User login
Is It Time to Air Grievances?
‘Twas the night before Festivus and all through the house, everyone was griping.
In case you’ve only been watching Friends reruns lately, Festivus is a holiday that originated 25 years ago in the last season of Seinfeld. George’s father created it as an alternative to Christmas hype. In addition to an aluminum pole, the holiday features the annual airing of grievances, when one is encouraged to voice complaints. Aluminum poles haven’t replaced Christmas trees, but the spirit of Festivus is still with us in the widespread airing of grievances in 2023.
Complaining isn’t just a post-pandemic problem. Hector spends quite a bit of time complaining about Paris in the Iliad. That was a few pandemics ago. And repining is ubiquitous in literature — as human as walking on two limbs it seems. Ostensibly, we complain to effect change: Something is wrong and we expect it to be different. But that’s not the whole story. No one believes the weather will improve or the Patriots will play better because we complain about them. So why do we bother?
Even if nothing changes on the outside, it does seem to alter our internal state, serving a healthy psychological function. Putting to words what is aggravating can have the same benefit of deep breathing. We describe it as “getting something off our chest” because that’s what it feels like. We feel unburdened just by saying it out loud. Think about the last time you complained: Cranky staff, prior auths, Medicare, disrespectful patients, many of your colleagues will nod in agreement, validating your feelings and making you feel less isolated.
There are also maladaptive reasons for whining. It’s obviously an elementary way to get attention or to remove responsibility. It can also be a political weapon (office politics included). It’s such a potent way to connect that it’s used to build alliances and clout. “Washington is doing a great job,” said no candidate ever. No, if you want to get people on your side, find something irritating and complain to everyone how annoying it is. This solidifies “us” versus “them,” which can harm organizations and families alike.
Yet, eliminating all complaints is neither feasible, nor probably advisable. You could try to make your office a complaint-free zone, but the likely result would be to push any griping to the remote corners where you can no longer hear them. These criticisms might have uncovered missed opportunities, identify problems, and even improve cohesion if done in a safe and transparent setting. If they are left unaddressed or if the underlying culture isn’t sound, then they can propagate and lead to factions that harm productivity.
Griping is as much part of the holiday season as jingle bells and jelly donuts. I don’t believe complaining is up now because people were grumpier in 2023. Rather I think people just craved connection more than ever. So join in: Traffic after the time change, Tesla service, (super) late patients, prior auths, perioral dermatitis, post-COVID telogen effluvium.
I feel better.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X (formerly Twitter). Write to him at dermnews@mdedge.com.
‘Twas the night before Festivus and all through the house, everyone was griping.
In case you’ve only been watching Friends reruns lately, Festivus is a holiday that originated 25 years ago in the last season of Seinfeld. George’s father created it as an alternative to Christmas hype. In addition to an aluminum pole, the holiday features the annual airing of grievances, when one is encouraged to voice complaints. Aluminum poles haven’t replaced Christmas trees, but the spirit of Festivus is still with us in the widespread airing of grievances in 2023.
Complaining isn’t just a post-pandemic problem. Hector spends quite a bit of time complaining about Paris in the Iliad. That was a few pandemics ago. And repining is ubiquitous in literature — as human as walking on two limbs it seems. Ostensibly, we complain to effect change: Something is wrong and we expect it to be different. But that’s not the whole story. No one believes the weather will improve or the Patriots will play better because we complain about them. So why do we bother?
Even if nothing changes on the outside, it does seem to alter our internal state, serving a healthy psychological function. Putting to words what is aggravating can have the same benefit of deep breathing. We describe it as “getting something off our chest” because that’s what it feels like. We feel unburdened just by saying it out loud. Think about the last time you complained: Cranky staff, prior auths, Medicare, disrespectful patients, many of your colleagues will nod in agreement, validating your feelings and making you feel less isolated.
There are also maladaptive reasons for whining. It’s obviously an elementary way to get attention or to remove responsibility. It can also be a political weapon (office politics included). It’s such a potent way to connect that it’s used to build alliances and clout. “Washington is doing a great job,” said no candidate ever. No, if you want to get people on your side, find something irritating and complain to everyone how annoying it is. This solidifies “us” versus “them,” which can harm organizations and families alike.
Yet, eliminating all complaints is neither feasible, nor probably advisable. You could try to make your office a complaint-free zone, but the likely result would be to push any griping to the remote corners where you can no longer hear them. These criticisms might have uncovered missed opportunities, identify problems, and even improve cohesion if done in a safe and transparent setting. If they are left unaddressed or if the underlying culture isn’t sound, then they can propagate and lead to factions that harm productivity.
Griping is as much part of the holiday season as jingle bells and jelly donuts. I don’t believe complaining is up now because people were grumpier in 2023. Rather I think people just craved connection more than ever. So join in: Traffic after the time change, Tesla service, (super) late patients, prior auths, perioral dermatitis, post-COVID telogen effluvium.
I feel better.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X (formerly Twitter). Write to him at dermnews@mdedge.com.
‘Twas the night before Festivus and all through the house, everyone was griping.
In case you’ve only been watching Friends reruns lately, Festivus is a holiday that originated 25 years ago in the last season of Seinfeld. George’s father created it as an alternative to Christmas hype. In addition to an aluminum pole, the holiday features the annual airing of grievances, when one is encouraged to voice complaints. Aluminum poles haven’t replaced Christmas trees, but the spirit of Festivus is still with us in the widespread airing of grievances in 2023.
Complaining isn’t just a post-pandemic problem. Hector spends quite a bit of time complaining about Paris in the Iliad. That was a few pandemics ago. And repining is ubiquitous in literature — as human as walking on two limbs it seems. Ostensibly, we complain to effect change: Something is wrong and we expect it to be different. But that’s not the whole story. No one believes the weather will improve or the Patriots will play better because we complain about them. So why do we bother?
Even if nothing changes on the outside, it does seem to alter our internal state, serving a healthy psychological function. Putting to words what is aggravating can have the same benefit of deep breathing. We describe it as “getting something off our chest” because that’s what it feels like. We feel unburdened just by saying it out loud. Think about the last time you complained: Cranky staff, prior auths, Medicare, disrespectful patients, many of your colleagues will nod in agreement, validating your feelings and making you feel less isolated.
There are also maladaptive reasons for whining. It’s obviously an elementary way to get attention or to remove responsibility. It can also be a political weapon (office politics included). It’s such a potent way to connect that it’s used to build alliances and clout. “Washington is doing a great job,” said no candidate ever. No, if you want to get people on your side, find something irritating and complain to everyone how annoying it is. This solidifies “us” versus “them,” which can harm organizations and families alike.
Yet, eliminating all complaints is neither feasible, nor probably advisable. You could try to make your office a complaint-free zone, but the likely result would be to push any griping to the remote corners where you can no longer hear them. These criticisms might have uncovered missed opportunities, identify problems, and even improve cohesion if done in a safe and transparent setting. If they are left unaddressed or if the underlying culture isn’t sound, then they can propagate and lead to factions that harm productivity.
Griping is as much part of the holiday season as jingle bells and jelly donuts. I don’t believe complaining is up now because people were grumpier in 2023. Rather I think people just craved connection more than ever. So join in: Traffic after the time change, Tesla service, (super) late patients, prior auths, perioral dermatitis, post-COVID telogen effluvium.
I feel better.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X (formerly Twitter). Write to him at dermnews@mdedge.com.
Life in the woods
“I went to the woods because I wished to live deliberately, to front only the essential facts of life, and see if I could not learn what it had to teach.” – Henry David Thoreau
I have many patients like Maxine. Tall, with a shock of white hair. Old, but still in charge. When you try to make eye contact, she looks right through you. First with her left eye. Then her right. Her face is inscrutable. What’s she thinking? Unlike many of my patients, however, this Maxine was a llama. Every morning my daughter and I tried to coax her into moving as we leaned on the cold steel gate that kept her in her pasture. We were visiting family in October and chose to stay on a working New England farm. The kids will love the animals, we thought, and we’ll appreciate the extra bedrooms.
Airbnb helped us find this charming fiber-farm in Rhode Island where they raise Leicester Longwool sheep, a historic breed that once roamed George Washington’s pastures, along with a few goats, ducks, chickens, and Maxine. It’s situated deep in the woods, which were yellow, orange, and red that week. As it happens, we were just a short drive due south of Walden Pond where Henry David Thoreau spent 2 years, 2 months and 2 days escaping “overcivilization” nearly 175 years ago. Hoisting our overweight bags over the uneven granite stone steps when we arrived, I realized this was going to be more like the Thoreau experiment than I intended. The farmhouse dated to the 1790s. There were wide, creaky floorboards, low ceilings, one staircase to the bedrooms (which could have aptly been called a ladder) and loads of book-laden shelves. Instructions posted in the kitchen warned that the heat is tricky to regulate – a redundant admonition as we watched our 3-year-old putting on her socks and shoes as she got into bed.
Now, if you’ve ever been on vacation with little kids, you know that it’s basically just childcare in a novel location. After barricading the staircase with luggage and unplugging lamps from their dicey outlets we set out to feed the chickens and try to pet a sheep. Walking the perimeter of the farm we saw stone walls that needed mending and stumbled across two ancient cemeteries, one had been for family, the other for slaves. I wondered how many farmers and weavers and menders had walked this trail with their kids over the generations.
The next morning, we learned that roosters do not in fact crow at dawn, they crow before dawn (which could also aptly be called nighttime). There were no commutes or late patients here. But there was work to be done. Chickens don’t care that it’s Sunday. It downpoured. Watching the sheep from the kitchen as I sipped my coffee, they didn’t seem to mind. Nor did our farmer hosts who trudged past them in tall boots, just as they had every other day of their farmer lives.
By the fifth day, we had fallen into the rhythms of the homestead. We cracked the blue, green, and brown eggs that our hosts placed outside our door in the early hours and made omelets that were as orange as the foliage. We finally learned to adjust the heat so we neither got chilblains nor had to open the windows and strip naked to cool down. The sky was a brilliant blue that last morning and Sloan ran around trying to catch leaves as they blew off the trees. She had no objective. No counting. No contest. Just chasing leaves as they fell. It was the ultimate atelic activity, done just for doing it. I joined her and found I was no better at this than a 3-year-old.
We might all benefit from a little time in the woods.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“I went to the woods because I wished to live deliberately, to front only the essential facts of life, and see if I could not learn what it had to teach.” – Henry David Thoreau
I have many patients like Maxine. Tall, with a shock of white hair. Old, but still in charge. When you try to make eye contact, she looks right through you. First with her left eye. Then her right. Her face is inscrutable. What’s she thinking? Unlike many of my patients, however, this Maxine was a llama. Every morning my daughter and I tried to coax her into moving as we leaned on the cold steel gate that kept her in her pasture. We were visiting family in October and chose to stay on a working New England farm. The kids will love the animals, we thought, and we’ll appreciate the extra bedrooms.
Airbnb helped us find this charming fiber-farm in Rhode Island where they raise Leicester Longwool sheep, a historic breed that once roamed George Washington’s pastures, along with a few goats, ducks, chickens, and Maxine. It’s situated deep in the woods, which were yellow, orange, and red that week. As it happens, we were just a short drive due south of Walden Pond where Henry David Thoreau spent 2 years, 2 months and 2 days escaping “overcivilization” nearly 175 years ago. Hoisting our overweight bags over the uneven granite stone steps when we arrived, I realized this was going to be more like the Thoreau experiment than I intended. The farmhouse dated to the 1790s. There were wide, creaky floorboards, low ceilings, one staircase to the bedrooms (which could have aptly been called a ladder) and loads of book-laden shelves. Instructions posted in the kitchen warned that the heat is tricky to regulate – a redundant admonition as we watched our 3-year-old putting on her socks and shoes as she got into bed.
Now, if you’ve ever been on vacation with little kids, you know that it’s basically just childcare in a novel location. After barricading the staircase with luggage and unplugging lamps from their dicey outlets we set out to feed the chickens and try to pet a sheep. Walking the perimeter of the farm we saw stone walls that needed mending and stumbled across two ancient cemeteries, one had been for family, the other for slaves. I wondered how many farmers and weavers and menders had walked this trail with their kids over the generations.
The next morning, we learned that roosters do not in fact crow at dawn, they crow before dawn (which could also aptly be called nighttime). There were no commutes or late patients here. But there was work to be done. Chickens don’t care that it’s Sunday. It downpoured. Watching the sheep from the kitchen as I sipped my coffee, they didn’t seem to mind. Nor did our farmer hosts who trudged past them in tall boots, just as they had every other day of their farmer lives.
By the fifth day, we had fallen into the rhythms of the homestead. We cracked the blue, green, and brown eggs that our hosts placed outside our door in the early hours and made omelets that were as orange as the foliage. We finally learned to adjust the heat so we neither got chilblains nor had to open the windows and strip naked to cool down. The sky was a brilliant blue that last morning and Sloan ran around trying to catch leaves as they blew off the trees. She had no objective. No counting. No contest. Just chasing leaves as they fell. It was the ultimate atelic activity, done just for doing it. I joined her and found I was no better at this than a 3-year-old.
We might all benefit from a little time in the woods.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“I went to the woods because I wished to live deliberately, to front only the essential facts of life, and see if I could not learn what it had to teach.” – Henry David Thoreau
I have many patients like Maxine. Tall, with a shock of white hair. Old, but still in charge. When you try to make eye contact, she looks right through you. First with her left eye. Then her right. Her face is inscrutable. What’s she thinking? Unlike many of my patients, however, this Maxine was a llama. Every morning my daughter and I tried to coax her into moving as we leaned on the cold steel gate that kept her in her pasture. We were visiting family in October and chose to stay on a working New England farm. The kids will love the animals, we thought, and we’ll appreciate the extra bedrooms.
Airbnb helped us find this charming fiber-farm in Rhode Island where they raise Leicester Longwool sheep, a historic breed that once roamed George Washington’s pastures, along with a few goats, ducks, chickens, and Maxine. It’s situated deep in the woods, which were yellow, orange, and red that week. As it happens, we were just a short drive due south of Walden Pond where Henry David Thoreau spent 2 years, 2 months and 2 days escaping “overcivilization” nearly 175 years ago. Hoisting our overweight bags over the uneven granite stone steps when we arrived, I realized this was going to be more like the Thoreau experiment than I intended. The farmhouse dated to the 1790s. There were wide, creaky floorboards, low ceilings, one staircase to the bedrooms (which could have aptly been called a ladder) and loads of book-laden shelves. Instructions posted in the kitchen warned that the heat is tricky to regulate – a redundant admonition as we watched our 3-year-old putting on her socks and shoes as she got into bed.
Now, if you’ve ever been on vacation with little kids, you know that it’s basically just childcare in a novel location. After barricading the staircase with luggage and unplugging lamps from their dicey outlets we set out to feed the chickens and try to pet a sheep. Walking the perimeter of the farm we saw stone walls that needed mending and stumbled across two ancient cemeteries, one had been for family, the other for slaves. I wondered how many farmers and weavers and menders had walked this trail with their kids over the generations.
The next morning, we learned that roosters do not in fact crow at dawn, they crow before dawn (which could also aptly be called nighttime). There were no commutes or late patients here. But there was work to be done. Chickens don’t care that it’s Sunday. It downpoured. Watching the sheep from the kitchen as I sipped my coffee, they didn’t seem to mind. Nor did our farmer hosts who trudged past them in tall boots, just as they had every other day of their farmer lives.
By the fifth day, we had fallen into the rhythms of the homestead. We cracked the blue, green, and brown eggs that our hosts placed outside our door in the early hours and made omelets that were as orange as the foliage. We finally learned to adjust the heat so we neither got chilblains nor had to open the windows and strip naked to cool down. The sky was a brilliant blue that last morning and Sloan ran around trying to catch leaves as they blew off the trees. She had no objective. No counting. No contest. Just chasing leaves as they fell. It was the ultimate atelic activity, done just for doing it. I joined her and found I was no better at this than a 3-year-old.
We might all benefit from a little time in the woods.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Suits or joggers? A doctor’s dress code
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
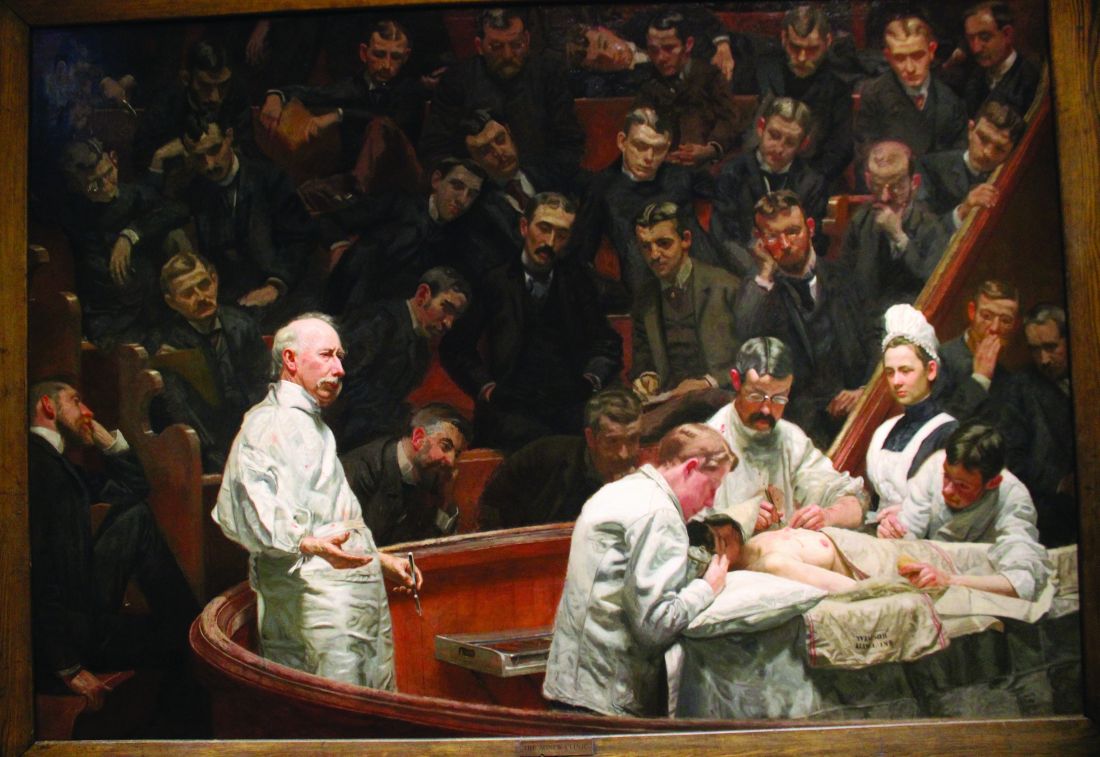
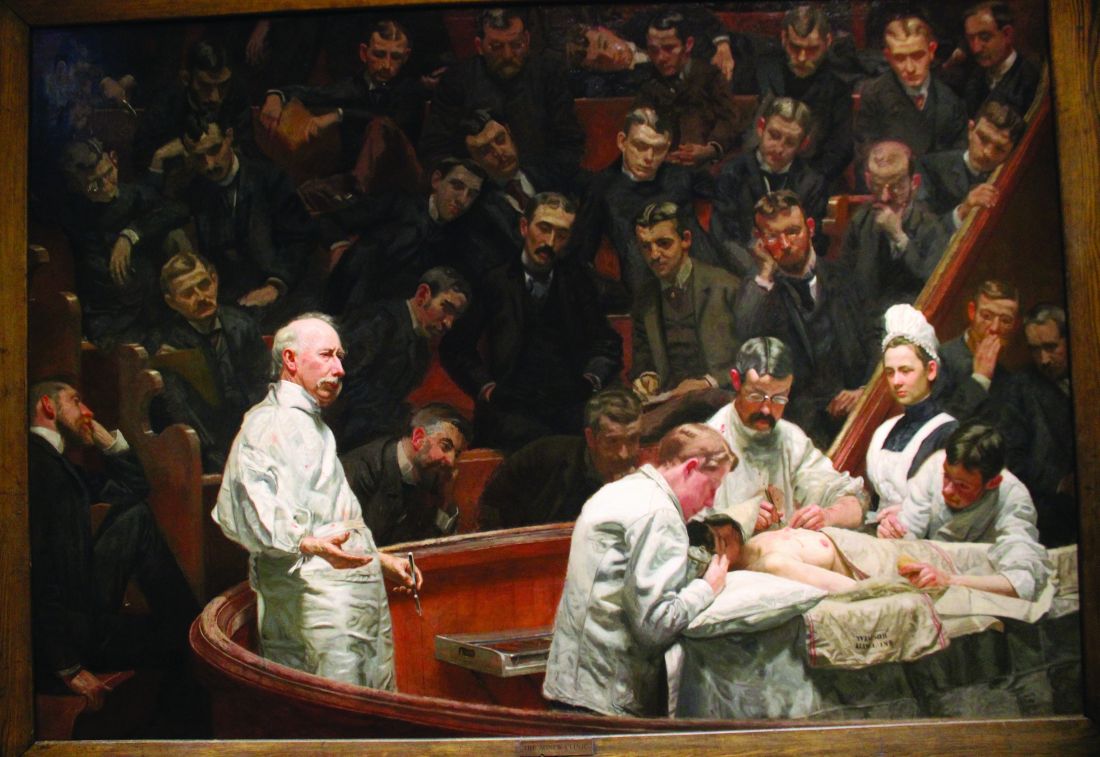
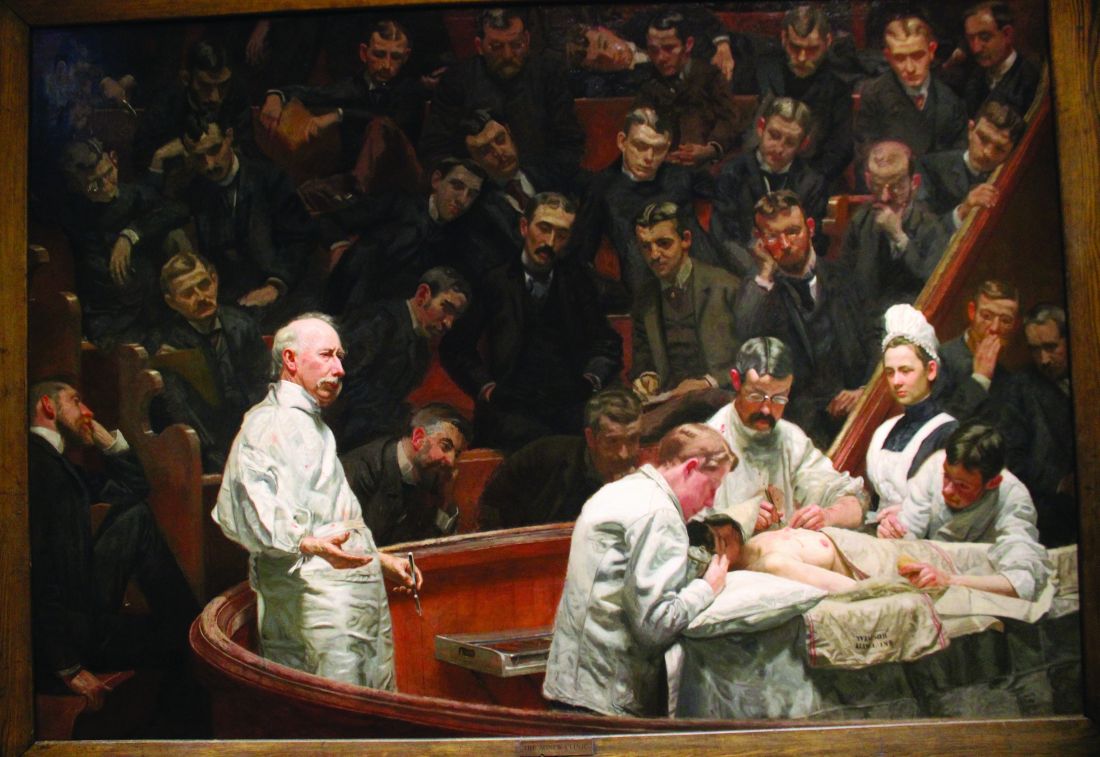
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
The differential diagnosis you’re missing
I’m not the smartest dermatologist in our department. We’re fortunate to have a few super-smarties, you know, the ones who can still recite all the genes in Jean Bolognia’s dermatology textbook and have “Dermpath Bowl Champion” plaques covering their walls. Yet as our chief, I often get requests for a second or third opinion, hoping somehow I’ll discover a diagnosis that others missed. Sometimes they are real diagnostic dilemmas. Oftentimes they’re just itchy.
Recently an itchy 73-year-old woman came to see me. She had seen several competent dermatologists, had comprehensive workups, and had reasonable, even aggressive, attempts at treating. Not much interesting in her history. Nothing on exam. Cancer workup was negative as was pretty much any autoimmune or allergic cause. Biopsy? Maybe a touch of “dermal hypersensitivity.” She was still upset at being told previously she might have scabies. “Scabies!” she said indignantly. “How could I have scabies? No one has touched this body in nearly 4 years!” That’s interesting, I thought.
The electronic medical record holds a lot of useful information. We spend hours combing through histories, labs, pathology, scans, drugs to search for clues that might help with diagnoses. One tab we hardly visit is demographics. Why should that matter, of course? Age, phone number, and address are typically not contributory. But for this woman there was a bit of data that mattered; I checked right after her remark. Marital status: Widowed. She couldn’t have had scabies because no one touches her. Anymore. As our comprehensive workup did not find a cause nor did treatments mitigate her symptoms, I wondered if loneliness might be a contributing factor. I asked if anyone else was itching, any family, any friends? “No, I live alone. I don’t have anyone.”
, and dementia for example. According to the U.S. Surgeon General, it increases the risk for premature death comparable to smoking 15 cigarettes a day. Yet, we rarely (ever?) ask people if they’re lonely. In part because we don’t have good treatments. Remedies for loneliness are mostly societal – reaching out to the widowed, creating spaces that encourage connection, organizing events that bring people together. I cannot type any of these into the EMR orders. However, merely mentioning that a patient could be lonely can be therapeutic. They might not recognize its impact or that they have agency to make it better. They also might not see how their lives still have meaning, an important comorbidity of loneliness.
Not long after her appointment was a 63-year-old man who complained of a burning scrotum. He worked as a knife sharpener, setting up a folding table at local groceries and farmers markets. COVID killed most of his gigs. Like the woman who didn’t have scabies, comprehensive workups turned up nothing. And seemingly nothing, including antibiotics, gabapentin, indomethacin, lidocaine, helped. At his last visit, we talked about his condition. We had also talked about the proper way to sharpen a knife. I came in prepared to offer something dramatic this visit, methotrexate, dupilumab? But before I could speak, he opened a recycled plastic grocery bag and dumped out knives of various sizes. Also a small ax. He then proceeded to show me how each knife has to be sharpened in its own way. Before leaving he handed me a well-worn Arkansas sharpening stone. “For you,” he said. I gave him no additional recommendations or treatments. He hasn’t been back to dermatology since.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
I’m not the smartest dermatologist in our department. We’re fortunate to have a few super-smarties, you know, the ones who can still recite all the genes in Jean Bolognia’s dermatology textbook and have “Dermpath Bowl Champion” plaques covering their walls. Yet as our chief, I often get requests for a second or third opinion, hoping somehow I’ll discover a diagnosis that others missed. Sometimes they are real diagnostic dilemmas. Oftentimes they’re just itchy.
Recently an itchy 73-year-old woman came to see me. She had seen several competent dermatologists, had comprehensive workups, and had reasonable, even aggressive, attempts at treating. Not much interesting in her history. Nothing on exam. Cancer workup was negative as was pretty much any autoimmune or allergic cause. Biopsy? Maybe a touch of “dermal hypersensitivity.” She was still upset at being told previously she might have scabies. “Scabies!” she said indignantly. “How could I have scabies? No one has touched this body in nearly 4 years!” That’s interesting, I thought.
The electronic medical record holds a lot of useful information. We spend hours combing through histories, labs, pathology, scans, drugs to search for clues that might help with diagnoses. One tab we hardly visit is demographics. Why should that matter, of course? Age, phone number, and address are typically not contributory. But for this woman there was a bit of data that mattered; I checked right after her remark. Marital status: Widowed. She couldn’t have had scabies because no one touches her. Anymore. As our comprehensive workup did not find a cause nor did treatments mitigate her symptoms, I wondered if loneliness might be a contributing factor. I asked if anyone else was itching, any family, any friends? “No, I live alone. I don’t have anyone.”
, and dementia for example. According to the U.S. Surgeon General, it increases the risk for premature death comparable to smoking 15 cigarettes a day. Yet, we rarely (ever?) ask people if they’re lonely. In part because we don’t have good treatments. Remedies for loneliness are mostly societal – reaching out to the widowed, creating spaces that encourage connection, organizing events that bring people together. I cannot type any of these into the EMR orders. However, merely mentioning that a patient could be lonely can be therapeutic. They might not recognize its impact or that they have agency to make it better. They also might not see how their lives still have meaning, an important comorbidity of loneliness.
Not long after her appointment was a 63-year-old man who complained of a burning scrotum. He worked as a knife sharpener, setting up a folding table at local groceries and farmers markets. COVID killed most of his gigs. Like the woman who didn’t have scabies, comprehensive workups turned up nothing. And seemingly nothing, including antibiotics, gabapentin, indomethacin, lidocaine, helped. At his last visit, we talked about his condition. We had also talked about the proper way to sharpen a knife. I came in prepared to offer something dramatic this visit, methotrexate, dupilumab? But before I could speak, he opened a recycled plastic grocery bag and dumped out knives of various sizes. Also a small ax. He then proceeded to show me how each knife has to be sharpened in its own way. Before leaving he handed me a well-worn Arkansas sharpening stone. “For you,” he said. I gave him no additional recommendations or treatments. He hasn’t been back to dermatology since.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
I’m not the smartest dermatologist in our department. We’re fortunate to have a few super-smarties, you know, the ones who can still recite all the genes in Jean Bolognia’s dermatology textbook and have “Dermpath Bowl Champion” plaques covering their walls. Yet as our chief, I often get requests for a second or third opinion, hoping somehow I’ll discover a diagnosis that others missed. Sometimes they are real diagnostic dilemmas. Oftentimes they’re just itchy.
Recently an itchy 73-year-old woman came to see me. She had seen several competent dermatologists, had comprehensive workups, and had reasonable, even aggressive, attempts at treating. Not much interesting in her history. Nothing on exam. Cancer workup was negative as was pretty much any autoimmune or allergic cause. Biopsy? Maybe a touch of “dermal hypersensitivity.” She was still upset at being told previously she might have scabies. “Scabies!” she said indignantly. “How could I have scabies? No one has touched this body in nearly 4 years!” That’s interesting, I thought.
The electronic medical record holds a lot of useful information. We spend hours combing through histories, labs, pathology, scans, drugs to search for clues that might help with diagnoses. One tab we hardly visit is demographics. Why should that matter, of course? Age, phone number, and address are typically not contributory. But for this woman there was a bit of data that mattered; I checked right after her remark. Marital status: Widowed. She couldn’t have had scabies because no one touches her. Anymore. As our comprehensive workup did not find a cause nor did treatments mitigate her symptoms, I wondered if loneliness might be a contributing factor. I asked if anyone else was itching, any family, any friends? “No, I live alone. I don’t have anyone.”
, and dementia for example. According to the U.S. Surgeon General, it increases the risk for premature death comparable to smoking 15 cigarettes a day. Yet, we rarely (ever?) ask people if they’re lonely. In part because we don’t have good treatments. Remedies for loneliness are mostly societal – reaching out to the widowed, creating spaces that encourage connection, organizing events that bring people together. I cannot type any of these into the EMR orders. However, merely mentioning that a patient could be lonely can be therapeutic. They might not recognize its impact or that they have agency to make it better. They also might not see how their lives still have meaning, an important comorbidity of loneliness.
Not long after her appointment was a 63-year-old man who complained of a burning scrotum. He worked as a knife sharpener, setting up a folding table at local groceries and farmers markets. COVID killed most of his gigs. Like the woman who didn’t have scabies, comprehensive workups turned up nothing. And seemingly nothing, including antibiotics, gabapentin, indomethacin, lidocaine, helped. At his last visit, we talked about his condition. We had also talked about the proper way to sharpen a knife. I came in prepared to offer something dramatic this visit, methotrexate, dupilumab? But before I could speak, he opened a recycled plastic grocery bag and dumped out knives of various sizes. Also a small ax. He then proceeded to show me how each knife has to be sharpened in its own way. Before leaving he handed me a well-worn Arkansas sharpening stone. “For you,” he said. I gave him no additional recommendations or treatments. He hasn’t been back to dermatology since.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Can we be too efficient?
“We were all of us cogs in a great machine which sometimes rolled forward, nobody knew where, sometimes backwards, nobody knew why.” – Ernst Toller
A nice feature of the Apple watch is the stopwatch. With it, I can discreetly click the timer and watch seconds tick away. Tap. There’s one lap. Tap. Two. Tap. That was a quick visit, 6 minutes and 42 seconds. Tap. Under 2 minutes to close the chart. Let’s see if I can beat it. Tap. Tap. What if I moved my Mayo stand over to this side of the room? How about a sign, “All patients must have clothes off if you want a skin exam.” You think ob.gyns. are quick from skin to baby in a stat C-section? You should see how fast I can go from alcohol wipe to Drysol on a biopsy. Seconds. Tick, tick, tap.
Every day I look for ways to go faster. This is not so I can be out the door by 3. Rather, it’s simply to make it through the day without having to log on after we put the kids to bed at night.
Speaking of bedtimes, another nice feature of the Apple watch is the timer. With it, I can set a timer and a lovely chimey alarm will go off. This comes in handy with 3-year-olds. “Sloan, in two minutes we are going to brush your teeth.” Ding. “Sloan, you have one minute to get your pajamas on.” Ding. “Sloanie, I’ll give you 3 more minutes to put the kitties away, then get into bed.” Ding, ding, ding ...
As you can see, using the stopwatch to time a bedtime routine would be demoralizing. If you’ve tried to put a toddler to bed in summer you know. They explore every option to avoid sleeping: one more book (that would make 3), “accidentally” putting their pajamas on backwards, offering to brush their teeth a second time. And once the light is off, “Papa, I have to potty.” No, bedtime routines cannot be standardized. They resist being made efficient.
In contrast, , Frederick Taylor. Taylor, a mechanical engineer, observed inefficiencies on the factory floor. His work was seminal in the development of the second industrial revolution. Before then no one had applied scientific rigor to productivity. His book, “The Principles of Scientific Management,” written in 1909, is considered the most influential management book of the 20th century. He was the first to use stopwatches to perform time studies, noting how long each task took with the belief that there was one best way. The worker was an extension of the machine, tuned by management such that he was as efficient as possible.

Others built on this idea including Frank and Lillian Gilbreth who added video recording, creating time and motion studies to further drive efficiency. This technique is still used in manufacturing and service industries today, including health care. In the 1980s, W. Edwards Deming modernized this effort, empowering workers with techniques taken from Japanese manufacturing. This, too, has been widely adopted in health care and evolved into the Lean and Lean Six Sigma quality movements about a decade ago. The common theme is to reduce waste to make health care as efficient as possible. Lately, this idea seems to have failed us.
The difficulty lies in the belief that efficient is always better. I’m unsure. Efficiency helps to reduce costs. It can also improve access. Yet, it comes at a cost. Eliminating slack concomitantly eliminates resilience. As such, when unexpected and significant changes impact a system, the gears of productivity jam. It’s in part why we are seeing rising wait times and patient dissatisfaction post pandemic. There was no slack and our system was too brittle.
A more insidious downside on the drive to efficiency lies in the nature of what we do. We aren’t factory workers punching out widgets, we’re physicians caring for people and people cannot be standardized. In this way, seeing patients is more like putting a toddler to bed than like assembling an iPhone. There will always be by-the-ways, basal cells hiding behind the ear, traffic jams, and bags of products that they want to review. Not sure how to use your fluorouracil? Let’s go over it again. Need to talk more about why you have granuloma annulare? Let me explain. Despite Taylor’s vision, some work simply cannot be optimized. And shouldn’t.
“Where’s my 11:30 patient who checked in half an hour ago?!” I asked my medical assistant. “Oh, she had to go to the bathroom.” Tap.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“We were all of us cogs in a great machine which sometimes rolled forward, nobody knew where, sometimes backwards, nobody knew why.” – Ernst Toller
A nice feature of the Apple watch is the stopwatch. With it, I can discreetly click the timer and watch seconds tick away. Tap. There’s one lap. Tap. Two. Tap. That was a quick visit, 6 minutes and 42 seconds. Tap. Under 2 minutes to close the chart. Let’s see if I can beat it. Tap. Tap. What if I moved my Mayo stand over to this side of the room? How about a sign, “All patients must have clothes off if you want a skin exam.” You think ob.gyns. are quick from skin to baby in a stat C-section? You should see how fast I can go from alcohol wipe to Drysol on a biopsy. Seconds. Tick, tick, tap.
Every day I look for ways to go faster. This is not so I can be out the door by 3. Rather, it’s simply to make it through the day without having to log on after we put the kids to bed at night.
Speaking of bedtimes, another nice feature of the Apple watch is the timer. With it, I can set a timer and a lovely chimey alarm will go off. This comes in handy with 3-year-olds. “Sloan, in two minutes we are going to brush your teeth.” Ding. “Sloan, you have one minute to get your pajamas on.” Ding. “Sloanie, I’ll give you 3 more minutes to put the kitties away, then get into bed.” Ding, ding, ding ...
As you can see, using the stopwatch to time a bedtime routine would be demoralizing. If you’ve tried to put a toddler to bed in summer you know. They explore every option to avoid sleeping: one more book (that would make 3), “accidentally” putting their pajamas on backwards, offering to brush their teeth a second time. And once the light is off, “Papa, I have to potty.” No, bedtime routines cannot be standardized. They resist being made efficient.
In contrast, , Frederick Taylor. Taylor, a mechanical engineer, observed inefficiencies on the factory floor. His work was seminal in the development of the second industrial revolution. Before then no one had applied scientific rigor to productivity. His book, “The Principles of Scientific Management,” written in 1909, is considered the most influential management book of the 20th century. He was the first to use stopwatches to perform time studies, noting how long each task took with the belief that there was one best way. The worker was an extension of the machine, tuned by management such that he was as efficient as possible.

Others built on this idea including Frank and Lillian Gilbreth who added video recording, creating time and motion studies to further drive efficiency. This technique is still used in manufacturing and service industries today, including health care. In the 1980s, W. Edwards Deming modernized this effort, empowering workers with techniques taken from Japanese manufacturing. This, too, has been widely adopted in health care and evolved into the Lean and Lean Six Sigma quality movements about a decade ago. The common theme is to reduce waste to make health care as efficient as possible. Lately, this idea seems to have failed us.
The difficulty lies in the belief that efficient is always better. I’m unsure. Efficiency helps to reduce costs. It can also improve access. Yet, it comes at a cost. Eliminating slack concomitantly eliminates resilience. As such, when unexpected and significant changes impact a system, the gears of productivity jam. It’s in part why we are seeing rising wait times and patient dissatisfaction post pandemic. There was no slack and our system was too brittle.
A more insidious downside on the drive to efficiency lies in the nature of what we do. We aren’t factory workers punching out widgets, we’re physicians caring for people and people cannot be standardized. In this way, seeing patients is more like putting a toddler to bed than like assembling an iPhone. There will always be by-the-ways, basal cells hiding behind the ear, traffic jams, and bags of products that they want to review. Not sure how to use your fluorouracil? Let’s go over it again. Need to talk more about why you have granuloma annulare? Let me explain. Despite Taylor’s vision, some work simply cannot be optimized. And shouldn’t.
“Where’s my 11:30 patient who checked in half an hour ago?!” I asked my medical assistant. “Oh, she had to go to the bathroom.” Tap.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“We were all of us cogs in a great machine which sometimes rolled forward, nobody knew where, sometimes backwards, nobody knew why.” – Ernst Toller
A nice feature of the Apple watch is the stopwatch. With it, I can discreetly click the timer and watch seconds tick away. Tap. There’s one lap. Tap. Two. Tap. That was a quick visit, 6 minutes and 42 seconds. Tap. Under 2 minutes to close the chart. Let’s see if I can beat it. Tap. Tap. What if I moved my Mayo stand over to this side of the room? How about a sign, “All patients must have clothes off if you want a skin exam.” You think ob.gyns. are quick from skin to baby in a stat C-section? You should see how fast I can go from alcohol wipe to Drysol on a biopsy. Seconds. Tick, tick, tap.
Every day I look for ways to go faster. This is not so I can be out the door by 3. Rather, it’s simply to make it through the day without having to log on after we put the kids to bed at night.
Speaking of bedtimes, another nice feature of the Apple watch is the timer. With it, I can set a timer and a lovely chimey alarm will go off. This comes in handy with 3-year-olds. “Sloan, in two minutes we are going to brush your teeth.” Ding. “Sloan, you have one minute to get your pajamas on.” Ding. “Sloanie, I’ll give you 3 more minutes to put the kitties away, then get into bed.” Ding, ding, ding ...
As you can see, using the stopwatch to time a bedtime routine would be demoralizing. If you’ve tried to put a toddler to bed in summer you know. They explore every option to avoid sleeping: one more book (that would make 3), “accidentally” putting their pajamas on backwards, offering to brush their teeth a second time. And once the light is off, “Papa, I have to potty.” No, bedtime routines cannot be standardized. They resist being made efficient.
In contrast, , Frederick Taylor. Taylor, a mechanical engineer, observed inefficiencies on the factory floor. His work was seminal in the development of the second industrial revolution. Before then no one had applied scientific rigor to productivity. His book, “The Principles of Scientific Management,” written in 1909, is considered the most influential management book of the 20th century. He was the first to use stopwatches to perform time studies, noting how long each task took with the belief that there was one best way. The worker was an extension of the machine, tuned by management such that he was as efficient as possible.

Others built on this idea including Frank and Lillian Gilbreth who added video recording, creating time and motion studies to further drive efficiency. This technique is still used in manufacturing and service industries today, including health care. In the 1980s, W. Edwards Deming modernized this effort, empowering workers with techniques taken from Japanese manufacturing. This, too, has been widely adopted in health care and evolved into the Lean and Lean Six Sigma quality movements about a decade ago. The common theme is to reduce waste to make health care as efficient as possible. Lately, this idea seems to have failed us.
The difficulty lies in the belief that efficient is always better. I’m unsure. Efficiency helps to reduce costs. It can also improve access. Yet, it comes at a cost. Eliminating slack concomitantly eliminates resilience. As such, when unexpected and significant changes impact a system, the gears of productivity jam. It’s in part why we are seeing rising wait times and patient dissatisfaction post pandemic. There was no slack and our system was too brittle.
A more insidious downside on the drive to efficiency lies in the nature of what we do. We aren’t factory workers punching out widgets, we’re physicians caring for people and people cannot be standardized. In this way, seeing patients is more like putting a toddler to bed than like assembling an iPhone. There will always be by-the-ways, basal cells hiding behind the ear, traffic jams, and bags of products that they want to review. Not sure how to use your fluorouracil? Let’s go over it again. Need to talk more about why you have granuloma annulare? Let me explain. Despite Taylor’s vision, some work simply cannot be optimized. And shouldn’t.
“Where’s my 11:30 patient who checked in half an hour ago?!” I asked my medical assistant. “Oh, she had to go to the bathroom.” Tap.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
The sacred office space
Church architecture describes visually the idea of the sacred, which is a fundamental need of man.
– Mario Botta, Swiss architect
My parents are visiting the Holy See today – prima volta in Italia! My mom waited years for this. She isn’t meeting the Pope or attending Mass. Yet, in the Whatsapp pics they sent me, you can see tears well up as she experiences St. Peter’s Basilica. It’s a visceral response to what is just a building and a poignant example of the significance of spaces.
More than just appreciating an edifice’s grandeur or exquisiteness, we are wired to connect with spaces emotionally. Beautiful or significant buildings move us, they make us feel something. Churches, synagogues, or mosques are good examples. They combine spiritual and aesthetic allure. But so too do gorgeous hotels, Apple stores, and posh restaurants. We crave the richness of an environment experienced through our five senses. The glory of sunlight through stained glass, the smell of luxurious scent pumped into a lobby, the weight of a silky new iPhone in your hand. We also have a sixth sense, that feeling we get from knowing that we are standing in a sacred place. A physical space that connects us with something wider and deeper than ourselves.
Virtual may be the peak of convenience, but in-real-life is the pinnacle of experience. Patients will be inconvenienced and pay higher costs to experience their appointment in person. This should not be surprising. Contemplate this: Every year, millions of people will travel across the globe to stand before a wall or walk seven times around a stone building. And millions everyday will perambulate around an Apple Store, willingly paying a higher price for the same product they can buy for less elsewhere. The willingness to pay for certain experiences is remarkably high.
Every day when I cover patient messages, I offer some patients an immediate, free solution to their problem. Just today I exchanged emails with a patient thinking I had addressed her concern by reassuring her that it was a benign seborrheic keratosis. Done. She then replied, “Thanks so much, Dr. Benabio! I still would like to schedule an appointment to come in person.” So much for the efficiency of digital medicine.
Before dismissing these patients as Luddites, understand what they want is the doctor’s office experience. The sights, the smells, the sacredness of what happens here. It is no coincidence that the first clinics were temples. In ancient Greece and Rome, the sick and the gashed made pilgrimages to one of at least 300 Asclepieia, temples of healing. During the medieval period, monasteries doubled as housing for the sick until the church began constructing stand-alone hospitals, often in cross-shaped design with an altar in the middle (eventually that became the nurses station, but without the wine).
Patients entrust us with their lives and their loved ones’ lives and a visit takes on far more significance than a simple service transaction. Forty years on, I can recall visits to Dr. Bellin’s office. He saw pediatric patients out of his Victorian home office with broad, creaky hardwood floors, stained glass, and cast iron radiators. The scent of isopropyl soaked cotton balls and typewriter ink is unforgettable. Far from sterile, it was warm, safe. It was a sacred place, one for which we still sometimes drive by when doing the tour of where I grew up.
We shall forge ahead and continue to offer virtual channels to serve our patients just as any service industry. But don’t force them there. At the same time Starbucks has been building its digital app, it is also building Starbucks Reserve Roasteries. Immense cathedral edifices with warm woods and luxurious brass, the smell of roasting coffee and warm leather perfuming the air. It is where patrons will travel long distances and endure long waits to pay a lot more for a cup of coffee.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Church architecture describes visually the idea of the sacred, which is a fundamental need of man.
– Mario Botta, Swiss architect
My parents are visiting the Holy See today – prima volta in Italia! My mom waited years for this. She isn’t meeting the Pope or attending Mass. Yet, in the Whatsapp pics they sent me, you can see tears well up as she experiences St. Peter’s Basilica. It’s a visceral response to what is just a building and a poignant example of the significance of spaces.
More than just appreciating an edifice’s grandeur or exquisiteness, we are wired to connect with spaces emotionally. Beautiful or significant buildings move us, they make us feel something. Churches, synagogues, or mosques are good examples. They combine spiritual and aesthetic allure. But so too do gorgeous hotels, Apple stores, and posh restaurants. We crave the richness of an environment experienced through our five senses. The glory of sunlight through stained glass, the smell of luxurious scent pumped into a lobby, the weight of a silky new iPhone in your hand. We also have a sixth sense, that feeling we get from knowing that we are standing in a sacred place. A physical space that connects us with something wider and deeper than ourselves.
Virtual may be the peak of convenience, but in-real-life is the pinnacle of experience. Patients will be inconvenienced and pay higher costs to experience their appointment in person. This should not be surprising. Contemplate this: Every year, millions of people will travel across the globe to stand before a wall or walk seven times around a stone building. And millions everyday will perambulate around an Apple Store, willingly paying a higher price for the same product they can buy for less elsewhere. The willingness to pay for certain experiences is remarkably high.
Every day when I cover patient messages, I offer some patients an immediate, free solution to their problem. Just today I exchanged emails with a patient thinking I had addressed her concern by reassuring her that it was a benign seborrheic keratosis. Done. She then replied, “Thanks so much, Dr. Benabio! I still would like to schedule an appointment to come in person.” So much for the efficiency of digital medicine.
Before dismissing these patients as Luddites, understand what they want is the doctor’s office experience. The sights, the smells, the sacredness of what happens here. It is no coincidence that the first clinics were temples. In ancient Greece and Rome, the sick and the gashed made pilgrimages to one of at least 300 Asclepieia, temples of healing. During the medieval period, monasteries doubled as housing for the sick until the church began constructing stand-alone hospitals, often in cross-shaped design with an altar in the middle (eventually that became the nurses station, but without the wine).
Patients entrust us with their lives and their loved ones’ lives and a visit takes on far more significance than a simple service transaction. Forty years on, I can recall visits to Dr. Bellin’s office. He saw pediatric patients out of his Victorian home office with broad, creaky hardwood floors, stained glass, and cast iron radiators. The scent of isopropyl soaked cotton balls and typewriter ink is unforgettable. Far from sterile, it was warm, safe. It was a sacred place, one for which we still sometimes drive by when doing the tour of where I grew up.
We shall forge ahead and continue to offer virtual channels to serve our patients just as any service industry. But don’t force them there. At the same time Starbucks has been building its digital app, it is also building Starbucks Reserve Roasteries. Immense cathedral edifices with warm woods and luxurious brass, the smell of roasting coffee and warm leather perfuming the air. It is where patrons will travel long distances and endure long waits to pay a lot more for a cup of coffee.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Church architecture describes visually the idea of the sacred, which is a fundamental need of man.
– Mario Botta, Swiss architect
My parents are visiting the Holy See today – prima volta in Italia! My mom waited years for this. She isn’t meeting the Pope or attending Mass. Yet, in the Whatsapp pics they sent me, you can see tears well up as she experiences St. Peter’s Basilica. It’s a visceral response to what is just a building and a poignant example of the significance of spaces.
More than just appreciating an edifice’s grandeur or exquisiteness, we are wired to connect with spaces emotionally. Beautiful or significant buildings move us, they make us feel something. Churches, synagogues, or mosques are good examples. They combine spiritual and aesthetic allure. But so too do gorgeous hotels, Apple stores, and posh restaurants. We crave the richness of an environment experienced through our five senses. The glory of sunlight through stained glass, the smell of luxurious scent pumped into a lobby, the weight of a silky new iPhone in your hand. We also have a sixth sense, that feeling we get from knowing that we are standing in a sacred place. A physical space that connects us with something wider and deeper than ourselves.
Virtual may be the peak of convenience, but in-real-life is the pinnacle of experience. Patients will be inconvenienced and pay higher costs to experience their appointment in person. This should not be surprising. Contemplate this: Every year, millions of people will travel across the globe to stand before a wall or walk seven times around a stone building. And millions everyday will perambulate around an Apple Store, willingly paying a higher price for the same product they can buy for less elsewhere. The willingness to pay for certain experiences is remarkably high.
Every day when I cover patient messages, I offer some patients an immediate, free solution to their problem. Just today I exchanged emails with a patient thinking I had addressed her concern by reassuring her that it was a benign seborrheic keratosis. Done. She then replied, “Thanks so much, Dr. Benabio! I still would like to schedule an appointment to come in person.” So much for the efficiency of digital medicine.
Before dismissing these patients as Luddites, understand what they want is the doctor’s office experience. The sights, the smells, the sacredness of what happens here. It is no coincidence that the first clinics were temples. In ancient Greece and Rome, the sick and the gashed made pilgrimages to one of at least 300 Asclepieia, temples of healing. During the medieval period, monasteries doubled as housing for the sick until the church began constructing stand-alone hospitals, often in cross-shaped design with an altar in the middle (eventually that became the nurses station, but without the wine).
Patients entrust us with their lives and their loved ones’ lives and a visit takes on far more significance than a simple service transaction. Forty years on, I can recall visits to Dr. Bellin’s office. He saw pediatric patients out of his Victorian home office with broad, creaky hardwood floors, stained glass, and cast iron radiators. The scent of isopropyl soaked cotton balls and typewriter ink is unforgettable. Far from sterile, it was warm, safe. It was a sacred place, one for which we still sometimes drive by when doing the tour of where I grew up.
We shall forge ahead and continue to offer virtual channels to serve our patients just as any service industry. But don’t force them there. At the same time Starbucks has been building its digital app, it is also building Starbucks Reserve Roasteries. Immense cathedral edifices with warm woods and luxurious brass, the smell of roasting coffee and warm leather perfuming the air. It is where patrons will travel long distances and endure long waits to pay a lot more for a cup of coffee.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
How not to establish rapport with your patient
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Morning PT
Tuesdays and Fridays are tough. Not so much because of clinic, but rather because of the 32 minutes before clinic that I’m on the Peloton bike. They are the mornings I dedicate to training VO2max.
Training VO2max, or maximal oxygen consumption, is simple. Spin for a leisurely, easy-breathing, 4 minutes, then for 4 minutes push yourself until you see the light of heaven and wish for death to come. Then relax for 4 minutes again. Repeat this cycle four to six times. Done justly, you will dread Tuesdays and Fridays too. The punishing cycle of a 4-minute push, then 4-minute recovery is, however, an excellent way to improve cardiovascular fitness. And no, I’m not training for the Boston Marathon, so why am I working so hard? Because I’m training for marathon clinic days for the next 20 years.
Now more than ever, I feel we have to be physically fit to deal with a physicians’ day’s work. It’s exhausting. The root cause is too much work, yes, but I believe being physically fit could help.
I was talking to an 86-year-old patient about this very topic recently. He was short, with a well-manicured goatee and shiny head. He stuck his arm out to shake my hand. “Glad we’re back to handshakes again, doc.” His grip was that of a 30-year-old. “Buff” you’d likely describe him: He is noticeably muscular, not a skinny old man. He’s an old Navy Master Chief who started a business in wholesale flowers, which distributes all over the United States. And he’s still working full time. Impressed, I asked his secret for such vigor. PT, he replied.
PT, or physical training, is a foundational element of the Navy. Every sailor starts his or her day with morning PT before carrying out their duties. Some 30 years later, this guy is still getting after it. He does push-ups, sit-ups, and pull-ups nearly every morning. Morning PT is what he attributes to his success not only in health, but also business. As he sees it, he has the business savvy and experience of an old guy and the energy and stamina of a college kid. A good combination for a successful life.
I’ve always been pretty fit. Lately, I’ve been trying to take it to the next level, to not just be “physically active,” but rather “high-performance fit.” There are plenty of sources for instruction; how to stay young and healthy isn’t a new idea after all. I mean, Herodotus wrote of finding the Fountain of Youth in the 5th century BCE. A couple thousand years later, it’s still on trend. One of my favorite sages giving health span advice is Peter Attia, MD. I’ve been a fan since I met him at TEDMED in 2013 and I marvel at the astounding body of work he has created since. A Johns Hopkins–trained surgeon, he has spent his career reviewing the scientific literature about longevity and sharing it as actionable content. His book, “Outlive: The Science and Art of Longevity” (New York: Penguin Random House, 2023) is a nice summary of his work. I recommend it.
Right now I’m switching between type 2 muscle fiber work (lots of jumping like my 2-year-old) and cardiovascular training including the aforementioned VO2max work. I cannot say that my patient inbox is any cleaner, or that I’m faster in the office, but I’m not flagging by the end of the day anymore. Master Chief challenged me to match his 10 pull-ups before he returns for his follow up visit. I’ll gladly give up Peloton sprints to work on that.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Tuesdays and Fridays are tough. Not so much because of clinic, but rather because of the 32 minutes before clinic that I’m on the Peloton bike. They are the mornings I dedicate to training VO2max.
Training VO2max, or maximal oxygen consumption, is simple. Spin for a leisurely, easy-breathing, 4 minutes, then for 4 minutes push yourself until you see the light of heaven and wish for death to come. Then relax for 4 minutes again. Repeat this cycle four to six times. Done justly, you will dread Tuesdays and Fridays too. The punishing cycle of a 4-minute push, then 4-minute recovery is, however, an excellent way to improve cardiovascular fitness. And no, I’m not training for the Boston Marathon, so why am I working so hard? Because I’m training for marathon clinic days for the next 20 years.
Now more than ever, I feel we have to be physically fit to deal with a physicians’ day’s work. It’s exhausting. The root cause is too much work, yes, but I believe being physically fit could help.
I was talking to an 86-year-old patient about this very topic recently. He was short, with a well-manicured goatee and shiny head. He stuck his arm out to shake my hand. “Glad we’re back to handshakes again, doc.” His grip was that of a 30-year-old. “Buff” you’d likely describe him: He is noticeably muscular, not a skinny old man. He’s an old Navy Master Chief who started a business in wholesale flowers, which distributes all over the United States. And he’s still working full time. Impressed, I asked his secret for such vigor. PT, he replied.
PT, or physical training, is a foundational element of the Navy. Every sailor starts his or her day with morning PT before carrying out their duties. Some 30 years later, this guy is still getting after it. He does push-ups, sit-ups, and pull-ups nearly every morning. Morning PT is what he attributes to his success not only in health, but also business. As he sees it, he has the business savvy and experience of an old guy and the energy and stamina of a college kid. A good combination for a successful life.
I’ve always been pretty fit. Lately, I’ve been trying to take it to the next level, to not just be “physically active,” but rather “high-performance fit.” There are plenty of sources for instruction; how to stay young and healthy isn’t a new idea after all. I mean, Herodotus wrote of finding the Fountain of Youth in the 5th century BCE. A couple thousand years later, it’s still on trend. One of my favorite sages giving health span advice is Peter Attia, MD. I’ve been a fan since I met him at TEDMED in 2013 and I marvel at the astounding body of work he has created since. A Johns Hopkins–trained surgeon, he has spent his career reviewing the scientific literature about longevity and sharing it as actionable content. His book, “Outlive: The Science and Art of Longevity” (New York: Penguin Random House, 2023) is a nice summary of his work. I recommend it.
Right now I’m switching between type 2 muscle fiber work (lots of jumping like my 2-year-old) and cardiovascular training including the aforementioned VO2max work. I cannot say that my patient inbox is any cleaner, or that I’m faster in the office, but I’m not flagging by the end of the day anymore. Master Chief challenged me to match his 10 pull-ups before he returns for his follow up visit. I’ll gladly give up Peloton sprints to work on that.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Tuesdays and Fridays are tough. Not so much because of clinic, but rather because of the 32 minutes before clinic that I’m on the Peloton bike. They are the mornings I dedicate to training VO2max.
Training VO2max, or maximal oxygen consumption, is simple. Spin for a leisurely, easy-breathing, 4 minutes, then for 4 minutes push yourself until you see the light of heaven and wish for death to come. Then relax for 4 minutes again. Repeat this cycle four to six times. Done justly, you will dread Tuesdays and Fridays too. The punishing cycle of a 4-minute push, then 4-minute recovery is, however, an excellent way to improve cardiovascular fitness. And no, I’m not training for the Boston Marathon, so why am I working so hard? Because I’m training for marathon clinic days for the next 20 years.
Now more than ever, I feel we have to be physically fit to deal with a physicians’ day’s work. It’s exhausting. The root cause is too much work, yes, but I believe being physically fit could help.
I was talking to an 86-year-old patient about this very topic recently. He was short, with a well-manicured goatee and shiny head. He stuck his arm out to shake my hand. “Glad we’re back to handshakes again, doc.” His grip was that of a 30-year-old. “Buff” you’d likely describe him: He is noticeably muscular, not a skinny old man. He’s an old Navy Master Chief who started a business in wholesale flowers, which distributes all over the United States. And he’s still working full time. Impressed, I asked his secret for such vigor. PT, he replied.
PT, or physical training, is a foundational element of the Navy. Every sailor starts his or her day with morning PT before carrying out their duties. Some 30 years later, this guy is still getting after it. He does push-ups, sit-ups, and pull-ups nearly every morning. Morning PT is what he attributes to his success not only in health, but also business. As he sees it, he has the business savvy and experience of an old guy and the energy and stamina of a college kid. A good combination for a successful life.
I’ve always been pretty fit. Lately, I’ve been trying to take it to the next level, to not just be “physically active,” but rather “high-performance fit.” There are plenty of sources for instruction; how to stay young and healthy isn’t a new idea after all. I mean, Herodotus wrote of finding the Fountain of Youth in the 5th century BCE. A couple thousand years later, it’s still on trend. One of my favorite sages giving health span advice is Peter Attia, MD. I’ve been a fan since I met him at TEDMED in 2013 and I marvel at the astounding body of work he has created since. A Johns Hopkins–trained surgeon, he has spent his career reviewing the scientific literature about longevity and sharing it as actionable content. His book, “Outlive: The Science and Art of Longevity” (New York: Penguin Random House, 2023) is a nice summary of his work. I recommend it.
Right now I’m switching between type 2 muscle fiber work (lots of jumping like my 2-year-old) and cardiovascular training including the aforementioned VO2max work. I cannot say that my patient inbox is any cleaner, or that I’m faster in the office, but I’m not flagging by the end of the day anymore. Master Chief challenged me to match his 10 pull-ups before he returns for his follow up visit. I’ll gladly give up Peloton sprints to work on that.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Get action! – Teddy Roosevelt
“Papa! Where donut?” asks my 2½ year-old sitting with her legs dangling and hands folded in a bustling Starbucks. We’ve been waiting for 8 minutes and we’ve reached her limit of tolerance. She’s unimpressed by the queued customers who compliment her curly blonde hair, many of whom have come and gone since we’ve been waiting. I agree – how long does it take to pour a kiddie milk and grab a donut? We can both see it in the case right there!
No one likes to wait. Truly, one of the great benefits of the modern world is that wait times are now incredibly short. Many Starbucks customers, unlike my daughter, ordered their drink ahead and waited exactly 0 minutes to get their drink. What about Amazon? I ordered a bird feeder this morning and it’s already hanging in the yard. It’s still daylight. Feel like Himalayan Momo Dumplings tonight? Your food could arrive in 37 minutes. The modern wait standard has been set impossibly high for us.
Yes, for some. We created a whole room just for waiting. Airlines call theirs “The Platinum Executive Lounge.” Ours is “The waiting room.”
Excess waiting is a significant reason why health care gets beat up in reviews. We’re unable to keep up with the new expectations. Waiting is also a significant cause of distress. Many patients report the most difficult part of their cancer diagnosis was the waiting for results, not the treatment. It’s because when under stress, we are hardwired to take action. Binding patients into inaction while they wait is very uncomfortable.
Fortunately, the psychology of waiting is well understood and there are best practices that can help. First, anxiety makes waiting much worse. Conveying confidence and reassuring patients they are in the right place and that everything will be OK makes the wait time feel shorter for them. Uncertainty also compounds their apprehension. If you believe the diagnosis will be melanoma, tell them that at the time of the biopsy and tell them what you expect next. This is better than saying, “Well, that could be cancer. We’ll see.”
Knowing a wait time is also much better than not. Have your staff advise patients on how much longer they can expect before seeing you (telling them they’re next isn’t as effective). Advise that test results should be back by the end of next week. Of course, under promise and over deliver. When the results are back on Tuesday, you’ve got a pleased patient.
Explaining that you had to add in an urgent patient helps. Even if it’s not your fault, it’s still better to apologize. For example, the 78 highway, the left anterior descending artery to our office, has been closed because of a sinkhole this month (not kidding). I’ve been apologizing to a lot of patients saying that all our patients are arriving late, which is putting us behind. As they can envision the linear parking lot that used to be a highway, it helps.
Lastly, as any child can tell you, waiting has to not only be, but to also appear, fair. The only thing worse than waiting for an appointment, or donut, is seeing someone who came in after you get their donut before you do. If you’re pulling both Mohs and cosmetics patients from the same waiting area, then your surgery patients will see a lot of patients come and go while they are sitting. Demarcating one sitting area for Mohs and one for clinics might help. So does ordering ahead. I’d show my daughter how to use the app so we don’t have to wait so long next week, but she’s 2 and I’m quite sure she already knows.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“Papa! Where donut?” asks my 2½ year-old sitting with her legs dangling and hands folded in a bustling Starbucks. We’ve been waiting for 8 minutes and we’ve reached her limit of tolerance. She’s unimpressed by the queued customers who compliment her curly blonde hair, many of whom have come and gone since we’ve been waiting. I agree – how long does it take to pour a kiddie milk and grab a donut? We can both see it in the case right there!
No one likes to wait. Truly, one of the great benefits of the modern world is that wait times are now incredibly short. Many Starbucks customers, unlike my daughter, ordered their drink ahead and waited exactly 0 minutes to get their drink. What about Amazon? I ordered a bird feeder this morning and it’s already hanging in the yard. It’s still daylight. Feel like Himalayan Momo Dumplings tonight? Your food could arrive in 37 minutes. The modern wait standard has been set impossibly high for us.
Yes, for some. We created a whole room just for waiting. Airlines call theirs “The Platinum Executive Lounge.” Ours is “The waiting room.”
Excess waiting is a significant reason why health care gets beat up in reviews. We’re unable to keep up with the new expectations. Waiting is also a significant cause of distress. Many patients report the most difficult part of their cancer diagnosis was the waiting for results, not the treatment. It’s because when under stress, we are hardwired to take action. Binding patients into inaction while they wait is very uncomfortable.
Fortunately, the psychology of waiting is well understood and there are best practices that can help. First, anxiety makes waiting much worse. Conveying confidence and reassuring patients they are in the right place and that everything will be OK makes the wait time feel shorter for them. Uncertainty also compounds their apprehension. If you believe the diagnosis will be melanoma, tell them that at the time of the biopsy and tell them what you expect next. This is better than saying, “Well, that could be cancer. We’ll see.”
Knowing a wait time is also much better than not. Have your staff advise patients on how much longer they can expect before seeing you (telling them they’re next isn’t as effective). Advise that test results should be back by the end of next week. Of course, under promise and over deliver. When the results are back on Tuesday, you’ve got a pleased patient.
Explaining that you had to add in an urgent patient helps. Even if it’s not your fault, it’s still better to apologize. For example, the 78 highway, the left anterior descending artery to our office, has been closed because of a sinkhole this month (not kidding). I’ve been apologizing to a lot of patients saying that all our patients are arriving late, which is putting us behind. As they can envision the linear parking lot that used to be a highway, it helps.
Lastly, as any child can tell you, waiting has to not only be, but to also appear, fair. The only thing worse than waiting for an appointment, or donut, is seeing someone who came in after you get their donut before you do. If you’re pulling both Mohs and cosmetics patients from the same waiting area, then your surgery patients will see a lot of patients come and go while they are sitting. Demarcating one sitting area for Mohs and one for clinics might help. So does ordering ahead. I’d show my daughter how to use the app so we don’t have to wait so long next week, but she’s 2 and I’m quite sure she already knows.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“Papa! Where donut?” asks my 2½ year-old sitting with her legs dangling and hands folded in a bustling Starbucks. We’ve been waiting for 8 minutes and we’ve reached her limit of tolerance. She’s unimpressed by the queued customers who compliment her curly blonde hair, many of whom have come and gone since we’ve been waiting. I agree – how long does it take to pour a kiddie milk and grab a donut? We can both see it in the case right there!
No one likes to wait. Truly, one of the great benefits of the modern world is that wait times are now incredibly short. Many Starbucks customers, unlike my daughter, ordered their drink ahead and waited exactly 0 minutes to get their drink. What about Amazon? I ordered a bird feeder this morning and it’s already hanging in the yard. It’s still daylight. Feel like Himalayan Momo Dumplings tonight? Your food could arrive in 37 minutes. The modern wait standard has been set impossibly high for us.
Yes, for some. We created a whole room just for waiting. Airlines call theirs “The Platinum Executive Lounge.” Ours is “The waiting room.”
Excess waiting is a significant reason why health care gets beat up in reviews. We’re unable to keep up with the new expectations. Waiting is also a significant cause of distress. Many patients report the most difficult part of their cancer diagnosis was the waiting for results, not the treatment. It’s because when under stress, we are hardwired to take action. Binding patients into inaction while they wait is very uncomfortable.
Fortunately, the psychology of waiting is well understood and there are best practices that can help. First, anxiety makes waiting much worse. Conveying confidence and reassuring patients they are in the right place and that everything will be OK makes the wait time feel shorter for them. Uncertainty also compounds their apprehension. If you believe the diagnosis will be melanoma, tell them that at the time of the biopsy and tell them what you expect next. This is better than saying, “Well, that could be cancer. We’ll see.”
Knowing a wait time is also much better than not. Have your staff advise patients on how much longer they can expect before seeing you (telling them they’re next isn’t as effective). Advise that test results should be back by the end of next week. Of course, under promise and over deliver. When the results are back on Tuesday, you’ve got a pleased patient.
Explaining that you had to add in an urgent patient helps. Even if it’s not your fault, it’s still better to apologize. For example, the 78 highway, the left anterior descending artery to our office, has been closed because of a sinkhole this month (not kidding). I’ve been apologizing to a lot of patients saying that all our patients are arriving late, which is putting us behind. As they can envision the linear parking lot that used to be a highway, it helps.
Lastly, as any child can tell you, waiting has to not only be, but to also appear, fair. The only thing worse than waiting for an appointment, or donut, is seeing someone who came in after you get their donut before you do. If you’re pulling both Mohs and cosmetics patients from the same waiting area, then your surgery patients will see a lot of patients come and go while they are sitting. Demarcating one sitting area for Mohs and one for clinics might help. So does ordering ahead. I’d show my daughter how to use the app so we don’t have to wait so long next week, but she’s 2 and I’m quite sure she already knows.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
How to become wise
The only true wisdom is in knowing you know nothing. – Socrates
At what age is one supposed to be wise? I feel like I’m falling behind. I’ve crossed the middle of life and can check the prerequisite experiences: Joy, tragedy, love, adventure, love again. I lived a jetsetter life with an overnight bag always packed. I’ve sported the “Dad AF” tee with a fully loaded dad-pack. I’ve seen the 50 states and had my picture wrapped on a city bus (super-weird when you pull up next to one). Yet, when a moment arrives to pop in pithy advice for a resident or drop a few reassuring lines for a grieving friend, I’m often unable to find the words. If life were a video game, I’ve not earned the wisdom level yet.
Who are the wise men and women in your life? It’s difficult to list them. This is because it’s a complex attribute and hard to explain. It’s also because the wise who walk among us are rare. Wise is more than being brilliant at bullous diseases or knowing how to sleep train a baby. Nor is wise the buddy who purchased $1,000 of Bitcoin in 2010 (although stay close with him, he probably owns a jet). Neither content experts nor lucky friends rise to the appellation. Both experience and empathy.
The ancients considered wisdom to be one of the vital virtues. It was personified in high-profile gods like Apollo and Athena. It’s rare and important enough to be seen as spiritual. It features heavily in the Bible, the Bhagavad Gita, the Meditations of Marcus Aurelius. In some cultures the wise are called elders or sages. In all cultures they are helpful, respected, sought after, appreciated. We need more wise people in this game of life. I want to be one. But there’s no Coursera for it.
To become wise you have to pass through many levels, put in a lot of reps, suffer through many sleepless nights. Like the third molar, also known as the wisdom tooth, it takes years. You also have to emerge stronger and smarter through those experiences. FDR would not have become one of the wisest presidents in history had it not been for his trials, and victories, over polio. Osler missed Cushing syndrome multiple times before he got it right. It seems you have to go to the mountain, like Batman, and fight a few battles to realize your full wisdom potential.
You must also reflect on your experiences and hone your insight. The management sage Peter Drucker would write what he expected to happen after a decision. Then he’d return to it to hone his intuition and judgment.
Lastly, you have to use your powers for good. Using insight to win your NCAA bracket pool isn’t wisdom. Helping a friend whose marriage is falling apart or colleague whose patient is suing them or a resident whose excision hit an arteriole surely is.
I’ve got a ways to go before anyone puts me on their wise friend list. I’m working on it though. Perhaps you will too – we are desperately short-staffed in this area. For now, I can start with writing better condolences.
“Who maintains that it is not a heavy blow? But it is part of being human.” – Seneca
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
The only true wisdom is in knowing you know nothing. – Socrates
At what age is one supposed to be wise? I feel like I’m falling behind. I’ve crossed the middle of life and can check the prerequisite experiences: Joy, tragedy, love, adventure, love again. I lived a jetsetter life with an overnight bag always packed. I’ve sported the “Dad AF” tee with a fully loaded dad-pack. I’ve seen the 50 states and had my picture wrapped on a city bus (super-weird when you pull up next to one). Yet, when a moment arrives to pop in pithy advice for a resident or drop a few reassuring lines for a grieving friend, I’m often unable to find the words. If life were a video game, I’ve not earned the wisdom level yet.
Who are the wise men and women in your life? It’s difficult to list them. This is because it’s a complex attribute and hard to explain. It’s also because the wise who walk among us are rare. Wise is more than being brilliant at bullous diseases or knowing how to sleep train a baby. Nor is wise the buddy who purchased $1,000 of Bitcoin in 2010 (although stay close with him, he probably owns a jet). Neither content experts nor lucky friends rise to the appellation. Both experience and empathy.
The ancients considered wisdom to be one of the vital virtues. It was personified in high-profile gods like Apollo and Athena. It’s rare and important enough to be seen as spiritual. It features heavily in the Bible, the Bhagavad Gita, the Meditations of Marcus Aurelius. In some cultures the wise are called elders or sages. In all cultures they are helpful, respected, sought after, appreciated. We need more wise people in this game of life. I want to be one. But there’s no Coursera for it.
To become wise you have to pass through many levels, put in a lot of reps, suffer through many sleepless nights. Like the third molar, also known as the wisdom tooth, it takes years. You also have to emerge stronger and smarter through those experiences. FDR would not have become one of the wisest presidents in history had it not been for his trials, and victories, over polio. Osler missed Cushing syndrome multiple times before he got it right. It seems you have to go to the mountain, like Batman, and fight a few battles to realize your full wisdom potential.
You must also reflect on your experiences and hone your insight. The management sage Peter Drucker would write what he expected to happen after a decision. Then he’d return to it to hone his intuition and judgment.
Lastly, you have to use your powers for good. Using insight to win your NCAA bracket pool isn’t wisdom. Helping a friend whose marriage is falling apart or colleague whose patient is suing them or a resident whose excision hit an arteriole surely is.
I’ve got a ways to go before anyone puts me on their wise friend list. I’m working on it though. Perhaps you will too – we are desperately short-staffed in this area. For now, I can start with writing better condolences.
“Who maintains that it is not a heavy blow? But it is part of being human.” – Seneca
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
The only true wisdom is in knowing you know nothing. – Socrates
At what age is one supposed to be wise? I feel like I’m falling behind. I’ve crossed the middle of life and can check the prerequisite experiences: Joy, tragedy, love, adventure, love again. I lived a jetsetter life with an overnight bag always packed. I’ve sported the “Dad AF” tee with a fully loaded dad-pack. I’ve seen the 50 states and had my picture wrapped on a city bus (super-weird when you pull up next to one). Yet, when a moment arrives to pop in pithy advice for a resident or drop a few reassuring lines for a grieving friend, I’m often unable to find the words. If life were a video game, I’ve not earned the wisdom level yet.
Who are the wise men and women in your life? It’s difficult to list them. This is because it’s a complex attribute and hard to explain. It’s also because the wise who walk among us are rare. Wise is more than being brilliant at bullous diseases or knowing how to sleep train a baby. Nor is wise the buddy who purchased $1,000 of Bitcoin in 2010 (although stay close with him, he probably owns a jet). Neither content experts nor lucky friends rise to the appellation. Both experience and empathy.
The ancients considered wisdom to be one of the vital virtues. It was personified in high-profile gods like Apollo and Athena. It’s rare and important enough to be seen as spiritual. It features heavily in the Bible, the Bhagavad Gita, the Meditations of Marcus Aurelius. In some cultures the wise are called elders or sages. In all cultures they are helpful, respected, sought after, appreciated. We need more wise people in this game of life. I want to be one. But there’s no Coursera for it.
To become wise you have to pass through many levels, put in a lot of reps, suffer through many sleepless nights. Like the third molar, also known as the wisdom tooth, it takes years. You also have to emerge stronger and smarter through those experiences. FDR would not have become one of the wisest presidents in history had it not been for his trials, and victories, over polio. Osler missed Cushing syndrome multiple times before he got it right. It seems you have to go to the mountain, like Batman, and fight a few battles to realize your full wisdom potential.
You must also reflect on your experiences and hone your insight. The management sage Peter Drucker would write what he expected to happen after a decision. Then he’d return to it to hone his intuition and judgment.
Lastly, you have to use your powers for good. Using insight to win your NCAA bracket pool isn’t wisdom. Helping a friend whose marriage is falling apart or colleague whose patient is suing them or a resident whose excision hit an arteriole surely is.
I’ve got a ways to go before anyone puts me on their wise friend list. I’m working on it though. Perhaps you will too – we are desperately short-staffed in this area. For now, I can start with writing better condolences.
“Who maintains that it is not a heavy blow? But it is part of being human.” – Seneca
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.








