User login
Severe early-life respiratory infections heighten pediatric OSA risk
AIRWAYS DISORDERS NETWORK
Pediatric Chest Medicine Section
Children with severe lower respiratory tract infections (LRTIs) within the first 2 years of life had a 2.06-fold increased risk of developing pediatric OSA by age 5, according to a study comparing patients hospitalized with LRTI to controls without severe LRTI.1 Prior studies linked LRTI and OSA, but the impact of LRTI severity was unknown.2,3,4 They used Kaplan-Meier survival estimates and Cox proportional hazards models to evaluate the risk of OSA.
Compared with patients with severe LRTIs, controls were more likely to have been full-term births, delivered vaginally, and breastfed. The OSA rate was significantly higher among children with severe LRTIs compared with controls (14.7% vs 6.8%). In the adjusted model controlling for relevant maternal and infant covariables, severe LRTI was significantly associated with increased OSA risk (HR, 2.06; 95% CI, 1.41-3.02; P < .001). Other factors such as prematurity (HR, 1.34; 95% CI, 1.01-1.77; P = .039) and maternal obesity (HR, 1.82; 95% CI, 1.32-2.52; P < .001) were also associated with increased OSA risk.
Maria Gutierrez, MD, of the Division of Pediatric Allergy, Immunology, and Rheumatology at Johns Hopkins University School of Medicine in Baltimore led the research. The study was published in Pediatric Pulmonology (2023 Dec 2. doi: 10.1002/ppul.26810). Study limitations included the use of electronic medical record data and potential lack of generalizability. The BBC is supported by the NIH.
– Agnes S. Montgomery, MD
Fellow-in-Training
References
1. Gayoso-Liviac MG, Nino G, Montgomery AS, Hong X, Wang X, Gutierrez MJ. Infants hospitalized with lower respiratory tract infections during the first two years of life have increased risk of pediatric obstructive sleep apnea. Pediatr Pulmonol. 2024;59:679-687.
2. Snow A, Dayyat E, Montgomery‐Downs HE, Kheirandish‐Gozal L, Gozal D. Pediatric obstructive sleep apnea: a potential late consequence of respiratory syncytial virus bronchiolitis. Pediatr Pulmonol. 2009;44(12):1186‐1191.
3. Chen VC‐H, Yang Y‐H, Kuo T‐Y, et al. Increased incidence of obstructive sleep apnea in hospitalized children after enterovirus infection: a nationwide population‐based cohort study. Pediatr Infect Dis J. 2018;37(9):872‐879.
4. Gutierrez MJ, Nino G, Landeo‐Gutierrez JS, et al. Lower respiratory tract infections in early life are associated with obstructive sleep apnea diagnosis during childhood in a large birth cohort. Sleep. 2021;44:12.
AIRWAYS DISORDERS NETWORK
Pediatric Chest Medicine Section
Children with severe lower respiratory tract infections (LRTIs) within the first 2 years of life had a 2.06-fold increased risk of developing pediatric OSA by age 5, according to a study comparing patients hospitalized with LRTI to controls without severe LRTI.1 Prior studies linked LRTI and OSA, but the impact of LRTI severity was unknown.2,3,4 They used Kaplan-Meier survival estimates and Cox proportional hazards models to evaluate the risk of OSA.
Compared with patients with severe LRTIs, controls were more likely to have been full-term births, delivered vaginally, and breastfed. The OSA rate was significantly higher among children with severe LRTIs compared with controls (14.7% vs 6.8%). In the adjusted model controlling for relevant maternal and infant covariables, severe LRTI was significantly associated with increased OSA risk (HR, 2.06; 95% CI, 1.41-3.02; P < .001). Other factors such as prematurity (HR, 1.34; 95% CI, 1.01-1.77; P = .039) and maternal obesity (HR, 1.82; 95% CI, 1.32-2.52; P < .001) were also associated with increased OSA risk.
Maria Gutierrez, MD, of the Division of Pediatric Allergy, Immunology, and Rheumatology at Johns Hopkins University School of Medicine in Baltimore led the research. The study was published in Pediatric Pulmonology (2023 Dec 2. doi: 10.1002/ppul.26810). Study limitations included the use of electronic medical record data and potential lack of generalizability. The BBC is supported by the NIH.
– Agnes S. Montgomery, MD
Fellow-in-Training
References
1. Gayoso-Liviac MG, Nino G, Montgomery AS, Hong X, Wang X, Gutierrez MJ. Infants hospitalized with lower respiratory tract infections during the first two years of life have increased risk of pediatric obstructive sleep apnea. Pediatr Pulmonol. 2024;59:679-687.
2. Snow A, Dayyat E, Montgomery‐Downs HE, Kheirandish‐Gozal L, Gozal D. Pediatric obstructive sleep apnea: a potential late consequence of respiratory syncytial virus bronchiolitis. Pediatr Pulmonol. 2009;44(12):1186‐1191.
3. Chen VC‐H, Yang Y‐H, Kuo T‐Y, et al. Increased incidence of obstructive sleep apnea in hospitalized children after enterovirus infection: a nationwide population‐based cohort study. Pediatr Infect Dis J. 2018;37(9):872‐879.
4. Gutierrez MJ, Nino G, Landeo‐Gutierrez JS, et al. Lower respiratory tract infections in early life are associated with obstructive sleep apnea diagnosis during childhood in a large birth cohort. Sleep. 2021;44:12.
AIRWAYS DISORDERS NETWORK
Pediatric Chest Medicine Section
Children with severe lower respiratory tract infections (LRTIs) within the first 2 years of life had a 2.06-fold increased risk of developing pediatric OSA by age 5, according to a study comparing patients hospitalized with LRTI to controls without severe LRTI.1 Prior studies linked LRTI and OSA, but the impact of LRTI severity was unknown.2,3,4 They used Kaplan-Meier survival estimates and Cox proportional hazards models to evaluate the risk of OSA.
Compared with patients with severe LRTIs, controls were more likely to have been full-term births, delivered vaginally, and breastfed. The OSA rate was significantly higher among children with severe LRTIs compared with controls (14.7% vs 6.8%). In the adjusted model controlling for relevant maternal and infant covariables, severe LRTI was significantly associated with increased OSA risk (HR, 2.06; 95% CI, 1.41-3.02; P < .001). Other factors such as prematurity (HR, 1.34; 95% CI, 1.01-1.77; P = .039) and maternal obesity (HR, 1.82; 95% CI, 1.32-2.52; P < .001) were also associated with increased OSA risk.
Maria Gutierrez, MD, of the Division of Pediatric Allergy, Immunology, and Rheumatology at Johns Hopkins University School of Medicine in Baltimore led the research. The study was published in Pediatric Pulmonology (2023 Dec 2. doi: 10.1002/ppul.26810). Study limitations included the use of electronic medical record data and potential lack of generalizability. The BBC is supported by the NIH.
– Agnes S. Montgomery, MD
Fellow-in-Training
References
1. Gayoso-Liviac MG, Nino G, Montgomery AS, Hong X, Wang X, Gutierrez MJ. Infants hospitalized with lower respiratory tract infections during the first two years of life have increased risk of pediatric obstructive sleep apnea. Pediatr Pulmonol. 2024;59:679-687.
2. Snow A, Dayyat E, Montgomery‐Downs HE, Kheirandish‐Gozal L, Gozal D. Pediatric obstructive sleep apnea: a potential late consequence of respiratory syncytial virus bronchiolitis. Pediatr Pulmonol. 2009;44(12):1186‐1191.
3. Chen VC‐H, Yang Y‐H, Kuo T‐Y, et al. Increased incidence of obstructive sleep apnea in hospitalized children after enterovirus infection: a nationwide population‐based cohort study. Pediatr Infect Dis J. 2018;37(9):872‐879.
4. Gutierrez MJ, Nino G, Landeo‐Gutierrez JS, et al. Lower respiratory tract infections in early life are associated with obstructive sleep apnea diagnosis during childhood in a large birth cohort. Sleep. 2021;44:12.
Electrical impedance tomography: Visualization and integration of the impact of mechanical ventilation
CRITICAL CARE NETWORK
Mechanical Ventilation and Airways Management Section
1,2,3 Continuous monitoring of the tidal volume, plateau pressure, and positive end-expiratory pressure (PEEP) is crucial to maintain LPV. Electrical impedance tomography (EIT) is a noninvasive, radiation-free, imaging method of the electrical conductivity distribution inside the human body.4 Integrating EIT into invasive mechanical ventilation allows imaging of the regional lung ventilation as affected by the mechanical ventilation settings as well as the patient position. It can also provide a personalized approach to determining the optimum ventilatory settings based on individual patient conditions.5,6
Optimum PEEP titration is crucial to prevent lung collapse as well as overdistension. In a single-center, randomized, crossover pilot study of 12 patients, optimum PEEP titration was carried out using a high PEEP/FiO2 table vs EIT in moderate to severe ARDS. The primary endpoint was the reduction of mechanical power, which was consistently lower in the EIT group.7 EIT also allows the assessment of regional compliance of the lungs. There are reports regarding the superiority of regional compliance of lung over global compliance in achieving better gas exchange, lung compliance, and weaning of mechanical ventilation.8 EIT could assess the patient’s response to prone positioning by illustrating the change in the functional residual capacity between supine and prone positioning.9 In addition, by visualization of the ventilated areas during spontaneous breathing and reduction of pressure support, EIT could help in weaning off the mechanical ventilation.10
In conclusion, EIT can be a tool to provide safe and personalized mechanical ventilation in patients with respiratory failure. However, there are limited data regarding its use and application, which might become an interesting subject for future clinical research.
– Akram M. Zaaqoq, MD, MPH
Member-at-Large
References
1. Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347-354.
2. Brower RG, Matthay MA, Morris A, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
3. Neto AS, Simonis FD, Barbas CSV, et al. Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome: a systematic review and individual patient data analysis. Crit Care Med. 2015;43(10):2155-2163.
4. Adler A, Boyle A. Electrical impedance tomography: tissue properties to image measures. IEEE Trans Biomed Eng. 2017;64(11):2494-2504.
5. Jang GY, Ayoub G, Kim YE, et al. Integrated EIT system for functional lung ventilation imaging. Biomed Eng Online. 2019;18(1):83.
6. Sella N, Pettenuzzo T, Zarantonello F, et al. Electrical impedance tomography: a compass for the safe route to optimal PEEP. Respir Med. 2021;187:106555.
7. Jimenez JV, Munroe E, Weirauch AJ, et al. Electric impedance tomography-guided PEEP titration reduces mechanical power in ARDS: a randomized crossover pilot trial. Crit Care. 2023;27(1):21.
8. Costa ELV, Borges JB, Melo A, et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35(6):1132-1137.9. Riera J, Pérez P, Cortés J, Roca O, Masclans JR, Rello J. Effect of high-flow nasal cannula and body position on end-expiratory lung volume: a cohort study using electrical impedance tomography. Respir Care. 2013;58(4):589-596.10. Wisse JJ, Goos TG, Jonkman AH, et al. Electrical impedance tomography as a monitoring tool during weaning from mechanical ventilation: an observational study during the spontaneous breathing trial. Respir Res. 2024;25(1):179.
CRITICAL CARE NETWORK
Mechanical Ventilation and Airways Management Section
1,2,3 Continuous monitoring of the tidal volume, plateau pressure, and positive end-expiratory pressure (PEEP) is crucial to maintain LPV. Electrical impedance tomography (EIT) is a noninvasive, radiation-free, imaging method of the electrical conductivity distribution inside the human body.4 Integrating EIT into invasive mechanical ventilation allows imaging of the regional lung ventilation as affected by the mechanical ventilation settings as well as the patient position. It can also provide a personalized approach to determining the optimum ventilatory settings based on individual patient conditions.5,6
Optimum PEEP titration is crucial to prevent lung collapse as well as overdistension. In a single-center, randomized, crossover pilot study of 12 patients, optimum PEEP titration was carried out using a high PEEP/FiO2 table vs EIT in moderate to severe ARDS. The primary endpoint was the reduction of mechanical power, which was consistently lower in the EIT group.7 EIT also allows the assessment of regional compliance of the lungs. There are reports regarding the superiority of regional compliance of lung over global compliance in achieving better gas exchange, lung compliance, and weaning of mechanical ventilation.8 EIT could assess the patient’s response to prone positioning by illustrating the change in the functional residual capacity between supine and prone positioning.9 In addition, by visualization of the ventilated areas during spontaneous breathing and reduction of pressure support, EIT could help in weaning off the mechanical ventilation.10
In conclusion, EIT can be a tool to provide safe and personalized mechanical ventilation in patients with respiratory failure. However, there are limited data regarding its use and application, which might become an interesting subject for future clinical research.
– Akram M. Zaaqoq, MD, MPH
Member-at-Large
References
1. Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347-354.
2. Brower RG, Matthay MA, Morris A, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
3. Neto AS, Simonis FD, Barbas CSV, et al. Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome: a systematic review and individual patient data analysis. Crit Care Med. 2015;43(10):2155-2163.
4. Adler A, Boyle A. Electrical impedance tomography: tissue properties to image measures. IEEE Trans Biomed Eng. 2017;64(11):2494-2504.
5. Jang GY, Ayoub G, Kim YE, et al. Integrated EIT system for functional lung ventilation imaging. Biomed Eng Online. 2019;18(1):83.
6. Sella N, Pettenuzzo T, Zarantonello F, et al. Electrical impedance tomography: a compass for the safe route to optimal PEEP. Respir Med. 2021;187:106555.
7. Jimenez JV, Munroe E, Weirauch AJ, et al. Electric impedance tomography-guided PEEP titration reduces mechanical power in ARDS: a randomized crossover pilot trial. Crit Care. 2023;27(1):21.
8. Costa ELV, Borges JB, Melo A, et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35(6):1132-1137.9. Riera J, Pérez P, Cortés J, Roca O, Masclans JR, Rello J. Effect of high-flow nasal cannula and body position on end-expiratory lung volume: a cohort study using electrical impedance tomography. Respir Care. 2013;58(4):589-596.10. Wisse JJ, Goos TG, Jonkman AH, et al. Electrical impedance tomography as a monitoring tool during weaning from mechanical ventilation: an observational study during the spontaneous breathing trial. Respir Res. 2024;25(1):179.
CRITICAL CARE NETWORK
Mechanical Ventilation and Airways Management Section
1,2,3 Continuous monitoring of the tidal volume, plateau pressure, and positive end-expiratory pressure (PEEP) is crucial to maintain LPV. Electrical impedance tomography (EIT) is a noninvasive, radiation-free, imaging method of the electrical conductivity distribution inside the human body.4 Integrating EIT into invasive mechanical ventilation allows imaging of the regional lung ventilation as affected by the mechanical ventilation settings as well as the patient position. It can also provide a personalized approach to determining the optimum ventilatory settings based on individual patient conditions.5,6
Optimum PEEP titration is crucial to prevent lung collapse as well as overdistension. In a single-center, randomized, crossover pilot study of 12 patients, optimum PEEP titration was carried out using a high PEEP/FiO2 table vs EIT in moderate to severe ARDS. The primary endpoint was the reduction of mechanical power, which was consistently lower in the EIT group.7 EIT also allows the assessment of regional compliance of the lungs. There are reports regarding the superiority of regional compliance of lung over global compliance in achieving better gas exchange, lung compliance, and weaning of mechanical ventilation.8 EIT could assess the patient’s response to prone positioning by illustrating the change in the functional residual capacity between supine and prone positioning.9 In addition, by visualization of the ventilated areas during spontaneous breathing and reduction of pressure support, EIT could help in weaning off the mechanical ventilation.10
In conclusion, EIT can be a tool to provide safe and personalized mechanical ventilation in patients with respiratory failure. However, there are limited data regarding its use and application, which might become an interesting subject for future clinical research.
– Akram M. Zaaqoq, MD, MPH
Member-at-Large
References
1. Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347-354.
2. Brower RG, Matthay MA, Morris A, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
3. Neto AS, Simonis FD, Barbas CSV, et al. Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome: a systematic review and individual patient data analysis. Crit Care Med. 2015;43(10):2155-2163.
4. Adler A, Boyle A. Electrical impedance tomography: tissue properties to image measures. IEEE Trans Biomed Eng. 2017;64(11):2494-2504.
5. Jang GY, Ayoub G, Kim YE, et al. Integrated EIT system for functional lung ventilation imaging. Biomed Eng Online. 2019;18(1):83.
6. Sella N, Pettenuzzo T, Zarantonello F, et al. Electrical impedance tomography: a compass for the safe route to optimal PEEP. Respir Med. 2021;187:106555.
7. Jimenez JV, Munroe E, Weirauch AJ, et al. Electric impedance tomography-guided PEEP titration reduces mechanical power in ARDS: a randomized crossover pilot trial. Crit Care. 2023;27(1):21.
8. Costa ELV, Borges JB, Melo A, et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35(6):1132-1137.9. Riera J, Pérez P, Cortés J, Roca O, Masclans JR, Rello J. Effect of high-flow nasal cannula and body position on end-expiratory lung volume: a cohort study using electrical impedance tomography. Respir Care. 2013;58(4):589-596.10. Wisse JJ, Goos TG, Jonkman AH, et al. Electrical impedance tomography as a monitoring tool during weaning from mechanical ventilation: an observational study during the spontaneous breathing trial. Respir Res. 2024;25(1):179.
Top reads from the CHEST journal portfolio
Malnutrition in critically ill patients, MODE trial findings, and guideline alignment in COPD
Journal CHEST® | The Association Between Malnutrition and High Protein Treatment on Outcomes in Critically Ill Patients
By: Charles Chin Han Lew, PhD, et al
Current international critical care guidelines based on expert opinion recommend high protein treatment (average 1.6 g/kg/d) for critically ill patients diagnosed with preexisting malnutrition to improve clinical outcomes. This multicenter, randomized controlled clinical trial investigated the effects of high vs usual protein treatment in 1,301 critically ill patients across 16 countries. Preexisting malnutrition was independently associated with the primary outcome of slower time to discharge alive (TTDA) (adjusted hazard ratio, 0.81; 95% CI, 0.67-0.98). However, high protein treatment in patients with and without preexisting malnutrition was not associated with TTDA (adjusted hazard ratios of 0.84 [95% CI, 0.63-1.11] and 0.97 [95% CI, 0.77-1.21]). Furthermore, no effect modification was observed (ratio of adjusted hazard ratio, 0.84; 95% CI, 0.58-1.20).
Most importantly, this study demonstrated an association between malnutrition and slower TTDA; however, this association was not modified by high protein treatment. This research challenges current international critical care nutrition guidelines.
– Commentary by Mary Jo S. Farmer, MD, PhD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Critical Care | Protocol and Statistical Analysis Plan for the Mode of Ventilation During Critical Illness (MODE) Trial
By: Kevin P. Seitz, MD, et al
The Mode of Ventilation During Critical Illness (MODE) trial is a cluster-randomized, multiple-crossover pilot study conducted in a medical ICU exploring how different mechanical ventilation modes affect ventilator-free days in critically ill patients. This trial aims to determine which ventilation mode maximizes the days patients spend alive without invasive ventilation. By switching between ventilation modes each month, the study ensures a thorough assessment under uniform clinical conditions. The trial’s protocol and statistical analysis plan were defined before the end of enrollment, which bolsters the rigor, reproducibility, and transparency of the findings. Initial findings indicate the necessity for an expanded, multicenter trial to definitively identify the optimal ventilation mode, as current data do not universally prefer one method over others. This research has significant implications for clinical practice, potentially altering mechanical ventilation guidelines and improving patient outcomes by reducing the time spent on mechanical ventilation.
– Commentary by Dharani Narendra, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary | Guideline Alignment and Medication Concordance in COPD
By: Meredith A. Chase, MD, MHS, et al
Over the past 10 years, a number of studies from generalists and specialists have consistently shown a lack of compliance between physician prescriptions and the Global Initiative for Chronic Obstructive Lung Disease strategy’s recommendations. This study aligns with prior research conducted in the same field. The inappropriate use of maintenance inhalers and the excessive use of inhaled corticosteroids are contributing factors to the skyrocketing expenses of managing COPD despite a slight decrease in prevalence. Overall, the results of all these studies are somewhat unsettling.
Nonetheless, there are a number of factors that are either unavoidable or difficult to address. First, primary care providers (PCPs) are less knowledgeable about the most recent recommendations and guidelines than specialists are. Second, the managed care companies and their PCPs are sometimes reluctant to refer patients to a specialist, resulting in delayed diagnosis and, at times, wrong diagnosis and mismanagement. Third, managed health care organizations have limited drugs for managing COPD on their formularies, limiting the ability of the provider to prescribe guideline-recommended treatments. Lastly, and very regrettably, the number of primary care doctors is decreasing, which is influencing patients’ ability to connect with someone who possesses the clinical expertise to assist them.
Future studies, projects, and endeavors ought to focus on solutions that could lessen these obstacles and provide patients and physicians more education, authority, and autonomy.
– Commentary by Humayun Anjum, MD, FCCP, Member of the CHEST Physician Editorial Board
Malnutrition in critically ill patients, MODE trial findings, and guideline alignment in COPD
Malnutrition in critically ill patients, MODE trial findings, and guideline alignment in COPD
Journal CHEST® | The Association Between Malnutrition and High Protein Treatment on Outcomes in Critically Ill Patients
By: Charles Chin Han Lew, PhD, et al
Current international critical care guidelines based on expert opinion recommend high protein treatment (average 1.6 g/kg/d) for critically ill patients diagnosed with preexisting malnutrition to improve clinical outcomes. This multicenter, randomized controlled clinical trial investigated the effects of high vs usual protein treatment in 1,301 critically ill patients across 16 countries. Preexisting malnutrition was independently associated with the primary outcome of slower time to discharge alive (TTDA) (adjusted hazard ratio, 0.81; 95% CI, 0.67-0.98). However, high protein treatment in patients with and without preexisting malnutrition was not associated with TTDA (adjusted hazard ratios of 0.84 [95% CI, 0.63-1.11] and 0.97 [95% CI, 0.77-1.21]). Furthermore, no effect modification was observed (ratio of adjusted hazard ratio, 0.84; 95% CI, 0.58-1.20).
Most importantly, this study demonstrated an association between malnutrition and slower TTDA; however, this association was not modified by high protein treatment. This research challenges current international critical care nutrition guidelines.
– Commentary by Mary Jo S. Farmer, MD, PhD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Critical Care | Protocol and Statistical Analysis Plan for the Mode of Ventilation During Critical Illness (MODE) Trial
By: Kevin P. Seitz, MD, et al
The Mode of Ventilation During Critical Illness (MODE) trial is a cluster-randomized, multiple-crossover pilot study conducted in a medical ICU exploring how different mechanical ventilation modes affect ventilator-free days in critically ill patients. This trial aims to determine which ventilation mode maximizes the days patients spend alive without invasive ventilation. By switching between ventilation modes each month, the study ensures a thorough assessment under uniform clinical conditions. The trial’s protocol and statistical analysis plan were defined before the end of enrollment, which bolsters the rigor, reproducibility, and transparency of the findings. Initial findings indicate the necessity for an expanded, multicenter trial to definitively identify the optimal ventilation mode, as current data do not universally prefer one method over others. This research has significant implications for clinical practice, potentially altering mechanical ventilation guidelines and improving patient outcomes by reducing the time spent on mechanical ventilation.
– Commentary by Dharani Narendra, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary | Guideline Alignment and Medication Concordance in COPD
By: Meredith A. Chase, MD, MHS, et al
Over the past 10 years, a number of studies from generalists and specialists have consistently shown a lack of compliance between physician prescriptions and the Global Initiative for Chronic Obstructive Lung Disease strategy’s recommendations. This study aligns with prior research conducted in the same field. The inappropriate use of maintenance inhalers and the excessive use of inhaled corticosteroids are contributing factors to the skyrocketing expenses of managing COPD despite a slight decrease in prevalence. Overall, the results of all these studies are somewhat unsettling.
Nonetheless, there are a number of factors that are either unavoidable or difficult to address. First, primary care providers (PCPs) are less knowledgeable about the most recent recommendations and guidelines than specialists are. Second, the managed care companies and their PCPs are sometimes reluctant to refer patients to a specialist, resulting in delayed diagnosis and, at times, wrong diagnosis and mismanagement. Third, managed health care organizations have limited drugs for managing COPD on their formularies, limiting the ability of the provider to prescribe guideline-recommended treatments. Lastly, and very regrettably, the number of primary care doctors is decreasing, which is influencing patients’ ability to connect with someone who possesses the clinical expertise to assist them.
Future studies, projects, and endeavors ought to focus on solutions that could lessen these obstacles and provide patients and physicians more education, authority, and autonomy.
– Commentary by Humayun Anjum, MD, FCCP, Member of the CHEST Physician Editorial Board
Journal CHEST® | The Association Between Malnutrition and High Protein Treatment on Outcomes in Critically Ill Patients
By: Charles Chin Han Lew, PhD, et al
Current international critical care guidelines based on expert opinion recommend high protein treatment (average 1.6 g/kg/d) for critically ill patients diagnosed with preexisting malnutrition to improve clinical outcomes. This multicenter, randomized controlled clinical trial investigated the effects of high vs usual protein treatment in 1,301 critically ill patients across 16 countries. Preexisting malnutrition was independently associated with the primary outcome of slower time to discharge alive (TTDA) (adjusted hazard ratio, 0.81; 95% CI, 0.67-0.98). However, high protein treatment in patients with and without preexisting malnutrition was not associated with TTDA (adjusted hazard ratios of 0.84 [95% CI, 0.63-1.11] and 0.97 [95% CI, 0.77-1.21]). Furthermore, no effect modification was observed (ratio of adjusted hazard ratio, 0.84; 95% CI, 0.58-1.20).
Most importantly, this study demonstrated an association between malnutrition and slower TTDA; however, this association was not modified by high protein treatment. This research challenges current international critical care nutrition guidelines.
– Commentary by Mary Jo S. Farmer, MD, PhD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Critical Care | Protocol and Statistical Analysis Plan for the Mode of Ventilation During Critical Illness (MODE) Trial
By: Kevin P. Seitz, MD, et al
The Mode of Ventilation During Critical Illness (MODE) trial is a cluster-randomized, multiple-crossover pilot study conducted in a medical ICU exploring how different mechanical ventilation modes affect ventilator-free days in critically ill patients. This trial aims to determine which ventilation mode maximizes the days patients spend alive without invasive ventilation. By switching between ventilation modes each month, the study ensures a thorough assessment under uniform clinical conditions. The trial’s protocol and statistical analysis plan were defined before the end of enrollment, which bolsters the rigor, reproducibility, and transparency of the findings. Initial findings indicate the necessity for an expanded, multicenter trial to definitively identify the optimal ventilation mode, as current data do not universally prefer one method over others. This research has significant implications for clinical practice, potentially altering mechanical ventilation guidelines and improving patient outcomes by reducing the time spent on mechanical ventilation.
– Commentary by Dharani Narendra, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary | Guideline Alignment and Medication Concordance in COPD
By: Meredith A. Chase, MD, MHS, et al
Over the past 10 years, a number of studies from generalists and specialists have consistently shown a lack of compliance between physician prescriptions and the Global Initiative for Chronic Obstructive Lung Disease strategy’s recommendations. This study aligns with prior research conducted in the same field. The inappropriate use of maintenance inhalers and the excessive use of inhaled corticosteroids are contributing factors to the skyrocketing expenses of managing COPD despite a slight decrease in prevalence. Overall, the results of all these studies are somewhat unsettling.
Nonetheless, there are a number of factors that are either unavoidable or difficult to address. First, primary care providers (PCPs) are less knowledgeable about the most recent recommendations and guidelines than specialists are. Second, the managed care companies and their PCPs are sometimes reluctant to refer patients to a specialist, resulting in delayed diagnosis and, at times, wrong diagnosis and mismanagement. Third, managed health care organizations have limited drugs for managing COPD on their formularies, limiting the ability of the provider to prescribe guideline-recommended treatments. Lastly, and very regrettably, the number of primary care doctors is decreasing, which is influencing patients’ ability to connect with someone who possesses the clinical expertise to assist them.
Future studies, projects, and endeavors ought to focus on solutions that could lessen these obstacles and provide patients and physicians more education, authority, and autonomy.
– Commentary by Humayun Anjum, MD, FCCP, Member of the CHEST Physician Editorial Board
Catch-and-Treat Strategy Identifies Undiagnosed Asthma and COPD
SAN DIEGO — You can’t treat patients if you can’t find them. But as investigators in a randomized controlled trial showed, a case-finding method based on spirometry results can identify individuals in the community with undiagnosed chronic obstructive pulmonary disease (COPD) or asthma whose lives could be significantly improved with proper care.
“By diagnosing people early and treating them intensively, you can really improve their quality of life,” said lead investigator Shawn D. Aaron, MD, from the Ottawa Hospital Research Institute and University of Ottawa, Ontario, Canada.
Even those patients in the study who were randomly assigned to receive care from a general practice physician had improvements in lung function and quality of life, although on a smaller scale than patients assigned to a specialty team, Dr. Aaron said at the American Thoracic Society’s international conference.
He reported results of the study in a late-breaking oral abstract session. The study findings were also published online in The New England Journal of Medicine.
Undiagnosed diseases
“The simple problem is that 70% of individuals with asthma or COPD are likely undiagnosed,” Dr. Aaron said.
He noted that the 2007-2012 US National Health and Nutritional Examination Survey found obstructive lung disease in 13% of randomly selected US adults, but 71% of these people had never been diagnosed with asthma or COPD.
“So our questions were in this study: One, can we find adults with undiagnosed asthma or COPD in the community? The second question was: If we find them, are they sick? And the third and most important question was: Can we treat them early and improve their health outcomes?” he said.
Asthma and COPD both present with similar respiratory symptoms, including dyspnea, cough, wheeze, and/or chest tightness, and the two conditions share expiratory airflow obstruction as a common physiologic impairment that can be detected with spirometry.
Study details
To identify participants, the investigators hired a commercial survey firm to contact households asking whether any member aged 18 years or older had respiratory symptoms such as shortness of breath, wheezing, increased mucus or sputum production, or prolonged cough in the past 6 months. Those who responded yes were then contacted by a trial coordinator, and the symptomatic household member was asked to complete the Asthma Screening Questionnaire over the phone. Participants aged 60 years or older and those younger than 60 years with a score of 6 or higher on the asthma screen also completed the COPD Diagnostic Questionnaire.
Those with a score of 6 or higher on the asthma screen or 20 or higher on the COPD screen were invited to undergo spirometry at a trial site.
The investigators ultimately identified 508 adults with undiagnosed asthma or COPD and randomly assigned them on an equal basis to an intervention group (253 patients) or control group (255 patients).
In the intervention group treatment was provided by a study pulmonologist and asthma-COPD educator who started guideline-based care. Patients were prescribed inhalers and were taught how to use them, and many were given action plans that included smoking cessation aids, exercise and weight counseling, and vaccinations against influenza and pneumonia.
Participants assigned to the control group would receive usual care provided by their primary care practitioner.
Improvements abound
During the 12 months of the study, 92% of patients in the intervention group and 60% in the control group were started on new medications for their condition.
Only 13.4% of those in the intervention group received either no respiratory treatments or a short-acting beta 2 agonist only during the entire trial period compared with 49.8% of controls, “so the usual care arm was undertreated relative to the intervention arm, and because of that under-treatment we saw a tremendous difference in the primary outcome,” Dr. Aaron said.
The primary outcome, the annualized rate of patient-initiated healthcare utilization for respiratory illness, was significantly lower in the intervention group, translating into an incidence rate ratio of 0.48 (P < .001).
Secondary outcomes were also better in the intervention group. For example, total scores on the St. George Respiratory Questionnaire (SGRQ) declined by 10.2 points from baseline in intervention group compared with a 6.8-point drop in the usual-care group. The mean difference was 3.5 points (P = .009). Lower scores on the 0-100 SGRQ scale indicate better health status.
Similarly, total scores on the COPD Assessment Test, a scale of 0-40 with lower scores indicating better health, declined by 3.8 points and 2.6 points, respectively, over 12 months, for a mean difference of 1.3 points (P = .03).
In addition, those in the intervention arm had a 119-mL improvement in forced expiratory volume in 1 second over the 12 months of the study compared with only a 22-mL improvement in the usual-care group.
Translatable results?
Dr. Aaron acknowledged that the investigators could have chosen to keep those who were assigned to the control group unaware of their diagnosis during the study but because all patients enrolled were symptomatic, it would have been unethical to do so. All participants were informed of their diagnosis at randomization, and the information was conveyed to each patient’s primary care practitioner as well.
In fact, many patients in the control group decided to seek treatment for either asthma or COPD after learning of their diagnosis, which may have contributed to improved outcomes in the control arm, he said.
“What this means is if you make the diagnosis early in the community, and at least have them see a primary care practitioner, they will improve their quality of life and their health status,” he concluded.
Ravi Kalhan, MD, MS, from the Northwestern University Feinberg School Of Medicine in Chicago, who co-moderated the session but was not involved in the study, said in an interview that the case-finding model used in the trial would be difficult to replicate elsewhere.
“This idea of seeking out undiagnosed people by doing spirometry, so-called ‘case finding’ as they described it, testing highly symptomatic people with spirometry, is really challenging in the US, because symptoms are not collected proactively very much,” he said.
Persons with acute respiratory symptoms in the US typically seek healthcare at urgent-care clinics or have unscheduled visits with their primary care physicians, “and by all accounts those people should have spirometry, but they just don’t in the US, as best as I can tell,” he added.
He agreed that getting patients to a specialist can result in better outcomes but said that implementing a systematic approach such as the one described in the study would be extremely difficult in the fragmented US healthcare system.
Dr. Kalhan’s co-moderator, Nuala J. Meyer, MD, MS, from the Hospital of the University of Pennsylvania, Philadelphia, told Chest Physician that “it was interesting that even those who were not in the intervention group but had these details passed on to their primary care physicians still had improvements,” and that it would be beneficial if primary care practitioners were routinely informed about the results of urgent care visits.
She added, however, that in the US the flow of information between urgent care clinics, primary care offices, and specialty clinics is problematic, suggesting that symptomatic patients may not always receive the additional care that they need.
The study was supported by the Canadian Institutes of Health Research. Dr. Aaron, Dr. Kalhan, and Dr. Meyer all reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — You can’t treat patients if you can’t find them. But as investigators in a randomized controlled trial showed, a case-finding method based on spirometry results can identify individuals in the community with undiagnosed chronic obstructive pulmonary disease (COPD) or asthma whose lives could be significantly improved with proper care.
“By diagnosing people early and treating them intensively, you can really improve their quality of life,” said lead investigator Shawn D. Aaron, MD, from the Ottawa Hospital Research Institute and University of Ottawa, Ontario, Canada.
Even those patients in the study who were randomly assigned to receive care from a general practice physician had improvements in lung function and quality of life, although on a smaller scale than patients assigned to a specialty team, Dr. Aaron said at the American Thoracic Society’s international conference.
He reported results of the study in a late-breaking oral abstract session. The study findings were also published online in The New England Journal of Medicine.
Undiagnosed diseases
“The simple problem is that 70% of individuals with asthma or COPD are likely undiagnosed,” Dr. Aaron said.
He noted that the 2007-2012 US National Health and Nutritional Examination Survey found obstructive lung disease in 13% of randomly selected US adults, but 71% of these people had never been diagnosed with asthma or COPD.
“So our questions were in this study: One, can we find adults with undiagnosed asthma or COPD in the community? The second question was: If we find them, are they sick? And the third and most important question was: Can we treat them early and improve their health outcomes?” he said.
Asthma and COPD both present with similar respiratory symptoms, including dyspnea, cough, wheeze, and/or chest tightness, and the two conditions share expiratory airflow obstruction as a common physiologic impairment that can be detected with spirometry.
Study details
To identify participants, the investigators hired a commercial survey firm to contact households asking whether any member aged 18 years or older had respiratory symptoms such as shortness of breath, wheezing, increased mucus or sputum production, or prolonged cough in the past 6 months. Those who responded yes were then contacted by a trial coordinator, and the symptomatic household member was asked to complete the Asthma Screening Questionnaire over the phone. Participants aged 60 years or older and those younger than 60 years with a score of 6 or higher on the asthma screen also completed the COPD Diagnostic Questionnaire.
Those with a score of 6 or higher on the asthma screen or 20 or higher on the COPD screen were invited to undergo spirometry at a trial site.
The investigators ultimately identified 508 adults with undiagnosed asthma or COPD and randomly assigned them on an equal basis to an intervention group (253 patients) or control group (255 patients).
In the intervention group treatment was provided by a study pulmonologist and asthma-COPD educator who started guideline-based care. Patients were prescribed inhalers and were taught how to use them, and many were given action plans that included smoking cessation aids, exercise and weight counseling, and vaccinations against influenza and pneumonia.
Participants assigned to the control group would receive usual care provided by their primary care practitioner.
Improvements abound
During the 12 months of the study, 92% of patients in the intervention group and 60% in the control group were started on new medications for their condition.
Only 13.4% of those in the intervention group received either no respiratory treatments or a short-acting beta 2 agonist only during the entire trial period compared with 49.8% of controls, “so the usual care arm was undertreated relative to the intervention arm, and because of that under-treatment we saw a tremendous difference in the primary outcome,” Dr. Aaron said.
The primary outcome, the annualized rate of patient-initiated healthcare utilization for respiratory illness, was significantly lower in the intervention group, translating into an incidence rate ratio of 0.48 (P < .001).
Secondary outcomes were also better in the intervention group. For example, total scores on the St. George Respiratory Questionnaire (SGRQ) declined by 10.2 points from baseline in intervention group compared with a 6.8-point drop in the usual-care group. The mean difference was 3.5 points (P = .009). Lower scores on the 0-100 SGRQ scale indicate better health status.
Similarly, total scores on the COPD Assessment Test, a scale of 0-40 with lower scores indicating better health, declined by 3.8 points and 2.6 points, respectively, over 12 months, for a mean difference of 1.3 points (P = .03).
In addition, those in the intervention arm had a 119-mL improvement in forced expiratory volume in 1 second over the 12 months of the study compared with only a 22-mL improvement in the usual-care group.
Translatable results?
Dr. Aaron acknowledged that the investigators could have chosen to keep those who were assigned to the control group unaware of their diagnosis during the study but because all patients enrolled were symptomatic, it would have been unethical to do so. All participants were informed of their diagnosis at randomization, and the information was conveyed to each patient’s primary care practitioner as well.
In fact, many patients in the control group decided to seek treatment for either asthma or COPD after learning of their diagnosis, which may have contributed to improved outcomes in the control arm, he said.
“What this means is if you make the diagnosis early in the community, and at least have them see a primary care practitioner, they will improve their quality of life and their health status,” he concluded.
Ravi Kalhan, MD, MS, from the Northwestern University Feinberg School Of Medicine in Chicago, who co-moderated the session but was not involved in the study, said in an interview that the case-finding model used in the trial would be difficult to replicate elsewhere.
“This idea of seeking out undiagnosed people by doing spirometry, so-called ‘case finding’ as they described it, testing highly symptomatic people with spirometry, is really challenging in the US, because symptoms are not collected proactively very much,” he said.
Persons with acute respiratory symptoms in the US typically seek healthcare at urgent-care clinics or have unscheduled visits with their primary care physicians, “and by all accounts those people should have spirometry, but they just don’t in the US, as best as I can tell,” he added.
He agreed that getting patients to a specialist can result in better outcomes but said that implementing a systematic approach such as the one described in the study would be extremely difficult in the fragmented US healthcare system.
Dr. Kalhan’s co-moderator, Nuala J. Meyer, MD, MS, from the Hospital of the University of Pennsylvania, Philadelphia, told Chest Physician that “it was interesting that even those who were not in the intervention group but had these details passed on to their primary care physicians still had improvements,” and that it would be beneficial if primary care practitioners were routinely informed about the results of urgent care visits.
She added, however, that in the US the flow of information between urgent care clinics, primary care offices, and specialty clinics is problematic, suggesting that symptomatic patients may not always receive the additional care that they need.
The study was supported by the Canadian Institutes of Health Research. Dr. Aaron, Dr. Kalhan, and Dr. Meyer all reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — You can’t treat patients if you can’t find them. But as investigators in a randomized controlled trial showed, a case-finding method based on spirometry results can identify individuals in the community with undiagnosed chronic obstructive pulmonary disease (COPD) or asthma whose lives could be significantly improved with proper care.
“By diagnosing people early and treating them intensively, you can really improve their quality of life,” said lead investigator Shawn D. Aaron, MD, from the Ottawa Hospital Research Institute and University of Ottawa, Ontario, Canada.
Even those patients in the study who were randomly assigned to receive care from a general practice physician had improvements in lung function and quality of life, although on a smaller scale than patients assigned to a specialty team, Dr. Aaron said at the American Thoracic Society’s international conference.
He reported results of the study in a late-breaking oral abstract session. The study findings were also published online in The New England Journal of Medicine.
Undiagnosed diseases
“The simple problem is that 70% of individuals with asthma or COPD are likely undiagnosed,” Dr. Aaron said.
He noted that the 2007-2012 US National Health and Nutritional Examination Survey found obstructive lung disease in 13% of randomly selected US adults, but 71% of these people had never been diagnosed with asthma or COPD.
“So our questions were in this study: One, can we find adults with undiagnosed asthma or COPD in the community? The second question was: If we find them, are they sick? And the third and most important question was: Can we treat them early and improve their health outcomes?” he said.
Asthma and COPD both present with similar respiratory symptoms, including dyspnea, cough, wheeze, and/or chest tightness, and the two conditions share expiratory airflow obstruction as a common physiologic impairment that can be detected with spirometry.
Study details
To identify participants, the investigators hired a commercial survey firm to contact households asking whether any member aged 18 years or older had respiratory symptoms such as shortness of breath, wheezing, increased mucus or sputum production, or prolonged cough in the past 6 months. Those who responded yes were then contacted by a trial coordinator, and the symptomatic household member was asked to complete the Asthma Screening Questionnaire over the phone. Participants aged 60 years or older and those younger than 60 years with a score of 6 or higher on the asthma screen also completed the COPD Diagnostic Questionnaire.
Those with a score of 6 or higher on the asthma screen or 20 or higher on the COPD screen were invited to undergo spirometry at a trial site.
The investigators ultimately identified 508 adults with undiagnosed asthma or COPD and randomly assigned them on an equal basis to an intervention group (253 patients) or control group (255 patients).
In the intervention group treatment was provided by a study pulmonologist and asthma-COPD educator who started guideline-based care. Patients were prescribed inhalers and were taught how to use them, and many were given action plans that included smoking cessation aids, exercise and weight counseling, and vaccinations against influenza and pneumonia.
Participants assigned to the control group would receive usual care provided by their primary care practitioner.
Improvements abound
During the 12 months of the study, 92% of patients in the intervention group and 60% in the control group were started on new medications for their condition.
Only 13.4% of those in the intervention group received either no respiratory treatments or a short-acting beta 2 agonist only during the entire trial period compared with 49.8% of controls, “so the usual care arm was undertreated relative to the intervention arm, and because of that under-treatment we saw a tremendous difference in the primary outcome,” Dr. Aaron said.
The primary outcome, the annualized rate of patient-initiated healthcare utilization for respiratory illness, was significantly lower in the intervention group, translating into an incidence rate ratio of 0.48 (P < .001).
Secondary outcomes were also better in the intervention group. For example, total scores on the St. George Respiratory Questionnaire (SGRQ) declined by 10.2 points from baseline in intervention group compared with a 6.8-point drop in the usual-care group. The mean difference was 3.5 points (P = .009). Lower scores on the 0-100 SGRQ scale indicate better health status.
Similarly, total scores on the COPD Assessment Test, a scale of 0-40 with lower scores indicating better health, declined by 3.8 points and 2.6 points, respectively, over 12 months, for a mean difference of 1.3 points (P = .03).
In addition, those in the intervention arm had a 119-mL improvement in forced expiratory volume in 1 second over the 12 months of the study compared with only a 22-mL improvement in the usual-care group.
Translatable results?
Dr. Aaron acknowledged that the investigators could have chosen to keep those who were assigned to the control group unaware of their diagnosis during the study but because all patients enrolled were symptomatic, it would have been unethical to do so. All participants were informed of their diagnosis at randomization, and the information was conveyed to each patient’s primary care practitioner as well.
In fact, many patients in the control group decided to seek treatment for either asthma or COPD after learning of their diagnosis, which may have contributed to improved outcomes in the control arm, he said.
“What this means is if you make the diagnosis early in the community, and at least have them see a primary care practitioner, they will improve their quality of life and their health status,” he concluded.
Ravi Kalhan, MD, MS, from the Northwestern University Feinberg School Of Medicine in Chicago, who co-moderated the session but was not involved in the study, said in an interview that the case-finding model used in the trial would be difficult to replicate elsewhere.
“This idea of seeking out undiagnosed people by doing spirometry, so-called ‘case finding’ as they described it, testing highly symptomatic people with spirometry, is really challenging in the US, because symptoms are not collected proactively very much,” he said.
Persons with acute respiratory symptoms in the US typically seek healthcare at urgent-care clinics or have unscheduled visits with their primary care physicians, “and by all accounts those people should have spirometry, but they just don’t in the US, as best as I can tell,” he added.
He agreed that getting patients to a specialist can result in better outcomes but said that implementing a systematic approach such as the one described in the study would be extremely difficult in the fragmented US healthcare system.
Dr. Kalhan’s co-moderator, Nuala J. Meyer, MD, MS, from the Hospital of the University of Pennsylvania, Philadelphia, told Chest Physician that “it was interesting that even those who were not in the intervention group but had these details passed on to their primary care physicians still had improvements,” and that it would be beneficial if primary care practitioners were routinely informed about the results of urgent care visits.
She added, however, that in the US the flow of information between urgent care clinics, primary care offices, and specialty clinics is problematic, suggesting that symptomatic patients may not always receive the additional care that they need.
The study was supported by the Canadian Institutes of Health Research. Dr. Aaron, Dr. Kalhan, and Dr. Meyer all reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
Treating High Stage cSCC: Better Results With Mohs Surgery vs Wide Local Excision, Study Finds
PHOENIX — . The benefit was seen across all outcome measures, including rates of recurrence, metastasis, and mortality.
These data support Mohs surgery as being the preferred surgical treatment option for high-stage cSCC, commented lead author David M. Wang, MD, Mohs Micrographic Surgery and Dermatologic Oncology Fellow, at Harvard’s Brigham and Women’s Hospital (BWH)/Dana-Farber Cancer Institute, Boston. “We found that across all outcomes, high-stage cSCC treated with WLE had a roughly twofold greater risk for recurrence, metastasis, or disease-specific death compared to Mohs,” he said at the annual meeting of the American College of Mohs Surgery (ACMS), where he presented the results.
External validation using data from a multicenter cSCC research collaboration from 12 contributing sites from across the United States, as well as international sites, was also conducted. “We performed the external validation by comparing results of the BWH-only cohort, which was the primary study, with the full multicenter data and with the full multicenter data minus the BWH cohort, and the findings were nearly identical in all three analyses,” Dr. Wang said.
Although patients diagnosed with cSCC usually have good outcomes, high-stage disease is associated with a higher risk for recurrence, metastasis, and death. Both Mohs surgery and WLE are used to treat cSCC, but a comparison of outcomes has not been well established in the setting of high-stage cSCC. Comparing the two surgical strategies can be problematic, as both patient and/or tumor characteristics can make it difficult to determine which outcomes can be attributed solely to the treatment type.
Mohs Superior Across the Board
In the retrospective cohort study, Dr. Wang and colleagues aimed to compare the results of Mohs surgery and WLE in patients with high-stage cSCC (BWH Staging System T2b or T3) and used statistical methods to balance baseline patient and tumor characteristics.
“To control for confounding by indication — differences in baseline patient or tumor characteristics — that are associated with both the treatment received and outcomes, we used propensity score weighting so that the baseline characteristics were balanced in the two treatment groups,” Dr. Wang told this news organization. “This statistical method aims to simulate randomization in a randomized controlled trial such that any differences in outcomes after propensity score weighting is attributed solely to the treatment received.”
The study used electronic medical records from a single tertiary care academic institution, and 216 patients with high-stage cSCC who had undergone surgery from January 2000 to December 2019 were included in the analysis. The median follow-up time was 33.1 months.
They found that overall, the risk for all adverse outcomes was lower among patients who had undergone Mohs surgery than among those treated with WLE, with the following results: Rates of local recurrence (5-year CI, 10.8% vs 22.1%, respectively; P = .003), nodal metastasis (11.9% vs 19.3%; P = .04), distant metastasis (4.7% vs 9.0%; P = .09), any recurrence (17.0% vs 34.2%; P < .001), and disease-specific death (8.5% vs 20.3%; P = .001).
“The data supports Mohs surgery as the preferred surgical treatment option for high-stage cSCC in accordance with NCCN [National Comprehensive Cancer Network] guidelines for very high-risk cSCC,” Dr. Wang said. He pointed out that the terminology “very high risk” in NCCN equates to “high stage” in other staging systems (BWH T2b or higher, AJCC T3 or higher).
There is still “a substantial proportion” of patients with high-stage cSCC who are eligible for Mohs but are treated with WLE, he added. “Our hope is that these findings provide additional data to support Mohs as the standard of care for primary surgical treatment of high-stage cSCC.”
Supports Benefits of Mohs
Weighing in on the research, Thomas E. Rohrer, MD, a dermatologic surgeon in Chestnut Hill, Massachusetts, noted that this was an excellent study that demonstrates benefits of Mohs surgery over straight excision on essentially all outcomes investigated and measured.
“The data clearly shows that Mohs should be used whenever possible,” he said. “There are some patients and facilities that do not have access or timely access to Mohs, so they would likely proceed with standard wide local excision. Otherwise, if there is the capability to perform Mohs, it would be preferred,” he added.
“There is no benefit to a standard excision over Mohs,” Dr. Rohrer emphasized. “If a surgeon is not sure if they have attained clear margins, they could and often do take a little more tissue to be certain.”
Also asked to comment on the data, Chad L. Prather, MD, a dermatologist in Baton Rouge, Louisiana, said, “We know that Mohs has been used for cancers that are not highly staged and we know it’s better than WLE, but this study shows that it is beneficial for higher stage cancers.”
However, he cautioned that unlike early-stage cancers, where Mohs is usually a definitive treatment, with higher stage disease it is a starting point. “As a takeaway, Mohs is superior, but it needs to be followed through,” he said. “These patients need to be closely followed as they are at a high risk for recurrence and metastasis and may need to be worked up for lymph node involvement and need additional therapy going forward.”
Dr. Prather also pointed out that there are circumstances when WLE may be a more suitable treatment. “Mohs is not very good if there is bony involvement,” he said. “This most often happens when the lesion is on the scalp and has invaded the skull. WLE may still be the preferred choice.”
Additionally, Mohs is not the best choice if the tumor is broken into multiple segments. “In these cases, WLE may be preferred,” Dr. Prather added. “But overall, Mohs is one of the best tools we have, and it stands to reason that it works well for high-risk tumors, as this study shows.”
The study was independently supported. Dr. Wang reported no relevant financial relationships. Dr. Rohrer and Dr. Prather had no relevant disclosures.
A version of this article appeared on Medscape.com.
PHOENIX — . The benefit was seen across all outcome measures, including rates of recurrence, metastasis, and mortality.
These data support Mohs surgery as being the preferred surgical treatment option for high-stage cSCC, commented lead author David M. Wang, MD, Mohs Micrographic Surgery and Dermatologic Oncology Fellow, at Harvard’s Brigham and Women’s Hospital (BWH)/Dana-Farber Cancer Institute, Boston. “We found that across all outcomes, high-stage cSCC treated with WLE had a roughly twofold greater risk for recurrence, metastasis, or disease-specific death compared to Mohs,” he said at the annual meeting of the American College of Mohs Surgery (ACMS), where he presented the results.
External validation using data from a multicenter cSCC research collaboration from 12 contributing sites from across the United States, as well as international sites, was also conducted. “We performed the external validation by comparing results of the BWH-only cohort, which was the primary study, with the full multicenter data and with the full multicenter data minus the BWH cohort, and the findings were nearly identical in all three analyses,” Dr. Wang said.
Although patients diagnosed with cSCC usually have good outcomes, high-stage disease is associated with a higher risk for recurrence, metastasis, and death. Both Mohs surgery and WLE are used to treat cSCC, but a comparison of outcomes has not been well established in the setting of high-stage cSCC. Comparing the two surgical strategies can be problematic, as both patient and/or tumor characteristics can make it difficult to determine which outcomes can be attributed solely to the treatment type.
Mohs Superior Across the Board
In the retrospective cohort study, Dr. Wang and colleagues aimed to compare the results of Mohs surgery and WLE in patients with high-stage cSCC (BWH Staging System T2b or T3) and used statistical methods to balance baseline patient and tumor characteristics.
“To control for confounding by indication — differences in baseline patient or tumor characteristics — that are associated with both the treatment received and outcomes, we used propensity score weighting so that the baseline characteristics were balanced in the two treatment groups,” Dr. Wang told this news organization. “This statistical method aims to simulate randomization in a randomized controlled trial such that any differences in outcomes after propensity score weighting is attributed solely to the treatment received.”
The study used electronic medical records from a single tertiary care academic institution, and 216 patients with high-stage cSCC who had undergone surgery from January 2000 to December 2019 were included in the analysis. The median follow-up time was 33.1 months.
They found that overall, the risk for all adverse outcomes was lower among patients who had undergone Mohs surgery than among those treated with WLE, with the following results: Rates of local recurrence (5-year CI, 10.8% vs 22.1%, respectively; P = .003), nodal metastasis (11.9% vs 19.3%; P = .04), distant metastasis (4.7% vs 9.0%; P = .09), any recurrence (17.0% vs 34.2%; P < .001), and disease-specific death (8.5% vs 20.3%; P = .001).
“The data supports Mohs surgery as the preferred surgical treatment option for high-stage cSCC in accordance with NCCN [National Comprehensive Cancer Network] guidelines for very high-risk cSCC,” Dr. Wang said. He pointed out that the terminology “very high risk” in NCCN equates to “high stage” in other staging systems (BWH T2b or higher, AJCC T3 or higher).
There is still “a substantial proportion” of patients with high-stage cSCC who are eligible for Mohs but are treated with WLE, he added. “Our hope is that these findings provide additional data to support Mohs as the standard of care for primary surgical treatment of high-stage cSCC.”
Supports Benefits of Mohs
Weighing in on the research, Thomas E. Rohrer, MD, a dermatologic surgeon in Chestnut Hill, Massachusetts, noted that this was an excellent study that demonstrates benefits of Mohs surgery over straight excision on essentially all outcomes investigated and measured.
“The data clearly shows that Mohs should be used whenever possible,” he said. “There are some patients and facilities that do not have access or timely access to Mohs, so they would likely proceed with standard wide local excision. Otherwise, if there is the capability to perform Mohs, it would be preferred,” he added.
“There is no benefit to a standard excision over Mohs,” Dr. Rohrer emphasized. “If a surgeon is not sure if they have attained clear margins, they could and often do take a little more tissue to be certain.”
Also asked to comment on the data, Chad L. Prather, MD, a dermatologist in Baton Rouge, Louisiana, said, “We know that Mohs has been used for cancers that are not highly staged and we know it’s better than WLE, but this study shows that it is beneficial for higher stage cancers.”
However, he cautioned that unlike early-stage cancers, where Mohs is usually a definitive treatment, with higher stage disease it is a starting point. “As a takeaway, Mohs is superior, but it needs to be followed through,” he said. “These patients need to be closely followed as they are at a high risk for recurrence and metastasis and may need to be worked up for lymph node involvement and need additional therapy going forward.”
Dr. Prather also pointed out that there are circumstances when WLE may be a more suitable treatment. “Mohs is not very good if there is bony involvement,” he said. “This most often happens when the lesion is on the scalp and has invaded the skull. WLE may still be the preferred choice.”
Additionally, Mohs is not the best choice if the tumor is broken into multiple segments. “In these cases, WLE may be preferred,” Dr. Prather added. “But overall, Mohs is one of the best tools we have, and it stands to reason that it works well for high-risk tumors, as this study shows.”
The study was independently supported. Dr. Wang reported no relevant financial relationships. Dr. Rohrer and Dr. Prather had no relevant disclosures.
A version of this article appeared on Medscape.com.
PHOENIX — . The benefit was seen across all outcome measures, including rates of recurrence, metastasis, and mortality.
These data support Mohs surgery as being the preferred surgical treatment option for high-stage cSCC, commented lead author David M. Wang, MD, Mohs Micrographic Surgery and Dermatologic Oncology Fellow, at Harvard’s Brigham and Women’s Hospital (BWH)/Dana-Farber Cancer Institute, Boston. “We found that across all outcomes, high-stage cSCC treated with WLE had a roughly twofold greater risk for recurrence, metastasis, or disease-specific death compared to Mohs,” he said at the annual meeting of the American College of Mohs Surgery (ACMS), where he presented the results.
External validation using data from a multicenter cSCC research collaboration from 12 contributing sites from across the United States, as well as international sites, was also conducted. “We performed the external validation by comparing results of the BWH-only cohort, which was the primary study, with the full multicenter data and with the full multicenter data minus the BWH cohort, and the findings were nearly identical in all three analyses,” Dr. Wang said.
Although patients diagnosed with cSCC usually have good outcomes, high-stage disease is associated with a higher risk for recurrence, metastasis, and death. Both Mohs surgery and WLE are used to treat cSCC, but a comparison of outcomes has not been well established in the setting of high-stage cSCC. Comparing the two surgical strategies can be problematic, as both patient and/or tumor characteristics can make it difficult to determine which outcomes can be attributed solely to the treatment type.
Mohs Superior Across the Board
In the retrospective cohort study, Dr. Wang and colleagues aimed to compare the results of Mohs surgery and WLE in patients with high-stage cSCC (BWH Staging System T2b or T3) and used statistical methods to balance baseline patient and tumor characteristics.
“To control for confounding by indication — differences in baseline patient or tumor characteristics — that are associated with both the treatment received and outcomes, we used propensity score weighting so that the baseline characteristics were balanced in the two treatment groups,” Dr. Wang told this news organization. “This statistical method aims to simulate randomization in a randomized controlled trial such that any differences in outcomes after propensity score weighting is attributed solely to the treatment received.”
The study used electronic medical records from a single tertiary care academic institution, and 216 patients with high-stage cSCC who had undergone surgery from January 2000 to December 2019 were included in the analysis. The median follow-up time was 33.1 months.
They found that overall, the risk for all adverse outcomes was lower among patients who had undergone Mohs surgery than among those treated with WLE, with the following results: Rates of local recurrence (5-year CI, 10.8% vs 22.1%, respectively; P = .003), nodal metastasis (11.9% vs 19.3%; P = .04), distant metastasis (4.7% vs 9.0%; P = .09), any recurrence (17.0% vs 34.2%; P < .001), and disease-specific death (8.5% vs 20.3%; P = .001).
“The data supports Mohs surgery as the preferred surgical treatment option for high-stage cSCC in accordance with NCCN [National Comprehensive Cancer Network] guidelines for very high-risk cSCC,” Dr. Wang said. He pointed out that the terminology “very high risk” in NCCN equates to “high stage” in other staging systems (BWH T2b or higher, AJCC T3 or higher).
There is still “a substantial proportion” of patients with high-stage cSCC who are eligible for Mohs but are treated with WLE, he added. “Our hope is that these findings provide additional data to support Mohs as the standard of care for primary surgical treatment of high-stage cSCC.”
Supports Benefits of Mohs
Weighing in on the research, Thomas E. Rohrer, MD, a dermatologic surgeon in Chestnut Hill, Massachusetts, noted that this was an excellent study that demonstrates benefits of Mohs surgery over straight excision on essentially all outcomes investigated and measured.
“The data clearly shows that Mohs should be used whenever possible,” he said. “There are some patients and facilities that do not have access or timely access to Mohs, so they would likely proceed with standard wide local excision. Otherwise, if there is the capability to perform Mohs, it would be preferred,” he added.
“There is no benefit to a standard excision over Mohs,” Dr. Rohrer emphasized. “If a surgeon is not sure if they have attained clear margins, they could and often do take a little more tissue to be certain.”
Also asked to comment on the data, Chad L. Prather, MD, a dermatologist in Baton Rouge, Louisiana, said, “We know that Mohs has been used for cancers that are not highly staged and we know it’s better than WLE, but this study shows that it is beneficial for higher stage cancers.”
However, he cautioned that unlike early-stage cancers, where Mohs is usually a definitive treatment, with higher stage disease it is a starting point. “As a takeaway, Mohs is superior, but it needs to be followed through,” he said. “These patients need to be closely followed as they are at a high risk for recurrence and metastasis and may need to be worked up for lymph node involvement and need additional therapy going forward.”
Dr. Prather also pointed out that there are circumstances when WLE may be a more suitable treatment. “Mohs is not very good if there is bony involvement,” he said. “This most often happens when the lesion is on the scalp and has invaded the skull. WLE may still be the preferred choice.”
Additionally, Mohs is not the best choice if the tumor is broken into multiple segments. “In these cases, WLE may be preferred,” Dr. Prather added. “But overall, Mohs is one of the best tools we have, and it stands to reason that it works well for high-risk tumors, as this study shows.”
The study was independently supported. Dr. Wang reported no relevant financial relationships. Dr. Rohrer and Dr. Prather had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM ACMS 2024
Pulmonary telerehabilitation for COPD: Promising, but more data needed
As COVID-19 cedes its pandemic-scale status to the past, its wake is revealing surprises and raising questions, particularly in relation to pulmonary medicine. The need for isolation at COVID’s outset kept many millions at home, creating conditions favorable for the rapid expansion of technologies that were taken up quickly in telehealth applications. The need was overwhelming. But just how effective telehealth actually is at replacing on-site programs for COPD pulmonary rehab has remained a research challenge, although results from early studies show unmistakable value. Creating conditions conducive to research into the strengths and weaknesses of pulmonary rehab, and determining how research can be applied effectively, remain formidable challenges.
Early studies of telehealth pulmonary rehabilitation have not uncovered any glaring erosion of pulmonary rehabilitation’s well-established benefits. But, at the same time, the relatively young field of pulmonary telerehabilitation for chronic obstructive pulmonary disease (COPD) has lacked coordinated efforts to determine its key practices and the instruments for measuring them, both basic elements for pursuing research questions.
A 2021 American Thoracic Society workshop report (AE Holland, https://doi.org/10.1513/AnnalsATS.202102-146ST) identified essential components of a pulmonary rehabilitation model through an online Delphi process involving about 50 international experts. Components ultimately included those with median scores of 2 or higher (strongly agree or agree that the item is essential) and high consensus (interquartile range, 0). Thirteen essential components fit into four categories (Patient Assessment, Program Components, Method of Delivery and Quality Assurance). The Patient Assessment category included seven items: (1) An initial center-based assessment by a health care professional, (2) An exercise test at the time of assessment, (3) A field exercise test, (4) Quality of life measure, (5) Dyspnea assessment, (6) Nutritional status evaluation, and (7) Occupational status evaluation. The Program Components: (8) Endurance training and (9) Resistance training). The Method of Delivery: (10) An exercise program that is individually prescribed, (11) An exercise program that is individually progressed, and (12) Team includes a health care professional with experience in exercise prescription and progression. The single Quality Assurance item: (13) Health care professionals are trained to deliver the components of the model that is deployed.
Cochrane Library review
2021 “Intervention Review” (“Telerehabilitation for chronic respiratory disease,” https://doi.org/10.1002/14651858.CD013040.pub2). Using their own databases (eg, Cochrane Airways Trials Register) and others, the authors included controlled trials published up to November 30, 2020 with at least 50% of the rehabilitation delivered by telerehabilitation. The authors’ analysis of 15 studies (with 32 reports) including 1904 participants (99% with COPD): “There was probably little or no difference between telerehabilitation and in-person pulmonary rehabilitation for exercise capacity measured as 6-Minute Walking Distance (mean difference 0.06 meters (m), 95% confidence interval (CI) -10.82 m to 10.94 m).” They reached the same conclusion for quality of life, and for breathlessness. Completion of rehabilitation programs, however, was more likely with telerehabilitation at 93% versus 70% for in-person rehabilitation. No adverse effects of telerehabilitation were observed over and above those for in-person or no rehabilitation. An obvious limitation of the findings is that the studies all pre-date COVID-19, which would have introduced very significant disincentives for in-person rehabilitation completion.
An older (2016) international randomized controlled study (Zanaboni et al, https://doi.org/10.1186/s12890-016-0288-z) comparing long-term telerehabilitation or unsupervised treadmill training at home with standard care included 120 participants with COPD and had 2-years of follow-up. Telerehabilitation consisted of individualized treadmill training at home. Participants had scheduled exercise sessions supervised by a physiotherapist via videoconferencing following a standardized protocol. Participants in the unsupervised training group were provided with a treadmill only to perform unsupervised exercise at home. They also received an exercise booklet, a paper exercise diary to record their training sessions, and an individualized training program but without regular review or progression of the program. For the primary outcomes of combined hospitalizations and emergency department presentations, incidence rate of hospitalizations and emergency department presentations was lower with telerehabilitation (1.18 events per person-year; 95% confidence interval [CI], 0.94–1.46) and with unsupervised training group (1.14; 95% CI, 0.92–1.41) than in the control group (1.88; 95% CI, 1.58–2.21; P < .001 compared with intervention groups). Both training groups had better health status at 1-year, and achieved and maintained clinically significant improvements in exercise capacity.
Access to pulmonary rehabilitation
Continuing evidence of clear telerehabilitation benefits is good news, especially in the light of impediments to attendance at in-clinic programs. Although the COVID-provoked disincentives have been diminishing, persisting access issues remain for substantial portions of eligible populations, according to a recent (2024) cross-sectional study (PA Kahn, WA Mathis, doi:10.1001/jamanetworkopen.2023.54867) looking at travel time to pulmonary rehabilitation programs as a marker for pulmonary rehabilitation access. The report, based on US Census designations (lower 48 states and Washington, D.C.) found that while 80.3% of the population lives in urban or suburban areas within a 30-minute drive of a pulmonary rehabilitation program, travel time exceeds that in rural and other sparsely populated areas with more than 14 million people residing in areas demanding more than 1-hour for travel. A further analysis showed also that nearly 30% of American Indian and Alaska Native populations live more than 60 minutes from a pulmonary rehabilitation program.
Aside from the obvious restraints for homebound patients or those lacking transportation or who need medical transport, other common impediments inhibit on-site pulmonary rehabilitation attendance, said Corinne Young, MSN, FNP-C, FCCP. Ms. Young is the director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board. “I have some patients who say ‘There’s no way I could do onsite pulmonary rehab because of my knee — or back, or shoulder.’ But in their own home environment they may feel more comfortable. They may be willing to try new things at their own pace, whereas for them a program may feel too regimented.” For others, Ms. Young said, aspects of a formal program are a clear plus factor. “They love to hear their progress at the end of — say a 12-week program — where their virtual respiratory therapist records and reports to them their six-minute walk and other test results. Feedback is a great reinforcer.” Quality of life improvements, Ms. Young commented, were one of the very impressive benefits that appeared in the initial studies of pulmonary rehabilitation for COPD patients. “Being patient-centric, you want to improve quality of life for them as much as possible and we see telerehabilitation as a great opportunity for many,” she added.
“I would like to see head-to-head data on outpatient versus at-home pulmonary rehabilitation on hospitalizations, time to exacerbation and, of course, mortality. We have all that for outpatient rehab, but it would be great to be able to compare them. Knowing that would influence what we recommend, especially for patients who could go either way. Also, you have to assess their motivation and discipline to know who might be more appropriate for unsupervised pulmonary rehabilitation.”
The current reality for Ms. Young is that in her Colorado Springs vicinity, where both in-patient programs are only 15 minutes apart, she knows of no telerehabilitation programs being offered. While there are contract telerehabilitation providers, Young said, and her organization (The Association of Pulmonary Advanced Practice Providers) has been approached by one, none are licensed in Colorado, and telerehabilitation is not a billable service.
“As of yet, I’m not aware of any telemedicine pulmonary rehab available at our institution,” said pulmonologist Mary Jo S. Farmer, MD, PhD, FCCP, Associate Professor of Medicine at UMass Chan Medical School – Baystate, Springfield, MA, and a member of the CHEST Physician Editorial Board. A brief internet search identified a telerehabilitation contract provider available only in Arizona.
Reimbursement will also be a foundational concern, Ms. Young commented. While a physician, nurse practitioner, or physician virtual visit for education may be billable, telerehabilitation reimbursement is new territory. “How that all is going to work out is a big unknown piece,” she said.
Minimal components
Effective pulmonary telerehabilitation programs, Ms. Young said, need to provide exercise with an aerobic device, either a treadmill, a stationary bike or even a Cubii-type under desk foot pedal/elliptical machine, and some resistance training (elastic bands, or weights, for example). “But 50% of pulmonary rehabilitation is education about breathing techniques, purse-lip breathing, and pulmonary nutrition.” Also essential: one-on-one discussion with a qualified medical practitioner who checks on oximeter use, inhaler technique, and titrating oxygen therapy. “At our elevation of 6500 feet, most of our patients are on that.” Optimal frequency of encounters between providers and remote patients has to be elucidated by future research, Ms. Young said.
Ms. Young commented further, “With outpatient pulmonary rehabilitation there often isn’t a lot of one-on-one, but rather a big group of people exercising at the same time. I think actually there may be the potential to have more individualization with pulmonary telerehabilitation. But the barriers, the reimbursement/financial part, and the red tape and bureaucracy have to be worked on.”
As COVID-19 cedes its pandemic-scale status to the past, its wake is revealing surprises and raising questions, particularly in relation to pulmonary medicine. The need for isolation at COVID’s outset kept many millions at home, creating conditions favorable for the rapid expansion of technologies that were taken up quickly in telehealth applications. The need was overwhelming. But just how effective telehealth actually is at replacing on-site programs for COPD pulmonary rehab has remained a research challenge, although results from early studies show unmistakable value. Creating conditions conducive to research into the strengths and weaknesses of pulmonary rehab, and determining how research can be applied effectively, remain formidable challenges.
Early studies of telehealth pulmonary rehabilitation have not uncovered any glaring erosion of pulmonary rehabilitation’s well-established benefits. But, at the same time, the relatively young field of pulmonary telerehabilitation for chronic obstructive pulmonary disease (COPD) has lacked coordinated efforts to determine its key practices and the instruments for measuring them, both basic elements for pursuing research questions.
A 2021 American Thoracic Society workshop report (AE Holland, https://doi.org/10.1513/AnnalsATS.202102-146ST) identified essential components of a pulmonary rehabilitation model through an online Delphi process involving about 50 international experts. Components ultimately included those with median scores of 2 or higher (strongly agree or agree that the item is essential) and high consensus (interquartile range, 0). Thirteen essential components fit into four categories (Patient Assessment, Program Components, Method of Delivery and Quality Assurance). The Patient Assessment category included seven items: (1) An initial center-based assessment by a health care professional, (2) An exercise test at the time of assessment, (3) A field exercise test, (4) Quality of life measure, (5) Dyspnea assessment, (6) Nutritional status evaluation, and (7) Occupational status evaluation. The Program Components: (8) Endurance training and (9) Resistance training). The Method of Delivery: (10) An exercise program that is individually prescribed, (11) An exercise program that is individually progressed, and (12) Team includes a health care professional with experience in exercise prescription and progression. The single Quality Assurance item: (13) Health care professionals are trained to deliver the components of the model that is deployed.
Cochrane Library review
2021 “Intervention Review” (“Telerehabilitation for chronic respiratory disease,” https://doi.org/10.1002/14651858.CD013040.pub2). Using their own databases (eg, Cochrane Airways Trials Register) and others, the authors included controlled trials published up to November 30, 2020 with at least 50% of the rehabilitation delivered by telerehabilitation. The authors’ analysis of 15 studies (with 32 reports) including 1904 participants (99% with COPD): “There was probably little or no difference between telerehabilitation and in-person pulmonary rehabilitation for exercise capacity measured as 6-Minute Walking Distance (mean difference 0.06 meters (m), 95% confidence interval (CI) -10.82 m to 10.94 m).” They reached the same conclusion for quality of life, and for breathlessness. Completion of rehabilitation programs, however, was more likely with telerehabilitation at 93% versus 70% for in-person rehabilitation. No adverse effects of telerehabilitation were observed over and above those for in-person or no rehabilitation. An obvious limitation of the findings is that the studies all pre-date COVID-19, which would have introduced very significant disincentives for in-person rehabilitation completion.
An older (2016) international randomized controlled study (Zanaboni et al, https://doi.org/10.1186/s12890-016-0288-z) comparing long-term telerehabilitation or unsupervised treadmill training at home with standard care included 120 participants with COPD and had 2-years of follow-up. Telerehabilitation consisted of individualized treadmill training at home. Participants had scheduled exercise sessions supervised by a physiotherapist via videoconferencing following a standardized protocol. Participants in the unsupervised training group were provided with a treadmill only to perform unsupervised exercise at home. They also received an exercise booklet, a paper exercise diary to record their training sessions, and an individualized training program but without regular review or progression of the program. For the primary outcomes of combined hospitalizations and emergency department presentations, incidence rate of hospitalizations and emergency department presentations was lower with telerehabilitation (1.18 events per person-year; 95% confidence interval [CI], 0.94–1.46) and with unsupervised training group (1.14; 95% CI, 0.92–1.41) than in the control group (1.88; 95% CI, 1.58–2.21; P < .001 compared with intervention groups). Both training groups had better health status at 1-year, and achieved and maintained clinically significant improvements in exercise capacity.
Access to pulmonary rehabilitation
Continuing evidence of clear telerehabilitation benefits is good news, especially in the light of impediments to attendance at in-clinic programs. Although the COVID-provoked disincentives have been diminishing, persisting access issues remain for substantial portions of eligible populations, according to a recent (2024) cross-sectional study (PA Kahn, WA Mathis, doi:10.1001/jamanetworkopen.2023.54867) looking at travel time to pulmonary rehabilitation programs as a marker for pulmonary rehabilitation access. The report, based on US Census designations (lower 48 states and Washington, D.C.) found that while 80.3% of the population lives in urban or suburban areas within a 30-minute drive of a pulmonary rehabilitation program, travel time exceeds that in rural and other sparsely populated areas with more than 14 million people residing in areas demanding more than 1-hour for travel. A further analysis showed also that nearly 30% of American Indian and Alaska Native populations live more than 60 minutes from a pulmonary rehabilitation program.
Aside from the obvious restraints for homebound patients or those lacking transportation or who need medical transport, other common impediments inhibit on-site pulmonary rehabilitation attendance, said Corinne Young, MSN, FNP-C, FCCP. Ms. Young is the director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board. “I have some patients who say ‘There’s no way I could do onsite pulmonary rehab because of my knee — or back, or shoulder.’ But in their own home environment they may feel more comfortable. They may be willing to try new things at their own pace, whereas for them a program may feel too regimented.” For others, Ms. Young said, aspects of a formal program are a clear plus factor. “They love to hear their progress at the end of — say a 12-week program — where their virtual respiratory therapist records and reports to them their six-minute walk and other test results. Feedback is a great reinforcer.” Quality of life improvements, Ms. Young commented, were one of the very impressive benefits that appeared in the initial studies of pulmonary rehabilitation for COPD patients. “Being patient-centric, you want to improve quality of life for them as much as possible and we see telerehabilitation as a great opportunity for many,” she added.
“I would like to see head-to-head data on outpatient versus at-home pulmonary rehabilitation on hospitalizations, time to exacerbation and, of course, mortality. We have all that for outpatient rehab, but it would be great to be able to compare them. Knowing that would influence what we recommend, especially for patients who could go either way. Also, you have to assess their motivation and discipline to know who might be more appropriate for unsupervised pulmonary rehabilitation.”
The current reality for Ms. Young is that in her Colorado Springs vicinity, where both in-patient programs are only 15 minutes apart, she knows of no telerehabilitation programs being offered. While there are contract telerehabilitation providers, Young said, and her organization (The Association of Pulmonary Advanced Practice Providers) has been approached by one, none are licensed in Colorado, and telerehabilitation is not a billable service.
“As of yet, I’m not aware of any telemedicine pulmonary rehab available at our institution,” said pulmonologist Mary Jo S. Farmer, MD, PhD, FCCP, Associate Professor of Medicine at UMass Chan Medical School – Baystate, Springfield, MA, and a member of the CHEST Physician Editorial Board. A brief internet search identified a telerehabilitation contract provider available only in Arizona.
Reimbursement will also be a foundational concern, Ms. Young commented. While a physician, nurse practitioner, or physician virtual visit for education may be billable, telerehabilitation reimbursement is new territory. “How that all is going to work out is a big unknown piece,” she said.
Minimal components
Effective pulmonary telerehabilitation programs, Ms. Young said, need to provide exercise with an aerobic device, either a treadmill, a stationary bike or even a Cubii-type under desk foot pedal/elliptical machine, and some resistance training (elastic bands, or weights, for example). “But 50% of pulmonary rehabilitation is education about breathing techniques, purse-lip breathing, and pulmonary nutrition.” Also essential: one-on-one discussion with a qualified medical practitioner who checks on oximeter use, inhaler technique, and titrating oxygen therapy. “At our elevation of 6500 feet, most of our patients are on that.” Optimal frequency of encounters between providers and remote patients has to be elucidated by future research, Ms. Young said.
Ms. Young commented further, “With outpatient pulmonary rehabilitation there often isn’t a lot of one-on-one, but rather a big group of people exercising at the same time. I think actually there may be the potential to have more individualization with pulmonary telerehabilitation. But the barriers, the reimbursement/financial part, and the red tape and bureaucracy have to be worked on.”
As COVID-19 cedes its pandemic-scale status to the past, its wake is revealing surprises and raising questions, particularly in relation to pulmonary medicine. The need for isolation at COVID’s outset kept many millions at home, creating conditions favorable for the rapid expansion of technologies that were taken up quickly in telehealth applications. The need was overwhelming. But just how effective telehealth actually is at replacing on-site programs for COPD pulmonary rehab has remained a research challenge, although results from early studies show unmistakable value. Creating conditions conducive to research into the strengths and weaknesses of pulmonary rehab, and determining how research can be applied effectively, remain formidable challenges.
Early studies of telehealth pulmonary rehabilitation have not uncovered any glaring erosion of pulmonary rehabilitation’s well-established benefits. But, at the same time, the relatively young field of pulmonary telerehabilitation for chronic obstructive pulmonary disease (COPD) has lacked coordinated efforts to determine its key practices and the instruments for measuring them, both basic elements for pursuing research questions.
A 2021 American Thoracic Society workshop report (AE Holland, https://doi.org/10.1513/AnnalsATS.202102-146ST) identified essential components of a pulmonary rehabilitation model through an online Delphi process involving about 50 international experts. Components ultimately included those with median scores of 2 or higher (strongly agree or agree that the item is essential) and high consensus (interquartile range, 0). Thirteen essential components fit into four categories (Patient Assessment, Program Components, Method of Delivery and Quality Assurance). The Patient Assessment category included seven items: (1) An initial center-based assessment by a health care professional, (2) An exercise test at the time of assessment, (3) A field exercise test, (4) Quality of life measure, (5) Dyspnea assessment, (6) Nutritional status evaluation, and (7) Occupational status evaluation. The Program Components: (8) Endurance training and (9) Resistance training). The Method of Delivery: (10) An exercise program that is individually prescribed, (11) An exercise program that is individually progressed, and (12) Team includes a health care professional with experience in exercise prescription and progression. The single Quality Assurance item: (13) Health care professionals are trained to deliver the components of the model that is deployed.
Cochrane Library review
2021 “Intervention Review” (“Telerehabilitation for chronic respiratory disease,” https://doi.org/10.1002/14651858.CD013040.pub2). Using their own databases (eg, Cochrane Airways Trials Register) and others, the authors included controlled trials published up to November 30, 2020 with at least 50% of the rehabilitation delivered by telerehabilitation. The authors’ analysis of 15 studies (with 32 reports) including 1904 participants (99% with COPD): “There was probably little or no difference between telerehabilitation and in-person pulmonary rehabilitation for exercise capacity measured as 6-Minute Walking Distance (mean difference 0.06 meters (m), 95% confidence interval (CI) -10.82 m to 10.94 m).” They reached the same conclusion for quality of life, and for breathlessness. Completion of rehabilitation programs, however, was more likely with telerehabilitation at 93% versus 70% for in-person rehabilitation. No adverse effects of telerehabilitation were observed over and above those for in-person or no rehabilitation. An obvious limitation of the findings is that the studies all pre-date COVID-19, which would have introduced very significant disincentives for in-person rehabilitation completion.
An older (2016) international randomized controlled study (Zanaboni et al, https://doi.org/10.1186/s12890-016-0288-z) comparing long-term telerehabilitation or unsupervised treadmill training at home with standard care included 120 participants with COPD and had 2-years of follow-up. Telerehabilitation consisted of individualized treadmill training at home. Participants had scheduled exercise sessions supervised by a physiotherapist via videoconferencing following a standardized protocol. Participants in the unsupervised training group were provided with a treadmill only to perform unsupervised exercise at home. They also received an exercise booklet, a paper exercise diary to record their training sessions, and an individualized training program but without regular review or progression of the program. For the primary outcomes of combined hospitalizations and emergency department presentations, incidence rate of hospitalizations and emergency department presentations was lower with telerehabilitation (1.18 events per person-year; 95% confidence interval [CI], 0.94–1.46) and with unsupervised training group (1.14; 95% CI, 0.92–1.41) than in the control group (1.88; 95% CI, 1.58–2.21; P < .001 compared with intervention groups). Both training groups had better health status at 1-year, and achieved and maintained clinically significant improvements in exercise capacity.
Access to pulmonary rehabilitation
Continuing evidence of clear telerehabilitation benefits is good news, especially in the light of impediments to attendance at in-clinic programs. Although the COVID-provoked disincentives have been diminishing, persisting access issues remain for substantial portions of eligible populations, according to a recent (2024) cross-sectional study (PA Kahn, WA Mathis, doi:10.1001/jamanetworkopen.2023.54867) looking at travel time to pulmonary rehabilitation programs as a marker for pulmonary rehabilitation access. The report, based on US Census designations (lower 48 states and Washington, D.C.) found that while 80.3% of the population lives in urban or suburban areas within a 30-minute drive of a pulmonary rehabilitation program, travel time exceeds that in rural and other sparsely populated areas with more than 14 million people residing in areas demanding more than 1-hour for travel. A further analysis showed also that nearly 30% of American Indian and Alaska Native populations live more than 60 minutes from a pulmonary rehabilitation program.
Aside from the obvious restraints for homebound patients or those lacking transportation or who need medical transport, other common impediments inhibit on-site pulmonary rehabilitation attendance, said Corinne Young, MSN, FNP-C, FCCP. Ms. Young is the director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board. “I have some patients who say ‘There’s no way I could do onsite pulmonary rehab because of my knee — or back, or shoulder.’ But in their own home environment they may feel more comfortable. They may be willing to try new things at their own pace, whereas for them a program may feel too regimented.” For others, Ms. Young said, aspects of a formal program are a clear plus factor. “They love to hear their progress at the end of — say a 12-week program — where their virtual respiratory therapist records and reports to them their six-minute walk and other test results. Feedback is a great reinforcer.” Quality of life improvements, Ms. Young commented, were one of the very impressive benefits that appeared in the initial studies of pulmonary rehabilitation for COPD patients. “Being patient-centric, you want to improve quality of life for them as much as possible and we see telerehabilitation as a great opportunity for many,” she added.
“I would like to see head-to-head data on outpatient versus at-home pulmonary rehabilitation on hospitalizations, time to exacerbation and, of course, mortality. We have all that for outpatient rehab, but it would be great to be able to compare them. Knowing that would influence what we recommend, especially for patients who could go either way. Also, you have to assess their motivation and discipline to know who might be more appropriate for unsupervised pulmonary rehabilitation.”
The current reality for Ms. Young is that in her Colorado Springs vicinity, where both in-patient programs are only 15 minutes apart, she knows of no telerehabilitation programs being offered. While there are contract telerehabilitation providers, Young said, and her organization (The Association of Pulmonary Advanced Practice Providers) has been approached by one, none are licensed in Colorado, and telerehabilitation is not a billable service.
“As of yet, I’m not aware of any telemedicine pulmonary rehab available at our institution,” said pulmonologist Mary Jo S. Farmer, MD, PhD, FCCP, Associate Professor of Medicine at UMass Chan Medical School – Baystate, Springfield, MA, and a member of the CHEST Physician Editorial Board. A brief internet search identified a telerehabilitation contract provider available only in Arizona.
Reimbursement will also be a foundational concern, Ms. Young commented. While a physician, nurse practitioner, or physician virtual visit for education may be billable, telerehabilitation reimbursement is new territory. “How that all is going to work out is a big unknown piece,” she said.
Minimal components
Effective pulmonary telerehabilitation programs, Ms. Young said, need to provide exercise with an aerobic device, either a treadmill, a stationary bike or even a Cubii-type under desk foot pedal/elliptical machine, and some resistance training (elastic bands, or weights, for example). “But 50% of pulmonary rehabilitation is education about breathing techniques, purse-lip breathing, and pulmonary nutrition.” Also essential: one-on-one discussion with a qualified medical practitioner who checks on oximeter use, inhaler technique, and titrating oxygen therapy. “At our elevation of 6500 feet, most of our patients are on that.” Optimal frequency of encounters between providers and remote patients has to be elucidated by future research, Ms. Young said.
Ms. Young commented further, “With outpatient pulmonary rehabilitation there often isn’t a lot of one-on-one, but rather a big group of people exercising at the same time. I think actually there may be the potential to have more individualization with pulmonary telerehabilitation. But the barriers, the reimbursement/financial part, and the red tape and bureaucracy have to be worked on.”
Recalcitrant Folliculitis Decalvans Treatment Outcomes With Biologics and Small Molecule Inhibitors
Folliculitis decalvans (FD) is classified as a rare primary neutrophilic cicatricial alopecia occurring predominantly in middle-aged adults. Although the true etiology is still unknown, the pathogenesis behind the inflammatory follicular lesions stems from possible Staphylococcus aureus infection and an impaired host immune system in response to released superantigens. 1 The clinical severity of this inflammatory scalp disorder can range from mild to severe and debilitating. Multiple treatment regimens have been developed with the goal of maintaining full remission. We provide a summary of tumor necrosis factor (TNF) inhibitors, Janus kinase (JAK) inhibitors, phosphodiesterase 4 (PDE4) inhibitors, and monoclonal antibodies being utilized for patients with therapy-recalcitrant FD.
Methods
We conducted a PubMed, Medline, and Google Scholar search for the terms refractory FD, recalcitrant FD, or therapy-resistant FD to identify articles published in English from 1998 to 2022. Articles that reported recalcitrant cases and subsequent therapy with TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies were included. Articles were excluded if recalcitrant cases were not clearly defined. Remission was defined as no recurrence in lesions or pustules or as a reduction in the inflammatory process with stabilization upon continuation or discontinuation of the therapy regimen. Two reviewers (T.F. and K.U.) independently searched for and screened each report.
Results
Treatment of recalcitrant FD with biologics or small molecule inhibitors was discussed in 9 studies with a combined total of 35 patients.2-10 The treatment regimens included TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies (Table).
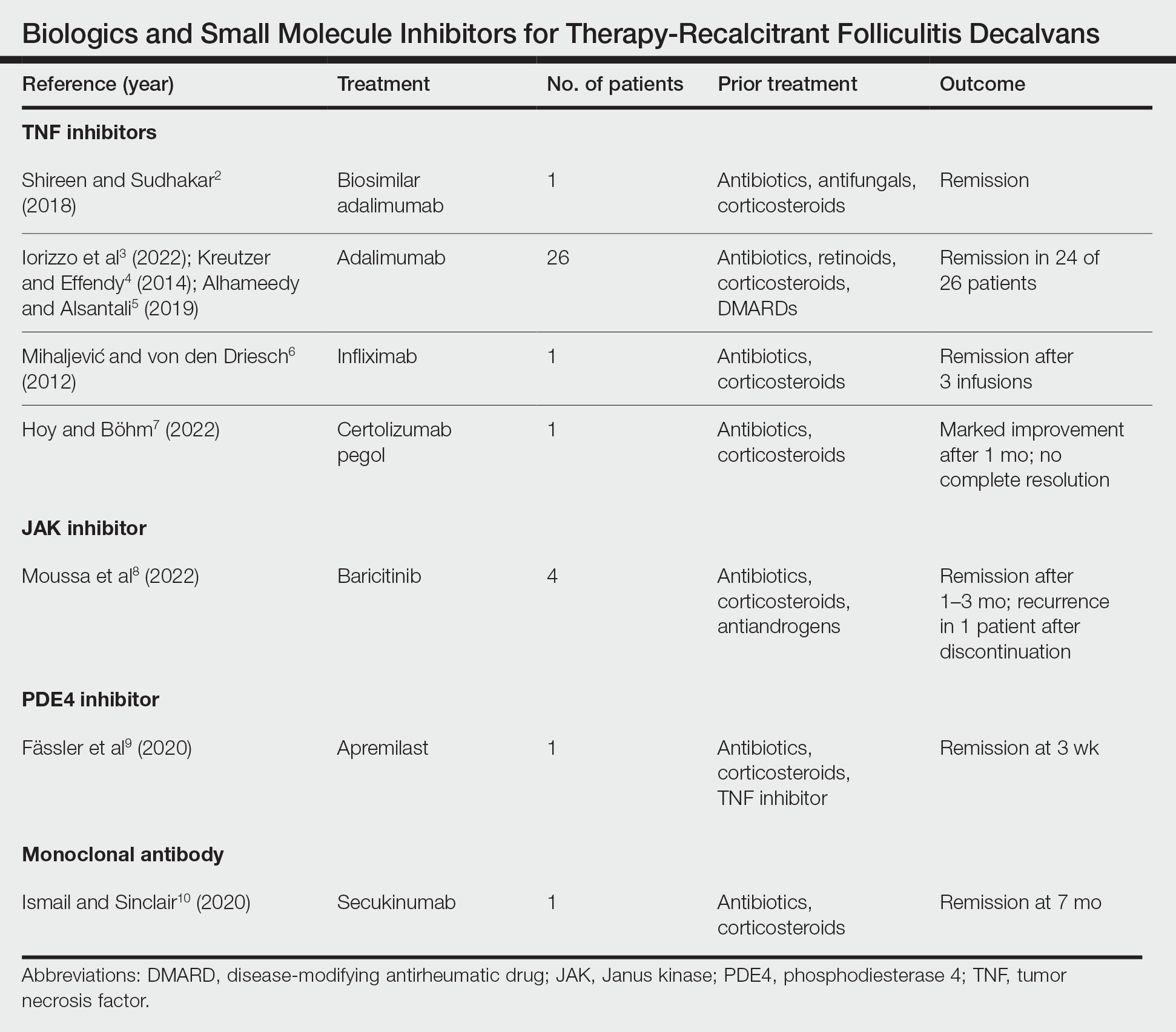
The TNF inhibitors were utilized in 6 reports with a combined total of 29 patients. Treatments included adalimumab or biosimilar adalimumab (27/29 patients), infliximab (1/29 patients), and certolizumab pegol (1/29 patients). Remission was reported in 26 of 29 cases. There were 2 nonresponders to adalimumab and marked improvement with certolizumab pegol without complete resolution. The use of the JAK inhibitor baricitinib in 4 patients resulted in remission. In all 4 patients, baricitinib was used with concurrent treatments, and remission was achieved in an average of 2.25 months. The use of a PDE4 inhibitor, apremilast, was reported in 1 case; remission was achieved in 3 weeks. Secukinumab, a monoclonal antibody that targets IL-17, was utilized in 1 patient. Marked improvement was seen after 2 months, with complete remission in 7 months.
Comment
Traditional treatment regimens for FD most often include a combination of topical and oral antibiotics; isotretinoin; and oral, topical, or intralesional corticosteroids. In the past, interventions typically were suppressive as opposed to curative; however, recent treatment advancements have shown promise in achieving lasting remission.
Most reports targeting treatment-resistant FD involved the use of TNF inhibitors, including adalimumab, biosimilar adalimumab, infliximab, and certolizumab pegol. Adalimumab was the most frequently used TNF inhibitor, with 24 of 26 treated patients achieving remission. Adalimumab may have been used the most in the treatment of FD because TNF is pronounced in other neutrophilic dermatoses that have been successfully treated with TNF inhibitors. It has been reported that adalimumab needs to be continued, as stoppage or interruption led to relapse.3
Although there are few reports of the use of JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies for FD, these treatment modalities show promise, as their use led to marked improvement or lasting remission with ongoing treatment. The use of the PDE4 inhibitor apremilast displayed the most rapid improvement of any of the reviewed treatments, with remission achieved in just 3 weeks.9 The rapid success of apremilast may be attributed to the inhibitory effect on neutrophils.
Miguel-Gómez et al11 provided a therapeutic protocol for FD based on the severity of disease (N=60). The protocol included rifampicin plus clindamycin for the treatment of severe disease, as 90.5% (19/21) of resistant cases showed clinical response, with remission of 5 months’ duration. Although this may be acceptable for some patients, others may require an alternative approach. Tietze et al12 showed that rifampicin and clindamycin had the lowest success rate for long-term remission, with 8 of 10 patients relapsing within 2 to 4 months. In addition, the emergence of antimicrobial resistance remains a major concern in the treatment of FD. Upon the review of the most recent reports of successful treatment of therapy-resistant FD, biologics and small molecule inhibitors have shown remission extending through a 12-month follow-up period. We suggest considering the addition of biologics and small molecule inhibitors to the treatment protocol for severe or resistant disease.
Limitations—In the articles reviewed, the definition of remission was inconsistent among authors—some characterized it as no recurrence in lesions or pustules and some as a reduction in the inflammatory process. True duration of remission was difficult to assess from case reports, as follow-up periods varied prior to publication. The studies included in this review consisted mainly of small sample sizes owing to the rarity of FD, and consequently, strength of evidence is lacking. Inherent to the nature of systematic reviews, publication bias may have occurred. Lastly, several studies were impacted by difficulty in obtaining optimal treatment due to financial hardship, and regimens were adjusted accordingly.
Conclusion
The relapsing nature of FD leads to frustration and poor quality of life for patients. There is a paucity of data to guide treatment when FD remains recalcitrant to traditional therapy. Therapies such as TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies have shown success in the treatment of this often difficult-to-treat disease. Small sample sizes in reports discussing treatment for resistant cases as well as conflicting results make it challenging to draw conclusions about treatment efficacy. Larger studies are needed to understand the long-term outcomes of treatment options. Regardless, disease severity, patient history, patient preferences, and treatment goals can guide the selection of therapeutic options.
- Otberg N, Kang H, Alzolibani AA, et al. Folliculitis decalvans. Dermatol Ther. 2008;21:238-244. doi:10.1111/j.1529-8019.2008.00204.x
- Shireen F, Sudhakar A. A case of isotretinoin therapy-refractory folliculitis decalvans treated successfully with biosimilar adalimumab (Exemptia). Int J Trichology. 2018;10:240-241.
- Iorizzo M, Starace M, Vano-Galvan S, et al. Refractory folliculitis decalvans treated with adalimumab: a case series of 23 patients. J Am Acad Dermatol. 2022;87:666-669. doi:10.1016/j.jaad.2022.02.044
- Kreutzer K, Effendy I. Therapy-resistant folliculitis decalvans and lichen planopilaris successfully treated with adalimumab. J Dtsch Dermatol Ges. 2014;12:74-76. doi:10.1111/ddg.12224
- Alhameedy MM, Alsantali AM. Therapy-recalcitrant folliculitis decalvans controlled successfully with adalimumab. Int J Trichology. 2019;11:241-243. doi:10.4103/ijt.ijt_92_19
- Mihaljevic´ N, von den Driesch P. Successful use of infliximab in a patient with recalcitrant folliculitis decalvans. J Dtsch Dermatol Ges. 2012;10:589-590. doi:10.1111/j.1610-0387.2012.07972.x
- Hoy M, Böhm M. Therapy-refractory folliculitis decalvans treated with certolizumab pegol. Int J Dermatol. 2022;61:e26-e28. doi:10.1111/ijd.15914
- Moussa A, Asfour L, Eisman S, et al. Successful treatment of folliculitis decalvans with baricitinib: a case series. Australas J Dermatol. 2022;63:279-281. doi:10.1111/ajd.13786
- Fässler M, Radonjic-Hoesli S, Feldmeyer L, et al. Successful treatment of refractory folliculitis decalvans with apremilast. JAAD Case Rep. 2020;6:1079-1081. doi:10.1016/j.jdcr.2020.08.019
- Ismail FF, Sinclair R. Successful treatment of refractory folliculitis decalvans with secukinumab. Australas J Dermatol. 2020;61:165-166. doi:10.1111/ajd.13190
- Miguel-Gómez L, Rodrigues-Barata AR, Molina-Ruiz A, et al. Folliculitis decalvans: effectiveness of therapies and prognostic factors in a multicenter series of 60 patients with long-term follow-up. J Am Acad Dermatol. 2018;79:878-883. doi:10.1016/j.jaad.2018.05.1240
- Tietze JK, Heppt MV, von Preußen A, et al. Oral isotretinoin as the most effective treatment in folliculitis decalvans: a retrospective comparison of different treatment regimens in 28 patients. J Eur Acad Dermatol Venereol. 2015;29:1816-1821. doi:10.1111/jdv.13052
Folliculitis decalvans (FD) is classified as a rare primary neutrophilic cicatricial alopecia occurring predominantly in middle-aged adults. Although the true etiology is still unknown, the pathogenesis behind the inflammatory follicular lesions stems from possible Staphylococcus aureus infection and an impaired host immune system in response to released superantigens. 1 The clinical severity of this inflammatory scalp disorder can range from mild to severe and debilitating. Multiple treatment regimens have been developed with the goal of maintaining full remission. We provide a summary of tumor necrosis factor (TNF) inhibitors, Janus kinase (JAK) inhibitors, phosphodiesterase 4 (PDE4) inhibitors, and monoclonal antibodies being utilized for patients with therapy-recalcitrant FD.
Methods
We conducted a PubMed, Medline, and Google Scholar search for the terms refractory FD, recalcitrant FD, or therapy-resistant FD to identify articles published in English from 1998 to 2022. Articles that reported recalcitrant cases and subsequent therapy with TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies were included. Articles were excluded if recalcitrant cases were not clearly defined. Remission was defined as no recurrence in lesions or pustules or as a reduction in the inflammatory process with stabilization upon continuation or discontinuation of the therapy regimen. Two reviewers (T.F. and K.U.) independently searched for and screened each report.
Results
Treatment of recalcitrant FD with biologics or small molecule inhibitors was discussed in 9 studies with a combined total of 35 patients.2-10 The treatment regimens included TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies (Table).
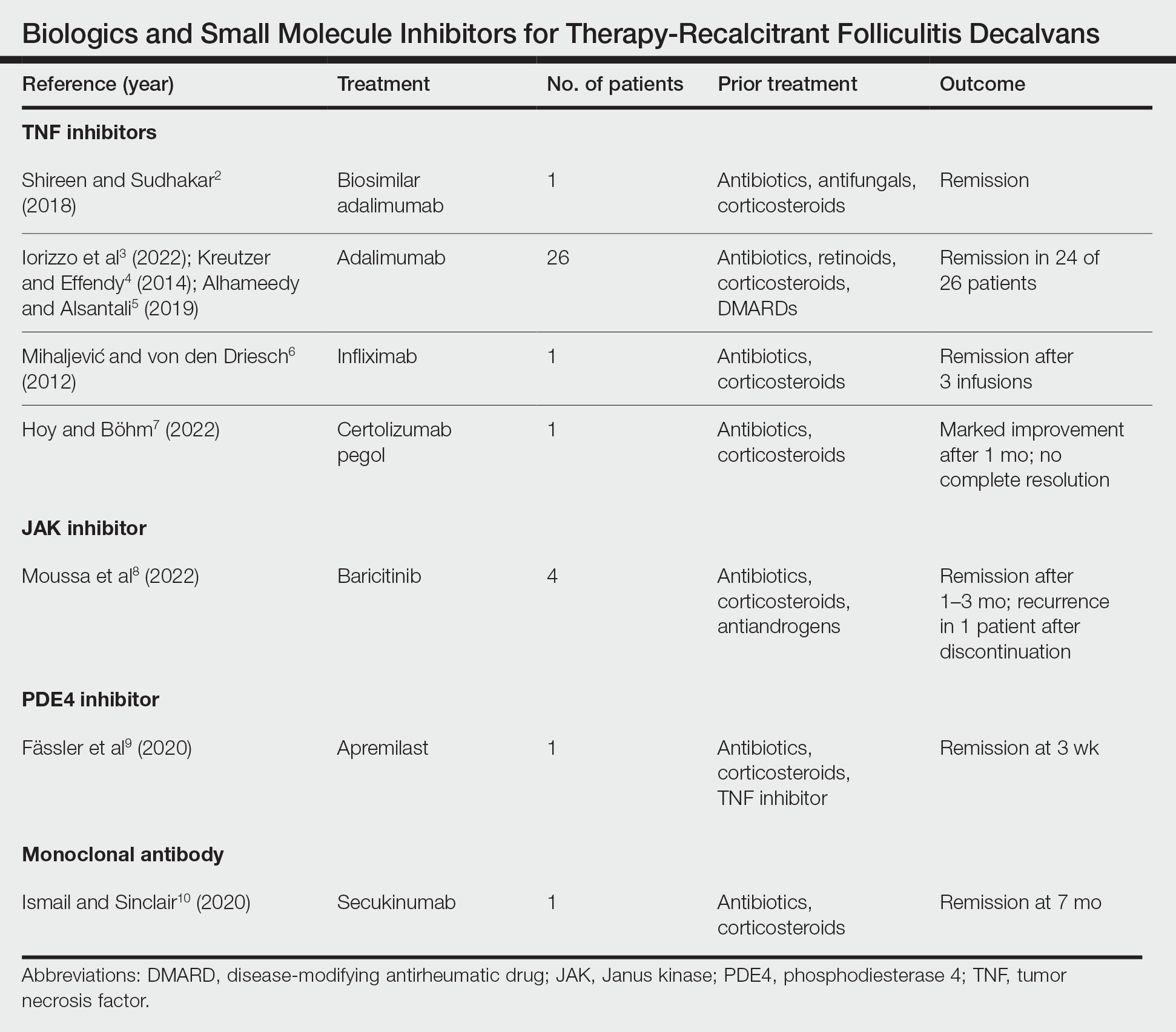
The TNF inhibitors were utilized in 6 reports with a combined total of 29 patients. Treatments included adalimumab or biosimilar adalimumab (27/29 patients), infliximab (1/29 patients), and certolizumab pegol (1/29 patients). Remission was reported in 26 of 29 cases. There were 2 nonresponders to adalimumab and marked improvement with certolizumab pegol without complete resolution. The use of the JAK inhibitor baricitinib in 4 patients resulted in remission. In all 4 patients, baricitinib was used with concurrent treatments, and remission was achieved in an average of 2.25 months. The use of a PDE4 inhibitor, apremilast, was reported in 1 case; remission was achieved in 3 weeks. Secukinumab, a monoclonal antibody that targets IL-17, was utilized in 1 patient. Marked improvement was seen after 2 months, with complete remission in 7 months.
Comment
Traditional treatment regimens for FD most often include a combination of topical and oral antibiotics; isotretinoin; and oral, topical, or intralesional corticosteroids. In the past, interventions typically were suppressive as opposed to curative; however, recent treatment advancements have shown promise in achieving lasting remission.
Most reports targeting treatment-resistant FD involved the use of TNF inhibitors, including adalimumab, biosimilar adalimumab, infliximab, and certolizumab pegol. Adalimumab was the most frequently used TNF inhibitor, with 24 of 26 treated patients achieving remission. Adalimumab may have been used the most in the treatment of FD because TNF is pronounced in other neutrophilic dermatoses that have been successfully treated with TNF inhibitors. It has been reported that adalimumab needs to be continued, as stoppage or interruption led to relapse.3
Although there are few reports of the use of JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies for FD, these treatment modalities show promise, as their use led to marked improvement or lasting remission with ongoing treatment. The use of the PDE4 inhibitor apremilast displayed the most rapid improvement of any of the reviewed treatments, with remission achieved in just 3 weeks.9 The rapid success of apremilast may be attributed to the inhibitory effect on neutrophils.
Miguel-Gómez et al11 provided a therapeutic protocol for FD based on the severity of disease (N=60). The protocol included rifampicin plus clindamycin for the treatment of severe disease, as 90.5% (19/21) of resistant cases showed clinical response, with remission of 5 months’ duration. Although this may be acceptable for some patients, others may require an alternative approach. Tietze et al12 showed that rifampicin and clindamycin had the lowest success rate for long-term remission, with 8 of 10 patients relapsing within 2 to 4 months. In addition, the emergence of antimicrobial resistance remains a major concern in the treatment of FD. Upon the review of the most recent reports of successful treatment of therapy-resistant FD, biologics and small molecule inhibitors have shown remission extending through a 12-month follow-up period. We suggest considering the addition of biologics and small molecule inhibitors to the treatment protocol for severe or resistant disease.
Limitations—In the articles reviewed, the definition of remission was inconsistent among authors—some characterized it as no recurrence in lesions or pustules and some as a reduction in the inflammatory process. True duration of remission was difficult to assess from case reports, as follow-up periods varied prior to publication. The studies included in this review consisted mainly of small sample sizes owing to the rarity of FD, and consequently, strength of evidence is lacking. Inherent to the nature of systematic reviews, publication bias may have occurred. Lastly, several studies were impacted by difficulty in obtaining optimal treatment due to financial hardship, and regimens were adjusted accordingly.
Conclusion
The relapsing nature of FD leads to frustration and poor quality of life for patients. There is a paucity of data to guide treatment when FD remains recalcitrant to traditional therapy. Therapies such as TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies have shown success in the treatment of this often difficult-to-treat disease. Small sample sizes in reports discussing treatment for resistant cases as well as conflicting results make it challenging to draw conclusions about treatment efficacy. Larger studies are needed to understand the long-term outcomes of treatment options. Regardless, disease severity, patient history, patient preferences, and treatment goals can guide the selection of therapeutic options.
Folliculitis decalvans (FD) is classified as a rare primary neutrophilic cicatricial alopecia occurring predominantly in middle-aged adults. Although the true etiology is still unknown, the pathogenesis behind the inflammatory follicular lesions stems from possible Staphylococcus aureus infection and an impaired host immune system in response to released superantigens. 1 The clinical severity of this inflammatory scalp disorder can range from mild to severe and debilitating. Multiple treatment regimens have been developed with the goal of maintaining full remission. We provide a summary of tumor necrosis factor (TNF) inhibitors, Janus kinase (JAK) inhibitors, phosphodiesterase 4 (PDE4) inhibitors, and monoclonal antibodies being utilized for patients with therapy-recalcitrant FD.
Methods
We conducted a PubMed, Medline, and Google Scholar search for the terms refractory FD, recalcitrant FD, or therapy-resistant FD to identify articles published in English from 1998 to 2022. Articles that reported recalcitrant cases and subsequent therapy with TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies were included. Articles were excluded if recalcitrant cases were not clearly defined. Remission was defined as no recurrence in lesions or pustules or as a reduction in the inflammatory process with stabilization upon continuation or discontinuation of the therapy regimen. Two reviewers (T.F. and K.U.) independently searched for and screened each report.
Results
Treatment of recalcitrant FD with biologics or small molecule inhibitors was discussed in 9 studies with a combined total of 35 patients.2-10 The treatment regimens included TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies (Table).
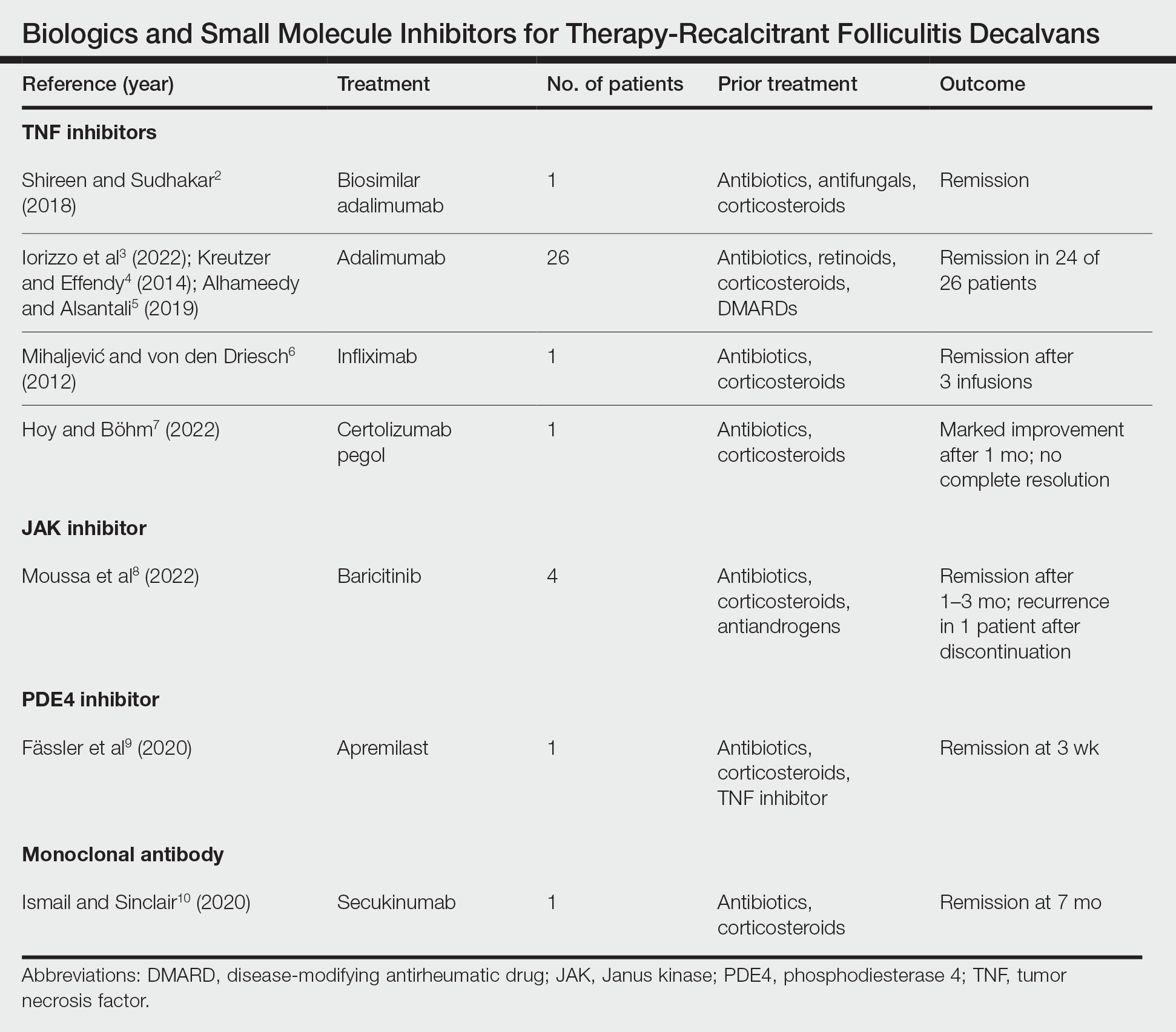
The TNF inhibitors were utilized in 6 reports with a combined total of 29 patients. Treatments included adalimumab or biosimilar adalimumab (27/29 patients), infliximab (1/29 patients), and certolizumab pegol (1/29 patients). Remission was reported in 26 of 29 cases. There were 2 nonresponders to adalimumab and marked improvement with certolizumab pegol without complete resolution. The use of the JAK inhibitor baricitinib in 4 patients resulted in remission. In all 4 patients, baricitinib was used with concurrent treatments, and remission was achieved in an average of 2.25 months. The use of a PDE4 inhibitor, apremilast, was reported in 1 case; remission was achieved in 3 weeks. Secukinumab, a monoclonal antibody that targets IL-17, was utilized in 1 patient. Marked improvement was seen after 2 months, with complete remission in 7 months.
Comment
Traditional treatment regimens for FD most often include a combination of topical and oral antibiotics; isotretinoin; and oral, topical, or intralesional corticosteroids. In the past, interventions typically were suppressive as opposed to curative; however, recent treatment advancements have shown promise in achieving lasting remission.
Most reports targeting treatment-resistant FD involved the use of TNF inhibitors, including adalimumab, biosimilar adalimumab, infliximab, and certolizumab pegol. Adalimumab was the most frequently used TNF inhibitor, with 24 of 26 treated patients achieving remission. Adalimumab may have been used the most in the treatment of FD because TNF is pronounced in other neutrophilic dermatoses that have been successfully treated with TNF inhibitors. It has been reported that adalimumab needs to be continued, as stoppage or interruption led to relapse.3
Although there are few reports of the use of JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies for FD, these treatment modalities show promise, as their use led to marked improvement or lasting remission with ongoing treatment. The use of the PDE4 inhibitor apremilast displayed the most rapid improvement of any of the reviewed treatments, with remission achieved in just 3 weeks.9 The rapid success of apremilast may be attributed to the inhibitory effect on neutrophils.
Miguel-Gómez et al11 provided a therapeutic protocol for FD based on the severity of disease (N=60). The protocol included rifampicin plus clindamycin for the treatment of severe disease, as 90.5% (19/21) of resistant cases showed clinical response, with remission of 5 months’ duration. Although this may be acceptable for some patients, others may require an alternative approach. Tietze et al12 showed that rifampicin and clindamycin had the lowest success rate for long-term remission, with 8 of 10 patients relapsing within 2 to 4 months. In addition, the emergence of antimicrobial resistance remains a major concern in the treatment of FD. Upon the review of the most recent reports of successful treatment of therapy-resistant FD, biologics and small molecule inhibitors have shown remission extending through a 12-month follow-up period. We suggest considering the addition of biologics and small molecule inhibitors to the treatment protocol for severe or resistant disease.
Limitations—In the articles reviewed, the definition of remission was inconsistent among authors—some characterized it as no recurrence in lesions or pustules and some as a reduction in the inflammatory process. True duration of remission was difficult to assess from case reports, as follow-up periods varied prior to publication. The studies included in this review consisted mainly of small sample sizes owing to the rarity of FD, and consequently, strength of evidence is lacking. Inherent to the nature of systematic reviews, publication bias may have occurred. Lastly, several studies were impacted by difficulty in obtaining optimal treatment due to financial hardship, and regimens were adjusted accordingly.
Conclusion
The relapsing nature of FD leads to frustration and poor quality of life for patients. There is a paucity of data to guide treatment when FD remains recalcitrant to traditional therapy. Therapies such as TNF inhibitors, JAK inhibitors, PDE4 inhibitors, and monoclonal antibodies have shown success in the treatment of this often difficult-to-treat disease. Small sample sizes in reports discussing treatment for resistant cases as well as conflicting results make it challenging to draw conclusions about treatment efficacy. Larger studies are needed to understand the long-term outcomes of treatment options. Regardless, disease severity, patient history, patient preferences, and treatment goals can guide the selection of therapeutic options.
- Otberg N, Kang H, Alzolibani AA, et al. Folliculitis decalvans. Dermatol Ther. 2008;21:238-244. doi:10.1111/j.1529-8019.2008.00204.x
- Shireen F, Sudhakar A. A case of isotretinoin therapy-refractory folliculitis decalvans treated successfully with biosimilar adalimumab (Exemptia). Int J Trichology. 2018;10:240-241.
- Iorizzo M, Starace M, Vano-Galvan S, et al. Refractory folliculitis decalvans treated with adalimumab: a case series of 23 patients. J Am Acad Dermatol. 2022;87:666-669. doi:10.1016/j.jaad.2022.02.044
- Kreutzer K, Effendy I. Therapy-resistant folliculitis decalvans and lichen planopilaris successfully treated with adalimumab. J Dtsch Dermatol Ges. 2014;12:74-76. doi:10.1111/ddg.12224
- Alhameedy MM, Alsantali AM. Therapy-recalcitrant folliculitis decalvans controlled successfully with adalimumab. Int J Trichology. 2019;11:241-243. doi:10.4103/ijt.ijt_92_19
- Mihaljevic´ N, von den Driesch P. Successful use of infliximab in a patient with recalcitrant folliculitis decalvans. J Dtsch Dermatol Ges. 2012;10:589-590. doi:10.1111/j.1610-0387.2012.07972.x
- Hoy M, Böhm M. Therapy-refractory folliculitis decalvans treated with certolizumab pegol. Int J Dermatol. 2022;61:e26-e28. doi:10.1111/ijd.15914
- Moussa A, Asfour L, Eisman S, et al. Successful treatment of folliculitis decalvans with baricitinib: a case series. Australas J Dermatol. 2022;63:279-281. doi:10.1111/ajd.13786
- Fässler M, Radonjic-Hoesli S, Feldmeyer L, et al. Successful treatment of refractory folliculitis decalvans with apremilast. JAAD Case Rep. 2020;6:1079-1081. doi:10.1016/j.jdcr.2020.08.019
- Ismail FF, Sinclair R. Successful treatment of refractory folliculitis decalvans with secukinumab. Australas J Dermatol. 2020;61:165-166. doi:10.1111/ajd.13190
- Miguel-Gómez L, Rodrigues-Barata AR, Molina-Ruiz A, et al. Folliculitis decalvans: effectiveness of therapies and prognostic factors in a multicenter series of 60 patients with long-term follow-up. J Am Acad Dermatol. 2018;79:878-883. doi:10.1016/j.jaad.2018.05.1240
- Tietze JK, Heppt MV, von Preußen A, et al. Oral isotretinoin as the most effective treatment in folliculitis decalvans: a retrospective comparison of different treatment regimens in 28 patients. J Eur Acad Dermatol Venereol. 2015;29:1816-1821. doi:10.1111/jdv.13052
- Otberg N, Kang H, Alzolibani AA, et al. Folliculitis decalvans. Dermatol Ther. 2008;21:238-244. doi:10.1111/j.1529-8019.2008.00204.x
- Shireen F, Sudhakar A. A case of isotretinoin therapy-refractory folliculitis decalvans treated successfully with biosimilar adalimumab (Exemptia). Int J Trichology. 2018;10:240-241.
- Iorizzo M, Starace M, Vano-Galvan S, et al. Refractory folliculitis decalvans treated with adalimumab: a case series of 23 patients. J Am Acad Dermatol. 2022;87:666-669. doi:10.1016/j.jaad.2022.02.044
- Kreutzer K, Effendy I. Therapy-resistant folliculitis decalvans and lichen planopilaris successfully treated with adalimumab. J Dtsch Dermatol Ges. 2014;12:74-76. doi:10.1111/ddg.12224
- Alhameedy MM, Alsantali AM. Therapy-recalcitrant folliculitis decalvans controlled successfully with adalimumab. Int J Trichology. 2019;11:241-243. doi:10.4103/ijt.ijt_92_19
- Mihaljevic´ N, von den Driesch P. Successful use of infliximab in a patient with recalcitrant folliculitis decalvans. J Dtsch Dermatol Ges. 2012;10:589-590. doi:10.1111/j.1610-0387.2012.07972.x
- Hoy M, Böhm M. Therapy-refractory folliculitis decalvans treated with certolizumab pegol. Int J Dermatol. 2022;61:e26-e28. doi:10.1111/ijd.15914
- Moussa A, Asfour L, Eisman S, et al. Successful treatment of folliculitis decalvans with baricitinib: a case series. Australas J Dermatol. 2022;63:279-281. doi:10.1111/ajd.13786
- Fässler M, Radonjic-Hoesli S, Feldmeyer L, et al. Successful treatment of refractory folliculitis decalvans with apremilast. JAAD Case Rep. 2020;6:1079-1081. doi:10.1016/j.jdcr.2020.08.019
- Ismail FF, Sinclair R. Successful treatment of refractory folliculitis decalvans with secukinumab. Australas J Dermatol. 2020;61:165-166. doi:10.1111/ajd.13190
- Miguel-Gómez L, Rodrigues-Barata AR, Molina-Ruiz A, et al. Folliculitis decalvans: effectiveness of therapies and prognostic factors in a multicenter series of 60 patients with long-term follow-up. J Am Acad Dermatol. 2018;79:878-883. doi:10.1016/j.jaad.2018.05.1240
- Tietze JK, Heppt MV, von Preußen A, et al. Oral isotretinoin as the most effective treatment in folliculitis decalvans: a retrospective comparison of different treatment regimens in 28 patients. J Eur Acad Dermatol Venereol. 2015;29:1816-1821. doi:10.1111/jdv.13052
Practice Points
- Tumor necrosis factor inhibitors, Janus kinase inhibitors, phosphodiesterase 4 inhibitors, and monoclonal antibodies have shown success in the treatment of folliculitis decalvans resistant to traditional therapies.
- The true etiology of folliculitis decalvans is still unknown, but possible factors include Staphylococcus aureus infection and an impaired host immune system, which may benefit from treatment with biologics and small molecule inhibitors.
Complementing, not competing
As we enter summer, it’s hard to believe that we’re halfway through my presidency. Registration for CHEST 2024 (October 6 to 9) is now open, and October will be here before we know it.
I’m happy to share that we received more than 4,000 abstract and case report submissions from clinicians at all stages of their careers, and, for the first year, we had a dedicated category to solicit submissions from physician assistants (PAs), nurse practitioners (NPs), respiratory therapists, and other members of the broader health care team.
In both my practice and my time as CHEST President, I’ve been reflecting on the benefits of the multidisciplinary team—especially in the ICU. Because this is a setting that relies heavily on a team aspect, every member of the care team is a great asset.
CHEST is working to ensure that all integral members of our professional health care teams have the resources they need to best serve our patients. We encourage advanced practice providers (APPs) to apply to serve on our committees during the current open call, and we recently launched a dedicated APP Intersection column, called APP Intersection, within this publication to elevate diverse perspectives. I anticipate more is on the horizon.
In my experience, I have seen tremendous success in partnering with and complementing each other, rather than competing for space when caring for a patient. Each and every one of us shares the same goal of providing the best patient care, and we each bring our own strengths.
Our future is ripe with opportunities to better serve the whole care team—MDs, PAs, NPs, and more—and it starts with recognizing the needs of everyone within the organization. To help CHEST better serve our members, I encourage you to take a short survey about your professional hurdles.
And please, do not hesitate to contact me (president@chestnet.org) with suggestions or just to introduce yourself.
All the best,
Jack
As we enter summer, it’s hard to believe that we’re halfway through my presidency. Registration for CHEST 2024 (October 6 to 9) is now open, and October will be here before we know it.
I’m happy to share that we received more than 4,000 abstract and case report submissions from clinicians at all stages of their careers, and, for the first year, we had a dedicated category to solicit submissions from physician assistants (PAs), nurse practitioners (NPs), respiratory therapists, and other members of the broader health care team.
In both my practice and my time as CHEST President, I’ve been reflecting on the benefits of the multidisciplinary team—especially in the ICU. Because this is a setting that relies heavily on a team aspect, every member of the care team is a great asset.
CHEST is working to ensure that all integral members of our professional health care teams have the resources they need to best serve our patients. We encourage advanced practice providers (APPs) to apply to serve on our committees during the current open call, and we recently launched a dedicated APP Intersection column, called APP Intersection, within this publication to elevate diverse perspectives. I anticipate more is on the horizon.
In my experience, I have seen tremendous success in partnering with and complementing each other, rather than competing for space when caring for a patient. Each and every one of us shares the same goal of providing the best patient care, and we each bring our own strengths.
Our future is ripe with opportunities to better serve the whole care team—MDs, PAs, NPs, and more—and it starts with recognizing the needs of everyone within the organization. To help CHEST better serve our members, I encourage you to take a short survey about your professional hurdles.
And please, do not hesitate to contact me (president@chestnet.org) with suggestions or just to introduce yourself.
All the best,
Jack
As we enter summer, it’s hard to believe that we’re halfway through my presidency. Registration for CHEST 2024 (October 6 to 9) is now open, and October will be here before we know it.
I’m happy to share that we received more than 4,000 abstract and case report submissions from clinicians at all stages of their careers, and, for the first year, we had a dedicated category to solicit submissions from physician assistants (PAs), nurse practitioners (NPs), respiratory therapists, and other members of the broader health care team.
In both my practice and my time as CHEST President, I’ve been reflecting on the benefits of the multidisciplinary team—especially in the ICU. Because this is a setting that relies heavily on a team aspect, every member of the care team is a great asset.
CHEST is working to ensure that all integral members of our professional health care teams have the resources they need to best serve our patients. We encourage advanced practice providers (APPs) to apply to serve on our committees during the current open call, and we recently launched a dedicated APP Intersection column, called APP Intersection, within this publication to elevate diverse perspectives. I anticipate more is on the horizon.
In my experience, I have seen tremendous success in partnering with and complementing each other, rather than competing for space when caring for a patient. Each and every one of us shares the same goal of providing the best patient care, and we each bring our own strengths.
Our future is ripe with opportunities to better serve the whole care team—MDs, PAs, NPs, and more—and it starts with recognizing the needs of everyone within the organization. To help CHEST better serve our members, I encourage you to take a short survey about your professional hurdles.
And please, do not hesitate to contact me (president@chestnet.org) with suggestions or just to introduce yourself.
All the best,
Jack
Nurse practitioners as advocates for health policy and patient care
APP INTERSECTION
In the intricate tapestry of health care, the roles of advanced practice registered nurses, also known as nurse practitioners (NPs), have evolved beyond the confines of clinical settings.
The journey into the realm of nursing often begins with a passion for healing and caring for others. However, for many, this path frequently leads to overcoming barriers to patient care, restrictions to practice, and lengthy red tape in the face of care teams that do not fully understand the scope and role of the NP.
Delving into health policy intricacies, efforts focus on understanding how legislative decisions directly impact patient care. Involvement in advocacy aims to improve health care access, promote patient-centered policies, and reduce disparities in the workforce and patient care.
Achieving sound primary care for people with multiple comorbid conditions requires the skills and abilities of all members of the health care workforce, including NPs.1 NPs have assumed an increasing role in recent decades as primary care providers for people with chronic diseases, while national trends show few physicians entering and staying in primary care.2,3,4,5 NPs are the nation’s fastest-growing primary care workforce, with nearly 90% of them trained to deliver primary care.6,7 Yet, NPs continue to experience reduced reimbursement for services compared with their physician counterparts.
Barriers to practice reduce the productivity and capacity of these health care professionals. Not permitting NPs to practice to the full extent of their licensure and education decreases the types and amounts of health care services that can be provided for people who need care.8As noted in the Future of Nursing 2020-2030 report, this restriction also has significant implications for addressing the disparities in access to health care between rural and urban areas. A recent systemic review revealed that full practice authority is associated with higher numbers of NPs in rural areas and in primary care where there is a shortage of physicians. Full practice authority is associated with increased access to care and utilization of health care services, lower cost of care, and no decrease in quality of care.9,10 As stated in the National Council of State Boards of Nursing 2022 Environmental Scan, regulators and nurse leaders are responsible for upholding rules and regulations of nursing practice as well as ensuring that standards of care are met and patients are protected.11
Of equal importance is regulator awareness of the degree to which barriers continue to impact NP practice and limit aspects of care that directly influence care quality and access. Nursing leaders can have a significant impact on removing nonregulatory barriers to practice, such as changing outdated hospital bylaws that restrict NP practice. In turn, regulators can support efforts to remove unnecessary barriers to NP practice.
Fueled by experience in reduced practice, NPs become catalysts for change, transcending the role of health care providers. At the core of the NP role lies a commitment to patient advocacy. Beyond diagnosing and treating illnesses, NPs champion patients’ rights, ensuring their voices in health care decision-making. Advocacy efforts range from expanding access to essential services to promoting preventive care and fighting discrimination. By embracing roles as caregivers and agents of change, NPs can help the health care system emerge equitable, accessible, and patient-centric.
Ms. Kavanaugh is Assistant Dean of Graduate Nursing, University of Mount Saint Vincent, Pulmonary Critical Care Nurse Practitioner, Stamford Hospital.
References
1. McMenamin, A., Turi, E., Schlak, A., & Poghosyan, L. (2023). A Systematic Review of Outcomes Related to Nurse Practitioner-Delivered Primary Care for Multiple Chronic Conditions. Medical care research and review: MCRR, 80(6), 563–581. https://doi.org/10.1177/10775587231186720
2. Fraze T, Briggs A, Whitcomb E, Peck K, & Meara E (2020). Role of nurse practitioners in caring for patients with complex health needs. Medical Care, 58(10), 853–860. 10.1097/mlr.0000000000001364
3. Xue Y, Goodwin J, Adhikari D, Raji M, & Kuo Y (2017). Trends in primary care provision to medicare beneficiaries by physicians, nurse practitioners, or physician assistants: 2008–2014. Journal of Primary Care & Community Health, 8(4), 256–263. 10.1177/2150131917736634
4. Buerhaus P (2018). Nurse practitioners: A solution to America’s primary care crisis. American Enterprise Institute. https://www.aei.org/research-products/report/nurse-practitioners-a-solution-to-americas-primary-care-crisis/
5. Xue Y, Goodwin J, Adhikari D, Raji M, & Kuo Y (2017). Trends in primary care provision to medicare beneficiaries by physicians, nurse practitioners, or physician assistants: 2008–2014. Journal of Primary Care & Community Health, 8(4), 256–263. 10.1177/2150131917736634
6. American Association of Nurse Practitioners. (2022). Nurse practitioners in primary care. https://www.aanp.org/advocacy/advocacy-resource/position-statements/nurse-practitioners-in-primary-care
7. Auerbach, D. I. (2012). Will the NP workforce grow in the future? New forecasts and implications for healthcare delivery. Medical Care, 50(7), 606-610. doi: http://dx.doi.org/10.1097/MLR.0b013e318249d6e7
8. National Academy of Medicine . The National Academies Press; 2021. The future of nursing 2020-2030: Charting a path to achieve health equity.
9. Yang BK, Trinkoff AM, Zito JM, Burcu M, Safer DJ, Storr CL, Johantgen ME, & Idzik S (2017). Nurse practitioner independent practice authority and mental health service delivery in U.S. Community Health Centers. Psychiatric Services, 68(10), 1032–1038. 10.1176/appi.ps.201600495
10. Xue Y., Kannan V., Greener E., Smith J.A., Brasch J., Johnson B.A., Spetz J. Full scope-of-practice regulation is associated with higher supply of nurse practitioners in rural and primary care health professional shortage counties. Journal of Nursing Regulation. 2018;8(4):5–13. doi: 10.1016/S2155-8256(17)30176-X.
11. National Council of State Boards of Nursing The NCSBN 2022 environmental scan: Resiliency, achievement, and public protection. Journal of Nursing Regulation. 2022;12:S3–S55. doi: 10.1016/S2155-8256(22)00015-1.
APP INTERSECTION
In the intricate tapestry of health care, the roles of advanced practice registered nurses, also known as nurse practitioners (NPs), have evolved beyond the confines of clinical settings.
The journey into the realm of nursing often begins with a passion for healing and caring for others. However, for many, this path frequently leads to overcoming barriers to patient care, restrictions to practice, and lengthy red tape in the face of care teams that do not fully understand the scope and role of the NP.
Delving into health policy intricacies, efforts focus on understanding how legislative decisions directly impact patient care. Involvement in advocacy aims to improve health care access, promote patient-centered policies, and reduce disparities in the workforce and patient care.
Achieving sound primary care for people with multiple comorbid conditions requires the skills and abilities of all members of the health care workforce, including NPs.1 NPs have assumed an increasing role in recent decades as primary care providers for people with chronic diseases, while national trends show few physicians entering and staying in primary care.2,3,4,5 NPs are the nation’s fastest-growing primary care workforce, with nearly 90% of them trained to deliver primary care.6,7 Yet, NPs continue to experience reduced reimbursement for services compared with their physician counterparts.
Barriers to practice reduce the productivity and capacity of these health care professionals. Not permitting NPs to practice to the full extent of their licensure and education decreases the types and amounts of health care services that can be provided for people who need care.8As noted in the Future of Nursing 2020-2030 report, this restriction also has significant implications for addressing the disparities in access to health care between rural and urban areas. A recent systemic review revealed that full practice authority is associated with higher numbers of NPs in rural areas and in primary care where there is a shortage of physicians. Full practice authority is associated with increased access to care and utilization of health care services, lower cost of care, and no decrease in quality of care.9,10 As stated in the National Council of State Boards of Nursing 2022 Environmental Scan, regulators and nurse leaders are responsible for upholding rules and regulations of nursing practice as well as ensuring that standards of care are met and patients are protected.11
Of equal importance is regulator awareness of the degree to which barriers continue to impact NP practice and limit aspects of care that directly influence care quality and access. Nursing leaders can have a significant impact on removing nonregulatory barriers to practice, such as changing outdated hospital bylaws that restrict NP practice. In turn, regulators can support efforts to remove unnecessary barriers to NP practice.
Fueled by experience in reduced practice, NPs become catalysts for change, transcending the role of health care providers. At the core of the NP role lies a commitment to patient advocacy. Beyond diagnosing and treating illnesses, NPs champion patients’ rights, ensuring their voices in health care decision-making. Advocacy efforts range from expanding access to essential services to promoting preventive care and fighting discrimination. By embracing roles as caregivers and agents of change, NPs can help the health care system emerge equitable, accessible, and patient-centric.
Ms. Kavanaugh is Assistant Dean of Graduate Nursing, University of Mount Saint Vincent, Pulmonary Critical Care Nurse Practitioner, Stamford Hospital.
References
1. McMenamin, A., Turi, E., Schlak, A., & Poghosyan, L. (2023). A Systematic Review of Outcomes Related to Nurse Practitioner-Delivered Primary Care for Multiple Chronic Conditions. Medical care research and review: MCRR, 80(6), 563–581. https://doi.org/10.1177/10775587231186720
2. Fraze T, Briggs A, Whitcomb E, Peck K, & Meara E (2020). Role of nurse practitioners in caring for patients with complex health needs. Medical Care, 58(10), 853–860. 10.1097/mlr.0000000000001364
3. Xue Y, Goodwin J, Adhikari D, Raji M, & Kuo Y (2017). Trends in primary care provision to medicare beneficiaries by physicians, nurse practitioners, or physician assistants: 2008–2014. Journal of Primary Care & Community Health, 8(4), 256–263. 10.1177/2150131917736634
4. Buerhaus P (2018). Nurse practitioners: A solution to America’s primary care crisis. American Enterprise Institute. https://www.aei.org/research-products/report/nurse-practitioners-a-solution-to-americas-primary-care-crisis/
5. Xue Y, Goodwin J, Adhikari D, Raji M, & Kuo Y (2017). Trends in primary care provision to medicare beneficiaries by physicians, nurse practitioners, or physician assistants: 2008–2014. Journal of Primary Care & Community Health, 8(4), 256–263. 10.1177/2150131917736634
6. American Association of Nurse Practitioners. (2022). Nurse practitioners in primary care. https://www.aanp.org/advocacy/advocacy-resource/position-statements/nurse-practitioners-in-primary-care
7. Auerbach, D. I. (2012). Will the NP workforce grow in the future? New forecasts and implications for healthcare delivery. Medical Care, 50(7), 606-610. doi: http://dx.doi.org/10.1097/MLR.0b013e318249d6e7
8. National Academy of Medicine . The National Academies Press; 2021. The future of nursing 2020-2030: Charting a path to achieve health equity.
9. Yang BK, Trinkoff AM, Zito JM, Burcu M, Safer DJ, Storr CL, Johantgen ME, & Idzik S (2017). Nurse practitioner independent practice authority and mental health service delivery in U.S. Community Health Centers. Psychiatric Services, 68(10), 1032–1038. 10.1176/appi.ps.201600495
10. Xue Y., Kannan V., Greener E., Smith J.A., Brasch J., Johnson B.A., Spetz J. Full scope-of-practice regulation is associated with higher supply of nurse practitioners in rural and primary care health professional shortage counties. Journal of Nursing Regulation. 2018;8(4):5–13. doi: 10.1016/S2155-8256(17)30176-X.
11. National Council of State Boards of Nursing The NCSBN 2022 environmental scan: Resiliency, achievement, and public protection. Journal of Nursing Regulation. 2022;12:S3–S55. doi: 10.1016/S2155-8256(22)00015-1.
APP INTERSECTION
In the intricate tapestry of health care, the roles of advanced practice registered nurses, also known as nurse practitioners (NPs), have evolved beyond the confines of clinical settings.
The journey into the realm of nursing often begins with a passion for healing and caring for others. However, for many, this path frequently leads to overcoming barriers to patient care, restrictions to practice, and lengthy red tape in the face of care teams that do not fully understand the scope and role of the NP.
Delving into health policy intricacies, efforts focus on understanding how legislative decisions directly impact patient care. Involvement in advocacy aims to improve health care access, promote patient-centered policies, and reduce disparities in the workforce and patient care.
Achieving sound primary care for people with multiple comorbid conditions requires the skills and abilities of all members of the health care workforce, including NPs.1 NPs have assumed an increasing role in recent decades as primary care providers for people with chronic diseases, while national trends show few physicians entering and staying in primary care.2,3,4,5 NPs are the nation’s fastest-growing primary care workforce, with nearly 90% of them trained to deliver primary care.6,7 Yet, NPs continue to experience reduced reimbursement for services compared with their physician counterparts.
Barriers to practice reduce the productivity and capacity of these health care professionals. Not permitting NPs to practice to the full extent of their licensure and education decreases the types and amounts of health care services that can be provided for people who need care.8As noted in the Future of Nursing 2020-2030 report, this restriction also has significant implications for addressing the disparities in access to health care between rural and urban areas. A recent systemic review revealed that full practice authority is associated with higher numbers of NPs in rural areas and in primary care where there is a shortage of physicians. Full practice authority is associated with increased access to care and utilization of health care services, lower cost of care, and no decrease in quality of care.9,10 As stated in the National Council of State Boards of Nursing 2022 Environmental Scan, regulators and nurse leaders are responsible for upholding rules and regulations of nursing practice as well as ensuring that standards of care are met and patients are protected.11
Of equal importance is regulator awareness of the degree to which barriers continue to impact NP practice and limit aspects of care that directly influence care quality and access. Nursing leaders can have a significant impact on removing nonregulatory barriers to practice, such as changing outdated hospital bylaws that restrict NP practice. In turn, regulators can support efforts to remove unnecessary barriers to NP practice.
Fueled by experience in reduced practice, NPs become catalysts for change, transcending the role of health care providers. At the core of the NP role lies a commitment to patient advocacy. Beyond diagnosing and treating illnesses, NPs champion patients’ rights, ensuring their voices in health care decision-making. Advocacy efforts range from expanding access to essential services to promoting preventive care and fighting discrimination. By embracing roles as caregivers and agents of change, NPs can help the health care system emerge equitable, accessible, and patient-centric.
Ms. Kavanaugh is Assistant Dean of Graduate Nursing, University of Mount Saint Vincent, Pulmonary Critical Care Nurse Practitioner, Stamford Hospital.
References
1. McMenamin, A., Turi, E., Schlak, A., & Poghosyan, L. (2023). A Systematic Review of Outcomes Related to Nurse Practitioner-Delivered Primary Care for Multiple Chronic Conditions. Medical care research and review: MCRR, 80(6), 563–581. https://doi.org/10.1177/10775587231186720
2. Fraze T, Briggs A, Whitcomb E, Peck K, & Meara E (2020). Role of nurse practitioners in caring for patients with complex health needs. Medical Care, 58(10), 853–860. 10.1097/mlr.0000000000001364
3. Xue Y, Goodwin J, Adhikari D, Raji M, & Kuo Y (2017). Trends in primary care provision to medicare beneficiaries by physicians, nurse practitioners, or physician assistants: 2008–2014. Journal of Primary Care & Community Health, 8(4), 256–263. 10.1177/2150131917736634
4. Buerhaus P (2018). Nurse practitioners: A solution to America’s primary care crisis. American Enterprise Institute. https://www.aei.org/research-products/report/nurse-practitioners-a-solution-to-americas-primary-care-crisis/
5. Xue Y, Goodwin J, Adhikari D, Raji M, & Kuo Y (2017). Trends in primary care provision to medicare beneficiaries by physicians, nurse practitioners, or physician assistants: 2008–2014. Journal of Primary Care & Community Health, 8(4), 256–263. 10.1177/2150131917736634
6. American Association of Nurse Practitioners. (2022). Nurse practitioners in primary care. https://www.aanp.org/advocacy/advocacy-resource/position-statements/nurse-practitioners-in-primary-care
7. Auerbach, D. I. (2012). Will the NP workforce grow in the future? New forecasts and implications for healthcare delivery. Medical Care, 50(7), 606-610. doi: http://dx.doi.org/10.1097/MLR.0b013e318249d6e7
8. National Academy of Medicine . The National Academies Press; 2021. The future of nursing 2020-2030: Charting a path to achieve health equity.
9. Yang BK, Trinkoff AM, Zito JM, Burcu M, Safer DJ, Storr CL, Johantgen ME, & Idzik S (2017). Nurse practitioner independent practice authority and mental health service delivery in U.S. Community Health Centers. Psychiatric Services, 68(10), 1032–1038. 10.1176/appi.ps.201600495
10. Xue Y., Kannan V., Greener E., Smith J.A., Brasch J., Johnson B.A., Spetz J. Full scope-of-practice regulation is associated with higher supply of nurse practitioners in rural and primary care health professional shortage counties. Journal of Nursing Regulation. 2018;8(4):5–13. doi: 10.1016/S2155-8256(17)30176-X.
11. National Council of State Boards of Nursing The NCSBN 2022 environmental scan: Resiliency, achievement, and public protection. Journal of Nursing Regulation. 2022;12:S3–S55. doi: 10.1016/S2155-8256(22)00015-1.
Military burn pits: Their evidence and implications for respiratory health
Military service is a hazard-ridden profession. It’s easy to recognize the direct dangers from warfighting, such as gunfire and explosions, but the risks from environmental, chemical, and other occupational exposures can be harder to see.
Combustion-based waste management systems, otherwise known as “burn pits,” were used in deployed environments by the US military from the 1990s to the early 2010s. These burn pits were commonly used to eliminate plastics, electronics, munitions, metals, wood, chemicals, and even human waste. At the height of the recent conflicts in Afghanistan, Iraq, and other southwest Asia locations, more than 70% of military installations employed at least one, and nearly 4 million service members were exposed to some degree to their emissions.
Reports of burn pits being related to organic disease have garnered widespread media attention. Initially, this came through anecdotal reports of post-deployment respiratory symptoms. Over time, the conditions attributed to burn pits expanded to include newly diagnosed respiratory diseases and malignancies.
Ultimately, Congress passed the 2022 Promise to Address Comprehensive Toxins (PACT) Act, presumptively linking more than 20 diagnoses to burn pits. The PACT Act provides countless veterans access to low-cost or free medical care for their respective conditions.
What do we know about burn pits and deployment-related respiratory disease?
Data from the Millennium Cohort Study noted an approximately 40% increase in respiratory symptoms among individuals returning from deployment but no increase in the frequency of diagnosed respiratory diseases.1 This study and others definitively established a temporal relationship between deployment and respiratory symptoms. Soon after, a retrospective, observational study of service members with post-deployment respiratory symptoms found a high prevalence of constrictive bronchiolitis (CB) identified by lung biopsy.2 Patients in this group reported exposure to burn pits and a sulfur mine fire in the Mosul area while deployed. Most had normal imaging and pulmonary function testing before biopsy, confounding the clinical significance of the CB finding. The publication of this report led to increased investigation of respiratory function during and after deployment.
In a series of prospective studies that included full pulmonary function testing, impulse oscillometry, cardiopulmonary exercise testing, bronchoscopy, and, occasionally, lung biopsy to evaluate post-deployment dyspnea, only a small minority received a diagnosis of clinically significant lung disease.3,4 Additionally, when comparing spirometry and impulse oscillometry results from before and after deployment, no decline in lung function was observed in a population of service members reporting regular burn pit exposure.5 These studies suggest that at the population level, deployment does not lead to abnormalities in the structure and function of the respiratory system.
The National Academies of Sciences published two separate reviews of burn pit exposure and outcomes in 2011 and 2020.6,7 They found insufficient evidence to support a causal relationship between burn pit exposure and pulmonary disease. They highlighted studies on the composition of emissions from the area surrounding the largest military burn pit in Iraq. Levels of particulate matter, volatile organic compounds, and polycyclic aromatic hydrocarbons were elevated when compared with those of a typical American city but were similar to the pollution levels seen in the region at the time. Given these findings, they suggested ambient air pollution may have contributed more to clinically significant disease than burn pit emissions.
How do we interpret this mixed data?
At the population level, we have yet to find conclusive data directly linking burn pit exposure to the development of any respiratory disease. Does this mean that burn pits are not harmful?
Not necessarily. Research on outcomes related to burn pit exposure is challenging given the heterogeneity in exposure volume. Much of the research is retrospective and subject to recall bias. Relationships may be distorted, and the precision of reported symptoms and exposure levels is altered. Given these challenges, it’s unsurprising that evidence of causality has yet to be proven. In addition, some portion of service members has been diagnosed with respiratory disease that could be related to burn pit exposure.
What is now indisputable is that deployment to southwest Asia leads to an increase in respiratory complaints. Whether veteran respiratory symptoms are due to burn pits, ambient pollution, environmental particulate matter, or dust storms is less clinically relevant. These symptoms require attention, investigation, and management.
What does this mean for the future medical care of service members and veterans?
Many veterans with post-deployment respiratory symptoms undergo extensive evaluations without obtaining a definitive diagnosis. A recent consensus statement on deployment-related respiratory symptoms provides a framework for evaluation in such cases.8 In keeping with that statement, we recommend veterans be referred to centers with expertise in this field, such as the Department of Veterans Affairs (VA) or military health centers, when deployment-related respiratory symptoms are reported. When the evaluation does not lead to a treatable diagnosis, these centers can provide multidisciplinary care to address the symptoms of dyspnea, cough, fatigue, and exercise intolerance to improve functional status.
Despite uncertainty in the evidence or challenges in diagnosis, both the Department of Defense (DoD) and VA remain fully committed to addressing the health concerns of service members and veterans. Notably, the VA has already screened more than 5 million veterans for toxic military exposures in accordance with the PACT Act and is providing ongoing screening and care for veterans with post-deployment respiratory symptoms. Furthermore, the DoD and VA have dedicated large portions of their research budgets to investigating the impacts of exposures during military service and optimizing the care of those with respiratory symptoms. With these commitments to patient care and research, our veterans’ respiratory health can now be optimized, and future risks can be mitigated.
Dr. Haynes is Fellow, Pulmonary and Critical Care Medicine, Walter Reed National Military Medical Center, Assistant Professor of Medicine, Uniformed Services University. Dr. Nations is Pulmonary and Critical Care Medicine, Deputy Chief of Staff for Operations, Washington DC VA Medical Center, Associate Professor of Medicine, Uniformed Services University.
References
1. Smith B, Wong CA, Smith TC, Boyko EJ, Gackstetter GD; Margaret A. K. Ryan for the Millennium Cohort Study Team. Newly reported respiratory symptoms and conditions among military personnel deployed to Iraq and Afghanistan: a prospective population-based study. Am J Epidemiol. 2009;170(11):1433-1442. Preprint. Posted online October 22, 2009. PMID: 19850627. doi: 10.1093/aje/kwp287
2. King MS, Eisenberg R, Newman JH, et al. Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan. N Engl J Med. 2011;365(3):222-230. Erratum in: N Engl J Med. 2011;365(18):1749. PMID: 21774710; PMCID: PMC3296566. doi: 10.1056/NEJMoa1101388
3. Morris MJ, Dodson DW, Lucero PF, et al. Study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE). Am J Respir Crit Care Med. 2014;190(1):77-84. PMID: 24922562. doi: 10.1164/rccm.201402-0372OC
4. Morris MJ, Walter RJ, McCann ET, et al. Clinical evaluation of deployed military personnel with chronic respiratory symptoms: study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE) III. Chest. 2020;157(6):1559-1567. Preprint. Posted online February 1, 2020. PMID: 32017933. doi: 10.1016/j.chest.2020.01.024
5. Morris MJ, Skabelund AJ, Rawlins FA 3rd, Gallup RA, Aden JK, Holley AB. Study of active duty military personnel for environmental deployment exposures: pre- and post-deployment spirometry (STAMPEDE II). Respir Care. 2019;64(5):536-544. Preprint. Posted online January 8, 2019.PMID: 30622173. doi: 10.4187/respcare.06396
6. Institute of Medicine. Long-Term Health Consequences of Exposure to Burn Pits in Iraq and Afghanistan. The National Academies Press; 2011. https://doi.org/10.17226/13209
7. National Academies of Sciences, Engineering, and Medicine. Respiratory Health Effects of Airborne Hazards Exposures in the Southwest Asia Theater of Military Operations. The National Academies Press; 2020. https://doi.org/10.17226/25837
8. Falvo MJ, Sotolongo AM, Osterholzer JJ, et al. Consensus statements on deployment-related respiratory disease, inclusive of constrictive bronchiolitis: a modified Delphi study. Chest. 2023;163(3):599-609. Preprint. Posted November 4, 2022. PMID: 36343686; PMCID: PMC10154857. doi: 10.1016/j.chest.2022.10.031
Military service is a hazard-ridden profession. It’s easy to recognize the direct dangers from warfighting, such as gunfire and explosions, but the risks from environmental, chemical, and other occupational exposures can be harder to see.
Combustion-based waste management systems, otherwise known as “burn pits,” were used in deployed environments by the US military from the 1990s to the early 2010s. These burn pits were commonly used to eliminate plastics, electronics, munitions, metals, wood, chemicals, and even human waste. At the height of the recent conflicts in Afghanistan, Iraq, and other southwest Asia locations, more than 70% of military installations employed at least one, and nearly 4 million service members were exposed to some degree to their emissions.
Reports of burn pits being related to organic disease have garnered widespread media attention. Initially, this came through anecdotal reports of post-deployment respiratory symptoms. Over time, the conditions attributed to burn pits expanded to include newly diagnosed respiratory diseases and malignancies.
Ultimately, Congress passed the 2022 Promise to Address Comprehensive Toxins (PACT) Act, presumptively linking more than 20 diagnoses to burn pits. The PACT Act provides countless veterans access to low-cost or free medical care for their respective conditions.
What do we know about burn pits and deployment-related respiratory disease?
Data from the Millennium Cohort Study noted an approximately 40% increase in respiratory symptoms among individuals returning from deployment but no increase in the frequency of diagnosed respiratory diseases.1 This study and others definitively established a temporal relationship between deployment and respiratory symptoms. Soon after, a retrospective, observational study of service members with post-deployment respiratory symptoms found a high prevalence of constrictive bronchiolitis (CB) identified by lung biopsy.2 Patients in this group reported exposure to burn pits and a sulfur mine fire in the Mosul area while deployed. Most had normal imaging and pulmonary function testing before biopsy, confounding the clinical significance of the CB finding. The publication of this report led to increased investigation of respiratory function during and after deployment.
In a series of prospective studies that included full pulmonary function testing, impulse oscillometry, cardiopulmonary exercise testing, bronchoscopy, and, occasionally, lung biopsy to evaluate post-deployment dyspnea, only a small minority received a diagnosis of clinically significant lung disease.3,4 Additionally, when comparing spirometry and impulse oscillometry results from before and after deployment, no decline in lung function was observed in a population of service members reporting regular burn pit exposure.5 These studies suggest that at the population level, deployment does not lead to abnormalities in the structure and function of the respiratory system.
The National Academies of Sciences published two separate reviews of burn pit exposure and outcomes in 2011 and 2020.6,7 They found insufficient evidence to support a causal relationship between burn pit exposure and pulmonary disease. They highlighted studies on the composition of emissions from the area surrounding the largest military burn pit in Iraq. Levels of particulate matter, volatile organic compounds, and polycyclic aromatic hydrocarbons were elevated when compared with those of a typical American city but were similar to the pollution levels seen in the region at the time. Given these findings, they suggested ambient air pollution may have contributed more to clinically significant disease than burn pit emissions.
How do we interpret this mixed data?
At the population level, we have yet to find conclusive data directly linking burn pit exposure to the development of any respiratory disease. Does this mean that burn pits are not harmful?
Not necessarily. Research on outcomes related to burn pit exposure is challenging given the heterogeneity in exposure volume. Much of the research is retrospective and subject to recall bias. Relationships may be distorted, and the precision of reported symptoms and exposure levels is altered. Given these challenges, it’s unsurprising that evidence of causality has yet to be proven. In addition, some portion of service members has been diagnosed with respiratory disease that could be related to burn pit exposure.
What is now indisputable is that deployment to southwest Asia leads to an increase in respiratory complaints. Whether veteran respiratory symptoms are due to burn pits, ambient pollution, environmental particulate matter, or dust storms is less clinically relevant. These symptoms require attention, investigation, and management.
What does this mean for the future medical care of service members and veterans?
Many veterans with post-deployment respiratory symptoms undergo extensive evaluations without obtaining a definitive diagnosis. A recent consensus statement on deployment-related respiratory symptoms provides a framework for evaluation in such cases.8 In keeping with that statement, we recommend veterans be referred to centers with expertise in this field, such as the Department of Veterans Affairs (VA) or military health centers, when deployment-related respiratory symptoms are reported. When the evaluation does not lead to a treatable diagnosis, these centers can provide multidisciplinary care to address the symptoms of dyspnea, cough, fatigue, and exercise intolerance to improve functional status.
Despite uncertainty in the evidence or challenges in diagnosis, both the Department of Defense (DoD) and VA remain fully committed to addressing the health concerns of service members and veterans. Notably, the VA has already screened more than 5 million veterans for toxic military exposures in accordance with the PACT Act and is providing ongoing screening and care for veterans with post-deployment respiratory symptoms. Furthermore, the DoD and VA have dedicated large portions of their research budgets to investigating the impacts of exposures during military service and optimizing the care of those with respiratory symptoms. With these commitments to patient care and research, our veterans’ respiratory health can now be optimized, and future risks can be mitigated.
Dr. Haynes is Fellow, Pulmonary and Critical Care Medicine, Walter Reed National Military Medical Center, Assistant Professor of Medicine, Uniformed Services University. Dr. Nations is Pulmonary and Critical Care Medicine, Deputy Chief of Staff for Operations, Washington DC VA Medical Center, Associate Professor of Medicine, Uniformed Services University.
References
1. Smith B, Wong CA, Smith TC, Boyko EJ, Gackstetter GD; Margaret A. K. Ryan for the Millennium Cohort Study Team. Newly reported respiratory symptoms and conditions among military personnel deployed to Iraq and Afghanistan: a prospective population-based study. Am J Epidemiol. 2009;170(11):1433-1442. Preprint. Posted online October 22, 2009. PMID: 19850627. doi: 10.1093/aje/kwp287
2. King MS, Eisenberg R, Newman JH, et al. Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan. N Engl J Med. 2011;365(3):222-230. Erratum in: N Engl J Med. 2011;365(18):1749. PMID: 21774710; PMCID: PMC3296566. doi: 10.1056/NEJMoa1101388
3. Morris MJ, Dodson DW, Lucero PF, et al. Study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE). Am J Respir Crit Care Med. 2014;190(1):77-84. PMID: 24922562. doi: 10.1164/rccm.201402-0372OC
4. Morris MJ, Walter RJ, McCann ET, et al. Clinical evaluation of deployed military personnel with chronic respiratory symptoms: study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE) III. Chest. 2020;157(6):1559-1567. Preprint. Posted online February 1, 2020. PMID: 32017933. doi: 10.1016/j.chest.2020.01.024
5. Morris MJ, Skabelund AJ, Rawlins FA 3rd, Gallup RA, Aden JK, Holley AB. Study of active duty military personnel for environmental deployment exposures: pre- and post-deployment spirometry (STAMPEDE II). Respir Care. 2019;64(5):536-544. Preprint. Posted online January 8, 2019.PMID: 30622173. doi: 10.4187/respcare.06396
6. Institute of Medicine. Long-Term Health Consequences of Exposure to Burn Pits in Iraq and Afghanistan. The National Academies Press; 2011. https://doi.org/10.17226/13209
7. National Academies of Sciences, Engineering, and Medicine. Respiratory Health Effects of Airborne Hazards Exposures in the Southwest Asia Theater of Military Operations. The National Academies Press; 2020. https://doi.org/10.17226/25837
8. Falvo MJ, Sotolongo AM, Osterholzer JJ, et al. Consensus statements on deployment-related respiratory disease, inclusive of constrictive bronchiolitis: a modified Delphi study. Chest. 2023;163(3):599-609. Preprint. Posted November 4, 2022. PMID: 36343686; PMCID: PMC10154857. doi: 10.1016/j.chest.2022.10.031
Military service is a hazard-ridden profession. It’s easy to recognize the direct dangers from warfighting, such as gunfire and explosions, but the risks from environmental, chemical, and other occupational exposures can be harder to see.
Combustion-based waste management systems, otherwise known as “burn pits,” were used in deployed environments by the US military from the 1990s to the early 2010s. These burn pits were commonly used to eliminate plastics, electronics, munitions, metals, wood, chemicals, and even human waste. At the height of the recent conflicts in Afghanistan, Iraq, and other southwest Asia locations, more than 70% of military installations employed at least one, and nearly 4 million service members were exposed to some degree to their emissions.
Reports of burn pits being related to organic disease have garnered widespread media attention. Initially, this came through anecdotal reports of post-deployment respiratory symptoms. Over time, the conditions attributed to burn pits expanded to include newly diagnosed respiratory diseases and malignancies.
Ultimately, Congress passed the 2022 Promise to Address Comprehensive Toxins (PACT) Act, presumptively linking more than 20 diagnoses to burn pits. The PACT Act provides countless veterans access to low-cost or free medical care for their respective conditions.
What do we know about burn pits and deployment-related respiratory disease?
Data from the Millennium Cohort Study noted an approximately 40% increase in respiratory symptoms among individuals returning from deployment but no increase in the frequency of diagnosed respiratory diseases.1 This study and others definitively established a temporal relationship between deployment and respiratory symptoms. Soon after, a retrospective, observational study of service members with post-deployment respiratory symptoms found a high prevalence of constrictive bronchiolitis (CB) identified by lung biopsy.2 Patients in this group reported exposure to burn pits and a sulfur mine fire in the Mosul area while deployed. Most had normal imaging and pulmonary function testing before biopsy, confounding the clinical significance of the CB finding. The publication of this report led to increased investigation of respiratory function during and after deployment.
In a series of prospective studies that included full pulmonary function testing, impulse oscillometry, cardiopulmonary exercise testing, bronchoscopy, and, occasionally, lung biopsy to evaluate post-deployment dyspnea, only a small minority received a diagnosis of clinically significant lung disease.3,4 Additionally, when comparing spirometry and impulse oscillometry results from before and after deployment, no decline in lung function was observed in a population of service members reporting regular burn pit exposure.5 These studies suggest that at the population level, deployment does not lead to abnormalities in the structure and function of the respiratory system.
The National Academies of Sciences published two separate reviews of burn pit exposure and outcomes in 2011 and 2020.6,7 They found insufficient evidence to support a causal relationship between burn pit exposure and pulmonary disease. They highlighted studies on the composition of emissions from the area surrounding the largest military burn pit in Iraq. Levels of particulate matter, volatile organic compounds, and polycyclic aromatic hydrocarbons were elevated when compared with those of a typical American city but were similar to the pollution levels seen in the region at the time. Given these findings, they suggested ambient air pollution may have contributed more to clinically significant disease than burn pit emissions.
How do we interpret this mixed data?
At the population level, we have yet to find conclusive data directly linking burn pit exposure to the development of any respiratory disease. Does this mean that burn pits are not harmful?
Not necessarily. Research on outcomes related to burn pit exposure is challenging given the heterogeneity in exposure volume. Much of the research is retrospective and subject to recall bias. Relationships may be distorted, and the precision of reported symptoms and exposure levels is altered. Given these challenges, it’s unsurprising that evidence of causality has yet to be proven. In addition, some portion of service members has been diagnosed with respiratory disease that could be related to burn pit exposure.
What is now indisputable is that deployment to southwest Asia leads to an increase in respiratory complaints. Whether veteran respiratory symptoms are due to burn pits, ambient pollution, environmental particulate matter, or dust storms is less clinically relevant. These symptoms require attention, investigation, and management.
What does this mean for the future medical care of service members and veterans?
Many veterans with post-deployment respiratory symptoms undergo extensive evaluations without obtaining a definitive diagnosis. A recent consensus statement on deployment-related respiratory symptoms provides a framework for evaluation in such cases.8 In keeping with that statement, we recommend veterans be referred to centers with expertise in this field, such as the Department of Veterans Affairs (VA) or military health centers, when deployment-related respiratory symptoms are reported. When the evaluation does not lead to a treatable diagnosis, these centers can provide multidisciplinary care to address the symptoms of dyspnea, cough, fatigue, and exercise intolerance to improve functional status.
Despite uncertainty in the evidence or challenges in diagnosis, both the Department of Defense (DoD) and VA remain fully committed to addressing the health concerns of service members and veterans. Notably, the VA has already screened more than 5 million veterans for toxic military exposures in accordance with the PACT Act and is providing ongoing screening and care for veterans with post-deployment respiratory symptoms. Furthermore, the DoD and VA have dedicated large portions of their research budgets to investigating the impacts of exposures during military service and optimizing the care of those with respiratory symptoms. With these commitments to patient care and research, our veterans’ respiratory health can now be optimized, and future risks can be mitigated.
Dr. Haynes is Fellow, Pulmonary and Critical Care Medicine, Walter Reed National Military Medical Center, Assistant Professor of Medicine, Uniformed Services University. Dr. Nations is Pulmonary and Critical Care Medicine, Deputy Chief of Staff for Operations, Washington DC VA Medical Center, Associate Professor of Medicine, Uniformed Services University.
References
1. Smith B, Wong CA, Smith TC, Boyko EJ, Gackstetter GD; Margaret A. K. Ryan for the Millennium Cohort Study Team. Newly reported respiratory symptoms and conditions among military personnel deployed to Iraq and Afghanistan: a prospective population-based study. Am J Epidemiol. 2009;170(11):1433-1442. Preprint. Posted online October 22, 2009. PMID: 19850627. doi: 10.1093/aje/kwp287
2. King MS, Eisenberg R, Newman JH, et al. Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan. N Engl J Med. 2011;365(3):222-230. Erratum in: N Engl J Med. 2011;365(18):1749. PMID: 21774710; PMCID: PMC3296566. doi: 10.1056/NEJMoa1101388
3. Morris MJ, Dodson DW, Lucero PF, et al. Study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE). Am J Respir Crit Care Med. 2014;190(1):77-84. PMID: 24922562. doi: 10.1164/rccm.201402-0372OC
4. Morris MJ, Walter RJ, McCann ET, et al. Clinical evaluation of deployed military personnel with chronic respiratory symptoms: study of active duty military for pulmonary disease related to environmental deployment exposures (STAMPEDE) III. Chest. 2020;157(6):1559-1567. Preprint. Posted online February 1, 2020. PMID: 32017933. doi: 10.1016/j.chest.2020.01.024
5. Morris MJ, Skabelund AJ, Rawlins FA 3rd, Gallup RA, Aden JK, Holley AB. Study of active duty military personnel for environmental deployment exposures: pre- and post-deployment spirometry (STAMPEDE II). Respir Care. 2019;64(5):536-544. Preprint. Posted online January 8, 2019.PMID: 30622173. doi: 10.4187/respcare.06396
6. Institute of Medicine. Long-Term Health Consequences of Exposure to Burn Pits in Iraq and Afghanistan. The National Academies Press; 2011. https://doi.org/10.17226/13209
7. National Academies of Sciences, Engineering, and Medicine. Respiratory Health Effects of Airborne Hazards Exposures in the Southwest Asia Theater of Military Operations. The National Academies Press; 2020. https://doi.org/10.17226/25837
8. Falvo MJ, Sotolongo AM, Osterholzer JJ, et al. Consensus statements on deployment-related respiratory disease, inclusive of constrictive bronchiolitis: a modified Delphi study. Chest. 2023;163(3):599-609. Preprint. Posted November 4, 2022. PMID: 36343686; PMCID: PMC10154857. doi: 10.1016/j.chest.2022.10.031