User login
European Society of Cardiology (ESC): Annual Congress
Quinine Doesn't Mix Well With Heart Failure, Ischemic Disease
MUNICH – Treatment with quinine increased the mortality of heart failure patients who also had ischemic heart disease and received a beta-blocker by a statistically significant 16% in a study of more than 136,000 Danish heart failure patients during 1997-2010.
Although experts suggest that such use of quinine is not commonplace in the United States, the analysis of Danish patient and population registries showed that quinine was used in the treatment of 10% of HF patients. Quinine, an antimalarial drug, is often prescribed off-label to treat leg cramps, a common problem in patients with HF, Dr. Charlotte Andersson said at the annual congress of the European Society of Cardiology.
"Clinicians should attempt to find a treatment for leg cramps other than prescribing quinine" in patients with chronic HF, especially those with ischemic heart disease, said Dr. Andersson, a cardiologist at Gentofte Hospital in Copenhagen. She also expressed surprise that the dangerous interaction was greatest among patients who also received a beta-blocker drug.
"I would have expected patients on beta-blockers to be protected, but they weren’t, so probably conduction blocks [caused by quinine] are the problem," she said. "We found the highest risk of death during the first week of quinine treatment in patients with ischemic heart disease and on a beta-blocker, but if quinine was used chronically it still increased the risk."
"This is very interesting and important information," commented Dr. Marco Metra, a cardiologist at the University of Brescia, Italy. "The question is, what is the mechanism of the interaction of quinine and beta-blockers? We think that beta-blockers are protective against arrhythmias caused by QT prolongation. In this case, [the problem may be] bradycardia" caused by a beta-blocker that interacts with an effect from quinine, he suggested.
Dr. Andersson and her associates reviewed Danish national patient and population registry records collected during 1997-2010, which included 136,427 patients discharged from a hospital with a diagnosis of heart failure and who were alive at least 30 days following discharge. Their average age was 74 years, 47% were women, and 65% died during a median follow-up of 2.8 years.
The records showed that 14,306 patients (10%) had received at least one course of treatment with quinine, at a dosage of 100 or 200 mg/day. Overall, patients who received quinine had a 3% increased risk of death after adjustment for age and HF severity, which was estimated based on the dosage of loop diuretics they received. This increased risk fell just short of statistical significance.
However, further analysis showed that specific subgroups of HF patients faced a higher mortality threat from quinine treatment. Patients with ischemic heart disease (37% of the HF population) who received treatment with a beta-blocker (60% of the HF patients with ischemic heart disease) had the highest mortality when they received quinine, 16% higher than for similar patients who did not get quinine, after adjustment for age and HF severity. This meant that for every 38 patients with this clinical profile treated with quinine, 1 died.
Among HF patients with ischemic heart disease who did not receive a beta-blocker, the mortality rate was elevated by a statistically significant 8% among quinine users compared with quinine nonusers; 1 death occurred for every 46 patients in this category. And among HF patients who received a beta-blocker but who did not have ischemic heart disease, quinine treatment raised mortality by a statistically significant 9%, or 1 death for every 97 patients treated with quinine who fit this clinical profile.
Dr. Andersson said that she and her associates had no disclosures.
MUNICH – Treatment with quinine increased the mortality of heart failure patients who also had ischemic heart disease and received a beta-blocker by a statistically significant 16% in a study of more than 136,000 Danish heart failure patients during 1997-2010.
Although experts suggest that such use of quinine is not commonplace in the United States, the analysis of Danish patient and population registries showed that quinine was used in the treatment of 10% of HF patients. Quinine, an antimalarial drug, is often prescribed off-label to treat leg cramps, a common problem in patients with HF, Dr. Charlotte Andersson said at the annual congress of the European Society of Cardiology.
"Clinicians should attempt to find a treatment for leg cramps other than prescribing quinine" in patients with chronic HF, especially those with ischemic heart disease, said Dr. Andersson, a cardiologist at Gentofte Hospital in Copenhagen. She also expressed surprise that the dangerous interaction was greatest among patients who also received a beta-blocker drug.
"I would have expected patients on beta-blockers to be protected, but they weren’t, so probably conduction blocks [caused by quinine] are the problem," she said. "We found the highest risk of death during the first week of quinine treatment in patients with ischemic heart disease and on a beta-blocker, but if quinine was used chronically it still increased the risk."
"This is very interesting and important information," commented Dr. Marco Metra, a cardiologist at the University of Brescia, Italy. "The question is, what is the mechanism of the interaction of quinine and beta-blockers? We think that beta-blockers are protective against arrhythmias caused by QT prolongation. In this case, [the problem may be] bradycardia" caused by a beta-blocker that interacts with an effect from quinine, he suggested.
Dr. Andersson and her associates reviewed Danish national patient and population registry records collected during 1997-2010, which included 136,427 patients discharged from a hospital with a diagnosis of heart failure and who were alive at least 30 days following discharge. Their average age was 74 years, 47% were women, and 65% died during a median follow-up of 2.8 years.
The records showed that 14,306 patients (10%) had received at least one course of treatment with quinine, at a dosage of 100 or 200 mg/day. Overall, patients who received quinine had a 3% increased risk of death after adjustment for age and HF severity, which was estimated based on the dosage of loop diuretics they received. This increased risk fell just short of statistical significance.
However, further analysis showed that specific subgroups of HF patients faced a higher mortality threat from quinine treatment. Patients with ischemic heart disease (37% of the HF population) who received treatment with a beta-blocker (60% of the HF patients with ischemic heart disease) had the highest mortality when they received quinine, 16% higher than for similar patients who did not get quinine, after adjustment for age and HF severity. This meant that for every 38 patients with this clinical profile treated with quinine, 1 died.
Among HF patients with ischemic heart disease who did not receive a beta-blocker, the mortality rate was elevated by a statistically significant 8% among quinine users compared with quinine nonusers; 1 death occurred for every 46 patients in this category. And among HF patients who received a beta-blocker but who did not have ischemic heart disease, quinine treatment raised mortality by a statistically significant 9%, or 1 death for every 97 patients treated with quinine who fit this clinical profile.
Dr. Andersson said that she and her associates had no disclosures.
MUNICH – Treatment with quinine increased the mortality of heart failure patients who also had ischemic heart disease and received a beta-blocker by a statistically significant 16% in a study of more than 136,000 Danish heart failure patients during 1997-2010.
Although experts suggest that such use of quinine is not commonplace in the United States, the analysis of Danish patient and population registries showed that quinine was used in the treatment of 10% of HF patients. Quinine, an antimalarial drug, is often prescribed off-label to treat leg cramps, a common problem in patients with HF, Dr. Charlotte Andersson said at the annual congress of the European Society of Cardiology.
"Clinicians should attempt to find a treatment for leg cramps other than prescribing quinine" in patients with chronic HF, especially those with ischemic heart disease, said Dr. Andersson, a cardiologist at Gentofte Hospital in Copenhagen. She also expressed surprise that the dangerous interaction was greatest among patients who also received a beta-blocker drug.
"I would have expected patients on beta-blockers to be protected, but they weren’t, so probably conduction blocks [caused by quinine] are the problem," she said. "We found the highest risk of death during the first week of quinine treatment in patients with ischemic heart disease and on a beta-blocker, but if quinine was used chronically it still increased the risk."
"This is very interesting and important information," commented Dr. Marco Metra, a cardiologist at the University of Brescia, Italy. "The question is, what is the mechanism of the interaction of quinine and beta-blockers? We think that beta-blockers are protective against arrhythmias caused by QT prolongation. In this case, [the problem may be] bradycardia" caused by a beta-blocker that interacts with an effect from quinine, he suggested.
Dr. Andersson and her associates reviewed Danish national patient and population registry records collected during 1997-2010, which included 136,427 patients discharged from a hospital with a diagnosis of heart failure and who were alive at least 30 days following discharge. Their average age was 74 years, 47% were women, and 65% died during a median follow-up of 2.8 years.
The records showed that 14,306 patients (10%) had received at least one course of treatment with quinine, at a dosage of 100 or 200 mg/day. Overall, patients who received quinine had a 3% increased risk of death after adjustment for age and HF severity, which was estimated based on the dosage of loop diuretics they received. This increased risk fell just short of statistical significance.
However, further analysis showed that specific subgroups of HF patients faced a higher mortality threat from quinine treatment. Patients with ischemic heart disease (37% of the HF population) who received treatment with a beta-blocker (60% of the HF patients with ischemic heart disease) had the highest mortality when they received quinine, 16% higher than for similar patients who did not get quinine, after adjustment for age and HF severity. This meant that for every 38 patients with this clinical profile treated with quinine, 1 died.
Among HF patients with ischemic heart disease who did not receive a beta-blocker, the mortality rate was elevated by a statistically significant 8% among quinine users compared with quinine nonusers; 1 death occurred for every 46 patients in this category. And among HF patients who received a beta-blocker but who did not have ischemic heart disease, quinine treatment raised mortality by a statistically significant 9%, or 1 death for every 97 patients treated with quinine who fit this clinical profile.
Dr. Andersson said that she and her associates had no disclosures.
AT THE ANNUAL CONGRESS OF THE EUROPEAN SOCIETY OF CARDIOLOGY
Major Finding: Among patients with heart failure and ischemic heart disease on beta-blocker treatment, quinine dosing boosted mortality by 16%.
Data Source: This was a review of Danish patient and population records that included 136,427 patients discharged with a diagnosis of heart failure during 1997-2010.
Disclosures: Dr. Andersson said that she and her associates had no disclosures.
Adding Clopidogrel to Anticoagulant Is Plenty for PCI
MUNICH – Patients who require chronic oral anticoagulant treatment and received a coronary stent had significantly fewer bleeding events and better outcomes if they received only added clopidogrel than if they were treated with clopidogrel plus aspirin on top of their anticoagulant in the WOEST trial.
As the first study to prospectively test the best combination of antiplatelet drugs to use on top of anticoagulant treatment in patients following coronary stenting, experts hailed the finding as important evidence to address a common and vexing clinical situation.
"We propose that a strategy of oral anticoagulants plus clopidogrel, but without aspirin could be applied in this group of high-risk patients who are on an oral anticoagulant and undergo percutaneous coronary intervention," said Dr. Willem Dewilde, lead investigator for the study, at the Annual Congress of the European Society of Cardiology.
"We are faced with a huge clinical problem, with an increasing number of patients with atrial fibrillation who undergo stent procedures, so this finding has major implications," commented Dr. David R. Holmes Jr., professor of medicine and a cardiologist at the Mayo Clinic in Rochester, Minn. "Bleeding is such a huge issue, and we now have scientific data that says [withholding aspirin] is safe and produces less bleeding."
"The taboo against discontinuing or omitting aspirin has been broken," commented Dr. Marco Valgimigli, director of the coronary catheterization laboratory at the University Hospital of Ferrara (Italy).
The WOEST (What is the Optimal Antiplatelet and Anticoagulant Therapy in Patients with Oral Anticoagulation and Coronary Stenting) trial enrolled 573 patients who required chronic oral anticoagulant treatment and were scheduled for coronary stenting at 15 centers in the Netherlands and Belgium. The patients averaged about 70 years of age, and about 80% were men. A total of 70% received daily, oral treatment with an anticoagulant for atrial fibrillation or flutter, about 10% for a mechanical valve, and the remaining 20% had other reasons for their regimen, including treatment of a pulmonary embolus. All patients received warfarin or another oral anticoagulant such as acenocoumarol. About two-thirds of the patients received a drug-eluting coronary stent, with the remainder receiving a bare-metal stent.
Following stenting, the researchers randomized patients to a regimen of their oral anticoagulant plus 75 mg clopidogrel daily (dual therapy), or their oral anticoagulant, clopidogrel, and 80 mg aspirin daily (triple therapy). The antiplatelet part of the regimen continued for at least 1 month in patients who received a bare-metal stent and for a year in those who got a drug-eluting stent.
After a year of follow-up, the incidence of the primary end point – total bleeding events – occurred in 20% of the 279 evaluable patients who received dual therapy and in 45% of 284 evaluable patients on triple therapy, a statistically significant difference, reported Dr. Dewilde, a cardiologist at TweeSteden Hospital in Tilberg, the Netherlands. The study’s secondary end point – the combined rate of death, myocardial infarction, target vessel revascularization, stroke, or stent thrombosis – occurred in 11% of patients on double therapy and 18% of those on triple therapy, a statistically significant difference.
Patients on dual therapy had a significantly lower rate of all-cause death, compared with the triple-therapy patients, 3% compared with 6%, and numerically lower levels of stent thrombosis, stroke, and myocardial infarction, although the differences for these individual end points were not statistically significant.
The dual-therapy patients also had significantly lower rates of minimal or minor bleeds, measured by the TIMI (Thrombolysis in Myocardial Infarction) criteria, and the rate of TIMI major bleeds was also lower on dual therapy, but not significantly. The dual-therapy patients had strikingly lower numbers of bleeds at gastrointestinal sites and skin sites, compared with the triple-therapy patients.
"TIMI minimal and minor bleeds are anything but minor from a clinical standpoint," noted Dr. Valgimigli. "Double therapy with clopidogrel and warfarin seems a very reasonable therapy based on WOEST, especially in DES-treated patients."
Dr. Dewilde and Dr. Holmes said that they had no disclosures. Dr. Valgimigli said that he has served on the speakers bureau for AstraZeneca, Eli Lilly, Iroko, and other companies that market vascular devices. He has also been on advisory boards for Eli Lilly, and several companies that make vascular devices. Dr. Smith said that he had no disclosures.
I have participated on committees that made recommendations on managing patients following percutaneous coronary interventions, and for secondary prevention of coronary disease, and in both cases, we realized that there was a major need for a randomized, controlled trial that examined exactly the question addressed by WOEST: What is the best and safest antiplatelet regimen to use on patients who have just received a coronary stent and who require oral anticoagulant therapy because they also have atrial fibrillation, a mechanical valve, or some other indication? Until now, the recommendations we came up with could only be based on expert opinion.
Because the WOEST trial is the first to address this important issue, it will need careful review so that we can decide how it should affect practice. This review will have to closely examine several important issues: Was the WOEST study adequately powered to legitimately address the issues of safety and efficacy in these patients, including the rate of stent thrombosis? Also, we will need to know the international normalized ratio (INR) that these patients maintained throughout the 1-year follow-up of the study. Were there differences in the INRs that could explain the bleeding differences? Another issue is the patient’s age.

|
|
Having data from a good, prospective, controlled trial that looked at the question of how to manage patients who received a coronary stent while on oral anticoagulant therapy is a significant step forward, but it would be premature to make changes in the recommended treatment of patients like these until all elements of the study’s design and findings undergo careful analysis.
Sidney C. Smith, M.D., is a professor of medicine and an interventional cardiologist at the Center for Heart & Vascular Care of the University of North Carolina in Chapel Hill. He chaired the committee of the American Heart Association and American College of Cardiology that issued recommendations for the secondary prevention of coronary disease in 2011 (Circulation 2011;124:2458-73). He said that he had no disclosures. Dr. Smith made these comments in an interview.
What is the Optimal Antiplatelet and Anticoagulant Therapy in Patients with Oral Anticoagulation and Coronary Stenting trial,
I have participated on committees that made recommendations on managing patients following percutaneous coronary interventions, and for secondary prevention of coronary disease, and in both cases, we realized that there was a major need for a randomized, controlled trial that examined exactly the question addressed by WOEST: What is the best and safest antiplatelet regimen to use on patients who have just received a coronary stent and who require oral anticoagulant therapy because they also have atrial fibrillation, a mechanical valve, or some other indication? Until now, the recommendations we came up with could only be based on expert opinion.
Because the WOEST trial is the first to address this important issue, it will need careful review so that we can decide how it should affect practice. This review will have to closely examine several important issues: Was the WOEST study adequately powered to legitimately address the issues of safety and efficacy in these patients, including the rate of stent thrombosis? Also, we will need to know the international normalized ratio (INR) that these patients maintained throughout the 1-year follow-up of the study. Were there differences in the INRs that could explain the bleeding differences? Another issue is the patient’s age.

|
|
Having data from a good, prospective, controlled trial that looked at the question of how to manage patients who received a coronary stent while on oral anticoagulant therapy is a significant step forward, but it would be premature to make changes in the recommended treatment of patients like these until all elements of the study’s design and findings undergo careful analysis.
Sidney C. Smith, M.D., is a professor of medicine and an interventional cardiologist at the Center for Heart & Vascular Care of the University of North Carolina in Chapel Hill. He chaired the committee of the American Heart Association and American College of Cardiology that issued recommendations for the secondary prevention of coronary disease in 2011 (Circulation 2011;124:2458-73). He said that he had no disclosures. Dr. Smith made these comments in an interview.
I have participated on committees that made recommendations on managing patients following percutaneous coronary interventions, and for secondary prevention of coronary disease, and in both cases, we realized that there was a major need for a randomized, controlled trial that examined exactly the question addressed by WOEST: What is the best and safest antiplatelet regimen to use on patients who have just received a coronary stent and who require oral anticoagulant therapy because they also have atrial fibrillation, a mechanical valve, or some other indication? Until now, the recommendations we came up with could only be based on expert opinion.
Because the WOEST trial is the first to address this important issue, it will need careful review so that we can decide how it should affect practice. This review will have to closely examine several important issues: Was the WOEST study adequately powered to legitimately address the issues of safety and efficacy in these patients, including the rate of stent thrombosis? Also, we will need to know the international normalized ratio (INR) that these patients maintained throughout the 1-year follow-up of the study. Were there differences in the INRs that could explain the bleeding differences? Another issue is the patient’s age.

|
|
Having data from a good, prospective, controlled trial that looked at the question of how to manage patients who received a coronary stent while on oral anticoagulant therapy is a significant step forward, but it would be premature to make changes in the recommended treatment of patients like these until all elements of the study’s design and findings undergo careful analysis.
Sidney C. Smith, M.D., is a professor of medicine and an interventional cardiologist at the Center for Heart & Vascular Care of the University of North Carolina in Chapel Hill. He chaired the committee of the American Heart Association and American College of Cardiology that issued recommendations for the secondary prevention of coronary disease in 2011 (Circulation 2011;124:2458-73). He said that he had no disclosures. Dr. Smith made these comments in an interview.
MUNICH – Patients who require chronic oral anticoagulant treatment and received a coronary stent had significantly fewer bleeding events and better outcomes if they received only added clopidogrel than if they were treated with clopidogrel plus aspirin on top of their anticoagulant in the WOEST trial.
As the first study to prospectively test the best combination of antiplatelet drugs to use on top of anticoagulant treatment in patients following coronary stenting, experts hailed the finding as important evidence to address a common and vexing clinical situation.
"We propose that a strategy of oral anticoagulants plus clopidogrel, but without aspirin could be applied in this group of high-risk patients who are on an oral anticoagulant and undergo percutaneous coronary intervention," said Dr. Willem Dewilde, lead investigator for the study, at the Annual Congress of the European Society of Cardiology.
"We are faced with a huge clinical problem, with an increasing number of patients with atrial fibrillation who undergo stent procedures, so this finding has major implications," commented Dr. David R. Holmes Jr., professor of medicine and a cardiologist at the Mayo Clinic in Rochester, Minn. "Bleeding is such a huge issue, and we now have scientific data that says [withholding aspirin] is safe and produces less bleeding."
"The taboo against discontinuing or omitting aspirin has been broken," commented Dr. Marco Valgimigli, director of the coronary catheterization laboratory at the University Hospital of Ferrara (Italy).
The WOEST (What is the Optimal Antiplatelet and Anticoagulant Therapy in Patients with Oral Anticoagulation and Coronary Stenting) trial enrolled 573 patients who required chronic oral anticoagulant treatment and were scheduled for coronary stenting at 15 centers in the Netherlands and Belgium. The patients averaged about 70 years of age, and about 80% were men. A total of 70% received daily, oral treatment with an anticoagulant for atrial fibrillation or flutter, about 10% for a mechanical valve, and the remaining 20% had other reasons for their regimen, including treatment of a pulmonary embolus. All patients received warfarin or another oral anticoagulant such as acenocoumarol. About two-thirds of the patients received a drug-eluting coronary stent, with the remainder receiving a bare-metal stent.
Following stenting, the researchers randomized patients to a regimen of their oral anticoagulant plus 75 mg clopidogrel daily (dual therapy), or their oral anticoagulant, clopidogrel, and 80 mg aspirin daily (triple therapy). The antiplatelet part of the regimen continued for at least 1 month in patients who received a bare-metal stent and for a year in those who got a drug-eluting stent.
After a year of follow-up, the incidence of the primary end point – total bleeding events – occurred in 20% of the 279 evaluable patients who received dual therapy and in 45% of 284 evaluable patients on triple therapy, a statistically significant difference, reported Dr. Dewilde, a cardiologist at TweeSteden Hospital in Tilberg, the Netherlands. The study’s secondary end point – the combined rate of death, myocardial infarction, target vessel revascularization, stroke, or stent thrombosis – occurred in 11% of patients on double therapy and 18% of those on triple therapy, a statistically significant difference.
Patients on dual therapy had a significantly lower rate of all-cause death, compared with the triple-therapy patients, 3% compared with 6%, and numerically lower levels of stent thrombosis, stroke, and myocardial infarction, although the differences for these individual end points were not statistically significant.
The dual-therapy patients also had significantly lower rates of minimal or minor bleeds, measured by the TIMI (Thrombolysis in Myocardial Infarction) criteria, and the rate of TIMI major bleeds was also lower on dual therapy, but not significantly. The dual-therapy patients had strikingly lower numbers of bleeds at gastrointestinal sites and skin sites, compared with the triple-therapy patients.
"TIMI minimal and minor bleeds are anything but minor from a clinical standpoint," noted Dr. Valgimigli. "Double therapy with clopidogrel and warfarin seems a very reasonable therapy based on WOEST, especially in DES-treated patients."
Dr. Dewilde and Dr. Holmes said that they had no disclosures. Dr. Valgimigli said that he has served on the speakers bureau for AstraZeneca, Eli Lilly, Iroko, and other companies that market vascular devices. He has also been on advisory boards for Eli Lilly, and several companies that make vascular devices. Dr. Smith said that he had no disclosures.
MUNICH – Patients who require chronic oral anticoagulant treatment and received a coronary stent had significantly fewer bleeding events and better outcomes if they received only added clopidogrel than if they were treated with clopidogrel plus aspirin on top of their anticoagulant in the WOEST trial.
As the first study to prospectively test the best combination of antiplatelet drugs to use on top of anticoagulant treatment in patients following coronary stenting, experts hailed the finding as important evidence to address a common and vexing clinical situation.
"We propose that a strategy of oral anticoagulants plus clopidogrel, but without aspirin could be applied in this group of high-risk patients who are on an oral anticoagulant and undergo percutaneous coronary intervention," said Dr. Willem Dewilde, lead investigator for the study, at the Annual Congress of the European Society of Cardiology.
"We are faced with a huge clinical problem, with an increasing number of patients with atrial fibrillation who undergo stent procedures, so this finding has major implications," commented Dr. David R. Holmes Jr., professor of medicine and a cardiologist at the Mayo Clinic in Rochester, Minn. "Bleeding is such a huge issue, and we now have scientific data that says [withholding aspirin] is safe and produces less bleeding."
"The taboo against discontinuing or omitting aspirin has been broken," commented Dr. Marco Valgimigli, director of the coronary catheterization laboratory at the University Hospital of Ferrara (Italy).
The WOEST (What is the Optimal Antiplatelet and Anticoagulant Therapy in Patients with Oral Anticoagulation and Coronary Stenting) trial enrolled 573 patients who required chronic oral anticoagulant treatment and were scheduled for coronary stenting at 15 centers in the Netherlands and Belgium. The patients averaged about 70 years of age, and about 80% were men. A total of 70% received daily, oral treatment with an anticoagulant for atrial fibrillation or flutter, about 10% for a mechanical valve, and the remaining 20% had other reasons for their regimen, including treatment of a pulmonary embolus. All patients received warfarin or another oral anticoagulant such as acenocoumarol. About two-thirds of the patients received a drug-eluting coronary stent, with the remainder receiving a bare-metal stent.
Following stenting, the researchers randomized patients to a regimen of their oral anticoagulant plus 75 mg clopidogrel daily (dual therapy), or their oral anticoagulant, clopidogrel, and 80 mg aspirin daily (triple therapy). The antiplatelet part of the regimen continued for at least 1 month in patients who received a bare-metal stent and for a year in those who got a drug-eluting stent.
After a year of follow-up, the incidence of the primary end point – total bleeding events – occurred in 20% of the 279 evaluable patients who received dual therapy and in 45% of 284 evaluable patients on triple therapy, a statistically significant difference, reported Dr. Dewilde, a cardiologist at TweeSteden Hospital in Tilberg, the Netherlands. The study’s secondary end point – the combined rate of death, myocardial infarction, target vessel revascularization, stroke, or stent thrombosis – occurred in 11% of patients on double therapy and 18% of those on triple therapy, a statistically significant difference.
Patients on dual therapy had a significantly lower rate of all-cause death, compared with the triple-therapy patients, 3% compared with 6%, and numerically lower levels of stent thrombosis, stroke, and myocardial infarction, although the differences for these individual end points were not statistically significant.
The dual-therapy patients also had significantly lower rates of minimal or minor bleeds, measured by the TIMI (Thrombolysis in Myocardial Infarction) criteria, and the rate of TIMI major bleeds was also lower on dual therapy, but not significantly. The dual-therapy patients had strikingly lower numbers of bleeds at gastrointestinal sites and skin sites, compared with the triple-therapy patients.
"TIMI minimal and minor bleeds are anything but minor from a clinical standpoint," noted Dr. Valgimigli. "Double therapy with clopidogrel and warfarin seems a very reasonable therapy based on WOEST, especially in DES-treated patients."
Dr. Dewilde and Dr. Holmes said that they had no disclosures. Dr. Valgimigli said that he has served on the speakers bureau for AstraZeneca, Eli Lilly, Iroko, and other companies that market vascular devices. He has also been on advisory boards for Eli Lilly, and several companies that make vascular devices. Dr. Smith said that he had no disclosures.
What is the Optimal Antiplatelet and Anticoagulant Therapy in Patients with Oral Anticoagulation and Coronary Stenting trial,
What is the Optimal Antiplatelet and Anticoagulant Therapy in Patients with Oral Anticoagulation and Coronary Stenting trial,
AT THE ANNUAL CONGRESS OF THE EUROPEAN SOCIETY OF CARDIOLOGY
Major Finding: In coronary-stented patients on oral anticoagulation, bleeds occurred in 20% on clopidogrel only and 45% on clopidogrel and aspirin.
Data Source: Data came from the WOEST study, which randomized 573 patients at 15 centers in the Netherlands and Belgium and followed them for 1 year.
Disclosures: Dr. Dewilde said that he and his associates on the WOEST study had no disclosures. Dr. Holmes said that he had no disclosures. Dr. Dr. Valgimigli said that he has served on the speakers bureau for AstraZeneca, Eli Lilly, Iroko, and other companies that market vascular devices. He has also been on advisory boards for Eli Lilly and several companies that make vascular devices
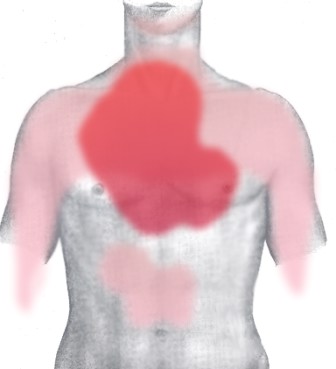
Stilling a Stroke Patient's Beating Heart
A racing heart may suggest pleasurable excitement, but the medical reality is that high heart rate can trigger hypertension and cardiovascular disease. Now, evidence for the first time also implicates a high number of beats per minutes in recent stroke patients in causing increased mortality, disability, and cognitive decline.
Although the new findings come from a post-hoc analysis of a big study, with about 20,000 patients, and so can’t be considered definitive, the strong suggestion that stroke patients with high heart rates have a significantly increased risk of death, reduced functional capacity, and dementia should pave the way for a prospective, controlled intervention trial.
When the results of the new analysis were reported last month at the annual congress of the European Society of Cardiology (and simultaneously published), it sounded like the next step would be a clinical trial designed to look at the outcomes of stroke patients who receive ivabradine, a drug that can safely and specifically slow heart rate.
To study the implications of a high heart rate in stroke patients, Dr. Michael Böhm and his associates analyzed data from 20,165 patients who had been enrolled in a treatment trial within 4 months after an ischemic stroke. That study, the Prevention Regimen for Effectively Avoiding Second Stroke trial, was designed to assess the benefit of anti-ischemia treatments and had no interventions that affected heart rate, so it conveniently provided a large database of stroke patients who had their heart rates measured at baseline and then were closely followed.
The results showed that stroke patients with initial heart rates above 76 beats per minute, when compared with those whose heart rates were 64 beats per minute or less, had a better than 50% increased risk of dying over the following 2.5 years; an increased rate of disability, as measured by the modified Rankin scale and the Barthel index at 3 months after entry; and increased dementia, as measured by the Mini Mental State Exam, at both 1 month and later following enrollment.
The findings "provide unique and intriguing findings, that heart rate predicts post-stroke physical and cognitive disability," Dr. Jeffrey S. Borer noted in a commentary he delivered at the meeting.
And the prevalence of stroke patients with a heart rate that high wasn’t small: 40% of the 20,000 patients examined reached that threshold. Twenty percent of the studied patients had a heart rate of 64 beats per minute or slower.
The way to potentially address this clinical need is to test whether slowing heart rate with ivabradine helps outcomes. Two years ago, at the same meeting, researchers reported using ivabradine to improve the outcomes of heart failure patients. The efficacy and safety results were persuasive enough that the newly revised heart-failure management recommendations of the European Society of Cardiology include ivabradine in its treatment algorhythm.
"Randomized, controlled trials of [ivabradine] in stroke survivors ... may be warranted," concluded the editorial that accompanied the published version of the new report.
–Mitchel Zoler (on Twitter @mitchelzoler)
A racing heart may suggest pleasurable excitement, but the medical reality is that high heart rate can trigger hypertension and cardiovascular disease. Now, evidence for the first time also implicates a high number of beats per minutes in recent stroke patients in causing increased mortality, disability, and cognitive decline.
Although the new findings come from a post-hoc analysis of a big study, with about 20,000 patients, and so can’t be considered definitive, the strong suggestion that stroke patients with high heart rates have a significantly increased risk of death, reduced functional capacity, and dementia should pave the way for a prospective, controlled intervention trial.
When the results of the new analysis were reported last month at the annual congress of the European Society of Cardiology (and simultaneously published), it sounded like the next step would be a clinical trial designed to look at the outcomes of stroke patients who receive ivabradine, a drug that can safely and specifically slow heart rate.
To study the implications of a high heart rate in stroke patients, Dr. Michael Böhm and his associates analyzed data from 20,165 patients who had been enrolled in a treatment trial within 4 months after an ischemic stroke. That study, the Prevention Regimen for Effectively Avoiding Second Stroke trial, was designed to assess the benefit of anti-ischemia treatments and had no interventions that affected heart rate, so it conveniently provided a large database of stroke patients who had their heart rates measured at baseline and then were closely followed.
The results showed that stroke patients with initial heart rates above 76 beats per minute, when compared with those whose heart rates were 64 beats per minute or less, had a better than 50% increased risk of dying over the following 2.5 years; an increased rate of disability, as measured by the modified Rankin scale and the Barthel index at 3 months after entry; and increased dementia, as measured by the Mini Mental State Exam, at both 1 month and later following enrollment.
The findings "provide unique and intriguing findings, that heart rate predicts post-stroke physical and cognitive disability," Dr. Jeffrey S. Borer noted in a commentary he delivered at the meeting.
And the prevalence of stroke patients with a heart rate that high wasn’t small: 40% of the 20,000 patients examined reached that threshold. Twenty percent of the studied patients had a heart rate of 64 beats per minute or slower.
The way to potentially address this clinical need is to test whether slowing heart rate with ivabradine helps outcomes. Two years ago, at the same meeting, researchers reported using ivabradine to improve the outcomes of heart failure patients. The efficacy and safety results were persuasive enough that the newly revised heart-failure management recommendations of the European Society of Cardiology include ivabradine in its treatment algorhythm.
"Randomized, controlled trials of [ivabradine] in stroke survivors ... may be warranted," concluded the editorial that accompanied the published version of the new report.
–Mitchel Zoler (on Twitter @mitchelzoler)
A racing heart may suggest pleasurable excitement, but the medical reality is that high heart rate can trigger hypertension and cardiovascular disease. Now, evidence for the first time also implicates a high number of beats per minutes in recent stroke patients in causing increased mortality, disability, and cognitive decline.
Although the new findings come from a post-hoc analysis of a big study, with about 20,000 patients, and so can’t be considered definitive, the strong suggestion that stroke patients with high heart rates have a significantly increased risk of death, reduced functional capacity, and dementia should pave the way for a prospective, controlled intervention trial.
When the results of the new analysis were reported last month at the annual congress of the European Society of Cardiology (and simultaneously published), it sounded like the next step would be a clinical trial designed to look at the outcomes of stroke patients who receive ivabradine, a drug that can safely and specifically slow heart rate.
To study the implications of a high heart rate in stroke patients, Dr. Michael Böhm and his associates analyzed data from 20,165 patients who had been enrolled in a treatment trial within 4 months after an ischemic stroke. That study, the Prevention Regimen for Effectively Avoiding Second Stroke trial, was designed to assess the benefit of anti-ischemia treatments and had no interventions that affected heart rate, so it conveniently provided a large database of stroke patients who had their heart rates measured at baseline and then were closely followed.
The results showed that stroke patients with initial heart rates above 76 beats per minute, when compared with those whose heart rates were 64 beats per minute or less, had a better than 50% increased risk of dying over the following 2.5 years; an increased rate of disability, as measured by the modified Rankin scale and the Barthel index at 3 months after entry; and increased dementia, as measured by the Mini Mental State Exam, at both 1 month and later following enrollment.
The findings "provide unique and intriguing findings, that heart rate predicts post-stroke physical and cognitive disability," Dr. Jeffrey S. Borer noted in a commentary he delivered at the meeting.
And the prevalence of stroke patients with a heart rate that high wasn’t small: 40% of the 20,000 patients examined reached that threshold. Twenty percent of the studied patients had a heart rate of 64 beats per minute or slower.
The way to potentially address this clinical need is to test whether slowing heart rate with ivabradine helps outcomes. Two years ago, at the same meeting, researchers reported using ivabradine to improve the outcomes of heart failure patients. The efficacy and safety results were persuasive enough that the newly revised heart-failure management recommendations of the European Society of Cardiology include ivabradine in its treatment algorhythm.
"Randomized, controlled trials of [ivabradine] in stroke survivors ... may be warranted," concluded the editorial that accompanied the published version of the new report.
–Mitchel Zoler (on Twitter @mitchelzoler)
Real-World TAVI Outcomes Spot On With Clinical Trial Results
MUNICH – In-hospital mortality and complications following transcatheter aortic valve implantation in the real-world setting are comparable with those achieved in randomized controlled studies, according to data from the first large-scale national registry capturing surgical and catheter-based procedures.
"In high-risk patients, the in-hospital mortality with TAVI is at least as good, if not better, as with the surgical approach," said Dr. Christian Hamm, who presented data from 13,860 patients in the German Aortic Valve Registry (GARY during a hotline session at the annual congress of the European Society of Cardiology.
In-hospital mortality was 2.2% for conventional aortic valve replacement surgery alone, 4.6% for conventional surgery with coronary artery bypass grafting (CABG), 5.5% for TAVI using a transvascular approach, and 7.8% for TAVI with a transapical approach.
After adjusting for the expected higher risk profile of TAVI patients, the risk of in-hospital death was not increased with transvascular TAVI, compared with surgery alone, although there was a trend toward increased risk with transapical TAVI in both younger patients and those aged 75 years and older, said Dr. Hamm, medical director of the Kerckhoff Heart and Thorax Centre, Bad Nauheim, Germany.
When asked by the media whether the higher mortality may be diminishing use of the transapical approach, GARY coauthor Dr. Friedrich-Wilhelm Mohr said that similar rates have been seen in the source registry and that these patients tend to have slightly more comorbidities and vascular disease.
"The current data in 2012 do not show a pull back," said Dr. Mohr, medical director of the Leipzig (Germany) Heart Center. "It’s almost the same situation as here: two-thirds transfemoral and one-third transapical."
Consistent with earlier observations, the rate of cerebrovascular events was lowest in patients undergoing surgery without CABG at 2.2% and was "in the range of 3.5%" for all other groups, Dr. Hamm reported.
Discussant Dr. Olaf Wendler said it’s convincing that cerebrovascular complications are lower than in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial, which reported a 5% major stroke rate among TAVI patients at 30 days.
"This may be less of a problem than we thought about transcatheter-valve treatment in the past," he said. "However, again we don’t have all the details, definitions of the adverse events, and we don’t have a clear idea of how adverse events were adjudicated in this registry."
Rates of vascular complications and new onset atrioventricular (AV) blockage were highest after transvascular TAVI, while renal failure was most common after the transapical approach, said Dr. Wendler, professor at King’s College Hospital in London.
Specifically, vascular complications were reported in 12% of transvascular patients, compared with 2.5% for the transapical approach, 2% for surgery plus CABG, and 1% for surgery alone.
Residual postimplant aortic regurgitation, which has been linked to long-term TAVI outcome, "seemed to be excellent because more than 90% of patients had no or grade I regurgitation," Dr. Hamm said. Only 7% of transvascular and 3% of transapical patients had grade II regurgitation, and only 1% of transapical and no transvascular patients had grade III or IV regurgitation.
Although between-valve comparisons were limited since the CoreValve was not implanted transapically, grade I or II aortic regurgitation was more common with the CoreValve (70%) than with the Edwards prosthesis (45.7%).
Despite the increasing shift of TAVI in lower-risk patients, data from GARY show that TAVI is being performed predominantly in high-risk patients, as recommended in various guidelines, Dr. Hamm said.
Participation in GARY is voluntary, with 92 of 99 German centers currently taking part. As of July 2012, more than 26,000 patients were included, of whom 23% were TAVI patients.
The current analysis included 13,860 patients from 53 cardiac surgery units and 69 cardiology units. Of these patients, 6,523 underwent surgery alone, 3,462 surgery plus CABG, 2,694 transvascular TAVI, and 1,181 transapical TAVI.
At baseline, TAVI patients were significantly older than surgical patients (average of 81 years transvascular and 80.3 years transapical vs. 68 years surgical); had significantly more comorbidities including atrial fibrillation, hypertension, and diabetes; and were significantly more likely to have a left ventricular ejection fraction below 30%.
Roughly half of elderly patients more than 75 years of age now receive TAVI in Germany, which is quite impressive and by far a higher number than any other country worldwide, said Dr. Wendler.
German investigators also have developed a novel risk scoring system called the AKL score, which, unlike the logistic EuroSCORE or Society of Thoracic Surgeons (STS) risk score, is based only on patients with aortic valve disease.
"The EuroSCORE, as many of us know, is not very suitable in this scenario," Dr. Hamm said.
When the GARY authors compared observed vs. expected in-hospital mortality based on patients’ EuroSCORE, the observed risk for mortality was much lower than predicted by the EuroSCORE.
When the same analysis was performed using the AKL score, however, the observed and expected mortality outcomes were very similar, suggesting the "AKL score much better reflects the real outcome of the patients," he said.
Dr. Wendler remarked that in low-risk patients, however, the observed in-hospital mortality was higher than what was predicted, "questioning if this is the right treatment for this group of patients."
GARY is supported by the German Heart Foundation and unrestricted grants from heart valve manufacturers. Dr. Hamm disclosed honoraria from Medtronic and Edwards Lifesciences and participation in clinical trials with Medtronic, Edwards, Symetis, and JenaValve. Dr. Mohr reported no conflicts of interest. Dr. Wendler reported research ties with Edwards and consulting for Edwards and St. Jude Medical.
MUNICH – In-hospital mortality and complications following transcatheter aortic valve implantation in the real-world setting are comparable with those achieved in randomized controlled studies, according to data from the first large-scale national registry capturing surgical and catheter-based procedures.
"In high-risk patients, the in-hospital mortality with TAVI is at least as good, if not better, as with the surgical approach," said Dr. Christian Hamm, who presented data from 13,860 patients in the German Aortic Valve Registry (GARY during a hotline session at the annual congress of the European Society of Cardiology.
In-hospital mortality was 2.2% for conventional aortic valve replacement surgery alone, 4.6% for conventional surgery with coronary artery bypass grafting (CABG), 5.5% for TAVI using a transvascular approach, and 7.8% for TAVI with a transapical approach.
After adjusting for the expected higher risk profile of TAVI patients, the risk of in-hospital death was not increased with transvascular TAVI, compared with surgery alone, although there was a trend toward increased risk with transapical TAVI in both younger patients and those aged 75 years and older, said Dr. Hamm, medical director of the Kerckhoff Heart and Thorax Centre, Bad Nauheim, Germany.
When asked by the media whether the higher mortality may be diminishing use of the transapical approach, GARY coauthor Dr. Friedrich-Wilhelm Mohr said that similar rates have been seen in the source registry and that these patients tend to have slightly more comorbidities and vascular disease.
"The current data in 2012 do not show a pull back," said Dr. Mohr, medical director of the Leipzig (Germany) Heart Center. "It’s almost the same situation as here: two-thirds transfemoral and one-third transapical."
Consistent with earlier observations, the rate of cerebrovascular events was lowest in patients undergoing surgery without CABG at 2.2% and was "in the range of 3.5%" for all other groups, Dr. Hamm reported.
Discussant Dr. Olaf Wendler said it’s convincing that cerebrovascular complications are lower than in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial, which reported a 5% major stroke rate among TAVI patients at 30 days.
"This may be less of a problem than we thought about transcatheter-valve treatment in the past," he said. "However, again we don’t have all the details, definitions of the adverse events, and we don’t have a clear idea of how adverse events were adjudicated in this registry."
Rates of vascular complications and new onset atrioventricular (AV) blockage were highest after transvascular TAVI, while renal failure was most common after the transapical approach, said Dr. Wendler, professor at King’s College Hospital in London.
Specifically, vascular complications were reported in 12% of transvascular patients, compared with 2.5% for the transapical approach, 2% for surgery plus CABG, and 1% for surgery alone.
Residual postimplant aortic regurgitation, which has been linked to long-term TAVI outcome, "seemed to be excellent because more than 90% of patients had no or grade I regurgitation," Dr. Hamm said. Only 7% of transvascular and 3% of transapical patients had grade II regurgitation, and only 1% of transapical and no transvascular patients had grade III or IV regurgitation.
Although between-valve comparisons were limited since the CoreValve was not implanted transapically, grade I or II aortic regurgitation was more common with the CoreValve (70%) than with the Edwards prosthesis (45.7%).
Despite the increasing shift of TAVI in lower-risk patients, data from GARY show that TAVI is being performed predominantly in high-risk patients, as recommended in various guidelines, Dr. Hamm said.
Participation in GARY is voluntary, with 92 of 99 German centers currently taking part. As of July 2012, more than 26,000 patients were included, of whom 23% were TAVI patients.
The current analysis included 13,860 patients from 53 cardiac surgery units and 69 cardiology units. Of these patients, 6,523 underwent surgery alone, 3,462 surgery plus CABG, 2,694 transvascular TAVI, and 1,181 transapical TAVI.
At baseline, TAVI patients were significantly older than surgical patients (average of 81 years transvascular and 80.3 years transapical vs. 68 years surgical); had significantly more comorbidities including atrial fibrillation, hypertension, and diabetes; and were significantly more likely to have a left ventricular ejection fraction below 30%.
Roughly half of elderly patients more than 75 years of age now receive TAVI in Germany, which is quite impressive and by far a higher number than any other country worldwide, said Dr. Wendler.
German investigators also have developed a novel risk scoring system called the AKL score, which, unlike the logistic EuroSCORE or Society of Thoracic Surgeons (STS) risk score, is based only on patients with aortic valve disease.
"The EuroSCORE, as many of us know, is not very suitable in this scenario," Dr. Hamm said.
When the GARY authors compared observed vs. expected in-hospital mortality based on patients’ EuroSCORE, the observed risk for mortality was much lower than predicted by the EuroSCORE.
When the same analysis was performed using the AKL score, however, the observed and expected mortality outcomes were very similar, suggesting the "AKL score much better reflects the real outcome of the patients," he said.
Dr. Wendler remarked that in low-risk patients, however, the observed in-hospital mortality was higher than what was predicted, "questioning if this is the right treatment for this group of patients."
GARY is supported by the German Heart Foundation and unrestricted grants from heart valve manufacturers. Dr. Hamm disclosed honoraria from Medtronic and Edwards Lifesciences and participation in clinical trials with Medtronic, Edwards, Symetis, and JenaValve. Dr. Mohr reported no conflicts of interest. Dr. Wendler reported research ties with Edwards and consulting for Edwards and St. Jude Medical.
MUNICH – In-hospital mortality and complications following transcatheter aortic valve implantation in the real-world setting are comparable with those achieved in randomized controlled studies, according to data from the first large-scale national registry capturing surgical and catheter-based procedures.
"In high-risk patients, the in-hospital mortality with TAVI is at least as good, if not better, as with the surgical approach," said Dr. Christian Hamm, who presented data from 13,860 patients in the German Aortic Valve Registry (GARY during a hotline session at the annual congress of the European Society of Cardiology.
In-hospital mortality was 2.2% for conventional aortic valve replacement surgery alone, 4.6% for conventional surgery with coronary artery bypass grafting (CABG), 5.5% for TAVI using a transvascular approach, and 7.8% for TAVI with a transapical approach.
After adjusting for the expected higher risk profile of TAVI patients, the risk of in-hospital death was not increased with transvascular TAVI, compared with surgery alone, although there was a trend toward increased risk with transapical TAVI in both younger patients and those aged 75 years and older, said Dr. Hamm, medical director of the Kerckhoff Heart and Thorax Centre, Bad Nauheim, Germany.
When asked by the media whether the higher mortality may be diminishing use of the transapical approach, GARY coauthor Dr. Friedrich-Wilhelm Mohr said that similar rates have been seen in the source registry and that these patients tend to have slightly more comorbidities and vascular disease.
"The current data in 2012 do not show a pull back," said Dr. Mohr, medical director of the Leipzig (Germany) Heart Center. "It’s almost the same situation as here: two-thirds transfemoral and one-third transapical."
Consistent with earlier observations, the rate of cerebrovascular events was lowest in patients undergoing surgery without CABG at 2.2% and was "in the range of 3.5%" for all other groups, Dr. Hamm reported.
Discussant Dr. Olaf Wendler said it’s convincing that cerebrovascular complications are lower than in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial, which reported a 5% major stroke rate among TAVI patients at 30 days.
"This may be less of a problem than we thought about transcatheter-valve treatment in the past," he said. "However, again we don’t have all the details, definitions of the adverse events, and we don’t have a clear idea of how adverse events were adjudicated in this registry."
Rates of vascular complications and new onset atrioventricular (AV) blockage were highest after transvascular TAVI, while renal failure was most common after the transapical approach, said Dr. Wendler, professor at King’s College Hospital in London.
Specifically, vascular complications were reported in 12% of transvascular patients, compared with 2.5% for the transapical approach, 2% for surgery plus CABG, and 1% for surgery alone.
Residual postimplant aortic regurgitation, which has been linked to long-term TAVI outcome, "seemed to be excellent because more than 90% of patients had no or grade I regurgitation," Dr. Hamm said. Only 7% of transvascular and 3% of transapical patients had grade II regurgitation, and only 1% of transapical and no transvascular patients had grade III or IV regurgitation.
Although between-valve comparisons were limited since the CoreValve was not implanted transapically, grade I or II aortic regurgitation was more common with the CoreValve (70%) than with the Edwards prosthesis (45.7%).
Despite the increasing shift of TAVI in lower-risk patients, data from GARY show that TAVI is being performed predominantly in high-risk patients, as recommended in various guidelines, Dr. Hamm said.
Participation in GARY is voluntary, with 92 of 99 German centers currently taking part. As of July 2012, more than 26,000 patients were included, of whom 23% were TAVI patients.
The current analysis included 13,860 patients from 53 cardiac surgery units and 69 cardiology units. Of these patients, 6,523 underwent surgery alone, 3,462 surgery plus CABG, 2,694 transvascular TAVI, and 1,181 transapical TAVI.
At baseline, TAVI patients were significantly older than surgical patients (average of 81 years transvascular and 80.3 years transapical vs. 68 years surgical); had significantly more comorbidities including atrial fibrillation, hypertension, and diabetes; and were significantly more likely to have a left ventricular ejection fraction below 30%.
Roughly half of elderly patients more than 75 years of age now receive TAVI in Germany, which is quite impressive and by far a higher number than any other country worldwide, said Dr. Wendler.
German investigators also have developed a novel risk scoring system called the AKL score, which, unlike the logistic EuroSCORE or Society of Thoracic Surgeons (STS) risk score, is based only on patients with aortic valve disease.
"The EuroSCORE, as many of us know, is not very suitable in this scenario," Dr. Hamm said.
When the GARY authors compared observed vs. expected in-hospital mortality based on patients’ EuroSCORE, the observed risk for mortality was much lower than predicted by the EuroSCORE.
When the same analysis was performed using the AKL score, however, the observed and expected mortality outcomes were very similar, suggesting the "AKL score much better reflects the real outcome of the patients," he said.
Dr. Wendler remarked that in low-risk patients, however, the observed in-hospital mortality was higher than what was predicted, "questioning if this is the right treatment for this group of patients."
GARY is supported by the German Heart Foundation and unrestricted grants from heart valve manufacturers. Dr. Hamm disclosed honoraria from Medtronic and Edwards Lifesciences and participation in clinical trials with Medtronic, Edwards, Symetis, and JenaValve. Dr. Mohr reported no conflicts of interest. Dr. Wendler reported research ties with Edwards and consulting for Edwards and St. Jude Medical.
AT THE ANNUAL CONGRESS OF THE EUROPEAN SOCIETY OF CARDIOLOGY
Major Finding: In-hospital mortality was 2.2% for conventional aortic valve replacement surgery, 4.6% for conventional surgery with coronary artery bypass grafting, 5.5% for transvascular TAVI, and 7.8% for transapical TAVI.
Data Source: Data are from 13,860 patients treated with TAVI in 2011 in the German Aortic Valve Registry.
Disclosures: GARY is supported by the German Heart Foundation and unrestricted grants from heart valve manufacturers. Dr. Hamm disclosed honoraria from Medtronic and Edwards Lifesciences and participation in clinical trials with Medtronic, Edwards, Symetis, and JenaValve. Dr. Mohr reported no conflicts of interest. Dr. Wendler reported research ties with Edwards and consulting for Edwards and St. Jude Medical.
Unstable Angina, We Hardly Knew Ye
Unstable angina died last week, at the European Society of Cardiology’s annual Congress in Munich.
The term "unstable angina" was 41 years old, and is survived by its close sibling, non–ST-segment elevation myocardial infarction (NSTEMI). The cause of death was increasing reliance on high-sensitivity (hs) cardiac troponin assays and the Third Universal Definition of MI that was released last week, and was in part designed to address the shifting acute coronary syndrome landscape created by hs cardiac troponin assays.
Cardiologists first coined unstable angina in 1971 and, in the years following, applied it to hundreds of thousands of patients annually, patients with chest pain caused by acute, ischemic cardiac episodes that failed to produce the electrocardiogram change – an ST-segment elevation – that is the hallmark of a full-blown myocardial infarction.
Over time, increased sophistication in the ability of cardiologists to discern cardiac pathology led to the term NSTEMI; as recently as last year, official cardiology diagnostic guidelines considered unstable angina and NSTEMI virtual twins. The distinction was that NSTEMI produced a measurable, pathognomonic rise in serum levels of cardiac troponin or other serum markers of cardiac damage, with no such rise discernable in unstable angina patients.
The Third Universal Definition changed that. As explained by Professor Freek Verheugt, a Dutch cardiologist who commented on the implications of the new definition last week at the ESC meeting, the new definition’s official adoption of hs cardiac troponin levels as the gold standard for myocardial infarction diagnosis left unstable angina in limbo. It had "disappeared," he said.
"If hs troponins are completely neutral in a patient with chest pain, it’s impossible that the patient has significant coronary disease," he explained to me in an interview. "They therefore have some other condition causing the chest pain. Troponin tests are so sensitive now that they exclude a cardiac cause" when no rise occurs.
In other words, patients with acute chest pain, no ST-segment elevation, and a discernable rise in hs cardiac troponin have NSTEMI. Patients with acute chest pain, no ST-segment elevation, and no rise in their hs cardiac troponin level must have a noncardiac cause for their pain.
Unstable angina, R.I.P.
–Mitchel Zoler (on Twitter @mitchelzoler)
Unstable angina died last week, at the European Society of Cardiology’s annual Congress in Munich.
The term "unstable angina" was 41 years old, and is survived by its close sibling, non–ST-segment elevation myocardial infarction (NSTEMI). The cause of death was increasing reliance on high-sensitivity (hs) cardiac troponin assays and the Third Universal Definition of MI that was released last week, and was in part designed to address the shifting acute coronary syndrome landscape created by hs cardiac troponin assays.
Cardiologists first coined unstable angina in 1971 and, in the years following, applied it to hundreds of thousands of patients annually, patients with chest pain caused by acute, ischemic cardiac episodes that failed to produce the electrocardiogram change – an ST-segment elevation – that is the hallmark of a full-blown myocardial infarction.
Over time, increased sophistication in the ability of cardiologists to discern cardiac pathology led to the term NSTEMI; as recently as last year, official cardiology diagnostic guidelines considered unstable angina and NSTEMI virtual twins. The distinction was that NSTEMI produced a measurable, pathognomonic rise in serum levels of cardiac troponin or other serum markers of cardiac damage, with no such rise discernable in unstable angina patients.
The Third Universal Definition changed that. As explained by Professor Freek Verheugt, a Dutch cardiologist who commented on the implications of the new definition last week at the ESC meeting, the new definition’s official adoption of hs cardiac troponin levels as the gold standard for myocardial infarction diagnosis left unstable angina in limbo. It had "disappeared," he said.
"If hs troponins are completely neutral in a patient with chest pain, it’s impossible that the patient has significant coronary disease," he explained to me in an interview. "They therefore have some other condition causing the chest pain. Troponin tests are so sensitive now that they exclude a cardiac cause" when no rise occurs.
In other words, patients with acute chest pain, no ST-segment elevation, and a discernable rise in hs cardiac troponin have NSTEMI. Patients with acute chest pain, no ST-segment elevation, and no rise in their hs cardiac troponin level must have a noncardiac cause for their pain.
Unstable angina, R.I.P.
–Mitchel Zoler (on Twitter @mitchelzoler)
Unstable angina died last week, at the European Society of Cardiology’s annual Congress in Munich.
The term "unstable angina" was 41 years old, and is survived by its close sibling, non–ST-segment elevation myocardial infarction (NSTEMI). The cause of death was increasing reliance on high-sensitivity (hs) cardiac troponin assays and the Third Universal Definition of MI that was released last week, and was in part designed to address the shifting acute coronary syndrome landscape created by hs cardiac troponin assays.
Cardiologists first coined unstable angina in 1971 and, in the years following, applied it to hundreds of thousands of patients annually, patients with chest pain caused by acute, ischemic cardiac episodes that failed to produce the electrocardiogram change – an ST-segment elevation – that is the hallmark of a full-blown myocardial infarction.
Over time, increased sophistication in the ability of cardiologists to discern cardiac pathology led to the term NSTEMI; as recently as last year, official cardiology diagnostic guidelines considered unstable angina and NSTEMI virtual twins. The distinction was that NSTEMI produced a measurable, pathognomonic rise in serum levels of cardiac troponin or other serum markers of cardiac damage, with no such rise discernable in unstable angina patients.
The Third Universal Definition changed that. As explained by Professor Freek Verheugt, a Dutch cardiologist who commented on the implications of the new definition last week at the ESC meeting, the new definition’s official adoption of hs cardiac troponin levels as the gold standard for myocardial infarction diagnosis left unstable angina in limbo. It had "disappeared," he said.
"If hs troponins are completely neutral in a patient with chest pain, it’s impossible that the patient has significant coronary disease," he explained to me in an interview. "They therefore have some other condition causing the chest pain. Troponin tests are so sensitive now that they exclude a cardiac cause" when no rise occurs.
In other words, patients with acute chest pain, no ST-segment elevation, and a discernable rise in hs cardiac troponin have NSTEMI. Patients with acute chest pain, no ST-segment elevation, and no rise in their hs cardiac troponin level must have a noncardiac cause for their pain.
Unstable angina, R.I.P.
–Mitchel Zoler (on Twitter @mitchelzoler)
GRACE: Insulin Glargine Fails to Halt Atherosclerosis Progression
MUNICH – Insulin glargine and omega-3 fatty acids failed to retard carotid atherosclerosis progression in patients with diabetes or prediabetes at high cardiovascular risk in the GRACE trial.
Compared with standard glycemic care, insulin glargine provided a nonsignificant difference of –0.0030 mm/year in the primary end point of rate of change in maximum carotid intima media thickness (CIMT) at 12 carotid sites.
For the secondary outcomes, which included four segments of the common carotid artery and eight segments of the common carotid and bifurcation sites, the long-acting basal insulin resulted in slight but statistically significant annualized differences in maximum CIMT of –0.0033 mm/year and –0.0045 mm/year, respectively.
"Although not conclusive, our study suggests a beneficial effect of insulin glargine on vascular disease progression," Dr. Eva Lonn said at the annual congress of the European Society of Cardiology. "These findings raise the possibility that longer term treatment might result in cardiovascular event reduction."
This hypothesis is currently under evaluation in extended follow-up of ORIGIN (Outcome Reduction With an Initial Glargine Intervention), the parent trial of GRACE (Glucose Reduction and Atherosclerosis Continuing Evaluation).
With regard to omega-3 fatty acids, no significant differences were observed for the primary outcome (difference 0.0009 mm/yr), or the secondary outcomes in the common carotid (–0.0004 mm/yr) and common carotid and bifurcation sites (0.0022 mm/year), reported Dr. Lonn, professor of medicine at McMaster University and director of the vascular research ultrasound laboratory at the Population Health Research Institute, both in Hamilton, Ontario.
Given the neutral effect of omega-3 fatty acids, the focus in diabetes should be on proven therapies such as lipid-lowering and blood pressure–lowering drugs and glycemic control, she said in an interview. There is no harm, however, should patients wish to take the supplements.
Discussant John E. Deanfield said there was no evidence of benefit or harm from either treatment, and pointed out that the results of GRACE are concordant with those reported from the larger ORIGIN trial.
In that trial, insulin glargine reduced the risk of developing type 2 diabetes by 28% among patients with prediabetes, but had a neutral effect on cardiovascular outcomes (N. Engl. J. Med. 2012;367:319-28). Omega-3 fatty acids reduced triglyceride levels, but also failed to reduce the rate of cardiovascular events (N. Engl. J. Med. 2012;367:309-18).
After a median clinical follow up of 6.2 years in GRACE, Dr. Lonn reported that rates of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke were similar between the insulin glargine and standard care groups (18.6% vs. 16.9%), as was all-cause mortality (17.1% vs. 17.4%).
Dr. Deanfield said the lack of benefit from either treatment was disappointing and suggested the GRACE authors might have been better served by choosing the common carotid segment as their primary outcome, rather than one of their secondary outcomes.
He also noted that there is controversy over whether IMT itself is the best measure of structural arterial disease, with a recent meta-analysis demonstrating a lack of relationship between progression of CIMT and hazard for cardiovascular events (Lancet 2012;379:2053-62).
"Finally, the reporting strategy for IMT in this trial – which shows the change in IMT levels over 5 years without giving us, as yet, the baseline absolute levels of IMT – is interesting and might be missing a trick in terms of our understanding of this signal," said Dr. Deanfield, professor of cardiology at University College London.
A total of 1,184 patients recruited from 32 centers in seven countries received open-label insulin glargine injection or standard glycemic care, and double-blinded therapy with a 1-g/day omega-3 supplement containing eicosapentaenoic acid 465 mg plus docosahexaenoic acid 375 mg or matching placebo.
Patients had to be at least 50 years old (mean age 63 years) and have prediabetes or newly diagnosed type 2 diabetes or early type 2 diabetes, and be at high cardiovascular risk.
At baseline, 49% had a history of cardiovascular disease, 80% had hypertension, 60% had hyperlipidemia and 10% were current smokers. CIMT efficacy results were based on 1,091 patients with at least one adequate carotid ultrasound. Median follow-up from baseline to last CIMT scan was 5 years.
Insulin glargine was well tolerated and safe, with the most common reasons for discontinuation being patient preference in 76 patients and hypoglycemia in 9, Dr. Lonn said.
The study was funded by Sanofi; omega-3 fatty acid supplements and matching placebo were provided by Pronova BioPharma. Dr. Lonn reported research grants, lecture fees, and/or consulting fees from Astra-Zeneca, Canadian Institutes of Health Research, GlaxoSmithKline, Heart and Stroke Foundation of Canada, Merck, Novartis, Servier, and Sanofi. Dr. Deanfield reported consulting and speakers bureau participation for Pfizer, Merck, Roche, Takeda, Novartis, Sanofi, and Danone.
MUNICH – Insulin glargine and omega-3 fatty acids failed to retard carotid atherosclerosis progression in patients with diabetes or prediabetes at high cardiovascular risk in the GRACE trial.
Compared with standard glycemic care, insulin glargine provided a nonsignificant difference of –0.0030 mm/year in the primary end point of rate of change in maximum carotid intima media thickness (CIMT) at 12 carotid sites.
For the secondary outcomes, which included four segments of the common carotid artery and eight segments of the common carotid and bifurcation sites, the long-acting basal insulin resulted in slight but statistically significant annualized differences in maximum CIMT of –0.0033 mm/year and –0.0045 mm/year, respectively.
"Although not conclusive, our study suggests a beneficial effect of insulin glargine on vascular disease progression," Dr. Eva Lonn said at the annual congress of the European Society of Cardiology. "These findings raise the possibility that longer term treatment might result in cardiovascular event reduction."
This hypothesis is currently under evaluation in extended follow-up of ORIGIN (Outcome Reduction With an Initial Glargine Intervention), the parent trial of GRACE (Glucose Reduction and Atherosclerosis Continuing Evaluation).
With regard to omega-3 fatty acids, no significant differences were observed for the primary outcome (difference 0.0009 mm/yr), or the secondary outcomes in the common carotid (–0.0004 mm/yr) and common carotid and bifurcation sites (0.0022 mm/year), reported Dr. Lonn, professor of medicine at McMaster University and director of the vascular research ultrasound laboratory at the Population Health Research Institute, both in Hamilton, Ontario.
Given the neutral effect of omega-3 fatty acids, the focus in diabetes should be on proven therapies such as lipid-lowering and blood pressure–lowering drugs and glycemic control, she said in an interview. There is no harm, however, should patients wish to take the supplements.
Discussant John E. Deanfield said there was no evidence of benefit or harm from either treatment, and pointed out that the results of GRACE are concordant with those reported from the larger ORIGIN trial.
In that trial, insulin glargine reduced the risk of developing type 2 diabetes by 28% among patients with prediabetes, but had a neutral effect on cardiovascular outcomes (N. Engl. J. Med. 2012;367:319-28). Omega-3 fatty acids reduced triglyceride levels, but also failed to reduce the rate of cardiovascular events (N. Engl. J. Med. 2012;367:309-18).
After a median clinical follow up of 6.2 years in GRACE, Dr. Lonn reported that rates of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke were similar between the insulin glargine and standard care groups (18.6% vs. 16.9%), as was all-cause mortality (17.1% vs. 17.4%).
Dr. Deanfield said the lack of benefit from either treatment was disappointing and suggested the GRACE authors might have been better served by choosing the common carotid segment as their primary outcome, rather than one of their secondary outcomes.
He also noted that there is controversy over whether IMT itself is the best measure of structural arterial disease, with a recent meta-analysis demonstrating a lack of relationship between progression of CIMT and hazard for cardiovascular events (Lancet 2012;379:2053-62).
"Finally, the reporting strategy for IMT in this trial – which shows the change in IMT levels over 5 years without giving us, as yet, the baseline absolute levels of IMT – is interesting and might be missing a trick in terms of our understanding of this signal," said Dr. Deanfield, professor of cardiology at University College London.
A total of 1,184 patients recruited from 32 centers in seven countries received open-label insulin glargine injection or standard glycemic care, and double-blinded therapy with a 1-g/day omega-3 supplement containing eicosapentaenoic acid 465 mg plus docosahexaenoic acid 375 mg or matching placebo.
Patients had to be at least 50 years old (mean age 63 years) and have prediabetes or newly diagnosed type 2 diabetes or early type 2 diabetes, and be at high cardiovascular risk.
At baseline, 49% had a history of cardiovascular disease, 80% had hypertension, 60% had hyperlipidemia and 10% were current smokers. CIMT efficacy results were based on 1,091 patients with at least one adequate carotid ultrasound. Median follow-up from baseline to last CIMT scan was 5 years.
Insulin glargine was well tolerated and safe, with the most common reasons for discontinuation being patient preference in 76 patients and hypoglycemia in 9, Dr. Lonn said.
The study was funded by Sanofi; omega-3 fatty acid supplements and matching placebo were provided by Pronova BioPharma. Dr. Lonn reported research grants, lecture fees, and/or consulting fees from Astra-Zeneca, Canadian Institutes of Health Research, GlaxoSmithKline, Heart and Stroke Foundation of Canada, Merck, Novartis, Servier, and Sanofi. Dr. Deanfield reported consulting and speakers bureau participation for Pfizer, Merck, Roche, Takeda, Novartis, Sanofi, and Danone.
MUNICH – Insulin glargine and omega-3 fatty acids failed to retard carotid atherosclerosis progression in patients with diabetes or prediabetes at high cardiovascular risk in the GRACE trial.
Compared with standard glycemic care, insulin glargine provided a nonsignificant difference of –0.0030 mm/year in the primary end point of rate of change in maximum carotid intima media thickness (CIMT) at 12 carotid sites.
For the secondary outcomes, which included four segments of the common carotid artery and eight segments of the common carotid and bifurcation sites, the long-acting basal insulin resulted in slight but statistically significant annualized differences in maximum CIMT of –0.0033 mm/year and –0.0045 mm/year, respectively.
"Although not conclusive, our study suggests a beneficial effect of insulin glargine on vascular disease progression," Dr. Eva Lonn said at the annual congress of the European Society of Cardiology. "These findings raise the possibility that longer term treatment might result in cardiovascular event reduction."
This hypothesis is currently under evaluation in extended follow-up of ORIGIN (Outcome Reduction With an Initial Glargine Intervention), the parent trial of GRACE (Glucose Reduction and Atherosclerosis Continuing Evaluation).
With regard to omega-3 fatty acids, no significant differences were observed for the primary outcome (difference 0.0009 mm/yr), or the secondary outcomes in the common carotid (–0.0004 mm/yr) and common carotid and bifurcation sites (0.0022 mm/year), reported Dr. Lonn, professor of medicine at McMaster University and director of the vascular research ultrasound laboratory at the Population Health Research Institute, both in Hamilton, Ontario.
Given the neutral effect of omega-3 fatty acids, the focus in diabetes should be on proven therapies such as lipid-lowering and blood pressure–lowering drugs and glycemic control, she said in an interview. There is no harm, however, should patients wish to take the supplements.
Discussant John E. Deanfield said there was no evidence of benefit or harm from either treatment, and pointed out that the results of GRACE are concordant with those reported from the larger ORIGIN trial.
In that trial, insulin glargine reduced the risk of developing type 2 diabetes by 28% among patients with prediabetes, but had a neutral effect on cardiovascular outcomes (N. Engl. J. Med. 2012;367:319-28). Omega-3 fatty acids reduced triglyceride levels, but also failed to reduce the rate of cardiovascular events (N. Engl. J. Med. 2012;367:309-18).
After a median clinical follow up of 6.2 years in GRACE, Dr. Lonn reported that rates of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke were similar between the insulin glargine and standard care groups (18.6% vs. 16.9%), as was all-cause mortality (17.1% vs. 17.4%).
Dr. Deanfield said the lack of benefit from either treatment was disappointing and suggested the GRACE authors might have been better served by choosing the common carotid segment as their primary outcome, rather than one of their secondary outcomes.
He also noted that there is controversy over whether IMT itself is the best measure of structural arterial disease, with a recent meta-analysis demonstrating a lack of relationship between progression of CIMT and hazard for cardiovascular events (Lancet 2012;379:2053-62).
"Finally, the reporting strategy for IMT in this trial – which shows the change in IMT levels over 5 years without giving us, as yet, the baseline absolute levels of IMT – is interesting and might be missing a trick in terms of our understanding of this signal," said Dr. Deanfield, professor of cardiology at University College London.
A total of 1,184 patients recruited from 32 centers in seven countries received open-label insulin glargine injection or standard glycemic care, and double-blinded therapy with a 1-g/day omega-3 supplement containing eicosapentaenoic acid 465 mg plus docosahexaenoic acid 375 mg or matching placebo.
Patients had to be at least 50 years old (mean age 63 years) and have prediabetes or newly diagnosed type 2 diabetes or early type 2 diabetes, and be at high cardiovascular risk.
At baseline, 49% had a history of cardiovascular disease, 80% had hypertension, 60% had hyperlipidemia and 10% were current smokers. CIMT efficacy results were based on 1,091 patients with at least one adequate carotid ultrasound. Median follow-up from baseline to last CIMT scan was 5 years.
Insulin glargine was well tolerated and safe, with the most common reasons for discontinuation being patient preference in 76 patients and hypoglycemia in 9, Dr. Lonn said.
The study was funded by Sanofi; omega-3 fatty acid supplements and matching placebo were provided by Pronova BioPharma. Dr. Lonn reported research grants, lecture fees, and/or consulting fees from Astra-Zeneca, Canadian Institutes of Health Research, GlaxoSmithKline, Heart and Stroke Foundation of Canada, Merck, Novartis, Servier, and Sanofi. Dr. Deanfield reported consulting and speakers bureau participation for Pfizer, Merck, Roche, Takeda, Novartis, Sanofi, and Danone.
AT THE ANNUAL CONGRESS OF THE EUROPEAN SOCIETY OF CARDIOLOGY
Major Finding: The rate of change in maximum carotid intima media thickness at 12 carotid sites was not significantly different between insulin glargine (difference, –0.003 mm/yr) or omega-3 fatty acids (difference 0.0009 mm/yr) and standard glycemic control.
Data Source: GRACE, a substudy of 1,184 patients in the ORIGIN trial with dysglycemia and at high cardiovascular risk.
Disclosures: The study was funded by Sanofi; omega-3 fatty acid supplements and matching placebo were provided by Pronova BioPharma. Dr. Lonn reported research grants, lecture fees, and/or consulting fees from Astra-Zeneca, Canadian Institutes of Health Research, GlaxoSmithKline, Heart and Stroke Foundation of Canada, Merck, Novartis, Servier, and Sanofi. Dr. Deanfield reported consulting and speakers bureau participation for Pfizer, Merck, Roche, Takeda, Novartis, Sanofi, and Danone.
A-Fib Ablation Shown Safe During Cardiac Surgery
MUNICH – Left atrial ablative treatment for atrial fibrillation was safe when administered during open heart surgery in a multicenter, randomized trial of 224 patients who all had atrial fibrillation and required heart surgery for another reason.
The treatment was also effective, resulting in a significantly higher rate of sinus rhythm among the patients treated with ablation compared with the control patients who underwent open-heart surgery alone, Dr. Petr Widimsky reported at the annual congress of the European Society of Cardiology.
Some experts who heard the findings expressed some skepticism about the pattern of anti-arrhythmic effects and other atrial fibrillation–related outcomes during follow-up.
"The rhythm outcomes had some surprises. All the benefit was in patients with long-standing, persistent atrial fibrillation; that’s very surprising because it contrasts with previous findings from both catheter ablation and surgical ablation," said Dr. Gerhard Hindricks, a professor of medicine and director of the department of electrophysiology at the Heart Center of Leipzig (Germany) University.
"The secondary outcomes were also a surprise, because the atrial fibrillation response did not translate into a change in treatment" in the use of anti-arrhythmic drugs, and the two groups showed no differences in the 1-year rates of stroke, major bleeding, and all-cause mortality despite the reported different rates of continued AF. In an editorial that accompanied the published paper, Dr. Hindricks cited the inadequacy of assessing atrial arrhythmia at 1-year follow-up with 24-hour Holter ECG monitoring. "This follow-up regimen is by far not enough to generate reliable and solid results," Dr. Hindricks and his coauthor wrote (Eur. Heart J. 2012;33 [doi: 10.1093/eurheartj/ehs294]).
Despite these unexpected findings, "surgical ablation of atrial fibrillation should be cautiously indicated in asymptomatic patients scheduled for cardiac surgery," Dr. Hindricks said in comments he made at the meeting.
"This was the largest" of several randomized, prospective studies that have assessed ablation of atrial fibrillation during cardiac surgery, said Dr. Riccardo Cappato, director of the Center of Clinical Arrhythmia and Electrophysiology at the Policlinico San Donato in Milan. "The increased probability of maintaining sinus rhythm in patients with permanent atrial fibrillation does not seem to have been at the expense of higher perioperative risk exposure."
The PRAGUE-12 study enrolled 224 patients with AF who required cardiac surgery for coronary artery bypass, valve repair or replacement, or both at three centers in the Czech Republic and Slovakia during 2007-2011. The investigators randomized 117 patients to undergo atrial ablation during their surgery, and 107 who received no ablation with their surgery and served as controls. The surgeons could use whichever energy source for ablation they preferred, but 97% used cryoablation. The ablation-lesion set was the same for all patients in that treatment arm.
The patients averaged about 70 years old, and about 58% were men. Roughly half the patients had long-standing persistent AF, about a quarter had persistent AF, and the remaining quarter had paroxysmal AF.
All patients underwent open surgery using a median sternotomy with cardiopulmonary bypass and cardioplegic heart arrest. Adding ablation to the procedures increased the total surgical time by an average of 20 minutes, and increased the period of cardiopulmonary bypass and the cross-clamp time by an average of 28 minutes.
The primary safety end point was the combined rate of death, stroke, myocardial ischemia, or renal failure requiring dialysis at 30 days after surgery; this occurred in 10% of the patients who had ablation and 15% of the control patients, a nonsignificant difference, reported Dr. Widimsky, professor and head of the Cardiocenter of Charles University in Prague. Each component of the combined adverse event was similar between the two study arms. At 1 year after surgery, the combined adverse event rate was 41% in the patients treated with AF ablation and 40% in the controls.
The study’s primary efficacy end point was the prevalence of sinus rhythm in patients as measured by 24-hour Holter ECG monitoring, which occurred in 60% of the patients who underwent ablation and in 36% of the controls, a significant difference. This difference was driven by the outcome difference among the subgroup of patients who entered the study with long-standing persistent AF. In this subgroup, the proportion of patients in sinus rhythm when assessed after 1 year was 53% in the ablated group and 14% in the controls, a significant difference. In contrast, the prevalence of sinus rhythm at 1 year did not differ significantly between the two treatment arms in patients who entered the study with paroxysmal AF, or in those who entered with persistent AF.
Concurrent with the presentation of PRAGUE-12, the results also appeared in an article published online (Eur. Heart J. 2012;33 [doi: 10.1093/eurheartj/ehs290]).
Dr. Widimsky and his associates said that they had no disclosures.
When Dr. James L. Cox introduced the Cox-Maze III procedure for the surgical disruption of atrial fibrillation, the technique involved prolonged cutting and sewing, and the added time on cardiopulmonary bypass and cross-clamping this produced led to a lot of morbidity, including neurologic complications and renal failure.
The current study used a modified Maze procedure that primarily used cryoablation. Because no cutting and sewing were involved, the surgery was much easier, and it produced fewer complications. Surgeons are interested in an atrial fibrillation procedure that is safe and increases the likelihood of leading to sinus rhythm.

|
Mitchel L. Zoler/IMNG Medical Media
|
This study is important because it shows that this method can be used safely and it improves the end point of resting sinus rhythm. It is paradoxical that the main rhythm benefit was in patients with long-standing persistent atrial fibrillation, because usually that is harder to treat. But this may have been a methodological issue, because they measured the 1-year rhythm outcome without doing prolonged, continuous ECG monitoring. It’s hard to define success in patients with paroxysmal atrial fibrillation unless you monitor patients continuously for a week.
The main message from this study was that the ablation procedure was safe during cardiac surgery and did not add much time or complexity to the surgery. I think these results will increase the use of ablation during cardiac surgery for other reasons. It is a major contribution.
Miguel Sousa Uva, M.D., a cardiac surgeon at Hospital da Cruz Vermelha in Lisbon, made these comments in an interview. He said that he had no disclosures.
When Dr. James L. Cox introduced the Cox-Maze III procedure for the surgical disruption of atrial fibrillation, the technique involved prolonged cutting and sewing, and the added time on cardiopulmonary bypass and cross-clamping this produced led to a lot of morbidity, including neurologic complications and renal failure.
The current study used a modified Maze procedure that primarily used cryoablation. Because no cutting and sewing were involved, the surgery was much easier, and it produced fewer complications. Surgeons are interested in an atrial fibrillation procedure that is safe and increases the likelihood of leading to sinus rhythm.

|
Mitchel L. Zoler/IMNG Medical Media
|
This study is important because it shows that this method can be used safely and it improves the end point of resting sinus rhythm. It is paradoxical that the main rhythm benefit was in patients with long-standing persistent atrial fibrillation, because usually that is harder to treat. But this may have been a methodological issue, because they measured the 1-year rhythm outcome without doing prolonged, continuous ECG monitoring. It’s hard to define success in patients with paroxysmal atrial fibrillation unless you monitor patients continuously for a week.
The main message from this study was that the ablation procedure was safe during cardiac surgery and did not add much time or complexity to the surgery. I think these results will increase the use of ablation during cardiac surgery for other reasons. It is a major contribution.
Miguel Sousa Uva, M.D., a cardiac surgeon at Hospital da Cruz Vermelha in Lisbon, made these comments in an interview. He said that he had no disclosures.
When Dr. James L. Cox introduced the Cox-Maze III procedure for the surgical disruption of atrial fibrillation, the technique involved prolonged cutting and sewing, and the added time on cardiopulmonary bypass and cross-clamping this produced led to a lot of morbidity, including neurologic complications and renal failure.
The current study used a modified Maze procedure that primarily used cryoablation. Because no cutting and sewing were involved, the surgery was much easier, and it produced fewer complications. Surgeons are interested in an atrial fibrillation procedure that is safe and increases the likelihood of leading to sinus rhythm.

|
Mitchel L. Zoler/IMNG Medical Media
|
This study is important because it shows that this method can be used safely and it improves the end point of resting sinus rhythm. It is paradoxical that the main rhythm benefit was in patients with long-standing persistent atrial fibrillation, because usually that is harder to treat. But this may have been a methodological issue, because they measured the 1-year rhythm outcome without doing prolonged, continuous ECG monitoring. It’s hard to define success in patients with paroxysmal atrial fibrillation unless you monitor patients continuously for a week.
The main message from this study was that the ablation procedure was safe during cardiac surgery and did not add much time or complexity to the surgery. I think these results will increase the use of ablation during cardiac surgery for other reasons. It is a major contribution.
Miguel Sousa Uva, M.D., a cardiac surgeon at Hospital da Cruz Vermelha in Lisbon, made these comments in an interview. He said that he had no disclosures.
MUNICH – Left atrial ablative treatment for atrial fibrillation was safe when administered during open heart surgery in a multicenter, randomized trial of 224 patients who all had atrial fibrillation and required heart surgery for another reason.
The treatment was also effective, resulting in a significantly higher rate of sinus rhythm among the patients treated with ablation compared with the control patients who underwent open-heart surgery alone, Dr. Petr Widimsky reported at the annual congress of the European Society of Cardiology.
Some experts who heard the findings expressed some skepticism about the pattern of anti-arrhythmic effects and other atrial fibrillation–related outcomes during follow-up.
"The rhythm outcomes had some surprises. All the benefit was in patients with long-standing, persistent atrial fibrillation; that’s very surprising because it contrasts with previous findings from both catheter ablation and surgical ablation," said Dr. Gerhard Hindricks, a professor of medicine and director of the department of electrophysiology at the Heart Center of Leipzig (Germany) University.
"The secondary outcomes were also a surprise, because the atrial fibrillation response did not translate into a change in treatment" in the use of anti-arrhythmic drugs, and the two groups showed no differences in the 1-year rates of stroke, major bleeding, and all-cause mortality despite the reported different rates of continued AF. In an editorial that accompanied the published paper, Dr. Hindricks cited the inadequacy of assessing atrial arrhythmia at 1-year follow-up with 24-hour Holter ECG monitoring. "This follow-up regimen is by far not enough to generate reliable and solid results," Dr. Hindricks and his coauthor wrote (Eur. Heart J. 2012;33 [doi: 10.1093/eurheartj/ehs294]).
Despite these unexpected findings, "surgical ablation of atrial fibrillation should be cautiously indicated in asymptomatic patients scheduled for cardiac surgery," Dr. Hindricks said in comments he made at the meeting.
"This was the largest" of several randomized, prospective studies that have assessed ablation of atrial fibrillation during cardiac surgery, said Dr. Riccardo Cappato, director of the Center of Clinical Arrhythmia and Electrophysiology at the Policlinico San Donato in Milan. "The increased probability of maintaining sinus rhythm in patients with permanent atrial fibrillation does not seem to have been at the expense of higher perioperative risk exposure."
The PRAGUE-12 study enrolled 224 patients with AF who required cardiac surgery for coronary artery bypass, valve repair or replacement, or both at three centers in the Czech Republic and Slovakia during 2007-2011. The investigators randomized 117 patients to undergo atrial ablation during their surgery, and 107 who received no ablation with their surgery and served as controls. The surgeons could use whichever energy source for ablation they preferred, but 97% used cryoablation. The ablation-lesion set was the same for all patients in that treatment arm.
The patients averaged about 70 years old, and about 58% were men. Roughly half the patients had long-standing persistent AF, about a quarter had persistent AF, and the remaining quarter had paroxysmal AF.
All patients underwent open surgery using a median sternotomy with cardiopulmonary bypass and cardioplegic heart arrest. Adding ablation to the procedures increased the total surgical time by an average of 20 minutes, and increased the period of cardiopulmonary bypass and the cross-clamp time by an average of 28 minutes.
The primary safety end point was the combined rate of death, stroke, myocardial ischemia, or renal failure requiring dialysis at 30 days after surgery; this occurred in 10% of the patients who had ablation and 15% of the control patients, a nonsignificant difference, reported Dr. Widimsky, professor and head of the Cardiocenter of Charles University in Prague. Each component of the combined adverse event was similar between the two study arms. At 1 year after surgery, the combined adverse event rate was 41% in the patients treated with AF ablation and 40% in the controls.
The study’s primary efficacy end point was the prevalence of sinus rhythm in patients as measured by 24-hour Holter ECG monitoring, which occurred in 60% of the patients who underwent ablation and in 36% of the controls, a significant difference. This difference was driven by the outcome difference among the subgroup of patients who entered the study with long-standing persistent AF. In this subgroup, the proportion of patients in sinus rhythm when assessed after 1 year was 53% in the ablated group and 14% in the controls, a significant difference. In contrast, the prevalence of sinus rhythm at 1 year did not differ significantly between the two treatment arms in patients who entered the study with paroxysmal AF, or in those who entered with persistent AF.
Concurrent with the presentation of PRAGUE-12, the results also appeared in an article published online (Eur. Heart J. 2012;33 [doi: 10.1093/eurheartj/ehs290]).
Dr. Widimsky and his associates said that they had no disclosures.
MUNICH – Left atrial ablative treatment for atrial fibrillation was safe when administered during open heart surgery in a multicenter, randomized trial of 224 patients who all had atrial fibrillation and required heart surgery for another reason.
The treatment was also effective, resulting in a significantly higher rate of sinus rhythm among the patients treated with ablation compared with the control patients who underwent open-heart surgery alone, Dr. Petr Widimsky reported at the annual congress of the European Society of Cardiology.
Some experts who heard the findings expressed some skepticism about the pattern of anti-arrhythmic effects and other atrial fibrillation–related outcomes during follow-up.
"The rhythm outcomes had some surprises. All the benefit was in patients with long-standing, persistent atrial fibrillation; that’s very surprising because it contrasts with previous findings from both catheter ablation and surgical ablation," said Dr. Gerhard Hindricks, a professor of medicine and director of the department of electrophysiology at the Heart Center of Leipzig (Germany) University.
"The secondary outcomes were also a surprise, because the atrial fibrillation response did not translate into a change in treatment" in the use of anti-arrhythmic drugs, and the two groups showed no differences in the 1-year rates of stroke, major bleeding, and all-cause mortality despite the reported different rates of continued AF. In an editorial that accompanied the published paper, Dr. Hindricks cited the inadequacy of assessing atrial arrhythmia at 1-year follow-up with 24-hour Holter ECG monitoring. "This follow-up regimen is by far not enough to generate reliable and solid results," Dr. Hindricks and his coauthor wrote (Eur. Heart J. 2012;33 [doi: 10.1093/eurheartj/ehs294]).
Despite these unexpected findings, "surgical ablation of atrial fibrillation should be cautiously indicated in asymptomatic patients scheduled for cardiac surgery," Dr. Hindricks said in comments he made at the meeting.
"This was the largest" of several randomized, prospective studies that have assessed ablation of atrial fibrillation during cardiac surgery, said Dr. Riccardo Cappato, director of the Center of Clinical Arrhythmia and Electrophysiology at the Policlinico San Donato in Milan. "The increased probability of maintaining sinus rhythm in patients with permanent atrial fibrillation does not seem to have been at the expense of higher perioperative risk exposure."
The PRAGUE-12 study enrolled 224 patients with AF who required cardiac surgery for coronary artery bypass, valve repair or replacement, or both at three centers in the Czech Republic and Slovakia during 2007-2011. The investigators randomized 117 patients to undergo atrial ablation during their surgery, and 107 who received no ablation with their surgery and served as controls. The surgeons could use whichever energy source for ablation they preferred, but 97% used cryoablation. The ablation-lesion set was the same for all patients in that treatment arm.
The patients averaged about 70 years old, and about 58% were men. Roughly half the patients had long-standing persistent AF, about a quarter had persistent AF, and the remaining quarter had paroxysmal AF.
All patients underwent open surgery using a median sternotomy with cardiopulmonary bypass and cardioplegic heart arrest. Adding ablation to the procedures increased the total surgical time by an average of 20 minutes, and increased the period of cardiopulmonary bypass and the cross-clamp time by an average of 28 minutes.
The primary safety end point was the combined rate of death, stroke, myocardial ischemia, or renal failure requiring dialysis at 30 days after surgery; this occurred in 10% of the patients who had ablation and 15% of the control patients, a nonsignificant difference, reported Dr. Widimsky, professor and head of the Cardiocenter of Charles University in Prague. Each component of the combined adverse event was similar between the two study arms. At 1 year after surgery, the combined adverse event rate was 41% in the patients treated with AF ablation and 40% in the controls.
The study’s primary efficacy end point was the prevalence of sinus rhythm in patients as measured by 24-hour Holter ECG monitoring, which occurred in 60% of the patients who underwent ablation and in 36% of the controls, a significant difference. This difference was driven by the outcome difference among the subgroup of patients who entered the study with long-standing persistent AF. In this subgroup, the proportion of patients in sinus rhythm when assessed after 1 year was 53% in the ablated group and 14% in the controls, a significant difference. In contrast, the prevalence of sinus rhythm at 1 year did not differ significantly between the two treatment arms in patients who entered the study with paroxysmal AF, or in those who entered with persistent AF.
Concurrent with the presentation of PRAGUE-12, the results also appeared in an article published online (Eur. Heart J. 2012;33 [doi: 10.1093/eurheartj/ehs290]).
Dr. Widimsky and his associates said that they had no disclosures.
AT THE ANNUAL CONGRESS OF THE EUROPEAN SOCIETY OF CARDIOLOGY
Major Finding: After 30 days, the adverse event rate was 10% in cardiac surgery patients also undergoing ablation and 15% in patients without ablation, a difference that was not significant.
Data Source: PRAGUE-12 was a randomized trial that enrolled 224 patients with atrial fibrillation who also required cardiac surgery for another reason at three centers in the Czech Republic and Slovakia.
Disclosures: Dr. Widimsky and his associates said that they had no disclosures.
Lifestyle Messages After PCI Need to Be Hit Harder
MUNICH – Despite undergoing a lifesaving coronary intervention, patients are failing to heed the message from physicians to adopt a heart-healthy lifestyle, according to a patient survey.
Among 1,703 Swedish patients surveyed within 8 weeks of an acute percutaneous coronary intervention (PCI), 16% were still smoking, 45% had inadequate dietary habits, and just 47% were physically active, Dr. Joep Perk reported at the annual congress of the European Society of Cardiology.
"When we asked them, ‘Why did you get your myocardial infarction?’ they said, ‘It’s in the family, it’s my age. It has nothing to do with smoking or running around eating," Dr. Perk said.
"They thought it was something you could not influence and had to go to the doctor to get mended, and the next time it breaks down, you have to go back to the doctor again."
Patients, however, may not get that chance.
Patients who reported persistent smoking and nonadherence to diet and exercise had a 3.8-fold higher risk of myocardial infarction (MI), stroke, or death within 6 months of PCI in the massive OASIS-5 (Organization to Assess Strategies in Acute Ischemic Syndromes 5) study, involving 18,809 patients from 41 countries, observed Dr. Perk, a senior professor at Linnaeus University in Kalmar, Sweden, and editor of the European Journal of Preventive Cardiology.
In contrast, quitting smoking dramatically reduced the risk of MI (odds ratio, 0.57), as did diet and exercise adherence (OR, 0.52), he said.
Using the 6% post-PCI rate for all cardiac events reported in OASIS-5, Dr. Perk and his colleagues conducted the SPICI (Study of Patient Information after Coronary Intervention) study, and estimated that the expected cardiac event rate in the Swedish population would be 1,100-1,200 events annually.
Thus, a prudent estimate indicates that at least 400-500 cases of MI, cardiac death, or stroke could be prevented if the Swedish post-PCI population would adhere 100% to a cardioprotective lifestyle, saving the lives of 150-200 persons yearly, he reported in the poster presentation.
Clearly, cardiac rehabilitation programs need to find news ways to reach their patients. Many of the patients in SPICI reported searching the Internet or asking friends and relatives for advice post PCI, while only 78% were invited to exercise training programs and 71% received nutritional counseling.
"There is fantastic room for improvement," Dr. Perk said in a press briefing. "We feel cardiac rehabilitation has lost touch with modern interventional cardiology."
Part of the problem is that some physicians may not be aware of the "really explosive information" in OASIS-5, or may focus their message on cure rather than grim statistics and the need to modify bad habits. Others may reach out to their patients too soon after PCI, when they are in a state of "shock" and unable to process information about lifestyle changes, Dr. Perk said in an interview.
"Timing is very important," he said. "Patients need time to think and consider what they can do themselves."
In this study, most patients expressed the belief that after PCI their disease was cured. Or they thought that if it were to come back, it would merely mean another trip to the PCI lab, an attitude that Dr. Perk considers "a fatal mistake."
Patients seemed to comprehend the need for lifestyle changes equally as poorly whether the message was delivered by physicians or nurses. Patient age and gender also had no significant impact on the uptake of healthy lifestyle choices, he said.
If physicians want to get their message across, he suggests they engage the patient’s partner and family, use modern educational technology such as interactive Internet-based models or support groups, and engage educators to help hone the communication skills of health professionals.
Dr. Michel Bertrand, past president of the European Society of Cardiology (ESC), said in an interview, "I am pessimistic because in spite of all that we tell our patients – ‘You need to stop smoking, you need to exercise, you need to have a good diet’ – they don’t do it."
He pointed to data from the cross-sectional EUROASPIRE I, II, and III studies showing that blood pressure, lipid targets, and smoking rates remained the same among patients with coronary heart disease despite a substantial increase in antihypertensive and lipid-lowering drugs (Lancet 2009;373:929-40).
In addition, investigators with the FAST-MI (French Registry of Acute ST-Elevation or non-ST-elevation Myocardial Infarction) study reported at the same ESC meeting that the proportion of female ST-segment elevation MI patients under age 60 more than doubled, from 11.8% to 25.5%, and the number under age 50 tripled, from 3.7% to 11.1% from 1995 to 2010 (JAMA Aug. 27 [doi: 10.1001/2012.jama.11348]).
Over the same period, the proportion of younger women (under age 60) who were current smokers jumped from 37% to 73%, and the prevalence of obesity rose from 18% to 27%.
"The problem is young women; they are smoking more and more and more," said Dr. Bertrand. "In my own experience, I have been obliged in the past to find the possibility to have heart transplantation for a woman under 30. Under 30! And why? It’s because [of] the pill and tobacco. This is a bomb. Tobacco is a bomb."
Click here to view a video interview with Dr. Perk.
Dr. Perk and Dr. Bertrand reported having no relevant conflicts.
MUNICH – Despite undergoing a lifesaving coronary intervention, patients are failing to heed the message from physicians to adopt a heart-healthy lifestyle, according to a patient survey.
Among 1,703 Swedish patients surveyed within 8 weeks of an acute percutaneous coronary intervention (PCI), 16% were still smoking, 45% had inadequate dietary habits, and just 47% were physically active, Dr. Joep Perk reported at the annual congress of the European Society of Cardiology.
"When we asked them, ‘Why did you get your myocardial infarction?’ they said, ‘It’s in the family, it’s my age. It has nothing to do with smoking or running around eating," Dr. Perk said.
"They thought it was something you could not influence and had to go to the doctor to get mended, and the next time it breaks down, you have to go back to the doctor again."
Patients, however, may not get that chance.
Patients who reported persistent smoking and nonadherence to diet and exercise had a 3.8-fold higher risk of myocardial infarction (MI), stroke, or death within 6 months of PCI in the massive OASIS-5 (Organization to Assess Strategies in Acute Ischemic Syndromes 5) study, involving 18,809 patients from 41 countries, observed Dr. Perk, a senior professor at Linnaeus University in Kalmar, Sweden, and editor of the European Journal of Preventive Cardiology.
In contrast, quitting smoking dramatically reduced the risk of MI (odds ratio, 0.57), as did diet and exercise adherence (OR, 0.52), he said.
Using the 6% post-PCI rate for all cardiac events reported in OASIS-5, Dr. Perk and his colleagues conducted the SPICI (Study of Patient Information after Coronary Intervention) study, and estimated that the expected cardiac event rate in the Swedish population would be 1,100-1,200 events annually.
Thus, a prudent estimate indicates that at least 400-500 cases of MI, cardiac death, or stroke could be prevented if the Swedish post-PCI population would adhere 100% to a cardioprotective lifestyle, saving the lives of 150-200 persons yearly, he reported in the poster presentation.
Clearly, cardiac rehabilitation programs need to find news ways to reach their patients. Many of the patients in SPICI reported searching the Internet or asking friends and relatives for advice post PCI, while only 78% were invited to exercise training programs and 71% received nutritional counseling.
"There is fantastic room for improvement," Dr. Perk said in a press briefing. "We feel cardiac rehabilitation has lost touch with modern interventional cardiology."
Part of the problem is that some physicians may not be aware of the "really explosive information" in OASIS-5, or may focus their message on cure rather than grim statistics and the need to modify bad habits. Others may reach out to their patients too soon after PCI, when they are in a state of "shock" and unable to process information about lifestyle changes, Dr. Perk said in an interview.
"Timing is very important," he said. "Patients need time to think and consider what they can do themselves."
In this study, most patients expressed the belief that after PCI their disease was cured. Or they thought that if it were to come back, it would merely mean another trip to the PCI lab, an attitude that Dr. Perk considers "a fatal mistake."
Patients seemed to comprehend the need for lifestyle changes equally as poorly whether the message was delivered by physicians or nurses. Patient age and gender also had no significant impact on the uptake of healthy lifestyle choices, he said.
If physicians want to get their message across, he suggests they engage the patient’s partner and family, use modern educational technology such as interactive Internet-based models or support groups, and engage educators to help hone the communication skills of health professionals.
Dr. Michel Bertrand, past president of the European Society of Cardiology (ESC), said in an interview, "I am pessimistic because in spite of all that we tell our patients – ‘You need to stop smoking, you need to exercise, you need to have a good diet’ – they don’t do it."
He pointed to data from the cross-sectional EUROASPIRE I, II, and III studies showing that blood pressure, lipid targets, and smoking rates remained the same among patients with coronary heart disease despite a substantial increase in antihypertensive and lipid-lowering drugs (Lancet 2009;373:929-40).
In addition, investigators with the FAST-MI (French Registry of Acute ST-Elevation or non-ST-elevation Myocardial Infarction) study reported at the same ESC meeting that the proportion of female ST-segment elevation MI patients under age 60 more than doubled, from 11.8% to 25.5%, and the number under age 50 tripled, from 3.7% to 11.1% from 1995 to 2010 (JAMA Aug. 27 [doi: 10.1001/2012.jama.11348]).
Over the same period, the proportion of younger women (under age 60) who were current smokers jumped from 37% to 73%, and the prevalence of obesity rose from 18% to 27%.
"The problem is young women; they are smoking more and more and more," said Dr. Bertrand. "In my own experience, I have been obliged in the past to find the possibility to have heart transplantation for a woman under 30. Under 30! And why? It’s because [of] the pill and tobacco. This is a bomb. Tobacco is a bomb."
Click here to view a video interview with Dr. Perk.
Dr. Perk and Dr. Bertrand reported having no relevant conflicts.
MUNICH – Despite undergoing a lifesaving coronary intervention, patients are failing to heed the message from physicians to adopt a heart-healthy lifestyle, according to a patient survey.
Among 1,703 Swedish patients surveyed within 8 weeks of an acute percutaneous coronary intervention (PCI), 16% were still smoking, 45% had inadequate dietary habits, and just 47% were physically active, Dr. Joep Perk reported at the annual congress of the European Society of Cardiology.
"When we asked them, ‘Why did you get your myocardial infarction?’ they said, ‘It’s in the family, it’s my age. It has nothing to do with smoking or running around eating," Dr. Perk said.
"They thought it was something you could not influence and had to go to the doctor to get mended, and the next time it breaks down, you have to go back to the doctor again."
Patients, however, may not get that chance.
Patients who reported persistent smoking and nonadherence to diet and exercise had a 3.8-fold higher risk of myocardial infarction (MI), stroke, or death within 6 months of PCI in the massive OASIS-5 (Organization to Assess Strategies in Acute Ischemic Syndromes 5) study, involving 18,809 patients from 41 countries, observed Dr. Perk, a senior professor at Linnaeus University in Kalmar, Sweden, and editor of the European Journal of Preventive Cardiology.
In contrast, quitting smoking dramatically reduced the risk of MI (odds ratio, 0.57), as did diet and exercise adherence (OR, 0.52), he said.
Using the 6% post-PCI rate for all cardiac events reported in OASIS-5, Dr. Perk and his colleagues conducted the SPICI (Study of Patient Information after Coronary Intervention) study, and estimated that the expected cardiac event rate in the Swedish population would be 1,100-1,200 events annually.
Thus, a prudent estimate indicates that at least 400-500 cases of MI, cardiac death, or stroke could be prevented if the Swedish post-PCI population would adhere 100% to a cardioprotective lifestyle, saving the lives of 150-200 persons yearly, he reported in the poster presentation.
Clearly, cardiac rehabilitation programs need to find news ways to reach their patients. Many of the patients in SPICI reported searching the Internet or asking friends and relatives for advice post PCI, while only 78% were invited to exercise training programs and 71% received nutritional counseling.
"There is fantastic room for improvement," Dr. Perk said in a press briefing. "We feel cardiac rehabilitation has lost touch with modern interventional cardiology."
Part of the problem is that some physicians may not be aware of the "really explosive information" in OASIS-5, or may focus their message on cure rather than grim statistics and the need to modify bad habits. Others may reach out to their patients too soon after PCI, when they are in a state of "shock" and unable to process information about lifestyle changes, Dr. Perk said in an interview.
"Timing is very important," he said. "Patients need time to think and consider what they can do themselves."
In this study, most patients expressed the belief that after PCI their disease was cured. Or they thought that if it were to come back, it would merely mean another trip to the PCI lab, an attitude that Dr. Perk considers "a fatal mistake."
Patients seemed to comprehend the need for lifestyle changes equally as poorly whether the message was delivered by physicians or nurses. Patient age and gender also had no significant impact on the uptake of healthy lifestyle choices, he said.
If physicians want to get their message across, he suggests they engage the patient’s partner and family, use modern educational technology such as interactive Internet-based models or support groups, and engage educators to help hone the communication skills of health professionals.
Dr. Michel Bertrand, past president of the European Society of Cardiology (ESC), said in an interview, "I am pessimistic because in spite of all that we tell our patients – ‘You need to stop smoking, you need to exercise, you need to have a good diet’ – they don’t do it."
He pointed to data from the cross-sectional EUROASPIRE I, II, and III studies showing that blood pressure, lipid targets, and smoking rates remained the same among patients with coronary heart disease despite a substantial increase in antihypertensive and lipid-lowering drugs (Lancet 2009;373:929-40).
In addition, investigators with the FAST-MI (French Registry of Acute ST-Elevation or non-ST-elevation Myocardial Infarction) study reported at the same ESC meeting that the proportion of female ST-segment elevation MI patients under age 60 more than doubled, from 11.8% to 25.5%, and the number under age 50 tripled, from 3.7% to 11.1% from 1995 to 2010 (JAMA Aug. 27 [doi: 10.1001/2012.jama.11348]).
Over the same period, the proportion of younger women (under age 60) who were current smokers jumped from 37% to 73%, and the prevalence of obesity rose from 18% to 27%.
"The problem is young women; they are smoking more and more and more," said Dr. Bertrand. "In my own experience, I have been obliged in the past to find the possibility to have heart transplantation for a woman under 30. Under 30! And why? It’s because [of] the pill and tobacco. This is a bomb. Tobacco is a bomb."
Click here to view a video interview with Dr. Perk.
Dr. Perk and Dr. Bertrand reported having no relevant conflicts.
AT THE ANNUAL CONGRESS OF THE EUROPEAN SOCIETY OF CARDIOLOGY
Major Finding: Among 1,703 Swedish patients surveyed within 8 weeks of an acute percutaneous coronary intervention (PCI), 16% were still smoking, 45% had inadequate dietary habits, and only 47% were physically active.
Data Source: Retrospective analysis of 1,800 patients who underwent acute percutaneous coronary intervention.
Disclosures: Dr. Perk and Dr. Bertrand report no relevant conflicts of interest.
FAME 2 Favorable PCI Results Driven by Revascularization
The use of fractional flow reserve to guide percutaneous coronary intervention, along with best medical management, sharply reduced the need for urgent revascularization in patients with stable coronary artery disease and at least one physiologically significant lesion.
However, FFR-guided percutaneous coronary intervention (PCI) had little effect on deaths or myocardial infarctions, when compared with best medical management alone, according to the results of the FAME 2 (Fractional Flow Reserve vs. Angiography for Multivessel Evaluation 2) trial, which was conducted at 28 sites in Europe and North America and halted early.
The percentage of patients who had an MI, death, or urgent revascularization (the combined primary end point) was significantly lower in the PCI group than in the medical therapy group (4.3% vs.12.7%; hazard ratio with PCI, 0.32). This difference was driven by a 13-fold increase in the need for urgent revascularization in the medical-therapy group. Notably, the rate of death from any cause and the rate of MI did not differ significantly between the PCI group and the medical therapy group.
Importantly, patient recruitment was stopped on Jan. 15, 2012, at the recommendation of an independent data and safety monitoring board because of the highly significant difference in the incidence rates of the primary end point between the PCI and medical-therapy groups.
The results of the study were released in the New England Journal of Medicine on Aug. 28 to coincide with the presentation of the study at the annual congress of the European Society of Cardiology (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMoa1205361]).
A total of 1,220 patients out a planned 1,832 were enrolled. Of those, 888 patients had at least one stenosis with an FFR of 0.80 or less: 447 patients were randomly assigned to FFR-guided PCI plus the best available medical therapy, and 441 patients to the best available medical therapy alone. The 332 patients with angiographically significant stenoses, but none with an FFR of 0.80 or less were enrolled in the registry and received the best available medical therapy alone. The mean duration of follow-up was 212 days.
Patients in stable condition who were appropriate candidates for PCI and who had angiographically assessed one-, two-, or three-vessel coronary artery disease suitable for PCI were included in the trial.
All patients were prescribed aspirin at a dose of 80-325 mg daily, metoprolol at a dose of 50 mg-200 mg daily (or any other beta-blocker), lisinopril (at least 5 mg daily, or another ACE inhibitor or an angiotensin receptor blocker)and atorvastatin (20-80 mg daily, or another statin).
All PCI patients were treated with second-generation drug-eluting stents.
Among the 56 patients who underwent urgent revascularization, the procedure was triggered by a MI in 12 patients (21%), by unstable angina accompanied by evidence of ischemia on ECG in 15 patients (27%), and by unstable angina diagnosed on the basis of clinical features in 29 patients (52%).
Patients in the PCI group were 86% less likely to undergo any revascularization and 83% less likely to undergo or nonurgent revascularization than were those in the medical therapy group.
The researchers identified several factors that may explain the differences between results in the present study and those in previous trials involving patients with stable coronary disease. "First, in previous trials in which various revascularization methods were compared with the best available medical therapy, patient enrollment was based primarily on angiographic findings, with or without noninvasive documentation of ischemia. It is likely that a sizable proportion of the patients had only limited ischemia," wrote lead investigator Dr. Bernard B. De Bruyne and his coinvestigators. Dr. De Bruyne is the codirector of the Cardiovascular Center at OLV Hospital in Aalst, Belgium.
"Even in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial, in which noninvasive testing was performed in 85% of the patients, less than one-third of the patients had more than 10% ischemia on myocardial perfusion imaging. In daily clinical practice, less than half of patients undergo noninvasive stress testing before elective PCI. In the current trial, all the patients who underwent randomization had at least one functionally significant stenosis," they observed (N. Engl. J. Med. 2007;356:1503-16).
Second, PCI was performed only in lesions with an FFR of 0.80 or less. "This FFR-guided approach is associated with a better clinical outcome than that with PCI performed on the basis of angiographic results alone. These features probably explain the similarity of event rates between patients who were treated with PCI plus the best available medical therapy and patients with equivalent baseline characteristics but no functionally significant lesions who were enrolled in the registry and treated with the best available medical therapy alone," according to the investigators.
Third, second-generation drug-eluting stents were used in PCIs. This strategy is associated with a low number of repeat revascularizations. Finally, the primary end point included urgent revascularization, a component that was not included in the primary end point of previous trials.
The study was sponsored by St. Jude Medical, which makes the two pressure wires used in the trial. The company was involved in the collection and source verification of the data but not in the conduct of the trial. Dr. De Bruyne reported receiving consulting/honorarium and travel fees from St. Jude Medical. Most of the investigators had significant financial relationships with St. Jude Medical, as well as with other device and pharmaceutical companies. One author is an employee of St. Jude Medical.
The recommendation to terminate FAME 2 by the independent data and safety monitoring board at 7 months’ follow-up was based solely on one highly significant treatment difference. That difference was in the end point of urgent revascularization, which was performed in 49 patients in the group that received the best available medical therapy alone vs. 7 patients in the group that underwent percutaneous coronary intervention and also received the best available medical therapy, Dr. William E. Boden wrote in an editorial accompanying the FAME 2 report (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMe1208620]).
"There were very few ‘hard’ events overall, with only four deaths (three in the medical-therapy group and one in the PCI group) and 29 myocardial infarctions (14 in the medical-therapy group and 15 in the PCI group). Of note, the definition of urgent revascularization was largely a clinical one and did not require evidence of ischemia or positive cardiac biomarkers in all patients; 29 of the 56 unplanned revascularizations (52%) were classified solely on the basis of clinical features, whereas in an exploratory subgroup analysis of the remaining 27 patients, there were fewer revascularizations triggered by a myocardial infarction or electrocardiographic evidence of ischemia in the PCI group than in the medical-therapy group," wrote Dr. Boden.
"Clearly, FFR [fractional flow reserve] holds potential promise for a more targeted approach to PCI that might be more clinically effective and cost effective than visually directed PCI for all angiographically significant stenoses," he continued. "Unfortunately, the early termination of the FAME 2 trial before full enrollment and follow-up were achieved, the neutral effects on the rate of death or myocardial infarction, and the lack of a significant, sustained treatment effect on the reduction of angina beyond 6 months leave more questions than answers."
The FAME 2 and COURAGE [Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation] trials are remarkably similar and showed that PCI reduced only the need for revascularization; in the COURAGE trial, there was a significant 40% reduction, whereas "neither the FAME 2 trial (with a mean 7 months of follow-up) nor the COURAGE trial (with a mean 55 months of follow-up) showed a benefit from PCI with respect to a reduction in the rate of death or myocardial infarction. The FAME 2 trial sought to establish the scientific basis for an FFR-guided PCI strategy for all functionally significant stenoses, but the results make this prospect somewhat unappealing," he wrote. Dr. Boden was the lead author of the COURAGE trial.
Current practice guidelines advocate the selective use of FFR to guide PCI decision making regarding borderline visual lesions (approximately 50%-70% stenosis). "It seems likely that the more routine use of FFR for all angiographically-significant stenoses would add considerable time, cost, and complexity to each PCI procedure and might also increase the risk of catheter-related complications such as coronary dissection and perforation," Dr. Boden pointed out.
Some of the uncertainty arising from FAME 2 may be resolved with the results of the ongoing ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial. The study is designed and powered to evaluate the long-term superiority of revascularization plus the best available medical therapy as compared with the best available medical therapy alone with respect to cardiovascular death or MI in patients with stable coronary artery disease and moderate-to-severe myocardial ischemia documented by means of noninvasive measures. "Until the results of ISCHEMIA are available, the case for a more durable clinical benefit of PCI beyond relief of angina or a reduction in the rate of subsequent revascularization is likely to remain both elusive and illusory," concluded Dr. Boden, who is a coprincipal investigator of ISCHEMIA.
Dr. Boden is the chief of medicine at the Albany Stratton Veterans Affairs Medical Center and vice chair of the department of medicine at Albany (N.Y.) Medical Center. He reported that he is a paid consultant for Arbor Pharmaceuticals and is a speaker for Abbott Laboratories and Gilead Sciences.
The recommendation to terminate FAME 2 by the independent data and safety monitoring board at 7 months’ follow-up was based solely on one highly significant treatment difference. That difference was in the end point of urgent revascularization, which was performed in 49 patients in the group that received the best available medical therapy alone vs. 7 patients in the group that underwent percutaneous coronary intervention and also received the best available medical therapy, Dr. William E. Boden wrote in an editorial accompanying the FAME 2 report (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMe1208620]).
"There were very few ‘hard’ events overall, with only four deaths (three in the medical-therapy group and one in the PCI group) and 29 myocardial infarctions (14 in the medical-therapy group and 15 in the PCI group). Of note, the definition of urgent revascularization was largely a clinical one and did not require evidence of ischemia or positive cardiac biomarkers in all patients; 29 of the 56 unplanned revascularizations (52%) were classified solely on the basis of clinical features, whereas in an exploratory subgroup analysis of the remaining 27 patients, there were fewer revascularizations triggered by a myocardial infarction or electrocardiographic evidence of ischemia in the PCI group than in the medical-therapy group," wrote Dr. Boden.
"Clearly, FFR [fractional flow reserve] holds potential promise for a more targeted approach to PCI that might be more clinically effective and cost effective than visually directed PCI for all angiographically significant stenoses," he continued. "Unfortunately, the early termination of the FAME 2 trial before full enrollment and follow-up were achieved, the neutral effects on the rate of death or myocardial infarction, and the lack of a significant, sustained treatment effect on the reduction of angina beyond 6 months leave more questions than answers."
The FAME 2 and COURAGE [Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation] trials are remarkably similar and showed that PCI reduced only the need for revascularization; in the COURAGE trial, there was a significant 40% reduction, whereas "neither the FAME 2 trial (with a mean 7 months of follow-up) nor the COURAGE trial (with a mean 55 months of follow-up) showed a benefit from PCI with respect to a reduction in the rate of death or myocardial infarction. The FAME 2 trial sought to establish the scientific basis for an FFR-guided PCI strategy for all functionally significant stenoses, but the results make this prospect somewhat unappealing," he wrote. Dr. Boden was the lead author of the COURAGE trial.
Current practice guidelines advocate the selective use of FFR to guide PCI decision making regarding borderline visual lesions (approximately 50%-70% stenosis). "It seems likely that the more routine use of FFR for all angiographically-significant stenoses would add considerable time, cost, and complexity to each PCI procedure and might also increase the risk of catheter-related complications such as coronary dissection and perforation," Dr. Boden pointed out.
Some of the uncertainty arising from FAME 2 may be resolved with the results of the ongoing ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial. The study is designed and powered to evaluate the long-term superiority of revascularization plus the best available medical therapy as compared with the best available medical therapy alone with respect to cardiovascular death or MI in patients with stable coronary artery disease and moderate-to-severe myocardial ischemia documented by means of noninvasive measures. "Until the results of ISCHEMIA are available, the case for a more durable clinical benefit of PCI beyond relief of angina or a reduction in the rate of subsequent revascularization is likely to remain both elusive and illusory," concluded Dr. Boden, who is a coprincipal investigator of ISCHEMIA.
Dr. Boden is the chief of medicine at the Albany Stratton Veterans Affairs Medical Center and vice chair of the department of medicine at Albany (N.Y.) Medical Center. He reported that he is a paid consultant for Arbor Pharmaceuticals and is a speaker for Abbott Laboratories and Gilead Sciences.
The recommendation to terminate FAME 2 by the independent data and safety monitoring board at 7 months’ follow-up was based solely on one highly significant treatment difference. That difference was in the end point of urgent revascularization, which was performed in 49 patients in the group that received the best available medical therapy alone vs. 7 patients in the group that underwent percutaneous coronary intervention and also received the best available medical therapy, Dr. William E. Boden wrote in an editorial accompanying the FAME 2 report (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMe1208620]).
"There were very few ‘hard’ events overall, with only four deaths (three in the medical-therapy group and one in the PCI group) and 29 myocardial infarctions (14 in the medical-therapy group and 15 in the PCI group). Of note, the definition of urgent revascularization was largely a clinical one and did not require evidence of ischemia or positive cardiac biomarkers in all patients; 29 of the 56 unplanned revascularizations (52%) were classified solely on the basis of clinical features, whereas in an exploratory subgroup analysis of the remaining 27 patients, there were fewer revascularizations triggered by a myocardial infarction or electrocardiographic evidence of ischemia in the PCI group than in the medical-therapy group," wrote Dr. Boden.
"Clearly, FFR [fractional flow reserve] holds potential promise for a more targeted approach to PCI that might be more clinically effective and cost effective than visually directed PCI for all angiographically significant stenoses," he continued. "Unfortunately, the early termination of the FAME 2 trial before full enrollment and follow-up were achieved, the neutral effects on the rate of death or myocardial infarction, and the lack of a significant, sustained treatment effect on the reduction of angina beyond 6 months leave more questions than answers."
The FAME 2 and COURAGE [Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation] trials are remarkably similar and showed that PCI reduced only the need for revascularization; in the COURAGE trial, there was a significant 40% reduction, whereas "neither the FAME 2 trial (with a mean 7 months of follow-up) nor the COURAGE trial (with a mean 55 months of follow-up) showed a benefit from PCI with respect to a reduction in the rate of death or myocardial infarction. The FAME 2 trial sought to establish the scientific basis for an FFR-guided PCI strategy for all functionally significant stenoses, but the results make this prospect somewhat unappealing," he wrote. Dr. Boden was the lead author of the COURAGE trial.
Current practice guidelines advocate the selective use of FFR to guide PCI decision making regarding borderline visual lesions (approximately 50%-70% stenosis). "It seems likely that the more routine use of FFR for all angiographically-significant stenoses would add considerable time, cost, and complexity to each PCI procedure and might also increase the risk of catheter-related complications such as coronary dissection and perforation," Dr. Boden pointed out.
Some of the uncertainty arising from FAME 2 may be resolved with the results of the ongoing ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial. The study is designed and powered to evaluate the long-term superiority of revascularization plus the best available medical therapy as compared with the best available medical therapy alone with respect to cardiovascular death or MI in patients with stable coronary artery disease and moderate-to-severe myocardial ischemia documented by means of noninvasive measures. "Until the results of ISCHEMIA are available, the case for a more durable clinical benefit of PCI beyond relief of angina or a reduction in the rate of subsequent revascularization is likely to remain both elusive and illusory," concluded Dr. Boden, who is a coprincipal investigator of ISCHEMIA.
Dr. Boden is the chief of medicine at the Albany Stratton Veterans Affairs Medical Center and vice chair of the department of medicine at Albany (N.Y.) Medical Center. He reported that he is a paid consultant for Arbor Pharmaceuticals and is a speaker for Abbott Laboratories and Gilead Sciences.
The use of fractional flow reserve to guide percutaneous coronary intervention, along with best medical management, sharply reduced the need for urgent revascularization in patients with stable coronary artery disease and at least one physiologically significant lesion.
However, FFR-guided percutaneous coronary intervention (PCI) had little effect on deaths or myocardial infarctions, when compared with best medical management alone, according to the results of the FAME 2 (Fractional Flow Reserve vs. Angiography for Multivessel Evaluation 2) trial, which was conducted at 28 sites in Europe and North America and halted early.
The percentage of patients who had an MI, death, or urgent revascularization (the combined primary end point) was significantly lower in the PCI group than in the medical therapy group (4.3% vs.12.7%; hazard ratio with PCI, 0.32). This difference was driven by a 13-fold increase in the need for urgent revascularization in the medical-therapy group. Notably, the rate of death from any cause and the rate of MI did not differ significantly between the PCI group and the medical therapy group.
Importantly, patient recruitment was stopped on Jan. 15, 2012, at the recommendation of an independent data and safety monitoring board because of the highly significant difference in the incidence rates of the primary end point between the PCI and medical-therapy groups.
The results of the study were released in the New England Journal of Medicine on Aug. 28 to coincide with the presentation of the study at the annual congress of the European Society of Cardiology (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMoa1205361]).
A total of 1,220 patients out a planned 1,832 were enrolled. Of those, 888 patients had at least one stenosis with an FFR of 0.80 or less: 447 patients were randomly assigned to FFR-guided PCI plus the best available medical therapy, and 441 patients to the best available medical therapy alone. The 332 patients with angiographically significant stenoses, but none with an FFR of 0.80 or less were enrolled in the registry and received the best available medical therapy alone. The mean duration of follow-up was 212 days.
Patients in stable condition who were appropriate candidates for PCI and who had angiographically assessed one-, two-, or three-vessel coronary artery disease suitable for PCI were included in the trial.
All patients were prescribed aspirin at a dose of 80-325 mg daily, metoprolol at a dose of 50 mg-200 mg daily (or any other beta-blocker), lisinopril (at least 5 mg daily, or another ACE inhibitor or an angiotensin receptor blocker)and atorvastatin (20-80 mg daily, or another statin).
All PCI patients were treated with second-generation drug-eluting stents.
Among the 56 patients who underwent urgent revascularization, the procedure was triggered by a MI in 12 patients (21%), by unstable angina accompanied by evidence of ischemia on ECG in 15 patients (27%), and by unstable angina diagnosed on the basis of clinical features in 29 patients (52%).
Patients in the PCI group were 86% less likely to undergo any revascularization and 83% less likely to undergo or nonurgent revascularization than were those in the medical therapy group.
The researchers identified several factors that may explain the differences between results in the present study and those in previous trials involving patients with stable coronary disease. "First, in previous trials in which various revascularization methods were compared with the best available medical therapy, patient enrollment was based primarily on angiographic findings, with or without noninvasive documentation of ischemia. It is likely that a sizable proportion of the patients had only limited ischemia," wrote lead investigator Dr. Bernard B. De Bruyne and his coinvestigators. Dr. De Bruyne is the codirector of the Cardiovascular Center at OLV Hospital in Aalst, Belgium.
"Even in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial, in which noninvasive testing was performed in 85% of the patients, less than one-third of the patients had more than 10% ischemia on myocardial perfusion imaging. In daily clinical practice, less than half of patients undergo noninvasive stress testing before elective PCI. In the current trial, all the patients who underwent randomization had at least one functionally significant stenosis," they observed (N. Engl. J. Med. 2007;356:1503-16).
Second, PCI was performed only in lesions with an FFR of 0.80 or less. "This FFR-guided approach is associated with a better clinical outcome than that with PCI performed on the basis of angiographic results alone. These features probably explain the similarity of event rates between patients who were treated with PCI plus the best available medical therapy and patients with equivalent baseline characteristics but no functionally significant lesions who were enrolled in the registry and treated with the best available medical therapy alone," according to the investigators.
Third, second-generation drug-eluting stents were used in PCIs. This strategy is associated with a low number of repeat revascularizations. Finally, the primary end point included urgent revascularization, a component that was not included in the primary end point of previous trials.
The study was sponsored by St. Jude Medical, which makes the two pressure wires used in the trial. The company was involved in the collection and source verification of the data but not in the conduct of the trial. Dr. De Bruyne reported receiving consulting/honorarium and travel fees from St. Jude Medical. Most of the investigators had significant financial relationships with St. Jude Medical, as well as with other device and pharmaceutical companies. One author is an employee of St. Jude Medical.
The use of fractional flow reserve to guide percutaneous coronary intervention, along with best medical management, sharply reduced the need for urgent revascularization in patients with stable coronary artery disease and at least one physiologically significant lesion.
However, FFR-guided percutaneous coronary intervention (PCI) had little effect on deaths or myocardial infarctions, when compared with best medical management alone, according to the results of the FAME 2 (Fractional Flow Reserve vs. Angiography for Multivessel Evaluation 2) trial, which was conducted at 28 sites in Europe and North America and halted early.
The percentage of patients who had an MI, death, or urgent revascularization (the combined primary end point) was significantly lower in the PCI group than in the medical therapy group (4.3% vs.12.7%; hazard ratio with PCI, 0.32). This difference was driven by a 13-fold increase in the need for urgent revascularization in the medical-therapy group. Notably, the rate of death from any cause and the rate of MI did not differ significantly between the PCI group and the medical therapy group.
Importantly, patient recruitment was stopped on Jan. 15, 2012, at the recommendation of an independent data and safety monitoring board because of the highly significant difference in the incidence rates of the primary end point between the PCI and medical-therapy groups.
The results of the study were released in the New England Journal of Medicine on Aug. 28 to coincide with the presentation of the study at the annual congress of the European Society of Cardiology (N. Engl. J. Med. 2012 Aug. 28 [doi:10.1056/NEJMoa1205361]).
A total of 1,220 patients out a planned 1,832 were enrolled. Of those, 888 patients had at least one stenosis with an FFR of 0.80 or less: 447 patients were randomly assigned to FFR-guided PCI plus the best available medical therapy, and 441 patients to the best available medical therapy alone. The 332 patients with angiographically significant stenoses, but none with an FFR of 0.80 or less were enrolled in the registry and received the best available medical therapy alone. The mean duration of follow-up was 212 days.
Patients in stable condition who were appropriate candidates for PCI and who had angiographically assessed one-, two-, or three-vessel coronary artery disease suitable for PCI were included in the trial.
All patients were prescribed aspirin at a dose of 80-325 mg daily, metoprolol at a dose of 50 mg-200 mg daily (or any other beta-blocker), lisinopril (at least 5 mg daily, or another ACE inhibitor or an angiotensin receptor blocker)and atorvastatin (20-80 mg daily, or another statin).
All PCI patients were treated with second-generation drug-eluting stents.
Among the 56 patients who underwent urgent revascularization, the procedure was triggered by a MI in 12 patients (21%), by unstable angina accompanied by evidence of ischemia on ECG in 15 patients (27%), and by unstable angina diagnosed on the basis of clinical features in 29 patients (52%).
Patients in the PCI group were 86% less likely to undergo any revascularization and 83% less likely to undergo or nonurgent revascularization than were those in the medical therapy group.
The researchers identified several factors that may explain the differences between results in the present study and those in previous trials involving patients with stable coronary disease. "First, in previous trials in which various revascularization methods were compared with the best available medical therapy, patient enrollment was based primarily on angiographic findings, with or without noninvasive documentation of ischemia. It is likely that a sizable proportion of the patients had only limited ischemia," wrote lead investigator Dr. Bernard B. De Bruyne and his coinvestigators. Dr. De Bruyne is the codirector of the Cardiovascular Center at OLV Hospital in Aalst, Belgium.
"Even in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial, in which noninvasive testing was performed in 85% of the patients, less than one-third of the patients had more than 10% ischemia on myocardial perfusion imaging. In daily clinical practice, less than half of patients undergo noninvasive stress testing before elective PCI. In the current trial, all the patients who underwent randomization had at least one functionally significant stenosis," they observed (N. Engl. J. Med. 2007;356:1503-16).
Second, PCI was performed only in lesions with an FFR of 0.80 or less. "This FFR-guided approach is associated with a better clinical outcome than that with PCI performed on the basis of angiographic results alone. These features probably explain the similarity of event rates between patients who were treated with PCI plus the best available medical therapy and patients with equivalent baseline characteristics but no functionally significant lesions who were enrolled in the registry and treated with the best available medical therapy alone," according to the investigators.
Third, second-generation drug-eluting stents were used in PCIs. This strategy is associated with a low number of repeat revascularizations. Finally, the primary end point included urgent revascularization, a component that was not included in the primary end point of previous trials.
The study was sponsored by St. Jude Medical, which makes the two pressure wires used in the trial. The company was involved in the collection and source verification of the data but not in the conduct of the trial. Dr. De Bruyne reported receiving consulting/honorarium and travel fees from St. Jude Medical. Most of the investigators had significant financial relationships with St. Jude Medical, as well as with other device and pharmaceutical companies. One author is an employee of St. Jude Medical.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: The percentage of patients who had an MI, death, or urgent revascularization (the combined primary end point) was significantly lower in patients who underwent FFR-guided PCI than in patients who received best medical management alone (4.3% vs.12.7%; hazard ratio with PCI, 0.32). This difference was driven by a 13-fold increase in the need for urgent revascularization in the medical therapy group.
Data Source: Data are from the FAME 2 trial, in 1,220 stable patients who had angiographically assessed coronary artery disease and were appropriate candidates for PCI. The trial was stopped early because of a highly significant difference in the primary outcome.
Disclosures: The study was sponsored by St. Jude Medical. Dr. De Bruyne reported receiving consulting/honorarium and travel fees from St. Jude Medical. Most of the investigators had significant financial relationships with St. Jude Medical, as well as with other device and pharmaceutical companies. One author is an employee of St. Jude Medical.
No Benefit of Balloon Pump in Acute MI With Shock
MUNICH – Although it is routinely used in clinical practice, the intra-aortic balloon pump provided no early mortality benefit in patients with myocardial infarction complicated by cardiogenic shock in the randomized IABP-SHOCK II study.
The primary end point of 30-day all-cause mortality was 41.3% in controls and 39.7% in patients receiving intra-aortic balloon pump (IABP) support, a difference that was not significant. None of the subgroups that were analyzed derived benefit.
Use of an IABP also failed to improve any of the secondary outcomes of the trial, the largest to date in patients with cardiogenic shock, Dr. Holger Thiele reported at the annual congress of the European Society of Cardiology (ESC).
However, "it’s too early to say that it’s the end of the pump," Dr. Thiele said in an interview. "Before we close this chapter, I think we have to wait for long-term follow-up data."
While awaiting 6- and 12-month mortality data, which could be reported by the end of 2013, use of IABPs is likely to go down because of the negative results of IABP-SHOCK II (Intraaortic Balloon Pump in Cardiogenic Shock II), he said.
Discussant Dr. Uta Hoppe, of the Paracelsus Medical University of Salzburg, Austria, agreed that it’s unlikely clinicians can improve the outcome of patients by implanting more IABPs.
"These data rather show that IABPs are not useful for most of these patients, and we still have to define the individuals that might derive benefit," she said. "Particularly, if the long-term data would support and confirm this neutral effect of IABP, I think that our guidelines have to be reconsidered."
Before the trial, IABP results were available from registries and only one randomized controlled trial of just 57 patients. Results were mixed, possibly explaining why the IABP is currently used in only about 35% of cardiogenic shock patients in Europe and 39% in the United States, said Dr. Thiele, professor of medicine at the University of Leipzig (Germany) Heart Center.
Despite the limited data, IABPs became part of contemporary practice and were carried forward through various iterations of the ESC guidelines and American College of Cardiology/American Heart Association guidelines with a class I recommendation.
The lack of solid data, however, was likely behind the decision to downgrade the IABP recommendation to IIb in the new ESC guidelines for ST-segment elevation acute MI, presented just 24 hours earlier at the meeting, Dr. Thiele said. It was also the impetus for IABP-SHOCK II.
In the trial, investigators at 37 German sites randomized 600 acute MI patients in cardiogenic shock to either percutaneous coronary intervention plus IABP insertion and optimal medical therapy or PCI plus medical therapy only.
Nearly 50% of patients underwent resuscitation before randomization, 80% had mild vessel disease that was the cause of the shock, and 96% underwent primary PCI. Notably, the timing of pump insertion was left up to the investigators, with 87% of IABPs inserted after the procedure.
There were no significant differences between groups in the secondary outcomes of renal function, serum lactate, and inflammatory reaction, Dr. Thiele said. There was a significant benefit on the Simplified Acute Physiology Score-II intensive care instrument, favoring the balloon pump on day 2 and day 3 post procedure, but this was attenuated and no longer significant on day 4.
Dr. Thiele said in an interview that he will likely stop using IABPs in cardiogenic shock patients because the trial has shown that 60% of patients will not need anything else, if treated according to guidelines with early revascularization and optimal management.
He went on to say that, although some may be tempted to turn to left ventricular assist devices in high-risk patients, data are almost nonexistent comparing assist devices with the balloon pump. Only 5.5% of patients received LVADs in IABP-SHOCK II, and mortality was high at 67%. "Nevertheless, if you have a young patient who is not responding to the standard therapy, then I would always put in such a percutaneous left ventricular assist device," he added.
The study was simultaneously published in the New England Journal of Medicine (2012 Aug. 27 [doi: 10.1056/NEJMoa1208410]).
In an accompanying editorial (2012 Aug. 27 [doi: 10.1056/NEJMe1209601]), Dr. Christopher M. O’Connor and Dr. Joseph G. Rogers, both of Duke University in Durham, N.C., called the results surprising, and said that "on the basis of the findings of the IABP-SHOCK II trial, we must move forward with the understanding that a cardiovascular condition with 40% mortality at 30 days remains unacceptable."
Dr. Thiele reported research funding from several pharmaceutical and device firms. Dr. Hoppe did not provide disclosures. The trial was funded by the German Research Foundation, the German Heart Research Foundation, and other organizations, as well as by Maquet Cardiopulmonary and Teleflex Medical.
MUNICH – Although it is routinely used in clinical practice, the intra-aortic balloon pump provided no early mortality benefit in patients with myocardial infarction complicated by cardiogenic shock in the randomized IABP-SHOCK II study.
The primary end point of 30-day all-cause mortality was 41.3% in controls and 39.7% in patients receiving intra-aortic balloon pump (IABP) support, a difference that was not significant. None of the subgroups that were analyzed derived benefit.
Use of an IABP also failed to improve any of the secondary outcomes of the trial, the largest to date in patients with cardiogenic shock, Dr. Holger Thiele reported at the annual congress of the European Society of Cardiology (ESC).
However, "it’s too early to say that it’s the end of the pump," Dr. Thiele said in an interview. "Before we close this chapter, I think we have to wait for long-term follow-up data."
While awaiting 6- and 12-month mortality data, which could be reported by the end of 2013, use of IABPs is likely to go down because of the negative results of IABP-SHOCK II (Intraaortic Balloon Pump in Cardiogenic Shock II), he said.
Discussant Dr. Uta Hoppe, of the Paracelsus Medical University of Salzburg, Austria, agreed that it’s unlikely clinicians can improve the outcome of patients by implanting more IABPs.
"These data rather show that IABPs are not useful for most of these patients, and we still have to define the individuals that might derive benefit," she said. "Particularly, if the long-term data would support and confirm this neutral effect of IABP, I think that our guidelines have to be reconsidered."
Before the trial, IABP results were available from registries and only one randomized controlled trial of just 57 patients. Results were mixed, possibly explaining why the IABP is currently used in only about 35% of cardiogenic shock patients in Europe and 39% in the United States, said Dr. Thiele, professor of medicine at the University of Leipzig (Germany) Heart Center.
Despite the limited data, IABPs became part of contemporary practice and were carried forward through various iterations of the ESC guidelines and American College of Cardiology/American Heart Association guidelines with a class I recommendation.
The lack of solid data, however, was likely behind the decision to downgrade the IABP recommendation to IIb in the new ESC guidelines for ST-segment elevation acute MI, presented just 24 hours earlier at the meeting, Dr. Thiele said. It was also the impetus for IABP-SHOCK II.
In the trial, investigators at 37 German sites randomized 600 acute MI patients in cardiogenic shock to either percutaneous coronary intervention plus IABP insertion and optimal medical therapy or PCI plus medical therapy only.
Nearly 50% of patients underwent resuscitation before randomization, 80% had mild vessel disease that was the cause of the shock, and 96% underwent primary PCI. Notably, the timing of pump insertion was left up to the investigators, with 87% of IABPs inserted after the procedure.
There were no significant differences between groups in the secondary outcomes of renal function, serum lactate, and inflammatory reaction, Dr. Thiele said. There was a significant benefit on the Simplified Acute Physiology Score-II intensive care instrument, favoring the balloon pump on day 2 and day 3 post procedure, but this was attenuated and no longer significant on day 4.
Dr. Thiele said in an interview that he will likely stop using IABPs in cardiogenic shock patients because the trial has shown that 60% of patients will not need anything else, if treated according to guidelines with early revascularization and optimal management.
He went on to say that, although some may be tempted to turn to left ventricular assist devices in high-risk patients, data are almost nonexistent comparing assist devices with the balloon pump. Only 5.5% of patients received LVADs in IABP-SHOCK II, and mortality was high at 67%. "Nevertheless, if you have a young patient who is not responding to the standard therapy, then I would always put in such a percutaneous left ventricular assist device," he added.
The study was simultaneously published in the New England Journal of Medicine (2012 Aug. 27 [doi: 10.1056/NEJMoa1208410]).
In an accompanying editorial (2012 Aug. 27 [doi: 10.1056/NEJMe1209601]), Dr. Christopher M. O’Connor and Dr. Joseph G. Rogers, both of Duke University in Durham, N.C., called the results surprising, and said that "on the basis of the findings of the IABP-SHOCK II trial, we must move forward with the understanding that a cardiovascular condition with 40% mortality at 30 days remains unacceptable."
Dr. Thiele reported research funding from several pharmaceutical and device firms. Dr. Hoppe did not provide disclosures. The trial was funded by the German Research Foundation, the German Heart Research Foundation, and other organizations, as well as by Maquet Cardiopulmonary and Teleflex Medical.
MUNICH – Although it is routinely used in clinical practice, the intra-aortic balloon pump provided no early mortality benefit in patients with myocardial infarction complicated by cardiogenic shock in the randomized IABP-SHOCK II study.
The primary end point of 30-day all-cause mortality was 41.3% in controls and 39.7% in patients receiving intra-aortic balloon pump (IABP) support, a difference that was not significant. None of the subgroups that were analyzed derived benefit.
Use of an IABP also failed to improve any of the secondary outcomes of the trial, the largest to date in patients with cardiogenic shock, Dr. Holger Thiele reported at the annual congress of the European Society of Cardiology (ESC).
However, "it’s too early to say that it’s the end of the pump," Dr. Thiele said in an interview. "Before we close this chapter, I think we have to wait for long-term follow-up data."
While awaiting 6- and 12-month mortality data, which could be reported by the end of 2013, use of IABPs is likely to go down because of the negative results of IABP-SHOCK II (Intraaortic Balloon Pump in Cardiogenic Shock II), he said.
Discussant Dr. Uta Hoppe, of the Paracelsus Medical University of Salzburg, Austria, agreed that it’s unlikely clinicians can improve the outcome of patients by implanting more IABPs.
"These data rather show that IABPs are not useful for most of these patients, and we still have to define the individuals that might derive benefit," she said. "Particularly, if the long-term data would support and confirm this neutral effect of IABP, I think that our guidelines have to be reconsidered."
Before the trial, IABP results were available from registries and only one randomized controlled trial of just 57 patients. Results were mixed, possibly explaining why the IABP is currently used in only about 35% of cardiogenic shock patients in Europe and 39% in the United States, said Dr. Thiele, professor of medicine at the University of Leipzig (Germany) Heart Center.
Despite the limited data, IABPs became part of contemporary practice and were carried forward through various iterations of the ESC guidelines and American College of Cardiology/American Heart Association guidelines with a class I recommendation.
The lack of solid data, however, was likely behind the decision to downgrade the IABP recommendation to IIb in the new ESC guidelines for ST-segment elevation acute MI, presented just 24 hours earlier at the meeting, Dr. Thiele said. It was also the impetus for IABP-SHOCK II.
In the trial, investigators at 37 German sites randomized 600 acute MI patients in cardiogenic shock to either percutaneous coronary intervention plus IABP insertion and optimal medical therapy or PCI plus medical therapy only.
Nearly 50% of patients underwent resuscitation before randomization, 80% had mild vessel disease that was the cause of the shock, and 96% underwent primary PCI. Notably, the timing of pump insertion was left up to the investigators, with 87% of IABPs inserted after the procedure.
There were no significant differences between groups in the secondary outcomes of renal function, serum lactate, and inflammatory reaction, Dr. Thiele said. There was a significant benefit on the Simplified Acute Physiology Score-II intensive care instrument, favoring the balloon pump on day 2 and day 3 post procedure, but this was attenuated and no longer significant on day 4.
Dr. Thiele said in an interview that he will likely stop using IABPs in cardiogenic shock patients because the trial has shown that 60% of patients will not need anything else, if treated according to guidelines with early revascularization and optimal management.
He went on to say that, although some may be tempted to turn to left ventricular assist devices in high-risk patients, data are almost nonexistent comparing assist devices with the balloon pump. Only 5.5% of patients received LVADs in IABP-SHOCK II, and mortality was high at 67%. "Nevertheless, if you have a young patient who is not responding to the standard therapy, then I would always put in such a percutaneous left ventricular assist device," he added.
The study was simultaneously published in the New England Journal of Medicine (2012 Aug. 27 [doi: 10.1056/NEJMoa1208410]).
In an accompanying editorial (2012 Aug. 27 [doi: 10.1056/NEJMe1209601]), Dr. Christopher M. O’Connor and Dr. Joseph G. Rogers, both of Duke University in Durham, N.C., called the results surprising, and said that "on the basis of the findings of the IABP-SHOCK II trial, we must move forward with the understanding that a cardiovascular condition with 40% mortality at 30 days remains unacceptable."
Dr. Thiele reported research funding from several pharmaceutical and device firms. Dr. Hoppe did not provide disclosures. The trial was funded by the German Research Foundation, the German Heart Research Foundation, and other organizations, as well as by Maquet Cardiopulmonary and Teleflex Medical.
AT THE ANNUAL CONGRESS OF THE EUROPEAN SOCIETY OF CARDIOLOGY
Major Finding: The primary end point of 30-day all-cause mortality was 41.3% in controls and 39.7% in patients receiving IABP support, a nonsignificant difference.
Data Source: IABP-SHOCK II was a phase IV trial that randomized 600 acute MI patients in cardiogenic shock to either PCI plus IABP insertion and optimal medical therapy or PCI plus medical therapy only.
Disclosures: Dr. Thiele reported research funding from several pharmaceutical and device firms. Dr. Hoppe did not provide disclosures. The trial was funded by the German Research Foundation, the German Heart Research Foundation, and other organizations, as well as by Maquet Cardiopulmonary and Teleflex Medical.