User login
Using seclusion to prevent COVID-19 transmission on inpatient psychiatry units
Mr. T, age 26, presents to the psychiatric emergency department with acutely worsening symptoms of schizophrenia. The treating team decides to admit him to the inpatient psychiatry unit. The patient agrees to admission bloodwork, but adamantly refuses a coronavirus disease 2019 (COVID-19) nasal swab, stating that he does not consent to “having COVID-19 injected into his nose.” His nurse pages the psychiatry resident on call, asking her for seclusion orders to be placed for the patient in order to quarantine him.
This case illustrates a quandary that has arisen during the COVID-19 era. Traditionally, the use of seclusion in inpatient psychiatry wards has been restricted to the management of violent or self-destructive behavior. Most guidelines advise that seclusion should be used only to ensure the immediate physical safety of a patient, staff members, or other patients.1 Using seclusion for other purposes, such as to quarantine patients suspected of having an infectious disease, raises ethical questions.
What is seclusion?
To best understand the questions that arise from the above scenario, a thorough understanding of the terminology used is needed. Although the terms “isolation,” “quarantine,” and “seclusion” are often used interchangeably, each has a distinct definition and unique history.
Isolation in a medical context refers to the practice of isolating people confirmed to have a disease from the general population. The earliest description of medical isolation dates back to the 7th century BC in the Book of Leviticus, which mentions a protocol for separating individuals infected with leprosy from those who are healthy.2
Quarantine hearkens back to the most fatal pandemic recorded in human history, the Black Death. In 1377, on the advice of the city’s chief physician, the Mediterranean seaport of Ragusa passed a law establishing an isolation period for all visitors from plague-endemic lands.2 Initially a 30-day isolation period (a trentino), this was extended to 40 days (a quarantino). Distinct from isolation, quarantine is the practice of limiting movements of apparently healthy individuals who may have been exposed to a disease but do not have a confirmed diagnosis.
Seclusion, a term used most often in psychiatry, is defined as “the involuntary confinement of a patient alone in a room or area from which the patient is physically prevented from leaving.”3 The use of seclusion rooms in psychiatric facilities was originally championed by the 19th century British psychiatrist John Conolly.4 In The Treatment of the Insane without Mechanical Restraints, Conolly argued that a padded seclusion room was far more humane and effective in calming a violent patient than mechanical restraints. After exhausting less restrictive measures, seclusion is one of the most common means of restraining violent patients in inpatient psychiatric facilities.
Why consider seclusion?
The discussion of using seclusion as a means of quarantine has arisen recently due to the COVID-19 pandemic. This infectious disease was first identified in December 2019 in Wuhan, China.5 Since then, it has spread rapidly across the world. As of mid-October 2020, >39 million cases across 189 countries had been reported.6 The primary means by which the virus is spread is through respiratory droplets released from infected individuals through coughing, sneezing, or talking.7 These droplets can remain airborne or fall onto surfaces that become fomites. Transmission is possible before symptoms appear in an infected individual or even from individuals who are asymptomatic.8
Continue to: The typical layout and requirements...
The typical layout and requirements of an inpatient psychiatric ward intensify the risk of COVID-19 transmission.9 Unlike most medical specialty wards, psychiatric wards are set up with a therapeutic milieu where patients have the opportunity to mingle and interact with each other and staff members. Patients are allowed to walk around the unit, spend time in group therapy, eat meals with each other, and have visitation hours. The therapeutic benefit of such a milieu, however, must be weighed against the risks that patients pose to staff members and other patients. While many facilities have restricted some of these activities to limit COVID-19 exposure, the overall risk of transmission is still elevated. Early in course of the pandemic, the virus spread to an inpatient psychiatric ward in South Korea. Although health officials put the ward on lockdown, given the heightened risk of transmission, the virus quickly spread from patient to patient. Out of 103 inpatients, 101 contracted COVID-19.10
To mitigate this risk, many inpatient psychiatric facilities have mandated that all newly admitted patients be tested for COVID-19. By obtaining COVID-19 testing, facilities are better able to risk stratify their patient population and appropriately protect all patients. A dilemma arises, however, when a patient refuses to consent to COVID-19 testing. In such cases, the infectious risk of the patient remains unknown. Given the potentially disastrous consequences of an unchecked COVID-19 infection running rampant in an inpatient ward, some facilities have elected to use seclusion as a means of quarantining the patient.
Is seclusion justifiable?
There are legitimate objections to using seclusion as a means of quarantine. Most guidelines state that the only time seclusion is ethical is when it is used to prevent immediate physical danger, either to the patient or others.11 Involuntary confinement entails considerable restriction of a patient’s rights and thus should be used only after all other options have been exhausted. People opposed to the use of seclusion point out that outside of the hospital, people are not forcibly restrained in order to enforce social distancing,12 so by extension, those who are inside the hospital should not be forced to seclude.
Seclusion also comes with potentially harmful effects. For the 14 days that a patient is in quarantine, they are cut off from most social contact, which is the opposite of the intended purpose of the therapeutic milieu in inpatient psychiatric wards. Several quantitative studies have shown that individuals who are quarantined tend to report a high prevalence of symptoms of psychological distress, including low mood, irritability, depression, stress, anger, and posttraumatic stress disorder.13
Furthermore, there is considerable evidence that a negative test does not definitively rule out a COVID-19 infection. Nasal swabs for COVID-19 have a false-negative rate of 27%.14 In other words, patients on an inpatient psychiatry ward who are free to walk around the unit and interact with others are only probably COVID-19 free, not definitively. This fact throws into question the original justification for seclusion—to protect other patients from COVID-19.
Continue to: Support for using seclusion as quarantine
Support for using seclusion as quarantine
Despite these objections, there are clear arguments in favor of using seclusion as a means of quarantine. First, the danger posed by an unidentified COVID-19 infection to the inpatient psychiatric population is not small. As of mid-October 2020, >217,000 Americans had died of COVID-19.6 Psychiatric patients, especially those who are acutely decompensated and hospitalized, have a heightened risk.15 Those with underlying medical issues are more likely to be seriously affected by an infection. Patients with serious mental illness have higher rates of medical comorbidities16 and premature death.17 The risk of a patient contracting and then dying from COVID-19 is elevated in an inpatient psychiatric ward. Even if a test is not 100% sensitive or specific, the balance of probability it provides is sufficient to make an informed decision about transmission risk.
In choosing to seclude a patient who refuses COVID-19 testing, the treating team must weigh one person’s autonomy against the safety of every other individual on the ward. From a purely utilitarian perspective, the lives of the many outweigh the discomfort of one. Addressing this balance, the American Medical Association (AMA) Code of Ethics states “Although physicians’ primary ethical obligation is to their individual patients, they also have a long-recognized public health responsibility. In the context of infectious disease, this may include the use of quarantine and isolation to reduce the transmission of disease and protect the health of the public. In such situations, physicians have a further responsibility to protect their own health to ensure that they remain able to provide care. These responsibilities potentially conflict with patients’ rights of self-determination and with physicians’ duty to advocate for the best interests of individual patients and to provide care in emergencies.”18
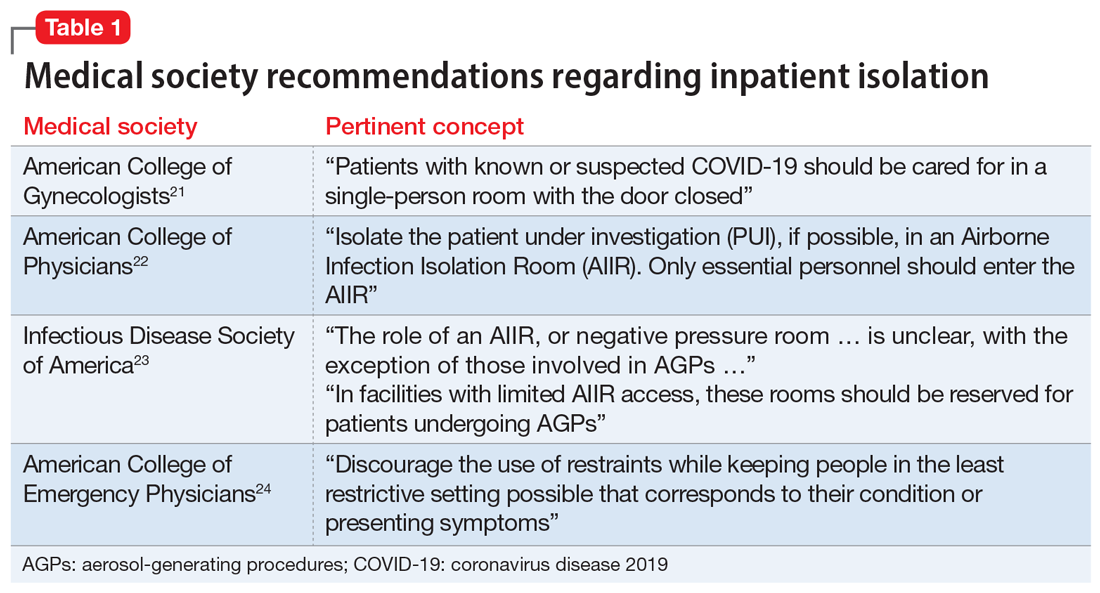
The AMA Code of Ethics further mentions that physicians should “support mandatory quarantine and isolation when a patient fails to adhere voluntarily.” Medical evidence supports both quarantine19 and enacting isolation measures for COVID-19–positive hospitalized patients.20 Table 121-24 summarizes the recommendations of major medical societies regarding isolation on hospital units.
Further, public health officials and law enforcement officials do in fact have the authority25 to enforce quarantine and restrict a citizen’s movement outside a hospital setting. Recent cases have illustrated how this has been enforced, particularly with the use of electronic monitoring units and even criminal sanctions.26,27
It is also important to consider that when used as quarantine, seclusion is not an indefinite action. Current recommendations suggest the longest period of time a patient would need to be in seclusion is 14 days. A patient could potentially reduce this period by agreeing to COVID-19 testing and obtaining a negative test result.
Continue to: Enacting inpatient quarantine
Enacting inpatient quarantine
In Mr. T’s case, the resident physician was asked to make a decision regarding seclusion on the spot. Prudent facilities will set policies and educate clinicians before they need to face this conundrum. The following practical considerations may guide implementation of seclusion as a measure of quarantine on an inpatient psychiatric unit:
- given the risk of asymptomatic carriers, all admitted patients should be tested for COVID-19
- patients who refuse a test should be evaluated by the psychiatrist on duty to determine if the patient has the capacity to make this decision
- if a patient demonstrates capacity to refuse and continues to refuse testing, seclusion orders should then be placed
- the facility should create a protocol to ensure consistent application of seclusion orders.
So that they can make an informed decision, patients should be educated about the risks of not undergoing testing. It is important to correctly frame a seclusion decision to the patient. Explain that seclusion is not a punitive measure, but rather a means of respecting the patient’s right to refuse testing while ensuring other patients’ right to be protected from COVID-19 transmission.
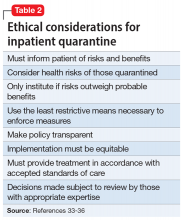
It is crucial to not allow psychiatric care to be diminished because a patient is isolated due to COVID-19. Psychiatrists have legal duties to provide care when a patient is admitted to their unit,28-30 and state laws generally outline patients’ rights while they are hospitalized.31 The use of technology can ensure these duties are fulfilled. Patient rounds and group treatment can be conducted through telehealth.10,32 When in-person interaction is required, caretakers should don proper personal protective equipment and interact with the patient as often as they would if the patient were not in seclusion. Table 233-36 summarizes further ethical considerations when implementing quarantine measures on a psychiatry unit.
The contemporary inpatient unit
The ideal design to optimize care and safety is to create designated COVID-19 psychiatric units. Indeed, the US Substance Abuse and Mental Health Services Administration recommends segregating floors based on infection status where possible.37 This minimizes the risk of transmission to other patients while maintaining the same standards of psychiatric treatment, including milieu and group therapy (which may also require adjustments). Such a unit already has precedent.38 Although designated COVID-19 psychiatric units present clinical and administrative hurdles,39 they may become more commonplace as the number of COVID-19–positive inpatients continues to rise.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has created challenges for inpatient psychiatric facilities. Although seclusion is a serious decision and should not be undertaken lightly, there are clear ethical and practical justifications for using it as a means of quarantine for patients who are COVID-19–positive or refuse testing.
Related Resources
- Askew L, Fisher P, Beazley P. What are adult psychiatric inpatients’ experience of seclusion: a systematic review of qualitative studies. J Psychiatr Ment Health Nurs. 2019; 26(7-8):274-285.
- Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
1. Knox DK, Holloman GH Jr. Use and avoidance of seclusion and restraint: consensus statement of the American Association for Emergency Psychiatry Project BETA Seclusion and Restraint Workgroup. West J Emerg Med. 2012;13(1):35-40.
2. Sehdev PS. The origin of quarantine. Clin Infect Dis. 2002;35(9):1071-1072.
3. 42 CFR § 482.13. Condition of participation: patient’s rights.
4. Colaizzi J. Seclusion & restraint: a historical perspective. J Psychosoc Nurs Ment Health Serv. 2005;43(2):31-37.
5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
6. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). ArcGIS. Johns Hopkins University. https://coronavirus.jhu.edu/map.html. Accessed October 16, 2020.
7. Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11.
8. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406-1407.
9. Li L. Challenges and priorities in responding to COVID-19 in inpatient psychiatry. Psychiatr Serv. 2020;71(6):624-626.
10. Kim MJ. ‘It was a medical disaster’: the psychiatric ward that saw 100 patients diagnosed with new coronavirus. Independent. https://www.independent.co.uk/news/world/asia/coronavirus-south-korea-outbreak-hospital-patients-lockdown-a9367486.html. Published March 1, 2020. Accessed July 12, 2020.
11. Petrini C. Ethical considerations for evaluating the issue of physical restraint in psychiatry. Ann Ist Super Sanita. 2013;49(3):281-285.
12. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed July 12, 2020.
13. Brooks SK, Webster RK, Smith, LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920.
14. Woloshin S, Patel N, Kesselheim AS. False negative tests for SARS-CoV-2 infection—challenges and implications. N Engl J Med. 2020;383(6):e38. doi: 10.1056/NEJMp2015897.
15. Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020;77(9):891-892.
16. Rao S, Raney L, Xiong GL. Reducing medical comorbidity and mortality in severe mental illness. Current Psychiatry. 2015;14(7):14-20.
17. Plana-Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. 2019;394(10211):1827-1835.
18. American Medical Association. Ethical use of quarantine and isolation. Code of Ethics Opinion 8.4. https://www.ama-assn.org/delivering-care/ethics/ethical-use-quarantine-isolation. Published November 14, 2016. Accessed July 12, 2020.
19. Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;4(4):CD013574.
20. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Duration of isolation & precautions for adults. https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Updated August 16, 2020. Accessed August 21, 2020.
21. American College of Gynecologists. Novel coronavirus 2019 (COVID-19). https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019. Updated August 12, 2020. Accessed August 26, 2020.
22. American College of Physicians. COVID-19: an ACP physician’s guide + resources. Chapter 14 of 31. Infection control: advice for physicians. https://assets.acponline.org/coronavirus/scormcontent/#/. Updated September 3, 2020. Accessed September 9, 2020.
23. Infectious Disease Society of America. Infectious Diseases Society of America Guidelines on Infection Prevention in Patients with Suspected or Known COVID-19. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/#toc-9-9. Updated April 20, 2020. Accessed August 26, 2020.
24. American College of Emergency Physicians. Joint Statement for Care of Patients with Behavioral Health Emergencies and Suspected or Confirmed COVID-19. https://www.acep.org/corona/covid-19-field-guide/special-populations/behavioral-health-patients/. Updated June 17, 2020. Accessed August 26, 2020.
25. Centers for Disease Control and Prevention. Quarantine and isolation. Legal authorities. https://www.cdc.gov/quarantine/aboutlawsregulationsquarantineisolation.html. Updated February 24, 2020. Accessed August 31, 2020.
26. Roberts A. Kentucky couple under house arrest after refusing to sign self-quarantine agreement. https://abcnews.go.com/US/kentucky-couple-house-arrest-refusing-sign-quarantine-agreement/story?id=71886479. Published July 20, 2020. Accessed July 24, 2020.
27. Satter R. To keep COVID-19 patients home, some U.S. states weigh house arrest tech. https://www.reuters.com/article/us-health-coronavirus-quarantine-tech/to-keep-covid-19-patients-home-some-us-states-weigh-house-arrest-tech-idUSKBN22J1U8. Published May 7, 2020. Accessed July 24, 2020.
28. Rouse v Cameron, 373, F2d 451 (DC Cir 1966).
29. Wyatt v Stickney, 325 F Supp 781 (MD Ala 1971).
30. Donaldson v O’Connor, 519, F2d 59 (5th Cir 1975).
31. Ohio Revised Code § 5122.290.
32. Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013;170(3):256-262.
33. Bostick NA, Levine MA, Sade RM. Ethical obligations of physicians participating in public health quarantine and isolation measures. Public Health Rep. 2008;123(1):3-8.
34. Upshur RE. Principles for the justification of public health intervention. Can J Public Health. 2002;93(2):101-103.
35. Barbera J, Macintyre A, Gostin L, et al. Large-scale quarantine following biological terrorism in the United States: scientific examination, logistic and legal limits, and possible consequences. JAMA. 2001;286(21):2711-2717.
36. Stanford Encyclopedia of Philosophy. Doctrine of double effect. https://plato.stanford.edu/entries/double-effect/. Revised December 24, 2018. Accessed July 12, 2020.
37. Substance Abuse and Mental Health Services Administration. Covid19: interim considerations for state psychiatric hospitals. https://www.samhsa.gov/sites/default/files/covid19-interim-considerations-for-state-psychiatric-hospitals.pdf. Updated May 8, 2020. Accessed July 24, 2020.
38. Augenstein TM, Pigeon WR, DiGiovanni SK, et al. Creating a novel inpatient psychiatric unit with integrated medical support for patients with COVID-19. N Engl J Med Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0249. Published June 22, 2020. Accessed July 12, 2020.
39. Bojdani E, Rajagopalan A, Chen A, et al. COVID-19 pandemic: impact on psychiatric care in the United States. Psychiatry Research. 2020;289:113069. doi: 10.1016/j.psychres.2020.113069.
Mr. T, age 26, presents to the psychiatric emergency department with acutely worsening symptoms of schizophrenia. The treating team decides to admit him to the inpatient psychiatry unit. The patient agrees to admission bloodwork, but adamantly refuses a coronavirus disease 2019 (COVID-19) nasal swab, stating that he does not consent to “having COVID-19 injected into his nose.” His nurse pages the psychiatry resident on call, asking her for seclusion orders to be placed for the patient in order to quarantine him.
This case illustrates a quandary that has arisen during the COVID-19 era. Traditionally, the use of seclusion in inpatient psychiatry wards has been restricted to the management of violent or self-destructive behavior. Most guidelines advise that seclusion should be used only to ensure the immediate physical safety of a patient, staff members, or other patients.1 Using seclusion for other purposes, such as to quarantine patients suspected of having an infectious disease, raises ethical questions.
What is seclusion?
To best understand the questions that arise from the above scenario, a thorough understanding of the terminology used is needed. Although the terms “isolation,” “quarantine,” and “seclusion” are often used interchangeably, each has a distinct definition and unique history.
Isolation in a medical context refers to the practice of isolating people confirmed to have a disease from the general population. The earliest description of medical isolation dates back to the 7th century BC in the Book of Leviticus, which mentions a protocol for separating individuals infected with leprosy from those who are healthy.2
Quarantine hearkens back to the most fatal pandemic recorded in human history, the Black Death. In 1377, on the advice of the city’s chief physician, the Mediterranean seaport of Ragusa passed a law establishing an isolation period for all visitors from plague-endemic lands.2 Initially a 30-day isolation period (a trentino), this was extended to 40 days (a quarantino). Distinct from isolation, quarantine is the practice of limiting movements of apparently healthy individuals who may have been exposed to a disease but do not have a confirmed diagnosis.
Seclusion, a term used most often in psychiatry, is defined as “the involuntary confinement of a patient alone in a room or area from which the patient is physically prevented from leaving.”3 The use of seclusion rooms in psychiatric facilities was originally championed by the 19th century British psychiatrist John Conolly.4 In The Treatment of the Insane without Mechanical Restraints, Conolly argued that a padded seclusion room was far more humane and effective in calming a violent patient than mechanical restraints. After exhausting less restrictive measures, seclusion is one of the most common means of restraining violent patients in inpatient psychiatric facilities.
Why consider seclusion?
The discussion of using seclusion as a means of quarantine has arisen recently due to the COVID-19 pandemic. This infectious disease was first identified in December 2019 in Wuhan, China.5 Since then, it has spread rapidly across the world. As of mid-October 2020, >39 million cases across 189 countries had been reported.6 The primary means by which the virus is spread is through respiratory droplets released from infected individuals through coughing, sneezing, or talking.7 These droplets can remain airborne or fall onto surfaces that become fomites. Transmission is possible before symptoms appear in an infected individual or even from individuals who are asymptomatic.8
Continue to: The typical layout and requirements...
The typical layout and requirements of an inpatient psychiatric ward intensify the risk of COVID-19 transmission.9 Unlike most medical specialty wards, psychiatric wards are set up with a therapeutic milieu where patients have the opportunity to mingle and interact with each other and staff members. Patients are allowed to walk around the unit, spend time in group therapy, eat meals with each other, and have visitation hours. The therapeutic benefit of such a milieu, however, must be weighed against the risks that patients pose to staff members and other patients. While many facilities have restricted some of these activities to limit COVID-19 exposure, the overall risk of transmission is still elevated. Early in course of the pandemic, the virus spread to an inpatient psychiatric ward in South Korea. Although health officials put the ward on lockdown, given the heightened risk of transmission, the virus quickly spread from patient to patient. Out of 103 inpatients, 101 contracted COVID-19.10
To mitigate this risk, many inpatient psychiatric facilities have mandated that all newly admitted patients be tested for COVID-19. By obtaining COVID-19 testing, facilities are better able to risk stratify their patient population and appropriately protect all patients. A dilemma arises, however, when a patient refuses to consent to COVID-19 testing. In such cases, the infectious risk of the patient remains unknown. Given the potentially disastrous consequences of an unchecked COVID-19 infection running rampant in an inpatient ward, some facilities have elected to use seclusion as a means of quarantining the patient.
Is seclusion justifiable?
There are legitimate objections to using seclusion as a means of quarantine. Most guidelines state that the only time seclusion is ethical is when it is used to prevent immediate physical danger, either to the patient or others.11 Involuntary confinement entails considerable restriction of a patient’s rights and thus should be used only after all other options have been exhausted. People opposed to the use of seclusion point out that outside of the hospital, people are not forcibly restrained in order to enforce social distancing,12 so by extension, those who are inside the hospital should not be forced to seclude.
Seclusion also comes with potentially harmful effects. For the 14 days that a patient is in quarantine, they are cut off from most social contact, which is the opposite of the intended purpose of the therapeutic milieu in inpatient psychiatric wards. Several quantitative studies have shown that individuals who are quarantined tend to report a high prevalence of symptoms of psychological distress, including low mood, irritability, depression, stress, anger, and posttraumatic stress disorder.13
Furthermore, there is considerable evidence that a negative test does not definitively rule out a COVID-19 infection. Nasal swabs for COVID-19 have a false-negative rate of 27%.14 In other words, patients on an inpatient psychiatry ward who are free to walk around the unit and interact with others are only probably COVID-19 free, not definitively. This fact throws into question the original justification for seclusion—to protect other patients from COVID-19.
Continue to: Support for using seclusion as quarantine
Support for using seclusion as quarantine
Despite these objections, there are clear arguments in favor of using seclusion as a means of quarantine. First, the danger posed by an unidentified COVID-19 infection to the inpatient psychiatric population is not small. As of mid-October 2020, >217,000 Americans had died of COVID-19.6 Psychiatric patients, especially those who are acutely decompensated and hospitalized, have a heightened risk.15 Those with underlying medical issues are more likely to be seriously affected by an infection. Patients with serious mental illness have higher rates of medical comorbidities16 and premature death.17 The risk of a patient contracting and then dying from COVID-19 is elevated in an inpatient psychiatric ward. Even if a test is not 100% sensitive or specific, the balance of probability it provides is sufficient to make an informed decision about transmission risk.
In choosing to seclude a patient who refuses COVID-19 testing, the treating team must weigh one person’s autonomy against the safety of every other individual on the ward. From a purely utilitarian perspective, the lives of the many outweigh the discomfort of one. Addressing this balance, the American Medical Association (AMA) Code of Ethics states “Although physicians’ primary ethical obligation is to their individual patients, they also have a long-recognized public health responsibility. In the context of infectious disease, this may include the use of quarantine and isolation to reduce the transmission of disease and protect the health of the public. In such situations, physicians have a further responsibility to protect their own health to ensure that they remain able to provide care. These responsibilities potentially conflict with patients’ rights of self-determination and with physicians’ duty to advocate for the best interests of individual patients and to provide care in emergencies.”18
The AMA Code of Ethics further mentions that physicians should “support mandatory quarantine and isolation when a patient fails to adhere voluntarily.” Medical evidence supports both quarantine19 and enacting isolation measures for COVID-19–positive hospitalized patients.20 Table 121-24 summarizes the recommendations of major medical societies regarding isolation on hospital units.
Further, public health officials and law enforcement officials do in fact have the authority25 to enforce quarantine and restrict a citizen’s movement outside a hospital setting. Recent cases have illustrated how this has been enforced, particularly with the use of electronic monitoring units and even criminal sanctions.26,27
It is also important to consider that when used as quarantine, seclusion is not an indefinite action. Current recommendations suggest the longest period of time a patient would need to be in seclusion is 14 days. A patient could potentially reduce this period by agreeing to COVID-19 testing and obtaining a negative test result.
Continue to: Enacting inpatient quarantine
Enacting inpatient quarantine
In Mr. T’s case, the resident physician was asked to make a decision regarding seclusion on the spot. Prudent facilities will set policies and educate clinicians before they need to face this conundrum. The following practical considerations may guide implementation of seclusion as a measure of quarantine on an inpatient psychiatric unit:
- given the risk of asymptomatic carriers, all admitted patients should be tested for COVID-19
- patients who refuse a test should be evaluated by the psychiatrist on duty to determine if the patient has the capacity to make this decision
- if a patient demonstrates capacity to refuse and continues to refuse testing, seclusion orders should then be placed
- the facility should create a protocol to ensure consistent application of seclusion orders.
So that they can make an informed decision, patients should be educated about the risks of not undergoing testing. It is important to correctly frame a seclusion decision to the patient. Explain that seclusion is not a punitive measure, but rather a means of respecting the patient’s right to refuse testing while ensuring other patients’ right to be protected from COVID-19 transmission.
It is crucial to not allow psychiatric care to be diminished because a patient is isolated due to COVID-19. Psychiatrists have legal duties to provide care when a patient is admitted to their unit,28-30 and state laws generally outline patients’ rights while they are hospitalized.31 The use of technology can ensure these duties are fulfilled. Patient rounds and group treatment can be conducted through telehealth.10,32 When in-person interaction is required, caretakers should don proper personal protective equipment and interact with the patient as often as they would if the patient were not in seclusion. Table 233-36 summarizes further ethical considerations when implementing quarantine measures on a psychiatry unit.
The contemporary inpatient unit
The ideal design to optimize care and safety is to create designated COVID-19 psychiatric units. Indeed, the US Substance Abuse and Mental Health Services Administration recommends segregating floors based on infection status where possible.37 This minimizes the risk of transmission to other patients while maintaining the same standards of psychiatric treatment, including milieu and group therapy (which may also require adjustments). Such a unit already has precedent.38 Although designated COVID-19 psychiatric units present clinical and administrative hurdles,39 they may become more commonplace as the number of COVID-19–positive inpatients continues to rise.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has created challenges for inpatient psychiatric facilities. Although seclusion is a serious decision and should not be undertaken lightly, there are clear ethical and practical justifications for using it as a means of quarantine for patients who are COVID-19–positive or refuse testing.
Related Resources
- Askew L, Fisher P, Beazley P. What are adult psychiatric inpatients’ experience of seclusion: a systematic review of qualitative studies. J Psychiatr Ment Health Nurs. 2019; 26(7-8):274-285.
- Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
Mr. T, age 26, presents to the psychiatric emergency department with acutely worsening symptoms of schizophrenia. The treating team decides to admit him to the inpatient psychiatry unit. The patient agrees to admission bloodwork, but adamantly refuses a coronavirus disease 2019 (COVID-19) nasal swab, stating that he does not consent to “having COVID-19 injected into his nose.” His nurse pages the psychiatry resident on call, asking her for seclusion orders to be placed for the patient in order to quarantine him.
This case illustrates a quandary that has arisen during the COVID-19 era. Traditionally, the use of seclusion in inpatient psychiatry wards has been restricted to the management of violent or self-destructive behavior. Most guidelines advise that seclusion should be used only to ensure the immediate physical safety of a patient, staff members, or other patients.1 Using seclusion for other purposes, such as to quarantine patients suspected of having an infectious disease, raises ethical questions.
What is seclusion?
To best understand the questions that arise from the above scenario, a thorough understanding of the terminology used is needed. Although the terms “isolation,” “quarantine,” and “seclusion” are often used interchangeably, each has a distinct definition and unique history.
Isolation in a medical context refers to the practice of isolating people confirmed to have a disease from the general population. The earliest description of medical isolation dates back to the 7th century BC in the Book of Leviticus, which mentions a protocol for separating individuals infected with leprosy from those who are healthy.2
Quarantine hearkens back to the most fatal pandemic recorded in human history, the Black Death. In 1377, on the advice of the city’s chief physician, the Mediterranean seaport of Ragusa passed a law establishing an isolation period for all visitors from plague-endemic lands.2 Initially a 30-day isolation period (a trentino), this was extended to 40 days (a quarantino). Distinct from isolation, quarantine is the practice of limiting movements of apparently healthy individuals who may have been exposed to a disease but do not have a confirmed diagnosis.
Seclusion, a term used most often in psychiatry, is defined as “the involuntary confinement of a patient alone in a room or area from which the patient is physically prevented from leaving.”3 The use of seclusion rooms in psychiatric facilities was originally championed by the 19th century British psychiatrist John Conolly.4 In The Treatment of the Insane without Mechanical Restraints, Conolly argued that a padded seclusion room was far more humane and effective in calming a violent patient than mechanical restraints. After exhausting less restrictive measures, seclusion is one of the most common means of restraining violent patients in inpatient psychiatric facilities.
Why consider seclusion?
The discussion of using seclusion as a means of quarantine has arisen recently due to the COVID-19 pandemic. This infectious disease was first identified in December 2019 in Wuhan, China.5 Since then, it has spread rapidly across the world. As of mid-October 2020, >39 million cases across 189 countries had been reported.6 The primary means by which the virus is spread is through respiratory droplets released from infected individuals through coughing, sneezing, or talking.7 These droplets can remain airborne or fall onto surfaces that become fomites. Transmission is possible before symptoms appear in an infected individual or even from individuals who are asymptomatic.8
Continue to: The typical layout and requirements...
The typical layout and requirements of an inpatient psychiatric ward intensify the risk of COVID-19 transmission.9 Unlike most medical specialty wards, psychiatric wards are set up with a therapeutic milieu where patients have the opportunity to mingle and interact with each other and staff members. Patients are allowed to walk around the unit, spend time in group therapy, eat meals with each other, and have visitation hours. The therapeutic benefit of such a milieu, however, must be weighed against the risks that patients pose to staff members and other patients. While many facilities have restricted some of these activities to limit COVID-19 exposure, the overall risk of transmission is still elevated. Early in course of the pandemic, the virus spread to an inpatient psychiatric ward in South Korea. Although health officials put the ward on lockdown, given the heightened risk of transmission, the virus quickly spread from patient to patient. Out of 103 inpatients, 101 contracted COVID-19.10
To mitigate this risk, many inpatient psychiatric facilities have mandated that all newly admitted patients be tested for COVID-19. By obtaining COVID-19 testing, facilities are better able to risk stratify their patient population and appropriately protect all patients. A dilemma arises, however, when a patient refuses to consent to COVID-19 testing. In such cases, the infectious risk of the patient remains unknown. Given the potentially disastrous consequences of an unchecked COVID-19 infection running rampant in an inpatient ward, some facilities have elected to use seclusion as a means of quarantining the patient.
Is seclusion justifiable?
There are legitimate objections to using seclusion as a means of quarantine. Most guidelines state that the only time seclusion is ethical is when it is used to prevent immediate physical danger, either to the patient or others.11 Involuntary confinement entails considerable restriction of a patient’s rights and thus should be used only after all other options have been exhausted. People opposed to the use of seclusion point out that outside of the hospital, people are not forcibly restrained in order to enforce social distancing,12 so by extension, those who are inside the hospital should not be forced to seclude.
Seclusion also comes with potentially harmful effects. For the 14 days that a patient is in quarantine, they are cut off from most social contact, which is the opposite of the intended purpose of the therapeutic milieu in inpatient psychiatric wards. Several quantitative studies have shown that individuals who are quarantined tend to report a high prevalence of symptoms of psychological distress, including low mood, irritability, depression, stress, anger, and posttraumatic stress disorder.13
Furthermore, there is considerable evidence that a negative test does not definitively rule out a COVID-19 infection. Nasal swabs for COVID-19 have a false-negative rate of 27%.14 In other words, patients on an inpatient psychiatry ward who are free to walk around the unit and interact with others are only probably COVID-19 free, not definitively. This fact throws into question the original justification for seclusion—to protect other patients from COVID-19.
Continue to: Support for using seclusion as quarantine
Support for using seclusion as quarantine
Despite these objections, there are clear arguments in favor of using seclusion as a means of quarantine. First, the danger posed by an unidentified COVID-19 infection to the inpatient psychiatric population is not small. As of mid-October 2020, >217,000 Americans had died of COVID-19.6 Psychiatric patients, especially those who are acutely decompensated and hospitalized, have a heightened risk.15 Those with underlying medical issues are more likely to be seriously affected by an infection. Patients with serious mental illness have higher rates of medical comorbidities16 and premature death.17 The risk of a patient contracting and then dying from COVID-19 is elevated in an inpatient psychiatric ward. Even if a test is not 100% sensitive or specific, the balance of probability it provides is sufficient to make an informed decision about transmission risk.
In choosing to seclude a patient who refuses COVID-19 testing, the treating team must weigh one person’s autonomy against the safety of every other individual on the ward. From a purely utilitarian perspective, the lives of the many outweigh the discomfort of one. Addressing this balance, the American Medical Association (AMA) Code of Ethics states “Although physicians’ primary ethical obligation is to their individual patients, they also have a long-recognized public health responsibility. In the context of infectious disease, this may include the use of quarantine and isolation to reduce the transmission of disease and protect the health of the public. In such situations, physicians have a further responsibility to protect their own health to ensure that they remain able to provide care. These responsibilities potentially conflict with patients’ rights of self-determination and with physicians’ duty to advocate for the best interests of individual patients and to provide care in emergencies.”18
The AMA Code of Ethics further mentions that physicians should “support mandatory quarantine and isolation when a patient fails to adhere voluntarily.” Medical evidence supports both quarantine19 and enacting isolation measures for COVID-19–positive hospitalized patients.20 Table 121-24 summarizes the recommendations of major medical societies regarding isolation on hospital units.
Further, public health officials and law enforcement officials do in fact have the authority25 to enforce quarantine and restrict a citizen’s movement outside a hospital setting. Recent cases have illustrated how this has been enforced, particularly with the use of electronic monitoring units and even criminal sanctions.26,27
It is also important to consider that when used as quarantine, seclusion is not an indefinite action. Current recommendations suggest the longest period of time a patient would need to be in seclusion is 14 days. A patient could potentially reduce this period by agreeing to COVID-19 testing and obtaining a negative test result.
Continue to: Enacting inpatient quarantine
Enacting inpatient quarantine
In Mr. T’s case, the resident physician was asked to make a decision regarding seclusion on the spot. Prudent facilities will set policies and educate clinicians before they need to face this conundrum. The following practical considerations may guide implementation of seclusion as a measure of quarantine on an inpatient psychiatric unit:
- given the risk of asymptomatic carriers, all admitted patients should be tested for COVID-19
- patients who refuse a test should be evaluated by the psychiatrist on duty to determine if the patient has the capacity to make this decision
- if a patient demonstrates capacity to refuse and continues to refuse testing, seclusion orders should then be placed
- the facility should create a protocol to ensure consistent application of seclusion orders.
So that they can make an informed decision, patients should be educated about the risks of not undergoing testing. It is important to correctly frame a seclusion decision to the patient. Explain that seclusion is not a punitive measure, but rather a means of respecting the patient’s right to refuse testing while ensuring other patients’ right to be protected from COVID-19 transmission.
It is crucial to not allow psychiatric care to be diminished because a patient is isolated due to COVID-19. Psychiatrists have legal duties to provide care when a patient is admitted to their unit,28-30 and state laws generally outline patients’ rights while they are hospitalized.31 The use of technology can ensure these duties are fulfilled. Patient rounds and group treatment can be conducted through telehealth.10,32 When in-person interaction is required, caretakers should don proper personal protective equipment and interact with the patient as often as they would if the patient were not in seclusion. Table 233-36 summarizes further ethical considerations when implementing quarantine measures on a psychiatry unit.
The contemporary inpatient unit
The ideal design to optimize care and safety is to create designated COVID-19 psychiatric units. Indeed, the US Substance Abuse and Mental Health Services Administration recommends segregating floors based on infection status where possible.37 This minimizes the risk of transmission to other patients while maintaining the same standards of psychiatric treatment, including milieu and group therapy (which may also require adjustments). Such a unit already has precedent.38 Although designated COVID-19 psychiatric units present clinical and administrative hurdles,39 they may become more commonplace as the number of COVID-19–positive inpatients continues to rise.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has created challenges for inpatient psychiatric facilities. Although seclusion is a serious decision and should not be undertaken lightly, there are clear ethical and practical justifications for using it as a means of quarantine for patients who are COVID-19–positive or refuse testing.
Related Resources
- Askew L, Fisher P, Beazley P. What are adult psychiatric inpatients’ experience of seclusion: a systematic review of qualitative studies. J Psychiatr Ment Health Nurs. 2019; 26(7-8):274-285.
- Komrad MS. Medical ethics in the time of COVID-19. Current Psychiatry. 2020;19(7):29-32,46.
1. Knox DK, Holloman GH Jr. Use and avoidance of seclusion and restraint: consensus statement of the American Association for Emergency Psychiatry Project BETA Seclusion and Restraint Workgroup. West J Emerg Med. 2012;13(1):35-40.
2. Sehdev PS. The origin of quarantine. Clin Infect Dis. 2002;35(9):1071-1072.
3. 42 CFR § 482.13. Condition of participation: patient’s rights.
4. Colaizzi J. Seclusion & restraint: a historical perspective. J Psychosoc Nurs Ment Health Serv. 2005;43(2):31-37.
5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
6. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). ArcGIS. Johns Hopkins University. https://coronavirus.jhu.edu/map.html. Accessed October 16, 2020.
7. Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11.
8. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406-1407.
9. Li L. Challenges and priorities in responding to COVID-19 in inpatient psychiatry. Psychiatr Serv. 2020;71(6):624-626.
10. Kim MJ. ‘It was a medical disaster’: the psychiatric ward that saw 100 patients diagnosed with new coronavirus. Independent. https://www.independent.co.uk/news/world/asia/coronavirus-south-korea-outbreak-hospital-patients-lockdown-a9367486.html. Published March 1, 2020. Accessed July 12, 2020.
11. Petrini C. Ethical considerations for evaluating the issue of physical restraint in psychiatry. Ann Ist Super Sanita. 2013;49(3):281-285.
12. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed July 12, 2020.
13. Brooks SK, Webster RK, Smith, LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920.
14. Woloshin S, Patel N, Kesselheim AS. False negative tests for SARS-CoV-2 infection—challenges and implications. N Engl J Med. 2020;383(6):e38. doi: 10.1056/NEJMp2015897.
15. Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020;77(9):891-892.
16. Rao S, Raney L, Xiong GL. Reducing medical comorbidity and mortality in severe mental illness. Current Psychiatry. 2015;14(7):14-20.
17. Plana-Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. 2019;394(10211):1827-1835.
18. American Medical Association. Ethical use of quarantine and isolation. Code of Ethics Opinion 8.4. https://www.ama-assn.org/delivering-care/ethics/ethical-use-quarantine-isolation. Published November 14, 2016. Accessed July 12, 2020.
19. Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;4(4):CD013574.
20. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Duration of isolation & precautions for adults. https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Updated August 16, 2020. Accessed August 21, 2020.
21. American College of Gynecologists. Novel coronavirus 2019 (COVID-19). https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019. Updated August 12, 2020. Accessed August 26, 2020.
22. American College of Physicians. COVID-19: an ACP physician’s guide + resources. Chapter 14 of 31. Infection control: advice for physicians. https://assets.acponline.org/coronavirus/scormcontent/#/. Updated September 3, 2020. Accessed September 9, 2020.
23. Infectious Disease Society of America. Infectious Diseases Society of America Guidelines on Infection Prevention in Patients with Suspected or Known COVID-19. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/#toc-9-9. Updated April 20, 2020. Accessed August 26, 2020.
24. American College of Emergency Physicians. Joint Statement for Care of Patients with Behavioral Health Emergencies and Suspected or Confirmed COVID-19. https://www.acep.org/corona/covid-19-field-guide/special-populations/behavioral-health-patients/. Updated June 17, 2020. Accessed August 26, 2020.
25. Centers for Disease Control and Prevention. Quarantine and isolation. Legal authorities. https://www.cdc.gov/quarantine/aboutlawsregulationsquarantineisolation.html. Updated February 24, 2020. Accessed August 31, 2020.
26. Roberts A. Kentucky couple under house arrest after refusing to sign self-quarantine agreement. https://abcnews.go.com/US/kentucky-couple-house-arrest-refusing-sign-quarantine-agreement/story?id=71886479. Published July 20, 2020. Accessed July 24, 2020.
27. Satter R. To keep COVID-19 patients home, some U.S. states weigh house arrest tech. https://www.reuters.com/article/us-health-coronavirus-quarantine-tech/to-keep-covid-19-patients-home-some-us-states-weigh-house-arrest-tech-idUSKBN22J1U8. Published May 7, 2020. Accessed July 24, 2020.
28. Rouse v Cameron, 373, F2d 451 (DC Cir 1966).
29. Wyatt v Stickney, 325 F Supp 781 (MD Ala 1971).
30. Donaldson v O’Connor, 519, F2d 59 (5th Cir 1975).
31. Ohio Revised Code § 5122.290.
32. Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013;170(3):256-262.
33. Bostick NA, Levine MA, Sade RM. Ethical obligations of physicians participating in public health quarantine and isolation measures. Public Health Rep. 2008;123(1):3-8.
34. Upshur RE. Principles for the justification of public health intervention. Can J Public Health. 2002;93(2):101-103.
35. Barbera J, Macintyre A, Gostin L, et al. Large-scale quarantine following biological terrorism in the United States: scientific examination, logistic and legal limits, and possible consequences. JAMA. 2001;286(21):2711-2717.
36. Stanford Encyclopedia of Philosophy. Doctrine of double effect. https://plato.stanford.edu/entries/double-effect/. Revised December 24, 2018. Accessed July 12, 2020.
37. Substance Abuse and Mental Health Services Administration. Covid19: interim considerations for state psychiatric hospitals. https://www.samhsa.gov/sites/default/files/covid19-interim-considerations-for-state-psychiatric-hospitals.pdf. Updated May 8, 2020. Accessed July 24, 2020.
38. Augenstein TM, Pigeon WR, DiGiovanni SK, et al. Creating a novel inpatient psychiatric unit with integrated medical support for patients with COVID-19. N Engl J Med Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0249. Published June 22, 2020. Accessed July 12, 2020.
39. Bojdani E, Rajagopalan A, Chen A, et al. COVID-19 pandemic: impact on psychiatric care in the United States. Psychiatry Research. 2020;289:113069. doi: 10.1016/j.psychres.2020.113069.
1. Knox DK, Holloman GH Jr. Use and avoidance of seclusion and restraint: consensus statement of the American Association for Emergency Psychiatry Project BETA Seclusion and Restraint Workgroup. West J Emerg Med. 2012;13(1):35-40.
2. Sehdev PS. The origin of quarantine. Clin Infect Dis. 2002;35(9):1071-1072.
3. 42 CFR § 482.13. Condition of participation: patient’s rights.
4. Colaizzi J. Seclusion & restraint: a historical perspective. J Psychosoc Nurs Ment Health Serv. 2005;43(2):31-37.
5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
6. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). ArcGIS. Johns Hopkins University. https://coronavirus.jhu.edu/map.html. Accessed October 16, 2020.
7. Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11.
8. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406-1407.
9. Li L. Challenges and priorities in responding to COVID-19 in inpatient psychiatry. Psychiatr Serv. 2020;71(6):624-626.
10. Kim MJ. ‘It was a medical disaster’: the psychiatric ward that saw 100 patients diagnosed with new coronavirus. Independent. https://www.independent.co.uk/news/world/asia/coronavirus-south-korea-outbreak-hospital-patients-lockdown-a9367486.html. Published March 1, 2020. Accessed July 12, 2020.
11. Petrini C. Ethical considerations for evaluating the issue of physical restraint in psychiatry. Ann Ist Super Sanita. 2013;49(3):281-285.
12. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed July 12, 2020.
13. Brooks SK, Webster RK, Smith, LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912-920.
14. Woloshin S, Patel N, Kesselheim AS. False negative tests for SARS-CoV-2 infection—challenges and implications. N Engl J Med. 2020;383(6):e38. doi: 10.1056/NEJMp2015897.
15. Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020;77(9):891-892.
16. Rao S, Raney L, Xiong GL. Reducing medical comorbidity and mortality in severe mental illness. Current Psychiatry. 2015;14(7):14-20.
17. Plana-Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. 2019;394(10211):1827-1835.
18. American Medical Association. Ethical use of quarantine and isolation. Code of Ethics Opinion 8.4. https://www.ama-assn.org/delivering-care/ethics/ethical-use-quarantine-isolation. Published November 14, 2016. Accessed July 12, 2020.
19. Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;4(4):CD013574.
20. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Duration of isolation & precautions for adults. https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Updated August 16, 2020. Accessed August 21, 2020.
21. American College of Gynecologists. Novel coronavirus 2019 (COVID-19). https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019. Updated August 12, 2020. Accessed August 26, 2020.
22. American College of Physicians. COVID-19: an ACP physician’s guide + resources. Chapter 14 of 31. Infection control: advice for physicians. https://assets.acponline.org/coronavirus/scormcontent/#/. Updated September 3, 2020. Accessed September 9, 2020.
23. Infectious Disease Society of America. Infectious Diseases Society of America Guidelines on Infection Prevention in Patients with Suspected or Known COVID-19. https://www.idsociety.org/practice-guideline/covid-19-guideline-infection-prevention/#toc-9-9. Updated April 20, 2020. Accessed August 26, 2020.
24. American College of Emergency Physicians. Joint Statement for Care of Patients with Behavioral Health Emergencies and Suspected or Confirmed COVID-19. https://www.acep.org/corona/covid-19-field-guide/special-populations/behavioral-health-patients/. Updated June 17, 2020. Accessed August 26, 2020.
25. Centers for Disease Control and Prevention. Quarantine and isolation. Legal authorities. https://www.cdc.gov/quarantine/aboutlawsregulationsquarantineisolation.html. Updated February 24, 2020. Accessed August 31, 2020.
26. Roberts A. Kentucky couple under house arrest after refusing to sign self-quarantine agreement. https://abcnews.go.com/US/kentucky-couple-house-arrest-refusing-sign-quarantine-agreement/story?id=71886479. Published July 20, 2020. Accessed July 24, 2020.
27. Satter R. To keep COVID-19 patients home, some U.S. states weigh house arrest tech. https://www.reuters.com/article/us-health-coronavirus-quarantine-tech/to-keep-covid-19-patients-home-some-us-states-weigh-house-arrest-tech-idUSKBN22J1U8. Published May 7, 2020. Accessed July 24, 2020.
28. Rouse v Cameron, 373, F2d 451 (DC Cir 1966).
29. Wyatt v Stickney, 325 F Supp 781 (MD Ala 1971).
30. Donaldson v O’Connor, 519, F2d 59 (5th Cir 1975).
31. Ohio Revised Code § 5122.290.
32. Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013;170(3):256-262.
33. Bostick NA, Levine MA, Sade RM. Ethical obligations of physicians participating in public health quarantine and isolation measures. Public Health Rep. 2008;123(1):3-8.
34. Upshur RE. Principles for the justification of public health intervention. Can J Public Health. 2002;93(2):101-103.
35. Barbera J, Macintyre A, Gostin L, et al. Large-scale quarantine following biological terrorism in the United States: scientific examination, logistic and legal limits, and possible consequences. JAMA. 2001;286(21):2711-2717.
36. Stanford Encyclopedia of Philosophy. Doctrine of double effect. https://plato.stanford.edu/entries/double-effect/. Revised December 24, 2018. Accessed July 12, 2020.
37. Substance Abuse and Mental Health Services Administration. Covid19: interim considerations for state psychiatric hospitals. https://www.samhsa.gov/sites/default/files/covid19-interim-considerations-for-state-psychiatric-hospitals.pdf. Updated May 8, 2020. Accessed July 24, 2020.
38. Augenstein TM, Pigeon WR, DiGiovanni SK, et al. Creating a novel inpatient psychiatric unit with integrated medical support for patients with COVID-19. N Engl J Med Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0249. Published June 22, 2020. Accessed July 12, 2020.
39. Bojdani E, Rajagopalan A, Chen A, et al. COVID-19 pandemic: impact on psychiatric care in the United States. Psychiatry Research. 2020;289:113069. doi: 10.1016/j.psychres.2020.113069.
Legal concerns after a patient suicide
Most psychiatrists will care for at least one patient who dies by suicide. Many clinicians consider this to be one of the most stressful and formative events of their careers, prompting strong emotions, logistical questions, and legal concerns. Because the aftermath of a patient suicide can be difficult, we offer guidance on how to cope with such events, and specifically how to address the legal concerns.
Attend to self-care. “At a cardiac arrest, the first procedure is to take your own pulse.” This advice, from Samuel Shem’s The House of God, highlights the importance of self-awareness during highly stressful events.1 When facing the aftermath of a patient suicide, be sure to attend to your own needs, such as eating, staying hydrated, and getting enough sleep. Identify and reach out to your support systems, such as friends and family. Your colleagues can be a source of support, both formally or informally. Reaching out to other psychiatrists, who likely have their own experience with patient suicide, can help process the event. A support group consisting of other psychiatrists also may be beneficial. Finally, avoid blaming yourself. Although you might perceive your patient’s suicide as a personal failing, suicide is notoriously difficult to predict and an unfortunate reality of working in this specialty.
Report the event. Follow your institution’s guidelines for reporting adverse events. You may be required to inform your supervisor, the risk management department, legal services, your malpractice provider, and/or the police. Your risk management department and malpractice provider may have their own regulations and recommendations.
Review the case. Institutions often have established processes for reviewing adverse events and, if applicable, suggesting constructive feedback or general quality improvements. A review process may provide an opportunity to look for potential negligence that could be an issue if there is a malpractice suit. Ideally, such processes are constructive and a time for reflection, rather than punitive or blaming. Trainees may find their supervisors’ presence and guidance to be particularly helpful during this review process.
Assess malpractice risk. Although psychiatrists have a relatively low risk of being sued for malpractice, many lawsuits against psychiatrists occur after a completed patient suicide.2 In a successful malpractice suit, the plaintiff needs to establish all 4 “Ds” of medical malpractice:
1) Duty, or an established physician–patient relationship
2) Damages from an adverse event
3) Dereliction of duty (negligence)
4) Direct causality between the deviation and the damages.
In the event of a patient suicide, both a doctor–patient relationship (duty) and an adverse outcome (damages) exist.3 Establishing dereliction of duty and direct causality rests on the plaintiff to prove. Good documentation can serve as evidence against accusations of negligence.3
Typically, a patient’s medical record will be used as evidence in a malpractice suit. After a suicide, do not alter this record, such as by editing your past assessments of the patient. If an addendum must be made, such as to document a conversation with suicide survivors (family and friends of the deceased), be sure to label it as such with the current date. An addendum should contain only facts; avoid adding information that attempts to explain your patient’s suicide, justifying or apologizing for past treatment decisions, or otherwise editorializing.
Continue to: Consider reaching out to suicide survivors
Consider reaching out to suicide survivors. The Health Insurance Portability and Accountability Act permits clinicians to use their best judgment when identifying individuals to contact and deciding what information to share after a patient’s death.4 Some states and practice settings have stricter confidentiality laws. Consider seeking legal counsel before interacting with suicide survivors.
Suicide survivors may experience feelings such as guilt, shame, and anger, and these feelings may lead suicide survivors to file a malpractice suit.3 Speaking with suicide survivors can help to address these feelings and potentially decrease the likelihood of them pursuing a malpractice suit. In addition, suicide survivors are at high risk for developing mental health issues, including suicidality. Contacting them can be an opportunity to encourage them to seek mental health treatment. It is important to clarify that any recommendations you provide in such situations do not constitute a doctor–patient relationship.
Should you offer an apology? Consider seeking legal counsel if you wish to apologize. Some states have “apology laws” that render a clinician’s apologetic statements inadmissible if a malpractice suit should occur.5 These laws might include empathic statements (“I’m sorry for your loss”) or disclosures of error (“I’m sorry for causing your loss”).5 It is unclear whether these laws affect the likelihood and/or outcome of malpractice suits.5
Focus on empathy. Experiencing a patient suicide can be one of the most challenging events in a psychiatrist’s career. Empathy is crucial, both towards the suicide survivors and to oneself.
1. Shem S. The House of God. New York, NY: Berkley Books; 2010.
2. Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA Intern Med. 2017;177(5):710-719.
3. Gutheil TG, Appelbaum PS. Clinical handbook of psychiatry and the law, 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2000.
4. Office of Civil Rights. How can a covered entity determine if a person is a family member prior to an individual’s death. US Department of Health and Human Services. https://www.hhs.gov/hipaa/for-professionals/faq/1505/how-can-a-covered-entity-determine-whether-a-person-is-a-family-member/index.html. Accessed September 9, 2020.
5. McMichael BJ, Van Horn RL, Viscusi WK. “Sorry” is never enough: how state apology laws fail to reduce medical malpractice liability risk. Stanford Law Rev. 2019;71(2):341-409.
Most psychiatrists will care for at least one patient who dies by suicide. Many clinicians consider this to be one of the most stressful and formative events of their careers, prompting strong emotions, logistical questions, and legal concerns. Because the aftermath of a patient suicide can be difficult, we offer guidance on how to cope with such events, and specifically how to address the legal concerns.
Attend to self-care. “At a cardiac arrest, the first procedure is to take your own pulse.” This advice, from Samuel Shem’s The House of God, highlights the importance of self-awareness during highly stressful events.1 When facing the aftermath of a patient suicide, be sure to attend to your own needs, such as eating, staying hydrated, and getting enough sleep. Identify and reach out to your support systems, such as friends and family. Your colleagues can be a source of support, both formally or informally. Reaching out to other psychiatrists, who likely have their own experience with patient suicide, can help process the event. A support group consisting of other psychiatrists also may be beneficial. Finally, avoid blaming yourself. Although you might perceive your patient’s suicide as a personal failing, suicide is notoriously difficult to predict and an unfortunate reality of working in this specialty.
Report the event. Follow your institution’s guidelines for reporting adverse events. You may be required to inform your supervisor, the risk management department, legal services, your malpractice provider, and/or the police. Your risk management department and malpractice provider may have their own regulations and recommendations.
Review the case. Institutions often have established processes for reviewing adverse events and, if applicable, suggesting constructive feedback or general quality improvements. A review process may provide an opportunity to look for potential negligence that could be an issue if there is a malpractice suit. Ideally, such processes are constructive and a time for reflection, rather than punitive or blaming. Trainees may find their supervisors’ presence and guidance to be particularly helpful during this review process.
Assess malpractice risk. Although psychiatrists have a relatively low risk of being sued for malpractice, many lawsuits against psychiatrists occur after a completed patient suicide.2 In a successful malpractice suit, the plaintiff needs to establish all 4 “Ds” of medical malpractice:
1) Duty, or an established physician–patient relationship
2) Damages from an adverse event
3) Dereliction of duty (negligence)
4) Direct causality between the deviation and the damages.
In the event of a patient suicide, both a doctor–patient relationship (duty) and an adverse outcome (damages) exist.3 Establishing dereliction of duty and direct causality rests on the plaintiff to prove. Good documentation can serve as evidence against accusations of negligence.3
Typically, a patient’s medical record will be used as evidence in a malpractice suit. After a suicide, do not alter this record, such as by editing your past assessments of the patient. If an addendum must be made, such as to document a conversation with suicide survivors (family and friends of the deceased), be sure to label it as such with the current date. An addendum should contain only facts; avoid adding information that attempts to explain your patient’s suicide, justifying or apologizing for past treatment decisions, or otherwise editorializing.
Continue to: Consider reaching out to suicide survivors
Consider reaching out to suicide survivors. The Health Insurance Portability and Accountability Act permits clinicians to use their best judgment when identifying individuals to contact and deciding what information to share after a patient’s death.4 Some states and practice settings have stricter confidentiality laws. Consider seeking legal counsel before interacting with suicide survivors.
Suicide survivors may experience feelings such as guilt, shame, and anger, and these feelings may lead suicide survivors to file a malpractice suit.3 Speaking with suicide survivors can help to address these feelings and potentially decrease the likelihood of them pursuing a malpractice suit. In addition, suicide survivors are at high risk for developing mental health issues, including suicidality. Contacting them can be an opportunity to encourage them to seek mental health treatment. It is important to clarify that any recommendations you provide in such situations do not constitute a doctor–patient relationship.
Should you offer an apology? Consider seeking legal counsel if you wish to apologize. Some states have “apology laws” that render a clinician’s apologetic statements inadmissible if a malpractice suit should occur.5 These laws might include empathic statements (“I’m sorry for your loss”) or disclosures of error (“I’m sorry for causing your loss”).5 It is unclear whether these laws affect the likelihood and/or outcome of malpractice suits.5
Focus on empathy. Experiencing a patient suicide can be one of the most challenging events in a psychiatrist’s career. Empathy is crucial, both towards the suicide survivors and to oneself.
Most psychiatrists will care for at least one patient who dies by suicide. Many clinicians consider this to be one of the most stressful and formative events of their careers, prompting strong emotions, logistical questions, and legal concerns. Because the aftermath of a patient suicide can be difficult, we offer guidance on how to cope with such events, and specifically how to address the legal concerns.
Attend to self-care. “At a cardiac arrest, the first procedure is to take your own pulse.” This advice, from Samuel Shem’s The House of God, highlights the importance of self-awareness during highly stressful events.1 When facing the aftermath of a patient suicide, be sure to attend to your own needs, such as eating, staying hydrated, and getting enough sleep. Identify and reach out to your support systems, such as friends and family. Your colleagues can be a source of support, both formally or informally. Reaching out to other psychiatrists, who likely have their own experience with patient suicide, can help process the event. A support group consisting of other psychiatrists also may be beneficial. Finally, avoid blaming yourself. Although you might perceive your patient’s suicide as a personal failing, suicide is notoriously difficult to predict and an unfortunate reality of working in this specialty.
Report the event. Follow your institution’s guidelines for reporting adverse events. You may be required to inform your supervisor, the risk management department, legal services, your malpractice provider, and/or the police. Your risk management department and malpractice provider may have their own regulations and recommendations.
Review the case. Institutions often have established processes for reviewing adverse events and, if applicable, suggesting constructive feedback or general quality improvements. A review process may provide an opportunity to look for potential negligence that could be an issue if there is a malpractice suit. Ideally, such processes are constructive and a time for reflection, rather than punitive or blaming. Trainees may find their supervisors’ presence and guidance to be particularly helpful during this review process.
Assess malpractice risk. Although psychiatrists have a relatively low risk of being sued for malpractice, many lawsuits against psychiatrists occur after a completed patient suicide.2 In a successful malpractice suit, the plaintiff needs to establish all 4 “Ds” of medical malpractice:
1) Duty, or an established physician–patient relationship
2) Damages from an adverse event
3) Dereliction of duty (negligence)
4) Direct causality between the deviation and the damages.
In the event of a patient suicide, both a doctor–patient relationship (duty) and an adverse outcome (damages) exist.3 Establishing dereliction of duty and direct causality rests on the plaintiff to prove. Good documentation can serve as evidence against accusations of negligence.3
Typically, a patient’s medical record will be used as evidence in a malpractice suit. After a suicide, do not alter this record, such as by editing your past assessments of the patient. If an addendum must be made, such as to document a conversation with suicide survivors (family and friends of the deceased), be sure to label it as such with the current date. An addendum should contain only facts; avoid adding information that attempts to explain your patient’s suicide, justifying or apologizing for past treatment decisions, or otherwise editorializing.
Continue to: Consider reaching out to suicide survivors
Consider reaching out to suicide survivors. The Health Insurance Portability and Accountability Act permits clinicians to use their best judgment when identifying individuals to contact and deciding what information to share after a patient’s death.4 Some states and practice settings have stricter confidentiality laws. Consider seeking legal counsel before interacting with suicide survivors.
Suicide survivors may experience feelings such as guilt, shame, and anger, and these feelings may lead suicide survivors to file a malpractice suit.3 Speaking with suicide survivors can help to address these feelings and potentially decrease the likelihood of them pursuing a malpractice suit. In addition, suicide survivors are at high risk for developing mental health issues, including suicidality. Contacting them can be an opportunity to encourage them to seek mental health treatment. It is important to clarify that any recommendations you provide in such situations do not constitute a doctor–patient relationship.
Should you offer an apology? Consider seeking legal counsel if you wish to apologize. Some states have “apology laws” that render a clinician’s apologetic statements inadmissible if a malpractice suit should occur.5 These laws might include empathic statements (“I’m sorry for your loss”) or disclosures of error (“I’m sorry for causing your loss”).5 It is unclear whether these laws affect the likelihood and/or outcome of malpractice suits.5
Focus on empathy. Experiencing a patient suicide can be one of the most challenging events in a psychiatrist’s career. Empathy is crucial, both towards the suicide survivors and to oneself.
1. Shem S. The House of God. New York, NY: Berkley Books; 2010.
2. Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA Intern Med. 2017;177(5):710-719.
3. Gutheil TG, Appelbaum PS. Clinical handbook of psychiatry and the law, 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2000.
4. Office of Civil Rights. How can a covered entity determine if a person is a family member prior to an individual’s death. US Department of Health and Human Services. https://www.hhs.gov/hipaa/for-professionals/faq/1505/how-can-a-covered-entity-determine-whether-a-person-is-a-family-member/index.html. Accessed September 9, 2020.
5. McMichael BJ, Van Horn RL, Viscusi WK. “Sorry” is never enough: how state apology laws fail to reduce medical malpractice liability risk. Stanford Law Rev. 2019;71(2):341-409.
1. Shem S. The House of God. New York, NY: Berkley Books; 2010.
2. Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA Intern Med. 2017;177(5):710-719.
3. Gutheil TG, Appelbaum PS. Clinical handbook of psychiatry and the law, 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2000.
4. Office of Civil Rights. How can a covered entity determine if a person is a family member prior to an individual’s death. US Department of Health and Human Services. https://www.hhs.gov/hipaa/for-professionals/faq/1505/how-can-a-covered-entity-determine-whether-a-person-is-a-family-member/index.html. Accessed September 9, 2020.
5. McMichael BJ, Van Horn RL, Viscusi WK. “Sorry” is never enough: how state apology laws fail to reduce medical malpractice liability risk. Stanford Law Rev. 2019;71(2):341-409.
Off-label prescribing: How to limit your liability
The FDA defines “off-label” prescribing as prescribing an FDA-approved medication for an unapproved use, such as for an unapproved clinical indication, for a higher-than-approved dose, or for a patient who is not part of the FDA-approved population (eg, children or geriatric patients).1 Off-label prescribing is common in psychiatry; approximately 13% of psychiatry patients are prescribed off-label psychotropic medications.2 The American Psychiatric Association strongly supports “the autonomous clinical decision-making authority of a physician” and “a physician’s lawful use of an FDA-approved drug product or medical device for an off-label indication when such use is based upon sound scientific evidence in conjunction with sound medical judgment.”3 Because many psychiatric diagnoses have no FDA-approved medications, off-label prescribing often may be a psychiatrist’s only pharmacologic option.
Unfortunately, off-label prescribing can increase a psychiatrist’s risk for liability when treatment falls short of patients’ expectations, or when patients allege that they were injured by the use of an off-label medication. Off-label prescribing does not automatically lead to losing a malpractice suit because the FDA states that physicians can prescribe approved medications for any scientifically supported use, including off-label.1 Medical malpractice lawsuits alleging negligence in prescribing practices, such as off-label prescribing, typically include allegations against the psychiatrist for failure to4:
- adequately assess the patient
- consult the patient’s medical records
- obtain informed consent from the patient
- appropriately prescribe a medication for the clinical indication, dosage, patient’s age, etc.
- monitor for adverse effects and therapeutic effectiveness.
Steps to minimize your risk
When prescribing a medication off-label, the following approaches can help reduce your liability risk:
Conduct a comprehensive clinical assessment. This should include requesting and reviewing your patient’s medical records.
Explain your motivation. Explain to your patient how prescribing an off-label medication can directly benefit him/her. Make it clear that you are not conducting experimental research by prescribing off-label because some patients might perceive this as a covert form of research.
Know the medications you prescribe. Although this sounds obvious, psychiatrists should thoroughly understand how each medication they prescribe is likely to clinically affect their patient. This information is available from many sources, including the FDA’s medication information sheets and the manufacturer’s medication package inserts. If possible, make sure that your off-label prescribing is supported by reputable, peer-reviewed literature.
Obtain informed consent. Tell your patient that the medication you are recommending is being prescribed off-label. Discuss the medication’s risks, benefits, adverse effects, associated “black-box” warnings, off-label uses, and alternatives to the off-label medication.4 Allow time for the patient to ask questions about these treatments.
Continue to: Document all steps
Document all steps. There is an adage in medicine that “If it’s not written, it wasn’t done.” To help reduce your liability risk when prescribing off-label, be sure to document the following4:
- your clinical assessment
- information you gleaned from the patient’s medical records
- your review of information regarding both therapeutic and adverse effects of the medication you want to prescribe
- your discussion of informed consent, including documentation that the patient is aware that the medication is being prescribed off-label
- your clinical rationale for why the off-label medication is in the patient’s best interest.
Also, document the steps you take to monitor for adverse events and therapeutic effectiveness.4 Overall, the goal of documentation should be to support the adequate continuing care of our patients.
1. US Food and Drug Administration. Understanding unapproved use of approved drugs “off label.” https://www.fda.gov/patients/learn-about-expanded-access-and-other-treatment-options/understanding-unapproved-use-approved-drugs-label. Updated February 5, 2018. Accessed August 6, 2020.
2. Vijay A, Becker JE, Ross JS. Patterns and predictors of off-label prescription of psychiatric drugs. PLoS One. 2018;13(7):e0198363. doi: 10.1371/journal.pone.0198363.
3. McLeer S, Mawhinney J; Council on Healthcare Systems and Financing. Position statement on off-label treatments. American Psychiatric Association. https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-2016-Off-Label-Treatment.pdf. Published July 2016. Accessed August 6, 2020.
4. Funicelli A. What to consider when prescribing off-label. Psychiatric News. 2019;54(14):12.
The FDA defines “off-label” prescribing as prescribing an FDA-approved medication for an unapproved use, such as for an unapproved clinical indication, for a higher-than-approved dose, or for a patient who is not part of the FDA-approved population (eg, children or geriatric patients).1 Off-label prescribing is common in psychiatry; approximately 13% of psychiatry patients are prescribed off-label psychotropic medications.2 The American Psychiatric Association strongly supports “the autonomous clinical decision-making authority of a physician” and “a physician’s lawful use of an FDA-approved drug product or medical device for an off-label indication when such use is based upon sound scientific evidence in conjunction with sound medical judgment.”3 Because many psychiatric diagnoses have no FDA-approved medications, off-label prescribing often may be a psychiatrist’s only pharmacologic option.
Unfortunately, off-label prescribing can increase a psychiatrist’s risk for liability when treatment falls short of patients’ expectations, or when patients allege that they were injured by the use of an off-label medication. Off-label prescribing does not automatically lead to losing a malpractice suit because the FDA states that physicians can prescribe approved medications for any scientifically supported use, including off-label.1 Medical malpractice lawsuits alleging negligence in prescribing practices, such as off-label prescribing, typically include allegations against the psychiatrist for failure to4:
- adequately assess the patient
- consult the patient’s medical records
- obtain informed consent from the patient
- appropriately prescribe a medication for the clinical indication, dosage, patient’s age, etc.
- monitor for adverse effects and therapeutic effectiveness.
Steps to minimize your risk
When prescribing a medication off-label, the following approaches can help reduce your liability risk:
Conduct a comprehensive clinical assessment. This should include requesting and reviewing your patient’s medical records.
Explain your motivation. Explain to your patient how prescribing an off-label medication can directly benefit him/her. Make it clear that you are not conducting experimental research by prescribing off-label because some patients might perceive this as a covert form of research.
Know the medications you prescribe. Although this sounds obvious, psychiatrists should thoroughly understand how each medication they prescribe is likely to clinically affect their patient. This information is available from many sources, including the FDA’s medication information sheets and the manufacturer’s medication package inserts. If possible, make sure that your off-label prescribing is supported by reputable, peer-reviewed literature.
Obtain informed consent. Tell your patient that the medication you are recommending is being prescribed off-label. Discuss the medication’s risks, benefits, adverse effects, associated “black-box” warnings, off-label uses, and alternatives to the off-label medication.4 Allow time for the patient to ask questions about these treatments.
Continue to: Document all steps
Document all steps. There is an adage in medicine that “If it’s not written, it wasn’t done.” To help reduce your liability risk when prescribing off-label, be sure to document the following4:
- your clinical assessment
- information you gleaned from the patient’s medical records
- your review of information regarding both therapeutic and adverse effects of the medication you want to prescribe
- your discussion of informed consent, including documentation that the patient is aware that the medication is being prescribed off-label
- your clinical rationale for why the off-label medication is in the patient’s best interest.
Also, document the steps you take to monitor for adverse events and therapeutic effectiveness.4 Overall, the goal of documentation should be to support the adequate continuing care of our patients.
The FDA defines “off-label” prescribing as prescribing an FDA-approved medication for an unapproved use, such as for an unapproved clinical indication, for a higher-than-approved dose, or for a patient who is not part of the FDA-approved population (eg, children or geriatric patients).1 Off-label prescribing is common in psychiatry; approximately 13% of psychiatry patients are prescribed off-label psychotropic medications.2 The American Psychiatric Association strongly supports “the autonomous clinical decision-making authority of a physician” and “a physician’s lawful use of an FDA-approved drug product or medical device for an off-label indication when such use is based upon sound scientific evidence in conjunction with sound medical judgment.”3 Because many psychiatric diagnoses have no FDA-approved medications, off-label prescribing often may be a psychiatrist’s only pharmacologic option.
Unfortunately, off-label prescribing can increase a psychiatrist’s risk for liability when treatment falls short of patients’ expectations, or when patients allege that they were injured by the use of an off-label medication. Off-label prescribing does not automatically lead to losing a malpractice suit because the FDA states that physicians can prescribe approved medications for any scientifically supported use, including off-label.1 Medical malpractice lawsuits alleging negligence in prescribing practices, such as off-label prescribing, typically include allegations against the psychiatrist for failure to4:
- adequately assess the patient
- consult the patient’s medical records
- obtain informed consent from the patient
- appropriately prescribe a medication for the clinical indication, dosage, patient’s age, etc.
- monitor for adverse effects and therapeutic effectiveness.
Steps to minimize your risk
When prescribing a medication off-label, the following approaches can help reduce your liability risk:
Conduct a comprehensive clinical assessment. This should include requesting and reviewing your patient’s medical records.
Explain your motivation. Explain to your patient how prescribing an off-label medication can directly benefit him/her. Make it clear that you are not conducting experimental research by prescribing off-label because some patients might perceive this as a covert form of research.
Know the medications you prescribe. Although this sounds obvious, psychiatrists should thoroughly understand how each medication they prescribe is likely to clinically affect their patient. This information is available from many sources, including the FDA’s medication information sheets and the manufacturer’s medication package inserts. If possible, make sure that your off-label prescribing is supported by reputable, peer-reviewed literature.
Obtain informed consent. Tell your patient that the medication you are recommending is being prescribed off-label. Discuss the medication’s risks, benefits, adverse effects, associated “black-box” warnings, off-label uses, and alternatives to the off-label medication.4 Allow time for the patient to ask questions about these treatments.
Continue to: Document all steps
Document all steps. There is an adage in medicine that “If it’s not written, it wasn’t done.” To help reduce your liability risk when prescribing off-label, be sure to document the following4:
- your clinical assessment
- information you gleaned from the patient’s medical records
- your review of information regarding both therapeutic and adverse effects of the medication you want to prescribe
- your discussion of informed consent, including documentation that the patient is aware that the medication is being prescribed off-label
- your clinical rationale for why the off-label medication is in the patient’s best interest.
Also, document the steps you take to monitor for adverse events and therapeutic effectiveness.4 Overall, the goal of documentation should be to support the adequate continuing care of our patients.
1. US Food and Drug Administration. Understanding unapproved use of approved drugs “off label.” https://www.fda.gov/patients/learn-about-expanded-access-and-other-treatment-options/understanding-unapproved-use-approved-drugs-label. Updated February 5, 2018. Accessed August 6, 2020.
2. Vijay A, Becker JE, Ross JS. Patterns and predictors of off-label prescription of psychiatric drugs. PLoS One. 2018;13(7):e0198363. doi: 10.1371/journal.pone.0198363.
3. McLeer S, Mawhinney J; Council on Healthcare Systems and Financing. Position statement on off-label treatments. American Psychiatric Association. https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-2016-Off-Label-Treatment.pdf. Published July 2016. Accessed August 6, 2020.
4. Funicelli A. What to consider when prescribing off-label. Psychiatric News. 2019;54(14):12.
1. US Food and Drug Administration. Understanding unapproved use of approved drugs “off label.” https://www.fda.gov/patients/learn-about-expanded-access-and-other-treatment-options/understanding-unapproved-use-approved-drugs-label. Updated February 5, 2018. Accessed August 6, 2020.
2. Vijay A, Becker JE, Ross JS. Patterns and predictors of off-label prescription of psychiatric drugs. PLoS One. 2018;13(7):e0198363. doi: 10.1371/journal.pone.0198363.
3. McLeer S, Mawhinney J; Council on Healthcare Systems and Financing. Position statement on off-label treatments. American Psychiatric Association. https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-2016-Off-Label-Treatment.pdf. Published July 2016. Accessed August 6, 2020.
4. Funicelli A. What to consider when prescribing off-label. Psychiatric News. 2019;54(14):12.