User login
CHMP recommends new formulation of pegaspargase
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending marketing authorization for lyophilized pegaspargase (ONCASPAR).
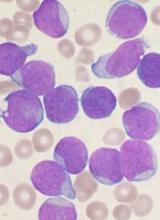
If approved, the product would be used as a component of antineoplastic therapy in patients of all ages who have acute lymphoblastic leukemia (ALL).
The product is a freeze-dried formulation of liquid pegaspargase, which is already approved for the aforementioned indication.
The CHMP’s recommendation regarding lyophilized pegaspargase will be submitted to the European Commission (EC).
The EC typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The EC’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
The CHMP’s recommendation regarding lyophilized pegaspargase is based on analytical and nonclinical studies, which indicate that lyophilized pegaspargase is comparable to the liquid formulation.
Once reconstituted, lyophilized pegaspargase demonstrates similar pharmacokinetics and pharmacodynamics as liquid pegaspargase.
“Lyophilized ONCASPAR builds on more than a decade of data and research with liquid ONCASPAR, and, with no change in dosing regimen, it offers a 3-times longer shelf life,” said Howard B. Mayer, MD, of Shire, the company that developed lyophilized pegaspargase.
“Prolonging shelf life to 24 months for this critically important therapy facilitates management of product inventory by enabling greater flexibility and longer-term planning. Once approved, with the extended shelf life of lyophilized ONCASPAR, we also hope to improve access to the medicine for ALL patients in countries currently not offering liquid ONCASPAR.”
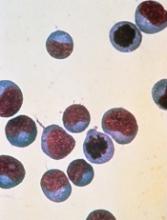
Lyophilized pegaspargase works in the same way as the liquid formulation. It rapidly depletes serum L-asparagine levels and interferes with protein synthesis, thereby depriving lymphoblasts of asparaginase and resulting in cell death. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending marketing authorization for lyophilized pegaspargase (ONCASPAR).
If approved, the product would be used as a component of antineoplastic therapy in patients of all ages who have acute lymphoblastic leukemia (ALL).
The product is a freeze-dried formulation of liquid pegaspargase, which is already approved for the aforementioned indication.
The CHMP’s recommendation regarding lyophilized pegaspargase will be submitted to the European Commission (EC).
The EC typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The EC’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
The CHMP’s recommendation regarding lyophilized pegaspargase is based on analytical and nonclinical studies, which indicate that lyophilized pegaspargase is comparable to the liquid formulation.
Once reconstituted, lyophilized pegaspargase demonstrates similar pharmacokinetics and pharmacodynamics as liquid pegaspargase.
“Lyophilized ONCASPAR builds on more than a decade of data and research with liquid ONCASPAR, and, with no change in dosing regimen, it offers a 3-times longer shelf life,” said Howard B. Mayer, MD, of Shire, the company that developed lyophilized pegaspargase.
“Prolonging shelf life to 24 months for this critically important therapy facilitates management of product inventory by enabling greater flexibility and longer-term planning. Once approved, with the extended shelf life of lyophilized ONCASPAR, we also hope to improve access to the medicine for ALL patients in countries currently not offering liquid ONCASPAR.”
Lyophilized pegaspargase works in the same way as the liquid formulation. It rapidly depletes serum L-asparagine levels and interferes with protein synthesis, thereby depriving lymphoblasts of asparaginase and resulting in cell death. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending marketing authorization for lyophilized pegaspargase (ONCASPAR).
If approved, the product would be used as a component of antineoplastic therapy in patients of all ages who have acute lymphoblastic leukemia (ALL).
The product is a freeze-dried formulation of liquid pegaspargase, which is already approved for the aforementioned indication.
The CHMP’s recommendation regarding lyophilized pegaspargase will be submitted to the European Commission (EC).
The EC typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The EC’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
The CHMP’s recommendation regarding lyophilized pegaspargase is based on analytical and nonclinical studies, which indicate that lyophilized pegaspargase is comparable to the liquid formulation.
Once reconstituted, lyophilized pegaspargase demonstrates similar pharmacokinetics and pharmacodynamics as liquid pegaspargase.
“Lyophilized ONCASPAR builds on more than a decade of data and research with liquid ONCASPAR, and, with no change in dosing regimen, it offers a 3-times longer shelf life,” said Howard B. Mayer, MD, of Shire, the company that developed lyophilized pegaspargase.
“Prolonging shelf life to 24 months for this critically important therapy facilitates management of product inventory by enabling greater flexibility and longer-term planning. Once approved, with the extended shelf life of lyophilized ONCASPAR, we also hope to improve access to the medicine for ALL patients in countries currently not offering liquid ONCASPAR.”
Lyophilized pegaspargase works in the same way as the liquid formulation. It rapidly depletes serum L-asparagine levels and interferes with protein synthesis, thereby depriving lymphoblasts of asparaginase and resulting in cell death. ![]()
Natural selection opportunities tied to cancer rates
Countries with the lowest opportunities for natural selection have higher cancer rates than countries with the highest opportunities for natural selection, according to a study published in Evolutionary Applications.
Researchers said this is because modern medicine is enabling people to survive cancers, and their genetic backgrounds are passing from one generation to the next.
The team said the rate of some cancers has doubled and even quadrupled over the past 100 to 150 years, and human evolution has moved away from “survival of the fittest.”
“Modern medicine has enabled the human species to live much longer than would otherwise be expected in the natural world,” said study author Maciej Henneberg, PhD, DSc, of the University of Adelaide in South Australia.
“Besides the obvious benefits that modern medicine gives, it also brings with it an unexpected side-effect—allowing genetic material to be passed from one generation to the next that predisposes people to have poor health, such as type 1 diabetes or cancer.”
“Because of the quality of our healthcare in western society, we have almost removed natural selection as the ‘janitor of the gene pool.’ Unfortunately, the accumulation of genetic mutations over time and across multiple generations is like a delayed death sentence.”
Country comparison
The researchers studied global cancer data from the World Health Organization as well as other health and socioeconomic data from the United Nations and the World Bank of 173 countries. The team compared the top 10 countries with the highest opportunities for natural selection to the 10 countries with the lowest opportunities for natural selection.
“We looked at countries that offered the greatest opportunity to survive cancer compared with those that didn’t,” said study author Wenpeng You, a PhD student at the University of Adelaide. “This does not only take into account factors such as socioeconomic status, urbanization, and quality of medical services but also low mortality and fertility rates, which are the 2 distinguishing features in the ‘better’ world.”
“Countries with low mortality rates may allow more people with cancer genetic background to reproduce and pass cancer genes/mutations to the next generation. Meanwhile, low fertility rates in these countries may not be able to have diverse biological variations to provide the opportunity for selecting a naturally fit population—for example, people without or with less cancer genetic background. Low mortality rate and low fertility rate in the ‘better’ world may have formed a self-reinforcing cycle which has accumulated cancer genetic background at a greater rate than previously thought.”
Based on the researchers’ analysis, the 20 countries are:
| Lowest opportunities for natural selection | Highest opportunities for natural selection |
| Iceland | Burkina Faso |
| Singapore | Chad |
| Japan | Central African Republic |
| Switzerland | Afghanistan |
| Sweden | Somalia |
| Luxembourg | Sierra Leone |
| Germany | Democratic Republic of the Congo |
| Italy | Guinea-Bissau |
| Cyprus | Burundi |
| Andorra | Cameroon |
Cancer incidence
The researchers found the rates of most cancers were higher in the 10 countries with the lowest opportunities for natural selection. The incidence of all cancers was 2.326 times higher in the low-opportunity countries than the high-opportunity ones.
The increased incidences of hematologic malignancies were as follows:
- Non-Hodgkin lymphoma—2.019 times higher in the low-opportunity countries
- Hodgkin lymphoma—3.314 times higher in the low-opportunity countries
- Leukemia—3.574 times higher in the low-opportunity countries
- Multiple myeloma—4.257 times higher in the low-opportunity countries .
Dr Henneberg said that, having removed natural selection as the “janitor of the gene pool,” our modern society is faced with a controversial issue.
“It may be that the only way humankind can be rid of cancer once and for all is through genetic engineering—to repair our genes and take cancer out of the equation,” he said. ![]()
Countries with the lowest opportunities for natural selection have higher cancer rates than countries with the highest opportunities for natural selection, according to a study published in Evolutionary Applications.
Researchers said this is because modern medicine is enabling people to survive cancers, and their genetic backgrounds are passing from one generation to the next.
The team said the rate of some cancers has doubled and even quadrupled over the past 100 to 150 years, and human evolution has moved away from “survival of the fittest.”
“Modern medicine has enabled the human species to live much longer than would otherwise be expected in the natural world,” said study author Maciej Henneberg, PhD, DSc, of the University of Adelaide in South Australia.
“Besides the obvious benefits that modern medicine gives, it also brings with it an unexpected side-effect—allowing genetic material to be passed from one generation to the next that predisposes people to have poor health, such as type 1 diabetes or cancer.”
“Because of the quality of our healthcare in western society, we have almost removed natural selection as the ‘janitor of the gene pool.’ Unfortunately, the accumulation of genetic mutations over time and across multiple generations is like a delayed death sentence.”
Country comparison
The researchers studied global cancer data from the World Health Organization as well as other health and socioeconomic data from the United Nations and the World Bank of 173 countries. The team compared the top 10 countries with the highest opportunities for natural selection to the 10 countries with the lowest opportunities for natural selection.
“We looked at countries that offered the greatest opportunity to survive cancer compared with those that didn’t,” said study author Wenpeng You, a PhD student at the University of Adelaide. “This does not only take into account factors such as socioeconomic status, urbanization, and quality of medical services but also low mortality and fertility rates, which are the 2 distinguishing features in the ‘better’ world.”
“Countries with low mortality rates may allow more people with cancer genetic background to reproduce and pass cancer genes/mutations to the next generation. Meanwhile, low fertility rates in these countries may not be able to have diverse biological variations to provide the opportunity for selecting a naturally fit population—for example, people without or with less cancer genetic background. Low mortality rate and low fertility rate in the ‘better’ world may have formed a self-reinforcing cycle which has accumulated cancer genetic background at a greater rate than previously thought.”
Based on the researchers’ analysis, the 20 countries are:
| Lowest opportunities for natural selection | Highest opportunities for natural selection |
| Iceland | Burkina Faso |
| Singapore | Chad |
| Japan | Central African Republic |
| Switzerland | Afghanistan |
| Sweden | Somalia |
| Luxembourg | Sierra Leone |
| Germany | Democratic Republic of the Congo |
| Italy | Guinea-Bissau |
| Cyprus | Burundi |
| Andorra | Cameroon |
Cancer incidence
The researchers found the rates of most cancers were higher in the 10 countries with the lowest opportunities for natural selection. The incidence of all cancers was 2.326 times higher in the low-opportunity countries than the high-opportunity ones.
The increased incidences of hematologic malignancies were as follows:
- Non-Hodgkin lymphoma—2.019 times higher in the low-opportunity countries
- Hodgkin lymphoma—3.314 times higher in the low-opportunity countries
- Leukemia—3.574 times higher in the low-opportunity countries
- Multiple myeloma—4.257 times higher in the low-opportunity countries .
Dr Henneberg said that, having removed natural selection as the “janitor of the gene pool,” our modern society is faced with a controversial issue.
“It may be that the only way humankind can be rid of cancer once and for all is through genetic engineering—to repair our genes and take cancer out of the equation,” he said. ![]()
Countries with the lowest opportunities for natural selection have higher cancer rates than countries with the highest opportunities for natural selection, according to a study published in Evolutionary Applications.
Researchers said this is because modern medicine is enabling people to survive cancers, and their genetic backgrounds are passing from one generation to the next.
The team said the rate of some cancers has doubled and even quadrupled over the past 100 to 150 years, and human evolution has moved away from “survival of the fittest.”
“Modern medicine has enabled the human species to live much longer than would otherwise be expected in the natural world,” said study author Maciej Henneberg, PhD, DSc, of the University of Adelaide in South Australia.
“Besides the obvious benefits that modern medicine gives, it also brings with it an unexpected side-effect—allowing genetic material to be passed from one generation to the next that predisposes people to have poor health, such as type 1 diabetes or cancer.”
“Because of the quality of our healthcare in western society, we have almost removed natural selection as the ‘janitor of the gene pool.’ Unfortunately, the accumulation of genetic mutations over time and across multiple generations is like a delayed death sentence.”
Country comparison
The researchers studied global cancer data from the World Health Organization as well as other health and socioeconomic data from the United Nations and the World Bank of 173 countries. The team compared the top 10 countries with the highest opportunities for natural selection to the 10 countries with the lowest opportunities for natural selection.
“We looked at countries that offered the greatest opportunity to survive cancer compared with those that didn’t,” said study author Wenpeng You, a PhD student at the University of Adelaide. “This does not only take into account factors such as socioeconomic status, urbanization, and quality of medical services but also low mortality and fertility rates, which are the 2 distinguishing features in the ‘better’ world.”
“Countries with low mortality rates may allow more people with cancer genetic background to reproduce and pass cancer genes/mutations to the next generation. Meanwhile, low fertility rates in these countries may not be able to have diverse biological variations to provide the opportunity for selecting a naturally fit population—for example, people without or with less cancer genetic background. Low mortality rate and low fertility rate in the ‘better’ world may have formed a self-reinforcing cycle which has accumulated cancer genetic background at a greater rate than previously thought.”
Based on the researchers’ analysis, the 20 countries are:
| Lowest opportunities for natural selection | Highest opportunities for natural selection |
| Iceland | Burkina Faso |
| Singapore | Chad |
| Japan | Central African Republic |
| Switzerland | Afghanistan |
| Sweden | Somalia |
| Luxembourg | Sierra Leone |
| Germany | Democratic Republic of the Congo |
| Italy | Guinea-Bissau |
| Cyprus | Burundi |
| Andorra | Cameroon |
Cancer incidence
The researchers found the rates of most cancers were higher in the 10 countries with the lowest opportunities for natural selection. The incidence of all cancers was 2.326 times higher in the low-opportunity countries than the high-opportunity ones.
The increased incidences of hematologic malignancies were as follows:
- Non-Hodgkin lymphoma—2.019 times higher in the low-opportunity countries
- Hodgkin lymphoma—3.314 times higher in the low-opportunity countries
- Leukemia—3.574 times higher in the low-opportunity countries
- Multiple myeloma—4.257 times higher in the low-opportunity countries .
Dr Henneberg said that, having removed natural selection as the “janitor of the gene pool,” our modern society is faced with a controversial issue.
“It may be that the only way humankind can be rid of cancer once and for all is through genetic engineering—to repair our genes and take cancer out of the equation,” he said. ![]()
Study supports prophylaxis in kids with ALL
Results of an observational study support targeted antibacterial prophylaxis in children undergoing induction therapy for acute lymphoblastic leukemia (ALL).
Prophylaxis effectively prevented febrile neutropenia and systemic infection in the children studied.
Prophylaxis with the drug levofloxacin reduced the use of treatment antibiotics and the incidence of Clostridium difficile infection.
“This research provides the first major evidence supporting targeted use of antibacterial prophylaxis for at-risk pediatric ALL patients, particularly use of the broad-spectrum antibiotic levofloxacin,” said study author Joshua Wolf, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Prophylactic antibiotic therapy with levofloxacin is routine for at-risk adult ALL patients, but it has remained controversial in children. Until this study, evidence supporting the safety and efficacy of prophylactic antibiotic therapy in children with ALL has been sparse.”
Dr Wolf and his colleagues described their study in Clinical Infectious Diseases.
The study included 344 patients newly diagnosed with ALL who were enrolled in the St. Jude Total XVI clinical trial (NCT00549848). Patients were enrolled from 2007 to 2016.
Until July 2014, the patients received prophylactic antibiotic therapy at the discretion of their physicians. Patients typically received cefepime, ciprofloxacin, or vancomycin plus cefepime or ciprofloxacin. And prophylaxis was typically started at the onset of neutropenia after chemotherapy.
Beginning in August 2014, hospital treatment guidelines changed to recommend prophylactic levofloxacin during induction for ALL patients who develop neutropenia expected to last at least 7 days.
Dr Wolf and his colleagues used the change to compare infection rates and other questions in the following patient groups.
| Patient characteristics | No prophylaxis (n=173) | Levofloxacin prophylaxis (n=69) | Other prophylaxis (n=102) |
| Median age in years (range) | 5.8 (3-11.9) | 6.8 (3.9-11.1) | 7 (3.6-11.9) |
| B-ALL | 83% | 78% | 79% |
| Low-risk ALL | 51% | 54% | 50% |
| Standard-risk ALL | 47% | 41% | 42% |
| High-risk ALL | 2% | 6% | 8% |
| Median duration of neutropenia in days (range) | 17 (11-24) | 18 (12-23) | 20 (17-25) |
| Median duration of profound neutropenia in days (range) | 6 (2-13) | 7 (4-12) | 11 (5-16) |
Results
Researchers reported that patients with neutropenia who received any prophylactic therapy were far less likely than those who did not to develop fever, documented or likely infections, or bloodstream infections.
In a multivariate analysis, the adjusted odds ratios in patients who received prophylaxis, compared to those who did not, were as follows.
- Febrile neutropenia—0.23, P<0.001
- Febrile neutropenia with clinically documented infection—0.30, P=0.002
- Febrile neutropenia with microbiologically documented infection—0.25, P<0.001
- Clinically documented infection—0.54, P=0.02
- Microbiologically documented infection—0.40, P<0.001
- Bloodstream infection—0.30, P=0.008
- C difficile infection—0.38, P=0.04
- Likely bacterial infection—0.26, P<0.001
- Any enterocolitis—0.44, P=0.03.
Analysis also revealed that patients who received levofloxacin had a greater reduction in C difficile infection than patients who received other prophylaxis. The adjusted odds ratio was 0.04 (P<0.001).
However, there was no significant difference between the prophylaxis groups when it came to other infections.
Patients who received levofloxacin prophylaxis had significantly less exposure to other antibiotics than patients who received other prophylaxis or no prophylaxis.
This included exposure to cefepime/ceftazidime (P<0.001 for both comparisons), vancomycin (P<0.001 for both), meropenem (P<0.001 for both), and aminoglycosides (P=0.002 for no prophylaxis, P=0.04 for other prophylaxis).
The reduction in exposure to other antibiotics may partly explain why C difficile infections declined in levofloxacin-treated patients, Dr Wolf said.
He also noted that antibiotic resistance did not significantly increase in this study, despite the greater use of levofloxacin to prevent infections.
“We are cautiously optimistic that any impact of levofloxacin on antibacterial resistance will be balanced by the reduction in use of other antibiotics,” Dr Wolf said, “but long-term monitoring of antibiotic resistance patterns in young ALL patients will be needed to prove this.” ![]()
Results of an observational study support targeted antibacterial prophylaxis in children undergoing induction therapy for acute lymphoblastic leukemia (ALL).
Prophylaxis effectively prevented febrile neutropenia and systemic infection in the children studied.
Prophylaxis with the drug levofloxacin reduced the use of treatment antibiotics and the incidence of Clostridium difficile infection.
“This research provides the first major evidence supporting targeted use of antibacterial prophylaxis for at-risk pediatric ALL patients, particularly use of the broad-spectrum antibiotic levofloxacin,” said study author Joshua Wolf, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Prophylactic antibiotic therapy with levofloxacin is routine for at-risk adult ALL patients, but it has remained controversial in children. Until this study, evidence supporting the safety and efficacy of prophylactic antibiotic therapy in children with ALL has been sparse.”
Dr Wolf and his colleagues described their study in Clinical Infectious Diseases.
The study included 344 patients newly diagnosed with ALL who were enrolled in the St. Jude Total XVI clinical trial (NCT00549848). Patients were enrolled from 2007 to 2016.
Until July 2014, the patients received prophylactic antibiotic therapy at the discretion of their physicians. Patients typically received cefepime, ciprofloxacin, or vancomycin plus cefepime or ciprofloxacin. And prophylaxis was typically started at the onset of neutropenia after chemotherapy.
Beginning in August 2014, hospital treatment guidelines changed to recommend prophylactic levofloxacin during induction for ALL patients who develop neutropenia expected to last at least 7 days.
Dr Wolf and his colleagues used the change to compare infection rates and other questions in the following patient groups.
| Patient characteristics | No prophylaxis (n=173) | Levofloxacin prophylaxis (n=69) | Other prophylaxis (n=102) |
| Median age in years (range) | 5.8 (3-11.9) | 6.8 (3.9-11.1) | 7 (3.6-11.9) |
| B-ALL | 83% | 78% | 79% |
| Low-risk ALL | 51% | 54% | 50% |
| Standard-risk ALL | 47% | 41% | 42% |
| High-risk ALL | 2% | 6% | 8% |
| Median duration of neutropenia in days (range) | 17 (11-24) | 18 (12-23) | 20 (17-25) |
| Median duration of profound neutropenia in days (range) | 6 (2-13) | 7 (4-12) | 11 (5-16) |
Results
Researchers reported that patients with neutropenia who received any prophylactic therapy were far less likely than those who did not to develop fever, documented or likely infections, or bloodstream infections.
In a multivariate analysis, the adjusted odds ratios in patients who received prophylaxis, compared to those who did not, were as follows.
- Febrile neutropenia—0.23, P<0.001
- Febrile neutropenia with clinically documented infection—0.30, P=0.002
- Febrile neutropenia with microbiologically documented infection—0.25, P<0.001
- Clinically documented infection—0.54, P=0.02
- Microbiologically documented infection—0.40, P<0.001
- Bloodstream infection—0.30, P=0.008
- C difficile infection—0.38, P=0.04
- Likely bacterial infection—0.26, P<0.001
- Any enterocolitis—0.44, P=0.03.
Analysis also revealed that patients who received levofloxacin had a greater reduction in C difficile infection than patients who received other prophylaxis. The adjusted odds ratio was 0.04 (P<0.001).
However, there was no significant difference between the prophylaxis groups when it came to other infections.
Patients who received levofloxacin prophylaxis had significantly less exposure to other antibiotics than patients who received other prophylaxis or no prophylaxis.
This included exposure to cefepime/ceftazidime (P<0.001 for both comparisons), vancomycin (P<0.001 for both), meropenem (P<0.001 for both), and aminoglycosides (P=0.002 for no prophylaxis, P=0.04 for other prophylaxis).
The reduction in exposure to other antibiotics may partly explain why C difficile infections declined in levofloxacin-treated patients, Dr Wolf said.
He also noted that antibiotic resistance did not significantly increase in this study, despite the greater use of levofloxacin to prevent infections.
“We are cautiously optimistic that any impact of levofloxacin on antibacterial resistance will be balanced by the reduction in use of other antibiotics,” Dr Wolf said, “but long-term monitoring of antibiotic resistance patterns in young ALL patients will be needed to prove this.” ![]()
Results of an observational study support targeted antibacterial prophylaxis in children undergoing induction therapy for acute lymphoblastic leukemia (ALL).
Prophylaxis effectively prevented febrile neutropenia and systemic infection in the children studied.
Prophylaxis with the drug levofloxacin reduced the use of treatment antibiotics and the incidence of Clostridium difficile infection.
“This research provides the first major evidence supporting targeted use of antibacterial prophylaxis for at-risk pediatric ALL patients, particularly use of the broad-spectrum antibiotic levofloxacin,” said study author Joshua Wolf, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Prophylactic antibiotic therapy with levofloxacin is routine for at-risk adult ALL patients, but it has remained controversial in children. Until this study, evidence supporting the safety and efficacy of prophylactic antibiotic therapy in children with ALL has been sparse.”
Dr Wolf and his colleagues described their study in Clinical Infectious Diseases.
The study included 344 patients newly diagnosed with ALL who were enrolled in the St. Jude Total XVI clinical trial (NCT00549848). Patients were enrolled from 2007 to 2016.
Until July 2014, the patients received prophylactic antibiotic therapy at the discretion of their physicians. Patients typically received cefepime, ciprofloxacin, or vancomycin plus cefepime or ciprofloxacin. And prophylaxis was typically started at the onset of neutropenia after chemotherapy.
Beginning in August 2014, hospital treatment guidelines changed to recommend prophylactic levofloxacin during induction for ALL patients who develop neutropenia expected to last at least 7 days.
Dr Wolf and his colleagues used the change to compare infection rates and other questions in the following patient groups.
| Patient characteristics | No prophylaxis (n=173) | Levofloxacin prophylaxis (n=69) | Other prophylaxis (n=102) |
| Median age in years (range) | 5.8 (3-11.9) | 6.8 (3.9-11.1) | 7 (3.6-11.9) |
| B-ALL | 83% | 78% | 79% |
| Low-risk ALL | 51% | 54% | 50% |
| Standard-risk ALL | 47% | 41% | 42% |
| High-risk ALL | 2% | 6% | 8% |
| Median duration of neutropenia in days (range) | 17 (11-24) | 18 (12-23) | 20 (17-25) |
| Median duration of profound neutropenia in days (range) | 6 (2-13) | 7 (4-12) | 11 (5-16) |
Results
Researchers reported that patients with neutropenia who received any prophylactic therapy were far less likely than those who did not to develop fever, documented or likely infections, or bloodstream infections.
In a multivariate analysis, the adjusted odds ratios in patients who received prophylaxis, compared to those who did not, were as follows.
- Febrile neutropenia—0.23, P<0.001
- Febrile neutropenia with clinically documented infection—0.30, P=0.002
- Febrile neutropenia with microbiologically documented infection—0.25, P<0.001
- Clinically documented infection—0.54, P=0.02
- Microbiologically documented infection—0.40, P<0.001
- Bloodstream infection—0.30, P=0.008
- C difficile infection—0.38, P=0.04
- Likely bacterial infection—0.26, P<0.001
- Any enterocolitis—0.44, P=0.03.
Analysis also revealed that patients who received levofloxacin had a greater reduction in C difficile infection than patients who received other prophylaxis. The adjusted odds ratio was 0.04 (P<0.001).
However, there was no significant difference between the prophylaxis groups when it came to other infections.
Patients who received levofloxacin prophylaxis had significantly less exposure to other antibiotics than patients who received other prophylaxis or no prophylaxis.
This included exposure to cefepime/ceftazidime (P<0.001 for both comparisons), vancomycin (P<0.001 for both), meropenem (P<0.001 for both), and aminoglycosides (P=0.002 for no prophylaxis, P=0.04 for other prophylaxis).
The reduction in exposure to other antibiotics may partly explain why C difficile infections declined in levofloxacin-treated patients, Dr Wolf said.
He also noted that antibiotic resistance did not significantly increase in this study, despite the greater use of levofloxacin to prevent infections.
“We are cautiously optimistic that any impact of levofloxacin on antibacterial resistance will be balanced by the reduction in use of other antibiotics,” Dr Wolf said, “but long-term monitoring of antibiotic resistance patterns in young ALL patients will be needed to prove this.” ![]()
NCCN completes resource on radiation therapy
The National Comprehensive Cancer Network® (NCCN) has announced the release of the newly completed NCCN Radiation Therapy Compendium™.
This resource includes information designed to support clinical decision-making regarding the use of radiation therapy in cancer patients.
The content is based on the NCCN Clinical Practice Guidelines in Oncology and includes information from the 41 guidelines that reference radiation therapy.
“By compiling every recommendation for radiation therapy in one place, we’ve made it significantly easier for specialists . . . to stay up-to-date on the very latest recommendations, regardless of how many different cancer types they treat,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“This targeted content provides radiation oncologists with the specific, cutting-edge information they need, without forcing them to sift through any extraneous information. It’s part of our ongoing effort to always provide the most pertinent data on emerging treatment practices in the clearest, most efficient way possible.”
The NCCN Radiation Therapy Compendium includes a full complement of radiation therapy recommendations found in the current NCCN guidelines, including specific treatment modalities such as 2D/3D conformal external beam radiation therapy, intensity modulated radiation therapy, intra-operative radiation therapy, stereotactic radiosurgery/stereotactic body radiotherapy/stereotactic ablative body radiotherapy, image-guided radiation therapy, low dose-rate/high dose-rate brachytherapy, radioisotope, and particle therapy.
NCCN first announced the launch of the Radiation Therapy Compendium in March at the NCCN Annual Conference: Improving the Quality, Effectiveness, and Efficiency of Cancer Care.
At the time, the NCCN released a preliminary version of the compendium featuring 24 cancer types. The newly completed version now contains all 41 disease sites that are currently being treated using radiation therapy.
The compendium will be updated on a continual basis in conjunction with the library of clinical guidelines.
For more information and to access the NCCN Radiation Therapy Compendium, visit NCCN.org/RTCompendium. The compendium is available free-of-charge through March 2018. ![]()
The National Comprehensive Cancer Network® (NCCN) has announced the release of the newly completed NCCN Radiation Therapy Compendium™.
This resource includes information designed to support clinical decision-making regarding the use of radiation therapy in cancer patients.
The content is based on the NCCN Clinical Practice Guidelines in Oncology and includes information from the 41 guidelines that reference radiation therapy.
“By compiling every recommendation for radiation therapy in one place, we’ve made it significantly easier for specialists . . . to stay up-to-date on the very latest recommendations, regardless of how many different cancer types they treat,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“This targeted content provides radiation oncologists with the specific, cutting-edge information they need, without forcing them to sift through any extraneous information. It’s part of our ongoing effort to always provide the most pertinent data on emerging treatment practices in the clearest, most efficient way possible.”
The NCCN Radiation Therapy Compendium includes a full complement of radiation therapy recommendations found in the current NCCN guidelines, including specific treatment modalities such as 2D/3D conformal external beam radiation therapy, intensity modulated radiation therapy, intra-operative radiation therapy, stereotactic radiosurgery/stereotactic body radiotherapy/stereotactic ablative body radiotherapy, image-guided radiation therapy, low dose-rate/high dose-rate brachytherapy, radioisotope, and particle therapy.
NCCN first announced the launch of the Radiation Therapy Compendium in March at the NCCN Annual Conference: Improving the Quality, Effectiveness, and Efficiency of Cancer Care.
At the time, the NCCN released a preliminary version of the compendium featuring 24 cancer types. The newly completed version now contains all 41 disease sites that are currently being treated using radiation therapy.
The compendium will be updated on a continual basis in conjunction with the library of clinical guidelines.
For more information and to access the NCCN Radiation Therapy Compendium, visit NCCN.org/RTCompendium. The compendium is available free-of-charge through March 2018. ![]()
The National Comprehensive Cancer Network® (NCCN) has announced the release of the newly completed NCCN Radiation Therapy Compendium™.
This resource includes information designed to support clinical decision-making regarding the use of radiation therapy in cancer patients.
The content is based on the NCCN Clinical Practice Guidelines in Oncology and includes information from the 41 guidelines that reference radiation therapy.
“By compiling every recommendation for radiation therapy in one place, we’ve made it significantly easier for specialists . . . to stay up-to-date on the very latest recommendations, regardless of how many different cancer types they treat,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“This targeted content provides radiation oncologists with the specific, cutting-edge information they need, without forcing them to sift through any extraneous information. It’s part of our ongoing effort to always provide the most pertinent data on emerging treatment practices in the clearest, most efficient way possible.”
The NCCN Radiation Therapy Compendium includes a full complement of radiation therapy recommendations found in the current NCCN guidelines, including specific treatment modalities such as 2D/3D conformal external beam radiation therapy, intensity modulated radiation therapy, intra-operative radiation therapy, stereotactic radiosurgery/stereotactic body radiotherapy/stereotactic ablative body radiotherapy, image-guided radiation therapy, low dose-rate/high dose-rate brachytherapy, radioisotope, and particle therapy.
NCCN first announced the launch of the Radiation Therapy Compendium in March at the NCCN Annual Conference: Improving the Quality, Effectiveness, and Efficiency of Cancer Care.
At the time, the NCCN released a preliminary version of the compendium featuring 24 cancer types. The newly completed version now contains all 41 disease sites that are currently being treated using radiation therapy.
The compendium will be updated on a continual basis in conjunction with the library of clinical guidelines.
For more information and to access the NCCN Radiation Therapy Compendium, visit NCCN.org/RTCompendium. The compendium is available free-of-charge through March 2018. ![]()
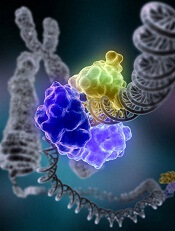
Predicting neurotoxicity after CAR T-cell therapy
Researchers say they have identified potential biomarkers that may be used to help identify patients at an increased risk of neurotoxicity after chimeric antigen receptor (CAR) T-cell therapy.
The team also created an algorithm intended to identify patients whose symptoms were most likely to be life-threatening.
The researchers discovered the biomarkers and developed the algorithm based on data from a trial of JCAR014, an anti-CD19 CAR T-cell therapy, in patients with B-cell malignancies.
Cameron J. Turtle, MBBS, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues described this research in Cancer Discovery.
“It’s essential that we understand the potential side effects of CAR T therapies” Dr Turtle said. “While use of these cell therapies is likely to dramatically increase because they’ve been so effective in patients with resistant or refractory B-cell malignancies, there is still much to learn.”
Dr Turtle and his colleagues sought to provide a detailed clinical, radiological, and pathological characterization of neurotoxicity arising from anti-CD19 CAR T-cell therapy.
So the team analyzed data from a phase 1/2 trial of 133 adults with relapsed and/or refractory CD19+ B-cell acute lymphoblastic leukemia, non-Hodgkin lymphoma, or chronic lymphocytic leukemia.
The patients received lymphodepleting chemotherapy followed by an infusion of JCAR014.
Neurotoxicity
Within 28 days of treatment, 53 patients (40%) developed grade 1 or higher neurologic adverse events (AEs), 28 patients (21%) had grade 3 or higher neurotoxicity, and 4 patients (3%) developed fatal neurotoxicity.
Of the 53 patients with any neurologic AE, 48 (91%) also had cytokine release syndrome (CRS). All neurologic AEs in the 5 patients who did not have CRS were mild (grade 1) and transient.
Neurologic AEs included delirium with preserved alertness (66%), headache (55%), language disturbance (34%), decreased level of consciousness (25%), seizures (8%), and macroscopic intracranial hemorrhage (2%).
For most patients, neurotoxicity resolved by day 28 after CAR T-cell infusion. The exceptions were 1 patient in whom a grade 1 neurologic AE resolved 2 months after CAR T-cell infusion and the 4 patients who died of neurotoxicity.
The 4 neurotoxicity-related deaths were due to:
- Acute cerebral edema (n=2)
- Multifocal brainstem hemorrhage and edema associated with disseminated intravascular coagulation (n=1)
- Cortical laminar necrosis with a persistent minimally conscious state until death (n=1).
Potential biomarkers
In a univariate analysis, neurotoxicity was significantly more frequent in patients who:
- Had CRS (P<0.0001)
- Received a high CAR T-cell dose (P<0.0001)
- Had pre-existing neurologic comorbidities at baseline (P=0.0059).
In a multivariable analysis (which did not include CRS as a variable), patients had an increased risk of neurotoxicity if they:
- Had pre-existing neurologic comorbidities (P=0.0023)
- Received cyclophosphamide and fludarabine lymphodepletion (P=0.0259)
- Received a higher CAR T-cell dose (P=0.0009)
- Had a higher burden of malignant CD19+ B cells in the bone marrow (P=0.0165).
The researchers noted that patients who developed grade 3 or higher neurotoxicity had more severe CRS (P<0.0001).
“It appears that cytokine release syndrome is probably necessary for most cases of severe neurotoxicity, but, in terms of what triggers a person with cytokine release syndrome to get neurotoxicity, that’s something we need to investigate further,” said study author Kevin Hay, MD, of Fred Hutchinson Cancer Research Center.
Dr Hay and his colleagues also found that patients with severe neurotoxicity exhibited evidence of endothelial activation, which could contribute to manifestations such as capillary leak, disseminated intravascular coagulation, and disruption of the blood-brain barrier.
Algorithm
The researchers developed a predictive classification tree algorithm to identify patients who have an increased risk of severe neurotoxicity.
The algorithm suggests patients who meet the following criteria in the first 36 hours after CAR T-cell infusion have a high risk of grade 4-5 neurotoxicity:
- Fever of 38.9°C or greater
- Serum levels of IL6 at 16 pg/mL or higher
- Serum levels of MCP1 at 1343.5 pg/mL or higher.
This algorithm predicted severe neurotoxicity with 100% sensitivity and 94% specificity. Eight patients were misclassified, 1 of whom did not subsequently develop grade 2-3 neurotoxicity and/or grade 2 or higher CRS.
Funding
This research was funded by Juno Therapeutics Inc. (the company developing JCAR014), the National Cancer Institute, Life Science Discovery Fund, the Bezos family, the University of British Columbia Clinical Investigator Program, and via institutional funds from Bloodworks Northwest.
Dr Turtle receives research funding from Juno Therapeutics, holds patents licensed by Juno, and has pending patent applications that could be licensed by nonprofit institutions and for-profit companies, including Juno.
The Fred Hutchinson Cancer Research Center has a financial interest in Juno and receives licensing and other payments from the company. ![]()
Researchers say they have identified potential biomarkers that may be used to help identify patients at an increased risk of neurotoxicity after chimeric antigen receptor (CAR) T-cell therapy.
The team also created an algorithm intended to identify patients whose symptoms were most likely to be life-threatening.
The researchers discovered the biomarkers and developed the algorithm based on data from a trial of JCAR014, an anti-CD19 CAR T-cell therapy, in patients with B-cell malignancies.
Cameron J. Turtle, MBBS, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues described this research in Cancer Discovery.
“It’s essential that we understand the potential side effects of CAR T therapies” Dr Turtle said. “While use of these cell therapies is likely to dramatically increase because they’ve been so effective in patients with resistant or refractory B-cell malignancies, there is still much to learn.”
Dr Turtle and his colleagues sought to provide a detailed clinical, radiological, and pathological characterization of neurotoxicity arising from anti-CD19 CAR T-cell therapy.
So the team analyzed data from a phase 1/2 trial of 133 adults with relapsed and/or refractory CD19+ B-cell acute lymphoblastic leukemia, non-Hodgkin lymphoma, or chronic lymphocytic leukemia.
The patients received lymphodepleting chemotherapy followed by an infusion of JCAR014.
Neurotoxicity
Within 28 days of treatment, 53 patients (40%) developed grade 1 or higher neurologic adverse events (AEs), 28 patients (21%) had grade 3 or higher neurotoxicity, and 4 patients (3%) developed fatal neurotoxicity.
Of the 53 patients with any neurologic AE, 48 (91%) also had cytokine release syndrome (CRS). All neurologic AEs in the 5 patients who did not have CRS were mild (grade 1) and transient.
Neurologic AEs included delirium with preserved alertness (66%), headache (55%), language disturbance (34%), decreased level of consciousness (25%), seizures (8%), and macroscopic intracranial hemorrhage (2%).
For most patients, neurotoxicity resolved by day 28 after CAR T-cell infusion. The exceptions were 1 patient in whom a grade 1 neurologic AE resolved 2 months after CAR T-cell infusion and the 4 patients who died of neurotoxicity.
The 4 neurotoxicity-related deaths were due to:
- Acute cerebral edema (n=2)
- Multifocal brainstem hemorrhage and edema associated with disseminated intravascular coagulation (n=1)
- Cortical laminar necrosis with a persistent minimally conscious state until death (n=1).
Potential biomarkers
In a univariate analysis, neurotoxicity was significantly more frequent in patients who:
- Had CRS (P<0.0001)
- Received a high CAR T-cell dose (P<0.0001)
- Had pre-existing neurologic comorbidities at baseline (P=0.0059).
In a multivariable analysis (which did not include CRS as a variable), patients had an increased risk of neurotoxicity if they:
- Had pre-existing neurologic comorbidities (P=0.0023)
- Received cyclophosphamide and fludarabine lymphodepletion (P=0.0259)
- Received a higher CAR T-cell dose (P=0.0009)
- Had a higher burden of malignant CD19+ B cells in the bone marrow (P=0.0165).
The researchers noted that patients who developed grade 3 or higher neurotoxicity had more severe CRS (P<0.0001).
“It appears that cytokine release syndrome is probably necessary for most cases of severe neurotoxicity, but, in terms of what triggers a person with cytokine release syndrome to get neurotoxicity, that’s something we need to investigate further,” said study author Kevin Hay, MD, of Fred Hutchinson Cancer Research Center.
Dr Hay and his colleagues also found that patients with severe neurotoxicity exhibited evidence of endothelial activation, which could contribute to manifestations such as capillary leak, disseminated intravascular coagulation, and disruption of the blood-brain barrier.
Algorithm
The researchers developed a predictive classification tree algorithm to identify patients who have an increased risk of severe neurotoxicity.
The algorithm suggests patients who meet the following criteria in the first 36 hours after CAR T-cell infusion have a high risk of grade 4-5 neurotoxicity:
- Fever of 38.9°C or greater
- Serum levels of IL6 at 16 pg/mL or higher
- Serum levels of MCP1 at 1343.5 pg/mL or higher.
This algorithm predicted severe neurotoxicity with 100% sensitivity and 94% specificity. Eight patients were misclassified, 1 of whom did not subsequently develop grade 2-3 neurotoxicity and/or grade 2 or higher CRS.
Funding
This research was funded by Juno Therapeutics Inc. (the company developing JCAR014), the National Cancer Institute, Life Science Discovery Fund, the Bezos family, the University of British Columbia Clinical Investigator Program, and via institutional funds from Bloodworks Northwest.
Dr Turtle receives research funding from Juno Therapeutics, holds patents licensed by Juno, and has pending patent applications that could be licensed by nonprofit institutions and for-profit companies, including Juno.
The Fred Hutchinson Cancer Research Center has a financial interest in Juno and receives licensing and other payments from the company. ![]()
Researchers say they have identified potential biomarkers that may be used to help identify patients at an increased risk of neurotoxicity after chimeric antigen receptor (CAR) T-cell therapy.
The team also created an algorithm intended to identify patients whose symptoms were most likely to be life-threatening.
The researchers discovered the biomarkers and developed the algorithm based on data from a trial of JCAR014, an anti-CD19 CAR T-cell therapy, in patients with B-cell malignancies.
Cameron J. Turtle, MBBS, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues described this research in Cancer Discovery.
“It’s essential that we understand the potential side effects of CAR T therapies” Dr Turtle said. “While use of these cell therapies is likely to dramatically increase because they’ve been so effective in patients with resistant or refractory B-cell malignancies, there is still much to learn.”
Dr Turtle and his colleagues sought to provide a detailed clinical, radiological, and pathological characterization of neurotoxicity arising from anti-CD19 CAR T-cell therapy.
So the team analyzed data from a phase 1/2 trial of 133 adults with relapsed and/or refractory CD19+ B-cell acute lymphoblastic leukemia, non-Hodgkin lymphoma, or chronic lymphocytic leukemia.
The patients received lymphodepleting chemotherapy followed by an infusion of JCAR014.
Neurotoxicity
Within 28 days of treatment, 53 patients (40%) developed grade 1 or higher neurologic adverse events (AEs), 28 patients (21%) had grade 3 or higher neurotoxicity, and 4 patients (3%) developed fatal neurotoxicity.
Of the 53 patients with any neurologic AE, 48 (91%) also had cytokine release syndrome (CRS). All neurologic AEs in the 5 patients who did not have CRS were mild (grade 1) and transient.
Neurologic AEs included delirium with preserved alertness (66%), headache (55%), language disturbance (34%), decreased level of consciousness (25%), seizures (8%), and macroscopic intracranial hemorrhage (2%).
For most patients, neurotoxicity resolved by day 28 after CAR T-cell infusion. The exceptions were 1 patient in whom a grade 1 neurologic AE resolved 2 months after CAR T-cell infusion and the 4 patients who died of neurotoxicity.
The 4 neurotoxicity-related deaths were due to:
- Acute cerebral edema (n=2)
- Multifocal brainstem hemorrhage and edema associated with disseminated intravascular coagulation (n=1)
- Cortical laminar necrosis with a persistent minimally conscious state until death (n=1).
Potential biomarkers
In a univariate analysis, neurotoxicity was significantly more frequent in patients who:
- Had CRS (P<0.0001)
- Received a high CAR T-cell dose (P<0.0001)
- Had pre-existing neurologic comorbidities at baseline (P=0.0059).
In a multivariable analysis (which did not include CRS as a variable), patients had an increased risk of neurotoxicity if they:
- Had pre-existing neurologic comorbidities (P=0.0023)
- Received cyclophosphamide and fludarabine lymphodepletion (P=0.0259)
- Received a higher CAR T-cell dose (P=0.0009)
- Had a higher burden of malignant CD19+ B cells in the bone marrow (P=0.0165).
The researchers noted that patients who developed grade 3 or higher neurotoxicity had more severe CRS (P<0.0001).
“It appears that cytokine release syndrome is probably necessary for most cases of severe neurotoxicity, but, in terms of what triggers a person with cytokine release syndrome to get neurotoxicity, that’s something we need to investigate further,” said study author Kevin Hay, MD, of Fred Hutchinson Cancer Research Center.
Dr Hay and his colleagues also found that patients with severe neurotoxicity exhibited evidence of endothelial activation, which could contribute to manifestations such as capillary leak, disseminated intravascular coagulation, and disruption of the blood-brain barrier.
Algorithm
The researchers developed a predictive classification tree algorithm to identify patients who have an increased risk of severe neurotoxicity.
The algorithm suggests patients who meet the following criteria in the first 36 hours after CAR T-cell infusion have a high risk of grade 4-5 neurotoxicity:
- Fever of 38.9°C or greater
- Serum levels of IL6 at 16 pg/mL or higher
- Serum levels of MCP1 at 1343.5 pg/mL or higher.
This algorithm predicted severe neurotoxicity with 100% sensitivity and 94% specificity. Eight patients were misclassified, 1 of whom did not subsequently develop grade 2-3 neurotoxicity and/or grade 2 or higher CRS.
Funding
This research was funded by Juno Therapeutics Inc. (the company developing JCAR014), the National Cancer Institute, Life Science Discovery Fund, the Bezos family, the University of British Columbia Clinical Investigator Program, and via institutional funds from Bloodworks Northwest.
Dr Turtle receives research funding from Juno Therapeutics, holds patents licensed by Juno, and has pending patent applications that could be licensed by nonprofit institutions and for-profit companies, including Juno.
The Fred Hutchinson Cancer Research Center has a financial interest in Juno and receives licensing and other payments from the company. ![]()
ALL therapies grow, so do the complexities of choosing the order of treatments
SAN FRANCISCO – A growing number of immunotherapy options for adults with acute lymphocytic leukemia (ALL) – rituximab, inotuzumab ozogamicin, blinatumomab and chimeric antigen receptor (CAR) T-cell therapy – have improved remission rates, but their collective effects on patient outcomes remain to be seen, David Maloney, MD, PhD, said at the National Comprehensive Cancer Network Annual Congress: Hematologic Malignancies.
The main challenge for the field is deciding when and how to use a variety of therapies, he said. “How are we going to put these together? What’s the order?” he asked. “Are we going to be able to decrease the need for allogeneic stem cell transplant? And, obviously, that’s the goal.”
About 30%-50% of adults with ALL exhibit CD20-positive cells, making them potentially treatable with rituximab. Data show a better event-free survival rate and a reduced relapse rate when rituximab is added to standard chemotherapy as compared with standard chemotherapy alone, Dr. Maloney of the clinical research division at the Fred Hutchinson Cancer Research Center, Seattle, noted (N Engl J Med. 2016 Sep 15;375[11]:1044-53). But the improvement was only “modest,” he said.
The anti-CD22 antibody inotuzumab ozogamicin has produced complete remission in 81% of relapsed or refractory ALL patients, compared with those getting standard therapy (N Engl J Med. 2016 Aug 25;375:740-53). Dr. Maloney said it seems well tolerated, but there is concern about an increase in veno-occlusive disease in patients who have undergone or will undergo an allogeneic stem cell transplant.
Blinatumomab produces moderate response rates and minimal residual disease–negative remissions, but delivery of the drug is “cumbersome,” requiring a 4-week continuous infusion, he said. The drug seems to be more effective in those with a lower burden of disease, he noted.
CAR T-cell therapy has produced MRD-negative complete responses in 94% of patients, based on results from a clinical trial at Fred Hutchinson. And using the chemotherapy drug fludarabine in combination with this therapy “dramatically” boosts the peak number of the CAR T cells and how long they persist, Dr. Maloney said. Still, CAR T-cell therapy is a work-intensive treatment requiring cells harvested from the patient, and the procedure often brings on cytokine-release syndrome and neurotoxicity, though both adverse events are typically reversible, he said.
It may be that using fewer CAR T cells can reduce toxicity without compromising treatment response, he said.
Questions remain over whether to transplant patients who are in remission after CAR T-cell therapy. “This is a hot debate,” he said. The decision will likely depend on their prior therapy, whether they’ve had a prior transplant, and the how robust the CAR T-cell expansion has been, he said.
Dr. Maloney reports financial relationships with Celgene, Gilead Sciences, Kite Pharma, and Roche.
SAN FRANCISCO – A growing number of immunotherapy options for adults with acute lymphocytic leukemia (ALL) – rituximab, inotuzumab ozogamicin, blinatumomab and chimeric antigen receptor (CAR) T-cell therapy – have improved remission rates, but their collective effects on patient outcomes remain to be seen, David Maloney, MD, PhD, said at the National Comprehensive Cancer Network Annual Congress: Hematologic Malignancies.
The main challenge for the field is deciding when and how to use a variety of therapies, he said. “How are we going to put these together? What’s the order?” he asked. “Are we going to be able to decrease the need for allogeneic stem cell transplant? And, obviously, that’s the goal.”
About 30%-50% of adults with ALL exhibit CD20-positive cells, making them potentially treatable with rituximab. Data show a better event-free survival rate and a reduced relapse rate when rituximab is added to standard chemotherapy as compared with standard chemotherapy alone, Dr. Maloney of the clinical research division at the Fred Hutchinson Cancer Research Center, Seattle, noted (N Engl J Med. 2016 Sep 15;375[11]:1044-53). But the improvement was only “modest,” he said.
The anti-CD22 antibody inotuzumab ozogamicin has produced complete remission in 81% of relapsed or refractory ALL patients, compared with those getting standard therapy (N Engl J Med. 2016 Aug 25;375:740-53). Dr. Maloney said it seems well tolerated, but there is concern about an increase in veno-occlusive disease in patients who have undergone or will undergo an allogeneic stem cell transplant.
Blinatumomab produces moderate response rates and minimal residual disease–negative remissions, but delivery of the drug is “cumbersome,” requiring a 4-week continuous infusion, he said. The drug seems to be more effective in those with a lower burden of disease, he noted.
CAR T-cell therapy has produced MRD-negative complete responses in 94% of patients, based on results from a clinical trial at Fred Hutchinson. And using the chemotherapy drug fludarabine in combination with this therapy “dramatically” boosts the peak number of the CAR T cells and how long they persist, Dr. Maloney said. Still, CAR T-cell therapy is a work-intensive treatment requiring cells harvested from the patient, and the procedure often brings on cytokine-release syndrome and neurotoxicity, though both adverse events are typically reversible, he said.
It may be that using fewer CAR T cells can reduce toxicity without compromising treatment response, he said.
Questions remain over whether to transplant patients who are in remission after CAR T-cell therapy. “This is a hot debate,” he said. The decision will likely depend on their prior therapy, whether they’ve had a prior transplant, and the how robust the CAR T-cell expansion has been, he said.
Dr. Maloney reports financial relationships with Celgene, Gilead Sciences, Kite Pharma, and Roche.
SAN FRANCISCO – A growing number of immunotherapy options for adults with acute lymphocytic leukemia (ALL) – rituximab, inotuzumab ozogamicin, blinatumomab and chimeric antigen receptor (CAR) T-cell therapy – have improved remission rates, but their collective effects on patient outcomes remain to be seen, David Maloney, MD, PhD, said at the National Comprehensive Cancer Network Annual Congress: Hematologic Malignancies.
The main challenge for the field is deciding when and how to use a variety of therapies, he said. “How are we going to put these together? What’s the order?” he asked. “Are we going to be able to decrease the need for allogeneic stem cell transplant? And, obviously, that’s the goal.”
About 30%-50% of adults with ALL exhibit CD20-positive cells, making them potentially treatable with rituximab. Data show a better event-free survival rate and a reduced relapse rate when rituximab is added to standard chemotherapy as compared with standard chemotherapy alone, Dr. Maloney of the clinical research division at the Fred Hutchinson Cancer Research Center, Seattle, noted (N Engl J Med. 2016 Sep 15;375[11]:1044-53). But the improvement was only “modest,” he said.
The anti-CD22 antibody inotuzumab ozogamicin has produced complete remission in 81% of relapsed or refractory ALL patients, compared with those getting standard therapy (N Engl J Med. 2016 Aug 25;375:740-53). Dr. Maloney said it seems well tolerated, but there is concern about an increase in veno-occlusive disease in patients who have undergone or will undergo an allogeneic stem cell transplant.
Blinatumomab produces moderate response rates and minimal residual disease–negative remissions, but delivery of the drug is “cumbersome,” requiring a 4-week continuous infusion, he said. The drug seems to be more effective in those with a lower burden of disease, he noted.
CAR T-cell therapy has produced MRD-negative complete responses in 94% of patients, based on results from a clinical trial at Fred Hutchinson. And using the chemotherapy drug fludarabine in combination with this therapy “dramatically” boosts the peak number of the CAR T cells and how long they persist, Dr. Maloney said. Still, CAR T-cell therapy is a work-intensive treatment requiring cells harvested from the patient, and the procedure often brings on cytokine-release syndrome and neurotoxicity, though both adverse events are typically reversible, he said.
It may be that using fewer CAR T cells can reduce toxicity without compromising treatment response, he said.
Questions remain over whether to transplant patients who are in remission after CAR T-cell therapy. “This is a hot debate,” he said. The decision will likely depend on their prior therapy, whether they’ve had a prior transplant, and the how robust the CAR T-cell expansion has been, he said.
Dr. Maloney reports financial relationships with Celgene, Gilead Sciences, Kite Pharma, and Roche.
EXPERT ANALYSIS FROM THE NCCN ANNUAL CONGRESS: HEMATOLOGIC MALIGNANCIES
Newer blood cancer drugs may not improve OS, QOL
A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

Team discovers oncogenic driver of T-ALL
Preclinical research suggests the TOX protein is an oncogenic driver of T-cell acute lymphoblastic leukemia (T-ALL).
Results indicate that TOX may be expressed in as many as 95% of human T-ALL cases, and the protein is required for the cancer’s growth and persistence.
“A major role for TOX in T-ALL is to elicit defects in DNA repair, leading to genetic changes that drive normal cells into cancer,” said study author David Langenau, PhD, of Massachusetts General Hospital in Boston.
“TOX then continues to be expressed within leukemic cells and is required for continued tumor growth. That means that, if we can successfully target TOX with small molecules in the future, the 95% of T-ALL patients whose tumors express TOX would have new treatment options for this aggressive leukemia.”
Dr Langenau and his colleagues described this new role for TOX in Cancer Discovery.
The team noted that T-ALL has several molecular subtypes, many of which are driven by common oncogenes such as MYC and NOTCH. However, evidence has suggested the cancer’s initiation is likely driven by aberrations in DNA repair.
To identify genes that might help drive T-ALL, the researchers performed a transgenic screen in zebrafish.
The team found that TOX collaborates with known oncogene pathways to transform T-cell precursors into leukemia cells by altering DNA repair and then expanding the population of transformed cells.
In human T-ALL cells, TOX was shown to suppress non-homologous end joining (NHEJ) repair, a pathway required for repairing double-strand DNA breaks that, when disrupted, is known to cause errant DNA repair and genomic instability.
Nearly all of the human T-ALL samples the researchers tested were found to express TOX. And TOX proved essential for the proliferation and survival of T-ALL.
Dr Langenau explained that TOX is known to have important roles in the development and maturation of several types of immune cells, yet its roles in leukemia initiation and genomic instability were not described until this work.
TOX belongs to a group of proteins known to regulate the configuration or expression of genes by binding to DNA molecules, yet its mechanism in T-ALL—blocking NHEJ repair by binding to DNA repair proteins rather than directly to DNA—was totally unexpected.
The researchers believe that, in addition to better understanding how TOX regulates the continued growth of T-ALL, it will be important to determine whether related proteins have similar molecular functions in other cancers. ![]()
Preclinical research suggests the TOX protein is an oncogenic driver of T-cell acute lymphoblastic leukemia (T-ALL).
Results indicate that TOX may be expressed in as many as 95% of human T-ALL cases, and the protein is required for the cancer’s growth and persistence.
“A major role for TOX in T-ALL is to elicit defects in DNA repair, leading to genetic changes that drive normal cells into cancer,” said study author David Langenau, PhD, of Massachusetts General Hospital in Boston.
“TOX then continues to be expressed within leukemic cells and is required for continued tumor growth. That means that, if we can successfully target TOX with small molecules in the future, the 95% of T-ALL patients whose tumors express TOX would have new treatment options for this aggressive leukemia.”
Dr Langenau and his colleagues described this new role for TOX in Cancer Discovery.
The team noted that T-ALL has several molecular subtypes, many of which are driven by common oncogenes such as MYC and NOTCH. However, evidence has suggested the cancer’s initiation is likely driven by aberrations in DNA repair.
To identify genes that might help drive T-ALL, the researchers performed a transgenic screen in zebrafish.
The team found that TOX collaborates with known oncogene pathways to transform T-cell precursors into leukemia cells by altering DNA repair and then expanding the population of transformed cells.
In human T-ALL cells, TOX was shown to suppress non-homologous end joining (NHEJ) repair, a pathway required for repairing double-strand DNA breaks that, when disrupted, is known to cause errant DNA repair and genomic instability.
Nearly all of the human T-ALL samples the researchers tested were found to express TOX. And TOX proved essential for the proliferation and survival of T-ALL.
Dr Langenau explained that TOX is known to have important roles in the development and maturation of several types of immune cells, yet its roles in leukemia initiation and genomic instability were not described until this work.
TOX belongs to a group of proteins known to regulate the configuration or expression of genes by binding to DNA molecules, yet its mechanism in T-ALL—blocking NHEJ repair by binding to DNA repair proteins rather than directly to DNA—was totally unexpected.
The researchers believe that, in addition to better understanding how TOX regulates the continued growth of T-ALL, it will be important to determine whether related proteins have similar molecular functions in other cancers. ![]()
Preclinical research suggests the TOX protein is an oncogenic driver of T-cell acute lymphoblastic leukemia (T-ALL).
Results indicate that TOX may be expressed in as many as 95% of human T-ALL cases, and the protein is required for the cancer’s growth and persistence.
“A major role for TOX in T-ALL is to elicit defects in DNA repair, leading to genetic changes that drive normal cells into cancer,” said study author David Langenau, PhD, of Massachusetts General Hospital in Boston.
“TOX then continues to be expressed within leukemic cells and is required for continued tumor growth. That means that, if we can successfully target TOX with small molecules in the future, the 95% of T-ALL patients whose tumors express TOX would have new treatment options for this aggressive leukemia.”
Dr Langenau and his colleagues described this new role for TOX in Cancer Discovery.
The team noted that T-ALL has several molecular subtypes, many of which are driven by common oncogenes such as MYC and NOTCH. However, evidence has suggested the cancer’s initiation is likely driven by aberrations in DNA repair.
To identify genes that might help drive T-ALL, the researchers performed a transgenic screen in zebrafish.
The team found that TOX collaborates with known oncogene pathways to transform T-cell precursors into leukemia cells by altering DNA repair and then expanding the population of transformed cells.
In human T-ALL cells, TOX was shown to suppress non-homologous end joining (NHEJ) repair, a pathway required for repairing double-strand DNA breaks that, when disrupted, is known to cause errant DNA repair and genomic instability.
Nearly all of the human T-ALL samples the researchers tested were found to express TOX. And TOX proved essential for the proliferation and survival of T-ALL.
Dr Langenau explained that TOX is known to have important roles in the development and maturation of several types of immune cells, yet its roles in leukemia initiation and genomic instability were not described until this work.
TOX belongs to a group of proteins known to regulate the configuration or expression of genes by binding to DNA molecules, yet its mechanism in T-ALL—blocking NHEJ repair by binding to DNA repair proteins rather than directly to DNA—was totally unexpected.
The researchers believe that, in addition to better understanding how TOX regulates the continued growth of T-ALL, it will be important to determine whether related proteins have similar molecular functions in other cancers.
FDA grants RMAT designation to HSCT adjunct
The US Food and Drug Administration (FDA) has granted Regenerative Medicine Advanced Therapy (RMAT) designation to ATIR101™, which is intended to be used as an adjunct to haploidentical hematopoietic stem cell transplant (HSCT).
ATIR101 is a personalized T-cell immunotherapy—a donor lymphocyte preparation selectively depleted of host-alloreactive T cells through the use of photo-dynamic therapy.
Recipient-reactive T cells from the donor are activated in a unidirectional mixed-lymphocyte reaction. The cells are then treated with TH9402 (a rhodamide-like dye), which is selectively retained in activated T cells.
Subsequent light exposure eliminates the activated recipient-reactive T cells but preserves the other T cells.
The final product is infused after CD34-selected haploidentical HSCT with the goal of preventing infectious complications, graft-versus-host disease (GVHD), and relapse.
About RMAT designation
The RMAT pathway is analogous to the breakthrough therapy designation designed for traditional drug candidates and medical devices. RMAT designation was specifically created by the US Congress in 2016 in the hopes of getting new cell therapies and advanced medicinal products to patients earlier.
Just like breakthrough designation, RMAT designation allows companies developing regenerative medicine therapies to interact with the FDA more frequently in the clinical testing process. In addition, RMAT-designated products may be eligible for priority review and accelerated approval.
A regenerative medicine is eligible for RMAT designation if it is intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition, and if preliminary clinical evidence indicates the treatment has the potential to address unmet medical needs for such a disease or condition.
“To receive the RMAT designation from the FDA is an important milestone for Kiadis Pharma and a recognition by the FDA of the significant potential for ATIR101 to help patients receive safer and more effective bone marrow transplantations,” said Arthur Lahr, CEO of Kiadis Pharma, the company developing ATIR101.
“We are now going to work even closer with the FDA to agree a path to make this cell therapy treatment available for patients in the US as soon as possible. In Europe, ATIR101 was filed for registration in April 2017, and we continue to prepare the company for the potential European launch in 2019.”
ATIR101 trials
Results of a phase 2 trial of ATIR101 were presented at the 42nd Annual Meeting of the European Society of Blood and Marrow Transplantation in 2016.
Patients who received ATIR101 after haploidentical HSCT had significant improvements in transplant-related mortality and overall survival when compared to historical controls who received a T-cell-depleted haploidentical HSCT without ATIR101.
None of the patients who received ATIR101 developed grade 3-4 GVHD, but a few patients did develop grade 2 GVHD.
A phase 3 trial of ATIR101 is now underway. The trial is expected to enroll 200 patients with acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndrome.
The patients will receive a haploidentical HSCT with either a T-cell-depleted graft and adjunctive treatment with ATIR101 or a T-cell-replete graft and post-transplant cyclophosphamide.
The US Food and Drug Administration (FDA) has granted Regenerative Medicine Advanced Therapy (RMAT) designation to ATIR101™, which is intended to be used as an adjunct to haploidentical hematopoietic stem cell transplant (HSCT).
ATIR101 is a personalized T-cell immunotherapy—a donor lymphocyte preparation selectively depleted of host-alloreactive T cells through the use of photo-dynamic therapy.
Recipient-reactive T cells from the donor are activated in a unidirectional mixed-lymphocyte reaction. The cells are then treated with TH9402 (a rhodamide-like dye), which is selectively retained in activated T cells.
Subsequent light exposure eliminates the activated recipient-reactive T cells but preserves the other T cells.
The final product is infused after CD34-selected haploidentical HSCT with the goal of preventing infectious complications, graft-versus-host disease (GVHD), and relapse.
About RMAT designation
The RMAT pathway is analogous to the breakthrough therapy designation designed for traditional drug candidates and medical devices. RMAT designation was specifically created by the US Congress in 2016 in the hopes of getting new cell therapies and advanced medicinal products to patients earlier.
Just like breakthrough designation, RMAT designation allows companies developing regenerative medicine therapies to interact with the FDA more frequently in the clinical testing process. In addition, RMAT-designated products may be eligible for priority review and accelerated approval.
A regenerative medicine is eligible for RMAT designation if it is intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition, and if preliminary clinical evidence indicates the treatment has the potential to address unmet medical needs for such a disease or condition.
“To receive the RMAT designation from the FDA is an important milestone for Kiadis Pharma and a recognition by the FDA of the significant potential for ATIR101 to help patients receive safer and more effective bone marrow transplantations,” said Arthur Lahr, CEO of Kiadis Pharma, the company developing ATIR101.
“We are now going to work even closer with the FDA to agree a path to make this cell therapy treatment available for patients in the US as soon as possible. In Europe, ATIR101 was filed for registration in April 2017, and we continue to prepare the company for the potential European launch in 2019.”
ATIR101 trials
Results of a phase 2 trial of ATIR101 were presented at the 42nd Annual Meeting of the European Society of Blood and Marrow Transplantation in 2016.
Patients who received ATIR101 after haploidentical HSCT had significant improvements in transplant-related mortality and overall survival when compared to historical controls who received a T-cell-depleted haploidentical HSCT without ATIR101.
None of the patients who received ATIR101 developed grade 3-4 GVHD, but a few patients did develop grade 2 GVHD.
A phase 3 trial of ATIR101 is now underway. The trial is expected to enroll 200 patients with acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndrome.
The patients will receive a haploidentical HSCT with either a T-cell-depleted graft and adjunctive treatment with ATIR101 or a T-cell-replete graft and post-transplant cyclophosphamide.
The US Food and Drug Administration (FDA) has granted Regenerative Medicine Advanced Therapy (RMAT) designation to ATIR101™, which is intended to be used as an adjunct to haploidentical hematopoietic stem cell transplant (HSCT).
ATIR101 is a personalized T-cell immunotherapy—a donor lymphocyte preparation selectively depleted of host-alloreactive T cells through the use of photo-dynamic therapy.
Recipient-reactive T cells from the donor are activated in a unidirectional mixed-lymphocyte reaction. The cells are then treated with TH9402 (a rhodamide-like dye), which is selectively retained in activated T cells.
Subsequent light exposure eliminates the activated recipient-reactive T cells but preserves the other T cells.
The final product is infused after CD34-selected haploidentical HSCT with the goal of preventing infectious complications, graft-versus-host disease (GVHD), and relapse.
About RMAT designation
The RMAT pathway is analogous to the breakthrough therapy designation designed for traditional drug candidates and medical devices. RMAT designation was specifically created by the US Congress in 2016 in the hopes of getting new cell therapies and advanced medicinal products to patients earlier.
Just like breakthrough designation, RMAT designation allows companies developing regenerative medicine therapies to interact with the FDA more frequently in the clinical testing process. In addition, RMAT-designated products may be eligible for priority review and accelerated approval.
A regenerative medicine is eligible for RMAT designation if it is intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition, and if preliminary clinical evidence indicates the treatment has the potential to address unmet medical needs for such a disease or condition.
“To receive the RMAT designation from the FDA is an important milestone for Kiadis Pharma and a recognition by the FDA of the significant potential for ATIR101 to help patients receive safer and more effective bone marrow transplantations,” said Arthur Lahr, CEO of Kiadis Pharma, the company developing ATIR101.
“We are now going to work even closer with the FDA to agree a path to make this cell therapy treatment available for patients in the US as soon as possible. In Europe, ATIR101 was filed for registration in April 2017, and we continue to prepare the company for the potential European launch in 2019.”
ATIR101 trials
Results of a phase 2 trial of ATIR101 were presented at the 42nd Annual Meeting of the European Society of Blood and Marrow Transplantation in 2016.
Patients who received ATIR101 after haploidentical HSCT had significant improvements in transplant-related mortality and overall survival when compared to historical controls who received a T-cell-depleted haploidentical HSCT without ATIR101.
None of the patients who received ATIR101 developed grade 3-4 GVHD, but a few patients did develop grade 2 GVHD.
A phase 3 trial of ATIR101 is now underway. The trial is expected to enroll 200 patients with acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndrome.
The patients will receive a haploidentical HSCT with either a T-cell-depleted graft and adjunctive treatment with ATIR101 or a T-cell-replete graft and post-transplant cyclophosphamide.
Team creates guidelines on CAR T-cell-related toxicity
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies.
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies.
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies.