User login
Helping quality improvement teams succeed
QI coaches may be the answer
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
QI coaches may be the answer
QI coaches may be the answer
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
New handoff tool can improve safety
Standardization of process reduces variation
Hospitalists know all too well that a significant source of medical errors is miscommunication during transitions: By interrupting the continuity of care, handoffs can increase the risk of adverse events.
Yet the transfer of patients from the ED to the hospitalist inpatient service has not been well studied, said Carmen Gonzalez, MD, lead author of a recent paper that examined the issue. “The scope of this study was to develop and test a handoff communication tool and a standardized process for transitioning patients from the ED to the hospitalist service at a comprehensive cancer center,” she explained.
In the study, the researchers found that the number of ICU transfers within 24 hours of admission and the number of rapid-response calls decreased after the implementation of a customized handoff tool. “The tool was named DE-PASS (DE-PASS: Decisive problem requiring admission, Evaluation time, Patient summary, Acute issues/action list, Situation unfinished/awareness, Signed out to), which was a modification of the I-PASS, and adapted to our workflow,” reported Dr. Gonzalez, who is based at the University of Texas MD Anderson Cancer Center, Houston. DE-PASS stratifies patients as stable/urgent/emergent and establishes requirements for communications between providers.
Results from the 1-month pilot revealed that, within a 24-hour period, DE-PASS reduced the number of intensive care unit transfers by 58%, the number of rapid-response team calls by 39%, and time to inpatient order by 31%.
“The standardization of the language and format of the handoff process of admission from the ED to the hospitalist service reduced handoff variations, increased provider satisfaction, and improved patient safety,” she noted.
The hospitalists expressed satisfaction with the tool. “This handoff tool helps stratify newly admitted patients based on their illness acuity, hence, assists the busy admitting hospitalist in prioritizing which patient needs to be attended first,” said study coauthor Norman Brito-Dellan, MD, also of MD Anderson Cancer Center. “In this study, DE-PASS reduced admission-to-evaluation times for unstable patients. These patients tend to be evaluated earlier, improving safety.”
Reference
1. Gonzalez CE et al. Handoff tool enabling standardized transitions between the emergency department and the hospitalist inpatient service at a major cancer center. American Journal of Medical Quality. 2018 May 21. doi: 10.1177/1062860618776096.
Standardization of process reduces variation
Standardization of process reduces variation
Hospitalists know all too well that a significant source of medical errors is miscommunication during transitions: By interrupting the continuity of care, handoffs can increase the risk of adverse events.
Yet the transfer of patients from the ED to the hospitalist inpatient service has not been well studied, said Carmen Gonzalez, MD, lead author of a recent paper that examined the issue. “The scope of this study was to develop and test a handoff communication tool and a standardized process for transitioning patients from the ED to the hospitalist service at a comprehensive cancer center,” she explained.
In the study, the researchers found that the number of ICU transfers within 24 hours of admission and the number of rapid-response calls decreased after the implementation of a customized handoff tool. “The tool was named DE-PASS (DE-PASS: Decisive problem requiring admission, Evaluation time, Patient summary, Acute issues/action list, Situation unfinished/awareness, Signed out to), which was a modification of the I-PASS, and adapted to our workflow,” reported Dr. Gonzalez, who is based at the University of Texas MD Anderson Cancer Center, Houston. DE-PASS stratifies patients as stable/urgent/emergent and establishes requirements for communications between providers.
Results from the 1-month pilot revealed that, within a 24-hour period, DE-PASS reduced the number of intensive care unit transfers by 58%, the number of rapid-response team calls by 39%, and time to inpatient order by 31%.
“The standardization of the language and format of the handoff process of admission from the ED to the hospitalist service reduced handoff variations, increased provider satisfaction, and improved patient safety,” she noted.
The hospitalists expressed satisfaction with the tool. “This handoff tool helps stratify newly admitted patients based on their illness acuity, hence, assists the busy admitting hospitalist in prioritizing which patient needs to be attended first,” said study coauthor Norman Brito-Dellan, MD, also of MD Anderson Cancer Center. “In this study, DE-PASS reduced admission-to-evaluation times for unstable patients. These patients tend to be evaluated earlier, improving safety.”
Reference
1. Gonzalez CE et al. Handoff tool enabling standardized transitions between the emergency department and the hospitalist inpatient service at a major cancer center. American Journal of Medical Quality. 2018 May 21. doi: 10.1177/1062860618776096.
Hospitalists know all too well that a significant source of medical errors is miscommunication during transitions: By interrupting the continuity of care, handoffs can increase the risk of adverse events.
Yet the transfer of patients from the ED to the hospitalist inpatient service has not been well studied, said Carmen Gonzalez, MD, lead author of a recent paper that examined the issue. “The scope of this study was to develop and test a handoff communication tool and a standardized process for transitioning patients from the ED to the hospitalist service at a comprehensive cancer center,” she explained.
In the study, the researchers found that the number of ICU transfers within 24 hours of admission and the number of rapid-response calls decreased after the implementation of a customized handoff tool. “The tool was named DE-PASS (DE-PASS: Decisive problem requiring admission, Evaluation time, Patient summary, Acute issues/action list, Situation unfinished/awareness, Signed out to), which was a modification of the I-PASS, and adapted to our workflow,” reported Dr. Gonzalez, who is based at the University of Texas MD Anderson Cancer Center, Houston. DE-PASS stratifies patients as stable/urgent/emergent and establishes requirements for communications between providers.
Results from the 1-month pilot revealed that, within a 24-hour period, DE-PASS reduced the number of intensive care unit transfers by 58%, the number of rapid-response team calls by 39%, and time to inpatient order by 31%.
“The standardization of the language and format of the handoff process of admission from the ED to the hospitalist service reduced handoff variations, increased provider satisfaction, and improved patient safety,” she noted.
The hospitalists expressed satisfaction with the tool. “This handoff tool helps stratify newly admitted patients based on their illness acuity, hence, assists the busy admitting hospitalist in prioritizing which patient needs to be attended first,” said study coauthor Norman Brito-Dellan, MD, also of MD Anderson Cancer Center. “In this study, DE-PASS reduced admission-to-evaluation times for unstable patients. These patients tend to be evaluated earlier, improving safety.”
Reference
1. Gonzalez CE et al. Handoff tool enabling standardized transitions between the emergency department and the hospitalist inpatient service at a major cancer center. American Journal of Medical Quality. 2018 May 21. doi: 10.1177/1062860618776096.
A novel approach to MIPS quality reporting for facility-based providers
A cornerstone of hospital medicine is the delivery of high-quality inpatient care by improving the performance of the systems and facilities in which hospitalists work. By extension, hospitalists are often held accountable, in varying ways, for improving the performance of facility metrics, such as those in the Hospital Value-Based Purchasing (HVBP), Inpatient Quality Reporting, and Hospital Readmissions Reduction programs.
Despite the work hospitalists were already doing to improve both efficiency and quality within their institutions, the 2010 Affordable Care Act introduced penalties for clinicians who did not submit qualifying provider-level data via the Physician Quality Reporting System program. Initially only an incentive program, PQRS was ultimately incorporated into the Physician Value-Based Payment (VBP) Modifier to make performance-based payment adjustments to Medicare physician payment. At this point, many hospitalists were not only accountable for helping to improve the metrics of their facilities, but also required to report individually or within their groups on provider-level measures, many of which were irrelevant to hospital medicine practice.
With this dual burden becoming evident, the Society of Hospital Medicine approached the Centers for Medicare & Medicaid Services with a possible solution. Could hospitalists elect to use their facilities’ metrics as a stand-in for the provider level metrics? Not only would this reduce the burden of reporting irrelevant metrics, but it would also help alleviate some of the disadvantages hospitalists face within Physician VBP.
The CMS was initially very supportive of the concept, but informed the SHM such alignment was not possible under existing law. In brief, the law required Physician VBP to remain completely within the Physician Fee Schedule and its related metrics; facility level metrics from a different payment system could not be used.
Undeterred, the SHM sought opportunities to change the law. As Congress was developing the Medicare Access and Chip Reauthorization Act (MACRA), the SHM worked closely with lawmakers to include language that would permit measures in “other payment systems” to be used for physician performance assessment. This language was retained in the final version of MACRA that was signed into law on April 16, 2015.
The SHM continued its advocacy, working closely with the CMS and its new authority to shape an option to align Medicare’s facility metrics and scores with provider reporting. Today that idea is a reality. Beginning this year, the CMS will have a new Merit-based Incentive Payment System (MIPS) reporting option available for hospitalists: facility-based measurement.
Facility-based measurement enables clinicians to receive a score for the Quality and Cost categories of the MIPS, without the need to collect and report on measures separately. Eligible providers would receive the MIPS score in those categories associated with the same percentile as their hospital’s score in HVBP. No more administrative work necessary to collect, clean and report on data for quality measures in the MIPS. If you are eligible, the CMS will automatically calculate a Quality and Cost score and combine this with your score from Improvement Activities and Promoting Interoperability (if you are not exempt) to give you a final MIPS score. If you decide to report on quality measures through the traditional MIPS pathway as well, the CMS will give you the higher of the scores.
There are certainly trade-offs associated with the facility-based measurement option. You do not have the burden of reporting measures on your own, but you do not get to pick what measures and what facility’s score you receive. Facility-level measures may be more difficult to improve performance, particularly as an individual, but the automatic application of facility-based measurement to eligible clinicians and groups serves as a backstop for MIPS reporting.
Aligning facility and clinician performance should encourage collaboration and innovation to meet these shared goals. As such, facility-based measurement represents a massive philosophical and practical shift in CMS measure reporting. As we enter these uncharted waters together, we hope to continue learning from your experiences and perspectives and working to refine facility-based measurement in the future.
For more information about facility-based reporting and the MIPS in general, visit www.macraforhm.org.
Mr. Lapps is government relations senior manager and Mr. Boswell is government relations director at the Society of Hospital Medicine.
Who is eligible for facility-based measurement?
- Individual providers who bill more than 75% of their Medicare Part B professional services in Place of Service 21 (Emergency Department), 22 (Hospital Outpatient), and 23 (Inpatient Hospital), billing at least one service in POS 21 or 23, and work in a hospital with an HVBP score.
- Groups who have at least 75% of their individual clinicians who meet the eligibility criteria.
- Nearly all hospitalists should qualify for facility-based measurement as individuals, while group eligibility depends on the demographics of their staff.
A cornerstone of hospital medicine is the delivery of high-quality inpatient care by improving the performance of the systems and facilities in which hospitalists work. By extension, hospitalists are often held accountable, in varying ways, for improving the performance of facility metrics, such as those in the Hospital Value-Based Purchasing (HVBP), Inpatient Quality Reporting, and Hospital Readmissions Reduction programs.
Despite the work hospitalists were already doing to improve both efficiency and quality within their institutions, the 2010 Affordable Care Act introduced penalties for clinicians who did not submit qualifying provider-level data via the Physician Quality Reporting System program. Initially only an incentive program, PQRS was ultimately incorporated into the Physician Value-Based Payment (VBP) Modifier to make performance-based payment adjustments to Medicare physician payment. At this point, many hospitalists were not only accountable for helping to improve the metrics of their facilities, but also required to report individually or within their groups on provider-level measures, many of which were irrelevant to hospital medicine practice.
With this dual burden becoming evident, the Society of Hospital Medicine approached the Centers for Medicare & Medicaid Services with a possible solution. Could hospitalists elect to use their facilities’ metrics as a stand-in for the provider level metrics? Not only would this reduce the burden of reporting irrelevant metrics, but it would also help alleviate some of the disadvantages hospitalists face within Physician VBP.
The CMS was initially very supportive of the concept, but informed the SHM such alignment was not possible under existing law. In brief, the law required Physician VBP to remain completely within the Physician Fee Schedule and its related metrics; facility level metrics from a different payment system could not be used.
Undeterred, the SHM sought opportunities to change the law. As Congress was developing the Medicare Access and Chip Reauthorization Act (MACRA), the SHM worked closely with lawmakers to include language that would permit measures in “other payment systems” to be used for physician performance assessment. This language was retained in the final version of MACRA that was signed into law on April 16, 2015.
The SHM continued its advocacy, working closely with the CMS and its new authority to shape an option to align Medicare’s facility metrics and scores with provider reporting. Today that idea is a reality. Beginning this year, the CMS will have a new Merit-based Incentive Payment System (MIPS) reporting option available for hospitalists: facility-based measurement.
Facility-based measurement enables clinicians to receive a score for the Quality and Cost categories of the MIPS, without the need to collect and report on measures separately. Eligible providers would receive the MIPS score in those categories associated with the same percentile as their hospital’s score in HVBP. No more administrative work necessary to collect, clean and report on data for quality measures in the MIPS. If you are eligible, the CMS will automatically calculate a Quality and Cost score and combine this with your score from Improvement Activities and Promoting Interoperability (if you are not exempt) to give you a final MIPS score. If you decide to report on quality measures through the traditional MIPS pathway as well, the CMS will give you the higher of the scores.
There are certainly trade-offs associated with the facility-based measurement option. You do not have the burden of reporting measures on your own, but you do not get to pick what measures and what facility’s score you receive. Facility-level measures may be more difficult to improve performance, particularly as an individual, but the automatic application of facility-based measurement to eligible clinicians and groups serves as a backstop for MIPS reporting.
Aligning facility and clinician performance should encourage collaboration and innovation to meet these shared goals. As such, facility-based measurement represents a massive philosophical and practical shift in CMS measure reporting. As we enter these uncharted waters together, we hope to continue learning from your experiences and perspectives and working to refine facility-based measurement in the future.
For more information about facility-based reporting and the MIPS in general, visit www.macraforhm.org.
Mr. Lapps is government relations senior manager and Mr. Boswell is government relations director at the Society of Hospital Medicine.
Who is eligible for facility-based measurement?
- Individual providers who bill more than 75% of their Medicare Part B professional services in Place of Service 21 (Emergency Department), 22 (Hospital Outpatient), and 23 (Inpatient Hospital), billing at least one service in POS 21 or 23, and work in a hospital with an HVBP score.
- Groups who have at least 75% of their individual clinicians who meet the eligibility criteria.
- Nearly all hospitalists should qualify for facility-based measurement as individuals, while group eligibility depends on the demographics of their staff.
A cornerstone of hospital medicine is the delivery of high-quality inpatient care by improving the performance of the systems and facilities in which hospitalists work. By extension, hospitalists are often held accountable, in varying ways, for improving the performance of facility metrics, such as those in the Hospital Value-Based Purchasing (HVBP), Inpatient Quality Reporting, and Hospital Readmissions Reduction programs.
Despite the work hospitalists were already doing to improve both efficiency and quality within their institutions, the 2010 Affordable Care Act introduced penalties for clinicians who did not submit qualifying provider-level data via the Physician Quality Reporting System program. Initially only an incentive program, PQRS was ultimately incorporated into the Physician Value-Based Payment (VBP) Modifier to make performance-based payment adjustments to Medicare physician payment. At this point, many hospitalists were not only accountable for helping to improve the metrics of their facilities, but also required to report individually or within their groups on provider-level measures, many of which were irrelevant to hospital medicine practice.
With this dual burden becoming evident, the Society of Hospital Medicine approached the Centers for Medicare & Medicaid Services with a possible solution. Could hospitalists elect to use their facilities’ metrics as a stand-in for the provider level metrics? Not only would this reduce the burden of reporting irrelevant metrics, but it would also help alleviate some of the disadvantages hospitalists face within Physician VBP.
The CMS was initially very supportive of the concept, but informed the SHM such alignment was not possible under existing law. In brief, the law required Physician VBP to remain completely within the Physician Fee Schedule and its related metrics; facility level metrics from a different payment system could not be used.
Undeterred, the SHM sought opportunities to change the law. As Congress was developing the Medicare Access and Chip Reauthorization Act (MACRA), the SHM worked closely with lawmakers to include language that would permit measures in “other payment systems” to be used for physician performance assessment. This language was retained in the final version of MACRA that was signed into law on April 16, 2015.
The SHM continued its advocacy, working closely with the CMS and its new authority to shape an option to align Medicare’s facility metrics and scores with provider reporting. Today that idea is a reality. Beginning this year, the CMS will have a new Merit-based Incentive Payment System (MIPS) reporting option available for hospitalists: facility-based measurement.
Facility-based measurement enables clinicians to receive a score for the Quality and Cost categories of the MIPS, without the need to collect and report on measures separately. Eligible providers would receive the MIPS score in those categories associated with the same percentile as their hospital’s score in HVBP. No more administrative work necessary to collect, clean and report on data for quality measures in the MIPS. If you are eligible, the CMS will automatically calculate a Quality and Cost score and combine this with your score from Improvement Activities and Promoting Interoperability (if you are not exempt) to give you a final MIPS score. If you decide to report on quality measures through the traditional MIPS pathway as well, the CMS will give you the higher of the scores.
There are certainly trade-offs associated with the facility-based measurement option. You do not have the burden of reporting measures on your own, but you do not get to pick what measures and what facility’s score you receive. Facility-level measures may be more difficult to improve performance, particularly as an individual, but the automatic application of facility-based measurement to eligible clinicians and groups serves as a backstop for MIPS reporting.
Aligning facility and clinician performance should encourage collaboration and innovation to meet these shared goals. As such, facility-based measurement represents a massive philosophical and practical shift in CMS measure reporting. As we enter these uncharted waters together, we hope to continue learning from your experiences and perspectives and working to refine facility-based measurement in the future.
For more information about facility-based reporting and the MIPS in general, visit www.macraforhm.org.
Mr. Lapps is government relations senior manager and Mr. Boswell is government relations director at the Society of Hospital Medicine.
Who is eligible for facility-based measurement?
- Individual providers who bill more than 75% of their Medicare Part B professional services in Place of Service 21 (Emergency Department), 22 (Hospital Outpatient), and 23 (Inpatient Hospital), billing at least one service in POS 21 or 23, and work in a hospital with an HVBP score.
- Groups who have at least 75% of their individual clinicians who meet the eligibility criteria.
- Nearly all hospitalists should qualify for facility-based measurement as individuals, while group eligibility depends on the demographics of their staff.
Benefiting from an egalitarian hospital culture
Cultural change linked to improved outcomes
Health care experts have long known of a link between patient outcomes and a hospital’s organizational culture, according to an article in the New York Times by Pauline W. Chen, MD.
“Heart attack patients who are treated at hospitals where nurses feel powerless and senior management is only sporadically involved in patient care tend to fare more poorly than patients hospitalized at institutions where nurses are asked regularly for their input and chief executives hold regular meetings with clinicians to review patient results,” she wrote.
But there is hope for change, Dr. Chen noted, and it’s demonstrable, citing a group of researchers that has written about strategies targeting hospital organizational culture called “Leadership Saves Lives.” The researchers showed hospitals could create significant cultural changes, which could impact patient outcomes, in just 2 years.
“Leadership Saves Lives requires that each hospital create a ‘Guiding Coalition,’ a group of staff members from across the entire institution. The coalition members participate in regular workshops, discussions, and national forums on ways hospitals might improve, then help their respective hospital translate newfound ideas and information into clinical practice,” she wrote.
The researchers monitored heart attack patients to assess the effect of Leadership Saves Lives in 10 hospitals that had below average patient outcomes. Over 2 years, all 10 hospitals changed significantly, but 6 hospitals experienced particularly profound cultural transformations.
“The staff of these hospitals spoke of an institutional shift from ‘because I said so’ to ‘focusing on the why’s,’ ” Dr. Chen wrote. “Instead of accepting that every heart attack patient had to undergo certain testing or take specific drugs because the chief of the department or administrator had previously established such clinical protocols, for example, it became more important to provide the data that proved such rituals were actually helpful. Staff members in these hospitals also said they received, and appreciated, increased support from senior management and a newfound freedom to voice opinions in ‘more of an equal role, no matter what position you are.’ ”
The degree of an institution’s cultural change was directly linked to patient outcomes, the researchers found. Indeed, hospitals that made more substantial changes in their work culture realized larger and more sustained drops in heart attack mortality rates.
References
1. Chen PW. A More Egalitarian Hospital Culture Is Better for Everyone. New York Times. https://www.nytimes.com/2018/05/31/well/live/doctors-patients-hospital-culture-better-health.html. Published May 31, 2018. Accessed June 1, 2018.
2. Curry LA et al. Organizational culture change in U.S. hospitals: A mixed methods longitudinal intervention study. Implementation Science. 2015 Mar 7. doi: 10.1186/s13012-015-0218-0. Accessed June 18, 2018.
Cultural change linked to improved outcomes
Cultural change linked to improved outcomes
Health care experts have long known of a link between patient outcomes and a hospital’s organizational culture, according to an article in the New York Times by Pauline W. Chen, MD.
“Heart attack patients who are treated at hospitals where nurses feel powerless and senior management is only sporadically involved in patient care tend to fare more poorly than patients hospitalized at institutions where nurses are asked regularly for their input and chief executives hold regular meetings with clinicians to review patient results,” she wrote.
But there is hope for change, Dr. Chen noted, and it’s demonstrable, citing a group of researchers that has written about strategies targeting hospital organizational culture called “Leadership Saves Lives.” The researchers showed hospitals could create significant cultural changes, which could impact patient outcomes, in just 2 years.
“Leadership Saves Lives requires that each hospital create a ‘Guiding Coalition,’ a group of staff members from across the entire institution. The coalition members participate in regular workshops, discussions, and national forums on ways hospitals might improve, then help their respective hospital translate newfound ideas and information into clinical practice,” she wrote.
The researchers monitored heart attack patients to assess the effect of Leadership Saves Lives in 10 hospitals that had below average patient outcomes. Over 2 years, all 10 hospitals changed significantly, but 6 hospitals experienced particularly profound cultural transformations.
“The staff of these hospitals spoke of an institutional shift from ‘because I said so’ to ‘focusing on the why’s,’ ” Dr. Chen wrote. “Instead of accepting that every heart attack patient had to undergo certain testing or take specific drugs because the chief of the department or administrator had previously established such clinical protocols, for example, it became more important to provide the data that proved such rituals were actually helpful. Staff members in these hospitals also said they received, and appreciated, increased support from senior management and a newfound freedom to voice opinions in ‘more of an equal role, no matter what position you are.’ ”
The degree of an institution’s cultural change was directly linked to patient outcomes, the researchers found. Indeed, hospitals that made more substantial changes in their work culture realized larger and more sustained drops in heart attack mortality rates.
References
1. Chen PW. A More Egalitarian Hospital Culture Is Better for Everyone. New York Times. https://www.nytimes.com/2018/05/31/well/live/doctors-patients-hospital-culture-better-health.html. Published May 31, 2018. Accessed June 1, 2018.
2. Curry LA et al. Organizational culture change in U.S. hospitals: A mixed methods longitudinal intervention study. Implementation Science. 2015 Mar 7. doi: 10.1186/s13012-015-0218-0. Accessed June 18, 2018.
Health care experts have long known of a link between patient outcomes and a hospital’s organizational culture, according to an article in the New York Times by Pauline W. Chen, MD.
“Heart attack patients who are treated at hospitals where nurses feel powerless and senior management is only sporadically involved in patient care tend to fare more poorly than patients hospitalized at institutions where nurses are asked regularly for their input and chief executives hold regular meetings with clinicians to review patient results,” she wrote.
But there is hope for change, Dr. Chen noted, and it’s demonstrable, citing a group of researchers that has written about strategies targeting hospital organizational culture called “Leadership Saves Lives.” The researchers showed hospitals could create significant cultural changes, which could impact patient outcomes, in just 2 years.
“Leadership Saves Lives requires that each hospital create a ‘Guiding Coalition,’ a group of staff members from across the entire institution. The coalition members participate in regular workshops, discussions, and national forums on ways hospitals might improve, then help their respective hospital translate newfound ideas and information into clinical practice,” she wrote.
The researchers monitored heart attack patients to assess the effect of Leadership Saves Lives in 10 hospitals that had below average patient outcomes. Over 2 years, all 10 hospitals changed significantly, but 6 hospitals experienced particularly profound cultural transformations.
“The staff of these hospitals spoke of an institutional shift from ‘because I said so’ to ‘focusing on the why’s,’ ” Dr. Chen wrote. “Instead of accepting that every heart attack patient had to undergo certain testing or take specific drugs because the chief of the department or administrator had previously established such clinical protocols, for example, it became more important to provide the data that proved such rituals were actually helpful. Staff members in these hospitals also said they received, and appreciated, increased support from senior management and a newfound freedom to voice opinions in ‘more of an equal role, no matter what position you are.’ ”
The degree of an institution’s cultural change was directly linked to patient outcomes, the researchers found. Indeed, hospitals that made more substantial changes in their work culture realized larger and more sustained drops in heart attack mortality rates.
References
1. Chen PW. A More Egalitarian Hospital Culture Is Better for Everyone. New York Times. https://www.nytimes.com/2018/05/31/well/live/doctors-patients-hospital-culture-better-health.html. Published May 31, 2018. Accessed June 1, 2018.
2. Curry LA et al. Organizational culture change in U.S. hospitals: A mixed methods longitudinal intervention study. Implementation Science. 2015 Mar 7. doi: 10.1186/s13012-015-0218-0. Accessed June 18, 2018.
Increasing inpatient attending supervision does not decrease medical errors
Clinical question: What is the effect of increasing attending physician supervision on a resident inpatient team for both patient safety and education?
Background: Residents need autonomy to help develop their clinical skills and to gain competence to practice independently; however, there is rising concern that increased supervision is needed for patient safety.
Study Design: Randomized, crossover clinical trial.
Setting: 1,100-bed academic medical center at Massachusetts General Hospital, Boston.
Synopsis: Twenty-two attending physicians participated in the study over 44 2-week teaching blocks with a total of 1,259 patient hospitalizations on the general medicine teaching service. In the intervention arm, attendings were present during work rounds; in the control arm, attendings discussed established patients with the resident via card flip. New patients were discussed at the bedside in both arms. There was no statistically significant difference in the number of medical errors or patient safety events between the two groups. Residents in the intervention group, however, felt less efficient and autonomous and were less able to make independent decisions. Limitations include this being a single-center study at a program emphasizing resident autonomy and therefore may limit generalizability. Current literature on supervision and patient safety has variable results. This study suggests that increasing attending supervision may not increase patient safety, but may negatively affect resident education and autonomy.
Bottom line: Attending physician presence on work rounds does not improve patient safety and may have deleterious effects on resident education.
Citation: Finn KM et al. Effect of increased inpatient attending physician supervision on medical errors, patient safety, and resident education. JAMA Intern Med. 2018;178(7):925-59
Dr. Ciarkowski is clinical instructor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Clinical question: What is the effect of increasing attending physician supervision on a resident inpatient team for both patient safety and education?
Background: Residents need autonomy to help develop their clinical skills and to gain competence to practice independently; however, there is rising concern that increased supervision is needed for patient safety.
Study Design: Randomized, crossover clinical trial.
Setting: 1,100-bed academic medical center at Massachusetts General Hospital, Boston.
Synopsis: Twenty-two attending physicians participated in the study over 44 2-week teaching blocks with a total of 1,259 patient hospitalizations on the general medicine teaching service. In the intervention arm, attendings were present during work rounds; in the control arm, attendings discussed established patients with the resident via card flip. New patients were discussed at the bedside in both arms. There was no statistically significant difference in the number of medical errors or patient safety events between the two groups. Residents in the intervention group, however, felt less efficient and autonomous and were less able to make independent decisions. Limitations include this being a single-center study at a program emphasizing resident autonomy and therefore may limit generalizability. Current literature on supervision and patient safety has variable results. This study suggests that increasing attending supervision may not increase patient safety, but may negatively affect resident education and autonomy.
Bottom line: Attending physician presence on work rounds does not improve patient safety and may have deleterious effects on resident education.
Citation: Finn KM et al. Effect of increased inpatient attending physician supervision on medical errors, patient safety, and resident education. JAMA Intern Med. 2018;178(7):925-59
Dr. Ciarkowski is clinical instructor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Clinical question: What is the effect of increasing attending physician supervision on a resident inpatient team for both patient safety and education?
Background: Residents need autonomy to help develop their clinical skills and to gain competence to practice independently; however, there is rising concern that increased supervision is needed for patient safety.
Study Design: Randomized, crossover clinical trial.
Setting: 1,100-bed academic medical center at Massachusetts General Hospital, Boston.
Synopsis: Twenty-two attending physicians participated in the study over 44 2-week teaching blocks with a total of 1,259 patient hospitalizations on the general medicine teaching service. In the intervention arm, attendings were present during work rounds; in the control arm, attendings discussed established patients with the resident via card flip. New patients were discussed at the bedside in both arms. There was no statistically significant difference in the number of medical errors or patient safety events between the two groups. Residents in the intervention group, however, felt less efficient and autonomous and were less able to make independent decisions. Limitations include this being a single-center study at a program emphasizing resident autonomy and therefore may limit generalizability. Current literature on supervision and patient safety has variable results. This study suggests that increasing attending supervision may not increase patient safety, but may negatively affect resident education and autonomy.
Bottom line: Attending physician presence on work rounds does not improve patient safety and may have deleterious effects on resident education.
Citation: Finn KM et al. Effect of increased inpatient attending physician supervision on medical errors, patient safety, and resident education. JAMA Intern Med. 2018;178(7):925-59
Dr. Ciarkowski is clinical instructor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
How can I improve opioid safety at my hospital?
Quality improvement is essential
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
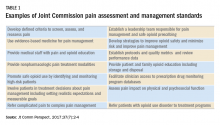
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
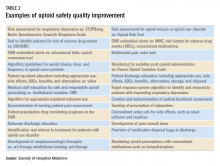
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Quality improvement is essential
Quality improvement is essential
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
How to assess an Antimicrobial Stewardship Program
A study compares the merits of DOT and DOTA
The currently recommended method for hospital antimicrobial stewardship programs (ASPs) to measure antibiotic use is Days of Therapy/1,000 patient-days, but there are a few disadvantages of using the DOT, said Maryrose Laguio-Vila, MD, coauthor of a recent study on stewardship.
“For accurate measurement, it requires information technology (IT) support to assist an ASP in generating reports of antibiotic prescriptions and administrations to patients, often from an electronic medical record (EMR). In hospitals where there is no EMR, DOT is probably not easily done and would have to be manually extracted (a herculean task),” she said. “Second, DOT tends to be an aggregate measurement of antibiotics used at an institution or hospital location; if an ASP does a specific intervention targeting a group of antibiotics or infectious indication, changes in the hospital-wide DOT or drug-class DOT may not accurately reflect the exact impact of an ASP’s intervention.”
The paper offers an alternative/supplemental method for ASPs to quantify their impact on antibiotic use without using an EMR or needing IT support: Days of Therapy Avoided. “DOTA can be tracked prospectively (or retrospectively) with each intervention an ASP makes, and calculates an exact amount of antibiotic use avoided,” Dr. Laguio-Vila said. “If the ASP also tracks the types of antibiotic recommendations made according to infectious indication, comparison of DOTA between indications – such as pneumonia versus UTI [urinary tract infection] – can lead to ideas of which type of indication needs clinical guidelines development, or order set revision, or which type of infection the ASP should target to reduce high-risk antibiotics.”
Also, she added, because most ASPs have several types of interventions at once (such as education on pneumonia guidelines, as well as penicillin-allergy assessment), aggregate assessments of institutional antibiotic use like the DOT cannot quantify how much impact a specific intervention has accomplished. DOTA may offer a fairer assessment of the direct changes in antibiotic use resulting from specific ASP activities, because tracking DOTA is extracted from each specific patient intervention.
“Now that the Joint Commission has a requirement that all hospitals seeking JC accreditation have some form of an ASP in place and measure antibiotic use in some way at their institution, there may be numerous hospitals facing the same challenges with calculating a DOT. DOTA would meet these requirements, but in a ‘low tech’ way,” Dr. Laguio-Vila said. “For hospitalists with interests in being the antibiotic steward or champion for their institution, DOTA is an option for measuring antibiotic use.”
Reference
Datta S et al. Days of therapy avoided: A novel method for measuring the impact of an antimicrobial stewardship program to stop antibiotics. J Hosp Med. 2018 Feb 8. doi: 10.12788/jhm.2927.
A study compares the merits of DOT and DOTA
A study compares the merits of DOT and DOTA
The currently recommended method for hospital antimicrobial stewardship programs (ASPs) to measure antibiotic use is Days of Therapy/1,000 patient-days, but there are a few disadvantages of using the DOT, said Maryrose Laguio-Vila, MD, coauthor of a recent study on stewardship.
“For accurate measurement, it requires information technology (IT) support to assist an ASP in generating reports of antibiotic prescriptions and administrations to patients, often from an electronic medical record (EMR). In hospitals where there is no EMR, DOT is probably not easily done and would have to be manually extracted (a herculean task),” she said. “Second, DOT tends to be an aggregate measurement of antibiotics used at an institution or hospital location; if an ASP does a specific intervention targeting a group of antibiotics or infectious indication, changes in the hospital-wide DOT or drug-class DOT may not accurately reflect the exact impact of an ASP’s intervention.”
The paper offers an alternative/supplemental method for ASPs to quantify their impact on antibiotic use without using an EMR or needing IT support: Days of Therapy Avoided. “DOTA can be tracked prospectively (or retrospectively) with each intervention an ASP makes, and calculates an exact amount of antibiotic use avoided,” Dr. Laguio-Vila said. “If the ASP also tracks the types of antibiotic recommendations made according to infectious indication, comparison of DOTA between indications – such as pneumonia versus UTI [urinary tract infection] – can lead to ideas of which type of indication needs clinical guidelines development, or order set revision, or which type of infection the ASP should target to reduce high-risk antibiotics.”
Also, she added, because most ASPs have several types of interventions at once (such as education on pneumonia guidelines, as well as penicillin-allergy assessment), aggregate assessments of institutional antibiotic use like the DOT cannot quantify how much impact a specific intervention has accomplished. DOTA may offer a fairer assessment of the direct changes in antibiotic use resulting from specific ASP activities, because tracking DOTA is extracted from each specific patient intervention.
“Now that the Joint Commission has a requirement that all hospitals seeking JC accreditation have some form of an ASP in place and measure antibiotic use in some way at their institution, there may be numerous hospitals facing the same challenges with calculating a DOT. DOTA would meet these requirements, but in a ‘low tech’ way,” Dr. Laguio-Vila said. “For hospitalists with interests in being the antibiotic steward or champion for their institution, DOTA is an option for measuring antibiotic use.”
Reference
Datta S et al. Days of therapy avoided: A novel method for measuring the impact of an antimicrobial stewardship program to stop antibiotics. J Hosp Med. 2018 Feb 8. doi: 10.12788/jhm.2927.
The currently recommended method for hospital antimicrobial stewardship programs (ASPs) to measure antibiotic use is Days of Therapy/1,000 patient-days, but there are a few disadvantages of using the DOT, said Maryrose Laguio-Vila, MD, coauthor of a recent study on stewardship.
“For accurate measurement, it requires information technology (IT) support to assist an ASP in generating reports of antibiotic prescriptions and administrations to patients, often from an electronic medical record (EMR). In hospitals where there is no EMR, DOT is probably not easily done and would have to be manually extracted (a herculean task),” she said. “Second, DOT tends to be an aggregate measurement of antibiotics used at an institution or hospital location; if an ASP does a specific intervention targeting a group of antibiotics or infectious indication, changes in the hospital-wide DOT or drug-class DOT may not accurately reflect the exact impact of an ASP’s intervention.”
The paper offers an alternative/supplemental method for ASPs to quantify their impact on antibiotic use without using an EMR or needing IT support: Days of Therapy Avoided. “DOTA can be tracked prospectively (or retrospectively) with each intervention an ASP makes, and calculates an exact amount of antibiotic use avoided,” Dr. Laguio-Vila said. “If the ASP also tracks the types of antibiotic recommendations made according to infectious indication, comparison of DOTA between indications – such as pneumonia versus UTI [urinary tract infection] – can lead to ideas of which type of indication needs clinical guidelines development, or order set revision, or which type of infection the ASP should target to reduce high-risk antibiotics.”
Also, she added, because most ASPs have several types of interventions at once (such as education on pneumonia guidelines, as well as penicillin-allergy assessment), aggregate assessments of institutional antibiotic use like the DOT cannot quantify how much impact a specific intervention has accomplished. DOTA may offer a fairer assessment of the direct changes in antibiotic use resulting from specific ASP activities, because tracking DOTA is extracted from each specific patient intervention.
“Now that the Joint Commission has a requirement that all hospitals seeking JC accreditation have some form of an ASP in place and measure antibiotic use in some way at their institution, there may be numerous hospitals facing the same challenges with calculating a DOT. DOTA would meet these requirements, but in a ‘low tech’ way,” Dr. Laguio-Vila said. “For hospitalists with interests in being the antibiotic steward or champion for their institution, DOTA is an option for measuring antibiotic use.”
Reference
Datta S et al. Days of therapy avoided: A novel method for measuring the impact of an antimicrobial stewardship program to stop antibiotics. J Hosp Med. 2018 Feb 8. doi: 10.12788/jhm.2927.
Bring Schwartz Rounds to your hospital
A more emotional approach to rounds
If you are not doing Schwartz Rounds, get them started. ASAP.
I recently completed a 4-year tenure as physician moderator for our hospital’s Schwartz Rounds. An amazing team at my hospital helped pull the bimonthly sessions together. These compassionate care rounds are a national initiative to help foster empathy and compassion in the health care setting.
We gather a panel of two to three people involved in our patient presentation who share and move quickly through the clinical details, and head on toward the thornier ethical issues, emotional triggers, and responses. The best sessions are when the audience’s voice is heard for the bulk of the time.
The emotional cadence flows from boiling in frustration, drowning in tears, followed by comfort, and ending in thoughts for the next session. It is a more powerful arc than an episode of the television program “This is Us.” Largely, because this was us. This was real life. Real-time catharsis in the hospital.
In the daily grind, we often skip the step of processing our frustration, sadness, and anger, moving right on to the next patient and walking into the next room with that stoic layer of equanimity. I walk the hallways and find I grab my phone to catch up on emails, walking to the wrong floor because I’m not paying attention. Always something to do, someone to talk to, a family to call, pagers going off, phone calls. When do we sit and reflect?
These Schwartz Rounds are those moments of reflection – a slowdown in the day to think more deeply about the case. We talk about everything and anything. We have discussions with opposing views:
“Everything should have been done!”
“How did you not stop care?!”
“I agree with the doctors.”
“I can see the patient’s view more clearly now.”
Our first Schwartz Rounds tended to be end-of-life stories, particularly regarding the family mantra of “Do everything.” The health care team watches the suffering of a patient, a family, in a seemingly futile situation. Conversations around the end of life, choices, and quality of life are cut short daily by family members who simply recite, “Do everything.”
After several of these sessions, a case swings us in the other direction. The elderly gentleman with treatable cancer, who could easily survive another 20 years, declines treatment. “I’m fine, doc; I’ve lived long enough.” His wife at his bedside, shaking her head, tells us, “I don’t know why he wants to give up. He’s been as stubborn as a mule since the day I met him.” I spend 30 minutes convincing him to stay. The nurse does the same. Now we have a patient with a “Do nothing.” The patient’s decisions conflict with the family and the health care team.
Every day in the hospital provides a new ethical dilemma, a frustrating case, a challenging patient. Fodder for rounds.
Read the full post at hospitalleader.org.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control.
Also on The Hospital Leader
- Incubating Success: How We Used Structured Feedback to Reduce A Dangerous Practice by Rich Bottner, PA-C & Victoria Valencia, MPH
- New SoHM Report Provides Unique Window into Hospital Medicine Practice Trends by Leslie Flores, MHA, SFHM
- IGNITE Change: Improving Care via Interprofessional Clinical Learning Environments by Vineet Arora, MD, MAPP, MHM
A more emotional approach to rounds
A more emotional approach to rounds
If you are not doing Schwartz Rounds, get them started. ASAP.
I recently completed a 4-year tenure as physician moderator for our hospital’s Schwartz Rounds. An amazing team at my hospital helped pull the bimonthly sessions together. These compassionate care rounds are a national initiative to help foster empathy and compassion in the health care setting.
We gather a panel of two to three people involved in our patient presentation who share and move quickly through the clinical details, and head on toward the thornier ethical issues, emotional triggers, and responses. The best sessions are when the audience’s voice is heard for the bulk of the time.
The emotional cadence flows from boiling in frustration, drowning in tears, followed by comfort, and ending in thoughts for the next session. It is a more powerful arc than an episode of the television program “This is Us.” Largely, because this was us. This was real life. Real-time catharsis in the hospital.
In the daily grind, we often skip the step of processing our frustration, sadness, and anger, moving right on to the next patient and walking into the next room with that stoic layer of equanimity. I walk the hallways and find I grab my phone to catch up on emails, walking to the wrong floor because I’m not paying attention. Always something to do, someone to talk to, a family to call, pagers going off, phone calls. When do we sit and reflect?
These Schwartz Rounds are those moments of reflection – a slowdown in the day to think more deeply about the case. We talk about everything and anything. We have discussions with opposing views:
“Everything should have been done!”
“How did you not stop care?!”
“I agree with the doctors.”
“I can see the patient’s view more clearly now.”
Our first Schwartz Rounds tended to be end-of-life stories, particularly regarding the family mantra of “Do everything.” The health care team watches the suffering of a patient, a family, in a seemingly futile situation. Conversations around the end of life, choices, and quality of life are cut short daily by family members who simply recite, “Do everything.”
After several of these sessions, a case swings us in the other direction. The elderly gentleman with treatable cancer, who could easily survive another 20 years, declines treatment. “I’m fine, doc; I’ve lived long enough.” His wife at his bedside, shaking her head, tells us, “I don’t know why he wants to give up. He’s been as stubborn as a mule since the day I met him.” I spend 30 minutes convincing him to stay. The nurse does the same. Now we have a patient with a “Do nothing.” The patient’s decisions conflict with the family and the health care team.
Every day in the hospital provides a new ethical dilemma, a frustrating case, a challenging patient. Fodder for rounds.
Read the full post at hospitalleader.org.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control.
Also on The Hospital Leader
- Incubating Success: How We Used Structured Feedback to Reduce A Dangerous Practice by Rich Bottner, PA-C & Victoria Valencia, MPH
- New SoHM Report Provides Unique Window into Hospital Medicine Practice Trends by Leslie Flores, MHA, SFHM
- IGNITE Change: Improving Care via Interprofessional Clinical Learning Environments by Vineet Arora, MD, MAPP, MHM
If you are not doing Schwartz Rounds, get them started. ASAP.
I recently completed a 4-year tenure as physician moderator for our hospital’s Schwartz Rounds. An amazing team at my hospital helped pull the bimonthly sessions together. These compassionate care rounds are a national initiative to help foster empathy and compassion in the health care setting.
We gather a panel of two to three people involved in our patient presentation who share and move quickly through the clinical details, and head on toward the thornier ethical issues, emotional triggers, and responses. The best sessions are when the audience’s voice is heard for the bulk of the time.
The emotional cadence flows from boiling in frustration, drowning in tears, followed by comfort, and ending in thoughts for the next session. It is a more powerful arc than an episode of the television program “This is Us.” Largely, because this was us. This was real life. Real-time catharsis in the hospital.
In the daily grind, we often skip the step of processing our frustration, sadness, and anger, moving right on to the next patient and walking into the next room with that stoic layer of equanimity. I walk the hallways and find I grab my phone to catch up on emails, walking to the wrong floor because I’m not paying attention. Always something to do, someone to talk to, a family to call, pagers going off, phone calls. When do we sit and reflect?
These Schwartz Rounds are those moments of reflection – a slowdown in the day to think more deeply about the case. We talk about everything and anything. We have discussions with opposing views:
“Everything should have been done!”
“How did you not stop care?!”
“I agree with the doctors.”
“I can see the patient’s view more clearly now.”
Our first Schwartz Rounds tended to be end-of-life stories, particularly regarding the family mantra of “Do everything.” The health care team watches the suffering of a patient, a family, in a seemingly futile situation. Conversations around the end of life, choices, and quality of life are cut short daily by family members who simply recite, “Do everything.”
After several of these sessions, a case swings us in the other direction. The elderly gentleman with treatable cancer, who could easily survive another 20 years, declines treatment. “I’m fine, doc; I’ve lived long enough.” His wife at his bedside, shaking her head, tells us, “I don’t know why he wants to give up. He’s been as stubborn as a mule since the day I met him.” I spend 30 minutes convincing him to stay. The nurse does the same. Now we have a patient with a “Do nothing.” The patient’s decisions conflict with the family and the health care team.
Every day in the hospital provides a new ethical dilemma, a frustrating case, a challenging patient. Fodder for rounds.
Read the full post at hospitalleader.org.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control.
Also on The Hospital Leader
- Incubating Success: How We Used Structured Feedback to Reduce A Dangerous Practice by Rich Bottner, PA-C & Victoria Valencia, MPH
- New SoHM Report Provides Unique Window into Hospital Medicine Practice Trends by Leslie Flores, MHA, SFHM
- IGNITE Change: Improving Care via Interprofessional Clinical Learning Environments by Vineet Arora, MD, MAPP, MHM
Giving hospitalists a larger clinical footprint
Something you did not know about warm handoffs
I am going to teach you something you do not know. I am almost sure of it.
Warm handoffs – a term you often hear within the confines of hospital walls when transferring a patient service to service or ward to ward. You do it in-house, but it’s unlikely you make the same connection when you discharge the same patient or transfer them to an outside entity.
But you have to be asleep under a rock not to have heard or read the changes afoot in the skilled nursing facility (SNF) realm, including the rise of the “SNFist”. Too much variation in use and spending; plus, we are learning patients do not need 25 days cooped up in a rehabilitation facility when 15 might do with a segue into home health for another 10 or 14. Patients like being home, and it costs a lot less.
Unfortunately, we do not do SNF handoffs in the same manner as ICUs. Our bad, and inpatient providers better adapt.
As hospitals decant and quality measures get an intimate look in the rehab space, SNFs will notice sicker patients, and the staff there will be more mindful of the sign outs and the data they receive. Know a Centers for Medicare & Medicaid Services value-based program started on October 1 (just like hospitals – penalties and all) and SNFists, whoever they might be – NP/PA/DO/MD – will also require of hospitals a step-up in information transfer, both in quality and timeliness.
Read the full post at hospitalleader.org.
Also on The Hospital Leader
- “Immigration & the Future of Healthcare: Looking to a Greater Good,” by Jordan Messler, MD, SFHM
- “We Must Become Comfortable Talking about Physician Suicide,” by Tracy Cardin, ACNP-BC, SFHM
- “A New Light in the Darkness: Using Hospital-Based Medication-Assisted Treatment to Tackle the Opioid Crisis,” by Richard Bottner, PA-C
Something you did not know about warm handoffs
Something you did not know about warm handoffs
I am going to teach you something you do not know. I am almost sure of it.
Warm handoffs – a term you often hear within the confines of hospital walls when transferring a patient service to service or ward to ward. You do it in-house, but it’s unlikely you make the same connection when you discharge the same patient or transfer them to an outside entity.
But you have to be asleep under a rock not to have heard or read the changes afoot in the skilled nursing facility (SNF) realm, including the rise of the “SNFist”. Too much variation in use and spending; plus, we are learning patients do not need 25 days cooped up in a rehabilitation facility when 15 might do with a segue into home health for another 10 or 14. Patients like being home, and it costs a lot less.
Unfortunately, we do not do SNF handoffs in the same manner as ICUs. Our bad, and inpatient providers better adapt.
As hospitals decant and quality measures get an intimate look in the rehab space, SNFs will notice sicker patients, and the staff there will be more mindful of the sign outs and the data they receive. Know a Centers for Medicare & Medicaid Services value-based program started on October 1 (just like hospitals – penalties and all) and SNFists, whoever they might be – NP/PA/DO/MD – will also require of hospitals a step-up in information transfer, both in quality and timeliness.
Read the full post at hospitalleader.org.
Also on The Hospital Leader
- “Immigration & the Future of Healthcare: Looking to a Greater Good,” by Jordan Messler, MD, SFHM
- “We Must Become Comfortable Talking about Physician Suicide,” by Tracy Cardin, ACNP-BC, SFHM
- “A New Light in the Darkness: Using Hospital-Based Medication-Assisted Treatment to Tackle the Opioid Crisis,” by Richard Bottner, PA-C
I am going to teach you something you do not know. I am almost sure of it.
Warm handoffs – a term you often hear within the confines of hospital walls when transferring a patient service to service or ward to ward. You do it in-house, but it’s unlikely you make the same connection when you discharge the same patient or transfer them to an outside entity.
But you have to be asleep under a rock not to have heard or read the changes afoot in the skilled nursing facility (SNF) realm, including the rise of the “SNFist”. Too much variation in use and spending; plus, we are learning patients do not need 25 days cooped up in a rehabilitation facility when 15 might do with a segue into home health for another 10 or 14. Patients like being home, and it costs a lot less.
Unfortunately, we do not do SNF handoffs in the same manner as ICUs. Our bad, and inpatient providers better adapt.
As hospitals decant and quality measures get an intimate look in the rehab space, SNFs will notice sicker patients, and the staff there will be more mindful of the sign outs and the data they receive. Know a Centers for Medicare & Medicaid Services value-based program started on October 1 (just like hospitals – penalties and all) and SNFists, whoever they might be – NP/PA/DO/MD – will also require of hospitals a step-up in information transfer, both in quality and timeliness.
Read the full post at hospitalleader.org.
Also on The Hospital Leader
- “Immigration & the Future of Healthcare: Looking to a Greater Good,” by Jordan Messler, MD, SFHM
- “We Must Become Comfortable Talking about Physician Suicide,” by Tracy Cardin, ACNP-BC, SFHM
- “A New Light in the Darkness: Using Hospital-Based Medication-Assisted Treatment to Tackle the Opioid Crisis,” by Richard Bottner, PA-C
Patient-centered primed communication and goals-of-care discussions
Clinical question: Can primed communication increase the frequency of goals-of-care conversations in the outpatient setting?
Background: Effective outpatient communication helps patients and families with serious illnesses with increased quality of life, improved quality of the dying process, and decreased resource utilization at the end of life.
Study design: Cluster-randomized trial.
Setting: Multicenter, primary care, and subspecialty clinics for adults in the Pacific Northwest.
Synopsis: Patients with advanced age and/or severe chronic medical conditions were selected to participate. The median survival for these patients was 2 years. Clinicians were eligible to participate if they had five or more of the selected patients in their panel.
In the intervention group (57 clinicians and 184 patients), all patients were surveyed to identify preferences, barriers, and facilitators for goals-of-care discussions. These data were compiled into “Jumpstart Tips” and distributed to providers before a visit with a study patient. The control group (57 clinicians and 211 patients) had patients complete these surveys but no information was provided to clinicians.
The “Jumpstart Tips” led to an increase in patient-reported (74% vs. 31%; P less than .001) and EHR-documented (62% vs. 17%; P less than .001) occurrences of goals-of-care discussions. Patients also reported increased quality of these conversations (4.6 vs. 2.1; P = .01).
However, no significant improvements were noted in goal-concordant care, depression, or anxiety scores, which may have been because of selection bias and overall difficulty in defining goal-concordant care.
Bottom line: Patient-centered primed communication can increase the frequency and quality of goals-of-care discussions in the outpatient setting.
Citation: Curtis JR et al. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: A randomized clinical trial. JAMA Intern Med. 2018 Jul 1;178(7):930-40.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Can primed communication increase the frequency of goals-of-care conversations in the outpatient setting?
Background: Effective outpatient communication helps patients and families with serious illnesses with increased quality of life, improved quality of the dying process, and decreased resource utilization at the end of life.
Study design: Cluster-randomized trial.
Setting: Multicenter, primary care, and subspecialty clinics for adults in the Pacific Northwest.
Synopsis: Patients with advanced age and/or severe chronic medical conditions were selected to participate. The median survival for these patients was 2 years. Clinicians were eligible to participate if they had five or more of the selected patients in their panel.
In the intervention group (57 clinicians and 184 patients), all patients were surveyed to identify preferences, barriers, and facilitators for goals-of-care discussions. These data were compiled into “Jumpstart Tips” and distributed to providers before a visit with a study patient. The control group (57 clinicians and 211 patients) had patients complete these surveys but no information was provided to clinicians.
The “Jumpstart Tips” led to an increase in patient-reported (74% vs. 31%; P less than .001) and EHR-documented (62% vs. 17%; P less than .001) occurrences of goals-of-care discussions. Patients also reported increased quality of these conversations (4.6 vs. 2.1; P = .01).
However, no significant improvements were noted in goal-concordant care, depression, or anxiety scores, which may have been because of selection bias and overall difficulty in defining goal-concordant care.
Bottom line: Patient-centered primed communication can increase the frequency and quality of goals-of-care discussions in the outpatient setting.
Citation: Curtis JR et al. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: A randomized clinical trial. JAMA Intern Med. 2018 Jul 1;178(7):930-40.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Can primed communication increase the frequency of goals-of-care conversations in the outpatient setting?
Background: Effective outpatient communication helps patients and families with serious illnesses with increased quality of life, improved quality of the dying process, and decreased resource utilization at the end of life.
Study design: Cluster-randomized trial.
Setting: Multicenter, primary care, and subspecialty clinics for adults in the Pacific Northwest.
Synopsis: Patients with advanced age and/or severe chronic medical conditions were selected to participate. The median survival for these patients was 2 years. Clinicians were eligible to participate if they had five or more of the selected patients in their panel.
In the intervention group (57 clinicians and 184 patients), all patients were surveyed to identify preferences, barriers, and facilitators for goals-of-care discussions. These data were compiled into “Jumpstart Tips” and distributed to providers before a visit with a study patient. The control group (57 clinicians and 211 patients) had patients complete these surveys but no information was provided to clinicians.
The “Jumpstart Tips” led to an increase in patient-reported (74% vs. 31%; P less than .001) and EHR-documented (62% vs. 17%; P less than .001) occurrences of goals-of-care discussions. Patients also reported increased quality of these conversations (4.6 vs. 2.1; P = .01).
However, no significant improvements were noted in goal-concordant care, depression, or anxiety scores, which may have been because of selection bias and overall difficulty in defining goal-concordant care.
Bottom line: Patient-centered primed communication can increase the frequency and quality of goals-of-care discussions in the outpatient setting.
Citation: Curtis JR et al. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: A randomized clinical trial. JAMA Intern Med. 2018 Jul 1;178(7):930-40.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.