User login
Amantadine Hydrochloride Reduces Levodopa-Induced Dyskinesia in Patients With Parkinson’s Disease
PORTLAND, OR—Amantadine hydrochloride extended-release capsules, compared with placebo, result in a statistically significant and clinically meaningful improvement in levodopa-induced dyskinesia in patients with Parkinson’s disease, according to phase III trial results presented at the Fourth World Parkinson Congress. The drug also reduces daily off time and is generally well tolerated, researchers said.
Amantadine hydrochloride extended-release capsules, known as ADS-5102, are being developed by Adamas Pharmaceuticals with the aim of improving the pharmacokinetic profile of immediate-release amantadine.
Rajesh Pahwa, MD, Professor of Neurology at University of Kansas Medical Center in Kansas City, and colleagues reported efficacy and safety results from the EASE LID 3 trial, one of three phase III trials of the drug.
EASE LID 3 was a randomized, double-blind, placebo-controlled study conducted at 39 sites in the United States and Europe. Seventy-seven patients with Parkinson’s disease were randomized to receive 340 mg of amantadine hydrochloride or placebo once daily at bedtime for the treatment of levodopa-induced dyskinesia. Participants had an average age of 64.8, 52% were men, and they had been diagnosed with Parkinson’s disease for an average of 10.6 years. They had received levodopa treatment for an average of 8.1 years. Patients’ mean duration of levodopa-induced dyskinesia was 3.9 years.
Treatment Improved Outcomes
The primary efficacy analysis compared the least square mean change from baseline to week 12 in Unified Dyskinesia Rating Scale total score in the ADS-5102 group with that in the placebo group. Key secondary efficacy analyses compared the least square mean change from baseline to week 12 in on time without troublesome dyskinesia and off time, as recorded in participants’ home diaries.
Thirty-eight patients were randomized to receive ADS-5102 and 39 patients were randomized to receive placebo. In the ADS-5102 group, the observed mean Unified Dyskinesia Rating Scale total score from baseline to week 12 decreased by 46%, compared with a 16% reduction in the placebo group. At 12 weeks, daily on time without troublesome dyskinesia increased by 4.0 hours in the ADS-5102 group and by 2.1 hours in the placebo group. Daily off time decreased by 0.5 hours in the ADS-5102 group and increased by 0.6 hours in the placebo group.
Adverse Events
Four patients, all in the ADS-5102 group, experienced serious adverse events. In one patient, the serious adverse event was considered related to the study drug (ie, constipation and urinary retention). The patient completed study treatment and did not discontinue participation in the trial.
Seven patients in the ADS-5102 group (19%) versus three patients in the placebo group (8%) discontinued treatment due to adverse events. In the ADS-5102 group, the most frequent adverse events (ie, they occurred in more than two patients) were dry mouth, nausea, decreased appetite, insomnia, orthostatic hypotension, constipation, fall, and hallucination.
“ADS-5102 resulted in statistically significant and clinically meaningful improvement in levodopa-induced dyskinesia, confirming results from earlier controlled clinical trials,” the researchers concluded.
Investigators are conducting an open-label safety study of ADS-5102 that includes patients from the phase III trials as well as patients with levodopa-induced dyskinesia who have undergone deep brain stimulation. Adamas also is investigating ADS-5102 for use in patients with multiple sclerosis with walking impairment.
—Jake Remaly
PORTLAND, OR—Amantadine hydrochloride extended-release capsules, compared with placebo, result in a statistically significant and clinically meaningful improvement in levodopa-induced dyskinesia in patients with Parkinson’s disease, according to phase III trial results presented at the Fourth World Parkinson Congress. The drug also reduces daily off time and is generally well tolerated, researchers said.
Amantadine hydrochloride extended-release capsules, known as ADS-5102, are being developed by Adamas Pharmaceuticals with the aim of improving the pharmacokinetic profile of immediate-release amantadine.
Rajesh Pahwa, MD, Professor of Neurology at University of Kansas Medical Center in Kansas City, and colleagues reported efficacy and safety results from the EASE LID 3 trial, one of three phase III trials of the drug.
EASE LID 3 was a randomized, double-blind, placebo-controlled study conducted at 39 sites in the United States and Europe. Seventy-seven patients with Parkinson’s disease were randomized to receive 340 mg of amantadine hydrochloride or placebo once daily at bedtime for the treatment of levodopa-induced dyskinesia. Participants had an average age of 64.8, 52% were men, and they had been diagnosed with Parkinson’s disease for an average of 10.6 years. They had received levodopa treatment for an average of 8.1 years. Patients’ mean duration of levodopa-induced dyskinesia was 3.9 years.
Treatment Improved Outcomes
The primary efficacy analysis compared the least square mean change from baseline to week 12 in Unified Dyskinesia Rating Scale total score in the ADS-5102 group with that in the placebo group. Key secondary efficacy analyses compared the least square mean change from baseline to week 12 in on time without troublesome dyskinesia and off time, as recorded in participants’ home diaries.
Thirty-eight patients were randomized to receive ADS-5102 and 39 patients were randomized to receive placebo. In the ADS-5102 group, the observed mean Unified Dyskinesia Rating Scale total score from baseline to week 12 decreased by 46%, compared with a 16% reduction in the placebo group. At 12 weeks, daily on time without troublesome dyskinesia increased by 4.0 hours in the ADS-5102 group and by 2.1 hours in the placebo group. Daily off time decreased by 0.5 hours in the ADS-5102 group and increased by 0.6 hours in the placebo group.
Adverse Events
Four patients, all in the ADS-5102 group, experienced serious adverse events. In one patient, the serious adverse event was considered related to the study drug (ie, constipation and urinary retention). The patient completed study treatment and did not discontinue participation in the trial.
Seven patients in the ADS-5102 group (19%) versus three patients in the placebo group (8%) discontinued treatment due to adverse events. In the ADS-5102 group, the most frequent adverse events (ie, they occurred in more than two patients) were dry mouth, nausea, decreased appetite, insomnia, orthostatic hypotension, constipation, fall, and hallucination.
“ADS-5102 resulted in statistically significant and clinically meaningful improvement in levodopa-induced dyskinesia, confirming results from earlier controlled clinical trials,” the researchers concluded.
Investigators are conducting an open-label safety study of ADS-5102 that includes patients from the phase III trials as well as patients with levodopa-induced dyskinesia who have undergone deep brain stimulation. Adamas also is investigating ADS-5102 for use in patients with multiple sclerosis with walking impairment.
—Jake Remaly
PORTLAND, OR—Amantadine hydrochloride extended-release capsules, compared with placebo, result in a statistically significant and clinically meaningful improvement in levodopa-induced dyskinesia in patients with Parkinson’s disease, according to phase III trial results presented at the Fourth World Parkinson Congress. The drug also reduces daily off time and is generally well tolerated, researchers said.
Amantadine hydrochloride extended-release capsules, known as ADS-5102, are being developed by Adamas Pharmaceuticals with the aim of improving the pharmacokinetic profile of immediate-release amantadine.
Rajesh Pahwa, MD, Professor of Neurology at University of Kansas Medical Center in Kansas City, and colleagues reported efficacy and safety results from the EASE LID 3 trial, one of three phase III trials of the drug.
EASE LID 3 was a randomized, double-blind, placebo-controlled study conducted at 39 sites in the United States and Europe. Seventy-seven patients with Parkinson’s disease were randomized to receive 340 mg of amantadine hydrochloride or placebo once daily at bedtime for the treatment of levodopa-induced dyskinesia. Participants had an average age of 64.8, 52% were men, and they had been diagnosed with Parkinson’s disease for an average of 10.6 years. They had received levodopa treatment for an average of 8.1 years. Patients’ mean duration of levodopa-induced dyskinesia was 3.9 years.
Treatment Improved Outcomes
The primary efficacy analysis compared the least square mean change from baseline to week 12 in Unified Dyskinesia Rating Scale total score in the ADS-5102 group with that in the placebo group. Key secondary efficacy analyses compared the least square mean change from baseline to week 12 in on time without troublesome dyskinesia and off time, as recorded in participants’ home diaries.
Thirty-eight patients were randomized to receive ADS-5102 and 39 patients were randomized to receive placebo. In the ADS-5102 group, the observed mean Unified Dyskinesia Rating Scale total score from baseline to week 12 decreased by 46%, compared with a 16% reduction in the placebo group. At 12 weeks, daily on time without troublesome dyskinesia increased by 4.0 hours in the ADS-5102 group and by 2.1 hours in the placebo group. Daily off time decreased by 0.5 hours in the ADS-5102 group and increased by 0.6 hours in the placebo group.
Adverse Events
Four patients, all in the ADS-5102 group, experienced serious adverse events. In one patient, the serious adverse event was considered related to the study drug (ie, constipation and urinary retention). The patient completed study treatment and did not discontinue participation in the trial.
Seven patients in the ADS-5102 group (19%) versus three patients in the placebo group (8%) discontinued treatment due to adverse events. In the ADS-5102 group, the most frequent adverse events (ie, they occurred in more than two patients) were dry mouth, nausea, decreased appetite, insomnia, orthostatic hypotension, constipation, fall, and hallucination.
“ADS-5102 resulted in statistically significant and clinically meaningful improvement in levodopa-induced dyskinesia, confirming results from earlier controlled clinical trials,” the researchers concluded.
Investigators are conducting an open-label safety study of ADS-5102 that includes patients from the phase III trials as well as patients with levodopa-induced dyskinesia who have undergone deep brain stimulation. Adamas also is investigating ADS-5102 for use in patients with multiple sclerosis with walking impairment.
—Jake Remaly
High-Intensity Exercise May Be Feasible in Patients With Parkinson’s Disease
PORTLAND, OR—High-intensity exercise is feasible and safe in patients with Parkinson's disease, according to trial results presented at the Fourth World Parkinson Congress. An eight-week high-intensity exercise and fall-prevention boot camp was well attended, and participants tolerated high-intensity aerobic, strength, and balance training exercises, researchers said.
Most contemporary exercise programs for people with Parkinson's disease are low to moderate in intensity. Recent studies, however, suggest that older adults can safely tolerate high-intensity exercise programs and attain more meaningful benefits. "The optimal parameters of exercise for Parkinson's disease have not been thoroughly explored," said Merrill R. Landers, PT, DPT, PhD, OCS, Professor of Physical Therapy, and James Navalta, PhD, Associate Professor of Kinesiology, both at the University of Nevada in Las Vegas.
To test the feasibility and safety of a high-intensity exercise and fall-prevention boot camp in people with Parkinson's disease, Drs. Landers and Navalta conducted a phase II, pragmatic, randomized clinical trial.
Twenty-seven participants were included in the study. Fourteen patients were randomized to the high-intensity exercise program, and 13 patients were randomized to a low-intensity control program (ie, Fitness Counts Exercise Program). Physiotherapists supervised the exercise programs at community exercise gyms.
Patients had an average age of about 64 and disease duration of nearly five years. Nineteen men and eight women enrolled in the study. Most patients were Hoehn and Yahr stage 2.
The high-intensity boot camp sessions consisted of 30 minutes of aerobic exercise (70% of heart rate maximum), 30 minutes of strengthening (50% to 80% of one-repetition maximum), 15 minutes of balance training, and 15 minutes of active rest and stretching. The control sessions consisted of 15 minutes of aerobic exercise (60% of heart rate maximum), 15 minutes of strengthening (less than 50% of one-repetition maximum), 10 minutes of balance training, 10 minutes of rest, and 10 minutes of stretching. There was not a significant difference in the rate of injuries, falls, or exercise side effects between groups. Adverse events were similar in the two arms. Compared with low-intensity exercise, high-intensity exercise produced greater improvements in balance, physical activity, parkinsonian symptoms, endurance, fatigue, and bone health.
"These results warrant further investigation in a large-scale comparative effectiveness trial," the researchers concluded.
—Jake Remaly
PORTLAND, OR—High-intensity exercise is feasible and safe in patients with Parkinson's disease, according to trial results presented at the Fourth World Parkinson Congress. An eight-week high-intensity exercise and fall-prevention boot camp was well attended, and participants tolerated high-intensity aerobic, strength, and balance training exercises, researchers said.
Most contemporary exercise programs for people with Parkinson's disease are low to moderate in intensity. Recent studies, however, suggest that older adults can safely tolerate high-intensity exercise programs and attain more meaningful benefits. "The optimal parameters of exercise for Parkinson's disease have not been thoroughly explored," said Merrill R. Landers, PT, DPT, PhD, OCS, Professor of Physical Therapy, and James Navalta, PhD, Associate Professor of Kinesiology, both at the University of Nevada in Las Vegas.
To test the feasibility and safety of a high-intensity exercise and fall-prevention boot camp in people with Parkinson's disease, Drs. Landers and Navalta conducted a phase II, pragmatic, randomized clinical trial.
Twenty-seven participants were included in the study. Fourteen patients were randomized to the high-intensity exercise program, and 13 patients were randomized to a low-intensity control program (ie, Fitness Counts Exercise Program). Physiotherapists supervised the exercise programs at community exercise gyms.
Patients had an average age of about 64 and disease duration of nearly five years. Nineteen men and eight women enrolled in the study. Most patients were Hoehn and Yahr stage 2.
The high-intensity boot camp sessions consisted of 30 minutes of aerobic exercise (70% of heart rate maximum), 30 minutes of strengthening (50% to 80% of one-repetition maximum), 15 minutes of balance training, and 15 minutes of active rest and stretching. The control sessions consisted of 15 minutes of aerobic exercise (60% of heart rate maximum), 15 minutes of strengthening (less than 50% of one-repetition maximum), 10 minutes of balance training, 10 minutes of rest, and 10 minutes of stretching. There was not a significant difference in the rate of injuries, falls, or exercise side effects between groups. Adverse events were similar in the two arms. Compared with low-intensity exercise, high-intensity exercise produced greater improvements in balance, physical activity, parkinsonian symptoms, endurance, fatigue, and bone health.
"These results warrant further investigation in a large-scale comparative effectiveness trial," the researchers concluded.
—Jake Remaly
PORTLAND, OR—High-intensity exercise is feasible and safe in patients with Parkinson's disease, according to trial results presented at the Fourth World Parkinson Congress. An eight-week high-intensity exercise and fall-prevention boot camp was well attended, and participants tolerated high-intensity aerobic, strength, and balance training exercises, researchers said.
Most contemporary exercise programs for people with Parkinson's disease are low to moderate in intensity. Recent studies, however, suggest that older adults can safely tolerate high-intensity exercise programs and attain more meaningful benefits. "The optimal parameters of exercise for Parkinson's disease have not been thoroughly explored," said Merrill R. Landers, PT, DPT, PhD, OCS, Professor of Physical Therapy, and James Navalta, PhD, Associate Professor of Kinesiology, both at the University of Nevada in Las Vegas.
To test the feasibility and safety of a high-intensity exercise and fall-prevention boot camp in people with Parkinson's disease, Drs. Landers and Navalta conducted a phase II, pragmatic, randomized clinical trial.
Twenty-seven participants were included in the study. Fourteen patients were randomized to the high-intensity exercise program, and 13 patients were randomized to a low-intensity control program (ie, Fitness Counts Exercise Program). Physiotherapists supervised the exercise programs at community exercise gyms.
Patients had an average age of about 64 and disease duration of nearly five years. Nineteen men and eight women enrolled in the study. Most patients were Hoehn and Yahr stage 2.
The high-intensity boot camp sessions consisted of 30 minutes of aerobic exercise (70% of heart rate maximum), 30 minutes of strengthening (50% to 80% of one-repetition maximum), 15 minutes of balance training, and 15 minutes of active rest and stretching. The control sessions consisted of 15 minutes of aerobic exercise (60% of heart rate maximum), 15 minutes of strengthening (less than 50% of one-repetition maximum), 10 minutes of balance training, 10 minutes of rest, and 10 minutes of stretching. There was not a significant difference in the rate of injuries, falls, or exercise side effects between groups. Adverse events were similar in the two arms. Compared with low-intensity exercise, high-intensity exercise produced greater improvements in balance, physical activity, parkinsonian symptoms, endurance, fatigue, and bone health.
"These results warrant further investigation in a large-scale comparative effectiveness trial," the researchers concluded.
—Jake Remaly
How Do Autonomic Symptoms Affect Patients With Early Parkinson’s Disease?
PORTLAND, OR—Autonomic symptoms are present in a majority of patients with early Parkinson's disease, and symptoms correlate with markers of disease severity and impaired quality of life, according to research presented at the Fourth World Parkinson Congress.
Although autonomic dysfunction is common in the later stages of Parkinson's disease, less is known about autonomic symptom presence and severity in early stages of Parkinson's disease. Naveed Malek, MD, Department of Neurology, Institute of Neurological Sciences, Queen Elizabeth University Hospital, in Glasgow, and colleagues conducted a study to explore the prevalence, range, and severity of autonomic symptoms in a cohort of patients who had been diagnosed with Parkinson's disease in the preceding 3.5 years.
The researchers analyzed detailed patient-reported symptoms of autonomic dysfunction that were assessed in the multicenter United Kingdom Tracking Parkinson's study using the Scale for Outcomes in Parkinson's Disease for Autonomic Symptoms (SCOPA-AUT).
The researchers assessed the relationship between baseline SCOPA-AUT score and baseline motor, nonmotor, and quality of life scores. The researchers adjusted for sex, age, and disease duration differences across groups.
A total of 1,738 patients (65.1% male, mean age 67.6) were included in the main analysis. Patients had a mean disease duration of 1.3 years and mean Movement Disorder Society Unified Parkinson's Disease Rating Scale motor score of 22.5. Hoehn and Yahr was stage 1 or 1.5 in 855 cases (49.2%), stage 2 or 2.5 in 783 cases (45.1%), and stage 3 or higher in 100 cases (5.8%).
Autonomic severity by SCOPA-AUT score increased significantly across the motor severity stages, from 10.7 for Hoehn and Yahr stages 1 and 1.5, to 12.7 for Hoehn and Yahr stages 2 and 2.5, and to 13.5 for Hoehn and Yahr stages 3 and higher. Urinary, bowel, and sexual dysfunctions were the most commonly reported autonomic symptoms. The results were between those previously reported in controls and in patients with Parkinson's disease at a mean duration of 10 years. Positive associations were present between autonomic severity and depression, sleep disturbance, and postural instability motor subtype.
"Our study highlights the extent to which we may expect to see autonomic features in early Parkinson's disease, and the relationship between autonomic features and diagnostic consideration, which is important in the balanced diagnostic judgment approach emphasized in recent consensus guidelines," Dr. Malek concluded.
—Jake Remaly
PORTLAND, OR—Autonomic symptoms are present in a majority of patients with early Parkinson's disease, and symptoms correlate with markers of disease severity and impaired quality of life, according to research presented at the Fourth World Parkinson Congress.
Although autonomic dysfunction is common in the later stages of Parkinson's disease, less is known about autonomic symptom presence and severity in early stages of Parkinson's disease. Naveed Malek, MD, Department of Neurology, Institute of Neurological Sciences, Queen Elizabeth University Hospital, in Glasgow, and colleagues conducted a study to explore the prevalence, range, and severity of autonomic symptoms in a cohort of patients who had been diagnosed with Parkinson's disease in the preceding 3.5 years.
The researchers analyzed detailed patient-reported symptoms of autonomic dysfunction that were assessed in the multicenter United Kingdom Tracking Parkinson's study using the Scale for Outcomes in Parkinson's Disease for Autonomic Symptoms (SCOPA-AUT).
The researchers assessed the relationship between baseline SCOPA-AUT score and baseline motor, nonmotor, and quality of life scores. The researchers adjusted for sex, age, and disease duration differences across groups.
A total of 1,738 patients (65.1% male, mean age 67.6) were included in the main analysis. Patients had a mean disease duration of 1.3 years and mean Movement Disorder Society Unified Parkinson's Disease Rating Scale motor score of 22.5. Hoehn and Yahr was stage 1 or 1.5 in 855 cases (49.2%), stage 2 or 2.5 in 783 cases (45.1%), and stage 3 or higher in 100 cases (5.8%).
Autonomic severity by SCOPA-AUT score increased significantly across the motor severity stages, from 10.7 for Hoehn and Yahr stages 1 and 1.5, to 12.7 for Hoehn and Yahr stages 2 and 2.5, and to 13.5 for Hoehn and Yahr stages 3 and higher. Urinary, bowel, and sexual dysfunctions were the most commonly reported autonomic symptoms. The results were between those previously reported in controls and in patients with Parkinson's disease at a mean duration of 10 years. Positive associations were present between autonomic severity and depression, sleep disturbance, and postural instability motor subtype.
"Our study highlights the extent to which we may expect to see autonomic features in early Parkinson's disease, and the relationship between autonomic features and diagnostic consideration, which is important in the balanced diagnostic judgment approach emphasized in recent consensus guidelines," Dr. Malek concluded.
—Jake Remaly
PORTLAND, OR—Autonomic symptoms are present in a majority of patients with early Parkinson's disease, and symptoms correlate with markers of disease severity and impaired quality of life, according to research presented at the Fourth World Parkinson Congress.
Although autonomic dysfunction is common in the later stages of Parkinson's disease, less is known about autonomic symptom presence and severity in early stages of Parkinson's disease. Naveed Malek, MD, Department of Neurology, Institute of Neurological Sciences, Queen Elizabeth University Hospital, in Glasgow, and colleagues conducted a study to explore the prevalence, range, and severity of autonomic symptoms in a cohort of patients who had been diagnosed with Parkinson's disease in the preceding 3.5 years.
The researchers analyzed detailed patient-reported symptoms of autonomic dysfunction that were assessed in the multicenter United Kingdom Tracking Parkinson's study using the Scale for Outcomes in Parkinson's Disease for Autonomic Symptoms (SCOPA-AUT).
The researchers assessed the relationship between baseline SCOPA-AUT score and baseline motor, nonmotor, and quality of life scores. The researchers adjusted for sex, age, and disease duration differences across groups.
A total of 1,738 patients (65.1% male, mean age 67.6) were included in the main analysis. Patients had a mean disease duration of 1.3 years and mean Movement Disorder Society Unified Parkinson's Disease Rating Scale motor score of 22.5. Hoehn and Yahr was stage 1 or 1.5 in 855 cases (49.2%), stage 2 or 2.5 in 783 cases (45.1%), and stage 3 or higher in 100 cases (5.8%).
Autonomic severity by SCOPA-AUT score increased significantly across the motor severity stages, from 10.7 for Hoehn and Yahr stages 1 and 1.5, to 12.7 for Hoehn and Yahr stages 2 and 2.5, and to 13.5 for Hoehn and Yahr stages 3 and higher. Urinary, bowel, and sexual dysfunctions were the most commonly reported autonomic symptoms. The results were between those previously reported in controls and in patients with Parkinson's disease at a mean duration of 10 years. Positive associations were present between autonomic severity and depression, sleep disturbance, and postural instability motor subtype.
"Our study highlights the extent to which we may expect to see autonomic features in early Parkinson's disease, and the relationship between autonomic features and diagnostic consideration, which is important in the balanced diagnostic judgment approach emphasized in recent consensus guidelines," Dr. Malek concluded.
—Jake Remaly
Common Genetic Variants Associated With Cognitive Impairment in Parkinson’s Disease
PORTLAND, OR—A large-scale analysis has identified several new putative susceptibility genes that may affect cognitive impairment in Parkinson's disease, researchers reported at the Fourth World Parkinson Congress.
Cognitive impairment is a common and disabling nonmotor feature of Parkinson's disease. Identifying genetic variants that influence cognitive deficits could clarify the pathophysiology of cognitive impairment, help identify potential therapies, and be useful when considering patient prognosis, said Ignacio F. Mata, PhD, Research Biologist at the Veterans Affairs Puget Sound Health Care System and Acting Assistant Professor of Neurology at the University of Washington in Seattle. Rate of cognitive decline in Parkinson's disease varies. "We are trying to understand why," Dr. Mata said.
Dr. Mata and colleagues conducted a genome-wide exploratory analysis of genetic risk factors for cognitive impairment in a multisite cohort. The investigators genotyped 1,105 patients from the Parkinson's Disease Cognitive Genetics Consortium for 249,336 variants using the NeuroX array, which includes variants that have been linked to neurologic diseases.
Participants completed tests of learning and memory (Hopkins Verbal Learning Test-Revised), working memory and executive function (Letter-Number Sequencing and Trail Making Test Parts A and B), language processing (semantic and phonemic verbal fluency), visuospatial abilities (Benton Judgment of Line Orientation), and global cognitive function (Montreal Cognitive Assessment).
The researchers used linear regression to test for associations between common variants and cognitive performance, with adjustment for important covariates (eg, age, sex, disease duration, and years of education). They analyzed rare variants using the optimal unified sequence kernel association test.
Participants' mean age was 68.8, 67.8% were male, and 17.5% had dementia. Mean disease duration was 8.4 years. Participants had 15.5 years of education on average.
The researchers identified 17 common genetic variants associated with cognitive performance. Three variants were associated with total recall, and two variants were associated with delayed recall on the revised Hopkins Verbal Learning Test. Five variants were associated with performance on the Trail Making Test, and seven variants were associated with performance on the Benton Judgment of Line Orientation test.
The researchers aim to perform a similar analysis using longitudinal data. They also plan to see if these findings can be replicated in an independent cohort.
—Jake Remaly
PORTLAND, OR—A large-scale analysis has identified several new putative susceptibility genes that may affect cognitive impairment in Parkinson's disease, researchers reported at the Fourth World Parkinson Congress.
Cognitive impairment is a common and disabling nonmotor feature of Parkinson's disease. Identifying genetic variants that influence cognitive deficits could clarify the pathophysiology of cognitive impairment, help identify potential therapies, and be useful when considering patient prognosis, said Ignacio F. Mata, PhD, Research Biologist at the Veterans Affairs Puget Sound Health Care System and Acting Assistant Professor of Neurology at the University of Washington in Seattle. Rate of cognitive decline in Parkinson's disease varies. "We are trying to understand why," Dr. Mata said.
Dr. Mata and colleagues conducted a genome-wide exploratory analysis of genetic risk factors for cognitive impairment in a multisite cohort. The investigators genotyped 1,105 patients from the Parkinson's Disease Cognitive Genetics Consortium for 249,336 variants using the NeuroX array, which includes variants that have been linked to neurologic diseases.
Participants completed tests of learning and memory (Hopkins Verbal Learning Test-Revised), working memory and executive function (Letter-Number Sequencing and Trail Making Test Parts A and B), language processing (semantic and phonemic verbal fluency), visuospatial abilities (Benton Judgment of Line Orientation), and global cognitive function (Montreal Cognitive Assessment).
The researchers used linear regression to test for associations between common variants and cognitive performance, with adjustment for important covariates (eg, age, sex, disease duration, and years of education). They analyzed rare variants using the optimal unified sequence kernel association test.
Participants' mean age was 68.8, 67.8% were male, and 17.5% had dementia. Mean disease duration was 8.4 years. Participants had 15.5 years of education on average.
The researchers identified 17 common genetic variants associated with cognitive performance. Three variants were associated with total recall, and two variants were associated with delayed recall on the revised Hopkins Verbal Learning Test. Five variants were associated with performance on the Trail Making Test, and seven variants were associated with performance on the Benton Judgment of Line Orientation test.
The researchers aim to perform a similar analysis using longitudinal data. They also plan to see if these findings can be replicated in an independent cohort.
—Jake Remaly
PORTLAND, OR—A large-scale analysis has identified several new putative susceptibility genes that may affect cognitive impairment in Parkinson's disease, researchers reported at the Fourth World Parkinson Congress.
Cognitive impairment is a common and disabling nonmotor feature of Parkinson's disease. Identifying genetic variants that influence cognitive deficits could clarify the pathophysiology of cognitive impairment, help identify potential therapies, and be useful when considering patient prognosis, said Ignacio F. Mata, PhD, Research Biologist at the Veterans Affairs Puget Sound Health Care System and Acting Assistant Professor of Neurology at the University of Washington in Seattle. Rate of cognitive decline in Parkinson's disease varies. "We are trying to understand why," Dr. Mata said.
Dr. Mata and colleagues conducted a genome-wide exploratory analysis of genetic risk factors for cognitive impairment in a multisite cohort. The investigators genotyped 1,105 patients from the Parkinson's Disease Cognitive Genetics Consortium for 249,336 variants using the NeuroX array, which includes variants that have been linked to neurologic diseases.
Participants completed tests of learning and memory (Hopkins Verbal Learning Test-Revised), working memory and executive function (Letter-Number Sequencing and Trail Making Test Parts A and B), language processing (semantic and phonemic verbal fluency), visuospatial abilities (Benton Judgment of Line Orientation), and global cognitive function (Montreal Cognitive Assessment).
The researchers used linear regression to test for associations between common variants and cognitive performance, with adjustment for important covariates (eg, age, sex, disease duration, and years of education). They analyzed rare variants using the optimal unified sequence kernel association test.
Participants' mean age was 68.8, 67.8% were male, and 17.5% had dementia. Mean disease duration was 8.4 years. Participants had 15.5 years of education on average.
The researchers identified 17 common genetic variants associated with cognitive performance. Three variants were associated with total recall, and two variants were associated with delayed recall on the revised Hopkins Verbal Learning Test. Five variants were associated with performance on the Trail Making Test, and seven variants were associated with performance on the Benton Judgment of Line Orientation test.
The researchers aim to perform a similar analysis using longitudinal data. They also plan to see if these findings can be replicated in an independent cohort.
—Jake Remaly
Ear-worn device helps Parkinson’s patients to improve their voice
PORTLAND, ORE. – A new device worn on one ear may help individuals with Parkinson’s disease to overcome speech deficits associated with the disease. When triggered by the wearer’s voice, the device, SpeechVive, provides a simulated room crowd noise or “babble” only when they are talking. Because it capitalizes on natural reflexes to this simulated background noise, improvement can occur independent of speech training.
Researchers led by Jessica Huber, PhD, a professor of speech, language, and hearing sciences at Purdue University in West Lafayette, Ind., investigated changes to speech after 3 months of daily use of the SpeechVive device by 16 individuals. The cohort had a mean age of 64.5 years (range: 56-78 years) and a mean disease duration of 8.1 years (range: 2-17 years). Six participants had previously had speech therapy (five with LSVT [Lee Silverman Voice Treatment] LOUD speech training exercises), and two had deep brain stimulation implants.
Similar to an earlier study of 39 participants, “We found a nice increase in loudness, that they just can wear the device, and they’re louder in their everyday communication,” Dr. Huber said in an interview during a poster session at the World Parkinson Congress. New to this study was a finding that the melody of speech was a little better, “so their questions are more like questions, and their statements are more like statements, so are the rising intonation on questions and the falling intonation on a statement.” Participants were also able to say more on one breath and to sound more natural with appropriate pauses because of the longer utterances.
After 3 months of use, participants as a group increased their sound pressure level (loudness) from 76.6 dB to 78.8 dB (a gain of 2.2 dB) from having the device OFF to ON. When it was then turned off, they had an intermediate sound pressure level of 77.7 dB (both P less than .0001 vs. pretest OFF). Intonation variability and intonation range also showed significant improvements for both statements and questions with the use of the device (all P less than or equal to .01). There were also improvements in a correct statement or question being produced, pausing patterns, and utterance length. No adverse events occurred in the study.
Dr. Huber said patients in the study were quite variable in their responses to SpeechVive for the different measures of speech. In general, she has found that about 75% of users get louder with the device, and some have clearer articulation or slower speech. Another 10%-15% have slower speech or better articulation without an increase in loudness.
A total of 50% of the users have a “carry-over” effect after using the device when they are not wearing it. “After about 8 weeks, they don’t need to keep wearing the device every day,” Dr. Huber noted. Others may wear it in the morning and have a lasting effect for the rest of the day, and some lose any benefit as soon as taking the device off. Not all patients reach a normal speech loudness, “but they’re going to get way better” than where they started, she said.
Available speech therapies
People with Parkinson’s disease (PD) often have reduced vocal loudness, increased speech rate, and slurred articulation. Available speech therapies have included adduction exercises, vocal function exercises, and LSVT LOUD speech training exercises. For some individuals with PD, these behavioral treatments may not carry over into daily life.
The SpeechVive consists of a piece placed into the ear canal and a piece that sits behind the ear, similar to a slightly larger version of a modern hearing aid. It is designed large enough that many patients, who have motor deficits, can don it themselves. Because it is on just one ear, users can hear other people talking and what is going on around them.
Dr. Huber noted several strengths of the device. First, it does not impose any cognitive load on the user because its effect is based on an automatic reflex. Second, little training is necessary. It is easy for the user to put on the device, and many of its beneficial effects occur as soon as it is activated. Third, compliance can be tracked using data stored by the device itself.
In a previous study, she saw that after using the device for 8 weeks, participants used more effective patterns with their respiratory and laryngeal mechanisms to produce louder speech. “It’s not like they’re working super hard after 8 weeks.” She thinks they are just not usually using their speech apparatus in the most efficient manner, and they become more efficient after using the device. They may also not sense how loud they are without it, so it helps patients “recalibrate” a sense of their own voices, something the LSVT LOUD training also does.
Jori Fleisher, MD, a movement disorders neurologist at the New York University Langone Medical Center, commented that the study shows an interesting approach to the common and difficult problem of hypophonia and dysphonia in people with Parkinson’s disease. “It can be very difficult to speak loud enough to be heard, and it often leads to people withdrawing socially and not speaking as much in conversation as they normally would,” she said. “LSVT LOUD works in practice when you’re actually doing the exercises, but often when people stop doing the exercises, their voice goes back toward their normal. So this is something that you can keep with you and sort of have constant prompting to overcome that tendency toward quieter voice. It has a lot of promise.”
She said she would like to see the data on compliance or adherence with using the device “because it seems like a great idea, but how much are people actually using it? ... Having more long-term follow-up to see whether this is something that people want to put into practice in their daily life would be very useful.” She also said she would like to see how long the carry-over effect lasts once people take off the device to be able to compare it with sessions of speech therapy or doing speech exercises.
SpeechVive is $2,495, which includes the device, a charger, and earpiece fittings. It is available only in the United States, but the company now has clearance to market it in Canada.
The research was funded by a grant from SpeechVive. Dr. Huber is the inventor of SpeechVive, has a patent on it, has a financial interest in the SpeechVive company, and sits on its board of directors. Dr. Fleisher reported having no financial conflicts.
PORTLAND, ORE. – A new device worn on one ear may help individuals with Parkinson’s disease to overcome speech deficits associated with the disease. When triggered by the wearer’s voice, the device, SpeechVive, provides a simulated room crowd noise or “babble” only when they are talking. Because it capitalizes on natural reflexes to this simulated background noise, improvement can occur independent of speech training.
Researchers led by Jessica Huber, PhD, a professor of speech, language, and hearing sciences at Purdue University in West Lafayette, Ind., investigated changes to speech after 3 months of daily use of the SpeechVive device by 16 individuals. The cohort had a mean age of 64.5 years (range: 56-78 years) and a mean disease duration of 8.1 years (range: 2-17 years). Six participants had previously had speech therapy (five with LSVT [Lee Silverman Voice Treatment] LOUD speech training exercises), and two had deep brain stimulation implants.
Similar to an earlier study of 39 participants, “We found a nice increase in loudness, that they just can wear the device, and they’re louder in their everyday communication,” Dr. Huber said in an interview during a poster session at the World Parkinson Congress. New to this study was a finding that the melody of speech was a little better, “so their questions are more like questions, and their statements are more like statements, so are the rising intonation on questions and the falling intonation on a statement.” Participants were also able to say more on one breath and to sound more natural with appropriate pauses because of the longer utterances.
After 3 months of use, participants as a group increased their sound pressure level (loudness) from 76.6 dB to 78.8 dB (a gain of 2.2 dB) from having the device OFF to ON. When it was then turned off, they had an intermediate sound pressure level of 77.7 dB (both P less than .0001 vs. pretest OFF). Intonation variability and intonation range also showed significant improvements for both statements and questions with the use of the device (all P less than or equal to .01). There were also improvements in a correct statement or question being produced, pausing patterns, and utterance length. No adverse events occurred in the study.
Dr. Huber said patients in the study were quite variable in their responses to SpeechVive for the different measures of speech. In general, she has found that about 75% of users get louder with the device, and some have clearer articulation or slower speech. Another 10%-15% have slower speech or better articulation without an increase in loudness.
A total of 50% of the users have a “carry-over” effect after using the device when they are not wearing it. “After about 8 weeks, they don’t need to keep wearing the device every day,” Dr. Huber noted. Others may wear it in the morning and have a lasting effect for the rest of the day, and some lose any benefit as soon as taking the device off. Not all patients reach a normal speech loudness, “but they’re going to get way better” than where they started, she said.
Available speech therapies
People with Parkinson’s disease (PD) often have reduced vocal loudness, increased speech rate, and slurred articulation. Available speech therapies have included adduction exercises, vocal function exercises, and LSVT LOUD speech training exercises. For some individuals with PD, these behavioral treatments may not carry over into daily life.
The SpeechVive consists of a piece placed into the ear canal and a piece that sits behind the ear, similar to a slightly larger version of a modern hearing aid. It is designed large enough that many patients, who have motor deficits, can don it themselves. Because it is on just one ear, users can hear other people talking and what is going on around them.
Dr. Huber noted several strengths of the device. First, it does not impose any cognitive load on the user because its effect is based on an automatic reflex. Second, little training is necessary. It is easy for the user to put on the device, and many of its beneficial effects occur as soon as it is activated. Third, compliance can be tracked using data stored by the device itself.
In a previous study, she saw that after using the device for 8 weeks, participants used more effective patterns with their respiratory and laryngeal mechanisms to produce louder speech. “It’s not like they’re working super hard after 8 weeks.” She thinks they are just not usually using their speech apparatus in the most efficient manner, and they become more efficient after using the device. They may also not sense how loud they are without it, so it helps patients “recalibrate” a sense of their own voices, something the LSVT LOUD training also does.
Jori Fleisher, MD, a movement disorders neurologist at the New York University Langone Medical Center, commented that the study shows an interesting approach to the common and difficult problem of hypophonia and dysphonia in people with Parkinson’s disease. “It can be very difficult to speak loud enough to be heard, and it often leads to people withdrawing socially and not speaking as much in conversation as they normally would,” she said. “LSVT LOUD works in practice when you’re actually doing the exercises, but often when people stop doing the exercises, their voice goes back toward their normal. So this is something that you can keep with you and sort of have constant prompting to overcome that tendency toward quieter voice. It has a lot of promise.”
She said she would like to see the data on compliance or adherence with using the device “because it seems like a great idea, but how much are people actually using it? ... Having more long-term follow-up to see whether this is something that people want to put into practice in their daily life would be very useful.” She also said she would like to see how long the carry-over effect lasts once people take off the device to be able to compare it with sessions of speech therapy or doing speech exercises.
SpeechVive is $2,495, which includes the device, a charger, and earpiece fittings. It is available only in the United States, but the company now has clearance to market it in Canada.
The research was funded by a grant from SpeechVive. Dr. Huber is the inventor of SpeechVive, has a patent on it, has a financial interest in the SpeechVive company, and sits on its board of directors. Dr. Fleisher reported having no financial conflicts.
PORTLAND, ORE. – A new device worn on one ear may help individuals with Parkinson’s disease to overcome speech deficits associated with the disease. When triggered by the wearer’s voice, the device, SpeechVive, provides a simulated room crowd noise or “babble” only when they are talking. Because it capitalizes on natural reflexes to this simulated background noise, improvement can occur independent of speech training.
Researchers led by Jessica Huber, PhD, a professor of speech, language, and hearing sciences at Purdue University in West Lafayette, Ind., investigated changes to speech after 3 months of daily use of the SpeechVive device by 16 individuals. The cohort had a mean age of 64.5 years (range: 56-78 years) and a mean disease duration of 8.1 years (range: 2-17 years). Six participants had previously had speech therapy (five with LSVT [Lee Silverman Voice Treatment] LOUD speech training exercises), and two had deep brain stimulation implants.
Similar to an earlier study of 39 participants, “We found a nice increase in loudness, that they just can wear the device, and they’re louder in their everyday communication,” Dr. Huber said in an interview during a poster session at the World Parkinson Congress. New to this study was a finding that the melody of speech was a little better, “so their questions are more like questions, and their statements are more like statements, so are the rising intonation on questions and the falling intonation on a statement.” Participants were also able to say more on one breath and to sound more natural with appropriate pauses because of the longer utterances.
After 3 months of use, participants as a group increased their sound pressure level (loudness) from 76.6 dB to 78.8 dB (a gain of 2.2 dB) from having the device OFF to ON. When it was then turned off, they had an intermediate sound pressure level of 77.7 dB (both P less than .0001 vs. pretest OFF). Intonation variability and intonation range also showed significant improvements for both statements and questions with the use of the device (all P less than or equal to .01). There were also improvements in a correct statement or question being produced, pausing patterns, and utterance length. No adverse events occurred in the study.
Dr. Huber said patients in the study were quite variable in their responses to SpeechVive for the different measures of speech. In general, she has found that about 75% of users get louder with the device, and some have clearer articulation or slower speech. Another 10%-15% have slower speech or better articulation without an increase in loudness.
A total of 50% of the users have a “carry-over” effect after using the device when they are not wearing it. “After about 8 weeks, they don’t need to keep wearing the device every day,” Dr. Huber noted. Others may wear it in the morning and have a lasting effect for the rest of the day, and some lose any benefit as soon as taking the device off. Not all patients reach a normal speech loudness, “but they’re going to get way better” than where they started, she said.
Available speech therapies
People with Parkinson’s disease (PD) often have reduced vocal loudness, increased speech rate, and slurred articulation. Available speech therapies have included adduction exercises, vocal function exercises, and LSVT LOUD speech training exercises. For some individuals with PD, these behavioral treatments may not carry over into daily life.
The SpeechVive consists of a piece placed into the ear canal and a piece that sits behind the ear, similar to a slightly larger version of a modern hearing aid. It is designed large enough that many patients, who have motor deficits, can don it themselves. Because it is on just one ear, users can hear other people talking and what is going on around them.
Dr. Huber noted several strengths of the device. First, it does not impose any cognitive load on the user because its effect is based on an automatic reflex. Second, little training is necessary. It is easy for the user to put on the device, and many of its beneficial effects occur as soon as it is activated. Third, compliance can be tracked using data stored by the device itself.
In a previous study, she saw that after using the device for 8 weeks, participants used more effective patterns with their respiratory and laryngeal mechanisms to produce louder speech. “It’s not like they’re working super hard after 8 weeks.” She thinks they are just not usually using their speech apparatus in the most efficient manner, and they become more efficient after using the device. They may also not sense how loud they are without it, so it helps patients “recalibrate” a sense of their own voices, something the LSVT LOUD training also does.
Jori Fleisher, MD, a movement disorders neurologist at the New York University Langone Medical Center, commented that the study shows an interesting approach to the common and difficult problem of hypophonia and dysphonia in people with Parkinson’s disease. “It can be very difficult to speak loud enough to be heard, and it often leads to people withdrawing socially and not speaking as much in conversation as they normally would,” she said. “LSVT LOUD works in practice when you’re actually doing the exercises, but often when people stop doing the exercises, their voice goes back toward their normal. So this is something that you can keep with you and sort of have constant prompting to overcome that tendency toward quieter voice. It has a lot of promise.”
She said she would like to see the data on compliance or adherence with using the device “because it seems like a great idea, but how much are people actually using it? ... Having more long-term follow-up to see whether this is something that people want to put into practice in their daily life would be very useful.” She also said she would like to see how long the carry-over effect lasts once people take off the device to be able to compare it with sessions of speech therapy or doing speech exercises.
SpeechVive is $2,495, which includes the device, a charger, and earpiece fittings. It is available only in the United States, but the company now has clearance to market it in Canada.
The research was funded by a grant from SpeechVive. Dr. Huber is the inventor of SpeechVive, has a patent on it, has a financial interest in the SpeechVive company, and sits on its board of directors. Dr. Fleisher reported having no financial conflicts.
AT WPC 2016
Key clinical point:
Major finding: Loudness increased 2.2 dB from 76.6 dB to 78.8 dB after 3 months of use. Intonation also improved.
Data source: A prospective study of 16 participants with hypophonia comparing speech parameters with and without the device after 3 months of use.
Disclosures: The research was funded by a grant from SpeechVive. Dr. Huber is the inventor of SpeechVive, has a patent on it, has a financial interest in the SpeechVive company, and sits on its board of directors. Dr. Fleisher reported having no financial conflicts.
Many overweight Parkinson’s patients have insulin resistance
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
AT WPC 2016
Key clinical point:
Major finding: Among 84 nondiabetic, Parkinson’s patients, 58% had insulin resistance, although their blood glucose and insulin levels were not abnormal.
Data source: Prospective, observational study of a total of 93 Parkinson’s patients.
Disclosures: The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
Biomarkers predict Parkinson’s among high-risk individuals
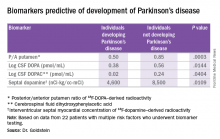
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
AT WPC 2016
Key clinical point:
Major finding: Among 22 individuals followed for at least 3 years, biomarkers were 100% positively or negatively predictive of developing Parkinson’s disease.
Data source: A prospective cohort study of 3,176 individuals supplying risk factor data, of whom 31 had three or more risk factors and biomarkers testing, and of whom 22 were followed for at least 3 years.
Disclosures: The study was run by the National Institute of Neurological Disorders and Stroke and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
Asleep deep brain stimulation placement offers advantages in Parkinson’s
PORTLAND, ORE. – Performing deep brain stimulation surgery for Parkinson’s disease using intraoperative CT imaging while the patient is under general anesthesia had clinical advantages and no disadvantages over surgery using microelectrode recording for lead placement with the patient awake, in a prospective, open-label study of 64 patients.
Regarding motor outcomes after asleep surgery, “We found that it was noninferior, so in other words, the change in scores following surgery were the same for asleep and awake patients,” physician assistant and study coauthor Shannon Anderson said during a poster session at the World Parkinson Congress. “What was surprising to us was that verbal fluency ... the ability to come up with the right word, actually improved in our asleep DBS [deep brain stimulation] group, which is a huge complication for patients [and] has a really negative impact on their life.”
Patients with Parkinson’s disease and motor complications (n = 64) were enrolled prospectively at the Oregon Health & Science University in Portland. Thirty received asleep procedures under general anesthesia with ICT guidance for lead targeting to the globus pallidus pars interna (GPi; n = 21) or to the subthalamic nucleus (STN; n = 9). Thirty-four patients received DBS devices with MER guidance (15 STN; 19 GPi). At baseline, the two groups were similar in age (mean 61.1-62.7 years) and off-medication motor subscale scores of the Unified Parkinson’s Disease Rating Scale (mUPDRS; mean 43.0-43.5). The university investigators optimized the DBS parameters at 1, 2, 3, and 6 months after implantation. The same surgeon performed all the procedures at the same medical center.
Motor improvements were similar between the asleep and awake cohorts. At 6 months, the ICT (asleep) group experienced a mean improvement in motor abilities of 14.3 (plus or minus 10.88) on the mUPDRS off-medication and on DBS, compared with an improvement of 17.6 (plus or minus 12.26) for the MER (awake) group (P = .25).
Better language measures with asleep DBS
Asleep DBS with ICT resulted in improvements in aspects of language, whereas awake patients lost language abilities. The asleep group showed a 0.8-point increase in phonemic fluency and a 1.0-point increase in semantic fluency at 6 months versus a worsening on both language measures (–3.5 points and –4.7 points, respectively; both P less than .001) if DBS was performed via MER on awake patients.
Although both cohorts showed significant improvements on the 39-item Parkinson’s Disease Questionnaire at 6 months, the cohorts did not differ in their degrees of improvement. Similarly, both had improvements on scores of activities of daily living, and both cohorts had a 4-4.5 hours/day increase in “on” time without dyskinesia and a 2.6-3.5 hours/day decrease in “on” time with dyskinesia.
Patients tolerated asleep DBS well, and there were no serious complications.
The sleep surgery is much shorter, “so it’s about 2 hours long as opposed to 4, 5, sometimes 8, 10 hours with the awake. There [are fewer] complications, so less risk of hemorrhage or seizures or things like that,” Ms. Anderson said. “In a separate study, we found that it’s a much more accurate placement of the electrodes so the target is much more accurate. So, all of those things considered, we feel the asleep version is definitely the superior choice between the two.”
Being asleep is much more comfortable for the patient, added study leader Matthew Brodsky, MD. “But the biggest advantage is that it’s a single pass into the brain as opposed to multiple passes.” The average number of passes using MER is two to three per side of the brain, and in some centers, four or more. “Problems such as speech prosody are related to pokes in the brain, if you will, rather than stimulation,” he said.
Ms. Anderson said MER “is a fantastic research tool, and it gives us a lot of information on the electrophysiology, but really, there’s no need for it in the clinical application of DBS.”
Based on the asleep procedure’s accuracy, lower rate of complications, shorter operating room time, and noninferiority in terms of motor outcomes, she said, “Our recommendation is that more centers, more neurosurgeons be trained in this technique ... We’d like to see the clinical field move toward that area and really reserve microelectrode recording for the research side of things.”
“If you talk to folks who are considering brain surgery for their Parkinson’s, for some of them, the idea of being awake in the operating room and undergoing this is a barrier that they can’t quite overcome,” Dr. Brodsky said. “So, having this as an option makes it easier for them to sign up for the process.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, said that the asleep procedure is the newer one and can target either the GPi or the STN. “The asleep DBS seems to have a little bit better improvement on speech afterwards than the awake DBS, and there could be several causes of this,” he said. “Some might be operative in that you can make smaller holes, you can get really nice guidance, you don’t have to sort of move around as in the awake DBS.”
In addition, CT scanning with the patients asleep in the operating room allows more time in the scanner and greater precision in anatomical placement of the DBS leads.
“If I had to choose, looking at this particular study, it would suggest that the asleep DBS is actually a better overall way to go,” Dr. Smeyne said. However, he had no objection to awake procedures “if the neurosurgeon has a record of good results with it ... But if you have the option ... that becomes an individual choice that you should discuss with the neurosurgeon.”
Some of the work presented in the study was supported by a research grant from Medtronic. Ms. Anderson and Dr. Brodsky reported having no other financial disclosures. Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – Performing deep brain stimulation surgery for Parkinson’s disease using intraoperative CT imaging while the patient is under general anesthesia had clinical advantages and no disadvantages over surgery using microelectrode recording for lead placement with the patient awake, in a prospective, open-label study of 64 patients.
Regarding motor outcomes after asleep surgery, “We found that it was noninferior, so in other words, the change in scores following surgery were the same for asleep and awake patients,” physician assistant and study coauthor Shannon Anderson said during a poster session at the World Parkinson Congress. “What was surprising to us was that verbal fluency ... the ability to come up with the right word, actually improved in our asleep DBS [deep brain stimulation] group, which is a huge complication for patients [and] has a really negative impact on their life.”
Patients with Parkinson’s disease and motor complications (n = 64) were enrolled prospectively at the Oregon Health & Science University in Portland. Thirty received asleep procedures under general anesthesia with ICT guidance for lead targeting to the globus pallidus pars interna (GPi; n = 21) or to the subthalamic nucleus (STN; n = 9). Thirty-four patients received DBS devices with MER guidance (15 STN; 19 GPi). At baseline, the two groups were similar in age (mean 61.1-62.7 years) and off-medication motor subscale scores of the Unified Parkinson’s Disease Rating Scale (mUPDRS; mean 43.0-43.5). The university investigators optimized the DBS parameters at 1, 2, 3, and 6 months after implantation. The same surgeon performed all the procedures at the same medical center.
Motor improvements were similar between the asleep and awake cohorts. At 6 months, the ICT (asleep) group experienced a mean improvement in motor abilities of 14.3 (plus or minus 10.88) on the mUPDRS off-medication and on DBS, compared with an improvement of 17.6 (plus or minus 12.26) for the MER (awake) group (P = .25).
Better language measures with asleep DBS
Asleep DBS with ICT resulted in improvements in aspects of language, whereas awake patients lost language abilities. The asleep group showed a 0.8-point increase in phonemic fluency and a 1.0-point increase in semantic fluency at 6 months versus a worsening on both language measures (–3.5 points and –4.7 points, respectively; both P less than .001) if DBS was performed via MER on awake patients.
Although both cohorts showed significant improvements on the 39-item Parkinson’s Disease Questionnaire at 6 months, the cohorts did not differ in their degrees of improvement. Similarly, both had improvements on scores of activities of daily living, and both cohorts had a 4-4.5 hours/day increase in “on” time without dyskinesia and a 2.6-3.5 hours/day decrease in “on” time with dyskinesia.
Patients tolerated asleep DBS well, and there were no serious complications.
The sleep surgery is much shorter, “so it’s about 2 hours long as opposed to 4, 5, sometimes 8, 10 hours with the awake. There [are fewer] complications, so less risk of hemorrhage or seizures or things like that,” Ms. Anderson said. “In a separate study, we found that it’s a much more accurate placement of the electrodes so the target is much more accurate. So, all of those things considered, we feel the asleep version is definitely the superior choice between the two.”
Being asleep is much more comfortable for the patient, added study leader Matthew Brodsky, MD. “But the biggest advantage is that it’s a single pass into the brain as opposed to multiple passes.” The average number of passes using MER is two to three per side of the brain, and in some centers, four or more. “Problems such as speech prosody are related to pokes in the brain, if you will, rather than stimulation,” he said.
Ms. Anderson said MER “is a fantastic research tool, and it gives us a lot of information on the electrophysiology, but really, there’s no need for it in the clinical application of DBS.”
Based on the asleep procedure’s accuracy, lower rate of complications, shorter operating room time, and noninferiority in terms of motor outcomes, she said, “Our recommendation is that more centers, more neurosurgeons be trained in this technique ... We’d like to see the clinical field move toward that area and really reserve microelectrode recording for the research side of things.”
“If you talk to folks who are considering brain surgery for their Parkinson’s, for some of them, the idea of being awake in the operating room and undergoing this is a barrier that they can’t quite overcome,” Dr. Brodsky said. “So, having this as an option makes it easier for them to sign up for the process.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, said that the asleep procedure is the newer one and can target either the GPi or the STN. “The asleep DBS seems to have a little bit better improvement on speech afterwards than the awake DBS, and there could be several causes of this,” he said. “Some might be operative in that you can make smaller holes, you can get really nice guidance, you don’t have to sort of move around as in the awake DBS.”
In addition, CT scanning with the patients asleep in the operating room allows more time in the scanner and greater precision in anatomical placement of the DBS leads.
“If I had to choose, looking at this particular study, it would suggest that the asleep DBS is actually a better overall way to go,” Dr. Smeyne said. However, he had no objection to awake procedures “if the neurosurgeon has a record of good results with it ... But if you have the option ... that becomes an individual choice that you should discuss with the neurosurgeon.”
Some of the work presented in the study was supported by a research grant from Medtronic. Ms. Anderson and Dr. Brodsky reported having no other financial disclosures. Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – Performing deep brain stimulation surgery for Parkinson’s disease using intraoperative CT imaging while the patient is under general anesthesia had clinical advantages and no disadvantages over surgery using microelectrode recording for lead placement with the patient awake, in a prospective, open-label study of 64 patients.
Regarding motor outcomes after asleep surgery, “We found that it was noninferior, so in other words, the change in scores following surgery were the same for asleep and awake patients,” physician assistant and study coauthor Shannon Anderson said during a poster session at the World Parkinson Congress. “What was surprising to us was that verbal fluency ... the ability to come up with the right word, actually improved in our asleep DBS [deep brain stimulation] group, which is a huge complication for patients [and] has a really negative impact on their life.”
Patients with Parkinson’s disease and motor complications (n = 64) were enrolled prospectively at the Oregon Health & Science University in Portland. Thirty received asleep procedures under general anesthesia with ICT guidance for lead targeting to the globus pallidus pars interna (GPi; n = 21) or to the subthalamic nucleus (STN; n = 9). Thirty-four patients received DBS devices with MER guidance (15 STN; 19 GPi). At baseline, the two groups were similar in age (mean 61.1-62.7 years) and off-medication motor subscale scores of the Unified Parkinson’s Disease Rating Scale (mUPDRS; mean 43.0-43.5). The university investigators optimized the DBS parameters at 1, 2, 3, and 6 months after implantation. The same surgeon performed all the procedures at the same medical center.
Motor improvements were similar between the asleep and awake cohorts. At 6 months, the ICT (asleep) group experienced a mean improvement in motor abilities of 14.3 (plus or minus 10.88) on the mUPDRS off-medication and on DBS, compared with an improvement of 17.6 (plus or minus 12.26) for the MER (awake) group (P = .25).
Better language measures with asleep DBS
Asleep DBS with ICT resulted in improvements in aspects of language, whereas awake patients lost language abilities. The asleep group showed a 0.8-point increase in phonemic fluency and a 1.0-point increase in semantic fluency at 6 months versus a worsening on both language measures (–3.5 points and –4.7 points, respectively; both P less than .001) if DBS was performed via MER on awake patients.
Although both cohorts showed significant improvements on the 39-item Parkinson’s Disease Questionnaire at 6 months, the cohorts did not differ in their degrees of improvement. Similarly, both had improvements on scores of activities of daily living, and both cohorts had a 4-4.5 hours/day increase in “on” time without dyskinesia and a 2.6-3.5 hours/day decrease in “on” time with dyskinesia.
Patients tolerated asleep DBS well, and there were no serious complications.
The sleep surgery is much shorter, “so it’s about 2 hours long as opposed to 4, 5, sometimes 8, 10 hours with the awake. There [are fewer] complications, so less risk of hemorrhage or seizures or things like that,” Ms. Anderson said. “In a separate study, we found that it’s a much more accurate placement of the electrodes so the target is much more accurate. So, all of those things considered, we feel the asleep version is definitely the superior choice between the two.”
Being asleep is much more comfortable for the patient, added study leader Matthew Brodsky, MD. “But the biggest advantage is that it’s a single pass into the brain as opposed to multiple passes.” The average number of passes using MER is two to three per side of the brain, and in some centers, four or more. “Problems such as speech prosody are related to pokes in the brain, if you will, rather than stimulation,” he said.
Ms. Anderson said MER “is a fantastic research tool, and it gives us a lot of information on the electrophysiology, but really, there’s no need for it in the clinical application of DBS.”
Based on the asleep procedure’s accuracy, lower rate of complications, shorter operating room time, and noninferiority in terms of motor outcomes, she said, “Our recommendation is that more centers, more neurosurgeons be trained in this technique ... We’d like to see the clinical field move toward that area and really reserve microelectrode recording for the research side of things.”
“If you talk to folks who are considering brain surgery for their Parkinson’s, for some of them, the idea of being awake in the operating room and undergoing this is a barrier that they can’t quite overcome,” Dr. Brodsky said. “So, having this as an option makes it easier for them to sign up for the process.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, said that the asleep procedure is the newer one and can target either the GPi or the STN. “The asleep DBS seems to have a little bit better improvement on speech afterwards than the awake DBS, and there could be several causes of this,” he said. “Some might be operative in that you can make smaller holes, you can get really nice guidance, you don’t have to sort of move around as in the awake DBS.”
In addition, CT scanning with the patients asleep in the operating room allows more time in the scanner and greater precision in anatomical placement of the DBS leads.
“If I had to choose, looking at this particular study, it would suggest that the asleep DBS is actually a better overall way to go,” Dr. Smeyne said. However, he had no objection to awake procedures “if the neurosurgeon has a record of good results with it ... But if you have the option ... that becomes an individual choice that you should discuss with the neurosurgeon.”
Some of the work presented in the study was supported by a research grant from Medtronic. Ms. Anderson and Dr. Brodsky reported having no other financial disclosures. Dr. Smeyne reported having no financial disclosures.
AT WPC 2016
Key clinical point:
Major finding: The asleep group showed a 0.8-point increase in phonemic fluency and a 1.0-point increase in semantic fluency at 6 months versus a worsening on both language measures (–3.5 points and –4.7 points, respectively; both P less than .001) if DBS was performed via MER on awake patients.
Data source: Prospective, open-label study of 64 patients receiving either awake or asleep deep brain stimulation placement.
Disclosures: Some of the work presented in the study was supported by a research grant from Medtronic. Ms. Anderson and Dr. Brodsky reported having no other financial disclosures. Dr. Smeyne reported having no financial disclosures.
Transcranial direct current stimulation enhances cognitive training in Parkinson’s
PORTLAND, ORE. – Combining transcranial direct current stimulation and cognitive training resulted in an improvement in a greater number of cognitive outcomes than either intervention alone in a small, randomized, controlled trial of patients with Parkinson’s disease and mild cognitive impairment.
Researchers at Curtin University in Perth, Western Australia, conducted the trial comparing the effects of standard (not individualized) cognitive training (SCT), tailored (individualized) cognitive training (TCT), transcranial direct current stimulation (tDCS), and a combination of tDCS with either form of cognitive training on cognitive outcomes, activities of daily living, and quality of life in such Parkinson’s patients with mild cognitive impairment. Previously, it was not known whether either form of cognitive training or tDCS or a combination of the two would be most efficacious in improving cognition in such patients.
Patients had cognitive deficits that did not interfere with functional independence and were responding to stable doses of antiparkinsonian medication. Forty-two eligible participants underwent neuropsychological testing at baseline and were randomly and equally assigned to one of six groups: SCT, TCT, tDCS, SCT+tDCS, TCT+tDCS, or control.
Cognitive training consisted of three 45-minute sessions per week for 4 weeks using Smartbrain Pro software in participants’ homes. tDCS involved constant 1.5 mA stimulation for 20 minutes in one session per week for 4 weeks at the university, with the anode placed over area F3 to stimulate the left dorsal lateral prefrontal cortex. Follow-up evaluations were at 12 weeks.
The following tests were used to evaluate each outcome: executive function – Stockings of Cambridge; attention/working memory – Stroop test; memory – paragraph recall; quality of life – PDQ-39; activities of daily living – Unified Parkinson’s Disease Rating Scale-II; and language – similarities test.
In general, combining tDCS with either form of cognitive training resulted in significantly greater improvements in more outcomes than any of the modalities alone. SCT showed positive results when compared against the control group in memory improvement at follow-up (effect size, 1.30), as well as quality of life and activities of daily living postintervention (effect sizes, 0.24 and 0.33, respectively). TCT showed benefits on quality of life at both time points (effect sizes 0.26 at postintervention and 0.12 at follow-up, respectively).
When combined with tDCS, SCT produced improvements in attention/working memory both postintervention and at 12-week follow-up (effect sizes, 0.60 and 0.24, respectively) as well as executive function at postintervention and follow-up (0.41 and 0.23). Improvement in activities of daily living and language were statistically significant only immediately postintervention.
Combining tDCS with TCT resulted in improvements postintervention and at follow-up on measures of memory (1.36 and 1.75) and executive function (0.19 and 0.92), as well as in language postintervention (1.06).
“The main takeaway was that the groups that completed both cognitive training and brain stimulation improved to a greater extent and in more outcomes than the groups that just completed the brain training or the stimulation individually,” Mr. Lawrence said. “The majority of the effects were shown immediately after the intervention, but some of the promising results ... actually maintained improvement at the 12-week follow-up, so that was after about 8 weeks, when they didn’t complete any intervention whatsoever.”
The improvements are probably clinically meaningful to patients since they themselves reported the outcomes on quality of life and activities of daily living scales, he said. He added that studies are coming out that look at the effect of brain stimulation and brain training at the same time, and they have shown improvement, but not many such studies have yet been done in Parkinson’s disease.
PORTLAND, ORE. – Combining transcranial direct current stimulation and cognitive training resulted in an improvement in a greater number of cognitive outcomes than either intervention alone in a small, randomized, controlled trial of patients with Parkinson’s disease and mild cognitive impairment.
Researchers at Curtin University in Perth, Western Australia, conducted the trial comparing the effects of standard (not individualized) cognitive training (SCT), tailored (individualized) cognitive training (TCT), transcranial direct current stimulation (tDCS), and a combination of tDCS with either form of cognitive training on cognitive outcomes, activities of daily living, and quality of life in such Parkinson’s patients with mild cognitive impairment. Previously, it was not known whether either form of cognitive training or tDCS or a combination of the two would be most efficacious in improving cognition in such patients.
Patients had cognitive deficits that did not interfere with functional independence and were responding to stable doses of antiparkinsonian medication. Forty-two eligible participants underwent neuropsychological testing at baseline and were randomly and equally assigned to one of six groups: SCT, TCT, tDCS, SCT+tDCS, TCT+tDCS, or control.
Cognitive training consisted of three 45-minute sessions per week for 4 weeks using Smartbrain Pro software in participants’ homes. tDCS involved constant 1.5 mA stimulation for 20 minutes in one session per week for 4 weeks at the university, with the anode placed over area F3 to stimulate the left dorsal lateral prefrontal cortex. Follow-up evaluations were at 12 weeks.
The following tests were used to evaluate each outcome: executive function – Stockings of Cambridge; attention/working memory – Stroop test; memory – paragraph recall; quality of life – PDQ-39; activities of daily living – Unified Parkinson’s Disease Rating Scale-II; and language – similarities test.
In general, combining tDCS with either form of cognitive training resulted in significantly greater improvements in more outcomes than any of the modalities alone. SCT showed positive results when compared against the control group in memory improvement at follow-up (effect size, 1.30), as well as quality of life and activities of daily living postintervention (effect sizes, 0.24 and 0.33, respectively). TCT showed benefits on quality of life at both time points (effect sizes 0.26 at postintervention and 0.12 at follow-up, respectively).
When combined with tDCS, SCT produced improvements in attention/working memory both postintervention and at 12-week follow-up (effect sizes, 0.60 and 0.24, respectively) as well as executive function at postintervention and follow-up (0.41 and 0.23). Improvement in activities of daily living and language were statistically significant only immediately postintervention.
Combining tDCS with TCT resulted in improvements postintervention and at follow-up on measures of memory (1.36 and 1.75) and executive function (0.19 and 0.92), as well as in language postintervention (1.06).
“The main takeaway was that the groups that completed both cognitive training and brain stimulation improved to a greater extent and in more outcomes than the groups that just completed the brain training or the stimulation individually,” Mr. Lawrence said. “The majority of the effects were shown immediately after the intervention, but some of the promising results ... actually maintained improvement at the 12-week follow-up, so that was after about 8 weeks, when they didn’t complete any intervention whatsoever.”
The improvements are probably clinically meaningful to patients since they themselves reported the outcomes on quality of life and activities of daily living scales, he said. He added that studies are coming out that look at the effect of brain stimulation and brain training at the same time, and they have shown improvement, but not many such studies have yet been done in Parkinson’s disease.
PORTLAND, ORE. – Combining transcranial direct current stimulation and cognitive training resulted in an improvement in a greater number of cognitive outcomes than either intervention alone in a small, randomized, controlled trial of patients with Parkinson’s disease and mild cognitive impairment.
Researchers at Curtin University in Perth, Western Australia, conducted the trial comparing the effects of standard (not individualized) cognitive training (SCT), tailored (individualized) cognitive training (TCT), transcranial direct current stimulation (tDCS), and a combination of tDCS with either form of cognitive training on cognitive outcomes, activities of daily living, and quality of life in such Parkinson’s patients with mild cognitive impairment. Previously, it was not known whether either form of cognitive training or tDCS or a combination of the two would be most efficacious in improving cognition in such patients.
Patients had cognitive deficits that did not interfere with functional independence and were responding to stable doses of antiparkinsonian medication. Forty-two eligible participants underwent neuropsychological testing at baseline and were randomly and equally assigned to one of six groups: SCT, TCT, tDCS, SCT+tDCS, TCT+tDCS, or control.
Cognitive training consisted of three 45-minute sessions per week for 4 weeks using Smartbrain Pro software in participants’ homes. tDCS involved constant 1.5 mA stimulation for 20 minutes in one session per week for 4 weeks at the university, with the anode placed over area F3 to stimulate the left dorsal lateral prefrontal cortex. Follow-up evaluations were at 12 weeks.
The following tests were used to evaluate each outcome: executive function – Stockings of Cambridge; attention/working memory – Stroop test; memory – paragraph recall; quality of life – PDQ-39; activities of daily living – Unified Parkinson’s Disease Rating Scale-II; and language – similarities test.
In general, combining tDCS with either form of cognitive training resulted in significantly greater improvements in more outcomes than any of the modalities alone. SCT showed positive results when compared against the control group in memory improvement at follow-up (effect size, 1.30), as well as quality of life and activities of daily living postintervention (effect sizes, 0.24 and 0.33, respectively). TCT showed benefits on quality of life at both time points (effect sizes 0.26 at postintervention and 0.12 at follow-up, respectively).
When combined with tDCS, SCT produced improvements in attention/working memory both postintervention and at 12-week follow-up (effect sizes, 0.60 and 0.24, respectively) as well as executive function at postintervention and follow-up (0.41 and 0.23). Improvement in activities of daily living and language were statistically significant only immediately postintervention.
Combining tDCS with TCT resulted in improvements postintervention and at follow-up on measures of memory (1.36 and 1.75) and executive function (0.19 and 0.92), as well as in language postintervention (1.06).
“The main takeaway was that the groups that completed both cognitive training and brain stimulation improved to a greater extent and in more outcomes than the groups that just completed the brain training or the stimulation individually,” Mr. Lawrence said. “The majority of the effects were shown immediately after the intervention, but some of the promising results ... actually maintained improvement at the 12-week follow-up, so that was after about 8 weeks, when they didn’t complete any intervention whatsoever.”
The improvements are probably clinically meaningful to patients since they themselves reported the outcomes on quality of life and activities of daily living scales, he said. He added that studies are coming out that look at the effect of brain stimulation and brain training at the same time, and they have shown improvement, but not many such studies have yet been done in Parkinson’s disease.
Key clinical point:
Major finding: tDCS adds cognitive benefit when combined with cognitive training alone.
Data source: Randomized, controlled trial of 42 patients with Parkinson’s disease and mild cognitive impairment.
Disclosures: There was no commercial funding of the study. Mr. Lawrence reported he had no financial disclosures.
Gait predicts cognitive decline in early Parkinson’s
PORTLAND, ORE. – Gait characteristics, rather than cognition, in early Parkinson’s disease predicted cognitive decline 3 years later in a small longitudinal study, suggesting that gait measures may provide a low cost clinical biomarker when combined with other predictors of cognitive decline in Parkinson’s disease.
Cognitive decline and dementia take a significant toll on patients’ personal, social, and economic affairs. Being able to identify at-risk individuals may allow for early behavioral and possibly pharmacological interventions. Gait has been shown to be a sensitive measure of cognitive decline in older adults, and the investigators here tested it as a predictor of cognitive decline in Parkinson’s disease (PD).
Led by Rosie Morris, PhD, of Newcastle University, Newcastle upon Tyne, England, researchers assessed gait characteristics and cognition in 119 patients within 4-6 months of a diagnosis of idiopathic PD and then 18 and 36 months later. The patients were recruited from the Incidence of Cognitive Impairment in Cohorts with Longitudinal Evaluation – Parkinson’s Disease (ICICLE-PD) study.
In this ICICLE-Gait substudy, participants walked for 2 minutes around a circuit that included a 7-meter instrumented walkway (GaitRite) that recorded 16 gait characteristics in the five independent domains of pace, variability, rhythm, asymmetry, and posture control. The investigators used the Montreal Cognitive Assessment (MoCA) battery of tests to assess global cognition, attention, fluctuating attention, executive function, working memory, visual memory, and visuospatial ability. They adjusted the results for covariates of age, education, gender, depression, and levodopa equivalent daily doses.
“We found that seven characteristics of gait were able to predict changes in measures of attention,” Dr. Morris said during a poster session at the World Parkinson Congress. The characteristics of gait were “mainly pace and variability and at diagnosis were sensitive to decline in tests of attention.”
With the multiple measures used in this study, a P value of less than or equal to .01 was considered statistically significant.
There were significant cognitive declines in the areas of attention, fluctuating attention, executive function, and visual memory. Fluctuating attention was predicted by measures of gait pace (step velocity, step length, and step swing: all P less than or equal to .007), gait variability (step stance and step length: both P less than or equal to .01), and postural control (P = .004). The pace measure of step length also predicted a decline in visual memory (P = .01).
Baseline MoCA predicted a decline in attention (P less than .001) but not in fluctuating attention or in visual memory.
The authors said that this study is the first “to demonstrate that discrete gait characteristics can predict measures of cognitive decline in early PD.” Asked why gait may predict cognitive decline, Dr. Morris postulated that certain characteristics of gait, such as speed and postural control, are related to cognition more so than other characteristics such as asymmetry.
These techniques may have clinical utility and not be merely of research interest. The parameters of gait may be measurable in the community using wearable sensors such as accelerometers “to measure discrete characteristics of gait ... So, ideally, it will be a possible future biomarker, and then we can measure them in the clinic and then identify risks from there,” she said, adding that she is planning research to explore the association of gait and cognition. Confounding factors yet to be examined are the effects of being on or off different medications and different medication cycles when patients are free-living in the community.
If researchers can validate that gait is a sensitive predictor of dementia, then the question becomes what to do about it. Dr. Morris suggested that physical therapy should incorporate more cognitive tasks.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center, said that the study is “really interesting because right now there’s a huge search underway for biomarkers” to reliably predict progression of Parkinson’s disease or predict who is at risk for the disease.
“These investigators looked at whether something as seemingly simple as gait – so the way that someone walks, the way that their balance is, the pace of their walking – could predict decline in cognition. And that’s something of great interest to clinicians and to researchers: How do we figure out which of our patients are going to experience cognitive decline and in what different domains?” she said.
Although the researchers in this study used sophisticated and sensitive measures of several aspects of gait not generally available to clinicians, Dr. Fleisher predicted that it may be possible to extrapolate the findings to look for specific aspects of gait variability (possibly through the use of wearable devices) so the technique may become widely useful.
Once a patient is seen to be at high risk for cognitive decline, she said, exercise may be an appropriate intervention. “We know huge benefits of exercise, which have been shown in various aspects of cognitive decline ... [to] slow the decline in cognitive function.” Dr. Fleisher said the best exercise is any one that a patient will continue to do, whether it is walking, dancing, or any other exercise that the person will stick with.
The study was supported in the United Kingdom by the National Institute for Health Research, the National Health Service, and Parkinson’s UK. There was no commercial funding. Dr. Morris reported having no financial disclosures. Dr. Fleisher had no financial disclosures.
PORTLAND, ORE. – Gait characteristics, rather than cognition, in early Parkinson’s disease predicted cognitive decline 3 years later in a small longitudinal study, suggesting that gait measures may provide a low cost clinical biomarker when combined with other predictors of cognitive decline in Parkinson’s disease.
Cognitive decline and dementia take a significant toll on patients’ personal, social, and economic affairs. Being able to identify at-risk individuals may allow for early behavioral and possibly pharmacological interventions. Gait has been shown to be a sensitive measure of cognitive decline in older adults, and the investigators here tested it as a predictor of cognitive decline in Parkinson’s disease (PD).
Led by Rosie Morris, PhD, of Newcastle University, Newcastle upon Tyne, England, researchers assessed gait characteristics and cognition in 119 patients within 4-6 months of a diagnosis of idiopathic PD and then 18 and 36 months later. The patients were recruited from the Incidence of Cognitive Impairment in Cohorts with Longitudinal Evaluation – Parkinson’s Disease (ICICLE-PD) study.
In this ICICLE-Gait substudy, participants walked for 2 minutes around a circuit that included a 7-meter instrumented walkway (GaitRite) that recorded 16 gait characteristics in the five independent domains of pace, variability, rhythm, asymmetry, and posture control. The investigators used the Montreal Cognitive Assessment (MoCA) battery of tests to assess global cognition, attention, fluctuating attention, executive function, working memory, visual memory, and visuospatial ability. They adjusted the results for covariates of age, education, gender, depression, and levodopa equivalent daily doses.
“We found that seven characteristics of gait were able to predict changes in measures of attention,” Dr. Morris said during a poster session at the World Parkinson Congress. The characteristics of gait were “mainly pace and variability and at diagnosis were sensitive to decline in tests of attention.”
With the multiple measures used in this study, a P value of less than or equal to .01 was considered statistically significant.
There were significant cognitive declines in the areas of attention, fluctuating attention, executive function, and visual memory. Fluctuating attention was predicted by measures of gait pace (step velocity, step length, and step swing: all P less than or equal to .007), gait variability (step stance and step length: both P less than or equal to .01), and postural control (P = .004). The pace measure of step length also predicted a decline in visual memory (P = .01).
Baseline MoCA predicted a decline in attention (P less than .001) but not in fluctuating attention or in visual memory.
The authors said that this study is the first “to demonstrate that discrete gait characteristics can predict measures of cognitive decline in early PD.” Asked why gait may predict cognitive decline, Dr. Morris postulated that certain characteristics of gait, such as speed and postural control, are related to cognition more so than other characteristics such as asymmetry.
These techniques may have clinical utility and not be merely of research interest. The parameters of gait may be measurable in the community using wearable sensors such as accelerometers “to measure discrete characteristics of gait ... So, ideally, it will be a possible future biomarker, and then we can measure them in the clinic and then identify risks from there,” she said, adding that she is planning research to explore the association of gait and cognition. Confounding factors yet to be examined are the effects of being on or off different medications and different medication cycles when patients are free-living in the community.
If researchers can validate that gait is a sensitive predictor of dementia, then the question becomes what to do about it. Dr. Morris suggested that physical therapy should incorporate more cognitive tasks.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center, said that the study is “really interesting because right now there’s a huge search underway for biomarkers” to reliably predict progression of Parkinson’s disease or predict who is at risk for the disease.
“These investigators looked at whether something as seemingly simple as gait – so the way that someone walks, the way that their balance is, the pace of their walking – could predict decline in cognition. And that’s something of great interest to clinicians and to researchers: How do we figure out which of our patients are going to experience cognitive decline and in what different domains?” she said.
Although the researchers in this study used sophisticated and sensitive measures of several aspects of gait not generally available to clinicians, Dr. Fleisher predicted that it may be possible to extrapolate the findings to look for specific aspects of gait variability (possibly through the use of wearable devices) so the technique may become widely useful.
Once a patient is seen to be at high risk for cognitive decline, she said, exercise may be an appropriate intervention. “We know huge benefits of exercise, which have been shown in various aspects of cognitive decline ... [to] slow the decline in cognitive function.” Dr. Fleisher said the best exercise is any one that a patient will continue to do, whether it is walking, dancing, or any other exercise that the person will stick with.
The study was supported in the United Kingdom by the National Institute for Health Research, the National Health Service, and Parkinson’s UK. There was no commercial funding. Dr. Morris reported having no financial disclosures. Dr. Fleisher had no financial disclosures.
PORTLAND, ORE. – Gait characteristics, rather than cognition, in early Parkinson’s disease predicted cognitive decline 3 years later in a small longitudinal study, suggesting that gait measures may provide a low cost clinical biomarker when combined with other predictors of cognitive decline in Parkinson’s disease.
Cognitive decline and dementia take a significant toll on patients’ personal, social, and economic affairs. Being able to identify at-risk individuals may allow for early behavioral and possibly pharmacological interventions. Gait has been shown to be a sensitive measure of cognitive decline in older adults, and the investigators here tested it as a predictor of cognitive decline in Parkinson’s disease (PD).
Led by Rosie Morris, PhD, of Newcastle University, Newcastle upon Tyne, England, researchers assessed gait characteristics and cognition in 119 patients within 4-6 months of a diagnosis of idiopathic PD and then 18 and 36 months later. The patients were recruited from the Incidence of Cognitive Impairment in Cohorts with Longitudinal Evaluation – Parkinson’s Disease (ICICLE-PD) study.
In this ICICLE-Gait substudy, participants walked for 2 minutes around a circuit that included a 7-meter instrumented walkway (GaitRite) that recorded 16 gait characteristics in the five independent domains of pace, variability, rhythm, asymmetry, and posture control. The investigators used the Montreal Cognitive Assessment (MoCA) battery of tests to assess global cognition, attention, fluctuating attention, executive function, working memory, visual memory, and visuospatial ability. They adjusted the results for covariates of age, education, gender, depression, and levodopa equivalent daily doses.
“We found that seven characteristics of gait were able to predict changes in measures of attention,” Dr. Morris said during a poster session at the World Parkinson Congress. The characteristics of gait were “mainly pace and variability and at diagnosis were sensitive to decline in tests of attention.”
With the multiple measures used in this study, a P value of less than or equal to .01 was considered statistically significant.
There were significant cognitive declines in the areas of attention, fluctuating attention, executive function, and visual memory. Fluctuating attention was predicted by measures of gait pace (step velocity, step length, and step swing: all P less than or equal to .007), gait variability (step stance and step length: both P less than or equal to .01), and postural control (P = .004). The pace measure of step length also predicted a decline in visual memory (P = .01).
Baseline MoCA predicted a decline in attention (P less than .001) but not in fluctuating attention or in visual memory.
The authors said that this study is the first “to demonstrate that discrete gait characteristics can predict measures of cognitive decline in early PD.” Asked why gait may predict cognitive decline, Dr. Morris postulated that certain characteristics of gait, such as speed and postural control, are related to cognition more so than other characteristics such as asymmetry.
These techniques may have clinical utility and not be merely of research interest. The parameters of gait may be measurable in the community using wearable sensors such as accelerometers “to measure discrete characteristics of gait ... So, ideally, it will be a possible future biomarker, and then we can measure them in the clinic and then identify risks from there,” she said, adding that she is planning research to explore the association of gait and cognition. Confounding factors yet to be examined are the effects of being on or off different medications and different medication cycles when patients are free-living in the community.
If researchers can validate that gait is a sensitive predictor of dementia, then the question becomes what to do about it. Dr. Morris suggested that physical therapy should incorporate more cognitive tasks.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center, said that the study is “really interesting because right now there’s a huge search underway for biomarkers” to reliably predict progression of Parkinson’s disease or predict who is at risk for the disease.
“These investigators looked at whether something as seemingly simple as gait – so the way that someone walks, the way that their balance is, the pace of their walking – could predict decline in cognition. And that’s something of great interest to clinicians and to researchers: How do we figure out which of our patients are going to experience cognitive decline and in what different domains?” she said.
Although the researchers in this study used sophisticated and sensitive measures of several aspects of gait not generally available to clinicians, Dr. Fleisher predicted that it may be possible to extrapolate the findings to look for specific aspects of gait variability (possibly through the use of wearable devices) so the technique may become widely useful.
Once a patient is seen to be at high risk for cognitive decline, she said, exercise may be an appropriate intervention. “We know huge benefits of exercise, which have been shown in various aspects of cognitive decline ... [to] slow the decline in cognitive function.” Dr. Fleisher said the best exercise is any one that a patient will continue to do, whether it is walking, dancing, or any other exercise that the person will stick with.
The study was supported in the United Kingdom by the National Institute for Health Research, the National Health Service, and Parkinson’s UK. There was no commercial funding. Dr. Morris reported having no financial disclosures. Dr. Fleisher had no financial disclosures.
AT WPC 2016
Key clinical point: Gait characteristics, not cognition, predict cognitive decline in early Parkinson’s.
Major finding: Gait pace, variability, and postural control predict cognitive decline.
Data source: Observational study of 119 patients with early idiopathic Parkinson’s disease assessed at baseline and at 36 months.
Disclosures: The study was supported in the United Kingdom by the National Institute for Health Research, the National Health Service, and Parkinson’s UK. There was no commercial funding. Dr. Morris and Dr. Fleisher had no financial disclosures.