User login
For MD-IQ use only
How do you run a hospital with no running water?
It’s bad enough that this month’s historic snowstorm left ordinary Texans scrambling for heat and resorting to melted snow for drinking, washing, and flushing. But what about hospitals, where sanitation is paramount and ample water is a sine qua non?
As pipes burst, pumps froze, and water pressure plummeted, patient care was affected as well as maintenance, food preparation, laundry, and heat. To counter the problems, several Texas hospitals stepped up to the plate with inventive responses.
“At the worst point, two of our hospitals, Houston Methodist West and Houston Methodist Baytown, had no city water supply, one for over 48 hours and the other for 72 hours,” said Marc L. Boom, MD, MBA, Houston Methodist’s president and CEO.
Although the main hospital had a reserve supply of potable water, a supply of water for laundry, cooking, and cleaning was another matter. “We introduced significant water restrictions and had to have 6,000-gallon tankers bring in extra water,” Dr. Boom said.
One hospital in the network got creative. When it rained the day after the ice storm, the staff rigged up a rain collection system using the huge bins that move linens around the hospital to collect nonpotable water for cleaning and flushing toilets, Dr. Boom said. Another hospital was able to provide showers for staff by bringing in bathroom trailers with self-contained water supplies of the kind used at some sporting events.
And at some facilities, patients were discharged into the lobby as they could not return home with transportation, electricity, and water systems crippled. With widespread challenges continuing, even as temperatures warmed, President Biden signed a major disaster declaration Feb. 20 that will provide emergency assistance to residents and businesses in more than a third of Texas counties, including those surrounding Houston, Dallas, and Austin.
Although conditions forced the rescheduling of some nonemergent surgeries, the water shortage had no impact on COVID-19 care, except for the unavailability of showers in the case of mobile patients. “At the worst, they just had to use bucket flushing for the toilets,” Dr. Boom said.
And in an unexpected win, when a Harris County freezer for COVID-19 vaccine storage failed and threatened to spoil 8,400 precious doses, Dr. Boom’s center was able to take delivery on 1,000 doses and administer them in 3 hours at a hastily set up ad hoc immunization center.
In all this, the lessons of the pandemic had a positive preparatory role. “2020 taught us to be agile as things change and to align our goals across different medical teams,” said Ben Saldana, MD, medical director of Houston Methodist’s emergency care centers. “And we were prepared for hurricanes, but not for snow.”
Increased pressure on emergency departments
As the outages continued and stress levels in the community rose, the network started seeing exacerbations of chronic conditions after the power shut-down incapacitated electrical devices running machines for heart assistance, oxygen delivery, and sleep apnea. “We started seeing food-borne illness and carbon monoxide poisoning, as well as more heart attacks, strokes, and sepsis,” Dr. Saldana said.
One serious strain on the network’s main hospital was the sudden need to accommodate large numbers of patients on dialysis, a procedure that uses a lot of water and is typically performed in small, vulnerable community facilities with limited infrastructure and no generators. “The hospitals are their backup and act as a safety net for them,” Boom said. Some hospital areas generally used for other types of conditions had to be marshaled for renal care.
Emergency rooms became pop-up dialysis centers, Dr. Saldana said. “And if the water pressure dropped, we had to cut dialysis time from the standard 4 hours to 2. That’s like putting a band-aid on patients.”
Fortunately, municipal water pressure in the Houston area has steadily risen and is almost back to normal. And according to Dr. Boom, the brutal storm may yet have a silver lining: a decline in county coronavirus cases as the storm and icy road conditions forced people to stay sequestered at home.
Further north in Austin, a number of hospitals lost municipal water pressure, creating a series of problems. Among them was St. David’s South Austin Medical Center, at which, according to reports in the Austin American-Statesman, staff members were at one point asked to use trash bags to remove waste from toilets, to refrain from showering, and to clean their hands only with sanitizer.
A statement issued by David Huffstutler, CEO of St. David’s HealthCare, acknowledged that the heating system is based on a water-fed boiler. When the building lost heat owing to lack of water, some patients had to be transferred elsewhere or discharged. The hospital distributed jugs and bottles of water for handwashing and drinking, and was working with city officials to obtain portable toilets.
Meanwhile, officials at Austin’s Dell Children’s Medical Center acknowledged in a memo that its toilets no longer had “flushing capabilities.” Other area hospitals in the Ascension Seton network were also suffering from compromised water supplies last week, according to local news reports.
Washroom facilities were affected elsewhere as well. A post on a medical association Facebook page referred to a memo ordering staff to use a single toilet in an outpatient area for bowel movements and warned them to limit their time there. No paper or other products were to be used in other toilets designated for urination.
‘The pandemic was the prelude to the ice storm’
Some hospitals fared better. Along the Coastal Bend, Corpus Christi Medical Center managed to maintain its electricity and water supply to ensure continuity of hospital services after the storm, according to a statement.
But back in Houston, Liz Youngblood, MBA, RN, president of Baylor St. Luke’s Medical Center, said a number of hospitals in her network experienced low water pressure after the storm.
“Fortunately, we had water conservation measures and low-water alerts in place for such emergencies,” she said. “And we rely on water tankers to help maintain enough pressure for the basics.”
Some of the challenges posed by the storm are quite similar to what St. Luke’s faced after Hurricane Harvey in 2017. “We had already made plans to address them and so we felt prepared,” Ms. Youngblood said.
And thanks to COVID-19, Texas hospitals have been operating in crisis mode for the past year. “The pandemic was the prelude to the ice storm,” said Gina Blocker, MD, a St. Luke’s ED physician, “so we had measures and teams in place. We did have some reduction in water pressure, though the pressure was still good.”
But the hospital was inundated with patients looking for shelter. “Some were just scared about what might happen to them if their heat didn’t come back on and they wanted to be where they could get care,” Dr. Blocker said. Others came in with expected storm-related injuries such as hypothermia and carbon monoxide poisoning.
According to Ms. Youngblood, little compromise in patient care was necessary except for the cancellation of some operations and vaccinations owing to the treacherous travel conditions. “But one of the biggest remaining issues is that we need plenty of blood, so we’re encouraging people to donate at their local centers.”
A version of this article first appeared on Medscape.com
It’s bad enough that this month’s historic snowstorm left ordinary Texans scrambling for heat and resorting to melted snow for drinking, washing, and flushing. But what about hospitals, where sanitation is paramount and ample water is a sine qua non?
As pipes burst, pumps froze, and water pressure plummeted, patient care was affected as well as maintenance, food preparation, laundry, and heat. To counter the problems, several Texas hospitals stepped up to the plate with inventive responses.
“At the worst point, two of our hospitals, Houston Methodist West and Houston Methodist Baytown, had no city water supply, one for over 48 hours and the other for 72 hours,” said Marc L. Boom, MD, MBA, Houston Methodist’s president and CEO.
Although the main hospital had a reserve supply of potable water, a supply of water for laundry, cooking, and cleaning was another matter. “We introduced significant water restrictions and had to have 6,000-gallon tankers bring in extra water,” Dr. Boom said.
One hospital in the network got creative. When it rained the day after the ice storm, the staff rigged up a rain collection system using the huge bins that move linens around the hospital to collect nonpotable water for cleaning and flushing toilets, Dr. Boom said. Another hospital was able to provide showers for staff by bringing in bathroom trailers with self-contained water supplies of the kind used at some sporting events.
And at some facilities, patients were discharged into the lobby as they could not return home with transportation, electricity, and water systems crippled. With widespread challenges continuing, even as temperatures warmed, President Biden signed a major disaster declaration Feb. 20 that will provide emergency assistance to residents and businesses in more than a third of Texas counties, including those surrounding Houston, Dallas, and Austin.
Although conditions forced the rescheduling of some nonemergent surgeries, the water shortage had no impact on COVID-19 care, except for the unavailability of showers in the case of mobile patients. “At the worst, they just had to use bucket flushing for the toilets,” Dr. Boom said.
And in an unexpected win, when a Harris County freezer for COVID-19 vaccine storage failed and threatened to spoil 8,400 precious doses, Dr. Boom’s center was able to take delivery on 1,000 doses and administer them in 3 hours at a hastily set up ad hoc immunization center.
In all this, the lessons of the pandemic had a positive preparatory role. “2020 taught us to be agile as things change and to align our goals across different medical teams,” said Ben Saldana, MD, medical director of Houston Methodist’s emergency care centers. “And we were prepared for hurricanes, but not for snow.”
Increased pressure on emergency departments
As the outages continued and stress levels in the community rose, the network started seeing exacerbations of chronic conditions after the power shut-down incapacitated electrical devices running machines for heart assistance, oxygen delivery, and sleep apnea. “We started seeing food-borne illness and carbon monoxide poisoning, as well as more heart attacks, strokes, and sepsis,” Dr. Saldana said.
One serious strain on the network’s main hospital was the sudden need to accommodate large numbers of patients on dialysis, a procedure that uses a lot of water and is typically performed in small, vulnerable community facilities with limited infrastructure and no generators. “The hospitals are their backup and act as a safety net for them,” Boom said. Some hospital areas generally used for other types of conditions had to be marshaled for renal care.
Emergency rooms became pop-up dialysis centers, Dr. Saldana said. “And if the water pressure dropped, we had to cut dialysis time from the standard 4 hours to 2. That’s like putting a band-aid on patients.”
Fortunately, municipal water pressure in the Houston area has steadily risen and is almost back to normal. And according to Dr. Boom, the brutal storm may yet have a silver lining: a decline in county coronavirus cases as the storm and icy road conditions forced people to stay sequestered at home.
Further north in Austin, a number of hospitals lost municipal water pressure, creating a series of problems. Among them was St. David’s South Austin Medical Center, at which, according to reports in the Austin American-Statesman, staff members were at one point asked to use trash bags to remove waste from toilets, to refrain from showering, and to clean their hands only with sanitizer.
A statement issued by David Huffstutler, CEO of St. David’s HealthCare, acknowledged that the heating system is based on a water-fed boiler. When the building lost heat owing to lack of water, some patients had to be transferred elsewhere or discharged. The hospital distributed jugs and bottles of water for handwashing and drinking, and was working with city officials to obtain portable toilets.
Meanwhile, officials at Austin’s Dell Children’s Medical Center acknowledged in a memo that its toilets no longer had “flushing capabilities.” Other area hospitals in the Ascension Seton network were also suffering from compromised water supplies last week, according to local news reports.
Washroom facilities were affected elsewhere as well. A post on a medical association Facebook page referred to a memo ordering staff to use a single toilet in an outpatient area for bowel movements and warned them to limit their time there. No paper or other products were to be used in other toilets designated for urination.
‘The pandemic was the prelude to the ice storm’
Some hospitals fared better. Along the Coastal Bend, Corpus Christi Medical Center managed to maintain its electricity and water supply to ensure continuity of hospital services after the storm, according to a statement.
But back in Houston, Liz Youngblood, MBA, RN, president of Baylor St. Luke’s Medical Center, said a number of hospitals in her network experienced low water pressure after the storm.
“Fortunately, we had water conservation measures and low-water alerts in place for such emergencies,” she said. “And we rely on water tankers to help maintain enough pressure for the basics.”
Some of the challenges posed by the storm are quite similar to what St. Luke’s faced after Hurricane Harvey in 2017. “We had already made plans to address them and so we felt prepared,” Ms. Youngblood said.
And thanks to COVID-19, Texas hospitals have been operating in crisis mode for the past year. “The pandemic was the prelude to the ice storm,” said Gina Blocker, MD, a St. Luke’s ED physician, “so we had measures and teams in place. We did have some reduction in water pressure, though the pressure was still good.”
But the hospital was inundated with patients looking for shelter. “Some were just scared about what might happen to them if their heat didn’t come back on and they wanted to be where they could get care,” Dr. Blocker said. Others came in with expected storm-related injuries such as hypothermia and carbon monoxide poisoning.
According to Ms. Youngblood, little compromise in patient care was necessary except for the cancellation of some operations and vaccinations owing to the treacherous travel conditions. “But one of the biggest remaining issues is that we need plenty of blood, so we’re encouraging people to donate at their local centers.”
A version of this article first appeared on Medscape.com
It’s bad enough that this month’s historic snowstorm left ordinary Texans scrambling for heat and resorting to melted snow for drinking, washing, and flushing. But what about hospitals, where sanitation is paramount and ample water is a sine qua non?
As pipes burst, pumps froze, and water pressure plummeted, patient care was affected as well as maintenance, food preparation, laundry, and heat. To counter the problems, several Texas hospitals stepped up to the plate with inventive responses.
“At the worst point, two of our hospitals, Houston Methodist West and Houston Methodist Baytown, had no city water supply, one for over 48 hours and the other for 72 hours,” said Marc L. Boom, MD, MBA, Houston Methodist’s president and CEO.
Although the main hospital had a reserve supply of potable water, a supply of water for laundry, cooking, and cleaning was another matter. “We introduced significant water restrictions and had to have 6,000-gallon tankers bring in extra water,” Dr. Boom said.
One hospital in the network got creative. When it rained the day after the ice storm, the staff rigged up a rain collection system using the huge bins that move linens around the hospital to collect nonpotable water for cleaning and flushing toilets, Dr. Boom said. Another hospital was able to provide showers for staff by bringing in bathroom trailers with self-contained water supplies of the kind used at some sporting events.
And at some facilities, patients were discharged into the lobby as they could not return home with transportation, electricity, and water systems crippled. With widespread challenges continuing, even as temperatures warmed, President Biden signed a major disaster declaration Feb. 20 that will provide emergency assistance to residents and businesses in more than a third of Texas counties, including those surrounding Houston, Dallas, and Austin.
Although conditions forced the rescheduling of some nonemergent surgeries, the water shortage had no impact on COVID-19 care, except for the unavailability of showers in the case of mobile patients. “At the worst, they just had to use bucket flushing for the toilets,” Dr. Boom said.
And in an unexpected win, when a Harris County freezer for COVID-19 vaccine storage failed and threatened to spoil 8,400 precious doses, Dr. Boom’s center was able to take delivery on 1,000 doses and administer them in 3 hours at a hastily set up ad hoc immunization center.
In all this, the lessons of the pandemic had a positive preparatory role. “2020 taught us to be agile as things change and to align our goals across different medical teams,” said Ben Saldana, MD, medical director of Houston Methodist’s emergency care centers. “And we were prepared for hurricanes, but not for snow.”
Increased pressure on emergency departments
As the outages continued and stress levels in the community rose, the network started seeing exacerbations of chronic conditions after the power shut-down incapacitated electrical devices running machines for heart assistance, oxygen delivery, and sleep apnea. “We started seeing food-borne illness and carbon monoxide poisoning, as well as more heart attacks, strokes, and sepsis,” Dr. Saldana said.
One serious strain on the network’s main hospital was the sudden need to accommodate large numbers of patients on dialysis, a procedure that uses a lot of water and is typically performed in small, vulnerable community facilities with limited infrastructure and no generators. “The hospitals are their backup and act as a safety net for them,” Boom said. Some hospital areas generally used for other types of conditions had to be marshaled for renal care.
Emergency rooms became pop-up dialysis centers, Dr. Saldana said. “And if the water pressure dropped, we had to cut dialysis time from the standard 4 hours to 2. That’s like putting a band-aid on patients.”
Fortunately, municipal water pressure in the Houston area has steadily risen and is almost back to normal. And according to Dr. Boom, the brutal storm may yet have a silver lining: a decline in county coronavirus cases as the storm and icy road conditions forced people to stay sequestered at home.
Further north in Austin, a number of hospitals lost municipal water pressure, creating a series of problems. Among them was St. David’s South Austin Medical Center, at which, according to reports in the Austin American-Statesman, staff members were at one point asked to use trash bags to remove waste from toilets, to refrain from showering, and to clean their hands only with sanitizer.
A statement issued by David Huffstutler, CEO of St. David’s HealthCare, acknowledged that the heating system is based on a water-fed boiler. When the building lost heat owing to lack of water, some patients had to be transferred elsewhere or discharged. The hospital distributed jugs and bottles of water for handwashing and drinking, and was working with city officials to obtain portable toilets.
Meanwhile, officials at Austin’s Dell Children’s Medical Center acknowledged in a memo that its toilets no longer had “flushing capabilities.” Other area hospitals in the Ascension Seton network were also suffering from compromised water supplies last week, according to local news reports.
Washroom facilities were affected elsewhere as well. A post on a medical association Facebook page referred to a memo ordering staff to use a single toilet in an outpatient area for bowel movements and warned them to limit their time there. No paper or other products were to be used in other toilets designated for urination.
‘The pandemic was the prelude to the ice storm’
Some hospitals fared better. Along the Coastal Bend, Corpus Christi Medical Center managed to maintain its electricity and water supply to ensure continuity of hospital services after the storm, according to a statement.
But back in Houston, Liz Youngblood, MBA, RN, president of Baylor St. Luke’s Medical Center, said a number of hospitals in her network experienced low water pressure after the storm.
“Fortunately, we had water conservation measures and low-water alerts in place for such emergencies,” she said. “And we rely on water tankers to help maintain enough pressure for the basics.”
Some of the challenges posed by the storm are quite similar to what St. Luke’s faced after Hurricane Harvey in 2017. “We had already made plans to address them and so we felt prepared,” Ms. Youngblood said.
And thanks to COVID-19, Texas hospitals have been operating in crisis mode for the past year. “The pandemic was the prelude to the ice storm,” said Gina Blocker, MD, a St. Luke’s ED physician, “so we had measures and teams in place. We did have some reduction in water pressure, though the pressure was still good.”
But the hospital was inundated with patients looking for shelter. “Some were just scared about what might happen to them if their heat didn’t come back on and they wanted to be where they could get care,” Dr. Blocker said. Others came in with expected storm-related injuries such as hypothermia and carbon monoxide poisoning.
According to Ms. Youngblood, little compromise in patient care was necessary except for the cancellation of some operations and vaccinations owing to the treacherous travel conditions. “But one of the biggest remaining issues is that we need plenty of blood, so we’re encouraging people to donate at their local centers.”
A version of this article first appeared on Medscape.com
Long-term CPAP use linked with more physical activity
in new research.
“The aim of this study was to determine whether long-term CPAP treatment affects self-reported physical activity among participants with moderate-severe OSA and comorbid CV disease,” wrote David Stevens, PhD, of Flinders University, Adelaide, Australia, and his colleagues. The findings were recently published in the Journal of Clinical Sleep Medicine.
Researchers conducted a secondary analysis of the Sleep apnea cardiovascular endpoints (SAVE) trial that enrolled 2,687 adults aged 45-75 years old with OSA and confirmed CVD. In the study, participants were randomized to receive either CPAP plus usual care or usual care alone.
Physical activity levels were self-reported using the Leisure-Time Exercise Questionnaire (LTEQ) at baseline and at 6-, 24-, and 48-month follow-up intervals. The physical functioning subscale of the 36-item short form questionnaire (SF-36) was used to determine if activity levels were consistent with expert recommendations and to evaluate the effects on any self-perceived limitation of physical activity.
Moderate physical activity was higher among CPAP users
After a mean follow-up duration of 3.7 years, participants in the CPAP arm had approximately 20% higher levels of moderate physical activity, compared with the control arm (adjusted mean scores]: 8.7 points vs. 7.3 points; 95% confidence interval, 7.5-9.9 vs. 6.1-8.5; P = .003).
However, no significant difference was observed between treatment arms for mild physical activity (adjusted mean scores, 14.4 points vs. 14.2 points; 95% CI, 13.5-15.3 vs. 13.3-15.1; P = 0.599) or vigorous physical activity (adjusted mean scores, 3.4 points vs. 2.9 points; 95% CI 2.6-4.2 vs. 2.1-3.7; P = .125).
In addition, participants in the CPAP group reported less limitation in physical activity (adjusted between-group difference in SF-36 physical functioning subscale score = 1.66; 95% CI, 0.87-2.45; P < .001) and were more likely to report activity levels consistent with guideline recommendations.
“We were pleasantly surprised to find that people assigned to CPAP reported more physical activity than their counterparts who received usual care, despite being given no specific exercise instructions,” Kelly A. Loffler, PhD, a coauthor of the study, said in an interview.
“While I don’t think this will result in any immediate changes to guidelines, it is a helpful reminder to clinicians who are treating such patients, that the symptomatic benefits people experience with CPAP present a window of opportunity to improve health more holistically,” Dr. Loffler explained.
The researchers acknowledged that a key limitation of the study was the use of self-reported outcome measures. In future studies, they recommended that recent technological innovations, such as the availability of activity tracking devices, should be used to measure physical activity.
They also noted that patients with excessive sleepiness and severe hypoxemia were excluded from the SAVE trial; thus, the findings may not be generalizable to all patients.
Study reinforces CPAP’s health benefits
Emerson M. Wickwire, PhD, associate professor of psychiatry and medicine at the University of Maryland, Baltimore, explained that CPAP treatment is associated with well-documented health benefits among patients with CVD, as well as enhanced quality of life.
“These results provide further evidence that treating OSA can provide direct and indirect health benefits, suggesting that increased physical activity can be a vital pathway to improved cardiovascular health and enjoyment of life,” Dr. Wickwire, who is also director of the Insomnia Program at the University of Maryland Midtown Medical Center, Baltimore, said in an interview.
Steven M. Scharf, MD, a pulmonologist who is director of the Sleep Disorders Center (Adults) at the University of Maryland, also said the study findings were consistent with previous research involving patients treated for OSA.
“It is no surprise that treatment of OSA improves patient’s daily physical functioning,” explained Dr. Scharf, who is also a clinical professor, in an interview. “These results are expected, but very welcome, and I was glad to see them.”
The study was funded by the National Health and Medical Research Council of Australia, the Respironics Sleep and Respiratory Research Foundation, and Philips Respironics. Some authors reported financial affiliations with medical device and pharmaceutical companies. Dr. Loffler, Dr. Wickwire, and Dr. Scharf reported no conflicts of interest related to this work.
in new research.
“The aim of this study was to determine whether long-term CPAP treatment affects self-reported physical activity among participants with moderate-severe OSA and comorbid CV disease,” wrote David Stevens, PhD, of Flinders University, Adelaide, Australia, and his colleagues. The findings were recently published in the Journal of Clinical Sleep Medicine.
Researchers conducted a secondary analysis of the Sleep apnea cardiovascular endpoints (SAVE) trial that enrolled 2,687 adults aged 45-75 years old with OSA and confirmed CVD. In the study, participants were randomized to receive either CPAP plus usual care or usual care alone.
Physical activity levels were self-reported using the Leisure-Time Exercise Questionnaire (LTEQ) at baseline and at 6-, 24-, and 48-month follow-up intervals. The physical functioning subscale of the 36-item short form questionnaire (SF-36) was used to determine if activity levels were consistent with expert recommendations and to evaluate the effects on any self-perceived limitation of physical activity.
Moderate physical activity was higher among CPAP users
After a mean follow-up duration of 3.7 years, participants in the CPAP arm had approximately 20% higher levels of moderate physical activity, compared with the control arm (adjusted mean scores]: 8.7 points vs. 7.3 points; 95% confidence interval, 7.5-9.9 vs. 6.1-8.5; P = .003).
However, no significant difference was observed between treatment arms for mild physical activity (adjusted mean scores, 14.4 points vs. 14.2 points; 95% CI, 13.5-15.3 vs. 13.3-15.1; P = 0.599) or vigorous physical activity (adjusted mean scores, 3.4 points vs. 2.9 points; 95% CI 2.6-4.2 vs. 2.1-3.7; P = .125).
In addition, participants in the CPAP group reported less limitation in physical activity (adjusted between-group difference in SF-36 physical functioning subscale score = 1.66; 95% CI, 0.87-2.45; P < .001) and were more likely to report activity levels consistent with guideline recommendations.
“We were pleasantly surprised to find that people assigned to CPAP reported more physical activity than their counterparts who received usual care, despite being given no specific exercise instructions,” Kelly A. Loffler, PhD, a coauthor of the study, said in an interview.
“While I don’t think this will result in any immediate changes to guidelines, it is a helpful reminder to clinicians who are treating such patients, that the symptomatic benefits people experience with CPAP present a window of opportunity to improve health more holistically,” Dr. Loffler explained.
The researchers acknowledged that a key limitation of the study was the use of self-reported outcome measures. In future studies, they recommended that recent technological innovations, such as the availability of activity tracking devices, should be used to measure physical activity.
They also noted that patients with excessive sleepiness and severe hypoxemia were excluded from the SAVE trial; thus, the findings may not be generalizable to all patients.
Study reinforces CPAP’s health benefits
Emerson M. Wickwire, PhD, associate professor of psychiatry and medicine at the University of Maryland, Baltimore, explained that CPAP treatment is associated with well-documented health benefits among patients with CVD, as well as enhanced quality of life.
“These results provide further evidence that treating OSA can provide direct and indirect health benefits, suggesting that increased physical activity can be a vital pathway to improved cardiovascular health and enjoyment of life,” Dr. Wickwire, who is also director of the Insomnia Program at the University of Maryland Midtown Medical Center, Baltimore, said in an interview.
Steven M. Scharf, MD, a pulmonologist who is director of the Sleep Disorders Center (Adults) at the University of Maryland, also said the study findings were consistent with previous research involving patients treated for OSA.
“It is no surprise that treatment of OSA improves patient’s daily physical functioning,” explained Dr. Scharf, who is also a clinical professor, in an interview. “These results are expected, but very welcome, and I was glad to see them.”
The study was funded by the National Health and Medical Research Council of Australia, the Respironics Sleep and Respiratory Research Foundation, and Philips Respironics. Some authors reported financial affiliations with medical device and pharmaceutical companies. Dr. Loffler, Dr. Wickwire, and Dr. Scharf reported no conflicts of interest related to this work.
in new research.
“The aim of this study was to determine whether long-term CPAP treatment affects self-reported physical activity among participants with moderate-severe OSA and comorbid CV disease,” wrote David Stevens, PhD, of Flinders University, Adelaide, Australia, and his colleagues. The findings were recently published in the Journal of Clinical Sleep Medicine.
Researchers conducted a secondary analysis of the Sleep apnea cardiovascular endpoints (SAVE) trial that enrolled 2,687 adults aged 45-75 years old with OSA and confirmed CVD. In the study, participants were randomized to receive either CPAP plus usual care or usual care alone.
Physical activity levels were self-reported using the Leisure-Time Exercise Questionnaire (LTEQ) at baseline and at 6-, 24-, and 48-month follow-up intervals. The physical functioning subscale of the 36-item short form questionnaire (SF-36) was used to determine if activity levels were consistent with expert recommendations and to evaluate the effects on any self-perceived limitation of physical activity.
Moderate physical activity was higher among CPAP users
After a mean follow-up duration of 3.7 years, participants in the CPAP arm had approximately 20% higher levels of moderate physical activity, compared with the control arm (adjusted mean scores]: 8.7 points vs. 7.3 points; 95% confidence interval, 7.5-9.9 vs. 6.1-8.5; P = .003).
However, no significant difference was observed between treatment arms for mild physical activity (adjusted mean scores, 14.4 points vs. 14.2 points; 95% CI, 13.5-15.3 vs. 13.3-15.1; P = 0.599) or vigorous physical activity (adjusted mean scores, 3.4 points vs. 2.9 points; 95% CI 2.6-4.2 vs. 2.1-3.7; P = .125).
In addition, participants in the CPAP group reported less limitation in physical activity (adjusted between-group difference in SF-36 physical functioning subscale score = 1.66; 95% CI, 0.87-2.45; P < .001) and were more likely to report activity levels consistent with guideline recommendations.
“We were pleasantly surprised to find that people assigned to CPAP reported more physical activity than their counterparts who received usual care, despite being given no specific exercise instructions,” Kelly A. Loffler, PhD, a coauthor of the study, said in an interview.
“While I don’t think this will result in any immediate changes to guidelines, it is a helpful reminder to clinicians who are treating such patients, that the symptomatic benefits people experience with CPAP present a window of opportunity to improve health more holistically,” Dr. Loffler explained.
The researchers acknowledged that a key limitation of the study was the use of self-reported outcome measures. In future studies, they recommended that recent technological innovations, such as the availability of activity tracking devices, should be used to measure physical activity.
They also noted that patients with excessive sleepiness and severe hypoxemia were excluded from the SAVE trial; thus, the findings may not be generalizable to all patients.
Study reinforces CPAP’s health benefits
Emerson M. Wickwire, PhD, associate professor of psychiatry and medicine at the University of Maryland, Baltimore, explained that CPAP treatment is associated with well-documented health benefits among patients with CVD, as well as enhanced quality of life.
“These results provide further evidence that treating OSA can provide direct and indirect health benefits, suggesting that increased physical activity can be a vital pathway to improved cardiovascular health and enjoyment of life,” Dr. Wickwire, who is also director of the Insomnia Program at the University of Maryland Midtown Medical Center, Baltimore, said in an interview.
Steven M. Scharf, MD, a pulmonologist who is director of the Sleep Disorders Center (Adults) at the University of Maryland, also said the study findings were consistent with previous research involving patients treated for OSA.
“It is no surprise that treatment of OSA improves patient’s daily physical functioning,” explained Dr. Scharf, who is also a clinical professor, in an interview. “These results are expected, but very welcome, and I was glad to see them.”
The study was funded by the National Health and Medical Research Council of Australia, the Respironics Sleep and Respiratory Research Foundation, and Philips Respironics. Some authors reported financial affiliations with medical device and pharmaceutical companies. Dr. Loffler, Dr. Wickwire, and Dr. Scharf reported no conflicts of interest related to this work.
FROM JOURNAL OF CLINICAL SLEEP MEDICINE
COMMENT & CONTROVERSY
9vHPV VACCINE: PREVENTION OF OROPHARYNGEAL CANCER
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2020)
HPV vaccine for older ObGyns?
I am 67 years old and recently retired. I breathed in the smoke from laser conizations, LEEPs (loop electrosurgical excision procedures), and cautery of condyloma for 35 years. Am I a good candidate for the HPV vaccine?
Gus Barkett, DO
Muskegon, Michigan
Dr. Barbieri responds
I thank Dr. Barkett for his important question. As you know, the US Food and Drug Administration has approved 9vHPV vaccination for people 27 to 45 years of age. I do not believe there are sufficient data to provide an evidence-based answer for physicians with occupational exposure to HPV who are more than 45 years of age. My recommendation would be to have a consult with an otolaryngologist expert in HPV-induced oral-pharyngeal cancer.
EXAMINING THE EVIDENCE: HOW EFFECTIVE IS SCREENING MAMMOGRAPHY FOR PREVENTING BREAST CANCER MORTALITY?
ANDREW M. KAUNITZ, MD (AUGUST 2020)
Discordant results on screening mammography
In regard to the discussion on screening mammography for preventing breast cancer mortality, I would like to call attention to a more recent study than the ones referenced in the article. The study by Duffy and colleagues was from Sweden and included almost 550,000 women.1 Results of the study showed a statistically significant reduction of 41% in 10-year mortality and a 25% reduction in the incidence of advanced-stage disease at the time of diagnosis in women who underwent routine screening mammograms. In Sweden, routine screening is defined as a mammogram every 18 months for women aged 40 to 54 years and every 24 months after that, up to age 69.
I do not know if we will ever come to a consensus on the utility of mammograms or how often they should be done, but I wanted to illustrate this counterpoint.
Lisa Gennari, MD
Cincinnati, Ohio
Reference
1. Duffy SW, Tabar L, Yen AM, et al. Mammography screening reduces rates of advanced and fatal breast cancers: results in 549,091 women. Cancer. 2020;126:2971-2979.
Dr. Kaunitz responds
I thank Dr. Gennari for her interest in the Examining the Evidence discussion that summarized the findings of an article from Australia published in late summer of last year.1 That article indicated that as screening mammograms became common in the state of Victoria over several decades, the incidence of advanced breast cancer doubled, mirroring findings from the United States, Holland, and Norway. During the same time period, breast cancer mortality declined substantially. The authors concluded that all of the decline in breast cancer mortality that they observed since 1994 could be attributed not to screening mammography but rather to the introduction and uptake of adjuvant therapy (tamoxifen and chemotherapy).
In contrast, in the article Dr. Gennari cites, also published last summer, the authors found that the widespread uptake of screening mammograms among women residing in 9 counties in Sweden was associated with a decline in the incidence of advanced breast cancer. I am not able to explain these discrepant findings. However, as the authors pointed out, they employed a new strategy: measuring the incidence of breast cancer that proved fatal one decade after diagnosis.
Differing findings and interpretations of data that address benefits and risks of screening mammography lead to differing recommendations from professional societies and confusion among clinicians and our patients. Although it can be challenging in the constraints of time allotted for well-woman visits, I try to engage in shared decision making with my patients regarding when to start/stop mammography as well as frequency of screening.
Reference
- Burton R, Stevenson C. Assessment of breast cancer mortality trends associated with mammographic screening and adjuvant therapy from 1986 to 2013 in the state of Victoria, Australia. JAMA Netw Open. 2020:3:e208249.
Continue to: NEW HORMONAL MEDICAL TREATMENT...
NEW HORMONAL MEDICAL TREATMENT IS AN IMPORTANT ADVANCE FOR AUB CAUSED BY UTERINE FIBROIDS
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2020)
New AUB medical treatment
I appreciate Dr. Barbieri’s concise and pertinent review of myomatous disease etiology and treatments. I have a question regarding therapy with Oriahnn (elagolix, estradiol, and norethindrone acetate capsules). Most myomatous-related bleeding occurs in premenopausal women. The elagolix suppresses luteinizing hormone and follicle stimulating hormone, and the norethindrone is added to protect the endometrium from the estradiol. Do the elagolix and norethindrone also provide contraception?
Geoffrey J. Zann, MD, MBA
Boca Raton, Florida
Dr. Barbieri responds
Dr. Zann raises an important clinical question that arises often in practice. The US Food and Drug Administration (FDA) has not approved Oriahnn as a contraceptive. The FDA prescribing information recommends: Advise women to use non-hormonal contraception during treatment and for one week after discontinuing Oriahnn. Oriahnn may delay the ability to recognize the occurrence of a pregnancy because it alters menstrual bleeding. Perform pregnancy testing if pregnancy is suspected and discontinue Oriahnn if pregnancy is confirmed.
In Oriahnn, the elagolix dose is 300 mg twice daily. If a patient reliably takes 600 mg of elagolix daily, it is highly unlikely that she will ovulate. However, in practice, many patients miss doses of their medication, reducing the contraceptive effectiveness. For example, the combined estrogen-progestin contraceptive is highly effective at suppressing ovulation, but the Centers for Disease Control and Prevention (CDC) estimates that 9% of women taking an estrogen-progestin contraceptive will become pregnant each year.1,2
Oriahnn also contains norethindrone acetate at a dose of 0.5 mg daily. The FDA has approved norethindrone at a dose of 0.35 mg daily as a contraceptive. The CDC estimates that 9% of women prescribed a progestin-only pill will become pregnant each year with typical use.1,2
I counsel my patients that if they reliably take their prescribed Oriahnn medication as directed, they are unlikely to become pregnant, and a backup method of contraception will further help to reduce their risk of becoming pregnant.
References
- Centers for Disease Control and Prevention. US selected practice recommendations for contraceptive use, 2013. MMWR Morbid Mortal Weekly Rep. 2013;62(RR-5):1-59.
- Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397-404.
9vHPV VACCINE: PREVENTION OF OROPHARYNGEAL CANCER
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2020)
HPV vaccine for older ObGyns?
I am 67 years old and recently retired. I breathed in the smoke from laser conizations, LEEPs (loop electrosurgical excision procedures), and cautery of condyloma for 35 years. Am I a good candidate for the HPV vaccine?
Gus Barkett, DO
Muskegon, Michigan
Dr. Barbieri responds
I thank Dr. Barkett for his important question. As you know, the US Food and Drug Administration has approved 9vHPV vaccination for people 27 to 45 years of age. I do not believe there are sufficient data to provide an evidence-based answer for physicians with occupational exposure to HPV who are more than 45 years of age. My recommendation would be to have a consult with an otolaryngologist expert in HPV-induced oral-pharyngeal cancer.
EXAMINING THE EVIDENCE: HOW EFFECTIVE IS SCREENING MAMMOGRAPHY FOR PREVENTING BREAST CANCER MORTALITY?
ANDREW M. KAUNITZ, MD (AUGUST 2020)
Discordant results on screening mammography
In regard to the discussion on screening mammography for preventing breast cancer mortality, I would like to call attention to a more recent study than the ones referenced in the article. The study by Duffy and colleagues was from Sweden and included almost 550,000 women.1 Results of the study showed a statistically significant reduction of 41% in 10-year mortality and a 25% reduction in the incidence of advanced-stage disease at the time of diagnosis in women who underwent routine screening mammograms. In Sweden, routine screening is defined as a mammogram every 18 months for women aged 40 to 54 years and every 24 months after that, up to age 69.
I do not know if we will ever come to a consensus on the utility of mammograms or how often they should be done, but I wanted to illustrate this counterpoint.
Lisa Gennari, MD
Cincinnati, Ohio
Reference
1. Duffy SW, Tabar L, Yen AM, et al. Mammography screening reduces rates of advanced and fatal breast cancers: results in 549,091 women. Cancer. 2020;126:2971-2979.
Dr. Kaunitz responds
I thank Dr. Gennari for her interest in the Examining the Evidence discussion that summarized the findings of an article from Australia published in late summer of last year.1 That article indicated that as screening mammograms became common in the state of Victoria over several decades, the incidence of advanced breast cancer doubled, mirroring findings from the United States, Holland, and Norway. During the same time period, breast cancer mortality declined substantially. The authors concluded that all of the decline in breast cancer mortality that they observed since 1994 could be attributed not to screening mammography but rather to the introduction and uptake of adjuvant therapy (tamoxifen and chemotherapy).
In contrast, in the article Dr. Gennari cites, also published last summer, the authors found that the widespread uptake of screening mammograms among women residing in 9 counties in Sweden was associated with a decline in the incidence of advanced breast cancer. I am not able to explain these discrepant findings. However, as the authors pointed out, they employed a new strategy: measuring the incidence of breast cancer that proved fatal one decade after diagnosis.
Differing findings and interpretations of data that address benefits and risks of screening mammography lead to differing recommendations from professional societies and confusion among clinicians and our patients. Although it can be challenging in the constraints of time allotted for well-woman visits, I try to engage in shared decision making with my patients regarding when to start/stop mammography as well as frequency of screening.
Reference
- Burton R, Stevenson C. Assessment of breast cancer mortality trends associated with mammographic screening and adjuvant therapy from 1986 to 2013 in the state of Victoria, Australia. JAMA Netw Open. 2020:3:e208249.
Continue to: NEW HORMONAL MEDICAL TREATMENT...
NEW HORMONAL MEDICAL TREATMENT IS AN IMPORTANT ADVANCE FOR AUB CAUSED BY UTERINE FIBROIDS
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2020)
New AUB medical treatment
I appreciate Dr. Barbieri’s concise and pertinent review of myomatous disease etiology and treatments. I have a question regarding therapy with Oriahnn (elagolix, estradiol, and norethindrone acetate capsules). Most myomatous-related bleeding occurs in premenopausal women. The elagolix suppresses luteinizing hormone and follicle stimulating hormone, and the norethindrone is added to protect the endometrium from the estradiol. Do the elagolix and norethindrone also provide contraception?
Geoffrey J. Zann, MD, MBA
Boca Raton, Florida
Dr. Barbieri responds
Dr. Zann raises an important clinical question that arises often in practice. The US Food and Drug Administration (FDA) has not approved Oriahnn as a contraceptive. The FDA prescribing information recommends: Advise women to use non-hormonal contraception during treatment and for one week after discontinuing Oriahnn. Oriahnn may delay the ability to recognize the occurrence of a pregnancy because it alters menstrual bleeding. Perform pregnancy testing if pregnancy is suspected and discontinue Oriahnn if pregnancy is confirmed.
In Oriahnn, the elagolix dose is 300 mg twice daily. If a patient reliably takes 600 mg of elagolix daily, it is highly unlikely that she will ovulate. However, in practice, many patients miss doses of their medication, reducing the contraceptive effectiveness. For example, the combined estrogen-progestin contraceptive is highly effective at suppressing ovulation, but the Centers for Disease Control and Prevention (CDC) estimates that 9% of women taking an estrogen-progestin contraceptive will become pregnant each year.1,2
Oriahnn also contains norethindrone acetate at a dose of 0.5 mg daily. The FDA has approved norethindrone at a dose of 0.35 mg daily as a contraceptive. The CDC estimates that 9% of women prescribed a progestin-only pill will become pregnant each year with typical use.1,2
I counsel my patients that if they reliably take their prescribed Oriahnn medication as directed, they are unlikely to become pregnant, and a backup method of contraception will further help to reduce their risk of becoming pregnant.
References
- Centers for Disease Control and Prevention. US selected practice recommendations for contraceptive use, 2013. MMWR Morbid Mortal Weekly Rep. 2013;62(RR-5):1-59.
- Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397-404.
9vHPV VACCINE: PREVENTION OF OROPHARYNGEAL CANCER
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2020)
HPV vaccine for older ObGyns?
I am 67 years old and recently retired. I breathed in the smoke from laser conizations, LEEPs (loop electrosurgical excision procedures), and cautery of condyloma for 35 years. Am I a good candidate for the HPV vaccine?
Gus Barkett, DO
Muskegon, Michigan
Dr. Barbieri responds
I thank Dr. Barkett for his important question. As you know, the US Food and Drug Administration has approved 9vHPV vaccination for people 27 to 45 years of age. I do not believe there are sufficient data to provide an evidence-based answer for physicians with occupational exposure to HPV who are more than 45 years of age. My recommendation would be to have a consult with an otolaryngologist expert in HPV-induced oral-pharyngeal cancer.
EXAMINING THE EVIDENCE: HOW EFFECTIVE IS SCREENING MAMMOGRAPHY FOR PREVENTING BREAST CANCER MORTALITY?
ANDREW M. KAUNITZ, MD (AUGUST 2020)
Discordant results on screening mammography
In regard to the discussion on screening mammography for preventing breast cancer mortality, I would like to call attention to a more recent study than the ones referenced in the article. The study by Duffy and colleagues was from Sweden and included almost 550,000 women.1 Results of the study showed a statistically significant reduction of 41% in 10-year mortality and a 25% reduction in the incidence of advanced-stage disease at the time of diagnosis in women who underwent routine screening mammograms. In Sweden, routine screening is defined as a mammogram every 18 months for women aged 40 to 54 years and every 24 months after that, up to age 69.
I do not know if we will ever come to a consensus on the utility of mammograms or how often they should be done, but I wanted to illustrate this counterpoint.
Lisa Gennari, MD
Cincinnati, Ohio
Reference
1. Duffy SW, Tabar L, Yen AM, et al. Mammography screening reduces rates of advanced and fatal breast cancers: results in 549,091 women. Cancer. 2020;126:2971-2979.
Dr. Kaunitz responds
I thank Dr. Gennari for her interest in the Examining the Evidence discussion that summarized the findings of an article from Australia published in late summer of last year.1 That article indicated that as screening mammograms became common in the state of Victoria over several decades, the incidence of advanced breast cancer doubled, mirroring findings from the United States, Holland, and Norway. During the same time period, breast cancer mortality declined substantially. The authors concluded that all of the decline in breast cancer mortality that they observed since 1994 could be attributed not to screening mammography but rather to the introduction and uptake of adjuvant therapy (tamoxifen and chemotherapy).
In contrast, in the article Dr. Gennari cites, also published last summer, the authors found that the widespread uptake of screening mammograms among women residing in 9 counties in Sweden was associated with a decline in the incidence of advanced breast cancer. I am not able to explain these discrepant findings. However, as the authors pointed out, they employed a new strategy: measuring the incidence of breast cancer that proved fatal one decade after diagnosis.
Differing findings and interpretations of data that address benefits and risks of screening mammography lead to differing recommendations from professional societies and confusion among clinicians and our patients. Although it can be challenging in the constraints of time allotted for well-woman visits, I try to engage in shared decision making with my patients regarding when to start/stop mammography as well as frequency of screening.
Reference
- Burton R, Stevenson C. Assessment of breast cancer mortality trends associated with mammographic screening and adjuvant therapy from 1986 to 2013 in the state of Victoria, Australia. JAMA Netw Open. 2020:3:e208249.
Continue to: NEW HORMONAL MEDICAL TREATMENT...
NEW HORMONAL MEDICAL TREATMENT IS AN IMPORTANT ADVANCE FOR AUB CAUSED BY UTERINE FIBROIDS
ROBERT L. BARBIERI, MD (EDITORIAL; AUGUST 2020)
New AUB medical treatment
I appreciate Dr. Barbieri’s concise and pertinent review of myomatous disease etiology and treatments. I have a question regarding therapy with Oriahnn (elagolix, estradiol, and norethindrone acetate capsules). Most myomatous-related bleeding occurs in premenopausal women. The elagolix suppresses luteinizing hormone and follicle stimulating hormone, and the norethindrone is added to protect the endometrium from the estradiol. Do the elagolix and norethindrone also provide contraception?
Geoffrey J. Zann, MD, MBA
Boca Raton, Florida
Dr. Barbieri responds
Dr. Zann raises an important clinical question that arises often in practice. The US Food and Drug Administration (FDA) has not approved Oriahnn as a contraceptive. The FDA prescribing information recommends: Advise women to use non-hormonal contraception during treatment and for one week after discontinuing Oriahnn. Oriahnn may delay the ability to recognize the occurrence of a pregnancy because it alters menstrual bleeding. Perform pregnancy testing if pregnancy is suspected and discontinue Oriahnn if pregnancy is confirmed.
In Oriahnn, the elagolix dose is 300 mg twice daily. If a patient reliably takes 600 mg of elagolix daily, it is highly unlikely that she will ovulate. However, in practice, many patients miss doses of their medication, reducing the contraceptive effectiveness. For example, the combined estrogen-progestin contraceptive is highly effective at suppressing ovulation, but the Centers for Disease Control and Prevention (CDC) estimates that 9% of women taking an estrogen-progestin contraceptive will become pregnant each year.1,2
Oriahnn also contains norethindrone acetate at a dose of 0.5 mg daily. The FDA has approved norethindrone at a dose of 0.35 mg daily as a contraceptive. The CDC estimates that 9% of women prescribed a progestin-only pill will become pregnant each year with typical use.1,2
I counsel my patients that if they reliably take their prescribed Oriahnn medication as directed, they are unlikely to become pregnant, and a backup method of contraception will further help to reduce their risk of becoming pregnant.
References
- Centers for Disease Control and Prevention. US selected practice recommendations for contraceptive use, 2013. MMWR Morbid Mortal Weekly Rep. 2013;62(RR-5):1-59.
- Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397-404.
FDA expands sacubitril/valsartan indication to embrace some HFpEF
The Food and Drug Administration has approved a groundbreaking expanded indication for sacubitril/valsartan (Entresto), making it the first drug in the United States indicated for chronic heart failure not specifically characterized by ejection fraction.
The new labeling, as provided by Novartis, grants physicians a good deal of discretion in prescribing sacubitril/valsartan for patients with HF beyond those with HF and reduced ejection fraction (HFrEF), for which the drug was approved in 2015 primarily on the basis of the PARADIGM-HF trial.
The indication now reads, “to reduce the risk of cardiovascular death and hospitalization for heart failure in adult patients with chronic heart failure. Benefits are most clearly evident in patients with left ventricular ejection fraction (LVEF) below normal.”
Of note, the labeling cautions that “LVEF is a variable measure, so use clinical judgment in deciding whom to treat.”
The expanded indication essentially extends the sacubitril/valsartan option to many patients with HF and preserved LVEF (HFpEF), who in practice are most likely to have an LVEF in the range adjacent to “reduced,” long defined as “preserved” but lately categorized as “mid-range.”
But the FDA did not get so specific. In granting the expanded indication, which Novartis announced Feb. 16 in a press release, the agency accommodated the Dec. 15 majority recommendation of its Cardiovascular and Renal Drugs Advisory Committee that the PARAGON-HF trial “provided sufficient evidence to support” an indication beyond HFrEF.
The nature of the PARAGON-HF trial, along with detailed discussion among committee members after their vote tally, made it clear that the 12-to-1 majority favored an indication that would include clinically appropriate patients with “below normal” LVEF.
PARAGON-HF had assigned more than 4,800 patients whose LVEF was 45% or higher and were in NYHA class 2-4 to receive sacubitril/valsartan or valsartan only. Those taking the combo drug showed a 13% drop in risk for HF hospitalization or cardiovascular deaths over an average of 3 years, which narrowly missed significance (P = .059).
But a subgroup analysis garnered attention for its hint of benefit for patients with “mid-range” LVEF, in this case, below the median of 57%. The finding was supported by a later PARAGON-HF and PARADIGM-HF meta-analysis that pointed to a significant benefit for patients with HFpEF at its lowest LVEF levels, especially in women.
The expanded approval “is a significant advancement, providing a treatment to many patients who were not eligible for treatment before, because their ejection fraction was above the region we normally considered reduced,” Scott Solomon, MD, of Brigham and Women’s Hospital, Boston, said in the Novartis press release. “We can now offer a treatment to a wider range of patients who have an LVEF below normal,” added Dr. Solomon, PARAGON-HF executive committee cochair.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a groundbreaking expanded indication for sacubitril/valsartan (Entresto), making it the first drug in the United States indicated for chronic heart failure not specifically characterized by ejection fraction.
The new labeling, as provided by Novartis, grants physicians a good deal of discretion in prescribing sacubitril/valsartan for patients with HF beyond those with HF and reduced ejection fraction (HFrEF), for which the drug was approved in 2015 primarily on the basis of the PARADIGM-HF trial.
The indication now reads, “to reduce the risk of cardiovascular death and hospitalization for heart failure in adult patients with chronic heart failure. Benefits are most clearly evident in patients with left ventricular ejection fraction (LVEF) below normal.”
Of note, the labeling cautions that “LVEF is a variable measure, so use clinical judgment in deciding whom to treat.”
The expanded indication essentially extends the sacubitril/valsartan option to many patients with HF and preserved LVEF (HFpEF), who in practice are most likely to have an LVEF in the range adjacent to “reduced,” long defined as “preserved” but lately categorized as “mid-range.”
But the FDA did not get so specific. In granting the expanded indication, which Novartis announced Feb. 16 in a press release, the agency accommodated the Dec. 15 majority recommendation of its Cardiovascular and Renal Drugs Advisory Committee that the PARAGON-HF trial “provided sufficient evidence to support” an indication beyond HFrEF.
The nature of the PARAGON-HF trial, along with detailed discussion among committee members after their vote tally, made it clear that the 12-to-1 majority favored an indication that would include clinically appropriate patients with “below normal” LVEF.
PARAGON-HF had assigned more than 4,800 patients whose LVEF was 45% or higher and were in NYHA class 2-4 to receive sacubitril/valsartan or valsartan only. Those taking the combo drug showed a 13% drop in risk for HF hospitalization or cardiovascular deaths over an average of 3 years, which narrowly missed significance (P = .059).
But a subgroup analysis garnered attention for its hint of benefit for patients with “mid-range” LVEF, in this case, below the median of 57%. The finding was supported by a later PARAGON-HF and PARADIGM-HF meta-analysis that pointed to a significant benefit for patients with HFpEF at its lowest LVEF levels, especially in women.
The expanded approval “is a significant advancement, providing a treatment to many patients who were not eligible for treatment before, because their ejection fraction was above the region we normally considered reduced,” Scott Solomon, MD, of Brigham and Women’s Hospital, Boston, said in the Novartis press release. “We can now offer a treatment to a wider range of patients who have an LVEF below normal,” added Dr. Solomon, PARAGON-HF executive committee cochair.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a groundbreaking expanded indication for sacubitril/valsartan (Entresto), making it the first drug in the United States indicated for chronic heart failure not specifically characterized by ejection fraction.
The new labeling, as provided by Novartis, grants physicians a good deal of discretion in prescribing sacubitril/valsartan for patients with HF beyond those with HF and reduced ejection fraction (HFrEF), for which the drug was approved in 2015 primarily on the basis of the PARADIGM-HF trial.
The indication now reads, “to reduce the risk of cardiovascular death and hospitalization for heart failure in adult patients with chronic heart failure. Benefits are most clearly evident in patients with left ventricular ejection fraction (LVEF) below normal.”
Of note, the labeling cautions that “LVEF is a variable measure, so use clinical judgment in deciding whom to treat.”
The expanded indication essentially extends the sacubitril/valsartan option to many patients with HF and preserved LVEF (HFpEF), who in practice are most likely to have an LVEF in the range adjacent to “reduced,” long defined as “preserved” but lately categorized as “mid-range.”
But the FDA did not get so specific. In granting the expanded indication, which Novartis announced Feb. 16 in a press release, the agency accommodated the Dec. 15 majority recommendation of its Cardiovascular and Renal Drugs Advisory Committee that the PARAGON-HF trial “provided sufficient evidence to support” an indication beyond HFrEF.
The nature of the PARAGON-HF trial, along with detailed discussion among committee members after their vote tally, made it clear that the 12-to-1 majority favored an indication that would include clinically appropriate patients with “below normal” LVEF.
PARAGON-HF had assigned more than 4,800 patients whose LVEF was 45% or higher and were in NYHA class 2-4 to receive sacubitril/valsartan or valsartan only. Those taking the combo drug showed a 13% drop in risk for HF hospitalization or cardiovascular deaths over an average of 3 years, which narrowly missed significance (P = .059).
But a subgroup analysis garnered attention for its hint of benefit for patients with “mid-range” LVEF, in this case, below the median of 57%. The finding was supported by a later PARAGON-HF and PARADIGM-HF meta-analysis that pointed to a significant benefit for patients with HFpEF at its lowest LVEF levels, especially in women.
The expanded approval “is a significant advancement, providing a treatment to many patients who were not eligible for treatment before, because their ejection fraction was above the region we normally considered reduced,” Scott Solomon, MD, of Brigham and Women’s Hospital, Boston, said in the Novartis press release. “We can now offer a treatment to a wider range of patients who have an LVEF below normal,” added Dr. Solomon, PARAGON-HF executive committee cochair.
A version of this article first appeared on Medscape.com.
Back in session
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”
Key trends in hospitalist compensation from the 2020 SoHM Report
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 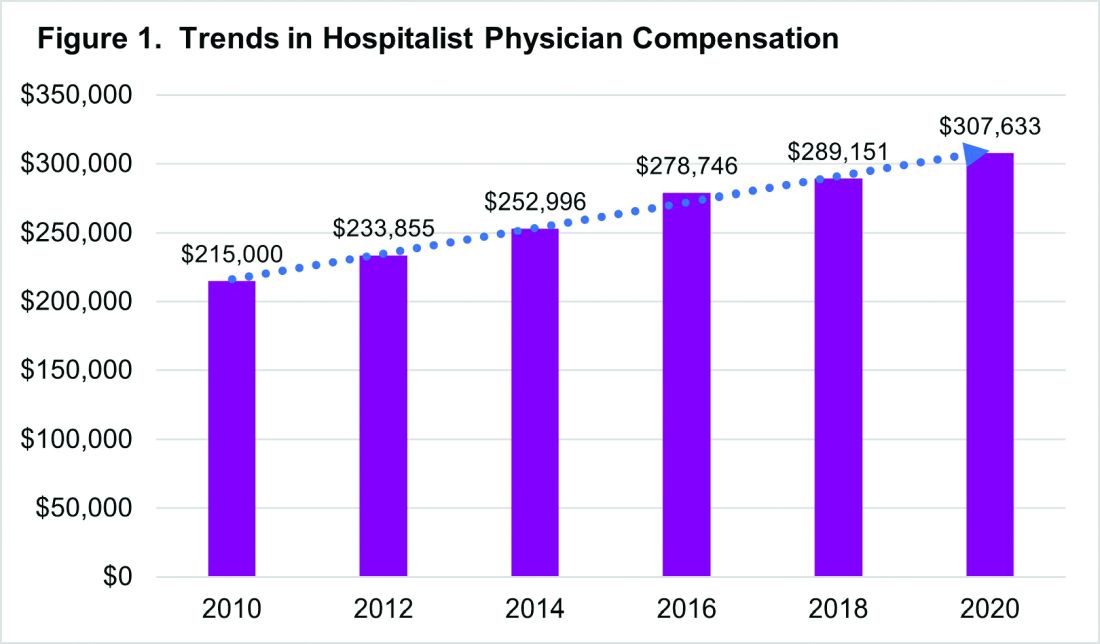
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 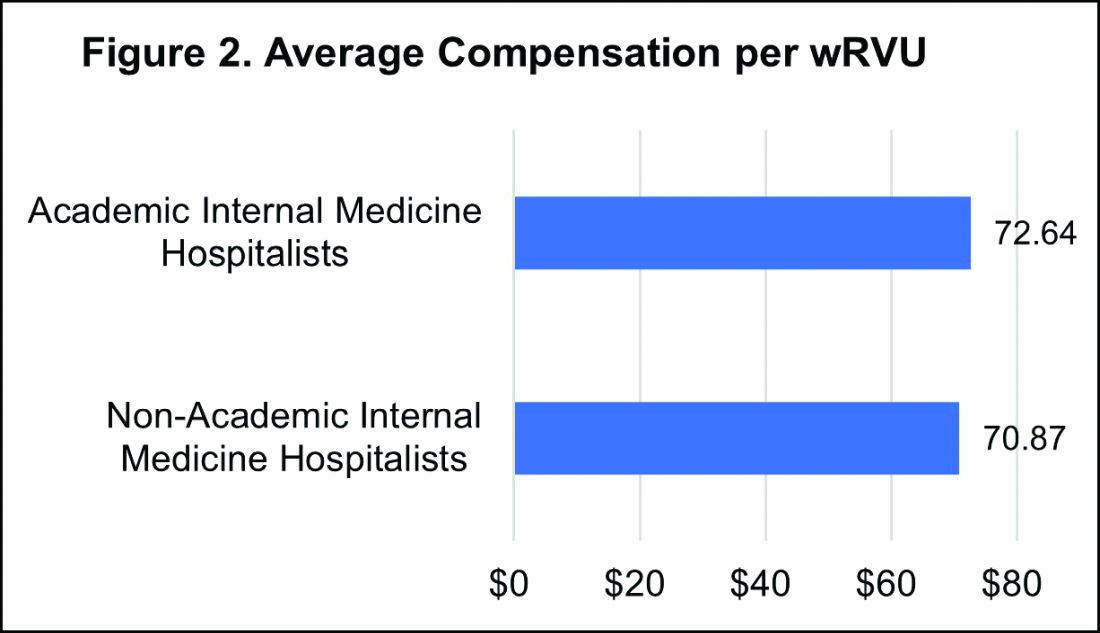
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 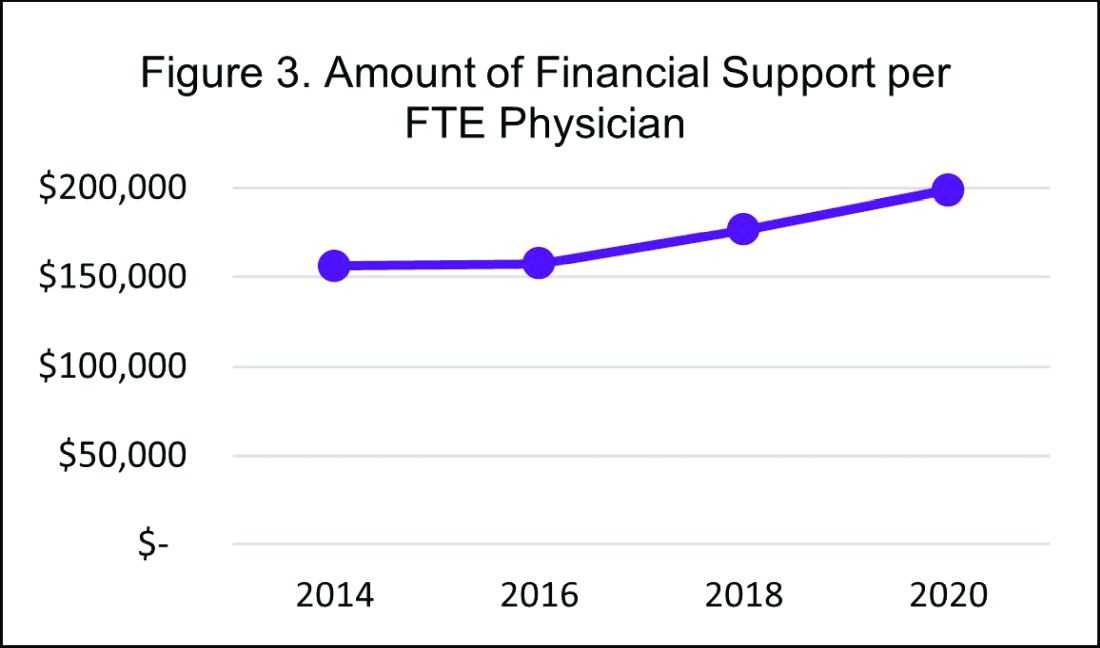
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 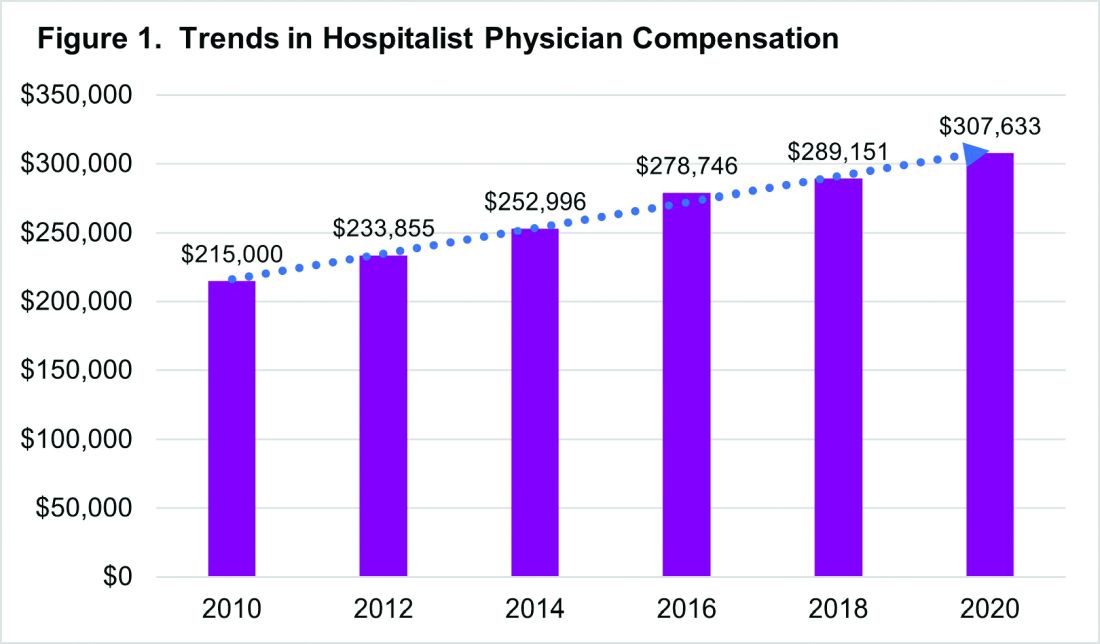
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 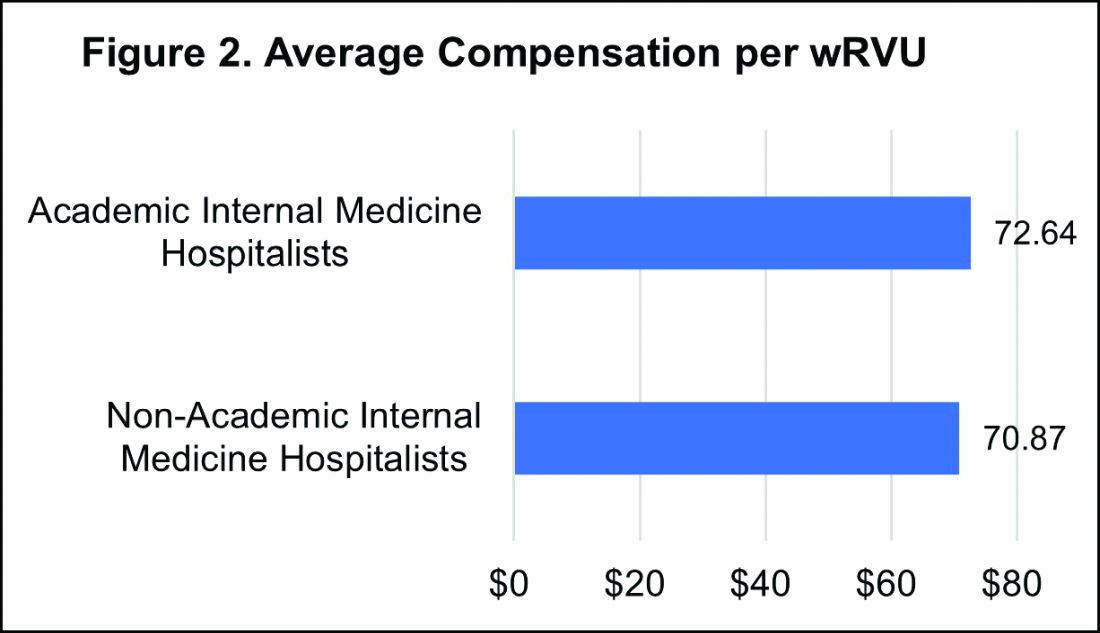
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 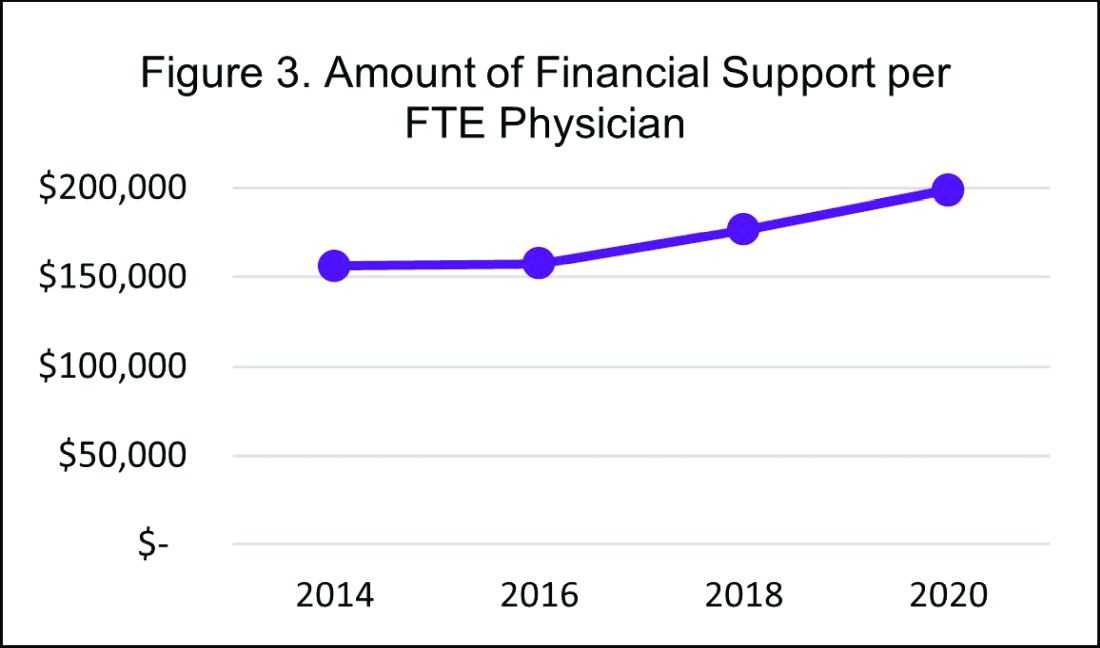
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 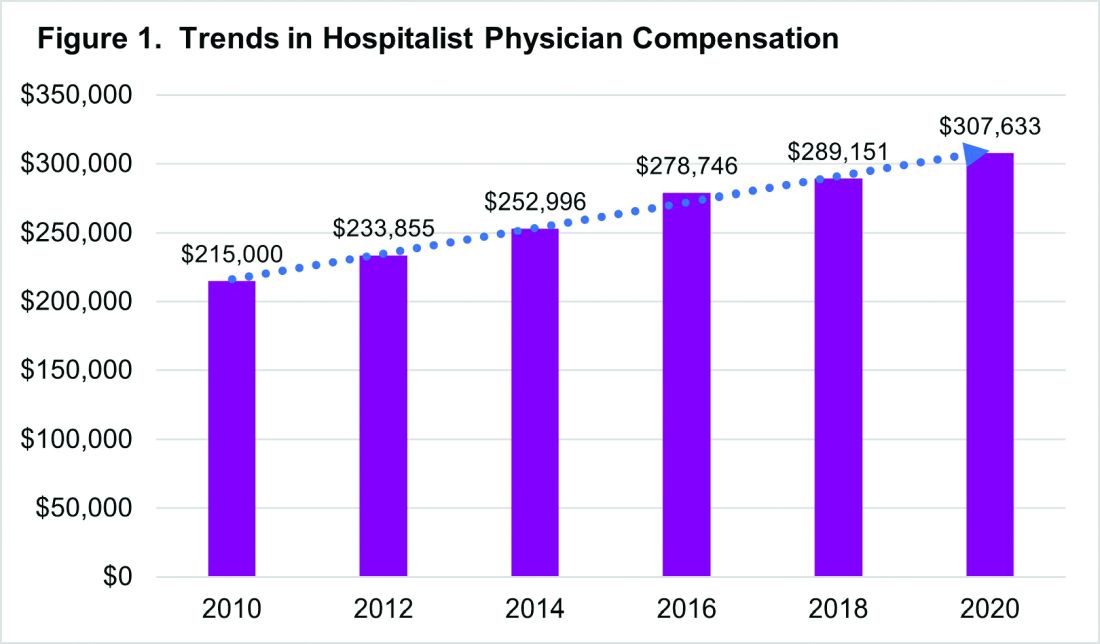
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 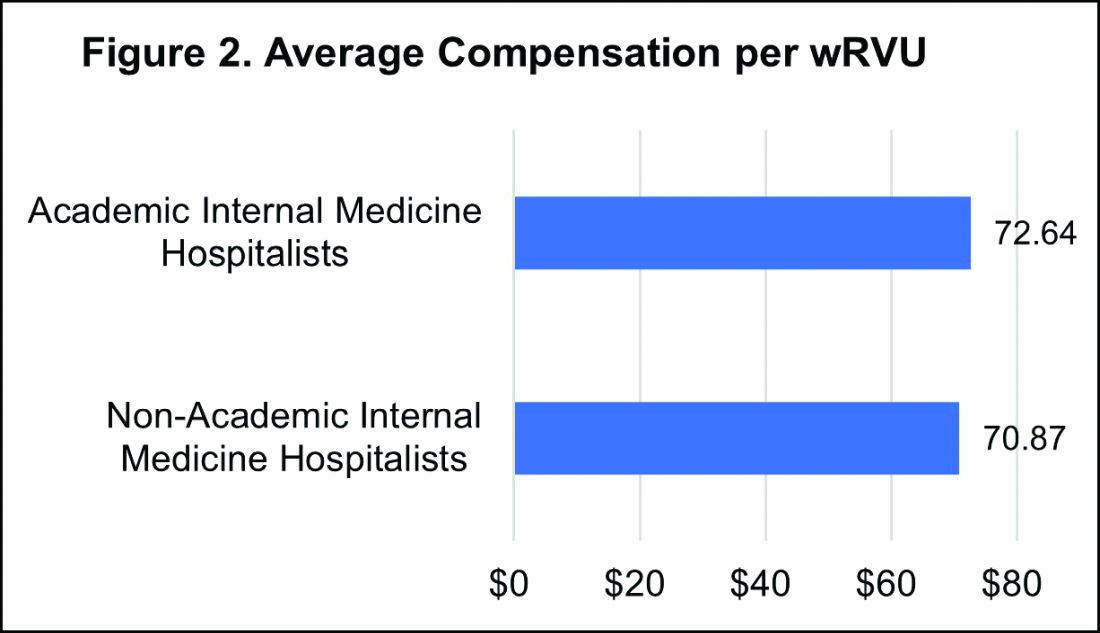
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 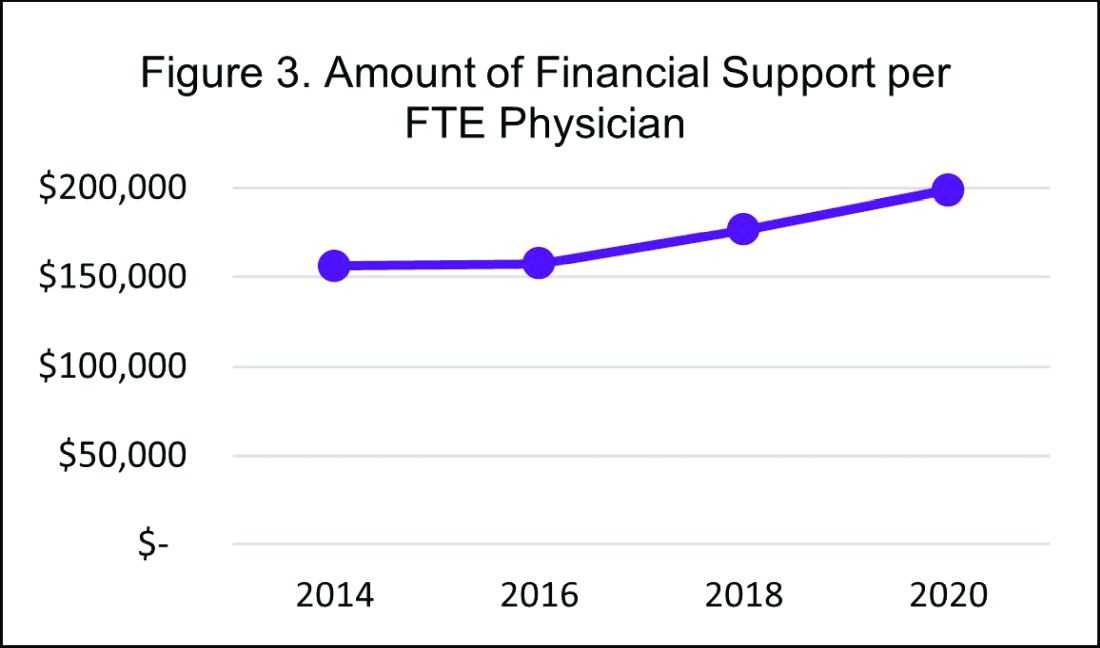
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
Stump Pemphigoid Demonstrating Circulating Anti–BP180 and BP230 Antibodies
To the Editor:
Bullous pemphigoid (BP) is a rare complication of lower limb amputation. Termed stump pemphigoid, it previously was described as a late complication arising on the stumps of leg amputees and tends to remain localized. We describe a case of stump pemphigoid presenting with an urticarial prodromal phase without generalized progression, confirmed by serum assay for circulating anti–basement membrane antibodies.
A 62-year-old man with a history of a right above-knee amputation initially presented with erythema as well as coalescing erosions and ulcers with fluid-filled vesicles and bullae on the amputation stump (Figure 1). The amputation was performed 15 years prior after a motorcycle accident. A skin biopsy of a vesicle on the amputation stump revealed subepidermal and focal intraepidermal clefting with hemorrhage and rare inflammatory cells composed of neutrophils and eosinophils (Figure 2). A tissue direct immunofluorescence test demonstrated linear C3 and IgG deposition along the dermoepidermal junction. Serum enzyme-linked immunosorbent assay (ELISA) demonstrated an anti-BP180 IgG of 50.90 U/mL and anti-BP230 IgG of 129.40 U/mL (reference range, <9.00 U/mL [for both]).

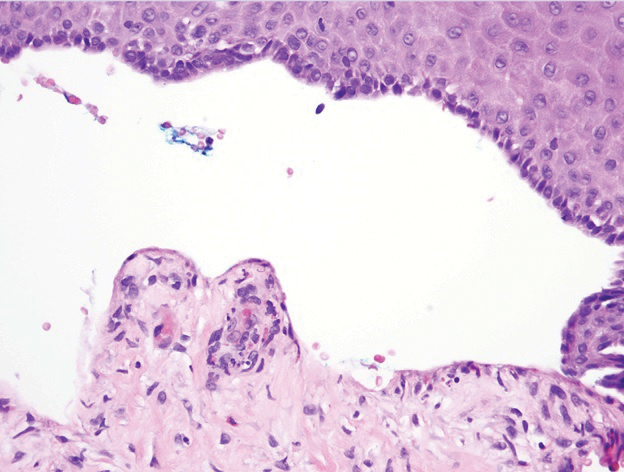
Topical clobetasol led to only modest improvement of blistering on the stump. Minor frictional trauma related to his leg prosthesis continued to trigger new vesicles and bullae on the stump. Oral prednisone 0.5 mg/kg daily was administered and tapered slowly over the course of 6 months. He also received oral niacinamide and doxycycline. He was completely clear after 3 weeks of initiating treatment and remained clear while prednisone was slowly tapered. One month after stopping prednisone he had recurrence of blisters on the stump only after he resumed wearing his prosthesis. Mycophenolate mofetil was started at a dosage of 1 g twice daily while he refrained from wearing the prosthesis. After 3 months he was able to wear the prosthesis without developing blisters. Two years after the initial presentation, repeat serum ELISA demonstrated normalization of the anti-BP180 IgG and anti-BP230 IgG titers. Thirty months after the initial presentation, mycophenolate mofetil was tapered and discontinued. The patient remained blisterfree and continued to wear his leg prosthesis without further blistering.
Amputees experience a high rate of skin complications on their stump,1 including friction blisters, shear injury, contact dermatitis, infections, and autoimmune blistering disorders (ie, BP, epidermolysis bullosa acquisita). The etiology of stump pemphigoid is not entirely understood but could be related to exposure of structural components of the hemidesmosome (eg, BP230, BP180), leading to autoantibody production as a consequence of either the underlying limb injury or from recurrent trauma related to limb prosthetics.2
Two previously reported cases of stump pemphigoid demonstrated a positive direct immunofluorescence antibody test.3,4 Another case demonstrated the presence of circulating IgG antibodies on indirect immunofluorescence to salt-split skin.5 We report a case of stump pemphigoid confirmed by presence of circulating anti–basement membrane antibodies on ELISA, supporting its use in the diagnostic workup and monitoring treatment response.
- Colgecen E, Korkmaz M, Ozyurt K, et al. A clinical evaluation of skin disorders of lower limb amputation sites. Int J Dermatol. 2016;55:468-472.
- Lo Schiavo A, Ruocco E, Brancaccio G, et al. Bullous pemphigoid: etiology, pathogenesis, and inducing factors: facts and controversies. Clin Dermatol. 2013;31:391-399.
- Reilly GD, Boulton AJ, Harrington CI. Stump pemphigoid: a new complication of the amputee. Br Med J (Clin Res Ed). 1983;287:875-876.
- de Jong MC, Kardaun SH, Tupker RA, et al. Immunomapping in localized bullous pemphigoid. Hautarzt. 1989;40:226-230.
- Brodell RT, Korman NJ. Stump pemphigoid. Cutis. 1996;57:245-246.
To the Editor:
Bullous pemphigoid (BP) is a rare complication of lower limb amputation. Termed stump pemphigoid, it previously was described as a late complication arising on the stumps of leg amputees and tends to remain localized. We describe a case of stump pemphigoid presenting with an urticarial prodromal phase without generalized progression, confirmed by serum assay for circulating anti–basement membrane antibodies.
A 62-year-old man with a history of a right above-knee amputation initially presented with erythema as well as coalescing erosions and ulcers with fluid-filled vesicles and bullae on the amputation stump (Figure 1). The amputation was performed 15 years prior after a motorcycle accident. A skin biopsy of a vesicle on the amputation stump revealed subepidermal and focal intraepidermal clefting with hemorrhage and rare inflammatory cells composed of neutrophils and eosinophils (Figure 2). A tissue direct immunofluorescence test demonstrated linear C3 and IgG deposition along the dermoepidermal junction. Serum enzyme-linked immunosorbent assay (ELISA) demonstrated an anti-BP180 IgG of 50.90 U/mL and anti-BP230 IgG of 129.40 U/mL (reference range, <9.00 U/mL [for both]).

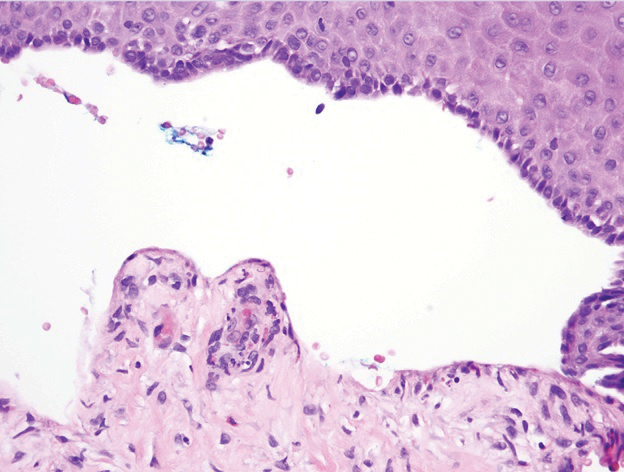
Topical clobetasol led to only modest improvement of blistering on the stump. Minor frictional trauma related to his leg prosthesis continued to trigger new vesicles and bullae on the stump. Oral prednisone 0.5 mg/kg daily was administered and tapered slowly over the course of 6 months. He also received oral niacinamide and doxycycline. He was completely clear after 3 weeks of initiating treatment and remained clear while prednisone was slowly tapered. One month after stopping prednisone he had recurrence of blisters on the stump only after he resumed wearing his prosthesis. Mycophenolate mofetil was started at a dosage of 1 g twice daily while he refrained from wearing the prosthesis. After 3 months he was able to wear the prosthesis without developing blisters. Two years after the initial presentation, repeat serum ELISA demonstrated normalization of the anti-BP180 IgG and anti-BP230 IgG titers. Thirty months after the initial presentation, mycophenolate mofetil was tapered and discontinued. The patient remained blisterfree and continued to wear his leg prosthesis without further blistering.
Amputees experience a high rate of skin complications on their stump,1 including friction blisters, shear injury, contact dermatitis, infections, and autoimmune blistering disorders (ie, BP, epidermolysis bullosa acquisita). The etiology of stump pemphigoid is not entirely understood but could be related to exposure of structural components of the hemidesmosome (eg, BP230, BP180), leading to autoantibody production as a consequence of either the underlying limb injury or from recurrent trauma related to limb prosthetics.2
Two previously reported cases of stump pemphigoid demonstrated a positive direct immunofluorescence antibody test.3,4 Another case demonstrated the presence of circulating IgG antibodies on indirect immunofluorescence to salt-split skin.5 We report a case of stump pemphigoid confirmed by presence of circulating anti–basement membrane antibodies on ELISA, supporting its use in the diagnostic workup and monitoring treatment response.
To the Editor:
Bullous pemphigoid (BP) is a rare complication of lower limb amputation. Termed stump pemphigoid, it previously was described as a late complication arising on the stumps of leg amputees and tends to remain localized. We describe a case of stump pemphigoid presenting with an urticarial prodromal phase without generalized progression, confirmed by serum assay for circulating anti–basement membrane antibodies.
A 62-year-old man with a history of a right above-knee amputation initially presented with erythema as well as coalescing erosions and ulcers with fluid-filled vesicles and bullae on the amputation stump (Figure 1). The amputation was performed 15 years prior after a motorcycle accident. A skin biopsy of a vesicle on the amputation stump revealed subepidermal and focal intraepidermal clefting with hemorrhage and rare inflammatory cells composed of neutrophils and eosinophils (Figure 2). A tissue direct immunofluorescence test demonstrated linear C3 and IgG deposition along the dermoepidermal junction. Serum enzyme-linked immunosorbent assay (ELISA) demonstrated an anti-BP180 IgG of 50.90 U/mL and anti-BP230 IgG of 129.40 U/mL (reference range, <9.00 U/mL [for both]).

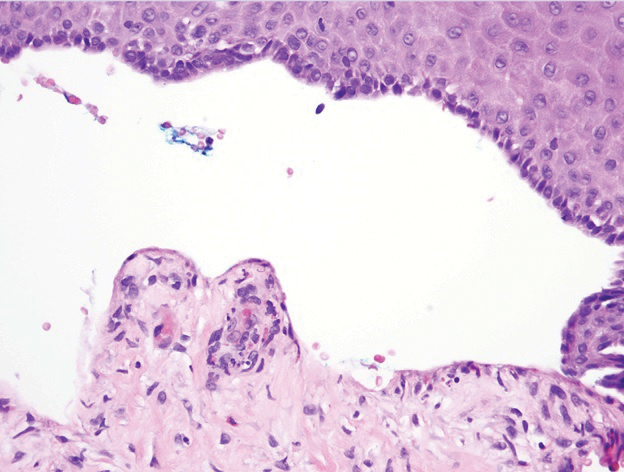
Topical clobetasol led to only modest improvement of blistering on the stump. Minor frictional trauma related to his leg prosthesis continued to trigger new vesicles and bullae on the stump. Oral prednisone 0.5 mg/kg daily was administered and tapered slowly over the course of 6 months. He also received oral niacinamide and doxycycline. He was completely clear after 3 weeks of initiating treatment and remained clear while prednisone was slowly tapered. One month after stopping prednisone he had recurrence of blisters on the stump only after he resumed wearing his prosthesis. Mycophenolate mofetil was started at a dosage of 1 g twice daily while he refrained from wearing the prosthesis. After 3 months he was able to wear the prosthesis without developing blisters. Two years after the initial presentation, repeat serum ELISA demonstrated normalization of the anti-BP180 IgG and anti-BP230 IgG titers. Thirty months after the initial presentation, mycophenolate mofetil was tapered and discontinued. The patient remained blisterfree and continued to wear his leg prosthesis without further blistering.
Amputees experience a high rate of skin complications on their stump,1 including friction blisters, shear injury, contact dermatitis, infections, and autoimmune blistering disorders (ie, BP, epidermolysis bullosa acquisita). The etiology of stump pemphigoid is not entirely understood but could be related to exposure of structural components of the hemidesmosome (eg, BP230, BP180), leading to autoantibody production as a consequence of either the underlying limb injury or from recurrent trauma related to limb prosthetics.2
Two previously reported cases of stump pemphigoid demonstrated a positive direct immunofluorescence antibody test.3,4 Another case demonstrated the presence of circulating IgG antibodies on indirect immunofluorescence to salt-split skin.5 We report a case of stump pemphigoid confirmed by presence of circulating anti–basement membrane antibodies on ELISA, supporting its use in the diagnostic workup and monitoring treatment response.
- Colgecen E, Korkmaz M, Ozyurt K, et al. A clinical evaluation of skin disorders of lower limb amputation sites. Int J Dermatol. 2016;55:468-472.
- Lo Schiavo A, Ruocco E, Brancaccio G, et al. Bullous pemphigoid: etiology, pathogenesis, and inducing factors: facts and controversies. Clin Dermatol. 2013;31:391-399.
- Reilly GD, Boulton AJ, Harrington CI. Stump pemphigoid: a new complication of the amputee. Br Med J (Clin Res Ed). 1983;287:875-876.
- de Jong MC, Kardaun SH, Tupker RA, et al. Immunomapping in localized bullous pemphigoid. Hautarzt. 1989;40:226-230.
- Brodell RT, Korman NJ. Stump pemphigoid. Cutis. 1996;57:245-246.
- Colgecen E, Korkmaz M, Ozyurt K, et al. A clinical evaluation of skin disorders of lower limb amputation sites. Int J Dermatol. 2016;55:468-472.
- Lo Schiavo A, Ruocco E, Brancaccio G, et al. Bullous pemphigoid: etiology, pathogenesis, and inducing factors: facts and controversies. Clin Dermatol. 2013;31:391-399.
- Reilly GD, Boulton AJ, Harrington CI. Stump pemphigoid: a new complication of the amputee. Br Med J (Clin Res Ed). 1983;287:875-876.
- de Jong MC, Kardaun SH, Tupker RA, et al. Immunomapping in localized bullous pemphigoid. Hautarzt. 1989;40:226-230.
- Brodell RT, Korman NJ. Stump pemphigoid. Cutis. 1996;57:245-246.
Practice Points
- Bullous pemphigoid (BP) can mimic friction blisters and should be considered in amputees who present with vesicles and bullae on their amputation stump.
- Circulating anti–basement membrane antibodies BP230 and BP180 IgG may aid in diagnosis when skin biopsy results are equivocal and also may be helpful in gauging treatment response.
Women and ACS: Focus on typical symptoms to improve outcomes
There are some differences in how women relative to men report symptoms of an acute coronary syndrome (ACS), but they should not be permitted to get in the way of prompt diagnosis and treatment, according to an expert review at the virtual Going Back to the Heart of Cardiology meeting.
“We need to get away from the idea that symptoms of a myocardial infarction in women are atypical, because women are also having typical symptoms,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix.
Sexes share key symptoms, but not treatment
Although “women are more likely to report additional symptoms,” chest pain “is pretty much equal between men and women” presenting with an ACS, according to Dr. Gulati.
There are several studies that have shown this, including the Variation in Recovery: Role of Gender on Outcomes of Young AMI patients (VIRGO). In VIRGO, which looked at ACS symptom presentation in younger patients (ages 18-55 years), 87.0% of women versus 89.5% of men presented with chest pain defined as pain, pressure, tightness, or discomfort.
Even among those who recognize that more women die of cardiovascular disease (CVD) disease than any other cause, nothing seems to erase the bias that women in an ED are less likely than men to be having a heart attack. About 60 million women in the United States have CVD, so no threat imposes a higher toll in morbidity and mortality.
In comparison, there are only about 3.5 million women with breast cancer. Even though this is a major cause of morbidity and mortality in women, it is dwarfed by CVD, according to statistics cited by Dr. Gulati. Yet, the data show women get inferior care by guideline-based standards.
“After a myocardial infarction, women relative to men are less likely to get aspirin or beta-blockers within 24 hours, they are less likely to undergo any type of invasive procedure, and they are less likely to meet the door-to-balloon time or receive any reperfusion therapy,” Dr. Gulati said. After a CVD event, “the only thing women do better is to die.”
Additional symptoms may muddy the diagnostic waters
In the setting of ACS, the problem is not that women fail to report symptoms that should lead clinicians to consider CVD, but that they report additional symptoms. For the clinician less inclined to consider CVD in women, particularly younger women, there is a greater risk of going down the wrong diagnostic pathway.
In other words, women report symptoms consistent with CVD, “but it is a question of whether we are hearing it,” Dr. Gulati said.
In the VIRGO study, 61.9% of women versus 54.8% of men (P < .001) presented three or more symptoms in addition to chest pain, such as epigastric symptoms, discomfort in the arms or neck, or palpitations. Women were more likely than men to attribute the symptoms to stress or anxiety (20.9% vs. 11.8%; P < .001), while less likely to consider them a result of muscle pain (15.4% vs. 21.2%; P = .029).
There are other gender differences for ACS. For example, women are more likely than men to presented ischemia without obstruction, but Dr. Gulati emphasized that lack of obstruction is not a reason to dismiss the potential for an underlying CV cause.
‘Yentl syndrome’ persists
“Women should not need to present exactly like men to be taken seriously,” she said, describing the “Yentl syndrome,” which now has its own Wikipedia page. A cardiovascular version of this syndrome was first described 30 years ago. Based on a movie of a woman who cross dresses in order to be allowed to undertake Jewish studies, the term captures the societal failure to adapt care for women who do not present disease the same way that men do.
Overall, inadequate urgency to pursue potential symptoms of ACS in women is just another manifestation of the “bikini approach to women’s health,” according to Dr. Gulati. This describes the focus on the breast and reproductive system to the exclusion or other organs and anatomy. Dr. Gulati speculated that this might be the reason that clinicians have failed to apply ACS guidelines to women with the same rigor that they apply to men.
This is hardly a new issue. Calls for improving cardiovascular care in women have been increasing in volume for more than past 20 years, but the issue has proven persistent, according to Dr. Gulati. As an example, she noted that the same types of gaps in care and in outcome reported in a 2008 registry study had not much changed in an article published 8 years later.
The solution is not complex, according to Dr. Gulati. In the ED, guideline-directed diagnostic tests should be offered to any man or woman, including younger women, who present with chest pain, ignoring gender bias that threatens misinterpretation of patient history and symptoms. Once CVD is diagnosed as promptly in women as it is in men, guideline-directed intervention would be expected to reduce the gender gap in outcomes.
“By applying standardized protocols, it will help us to the same for women as we do for men,” Dr. Gulati said.
The meeting was sponsored by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
There are some differences in how women relative to men report symptoms of an acute coronary syndrome (ACS), but they should not be permitted to get in the way of prompt diagnosis and treatment, according to an expert review at the virtual Going Back to the Heart of Cardiology meeting.
“We need to get away from the idea that symptoms of a myocardial infarction in women are atypical, because women are also having typical symptoms,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix.
Sexes share key symptoms, but not treatment
Although “women are more likely to report additional symptoms,” chest pain “is pretty much equal between men and women” presenting with an ACS, according to Dr. Gulati.
There are several studies that have shown this, including the Variation in Recovery: Role of Gender on Outcomes of Young AMI patients (VIRGO). In VIRGO, which looked at ACS symptom presentation in younger patients (ages 18-55 years), 87.0% of women versus 89.5% of men presented with chest pain defined as pain, pressure, tightness, or discomfort.
Even among those who recognize that more women die of cardiovascular disease (CVD) disease than any other cause, nothing seems to erase the bias that women in an ED are less likely than men to be having a heart attack. About 60 million women in the United States have CVD, so no threat imposes a higher toll in morbidity and mortality.
In comparison, there are only about 3.5 million women with breast cancer. Even though this is a major cause of morbidity and mortality in women, it is dwarfed by CVD, according to statistics cited by Dr. Gulati. Yet, the data show women get inferior care by guideline-based standards.
“After a myocardial infarction, women relative to men are less likely to get aspirin or beta-blockers within 24 hours, they are less likely to undergo any type of invasive procedure, and they are less likely to meet the door-to-balloon time or receive any reperfusion therapy,” Dr. Gulati said. After a CVD event, “the only thing women do better is to die.”
Additional symptoms may muddy the diagnostic waters
In the setting of ACS, the problem is not that women fail to report symptoms that should lead clinicians to consider CVD, but that they report additional symptoms. For the clinician less inclined to consider CVD in women, particularly younger women, there is a greater risk of going down the wrong diagnostic pathway.
In other words, women report symptoms consistent with CVD, “but it is a question of whether we are hearing it,” Dr. Gulati said.
In the VIRGO study, 61.9% of women versus 54.8% of men (P < .001) presented three or more symptoms in addition to chest pain, such as epigastric symptoms, discomfort in the arms or neck, or palpitations. Women were more likely than men to attribute the symptoms to stress or anxiety (20.9% vs. 11.8%; P < .001), while less likely to consider them a result of muscle pain (15.4% vs. 21.2%; P = .029).
There are other gender differences for ACS. For example, women are more likely than men to presented ischemia without obstruction, but Dr. Gulati emphasized that lack of obstruction is not a reason to dismiss the potential for an underlying CV cause.
‘Yentl syndrome’ persists
“Women should not need to present exactly like men to be taken seriously,” she said, describing the “Yentl syndrome,” which now has its own Wikipedia page. A cardiovascular version of this syndrome was first described 30 years ago. Based on a movie of a woman who cross dresses in order to be allowed to undertake Jewish studies, the term captures the societal failure to adapt care for women who do not present disease the same way that men do.
Overall, inadequate urgency to pursue potential symptoms of ACS in women is just another manifestation of the “bikini approach to women’s health,” according to Dr. Gulati. This describes the focus on the breast and reproductive system to the exclusion or other organs and anatomy. Dr. Gulati speculated that this might be the reason that clinicians have failed to apply ACS guidelines to women with the same rigor that they apply to men.
This is hardly a new issue. Calls for improving cardiovascular care in women have been increasing in volume for more than past 20 years, but the issue has proven persistent, according to Dr. Gulati. As an example, she noted that the same types of gaps in care and in outcome reported in a 2008 registry study had not much changed in an article published 8 years later.
The solution is not complex, according to Dr. Gulati. In the ED, guideline-directed diagnostic tests should be offered to any man or woman, including younger women, who present with chest pain, ignoring gender bias that threatens misinterpretation of patient history and symptoms. Once CVD is diagnosed as promptly in women as it is in men, guideline-directed intervention would be expected to reduce the gender gap in outcomes.
“By applying standardized protocols, it will help us to the same for women as we do for men,” Dr. Gulati said.
The meeting was sponsored by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
There are some differences in how women relative to men report symptoms of an acute coronary syndrome (ACS), but they should not be permitted to get in the way of prompt diagnosis and treatment, according to an expert review at the virtual Going Back to the Heart of Cardiology meeting.
“We need to get away from the idea that symptoms of a myocardial infarction in women are atypical, because women are also having typical symptoms,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix.
Sexes share key symptoms, but not treatment
Although “women are more likely to report additional symptoms,” chest pain “is pretty much equal between men and women” presenting with an ACS, according to Dr. Gulati.
There are several studies that have shown this, including the Variation in Recovery: Role of Gender on Outcomes of Young AMI patients (VIRGO). In VIRGO, which looked at ACS symptom presentation in younger patients (ages 18-55 years), 87.0% of women versus 89.5% of men presented with chest pain defined as pain, pressure, tightness, or discomfort.
Even among those who recognize that more women die of cardiovascular disease (CVD) disease than any other cause, nothing seems to erase the bias that women in an ED are less likely than men to be having a heart attack. About 60 million women in the United States have CVD, so no threat imposes a higher toll in morbidity and mortality.
In comparison, there are only about 3.5 million women with breast cancer. Even though this is a major cause of morbidity and mortality in women, it is dwarfed by CVD, according to statistics cited by Dr. Gulati. Yet, the data show women get inferior care by guideline-based standards.
“After a myocardial infarction, women relative to men are less likely to get aspirin or beta-blockers within 24 hours, they are less likely to undergo any type of invasive procedure, and they are less likely to meet the door-to-balloon time or receive any reperfusion therapy,” Dr. Gulati said. After a CVD event, “the only thing women do better is to die.”
Additional symptoms may muddy the diagnostic waters
In the setting of ACS, the problem is not that women fail to report symptoms that should lead clinicians to consider CVD, but that they report additional symptoms. For the clinician less inclined to consider CVD in women, particularly younger women, there is a greater risk of going down the wrong diagnostic pathway.
In other words, women report symptoms consistent with CVD, “but it is a question of whether we are hearing it,” Dr. Gulati said.
In the VIRGO study, 61.9% of women versus 54.8% of men (P < .001) presented three or more symptoms in addition to chest pain, such as epigastric symptoms, discomfort in the arms or neck, or palpitations. Women were more likely than men to attribute the symptoms to stress or anxiety (20.9% vs. 11.8%; P < .001), while less likely to consider them a result of muscle pain (15.4% vs. 21.2%; P = .029).
There are other gender differences for ACS. For example, women are more likely than men to presented ischemia without obstruction, but Dr. Gulati emphasized that lack of obstruction is not a reason to dismiss the potential for an underlying CV cause.
‘Yentl syndrome’ persists
“Women should not need to present exactly like men to be taken seriously,” she said, describing the “Yentl syndrome,” which now has its own Wikipedia page. A cardiovascular version of this syndrome was first described 30 years ago. Based on a movie of a woman who cross dresses in order to be allowed to undertake Jewish studies, the term captures the societal failure to adapt care for women who do not present disease the same way that men do.
Overall, inadequate urgency to pursue potential symptoms of ACS in women is just another manifestation of the “bikini approach to women’s health,” according to Dr. Gulati. This describes the focus on the breast and reproductive system to the exclusion or other organs and anatomy. Dr. Gulati speculated that this might be the reason that clinicians have failed to apply ACS guidelines to women with the same rigor that they apply to men.
This is hardly a new issue. Calls for improving cardiovascular care in women have been increasing in volume for more than past 20 years, but the issue has proven persistent, according to Dr. Gulati. As an example, she noted that the same types of gaps in care and in outcome reported in a 2008 registry study had not much changed in an article published 8 years later.
The solution is not complex, according to Dr. Gulati. In the ED, guideline-directed diagnostic tests should be offered to any man or woman, including younger women, who present with chest pain, ignoring gender bias that threatens misinterpretation of patient history and symptoms. Once CVD is diagnosed as promptly in women as it is in men, guideline-directed intervention would be expected to reduce the gender gap in outcomes.
“By applying standardized protocols, it will help us to the same for women as we do for men,” Dr. Gulati said.
The meeting was sponsored by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
FROM GOING BACK TO THE HEART OF CARDIOLOGY
Finding a new approach to difficult diagnoses
Reducing – or managing – uncertainty
Beyond its clinical objective, the Socrates Project also seeks to further the discovery of previously unrecognized disease processes.
Many patients do not have a diagnosis that explains their signs and symptoms, despite a thorough evaluation, said Benjamin Singer, MD, assistant professor of pulmonology and critical care at Northwestern Medicine in Chicago. To address that problem, he and his colleagues launched the Socrates Project. The service is intended for difficult diagnoses and is based on Socratic principles, particularly the role of iterative hypothesis testing in the process of diagnosis.
“We began the Socrates Project to assist physicians caring for patients who lack a specific diagnosis. In creating this service, we have found ourselves to be doctors for doctors – formalizing the curbside consultation,” Dr. Singer said.
Northwestern Medicine launched the Socrates Project in 2015. It’s a physician-to-physician consultation service that assists doctors working to diagnose conditions that have so far eluded detection. “Our service’s goal is to improve patient care by providing an opinion to the referring physician on diagnostic possibilities for a particular case and ideas to reduce – or at least manage – diagnostic uncertainty,” they write. “Our service model is similar to a tumor board, which exists as an interdisciplinary group operating in parallel to the clinical services, to provide consensus-based recommendations.”
Hospitalists at other institutions may be interested in starting a similar type of service at their own institution or collaborating with institutions who offer this type of service, Dr. Singer said.
At Northwestern Medicine, they are at work on the project’s next steps. “We are working to generate systematic data about our practice, particularly the types of referrals and outcomes,” he said.
Reference
1. Singer BD, et al. The Socrates Project for Difficult Diagnosis at Northwestern Medicine. J Hosp Med. 2020 February;15(2):116-125. doi:10.12788/jhm.3335.
Reducing – or managing – uncertainty
Reducing – or managing – uncertainty
Beyond its clinical objective, the Socrates Project also seeks to further the discovery of previously unrecognized disease processes.
Many patients do not have a diagnosis that explains their signs and symptoms, despite a thorough evaluation, said Benjamin Singer, MD, assistant professor of pulmonology and critical care at Northwestern Medicine in Chicago. To address that problem, he and his colleagues launched the Socrates Project. The service is intended for difficult diagnoses and is based on Socratic principles, particularly the role of iterative hypothesis testing in the process of diagnosis.
“We began the Socrates Project to assist physicians caring for patients who lack a specific diagnosis. In creating this service, we have found ourselves to be doctors for doctors – formalizing the curbside consultation,” Dr. Singer said.
Northwestern Medicine launched the Socrates Project in 2015. It’s a physician-to-physician consultation service that assists doctors working to diagnose conditions that have so far eluded detection. “Our service’s goal is to improve patient care by providing an opinion to the referring physician on diagnostic possibilities for a particular case and ideas to reduce – or at least manage – diagnostic uncertainty,” they write. “Our service model is similar to a tumor board, which exists as an interdisciplinary group operating in parallel to the clinical services, to provide consensus-based recommendations.”
Hospitalists at other institutions may be interested in starting a similar type of service at their own institution or collaborating with institutions who offer this type of service, Dr. Singer said.
At Northwestern Medicine, they are at work on the project’s next steps. “We are working to generate systematic data about our practice, particularly the types of referrals and outcomes,” he said.
Reference
1. Singer BD, et al. The Socrates Project for Difficult Diagnosis at Northwestern Medicine. J Hosp Med. 2020 February;15(2):116-125. doi:10.12788/jhm.3335.
Beyond its clinical objective, the Socrates Project also seeks to further the discovery of previously unrecognized disease processes.
Many patients do not have a diagnosis that explains their signs and symptoms, despite a thorough evaluation, said Benjamin Singer, MD, assistant professor of pulmonology and critical care at Northwestern Medicine in Chicago. To address that problem, he and his colleagues launched the Socrates Project. The service is intended for difficult diagnoses and is based on Socratic principles, particularly the role of iterative hypothesis testing in the process of diagnosis.
“We began the Socrates Project to assist physicians caring for patients who lack a specific diagnosis. In creating this service, we have found ourselves to be doctors for doctors – formalizing the curbside consultation,” Dr. Singer said.
Northwestern Medicine launched the Socrates Project in 2015. It’s a physician-to-physician consultation service that assists doctors working to diagnose conditions that have so far eluded detection. “Our service’s goal is to improve patient care by providing an opinion to the referring physician on diagnostic possibilities for a particular case and ideas to reduce – or at least manage – diagnostic uncertainty,” they write. “Our service model is similar to a tumor board, which exists as an interdisciplinary group operating in parallel to the clinical services, to provide consensus-based recommendations.”
Hospitalists at other institutions may be interested in starting a similar type of service at their own institution or collaborating with institutions who offer this type of service, Dr. Singer said.
At Northwestern Medicine, they are at work on the project’s next steps. “We are working to generate systematic data about our practice, particularly the types of referrals and outcomes,” he said.
Reference
1. Singer BD, et al. The Socrates Project for Difficult Diagnosis at Northwestern Medicine. J Hosp Med. 2020 February;15(2):116-125. doi:10.12788/jhm.3335.
Coffee lowers heart failure risk in unique study
Higher coffee consumption is associated with a lower risk of heart failure, according to a machine learning–based algorithm that analyzed data from three large observational trials.
“Coffee consumption actually was predictive on top of known risk factors originally identified from those three trials.” The study is significant because it underscores the potential of big data for individualizing patient management, lead investigator David Kao, MD, said in an interview. “We in fact adjusted for the scores that are commonly used to predict heart disease, and coffee consumption remained a predictor even on top of that.”
The study used supervised machine learning to analyze data on diet and other variables from three well-known observational studies: Framingham Heart Study (FHS), Cardiovascular Heart Study (CHS), and ARIC (Atherosclerosis Risk in Communities). The goal of the study, published online on Feb. 9, 2021*, was to identify potential novel risk factors for incident coronary heart disease, stroke, and heart failure.
“The main difference of the relationship between coffee and heart disease, compared with prior analyses, is that we’re able to find it in these well-known and well-accepted studies that have helped us find risk factors before,” Dr. Kao said
The study included 2,732 FHS participants aged 30-62 years, 3,704 CHS patients aged 65 and older, and 14,925 ARIC subjects aged 45-64, all of whom had no history of cardiovascular disease events when they enrolled. Primary outcomes for the machine-learning study were times to incident coronary heart disease, heart failure, and stroke.
Mathematics, not hypotheses
To compensate for variations in methodologies between the three observational trials, the study used 204 data measurements collected at the first FHS exam, including 16 dietary variables and for which similar data were collected for the other two studies.
The machine-learning model used what’s known as a random forest analysis to identify the leading potential risk factors from among the 204 variables. To confirm findings between studies, the authors used a technique called “data harmonization” to smooth variations in the methodologies of the trials, not only with participant age and duration and date of the trials, but also in how data on coffee consumption were gathered. For example, FHS collected that data as cups per day, whereas CHS and ARIC collected that as monthly, weekly, and daily consumption. The study converted the coffee consumption data from CHS and ARIC to cups per day to conform to FHS data.
Random forest analysis is a type of machine learning that randomly creates a cluster of decision trees – the “forest” – to determine which variables, such as dietary factors, are important in predicting a result. The analysis uses mathematics, not hypotheses, to identify important variables.
Heart failure and risk reduced
In this study, the analysis determined that each cup of caffeinated coffee daily was linked with a 5% reduction in the risk of heart failure (hazard ratio, 0.95; P = .02) and 6% reduction in stroke risk (HR, 0.94; P = .02), but had no significant impact on risk for coronary heart disease or cardiovascular disease.
When the data were adjusted for the FHS CVD risk score, increasing coffee consumption remained significantly associated with an identical lower risk of heart failure (P = .03) but not stroke (P = .33).
While the study supports an association between coffee consumption and heart failure risk, it doesn’t establish causation, noted Alice H. Lichtenstein, DSc, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston. “The authors could not rule out the possibility that caffeinated coffee intake was a proxy for other heart-healthy lifestyle behaviors,” Dr. Lichtenstein said. “Perhaps the best message from the study is that there appears to be no adverse effects of drinking moderate amounts of caffeinated coffee, and there may be benefits.”
She added a note of caution. “This result does not suggest coffee intake should be increased, nor does it give license to increasing coffee drinks with a lot of added cream and sugar.”
Machine learning mines observational trials
Dr. Kao explained the rationale for applying a machine-learning algorithm to the three observational trials. “When these trials were designed in general, they had an idea of what they were looking for in terms of what might be a risk factor,” said Dr. Kao, of the University of Colorado at Denver, Aurora. “What we were interested in doing was to look for risk factors that nobody really thought about ahead of time and let the data show us what might be a predictor without any bias of what we imagined to be true.”
He described the role of machine learning in extracting and “filtering” data from the trials. “Machine learning allows us to look at a very large number of factors or variables and identify the most important ones in predicting a specific outcome,” he said. This study evaluated the 204 variables and focused on dietary factors because they’re modifiable.
“We looked at them in these different studies where we could, and coffee was the one that was reproducible in all of them,” he said. “Machine learning helped filter down these very large numbers of variables in ways you can’t do with traditional statistics. It’s useful in studies like this because they gather thousands and thousands of variables that generally nobody uses, but these methods allow you to actually do something with them – to determine which ones are most important.”
He added: “These methods I think will take us toward personalized medicine where you’re really individualizing a plan for keeping a patient healthy. We still have a lot of work to do, but there’s a lot of promise for really helping each of us to figure out the ways we can become the healthiest that we can be.”
The study was supported with funding from the National Heart, Lung, and Blood Institute and the American Heart Association. Dr. Kao and coauthors, as well as Dr. Lichtenstein, had no relevant financial relationships to disclose.
*Correction, 2/10/21: An earlier version of this article misstated the study's publication date.
Higher coffee consumption is associated with a lower risk of heart failure, according to a machine learning–based algorithm that analyzed data from three large observational trials.
“Coffee consumption actually was predictive on top of known risk factors originally identified from those three trials.” The study is significant because it underscores the potential of big data for individualizing patient management, lead investigator David Kao, MD, said in an interview. “We in fact adjusted for the scores that are commonly used to predict heart disease, and coffee consumption remained a predictor even on top of that.”
The study used supervised machine learning to analyze data on diet and other variables from three well-known observational studies: Framingham Heart Study (FHS), Cardiovascular Heart Study (CHS), and ARIC (Atherosclerosis Risk in Communities). The goal of the study, published online on Feb. 9, 2021*, was to identify potential novel risk factors for incident coronary heart disease, stroke, and heart failure.
“The main difference of the relationship between coffee and heart disease, compared with prior analyses, is that we’re able to find it in these well-known and well-accepted studies that have helped us find risk factors before,” Dr. Kao said
The study included 2,732 FHS participants aged 30-62 years, 3,704 CHS patients aged 65 and older, and 14,925 ARIC subjects aged 45-64, all of whom had no history of cardiovascular disease events when they enrolled. Primary outcomes for the machine-learning study were times to incident coronary heart disease, heart failure, and stroke.
Mathematics, not hypotheses
To compensate for variations in methodologies between the three observational trials, the study used 204 data measurements collected at the first FHS exam, including 16 dietary variables and for which similar data were collected for the other two studies.
The machine-learning model used what’s known as a random forest analysis to identify the leading potential risk factors from among the 204 variables. To confirm findings between studies, the authors used a technique called “data harmonization” to smooth variations in the methodologies of the trials, not only with participant age and duration and date of the trials, but also in how data on coffee consumption were gathered. For example, FHS collected that data as cups per day, whereas CHS and ARIC collected that as monthly, weekly, and daily consumption. The study converted the coffee consumption data from CHS and ARIC to cups per day to conform to FHS data.
Random forest analysis is a type of machine learning that randomly creates a cluster of decision trees – the “forest” – to determine which variables, such as dietary factors, are important in predicting a result. The analysis uses mathematics, not hypotheses, to identify important variables.
Heart failure and risk reduced
In this study, the analysis determined that each cup of caffeinated coffee daily was linked with a 5% reduction in the risk of heart failure (hazard ratio, 0.95; P = .02) and 6% reduction in stroke risk (HR, 0.94; P = .02), but had no significant impact on risk for coronary heart disease or cardiovascular disease.
When the data were adjusted for the FHS CVD risk score, increasing coffee consumption remained significantly associated with an identical lower risk of heart failure (P = .03) but not stroke (P = .33).
While the study supports an association between coffee consumption and heart failure risk, it doesn’t establish causation, noted Alice H. Lichtenstein, DSc, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston. “The authors could not rule out the possibility that caffeinated coffee intake was a proxy for other heart-healthy lifestyle behaviors,” Dr. Lichtenstein said. “Perhaps the best message from the study is that there appears to be no adverse effects of drinking moderate amounts of caffeinated coffee, and there may be benefits.”
She added a note of caution. “This result does not suggest coffee intake should be increased, nor does it give license to increasing coffee drinks with a lot of added cream and sugar.”
Machine learning mines observational trials
Dr. Kao explained the rationale for applying a machine-learning algorithm to the three observational trials. “When these trials were designed in general, they had an idea of what they were looking for in terms of what might be a risk factor,” said Dr. Kao, of the University of Colorado at Denver, Aurora. “What we were interested in doing was to look for risk factors that nobody really thought about ahead of time and let the data show us what might be a predictor without any bias of what we imagined to be true.”
He described the role of machine learning in extracting and “filtering” data from the trials. “Machine learning allows us to look at a very large number of factors or variables and identify the most important ones in predicting a specific outcome,” he said. This study evaluated the 204 variables and focused on dietary factors because they’re modifiable.
“We looked at them in these different studies where we could, and coffee was the one that was reproducible in all of them,” he said. “Machine learning helped filter down these very large numbers of variables in ways you can’t do with traditional statistics. It’s useful in studies like this because they gather thousands and thousands of variables that generally nobody uses, but these methods allow you to actually do something with them – to determine which ones are most important.”
He added: “These methods I think will take us toward personalized medicine where you’re really individualizing a plan for keeping a patient healthy. We still have a lot of work to do, but there’s a lot of promise for really helping each of us to figure out the ways we can become the healthiest that we can be.”
The study was supported with funding from the National Heart, Lung, and Blood Institute and the American Heart Association. Dr. Kao and coauthors, as well as Dr. Lichtenstein, had no relevant financial relationships to disclose.
*Correction, 2/10/21: An earlier version of this article misstated the study's publication date.
Higher coffee consumption is associated with a lower risk of heart failure, according to a machine learning–based algorithm that analyzed data from three large observational trials.
“Coffee consumption actually was predictive on top of known risk factors originally identified from those three trials.” The study is significant because it underscores the potential of big data for individualizing patient management, lead investigator David Kao, MD, said in an interview. “We in fact adjusted for the scores that are commonly used to predict heart disease, and coffee consumption remained a predictor even on top of that.”
The study used supervised machine learning to analyze data on diet and other variables from three well-known observational studies: Framingham Heart Study (FHS), Cardiovascular Heart Study (CHS), and ARIC (Atherosclerosis Risk in Communities). The goal of the study, published online on Feb. 9, 2021*, was to identify potential novel risk factors for incident coronary heart disease, stroke, and heart failure.
“The main difference of the relationship between coffee and heart disease, compared with prior analyses, is that we’re able to find it in these well-known and well-accepted studies that have helped us find risk factors before,” Dr. Kao said
The study included 2,732 FHS participants aged 30-62 years, 3,704 CHS patients aged 65 and older, and 14,925 ARIC subjects aged 45-64, all of whom had no history of cardiovascular disease events when they enrolled. Primary outcomes for the machine-learning study were times to incident coronary heart disease, heart failure, and stroke.
Mathematics, not hypotheses
To compensate for variations in methodologies between the three observational trials, the study used 204 data measurements collected at the first FHS exam, including 16 dietary variables and for which similar data were collected for the other two studies.
The machine-learning model used what’s known as a random forest analysis to identify the leading potential risk factors from among the 204 variables. To confirm findings between studies, the authors used a technique called “data harmonization” to smooth variations in the methodologies of the trials, not only with participant age and duration and date of the trials, but also in how data on coffee consumption were gathered. For example, FHS collected that data as cups per day, whereas CHS and ARIC collected that as monthly, weekly, and daily consumption. The study converted the coffee consumption data from CHS and ARIC to cups per day to conform to FHS data.
Random forest analysis is a type of machine learning that randomly creates a cluster of decision trees – the “forest” – to determine which variables, such as dietary factors, are important in predicting a result. The analysis uses mathematics, not hypotheses, to identify important variables.
Heart failure and risk reduced
In this study, the analysis determined that each cup of caffeinated coffee daily was linked with a 5% reduction in the risk of heart failure (hazard ratio, 0.95; P = .02) and 6% reduction in stroke risk (HR, 0.94; P = .02), but had no significant impact on risk for coronary heart disease or cardiovascular disease.
When the data were adjusted for the FHS CVD risk score, increasing coffee consumption remained significantly associated with an identical lower risk of heart failure (P = .03) but not stroke (P = .33).
While the study supports an association between coffee consumption and heart failure risk, it doesn’t establish causation, noted Alice H. Lichtenstein, DSc, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston. “The authors could not rule out the possibility that caffeinated coffee intake was a proxy for other heart-healthy lifestyle behaviors,” Dr. Lichtenstein said. “Perhaps the best message from the study is that there appears to be no adverse effects of drinking moderate amounts of caffeinated coffee, and there may be benefits.”
She added a note of caution. “This result does not suggest coffee intake should be increased, nor does it give license to increasing coffee drinks with a lot of added cream and sugar.”
Machine learning mines observational trials
Dr. Kao explained the rationale for applying a machine-learning algorithm to the three observational trials. “When these trials were designed in general, they had an idea of what they were looking for in terms of what might be a risk factor,” said Dr. Kao, of the University of Colorado at Denver, Aurora. “What we were interested in doing was to look for risk factors that nobody really thought about ahead of time and let the data show us what might be a predictor without any bias of what we imagined to be true.”
He described the role of machine learning in extracting and “filtering” data from the trials. “Machine learning allows us to look at a very large number of factors or variables and identify the most important ones in predicting a specific outcome,” he said. This study evaluated the 204 variables and focused on dietary factors because they’re modifiable.
“We looked at them in these different studies where we could, and coffee was the one that was reproducible in all of them,” he said. “Machine learning helped filter down these very large numbers of variables in ways you can’t do with traditional statistics. It’s useful in studies like this because they gather thousands and thousands of variables that generally nobody uses, but these methods allow you to actually do something with them – to determine which ones are most important.”
He added: “These methods I think will take us toward personalized medicine where you’re really individualizing a plan for keeping a patient healthy. We still have a lot of work to do, but there’s a lot of promise for really helping each of us to figure out the ways we can become the healthiest that we can be.”
The study was supported with funding from the National Heart, Lung, and Blood Institute and the American Heart Association. Dr. Kao and coauthors, as well as Dr. Lichtenstein, had no relevant financial relationships to disclose.
*Correction, 2/10/21: An earlier version of this article misstated the study's publication date.
FROM CIRCULATION: HEART FAILURE