User login
Addressing the shortage of psychiatrists: What keeps us from seeing more patients?
Recently I was contacted by a reporter who wanted to speak to me about why it’s so difficult for patients to find a psychiatrist. She’d found me by Googling “Why psychiatrists don’t take insurance” and already had read an article I’d written with that title. That day, it had snowed hard enough that most of my patients had canceled; the grocery store had closed; and I had plenty of time to chat with a reporter. The other thing I noted – perhaps because other psychiatrists had unexpected free time because of the snow – was that Maryland Psychiatric Society’s listserv was getting a lot of posts. The posts focused on issues to do with maintenance of certification (MOC) or with the fact that every physician in the state was now going to be required to have a CME credit on opioid prescribing for licensure renewal, and there would be a requirement for physicians to take a course on substance abuse to renew their CDS registration. The hope is that these courses will reduce deaths caused by narcotic overdose, and the courses would be required for all physicians without regard to whether they are relevant to their practice.
The reporter and I started with a discussion of why so many psychiatrists have chosen not to accept health insurance (myself included). She then told me about an insured man who had been diagnosed with schizophrenia and substance abuse who was unable to get an appointment with a psychiatrist. She asked me an interesting question: “Don’t psychiatrists want the challenge of treating the difficult cases?” The patient in question never did find a psychiatrist in time and he ended up committing a murder then dying by suicide – an awful tragedy that highlights access to care problems.
In addition to a private practice, I have worked in community mental health centers, and I discussed how that setting is often better suited for patients with serious psychiatric illnesses. More services are offered, and having a variety of mental health professionals in the same facility promotes better coordination of care between psychiatrists, therapists, and case managers, as well as with family, residential care providers, and day programs. The problem is that demand for treatment at outpatient clinics is high, and sometimes the waits for an initial appointment are long, or clinics even may stop accepting new patients at times when they get overloaded.
We talked about the logistics and trade-offs of working in a clinic vs. a private practice, and the reasons why working full time in a high-volume clinic might lead physicians to want a change after a few years. And then the reporter asked me another interesting question – with such long waits, why don’t the clinics hire more doctors? I explained that there was a shortage of psychiatrists and began to talk with her about demands on physician time that take time away from patient care. With the e-mails flying about MOC and new course requirements, it was a place to start, but the snow was still falling, and she heard a lot about the factors that drain physician time and money, both limiting how many patients a psychiatrist can see and driving up the cost of care.
By the time I got off the phone, I decided to tally all of the things that we are required to do to see patients. I was able to get some quick help on the listserv, from friends, and on Twitter.
Every time an agency or insurance company sets up a requirement for a physician, there is a small diversion of time. There is no limit on how many different requirements can be set or whether they need to be relevant to the physician’s work. While I realize there is little sympathy for physicians who, for the most part, are still blessed to earn a good living while doing meaningful work, these diversions add hours to a doctor’s day and cause them to burn out more quickly. So the insurance company that demands that a physician devote 20 minutes to get authorization to prescribe a medication that costs pennies a pill is actually harming society. And no one oversees the big picture.
That said, here was the list we came up with of factors that drain time and money in a clinical practice. Please note that some of these items – for example, uncompensated time returning calls to patients or keeping clinical records – are just part of being a doctor; they’re not something that should be eliminated. Similarly, issues related to having a space to work are part of having a business. I wanted the list to be complete to illustrate the demands on a psychiatrist, not to suggest that none of these things are important. Obviously, some doctors are faster or slower at certain tasks, and people vary greatly in how much time they devote to clinical practice vs. teaching, research, or writing articles for Clinical Psychiatry News. I obtained information in a very quick and casual manner; none of this should be construed as scientific.
Here is the list:
• Maintenance of certification requirements and testing. This is required every 10 years and one estimate was that the cost to register, take the test, and purchase review materials came to $2,800, with a time investment of about 50 hours. Some specialties are pushing back against MOC, and some physicians are forgoing board certification. Psychiatrists who subspecialize usually do MOC for general psychiatry and all their subspecialties.
• CME. Twenty to 50 hours per year depending on your state, and presumably physicians choose courses that enrich their ability to practice medicine. This can be expensive, depending on how the physician decides to get these credits, and many valuable learning events do not qualify for CME.
• Writing clinical notes. Again, this is part of routine medical care. Notes must justify the CPT codes on insurance claims, and very specific areas of inquiry and examination are needed to justify billing specific codes. Agency requirements may be different from what is clinically indicated for the care of the patient, and this uses some of the appointment time in a way that may not be helpful to medical care. Copying, faxing, or sending notes to other clinicians and time spent requesting records all add to the mix. One psychiatrist noted that the overall administrative responsibilities for seeing patients takes half an hour for every hour spent with a patient. Others estimated that anywhere from 30 minutes to 2 hours per day are devoted to writing notes, and some mentioned doing this in the evening at home. One child psychiatrist with a large high-volume practice noted that he is required to keep charts until a patient reaches adulthood, and that storing, locating, and shredding charts was a time drain.
• Billing the patient. One private practice psychiatrist estimated this takes approximately 8 hours a month, include record-keeping and rebilling patients who failed to pay. Some psychiatrists have a secretary or billing staff.
• Patient insurance. Time spent preauthorizing care, including time spent to preauthorize hospitalizations or to justify each day of inpatient treatment. (No time estimates were offered.)
• Filing claims. The psychiatrists I spoke with who participate with insurers all had support staff to do this.
• Preauthorizing medications. This was by far the biggest complaint by psychiatrists. One noted that it had taken her 2 hours the night before to get a medication authorized; another had spent an hour that day on it. Another rough figure I got was 20-60 minutes a week, and it was noted that preauthorization often is required for very inexpensive medications. Another psychiatrist said her office manager spends a couple of hours a week on preauthorizations and that she had to give her a raise to get her to agree to do it. Personally, I feel insurance companies should not be permitted to divert physician time away from care for inexpensive medications. Does it really make sense to have a physician spend 20 minutes of uncompensated time getting authorization for a medication that costs $10 a month?
• Paperwork related to being credentialed with insurance companies. This was estimated at 40 minutes every 3 months.
• Credentialing. Cost and paperwork for malpractice insurance varies by state and, some malpractice agencies require doctors to do specific forms of training. In addition, practicing requires renewal of a DEA number, CDS renewal (in Maryland), and state licensure.
• Electronic medical records (EMR). Medicare has provided financial incentives to doctors for the meaningful use of certified electronic health record (EHR) technology to improve patient care and now penalizes doctors who do not have this technology. One psychiatrist told me that she spent hundreds of hours working on this, but something went wrong so she is still penalized. Another said she spent 3 hours in a 3-month period attesting to her compliance with meaningful use. Everyone I spoke to said using an electronic record – related to Medicare’s meaningful use or not – increased the time it takes them to write notes. One psychiatrist reduced her clinical care to 1 day a week, and I left a community clinic when the effort of learning to use EPIC overwhelmed me.
• E-prescribing. One colleague in New York wrote, “E-prescribing takes up a lot of time, especially since I don’t do it during sessions. For a noncontrolled medication, it’s maybe 4-5 minutes per prescription. For controlled, it’s 3-4 minutes more, because I have to check I-STOP and use the token, and then record the I-STOP number. And for all prescriptions, I hand write an entry in the medication record, just for backup.” She noted it took several hours to set up the system. Most psychiatrists still spend significant time calling in prescriptions that patients have forgotten to request during appointments, and pharmacists often call to have refills authorized. This can be quite time consuming, and sometimes refills are requested automatically for medications the patients no longer take, and time spent on hold can be significant. My own experience was that e-prescribing took significantly longer than paper prescribing, and that handing a patient a prescription during a session is simply part of medical care and not a “drain,” per se.
• Secretarial. No one was able to give me an estimate of how many hours per week were spent directing, managing, and training support staff, or of how many hours this freed up to see patients. One psychiatrist in a large practice noted that they have 32 full- and part-time professions, including 3 psychiatrists; they participate with insurance, and this requires 18 full-time support staff.
• Office-related issues. Rent – this is both taste and geographically driven, and there are several ways to come by office space. Other factors are time related to restocking supplies, furnishings, technological hardware, phones, faxes, pagers, mobile lines, postage, technology support, cleaning, and assorted office-related issues. I have no time estimates on this; some people have support staff who do most of it, and again, this is part of the routine practice of having a business. It takes time, but it’s not irrelevant. Also, time is spent keeping an office both OSHA and HIPAA compliant.
• Hospital/agency-related requirements:
– Risk management seminars.
– CPR training.
– Health maintenance (required TB testing and flu shot).
• Required learning modules. When I worked 4 hours a week at a hospital clinic, there were many requirements. I watched modules on how to use elevators in buildings I never entered, how to place a central line, hand-washing and infection control, and how to store chemicals I never used. I believe that Maryland state employees may be required to have training in trauma-informed-care.
• Uncompensated time returning calls/communications to patients, families, other clinicians, and prospective patients who then decide not to come in, as well as filling out paperwork for disability claims, other agencies, and writing letters for patients. While this also is part of routine medical care, several people mentioned that other professionals can bill for this work and that insurers can force unnecessary care because only face-to-face treatment gets reimbursed, so issues that might be resolved on the phone or by telepsychiatry then require an office visit.
One colleague was kind enough to examine her own full-time practice and sum up her activities. She came up with an estimate that she devoted 40 hours per month to administrative issues that divert time from seeing patients. This did not include the time she recently devoted to MOC.
Obviously, I want to make the point that part of the psychiatrist shortage is related to the fact that there are administrative demands – many that don’t improve clinical care – that decrease the number of patients we can see and increase the cost of care. In addition to the weekly toll, many of these time drains are frustrating, and serve as disincentives to seeing patients with what time is available. The statistics prove that psychiatrists are less willing than other specialists to participate with insurance networks, and I suspect the litany of clinically irrelevant requirements may lead to earlier retirement by people who might otherwise be willing to practice for more years.
One might ask, at what point do we fight back against spending our time meeting the agendas of agencies and insurers when they aren’t relevant to the care that is needed to help patients?
With thanks to Dr. Mahmood Jarhomi, Dr. Patricia Sullivan, Dr. Sue Kim, Dr. Laura Gaffney, Dr. Maria Yang, Dr. Marsden McGuire, Dr. Annette Hanson, Dr. Robert Herman, Dr. Kimberly Hogan Pesaniello, Dr. Peter Kahn, Dr. Mark Komrad, Dr. Susan Molchan, Dr. Suzy Nashed, and Dr. Rebecca Twersky-Kengmana.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Recently I was contacted by a reporter who wanted to speak to me about why it’s so difficult for patients to find a psychiatrist. She’d found me by Googling “Why psychiatrists don’t take insurance” and already had read an article I’d written with that title. That day, it had snowed hard enough that most of my patients had canceled; the grocery store had closed; and I had plenty of time to chat with a reporter. The other thing I noted – perhaps because other psychiatrists had unexpected free time because of the snow – was that Maryland Psychiatric Society’s listserv was getting a lot of posts. The posts focused on issues to do with maintenance of certification (MOC) or with the fact that every physician in the state was now going to be required to have a CME credit on opioid prescribing for licensure renewal, and there would be a requirement for physicians to take a course on substance abuse to renew their CDS registration. The hope is that these courses will reduce deaths caused by narcotic overdose, and the courses would be required for all physicians without regard to whether they are relevant to their practice.
The reporter and I started with a discussion of why so many psychiatrists have chosen not to accept health insurance (myself included). She then told me about an insured man who had been diagnosed with schizophrenia and substance abuse who was unable to get an appointment with a psychiatrist. She asked me an interesting question: “Don’t psychiatrists want the challenge of treating the difficult cases?” The patient in question never did find a psychiatrist in time and he ended up committing a murder then dying by suicide – an awful tragedy that highlights access to care problems.
In addition to a private practice, I have worked in community mental health centers, and I discussed how that setting is often better suited for patients with serious psychiatric illnesses. More services are offered, and having a variety of mental health professionals in the same facility promotes better coordination of care between psychiatrists, therapists, and case managers, as well as with family, residential care providers, and day programs. The problem is that demand for treatment at outpatient clinics is high, and sometimes the waits for an initial appointment are long, or clinics even may stop accepting new patients at times when they get overloaded.
We talked about the logistics and trade-offs of working in a clinic vs. a private practice, and the reasons why working full time in a high-volume clinic might lead physicians to want a change after a few years. And then the reporter asked me another interesting question – with such long waits, why don’t the clinics hire more doctors? I explained that there was a shortage of psychiatrists and began to talk with her about demands on physician time that take time away from patient care. With the e-mails flying about MOC and new course requirements, it was a place to start, but the snow was still falling, and she heard a lot about the factors that drain physician time and money, both limiting how many patients a psychiatrist can see and driving up the cost of care.
By the time I got off the phone, I decided to tally all of the things that we are required to do to see patients. I was able to get some quick help on the listserv, from friends, and on Twitter.
Every time an agency or insurance company sets up a requirement for a physician, there is a small diversion of time. There is no limit on how many different requirements can be set or whether they need to be relevant to the physician’s work. While I realize there is little sympathy for physicians who, for the most part, are still blessed to earn a good living while doing meaningful work, these diversions add hours to a doctor’s day and cause them to burn out more quickly. So the insurance company that demands that a physician devote 20 minutes to get authorization to prescribe a medication that costs pennies a pill is actually harming society. And no one oversees the big picture.
That said, here was the list we came up with of factors that drain time and money in a clinical practice. Please note that some of these items – for example, uncompensated time returning calls to patients or keeping clinical records – are just part of being a doctor; they’re not something that should be eliminated. Similarly, issues related to having a space to work are part of having a business. I wanted the list to be complete to illustrate the demands on a psychiatrist, not to suggest that none of these things are important. Obviously, some doctors are faster or slower at certain tasks, and people vary greatly in how much time they devote to clinical practice vs. teaching, research, or writing articles for Clinical Psychiatry News. I obtained information in a very quick and casual manner; none of this should be construed as scientific.
Here is the list:
• Maintenance of certification requirements and testing. This is required every 10 years and one estimate was that the cost to register, take the test, and purchase review materials came to $2,800, with a time investment of about 50 hours. Some specialties are pushing back against MOC, and some physicians are forgoing board certification. Psychiatrists who subspecialize usually do MOC for general psychiatry and all their subspecialties.
• CME. Twenty to 50 hours per year depending on your state, and presumably physicians choose courses that enrich their ability to practice medicine. This can be expensive, depending on how the physician decides to get these credits, and many valuable learning events do not qualify for CME.
• Writing clinical notes. Again, this is part of routine medical care. Notes must justify the CPT codes on insurance claims, and very specific areas of inquiry and examination are needed to justify billing specific codes. Agency requirements may be different from what is clinically indicated for the care of the patient, and this uses some of the appointment time in a way that may not be helpful to medical care. Copying, faxing, or sending notes to other clinicians and time spent requesting records all add to the mix. One psychiatrist noted that the overall administrative responsibilities for seeing patients takes half an hour for every hour spent with a patient. Others estimated that anywhere from 30 minutes to 2 hours per day are devoted to writing notes, and some mentioned doing this in the evening at home. One child psychiatrist with a large high-volume practice noted that he is required to keep charts until a patient reaches adulthood, and that storing, locating, and shredding charts was a time drain.
• Billing the patient. One private practice psychiatrist estimated this takes approximately 8 hours a month, include record-keeping and rebilling patients who failed to pay. Some psychiatrists have a secretary or billing staff.
• Patient insurance. Time spent preauthorizing care, including time spent to preauthorize hospitalizations or to justify each day of inpatient treatment. (No time estimates were offered.)
• Filing claims. The psychiatrists I spoke with who participate with insurers all had support staff to do this.
• Preauthorizing medications. This was by far the biggest complaint by psychiatrists. One noted that it had taken her 2 hours the night before to get a medication authorized; another had spent an hour that day on it. Another rough figure I got was 20-60 minutes a week, and it was noted that preauthorization often is required for very inexpensive medications. Another psychiatrist said her office manager spends a couple of hours a week on preauthorizations and that she had to give her a raise to get her to agree to do it. Personally, I feel insurance companies should not be permitted to divert physician time away from care for inexpensive medications. Does it really make sense to have a physician spend 20 minutes of uncompensated time getting authorization for a medication that costs $10 a month?
• Paperwork related to being credentialed with insurance companies. This was estimated at 40 minutes every 3 months.
• Credentialing. Cost and paperwork for malpractice insurance varies by state and, some malpractice agencies require doctors to do specific forms of training. In addition, practicing requires renewal of a DEA number, CDS renewal (in Maryland), and state licensure.
• Electronic medical records (EMR). Medicare has provided financial incentives to doctors for the meaningful use of certified electronic health record (EHR) technology to improve patient care and now penalizes doctors who do not have this technology. One psychiatrist told me that she spent hundreds of hours working on this, but something went wrong so she is still penalized. Another said she spent 3 hours in a 3-month period attesting to her compliance with meaningful use. Everyone I spoke to said using an electronic record – related to Medicare’s meaningful use or not – increased the time it takes them to write notes. One psychiatrist reduced her clinical care to 1 day a week, and I left a community clinic when the effort of learning to use EPIC overwhelmed me.
• E-prescribing. One colleague in New York wrote, “E-prescribing takes up a lot of time, especially since I don’t do it during sessions. For a noncontrolled medication, it’s maybe 4-5 minutes per prescription. For controlled, it’s 3-4 minutes more, because I have to check I-STOP and use the token, and then record the I-STOP number. And for all prescriptions, I hand write an entry in the medication record, just for backup.” She noted it took several hours to set up the system. Most psychiatrists still spend significant time calling in prescriptions that patients have forgotten to request during appointments, and pharmacists often call to have refills authorized. This can be quite time consuming, and sometimes refills are requested automatically for medications the patients no longer take, and time spent on hold can be significant. My own experience was that e-prescribing took significantly longer than paper prescribing, and that handing a patient a prescription during a session is simply part of medical care and not a “drain,” per se.
• Secretarial. No one was able to give me an estimate of how many hours per week were spent directing, managing, and training support staff, or of how many hours this freed up to see patients. One psychiatrist in a large practice noted that they have 32 full- and part-time professions, including 3 psychiatrists; they participate with insurance, and this requires 18 full-time support staff.
• Office-related issues. Rent – this is both taste and geographically driven, and there are several ways to come by office space. Other factors are time related to restocking supplies, furnishings, technological hardware, phones, faxes, pagers, mobile lines, postage, technology support, cleaning, and assorted office-related issues. I have no time estimates on this; some people have support staff who do most of it, and again, this is part of the routine practice of having a business. It takes time, but it’s not irrelevant. Also, time is spent keeping an office both OSHA and HIPAA compliant.
• Hospital/agency-related requirements:
– Risk management seminars.
– CPR training.
– Health maintenance (required TB testing and flu shot).
• Required learning modules. When I worked 4 hours a week at a hospital clinic, there were many requirements. I watched modules on how to use elevators in buildings I never entered, how to place a central line, hand-washing and infection control, and how to store chemicals I never used. I believe that Maryland state employees may be required to have training in trauma-informed-care.
• Uncompensated time returning calls/communications to patients, families, other clinicians, and prospective patients who then decide not to come in, as well as filling out paperwork for disability claims, other agencies, and writing letters for patients. While this also is part of routine medical care, several people mentioned that other professionals can bill for this work and that insurers can force unnecessary care because only face-to-face treatment gets reimbursed, so issues that might be resolved on the phone or by telepsychiatry then require an office visit.
One colleague was kind enough to examine her own full-time practice and sum up her activities. She came up with an estimate that she devoted 40 hours per month to administrative issues that divert time from seeing patients. This did not include the time she recently devoted to MOC.
Obviously, I want to make the point that part of the psychiatrist shortage is related to the fact that there are administrative demands – many that don’t improve clinical care – that decrease the number of patients we can see and increase the cost of care. In addition to the weekly toll, many of these time drains are frustrating, and serve as disincentives to seeing patients with what time is available. The statistics prove that psychiatrists are less willing than other specialists to participate with insurance networks, and I suspect the litany of clinically irrelevant requirements may lead to earlier retirement by people who might otherwise be willing to practice for more years.
One might ask, at what point do we fight back against spending our time meeting the agendas of agencies and insurers when they aren’t relevant to the care that is needed to help patients?
With thanks to Dr. Mahmood Jarhomi, Dr. Patricia Sullivan, Dr. Sue Kim, Dr. Laura Gaffney, Dr. Maria Yang, Dr. Marsden McGuire, Dr. Annette Hanson, Dr. Robert Herman, Dr. Kimberly Hogan Pesaniello, Dr. Peter Kahn, Dr. Mark Komrad, Dr. Susan Molchan, Dr. Suzy Nashed, and Dr. Rebecca Twersky-Kengmana.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Recently I was contacted by a reporter who wanted to speak to me about why it’s so difficult for patients to find a psychiatrist. She’d found me by Googling “Why psychiatrists don’t take insurance” and already had read an article I’d written with that title. That day, it had snowed hard enough that most of my patients had canceled; the grocery store had closed; and I had plenty of time to chat with a reporter. The other thing I noted – perhaps because other psychiatrists had unexpected free time because of the snow – was that Maryland Psychiatric Society’s listserv was getting a lot of posts. The posts focused on issues to do with maintenance of certification (MOC) or with the fact that every physician in the state was now going to be required to have a CME credit on opioid prescribing for licensure renewal, and there would be a requirement for physicians to take a course on substance abuse to renew their CDS registration. The hope is that these courses will reduce deaths caused by narcotic overdose, and the courses would be required for all physicians without regard to whether they are relevant to their practice.
The reporter and I started with a discussion of why so many psychiatrists have chosen not to accept health insurance (myself included). She then told me about an insured man who had been diagnosed with schizophrenia and substance abuse who was unable to get an appointment with a psychiatrist. She asked me an interesting question: “Don’t psychiatrists want the challenge of treating the difficult cases?” The patient in question never did find a psychiatrist in time and he ended up committing a murder then dying by suicide – an awful tragedy that highlights access to care problems.
In addition to a private practice, I have worked in community mental health centers, and I discussed how that setting is often better suited for patients with serious psychiatric illnesses. More services are offered, and having a variety of mental health professionals in the same facility promotes better coordination of care between psychiatrists, therapists, and case managers, as well as with family, residential care providers, and day programs. The problem is that demand for treatment at outpatient clinics is high, and sometimes the waits for an initial appointment are long, or clinics even may stop accepting new patients at times when they get overloaded.
We talked about the logistics and trade-offs of working in a clinic vs. a private practice, and the reasons why working full time in a high-volume clinic might lead physicians to want a change after a few years. And then the reporter asked me another interesting question – with such long waits, why don’t the clinics hire more doctors? I explained that there was a shortage of psychiatrists and began to talk with her about demands on physician time that take time away from patient care. With the e-mails flying about MOC and new course requirements, it was a place to start, but the snow was still falling, and she heard a lot about the factors that drain physician time and money, both limiting how many patients a psychiatrist can see and driving up the cost of care.
By the time I got off the phone, I decided to tally all of the things that we are required to do to see patients. I was able to get some quick help on the listserv, from friends, and on Twitter.
Every time an agency or insurance company sets up a requirement for a physician, there is a small diversion of time. There is no limit on how many different requirements can be set or whether they need to be relevant to the physician’s work. While I realize there is little sympathy for physicians who, for the most part, are still blessed to earn a good living while doing meaningful work, these diversions add hours to a doctor’s day and cause them to burn out more quickly. So the insurance company that demands that a physician devote 20 minutes to get authorization to prescribe a medication that costs pennies a pill is actually harming society. And no one oversees the big picture.
That said, here was the list we came up with of factors that drain time and money in a clinical practice. Please note that some of these items – for example, uncompensated time returning calls to patients or keeping clinical records – are just part of being a doctor; they’re not something that should be eliminated. Similarly, issues related to having a space to work are part of having a business. I wanted the list to be complete to illustrate the demands on a psychiatrist, not to suggest that none of these things are important. Obviously, some doctors are faster or slower at certain tasks, and people vary greatly in how much time they devote to clinical practice vs. teaching, research, or writing articles for Clinical Psychiatry News. I obtained information in a very quick and casual manner; none of this should be construed as scientific.
Here is the list:
• Maintenance of certification requirements and testing. This is required every 10 years and one estimate was that the cost to register, take the test, and purchase review materials came to $2,800, with a time investment of about 50 hours. Some specialties are pushing back against MOC, and some physicians are forgoing board certification. Psychiatrists who subspecialize usually do MOC for general psychiatry and all their subspecialties.
• CME. Twenty to 50 hours per year depending on your state, and presumably physicians choose courses that enrich their ability to practice medicine. This can be expensive, depending on how the physician decides to get these credits, and many valuable learning events do not qualify for CME.
• Writing clinical notes. Again, this is part of routine medical care. Notes must justify the CPT codes on insurance claims, and very specific areas of inquiry and examination are needed to justify billing specific codes. Agency requirements may be different from what is clinically indicated for the care of the patient, and this uses some of the appointment time in a way that may not be helpful to medical care. Copying, faxing, or sending notes to other clinicians and time spent requesting records all add to the mix. One psychiatrist noted that the overall administrative responsibilities for seeing patients takes half an hour for every hour spent with a patient. Others estimated that anywhere from 30 minutes to 2 hours per day are devoted to writing notes, and some mentioned doing this in the evening at home. One child psychiatrist with a large high-volume practice noted that he is required to keep charts until a patient reaches adulthood, and that storing, locating, and shredding charts was a time drain.
• Billing the patient. One private practice psychiatrist estimated this takes approximately 8 hours a month, include record-keeping and rebilling patients who failed to pay. Some psychiatrists have a secretary or billing staff.
• Patient insurance. Time spent preauthorizing care, including time spent to preauthorize hospitalizations or to justify each day of inpatient treatment. (No time estimates were offered.)
• Filing claims. The psychiatrists I spoke with who participate with insurers all had support staff to do this.
• Preauthorizing medications. This was by far the biggest complaint by psychiatrists. One noted that it had taken her 2 hours the night before to get a medication authorized; another had spent an hour that day on it. Another rough figure I got was 20-60 minutes a week, and it was noted that preauthorization often is required for very inexpensive medications. Another psychiatrist said her office manager spends a couple of hours a week on preauthorizations and that she had to give her a raise to get her to agree to do it. Personally, I feel insurance companies should not be permitted to divert physician time away from care for inexpensive medications. Does it really make sense to have a physician spend 20 minutes of uncompensated time getting authorization for a medication that costs $10 a month?
• Paperwork related to being credentialed with insurance companies. This was estimated at 40 minutes every 3 months.
• Credentialing. Cost and paperwork for malpractice insurance varies by state and, some malpractice agencies require doctors to do specific forms of training. In addition, practicing requires renewal of a DEA number, CDS renewal (in Maryland), and state licensure.
• Electronic medical records (EMR). Medicare has provided financial incentives to doctors for the meaningful use of certified electronic health record (EHR) technology to improve patient care and now penalizes doctors who do not have this technology. One psychiatrist told me that she spent hundreds of hours working on this, but something went wrong so she is still penalized. Another said she spent 3 hours in a 3-month period attesting to her compliance with meaningful use. Everyone I spoke to said using an electronic record – related to Medicare’s meaningful use or not – increased the time it takes them to write notes. One psychiatrist reduced her clinical care to 1 day a week, and I left a community clinic when the effort of learning to use EPIC overwhelmed me.
• E-prescribing. One colleague in New York wrote, “E-prescribing takes up a lot of time, especially since I don’t do it during sessions. For a noncontrolled medication, it’s maybe 4-5 minutes per prescription. For controlled, it’s 3-4 minutes more, because I have to check I-STOP and use the token, and then record the I-STOP number. And for all prescriptions, I hand write an entry in the medication record, just for backup.” She noted it took several hours to set up the system. Most psychiatrists still spend significant time calling in prescriptions that patients have forgotten to request during appointments, and pharmacists often call to have refills authorized. This can be quite time consuming, and sometimes refills are requested automatically for medications the patients no longer take, and time spent on hold can be significant. My own experience was that e-prescribing took significantly longer than paper prescribing, and that handing a patient a prescription during a session is simply part of medical care and not a “drain,” per se.
• Secretarial. No one was able to give me an estimate of how many hours per week were spent directing, managing, and training support staff, or of how many hours this freed up to see patients. One psychiatrist in a large practice noted that they have 32 full- and part-time professions, including 3 psychiatrists; they participate with insurance, and this requires 18 full-time support staff.
• Office-related issues. Rent – this is both taste and geographically driven, and there are several ways to come by office space. Other factors are time related to restocking supplies, furnishings, technological hardware, phones, faxes, pagers, mobile lines, postage, technology support, cleaning, and assorted office-related issues. I have no time estimates on this; some people have support staff who do most of it, and again, this is part of the routine practice of having a business. It takes time, but it’s not irrelevant. Also, time is spent keeping an office both OSHA and HIPAA compliant.
• Hospital/agency-related requirements:
– Risk management seminars.
– CPR training.
– Health maintenance (required TB testing and flu shot).
• Required learning modules. When I worked 4 hours a week at a hospital clinic, there were many requirements. I watched modules on how to use elevators in buildings I never entered, how to place a central line, hand-washing and infection control, and how to store chemicals I never used. I believe that Maryland state employees may be required to have training in trauma-informed-care.
• Uncompensated time returning calls/communications to patients, families, other clinicians, and prospective patients who then decide not to come in, as well as filling out paperwork for disability claims, other agencies, and writing letters for patients. While this also is part of routine medical care, several people mentioned that other professionals can bill for this work and that insurers can force unnecessary care because only face-to-face treatment gets reimbursed, so issues that might be resolved on the phone or by telepsychiatry then require an office visit.
One colleague was kind enough to examine her own full-time practice and sum up her activities. She came up with an estimate that she devoted 40 hours per month to administrative issues that divert time from seeing patients. This did not include the time she recently devoted to MOC.
Obviously, I want to make the point that part of the psychiatrist shortage is related to the fact that there are administrative demands – many that don’t improve clinical care – that decrease the number of patients we can see and increase the cost of care. In addition to the weekly toll, many of these time drains are frustrating, and serve as disincentives to seeing patients with what time is available. The statistics prove that psychiatrists are less willing than other specialists to participate with insurance networks, and I suspect the litany of clinically irrelevant requirements may lead to earlier retirement by people who might otherwise be willing to practice for more years.
One might ask, at what point do we fight back against spending our time meeting the agendas of agencies and insurers when they aren’t relevant to the care that is needed to help patients?
With thanks to Dr. Mahmood Jarhomi, Dr. Patricia Sullivan, Dr. Sue Kim, Dr. Laura Gaffney, Dr. Maria Yang, Dr. Marsden McGuire, Dr. Annette Hanson, Dr. Robert Herman, Dr. Kimberly Hogan Pesaniello, Dr. Peter Kahn, Dr. Mark Komrad, Dr. Susan Molchan, Dr. Suzy Nashed, and Dr. Rebecca Twersky-Kengmana.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Concerns raised by ‘Death With Dignity’ laws
Recently, bills aimed at allowing for physician-assisted suicide – also referred to as “Death With Dignity” laws – have been introduced in New Jersey, the District of Columbia, Maryland, Colorado, California, and Hawaii. Debates over the issue of end-of-life care are contentious and distressing, often accompanied by the tearful testimony of those who have cared for a family member throughout a long terminal illness. It’s hard to listen to these stories and not be moved personally, and to draw upon one’s own life experience with bereavement after a loved one’s suicide or disease.
For psychiatrists, the challenge is to think about assisted suicide not in terms of what we would want for ourselves, but what is best for our patients and the medical profession. Proponents argue that respect for patient autonomy should take priority, even if by respecting autonomy the end result is death. Opponents believe that by granting a request to die to a few people, many more vulnerable people may be abused or harmed inadvertently.
In my opinion, after extensive review of the bills and the effects of existing laws in Oregon and Washington, there are too many problems with assisted-suicide laws to safeguard or regulate this practice effectively.
The chief issue is that there is no mandate for any mental health evaluation for any qualified patient who requests assisted suicide. The primary physician and consulting physicians who certify competence may refer to a psychiatrist or psychologist, but this is only if there is a suspicion of incapacity. In Oregon, where this has been legal for 18 years, less than 5% of patients are referred for a competency assessment by a mental health professional although as many as 25% of terminally ill individuals may be suffering from clinical depression. In Oregon, individuals with HIV are 18 times more likely to die of assisted suicide than natural illness, which is particularly concerning given that HIV is known to affect the brain, and is associated with an increased risk of clinical depression and mania. The law allows a qualified patient to bar physicians from contacting or notifying family, which would make a psychiatrist’s competency assessment difficult if not impossible when the patient is suffering from a condition like dementia and can’t give a history himself.
The assisted-suicide process contains no mechanism to challenge the adequacy of the nonpsychiatrist’s assessment of capacity and noncoercion. There is no mechanism for judicial oversight, no mechanism to allow an interested party to raise the question of incompetence, and no existing standard of care for the assessment of capacity in this situation. Some bills protect the identity of the physicians and the patient, or bar medical records from subpoena or discovery, which would make any investigation for civil or criminal purposes difficult. In Oregon, 18 physicians were referred for board investigation, but none were sanctioned because the law required no more than “good faith” compliance with procedures – essentially only a requirement that the proper forms be filled out and filed promptly. This level of review is clearly inadequate when the process involves the death of an individual.
Some evidence suggests that having a physician-assisted law on the books may affect suicide rates in the general population. In Oregon, the suicide rate has risen out of proportion to the rest of the country, even excluding assisted-suicide deaths. (All laws require that assisted deaths be reported as a death from natural illness rather than suicide.) No formal study has been made of this issue, but there should be some provision to review and suspend the practice if this turns out to be the case.
All existing assisted-suicide laws recommend but do not require that a death be attended. Thus, despite the intent of the law, there is no way to ensure that the suicide is actually voluntary once the lethal medication is in hand. The law allows a physician to dispense medications to facilitate the ingestion of pentobarbital. This is necessary, because some patients have been unable to ingest the volume of liquid necessary to take the whole dose and have regurgitated the medication. Allowing premedication with an antiemetic is sometimes necessary. In theory, this aspect of the law could allow a health care practitioner to inject the antiemetic – an active involvement that would cross the line into euthanasia.
With regard to institutionalized patients, psychiatrists would be in a particularly challenging position. Presently, all patients admitted to hospitals are offered an opportunity to sign medical advance directives. At our forensic hospital in Maryland, admitting physicians assess the patient’s capacity to sign these directives. In theory, an insanity acquittee or long-term patient with a serious medical illness could request assisted suicide if competent. By law, the primary physician – a ward psychiatrist – would ultimately be required to write the lethal prescription or refer to another physician who would. If the patient were incompetent to request assisted suicide, the ward psychiatrist would be required to treat the mental illness knowing that it could eventually lead to the patient’s death. This situation is analogous to the dilemma of the correctional psychiatrist who treats an incompetent death row inmate.
There are many other problems with assisted-suicide legislation. At the very least, states should require a formal certification process to ensure that physicians who provide lethal medication have adequate training and experience to administer and interpret screening tests for psychiatric disorders, to do capacity assessments, and to make prognostic decisions relevant to their board certification and training. In all existing assisted-suicide bills and laws, the only requirement for a physician to provide lethal medication is that he or she must have the “qualifications and experience” to make a diagnosis and prognosis. There is no specific requirement that the attending or consulting physician actually be board certified to treat the illness in question. Thus, in theory, an attending or consulting physician could certify terminal illness without proven competence to do so.
Also, no clear safeguard exists to detect, investigate, and prosecute a hypothetical malicious or unscrupulous physician. In Oregon, three physicians write 20% of lethal prescriptions. It only takes one physician to do a lot of harm.
The American Medical Association has had a position statement on this topic for more than 20 years. The AMA takes the position that physician-assisted suicide is categorically unethical and bars doctors from participation. This, from the standpoint of a state health department, is probably the key issue: Should a legislature have the authority to allow physician behavior that a licensing board and professional organizations already have held to be unethical and not the practice of medicine? One of the core characteristics of a profession is the ability to monitor, police, and ensure the integrity of its members. Legislatures are unwise to undermine this.
Dr. Hanson is a forensic psychiatrist and co-author of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Recently, bills aimed at allowing for physician-assisted suicide – also referred to as “Death With Dignity” laws – have been introduced in New Jersey, the District of Columbia, Maryland, Colorado, California, and Hawaii. Debates over the issue of end-of-life care are contentious and distressing, often accompanied by the tearful testimony of those who have cared for a family member throughout a long terminal illness. It’s hard to listen to these stories and not be moved personally, and to draw upon one’s own life experience with bereavement after a loved one’s suicide or disease.
For psychiatrists, the challenge is to think about assisted suicide not in terms of what we would want for ourselves, but what is best for our patients and the medical profession. Proponents argue that respect for patient autonomy should take priority, even if by respecting autonomy the end result is death. Opponents believe that by granting a request to die to a few people, many more vulnerable people may be abused or harmed inadvertently.
In my opinion, after extensive review of the bills and the effects of existing laws in Oregon and Washington, there are too many problems with assisted-suicide laws to safeguard or regulate this practice effectively.
The chief issue is that there is no mandate for any mental health evaluation for any qualified patient who requests assisted suicide. The primary physician and consulting physicians who certify competence may refer to a psychiatrist or psychologist, but this is only if there is a suspicion of incapacity. In Oregon, where this has been legal for 18 years, less than 5% of patients are referred for a competency assessment by a mental health professional although as many as 25% of terminally ill individuals may be suffering from clinical depression. In Oregon, individuals with HIV are 18 times more likely to die of assisted suicide than natural illness, which is particularly concerning given that HIV is known to affect the brain, and is associated with an increased risk of clinical depression and mania. The law allows a qualified patient to bar physicians from contacting or notifying family, which would make a psychiatrist’s competency assessment difficult if not impossible when the patient is suffering from a condition like dementia and can’t give a history himself.
The assisted-suicide process contains no mechanism to challenge the adequacy of the nonpsychiatrist’s assessment of capacity and noncoercion. There is no mechanism for judicial oversight, no mechanism to allow an interested party to raise the question of incompetence, and no existing standard of care for the assessment of capacity in this situation. Some bills protect the identity of the physicians and the patient, or bar medical records from subpoena or discovery, which would make any investigation for civil or criminal purposes difficult. In Oregon, 18 physicians were referred for board investigation, but none were sanctioned because the law required no more than “good faith” compliance with procedures – essentially only a requirement that the proper forms be filled out and filed promptly. This level of review is clearly inadequate when the process involves the death of an individual.
Some evidence suggests that having a physician-assisted law on the books may affect suicide rates in the general population. In Oregon, the suicide rate has risen out of proportion to the rest of the country, even excluding assisted-suicide deaths. (All laws require that assisted deaths be reported as a death from natural illness rather than suicide.) No formal study has been made of this issue, but there should be some provision to review and suspend the practice if this turns out to be the case.
All existing assisted-suicide laws recommend but do not require that a death be attended. Thus, despite the intent of the law, there is no way to ensure that the suicide is actually voluntary once the lethal medication is in hand. The law allows a physician to dispense medications to facilitate the ingestion of pentobarbital. This is necessary, because some patients have been unable to ingest the volume of liquid necessary to take the whole dose and have regurgitated the medication. Allowing premedication with an antiemetic is sometimes necessary. In theory, this aspect of the law could allow a health care practitioner to inject the antiemetic – an active involvement that would cross the line into euthanasia.
With regard to institutionalized patients, psychiatrists would be in a particularly challenging position. Presently, all patients admitted to hospitals are offered an opportunity to sign medical advance directives. At our forensic hospital in Maryland, admitting physicians assess the patient’s capacity to sign these directives. In theory, an insanity acquittee or long-term patient with a serious medical illness could request assisted suicide if competent. By law, the primary physician – a ward psychiatrist – would ultimately be required to write the lethal prescription or refer to another physician who would. If the patient were incompetent to request assisted suicide, the ward psychiatrist would be required to treat the mental illness knowing that it could eventually lead to the patient’s death. This situation is analogous to the dilemma of the correctional psychiatrist who treats an incompetent death row inmate.
There are many other problems with assisted-suicide legislation. At the very least, states should require a formal certification process to ensure that physicians who provide lethal medication have adequate training and experience to administer and interpret screening tests for psychiatric disorders, to do capacity assessments, and to make prognostic decisions relevant to their board certification and training. In all existing assisted-suicide bills and laws, the only requirement for a physician to provide lethal medication is that he or she must have the “qualifications and experience” to make a diagnosis and prognosis. There is no specific requirement that the attending or consulting physician actually be board certified to treat the illness in question. Thus, in theory, an attending or consulting physician could certify terminal illness without proven competence to do so.
Also, no clear safeguard exists to detect, investigate, and prosecute a hypothetical malicious or unscrupulous physician. In Oregon, three physicians write 20% of lethal prescriptions. It only takes one physician to do a lot of harm.
The American Medical Association has had a position statement on this topic for more than 20 years. The AMA takes the position that physician-assisted suicide is categorically unethical and bars doctors from participation. This, from the standpoint of a state health department, is probably the key issue: Should a legislature have the authority to allow physician behavior that a licensing board and professional organizations already have held to be unethical and not the practice of medicine? One of the core characteristics of a profession is the ability to monitor, police, and ensure the integrity of its members. Legislatures are unwise to undermine this.
Dr. Hanson is a forensic psychiatrist and co-author of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Recently, bills aimed at allowing for physician-assisted suicide – also referred to as “Death With Dignity” laws – have been introduced in New Jersey, the District of Columbia, Maryland, Colorado, California, and Hawaii. Debates over the issue of end-of-life care are contentious and distressing, often accompanied by the tearful testimony of those who have cared for a family member throughout a long terminal illness. It’s hard to listen to these stories and not be moved personally, and to draw upon one’s own life experience with bereavement after a loved one’s suicide or disease.
For psychiatrists, the challenge is to think about assisted suicide not in terms of what we would want for ourselves, but what is best for our patients and the medical profession. Proponents argue that respect for patient autonomy should take priority, even if by respecting autonomy the end result is death. Opponents believe that by granting a request to die to a few people, many more vulnerable people may be abused or harmed inadvertently.
In my opinion, after extensive review of the bills and the effects of existing laws in Oregon and Washington, there are too many problems with assisted-suicide laws to safeguard or regulate this practice effectively.
The chief issue is that there is no mandate for any mental health evaluation for any qualified patient who requests assisted suicide. The primary physician and consulting physicians who certify competence may refer to a psychiatrist or psychologist, but this is only if there is a suspicion of incapacity. In Oregon, where this has been legal for 18 years, less than 5% of patients are referred for a competency assessment by a mental health professional although as many as 25% of terminally ill individuals may be suffering from clinical depression. In Oregon, individuals with HIV are 18 times more likely to die of assisted suicide than natural illness, which is particularly concerning given that HIV is known to affect the brain, and is associated with an increased risk of clinical depression and mania. The law allows a qualified patient to bar physicians from contacting or notifying family, which would make a psychiatrist’s competency assessment difficult if not impossible when the patient is suffering from a condition like dementia and can’t give a history himself.
The assisted-suicide process contains no mechanism to challenge the adequacy of the nonpsychiatrist’s assessment of capacity and noncoercion. There is no mechanism for judicial oversight, no mechanism to allow an interested party to raise the question of incompetence, and no existing standard of care for the assessment of capacity in this situation. Some bills protect the identity of the physicians and the patient, or bar medical records from subpoena or discovery, which would make any investigation for civil or criminal purposes difficult. In Oregon, 18 physicians were referred for board investigation, but none were sanctioned because the law required no more than “good faith” compliance with procedures – essentially only a requirement that the proper forms be filled out and filed promptly. This level of review is clearly inadequate when the process involves the death of an individual.
Some evidence suggests that having a physician-assisted law on the books may affect suicide rates in the general population. In Oregon, the suicide rate has risen out of proportion to the rest of the country, even excluding assisted-suicide deaths. (All laws require that assisted deaths be reported as a death from natural illness rather than suicide.) No formal study has been made of this issue, but there should be some provision to review and suspend the practice if this turns out to be the case.
All existing assisted-suicide laws recommend but do not require that a death be attended. Thus, despite the intent of the law, there is no way to ensure that the suicide is actually voluntary once the lethal medication is in hand. The law allows a physician to dispense medications to facilitate the ingestion of pentobarbital. This is necessary, because some patients have been unable to ingest the volume of liquid necessary to take the whole dose and have regurgitated the medication. Allowing premedication with an antiemetic is sometimes necessary. In theory, this aspect of the law could allow a health care practitioner to inject the antiemetic – an active involvement that would cross the line into euthanasia.
With regard to institutionalized patients, psychiatrists would be in a particularly challenging position. Presently, all patients admitted to hospitals are offered an opportunity to sign medical advance directives. At our forensic hospital in Maryland, admitting physicians assess the patient’s capacity to sign these directives. In theory, an insanity acquittee or long-term patient with a serious medical illness could request assisted suicide if competent. By law, the primary physician – a ward psychiatrist – would ultimately be required to write the lethal prescription or refer to another physician who would. If the patient were incompetent to request assisted suicide, the ward psychiatrist would be required to treat the mental illness knowing that it could eventually lead to the patient’s death. This situation is analogous to the dilemma of the correctional psychiatrist who treats an incompetent death row inmate.
There are many other problems with assisted-suicide legislation. At the very least, states should require a formal certification process to ensure that physicians who provide lethal medication have adequate training and experience to administer and interpret screening tests for psychiatric disorders, to do capacity assessments, and to make prognostic decisions relevant to their board certification and training. In all existing assisted-suicide bills and laws, the only requirement for a physician to provide lethal medication is that he or she must have the “qualifications and experience” to make a diagnosis and prognosis. There is no specific requirement that the attending or consulting physician actually be board certified to treat the illness in question. Thus, in theory, an attending or consulting physician could certify terminal illness without proven competence to do so.
Also, no clear safeguard exists to detect, investigate, and prosecute a hypothetical malicious or unscrupulous physician. In Oregon, three physicians write 20% of lethal prescriptions. It only takes one physician to do a lot of harm.
The American Medical Association has had a position statement on this topic for more than 20 years. The AMA takes the position that physician-assisted suicide is categorically unethical and bars doctors from participation. This, from the standpoint of a state health department, is probably the key issue: Should a legislature have the authority to allow physician behavior that a licensing board and professional organizations already have held to be unethical and not the practice of medicine? One of the core characteristics of a profession is the ability to monitor, police, and ensure the integrity of its members. Legislatures are unwise to undermine this.
Dr. Hanson is a forensic psychiatrist and co-author of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Should APA have endorsed the Helping Families in Mental Health Crisis Act?
After the school shooting in Newtown, Conn., in December 2012, we saw an unprecedented amount of proposed legislation at both the state and national levels. The legislation was aimed at fixing whatever it is that is broken in our country that either causes or allows a young man to kill more than two dozen innocent people. Some legislators focused on gun control, while others focused on changing the mental health system, with the idea that the shooter’s actions were caused by his untreated mental illness.
Rep. Tim Murphy, Ph.D., has the distinction of being the only clinical psychologist in Congress, so it’s certainly understandable that he would focus on making long-overdue changes to our troubled mental health system. In addition, Rep. Murphy, a Republican from Pennsylvania, has a strong history of voting against legislation that would curb gun rights, and he carries an “A” grade from the National Rifle Association. When Rep. Murphy publicly promised the families of the Newtown victims that he would enact change, it was clear that his passion was for changing the mental health system. In 2013, Rep. Murphy, with bipartisan support, proposed The Helping Families in Mental Health Crisis Act.
The Murphy bill proposed sweeping and complex changes, and the text was 135 pages long. A major component of the bill was to create a position for an assistant secretary for mental health and substance use disorders within the Department of Health & Human Services to coordinate federal programs and ensure that evidence-based treatments were being used.
The bill also called for shifting money from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health in the wake of recent thought that SAMHSA has become insensitive to severe mental illness and too oriented toward a recovery model that carries a vague antipsychiatry sentiment.
From there, the issues of patients’ rights versus a doctor-knows-best sentiment have influenced the act, as though one can’t be in favor of both. Perhaps the most controversial requirements include a provision that mandates all states to have outpatient civil commitment programs and a provision that says that health care providers may release information to caretakers of patients with psychiatric disorders without the patient’s consent if the information is felt to be necessary for the patient’s safety or welfare.
This last point is likely to be interpreted as suggesting that psychiatric patients don’t have the same right to confidentiality that other patients have, which would be true. It has the potential to be stigmatizing and infantilizing, and there are people who will not seek care because of the perception this creates. In addition, it may create tension between family members who feel the law now entitles them to information and psychiatrists who don’t see this is as necessary or who fear that releasing information will damage the therapeutic relationship.
Many components of the Helping Families in Mental Health Crisis Act have been applauded universally, but the American Psychiatric Association did not formally support the bill, and an opposing bill was proposed in Congress by Rep. Ron Barber, a Democrat from Arizona who took Gabrielle Giffords’ seat after an assassination attempt by a mentally ill man left her unable to serve. Both bills died when the congressional session ended in December, and Mr. Barber lost a re-election bid and has not returned to Congress.
A new Congress has convened, and Rep. Murphy will be re-introducing the Helping Families in Mental Health Crisis Act with numerous changes. Although the APA did not endorse the previous legislation, the association last week announced, with unanimous backing by the Board of Trustees, its support for the Murphy bill.
“We are pleased that Chairman Murphy is refining and reintroducing his comprehensive mental health reform bill, the Helping Families in Mental Health Crisis Act,” APA President Paul Summergrad said in the last week of January. At an event in early February, he said that he intends to add reforms that align well with APA priorities, including boosting the psychiatric workforce and monitoring and enforcement of mental health parity.
“In December the APA Board of Trustees carefully reviewed its strategy, principles and options for reform and unanimously voted to fully support the efforts of Chairman Murphy and his lead Democratic cosponsor, Rep. Eddie Bernice Johnson. Their efforts are historic in scope, and we are hopeful that Congress will through the legislative process act to pass comprehensive mental health reform with the bipartisan support it deserves.”
Still, I heard the news and was terribly disappointed in the APA. The decision to support this sweeping legislation was made without a vote by the Assembly, with the knowledge that some of these issues are quite polarizing. In addition to the HIPAA disqualification, the issue of outpatient civil commitment, in particular, is controversial. Although proponents are quick to point to research that show its benefits – the research has been done specifically on Kendra’s Law in New York, where $125 million was placed into that state’s mental health system to shore up services – we don’t have the research to know if what helps is providing more services or strong-armed coercion. The text of the bill will be released in the coming weeks. At the very least, couldn’t the APA have waited to see exactly what it is we endorsed?
Dr. Miller is writing a book on involuntary psychiatric care.
After the school shooting in Newtown, Conn., in December 2012, we saw an unprecedented amount of proposed legislation at both the state and national levels. The legislation was aimed at fixing whatever it is that is broken in our country that either causes or allows a young man to kill more than two dozen innocent people. Some legislators focused on gun control, while others focused on changing the mental health system, with the idea that the shooter’s actions were caused by his untreated mental illness.
Rep. Tim Murphy, Ph.D., has the distinction of being the only clinical psychologist in Congress, so it’s certainly understandable that he would focus on making long-overdue changes to our troubled mental health system. In addition, Rep. Murphy, a Republican from Pennsylvania, has a strong history of voting against legislation that would curb gun rights, and he carries an “A” grade from the National Rifle Association. When Rep. Murphy publicly promised the families of the Newtown victims that he would enact change, it was clear that his passion was for changing the mental health system. In 2013, Rep. Murphy, with bipartisan support, proposed The Helping Families in Mental Health Crisis Act.
The Murphy bill proposed sweeping and complex changes, and the text was 135 pages long. A major component of the bill was to create a position for an assistant secretary for mental health and substance use disorders within the Department of Health & Human Services to coordinate federal programs and ensure that evidence-based treatments were being used.
The bill also called for shifting money from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health in the wake of recent thought that SAMHSA has become insensitive to severe mental illness and too oriented toward a recovery model that carries a vague antipsychiatry sentiment.
From there, the issues of patients’ rights versus a doctor-knows-best sentiment have influenced the act, as though one can’t be in favor of both. Perhaps the most controversial requirements include a provision that mandates all states to have outpatient civil commitment programs and a provision that says that health care providers may release information to caretakers of patients with psychiatric disorders without the patient’s consent if the information is felt to be necessary for the patient’s safety or welfare.
This last point is likely to be interpreted as suggesting that psychiatric patients don’t have the same right to confidentiality that other patients have, which would be true. It has the potential to be stigmatizing and infantilizing, and there are people who will not seek care because of the perception this creates. In addition, it may create tension between family members who feel the law now entitles them to information and psychiatrists who don’t see this is as necessary or who fear that releasing information will damage the therapeutic relationship.
Many components of the Helping Families in Mental Health Crisis Act have been applauded universally, but the American Psychiatric Association did not formally support the bill, and an opposing bill was proposed in Congress by Rep. Ron Barber, a Democrat from Arizona who took Gabrielle Giffords’ seat after an assassination attempt by a mentally ill man left her unable to serve. Both bills died when the congressional session ended in December, and Mr. Barber lost a re-election bid and has not returned to Congress.
A new Congress has convened, and Rep. Murphy will be re-introducing the Helping Families in Mental Health Crisis Act with numerous changes. Although the APA did not endorse the previous legislation, the association last week announced, with unanimous backing by the Board of Trustees, its support for the Murphy bill.
“We are pleased that Chairman Murphy is refining and reintroducing his comprehensive mental health reform bill, the Helping Families in Mental Health Crisis Act,” APA President Paul Summergrad said in the last week of January. At an event in early February, he said that he intends to add reforms that align well with APA priorities, including boosting the psychiatric workforce and monitoring and enforcement of mental health parity.
“In December the APA Board of Trustees carefully reviewed its strategy, principles and options for reform and unanimously voted to fully support the efforts of Chairman Murphy and his lead Democratic cosponsor, Rep. Eddie Bernice Johnson. Their efforts are historic in scope, and we are hopeful that Congress will through the legislative process act to pass comprehensive mental health reform with the bipartisan support it deserves.”
Still, I heard the news and was terribly disappointed in the APA. The decision to support this sweeping legislation was made without a vote by the Assembly, with the knowledge that some of these issues are quite polarizing. In addition to the HIPAA disqualification, the issue of outpatient civil commitment, in particular, is controversial. Although proponents are quick to point to research that show its benefits – the research has been done specifically on Kendra’s Law in New York, where $125 million was placed into that state’s mental health system to shore up services – we don’t have the research to know if what helps is providing more services or strong-armed coercion. The text of the bill will be released in the coming weeks. At the very least, couldn’t the APA have waited to see exactly what it is we endorsed?
Dr. Miller is writing a book on involuntary psychiatric care.
After the school shooting in Newtown, Conn., in December 2012, we saw an unprecedented amount of proposed legislation at both the state and national levels. The legislation was aimed at fixing whatever it is that is broken in our country that either causes or allows a young man to kill more than two dozen innocent people. Some legislators focused on gun control, while others focused on changing the mental health system, with the idea that the shooter’s actions were caused by his untreated mental illness.
Rep. Tim Murphy, Ph.D., has the distinction of being the only clinical psychologist in Congress, so it’s certainly understandable that he would focus on making long-overdue changes to our troubled mental health system. In addition, Rep. Murphy, a Republican from Pennsylvania, has a strong history of voting against legislation that would curb gun rights, and he carries an “A” grade from the National Rifle Association. When Rep. Murphy publicly promised the families of the Newtown victims that he would enact change, it was clear that his passion was for changing the mental health system. In 2013, Rep. Murphy, with bipartisan support, proposed The Helping Families in Mental Health Crisis Act.
The Murphy bill proposed sweeping and complex changes, and the text was 135 pages long. A major component of the bill was to create a position for an assistant secretary for mental health and substance use disorders within the Department of Health & Human Services to coordinate federal programs and ensure that evidence-based treatments were being used.
The bill also called for shifting money from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health in the wake of recent thought that SAMHSA has become insensitive to severe mental illness and too oriented toward a recovery model that carries a vague antipsychiatry sentiment.
From there, the issues of patients’ rights versus a doctor-knows-best sentiment have influenced the act, as though one can’t be in favor of both. Perhaps the most controversial requirements include a provision that mandates all states to have outpatient civil commitment programs and a provision that says that health care providers may release information to caretakers of patients with psychiatric disorders without the patient’s consent if the information is felt to be necessary for the patient’s safety or welfare.
This last point is likely to be interpreted as suggesting that psychiatric patients don’t have the same right to confidentiality that other patients have, which would be true. It has the potential to be stigmatizing and infantilizing, and there are people who will not seek care because of the perception this creates. In addition, it may create tension between family members who feel the law now entitles them to information and psychiatrists who don’t see this is as necessary or who fear that releasing information will damage the therapeutic relationship.
Many components of the Helping Families in Mental Health Crisis Act have been applauded universally, but the American Psychiatric Association did not formally support the bill, and an opposing bill was proposed in Congress by Rep. Ron Barber, a Democrat from Arizona who took Gabrielle Giffords’ seat after an assassination attempt by a mentally ill man left her unable to serve. Both bills died when the congressional session ended in December, and Mr. Barber lost a re-election bid and has not returned to Congress.
A new Congress has convened, and Rep. Murphy will be re-introducing the Helping Families in Mental Health Crisis Act with numerous changes. Although the APA did not endorse the previous legislation, the association last week announced, with unanimous backing by the Board of Trustees, its support for the Murphy bill.
“We are pleased that Chairman Murphy is refining and reintroducing his comprehensive mental health reform bill, the Helping Families in Mental Health Crisis Act,” APA President Paul Summergrad said in the last week of January. At an event in early February, he said that he intends to add reforms that align well with APA priorities, including boosting the psychiatric workforce and monitoring and enforcement of mental health parity.
“In December the APA Board of Trustees carefully reviewed its strategy, principles and options for reform and unanimously voted to fully support the efforts of Chairman Murphy and his lead Democratic cosponsor, Rep. Eddie Bernice Johnson. Their efforts are historic in scope, and we are hopeful that Congress will through the legislative process act to pass comprehensive mental health reform with the bipartisan support it deserves.”
Still, I heard the news and was terribly disappointed in the APA. The decision to support this sweeping legislation was made without a vote by the Assembly, with the knowledge that some of these issues are quite polarizing. In addition to the HIPAA disqualification, the issue of outpatient civil commitment, in particular, is controversial. Although proponents are quick to point to research that show its benefits – the research has been done specifically on Kendra’s Law in New York, where $125 million was placed into that state’s mental health system to shore up services – we don’t have the research to know if what helps is providing more services or strong-armed coercion. The text of the bill will be released in the coming weeks. At the very least, couldn’t the APA have waited to see exactly what it is we endorsed?
Dr. Miller is writing a book on involuntary psychiatric care.
Shrink Rap News: National study shows many offenders receive treatment only in prison
In a study published in the December 2014 issue of American Journal of Public Health, Jennifer M. Reingle Gonzalez, Ph.D., and Nadine M. Connell, Ph.D., of the University of Texas Health Science Center at Houston interviewed a nationally representative sample of all state and federal prisoners with psychiatric disorders to determine whether they had been screened for services at intake and to assess whether screening led to continuity of community treatment.
The subjects were chosen first by selecting a random sample of correctional facilities of varying sizes, from diverse geographic regions. From those facilities, 18,185 prisoners were chosen from among all those incarcerated on a single day in September 2002. Each subject was interviewed personally but also given computer-assisted interviews at different times to ensure recollection accuracy and the confidentiality of clinical data (Am. J. Public Health 2014;104:2328-33).
In the direct interview, each prisoner was asked if he or she had ever been diagnosed with a mental health condition such as depression, bipolar disorder, schizophrenia, posttraumatic stress disorder, an anxiety disorder, or a personality disorder. If any condition had ever been diagnosed, the inmates were then asked if they were taking a psychiatric medication upon admission to the facility. If they were in treatment at intake, they were asked if they had ever been on medication since that time. Finally, they were asked if they had had a medical examination while incarcerated.
Almost all prisoners (90%) were screened at intake and received a medical evaluation. The researchers found that 5,207 (26.2%) of the inmates received at least one lifetime mental health diagnosis, with depression being the most common. Eighteen percent reported taking medication for a psychiatric disorder at the time of intake, but of these, only about half were taking medication after incarceration. Medication continuance was twice as likely for schizophrenia as for depression, and those who received an intake screen were significantly more likely to be referred to a physician and receive medication. Notably, 27% of state and 16% of federal prisoners received medication only in prison.
The investigators attributed the discontinuity in treatment after incarceration to a lack of trained mental health professionals to diagnose and treat psychiatric disorders, and to a rise in prison populations out of proportion to available treatment services. The findings of this study supported the investigators’ recommendation for all facilities to employ intake screening to identify and refer prisoners in need of psychiatric care.
This research is important to forensic psychiatrists working in correctional systems and to those working as administrators or external court-appointed monitors, because it highlights the importance and efficacy of intake screening for prisoners with psychiatric disorders.
Unfortunately, traditional media coverage of this research was predictably provocative. Headlines blared: “Mental health care lacking in state and federal prisons.” The researchers themselves also implied that failure to continue medication in prison indicated some systemic deficiency. While an evaluation by a physician was correlated with the prescription of medication, this was not a perfect correlation. The authors did not discuss any of the valid reasons why medication might not be continued in prison.
The most common reason medication is not continued is that inmates are more likely to be abstinent from drugs and alcohol, and thus may require less or even no antidepressant medication after detoxification. This could account for as much as half of the treatment discontinuity, because as many as 20% of the prisoners had been diagnosed with depression. Also, evidence is mounting that indefinite medication may not be necessary for all conditions. Following a clinical assessment, a correctional physician may have determined that the prisoner had successfully completed maintenance therapy. The final reason why medication is not continued is that the inmate may simply have refused the offered treatment; some prisoners do choose to go without medication completely rather than risk a change to a different regimen.
All of this assumes that the subjects accurately reported both their psychiatric history and their mental health service contact following incarceration. Without access to current records or past documentation, this remains an open question. In my prison system, our electronic health record does contain some data provided by the public health care system. In rare cases, this information is consistent with what the patient reports, but this is the exception rather than the rule.
Finally, the most telling aspect of this research is what it reveals about free society care: A quarter of the inmates received treatment only in prison. That is the real finding worthy of a headline.
Dr. Hanson is a forensic psychiatrist and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
In a study published in the December 2014 issue of American Journal of Public Health, Jennifer M. Reingle Gonzalez, Ph.D., and Nadine M. Connell, Ph.D., of the University of Texas Health Science Center at Houston interviewed a nationally representative sample of all state and federal prisoners with psychiatric disorders to determine whether they had been screened for services at intake and to assess whether screening led to continuity of community treatment.
The subjects were chosen first by selecting a random sample of correctional facilities of varying sizes, from diverse geographic regions. From those facilities, 18,185 prisoners were chosen from among all those incarcerated on a single day in September 2002. Each subject was interviewed personally but also given computer-assisted interviews at different times to ensure recollection accuracy and the confidentiality of clinical data (Am. J. Public Health 2014;104:2328-33).
In the direct interview, each prisoner was asked if he or she had ever been diagnosed with a mental health condition such as depression, bipolar disorder, schizophrenia, posttraumatic stress disorder, an anxiety disorder, or a personality disorder. If any condition had ever been diagnosed, the inmates were then asked if they were taking a psychiatric medication upon admission to the facility. If they were in treatment at intake, they were asked if they had ever been on medication since that time. Finally, they were asked if they had had a medical examination while incarcerated.
Almost all prisoners (90%) were screened at intake and received a medical evaluation. The researchers found that 5,207 (26.2%) of the inmates received at least one lifetime mental health diagnosis, with depression being the most common. Eighteen percent reported taking medication for a psychiatric disorder at the time of intake, but of these, only about half were taking medication after incarceration. Medication continuance was twice as likely for schizophrenia as for depression, and those who received an intake screen were significantly more likely to be referred to a physician and receive medication. Notably, 27% of state and 16% of federal prisoners received medication only in prison.
The investigators attributed the discontinuity in treatment after incarceration to a lack of trained mental health professionals to diagnose and treat psychiatric disorders, and to a rise in prison populations out of proportion to available treatment services. The findings of this study supported the investigators’ recommendation for all facilities to employ intake screening to identify and refer prisoners in need of psychiatric care.
This research is important to forensic psychiatrists working in correctional systems and to those working as administrators or external court-appointed monitors, because it highlights the importance and efficacy of intake screening for prisoners with psychiatric disorders.
Unfortunately, traditional media coverage of this research was predictably provocative. Headlines blared: “Mental health care lacking in state and federal prisons.” The researchers themselves also implied that failure to continue medication in prison indicated some systemic deficiency. While an evaluation by a physician was correlated with the prescription of medication, this was not a perfect correlation. The authors did not discuss any of the valid reasons why medication might not be continued in prison.
The most common reason medication is not continued is that inmates are more likely to be abstinent from drugs and alcohol, and thus may require less or even no antidepressant medication after detoxification. This could account for as much as half of the treatment discontinuity, because as many as 20% of the prisoners had been diagnosed with depression. Also, evidence is mounting that indefinite medication may not be necessary for all conditions. Following a clinical assessment, a correctional physician may have determined that the prisoner had successfully completed maintenance therapy. The final reason why medication is not continued is that the inmate may simply have refused the offered treatment; some prisoners do choose to go without medication completely rather than risk a change to a different regimen.
All of this assumes that the subjects accurately reported both their psychiatric history and their mental health service contact following incarceration. Without access to current records or past documentation, this remains an open question. In my prison system, our electronic health record does contain some data provided by the public health care system. In rare cases, this information is consistent with what the patient reports, but this is the exception rather than the rule.
Finally, the most telling aspect of this research is what it reveals about free society care: A quarter of the inmates received treatment only in prison. That is the real finding worthy of a headline.
Dr. Hanson is a forensic psychiatrist and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
In a study published in the December 2014 issue of American Journal of Public Health, Jennifer M. Reingle Gonzalez, Ph.D., and Nadine M. Connell, Ph.D., of the University of Texas Health Science Center at Houston interviewed a nationally representative sample of all state and federal prisoners with psychiatric disorders to determine whether they had been screened for services at intake and to assess whether screening led to continuity of community treatment.
The subjects were chosen first by selecting a random sample of correctional facilities of varying sizes, from diverse geographic regions. From those facilities, 18,185 prisoners were chosen from among all those incarcerated on a single day in September 2002. Each subject was interviewed personally but also given computer-assisted interviews at different times to ensure recollection accuracy and the confidentiality of clinical data (Am. J. Public Health 2014;104:2328-33).
In the direct interview, each prisoner was asked if he or she had ever been diagnosed with a mental health condition such as depression, bipolar disorder, schizophrenia, posttraumatic stress disorder, an anxiety disorder, or a personality disorder. If any condition had ever been diagnosed, the inmates were then asked if they were taking a psychiatric medication upon admission to the facility. If they were in treatment at intake, they were asked if they had ever been on medication since that time. Finally, they were asked if they had had a medical examination while incarcerated.
Almost all prisoners (90%) were screened at intake and received a medical evaluation. The researchers found that 5,207 (26.2%) of the inmates received at least one lifetime mental health diagnosis, with depression being the most common. Eighteen percent reported taking medication for a psychiatric disorder at the time of intake, but of these, only about half were taking medication after incarceration. Medication continuance was twice as likely for schizophrenia as for depression, and those who received an intake screen were significantly more likely to be referred to a physician and receive medication. Notably, 27% of state and 16% of federal prisoners received medication only in prison.
The investigators attributed the discontinuity in treatment after incarceration to a lack of trained mental health professionals to diagnose and treat psychiatric disorders, and to a rise in prison populations out of proportion to available treatment services. The findings of this study supported the investigators’ recommendation for all facilities to employ intake screening to identify and refer prisoners in need of psychiatric care.
This research is important to forensic psychiatrists working in correctional systems and to those working as administrators or external court-appointed monitors, because it highlights the importance and efficacy of intake screening for prisoners with psychiatric disorders.
Unfortunately, traditional media coverage of this research was predictably provocative. Headlines blared: “Mental health care lacking in state and federal prisons.” The researchers themselves also implied that failure to continue medication in prison indicated some systemic deficiency. While an evaluation by a physician was correlated with the prescription of medication, this was not a perfect correlation. The authors did not discuss any of the valid reasons why medication might not be continued in prison.
The most common reason medication is not continued is that inmates are more likely to be abstinent from drugs and alcohol, and thus may require less or even no antidepressant medication after detoxification. This could account for as much as half of the treatment discontinuity, because as many as 20% of the prisoners had been diagnosed with depression. Also, evidence is mounting that indefinite medication may not be necessary for all conditions. Following a clinical assessment, a correctional physician may have determined that the prisoner had successfully completed maintenance therapy. The final reason why medication is not continued is that the inmate may simply have refused the offered treatment; some prisoners do choose to go without medication completely rather than risk a change to a different regimen.
All of this assumes that the subjects accurately reported both their psychiatric history and their mental health service contact following incarceration. Without access to current records or past documentation, this remains an open question. In my prison system, our electronic health record does contain some data provided by the public health care system. In rare cases, this information is consistent with what the patient reports, but this is the exception rather than the rule.
Finally, the most telling aspect of this research is what it reveals about free society care: A quarter of the inmates received treatment only in prison. That is the real finding worthy of a headline.
Dr. Hanson is a forensic psychiatrist and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Shrink Rap News: Writing about involuntary treatment is harder than you might think
There are many controversies in psychiatry, but the most controversial issue continues to be that of involuntary treatment. Over the past year, I have been working on a book on forced care, along with Dr. Annette Hanson, the forensic psychiatrist who also writes this Shrink Rap News column. The work I’ve been doing for the manuscript – identifying and interviewing the people with a stake in the issue – has placed me in a funny role of being more journalist than physician. It’s a role I mostly love, and if you’ve hit the midpoint of your career and have an opportunity to dedicate some of your time to doing something completely different, I highly recommend shifting gears for a little while.
One of the things I have found most surprising is the reactions of people when I ask to include them. While most people are willing, almost all hesitate a little. Some are quite eager to participate, and one group in Richmond who uses involuntary electroconvulsive therapy heard of my project and extended an invitation for me to come visit, interview them, watch the procedure, and speak with one of their patients. Many people are proud of the work they do and eager to showcase it; they want to have their viewpoint included. With others, I have needed to ask repeatedly, listen to their concerns, and offer reassurances. I’ve taken to telling people they can read a draft of what I write about them – I learned early in the process that without this offer, few people would be willing to speak to me.
I wish I could say that I’ve noticed a pattern to who is comfortable speaking and who is not. Many of the psychiatrists and researchers I’ve approached have given their time willingly without hesitation ( or at least without that much hesitation), including Dr. E. Fuller Torrey; Dr. Paul Appelbaum; Jeffrey Swanson, Ph.D.; Dr. Steven Sharfstein; Dr. Daniel Fisher; Vermont Psychiatric Society President Margaret Bolton; Dr. Bruce Hershfield; and American Psychiatric Association President Paul Summergrad, to name just a few of the many people who have shared their time, experiences, and wisdom with me. It was not as easy for me to find a psychiatrist I could observe working on an inpatient unit, and the project might have been halted in its tracks if not for the enthusiasm of Johns Hopkins psychiatry chair Raymond DePaulo, who allowed me to shadow his team while they tended to inpatients. It was surprisingly easy to find a Crisis Intervention Team police officer to ride with, a little more effort to engage a mental health court judge.
Those who oppose forced treatment initially were more difficult to engage, but with perseverance, I was able to persuade the leadership of MindFreedom International to speak with me, and well, I ambushed a barely willing Scientologist while I was in New York for APA last May. In terms of patient participation, this hesitation did not hold true – many people volunteered to speak with me about how involuntary treatment harmed them, and it was much more difficult to find patients who felt helped by the treatment that was thrust upon them. Two absolutely wonderful women gave generously of themselves so that this project would have real voices to it: both “Lily” and “Eleanor” relived difficult experiences for me and allowed me to obtain their medical records and to speak with their families and their doctors. None of this was easy for them, but it did provide me with an education I would have gotten no other way as they reflected back on the meaning it had to them to have been committed to psychiatric units.
The subject of involuntary outpatient commitment has been particularly difficult to research, in part because I live in Maryland, a state which has no provision for this. I spoke with one family member in Arizona who initially was eager to be interviewed, along with her adult child who has come to feel that involuntary care has been very helpful. When I called back, the mom had changed her mind about participating: “You’re writing a book with a balanced view. There no balance or controversy here for me; it’s a medical problem that needs treatment. ” Unless I could promise to support, unequivocally, the views she held without qualification, she was not interested in participating in our book, even if it would provide an avenue to express her beliefs about the value of outpatient commitment. For similar reasons, I had to approach Ron Honberg, J.D., at the national office of the National Alliance on Mental Illness (NAMI); the Maryland NAMI members did not want me to speak with me after two articles I wrote for this Clinical Psychiatry News column suggested that I was not wholeheartedly in favor of outpatient commitment. I was told the topic was “too sensitive” for their members to discuss with me. So while I’ve learned that the topic inspires a great deal of emotion, there are still surprises with every step.
With all that as a prelude, I am continuing to look for people to interview who are the subjects of mandated civil outpatient treatment orders, as well as their family members. I thought perhaps readers might be able to help me, and I am interested in hearing both the good and the bad. If you, your patients, or their families would like to participate, by all means contact me at DinahMiller@yahoo.com.
Dr. Miller is a coauthor of Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: Johns Hopkins University Press, 2011).
There are many controversies in psychiatry, but the most controversial issue continues to be that of involuntary treatment. Over the past year, I have been working on a book on forced care, along with Dr. Annette Hanson, the forensic psychiatrist who also writes this Shrink Rap News column. The work I’ve been doing for the manuscript – identifying and interviewing the people with a stake in the issue – has placed me in a funny role of being more journalist than physician. It’s a role I mostly love, and if you’ve hit the midpoint of your career and have an opportunity to dedicate some of your time to doing something completely different, I highly recommend shifting gears for a little while.
One of the things I have found most surprising is the reactions of people when I ask to include them. While most people are willing, almost all hesitate a little. Some are quite eager to participate, and one group in Richmond who uses involuntary electroconvulsive therapy heard of my project and extended an invitation for me to come visit, interview them, watch the procedure, and speak with one of their patients. Many people are proud of the work they do and eager to showcase it; they want to have their viewpoint included. With others, I have needed to ask repeatedly, listen to their concerns, and offer reassurances. I’ve taken to telling people they can read a draft of what I write about them – I learned early in the process that without this offer, few people would be willing to speak to me.
I wish I could say that I’ve noticed a pattern to who is comfortable speaking and who is not. Many of the psychiatrists and researchers I’ve approached have given their time willingly without hesitation ( or at least without that much hesitation), including Dr. E. Fuller Torrey; Dr. Paul Appelbaum; Jeffrey Swanson, Ph.D.; Dr. Steven Sharfstein; Dr. Daniel Fisher; Vermont Psychiatric Society President Margaret Bolton; Dr. Bruce Hershfield; and American Psychiatric Association President Paul Summergrad, to name just a few of the many people who have shared their time, experiences, and wisdom with me. It was not as easy for me to find a psychiatrist I could observe working on an inpatient unit, and the project might have been halted in its tracks if not for the enthusiasm of Johns Hopkins psychiatry chair Raymond DePaulo, who allowed me to shadow his team while they tended to inpatients. It was surprisingly easy to find a Crisis Intervention Team police officer to ride with, a little more effort to engage a mental health court judge.
Those who oppose forced treatment initially were more difficult to engage, but with perseverance, I was able to persuade the leadership of MindFreedom International to speak with me, and well, I ambushed a barely willing Scientologist while I was in New York for APA last May. In terms of patient participation, this hesitation did not hold true – many people volunteered to speak with me about how involuntary treatment harmed them, and it was much more difficult to find patients who felt helped by the treatment that was thrust upon them. Two absolutely wonderful women gave generously of themselves so that this project would have real voices to it: both “Lily” and “Eleanor” relived difficult experiences for me and allowed me to obtain their medical records and to speak with their families and their doctors. None of this was easy for them, but it did provide me with an education I would have gotten no other way as they reflected back on the meaning it had to them to have been committed to psychiatric units.
The subject of involuntary outpatient commitment has been particularly difficult to research, in part because I live in Maryland, a state which has no provision for this. I spoke with one family member in Arizona who initially was eager to be interviewed, along with her adult child who has come to feel that involuntary care has been very helpful. When I called back, the mom had changed her mind about participating: “You’re writing a book with a balanced view. There no balance or controversy here for me; it’s a medical problem that needs treatment. ” Unless I could promise to support, unequivocally, the views she held without qualification, she was not interested in participating in our book, even if it would provide an avenue to express her beliefs about the value of outpatient commitment. For similar reasons, I had to approach Ron Honberg, J.D., at the national office of the National Alliance on Mental Illness (NAMI); the Maryland NAMI members did not want me to speak with me after two articles I wrote for this Clinical Psychiatry News column suggested that I was not wholeheartedly in favor of outpatient commitment. I was told the topic was “too sensitive” for their members to discuss with me. So while I’ve learned that the topic inspires a great deal of emotion, there are still surprises with every step.
With all that as a prelude, I am continuing to look for people to interview who are the subjects of mandated civil outpatient treatment orders, as well as their family members. I thought perhaps readers might be able to help me, and I am interested in hearing both the good and the bad. If you, your patients, or their families would like to participate, by all means contact me at DinahMiller@yahoo.com.
Dr. Miller is a coauthor of Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: Johns Hopkins University Press, 2011).
There are many controversies in psychiatry, but the most controversial issue continues to be that of involuntary treatment. Over the past year, I have been working on a book on forced care, along with Dr. Annette Hanson, the forensic psychiatrist who also writes this Shrink Rap News column. The work I’ve been doing for the manuscript – identifying and interviewing the people with a stake in the issue – has placed me in a funny role of being more journalist than physician. It’s a role I mostly love, and if you’ve hit the midpoint of your career and have an opportunity to dedicate some of your time to doing something completely different, I highly recommend shifting gears for a little while.
One of the things I have found most surprising is the reactions of people when I ask to include them. While most people are willing, almost all hesitate a little. Some are quite eager to participate, and one group in Richmond who uses involuntary electroconvulsive therapy heard of my project and extended an invitation for me to come visit, interview them, watch the procedure, and speak with one of their patients. Many people are proud of the work they do and eager to showcase it; they want to have their viewpoint included. With others, I have needed to ask repeatedly, listen to their concerns, and offer reassurances. I’ve taken to telling people they can read a draft of what I write about them – I learned early in the process that without this offer, few people would be willing to speak to me.
I wish I could say that I’ve noticed a pattern to who is comfortable speaking and who is not. Many of the psychiatrists and researchers I’ve approached have given their time willingly without hesitation ( or at least without that much hesitation), including Dr. E. Fuller Torrey; Dr. Paul Appelbaum; Jeffrey Swanson, Ph.D.; Dr. Steven Sharfstein; Dr. Daniel Fisher; Vermont Psychiatric Society President Margaret Bolton; Dr. Bruce Hershfield; and American Psychiatric Association President Paul Summergrad, to name just a few of the many people who have shared their time, experiences, and wisdom with me. It was not as easy for me to find a psychiatrist I could observe working on an inpatient unit, and the project might have been halted in its tracks if not for the enthusiasm of Johns Hopkins psychiatry chair Raymond DePaulo, who allowed me to shadow his team while they tended to inpatients. It was surprisingly easy to find a Crisis Intervention Team police officer to ride with, a little more effort to engage a mental health court judge.
Those who oppose forced treatment initially were more difficult to engage, but with perseverance, I was able to persuade the leadership of MindFreedom International to speak with me, and well, I ambushed a barely willing Scientologist while I was in New York for APA last May. In terms of patient participation, this hesitation did not hold true – many people volunteered to speak with me about how involuntary treatment harmed them, and it was much more difficult to find patients who felt helped by the treatment that was thrust upon them. Two absolutely wonderful women gave generously of themselves so that this project would have real voices to it: both “Lily” and “Eleanor” relived difficult experiences for me and allowed me to obtain their medical records and to speak with their families and their doctors. None of this was easy for them, but it did provide me with an education I would have gotten no other way as they reflected back on the meaning it had to them to have been committed to psychiatric units.
The subject of involuntary outpatient commitment has been particularly difficult to research, in part because I live in Maryland, a state which has no provision for this. I spoke with one family member in Arizona who initially was eager to be interviewed, along with her adult child who has come to feel that involuntary care has been very helpful. When I called back, the mom had changed her mind about participating: “You’re writing a book with a balanced view. There no balance or controversy here for me; it’s a medical problem that needs treatment. ” Unless I could promise to support, unequivocally, the views she held without qualification, she was not interested in participating in our book, even if it would provide an avenue to express her beliefs about the value of outpatient commitment. For similar reasons, I had to approach Ron Honberg, J.D., at the national office of the National Alliance on Mental Illness (NAMI); the Maryland NAMI members did not want me to speak with me after two articles I wrote for this Clinical Psychiatry News column suggested that I was not wholeheartedly in favor of outpatient commitment. I was told the topic was “too sensitive” for their members to discuss with me. So while I’ve learned that the topic inspires a great deal of emotion, there are still surprises with every step.
With all that as a prelude, I am continuing to look for people to interview who are the subjects of mandated civil outpatient treatment orders, as well as their family members. I thought perhaps readers might be able to help me, and I am interested in hearing both the good and the bad. If you, your patients, or their families would like to participate, by all means contact me at DinahMiller@yahoo.com.
Dr. Miller is a coauthor of Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: Johns Hopkins University Press, 2011).
Death penalty opponents rally to protest execution date for mentally ill prisoner
According to the last Gallup poll, most Americans still favor the death penalty. Nevertheless, over the years, the number of capital-eligible defendants has been gradually whittled down because of challenges over the execution of juveniles, the intellectually disabled, and for defendants guilty of crimes other than murder. The latest challenge came up again in December, when lawyers for Texas death row inmate Scott Panetti sought a reprievealleging that he was incompetent to understand the reason for his execution.
Scott Panetti had a longstanding history of schizoaffective disorder dating back to the age of 20 years and had been hospitalized for treatment of his hallucinations and delusions at least 14 times. He once was convinced that the devil had possessed his home and had buried several valuables next to the house to “cleanse” it. His wife sought emergency intervention once when he threatened to kill her. In 1992, dressed in camouflage, he broke into the home of his estranged wife’s parents and killed them in front of her. He took his wife and young daughter hostage overnight but eventually surrendered to police.
At trial he wanted to represent himself, so the court ordered an evaluation of his competence to waive counsel. He was found competent and proceeded to present his own insanity defense to a jury. By the time of trial, he had been off medication for 2 months, and his behavior during the hearing was later described as bizarre and confusing at best. He came to court dressed in a cowboy suit, referred to himself as his alter-ego “Sarge,” and attempted to subpoena the Pope. He was convicted, in part, because jurors feared his behavior enough that they wanted to ensure he would never be released. He was sentenced to death.
Panetti received appointed counsel for his appeal after he was found incompetent to waive representation. His execution date was set in 2003, but the defense filed a motion alleging that he was incompetent to be put to death. The motion was accompanied by supporting documentation from a psychologist that Panetti did not understand the reasons for his punishment. The court appointed two experts who disagreed, stating that Panetti knew that he was about to be put to death and that he had the ability to understand the reason for the execution. They also implied that Panetti’s bizarre behavior in court was a calculated plan to present himself as insane.
Without a hearing, the court found Panetti competent. Panetti appealed to the Supreme Court, stating that under an earlier Supreme Court case, Ford v. Wainwright, he had a right to have a hearing on the competency issue, which would allow him to challenge the state’s experts and to present contrary medical evidence. The question at appeal was not whether execution of the mentally ill per se was cruel and unusual, but what standard should be applied to determine competency, and whether Texas followed the proper procedure to determine it.
Under Ford v. Wainwright, the bar was set extremely low. In order to be competent for execution, a defendant had only to know that he was being put to death, and that the death sentence was a punishment for a crime he had committed. This was a standard that required no more than intellectual or factual knowledge. Panetti was found competent to be executed because he could recite these facts. However, he disagreed with the facts: He believed that he was being executed by the state to prevent him from preaching the gospel. The Court of Appeals held that delusions alone would not necessarily mean that someone was incompetent. In 2007, the Supreme Court held in Panetti v. Quartermanthat competency requires a prisoner to have a rational as well as a factual understanding of the execution.
The American Psychiatric Association, the American Psychological Association, and the National Alliance on Mental Illness all joined to file an amicus brief on the case. In the brief, all the organizations agreed that “a prisoner is not competent to be executed if he ‘has a mental disorder or disability that significantly impairs his or her capacity to understand the nature and purpose of the punishment, or to appreciate the reason for its imposition in the prisoner’s own case.’ ” In other words, punishment is futile if the person in question doesn’t have the ability to understand that he is being punished.
The case was sent back for a formal hearing, and Panetti was again found competent. This time, the Supreme Court refused to hear his appeal. An execution date was set for Dec. 3 but was stayed 7 hours before he was to be put to death. Another competency assessment is probably on the horizon, given that 7 years have passed since the last one. The outcome this time will probably be the same, since Panetti reportedly has been on no medications for most of the last 20 years, and he has not been diagnosed with a psychotic illness in the prison system by any of the 14 mental health staff who have evaluated him.
Of course, none of this litigation to date settles the question of whether our judiciary should be executing anyone, with or without a mental illness. But until that question is settled, psychiatry will struggle along with the courts to decide exactly how ill is too ill to die.
Dr. Hanson is a forensic psychiatrist and coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work.” The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
According to the last Gallup poll, most Americans still favor the death penalty. Nevertheless, over the years, the number of capital-eligible defendants has been gradually whittled down because of challenges over the execution of juveniles, the intellectually disabled, and for defendants guilty of crimes other than murder. The latest challenge came up again in December, when lawyers for Texas death row inmate Scott Panetti sought a reprievealleging that he was incompetent to understand the reason for his execution.
Scott Panetti had a longstanding history of schizoaffective disorder dating back to the age of 20 years and had been hospitalized for treatment of his hallucinations and delusions at least 14 times. He once was convinced that the devil had possessed his home and had buried several valuables next to the house to “cleanse” it. His wife sought emergency intervention once when he threatened to kill her. In 1992, dressed in camouflage, he broke into the home of his estranged wife’s parents and killed them in front of her. He took his wife and young daughter hostage overnight but eventually surrendered to police.
At trial he wanted to represent himself, so the court ordered an evaluation of his competence to waive counsel. He was found competent and proceeded to present his own insanity defense to a jury. By the time of trial, he had been off medication for 2 months, and his behavior during the hearing was later described as bizarre and confusing at best. He came to court dressed in a cowboy suit, referred to himself as his alter-ego “Sarge,” and attempted to subpoena the Pope. He was convicted, in part, because jurors feared his behavior enough that they wanted to ensure he would never be released. He was sentenced to death.
Panetti received appointed counsel for his appeal after he was found incompetent to waive representation. His execution date was set in 2003, but the defense filed a motion alleging that he was incompetent to be put to death. The motion was accompanied by supporting documentation from a psychologist that Panetti did not understand the reasons for his punishment. The court appointed two experts who disagreed, stating that Panetti knew that he was about to be put to death and that he had the ability to understand the reason for the execution. They also implied that Panetti’s bizarre behavior in court was a calculated plan to present himself as insane.
Without a hearing, the court found Panetti competent. Panetti appealed to the Supreme Court, stating that under an earlier Supreme Court case, Ford v. Wainwright, he had a right to have a hearing on the competency issue, which would allow him to challenge the state’s experts and to present contrary medical evidence. The question at appeal was not whether execution of the mentally ill per se was cruel and unusual, but what standard should be applied to determine competency, and whether Texas followed the proper procedure to determine it.
Under Ford v. Wainwright, the bar was set extremely low. In order to be competent for execution, a defendant had only to know that he was being put to death, and that the death sentence was a punishment for a crime he had committed. This was a standard that required no more than intellectual or factual knowledge. Panetti was found competent to be executed because he could recite these facts. However, he disagreed with the facts: He believed that he was being executed by the state to prevent him from preaching the gospel. The Court of Appeals held that delusions alone would not necessarily mean that someone was incompetent. In 2007, the Supreme Court held in Panetti v. Quartermanthat competency requires a prisoner to have a rational as well as a factual understanding of the execution.
The American Psychiatric Association, the American Psychological Association, and the National Alliance on Mental Illness all joined to file an amicus brief on the case. In the brief, all the organizations agreed that “a prisoner is not competent to be executed if he ‘has a mental disorder or disability that significantly impairs his or her capacity to understand the nature and purpose of the punishment, or to appreciate the reason for its imposition in the prisoner’s own case.’ ” In other words, punishment is futile if the person in question doesn’t have the ability to understand that he is being punished.
The case was sent back for a formal hearing, and Panetti was again found competent. This time, the Supreme Court refused to hear his appeal. An execution date was set for Dec. 3 but was stayed 7 hours before he was to be put to death. Another competency assessment is probably on the horizon, given that 7 years have passed since the last one. The outcome this time will probably be the same, since Panetti reportedly has been on no medications for most of the last 20 years, and he has not been diagnosed with a psychotic illness in the prison system by any of the 14 mental health staff who have evaluated him.
Of course, none of this litigation to date settles the question of whether our judiciary should be executing anyone, with or without a mental illness. But until that question is settled, psychiatry will struggle along with the courts to decide exactly how ill is too ill to die.
Dr. Hanson is a forensic psychiatrist and coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work.” The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
According to the last Gallup poll, most Americans still favor the death penalty. Nevertheless, over the years, the number of capital-eligible defendants has been gradually whittled down because of challenges over the execution of juveniles, the intellectually disabled, and for defendants guilty of crimes other than murder. The latest challenge came up again in December, when lawyers for Texas death row inmate Scott Panetti sought a reprievealleging that he was incompetent to understand the reason for his execution.
Scott Panetti had a longstanding history of schizoaffective disorder dating back to the age of 20 years and had been hospitalized for treatment of his hallucinations and delusions at least 14 times. He once was convinced that the devil had possessed his home and had buried several valuables next to the house to “cleanse” it. His wife sought emergency intervention once when he threatened to kill her. In 1992, dressed in camouflage, he broke into the home of his estranged wife’s parents and killed them in front of her. He took his wife and young daughter hostage overnight but eventually surrendered to police.
At trial he wanted to represent himself, so the court ordered an evaluation of his competence to waive counsel. He was found competent and proceeded to present his own insanity defense to a jury. By the time of trial, he had been off medication for 2 months, and his behavior during the hearing was later described as bizarre and confusing at best. He came to court dressed in a cowboy suit, referred to himself as his alter-ego “Sarge,” and attempted to subpoena the Pope. He was convicted, in part, because jurors feared his behavior enough that they wanted to ensure he would never be released. He was sentenced to death.
Panetti received appointed counsel for his appeal after he was found incompetent to waive representation. His execution date was set in 2003, but the defense filed a motion alleging that he was incompetent to be put to death. The motion was accompanied by supporting documentation from a psychologist that Panetti did not understand the reasons for his punishment. The court appointed two experts who disagreed, stating that Panetti knew that he was about to be put to death and that he had the ability to understand the reason for the execution. They also implied that Panetti’s bizarre behavior in court was a calculated plan to present himself as insane.
Without a hearing, the court found Panetti competent. Panetti appealed to the Supreme Court, stating that under an earlier Supreme Court case, Ford v. Wainwright, he had a right to have a hearing on the competency issue, which would allow him to challenge the state’s experts and to present contrary medical evidence. The question at appeal was not whether execution of the mentally ill per se was cruel and unusual, but what standard should be applied to determine competency, and whether Texas followed the proper procedure to determine it.
Under Ford v. Wainwright, the bar was set extremely low. In order to be competent for execution, a defendant had only to know that he was being put to death, and that the death sentence was a punishment for a crime he had committed. This was a standard that required no more than intellectual or factual knowledge. Panetti was found competent to be executed because he could recite these facts. However, he disagreed with the facts: He believed that he was being executed by the state to prevent him from preaching the gospel. The Court of Appeals held that delusions alone would not necessarily mean that someone was incompetent. In 2007, the Supreme Court held in Panetti v. Quartermanthat competency requires a prisoner to have a rational as well as a factual understanding of the execution.
The American Psychiatric Association, the American Psychological Association, and the National Alliance on Mental Illness all joined to file an amicus brief on the case. In the brief, all the organizations agreed that “a prisoner is not competent to be executed if he ‘has a mental disorder or disability that significantly impairs his or her capacity to understand the nature and purpose of the punishment, or to appreciate the reason for its imposition in the prisoner’s own case.’ ” In other words, punishment is futile if the person in question doesn’t have the ability to understand that he is being punished.
The case was sent back for a formal hearing, and Panetti was again found competent. This time, the Supreme Court refused to hear his appeal. An execution date was set for Dec. 3 but was stayed 7 hours before he was to be put to death. Another competency assessment is probably on the horizon, given that 7 years have passed since the last one. The outcome this time will probably be the same, since Panetti reportedly has been on no medications for most of the last 20 years, and he has not been diagnosed with a psychotic illness in the prison system by any of the 14 mental health staff who have evaluated him.
Of course, none of this litigation to date settles the question of whether our judiciary should be executing anyone, with or without a mental illness. But until that question is settled, psychiatry will struggle along with the courts to decide exactly how ill is too ill to die.
Dr. Hanson is a forensic psychiatrist and coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work.” The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Shrink Rap News: Correctional health care costs are worth defending
One serious problem with being an advocate of correctional mental health services is that you run the risk of coming across as an apologist, a Pollyanna, or a defender of the status quo. This is true even though every week I meet someone with an addiction problem so severe that he’d be unable to voluntarily seek or stay in treatment in the community. For someone like that, an arrest can be lifesaving. But to point this out will lead people to believe that I must oppose ready access to community care, pretrial diversion, alternative sentencing, mental health courts, or anything related to alternatives to incarceration.
That isn’t the case. Many problems require more than one solution. What I oppose is the idea that the solution has to be a simple dichotomous choice between arrest and incarceration versus community care. I’ve found discussions about criminalization of people with mental illnesses to be polarizing and unproductive. There will always be people with mental illnesses in jail and prison, because – like people with diabetes, heart disease, or AIDS – they sometimes commit very serious crimes. As a care provider, my view is that a patient’s need for treatment is independent of criminal culpability. An ill person deserves appropriate and skilled health care, regardless of the treatment setting. Moving someone from an understaffed, overcrowded correctional facility to an understaffed, overcrowded state hospital hardly solves the problem.
People make the argument that money spent on corrections would be better spent elsewhere, on services for at-risk youth, or on community substance abuse and mental health programs. I agree that all these programs are needed, but what rarely gets mentioned is that when money is diverted from jails and prisons, part of that money also includes funding for inmate health care. Taking away this money is like stealing a coat from a blind beggar in the winter time. If you want to make a serious problem worse, by all means, take away what little we have.
How much money are we talking here, anyway?
By some estimates, the money spent on health care for all American prisons is about $7.7 billion per year. That includes physician and related health care professional costs, laboratory and diagnostic testing, hospitalization costs, as well as medications. Fourteen percent of that, or about $1 billion, goes to mental health care. Those costs are expected to rise as the prison population continues to age. Meanwhile, federal spending on mandatory health care programs in 2013 was about $1 trillion. When the prison health care budget represents less than 1% of health care spending nationally, this doesn’t seem to be enough to be quibbling about and certainly not enough to be cutting or diverting elsewhere.
But of course, the correctional nihilists will respond, “You get what you pay for.” Inevitably, low-cost care becomes equivalent to low-quality care in the eyes of many Americans. But if you compare American medical outcomes globally, it’s been well established that we have fallen behind many countries in life expectancy and infant mortality, despite heavy investment in a broad spectrum of services and interventions.
Let’s compare that to prison. Because of data gathered through the 2000 Federal Death in Custody Reporting Act, as well as other studies, prisons have been able to demonstrate reduced mortality, compared with age-matched men in free society, particularly for minorities. That mortality rate doubles after release. Clearly, prisons appear to be keeping people alive more efficiently and at a fraction of the cost of our community services.
This is not to imply that incarceration should be the answer to every social problem. This is my response to the naysayers and nihilists who believe that jails and prisons are so far gone they are not worth investing in. The lives of many prisoners depend on that investment.
Dr. Hanson is a forensic psychiatrist and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
One serious problem with being an advocate of correctional mental health services is that you run the risk of coming across as an apologist, a Pollyanna, or a defender of the status quo. This is true even though every week I meet someone with an addiction problem so severe that he’d be unable to voluntarily seek or stay in treatment in the community. For someone like that, an arrest can be lifesaving. But to point this out will lead people to believe that I must oppose ready access to community care, pretrial diversion, alternative sentencing, mental health courts, or anything related to alternatives to incarceration.
That isn’t the case. Many problems require more than one solution. What I oppose is the idea that the solution has to be a simple dichotomous choice between arrest and incarceration versus community care. I’ve found discussions about criminalization of people with mental illnesses to be polarizing and unproductive. There will always be people with mental illnesses in jail and prison, because – like people with diabetes, heart disease, or AIDS – they sometimes commit very serious crimes. As a care provider, my view is that a patient’s need for treatment is independent of criminal culpability. An ill person deserves appropriate and skilled health care, regardless of the treatment setting. Moving someone from an understaffed, overcrowded correctional facility to an understaffed, overcrowded state hospital hardly solves the problem.
People make the argument that money spent on corrections would be better spent elsewhere, on services for at-risk youth, or on community substance abuse and mental health programs. I agree that all these programs are needed, but what rarely gets mentioned is that when money is diverted from jails and prisons, part of that money also includes funding for inmate health care. Taking away this money is like stealing a coat from a blind beggar in the winter time. If you want to make a serious problem worse, by all means, take away what little we have.
How much money are we talking here, anyway?
By some estimates, the money spent on health care for all American prisons is about $7.7 billion per year. That includes physician and related health care professional costs, laboratory and diagnostic testing, hospitalization costs, as well as medications. Fourteen percent of that, or about $1 billion, goes to mental health care. Those costs are expected to rise as the prison population continues to age. Meanwhile, federal spending on mandatory health care programs in 2013 was about $1 trillion. When the prison health care budget represents less than 1% of health care spending nationally, this doesn’t seem to be enough to be quibbling about and certainly not enough to be cutting or diverting elsewhere.
But of course, the correctional nihilists will respond, “You get what you pay for.” Inevitably, low-cost care becomes equivalent to low-quality care in the eyes of many Americans. But if you compare American medical outcomes globally, it’s been well established that we have fallen behind many countries in life expectancy and infant mortality, despite heavy investment in a broad spectrum of services and interventions.
Let’s compare that to prison. Because of data gathered through the 2000 Federal Death in Custody Reporting Act, as well as other studies, prisons have been able to demonstrate reduced mortality, compared with age-matched men in free society, particularly for minorities. That mortality rate doubles after release. Clearly, prisons appear to be keeping people alive more efficiently and at a fraction of the cost of our community services.
This is not to imply that incarceration should be the answer to every social problem. This is my response to the naysayers and nihilists who believe that jails and prisons are so far gone they are not worth investing in. The lives of many prisoners depend on that investment.
Dr. Hanson is a forensic psychiatrist and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
One serious problem with being an advocate of correctional mental health services is that you run the risk of coming across as an apologist, a Pollyanna, or a defender of the status quo. This is true even though every week I meet someone with an addiction problem so severe that he’d be unable to voluntarily seek or stay in treatment in the community. For someone like that, an arrest can be lifesaving. But to point this out will lead people to believe that I must oppose ready access to community care, pretrial diversion, alternative sentencing, mental health courts, or anything related to alternatives to incarceration.
That isn’t the case. Many problems require more than one solution. What I oppose is the idea that the solution has to be a simple dichotomous choice between arrest and incarceration versus community care. I’ve found discussions about criminalization of people with mental illnesses to be polarizing and unproductive. There will always be people with mental illnesses in jail and prison, because – like people with diabetes, heart disease, or AIDS – they sometimes commit very serious crimes. As a care provider, my view is that a patient’s need for treatment is independent of criminal culpability. An ill person deserves appropriate and skilled health care, regardless of the treatment setting. Moving someone from an understaffed, overcrowded correctional facility to an understaffed, overcrowded state hospital hardly solves the problem.
People make the argument that money spent on corrections would be better spent elsewhere, on services for at-risk youth, or on community substance abuse and mental health programs. I agree that all these programs are needed, but what rarely gets mentioned is that when money is diverted from jails and prisons, part of that money also includes funding for inmate health care. Taking away this money is like stealing a coat from a blind beggar in the winter time. If you want to make a serious problem worse, by all means, take away what little we have.
How much money are we talking here, anyway?
By some estimates, the money spent on health care for all American prisons is about $7.7 billion per year. That includes physician and related health care professional costs, laboratory and diagnostic testing, hospitalization costs, as well as medications. Fourteen percent of that, or about $1 billion, goes to mental health care. Those costs are expected to rise as the prison population continues to age. Meanwhile, federal spending on mandatory health care programs in 2013 was about $1 trillion. When the prison health care budget represents less than 1% of health care spending nationally, this doesn’t seem to be enough to be quibbling about and certainly not enough to be cutting or diverting elsewhere.
But of course, the correctional nihilists will respond, “You get what you pay for.” Inevitably, low-cost care becomes equivalent to low-quality care in the eyes of many Americans. But if you compare American medical outcomes globally, it’s been well established that we have fallen behind many countries in life expectancy and infant mortality, despite heavy investment in a broad spectrum of services and interventions.
Let’s compare that to prison. Because of data gathered through the 2000 Federal Death in Custody Reporting Act, as well as other studies, prisons have been able to demonstrate reduced mortality, compared with age-matched men in free society, particularly for minorities. That mortality rate doubles after release. Clearly, prisons appear to be keeping people alive more efficiently and at a fraction of the cost of our community services.
This is not to imply that incarceration should be the answer to every social problem. This is my response to the naysayers and nihilists who believe that jails and prisons are so far gone they are not worth investing in. The lives of many prisoners depend on that investment.
Dr. Hanson is a forensic psychiatrist and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Shrink Rap News: The surprisingly high cost of Abilify
Recently, I gave a patient a prescription for Abilify. I wrote for 30 tablets of the lowest dose, 2 mg. While I knew it was expensive, I was shocked when the patient returned a few days later and told me it had cost $1,100 to fill the prescription; he not yet met the deductible for his health insurance and he had paid cash for the medication.
According to Medscape (and Twitter, too), Abilify is the medication that grosses more money than any other pharmaceutical in the United States. In the 12-month period from July 2013 to June 2014, sales of Abilify totaled $7.2 billion. An atypical antipsychotic medication that is widely marketed to TV viewers as an augmenting agent to treat major depression, Abilify is the 14th most-prescribed medication in the United States. If you’re wondering, the most prescribed medications are Synthroid, Crestor, and Nexium. Abilify has been available in this country since 2002, initially with an indication for schizophrenia. Since then, indications have expanded to include bipolar disorder, irritability in autism, as well as augmentation for major depression.
Still, $1,100 for 30 tablets? I wondered if the high cost was attributed to where the patient went – a boutique independent pharmacy. I decided to make some calls to local pharmacists (see the table), and queried druggists at CVS, Walmart, and Lykos, an independent pharmacy in Towson, Md. I also checked with a Walmart in Vermont to see if the prices were the same in another part of the country, and they were. Let me share with you what I learned.
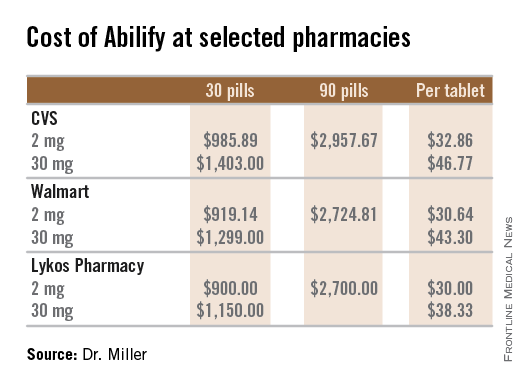
For the three pharmacies I called, a single 2-mg tablet of Abilify cost between $30 and $33, so the cost was less than the $1,100 my patient paid. There is no discount for buying in bulk, and the price per pill stays virtually the same whether a patient buys 1 pill, 30 pills, or 90 pills. I checked with two pharmacies, and the price for a tablet is the same for the dosages of 2 mg, 5 mg, 10 mg, and 15 mg. The price rises to $38-$47 per pill for the 20-mg and 30-mg dose.
As physicians in a health care system where resources are limited, it is incumbent upon us to at least consider the cost of the tests and treatments we order, but we often have no way of knowing what these costs actually are. Was I missing something? Is everyone else aware that Abilify is this costly? I did a quick survey of a handful of psychiatrists by text message (please don’t count this as science), requesting a guess for the cost of a single 2-mg tablet of Abilify. The responses I received ranged from $7 to $20, and a lone respondent answered $40. For the most part, the cost of medications remains opaque to the prescriber.
If I had to do it again, I still would have prescribed Abilify to this particular patient. I would have suggested he buy only a few tablets to start, and I would have prescribed the 5-mg dose and recommended splitting the pills to halve the cost. In a December 2006 article in Current Psychiatry, “Pros and cons of pill splitting,” Dr. Rakesh Jain and Dr. Shailesh Jain note that it is safe to divide Abilify tablets. Filling only a few tablets seems like the prudent thing to do with such an expensive medication, at least until it is clear that it is tolerable to the patient, but as we know, filling less than a month’s supply often creates hurdles and increased copays when health insurance is paying for the prescription. And with requirements for preauthorization, I’m not certain if it’s even possible for a patient to take home just a few to try.
When I informed the psychiatrists I queried that Abilify costs $30-$33 per 2-mg dose, they expressed their surprise. One friend, however, put it most aptly with her reply of simply, “Good grief.”
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Recently, I gave a patient a prescription for Abilify. I wrote for 30 tablets of the lowest dose, 2 mg. While I knew it was expensive, I was shocked when the patient returned a few days later and told me it had cost $1,100 to fill the prescription; he not yet met the deductible for his health insurance and he had paid cash for the medication.
According to Medscape (and Twitter, too), Abilify is the medication that grosses more money than any other pharmaceutical in the United States. In the 12-month period from July 2013 to June 2014, sales of Abilify totaled $7.2 billion. An atypical antipsychotic medication that is widely marketed to TV viewers as an augmenting agent to treat major depression, Abilify is the 14th most-prescribed medication in the United States. If you’re wondering, the most prescribed medications are Synthroid, Crestor, and Nexium. Abilify has been available in this country since 2002, initially with an indication for schizophrenia. Since then, indications have expanded to include bipolar disorder, irritability in autism, as well as augmentation for major depression.
Still, $1,100 for 30 tablets? I wondered if the high cost was attributed to where the patient went – a boutique independent pharmacy. I decided to make some calls to local pharmacists (see the table), and queried druggists at CVS, Walmart, and Lykos, an independent pharmacy in Towson, Md. I also checked with a Walmart in Vermont to see if the prices were the same in another part of the country, and they were. Let me share with you what I learned.
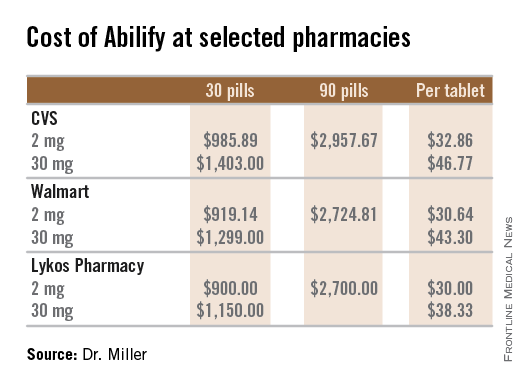
For the three pharmacies I called, a single 2-mg tablet of Abilify cost between $30 and $33, so the cost was less than the $1,100 my patient paid. There is no discount for buying in bulk, and the price per pill stays virtually the same whether a patient buys 1 pill, 30 pills, or 90 pills. I checked with two pharmacies, and the price for a tablet is the same for the dosages of 2 mg, 5 mg, 10 mg, and 15 mg. The price rises to $38-$47 per pill for the 20-mg and 30-mg dose.
As physicians in a health care system where resources are limited, it is incumbent upon us to at least consider the cost of the tests and treatments we order, but we often have no way of knowing what these costs actually are. Was I missing something? Is everyone else aware that Abilify is this costly? I did a quick survey of a handful of psychiatrists by text message (please don’t count this as science), requesting a guess for the cost of a single 2-mg tablet of Abilify. The responses I received ranged from $7 to $20, and a lone respondent answered $40. For the most part, the cost of medications remains opaque to the prescriber.
If I had to do it again, I still would have prescribed Abilify to this particular patient. I would have suggested he buy only a few tablets to start, and I would have prescribed the 5-mg dose and recommended splitting the pills to halve the cost. In a December 2006 article in Current Psychiatry, “Pros and cons of pill splitting,” Dr. Rakesh Jain and Dr. Shailesh Jain note that it is safe to divide Abilify tablets. Filling only a few tablets seems like the prudent thing to do with such an expensive medication, at least until it is clear that it is tolerable to the patient, but as we know, filling less than a month’s supply often creates hurdles and increased copays when health insurance is paying for the prescription. And with requirements for preauthorization, I’m not certain if it’s even possible for a patient to take home just a few to try.
When I informed the psychiatrists I queried that Abilify costs $30-$33 per 2-mg dose, they expressed their surprise. One friend, however, put it most aptly with her reply of simply, “Good grief.”
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Recently, I gave a patient a prescription for Abilify. I wrote for 30 tablets of the lowest dose, 2 mg. While I knew it was expensive, I was shocked when the patient returned a few days later and told me it had cost $1,100 to fill the prescription; he not yet met the deductible for his health insurance and he had paid cash for the medication.
According to Medscape (and Twitter, too), Abilify is the medication that grosses more money than any other pharmaceutical in the United States. In the 12-month period from July 2013 to June 2014, sales of Abilify totaled $7.2 billion. An atypical antipsychotic medication that is widely marketed to TV viewers as an augmenting agent to treat major depression, Abilify is the 14th most-prescribed medication in the United States. If you’re wondering, the most prescribed medications are Synthroid, Crestor, and Nexium. Abilify has been available in this country since 2002, initially with an indication for schizophrenia. Since then, indications have expanded to include bipolar disorder, irritability in autism, as well as augmentation for major depression.
Still, $1,100 for 30 tablets? I wondered if the high cost was attributed to where the patient went – a boutique independent pharmacy. I decided to make some calls to local pharmacists (see the table), and queried druggists at CVS, Walmart, and Lykos, an independent pharmacy in Towson, Md. I also checked with a Walmart in Vermont to see if the prices were the same in another part of the country, and they were. Let me share with you what I learned.
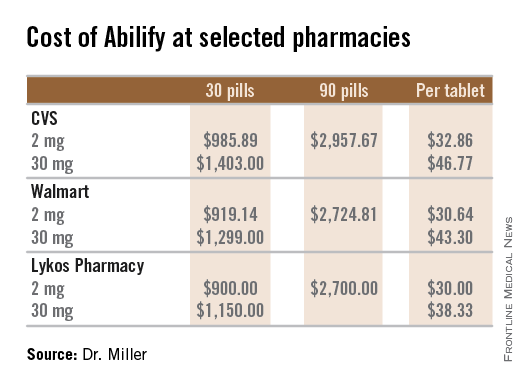
For the three pharmacies I called, a single 2-mg tablet of Abilify cost between $30 and $33, so the cost was less than the $1,100 my patient paid. There is no discount for buying in bulk, and the price per pill stays virtually the same whether a patient buys 1 pill, 30 pills, or 90 pills. I checked with two pharmacies, and the price for a tablet is the same for the dosages of 2 mg, 5 mg, 10 mg, and 15 mg. The price rises to $38-$47 per pill for the 20-mg and 30-mg dose.
As physicians in a health care system where resources are limited, it is incumbent upon us to at least consider the cost of the tests and treatments we order, but we often have no way of knowing what these costs actually are. Was I missing something? Is everyone else aware that Abilify is this costly? I did a quick survey of a handful of psychiatrists by text message (please don’t count this as science), requesting a guess for the cost of a single 2-mg tablet of Abilify. The responses I received ranged from $7 to $20, and a lone respondent answered $40. For the most part, the cost of medications remains opaque to the prescriber.
If I had to do it again, I still would have prescribed Abilify to this particular patient. I would have suggested he buy only a few tablets to start, and I would have prescribed the 5-mg dose and recommended splitting the pills to halve the cost. In a December 2006 article in Current Psychiatry, “Pros and cons of pill splitting,” Dr. Rakesh Jain and Dr. Shailesh Jain note that it is safe to divide Abilify tablets. Filling only a few tablets seems like the prudent thing to do with such an expensive medication, at least until it is clear that it is tolerable to the patient, but as we know, filling less than a month’s supply often creates hurdles and increased copays when health insurance is paying for the prescription. And with requirements for preauthorization, I’m not certain if it’s even possible for a patient to take home just a few to try.
When I informed the psychiatrists I queried that Abilify costs $30-$33 per 2-mg dose, they expressed their surprise. One friend, however, put it most aptly with her reply of simply, “Good grief.”
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Shrink Rap News: California hospital system offers new resource for treating violence
For a clinician working in a forensic setting, the assessment and management of violence is a core clinical skill. Unfortunately, evidence-based practices are often lacking for those patients with serious, treatment-resistant psychoses who defy current guidelines, or for those with severe personality disorders.
This is why I was pleased to see a new resource put out by the California Department of State Hospitals entitled, appropriately enough, the California State Hospital Violence Assessment and Treatment (Cal-VAT) guidelines (CNS Spectrums 2014;19:449-65). The authors, led by Dr. Stephen M. Stahl, are respected experts in forensic psychiatry, psychopharmacology, and psychology. The document is a thorough and thoughtfully organized work that can be employed in both forensic and nonforensic settings.
Too often, the general public will view violence as the sine qua non of mental illness. Rather, violence is often attributable to an amalgam of risk factors, and even the best psychiatrist can be hard-pressed to tease out which aspect is the predominant driving force behind aggressive behavior. Dr. Stahl and his colleagues do an excellent job laying out the most common etiologies: psychosis and disorders associated with impulsivity, psychopathy, medical conditions, and adverse reactions to medication. They provide a structured and logical approach to pharmacologic management, complete with flowcharts and a discussion of general treatment principles relevant to each etiology. They suggest both primary or acute pharmacologic interventions as well as adjunctive therapies and long-term treatment options.
Compared with other papers I’ve read related to the treatment of violence, the Cal-VAT provides a more comprehensive approach by also considering environmental and staffing factors that contribute to violence, and by outlining nonpharmacologic strategies. I found these additional considerations to be just as important as the prescribing recommendations, so much so that I wanted to emphasize them in this column. Understaffing, high staff turnover, inexperience, and inadequate staff training will affect both morale and unit safety. The Cal-VAT guidelines recommend peer support for colleagues as well as postincident opportunities for staff to process violent incidents by patients. Training in de-escalation techniques and violence prevention, as well as good communication between team members, also can minimize the level of tension on a ward.
I was somewhat more skeptical regarding recommendations for the management of predatory aggression, but again, the Cal-VAT cautions that treatment gains in this domain might be modest or nonexistent. I strongly agree with the need for treatment in a highly structured environment for patients high in sociopathy, along with consistent strong boundaries and close external supervision. Good communication between security and clinical staff is also essential.
The guidelines were developed for hospitals, and in a hospital setting, security measures like management of contraband or adequate security staff are just as important as in the correctional setting. However, some of the recommendations in the Cal-VAT may not be practical for a correctional setting, where formularies may be limited and there may not be a means for providing PRN medication. For example, the use of clozapine in a correctional setting may not be practical when weekly blood draws can’t be guaranteed. Nevertheless, the guidelines provide a useful framework for risk assessment and violence risk management.
The Cal-VAT assumes that there are options for moving a patient to a higher level of care within a facility when the violence risk becomes too great. Given that many public hospitals now have a high proportion of forensic patients, a change in ward may not be sufficient to manage this risk. As a profession, we can move violence management forward by addressing this last remaining barrier – the resistance some systems put up against accepting the difficult-to-treat patient. Correctional facilities should be willing to provide the treatment resources needed for mentally ill prisoners high in sociopathy, and hospitals must be equally willing to accept severely ill offenders who cannot be medicated within a jail or prison. For a full spectrum of care, violence management requires a system-level commitment by both public mental health and corrections.
Dr. Hanson is a forensic psychiatrist and coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work.” The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
For a clinician working in a forensic setting, the assessment and management of violence is a core clinical skill. Unfortunately, evidence-based practices are often lacking for those patients with serious, treatment-resistant psychoses who defy current guidelines, or for those with severe personality disorders.
This is why I was pleased to see a new resource put out by the California Department of State Hospitals entitled, appropriately enough, the California State Hospital Violence Assessment and Treatment (Cal-VAT) guidelines (CNS Spectrums 2014;19:449-65). The authors, led by Dr. Stephen M. Stahl, are respected experts in forensic psychiatry, psychopharmacology, and psychology. The document is a thorough and thoughtfully organized work that can be employed in both forensic and nonforensic settings.
Too often, the general public will view violence as the sine qua non of mental illness. Rather, violence is often attributable to an amalgam of risk factors, and even the best psychiatrist can be hard-pressed to tease out which aspect is the predominant driving force behind aggressive behavior. Dr. Stahl and his colleagues do an excellent job laying out the most common etiologies: psychosis and disorders associated with impulsivity, psychopathy, medical conditions, and adverse reactions to medication. They provide a structured and logical approach to pharmacologic management, complete with flowcharts and a discussion of general treatment principles relevant to each etiology. They suggest both primary or acute pharmacologic interventions as well as adjunctive therapies and long-term treatment options.
Compared with other papers I’ve read related to the treatment of violence, the Cal-VAT provides a more comprehensive approach by also considering environmental and staffing factors that contribute to violence, and by outlining nonpharmacologic strategies. I found these additional considerations to be just as important as the prescribing recommendations, so much so that I wanted to emphasize them in this column. Understaffing, high staff turnover, inexperience, and inadequate staff training will affect both morale and unit safety. The Cal-VAT guidelines recommend peer support for colleagues as well as postincident opportunities for staff to process violent incidents by patients. Training in de-escalation techniques and violence prevention, as well as good communication between team members, also can minimize the level of tension on a ward.
I was somewhat more skeptical regarding recommendations for the management of predatory aggression, but again, the Cal-VAT cautions that treatment gains in this domain might be modest or nonexistent. I strongly agree with the need for treatment in a highly structured environment for patients high in sociopathy, along with consistent strong boundaries and close external supervision. Good communication between security and clinical staff is also essential.
The guidelines were developed for hospitals, and in a hospital setting, security measures like management of contraband or adequate security staff are just as important as in the correctional setting. However, some of the recommendations in the Cal-VAT may not be practical for a correctional setting, where formularies may be limited and there may not be a means for providing PRN medication. For example, the use of clozapine in a correctional setting may not be practical when weekly blood draws can’t be guaranteed. Nevertheless, the guidelines provide a useful framework for risk assessment and violence risk management.
The Cal-VAT assumes that there are options for moving a patient to a higher level of care within a facility when the violence risk becomes too great. Given that many public hospitals now have a high proportion of forensic patients, a change in ward may not be sufficient to manage this risk. As a profession, we can move violence management forward by addressing this last remaining barrier – the resistance some systems put up against accepting the difficult-to-treat patient. Correctional facilities should be willing to provide the treatment resources needed for mentally ill prisoners high in sociopathy, and hospitals must be equally willing to accept severely ill offenders who cannot be medicated within a jail or prison. For a full spectrum of care, violence management requires a system-level commitment by both public mental health and corrections.
Dr. Hanson is a forensic psychiatrist and coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work.” The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
For a clinician working in a forensic setting, the assessment and management of violence is a core clinical skill. Unfortunately, evidence-based practices are often lacking for those patients with serious, treatment-resistant psychoses who defy current guidelines, or for those with severe personality disorders.
This is why I was pleased to see a new resource put out by the California Department of State Hospitals entitled, appropriately enough, the California State Hospital Violence Assessment and Treatment (Cal-VAT) guidelines (CNS Spectrums 2014;19:449-65). The authors, led by Dr. Stephen M. Stahl, are respected experts in forensic psychiatry, psychopharmacology, and psychology. The document is a thorough and thoughtfully organized work that can be employed in both forensic and nonforensic settings.
Too often, the general public will view violence as the sine qua non of mental illness. Rather, violence is often attributable to an amalgam of risk factors, and even the best psychiatrist can be hard-pressed to tease out which aspect is the predominant driving force behind aggressive behavior. Dr. Stahl and his colleagues do an excellent job laying out the most common etiologies: psychosis and disorders associated with impulsivity, psychopathy, medical conditions, and adverse reactions to medication. They provide a structured and logical approach to pharmacologic management, complete with flowcharts and a discussion of general treatment principles relevant to each etiology. They suggest both primary or acute pharmacologic interventions as well as adjunctive therapies and long-term treatment options.
Compared with other papers I’ve read related to the treatment of violence, the Cal-VAT provides a more comprehensive approach by also considering environmental and staffing factors that contribute to violence, and by outlining nonpharmacologic strategies. I found these additional considerations to be just as important as the prescribing recommendations, so much so that I wanted to emphasize them in this column. Understaffing, high staff turnover, inexperience, and inadequate staff training will affect both morale and unit safety. The Cal-VAT guidelines recommend peer support for colleagues as well as postincident opportunities for staff to process violent incidents by patients. Training in de-escalation techniques and violence prevention, as well as good communication between team members, also can minimize the level of tension on a ward.
I was somewhat more skeptical regarding recommendations for the management of predatory aggression, but again, the Cal-VAT cautions that treatment gains in this domain might be modest or nonexistent. I strongly agree with the need for treatment in a highly structured environment for patients high in sociopathy, along with consistent strong boundaries and close external supervision. Good communication between security and clinical staff is also essential.
The guidelines were developed for hospitals, and in a hospital setting, security measures like management of contraband or adequate security staff are just as important as in the correctional setting. However, some of the recommendations in the Cal-VAT may not be practical for a correctional setting, where formularies may be limited and there may not be a means for providing PRN medication. For example, the use of clozapine in a correctional setting may not be practical when weekly blood draws can’t be guaranteed. Nevertheless, the guidelines provide a useful framework for risk assessment and violence risk management.
The Cal-VAT assumes that there are options for moving a patient to a higher level of care within a facility when the violence risk becomes too great. Given that many public hospitals now have a high proportion of forensic patients, a change in ward may not be sufficient to manage this risk. As a profession, we can move violence management forward by addressing this last remaining barrier – the resistance some systems put up against accepting the difficult-to-treat patient. Correctional facilities should be willing to provide the treatment resources needed for mentally ill prisoners high in sociopathy, and hospitals must be equally willing to accept severely ill offenders who cannot be medicated within a jail or prison. For a full spectrum of care, violence management requires a system-level commitment by both public mental health and corrections.
Dr. Hanson is a forensic psychiatrist and coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work.” The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Shrink Rap News: Helping patients access outpatient psychiatric care
How often does someone ask you for help in getting an appointment with a psychiatrist? With the “double expansion” in access to mental health care – because of the Mental Health Parity and Addiction Equity Act, and the Affordable Care Act (ACA) – many more people are seeking help for mental health and substance use problems. But without more practitioners being produced, the waiting lists are getting longer.
A recent study found that 40% (146 of 360) of psychiatrists listed on insurance plans in three states could not be reached. Of the 214 who were reachable, 43% were unavailable, either because the psychiatrists were not accepting new patients or because they did not treat adult outpatients (e.g., inpatient only). Of the 123 psychiatrists left, the callers were able to schedule appointments with 93 (76%) of them. These results are similar to a 2007 study, where 44% of mental health professionals from seven health plans were unreachable.
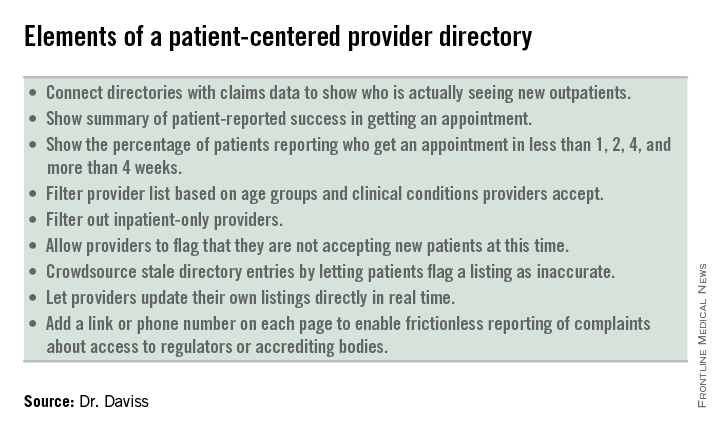
Problems with access to psychiatric care is not a new problem. Mental health carve-outs are used by managed care organizations (MCOs) to manage the mental health benefits, but create inefficiency in claims management and clinical care coordination. While this model seems to be losing popularity, these managed behavioral health organizations (MBHOs) often do not integrate well with the MCO, may not share the same standards for network adequacy, and often have different provider directories from those of the MCO, making it more complex for patients to access providers.
While the Parity Act has somewhat improved the problem of rate disparities, the historically low rates paid to psychiatrists by MBHOs have led to high levels of insurance nonparticipation, as much as 50%. Compounding this problem is the fact that plan members often find it hard to access those practitioners who do participate with their insurance.
The Maryland Psychological Association conducted in 2007 with Open Minds a “secret shopper” survey of more than 900 behavioral health providers from seven different online carrier directories in Maryland. Their goal was to assess the extent to which problems with access to care were related to inadequate insurance provider directories.
They found that 44% of the listed providers were unreachable based on the contact information in the directories, and only a small proportion was actually able to see the new “patient” in an appropriate time frame. The average wait time for a psychiatrist was 20 days, for a psychologist was 15 days, and for other mental health professionals was 11 days.
The study, published (Psychiatric Serv. 2014 Oct. 15 [doi:10.1176/appi.ps.2014000051]), illustrates how hard it can be to get an appointment with a psychiatrist, regardless of who the payer is. The authors called 360 psychiatrists who were listed in the Blue Cross Blue Shield (BCBS) online directories in Boston, Chicago, and Houston. Callers posed as people with depressive symptoms seeking initial appointments. In each city, a third of the psychiatrists received a call from a caller saying they were either Medicare, BCBS, or self-pay. Voicemails were left when possible that included the type of payer. Callers followed up for a second round of calls if they did not hear back.
“Obtaining an outpatient appointment with a psychiatrist was difficult in the three cities we surveyed, and the appointments given were an average of 1 month away,” the authors wrote. Between 20%-27% of the phone numbers in the insurance company directories were wrong numbers, which led, instead, to places like McDonald’s and retail stores. In fact, they were able to reach only one-third of the psychiatrists.
The ACA requires Health Insurance Exchanges to have network provider directories that distinguish those providers who are currently accepting new outpatients. Unfortunately, the act left it up to the states to define network adequacy. For example, in Maryland, the definition of what constitutes an adequate network is left to each qualified health plan to define.
The problem with the health plans’ provider directories is that they are inaccurate, making it look like they have more available providers than they actually do. The plans have no incentive to expose the inadequacy of their network directories, while the regulators lack the staff to police them sufficiently. Meanwhile, provider groups benefit from being included on more lists, and plan members fail to effectively complain to the plans, employers, and regulators.
What the industry needs is to move away from these misleading, payer-centered provider directories and move toward transparent, patient-centered provider directories that include elements of crowdsourcing, provider control, and frictionless reporting. Making these changes will give consumers, employers, and regulators more information on provider availability, wait times, and true access to care.
Dr. Daviss is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, chair of the APA Committee on Electronic Health Records, cochair of the CCHIT Behavioral Health Work Group, and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. He is found on Twitter @HITshrink, at drdaviss@gmail.com, and on the Shrink Rap blog.
How often does someone ask you for help in getting an appointment with a psychiatrist? With the “double expansion” in access to mental health care – because of the Mental Health Parity and Addiction Equity Act, and the Affordable Care Act (ACA) – many more people are seeking help for mental health and substance use problems. But without more practitioners being produced, the waiting lists are getting longer.
A recent study found that 40% (146 of 360) of psychiatrists listed on insurance plans in three states could not be reached. Of the 214 who were reachable, 43% were unavailable, either because the psychiatrists were not accepting new patients or because they did not treat adult outpatients (e.g., inpatient only). Of the 123 psychiatrists left, the callers were able to schedule appointments with 93 (76%) of them. These results are similar to a 2007 study, where 44% of mental health professionals from seven health plans were unreachable.
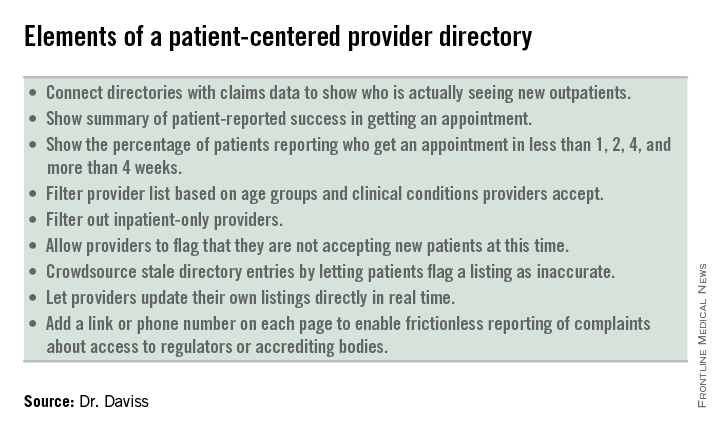
Problems with access to psychiatric care is not a new problem. Mental health carve-outs are used by managed care organizations (MCOs) to manage the mental health benefits, but create inefficiency in claims management and clinical care coordination. While this model seems to be losing popularity, these managed behavioral health organizations (MBHOs) often do not integrate well with the MCO, may not share the same standards for network adequacy, and often have different provider directories from those of the MCO, making it more complex for patients to access providers.
While the Parity Act has somewhat improved the problem of rate disparities, the historically low rates paid to psychiatrists by MBHOs have led to high levels of insurance nonparticipation, as much as 50%. Compounding this problem is the fact that plan members often find it hard to access those practitioners who do participate with their insurance.
The Maryland Psychological Association conducted in 2007 with Open Minds a “secret shopper” survey of more than 900 behavioral health providers from seven different online carrier directories in Maryland. Their goal was to assess the extent to which problems with access to care were related to inadequate insurance provider directories.
They found that 44% of the listed providers were unreachable based on the contact information in the directories, and only a small proportion was actually able to see the new “patient” in an appropriate time frame. The average wait time for a psychiatrist was 20 days, for a psychologist was 15 days, and for other mental health professionals was 11 days.
The study, published (Psychiatric Serv. 2014 Oct. 15 [doi:10.1176/appi.ps.2014000051]), illustrates how hard it can be to get an appointment with a psychiatrist, regardless of who the payer is. The authors called 360 psychiatrists who were listed in the Blue Cross Blue Shield (BCBS) online directories in Boston, Chicago, and Houston. Callers posed as people with depressive symptoms seeking initial appointments. In each city, a third of the psychiatrists received a call from a caller saying they were either Medicare, BCBS, or self-pay. Voicemails were left when possible that included the type of payer. Callers followed up for a second round of calls if they did not hear back.
“Obtaining an outpatient appointment with a psychiatrist was difficult in the three cities we surveyed, and the appointments given were an average of 1 month away,” the authors wrote. Between 20%-27% of the phone numbers in the insurance company directories were wrong numbers, which led, instead, to places like McDonald’s and retail stores. In fact, they were able to reach only one-third of the psychiatrists.
The ACA requires Health Insurance Exchanges to have network provider directories that distinguish those providers who are currently accepting new outpatients. Unfortunately, the act left it up to the states to define network adequacy. For example, in Maryland, the definition of what constitutes an adequate network is left to each qualified health plan to define.
The problem with the health plans’ provider directories is that they are inaccurate, making it look like they have more available providers than they actually do. The plans have no incentive to expose the inadequacy of their network directories, while the regulators lack the staff to police them sufficiently. Meanwhile, provider groups benefit from being included on more lists, and plan members fail to effectively complain to the plans, employers, and regulators.
What the industry needs is to move away from these misleading, payer-centered provider directories and move toward transparent, patient-centered provider directories that include elements of crowdsourcing, provider control, and frictionless reporting. Making these changes will give consumers, employers, and regulators more information on provider availability, wait times, and true access to care.
Dr. Daviss is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, chair of the APA Committee on Electronic Health Records, cochair of the CCHIT Behavioral Health Work Group, and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. He is found on Twitter @HITshrink, at drdaviss@gmail.com, and on the Shrink Rap blog.
How often does someone ask you for help in getting an appointment with a psychiatrist? With the “double expansion” in access to mental health care – because of the Mental Health Parity and Addiction Equity Act, and the Affordable Care Act (ACA) – many more people are seeking help for mental health and substance use problems. But without more practitioners being produced, the waiting lists are getting longer.
A recent study found that 40% (146 of 360) of psychiatrists listed on insurance plans in three states could not be reached. Of the 214 who were reachable, 43% were unavailable, either because the psychiatrists were not accepting new patients or because they did not treat adult outpatients (e.g., inpatient only). Of the 123 psychiatrists left, the callers were able to schedule appointments with 93 (76%) of them. These results are similar to a 2007 study, where 44% of mental health professionals from seven health plans were unreachable.
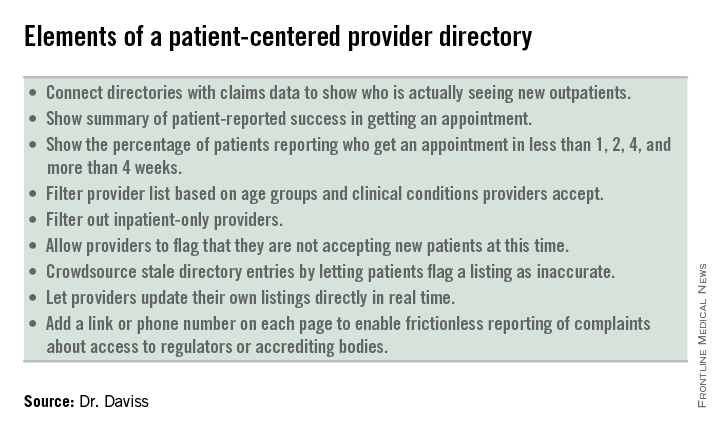
Problems with access to psychiatric care is not a new problem. Mental health carve-outs are used by managed care organizations (MCOs) to manage the mental health benefits, but create inefficiency in claims management and clinical care coordination. While this model seems to be losing popularity, these managed behavioral health organizations (MBHOs) often do not integrate well with the MCO, may not share the same standards for network adequacy, and often have different provider directories from those of the MCO, making it more complex for patients to access providers.
While the Parity Act has somewhat improved the problem of rate disparities, the historically low rates paid to psychiatrists by MBHOs have led to high levels of insurance nonparticipation, as much as 50%. Compounding this problem is the fact that plan members often find it hard to access those practitioners who do participate with their insurance.
The Maryland Psychological Association conducted in 2007 with Open Minds a “secret shopper” survey of more than 900 behavioral health providers from seven different online carrier directories in Maryland. Their goal was to assess the extent to which problems with access to care were related to inadequate insurance provider directories.
They found that 44% of the listed providers were unreachable based on the contact information in the directories, and only a small proportion was actually able to see the new “patient” in an appropriate time frame. The average wait time for a psychiatrist was 20 days, for a psychologist was 15 days, and for other mental health professionals was 11 days.
The study, published (Psychiatric Serv. 2014 Oct. 15 [doi:10.1176/appi.ps.2014000051]), illustrates how hard it can be to get an appointment with a psychiatrist, regardless of who the payer is. The authors called 360 psychiatrists who were listed in the Blue Cross Blue Shield (BCBS) online directories in Boston, Chicago, and Houston. Callers posed as people with depressive symptoms seeking initial appointments. In each city, a third of the psychiatrists received a call from a caller saying they were either Medicare, BCBS, or self-pay. Voicemails were left when possible that included the type of payer. Callers followed up for a second round of calls if they did not hear back.
“Obtaining an outpatient appointment with a psychiatrist was difficult in the three cities we surveyed, and the appointments given were an average of 1 month away,” the authors wrote. Between 20%-27% of the phone numbers in the insurance company directories were wrong numbers, which led, instead, to places like McDonald’s and retail stores. In fact, they were able to reach only one-third of the psychiatrists.
The ACA requires Health Insurance Exchanges to have network provider directories that distinguish those providers who are currently accepting new outpatients. Unfortunately, the act left it up to the states to define network adequacy. For example, in Maryland, the definition of what constitutes an adequate network is left to each qualified health plan to define.
The problem with the health plans’ provider directories is that they are inaccurate, making it look like they have more available providers than they actually do. The plans have no incentive to expose the inadequacy of their network directories, while the regulators lack the staff to police them sufficiently. Meanwhile, provider groups benefit from being included on more lists, and plan members fail to effectively complain to the plans, employers, and regulators.
What the industry needs is to move away from these misleading, payer-centered provider directories and move toward transparent, patient-centered provider directories that include elements of crowdsourcing, provider control, and frictionless reporting. Making these changes will give consumers, employers, and regulators more information on provider availability, wait times, and true access to care.
Dr. Daviss is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, chair of the APA Committee on Electronic Health Records, cochair of the CCHIT Behavioral Health Work Group, and coauthor of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. He is found on Twitter @HITshrink, at drdaviss@gmail.com, and on the Shrink Rap blog.











