, and fatal TEAEs were similar in both groups (1.0% and 2.0%, respectively).
Banerjee said that “one theoretical risk of using daratumumab monotherapy to treat perceived high-risk SMM is that if the patient actually has active multiple myeloma, you are undertreating them. For anyone with HR-SMM, active multiple myeloma must be completely ruled out. I always insist on both a PET-CT and a whole-body MRI to evaluate the bone marrow comprehensively.”
For now, Banerjee said, clinicians should wait for the US Food and Drug Administration approval before prescribing daratumumab for high-risk SMM.
Are there alternatives to reduce the risk for SMM turning into MM? “Generally, I advise close observation in most cases, but we do have clinical trials in this space,” Banerjee said. “Technically, it is possible to consider lenalidomide monotherapy in SMM based on the results of a large phase 3 study. But lenalidomide is expensive and has many side effects. Insurance companies often won’t cover it fully, and patients almost always have at least one side effect.”
Also, he added, “only half of patients saw their high-risk SMM disease burden drop. Lenalidomide also has a clear link to rare, delayed toxicities such as second primary malignancies, which makes us nervous.”
Janssen Pharmaceuticals, the maker of daratumumab, funded the study. Dimopoulos disclosed ties with Sanofi, Regeneron, Menarini, Takeda, GSK, BMS, Janssen Pharmaceuticals, BeiGene, Swixx, AstraZeneca, and Amgen. Banerjee disclosed ties with AbbVie, Adaptive, BMS, Caribou, Genentech/Roche, GSK, Karyopharm Therapeutics, Legend, Johnson & Johnson, Novartis, Pack, Pfizer, Prothena, Sanofi Pasteur, and SparkCures. Some other authors reported various and multiple disclosures, including ties with Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Among 390 patients with SMM (194 assigned to daratumumab and 196 to active monitoring), progression to active MM or death over a follow-up of 65.2 (0-76.6) months was 51% lower in the daratumumab group vs active monitoring (34.5% vs 50.5%, hazard ratio [HR], 0.49; 95% CI, 0.36-0.67; P < .0001), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting and in a simultaneous publication in the New England Journal of Medicine.
Rahul Banerjee, MD, an assistant professor with the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, who wasn’t involved with the research, said the study “is a big deal, and I suspect this will ultimately lead to an FDA [Food and Drug Administration] approval for daratumumab in this setting. If using daratumumab up-front can prevent further myeloma and therefore make patients live longer, this would be immediately adopted at many practices.”
As study first author Meletios Athanasios Dimopoulos, MD, of National and Kapodistrian University of Athens and Alexandra General Hospital in Greece, noted at a news briefing, SMM is common, affecting 0.5% of the population aged over 40, per a 2023 Iceland study.
“Standard practice is close follow-up without immediate intervention. However, this oftentimes ends in organ tissue damage, and hypercalcemia, bone lesions, renal impairment, and anemia,” Dimopoulos said.
According to him, researchers launched the AQUILA study in light of indications that daratumumab may benefit patients with intermediate- and high-risk SMM.
For the study, researchers recruited patients from 2017 to 2019 in 23 countries with confirmed high-risk SMM for ≤ 5 years (median age, 64 [31-86] years; 47%-49% men; 83% White).
In the daratumumab group, the drug was administered in 28-day cycles until cycle 39, 36 months, or disease progression, whichever came first (median treatment duration, 38 months [35 months]).
At 5 years, progression-free survival (PFS) — the primary endpoint — was 63.1% (daratumumab) and 40.8% (active monitoring). Researchers estimated 60-month PFS rates at 63.1% and 40.8%, respectively, and overall response rates were 63.4% vs 2.0% (P < .0001), respectively.
The 60-month overall survival rates were 93.0% and 86.9% (HR, 0.52; 95% CI, 0.27-0.98) with 15 deaths in the daratumumab and 26 in the active monitoring group.
“During the follow-up period, there was continuous improvement in favor of the daratumumab arm,” Dimopoulos said. “Even after treatment was discontinued at 3 years, or even at 5 or 6 years, there was a continuous benefit from treatment with daratumumab.”
By clinical cutoff in May 2024, 65% of patients taking daratumumab had finished 39 cycles/3 years of treatment vs 40.8% in the active monitoring group. Progressive disease was the most common reason that patients stopped treatment (21.8% and 41.8% of patients in the groups, respectively).
Grade 3/4 treatment-emergent adverse events (TEAEs) occurred in 40.4% (daratumumab) and 30.1% (active monitoring) of patients. The most common was hypertension (5.7% and 4.6%, respectively).
In the daratumumab group, 5.7% discontinued therapy because of TEAEs, which the researchers described as a “low” number, and fatal TEAEs were similar in both groups (1.0% and 2.0%, respectively).
Banerjee said that “one theoretical risk of using daratumumab monotherapy to treat perceived high-risk SMM is that if the patient actually has active multiple myeloma, you are undertreating them. For anyone with HR-SMM, active multiple myeloma must be completely ruled out. I always insist on both a PET-CT and a whole-body MRI to evaluate the bone marrow comprehensively.”
For now, Banerjee said, clinicians should wait for the US Food and Drug Administration approval before prescribing daratumumab for high-risk SMM.
Are there alternatives to reduce the risk for SMM turning into MM? “Generally, I advise close observation in most cases, but we do have clinical trials in this space,” Banerjee said. “Technically, it is possible to consider lenalidomide monotherapy in SMM based on the results of a large phase 3 study. But lenalidomide is expensive and has many side effects. Insurance companies often won’t cover it fully, and patients almost always have at least one side effect.”
Also, he added, “only half of patients saw their high-risk SMM disease burden drop. Lenalidomide also has a clear link to rare, delayed toxicities such as second primary malignancies, which makes us nervous.”
Janssen Pharmaceuticals, the maker of daratumumab, funded the study. Dimopoulos disclosed ties with Sanofi, Regeneron, Menarini, Takeda, GSK, BMS, Janssen Pharmaceuticals, BeiGene, Swixx, AstraZeneca, and Amgen. Banerjee disclosed ties with AbbVie, Adaptive, BMS, Caribou, Genentech/Roche, GSK, Karyopharm Therapeutics, Legend, Johnson & Johnson, Novartis, Pack, Pfizer, Prothena, Sanofi Pasteur, and SparkCures. Some other authors reported various and multiple disclosures, including ties with Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM ASH 2024
Multiple Myeloma: Dexamethasone-Sparing Approach Benefits Frail Older Adults
The study “is the first randomized phase 3 study dedicated to frail patients,” said first author Salomon Manier, MD, PhD, an associate professor of hematology at Lille University Hospital, Lille, France. He presented the findings this week at the American Society of Hematology (ASH) 2024 Annual Meeting in San Diego.
“It shows that daratumumab-lenalidomide [with limited dexamethasone] led to a significant reduced risk of progression or death by 49% in frail patients, with a favorable safety profile and an improved health-related quality of life,” Manier said.
Older adult patients who are newly diagnosed with MM have varying levels of fitness or frailty and have been shown to have shorter survival, with higher rates of nonhematologic adverse events and treatment discontinuation.
While the regimen of daratumumab, lenalidomide, and dexamethasone has become a standard of care, with efficacy and tolerance, including for patients with frailty, the infection and pneumonia rates with the approach can be high, particularly for patients with frailty.
To evaluate if an alternative, dexamethasone-sparing approach could improve outcomes while limiting toxicity for older adults, Manier and his colleagues conducted the prospective, open-label phase 3 IFM2017-03 trial, involving 295 patients (age, 65 years) with newly diagnosed MM at 90 centers in France.
The patients had a median age of 81, with 84% older than 75 years and 61% older than 80 years. All had an Eastern Cooperative Oncology Group proxy frailty score ≥ 2.
The patients were randomized 1:2 to treatment either with the Rd regimen of 28-day cycles of lenalidomide (25 mg/d, 21/28) and dexamethasone (20 mg once weekly) or with the dexamethasone-sparing regimen (DR) of daratumumab (1800 mg subcutaneous once weekly for 8 weeks, once every 2 weeks for 16 weeks, and once every 4 weeks thereafter), lenalidomide (25 mg/d, 21/28), and two cycles of dexamethasone (20 mg once weekly for 8 weeks then stopping).
The randomization included stratification based on age and cancer stage. Baseline characteristics were well balanced in the two groups.
Both regimens were administered until disease progression or unacceptable toxicity.
As of the data cut-off in November 2024, with a median follow-up of 46.3 months, 81 of the original 200 patients in the DR arm remained on treatment, and 11 of 95 continued in the Rd arm.
The overall median treatment duration among the 200 original patients in the DR arm was 31.6 months and 14.3 months in the Rd arm.
The study met its primary endpoint of progression-free survival (PFS), with a median rate of 53.4 months in the DR arm vs 22.5 months in the Rd arm (hazard ratio [HR], 0.51; P < .0001).
The improved PFS in the DR arm was observed across all subgroups based on age, Charlson comorbidity index, cancer stage, cytogenetics, and creatinine clearance; however, those with lower frailty scores had better outcomes in both groups.
A median overall survival was not reached in the DR arm vs 47.2 months in the Rd arm (HR, 0.52; P = .0001).
The DR arm also showed a higher overall best response rate of 94% vs 86% (P = .005), respectively, with deeper responses in the DR arm at all time points, including the earliest points at 4 months.
In terms of adverse events (AEs), at least one AE of grade ≥ 3 occurred in 89% in the DR arm and 79% in the Rd arm.
Those in the DR arm had significantly more grade 3 or higher hematologic AEs with neutropenia (62% vs 34%); however, grade ≥ 3 infections were similar, with 19% in the DR arm and 21% in the Rd arm. Infections involving pneumonia occurred in 6% and 8%, respectively.
There were no significant differences between the two arms in discontinuations due to AEs (30% in the DR arm and 34% in the Rd arm).
While health-related quality of life measures at baseline were well balanced between the two groups, those in the DR arm reported significantly shorter times to clinically meaningful improvement in all domains of the EORTC Core Quality of Life questionnaire (EORTC QLQ-C30).
“The safety profile was significantly improved and was favorable, without increased infection or pneumonia rates, with similar rates of treatment discontinuation,” Manier said.
Based on the findings, “we believe that the dexamethasone-sparing strategy is effective and safe for treating these frail patients with multiple myeloma,” he added.
Commenting on the study, Manni Mohyuddin, MD, an assistant professor in the multiple myeloma program at the Huntsman Cancer Institute, University of Utah, Salt Lake City, noted that, with the popularity of triplet regimens such as daratumumab, lenalidomide, and dexamethasone, the Rd regimen in the study is not as commonly used.
“But what this trial tells us is that efficacy outcomes in such a group of patients are encouraging despite getting rid of dexamethasone so quickly,” he said in an interview.
However, “while the tide is changing, dexamethasone is still given long-term, week after week after week in most myeloma protocols and in the community,” he noted. “Hopefully, this trial, and some of the other work, will lead to a change in this space.”
Mohyuddin suggests one approach can involve starting off with just daratumumab and a low dose of dexamethasone, then adding lenalidomide at a lower dose later in a sequential/graded approach.
“Other approaches that should be studied should be bispecific antibodies used sparingly, with less frequent dosing, or finite period,” he added. “There is lot to refine.”
Mohyuddin added a critique that the study’s endpoint of PFS may not have been ideal for the population of elderly and frail patients.
“Older people generally prioritize functional independence and quality of life, and perhaps a more patient-centered endpoint could have led to an even more informative study,” he said.
Manier’s disclosures included consultancy with Takeda Pharmaceuticals, Sanofi, Novartis, Janssen, GlaxoSmithKline, Celgene/BMS, Amgen, Adaptive Biotechnologies, Roche, Regeneron, and AbbVie. Mohyuddin had no disclosures.
A version of this article appeared on Medscape.com.
The study “is the first randomized phase 3 study dedicated to frail patients,” said first author Salomon Manier, MD, PhD, an associate professor of hematology at Lille University Hospital, Lille, France. He presented the findings this week at the American Society of Hematology (ASH) 2024 Annual Meeting in San Diego.
“It shows that daratumumab-lenalidomide [with limited dexamethasone] led to a significant reduced risk of progression or death by 49% in frail patients, with a favorable safety profile and an improved health-related quality of life,” Manier said.
Older adult patients who are newly diagnosed with MM have varying levels of fitness or frailty and have been shown to have shorter survival, with higher rates of nonhematologic adverse events and treatment discontinuation.
While the regimen of daratumumab, lenalidomide, and dexamethasone has become a standard of care, with efficacy and tolerance, including for patients with frailty, the infection and pneumonia rates with the approach can be high, particularly for patients with frailty.
To evaluate if an alternative, dexamethasone-sparing approach could improve outcomes while limiting toxicity for older adults, Manier and his colleagues conducted the prospective, open-label phase 3 IFM2017-03 trial, involving 295 patients (age, 65 years) with newly diagnosed MM at 90 centers in France.
The patients had a median age of 81, with 84% older than 75 years and 61% older than 80 years. All had an Eastern Cooperative Oncology Group proxy frailty score ≥ 2.
The patients were randomized 1:2 to treatment either with the Rd regimen of 28-day cycles of lenalidomide (25 mg/d, 21/28) and dexamethasone (20 mg once weekly) or with the dexamethasone-sparing regimen (DR) of daratumumab (1800 mg subcutaneous once weekly for 8 weeks, once every 2 weeks for 16 weeks, and once every 4 weeks thereafter), lenalidomide (25 mg/d, 21/28), and two cycles of dexamethasone (20 mg once weekly for 8 weeks then stopping).
The randomization included stratification based on age and cancer stage. Baseline characteristics were well balanced in the two groups.
Both regimens were administered until disease progression or unacceptable toxicity.
As of the data cut-off in November 2024, with a median follow-up of 46.3 months, 81 of the original 200 patients in the DR arm remained on treatment, and 11 of 95 continued in the Rd arm.
The overall median treatment duration among the 200 original patients in the DR arm was 31.6 months and 14.3 months in the Rd arm.
The study met its primary endpoint of progression-free survival (PFS), with a median rate of 53.4 months in the DR arm vs 22.5 months in the Rd arm (hazard ratio [HR], 0.51; P < .0001).
The improved PFS in the DR arm was observed across all subgroups based on age, Charlson comorbidity index, cancer stage, cytogenetics, and creatinine clearance; however, those with lower frailty scores had better outcomes in both groups.
A median overall survival was not reached in the DR arm vs 47.2 months in the Rd arm (HR, 0.52; P = .0001).
The DR arm also showed a higher overall best response rate of 94% vs 86% (P = .005), respectively, with deeper responses in the DR arm at all time points, including the earliest points at 4 months.
In terms of adverse events (AEs), at least one AE of grade ≥ 3 occurred in 89% in the DR arm and 79% in the Rd arm.
Those in the DR arm had significantly more grade 3 or higher hematologic AEs with neutropenia (62% vs 34%); however, grade ≥ 3 infections were similar, with 19% in the DR arm and 21% in the Rd arm. Infections involving pneumonia occurred in 6% and 8%, respectively.
There were no significant differences between the two arms in discontinuations due to AEs (30% in the DR arm and 34% in the Rd arm).
While health-related quality of life measures at baseline were well balanced between the two groups, those in the DR arm reported significantly shorter times to clinically meaningful improvement in all domains of the EORTC Core Quality of Life questionnaire (EORTC QLQ-C30).
“The safety profile was significantly improved and was favorable, without increased infection or pneumonia rates, with similar rates of treatment discontinuation,” Manier said.
Based on the findings, “we believe that the dexamethasone-sparing strategy is effective and safe for treating these frail patients with multiple myeloma,” he added.
Commenting on the study, Manni Mohyuddin, MD, an assistant professor in the multiple myeloma program at the Huntsman Cancer Institute, University of Utah, Salt Lake City, noted that, with the popularity of triplet regimens such as daratumumab, lenalidomide, and dexamethasone, the Rd regimen in the study is not as commonly used.
“But what this trial tells us is that efficacy outcomes in such a group of patients are encouraging despite getting rid of dexamethasone so quickly,” he said in an interview.
However, “while the tide is changing, dexamethasone is still given long-term, week after week after week in most myeloma protocols and in the community,” he noted. “Hopefully, this trial, and some of the other work, will lead to a change in this space.”
Mohyuddin suggests one approach can involve starting off with just daratumumab and a low dose of dexamethasone, then adding lenalidomide at a lower dose later in a sequential/graded approach.
“Other approaches that should be studied should be bispecific antibodies used sparingly, with less frequent dosing, or finite period,” he added. “There is lot to refine.”
Mohyuddin added a critique that the study’s endpoint of PFS may not have been ideal for the population of elderly and frail patients.
“Older people generally prioritize functional independence and quality of life, and perhaps a more patient-centered endpoint could have led to an even more informative study,” he said.
Manier’s disclosures included consultancy with Takeda Pharmaceuticals, Sanofi, Novartis, Janssen, GlaxoSmithKline, Celgene/BMS, Amgen, Adaptive Biotechnologies, Roche, Regeneron, and AbbVie. Mohyuddin had no disclosures.
A version of this article appeared on Medscape.com.
The study “is the first randomized phase 3 study dedicated to frail patients,” said first author Salomon Manier, MD, PhD, an associate professor of hematology at Lille University Hospital, Lille, France. He presented the findings this week at the American Society of Hematology (ASH) 2024 Annual Meeting in San Diego.
“It shows that daratumumab-lenalidomide [with limited dexamethasone] led to a significant reduced risk of progression or death by 49% in frail patients, with a favorable safety profile and an improved health-related quality of life,” Manier said.
Older adult patients who are newly diagnosed with MM have varying levels of fitness or frailty and have been shown to have shorter survival, with higher rates of nonhematologic adverse events and treatment discontinuation.
While the regimen of daratumumab, lenalidomide, and dexamethasone has become a standard of care, with efficacy and tolerance, including for patients with frailty, the infection and pneumonia rates with the approach can be high, particularly for patients with frailty.
To evaluate if an alternative, dexamethasone-sparing approach could improve outcomes while limiting toxicity for older adults, Manier and his colleagues conducted the prospective, open-label phase 3 IFM2017-03 trial, involving 295 patients (age, 65 years) with newly diagnosed MM at 90 centers in France.
The patients had a median age of 81, with 84% older than 75 years and 61% older than 80 years. All had an Eastern Cooperative Oncology Group proxy frailty score ≥ 2.
The patients were randomized 1:2 to treatment either with the Rd regimen of 28-day cycles of lenalidomide (25 mg/d, 21/28) and dexamethasone (20 mg once weekly) or with the dexamethasone-sparing regimen (DR) of daratumumab (1800 mg subcutaneous once weekly for 8 weeks, once every 2 weeks for 16 weeks, and once every 4 weeks thereafter), lenalidomide (25 mg/d, 21/28), and two cycles of dexamethasone (20 mg once weekly for 8 weeks then stopping).
The randomization included stratification based on age and cancer stage. Baseline characteristics were well balanced in the two groups.
Both regimens were administered until disease progression or unacceptable toxicity.
As of the data cut-off in November 2024, with a median follow-up of 46.3 months, 81 of the original 200 patients in the DR arm remained on treatment, and 11 of 95 continued in the Rd arm.
The overall median treatment duration among the 200 original patients in the DR arm was 31.6 months and 14.3 months in the Rd arm.
The study met its primary endpoint of progression-free survival (PFS), with a median rate of 53.4 months in the DR arm vs 22.5 months in the Rd arm (hazard ratio [HR], 0.51; P < .0001).
The improved PFS in the DR arm was observed across all subgroups based on age, Charlson comorbidity index, cancer stage, cytogenetics, and creatinine clearance; however, those with lower frailty scores had better outcomes in both groups.
A median overall survival was not reached in the DR arm vs 47.2 months in the Rd arm (HR, 0.52; P = .0001).
The DR arm also showed a higher overall best response rate of 94% vs 86% (P = .005), respectively, with deeper responses in the DR arm at all time points, including the earliest points at 4 months.
In terms of adverse events (AEs), at least one AE of grade ≥ 3 occurred in 89% in the DR arm and 79% in the Rd arm.
Those in the DR arm had significantly more grade 3 or higher hematologic AEs with neutropenia (62% vs 34%); however, grade ≥ 3 infections were similar, with 19% in the DR arm and 21% in the Rd arm. Infections involving pneumonia occurred in 6% and 8%, respectively.
There were no significant differences between the two arms in discontinuations due to AEs (30% in the DR arm and 34% in the Rd arm).
While health-related quality of life measures at baseline were well balanced between the two groups, those in the DR arm reported significantly shorter times to clinically meaningful improvement in all domains of the EORTC Core Quality of Life questionnaire (EORTC QLQ-C30).
“The safety profile was significantly improved and was favorable, without increased infection or pneumonia rates, with similar rates of treatment discontinuation,” Manier said.
Based on the findings, “we believe that the dexamethasone-sparing strategy is effective and safe for treating these frail patients with multiple myeloma,” he added.
Commenting on the study, Manni Mohyuddin, MD, an assistant professor in the multiple myeloma program at the Huntsman Cancer Institute, University of Utah, Salt Lake City, noted that, with the popularity of triplet regimens such as daratumumab, lenalidomide, and dexamethasone, the Rd regimen in the study is not as commonly used.
“But what this trial tells us is that efficacy outcomes in such a group of patients are encouraging despite getting rid of dexamethasone so quickly,” he said in an interview.
However, “while the tide is changing, dexamethasone is still given long-term, week after week after week in most myeloma protocols and in the community,” he noted. “Hopefully, this trial, and some of the other work, will lead to a change in this space.”
Mohyuddin suggests one approach can involve starting off with just daratumumab and a low dose of dexamethasone, then adding lenalidomide at a lower dose later in a sequential/graded approach.
“Other approaches that should be studied should be bispecific antibodies used sparingly, with less frequent dosing, or finite period,” he added. “There is lot to refine.”
Mohyuddin added a critique that the study’s endpoint of PFS may not have been ideal for the population of elderly and frail patients.
“Older people generally prioritize functional independence and quality of life, and perhaps a more patient-centered endpoint could have led to an even more informative study,” he said.
Manier’s disclosures included consultancy with Takeda Pharmaceuticals, Sanofi, Novartis, Janssen, GlaxoSmithKline, Celgene/BMS, Amgen, Adaptive Biotechnologies, Roche, Regeneron, and AbbVie. Mohyuddin had no disclosures.
A version of this article appeared on Medscape.com.
FROM ASH 2024