User login
Today’s Product Theaters
12:30 - 1:30 p.m., Product Theater 1
Expert Conversations in Heart Failure: Connecting the Pieces
Thomas Arne, Jr., DO
Sergey Kachur, MDSponsored by Novartis Pharmaceuticals
12:30 - 1:30 p.m., Product Theater 2 Opioid-Induced Constipation
Jeff Gudin, MD
Director, Pain and Palliative Care
Englewood Hospital and Medical Center
Englewood, NJ
Sponsored by Salix Pharmaceuticals
12:30 - 1:30 p.m., Product Theater 3
Challenges of Treating DVT and PE in the Hospital and After Discharge
Dr. Andrew Miller, Emergency Medicine, Lehigh Valley Hospital, Allentown, PA
Sponsored by Pfizer
12:30 - 1:30 p.m., Product Theater 1
Expert Conversations in Heart Failure: Connecting the Pieces
Thomas Arne, Jr., DO
Sergey Kachur, MDSponsored by Novartis Pharmaceuticals
12:30 - 1:30 p.m., Product Theater 2 Opioid-Induced Constipation
Jeff Gudin, MD
Director, Pain and Palliative Care
Englewood Hospital and Medical Center
Englewood, NJ
Sponsored by Salix Pharmaceuticals
12:30 - 1:30 p.m., Product Theater 3
Challenges of Treating DVT and PE in the Hospital and After Discharge
Dr. Andrew Miller, Emergency Medicine, Lehigh Valley Hospital, Allentown, PA
Sponsored by Pfizer
12:30 - 1:30 p.m., Product Theater 1
Expert Conversations in Heart Failure: Connecting the Pieces
Thomas Arne, Jr., DO
Sergey Kachur, MDSponsored by Novartis Pharmaceuticals
12:30 - 1:30 p.m., Product Theater 2 Opioid-Induced Constipation
Jeff Gudin, MD
Director, Pain and Palliative Care
Englewood Hospital and Medical Center
Englewood, NJ
Sponsored by Salix Pharmaceuticals
12:30 - 1:30 p.m., Product Theater 3
Challenges of Treating DVT and PE in the Hospital and After Discharge
Dr. Andrew Miller, Emergency Medicine, Lehigh Valley Hospital, Allentown, PA
Sponsored by Pfizer
SHM CEO to highlight need to prepare for change
If there’s one thing hospital medicine is not, it’s static. And that’s truer today than it’s ever been in the more than 20 years since the field came into existence: As the role of hospitalists continue to expand, it’s now in the setting of a rapidly changing health care scene.
So when Society of Hospital Medicine CEO Larry Wellikson, MD, MHM, takes the annual conference podium this morning for his talk on “Future Challenges for Hospital Medicine,” he’ll have a lot to cover.
His overall message, though, will boil down to this: Learn the skills you’ll need.
With hospitalists managing acute and palliative care and being involved in surgical comanagement, many may need additional training.
“There’s a blurring of our role as we link to the emergency department or critical care units, or even a blurring of where does inpatient care end and outpatient care begin?” he said. “Many of these roles hospitalists haven’t been completely trained for.” He’ll also remind the audience that one of SHM’s main roles is to help provide that training.
He said the urgency of learning new skills is only intensified by the health care field’s transition from volume-based payment to value-based payment and by consolidation of previously separate pieces of the landscape, such as the acquisition of Aetna by CVS, with its nearly 10,000 pharmacy locations and more than 1,000 MinuteClinics.
“The real cost for them is hospitalization,” Dr. Wellikson said. “Any money they spend on hospitalization is money they don’t have left over. That puts pressure on hospitalists.”
And it could mean a role shift.
“Maybe our role now becomes that we see that patient after they leave the hospital to make sure that we complete their hospital care and keep them moving in the right direction, because we don’t want them to bounce back into our hospital,” he said.
On whether all the changes in health care are good or bad for hospitalists, Dr. Wellikson said that “good is a relative term.”
“The most important thing in life is to be relevant and to be needed,” he said. “As you add on new things, you have to acquire those competencies. That’s the challenge.”
Dr. Wellikson will also discuss the expansion of hospital medicine and SHM internationally.
“We’re now working with hospitalists in Japan, in Brazil, in Holland, in Canada,” he said. “We’re working in England and Singapore. And each of these places is different.”
His talk will dovetail with a theme that is more prominent in the annual conference program this year: helping hospitalists in mid-career navigate new opportunities.
“The good news on career development is you have so many different directions you can go,” said Dr. Wellikson, pointing to hospitalists who’ve become CEOs and CMOs. But he added that these opportunities require new skills, which goes back to the importance of training.
As a hospitalist, he said, you have to “make sure that you have the ability to gather the new skills to meet new challenges. Just because you become a manager doesn’t mean that magically you know how to manage. How do you keep your skills up as your scope expands or your opportunities grow? What happens more often in hospital medicine is that hospitalists get promoted into a position that can be overwhelming, which leads to burnout or career problems.”
Future Challenges for Hospital Medicine
Tuesday, 9:35-10:00 a.m.
Palms Ballroom
If there’s one thing hospital medicine is not, it’s static. And that’s truer today than it’s ever been in the more than 20 years since the field came into existence: As the role of hospitalists continue to expand, it’s now in the setting of a rapidly changing health care scene.
So when Society of Hospital Medicine CEO Larry Wellikson, MD, MHM, takes the annual conference podium this morning for his talk on “Future Challenges for Hospital Medicine,” he’ll have a lot to cover.
His overall message, though, will boil down to this: Learn the skills you’ll need.
With hospitalists managing acute and palliative care and being involved in surgical comanagement, many may need additional training.
“There’s a blurring of our role as we link to the emergency department or critical care units, or even a blurring of where does inpatient care end and outpatient care begin?” he said. “Many of these roles hospitalists haven’t been completely trained for.” He’ll also remind the audience that one of SHM’s main roles is to help provide that training.
He said the urgency of learning new skills is only intensified by the health care field’s transition from volume-based payment to value-based payment and by consolidation of previously separate pieces of the landscape, such as the acquisition of Aetna by CVS, with its nearly 10,000 pharmacy locations and more than 1,000 MinuteClinics.
“The real cost for them is hospitalization,” Dr. Wellikson said. “Any money they spend on hospitalization is money they don’t have left over. That puts pressure on hospitalists.”
And it could mean a role shift.
“Maybe our role now becomes that we see that patient after they leave the hospital to make sure that we complete their hospital care and keep them moving in the right direction, because we don’t want them to bounce back into our hospital,” he said.
On whether all the changes in health care are good or bad for hospitalists, Dr. Wellikson said that “good is a relative term.”
“The most important thing in life is to be relevant and to be needed,” he said. “As you add on new things, you have to acquire those competencies. That’s the challenge.”
Dr. Wellikson will also discuss the expansion of hospital medicine and SHM internationally.
“We’re now working with hospitalists in Japan, in Brazil, in Holland, in Canada,” he said. “We’re working in England and Singapore. And each of these places is different.”
His talk will dovetail with a theme that is more prominent in the annual conference program this year: helping hospitalists in mid-career navigate new opportunities.
“The good news on career development is you have so many different directions you can go,” said Dr. Wellikson, pointing to hospitalists who’ve become CEOs and CMOs. But he added that these opportunities require new skills, which goes back to the importance of training.
As a hospitalist, he said, you have to “make sure that you have the ability to gather the new skills to meet new challenges. Just because you become a manager doesn’t mean that magically you know how to manage. How do you keep your skills up as your scope expands or your opportunities grow? What happens more often in hospital medicine is that hospitalists get promoted into a position that can be overwhelming, which leads to burnout or career problems.”
Future Challenges for Hospital Medicine
Tuesday, 9:35-10:00 a.m.
Palms Ballroom
If there’s one thing hospital medicine is not, it’s static. And that’s truer today than it’s ever been in the more than 20 years since the field came into existence: As the role of hospitalists continue to expand, it’s now in the setting of a rapidly changing health care scene.
So when Society of Hospital Medicine CEO Larry Wellikson, MD, MHM, takes the annual conference podium this morning for his talk on “Future Challenges for Hospital Medicine,” he’ll have a lot to cover.
His overall message, though, will boil down to this: Learn the skills you’ll need.
With hospitalists managing acute and palliative care and being involved in surgical comanagement, many may need additional training.
“There’s a blurring of our role as we link to the emergency department or critical care units, or even a blurring of where does inpatient care end and outpatient care begin?” he said. “Many of these roles hospitalists haven’t been completely trained for.” He’ll also remind the audience that one of SHM’s main roles is to help provide that training.
He said the urgency of learning new skills is only intensified by the health care field’s transition from volume-based payment to value-based payment and by consolidation of previously separate pieces of the landscape, such as the acquisition of Aetna by CVS, with its nearly 10,000 pharmacy locations and more than 1,000 MinuteClinics.
“The real cost for them is hospitalization,” Dr. Wellikson said. “Any money they spend on hospitalization is money they don’t have left over. That puts pressure on hospitalists.”
And it could mean a role shift.
“Maybe our role now becomes that we see that patient after they leave the hospital to make sure that we complete their hospital care and keep them moving in the right direction, because we don’t want them to bounce back into our hospital,” he said.
On whether all the changes in health care are good or bad for hospitalists, Dr. Wellikson said that “good is a relative term.”
“The most important thing in life is to be relevant and to be needed,” he said. “As you add on new things, you have to acquire those competencies. That’s the challenge.”
Dr. Wellikson will also discuss the expansion of hospital medicine and SHM internationally.
“We’re now working with hospitalists in Japan, in Brazil, in Holland, in Canada,” he said. “We’re working in England and Singapore. And each of these places is different.”
His talk will dovetail with a theme that is more prominent in the annual conference program this year: helping hospitalists in mid-career navigate new opportunities.
“The good news on career development is you have so many different directions you can go,” said Dr. Wellikson, pointing to hospitalists who’ve become CEOs and CMOs. But he added that these opportunities require new skills, which goes back to the importance of training.
As a hospitalist, he said, you have to “make sure that you have the ability to gather the new skills to meet new challenges. Just because you become a manager doesn’t mean that magically you know how to manage. How do you keep your skills up as your scope expands or your opportunities grow? What happens more often in hospital medicine is that hospitalists get promoted into a position that can be overwhelming, which leads to burnout or career problems.”
Future Challenges for Hospital Medicine
Tuesday, 9:35-10:00 a.m.
Palms Ballroom
Culture change can improve NP, PA practice
Creating an atmosphere conducive to productive teamwork can help maximize nurse practitioners’ and physician assistants’ potential, say experts presenting at the Tuesday session “How Best NP/PA and MD Hospitalists Can Work Together.”
Session leaders Brian Wolfe, MD, FHM, a general internist at the University of Michigan, Ann Arbor, and Tracy Cardin, ACNP-BC,SFHM, the associate director of clinical integration at Adfinitas Health, Hanover, Md., will break down strategies to help incorporate different perspectives into your practice to improve its culture.
“I think culture beats strategy any day of the week, and the cultural threads we can draw from our different experiences are a lot more powerful, and a lot more translatable, across different institutions,” Dr. Wolfe said in an interview. “The purpose of this session is to get away from saying ‘Well, this is the way we do it,’ and instead say, ‘This is what kind of cultural vision we have for our NPs and PAs, and this is where we succeed, and these are the ways we fail.’ ”
Attendees will learn about what PAs and NPs are looking for in their work, what some providers are doing to change their hospital culture, and the business data behind those decisions.
“NPs and PAs are looking for autonomy, mastery, and purpose,” said Dr. Wolfe. “While some of that comes from where you work and how long your hours are, a lot of it has to do with how the culture treats you as a nurse practitioner or physician assistant and where your place is.”
Following Dr. Wolfe’s initial presentation, the facilitators will analyze cases with evident structural problems in order to uncover the underlying cultural issues.
By hearing about concrete, everyday examples, attendees will be able to recognize some of the problems within their own networks that they might deal with on a regular basis and come away with long-term solutions.
“Nobody really acknowledges these issues on a day-to-day basis, but they can be extremely influential,” Ms. Cardin said in an interview. “Once you’re aware of the cultural impacts on the functionality of your group, then you can begin chipping away at them and altering culture to provide for a more successful path.”
Attendees will leave the session with solutions that can boost productivity and spending, according to Dr. Wolfe.
“As a physician leader, you want to recruit and retain high-level people who can operate at the top of their licenses and can push your practice beyond its structures,” said Dr. Wolfe. “The other piece is that there is no defined cost for retraining, and if you don’t address the issues that will drive your PAs and NPs to leave, you’ll be stuck with a constant turnover, which leads to lower performance and less efficiency.”
How Best NP/PA and MD Hospitalists Can Work Together:
Incorporating NPs/PAs into the workforce and Workplace Culture
Tuesday, 4:30-6 p.m.
Grand Ballroom 1-3
Creating an atmosphere conducive to productive teamwork can help maximize nurse practitioners’ and physician assistants’ potential, say experts presenting at the Tuesday session “How Best NP/PA and MD Hospitalists Can Work Together.”
Session leaders Brian Wolfe, MD, FHM, a general internist at the University of Michigan, Ann Arbor, and Tracy Cardin, ACNP-BC,SFHM, the associate director of clinical integration at Adfinitas Health, Hanover, Md., will break down strategies to help incorporate different perspectives into your practice to improve its culture.
“I think culture beats strategy any day of the week, and the cultural threads we can draw from our different experiences are a lot more powerful, and a lot more translatable, across different institutions,” Dr. Wolfe said in an interview. “The purpose of this session is to get away from saying ‘Well, this is the way we do it,’ and instead say, ‘This is what kind of cultural vision we have for our NPs and PAs, and this is where we succeed, and these are the ways we fail.’ ”
Attendees will learn about what PAs and NPs are looking for in their work, what some providers are doing to change their hospital culture, and the business data behind those decisions.
“NPs and PAs are looking for autonomy, mastery, and purpose,” said Dr. Wolfe. “While some of that comes from where you work and how long your hours are, a lot of it has to do with how the culture treats you as a nurse practitioner or physician assistant and where your place is.”
Following Dr. Wolfe’s initial presentation, the facilitators will analyze cases with evident structural problems in order to uncover the underlying cultural issues.
By hearing about concrete, everyday examples, attendees will be able to recognize some of the problems within their own networks that they might deal with on a regular basis and come away with long-term solutions.
“Nobody really acknowledges these issues on a day-to-day basis, but they can be extremely influential,” Ms. Cardin said in an interview. “Once you’re aware of the cultural impacts on the functionality of your group, then you can begin chipping away at them and altering culture to provide for a more successful path.”
Attendees will leave the session with solutions that can boost productivity and spending, according to Dr. Wolfe.
“As a physician leader, you want to recruit and retain high-level people who can operate at the top of their licenses and can push your practice beyond its structures,” said Dr. Wolfe. “The other piece is that there is no defined cost for retraining, and if you don’t address the issues that will drive your PAs and NPs to leave, you’ll be stuck with a constant turnover, which leads to lower performance and less efficiency.”
How Best NP/PA and MD Hospitalists Can Work Together:
Incorporating NPs/PAs into the workforce and Workplace Culture
Tuesday, 4:30-6 p.m.
Grand Ballroom 1-3
Creating an atmosphere conducive to productive teamwork can help maximize nurse practitioners’ and physician assistants’ potential, say experts presenting at the Tuesday session “How Best NP/PA and MD Hospitalists Can Work Together.”
Session leaders Brian Wolfe, MD, FHM, a general internist at the University of Michigan, Ann Arbor, and Tracy Cardin, ACNP-BC,SFHM, the associate director of clinical integration at Adfinitas Health, Hanover, Md., will break down strategies to help incorporate different perspectives into your practice to improve its culture.
“I think culture beats strategy any day of the week, and the cultural threads we can draw from our different experiences are a lot more powerful, and a lot more translatable, across different institutions,” Dr. Wolfe said in an interview. “The purpose of this session is to get away from saying ‘Well, this is the way we do it,’ and instead say, ‘This is what kind of cultural vision we have for our NPs and PAs, and this is where we succeed, and these are the ways we fail.’ ”
Attendees will learn about what PAs and NPs are looking for in their work, what some providers are doing to change their hospital culture, and the business data behind those decisions.
“NPs and PAs are looking for autonomy, mastery, and purpose,” said Dr. Wolfe. “While some of that comes from where you work and how long your hours are, a lot of it has to do with how the culture treats you as a nurse practitioner or physician assistant and where your place is.”
Following Dr. Wolfe’s initial presentation, the facilitators will analyze cases with evident structural problems in order to uncover the underlying cultural issues.
By hearing about concrete, everyday examples, attendees will be able to recognize some of the problems within their own networks that they might deal with on a regular basis and come away with long-term solutions.
“Nobody really acknowledges these issues on a day-to-day basis, but they can be extremely influential,” Ms. Cardin said in an interview. “Once you’re aware of the cultural impacts on the functionality of your group, then you can begin chipping away at them and altering culture to provide for a more successful path.”
Attendees will leave the session with solutions that can boost productivity and spending, according to Dr. Wolfe.
“As a physician leader, you want to recruit and retain high-level people who can operate at the top of their licenses and can push your practice beyond its structures,” said Dr. Wolfe. “The other piece is that there is no defined cost for retraining, and if you don’t address the issues that will drive your PAs and NPs to leave, you’ll be stuck with a constant turnover, which leads to lower performance and less efficiency.”
How Best NP/PA and MD Hospitalists Can Work Together:
Incorporating NPs/PAs into the workforce and Workplace Culture
Tuesday, 4:30-6 p.m.
Grand Ballroom 1-3
‘Update in HM’ to highlight practice pearls
Barbara Slawski, MD, MS, SFHM, and Cynthia Cooper, MD, hadn’t met in person until early 2018. But that doesn’t mean they haven’t spent a lot of time together.
Once a month, the two hospitalists checked in with one another through wide-ranging phone calls. Together, they have combed the medical literature and conferred over the past year, making long lists of candidate studies for the “Top 20” journal articles of the year for practicing hospitalists.
The two physicians will comoderate Tuesday’s “Update in Hospital Medicine” session, where they will summarize research findings of these “Top 20” articles. Their hope is to present research that each attendee can bring home to improve patient outcomes on a daily basis, while making for a smoother and more efficient practice.
Dr. Slawski, chief of the section of perioperative medicine at the Medical College of Wisconsin in Milwaukee, said the presentations will not simply summarize study results but also will help attendees focus on the key findings – the clinical pearls – that represent real opportunities to update practice.
Since hospital medicine crosses so many disciplines, each physician said, in separate interviews, that doing justice to the literature has been time consuming and intellectually challenging – but worthwhile.
Dr. Cooper, a hospitalist at Massachusetts General Hospital, Boston, said that, although she and Dr. Slawski practice in geographically diverse areas, their practice settings – academic medical centers – have many similarities. She said that, as she reviewed the medical literature over the past year, she gave considerable thought to the particular challenges and demands of hospitalists who practice in community hospitals and rural settings, where the level of support and access to subspecialty consults might be very different from the academic milieu.
“We hope that our unique approaches lend more breadth to the session,” said Dr. Slawski. “We want to make sure we have a good representation of SHM’s constituency, and that we present high-impact studies.”
To hit the mark of articles that are relevant for all, Dr. Cooper said she wants to make sure to focus on the practicalities of hospital-based practice – possible topics include prediction scores, hepatic encephalopathy, and the management of sepsis.
Neither Dr. Slawski nor Dr. Cooper reported any relevant conflicts of interest.
Update in Hospital Medicine
Tuesday, 1:40-2:40 p.m.
Palms Ballroom
Barbara Slawski, MD, MS, SFHM, and Cynthia Cooper, MD, hadn’t met in person until early 2018. But that doesn’t mean they haven’t spent a lot of time together.
Once a month, the two hospitalists checked in with one another through wide-ranging phone calls. Together, they have combed the medical literature and conferred over the past year, making long lists of candidate studies for the “Top 20” journal articles of the year for practicing hospitalists.
The two physicians will comoderate Tuesday’s “Update in Hospital Medicine” session, where they will summarize research findings of these “Top 20” articles. Their hope is to present research that each attendee can bring home to improve patient outcomes on a daily basis, while making for a smoother and more efficient practice.
Dr. Slawski, chief of the section of perioperative medicine at the Medical College of Wisconsin in Milwaukee, said the presentations will not simply summarize study results but also will help attendees focus on the key findings – the clinical pearls – that represent real opportunities to update practice.
Since hospital medicine crosses so many disciplines, each physician said, in separate interviews, that doing justice to the literature has been time consuming and intellectually challenging – but worthwhile.
Dr. Cooper, a hospitalist at Massachusetts General Hospital, Boston, said that, although she and Dr. Slawski practice in geographically diverse areas, their practice settings – academic medical centers – have many similarities. She said that, as she reviewed the medical literature over the past year, she gave considerable thought to the particular challenges and demands of hospitalists who practice in community hospitals and rural settings, where the level of support and access to subspecialty consults might be very different from the academic milieu.
“We hope that our unique approaches lend more breadth to the session,” said Dr. Slawski. “We want to make sure we have a good representation of SHM’s constituency, and that we present high-impact studies.”
To hit the mark of articles that are relevant for all, Dr. Cooper said she wants to make sure to focus on the practicalities of hospital-based practice – possible topics include prediction scores, hepatic encephalopathy, and the management of sepsis.
Neither Dr. Slawski nor Dr. Cooper reported any relevant conflicts of interest.
Update in Hospital Medicine
Tuesday, 1:40-2:40 p.m.
Palms Ballroom
Barbara Slawski, MD, MS, SFHM, and Cynthia Cooper, MD, hadn’t met in person until early 2018. But that doesn’t mean they haven’t spent a lot of time together.
Once a month, the two hospitalists checked in with one another through wide-ranging phone calls. Together, they have combed the medical literature and conferred over the past year, making long lists of candidate studies for the “Top 20” journal articles of the year for practicing hospitalists.
The two physicians will comoderate Tuesday’s “Update in Hospital Medicine” session, where they will summarize research findings of these “Top 20” articles. Their hope is to present research that each attendee can bring home to improve patient outcomes on a daily basis, while making for a smoother and more efficient practice.
Dr. Slawski, chief of the section of perioperative medicine at the Medical College of Wisconsin in Milwaukee, said the presentations will not simply summarize study results but also will help attendees focus on the key findings – the clinical pearls – that represent real opportunities to update practice.
Since hospital medicine crosses so many disciplines, each physician said, in separate interviews, that doing justice to the literature has been time consuming and intellectually challenging – but worthwhile.
Dr. Cooper, a hospitalist at Massachusetts General Hospital, Boston, said that, although she and Dr. Slawski practice in geographically diverse areas, their practice settings – academic medical centers – have many similarities. She said that, as she reviewed the medical literature over the past year, she gave considerable thought to the particular challenges and demands of hospitalists who practice in community hospitals and rural settings, where the level of support and access to subspecialty consults might be very different from the academic milieu.
“We hope that our unique approaches lend more breadth to the session,” said Dr. Slawski. “We want to make sure we have a good representation of SHM’s constituency, and that we present high-impact studies.”
To hit the mark of articles that are relevant for all, Dr. Cooper said she wants to make sure to focus on the practicalities of hospital-based practice – possible topics include prediction scores, hepatic encephalopathy, and the management of sepsis.
Neither Dr. Slawski nor Dr. Cooper reported any relevant conflicts of interest.
Update in Hospital Medicine
Tuesday, 1:40-2:40 p.m.
Palms Ballroom
Welcome to Day 2 of HM18!
I hope all of you enjoyed Day 1 as much as I did. The quality and variety of the presentations yesterday were stellar, and I am sure today will be the same.
The day begins with the Best of Research and Innovations, where the cream of the crop from the hundreds of submitted projects will be presented and recognized. Following that will be the Awards of Excellence, Society of Hospital Medicine’s annual celebration of the very best of our members for their years of stellar contributions in areas such as teaching, clinical excellence, and service to hospital medicine. You will be inspired by the accomplishments of our colleagues who are receiving these awards. They demonstrate to all of us how our specialty improves the health care delivered in our nation’s hospitals.
Our plenary speaker of the morning will be our very own Larry Wellikson, MD, MHM, who will give us his own perspectives on “Future Challenges for Hospital Medicine,” calling on his more than 2 decades of experience as the creative and accomplished CEO of SHM.
After the morning sessions, please join us for a real treat at noon when we have the honor of hearing from our visiting colleagues from the Japanese Society of Hospital General Medicine who will talk to us about hospital medicine in Japan. As much as we come to HM18 to learn from our U.S. colleagues who are doing extraordinary things here at home, this is a unique opportunity to learn from the leaders of one of our international partners how they are shaping the rapidly growing hospitalist movement in Japan.
That will be closely followed by the can’t-miss “Update in Hospital Medicine,” presented this year by Cindy Cooper, MD, and Barbara Slawski, MD, MS, SFHM. And especially important to our students, residents, and younger members, there is an evening session entitled, “Mastering the Job Interview,” a workshop for those who should always be looking to hone the nonclinical skills essential to long-term career success.
Like Day 1, this is a day chockfull of clinical and management presentations to meet everyone’s needs. There are too many to call out, but allow me to pick my personal favorite titles of the day, starting with “Waiting in Line for ‘It’s a Small World’ and Other Things We Do for No Reason” and “Let It Flow: CPAP, BIPAP, and High-Flow Oxygen.”
Yesterday kicked off HM18 with aplomb, and tomorrow we wrap up. So make the most of Day 2 today, and take advantage of the terrific work of our fellow hospitalists. During the breaks, visit the Exhibit Hall to explore, mingle, and thank our exhibitors for supporting our society and our conference.
Please stop by to greet the SHM staff who have made this conference another great success at the SHM Pavilion in the Exhibit Hall. While you’re there, take a chance to meet and chat with SHM board members who will be there throughout the conference.
Enjoy!
Dr. Greeno is president of the Society of Hospital Medicine and chief strategy officer at IPC Healthcare.
I hope all of you enjoyed Day 1 as much as I did. The quality and variety of the presentations yesterday were stellar, and I am sure today will be the same.
The day begins with the Best of Research and Innovations, where the cream of the crop from the hundreds of submitted projects will be presented and recognized. Following that will be the Awards of Excellence, Society of Hospital Medicine’s annual celebration of the very best of our members for their years of stellar contributions in areas such as teaching, clinical excellence, and service to hospital medicine. You will be inspired by the accomplishments of our colleagues who are receiving these awards. They demonstrate to all of us how our specialty improves the health care delivered in our nation’s hospitals.
Our plenary speaker of the morning will be our very own Larry Wellikson, MD, MHM, who will give us his own perspectives on “Future Challenges for Hospital Medicine,” calling on his more than 2 decades of experience as the creative and accomplished CEO of SHM.
After the morning sessions, please join us for a real treat at noon when we have the honor of hearing from our visiting colleagues from the Japanese Society of Hospital General Medicine who will talk to us about hospital medicine in Japan. As much as we come to HM18 to learn from our U.S. colleagues who are doing extraordinary things here at home, this is a unique opportunity to learn from the leaders of one of our international partners how they are shaping the rapidly growing hospitalist movement in Japan.
That will be closely followed by the can’t-miss “Update in Hospital Medicine,” presented this year by Cindy Cooper, MD, and Barbara Slawski, MD, MS, SFHM. And especially important to our students, residents, and younger members, there is an evening session entitled, “Mastering the Job Interview,” a workshop for those who should always be looking to hone the nonclinical skills essential to long-term career success.
Like Day 1, this is a day chockfull of clinical and management presentations to meet everyone’s needs. There are too many to call out, but allow me to pick my personal favorite titles of the day, starting with “Waiting in Line for ‘It’s a Small World’ and Other Things We Do for No Reason” and “Let It Flow: CPAP, BIPAP, and High-Flow Oxygen.”
Yesterday kicked off HM18 with aplomb, and tomorrow we wrap up. So make the most of Day 2 today, and take advantage of the terrific work of our fellow hospitalists. During the breaks, visit the Exhibit Hall to explore, mingle, and thank our exhibitors for supporting our society and our conference.
Please stop by to greet the SHM staff who have made this conference another great success at the SHM Pavilion in the Exhibit Hall. While you’re there, take a chance to meet and chat with SHM board members who will be there throughout the conference.
Enjoy!
Dr. Greeno is president of the Society of Hospital Medicine and chief strategy officer at IPC Healthcare.
I hope all of you enjoyed Day 1 as much as I did. The quality and variety of the presentations yesterday were stellar, and I am sure today will be the same.
The day begins with the Best of Research and Innovations, where the cream of the crop from the hundreds of submitted projects will be presented and recognized. Following that will be the Awards of Excellence, Society of Hospital Medicine’s annual celebration of the very best of our members for their years of stellar contributions in areas such as teaching, clinical excellence, and service to hospital medicine. You will be inspired by the accomplishments of our colleagues who are receiving these awards. They demonstrate to all of us how our specialty improves the health care delivered in our nation’s hospitals.
Our plenary speaker of the morning will be our very own Larry Wellikson, MD, MHM, who will give us his own perspectives on “Future Challenges for Hospital Medicine,” calling on his more than 2 decades of experience as the creative and accomplished CEO of SHM.
After the morning sessions, please join us for a real treat at noon when we have the honor of hearing from our visiting colleagues from the Japanese Society of Hospital General Medicine who will talk to us about hospital medicine in Japan. As much as we come to HM18 to learn from our U.S. colleagues who are doing extraordinary things here at home, this is a unique opportunity to learn from the leaders of one of our international partners how they are shaping the rapidly growing hospitalist movement in Japan.
That will be closely followed by the can’t-miss “Update in Hospital Medicine,” presented this year by Cindy Cooper, MD, and Barbara Slawski, MD, MS, SFHM. And especially important to our students, residents, and younger members, there is an evening session entitled, “Mastering the Job Interview,” a workshop for those who should always be looking to hone the nonclinical skills essential to long-term career success.
Like Day 1, this is a day chockfull of clinical and management presentations to meet everyone’s needs. There are too many to call out, but allow me to pick my personal favorite titles of the day, starting with “Waiting in Line for ‘It’s a Small World’ and Other Things We Do for No Reason” and “Let It Flow: CPAP, BIPAP, and High-Flow Oxygen.”
Yesterday kicked off HM18 with aplomb, and tomorrow we wrap up. So make the most of Day 2 today, and take advantage of the terrific work of our fellow hospitalists. During the breaks, visit the Exhibit Hall to explore, mingle, and thank our exhibitors for supporting our society and our conference.
Please stop by to greet the SHM staff who have made this conference another great success at the SHM Pavilion in the Exhibit Hall. While you’re there, take a chance to meet and chat with SHM board members who will be there throughout the conference.
Enjoy!
Dr. Greeno is president of the Society of Hospital Medicine and chief strategy officer at IPC Healthcare.
Tuesday’s satellite symposia schedule, information
Valuable Strategies to Reduce the Risk for and Clinical Impact of Hyperkalemia
7:30 – 9:30 p.m. – Canary Room 1-2
Dinner provided at 7:30 p.m.
Presenters: Biff F. Palmer, MD, professor of internal medicine, University of Texas Southwestern Medical Center, Dallas; Robert Toto, MD, associate dean, clinical and translational research, director, Center for Translational Medicine, UT Southwestern Medical Center, Dallas.
Overview: The goal of the case-based symposium is to highlight patients at increased risk of recurrent or sustained hyperkalemia and how these patients may be managed with evidence-based treatment so that they are able to continue renin-angiotensin-aldosterone system inhibitor therapy, if appropriate. The presenters will share their experiences in managing these patients, including suggestions for the hospitalist’s role in continued care.
Accreditation: This activity has been approved for AMA PRA Category 1 Credit(s)™. See final CE activity announcement for specific details.
This activity is supported by an educational grant from Relypsa Inc.
Hepatology News Tonight: Managing Complication of Cirrhosis
7:30 – 9:30 p.m. – Canary Room 3-4
Registration will be at 7:00 p.m.
Dinner provided at 7:30 p.m.
Presenters: Naoky Tsai, MD, clinical professor of medicine, John A. Burns School of Medicine, University of Hawaii, Manoa, Honolulu; Ashwani K. Singal MD, MS, associate professor of medicine and director of UAB Porphyria Center, division of gastroenterology and hepatology, University of Alabama at Birmingham.
Overview: This educational update will highlight the most clinically relevant advances in the management of patients with cirrhosis and hepatic encephalopathy (HE). The symposium will deliver emerging science and incorporate expert opinions on best practices for the diagnosis and management of patients with cirrhosis and HE.
Target audience: This activity has been designed to meet the educational needs of physicians, advanced practice providers, and allied health professionals who provide care for hospitalized patients with liver disease.
Learning objectives:
- Understand the complications and the consequences of chronic liver disease.
- Describe the economic, patient, and caregiver burdens associated with cirrhosis and HE.
- Demonstrate the ability to properly treat HE patients and prevent recurrence of disease.
Accredited by: Rehoboth McKindley Christian Health Care Services
Provided by: Chronic Liver Disease Foundation (CLDF)
Register: http://www.chronicliverdisease.org/
Supported by an educational grant from Salix Pharmaceuticals.
Valuable Strategies to Reduce the Risk for and Clinical Impact of Hyperkalemia
7:30 – 9:30 p.m. – Canary Room 1-2
Dinner provided at 7:30 p.m.
Presenters: Biff F. Palmer, MD, professor of internal medicine, University of Texas Southwestern Medical Center, Dallas; Robert Toto, MD, associate dean, clinical and translational research, director, Center for Translational Medicine, UT Southwestern Medical Center, Dallas.
Overview: The goal of the case-based symposium is to highlight patients at increased risk of recurrent or sustained hyperkalemia and how these patients may be managed with evidence-based treatment so that they are able to continue renin-angiotensin-aldosterone system inhibitor therapy, if appropriate. The presenters will share their experiences in managing these patients, including suggestions for the hospitalist’s role in continued care.
Accreditation: This activity has been approved for AMA PRA Category 1 Credit(s)™. See final CE activity announcement for specific details.
This activity is supported by an educational grant from Relypsa Inc.
Hepatology News Tonight: Managing Complication of Cirrhosis
7:30 – 9:30 p.m. – Canary Room 3-4
Registration will be at 7:00 p.m.
Dinner provided at 7:30 p.m.
Presenters: Naoky Tsai, MD, clinical professor of medicine, John A. Burns School of Medicine, University of Hawaii, Manoa, Honolulu; Ashwani K. Singal MD, MS, associate professor of medicine and director of UAB Porphyria Center, division of gastroenterology and hepatology, University of Alabama at Birmingham.
Overview: This educational update will highlight the most clinically relevant advances in the management of patients with cirrhosis and hepatic encephalopathy (HE). The symposium will deliver emerging science and incorporate expert opinions on best practices for the diagnosis and management of patients with cirrhosis and HE.
Target audience: This activity has been designed to meet the educational needs of physicians, advanced practice providers, and allied health professionals who provide care for hospitalized patients with liver disease.
Learning objectives:
- Understand the complications and the consequences of chronic liver disease.
- Describe the economic, patient, and caregiver burdens associated with cirrhosis and HE.
- Demonstrate the ability to properly treat HE patients and prevent recurrence of disease.
Accredited by: Rehoboth McKindley Christian Health Care Services
Provided by: Chronic Liver Disease Foundation (CLDF)
Register: http://www.chronicliverdisease.org/
Supported by an educational grant from Salix Pharmaceuticals.
Valuable Strategies to Reduce the Risk for and Clinical Impact of Hyperkalemia
7:30 – 9:30 p.m. – Canary Room 1-2
Dinner provided at 7:30 p.m.
Presenters: Biff F. Palmer, MD, professor of internal medicine, University of Texas Southwestern Medical Center, Dallas; Robert Toto, MD, associate dean, clinical and translational research, director, Center for Translational Medicine, UT Southwestern Medical Center, Dallas.
Overview: The goal of the case-based symposium is to highlight patients at increased risk of recurrent or sustained hyperkalemia and how these patients may be managed with evidence-based treatment so that they are able to continue renin-angiotensin-aldosterone system inhibitor therapy, if appropriate. The presenters will share their experiences in managing these patients, including suggestions for the hospitalist’s role in continued care.
Accreditation: This activity has been approved for AMA PRA Category 1 Credit(s)™. See final CE activity announcement for specific details.
This activity is supported by an educational grant from Relypsa Inc.
Hepatology News Tonight: Managing Complication of Cirrhosis
7:30 – 9:30 p.m. – Canary Room 3-4
Registration will be at 7:00 p.m.
Dinner provided at 7:30 p.m.
Presenters: Naoky Tsai, MD, clinical professor of medicine, John A. Burns School of Medicine, University of Hawaii, Manoa, Honolulu; Ashwani K. Singal MD, MS, associate professor of medicine and director of UAB Porphyria Center, division of gastroenterology and hepatology, University of Alabama at Birmingham.
Overview: This educational update will highlight the most clinically relevant advances in the management of patients with cirrhosis and hepatic encephalopathy (HE). The symposium will deliver emerging science and incorporate expert opinions on best practices for the diagnosis and management of patients with cirrhosis and HE.
Target audience: This activity has been designed to meet the educational needs of physicians, advanced practice providers, and allied health professionals who provide care for hospitalized patients with liver disease.
Learning objectives:
- Understand the complications and the consequences of chronic liver disease.
- Describe the economic, patient, and caregiver burdens associated with cirrhosis and HE.
- Demonstrate the ability to properly treat HE patients and prevent recurrence of disease.
Accredited by: Rehoboth McKindley Christian Health Care Services
Provided by: Chronic Liver Disease Foundation (CLDF)
Register: http://www.chronicliverdisease.org/
Supported by an educational grant from Salix Pharmaceuticals.
RIV plenary showcases best research
The best research in hospital medicine will be front and center today in the “Best of Research and Innovations in 2018” part of this morning’s plenary session.
New research also will figure prominently in the second “Clinical Vignettes Poster Competition” at lunchtime today.
During the plenary session, investigators will present the top-rated research among hundreds of submissions, said Ethan Cumbler, MD, FHM, chair of the Research, Innovations, Vignettes (RIV) competition and professor of medicine and medical director of the University of Colorado Acute Care Center for the Elderly, Denver, unit. Three independent, blinded reviewers chose the abstracts for oral presentation after rating them based on originality, scientific rigor, and importance to hospital medicine, he said. These oral presentations are meant not only to provide information to other hospitalists but also to inspire hospitalists to engage in research themselves.
“I think about it as a collective celebration of how far the field of hospital medicine has advanced in the last year and its potential moving forward,” Dr. Cumbler said. “My fundamental view is every hospitalist can and should be examining what they’re doing, thinking about how to do it better, and, by God, sharing it with the rest of us when they figure out that something can work better.”
Even as a veteran hospitalist, Dr. Cumbler said he still gets inspired by research presented in the RIV.
“When I see the RIV posters or come to hear the oral presentations, I get inspired, because I get to see what other people are doing in their local microenvironments, in their laboratories, in their hospitals,” he said. “And often I think ... ‘We could be doing stuff just that exciting.’ Often, it’s a chance to collaborate with the people whose work is inspiring you, or to take a great idea and run with it.”
At the Clinical Vignettes competition, research will focus on lessons learned from specific cases, Dr. Cumbler said.
“A typical clinical vignette would be a case presentation, maybe a diagnostic image or a description of the test that clinched the diagnosis, and then, most importantly, the lessons from that case, which are more widely applicable,” he said. “One of the things I love about Clinical Vignettes is it gives you a chance to highlight your best catches, but it also lets you, with humility, share your misses so that other people can learn from your experience.”
He said he hopes the sharing of research in formal oral presentations – and in the poster hall – continues to advance the hospital medicine literature.
“It’s come an incredible distance over the last 10 years, 15 years,” he said. “When I look at where we are heading next, I think it is into more multicenter research, multiple-institution quality improvement. I really see us graduating from proof-of-concept and pilot work into the kind of trials which answer questions – the big questions that face medicine.”
Best of Research and Innovations in 2018
8-9 a.m., Palms Ballroom
Clinical Vignettes #2
Poster Competition
12-1:30 p.m., Cypress Ballroom
The best research in hospital medicine will be front and center today in the “Best of Research and Innovations in 2018” part of this morning’s plenary session.
New research also will figure prominently in the second “Clinical Vignettes Poster Competition” at lunchtime today.
During the plenary session, investigators will present the top-rated research among hundreds of submissions, said Ethan Cumbler, MD, FHM, chair of the Research, Innovations, Vignettes (RIV) competition and professor of medicine and medical director of the University of Colorado Acute Care Center for the Elderly, Denver, unit. Three independent, blinded reviewers chose the abstracts for oral presentation after rating them based on originality, scientific rigor, and importance to hospital medicine, he said. These oral presentations are meant not only to provide information to other hospitalists but also to inspire hospitalists to engage in research themselves.
“I think about it as a collective celebration of how far the field of hospital medicine has advanced in the last year and its potential moving forward,” Dr. Cumbler said. “My fundamental view is every hospitalist can and should be examining what they’re doing, thinking about how to do it better, and, by God, sharing it with the rest of us when they figure out that something can work better.”
Even as a veteran hospitalist, Dr. Cumbler said he still gets inspired by research presented in the RIV.
“When I see the RIV posters or come to hear the oral presentations, I get inspired, because I get to see what other people are doing in their local microenvironments, in their laboratories, in their hospitals,” he said. “And often I think ... ‘We could be doing stuff just that exciting.’ Often, it’s a chance to collaborate with the people whose work is inspiring you, or to take a great idea and run with it.”
At the Clinical Vignettes competition, research will focus on lessons learned from specific cases, Dr. Cumbler said.
“A typical clinical vignette would be a case presentation, maybe a diagnostic image or a description of the test that clinched the diagnosis, and then, most importantly, the lessons from that case, which are more widely applicable,” he said. “One of the things I love about Clinical Vignettes is it gives you a chance to highlight your best catches, but it also lets you, with humility, share your misses so that other people can learn from your experience.”
He said he hopes the sharing of research in formal oral presentations – and in the poster hall – continues to advance the hospital medicine literature.
“It’s come an incredible distance over the last 10 years, 15 years,” he said. “When I look at where we are heading next, I think it is into more multicenter research, multiple-institution quality improvement. I really see us graduating from proof-of-concept and pilot work into the kind of trials which answer questions – the big questions that face medicine.”
Best of Research and Innovations in 2018
8-9 a.m., Palms Ballroom
Clinical Vignettes #2
Poster Competition
12-1:30 p.m., Cypress Ballroom
The best research in hospital medicine will be front and center today in the “Best of Research and Innovations in 2018” part of this morning’s plenary session.
New research also will figure prominently in the second “Clinical Vignettes Poster Competition” at lunchtime today.
During the plenary session, investigators will present the top-rated research among hundreds of submissions, said Ethan Cumbler, MD, FHM, chair of the Research, Innovations, Vignettes (RIV) competition and professor of medicine and medical director of the University of Colorado Acute Care Center for the Elderly, Denver, unit. Three independent, blinded reviewers chose the abstracts for oral presentation after rating them based on originality, scientific rigor, and importance to hospital medicine, he said. These oral presentations are meant not only to provide information to other hospitalists but also to inspire hospitalists to engage in research themselves.
“I think about it as a collective celebration of how far the field of hospital medicine has advanced in the last year and its potential moving forward,” Dr. Cumbler said. “My fundamental view is every hospitalist can and should be examining what they’re doing, thinking about how to do it better, and, by God, sharing it with the rest of us when they figure out that something can work better.”
Even as a veteran hospitalist, Dr. Cumbler said he still gets inspired by research presented in the RIV.
“When I see the RIV posters or come to hear the oral presentations, I get inspired, because I get to see what other people are doing in their local microenvironments, in their laboratories, in their hospitals,” he said. “And often I think ... ‘We could be doing stuff just that exciting.’ Often, it’s a chance to collaborate with the people whose work is inspiring you, or to take a great idea and run with it.”
At the Clinical Vignettes competition, research will focus on lessons learned from specific cases, Dr. Cumbler said.
“A typical clinical vignette would be a case presentation, maybe a diagnostic image or a description of the test that clinched the diagnosis, and then, most importantly, the lessons from that case, which are more widely applicable,” he said. “One of the things I love about Clinical Vignettes is it gives you a chance to highlight your best catches, but it also lets you, with humility, share your misses so that other people can learn from your experience.”
He said he hopes the sharing of research in formal oral presentations – and in the poster hall – continues to advance the hospital medicine literature.
“It’s come an incredible distance over the last 10 years, 15 years,” he said. “When I look at where we are heading next, I think it is into more multicenter research, multiple-institution quality improvement. I really see us graduating from proof-of-concept and pilot work into the kind of trials which answer questions – the big questions that face medicine.”
Best of Research and Innovations in 2018
8-9 a.m., Palms Ballroom
Clinical Vignettes #2
Poster Competition
12-1:30 p.m., Cypress Ballroom
Winners chosen at the SHM Clinical Vignettes competition
ORLANDO – Researchers presenting a case of starving ketoacidosis in a woman who was on a “Paleo” diet while breastfeeding won the Clinical Vignettes competition held Monday at HM18. The announcement capped a flurry of presenting and judging of posters on single cases that were captivating in both the stories they told and the lessons they taught.
The trainee award winner in the competition were presenters of a case of licorice-induced hypokalemia that, clinicians learned, was brought about by the drinking of an obscure kind of tea. The two others that made it into the final round of judging were on cases of syphilitic hepatitis and cardiac amyloidosis.
By chance, both of the winners highlighted dietary triggers, said Stephanie Sherman, MD, chair of the annual meeting’s clinical vignettes committee.
“The common themes in both of these were the importance of dietary history when interviewing patients,” Dr. Sherman said. “And then both had a beautiful review of the physiology that’s normal and how it gets broken in these situations.”
The Clinical Vignettes portion of the RIV competition, which also includes research and innovations categories, was separate this year because of space constraints, Dr. Sherman said.
Judges said they looked not only at how interesting and applicable each case was, but also the quality of the oral presentation and the poster’s visual appeal and clarity.
The ketoacidosis case, presented by Timothy Judson, MD, a resident at University of California, San Francisco, involved a 40-year-old woman who was previously healthy and had given birth 9 weeks earlier. Since the birth, the woman had been on a Paleo diet, a low-carbohydrate, ketogenic diet. She also was breastfeeding her newborn and continuing to breastfeed her 2-year-old son.
She presented with nonbilious, nonbloody emesis. On physical exam, she was found to be tachycardic, with diffuse tenderness of the abdomen. She was positive for ketones and had an elevated acetone level and elevated osmolar gap, the difference between the measured and calculated solutes in the serum.
Clinicians identified that low carbohydrate intake, high fat intake, and a high metabolic state, such as that brought on by breastfeeding, can contribute to ketoacidosis. She was treated with IV glucose-containing fluids, bicarbonate, fomepizole, and thiamine.
The case shows that patients should be warned about ketoacidosis risk when they start an ultra-low carbohydrate diet, especially if they are breastfeeding or lactating, Dr. Hudson said.
“Usually they’re safe, but they may not be if you’re in a high metabolic state,” he told judges.
“We take care of so many patients on a daily basis and we rarely get to tell their stories,” he said. “To be able to tell the story of the patients and give the learning points that we took away to others, I think is very rewarding.”
The winner of the trainee award, Maxwell Bressman, MD, a resident at Montefiore Medical Center in New York, presented the case of a 62-year-old woman with hypertension who had profound generalized weakness and an inability to walk.
“She actually came to the hospital because she couldn’t lift a cup of tea,” Dr. Bressman told judges.
Clinicians traced her problem to that very tea – a licorice-containing brew – after an ECG indicated hypokalemia. A breakdown product of licorice, glycyrrhizic acid, can prevent the breakdown of cortisol into cortisone, causing increased absorption of sodium in exchange for potassium, he explained.
“I really like interesting cases – it’s something I’ve thought about throughout medical school,” Dr. Bressman said. “It’s been incredibly fun. We have great cases at Montefiore. ... It’s taught me to think very broadly and with an expansive differential.”
ORLANDO – Researchers presenting a case of starving ketoacidosis in a woman who was on a “Paleo” diet while breastfeeding won the Clinical Vignettes competition held Monday at HM18. The announcement capped a flurry of presenting and judging of posters on single cases that were captivating in both the stories they told and the lessons they taught.
The trainee award winner in the competition were presenters of a case of licorice-induced hypokalemia that, clinicians learned, was brought about by the drinking of an obscure kind of tea. The two others that made it into the final round of judging were on cases of syphilitic hepatitis and cardiac amyloidosis.
By chance, both of the winners highlighted dietary triggers, said Stephanie Sherman, MD, chair of the annual meeting’s clinical vignettes committee.
“The common themes in both of these were the importance of dietary history when interviewing patients,” Dr. Sherman said. “And then both had a beautiful review of the physiology that’s normal and how it gets broken in these situations.”
The Clinical Vignettes portion of the RIV competition, which also includes research and innovations categories, was separate this year because of space constraints, Dr. Sherman said.
Judges said they looked not only at how interesting and applicable each case was, but also the quality of the oral presentation and the poster’s visual appeal and clarity.
The ketoacidosis case, presented by Timothy Judson, MD, a resident at University of California, San Francisco, involved a 40-year-old woman who was previously healthy and had given birth 9 weeks earlier. Since the birth, the woman had been on a Paleo diet, a low-carbohydrate, ketogenic diet. She also was breastfeeding her newborn and continuing to breastfeed her 2-year-old son.
She presented with nonbilious, nonbloody emesis. On physical exam, she was found to be tachycardic, with diffuse tenderness of the abdomen. She was positive for ketones and had an elevated acetone level and elevated osmolar gap, the difference between the measured and calculated solutes in the serum.
Clinicians identified that low carbohydrate intake, high fat intake, and a high metabolic state, such as that brought on by breastfeeding, can contribute to ketoacidosis. She was treated with IV glucose-containing fluids, bicarbonate, fomepizole, and thiamine.
The case shows that patients should be warned about ketoacidosis risk when they start an ultra-low carbohydrate diet, especially if they are breastfeeding or lactating, Dr. Hudson said.
“Usually they’re safe, but they may not be if you’re in a high metabolic state,” he told judges.
“We take care of so many patients on a daily basis and we rarely get to tell their stories,” he said. “To be able to tell the story of the patients and give the learning points that we took away to others, I think is very rewarding.”
The winner of the trainee award, Maxwell Bressman, MD, a resident at Montefiore Medical Center in New York, presented the case of a 62-year-old woman with hypertension who had profound generalized weakness and an inability to walk.
“She actually came to the hospital because she couldn’t lift a cup of tea,” Dr. Bressman told judges.
Clinicians traced her problem to that very tea – a licorice-containing brew – after an ECG indicated hypokalemia. A breakdown product of licorice, glycyrrhizic acid, can prevent the breakdown of cortisol into cortisone, causing increased absorption of sodium in exchange for potassium, he explained.
“I really like interesting cases – it’s something I’ve thought about throughout medical school,” Dr. Bressman said. “It’s been incredibly fun. We have great cases at Montefiore. ... It’s taught me to think very broadly and with an expansive differential.”
ORLANDO – Researchers presenting a case of starving ketoacidosis in a woman who was on a “Paleo” diet while breastfeeding won the Clinical Vignettes competition held Monday at HM18. The announcement capped a flurry of presenting and judging of posters on single cases that were captivating in both the stories they told and the lessons they taught.
The trainee award winner in the competition were presenters of a case of licorice-induced hypokalemia that, clinicians learned, was brought about by the drinking of an obscure kind of tea. The two others that made it into the final round of judging were on cases of syphilitic hepatitis and cardiac amyloidosis.
By chance, both of the winners highlighted dietary triggers, said Stephanie Sherman, MD, chair of the annual meeting’s clinical vignettes committee.
“The common themes in both of these were the importance of dietary history when interviewing patients,” Dr. Sherman said. “And then both had a beautiful review of the physiology that’s normal and how it gets broken in these situations.”
The Clinical Vignettes portion of the RIV competition, which also includes research and innovations categories, was separate this year because of space constraints, Dr. Sherman said.
Judges said they looked not only at how interesting and applicable each case was, but also the quality of the oral presentation and the poster’s visual appeal and clarity.
The ketoacidosis case, presented by Timothy Judson, MD, a resident at University of California, San Francisco, involved a 40-year-old woman who was previously healthy and had given birth 9 weeks earlier. Since the birth, the woman had been on a Paleo diet, a low-carbohydrate, ketogenic diet. She also was breastfeeding her newborn and continuing to breastfeed her 2-year-old son.
She presented with nonbilious, nonbloody emesis. On physical exam, she was found to be tachycardic, with diffuse tenderness of the abdomen. She was positive for ketones and had an elevated acetone level and elevated osmolar gap, the difference between the measured and calculated solutes in the serum.
Clinicians identified that low carbohydrate intake, high fat intake, and a high metabolic state, such as that brought on by breastfeeding, can contribute to ketoacidosis. She was treated with IV glucose-containing fluids, bicarbonate, fomepizole, and thiamine.
The case shows that patients should be warned about ketoacidosis risk when they start an ultra-low carbohydrate diet, especially if they are breastfeeding or lactating, Dr. Hudson said.
“Usually they’re safe, but they may not be if you’re in a high metabolic state,” he told judges.
“We take care of so many patients on a daily basis and we rarely get to tell their stories,” he said. “To be able to tell the story of the patients and give the learning points that we took away to others, I think is very rewarding.”
The winner of the trainee award, Maxwell Bressman, MD, a resident at Montefiore Medical Center in New York, presented the case of a 62-year-old woman with hypertension who had profound generalized weakness and an inability to walk.
“She actually came to the hospital because she couldn’t lift a cup of tea,” Dr. Bressman told judges.
Clinicians traced her problem to that very tea – a licorice-containing brew – after an ECG indicated hypokalemia. A breakdown product of licorice, glycyrrhizic acid, can prevent the breakdown of cortisol into cortisone, causing increased absorption of sodium in exchange for potassium, he explained.
“I really like interesting cases – it’s something I’ve thought about throughout medical school,” Dr. Bressman said. “It’s been incredibly fun. We have great cases at Montefiore. ... It’s taught me to think very broadly and with an expansive differential.”
REPORTING FROM HOSPITAL MEDICINE 2018
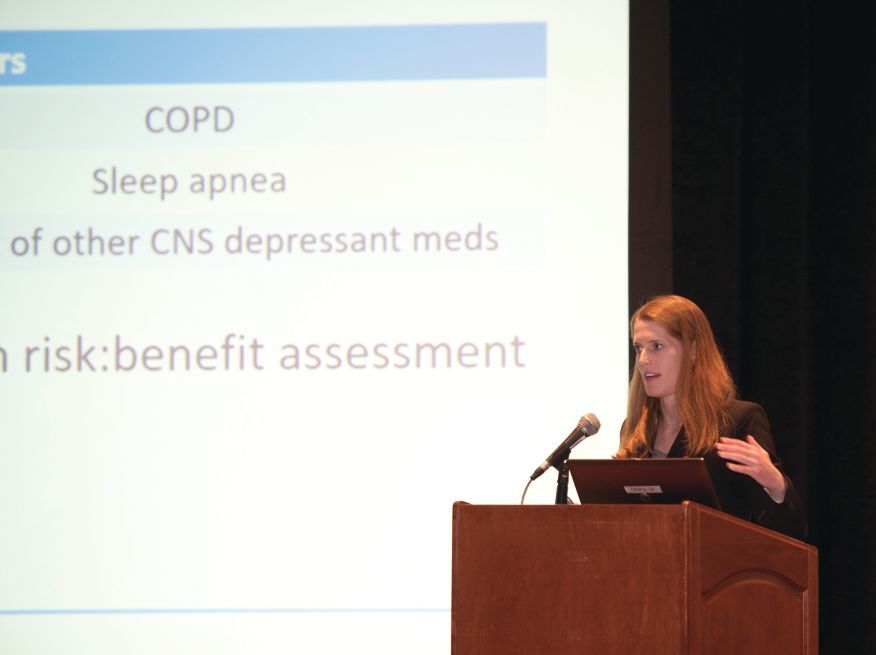
New guidance for inpatient opioid prescribing
ORLANDO – A new guidance statement for opioid prescribing for hospitalized adults who have acute noncancer pain has been issued by the Society for Hospital Medicine.
The statement comes after an exhaustive systematic review that found just four existing guidelines met inclusion criteria, though none focused specifically on acute pain in hospitalized adults.
Among the key issues taken from the existing guidelines and addressed in the new SHM guidance statement are deciding when opioids – or a nonopioid alternative – should be used, as well as selection of appropriate dose, route, and duration of administration. The guidance statement advises that clinicians prescribe the lowest effective opioid dose for the shortest duration possible.
Best practices for screening and monitoring before and during opioid initiation is another major focus, as is minimizing opioid-related adverse events, both by careful patient selection and by judicious prescribing.
Finally, the statement acknowledges that, when a discharge medication list includes an opioid prescription, there is potential risk for misuse or diversion. Accordingly, the recommendation is to limit the duration of outpatient prescribing to 7 days of medication, with consideration of a 3-5 day prescription.
An interactive session at the 2018 SHM annual meeting presenting the guidance statement focused less on marching through the guidance’s 16 specific statements, and more on teasing out the why, when, how – and how long – of inpatient opioid prescribing.
The well-attended session, led by two of the guideline authors, Shoshana Herzig, MD, MPH, and Teryl K. Nuckols, MD, FHM, began with Dr. Herzig, director of hospital medicine research at Beth Israel Deaconess Medical Center, Boston, making a compelling case for why guidance is needed for inpatient opioid prescribing for acute pain.
“Few would disagree that, at the end of the day, we are the final common pathway” for hospitalized patients who receive opioids, said Dr. Herzig. And there’s ample evidence that troublesome opioid prescribing is widespread, she said, adding that associated problems aren’t limited to such inpatient adverse events as falls, respiratory arrest, and acute kidney injury; plenty of opioid-exposed patients who leave the hospital continue to use opioids in problematic ways after discharge.
Of patients who were opioid naive and filled outpatient opioid prescriptions on discharge, “Almost half of patients were still using opioids 90 days later,” Dr. Herzig said. “Hospitals contribute to opioid initiation in millions of patients each year, so our prescribing patterns in the hospital do matter.”
“We tend to prescribe high doses,” said Dr. Herzig – an average of a 68-mg oral morphine equivalent (OME) dose on days that opioids were received, according to a 2014 study she coauthored. Overall, Dr. Herzig and her colleagues found that about 40% of patients who received opioids had a daily dose of at least 50 mg OME, and about a quarter received a daily dose at or exceeding 100 mg OME (Herzig et al. J Hosp Med. 2014 Feb;9[2]:73-81).
Further, she said, “We tend to prescribe a bit haphazardly.” The same study found wide variation in regional inpatient opioid-prescribing practices, with inpatients in the U.S. Midwest, South, and West seeing adjusted relative rates of exposure to opioids of 1.26, 1.33, and 1.37, compared with the Northeast, she said.
Among the more concerning findings, she said, was that “hospitals that prescribe opioids more frequently appear to do so less safely.” In hospitals that fell into the top quartile for inpatient opioid exposure, the overall rate of opioid-related adverse events was 0.39%, compared with 0.21% for hospitals in the bottom quartile of opioid prescribing, for an overall adjusted relative risk of 1.23 in opioid-exposed patients in the hospitals with the highest prescribing, said Dr. Herzig.
Dr. Nuckols, director of the division of general internal medicine at Cedars-Sinai Medical Center, Los Angeles, engaged attendees to identify challenges in acute pain management among hospitalized adults.
The audience was quick and prolific with answers, which included varying physician standards for opioid prescribing; patient expectations for pain management – and sometimes denial that opioid use has become a disorder; varying expectations for pain management among care team members who may be reluctant to let go of pain as “the fifth vital sign;” difficulty accessing and being reimbursed for nonpharmacologic strategies; and, acknowledged by all, patient satisfaction scores.
To this last point, Dr. Nuckols said that there have been “a few recent changes for the better.” The Joint Commission is revising its standards to move away from pain as a vital sign, toward a focused assessment of pain that considers how patients are responding to pain, as well as functional status. However, she said, “There aren’t any validated measures yet for how we’re going to do this.”
Similar shifts are underway with pain-related HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems) questions, which have undergone a “big pullback” from an emphasis on complete control of pain, and now put more focus on whether caregivers asked about pain and talked with inpatients about ways to treat pain, said Dr. Nuckols.
Speaking to the process of developing the guidance statement, Dr. Nuckols said that “I think it’s important to note that the empirical literature about managing pain for inpatients … is almost nonexistent.” Of the four criteria that met inclusion criteria – “and we were tough raters when it comes to the guidelines” – most were based on expert consensus, she said, and most had primarily an outpatient focus.
Themes that emerged from the review process included consideration of a nonopioid strategy before initiating an opioid. These might include pharmacologic interventions such as acetaminophen or a nonsteroidal anti-inflammatory for nociceptive pain, pregabalin, gabapentin, or other medication to manage neuropathic pain, or nonpharmacologic interventions such as heat, ice, or distraction. All of these should also be considered as adjuncts to minimize opioid dosing as well, said Dr. Nuckols, citing well-documented synergy with multiple modalities of pain treatment.
Careful patient selection is also key, said Dr. Nuckols. She noted that she asks herself, “How likely is this patient to get into trouble?” with inpatient opioid administration. A concept that goes hand-in-hand, she said, is choosing the appropriate dose and route.
Dr. Herzig picked up this theme, noting that route of administration matters. A speedy route, such as intravenous administration, has been shown to reinforce the potentially addictive effect of opioids. There are times when IV is the route to use, such as when the patient can’t take medication by mouth or when immediate pain control truly is needed. However, oral medication is just as effective, albeit slightly slower acting, she said.
Conversion from IV to oral opioids is a potential time for trouble, said Dr. Herzig. “Always use an opioid conversion chart,” she said. Cross-tolerance can be incomplete between opioids, so safe practice is to begin with about 50% of the OME dose with the new medication and titrate up. And don’t use a long-acting opioid for acute pain, she said, noting that not only will there be a long half-life and washout period if the dose is too high, but patient risk for later opioid use disorder is also upped with this strategy. “You can always add more, but it’s hard to take away,” said Dr. Herzig.
On discharge, consider whether an opioid should be prescribed at all, said Dr. Herzig. The guidance statement advises generally prescribing less than a 7-day supply, with the rationale that, if posthospitalization acute pain is severe enough to require an opioid at that point, the patient should have outpatient follow-up.
This approach doesn’t undertreat outpatient pain, said Dr. Herzig, pointing to studies that show that, at discharge, “the majority of opioids that patients are getting, they are not taking – which tells us that by definition we are overprescribing.”
The authors of the guidance statement wanted to address two important topics that were not sufficiently evidence backed, Dr. Herzig said. They had hoped to give clear guidance about best practices for communication and follow-up with outpatient providers after hospital discharge. Though they didn’t find clear guidance in this area, “We do believe that outpatient providers need to be kept in the loop.”
A second area, currently a hot button topic both in the medical community and in the lay press, is whether a naloxone prescription should accompany an opioid prescription at discharge. “There just aren’t studies for this,” said Dr. Herzig.
The full text of the guidance statement may be found here: https://www.journalofhospitalmedicine.com/jhospmed/article/161927/hospital-medicine/improving-safety-opioid-use-acute-noncancer-pain.
ORLANDO – A new guidance statement for opioid prescribing for hospitalized adults who have acute noncancer pain has been issued by the Society for Hospital Medicine.
The statement comes after an exhaustive systematic review that found just four existing guidelines met inclusion criteria, though none focused specifically on acute pain in hospitalized adults.
Among the key issues taken from the existing guidelines and addressed in the new SHM guidance statement are deciding when opioids – or a nonopioid alternative – should be used, as well as selection of appropriate dose, route, and duration of administration. The guidance statement advises that clinicians prescribe the lowest effective opioid dose for the shortest duration possible.
Best practices for screening and monitoring before and during opioid initiation is another major focus, as is minimizing opioid-related adverse events, both by careful patient selection and by judicious prescribing.
Finally, the statement acknowledges that, when a discharge medication list includes an opioid prescription, there is potential risk for misuse or diversion. Accordingly, the recommendation is to limit the duration of outpatient prescribing to 7 days of medication, with consideration of a 3-5 day prescription.
An interactive session at the 2018 SHM annual meeting presenting the guidance statement focused less on marching through the guidance’s 16 specific statements, and more on teasing out the why, when, how – and how long – of inpatient opioid prescribing.
The well-attended session, led by two of the guideline authors, Shoshana Herzig, MD, MPH, and Teryl K. Nuckols, MD, FHM, began with Dr. Herzig, director of hospital medicine research at Beth Israel Deaconess Medical Center, Boston, making a compelling case for why guidance is needed for inpatient opioid prescribing for acute pain.
“Few would disagree that, at the end of the day, we are the final common pathway” for hospitalized patients who receive opioids, said Dr. Herzig. And there’s ample evidence that troublesome opioid prescribing is widespread, she said, adding that associated problems aren’t limited to such inpatient adverse events as falls, respiratory arrest, and acute kidney injury; plenty of opioid-exposed patients who leave the hospital continue to use opioids in problematic ways after discharge.
Of patients who were opioid naive and filled outpatient opioid prescriptions on discharge, “Almost half of patients were still using opioids 90 days later,” Dr. Herzig said. “Hospitals contribute to opioid initiation in millions of patients each year, so our prescribing patterns in the hospital do matter.”
“We tend to prescribe high doses,” said Dr. Herzig – an average of a 68-mg oral morphine equivalent (OME) dose on days that opioids were received, according to a 2014 study she coauthored. Overall, Dr. Herzig and her colleagues found that about 40% of patients who received opioids had a daily dose of at least 50 mg OME, and about a quarter received a daily dose at or exceeding 100 mg OME (Herzig et al. J Hosp Med. 2014 Feb;9[2]:73-81).
Further, she said, “We tend to prescribe a bit haphazardly.” The same study found wide variation in regional inpatient opioid-prescribing practices, with inpatients in the U.S. Midwest, South, and West seeing adjusted relative rates of exposure to opioids of 1.26, 1.33, and 1.37, compared with the Northeast, she said.
Among the more concerning findings, she said, was that “hospitals that prescribe opioids more frequently appear to do so less safely.” In hospitals that fell into the top quartile for inpatient opioid exposure, the overall rate of opioid-related adverse events was 0.39%, compared with 0.21% for hospitals in the bottom quartile of opioid prescribing, for an overall adjusted relative risk of 1.23 in opioid-exposed patients in the hospitals with the highest prescribing, said Dr. Herzig.
Dr. Nuckols, director of the division of general internal medicine at Cedars-Sinai Medical Center, Los Angeles, engaged attendees to identify challenges in acute pain management among hospitalized adults.
The audience was quick and prolific with answers, which included varying physician standards for opioid prescribing; patient expectations for pain management – and sometimes denial that opioid use has become a disorder; varying expectations for pain management among care team members who may be reluctant to let go of pain as “the fifth vital sign;” difficulty accessing and being reimbursed for nonpharmacologic strategies; and, acknowledged by all, patient satisfaction scores.
To this last point, Dr. Nuckols said that there have been “a few recent changes for the better.” The Joint Commission is revising its standards to move away from pain as a vital sign, toward a focused assessment of pain that considers how patients are responding to pain, as well as functional status. However, she said, “There aren’t any validated measures yet for how we’re going to do this.”
Similar shifts are underway with pain-related HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems) questions, which have undergone a “big pullback” from an emphasis on complete control of pain, and now put more focus on whether caregivers asked about pain and talked with inpatients about ways to treat pain, said Dr. Nuckols.
Speaking to the process of developing the guidance statement, Dr. Nuckols said that “I think it’s important to note that the empirical literature about managing pain for inpatients … is almost nonexistent.” Of the four criteria that met inclusion criteria – “and we were tough raters when it comes to the guidelines” – most were based on expert consensus, she said, and most had primarily an outpatient focus.
Themes that emerged from the review process included consideration of a nonopioid strategy before initiating an opioid. These might include pharmacologic interventions such as acetaminophen or a nonsteroidal anti-inflammatory for nociceptive pain, pregabalin, gabapentin, or other medication to manage neuropathic pain, or nonpharmacologic interventions such as heat, ice, or distraction. All of these should also be considered as adjuncts to minimize opioid dosing as well, said Dr. Nuckols, citing well-documented synergy with multiple modalities of pain treatment.
Careful patient selection is also key, said Dr. Nuckols. She noted that she asks herself, “How likely is this patient to get into trouble?” with inpatient opioid administration. A concept that goes hand-in-hand, she said, is choosing the appropriate dose and route.
Dr. Herzig picked up this theme, noting that route of administration matters. A speedy route, such as intravenous administration, has been shown to reinforce the potentially addictive effect of opioids. There are times when IV is the route to use, such as when the patient can’t take medication by mouth or when immediate pain control truly is needed. However, oral medication is just as effective, albeit slightly slower acting, she said.
Conversion from IV to oral opioids is a potential time for trouble, said Dr. Herzig. “Always use an opioid conversion chart,” she said. Cross-tolerance can be incomplete between opioids, so safe practice is to begin with about 50% of the OME dose with the new medication and titrate up. And don’t use a long-acting opioid for acute pain, she said, noting that not only will there be a long half-life and washout period if the dose is too high, but patient risk for later opioid use disorder is also upped with this strategy. “You can always add more, but it’s hard to take away,” said Dr. Herzig.
On discharge, consider whether an opioid should be prescribed at all, said Dr. Herzig. The guidance statement advises generally prescribing less than a 7-day supply, with the rationale that, if posthospitalization acute pain is severe enough to require an opioid at that point, the patient should have outpatient follow-up.
This approach doesn’t undertreat outpatient pain, said Dr. Herzig, pointing to studies that show that, at discharge, “the majority of opioids that patients are getting, they are not taking – which tells us that by definition we are overprescribing.”
The authors of the guidance statement wanted to address two important topics that were not sufficiently evidence backed, Dr. Herzig said. They had hoped to give clear guidance about best practices for communication and follow-up with outpatient providers after hospital discharge. Though they didn’t find clear guidance in this area, “We do believe that outpatient providers need to be kept in the loop.”
A second area, currently a hot button topic both in the medical community and in the lay press, is whether a naloxone prescription should accompany an opioid prescription at discharge. “There just aren’t studies for this,” said Dr. Herzig.
The full text of the guidance statement may be found here: https://www.journalofhospitalmedicine.com/jhospmed/article/161927/hospital-medicine/improving-safety-opioid-use-acute-noncancer-pain.
ORLANDO – A new guidance statement for opioid prescribing for hospitalized adults who have acute noncancer pain has been issued by the Society for Hospital Medicine.
The statement comes after an exhaustive systematic review that found just four existing guidelines met inclusion criteria, though none focused specifically on acute pain in hospitalized adults.
Among the key issues taken from the existing guidelines and addressed in the new SHM guidance statement are deciding when opioids – or a nonopioid alternative – should be used, as well as selection of appropriate dose, route, and duration of administration. The guidance statement advises that clinicians prescribe the lowest effective opioid dose for the shortest duration possible.
Best practices for screening and monitoring before and during opioid initiation is another major focus, as is minimizing opioid-related adverse events, both by careful patient selection and by judicious prescribing.
Finally, the statement acknowledges that, when a discharge medication list includes an opioid prescription, there is potential risk for misuse or diversion. Accordingly, the recommendation is to limit the duration of outpatient prescribing to 7 days of medication, with consideration of a 3-5 day prescription.
An interactive session at the 2018 SHM annual meeting presenting the guidance statement focused less on marching through the guidance’s 16 specific statements, and more on teasing out the why, when, how – and how long – of inpatient opioid prescribing.
The well-attended session, led by two of the guideline authors, Shoshana Herzig, MD, MPH, and Teryl K. Nuckols, MD, FHM, began with Dr. Herzig, director of hospital medicine research at Beth Israel Deaconess Medical Center, Boston, making a compelling case for why guidance is needed for inpatient opioid prescribing for acute pain.
“Few would disagree that, at the end of the day, we are the final common pathway” for hospitalized patients who receive opioids, said Dr. Herzig. And there’s ample evidence that troublesome opioid prescribing is widespread, she said, adding that associated problems aren’t limited to such inpatient adverse events as falls, respiratory arrest, and acute kidney injury; plenty of opioid-exposed patients who leave the hospital continue to use opioids in problematic ways after discharge.
Of patients who were opioid naive and filled outpatient opioid prescriptions on discharge, “Almost half of patients were still using opioids 90 days later,” Dr. Herzig said. “Hospitals contribute to opioid initiation in millions of patients each year, so our prescribing patterns in the hospital do matter.”
“We tend to prescribe high doses,” said Dr. Herzig – an average of a 68-mg oral morphine equivalent (OME) dose on days that opioids were received, according to a 2014 study she coauthored. Overall, Dr. Herzig and her colleagues found that about 40% of patients who received opioids had a daily dose of at least 50 mg OME, and about a quarter received a daily dose at or exceeding 100 mg OME (Herzig et al. J Hosp Med. 2014 Feb;9[2]:73-81).
Further, she said, “We tend to prescribe a bit haphazardly.” The same study found wide variation in regional inpatient opioid-prescribing practices, with inpatients in the U.S. Midwest, South, and West seeing adjusted relative rates of exposure to opioids of 1.26, 1.33, and 1.37, compared with the Northeast, she said.
Among the more concerning findings, she said, was that “hospitals that prescribe opioids more frequently appear to do so less safely.” In hospitals that fell into the top quartile for inpatient opioid exposure, the overall rate of opioid-related adverse events was 0.39%, compared with 0.21% for hospitals in the bottom quartile of opioid prescribing, for an overall adjusted relative risk of 1.23 in opioid-exposed patients in the hospitals with the highest prescribing, said Dr. Herzig.
Dr. Nuckols, director of the division of general internal medicine at Cedars-Sinai Medical Center, Los Angeles, engaged attendees to identify challenges in acute pain management among hospitalized adults.
The audience was quick and prolific with answers, which included varying physician standards for opioid prescribing; patient expectations for pain management – and sometimes denial that opioid use has become a disorder; varying expectations for pain management among care team members who may be reluctant to let go of pain as “the fifth vital sign;” difficulty accessing and being reimbursed for nonpharmacologic strategies; and, acknowledged by all, patient satisfaction scores.
To this last point, Dr. Nuckols said that there have been “a few recent changes for the better.” The Joint Commission is revising its standards to move away from pain as a vital sign, toward a focused assessment of pain that considers how patients are responding to pain, as well as functional status. However, she said, “There aren’t any validated measures yet for how we’re going to do this.”
Similar shifts are underway with pain-related HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems) questions, which have undergone a “big pullback” from an emphasis on complete control of pain, and now put more focus on whether caregivers asked about pain and talked with inpatients about ways to treat pain, said Dr. Nuckols.
Speaking to the process of developing the guidance statement, Dr. Nuckols said that “I think it’s important to note that the empirical literature about managing pain for inpatients … is almost nonexistent.” Of the four criteria that met inclusion criteria – “and we were tough raters when it comes to the guidelines” – most were based on expert consensus, she said, and most had primarily an outpatient focus.
Themes that emerged from the review process included consideration of a nonopioid strategy before initiating an opioid. These might include pharmacologic interventions such as acetaminophen or a nonsteroidal anti-inflammatory for nociceptive pain, pregabalin, gabapentin, or other medication to manage neuropathic pain, or nonpharmacologic interventions such as heat, ice, or distraction. All of these should also be considered as adjuncts to minimize opioid dosing as well, said Dr. Nuckols, citing well-documented synergy with multiple modalities of pain treatment.
Careful patient selection is also key, said Dr. Nuckols. She noted that she asks herself, “How likely is this patient to get into trouble?” with inpatient opioid administration. A concept that goes hand-in-hand, she said, is choosing the appropriate dose and route.
Dr. Herzig picked up this theme, noting that route of administration matters. A speedy route, such as intravenous administration, has been shown to reinforce the potentially addictive effect of opioids. There are times when IV is the route to use, such as when the patient can’t take medication by mouth or when immediate pain control truly is needed. However, oral medication is just as effective, albeit slightly slower acting, she said.
Conversion from IV to oral opioids is a potential time for trouble, said Dr. Herzig. “Always use an opioid conversion chart,” she said. Cross-tolerance can be incomplete between opioids, so safe practice is to begin with about 50% of the OME dose with the new medication and titrate up. And don’t use a long-acting opioid for acute pain, she said, noting that not only will there be a long half-life and washout period if the dose is too high, but patient risk for later opioid use disorder is also upped with this strategy. “You can always add more, but it’s hard to take away,” said Dr. Herzig.
On discharge, consider whether an opioid should be prescribed at all, said Dr. Herzig. The guidance statement advises generally prescribing less than a 7-day supply, with the rationale that, if posthospitalization acute pain is severe enough to require an opioid at that point, the patient should have outpatient follow-up.
This approach doesn’t undertreat outpatient pain, said Dr. Herzig, pointing to studies that show that, at discharge, “the majority of opioids that patients are getting, they are not taking – which tells us that by definition we are overprescribing.”
The authors of the guidance statement wanted to address two important topics that were not sufficiently evidence backed, Dr. Herzig said. They had hoped to give clear guidance about best practices for communication and follow-up with outpatient providers after hospital discharge. Though they didn’t find clear guidance in this area, “We do believe that outpatient providers need to be kept in the loop.”
A second area, currently a hot button topic both in the medical community and in the lay press, is whether a naloxone prescription should accompany an opioid prescription at discharge. “There just aren’t studies for this,” said Dr. Herzig.
The full text of the guidance statement may be found here: https://www.journalofhospitalmedicine.com/jhospmed/article/161927/hospital-medicine/improving-safety-opioid-use-acute-noncancer-pain.
REPORTING FROM HM18
Video : The SHM Research Committee: Expanding the role and footprint of research in hospital medicine
ORLANDO – In a video interview, Stephanie Mueller, MD, SFHM, of Brigham and Women’s Hospital, Boston, discusses the scope and importance of the SHM Research Committee.
One of its most important roles is overseeing the yearly Scientific Abstract and Poster Competition, known as the Research, Innovations and Clinical Vignettes (RIV) portion of the annual conference, which brings the best of current research in hospital medicine, especially in the increasingly important area of value in patient care, to the members.
In discussing the work of the committee, Dr. Mueller – who is in her third year as a member – adds that they “are working to expand the research footprint within the Society of Hospital Medicine,” including implementing initiatives such as the VIP program, which is a visiting professorship in which junior and mid-level faculty can do an exchange program between institutions.
ORLANDO – In a video interview, Stephanie Mueller, MD, SFHM, of Brigham and Women’s Hospital, Boston, discusses the scope and importance of the SHM Research Committee.
One of its most important roles is overseeing the yearly Scientific Abstract and Poster Competition, known as the Research, Innovations and Clinical Vignettes (RIV) portion of the annual conference, which brings the best of current research in hospital medicine, especially in the increasingly important area of value in patient care, to the members.
In discussing the work of the committee, Dr. Mueller – who is in her third year as a member – adds that they “are working to expand the research footprint within the Society of Hospital Medicine,” including implementing initiatives such as the VIP program, which is a visiting professorship in which junior and mid-level faculty can do an exchange program between institutions.
ORLANDO – In a video interview, Stephanie Mueller, MD, SFHM, of Brigham and Women’s Hospital, Boston, discusses the scope and importance of the SHM Research Committee.
One of its most important roles is overseeing the yearly Scientific Abstract and Poster Competition, known as the Research, Innovations and Clinical Vignettes (RIV) portion of the annual conference, which brings the best of current research in hospital medicine, especially in the increasingly important area of value in patient care, to the members.
In discussing the work of the committee, Dr. Mueller – who is in her third year as a member – adds that they “are working to expand the research footprint within the Society of Hospital Medicine,” including implementing initiatives such as the VIP program, which is a visiting professorship in which junior and mid-level faculty can do an exchange program between institutions.
REPORTING FROM HOSPITAL MEDICINE 2018