User login
The Hospitalist only
How To Avoid Medicare Denials for Critical-Care Billing
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
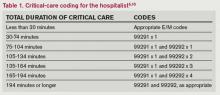
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Feds Extend HIPAA Obligations, Violation Penalties
On Jan. 17, 2013, the Office for Civil Rights (OCR) of the U.S. Department of Health and Human Services (HHS) issued an omnibus Final Rule implementing various provisions of the Health Information Technology for Economic and Clinical Health, or HITECH, Act. The Final Rule revises the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the interim final Breach Notification Rule.
The HITECH Act, which took effect as part of the American Recovery and Reinvestment Act of 2009, expanded the obligations of covered entities and business associates to protect the confidentiality and security of protected health information (PHI).
Under HIPAA, “covered entities” may disclose PHI to “business associates,” and permit business associates to create and receive PHI on behalf of the covered entity, subject to the terms of a business-associate agreement between the parties. A “covered entity” is defined as a health plan, healthcare clearinghouse, or healthcare provider (e.g. physician practice or hospital) that transmits health information electronically. In general, the HIPAA regulations have traditionally defined a “business associate” as a person (other than a member of the covered entity’s workforce) or entity who, on behalf of a covered entity, performs a function or activity involving the use or disclosure of PHI, such as the performance of financial, legal, actuarial, accounting, consulting, data aggregation, management, administrative, or accreditation services to or for a covered entity.
Prior to the HITECH Act, business associates were contractually obligated to maintain the privacy and security of PHI but could not be sanctioned for failing to comply with HIPAA. The HITECH Act expands those obligations and exposure of business associates by:
- Applying many of the privacy and security standards to business associates;
- Subjecting business associates to the breach-notification requirements; and
- Imposing civil and criminal penalties on business associates for HIPAA violations.
In addition, the HITECH Act strengthened the penalties and enforcement mechanisms under HIPAA and required periodic audits to ensure that covered entities and business associates are compliant.
Expansion of Breach-Notification Requirements
The Final Rule expands the breach-notification obligations of covered entities and business associates by revising the definition of “breach” and the risk-assessment process for determining whether notification is required. A use or disclosure of unsecured PHI that is not permitted under the Privacy Rule is presumed to be a breach (and therefore requires notification to the individual, OCR, and possibly the media) unless the incident satisfies an exception, or the covered entity or business associate demonstrates a low probability that PHI has been compromised.1 This risk analysis is based on at least the following four factors:
- The nature and extent of the PHI, including the types of identifiers and the likelihood of re-identification;
- The unauthorized person who used or accessed the PHI;
- Whether the PHI was actually acquired or viewed; and
- The extent to which the risk is mitigated (e.g. by obtaining reliable assurances by a recipient of PHI that the information will be destroyed or will not be used or disclosed).
Expansion of Business-Associate Obligations
The Final Rule implements the HITECH Act’s expansion of business associates’ HIPAA obligations by applying the Privacy and Security Rules directly to business associates and by imposing civil and criminal penalties on business associates for HIPAA violations. It also extends obligations and potential penalties to subcontractors of business associates if a business associate delegates a function, activity, or service to the subcontractor, and the subcontractor creates, receives, maintains, or transmits PHI on behalf of the business associate. Any business associate that delegates a function involving the use or disclosure of PHI to a subcontractor will be required to enter into a business-associate agreement with the subcontractor.
Additional Provisions
The Final Rule addresses the following additional issues by:
- Requiring covered entities to modify their Notices of Privacy Practices;
- Allowing individuals to obtain a copy of PHI in an electronic format if the covered entity uses an electronic health record;
- Restricting marketing activities;
- Allowing covered entities to disclose relevant PHI of a deceased person to a family member, close friend, or other person designated by the deceased, unless the disclosure is inconsistent with the deceased person’s known prior expressed preference;
- Requiring covered entities to agree to an individual’s request to restrict disclosure of PHI to a health plan when the individual (or someone other than the health plan) pays for the healthcare item or service in full;
- Revising the definition of PHI to exclude information about a person who has been deceased for more than 50 years;
- Prohibiting the sale of PHI without authorization from the individual, and adding a requirement of authorization in order for a covered entity to receive remuneration for disclosing PHI;
- Clarifying OCR’s view that covered entities are allowed to send electronic PHI to individuals in unencrypted e-mails only after notifying the individual of the risk;
- Prohibiting health plans from using or disclosing genetic information for underwriting, as required by the Genetic Information Nondiscrimination Act of 2008 (GINA);
- Allowing disclosure of proof of immunization to schools if agreed by the parent, guardian, or individual;
- Permitting compound authorizations for clinical-research studies; and
- Revising the Enforcement Rule (which was previously revised in 2009 as an interim Final Rule), which:
- Requires the secretary of HHS to investigate a HIPAA complaint if a preliminary investigation indicates a possible violation due to willful neglect;
- Permits HHS to disclose PHI to other government agencies (including state attorneys general) for civil or criminal law-enforcement purposes; and
- Revises standards for determining the levels of civil money penalties.
Effective Date, Compliance Date
Although most provisions of the Final Rule became effective on March 26, many provisions impacting covered entities and business associates (including subcontractors) required compliance by Sept. 23. However, if certain conditions are met, the Final Rule allows additional time to revise business associate agreements to make them compliant. In particular, transition provisions will allow covered entities and business associates to continue to operate under existing business-associate agreements for up to one year beyond the compliance date (until Sept. 22, 2014) if the business-associate agreement:
- Is in writing;
- Is in place prior to Jan. 25, 2013 (the publication date of the Final Rule);
- Is compliant with the Privacy and Security Rules, in effect immediately prior to Jan. 25, 2013; and
- Is not modified or renewed.
This additional time for grandfathered business-associate agreements applies only to the written-documentation requirement. Covered entities, business associates and subcontractors will be required to comply with all other HIPAA requirements beginning on the compliance date, even if the business-associate agreement qualifies for grandfathered status
Steven M. Harris, Esq., is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at sharris@mcdonaldhopkins.com.
Footnote
The exceptions relate to (i) unintentional, good-faith access, acquisition or use by members of the covered entity’s or business associate’s workforce, (ii) inadvertent disclosure limited to persons with authorized access and not resulting in further unpermitted use or disclosure, and (iii) good-faith belief that the unauthorized recipient would be unable to retain the PHI.
On Jan. 17, 2013, the Office for Civil Rights (OCR) of the U.S. Department of Health and Human Services (HHS) issued an omnibus Final Rule implementing various provisions of the Health Information Technology for Economic and Clinical Health, or HITECH, Act. The Final Rule revises the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the interim final Breach Notification Rule.
The HITECH Act, which took effect as part of the American Recovery and Reinvestment Act of 2009, expanded the obligations of covered entities and business associates to protect the confidentiality and security of protected health information (PHI).
Under HIPAA, “covered entities” may disclose PHI to “business associates,” and permit business associates to create and receive PHI on behalf of the covered entity, subject to the terms of a business-associate agreement between the parties. A “covered entity” is defined as a health plan, healthcare clearinghouse, or healthcare provider (e.g. physician practice or hospital) that transmits health information electronically. In general, the HIPAA regulations have traditionally defined a “business associate” as a person (other than a member of the covered entity’s workforce) or entity who, on behalf of a covered entity, performs a function or activity involving the use or disclosure of PHI, such as the performance of financial, legal, actuarial, accounting, consulting, data aggregation, management, administrative, or accreditation services to or for a covered entity.
Prior to the HITECH Act, business associates were contractually obligated to maintain the privacy and security of PHI but could not be sanctioned for failing to comply with HIPAA. The HITECH Act expands those obligations and exposure of business associates by:
- Applying many of the privacy and security standards to business associates;
- Subjecting business associates to the breach-notification requirements; and
- Imposing civil and criminal penalties on business associates for HIPAA violations.
In addition, the HITECH Act strengthened the penalties and enforcement mechanisms under HIPAA and required periodic audits to ensure that covered entities and business associates are compliant.
Expansion of Breach-Notification Requirements
The Final Rule expands the breach-notification obligations of covered entities and business associates by revising the definition of “breach” and the risk-assessment process for determining whether notification is required. A use or disclosure of unsecured PHI that is not permitted under the Privacy Rule is presumed to be a breach (and therefore requires notification to the individual, OCR, and possibly the media) unless the incident satisfies an exception, or the covered entity or business associate demonstrates a low probability that PHI has been compromised.1 This risk analysis is based on at least the following four factors:
- The nature and extent of the PHI, including the types of identifiers and the likelihood of re-identification;
- The unauthorized person who used or accessed the PHI;
- Whether the PHI was actually acquired or viewed; and
- The extent to which the risk is mitigated (e.g. by obtaining reliable assurances by a recipient of PHI that the information will be destroyed or will not be used or disclosed).
Expansion of Business-Associate Obligations
The Final Rule implements the HITECH Act’s expansion of business associates’ HIPAA obligations by applying the Privacy and Security Rules directly to business associates and by imposing civil and criminal penalties on business associates for HIPAA violations. It also extends obligations and potential penalties to subcontractors of business associates if a business associate delegates a function, activity, or service to the subcontractor, and the subcontractor creates, receives, maintains, or transmits PHI on behalf of the business associate. Any business associate that delegates a function involving the use or disclosure of PHI to a subcontractor will be required to enter into a business-associate agreement with the subcontractor.
Additional Provisions
The Final Rule addresses the following additional issues by:
- Requiring covered entities to modify their Notices of Privacy Practices;
- Allowing individuals to obtain a copy of PHI in an electronic format if the covered entity uses an electronic health record;
- Restricting marketing activities;
- Allowing covered entities to disclose relevant PHI of a deceased person to a family member, close friend, or other person designated by the deceased, unless the disclosure is inconsistent with the deceased person’s known prior expressed preference;
- Requiring covered entities to agree to an individual’s request to restrict disclosure of PHI to a health plan when the individual (or someone other than the health plan) pays for the healthcare item or service in full;
- Revising the definition of PHI to exclude information about a person who has been deceased for more than 50 years;
- Prohibiting the sale of PHI without authorization from the individual, and adding a requirement of authorization in order for a covered entity to receive remuneration for disclosing PHI;
- Clarifying OCR’s view that covered entities are allowed to send electronic PHI to individuals in unencrypted e-mails only after notifying the individual of the risk;
- Prohibiting health plans from using or disclosing genetic information for underwriting, as required by the Genetic Information Nondiscrimination Act of 2008 (GINA);
- Allowing disclosure of proof of immunization to schools if agreed by the parent, guardian, or individual;
- Permitting compound authorizations for clinical-research studies; and
- Revising the Enforcement Rule (which was previously revised in 2009 as an interim Final Rule), which:
- Requires the secretary of HHS to investigate a HIPAA complaint if a preliminary investigation indicates a possible violation due to willful neglect;
- Permits HHS to disclose PHI to other government agencies (including state attorneys general) for civil or criminal law-enforcement purposes; and
- Revises standards for determining the levels of civil money penalties.
Effective Date, Compliance Date
Although most provisions of the Final Rule became effective on March 26, many provisions impacting covered entities and business associates (including subcontractors) required compliance by Sept. 23. However, if certain conditions are met, the Final Rule allows additional time to revise business associate agreements to make them compliant. In particular, transition provisions will allow covered entities and business associates to continue to operate under existing business-associate agreements for up to one year beyond the compliance date (until Sept. 22, 2014) if the business-associate agreement:
- Is in writing;
- Is in place prior to Jan. 25, 2013 (the publication date of the Final Rule);
- Is compliant with the Privacy and Security Rules, in effect immediately prior to Jan. 25, 2013; and
- Is not modified or renewed.
This additional time for grandfathered business-associate agreements applies only to the written-documentation requirement. Covered entities, business associates and subcontractors will be required to comply with all other HIPAA requirements beginning on the compliance date, even if the business-associate agreement qualifies for grandfathered status
Steven M. Harris, Esq., is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at sharris@mcdonaldhopkins.com.
Footnote
The exceptions relate to (i) unintentional, good-faith access, acquisition or use by members of the covered entity’s or business associate’s workforce, (ii) inadvertent disclosure limited to persons with authorized access and not resulting in further unpermitted use or disclosure, and (iii) good-faith belief that the unauthorized recipient would be unable to retain the PHI.
On Jan. 17, 2013, the Office for Civil Rights (OCR) of the U.S. Department of Health and Human Services (HHS) issued an omnibus Final Rule implementing various provisions of the Health Information Technology for Economic and Clinical Health, or HITECH, Act. The Final Rule revises the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the interim final Breach Notification Rule.
The HITECH Act, which took effect as part of the American Recovery and Reinvestment Act of 2009, expanded the obligations of covered entities and business associates to protect the confidentiality and security of protected health information (PHI).
Under HIPAA, “covered entities” may disclose PHI to “business associates,” and permit business associates to create and receive PHI on behalf of the covered entity, subject to the terms of a business-associate agreement between the parties. A “covered entity” is defined as a health plan, healthcare clearinghouse, or healthcare provider (e.g. physician practice or hospital) that transmits health information electronically. In general, the HIPAA regulations have traditionally defined a “business associate” as a person (other than a member of the covered entity’s workforce) or entity who, on behalf of a covered entity, performs a function or activity involving the use or disclosure of PHI, such as the performance of financial, legal, actuarial, accounting, consulting, data aggregation, management, administrative, or accreditation services to or for a covered entity.
Prior to the HITECH Act, business associates were contractually obligated to maintain the privacy and security of PHI but could not be sanctioned for failing to comply with HIPAA. The HITECH Act expands those obligations and exposure of business associates by:
- Applying many of the privacy and security standards to business associates;
- Subjecting business associates to the breach-notification requirements; and
- Imposing civil and criminal penalties on business associates for HIPAA violations.
In addition, the HITECH Act strengthened the penalties and enforcement mechanisms under HIPAA and required periodic audits to ensure that covered entities and business associates are compliant.
Expansion of Breach-Notification Requirements
The Final Rule expands the breach-notification obligations of covered entities and business associates by revising the definition of “breach” and the risk-assessment process for determining whether notification is required. A use or disclosure of unsecured PHI that is not permitted under the Privacy Rule is presumed to be a breach (and therefore requires notification to the individual, OCR, and possibly the media) unless the incident satisfies an exception, or the covered entity or business associate demonstrates a low probability that PHI has been compromised.1 This risk analysis is based on at least the following four factors:
- The nature and extent of the PHI, including the types of identifiers and the likelihood of re-identification;
- The unauthorized person who used or accessed the PHI;
- Whether the PHI was actually acquired or viewed; and
- The extent to which the risk is mitigated (e.g. by obtaining reliable assurances by a recipient of PHI that the information will be destroyed or will not be used or disclosed).
Expansion of Business-Associate Obligations
The Final Rule implements the HITECH Act’s expansion of business associates’ HIPAA obligations by applying the Privacy and Security Rules directly to business associates and by imposing civil and criminal penalties on business associates for HIPAA violations. It also extends obligations and potential penalties to subcontractors of business associates if a business associate delegates a function, activity, or service to the subcontractor, and the subcontractor creates, receives, maintains, or transmits PHI on behalf of the business associate. Any business associate that delegates a function involving the use or disclosure of PHI to a subcontractor will be required to enter into a business-associate agreement with the subcontractor.
Additional Provisions
The Final Rule addresses the following additional issues by:
- Requiring covered entities to modify their Notices of Privacy Practices;
- Allowing individuals to obtain a copy of PHI in an electronic format if the covered entity uses an electronic health record;
- Restricting marketing activities;
- Allowing covered entities to disclose relevant PHI of a deceased person to a family member, close friend, or other person designated by the deceased, unless the disclosure is inconsistent with the deceased person’s known prior expressed preference;
- Requiring covered entities to agree to an individual’s request to restrict disclosure of PHI to a health plan when the individual (or someone other than the health plan) pays for the healthcare item or service in full;
- Revising the definition of PHI to exclude information about a person who has been deceased for more than 50 years;
- Prohibiting the sale of PHI without authorization from the individual, and adding a requirement of authorization in order for a covered entity to receive remuneration for disclosing PHI;
- Clarifying OCR’s view that covered entities are allowed to send electronic PHI to individuals in unencrypted e-mails only after notifying the individual of the risk;
- Prohibiting health plans from using or disclosing genetic information for underwriting, as required by the Genetic Information Nondiscrimination Act of 2008 (GINA);
- Allowing disclosure of proof of immunization to schools if agreed by the parent, guardian, or individual;
- Permitting compound authorizations for clinical-research studies; and
- Revising the Enforcement Rule (which was previously revised in 2009 as an interim Final Rule), which:
- Requires the secretary of HHS to investigate a HIPAA complaint if a preliminary investigation indicates a possible violation due to willful neglect;
- Permits HHS to disclose PHI to other government agencies (including state attorneys general) for civil or criminal law-enforcement purposes; and
- Revises standards for determining the levels of civil money penalties.
Effective Date, Compliance Date
Although most provisions of the Final Rule became effective on March 26, many provisions impacting covered entities and business associates (including subcontractors) required compliance by Sept. 23. However, if certain conditions are met, the Final Rule allows additional time to revise business associate agreements to make them compliant. In particular, transition provisions will allow covered entities and business associates to continue to operate under existing business-associate agreements for up to one year beyond the compliance date (until Sept. 22, 2014) if the business-associate agreement:
- Is in writing;
- Is in place prior to Jan. 25, 2013 (the publication date of the Final Rule);
- Is compliant with the Privacy and Security Rules, in effect immediately prior to Jan. 25, 2013; and
- Is not modified or renewed.
This additional time for grandfathered business-associate agreements applies only to the written-documentation requirement. Covered entities, business associates and subcontractors will be required to comply with all other HIPAA requirements beginning on the compliance date, even if the business-associate agreement qualifies for grandfathered status
Steven M. Harris, Esq., is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at sharris@mcdonaldhopkins.com.
Footnote
The exceptions relate to (i) unintentional, good-faith access, acquisition or use by members of the covered entity’s or business associate’s workforce, (ii) inadvertent disclosure limited to persons with authorized access and not resulting in further unpermitted use or disclosure, and (iii) good-faith belief that the unauthorized recipient would be unable to retain the PHI.
Hospitalist Compensation Models Evolve Toward Production, Performance-Based Variables
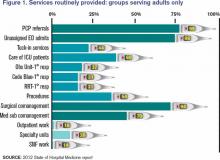
Hospitalists have long recognized that compensation varies significantly by geographic location and by the type of hospitalist medicine group (HMG) you work in: private vs. hospital-owned vs. national-management-owned. A review of SHM’s 2012 State of Hospital Medicine report suggests that hospitalist compensation is also evolving toward a model that more routinely includes both some production variable and performance-based pay (see Figure 1). Although the proportion of compensation paid as a base salary has been trending up over the last few years, so has the proportion paid as a performance incentive.
Source: 2012 State of Hospital Medicine report; www.hospitalmedicine.org/survey
The pay distribution of adult-medicine hospitalists employed by management companies is composed of a high base percentage (mean 88.3% by survey data) and relatively low production and performance variables (mean 6.8% and 4.9%, respectively) compared with other employment models. Contrast that with private hospitalist-only groups, where the mean base is 76.3% with an emphasis on a production component (19.4%) and slightly less on performance pay at 4.2%.
Of the three employment models, however, hospital-/health-system-employed groups have the highest proportion of compensation based on performance metrics with a mean of 7.8%. This makes sense given the financial penalties hospitals and health systems are facing from the Centers for Medicare & Medicaid Services (CMS) around pay-for-performance measures. Hospitals are looking for help from hospitalists in improving quality of care and patient satisfaction and avoiding incurring future penalties. Compensation models in these groups reflect the goals of aligning performance on these measures with financial incentives/risk for hospitalists working in these environments.
What are the top performance metrics hospitalists are being compensated for? CMS’ hospital value-based purchasing (HVBP) core measures and patient satisfaction scores are at the top of the list. More than 70% of all HMGs identify these two measures as part of their performance pay incentive, which is seen consistently by geographic location and by type of hospitalist group.
Beyond these top two metrics, management-company-employed groups also focus on ED throughput measures and early morning discharge times, with more than 70% of these groups having pay incentives aligned with these goals. They also have a higher proportion of their groups participating in several other measures, such as clinical protocols, medication reconciliation, EHR utilization, transitions of care, and readmission rates. In comparison, both hospital-employed and private groups have a wider variety of performance measures in which they participate. Differences are seen geographically, too, with hospitalists located in the Western region having a wider variety of performance measures than other regions.
How hospitalists are compensated for their work will likely continue to evolve. Overall, for nonacademic HMGs serving adults only, we are seeing an upward trend in percentage paid as base pay (from 76% in 2010 to 81% in 2012) and in performance (from 5% in 2010 to 7% in 2012). Hospitalists should anticipate that performance-based pay will continue to account for an increasingly larger percentage of their overall compensation, especially as CMS’ pay-for-performance measures for hospital systems really start to take effect.
Hospital CEOs and CFOs are looking to hospitalists to help deliver on quality, satisfaction, and other performance measures. Incentives will be put in place to reward those groups who do it well.
Dr. Sites is senior medical director of hospitalist programs at Providence Health and Services in Oregon. She is a member of SHM’s Practice Analysis Committee.
Hospitalists have long recognized that compensation varies significantly by geographic location and by the type of hospitalist medicine group (HMG) you work in: private vs. hospital-owned vs. national-management-owned. A review of SHM’s 2012 State of Hospital Medicine report suggests that hospitalist compensation is also evolving toward a model that more routinely includes both some production variable and performance-based pay (see Figure 1). Although the proportion of compensation paid as a base salary has been trending up over the last few years, so has the proportion paid as a performance incentive.
Source: 2012 State of Hospital Medicine report; www.hospitalmedicine.org/survey
The pay distribution of adult-medicine hospitalists employed by management companies is composed of a high base percentage (mean 88.3% by survey data) and relatively low production and performance variables (mean 6.8% and 4.9%, respectively) compared with other employment models. Contrast that with private hospitalist-only groups, where the mean base is 76.3% with an emphasis on a production component (19.4%) and slightly less on performance pay at 4.2%.
Of the three employment models, however, hospital-/health-system-employed groups have the highest proportion of compensation based on performance metrics with a mean of 7.8%. This makes sense given the financial penalties hospitals and health systems are facing from the Centers for Medicare & Medicaid Services (CMS) around pay-for-performance measures. Hospitals are looking for help from hospitalists in improving quality of care and patient satisfaction and avoiding incurring future penalties. Compensation models in these groups reflect the goals of aligning performance on these measures with financial incentives/risk for hospitalists working in these environments.
What are the top performance metrics hospitalists are being compensated for? CMS’ hospital value-based purchasing (HVBP) core measures and patient satisfaction scores are at the top of the list. More than 70% of all HMGs identify these two measures as part of their performance pay incentive, which is seen consistently by geographic location and by type of hospitalist group.
Beyond these top two metrics, management-company-employed groups also focus on ED throughput measures and early morning discharge times, with more than 70% of these groups having pay incentives aligned with these goals. They also have a higher proportion of their groups participating in several other measures, such as clinical protocols, medication reconciliation, EHR utilization, transitions of care, and readmission rates. In comparison, both hospital-employed and private groups have a wider variety of performance measures in which they participate. Differences are seen geographically, too, with hospitalists located in the Western region having a wider variety of performance measures than other regions.
How hospitalists are compensated for their work will likely continue to evolve. Overall, for nonacademic HMGs serving adults only, we are seeing an upward trend in percentage paid as base pay (from 76% in 2010 to 81% in 2012) and in performance (from 5% in 2010 to 7% in 2012). Hospitalists should anticipate that performance-based pay will continue to account for an increasingly larger percentage of their overall compensation, especially as CMS’ pay-for-performance measures for hospital systems really start to take effect.
Hospital CEOs and CFOs are looking to hospitalists to help deliver on quality, satisfaction, and other performance measures. Incentives will be put in place to reward those groups who do it well.
Dr. Sites is senior medical director of hospitalist programs at Providence Health and Services in Oregon. She is a member of SHM’s Practice Analysis Committee.
Hospitalists have long recognized that compensation varies significantly by geographic location and by the type of hospitalist medicine group (HMG) you work in: private vs. hospital-owned vs. national-management-owned. A review of SHM’s 2012 State of Hospital Medicine report suggests that hospitalist compensation is also evolving toward a model that more routinely includes both some production variable and performance-based pay (see Figure 1). Although the proportion of compensation paid as a base salary has been trending up over the last few years, so has the proportion paid as a performance incentive.
Source: 2012 State of Hospital Medicine report; www.hospitalmedicine.org/survey
The pay distribution of adult-medicine hospitalists employed by management companies is composed of a high base percentage (mean 88.3% by survey data) and relatively low production and performance variables (mean 6.8% and 4.9%, respectively) compared with other employment models. Contrast that with private hospitalist-only groups, where the mean base is 76.3% with an emphasis on a production component (19.4%) and slightly less on performance pay at 4.2%.
Of the three employment models, however, hospital-/health-system-employed groups have the highest proportion of compensation based on performance metrics with a mean of 7.8%. This makes sense given the financial penalties hospitals and health systems are facing from the Centers for Medicare & Medicaid Services (CMS) around pay-for-performance measures. Hospitals are looking for help from hospitalists in improving quality of care and patient satisfaction and avoiding incurring future penalties. Compensation models in these groups reflect the goals of aligning performance on these measures with financial incentives/risk for hospitalists working in these environments.
What are the top performance metrics hospitalists are being compensated for? CMS’ hospital value-based purchasing (HVBP) core measures and patient satisfaction scores are at the top of the list. More than 70% of all HMGs identify these two measures as part of their performance pay incentive, which is seen consistently by geographic location and by type of hospitalist group.
Beyond these top two metrics, management-company-employed groups also focus on ED throughput measures and early morning discharge times, with more than 70% of these groups having pay incentives aligned with these goals. They also have a higher proportion of their groups participating in several other measures, such as clinical protocols, medication reconciliation, EHR utilization, transitions of care, and readmission rates. In comparison, both hospital-employed and private groups have a wider variety of performance measures in which they participate. Differences are seen geographically, too, with hospitalists located in the Western region having a wider variety of performance measures than other regions.
How hospitalists are compensated for their work will likely continue to evolve. Overall, for nonacademic HMGs serving adults only, we are seeing an upward trend in percentage paid as base pay (from 76% in 2010 to 81% in 2012) and in performance (from 5% in 2010 to 7% in 2012). Hospitalists should anticipate that performance-based pay will continue to account for an increasingly larger percentage of their overall compensation, especially as CMS’ pay-for-performance measures for hospital systems really start to take effect.
Hospital CEOs and CFOs are looking to hospitalists to help deliver on quality, satisfaction, and other performance measures. Incentives will be put in place to reward those groups who do it well.
Dr. Sites is senior medical director of hospitalist programs at Providence Health and Services in Oregon. She is a member of SHM’s Practice Analysis Committee.
Hospitalist Groups Extract New Solutions Via Data Mining
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
Inside Hospitalists' Evolving Scope of Practice
In the October 2012 issue of The Hospitalist, the “Survey Insights” article discussed hospitalists’ evolving scope of practice based on information published in the 2012 State of Hospital Medicine report. The report remains the most authoritative, comprehensive source of information about our rapidly developing specialty, and this important topic is worthy of continued attention.
As I begin to orient a new class of hospitalists in my own HM group (HMG), I emphasize the five S’s of HMGs: scope, salary, schedule, structure, and society. HMGs define who they are largely by these constructs. As a specialty, we will define who we are by how we develop these constructs as a community. And it may indeed be the scope that most confirms our identity.
The survey (www.hospitalmedicine.org/survey) paints a self-portrait: What do we see when we look at that image? Figure 1 (below) lists information about services routinely provided by hospitalists, and one could divide the findings into three general categories.
First and foremost, there is the core work. It is clear that virtually all HMGs attended to primary-care-physician referrals and unassigned ED hospitalizations, and they also served as at least consultants for surgical comanagement. Most HMGs are now doing medical subspecialty comanagement, and the data would indicate that we are admitting and attending many of these patients. This raises the question about whether our identity will morph to that of the “universal admitter.” Many contend that health-care change forces will continue to pressure in this direction unless, and until, medical subspecialties develop their own dedicated hospitalists. Many hospitals may not be able to resource this; hence, there will likely be persistent pressure for the HMGs to provide this scope of care.
Perhaps half of HMGs provide the second group of services, which includes primary clinical care for rapid-response teams, code blue teams, and observation units. Forty-four percent of adult hospitalist programs provide a “tuck-in” service (nighttime coverage for other providers), and about 50% of HMGs reported performing procedures. Although this graph might suggest a decline in the proportion of groups caring for ICU patients compared with the 78% that was reported in 2011, this data set includes academic practices (the 2011 data didn’t). For nonacademic adult medicine practices, the proportion doing ICU work actually rose to 83.5% in 2012 from 78% in 2011. Larger hospitals and university settings are increasingly employing intensivists for ICU coverage, but the national deficit of intensivists will likely continue the external pressure for hospitalists to provide ICU care in many settings.
The final group of services represents the “road less traveled”—work in outpatient settings in such specialty units as long-term acute care, psychiatric wings, and skilled nursing facilities. These might prove to be niche opportunities or possible distractions.
There remains, however, the core work that identifies our specialty. We all do it, people depend on us to have it done, and it largely defines who we are as individuals, as HMGs, and as the fastest-growing specialty in American medical history.
Dr. Landis is medical director of Wellspan Hospitalists in York, Pa., and a member of SHM’s Practice Analysis Committee.
In the October 2012 issue of The Hospitalist, the “Survey Insights” article discussed hospitalists’ evolving scope of practice based on information published in the 2012 State of Hospital Medicine report. The report remains the most authoritative, comprehensive source of information about our rapidly developing specialty, and this important topic is worthy of continued attention.
As I begin to orient a new class of hospitalists in my own HM group (HMG), I emphasize the five S’s of HMGs: scope, salary, schedule, structure, and society. HMGs define who they are largely by these constructs. As a specialty, we will define who we are by how we develop these constructs as a community. And it may indeed be the scope that most confirms our identity.
The survey (www.hospitalmedicine.org/survey) paints a self-portrait: What do we see when we look at that image? Figure 1 (below) lists information about services routinely provided by hospitalists, and one could divide the findings into three general categories.
First and foremost, there is the core work. It is clear that virtually all HMGs attended to primary-care-physician referrals and unassigned ED hospitalizations, and they also served as at least consultants for surgical comanagement. Most HMGs are now doing medical subspecialty comanagement, and the data would indicate that we are admitting and attending many of these patients. This raises the question about whether our identity will morph to that of the “universal admitter.” Many contend that health-care change forces will continue to pressure in this direction unless, and until, medical subspecialties develop their own dedicated hospitalists. Many hospitals may not be able to resource this; hence, there will likely be persistent pressure for the HMGs to provide this scope of care.
Perhaps half of HMGs provide the second group of services, which includes primary clinical care for rapid-response teams, code blue teams, and observation units. Forty-four percent of adult hospitalist programs provide a “tuck-in” service (nighttime coverage for other providers), and about 50% of HMGs reported performing procedures. Although this graph might suggest a decline in the proportion of groups caring for ICU patients compared with the 78% that was reported in 2011, this data set includes academic practices (the 2011 data didn’t). For nonacademic adult medicine practices, the proportion doing ICU work actually rose to 83.5% in 2012 from 78% in 2011. Larger hospitals and university settings are increasingly employing intensivists for ICU coverage, but the national deficit of intensivists will likely continue the external pressure for hospitalists to provide ICU care in many settings.
The final group of services represents the “road less traveled”—work in outpatient settings in such specialty units as long-term acute care, psychiatric wings, and skilled nursing facilities. These might prove to be niche opportunities or possible distractions.
There remains, however, the core work that identifies our specialty. We all do it, people depend on us to have it done, and it largely defines who we are as individuals, as HMGs, and as the fastest-growing specialty in American medical history.
Dr. Landis is medical director of Wellspan Hospitalists in York, Pa., and a member of SHM’s Practice Analysis Committee.
In the October 2012 issue of The Hospitalist, the “Survey Insights” article discussed hospitalists’ evolving scope of practice based on information published in the 2012 State of Hospital Medicine report. The report remains the most authoritative, comprehensive source of information about our rapidly developing specialty, and this important topic is worthy of continued attention.
As I begin to orient a new class of hospitalists in my own HM group (HMG), I emphasize the five S’s of HMGs: scope, salary, schedule, structure, and society. HMGs define who they are largely by these constructs. As a specialty, we will define who we are by how we develop these constructs as a community. And it may indeed be the scope that most confirms our identity.
The survey (www.hospitalmedicine.org/survey) paints a self-portrait: What do we see when we look at that image? Figure 1 (below) lists information about services routinely provided by hospitalists, and one could divide the findings into three general categories.
First and foremost, there is the core work. It is clear that virtually all HMGs attended to primary-care-physician referrals and unassigned ED hospitalizations, and they also served as at least consultants for surgical comanagement. Most HMGs are now doing medical subspecialty comanagement, and the data would indicate that we are admitting and attending many of these patients. This raises the question about whether our identity will morph to that of the “universal admitter.” Many contend that health-care change forces will continue to pressure in this direction unless, and until, medical subspecialties develop their own dedicated hospitalists. Many hospitals may not be able to resource this; hence, there will likely be persistent pressure for the HMGs to provide this scope of care.
Perhaps half of HMGs provide the second group of services, which includes primary clinical care for rapid-response teams, code blue teams, and observation units. Forty-four percent of adult hospitalist programs provide a “tuck-in” service (nighttime coverage for other providers), and about 50% of HMGs reported performing procedures. Although this graph might suggest a decline in the proportion of groups caring for ICU patients compared with the 78% that was reported in 2011, this data set includes academic practices (the 2011 data didn’t). For nonacademic adult medicine practices, the proportion doing ICU work actually rose to 83.5% in 2012 from 78% in 2011. Larger hospitals and university settings are increasingly employing intensivists for ICU coverage, but the national deficit of intensivists will likely continue the external pressure for hospitalists to provide ICU care in many settings.
The final group of services represents the “road less traveled”—work in outpatient settings in such specialty units as long-term acute care, psychiatric wings, and skilled nursing facilities. These might prove to be niche opportunities or possible distractions.
There remains, however, the core work that identifies our specialty. We all do it, people depend on us to have it done, and it largely defines who we are as individuals, as HMGs, and as the fastest-growing specialty in American medical history.
Dr. Landis is medical director of Wellspan Hospitalists in York, Pa., and a member of SHM’s Practice Analysis Committee.
Multiple Approaches to Combat High Hospital Patient Census
In this age of cost containment and fiscal frugality, how do you handle high-census periods without jeopardizing patient care?
–Michael P. Mason, Tulsa, Okla.
Dr. Hospitalist responds:
Your group must first define the term “high census,” because workload is based on many factors. Seeing 20 patients a day in a large inner-city hospital is much different from seeing 20 patients in a suburban hospital in an affluent part of town. Also, seeing 20 patients geographically located on the same floor is much easier than 20 patients spread all over the hospital. Mid-level or nurse case-management support also makes a difference.
Once defined, there are many different ways to handle the high census; each hospitalist group must decide what works for them.
Many groups rely on their compensation structure to entice their physicians to see higher numbers of patients. The pay structure may be production-based and entice many of the group members to see more patients. Typically, for the member that does not want to see the large volumes, there are usually colleagues who are more than happy to cover the excess patients.
Some groups employ a hybrid system, with their compensation based on production and salary. Generally, bonuses or incentives are applied after meeting a specific relative value unit (RVU) threshold. These thresholds vary and usually are raised periodically based on the percentage of staff able to collect. Again, some group members may volunteer to see the excess patients for higher compensation. It is up to the group to develop mechanisms to measure the quality of care of these high producers and monitor for burnout.
Then there are groups that have no volume incentives and everyone is paid a salary. Many groups that utilize any of these compensation models have group members “on call” to come in when needed and see the excess patients. Many pay the on-call person some nominal amount just for being on call, or a per-patient or hourly rate if they have to come in. Others make it a mandatory part of the schedule without any additional compensation.
Many groups have integrated advanced-practice providers (nurse practitioners and physician assistants) into their systems. They can help hospitalists improve efficiency by seeing patients that are less ill or awaiting placement, or by performing such labor-intensive tasks as admissions and discharges.
HM groups should collaborate with the hospital’s chief financial officer. Like clinicians, most administrators recognize it is very difficult to deliver high-quality and efficient care when the numbers get high. It is in their best interest to help devise strategies and models that deliver quality care and the metrics needed to sustain support.
HM has become such a large specialty that there is no-one-size-fits-all solution to high censuses. In the end, you have to be comfortable with the system created by your group, work to help improve it, or seek a better fit.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to drhospit@wiley.com.
In this age of cost containment and fiscal frugality, how do you handle high-census periods without jeopardizing patient care?
–Michael P. Mason, Tulsa, Okla.
Dr. Hospitalist responds:
Your group must first define the term “high census,” because workload is based on many factors. Seeing 20 patients a day in a large inner-city hospital is much different from seeing 20 patients in a suburban hospital in an affluent part of town. Also, seeing 20 patients geographically located on the same floor is much easier than 20 patients spread all over the hospital. Mid-level or nurse case-management support also makes a difference.
Once defined, there are many different ways to handle the high census; each hospitalist group must decide what works for them.
Many groups rely on their compensation structure to entice their physicians to see higher numbers of patients. The pay structure may be production-based and entice many of the group members to see more patients. Typically, for the member that does not want to see the large volumes, there are usually colleagues who are more than happy to cover the excess patients.
Some groups employ a hybrid system, with their compensation based on production and salary. Generally, bonuses or incentives are applied after meeting a specific relative value unit (RVU) threshold. These thresholds vary and usually are raised periodically based on the percentage of staff able to collect. Again, some group members may volunteer to see the excess patients for higher compensation. It is up to the group to develop mechanisms to measure the quality of care of these high producers and monitor for burnout.
Then there are groups that have no volume incentives and everyone is paid a salary. Many groups that utilize any of these compensation models have group members “on call” to come in when needed and see the excess patients. Many pay the on-call person some nominal amount just for being on call, or a per-patient or hourly rate if they have to come in. Others make it a mandatory part of the schedule without any additional compensation.
Many groups have integrated advanced-practice providers (nurse practitioners and physician assistants) into their systems. They can help hospitalists improve efficiency by seeing patients that are less ill or awaiting placement, or by performing such labor-intensive tasks as admissions and discharges.
HM groups should collaborate with the hospital’s chief financial officer. Like clinicians, most administrators recognize it is very difficult to deliver high-quality and efficient care when the numbers get high. It is in their best interest to help devise strategies and models that deliver quality care and the metrics needed to sustain support.
HM has become such a large specialty that there is no-one-size-fits-all solution to high censuses. In the end, you have to be comfortable with the system created by your group, work to help improve it, or seek a better fit.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to drhospit@wiley.com.
In this age of cost containment and fiscal frugality, how do you handle high-census periods without jeopardizing patient care?
–Michael P. Mason, Tulsa, Okla.
Dr. Hospitalist responds:
Your group must first define the term “high census,” because workload is based on many factors. Seeing 20 patients a day in a large inner-city hospital is much different from seeing 20 patients in a suburban hospital in an affluent part of town. Also, seeing 20 patients geographically located on the same floor is much easier than 20 patients spread all over the hospital. Mid-level or nurse case-management support also makes a difference.
Once defined, there are many different ways to handle the high census; each hospitalist group must decide what works for them.
Many groups rely on their compensation structure to entice their physicians to see higher numbers of patients. The pay structure may be production-based and entice many of the group members to see more patients. Typically, for the member that does not want to see the large volumes, there are usually colleagues who are more than happy to cover the excess patients.
Some groups employ a hybrid system, with their compensation based on production and salary. Generally, bonuses or incentives are applied after meeting a specific relative value unit (RVU) threshold. These thresholds vary and usually are raised periodically based on the percentage of staff able to collect. Again, some group members may volunteer to see the excess patients for higher compensation. It is up to the group to develop mechanisms to measure the quality of care of these high producers and monitor for burnout.
Then there are groups that have no volume incentives and everyone is paid a salary. Many groups that utilize any of these compensation models have group members “on call” to come in when needed and see the excess patients. Many pay the on-call person some nominal amount just for being on call, or a per-patient or hourly rate if they have to come in. Others make it a mandatory part of the schedule without any additional compensation.
Many groups have integrated advanced-practice providers (nurse practitioners and physician assistants) into their systems. They can help hospitalists improve efficiency by seeing patients that are less ill or awaiting placement, or by performing such labor-intensive tasks as admissions and discharges.
HM groups should collaborate with the hospital’s chief financial officer. Like clinicians, most administrators recognize it is very difficult to deliver high-quality and efficient care when the numbers get high. It is in their best interest to help devise strategies and models that deliver quality care and the metrics needed to sustain support.
HM has become such a large specialty that there is no-one-size-fits-all solution to high censuses. In the end, you have to be comfortable with the system created by your group, work to help improve it, or seek a better fit.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to drhospit@wiley.com.
Among Physicians, 59% Would Not Recommend a Medical Career
Percentage of practicing physicians who would not recommend a medical career to a young person, according to Filling The Void: 2013 Physician Outlook Practice Trends, a national physician practice survey conducted by health-care staffing firm Jackson Healthcare.6 “Physician discontent appears to be creating a void in the health-care field,” with dissatisfaction and burnout leading to early retirement, the report stated. Discontent is driven by decreased autonomy, decreased reimbursement, administrative and regulatory distractions, corporatization of medicine, and fear of litigation, according to the report. Thirty-six percent of the respondents reported a generally negative outlook about their career, compared with only 16% who had a generally favorable outlook.
Larry Beresford is a freelance writer in San Francisco.
References
- Hartocollis A. With money at risk, hospitals push staff to wash hands. The New York Times website. Available at: http://www.nytimes.com/2013/05/29/nyregion/hospitals-struggle-to-get-workers-to-wash-their-hands.html?pagewanted=all&_r=0. Accessed May 28, 2013.
- Cumbler E, Castillo L, Satorie L, et al. Culture change in infection control: applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013 May 10 [Epub ahead of print].
- Bernhard B. High tech hand washing comes to St. Louis hospital. St. Louis Post-Dispatch website. Available at: http://www.stltoday.com/lifestyles/health-med-fit/health/high-tech-hand-washing-comes-to-st-louis-hospital/article_9379065d-85ff-5643-bae2-899254cb22fa.html. Accessed June 27, 2013.
- Lowe TJ, Partovian C, Kroch E, Martin J, Bankowitz R. Measuring cardiac waste: the Premier cardiac waste measures. Am J Med Qual. 2013 May 29 [Epub ahead of print].
- Elixhauser A, Steiner C. Readmissions to U.S. hospitals by diagnosis, 2010. Healthcare Cost and Utilization Project website. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb153.pdf. Accessed July 15, 2013.
- Jackson Healthcare. Filling the void: 2013 physician outlook & practice trends. Jackson Healthcare website. Available at: http://www.jacksonhealthcare.com/media/193525/jc-2013physiciantrends-void_ebk0513.pdf. Accessed July 15, 2013.
Percentage of practicing physicians who would not recommend a medical career to a young person, according to Filling The Void: 2013 Physician Outlook Practice Trends, a national physician practice survey conducted by health-care staffing firm Jackson Healthcare.6 “Physician discontent appears to be creating a void in the health-care field,” with dissatisfaction and burnout leading to early retirement, the report stated. Discontent is driven by decreased autonomy, decreased reimbursement, administrative and regulatory distractions, corporatization of medicine, and fear of litigation, according to the report. Thirty-six percent of the respondents reported a generally negative outlook about their career, compared with only 16% who had a generally favorable outlook.
Larry Beresford is a freelance writer in San Francisco.
References
- Hartocollis A. With money at risk, hospitals push staff to wash hands. The New York Times website. Available at: http://www.nytimes.com/2013/05/29/nyregion/hospitals-struggle-to-get-workers-to-wash-their-hands.html?pagewanted=all&_r=0. Accessed May 28, 2013.
- Cumbler E, Castillo L, Satorie L, et al. Culture change in infection control: applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013 May 10 [Epub ahead of print].
- Bernhard B. High tech hand washing comes to St. Louis hospital. St. Louis Post-Dispatch website. Available at: http://www.stltoday.com/lifestyles/health-med-fit/health/high-tech-hand-washing-comes-to-st-louis-hospital/article_9379065d-85ff-5643-bae2-899254cb22fa.html. Accessed June 27, 2013.
- Lowe TJ, Partovian C, Kroch E, Martin J, Bankowitz R. Measuring cardiac waste: the Premier cardiac waste measures. Am J Med Qual. 2013 May 29 [Epub ahead of print].
- Elixhauser A, Steiner C. Readmissions to U.S. hospitals by diagnosis, 2010. Healthcare Cost and Utilization Project website. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb153.pdf. Accessed July 15, 2013.
- Jackson Healthcare. Filling the void: 2013 physician outlook & practice trends. Jackson Healthcare website. Available at: http://www.jacksonhealthcare.com/media/193525/jc-2013physiciantrends-void_ebk0513.pdf. Accessed July 15, 2013.
Percentage of practicing physicians who would not recommend a medical career to a young person, according to Filling The Void: 2013 Physician Outlook Practice Trends, a national physician practice survey conducted by health-care staffing firm Jackson Healthcare.6 “Physician discontent appears to be creating a void in the health-care field,” with dissatisfaction and burnout leading to early retirement, the report stated. Discontent is driven by decreased autonomy, decreased reimbursement, administrative and regulatory distractions, corporatization of medicine, and fear of litigation, according to the report. Thirty-six percent of the respondents reported a generally negative outlook about their career, compared with only 16% who had a generally favorable outlook.
Larry Beresford is a freelance writer in San Francisco.
References
- Hartocollis A. With money at risk, hospitals push staff to wash hands. The New York Times website. Available at: http://www.nytimes.com/2013/05/29/nyregion/hospitals-struggle-to-get-workers-to-wash-their-hands.html?pagewanted=all&_r=0. Accessed May 28, 2013.
- Cumbler E, Castillo L, Satorie L, et al. Culture change in infection control: applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013 May 10 [Epub ahead of print].
- Bernhard B. High tech hand washing comes to St. Louis hospital. St. Louis Post-Dispatch website. Available at: http://www.stltoday.com/lifestyles/health-med-fit/health/high-tech-hand-washing-comes-to-st-louis-hospital/article_9379065d-85ff-5643-bae2-899254cb22fa.html. Accessed June 27, 2013.
- Lowe TJ, Partovian C, Kroch E, Martin J, Bankowitz R. Measuring cardiac waste: the Premier cardiac waste measures. Am J Med Qual. 2013 May 29 [Epub ahead of print].
- Elixhauser A, Steiner C. Readmissions to U.S. hospitals by diagnosis, 2010. Healthcare Cost and Utilization Project website. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb153.pdf. Accessed July 15, 2013.
- Jackson Healthcare. Filling the void: 2013 physician outlook & practice trends. Jackson Healthcare website. Available at: http://www.jacksonhealthcare.com/media/193525/jc-2013physiciantrends-void_ebk0513.pdf. Accessed July 15, 2013.
Study Investigator Explains Why Copper Surfaces Can Help Prevent Infections
Click here to listen to more of our interview with Dr. Schmidt
Click here to listen to more of our interview with Dr. Schmidt
Click here to listen to more of our interview with Dr. Schmidt
MGMA Physician Compensation Survey Raises Questions About Performance Pay
Sorting out whether a hospitalist’s bonus and other compensation elements are in line with survey data often leads to confusion. The 2013 MGMA Physician Compensation and Production Survey report, based on 2012 data, shows median compensation of $240,352 for internal-medicine hospitalists (I’ll round it to $240,000 for the rest of this piece). So is your compensation in line with survey medians if your base pay is $230,000 and you have a performance bonus of up to $20,000?
The problem is that you can’t know in advance how much of the $20,000 performance bonus you will earn. And isn’t a bonus supposed to be on top of typical compensation? To be in line with the survey, shouldn’t your base pay equal the $240,000 median, with any available bonus dollars on top of that? (Base pay means all forms of compensation other than a performance bonus; it could be productivity-based compensation, pay connected to numbers of shifts or hours worked, or a fixed annual salary, etc.)
The short answer is no, and to demonstrate why, I’ll first review some facts about the survey itself, then apply that knowledge to the hospitalist marketplace.
I want to emphasize that in this article, I’m not taking a position on the right amount of workload, compensation, or bonus for any hospitalist practice. And I’m using survey medians just to simplify the discussion, not because they’re optimal for any particular practice.
Survey Data
The most important thing to know about the survey data is that the $240,000 figure takes into account all forms of pay, including extra shift pay and any bonuses that might have been paid to each provider in the data set. Such benefits as health insurance and retirement-plan contribution are not included in this figure.
There are several ways a hospitalist might have earned compensation that matches the survey median. He or she might have a fixed annual salary equal to the median with no bonus available or had a meaningful bonus (e.g. $10,000 to $20,000) available and failed to earn any of it. Or the base might have come to $230,000, and he or she earned half of the available $20,000 performance bonus. Many other permutations of bonus and other salary elements could occur to arrive at the same $240,000 figure.
The important thing to remember is that whatever bonus dollars were paid, they are included in the salary figure from the survey—not added on top of that figure. So if all bonus dollars earned were subtracted from the survey, the total “nonbonus” compensation would be lower than $240,000.
How much lower?
Typical Hospitalist Bonus Amounts
The MGMA survey doesn’t report the portion of compensation tied to a bonus, but SHM’s does. SHM’s 2012 State of Hospital Medicine Report, based on 2011 data (www.hospitalmedicine.org/survey), is based on the most recent data available, and it showed (on page 60) that an average of 7% of pay was tied to performance for nonacademic hospitalist groups serving adults only. This included any payments for good individual or group performance on quality, efficiency, service, satisfaction, and/or other nonproduction measures. In conversation, this often is referred to as a “bonus” rather than “performance compensation.”
One way to estimate the nonbonus compensation would be to reduce the total pay by 7%, which comes to $223,200. Keep in mind that there are all kinds of mathematical and methodological problems in manipulating the reported survey numbers from two separate surveys to derive additional benchmarks. But this seems like a reasonable guess.
An increasing portion of hospitalist groups have some pay tied to performance, and the portion of total pay tied to performance seems to be going up at least a little. It was 5% of pay in 2010 and 4% in 2011, compared with 7% in the 2012 survey.
Keep in mind two things. First, this 7% reflects the performance or bonus dollars actually paid out, not the total amount available. In other words, even if the median total bonus dollars available were 20% of compensation, hospitalists earned less than that. Some hospitalists earned all dollars available, and some earned only a portion of what was available. And second, some hospitalists fail to earn any bonus or don’t have one available at all. So the survey would show for them zero compensation tied to bonus.
Making Sense of the Numbers
If you follow the reasoning above, then you probably agree that if your goal is to match mean compensation from the MGMA survey (I’m not suggesting that is the best goal, merely using it for simplicity), then you would set nonbonus compensation 7% below median—as long as you’re likely to get the same portion of a bonus as the median practice.
In some practices, performance thresholds are set at a level that is very easy to achieve, meaning the hospitalists are almost guaranteed to get all of the bonus compensation available. To be consistent with survey medians, it would be appropriate for them to set nonbonus compensation by subtracting all bonus dollars from the survey median. For example, if a $20,000 bonus is available and all of it is likely to be earned by the hospitalists, then total nonbonus compensation would be $220,000.
However, what if the bonus requires significant improvements in performance by the doctors (which seems most appropriate to me; why have a bonus otherwise?) and it is likely they will earn only 25% of all bonus dollars available? If the total available bonus is $20,000, then something like 25%, or $5,000, should be subtracted from the median to yield a total nonbonus compensation of $235,000.
Simple Thinking
I think it makes most sense to set total nonbonus compensation below the targeted total compensation. Failure to achieve any performance thresholds means no bonus and compensation will be below target that year. Meeting some thresholds (some improvement in performance) should result in matching the target compensation, and truly terrific performance that meets or exceeds all thresholds should result in the doctor being paid above the target.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Sorting out whether a hospitalist’s bonus and other compensation elements are in line with survey data often leads to confusion. The 2013 MGMA Physician Compensation and Production Survey report, based on 2012 data, shows median compensation of $240,352 for internal-medicine hospitalists (I’ll round it to $240,000 for the rest of this piece). So is your compensation in line with survey medians if your base pay is $230,000 and you have a performance bonus of up to $20,000?
The problem is that you can’t know in advance how much of the $20,000 performance bonus you will earn. And isn’t a bonus supposed to be on top of typical compensation? To be in line with the survey, shouldn’t your base pay equal the $240,000 median, with any available bonus dollars on top of that? (Base pay means all forms of compensation other than a performance bonus; it could be productivity-based compensation, pay connected to numbers of shifts or hours worked, or a fixed annual salary, etc.)
The short answer is no, and to demonstrate why, I’ll first review some facts about the survey itself, then apply that knowledge to the hospitalist marketplace.
I want to emphasize that in this article, I’m not taking a position on the right amount of workload, compensation, or bonus for any hospitalist practice. And I’m using survey medians just to simplify the discussion, not because they’re optimal for any particular practice.
Survey Data
The most important thing to know about the survey data is that the $240,000 figure takes into account all forms of pay, including extra shift pay and any bonuses that might have been paid to each provider in the data set. Such benefits as health insurance and retirement-plan contribution are not included in this figure.
There are several ways a hospitalist might have earned compensation that matches the survey median. He or she might have a fixed annual salary equal to the median with no bonus available or had a meaningful bonus (e.g. $10,000 to $20,000) available and failed to earn any of it. Or the base might have come to $230,000, and he or she earned half of the available $20,000 performance bonus. Many other permutations of bonus and other salary elements could occur to arrive at the same $240,000 figure.
The important thing to remember is that whatever bonus dollars were paid, they are included in the salary figure from the survey—not added on top of that figure. So if all bonus dollars earned were subtracted from the survey, the total “nonbonus” compensation would be lower than $240,000.
How much lower?
Typical Hospitalist Bonus Amounts
The MGMA survey doesn’t report the portion of compensation tied to a bonus, but SHM’s does. SHM’s 2012 State of Hospital Medicine Report, based on 2011 data (www.hospitalmedicine.org/survey), is based on the most recent data available, and it showed (on page 60) that an average of 7% of pay was tied to performance for nonacademic hospitalist groups serving adults only. This included any payments for good individual or group performance on quality, efficiency, service, satisfaction, and/or other nonproduction measures. In conversation, this often is referred to as a “bonus” rather than “performance compensation.”
One way to estimate the nonbonus compensation would be to reduce the total pay by 7%, which comes to $223,200. Keep in mind that there are all kinds of mathematical and methodological problems in manipulating the reported survey numbers from two separate surveys to derive additional benchmarks. But this seems like a reasonable guess.
An increasing portion of hospitalist groups have some pay tied to performance, and the portion of total pay tied to performance seems to be going up at least a little. It was 5% of pay in 2010 and 4% in 2011, compared with 7% in the 2012 survey.
Keep in mind two things. First, this 7% reflects the performance or bonus dollars actually paid out, not the total amount available. In other words, even if the median total bonus dollars available were 20% of compensation, hospitalists earned less than that. Some hospitalists earned all dollars available, and some earned only a portion of what was available. And second, some hospitalists fail to earn any bonus or don’t have one available at all. So the survey would show for them zero compensation tied to bonus.
Making Sense of the Numbers
If you follow the reasoning above, then you probably agree that if your goal is to match mean compensation from the MGMA survey (I’m not suggesting that is the best goal, merely using it for simplicity), then you would set nonbonus compensation 7% below median—as long as you’re likely to get the same portion of a bonus as the median practice.
In some practices, performance thresholds are set at a level that is very easy to achieve, meaning the hospitalists are almost guaranteed to get all of the bonus compensation available. To be consistent with survey medians, it would be appropriate for them to set nonbonus compensation by subtracting all bonus dollars from the survey median. For example, if a $20,000 bonus is available and all of it is likely to be earned by the hospitalists, then total nonbonus compensation would be $220,000.
However, what if the bonus requires significant improvements in performance by the doctors (which seems most appropriate to me; why have a bonus otherwise?) and it is likely they will earn only 25% of all bonus dollars available? If the total available bonus is $20,000, then something like 25%, or $5,000, should be subtracted from the median to yield a total nonbonus compensation of $235,000.
Simple Thinking
I think it makes most sense to set total nonbonus compensation below the targeted total compensation. Failure to achieve any performance thresholds means no bonus and compensation will be below target that year. Meeting some thresholds (some improvement in performance) should result in matching the target compensation, and truly terrific performance that meets or exceeds all thresholds should result in the doctor being paid above the target.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Sorting out whether a hospitalist’s bonus and other compensation elements are in line with survey data often leads to confusion. The 2013 MGMA Physician Compensation and Production Survey report, based on 2012 data, shows median compensation of $240,352 for internal-medicine hospitalists (I’ll round it to $240,000 for the rest of this piece). So is your compensation in line with survey medians if your base pay is $230,000 and you have a performance bonus of up to $20,000?
The problem is that you can’t know in advance how much of the $20,000 performance bonus you will earn. And isn’t a bonus supposed to be on top of typical compensation? To be in line with the survey, shouldn’t your base pay equal the $240,000 median, with any available bonus dollars on top of that? (Base pay means all forms of compensation other than a performance bonus; it could be productivity-based compensation, pay connected to numbers of shifts or hours worked, or a fixed annual salary, etc.)
The short answer is no, and to demonstrate why, I’ll first review some facts about the survey itself, then apply that knowledge to the hospitalist marketplace.
I want to emphasize that in this article, I’m not taking a position on the right amount of workload, compensation, or bonus for any hospitalist practice. And I’m using survey medians just to simplify the discussion, not because they’re optimal for any particular practice.
Survey Data
The most important thing to know about the survey data is that the $240,000 figure takes into account all forms of pay, including extra shift pay and any bonuses that might have been paid to each provider in the data set. Such benefits as health insurance and retirement-plan contribution are not included in this figure.
There are several ways a hospitalist might have earned compensation that matches the survey median. He or she might have a fixed annual salary equal to the median with no bonus available or had a meaningful bonus (e.g. $10,000 to $20,000) available and failed to earn any of it. Or the base might have come to $230,000, and he or she earned half of the available $20,000 performance bonus. Many other permutations of bonus and other salary elements could occur to arrive at the same $240,000 figure.
The important thing to remember is that whatever bonus dollars were paid, they are included in the salary figure from the survey—not added on top of that figure. So if all bonus dollars earned were subtracted from the survey, the total “nonbonus” compensation would be lower than $240,000.
How much lower?
Typical Hospitalist Bonus Amounts
The MGMA survey doesn’t report the portion of compensation tied to a bonus, but SHM’s does. SHM’s 2012 State of Hospital Medicine Report, based on 2011 data (www.hospitalmedicine.org/survey), is based on the most recent data available, and it showed (on page 60) that an average of 7% of pay was tied to performance for nonacademic hospitalist groups serving adults only. This included any payments for good individual or group performance on quality, efficiency, service, satisfaction, and/or other nonproduction measures. In conversation, this often is referred to as a “bonus” rather than “performance compensation.”
One way to estimate the nonbonus compensation would be to reduce the total pay by 7%, which comes to $223,200. Keep in mind that there are all kinds of mathematical and methodological problems in manipulating the reported survey numbers from two separate surveys to derive additional benchmarks. But this seems like a reasonable guess.
An increasing portion of hospitalist groups have some pay tied to performance, and the portion of total pay tied to performance seems to be going up at least a little. It was 5% of pay in 2010 and 4% in 2011, compared with 7% in the 2012 survey.
Keep in mind two things. First, this 7% reflects the performance or bonus dollars actually paid out, not the total amount available. In other words, even if the median total bonus dollars available were 20% of compensation, hospitalists earned less than that. Some hospitalists earned all dollars available, and some earned only a portion of what was available. And second, some hospitalists fail to earn any bonus or don’t have one available at all. So the survey would show for them zero compensation tied to bonus.
Making Sense of the Numbers
If you follow the reasoning above, then you probably agree that if your goal is to match mean compensation from the MGMA survey (I’m not suggesting that is the best goal, merely using it for simplicity), then you would set nonbonus compensation 7% below median—as long as you’re likely to get the same portion of a bonus as the median practice.
In some practices, performance thresholds are set at a level that is very easy to achieve, meaning the hospitalists are almost guaranteed to get all of the bonus compensation available. To be consistent with survey medians, it would be appropriate for them to set nonbonus compensation by subtracting all bonus dollars from the survey median. For example, if a $20,000 bonus is available and all of it is likely to be earned by the hospitalists, then total nonbonus compensation would be $220,000.
However, what if the bonus requires significant improvements in performance by the doctors (which seems most appropriate to me; why have a bonus otherwise?) and it is likely they will earn only 25% of all bonus dollars available? If the total available bonus is $20,000, then something like 25%, or $5,000, should be subtracted from the median to yield a total nonbonus compensation of $235,000.
Simple Thinking
I think it makes most sense to set total nonbonus compensation below the targeted total compensation. Failure to achieve any performance thresholds means no bonus and compensation will be below target that year. Meeting some thresholds (some improvement in performance) should result in matching the target compensation, and truly terrific performance that meets or exceeds all thresholds should result in the doctor being paid above the target.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Patient Satisfaction Surveys Not Accurate Measure of Hospitalists’ Performance
Feeling frustrated with your group’s patient-satisfaction performance? Wondering why your chief (fill in the blank) officer glazes over when you try to explain why your hospitalist group’s Hospital Consumer Assessment of Healthcare Providers and System (HCAHPS) scores for doctor communication are in a percentile rivaling the numeric age of your children?
It is likely that the C-suite administrator overseeing your hospitalist group has a portion of their pay based on HCAHPS or other patient-satisfaction (also called patient experience) scores. And for good reason: The Centers for Medicare & Medicaid Services (CMS) Hospital Value-Based Purchasing (HVBP) program that started Oct. 1, 2012, has placed your hospital’s Medicare reimbursement at risk based on its HCAHPS scores.
HVBP and Patient Satisfaction
Patient satisfaction will remain an important part of HVBP in the coming years. Table 1 (below) shows the domains that will be included in fiscal years 2014 (which starts Oct. 1, 2013), 2015, and 2016. Table 2 (below) depicts the percent weighting the patient-satisfaction domain will receive through 2016. You may recall that HVBP is a program in which all hospitals place 1% to 2% (2013 through 2017, starting at 1% and increasing each year by 0.25% so that by 2017%, it is 2%) of their CMS inpatient payments in a withhold pool and, based on performance, can make back some, all, or an amount in excess of the amount placed in the withhold pool.
Source: Federal Register Vol. 78, No. 91; May 10, 2013; Proposed Rules, pp. 27609-27622.
Source: Federal Register Vol.78, No.91; May 10, 2013; Proposed Rules, pp. 27609-27622.
End In Itself
A colleague of mine recently asked, “Is an increase in patient satisfaction associated with higher quality of care and better patient safety?” The point here: It doesn’t matter. Patient satisfaction is an end in itself, and we should strive to maximize it, or at least put ourselves in the place of the patient and design care accordingly.
For Hospitalists: A Starting Point
There is a conundrum for hospitalists vis-à-vis patient satisfaction. Follow this chain of logic: The hospitals at which we work are incented to perform well on the HCAHPS domains. Hospitals pay a lot for hospitalists. Hospitalists can impact many of the HCAHPS domains. So shouldn’t hospitalists be judged according to HCAHPS scores?
Yes and no.
HCAHPS as a survey is intended to measure a patient’s overall experience of receiving care in the hospital. For example, from the “Doctor Communication” domain, we have questions like “how often did doctors treat you with courtesy and respect?” And “how often did doctors explain things in a way you could understand?”
These questions, like all in HCAHPS, are not designed to get at individual doctor performance, or even performance of a group of doctors, such as hospitalists. Instead, they are designed to measure a patient’s overall experience with the hospitalization, and “Doctor Communication” questions are designed to assess satisfaction with “doctors” collectively.
The Need for Hospitalist-Specific Satisfaction Surveys
So while HCAHPS is not designed to measure hospitalist performance with regard to patient satisfaction, it is a reasonable interim step for hospitals to judge hospitalists according to HCAHPS. However, this should be a bridge to a strategy that adopts hospitalist-specific patient-satisfaction questionnaires in the future and not an end in itself.
Why? Perhaps the biggest reason is that HCAHPS scores are neither specific nor timely enough to form the basis of improvement efforts for hospitalists. If a hospitalist receives a low score on the “Doctor Communication” domain, the scores are likely to be three to nine months old. How can we legitimately assign (and then modify) behaviors based on those scores?
Further, because the survey is not built to measure patient satisfaction specifically with hospitalists, the results are unlikely to engender meaningful and sustained behavior change. Hospitalists I talk to are generally bewildered and confused by HCAHPS scores attributed to them or their groups. Even if they understand the scores, I almost never see true quality improvement (plan-do-study-act) based on specific HCAHPS results. Instead, I see hospitalists trying to adhere to “best practices,” with no adjustments made along the way based on performance.
Nearly all the prominent patient satisfaction vendors have developed a survey instrument specifically designed for hospitalists. Each has an approach to appropriately attribute performance to the hospitalist in question, and each has a battery of questions that is designed to capture patient satisfaction with the hospitalist. Although use of these surveys involves an added financial commitment, I submit that because hospitalists have an unparalleled proximity to hospitalized patients, such an investment is worthy of consideration and has an accompanying business case, thanks to HVBP. The results of these surveys may form the basis of legitimate, targeted feedback to hospitalists, who may then adjust their approach to patient interactions. Such performance improvement should result in improved HCAHPS scores.
In sum, hospitalists should pay close attention to patient satisfaction and embrace HCAHPS. However, we should be looking beyond HCAHPS to survey instruments that fairly and accurately measure our performance. Such surveys will be more widely accepted by the hospitalists they are measuring, and will allow hospitalists to perform meaningful quality improvement based on the results. Although hospitalist-specific surveys will require an investment, the increased patient satisfaction that results should be the basis of a favorable return on that investment.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at wfwhit@comcast.net.
Feeling frustrated with your group’s patient-satisfaction performance? Wondering why your chief (fill in the blank) officer glazes over when you try to explain why your hospitalist group’s Hospital Consumer Assessment of Healthcare Providers and System (HCAHPS) scores for doctor communication are in a percentile rivaling the numeric age of your children?
It is likely that the C-suite administrator overseeing your hospitalist group has a portion of their pay based on HCAHPS or other patient-satisfaction (also called patient experience) scores. And for good reason: The Centers for Medicare & Medicaid Services (CMS) Hospital Value-Based Purchasing (HVBP) program that started Oct. 1, 2012, has placed your hospital’s Medicare reimbursement at risk based on its HCAHPS scores.
HVBP and Patient Satisfaction
Patient satisfaction will remain an important part of HVBP in the coming years. Table 1 (below) shows the domains that will be included in fiscal years 2014 (which starts Oct. 1, 2013), 2015, and 2016. Table 2 (below) depicts the percent weighting the patient-satisfaction domain will receive through 2016. You may recall that HVBP is a program in which all hospitals place 1% to 2% (2013 through 2017, starting at 1% and increasing each year by 0.25% so that by 2017%, it is 2%) of their CMS inpatient payments in a withhold pool and, based on performance, can make back some, all, or an amount in excess of the amount placed in the withhold pool.
Source: Federal Register Vol. 78, No. 91; May 10, 2013; Proposed Rules, pp. 27609-27622.
Source: Federal Register Vol.78, No.91; May 10, 2013; Proposed Rules, pp. 27609-27622.
End In Itself
A colleague of mine recently asked, “Is an increase in patient satisfaction associated with higher quality of care and better patient safety?” The point here: It doesn’t matter. Patient satisfaction is an end in itself, and we should strive to maximize it, or at least put ourselves in the place of the patient and design care accordingly.
For Hospitalists: A Starting Point
There is a conundrum for hospitalists vis-à-vis patient satisfaction. Follow this chain of logic: The hospitals at which we work are incented to perform well on the HCAHPS domains. Hospitals pay a lot for hospitalists. Hospitalists can impact many of the HCAHPS domains. So shouldn’t hospitalists be judged according to HCAHPS scores?
Yes and no.
HCAHPS as a survey is intended to measure a patient’s overall experience of receiving care in the hospital. For example, from the “Doctor Communication” domain, we have questions like “how often did doctors treat you with courtesy and respect?” And “how often did doctors explain things in a way you could understand?”
These questions, like all in HCAHPS, are not designed to get at individual doctor performance, or even performance of a group of doctors, such as hospitalists. Instead, they are designed to measure a patient’s overall experience with the hospitalization, and “Doctor Communication” questions are designed to assess satisfaction with “doctors” collectively.
The Need for Hospitalist-Specific Satisfaction Surveys
So while HCAHPS is not designed to measure hospitalist performance with regard to patient satisfaction, it is a reasonable interim step for hospitals to judge hospitalists according to HCAHPS. However, this should be a bridge to a strategy that adopts hospitalist-specific patient-satisfaction questionnaires in the future and not an end in itself.
Why? Perhaps the biggest reason is that HCAHPS scores are neither specific nor timely enough to form the basis of improvement efforts for hospitalists. If a hospitalist receives a low score on the “Doctor Communication” domain, the scores are likely to be three to nine months old. How can we legitimately assign (and then modify) behaviors based on those scores?
Further, because the survey is not built to measure patient satisfaction specifically with hospitalists, the results are unlikely to engender meaningful and sustained behavior change. Hospitalists I talk to are generally bewildered and confused by HCAHPS scores attributed to them or their groups. Even if they understand the scores, I almost never see true quality improvement (plan-do-study-act) based on specific HCAHPS results. Instead, I see hospitalists trying to adhere to “best practices,” with no adjustments made along the way based on performance.
Nearly all the prominent patient satisfaction vendors have developed a survey instrument specifically designed for hospitalists. Each has an approach to appropriately attribute performance to the hospitalist in question, and each has a battery of questions that is designed to capture patient satisfaction with the hospitalist. Although use of these surveys involves an added financial commitment, I submit that because hospitalists have an unparalleled proximity to hospitalized patients, such an investment is worthy of consideration and has an accompanying business case, thanks to HVBP. The results of these surveys may form the basis of legitimate, targeted feedback to hospitalists, who may then adjust their approach to patient interactions. Such performance improvement should result in improved HCAHPS scores.
In sum, hospitalists should pay close attention to patient satisfaction and embrace HCAHPS. However, we should be looking beyond HCAHPS to survey instruments that fairly and accurately measure our performance. Such surveys will be more widely accepted by the hospitalists they are measuring, and will allow hospitalists to perform meaningful quality improvement based on the results. Although hospitalist-specific surveys will require an investment, the increased patient satisfaction that results should be the basis of a favorable return on that investment.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at wfwhit@comcast.net.
Feeling frustrated with your group’s patient-satisfaction performance? Wondering why your chief (fill in the blank) officer glazes over when you try to explain why your hospitalist group’s Hospital Consumer Assessment of Healthcare Providers and System (HCAHPS) scores for doctor communication are in a percentile rivaling the numeric age of your children?
It is likely that the C-suite administrator overseeing your hospitalist group has a portion of their pay based on HCAHPS or other patient-satisfaction (also called patient experience) scores. And for good reason: The Centers for Medicare & Medicaid Services (CMS) Hospital Value-Based Purchasing (HVBP) program that started Oct. 1, 2012, has placed your hospital’s Medicare reimbursement at risk based on its HCAHPS scores.
HVBP and Patient Satisfaction
Patient satisfaction will remain an important part of HVBP in the coming years. Table 1 (below) shows the domains that will be included in fiscal years 2014 (which starts Oct. 1, 2013), 2015, and 2016. Table 2 (below) depicts the percent weighting the patient-satisfaction domain will receive through 2016. You may recall that HVBP is a program in which all hospitals place 1% to 2% (2013 through 2017, starting at 1% and increasing each year by 0.25% so that by 2017%, it is 2%) of their CMS inpatient payments in a withhold pool and, based on performance, can make back some, all, or an amount in excess of the amount placed in the withhold pool.
Source: Federal Register Vol. 78, No. 91; May 10, 2013; Proposed Rules, pp. 27609-27622.
Source: Federal Register Vol.78, No.91; May 10, 2013; Proposed Rules, pp. 27609-27622.
End In Itself
A colleague of mine recently asked, “Is an increase in patient satisfaction associated with higher quality of care and better patient safety?” The point here: It doesn’t matter. Patient satisfaction is an end in itself, and we should strive to maximize it, or at least put ourselves in the place of the patient and design care accordingly.
For Hospitalists: A Starting Point
There is a conundrum for hospitalists vis-à-vis patient satisfaction. Follow this chain of logic: The hospitals at which we work are incented to perform well on the HCAHPS domains. Hospitals pay a lot for hospitalists. Hospitalists can impact many of the HCAHPS domains. So shouldn’t hospitalists be judged according to HCAHPS scores?
Yes and no.
HCAHPS as a survey is intended to measure a patient’s overall experience of receiving care in the hospital. For example, from the “Doctor Communication” domain, we have questions like “how often did doctors treat you with courtesy and respect?” And “how often did doctors explain things in a way you could understand?”
These questions, like all in HCAHPS, are not designed to get at individual doctor performance, or even performance of a group of doctors, such as hospitalists. Instead, they are designed to measure a patient’s overall experience with the hospitalization, and “Doctor Communication” questions are designed to assess satisfaction with “doctors” collectively.
The Need for Hospitalist-Specific Satisfaction Surveys
So while HCAHPS is not designed to measure hospitalist performance with regard to patient satisfaction, it is a reasonable interim step for hospitals to judge hospitalists according to HCAHPS. However, this should be a bridge to a strategy that adopts hospitalist-specific patient-satisfaction questionnaires in the future and not an end in itself.
Why? Perhaps the biggest reason is that HCAHPS scores are neither specific nor timely enough to form the basis of improvement efforts for hospitalists. If a hospitalist receives a low score on the “Doctor Communication” domain, the scores are likely to be three to nine months old. How can we legitimately assign (and then modify) behaviors based on those scores?
Further, because the survey is not built to measure patient satisfaction specifically with hospitalists, the results are unlikely to engender meaningful and sustained behavior change. Hospitalists I talk to are generally bewildered and confused by HCAHPS scores attributed to them or their groups. Even if they understand the scores, I almost never see true quality improvement (plan-do-study-act) based on specific HCAHPS results. Instead, I see hospitalists trying to adhere to “best practices,” with no adjustments made along the way based on performance.
Nearly all the prominent patient satisfaction vendors have developed a survey instrument specifically designed for hospitalists. Each has an approach to appropriately attribute performance to the hospitalist in question, and each has a battery of questions that is designed to capture patient satisfaction with the hospitalist. Although use of these surveys involves an added financial commitment, I submit that because hospitalists have an unparalleled proximity to hospitalized patients, such an investment is worthy of consideration and has an accompanying business case, thanks to HVBP. The results of these surveys may form the basis of legitimate, targeted feedback to hospitalists, who may then adjust their approach to patient interactions. Such performance improvement should result in improved HCAHPS scores.
In sum, hospitalists should pay close attention to patient satisfaction and embrace HCAHPS. However, we should be looking beyond HCAHPS to survey instruments that fairly and accurately measure our performance. Such surveys will be more widely accepted by the hospitalists they are measuring, and will allow hospitalists to perform meaningful quality improvement based on the results. Although hospitalist-specific surveys will require an investment, the increased patient satisfaction that results should be the basis of a favorable return on that investment.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at wfwhit@comcast.net.