User login
American Society of Hematology (ASH): ASH 2016
PERSIST-2 might allay some concerns about pacritinib in myelofibrosis
SAN DIEGO – Late-breaking results from the phase III PERSIST-2 trial may ease at least some safety concerns surrounding the use of pacritinib in patients with myelofibrosis, investigators said at the annual meeting of the American Society of Hematology.
In February 2016, the Food and Drug Administration imposed a clinical hold on studies of pacritinib in the wake of concerns about excess deaths, cardiotoxicities, and hemorrhage. But in the final data analysis presented at ASH, rates of these outcomes were low and similar among patients randomized to pacritinib once daily, pacritinib twice daily, or best available treatment for myelofibrosis, including ruxolitinib, lead investigator John Mascarenhas, MD, said.
Indeed, more patients died of progressive disease after stopping pacritinib than died of treatment-associated adverse events, said Dr. Mascarenhas of Icahn School of Medicine at Mount Sinai, New York.
Pacritinib is an oral kinase inhibitor with specificity for JAK2, FLT3, IRAK1, and CFS1R. In the previous phase III PERSIST-1 trial, patients who received pacritinib had a fourfold greater probability of experiencing at least a 35% decrease in splenic volume than did patients who received best available treatment (P = .003).
PERSIST-2 also yielded clear efficacy signals, particularly when patients took pacritinib twice daily, said Dr. Mascarenhas. Between baseline and week 24, splenic volume dropped by at least 35% in 22% of these patients (95% confidence interval, 13%-33%), compared with 3% of patients on best available treatment (95% CI, 0.3%-10%; P = .001). Patients who took pacritinib twice daily also had a 32% (95% CI, 22%-44%) chance of experiencing at least a 50% drop in symptoms such as fatigue, bone pain, itching, and abdominal pain, compared with 14% (95% CI, 7%-24%) of patients on best available treatment (P = .01).
Demographic and disease risk characteristics did not significantly affect the chances of reaching these coprimary endpoints, Dr. Mascarenhas noted. “My humble opinion as a clinical investigator is that [pacritinib] is an effective drug, with a favorable benefit-to-risk ratio,” he said.
Several hematologists who were not involved in this trial agreed. “I don’t see why you are nervous [about presenting these results],” noted hematologist Kanti Rai, MD, of the Feinstein Institute for Medical Research in Manhasset, N.Y., told Dr. Mascarenhas during the discussion after the data were presented, prompting laughter from the audience.
It remains to be seen whether the FDA will find the data convincing enough to lift the clinical hold on pacritinib. Ruxolitinib (Jakafi) is approved to treat splenomegaly and symptom burden in myelofibrosis but is associated with dose-limiting cytopenias and cannot be used in patients with platelet counts of less than 50,000/mcL.
PERSIST-2 compared pacritinib 400 mg once daily with pacritinib 200 mg twice daily and best available treatment, including ruxolitinib, in patients with primary or secondary myelofibrosis and less than 100,000 platelets/mcL. About half of the study patients had less than 50,000 platelets/mcL, and more than 40% had previously received ruxolitinib.
When the clinical hold on pacritinib went into effect, 221 patients had reached the 24-week designated study endpoint and were included in the intention-to-treat analysis, Dr. Mascarenhas reported. Censored Kaplan-Meier curves of overall survival favored pacritinib over best available treatment, although the difference in survival rates did not reach statistical significance (hazard ratio, 0.68; 95% CI, 0.3-1.5). A total of 9% of patients in the twice-daily pacritinib group died, compared with 14% of patients receiving pacritinib once daily or best available treatment.
Twice-daily pacritinib most often led to diarrhea (48% of patients), nausea (32%), thrombocytopenia (34%), and anemia (24%). Overall rates of serious treatment-emergent adverse events were seen in 47% of the two pacritinib groups and in 31% of patients receiving best available treatment. The most common serious treatment-emergent adverse event with twice daily pacritinib was anemia (8% of patients), followed by thrombocytopenia and pneumonia (6%). Heart failure, atrial fibrillation, and cardiac arrest were rare and similar across all three treatment groups, as were epistaxis and subdural hematoma.
This is the first randomized, controlled trial of patients with myelofibrosis and thrombocytopenia, according to Dr. Mascarenhas. “This was a patient population with low platelets and at risk of poor outcomes, and they did pretty well,” he said. “There really is no therapeutic option for patients with myelofibrosis and low platelets, and [pacritinib] offers patients in this vulnerable situation an opportunity for symptom relief. I hope to see it move forward.”
CTI Biopharma sponsored the study. Dr. Mascarenhas disclosed research funding from CTI Biopharma.
SAN DIEGO – Late-breaking results from the phase III PERSIST-2 trial may ease at least some safety concerns surrounding the use of pacritinib in patients with myelofibrosis, investigators said at the annual meeting of the American Society of Hematology.
In February 2016, the Food and Drug Administration imposed a clinical hold on studies of pacritinib in the wake of concerns about excess deaths, cardiotoxicities, and hemorrhage. But in the final data analysis presented at ASH, rates of these outcomes were low and similar among patients randomized to pacritinib once daily, pacritinib twice daily, or best available treatment for myelofibrosis, including ruxolitinib, lead investigator John Mascarenhas, MD, said.
Indeed, more patients died of progressive disease after stopping pacritinib than died of treatment-associated adverse events, said Dr. Mascarenhas of Icahn School of Medicine at Mount Sinai, New York.
Pacritinib is an oral kinase inhibitor with specificity for JAK2, FLT3, IRAK1, and CFS1R. In the previous phase III PERSIST-1 trial, patients who received pacritinib had a fourfold greater probability of experiencing at least a 35% decrease in splenic volume than did patients who received best available treatment (P = .003).
PERSIST-2 also yielded clear efficacy signals, particularly when patients took pacritinib twice daily, said Dr. Mascarenhas. Between baseline and week 24, splenic volume dropped by at least 35% in 22% of these patients (95% confidence interval, 13%-33%), compared with 3% of patients on best available treatment (95% CI, 0.3%-10%; P = .001). Patients who took pacritinib twice daily also had a 32% (95% CI, 22%-44%) chance of experiencing at least a 50% drop in symptoms such as fatigue, bone pain, itching, and abdominal pain, compared with 14% (95% CI, 7%-24%) of patients on best available treatment (P = .01).
Demographic and disease risk characteristics did not significantly affect the chances of reaching these coprimary endpoints, Dr. Mascarenhas noted. “My humble opinion as a clinical investigator is that [pacritinib] is an effective drug, with a favorable benefit-to-risk ratio,” he said.
Several hematologists who were not involved in this trial agreed. “I don’t see why you are nervous [about presenting these results],” noted hematologist Kanti Rai, MD, of the Feinstein Institute for Medical Research in Manhasset, N.Y., told Dr. Mascarenhas during the discussion after the data were presented, prompting laughter from the audience.
It remains to be seen whether the FDA will find the data convincing enough to lift the clinical hold on pacritinib. Ruxolitinib (Jakafi) is approved to treat splenomegaly and symptom burden in myelofibrosis but is associated with dose-limiting cytopenias and cannot be used in patients with platelet counts of less than 50,000/mcL.
PERSIST-2 compared pacritinib 400 mg once daily with pacritinib 200 mg twice daily and best available treatment, including ruxolitinib, in patients with primary or secondary myelofibrosis and less than 100,000 platelets/mcL. About half of the study patients had less than 50,000 platelets/mcL, and more than 40% had previously received ruxolitinib.
When the clinical hold on pacritinib went into effect, 221 patients had reached the 24-week designated study endpoint and were included in the intention-to-treat analysis, Dr. Mascarenhas reported. Censored Kaplan-Meier curves of overall survival favored pacritinib over best available treatment, although the difference in survival rates did not reach statistical significance (hazard ratio, 0.68; 95% CI, 0.3-1.5). A total of 9% of patients in the twice-daily pacritinib group died, compared with 14% of patients receiving pacritinib once daily or best available treatment.
Twice-daily pacritinib most often led to diarrhea (48% of patients), nausea (32%), thrombocytopenia (34%), and anemia (24%). Overall rates of serious treatment-emergent adverse events were seen in 47% of the two pacritinib groups and in 31% of patients receiving best available treatment. The most common serious treatment-emergent adverse event with twice daily pacritinib was anemia (8% of patients), followed by thrombocytopenia and pneumonia (6%). Heart failure, atrial fibrillation, and cardiac arrest were rare and similar across all three treatment groups, as were epistaxis and subdural hematoma.
This is the first randomized, controlled trial of patients with myelofibrosis and thrombocytopenia, according to Dr. Mascarenhas. “This was a patient population with low platelets and at risk of poor outcomes, and they did pretty well,” he said. “There really is no therapeutic option for patients with myelofibrosis and low platelets, and [pacritinib] offers patients in this vulnerable situation an opportunity for symptom relief. I hope to see it move forward.”
CTI Biopharma sponsored the study. Dr. Mascarenhas disclosed research funding from CTI Biopharma.
SAN DIEGO – Late-breaking results from the phase III PERSIST-2 trial may ease at least some safety concerns surrounding the use of pacritinib in patients with myelofibrosis, investigators said at the annual meeting of the American Society of Hematology.
In February 2016, the Food and Drug Administration imposed a clinical hold on studies of pacritinib in the wake of concerns about excess deaths, cardiotoxicities, and hemorrhage. But in the final data analysis presented at ASH, rates of these outcomes were low and similar among patients randomized to pacritinib once daily, pacritinib twice daily, or best available treatment for myelofibrosis, including ruxolitinib, lead investigator John Mascarenhas, MD, said.
Indeed, more patients died of progressive disease after stopping pacritinib than died of treatment-associated adverse events, said Dr. Mascarenhas of Icahn School of Medicine at Mount Sinai, New York.
Pacritinib is an oral kinase inhibitor with specificity for JAK2, FLT3, IRAK1, and CFS1R. In the previous phase III PERSIST-1 trial, patients who received pacritinib had a fourfold greater probability of experiencing at least a 35% decrease in splenic volume than did patients who received best available treatment (P = .003).
PERSIST-2 also yielded clear efficacy signals, particularly when patients took pacritinib twice daily, said Dr. Mascarenhas. Between baseline and week 24, splenic volume dropped by at least 35% in 22% of these patients (95% confidence interval, 13%-33%), compared with 3% of patients on best available treatment (95% CI, 0.3%-10%; P = .001). Patients who took pacritinib twice daily also had a 32% (95% CI, 22%-44%) chance of experiencing at least a 50% drop in symptoms such as fatigue, bone pain, itching, and abdominal pain, compared with 14% (95% CI, 7%-24%) of patients on best available treatment (P = .01).
Demographic and disease risk characteristics did not significantly affect the chances of reaching these coprimary endpoints, Dr. Mascarenhas noted. “My humble opinion as a clinical investigator is that [pacritinib] is an effective drug, with a favorable benefit-to-risk ratio,” he said.
Several hematologists who were not involved in this trial agreed. “I don’t see why you are nervous [about presenting these results],” noted hematologist Kanti Rai, MD, of the Feinstein Institute for Medical Research in Manhasset, N.Y., told Dr. Mascarenhas during the discussion after the data were presented, prompting laughter from the audience.
It remains to be seen whether the FDA will find the data convincing enough to lift the clinical hold on pacritinib. Ruxolitinib (Jakafi) is approved to treat splenomegaly and symptom burden in myelofibrosis but is associated with dose-limiting cytopenias and cannot be used in patients with platelet counts of less than 50,000/mcL.
PERSIST-2 compared pacritinib 400 mg once daily with pacritinib 200 mg twice daily and best available treatment, including ruxolitinib, in patients with primary or secondary myelofibrosis and less than 100,000 platelets/mcL. About half of the study patients had less than 50,000 platelets/mcL, and more than 40% had previously received ruxolitinib.
When the clinical hold on pacritinib went into effect, 221 patients had reached the 24-week designated study endpoint and were included in the intention-to-treat analysis, Dr. Mascarenhas reported. Censored Kaplan-Meier curves of overall survival favored pacritinib over best available treatment, although the difference in survival rates did not reach statistical significance (hazard ratio, 0.68; 95% CI, 0.3-1.5). A total of 9% of patients in the twice-daily pacritinib group died, compared with 14% of patients receiving pacritinib once daily or best available treatment.
Twice-daily pacritinib most often led to diarrhea (48% of patients), nausea (32%), thrombocytopenia (34%), and anemia (24%). Overall rates of serious treatment-emergent adverse events were seen in 47% of the two pacritinib groups and in 31% of patients receiving best available treatment. The most common serious treatment-emergent adverse event with twice daily pacritinib was anemia (8% of patients), followed by thrombocytopenia and pneumonia (6%). Heart failure, atrial fibrillation, and cardiac arrest were rare and similar across all three treatment groups, as were epistaxis and subdural hematoma.
This is the first randomized, controlled trial of patients with myelofibrosis and thrombocytopenia, according to Dr. Mascarenhas. “This was a patient population with low platelets and at risk of poor outcomes, and they did pretty well,” he said. “There really is no therapeutic option for patients with myelofibrosis and low platelets, and [pacritinib] offers patients in this vulnerable situation an opportunity for symptom relief. I hope to see it move forward.”
CTI Biopharma sponsored the study. Dr. Mascarenhas disclosed research funding from CTI Biopharma.
AT ASH 2016
Key clinical point: Pacritinib topped best available treatments for myelofibrosis and was not associated with increased risk of death or cardiac or bleeding events.
Major finding: Rates of death, cardiac events, and bleeding events were low and similar among groups. Splenic volume dropped by at least 35% in 22% of patients receiving twice daily pacritinib, compared with 3% of patients on best available treatment, including ruxolitinib (P = .001). Total symptom scores fell by at least 50% in 32% of patients receiving twice daily pacritinib and 14% of patients on best available treatment (P = .01).
Data source: A randomized phase III trial comparing pacritinib 400 mg once daily, pacritinib 200 mg twice daily, and best available treatment, including ruxolitinib, for 24 weeks in 221 patients with primary or secondary myelofibrosis and less than 100,000 platelets/mcL.
Disclosures: CTI Biopharma sponsored the study. Dr. Mascarenhas disclosed research funding from CTI Biopharma.
Adding epoetin alfa to lenalidomide boosted myelodysplastic syndrome responses
SAN DIEGO – Dual therapy with lenalidomide and epoetin alfa was safe and led to freedom from transfusion significantly more often than lenalidomide alone in patients with erythropoietin-refractory, lower-risk, non-del(5q) myelodysplastic syndromes, according to a randomized phase III head-to-head trial.
After 16 weeks of treatment, 33% of patients who received both lenalidomide and epoetin alfa met International Working Group 2000 criteria for major erythroid response, compared with only 14% of patients receiving lenalidomide monotherapy (P = .03), Alan F. List, MD, reported at the annual meeting of the American Society of Hematology.
Recombinant human erythropoietin improves anemia in some cases of MDS, but salvage options are limited. “Cytokine therapy is generally ineffective in patients with high transfusion burden or elevated serum erythropoietin level,” Dr. List said.
Lenalidomide (Revlimid) promotes the in vitro expansion of primitive erythroid precursors, and in a recent phase III, placebo-controlled trial, the immunomodulator improved erythropoiesis in about 25% of lower-risk, non-del(5q) MDS patients who were azanucleoside-naïve and transfusion-dependent, with effects lasting about 8 months. In another pilot study, adding epoetin alfa to lenalidomide induced erythroid responses in 28% of MDS patients who were not responding to lenalidomide alone. “This suggests that lenalidomide overcomes resistance and augments response to recombinant human erythropoietin,” Dr. List explained.
For their phase III trial, he and his associates randomly assigned erythropoietin-refractory, lower-risk, non-del(5q) MDS patients with hemoglobin levels under 9.5 g/dL to receive lenalidomide (10 mg per day for 21 days every 28 days) with or without epoetin alfa (weekly dose, 60,000 units subcutaneously). A total of 14% of patients had previously received azanucleoside therapy, about 92% had received erythropoietic stimulating agents, and median serum erythropoietin levels were 167 and 143 mU per mL in the monotherapy and dual therapy arms, respectively.
In accordance with International Working Group 2000 criteria, the researchers defined major erythroid response as transfusion independence for least 8 consecutive weeks, with at least a 1 g/dL increase in hemoglobin levels if patients were transfusion-dependent at baseline, and at least a 2 g/dL rise in hemoglobin if they were transfusion-independent.
In an interim analysis of 163 patients, 26% of the dual therapy group and 11% of lenalidomide-only patients met this primary endpoint (P = .02). These results met predefined criteria for stopping the study, after which 34 lenalidomide nonresponders crossed over to dual therapy. In all, 21% of these patients also had a major erythroid response, Dr. List said.
A multivariable analysis that included disease duration, International Prognostic Scoring System low versus intermediate-1 risk status, baseline erythropoietin level, and prior azanucleoside exposure showed that only dual lenalidomide–epoetin alfa therapy predicted major erythroid response. Specifically, dual therapy increased the odds of this outcome by about 63% when compared with lenalidomide monotherapy (P = .03).
Secondary analyses linked major erythroid response to having more low than high molecular weight CD45 isoform. In fact, the median ratio of high to low molecular weight CD45 was 1.5 among responders and 4.2 among nonresponders (P = .04) This finding fits the hypothesis that larger CD45 isoforms keep lenalidomide from enhancing erythropoietin receptor signaling, Dr. List said. Indeed, rates of major erythroid response to lenalidomide–epoetin alfa therapy were 73% when patients had a low isoform ratio, but were only 18% when they had a high isoform ratio (P = .03). The CD45 isoform ratio distinguished responders from nonresponders with a sensitivity and specificity of 80% and 75%, respectively, Dr. List said.
Grade 3 or higher nonhematologic events affected about a quarter of patients in each arm, and rates of individual events were similar. The most common serious adverse event was fatigue (5% of patients), followed by elevated serum creatinine (3.7%). About 10% of patients in each arm died while on study.
The National Institutes of Health supported the study. Dr. List had no relevant financial disclosures.
SAN DIEGO – Dual therapy with lenalidomide and epoetin alfa was safe and led to freedom from transfusion significantly more often than lenalidomide alone in patients with erythropoietin-refractory, lower-risk, non-del(5q) myelodysplastic syndromes, according to a randomized phase III head-to-head trial.
After 16 weeks of treatment, 33% of patients who received both lenalidomide and epoetin alfa met International Working Group 2000 criteria for major erythroid response, compared with only 14% of patients receiving lenalidomide monotherapy (P = .03), Alan F. List, MD, reported at the annual meeting of the American Society of Hematology.
Recombinant human erythropoietin improves anemia in some cases of MDS, but salvage options are limited. “Cytokine therapy is generally ineffective in patients with high transfusion burden or elevated serum erythropoietin level,” Dr. List said.
Lenalidomide (Revlimid) promotes the in vitro expansion of primitive erythroid precursors, and in a recent phase III, placebo-controlled trial, the immunomodulator improved erythropoiesis in about 25% of lower-risk, non-del(5q) MDS patients who were azanucleoside-naïve and transfusion-dependent, with effects lasting about 8 months. In another pilot study, adding epoetin alfa to lenalidomide induced erythroid responses in 28% of MDS patients who were not responding to lenalidomide alone. “This suggests that lenalidomide overcomes resistance and augments response to recombinant human erythropoietin,” Dr. List explained.
For their phase III trial, he and his associates randomly assigned erythropoietin-refractory, lower-risk, non-del(5q) MDS patients with hemoglobin levels under 9.5 g/dL to receive lenalidomide (10 mg per day for 21 days every 28 days) with or without epoetin alfa (weekly dose, 60,000 units subcutaneously). A total of 14% of patients had previously received azanucleoside therapy, about 92% had received erythropoietic stimulating agents, and median serum erythropoietin levels were 167 and 143 mU per mL in the monotherapy and dual therapy arms, respectively.
In accordance with International Working Group 2000 criteria, the researchers defined major erythroid response as transfusion independence for least 8 consecutive weeks, with at least a 1 g/dL increase in hemoglobin levels if patients were transfusion-dependent at baseline, and at least a 2 g/dL rise in hemoglobin if they were transfusion-independent.
In an interim analysis of 163 patients, 26% of the dual therapy group and 11% of lenalidomide-only patients met this primary endpoint (P = .02). These results met predefined criteria for stopping the study, after which 34 lenalidomide nonresponders crossed over to dual therapy. In all, 21% of these patients also had a major erythroid response, Dr. List said.
A multivariable analysis that included disease duration, International Prognostic Scoring System low versus intermediate-1 risk status, baseline erythropoietin level, and prior azanucleoside exposure showed that only dual lenalidomide–epoetin alfa therapy predicted major erythroid response. Specifically, dual therapy increased the odds of this outcome by about 63% when compared with lenalidomide monotherapy (P = .03).
Secondary analyses linked major erythroid response to having more low than high molecular weight CD45 isoform. In fact, the median ratio of high to low molecular weight CD45 was 1.5 among responders and 4.2 among nonresponders (P = .04) This finding fits the hypothesis that larger CD45 isoforms keep lenalidomide from enhancing erythropoietin receptor signaling, Dr. List said. Indeed, rates of major erythroid response to lenalidomide–epoetin alfa therapy were 73% when patients had a low isoform ratio, but were only 18% when they had a high isoform ratio (P = .03). The CD45 isoform ratio distinguished responders from nonresponders with a sensitivity and specificity of 80% and 75%, respectively, Dr. List said.
Grade 3 or higher nonhematologic events affected about a quarter of patients in each arm, and rates of individual events were similar. The most common serious adverse event was fatigue (5% of patients), followed by elevated serum creatinine (3.7%). About 10% of patients in each arm died while on study.
The National Institutes of Health supported the study. Dr. List had no relevant financial disclosures.
SAN DIEGO – Dual therapy with lenalidomide and epoetin alfa was safe and led to freedom from transfusion significantly more often than lenalidomide alone in patients with erythropoietin-refractory, lower-risk, non-del(5q) myelodysplastic syndromes, according to a randomized phase III head-to-head trial.
After 16 weeks of treatment, 33% of patients who received both lenalidomide and epoetin alfa met International Working Group 2000 criteria for major erythroid response, compared with only 14% of patients receiving lenalidomide monotherapy (P = .03), Alan F. List, MD, reported at the annual meeting of the American Society of Hematology.
Recombinant human erythropoietin improves anemia in some cases of MDS, but salvage options are limited. “Cytokine therapy is generally ineffective in patients with high transfusion burden or elevated serum erythropoietin level,” Dr. List said.
Lenalidomide (Revlimid) promotes the in vitro expansion of primitive erythroid precursors, and in a recent phase III, placebo-controlled trial, the immunomodulator improved erythropoiesis in about 25% of lower-risk, non-del(5q) MDS patients who were azanucleoside-naïve and transfusion-dependent, with effects lasting about 8 months. In another pilot study, adding epoetin alfa to lenalidomide induced erythroid responses in 28% of MDS patients who were not responding to lenalidomide alone. “This suggests that lenalidomide overcomes resistance and augments response to recombinant human erythropoietin,” Dr. List explained.
For their phase III trial, he and his associates randomly assigned erythropoietin-refractory, lower-risk, non-del(5q) MDS patients with hemoglobin levels under 9.5 g/dL to receive lenalidomide (10 mg per day for 21 days every 28 days) with or without epoetin alfa (weekly dose, 60,000 units subcutaneously). A total of 14% of patients had previously received azanucleoside therapy, about 92% had received erythropoietic stimulating agents, and median serum erythropoietin levels were 167 and 143 mU per mL in the monotherapy and dual therapy arms, respectively.
In accordance with International Working Group 2000 criteria, the researchers defined major erythroid response as transfusion independence for least 8 consecutive weeks, with at least a 1 g/dL increase in hemoglobin levels if patients were transfusion-dependent at baseline, and at least a 2 g/dL rise in hemoglobin if they were transfusion-independent.
In an interim analysis of 163 patients, 26% of the dual therapy group and 11% of lenalidomide-only patients met this primary endpoint (P = .02). These results met predefined criteria for stopping the study, after which 34 lenalidomide nonresponders crossed over to dual therapy. In all, 21% of these patients also had a major erythroid response, Dr. List said.
A multivariable analysis that included disease duration, International Prognostic Scoring System low versus intermediate-1 risk status, baseline erythropoietin level, and prior azanucleoside exposure showed that only dual lenalidomide–epoetin alfa therapy predicted major erythroid response. Specifically, dual therapy increased the odds of this outcome by about 63% when compared with lenalidomide monotherapy (P = .03).
Secondary analyses linked major erythroid response to having more low than high molecular weight CD45 isoform. In fact, the median ratio of high to low molecular weight CD45 was 1.5 among responders and 4.2 among nonresponders (P = .04) This finding fits the hypothesis that larger CD45 isoforms keep lenalidomide from enhancing erythropoietin receptor signaling, Dr. List said. Indeed, rates of major erythroid response to lenalidomide–epoetin alfa therapy were 73% when patients had a low isoform ratio, but were only 18% when they had a high isoform ratio (P = .03). The CD45 isoform ratio distinguished responders from nonresponders with a sensitivity and specificity of 80% and 75%, respectively, Dr. List said.
Grade 3 or higher nonhematologic events affected about a quarter of patients in each arm, and rates of individual events were similar. The most common serious adverse event was fatigue (5% of patients), followed by elevated serum creatinine (3.7%). About 10% of patients in each arm died while on study.
The National Institutes of Health supported the study. Dr. List had no relevant financial disclosures.
Key clinical point: Dual therapy with lenalidomide and epoetin alfa was more effective than lenalidomide monotherapy in patients with erythropoietin-refractory, lower-risk, non-del(5q) myelodysplastic syndrome.
Major finding: After 16 weeks of treatment, 33% of patients who received both agents met International Working Group 2000 criteria for major erythroid response, compared with 14% of patients receiving lenalidomide monotherapy (P = .03).
Data source: An interim analysis of 163 patients in the phase III ECOG-ACRIN E2905 Intergroup Study.
Disclosures: The National Institutes of Health supported the study. Dr. List had no relevant financial disclosures.
Daratumumab combo holds up across POLLUX myeloma subgroups
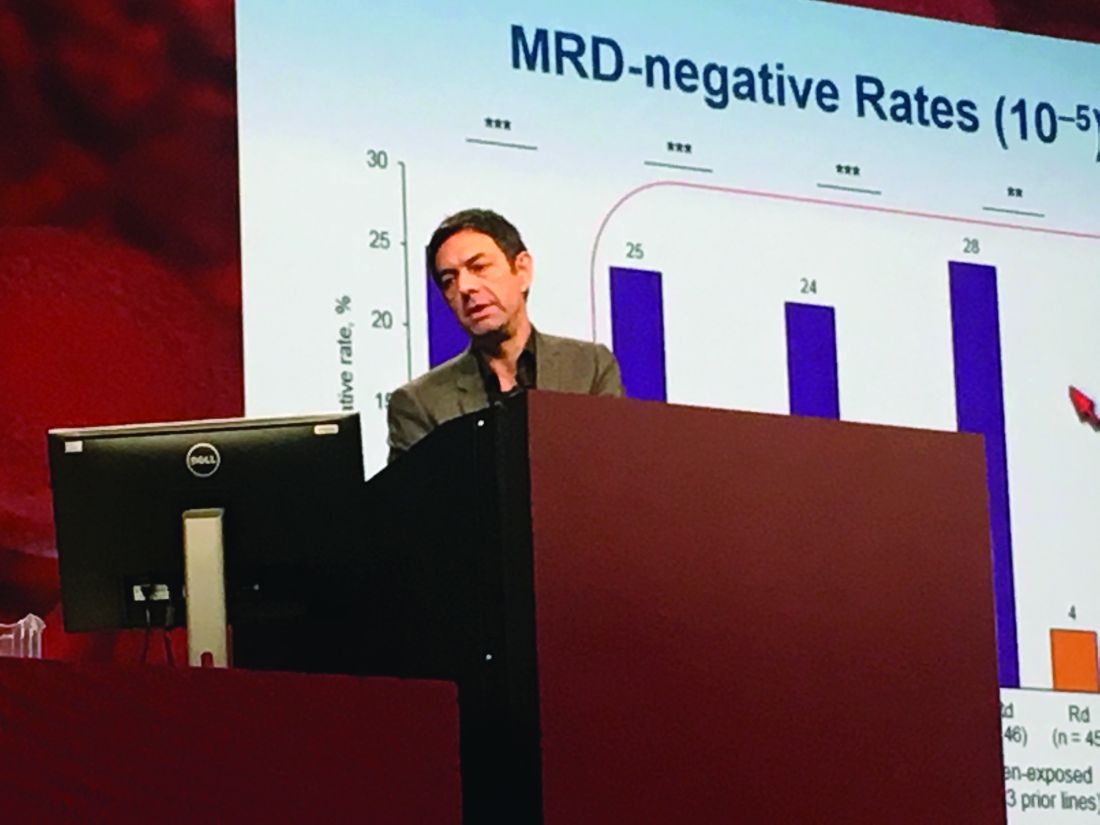
SAN DIEGO – Adding daratumumab (D) to lenalidomide and dexamethasone (Rd) significantly improved outcomes in relapsed and refractory multiple myeloma, even when patients had previously received lenalidomide, were refractory to bortezomib, or had high-risk tumor cytogenetics, based on updated analyses from the multicenter, randomized, phase III, open-label POLLUX trial.
The findings underscore the “significant benefit of combining daratumumab with lenalidomide and dexamethasone for relapsed or refractory multiple myeloma,” said lead investigator Philippe Moreau, MD, of University Hospital Hotel-Dieu in Nantes, France.
Among a large subgroup of 524 POLLUX patients who had received one to three prior lines of therapy, estimated median progression-free survival (PFS) has not been reached in the daratumumab, lenalidomide, and dexamethasone (DRd) arm, versus 18.4 months in the lenalidomide and dexamethasone (Rd) arm (hazard ratio, 0.36; 95% CI: 0.26 to 0.49; P less than .0001), Dr. Moreau said at the annual meeting of the American Society of Hematology.
That means adding daratumumab to Rd led to a 64% reduction in the risk of disease progression or death among patients with relapsed or refractory multiple myeloma, he noted. Fully 77% of DRd patients were alive without having progressed at 18 months, and responses “continued to deepen in the DRd group with longer follow-up,” he added.
Additional analyses supported the use of DRd in relapsed or refractory multiple myeloma, “irrespective of prior lenalidomide treatment or bortezomib refractoriness,” Dr. Moreau continued. He reported that DRd significantly improved PFS over Rd alone not only among 445 lenalidomide-naive patients (HR, 0.37; P less than .0001), but also among 91 lenalidomide-exposed patients (HR, 0.45; P = .04), 140 patients who were refractory to their most recent line of therapy (HR, 0.45; P = .001), and 99 bortezomib- refractory patients (HR 0.51; P = .02).
Daratumumab (Darzalex), a human CD38 IgG1k monoclonal antibody, was first approved as monotherapy for multiple myeloma in patients who had received at least three prior lines of therapy or had double-refractory disease. In 2016, results from the twin POLLUX and CASTOR studies won daratumumab a Food and Drug Administration breakthrough designation status for use with Rd in patients who had received at least one prior line.
The POLLUX trial included 569 patients with multiple myeloma who had received a median of 1 and up to 11 prior lines of therapy. Patients were randomized to either Rd alone or to Rd plus intravenous daratumumab (16 mg/kg) once a week during the first two 28-day treatment cycles, every 2 weeks during cycles 3-6, and once only on day 1 of subsequent cycles.
POLLUX patients were fairly heavily pretreated, Dr. Moreau noted. Thirteen percent had received three prior lines of therapy, 86% had received a proteasome inhibitor, 18% had received lenalidomide, 21% were refractory to bortezomib, and 28% were refractory to their most recent line of therapy.
Researchers performed “stringent, unbiased” assessments of minimal residual disease (MRD) negativity not only when a complete response was suspected, but also 3 and 6 months later, Dr. Moreau said. He emphasized that rates of MRD negativity in lenalidomide-exposed, bortezomib-refractory subgroups in POLLUX almost exactly matched those in the intent-to-treat population (25% on DRd vs. 6% on Rd; P less than .0001).
A total of 17% of DRd patients and 25% of Rd patients had high-risk cytogenetic profiles, and DRd performed well in these individuals, Dr. Moreau reported. Fully 85% of all evaluable high-risk patients had at least a partial response to DRd, and 33% had a complete response, versus only 67% and 6% of high-risk Rd patients, respectively. Among patients with standard-risk cytogenetics, rates of best overall response were 95% on DRd and 82% on Rd, and rates of complete response were 52% on DRd and 24% on Rd.
POLLUX yielded no new safety signals for DRd, Dr. Moreau said. Rates of primary and secondary malignancies were less than 2%. Neutropenia, the most common adverse effect, was managed by interrupting treatment, reducing the dose of lenalidomide, and administering growth factor.
Janssen Research & Development funded the study. Dr. Moreau had no relevant financial disclosures.
SAN DIEGO – Adding daratumumab (D) to lenalidomide and dexamethasone (Rd) significantly improved outcomes in relapsed and refractory multiple myeloma, even when patients had previously received lenalidomide, were refractory to bortezomib, or had high-risk tumor cytogenetics, based on updated analyses from the multicenter, randomized, phase III, open-label POLLUX trial.
The findings underscore the “significant benefit of combining daratumumab with lenalidomide and dexamethasone for relapsed or refractory multiple myeloma,” said lead investigator Philippe Moreau, MD, of University Hospital Hotel-Dieu in Nantes, France.
Among a large subgroup of 524 POLLUX patients who had received one to three prior lines of therapy, estimated median progression-free survival (PFS) has not been reached in the daratumumab, lenalidomide, and dexamethasone (DRd) arm, versus 18.4 months in the lenalidomide and dexamethasone (Rd) arm (hazard ratio, 0.36; 95% CI: 0.26 to 0.49; P less than .0001), Dr. Moreau said at the annual meeting of the American Society of Hematology.
That means adding daratumumab to Rd led to a 64% reduction in the risk of disease progression or death among patients with relapsed or refractory multiple myeloma, he noted. Fully 77% of DRd patients were alive without having progressed at 18 months, and responses “continued to deepen in the DRd group with longer follow-up,” he added.
Additional analyses supported the use of DRd in relapsed or refractory multiple myeloma, “irrespective of prior lenalidomide treatment or bortezomib refractoriness,” Dr. Moreau continued. He reported that DRd significantly improved PFS over Rd alone not only among 445 lenalidomide-naive patients (HR, 0.37; P less than .0001), but also among 91 lenalidomide-exposed patients (HR, 0.45; P = .04), 140 patients who were refractory to their most recent line of therapy (HR, 0.45; P = .001), and 99 bortezomib- refractory patients (HR 0.51; P = .02).
Daratumumab (Darzalex), a human CD38 IgG1k monoclonal antibody, was first approved as monotherapy for multiple myeloma in patients who had received at least three prior lines of therapy or had double-refractory disease. In 2016, results from the twin POLLUX and CASTOR studies won daratumumab a Food and Drug Administration breakthrough designation status for use with Rd in patients who had received at least one prior line.
The POLLUX trial included 569 patients with multiple myeloma who had received a median of 1 and up to 11 prior lines of therapy. Patients were randomized to either Rd alone or to Rd plus intravenous daratumumab (16 mg/kg) once a week during the first two 28-day treatment cycles, every 2 weeks during cycles 3-6, and once only on day 1 of subsequent cycles.
POLLUX patients were fairly heavily pretreated, Dr. Moreau noted. Thirteen percent had received three prior lines of therapy, 86% had received a proteasome inhibitor, 18% had received lenalidomide, 21% were refractory to bortezomib, and 28% were refractory to their most recent line of therapy.
Researchers performed “stringent, unbiased” assessments of minimal residual disease (MRD) negativity not only when a complete response was suspected, but also 3 and 6 months later, Dr. Moreau said. He emphasized that rates of MRD negativity in lenalidomide-exposed, bortezomib-refractory subgroups in POLLUX almost exactly matched those in the intent-to-treat population (25% on DRd vs. 6% on Rd; P less than .0001).
A total of 17% of DRd patients and 25% of Rd patients had high-risk cytogenetic profiles, and DRd performed well in these individuals, Dr. Moreau reported. Fully 85% of all evaluable high-risk patients had at least a partial response to DRd, and 33% had a complete response, versus only 67% and 6% of high-risk Rd patients, respectively. Among patients with standard-risk cytogenetics, rates of best overall response were 95% on DRd and 82% on Rd, and rates of complete response were 52% on DRd and 24% on Rd.
POLLUX yielded no new safety signals for DRd, Dr. Moreau said. Rates of primary and secondary malignancies were less than 2%. Neutropenia, the most common adverse effect, was managed by interrupting treatment, reducing the dose of lenalidomide, and administering growth factor.
Janssen Research & Development funded the study. Dr. Moreau had no relevant financial disclosures.
SAN DIEGO – Adding daratumumab (D) to lenalidomide and dexamethasone (Rd) significantly improved outcomes in relapsed and refractory multiple myeloma, even when patients had previously received lenalidomide, were refractory to bortezomib, or had high-risk tumor cytogenetics, based on updated analyses from the multicenter, randomized, phase III, open-label POLLUX trial.
The findings underscore the “significant benefit of combining daratumumab with lenalidomide and dexamethasone for relapsed or refractory multiple myeloma,” said lead investigator Philippe Moreau, MD, of University Hospital Hotel-Dieu in Nantes, France.
Among a large subgroup of 524 POLLUX patients who had received one to three prior lines of therapy, estimated median progression-free survival (PFS) has not been reached in the daratumumab, lenalidomide, and dexamethasone (DRd) arm, versus 18.4 months in the lenalidomide and dexamethasone (Rd) arm (hazard ratio, 0.36; 95% CI: 0.26 to 0.49; P less than .0001), Dr. Moreau said at the annual meeting of the American Society of Hematology.
That means adding daratumumab to Rd led to a 64% reduction in the risk of disease progression or death among patients with relapsed or refractory multiple myeloma, he noted. Fully 77% of DRd patients were alive without having progressed at 18 months, and responses “continued to deepen in the DRd group with longer follow-up,” he added.
Additional analyses supported the use of DRd in relapsed or refractory multiple myeloma, “irrespective of prior lenalidomide treatment or bortezomib refractoriness,” Dr. Moreau continued. He reported that DRd significantly improved PFS over Rd alone not only among 445 lenalidomide-naive patients (HR, 0.37; P less than .0001), but also among 91 lenalidomide-exposed patients (HR, 0.45; P = .04), 140 patients who were refractory to their most recent line of therapy (HR, 0.45; P = .001), and 99 bortezomib- refractory patients (HR 0.51; P = .02).
Daratumumab (Darzalex), a human CD38 IgG1k monoclonal antibody, was first approved as monotherapy for multiple myeloma in patients who had received at least three prior lines of therapy or had double-refractory disease. In 2016, results from the twin POLLUX and CASTOR studies won daratumumab a Food and Drug Administration breakthrough designation status for use with Rd in patients who had received at least one prior line.
The POLLUX trial included 569 patients with multiple myeloma who had received a median of 1 and up to 11 prior lines of therapy. Patients were randomized to either Rd alone or to Rd plus intravenous daratumumab (16 mg/kg) once a week during the first two 28-day treatment cycles, every 2 weeks during cycles 3-6, and once only on day 1 of subsequent cycles.
POLLUX patients were fairly heavily pretreated, Dr. Moreau noted. Thirteen percent had received three prior lines of therapy, 86% had received a proteasome inhibitor, 18% had received lenalidomide, 21% were refractory to bortezomib, and 28% were refractory to their most recent line of therapy.
Researchers performed “stringent, unbiased” assessments of minimal residual disease (MRD) negativity not only when a complete response was suspected, but also 3 and 6 months later, Dr. Moreau said. He emphasized that rates of MRD negativity in lenalidomide-exposed, bortezomib-refractory subgroups in POLLUX almost exactly matched those in the intent-to-treat population (25% on DRd vs. 6% on Rd; P less than .0001).
A total of 17% of DRd patients and 25% of Rd patients had high-risk cytogenetic profiles, and DRd performed well in these individuals, Dr. Moreau reported. Fully 85% of all evaluable high-risk patients had at least a partial response to DRd, and 33% had a complete response, versus only 67% and 6% of high-risk Rd patients, respectively. Among patients with standard-risk cytogenetics, rates of best overall response were 95% on DRd and 82% on Rd, and rates of complete response were 52% on DRd and 24% on Rd.
POLLUX yielded no new safety signals for DRd, Dr. Moreau said. Rates of primary and secondary malignancies were less than 2%. Neutropenia, the most common adverse effect, was managed by interrupting treatment, reducing the dose of lenalidomide, and administering growth factor.
Janssen Research & Development funded the study. Dr. Moreau had no relevant financial disclosures.
AT ASH 2016
Key clinical point: Adding daratumumab (D) to lenalidomide and dexamethasone (Rd) significantly improved outcomes in patients with relapsed and refractory multiple myeloma, regardless of factors such as bortezomib refractoriness, lenalidomide exposure, or high-risk tumor cytogenetics.
Major finding: DRd significantly improved PFS over Rd not only among 445 lenalidomide-naive patients (HR, 0.37; P less than .0001), but also among 91 lenalidomide-exposed patients (HR, 0.45; P = .04), 140 patients who were refractory to their most recent line of therapy (HR, 0.45; P = .001), and 99 bortezomib-refractory patients (HR 0.51; P = .02).
Data source: POLLUX, a multicenter, randomized, phase III, open-label trial of 569 patients with multiple myeloma who had received one or more previous lines of therapy.
Disclosures: Janssen Research & Development funded the study. Dr. Moreau had no relevant financial disclosures.
Artificial RBCs show promise in preclinical study

Photo by Aaron Logan
SAN DIEGO—Researchers have developed artificial red blood cells (RBCs) that appear able to emulate functions of natural red blood cells (RBCs), at least in rodents.
The artificial RBCs, known as ErythroMer, are designed to be freeze-dried, stored at ambient temperatures, and reconstituted with water when needed.
If ErythroMer proves safe and effective in humans, it could represent an alternative to blood transfusions that might be useful in situations where donated blood is difficult to obtain or store.
“There are currently no simple, practical means to bring transfusion to most trauma victims outside of hospitals,” said Allan Doctor, MD, of Washington University in Saint Louis, Missouri.
“ErythroMer would be a blood substitute that a medic can carry in his or her pack and literally take it out, add water, and inject it.”
Dr Doctor presented details on ErythroMer at the 2016 ASH Annual Meeting (abstract 1027).
Design
“Due to significant advances in synthetic chemistry and nanomedicine, we’re now able to encapsulate biologics with programmable polymers to generate nanoparticles that can emulate normal cellular physiology,” Dr Doctor noted.
With ErythroMer, he and his colleagues encapsulated human hemoglobin, methylene blue, and 2,3-DPG in an amphiphilic polymer shell. The polymer and its payload components, through microfluidization, self-assemble into toroids that are about one-fiftieth the size of human RBCs.
ErythroMer is designed to be pH-responsive, so that, in areas of high pH, 2,3-DPG is sequestered in the inner surface of the particle shell and does not bind to hemoglobin. In areas of low pH, 2,3-DPG is released from the shell and binds to hemoglobin, facilitating oxygen offloading. The role of methylene blue is to inhibit auto-oxidation of hemoglobin.
The last step in synthesis of the particle is crosslinking of the surface, which neutralizes the surface charge, stabilizes the particle, and generates a selective diffusion barrier to nitric oxide. The particle can be lyophilized for extended storage and later reconstituted.
Testing
Tests showed that ErythroMer matches the oxygen binding feature of human RBCs within 10%, a level researchers say should be sufficient to stabilize a bleeding patient until a blood transfusion can be obtained.
Experiments in mice showed that ErythroMer captures oxygen in the lungs and releases it to tissues in a pattern that is indistinguishable from that seen in a control group of mice injected with their own blood.
In rats, ErythroMer effectively resuscitated animals in shock following acute loss of 40% of their blood volume.
So far, tests suggest ErythroMer has overcome barriers that halted the development of previous blood substitutes.
However, Dr Doctor noted that ErythroMer does have its weaknesses. The particles are cleared rapidly from the bloodstream (in 3 to 7 hours), and hemoglobin sourcing presents a challenge. The researchers are now exploring the possibility of using recombinant hemoglobin genetically engineered in yeast.
The team hopes to further optimize ErythroMer’s shell, extend circulation time, confirm the efficacy of ErythroMer in a larger animal model (rabbits), evaluate the impact of the product on the coagulation and immune systems, and scale up production.
If further testing goes well, the researchers estimate that ErythroMer could be ready for use by field medics and emergency responders within 10 to 12 years.
ErythroMer development has been supported by the Children’s Discovery Institute at Washington University and St. Louis Children’s Hospital, the Skandalaris Center at Washington University, and the BioSTL Fundamentals Program.
This research was funded by the National Institute of General Medical Sciences; the National Heart, Lung, and Blood Institute; the National Institute of Child Health and Human Development, the US Department of Defense; the American Heart Association; Doris Duke Foundation; and Children’s Discovery Institute. ![]()

Photo by Aaron Logan
SAN DIEGO—Researchers have developed artificial red blood cells (RBCs) that appear able to emulate functions of natural red blood cells (RBCs), at least in rodents.
The artificial RBCs, known as ErythroMer, are designed to be freeze-dried, stored at ambient temperatures, and reconstituted with water when needed.
If ErythroMer proves safe and effective in humans, it could represent an alternative to blood transfusions that might be useful in situations where donated blood is difficult to obtain or store.
“There are currently no simple, practical means to bring transfusion to most trauma victims outside of hospitals,” said Allan Doctor, MD, of Washington University in Saint Louis, Missouri.
“ErythroMer would be a blood substitute that a medic can carry in his or her pack and literally take it out, add water, and inject it.”
Dr Doctor presented details on ErythroMer at the 2016 ASH Annual Meeting (abstract 1027).
Design
“Due to significant advances in synthetic chemistry and nanomedicine, we’re now able to encapsulate biologics with programmable polymers to generate nanoparticles that can emulate normal cellular physiology,” Dr Doctor noted.
With ErythroMer, he and his colleagues encapsulated human hemoglobin, methylene blue, and 2,3-DPG in an amphiphilic polymer shell. The polymer and its payload components, through microfluidization, self-assemble into toroids that are about one-fiftieth the size of human RBCs.
ErythroMer is designed to be pH-responsive, so that, in areas of high pH, 2,3-DPG is sequestered in the inner surface of the particle shell and does not bind to hemoglobin. In areas of low pH, 2,3-DPG is released from the shell and binds to hemoglobin, facilitating oxygen offloading. The role of methylene blue is to inhibit auto-oxidation of hemoglobin.
The last step in synthesis of the particle is crosslinking of the surface, which neutralizes the surface charge, stabilizes the particle, and generates a selective diffusion barrier to nitric oxide. The particle can be lyophilized for extended storage and later reconstituted.
Testing
Tests showed that ErythroMer matches the oxygen binding feature of human RBCs within 10%, a level researchers say should be sufficient to stabilize a bleeding patient until a blood transfusion can be obtained.
Experiments in mice showed that ErythroMer captures oxygen in the lungs and releases it to tissues in a pattern that is indistinguishable from that seen in a control group of mice injected with their own blood.
In rats, ErythroMer effectively resuscitated animals in shock following acute loss of 40% of their blood volume.
So far, tests suggest ErythroMer has overcome barriers that halted the development of previous blood substitutes.
However, Dr Doctor noted that ErythroMer does have its weaknesses. The particles are cleared rapidly from the bloodstream (in 3 to 7 hours), and hemoglobin sourcing presents a challenge. The researchers are now exploring the possibility of using recombinant hemoglobin genetically engineered in yeast.
The team hopes to further optimize ErythroMer’s shell, extend circulation time, confirm the efficacy of ErythroMer in a larger animal model (rabbits), evaluate the impact of the product on the coagulation and immune systems, and scale up production.
If further testing goes well, the researchers estimate that ErythroMer could be ready for use by field medics and emergency responders within 10 to 12 years.
ErythroMer development has been supported by the Children’s Discovery Institute at Washington University and St. Louis Children’s Hospital, the Skandalaris Center at Washington University, and the BioSTL Fundamentals Program.
This research was funded by the National Institute of General Medical Sciences; the National Heart, Lung, and Blood Institute; the National Institute of Child Health and Human Development, the US Department of Defense; the American Heart Association; Doris Duke Foundation; and Children’s Discovery Institute. ![]()

Photo by Aaron Logan
SAN DIEGO—Researchers have developed artificial red blood cells (RBCs) that appear able to emulate functions of natural red blood cells (RBCs), at least in rodents.
The artificial RBCs, known as ErythroMer, are designed to be freeze-dried, stored at ambient temperatures, and reconstituted with water when needed.
If ErythroMer proves safe and effective in humans, it could represent an alternative to blood transfusions that might be useful in situations where donated blood is difficult to obtain or store.
“There are currently no simple, practical means to bring transfusion to most trauma victims outside of hospitals,” said Allan Doctor, MD, of Washington University in Saint Louis, Missouri.
“ErythroMer would be a blood substitute that a medic can carry in his or her pack and literally take it out, add water, and inject it.”
Dr Doctor presented details on ErythroMer at the 2016 ASH Annual Meeting (abstract 1027).
Design
“Due to significant advances in synthetic chemistry and nanomedicine, we’re now able to encapsulate biologics with programmable polymers to generate nanoparticles that can emulate normal cellular physiology,” Dr Doctor noted.
With ErythroMer, he and his colleagues encapsulated human hemoglobin, methylene blue, and 2,3-DPG in an amphiphilic polymer shell. The polymer and its payload components, through microfluidization, self-assemble into toroids that are about one-fiftieth the size of human RBCs.
ErythroMer is designed to be pH-responsive, so that, in areas of high pH, 2,3-DPG is sequestered in the inner surface of the particle shell and does not bind to hemoglobin. In areas of low pH, 2,3-DPG is released from the shell and binds to hemoglobin, facilitating oxygen offloading. The role of methylene blue is to inhibit auto-oxidation of hemoglobin.
The last step in synthesis of the particle is crosslinking of the surface, which neutralizes the surface charge, stabilizes the particle, and generates a selective diffusion barrier to nitric oxide. The particle can be lyophilized for extended storage and later reconstituted.
Testing
Tests showed that ErythroMer matches the oxygen binding feature of human RBCs within 10%, a level researchers say should be sufficient to stabilize a bleeding patient until a blood transfusion can be obtained.
Experiments in mice showed that ErythroMer captures oxygen in the lungs and releases it to tissues in a pattern that is indistinguishable from that seen in a control group of mice injected with their own blood.
In rats, ErythroMer effectively resuscitated animals in shock following acute loss of 40% of their blood volume.
So far, tests suggest ErythroMer has overcome barriers that halted the development of previous blood substitutes.
However, Dr Doctor noted that ErythroMer does have its weaknesses. The particles are cleared rapidly from the bloodstream (in 3 to 7 hours), and hemoglobin sourcing presents a challenge. The researchers are now exploring the possibility of using recombinant hemoglobin genetically engineered in yeast.
The team hopes to further optimize ErythroMer’s shell, extend circulation time, confirm the efficacy of ErythroMer in a larger animal model (rabbits), evaluate the impact of the product on the coagulation and immune systems, and scale up production.
If further testing goes well, the researchers estimate that ErythroMer could be ready for use by field medics and emergency responders within 10 to 12 years.
ErythroMer development has been supported by the Children’s Discovery Institute at Washington University and St. Louis Children’s Hospital, the Skandalaris Center at Washington University, and the BioSTL Fundamentals Program.
This research was funded by the National Institute of General Medical Sciences; the National Heart, Lung, and Blood Institute; the National Institute of Child Health and Human Development, the US Department of Defense; the American Heart Association; Doris Duke Foundation; and Children’s Discovery Institute. ![]()
Combos prove no better than 7+3 for AML
Photo courtesy of
MD Anderson Cancer Center
SAN DIEGO—Neither a 2-drug combination nor a 3-drug combination is superior to 7+3 chemotherapy in younger patients with previously untreated acute myeloid leukemia (AML), according to a phase 3 trial.
Treatment
with idarubicin and high-dose cytarabine (IA), with or without
vorinostat (V), was no more effective than standard cytarabine plus
daunorubicin (7+3) in this trial.
In fact, among patients with favorable cytogenetics, outcomes with IA or IA+V were inferior to outcomes with 7+3.
Guillermo Garcia-Manero, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these results at the 2016 ASH Annual Meeting (abstract 901*).
In a phase 2 trial, Dr Garcia-Manero and his colleagues found that IA+V produced a high response rate (85%) in patients with previously untreated AML or high-risk myelodysplastic syndromes.
So the researchers conducted a phase 3 study (SWOG S1203) to determine if IA or IA+V could improve outcomes for younger AML patients when compared to 7+3.
Treatment
Induction therapy was as follows:
- 7+3 arm—daunorubicin** at 90 mg/m2 once daily on days 1 to 3 with cytarabine at 100 mg/m2 once daily on days 1 to 7.
- IA arm—idarubicin at 12 mg/m2 once daily on days 1 to 3 with cytarabine at 1.5 gm/m2 once daily on days 1 to 4.
- IA+V arm—vorinostat at 500 mg orally 3 times a day on days 1 to 3, idarubicin at 12 mg/m2 once daily on days 4 to 6, and cytarabine at 1.5 gm/m2 once daily on days 4 to 7.
Consolidation was as follows:
- 7+3 arm—standard high-dose cytarabine at 3 gm/m2 over 3 hours every 12 hours x 6 doses for 1 to 4 cycles, depending on transplant availability.
- IA arm—idarubicin at 8 mg/m2 once daily on days 1 to 2 with cytarabine at 0.75 mg/m2 for 3 days on days 1 to 3 for 4 cycles.
- IA+V arm—vorinostat at 500 mg orally 3 times a day on days 1 to 3, idarubicin at 8 mg/m2 once daily on days 4 to 5, and cytarabine at 0.75 gm/m2 once daily on days 4 to 6.
The number of consolidation cycles varied depending on transplant indication. In all, 43% of patients (n=317) proceeded to allogeneic transplant. (Details on these patients were presented at ASH as abstract 1166.)
Patients in the IA+V arm also received maintenance with vorinostat at 300 mg 3 times a day for 14 days every 28 days.
**There was a shortage of daunorubicin during this trial. So if daunorubicin was not available, patients received idarubicin at 12 mg/m2 once daily on days 1 to 3. Dr Garcia-Manero could not provide data on how many patients assigned to daunorubicin actually received idarubicin.
Patients
There were a total of 738 eligible patients—261 in the 7+3 arm, 261 in the IA arm, and 216 in the IA+V arm. Dr Garcia-Manero said baseline characteristics were well balanced among the arms.
Overall, the median age was 49 (range, 18-60), 49% of patients were female, and 13% had a performance status of 2-3.
Thirteen percent of patients had favorable cytogenetics, 22% had high-risk cytogenetics, 16% had FLT3-ITD, and 21% had mutated NPM1.
Results
The complete response rates were 62% overall, 63% for 7+3, 64% for IA, and 60% for IA+V (P=0.58).
The rates of complete response with incomplete count recovery were 15%, 13%, 16%, and 17%, respectively. The failure rates were 23%, 25%, 21%, and 23%, respectively.
The rate of mortality within 30 days was 4% overall, 3% for 7+3, 6% for IA, and 4% for IA+V (P=0.013). The rate of mortality within 60 days was 7%, 5%, 9%, and 9%, respectively (P=0.097).
The rate of event-free survival was 42% overall, 43% for 7+3, 43% for IA, and 40% for IA+V.
There was no significant difference in event-free survival between IA+V and IA (P=0.66), IA+V and 7+3 (P=0.91), or IA and 7+3 (P=0.76).
The rate of overall survival (OS) was 62% overall, 62% for 7+3, 63% for IA, and 59% for IA+V.
There was no significant difference in OS between IA+V and IA (P=0.6), IA+V and 7+3 (P=0.67), or IA and 7+3 (P=0.92).
Among patients with favorable cytogenetics, there was no significant difference in OS between IA and IA+V (P=0.8). However, patients who received IA (P=0.011) or IA+V (P=0.012) had significantly better OS than patients who received 7+3.
There were more grade 5 adverse events (AEs) in the IA (n=19) and IA+V arms (n=16) than in the 7+3 arm (n=6).
Grade 5 AEs in the 7+3 arm were classified as follows: cardiac disorder (n=1), gastrointestinal disorder (n=1), general disorders (n=2), hepatobiliary disorder (n=1), and respiratory/thoracic/mediastinal disorder (n=1).
Grade 5 AEs in the IA arm included cardiac disorders (n=3), gastrointestinal disorder (n=1), general disorders (n=2), infections and infestations (n=7), nervous system disorder (n=1), respiratory/thoracic/mediastinal disorders (n=4), and vascular disorder (n=1).
Grade 5 AEs in the IA+V arm included cardiac disorder (n=1), general disorders (n=2), infections and infestations (n=7), nervous system disorder (n=1), and respiratory/thoracic/mediastinal disorders (n=5).
“In newly diagnosed adults with AML ages 18 to 60, neither IA [plus] vorinostat nor IA were superior to standard 7+3,” Dr Garcia-Manero said in closing.
“Indeed, 7+3 was superior to IA and IA [plus] vorinostat for those patients with favorable cytogenetics, reinforcing the need for high-dose ara-C during the consolidation phase. Newer studies with other combinations, including, perhaps, nucleoside analogues, monoclonal antibodies, or targeted agents are needed.” ![]()
*Some data in the abstract differ from the presentation.
Photo courtesy of
MD Anderson Cancer Center
SAN DIEGO—Neither a 2-drug combination nor a 3-drug combination is superior to 7+3 chemotherapy in younger patients with previously untreated acute myeloid leukemia (AML), according to a phase 3 trial.
Treatment
with idarubicin and high-dose cytarabine (IA), with or without
vorinostat (V), was no more effective than standard cytarabine plus
daunorubicin (7+3) in this trial.
In fact, among patients with favorable cytogenetics, outcomes with IA or IA+V were inferior to outcomes with 7+3.
Guillermo Garcia-Manero, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these results at the 2016 ASH Annual Meeting (abstract 901*).
In a phase 2 trial, Dr Garcia-Manero and his colleagues found that IA+V produced a high response rate (85%) in patients with previously untreated AML or high-risk myelodysplastic syndromes.
So the researchers conducted a phase 3 study (SWOG S1203) to determine if IA or IA+V could improve outcomes for younger AML patients when compared to 7+3.
Treatment
Induction therapy was as follows:
- 7+3 arm—daunorubicin** at 90 mg/m2 once daily on days 1 to 3 with cytarabine at 100 mg/m2 once daily on days 1 to 7.
- IA arm—idarubicin at 12 mg/m2 once daily on days 1 to 3 with cytarabine at 1.5 gm/m2 once daily on days 1 to 4.
- IA+V arm—vorinostat at 500 mg orally 3 times a day on days 1 to 3, idarubicin at 12 mg/m2 once daily on days 4 to 6, and cytarabine at 1.5 gm/m2 once daily on days 4 to 7.
Consolidation was as follows:
- 7+3 arm—standard high-dose cytarabine at 3 gm/m2 over 3 hours every 12 hours x 6 doses for 1 to 4 cycles, depending on transplant availability.
- IA arm—idarubicin at 8 mg/m2 once daily on days 1 to 2 with cytarabine at 0.75 mg/m2 for 3 days on days 1 to 3 for 4 cycles.
- IA+V arm—vorinostat at 500 mg orally 3 times a day on days 1 to 3, idarubicin at 8 mg/m2 once daily on days 4 to 5, and cytarabine at 0.75 gm/m2 once daily on days 4 to 6.
The number of consolidation cycles varied depending on transplant indication. In all, 43% of patients (n=317) proceeded to allogeneic transplant. (Details on these patients were presented at ASH as abstract 1166.)
Patients in the IA+V arm also received maintenance with vorinostat at 300 mg 3 times a day for 14 days every 28 days.
**There was a shortage of daunorubicin during this trial. So if daunorubicin was not available, patients received idarubicin at 12 mg/m2 once daily on days 1 to 3. Dr Garcia-Manero could not provide data on how many patients assigned to daunorubicin actually received idarubicin.
Patients
There were a total of 738 eligible patients—261 in the 7+3 arm, 261 in the IA arm, and 216 in the IA+V arm. Dr Garcia-Manero said baseline characteristics were well balanced among the arms.
Overall, the median age was 49 (range, 18-60), 49% of patients were female, and 13% had a performance status of 2-3.
Thirteen percent of patients had favorable cytogenetics, 22% had high-risk cytogenetics, 16% had FLT3-ITD, and 21% had mutated NPM1.
Results
The complete response rates were 62% overall, 63% for 7+3, 64% for IA, and 60% for IA+V (P=0.58).
The rates of complete response with incomplete count recovery were 15%, 13%, 16%, and 17%, respectively. The failure rates were 23%, 25%, 21%, and 23%, respectively.
The rate of mortality within 30 days was 4% overall, 3% for 7+3, 6% for IA, and 4% for IA+V (P=0.013). The rate of mortality within 60 days was 7%, 5%, 9%, and 9%, respectively (P=0.097).
The rate of event-free survival was 42% overall, 43% for 7+3, 43% for IA, and 40% for IA+V.
There was no significant difference in event-free survival between IA+V and IA (P=0.66), IA+V and 7+3 (P=0.91), or IA and 7+3 (P=0.76).
The rate of overall survival (OS) was 62% overall, 62% for 7+3, 63% for IA, and 59% for IA+V.
There was no significant difference in OS between IA+V and IA (P=0.6), IA+V and 7+3 (P=0.67), or IA and 7+3 (P=0.92).
Among patients with favorable cytogenetics, there was no significant difference in OS between IA and IA+V (P=0.8). However, patients who received IA (P=0.011) or IA+V (P=0.012) had significantly better OS than patients who received 7+3.
There were more grade 5 adverse events (AEs) in the IA (n=19) and IA+V arms (n=16) than in the 7+3 arm (n=6).
Grade 5 AEs in the 7+3 arm were classified as follows: cardiac disorder (n=1), gastrointestinal disorder (n=1), general disorders (n=2), hepatobiliary disorder (n=1), and respiratory/thoracic/mediastinal disorder (n=1).
Grade 5 AEs in the IA arm included cardiac disorders (n=3), gastrointestinal disorder (n=1), general disorders (n=2), infections and infestations (n=7), nervous system disorder (n=1), respiratory/thoracic/mediastinal disorders (n=4), and vascular disorder (n=1).
Grade 5 AEs in the IA+V arm included cardiac disorder (n=1), general disorders (n=2), infections and infestations (n=7), nervous system disorder (n=1), and respiratory/thoracic/mediastinal disorders (n=5).
“In newly diagnosed adults with AML ages 18 to 60, neither IA [plus] vorinostat nor IA were superior to standard 7+3,” Dr Garcia-Manero said in closing.
“Indeed, 7+3 was superior to IA and IA [plus] vorinostat for those patients with favorable cytogenetics, reinforcing the need for high-dose ara-C during the consolidation phase. Newer studies with other combinations, including, perhaps, nucleoside analogues, monoclonal antibodies, or targeted agents are needed.” ![]()
*Some data in the abstract differ from the presentation.
Photo courtesy of
MD Anderson Cancer Center
SAN DIEGO—Neither a 2-drug combination nor a 3-drug combination is superior to 7+3 chemotherapy in younger patients with previously untreated acute myeloid leukemia (AML), according to a phase 3 trial.
Treatment
with idarubicin and high-dose cytarabine (IA), with or without
vorinostat (V), was no more effective than standard cytarabine plus
daunorubicin (7+3) in this trial.
In fact, among patients with favorable cytogenetics, outcomes with IA or IA+V were inferior to outcomes with 7+3.
Guillermo Garcia-Manero, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these results at the 2016 ASH Annual Meeting (abstract 901*).
In a phase 2 trial, Dr Garcia-Manero and his colleagues found that IA+V produced a high response rate (85%) in patients with previously untreated AML or high-risk myelodysplastic syndromes.
So the researchers conducted a phase 3 study (SWOG S1203) to determine if IA or IA+V could improve outcomes for younger AML patients when compared to 7+3.
Treatment
Induction therapy was as follows:
- 7+3 arm—daunorubicin** at 90 mg/m2 once daily on days 1 to 3 with cytarabine at 100 mg/m2 once daily on days 1 to 7.
- IA arm—idarubicin at 12 mg/m2 once daily on days 1 to 3 with cytarabine at 1.5 gm/m2 once daily on days 1 to 4.
- IA+V arm—vorinostat at 500 mg orally 3 times a day on days 1 to 3, idarubicin at 12 mg/m2 once daily on days 4 to 6, and cytarabine at 1.5 gm/m2 once daily on days 4 to 7.
Consolidation was as follows:
- 7+3 arm—standard high-dose cytarabine at 3 gm/m2 over 3 hours every 12 hours x 6 doses for 1 to 4 cycles, depending on transplant availability.
- IA arm—idarubicin at 8 mg/m2 once daily on days 1 to 2 with cytarabine at 0.75 mg/m2 for 3 days on days 1 to 3 for 4 cycles.
- IA+V arm—vorinostat at 500 mg orally 3 times a day on days 1 to 3, idarubicin at 8 mg/m2 once daily on days 4 to 5, and cytarabine at 0.75 gm/m2 once daily on days 4 to 6.
The number of consolidation cycles varied depending on transplant indication. In all, 43% of patients (n=317) proceeded to allogeneic transplant. (Details on these patients were presented at ASH as abstract 1166.)
Patients in the IA+V arm also received maintenance with vorinostat at 300 mg 3 times a day for 14 days every 28 days.
**There was a shortage of daunorubicin during this trial. So if daunorubicin was not available, patients received idarubicin at 12 mg/m2 once daily on days 1 to 3. Dr Garcia-Manero could not provide data on how many patients assigned to daunorubicin actually received idarubicin.
Patients
There were a total of 738 eligible patients—261 in the 7+3 arm, 261 in the IA arm, and 216 in the IA+V arm. Dr Garcia-Manero said baseline characteristics were well balanced among the arms.
Overall, the median age was 49 (range, 18-60), 49% of patients were female, and 13% had a performance status of 2-3.
Thirteen percent of patients had favorable cytogenetics, 22% had high-risk cytogenetics, 16% had FLT3-ITD, and 21% had mutated NPM1.
Results
The complete response rates were 62% overall, 63% for 7+3, 64% for IA, and 60% for IA+V (P=0.58).
The rates of complete response with incomplete count recovery were 15%, 13%, 16%, and 17%, respectively. The failure rates were 23%, 25%, 21%, and 23%, respectively.
The rate of mortality within 30 days was 4% overall, 3% for 7+3, 6% for IA, and 4% for IA+V (P=0.013). The rate of mortality within 60 days was 7%, 5%, 9%, and 9%, respectively (P=0.097).
The rate of event-free survival was 42% overall, 43% for 7+3, 43% for IA, and 40% for IA+V.
There was no significant difference in event-free survival between IA+V and IA (P=0.66), IA+V and 7+3 (P=0.91), or IA and 7+3 (P=0.76).
The rate of overall survival (OS) was 62% overall, 62% for 7+3, 63% for IA, and 59% for IA+V.
There was no significant difference in OS between IA+V and IA (P=0.6), IA+V and 7+3 (P=0.67), or IA and 7+3 (P=0.92).
Among patients with favorable cytogenetics, there was no significant difference in OS between IA and IA+V (P=0.8). However, patients who received IA (P=0.011) or IA+V (P=0.012) had significantly better OS than patients who received 7+3.
There were more grade 5 adverse events (AEs) in the IA (n=19) and IA+V arms (n=16) than in the 7+3 arm (n=6).
Grade 5 AEs in the 7+3 arm were classified as follows: cardiac disorder (n=1), gastrointestinal disorder (n=1), general disorders (n=2), hepatobiliary disorder (n=1), and respiratory/thoracic/mediastinal disorder (n=1).
Grade 5 AEs in the IA arm included cardiac disorders (n=3), gastrointestinal disorder (n=1), general disorders (n=2), infections and infestations (n=7), nervous system disorder (n=1), respiratory/thoracic/mediastinal disorders (n=4), and vascular disorder (n=1).
Grade 5 AEs in the IA+V arm included cardiac disorder (n=1), general disorders (n=2), infections and infestations (n=7), nervous system disorder (n=1), and respiratory/thoracic/mediastinal disorders (n=5).
“In newly diagnosed adults with AML ages 18 to 60, neither IA [plus] vorinostat nor IA were superior to standard 7+3,” Dr Garcia-Manero said in closing.
“Indeed, 7+3 was superior to IA and IA [plus] vorinostat for those patients with favorable cytogenetics, reinforcing the need for high-dose ara-C during the consolidation phase. Newer studies with other combinations, including, perhaps, nucleoside analogues, monoclonal antibodies, or targeted agents are needed.” ![]()
*Some data in the abstract differ from the presentation.
All cases of CRS are not created equal

2016 ASH Annual Meeting
SAN DIEGO—Investigators have found that life-threatening cytokine release syndrome (CRS) and its symptoms are due to the release of macrophage activation syndrome (MAS) cytokines, such as IL-6, IL-8, and IL2RA.
MAS cytokines, at least in vitro, are not made by chimeric antigen receptor (CAR) T cells and are not necessary for CAR T-cell efficacy, the team says.
The cytokines are produced by antigen-presenting cells (APCs) in response to CAR-mediated killing of leukemia.
What’s more, they say, is that this is likely to be different for each CAR structure and possibly even tumor type.
“Understanding these mechanisms, as it relates to our treatment, will be critical to understanding how best to take care of patients and maintain efficacy without toxicity,” said David Barrett, MD, PhD, of the University of Pennsylvania in Philadelphia.
Dr Barrett discussed the relationship between IL-6, CRS, and CAR T-cell therapy at the 2016 ASH Annual Meeting (abstract 654).
“Every CAR system is slightly different,” he explained, “and it’s very important to understand that when we’re talking about efficacy and toxicity.”
Dr Barrett focused on CTL019 (also known as CART19), the CD19-directed 4-1BB CD3ζ CAR used at the Children’s Hospital of Philadelphia (CHOP).
In pediatric acute lymphoblastic leukemia (ALL), CTL019 produced a 93% response rate at 1 month and an overall survival rate of 79% at 12 months in 59 patients.
“Some relapses take place,” Dr Barrett noted. “This is not a perfect therapy, although it has been transformative in the care of patients.”
Eighty-eight percent of the patients experienced CRS of any grade, and 2 died from it. CRS causes high fever and myalgias, and severe CRS causes unstable hypotension that can require mechanical ventilation.
Tocilizumab, the IL-6R blocking antibody, was used in 27% of the patients, generally for grade 4 CRS.
CRS with CTL019
Dr Barrett described CRS in the first patient treated with CTL019 at CHOP in April 2012. The CRS was quite severe, with high fevers and unstable hypotension requiring multiple vasopressors and the need for mechanical ventilation.
“[W]e had no idea what was happening,” he said. “We didn’t understand what the source of the illness was.”
The patient did not respond to steroids or to etanercept, which Dr Barrett indicated is known to help in acute respiratory distress in transplant patients.
“And it was only through some incredible clinical acumen of the treating physicians as well as incredible critical care that was delivered by our ICU that kept this patient alive long enough for us to try tocilizumab,” Dr Barrett continued, “which, thankfully, worked by blocking the most severe side effects in this patient and allowed her to survive.”
Dr Barrett described the course of another patient who developed grade 4 CRS that continued to get worse even after he received tocilizumab, siltuximab, and steroids.
The patient required vasoactive drugs, had seizures, required milrinone, and was placed on a ventilator. One year after receiving CAR T-cell therapy, he recovered.
“This is an incredibly terrifying syndrome to take care of when we don’t understand what’s triggering it or how to stop it,” Dr Barrett emphasized.
Studying CRS
IL-6 is clearly a critical cytokine in the toxicity of CAR T-cell therapy, Dr Barrett said, but IFNγ and other cytokines are also important.
He and his colleagues performed a comprehensive cytokine analysis of pediatric patients treated with CTL019—specifically, engineered T cells composed of an anti-CD19 single-chain variable fragment, CD3ζ activation domain, a 4-1BB costimulatory domain, and transduced with a lentivirus grown on CD3/CD28 beads with a little bit of IL-2.
With that specific CAR, Dr Barrett said they observed a MAS pattern—IFNγ, IL-10, IL-6, and IL-8, which are most elevated in grades 4 and 5 CRS.
“[S]o this pattern, and this clinical syndrome [CRS] was what we believe was driving toxicity in this model,” he said.
To figure out why this was happening, the investigators created 4-1BB CAR-mediated CRS in a mouse model.
The team took leukemia cells from the first patient treated and clinical T cells from her CAR product and put them in an NSG mouse model that they had used for preclinical development.
The investigators then measured cytokine production in the serum of animals 3 and 7 days post-treatment with CTL019.
“And nothing happened,” Dr Barrett said. “The mice didn’t get sick, they cleared their leukemia, and when you looked for cytokines, you found IFNγ, IL-2, and GM-CSF, but you did not find IL-6.”
The team had also included etanercept and tocilizumab in this model, but since the mice didn’t make the toxic cytokines, the antibodies didn’t do anything.
“So why did she get so sick but yet her cancer and her CAR T cells did not make these mice sick and not generate these cytokines?” Dr Barrett asked.
The investigators hypothesized that APCs—not the CAR T cells—were responsible for the toxic cytokines secreted.
“[I]t would be the CAR T-cell-mediated killing of leukemia which would induce this cytokine release from the antigen-presenting cell lineages,” Dr Barrett explained.
To test this theory, the investigators co-cultured CTL019 and Nalm-6 leukemia, with or without cells derived from peripheral blood monocytes.
The team found that IL-6 levels were elevated several logs when CAR T cells killed leukemia in the presence of the APCs.
On the other hand, co-culture of only CTL019 and Nalm-6 produced high levels of GM-CSF, IFNγ, IL-2, and IL-10 but no detectable IL-6 or IL-8.
Transwell in vitro experiments separating CTL019 and Nalm-6 from the APCs showed the same pattern.
The investigators thus confirmed that IL-6 is made by APCs in response to CAR-mediated killing of leukemia.
Nanostring profiling
The team then performed nanostring RNA analysis of separated cell populations recovered from that experiment.
They found that IL-6 and IL-8 are produced by APCs but not by CTL019. IL-2 and IFNγ are produced by CTL019 and not by APCs, and GM-CSF was produced from CTL019.
“There was a clear separation in cytokine production in this model,” Dr Barrett said.
The investigators also observed that the CTL019 nanostring profile was unaffected by proximity to the APCs and all the IL-6 they make.
“CART19 T cells did not seem to care, on a transcriptional level, that all this IL-6 was floating around,” Dr Barrett said.
In contrast, the APCs do change, he said, when CAR T cells are killing leukemia nearby.
“There are dozens and dozens of changes,” he said, “including many in chemokines and IL-6 and IL-8.”
The investigators performed multiple in vitro killing assays and found no difference in CAR T-cell killing potential in the presence or absence of the MAS cytokines.
They also performed peripheral blood analysis of patients experiencing CRS of grades 2 to 5. The team observed that clinical CRS may be divided into MAS and not-MAS patterns. In addition, they detected no IL-6 transcript in any of the CAR T cells isolated from these patients.
“I think we’re going to discover that cytokine release syndrome is a clinical entity that has multiple mechanisms,” Dr Barrett said. “And so it’s very important, when we are talking about our models and talking about our results, to be sure that we’re all speaking the same language.” ![]()

2016 ASH Annual Meeting
SAN DIEGO—Investigators have found that life-threatening cytokine release syndrome (CRS) and its symptoms are due to the release of macrophage activation syndrome (MAS) cytokines, such as IL-6, IL-8, and IL2RA.
MAS cytokines, at least in vitro, are not made by chimeric antigen receptor (CAR) T cells and are not necessary for CAR T-cell efficacy, the team says.
The cytokines are produced by antigen-presenting cells (APCs) in response to CAR-mediated killing of leukemia.
What’s more, they say, is that this is likely to be different for each CAR structure and possibly even tumor type.
“Understanding these mechanisms, as it relates to our treatment, will be critical to understanding how best to take care of patients and maintain efficacy without toxicity,” said David Barrett, MD, PhD, of the University of Pennsylvania in Philadelphia.
Dr Barrett discussed the relationship between IL-6, CRS, and CAR T-cell therapy at the 2016 ASH Annual Meeting (abstract 654).
“Every CAR system is slightly different,” he explained, “and it’s very important to understand that when we’re talking about efficacy and toxicity.”
Dr Barrett focused on CTL019 (also known as CART19), the CD19-directed 4-1BB CD3ζ CAR used at the Children’s Hospital of Philadelphia (CHOP).
In pediatric acute lymphoblastic leukemia (ALL), CTL019 produced a 93% response rate at 1 month and an overall survival rate of 79% at 12 months in 59 patients.
“Some relapses take place,” Dr Barrett noted. “This is not a perfect therapy, although it has been transformative in the care of patients.”
Eighty-eight percent of the patients experienced CRS of any grade, and 2 died from it. CRS causes high fever and myalgias, and severe CRS causes unstable hypotension that can require mechanical ventilation.
Tocilizumab, the IL-6R blocking antibody, was used in 27% of the patients, generally for grade 4 CRS.
CRS with CTL019
Dr Barrett described CRS in the first patient treated with CTL019 at CHOP in April 2012. The CRS was quite severe, with high fevers and unstable hypotension requiring multiple vasopressors and the need for mechanical ventilation.
“[W]e had no idea what was happening,” he said. “We didn’t understand what the source of the illness was.”
The patient did not respond to steroids or to etanercept, which Dr Barrett indicated is known to help in acute respiratory distress in transplant patients.
“And it was only through some incredible clinical acumen of the treating physicians as well as incredible critical care that was delivered by our ICU that kept this patient alive long enough for us to try tocilizumab,” Dr Barrett continued, “which, thankfully, worked by blocking the most severe side effects in this patient and allowed her to survive.”
Dr Barrett described the course of another patient who developed grade 4 CRS that continued to get worse even after he received tocilizumab, siltuximab, and steroids.
The patient required vasoactive drugs, had seizures, required milrinone, and was placed on a ventilator. One year after receiving CAR T-cell therapy, he recovered.
“This is an incredibly terrifying syndrome to take care of when we don’t understand what’s triggering it or how to stop it,” Dr Barrett emphasized.
Studying CRS
IL-6 is clearly a critical cytokine in the toxicity of CAR T-cell therapy, Dr Barrett said, but IFNγ and other cytokines are also important.
He and his colleagues performed a comprehensive cytokine analysis of pediatric patients treated with CTL019—specifically, engineered T cells composed of an anti-CD19 single-chain variable fragment, CD3ζ activation domain, a 4-1BB costimulatory domain, and transduced with a lentivirus grown on CD3/CD28 beads with a little bit of IL-2.
With that specific CAR, Dr Barrett said they observed a MAS pattern—IFNγ, IL-10, IL-6, and IL-8, which are most elevated in grades 4 and 5 CRS.
“[S]o this pattern, and this clinical syndrome [CRS] was what we believe was driving toxicity in this model,” he said.
To figure out why this was happening, the investigators created 4-1BB CAR-mediated CRS in a mouse model.
The team took leukemia cells from the first patient treated and clinical T cells from her CAR product and put them in an NSG mouse model that they had used for preclinical development.
The investigators then measured cytokine production in the serum of animals 3 and 7 days post-treatment with CTL019.
“And nothing happened,” Dr Barrett said. “The mice didn’t get sick, they cleared their leukemia, and when you looked for cytokines, you found IFNγ, IL-2, and GM-CSF, but you did not find IL-6.”
The team had also included etanercept and tocilizumab in this model, but since the mice didn’t make the toxic cytokines, the antibodies didn’t do anything.
“So why did she get so sick but yet her cancer and her CAR T cells did not make these mice sick and not generate these cytokines?” Dr Barrett asked.
The investigators hypothesized that APCs—not the CAR T cells—were responsible for the toxic cytokines secreted.
“[I]t would be the CAR T-cell-mediated killing of leukemia which would induce this cytokine release from the antigen-presenting cell lineages,” Dr Barrett explained.
To test this theory, the investigators co-cultured CTL019 and Nalm-6 leukemia, with or without cells derived from peripheral blood monocytes.
The team found that IL-6 levels were elevated several logs when CAR T cells killed leukemia in the presence of the APCs.
On the other hand, co-culture of only CTL019 and Nalm-6 produced high levels of GM-CSF, IFNγ, IL-2, and IL-10 but no detectable IL-6 or IL-8.
Transwell in vitro experiments separating CTL019 and Nalm-6 from the APCs showed the same pattern.
The investigators thus confirmed that IL-6 is made by APCs in response to CAR-mediated killing of leukemia.
Nanostring profiling
The team then performed nanostring RNA analysis of separated cell populations recovered from that experiment.
They found that IL-6 and IL-8 are produced by APCs but not by CTL019. IL-2 and IFNγ are produced by CTL019 and not by APCs, and GM-CSF was produced from CTL019.
“There was a clear separation in cytokine production in this model,” Dr Barrett said.
The investigators also observed that the CTL019 nanostring profile was unaffected by proximity to the APCs and all the IL-6 they make.
“CART19 T cells did not seem to care, on a transcriptional level, that all this IL-6 was floating around,” Dr Barrett said.
In contrast, the APCs do change, he said, when CAR T cells are killing leukemia nearby.
“There are dozens and dozens of changes,” he said, “including many in chemokines and IL-6 and IL-8.”
The investigators performed multiple in vitro killing assays and found no difference in CAR T-cell killing potential in the presence or absence of the MAS cytokines.
They also performed peripheral blood analysis of patients experiencing CRS of grades 2 to 5. The team observed that clinical CRS may be divided into MAS and not-MAS patterns. In addition, they detected no IL-6 transcript in any of the CAR T cells isolated from these patients.
“I think we’re going to discover that cytokine release syndrome is a clinical entity that has multiple mechanisms,” Dr Barrett said. “And so it’s very important, when we are talking about our models and talking about our results, to be sure that we’re all speaking the same language.” ![]()

2016 ASH Annual Meeting
SAN DIEGO—Investigators have found that life-threatening cytokine release syndrome (CRS) and its symptoms are due to the release of macrophage activation syndrome (MAS) cytokines, such as IL-6, IL-8, and IL2RA.
MAS cytokines, at least in vitro, are not made by chimeric antigen receptor (CAR) T cells and are not necessary for CAR T-cell efficacy, the team says.
The cytokines are produced by antigen-presenting cells (APCs) in response to CAR-mediated killing of leukemia.
What’s more, they say, is that this is likely to be different for each CAR structure and possibly even tumor type.
“Understanding these mechanisms, as it relates to our treatment, will be critical to understanding how best to take care of patients and maintain efficacy without toxicity,” said David Barrett, MD, PhD, of the University of Pennsylvania in Philadelphia.
Dr Barrett discussed the relationship between IL-6, CRS, and CAR T-cell therapy at the 2016 ASH Annual Meeting (abstract 654).
“Every CAR system is slightly different,” he explained, “and it’s very important to understand that when we’re talking about efficacy and toxicity.”
Dr Barrett focused on CTL019 (also known as CART19), the CD19-directed 4-1BB CD3ζ CAR used at the Children’s Hospital of Philadelphia (CHOP).
In pediatric acute lymphoblastic leukemia (ALL), CTL019 produced a 93% response rate at 1 month and an overall survival rate of 79% at 12 months in 59 patients.
“Some relapses take place,” Dr Barrett noted. “This is not a perfect therapy, although it has been transformative in the care of patients.”
Eighty-eight percent of the patients experienced CRS of any grade, and 2 died from it. CRS causes high fever and myalgias, and severe CRS causes unstable hypotension that can require mechanical ventilation.
Tocilizumab, the IL-6R blocking antibody, was used in 27% of the patients, generally for grade 4 CRS.
CRS with CTL019
Dr Barrett described CRS in the first patient treated with CTL019 at CHOP in April 2012. The CRS was quite severe, with high fevers and unstable hypotension requiring multiple vasopressors and the need for mechanical ventilation.
“[W]e had no idea what was happening,” he said. “We didn’t understand what the source of the illness was.”
The patient did not respond to steroids or to etanercept, which Dr Barrett indicated is known to help in acute respiratory distress in transplant patients.
“And it was only through some incredible clinical acumen of the treating physicians as well as incredible critical care that was delivered by our ICU that kept this patient alive long enough for us to try tocilizumab,” Dr Barrett continued, “which, thankfully, worked by blocking the most severe side effects in this patient and allowed her to survive.”
Dr Barrett described the course of another patient who developed grade 4 CRS that continued to get worse even after he received tocilizumab, siltuximab, and steroids.
The patient required vasoactive drugs, had seizures, required milrinone, and was placed on a ventilator. One year after receiving CAR T-cell therapy, he recovered.
“This is an incredibly terrifying syndrome to take care of when we don’t understand what’s triggering it or how to stop it,” Dr Barrett emphasized.
Studying CRS
IL-6 is clearly a critical cytokine in the toxicity of CAR T-cell therapy, Dr Barrett said, but IFNγ and other cytokines are also important.
He and his colleagues performed a comprehensive cytokine analysis of pediatric patients treated with CTL019—specifically, engineered T cells composed of an anti-CD19 single-chain variable fragment, CD3ζ activation domain, a 4-1BB costimulatory domain, and transduced with a lentivirus grown on CD3/CD28 beads with a little bit of IL-2.
With that specific CAR, Dr Barrett said they observed a MAS pattern—IFNγ, IL-10, IL-6, and IL-8, which are most elevated in grades 4 and 5 CRS.
“[S]o this pattern, and this clinical syndrome [CRS] was what we believe was driving toxicity in this model,” he said.
To figure out why this was happening, the investigators created 4-1BB CAR-mediated CRS in a mouse model.
The team took leukemia cells from the first patient treated and clinical T cells from her CAR product and put them in an NSG mouse model that they had used for preclinical development.
The investigators then measured cytokine production in the serum of animals 3 and 7 days post-treatment with CTL019.
“And nothing happened,” Dr Barrett said. “The mice didn’t get sick, they cleared their leukemia, and when you looked for cytokines, you found IFNγ, IL-2, and GM-CSF, but you did not find IL-6.”
The team had also included etanercept and tocilizumab in this model, but since the mice didn’t make the toxic cytokines, the antibodies didn’t do anything.
“So why did she get so sick but yet her cancer and her CAR T cells did not make these mice sick and not generate these cytokines?” Dr Barrett asked.
The investigators hypothesized that APCs—not the CAR T cells—were responsible for the toxic cytokines secreted.
“[I]t would be the CAR T-cell-mediated killing of leukemia which would induce this cytokine release from the antigen-presenting cell lineages,” Dr Barrett explained.
To test this theory, the investigators co-cultured CTL019 and Nalm-6 leukemia, with or without cells derived from peripheral blood monocytes.
The team found that IL-6 levels were elevated several logs when CAR T cells killed leukemia in the presence of the APCs.
On the other hand, co-culture of only CTL019 and Nalm-6 produced high levels of GM-CSF, IFNγ, IL-2, and IL-10 but no detectable IL-6 or IL-8.
Transwell in vitro experiments separating CTL019 and Nalm-6 from the APCs showed the same pattern.
The investigators thus confirmed that IL-6 is made by APCs in response to CAR-mediated killing of leukemia.
Nanostring profiling
The team then performed nanostring RNA analysis of separated cell populations recovered from that experiment.
They found that IL-6 and IL-8 are produced by APCs but not by CTL019. IL-2 and IFNγ are produced by CTL019 and not by APCs, and GM-CSF was produced from CTL019.
“There was a clear separation in cytokine production in this model,” Dr Barrett said.
The investigators also observed that the CTL019 nanostring profile was unaffected by proximity to the APCs and all the IL-6 they make.
“CART19 T cells did not seem to care, on a transcriptional level, that all this IL-6 was floating around,” Dr Barrett said.
In contrast, the APCs do change, he said, when CAR T cells are killing leukemia nearby.
“There are dozens and dozens of changes,” he said, “including many in chemokines and IL-6 and IL-8.”
The investigators performed multiple in vitro killing assays and found no difference in CAR T-cell killing potential in the presence or absence of the MAS cytokines.
They also performed peripheral blood analysis of patients experiencing CRS of grades 2 to 5. The team observed that clinical CRS may be divided into MAS and not-MAS patterns. In addition, they detected no IL-6 transcript in any of the CAR T cells isolated from these patients.
“I think we’re going to discover that cytokine release syndrome is a clinical entity that has multiple mechanisms,” Dr Barrett said. “And so it’s very important, when we are talking about our models and talking about our results, to be sure that we’re all speaking the same language.” ![]()
HU trial to prevent stroke in SCA feasible in Nigeria

© Todd Buchanan 2016
SAN DIEGO—High rates of recruitment (90%), enrollment (92%), and adherence to study drug and follow-up visits have confirmed the feasibility of conducting a trial of hydroxyurea (HU) for stroke prevention in Nigeria (the SPIN trial), researchers say.
The 235 children with sickle cell anemia (SCA)enrolled on the SPIN trial did not miss any of the scheduled monthly visits, and drug adherence was 84% based on the increase in their mean corpuscular volume (MCV) by 10 fL.
These data provide strong evidence, researchers believe, for patient and family acceptability of the trial and potential safety of a moderate dose of HU to prevent stroke in children with SCA in Nigeria.
Nigeria has the largest burden of sickle cell disease (SCD) in the world, Najibah Galadanci, MBBS, of Bayero University/Aminu Kano Teaching Hospital in Nigeria, said at the 2016 ASH Annual Meeting.
Every year, about 150,000 children in Nigeria are born with SCD. This compares with 2400 children in the United States and 300 children in the United Kingdom.
“And it is estimated that 15,000 children with SCA per year in Nigeria will have strokes,” Dr Galadanci added.
She presented data from the SPIN trial (NCT01801423) at ASH as abstract 122.
At present, she explained, primary stroke prevention consists of regular blood transfusions for patients with transcranial Doppler (TCD) measurements higher than 200 cm/second.
However, distinct challenges with this prevention method exist in sub-Saharan Africa, such as inadequate blood supply, cost, unsafe transfusion practice, and the high probability of blood-borne infections.
HU is the only drug approved by the US Food and Drug administration to treat SCD. It increases total hemoglobin level, which is associated with a decreased risk of strokes.
In addition, HU significantly decreases TCD ultrasound velocity in children with SCD and abnormal TCD and is cost-effective and practical in sub-Saharan Africa.
So investigators at Aminu Kano teaching hospital in Nigeria undertook to study the feasibility of using HU to prevent stroke in children with SCD.
The team based their decision on 3 main components: recruitment rate, retention rate, and adherence to study medication.
SPIN trial
Children ages 5 to 12 were eligible if they had a diagnosis of SCA, either HbSS or HbSb0. They had to have 2 independent readings of elevated TCD velocity of 200 to 219 cm/second or 1 reading of 220 cm/second or higher.
Investigators enrolled 25 children on the treatment arm. The children received a moderate dose (20 mg/kg/day) of HU for 3 years.
Investigators also enrolled a comparison group of 210 children with SCA who had a TCD velocity of less than 200 cm/second.
The median follow-up was 2.1 years. The median age was 6.8 years and 8 years in the treatment and comparison groups, respectively.
The treatment group had a total of 603 follow-up visits.
The recruitment rate was 90% (335 of 370 families), the enrollment rate for the treatment arm was 92% (25 of 27 patients), and the adherence rate to monthly visits was 100%. Eighty-four percent of patients (21/25) adhered to the medication regimen, based on their increased MCV.
HU therapy
Investigators observed no laboratory evidence of severe myelosuppression or toxicity.
Of 712 complete blood counts performed on 25 study participants, 2 patients had repeated hemoglobin counts of less than 6 g/dL, and no participant had a repeat platelet count below 80 x 109/L nor a repeat absolute neutrophil count of less than 1.2 x 109/L.
Investigators found no significant difference overall (P=0.37) in the rate of hospitalization between the treatment and comparison groups based on hospitalizations for acute chest syndrome, pain, stroke, transfusion, malaria, and infection.
Investigators also found no significant difference (P=0.67) in rates of severe adverse events between the study and comparison groups.
Twelve deaths occurred during the study period, 2 in the treatment group (2.69/100 patient years) and 10 in the comparison group (1.81/100 patient years).
Deaths in the treatment arm were due to sepsis and progressive renal disease. Deaths in the comparison group were due to severe anemia, infection, and malaria.
“The most interesting finding of our study,” Dr Galadanci indicated, “was the 85% reduction in TCD velocity after starting hydroxyurea therapy.”
Baseline TCD measurements went from 211 cm/second to 165 cm/second at 24 months.
Dr Galadanci said next steps include conducting a phase 3, multicenter, randomized controlled trial (NCT 02560935) comparing low-dose (10 mg/kg/day) and moderate-dose (20 mg/kg/day) HU therapy for preventing primary strokes in children with SCA living in Nigeria (SPRING Trial).
Investigators hypothesize there will be a 66% reduction over 3 years in relative risk of primary strokes in children with SCA and elevated TCD velocity in the moderate-dose group compared to the low-dose group. ![]()

© Todd Buchanan 2016
SAN DIEGO—High rates of recruitment (90%), enrollment (92%), and adherence to study drug and follow-up visits have confirmed the feasibility of conducting a trial of hydroxyurea (HU) for stroke prevention in Nigeria (the SPIN trial), researchers say.
The 235 children with sickle cell anemia (SCA)enrolled on the SPIN trial did not miss any of the scheduled monthly visits, and drug adherence was 84% based on the increase in their mean corpuscular volume (MCV) by 10 fL.
These data provide strong evidence, researchers believe, for patient and family acceptability of the trial and potential safety of a moderate dose of HU to prevent stroke in children with SCA in Nigeria.
Nigeria has the largest burden of sickle cell disease (SCD) in the world, Najibah Galadanci, MBBS, of Bayero University/Aminu Kano Teaching Hospital in Nigeria, said at the 2016 ASH Annual Meeting.
Every year, about 150,000 children in Nigeria are born with SCD. This compares with 2400 children in the United States and 300 children in the United Kingdom.
“And it is estimated that 15,000 children with SCA per year in Nigeria will have strokes,” Dr Galadanci added.
She presented data from the SPIN trial (NCT01801423) at ASH as abstract 122.
At present, she explained, primary stroke prevention consists of regular blood transfusions for patients with transcranial Doppler (TCD) measurements higher than 200 cm/second.
However, distinct challenges with this prevention method exist in sub-Saharan Africa, such as inadequate blood supply, cost, unsafe transfusion practice, and the high probability of blood-borne infections.
HU is the only drug approved by the US Food and Drug administration to treat SCD. It increases total hemoglobin level, which is associated with a decreased risk of strokes.
In addition, HU significantly decreases TCD ultrasound velocity in children with SCD and abnormal TCD and is cost-effective and practical in sub-Saharan Africa.
So investigators at Aminu Kano teaching hospital in Nigeria undertook to study the feasibility of using HU to prevent stroke in children with SCD.
The team based their decision on 3 main components: recruitment rate, retention rate, and adherence to study medication.
SPIN trial
Children ages 5 to 12 were eligible if they had a diagnosis of SCA, either HbSS or HbSb0. They had to have 2 independent readings of elevated TCD velocity of 200 to 219 cm/second or 1 reading of 220 cm/second or higher.
Investigators enrolled 25 children on the treatment arm. The children received a moderate dose (20 mg/kg/day) of HU for 3 years.
Investigators also enrolled a comparison group of 210 children with SCA who had a TCD velocity of less than 200 cm/second.
The median follow-up was 2.1 years. The median age was 6.8 years and 8 years in the treatment and comparison groups, respectively.
The treatment group had a total of 603 follow-up visits.
The recruitment rate was 90% (335 of 370 families), the enrollment rate for the treatment arm was 92% (25 of 27 patients), and the adherence rate to monthly visits was 100%. Eighty-four percent of patients (21/25) adhered to the medication regimen, based on their increased MCV.
HU therapy
Investigators observed no laboratory evidence of severe myelosuppression or toxicity.
Of 712 complete blood counts performed on 25 study participants, 2 patients had repeated hemoglobin counts of less than 6 g/dL, and no participant had a repeat platelet count below 80 x 109/L nor a repeat absolute neutrophil count of less than 1.2 x 109/L.
Investigators found no significant difference overall (P=0.37) in the rate of hospitalization between the treatment and comparison groups based on hospitalizations for acute chest syndrome, pain, stroke, transfusion, malaria, and infection.
Investigators also found no significant difference (P=0.67) in rates of severe adverse events between the study and comparison groups.
Twelve deaths occurred during the study period, 2 in the treatment group (2.69/100 patient years) and 10 in the comparison group (1.81/100 patient years).
Deaths in the treatment arm were due to sepsis and progressive renal disease. Deaths in the comparison group were due to severe anemia, infection, and malaria.
“The most interesting finding of our study,” Dr Galadanci indicated, “was the 85% reduction in TCD velocity after starting hydroxyurea therapy.”
Baseline TCD measurements went from 211 cm/second to 165 cm/second at 24 months.
Dr Galadanci said next steps include conducting a phase 3, multicenter, randomized controlled trial (NCT 02560935) comparing low-dose (10 mg/kg/day) and moderate-dose (20 mg/kg/day) HU therapy for preventing primary strokes in children with SCA living in Nigeria (SPRING Trial).
Investigators hypothesize there will be a 66% reduction over 3 years in relative risk of primary strokes in children with SCA and elevated TCD velocity in the moderate-dose group compared to the low-dose group. ![]()

© Todd Buchanan 2016
SAN DIEGO—High rates of recruitment (90%), enrollment (92%), and adherence to study drug and follow-up visits have confirmed the feasibility of conducting a trial of hydroxyurea (HU) for stroke prevention in Nigeria (the SPIN trial), researchers say.
The 235 children with sickle cell anemia (SCA)enrolled on the SPIN trial did not miss any of the scheduled monthly visits, and drug adherence was 84% based on the increase in their mean corpuscular volume (MCV) by 10 fL.
These data provide strong evidence, researchers believe, for patient and family acceptability of the trial and potential safety of a moderate dose of HU to prevent stroke in children with SCA in Nigeria.
Nigeria has the largest burden of sickle cell disease (SCD) in the world, Najibah Galadanci, MBBS, of Bayero University/Aminu Kano Teaching Hospital in Nigeria, said at the 2016 ASH Annual Meeting.
Every year, about 150,000 children in Nigeria are born with SCD. This compares with 2400 children in the United States and 300 children in the United Kingdom.
“And it is estimated that 15,000 children with SCA per year in Nigeria will have strokes,” Dr Galadanci added.
She presented data from the SPIN trial (NCT01801423) at ASH as abstract 122.
At present, she explained, primary stroke prevention consists of regular blood transfusions for patients with transcranial Doppler (TCD) measurements higher than 200 cm/second.
However, distinct challenges with this prevention method exist in sub-Saharan Africa, such as inadequate blood supply, cost, unsafe transfusion practice, and the high probability of blood-borne infections.
HU is the only drug approved by the US Food and Drug administration to treat SCD. It increases total hemoglobin level, which is associated with a decreased risk of strokes.
In addition, HU significantly decreases TCD ultrasound velocity in children with SCD and abnormal TCD and is cost-effective and practical in sub-Saharan Africa.
So investigators at Aminu Kano teaching hospital in Nigeria undertook to study the feasibility of using HU to prevent stroke in children with SCD.
The team based their decision on 3 main components: recruitment rate, retention rate, and adherence to study medication.
SPIN trial
Children ages 5 to 12 were eligible if they had a diagnosis of SCA, either HbSS or HbSb0. They had to have 2 independent readings of elevated TCD velocity of 200 to 219 cm/second or 1 reading of 220 cm/second or higher.
Investigators enrolled 25 children on the treatment arm. The children received a moderate dose (20 mg/kg/day) of HU for 3 years.
Investigators also enrolled a comparison group of 210 children with SCA who had a TCD velocity of less than 200 cm/second.
The median follow-up was 2.1 years. The median age was 6.8 years and 8 years in the treatment and comparison groups, respectively.
The treatment group had a total of 603 follow-up visits.
The recruitment rate was 90% (335 of 370 families), the enrollment rate for the treatment arm was 92% (25 of 27 patients), and the adherence rate to monthly visits was 100%. Eighty-four percent of patients (21/25) adhered to the medication regimen, based on their increased MCV.
HU therapy
Investigators observed no laboratory evidence of severe myelosuppression or toxicity.
Of 712 complete blood counts performed on 25 study participants, 2 patients had repeated hemoglobin counts of less than 6 g/dL, and no participant had a repeat platelet count below 80 x 109/L nor a repeat absolute neutrophil count of less than 1.2 x 109/L.
Investigators found no significant difference overall (P=0.37) in the rate of hospitalization between the treatment and comparison groups based on hospitalizations for acute chest syndrome, pain, stroke, transfusion, malaria, and infection.
Investigators also found no significant difference (P=0.67) in rates of severe adverse events between the study and comparison groups.
Twelve deaths occurred during the study period, 2 in the treatment group (2.69/100 patient years) and 10 in the comparison group (1.81/100 patient years).
Deaths in the treatment arm were due to sepsis and progressive renal disease. Deaths in the comparison group were due to severe anemia, infection, and malaria.
“The most interesting finding of our study,” Dr Galadanci indicated, “was the 85% reduction in TCD velocity after starting hydroxyurea therapy.”
Baseline TCD measurements went from 211 cm/second to 165 cm/second at 24 months.
Dr Galadanci said next steps include conducting a phase 3, multicenter, randomized controlled trial (NCT 02560935) comparing low-dose (10 mg/kg/day) and moderate-dose (20 mg/kg/day) HU therapy for preventing primary strokes in children with SCA living in Nigeria (SPRING Trial).
Investigators hypothesize there will be a 66% reduction over 3 years in relative risk of primary strokes in children with SCA and elevated TCD velocity in the moderate-dose group compared to the low-dose group. ![]()
Old drug, new tricks possible in MM

SAN DIEGO—An antiretroviral drug used to treat the human immunodeficiency virus (HIV) may find a role in the treatment of multiple myeloma (MM) patients who are proteasome inhibitor (PI)-refractory.
According to investigators, nelfinavir may sensitize refractory patients so that PI-based treatments become an option for them.
In a phase 2 study of 34 patients, nelfinavir in combination with bortezomib and dexamethasone produced an objective response rate of 65%, which investigators called an “exceptional” response in this heavily pretreated, mostly dual-refractory patient population.
Christoph Driessen, MD, PhD, of Kantonsspital St Gallen in Switzerland, discussed the findings of this study, known as SAKK 39/13, at the 2016 ASH Annual Meeting as abstract 487.
Dr Driessen explained that downregulation of IRE1/XBP1 produces PI resistance, and this downregulation occurs in PI-refractory MM patients.
High expression of IRE1/XBP1 correlates with bortezomib sensitivity, and pharmacologic upregulation of IRE1/XBP1 re-sensitizes myeloma cells to PI treatment.
Nelfinavir, which overcomes PI resistance in vitro, is approved for oral HIV therapy.
“It’s an old drug, it’s a generic drug,” Dr Driessen said, and it’s approved at a dose of 2 x 1250 mg daily.
So the SAKK investigators undertook a phase 1 trial of nelfinavir in MM patients.
In an exploratory extension cohort, they found that 5 of 6 MM patients double-refractory to bortezomib and lenalidomide experienced clinical benefit from nelfinavir at the recommended phase 2 dose (2 x 2500 mg daily) in addition to standard treatment with bortezomib and dexamethasone.
Three patients achieved a partial response (PR) and 3 a minor response (MR).
The investigators’ objective in the phase 2 study was to determine whether the addition of nelfinavir to approved bortezomib-dexamethasone therapy is sufficiently active to merit further investigation in a randomized trial.
Study design
Patients in this prospective, single-arm, multicenter, open-label trial received the following treatment:
- Nelfinavir at 2 x 2500 mg orally on days 1–14
- Bortezomib at 1.3 mg/m2 intravenously or subcutaneously on days 1, 4, 8, and 11
- Dexamethasone at 20 mg orally on days 1-2, 4-5, 8-9, and 11-12 of each 21-day cycle.
Trial therapy lasted for a maximum of 6 cycles (18 weeks).
Dr Driessen explained that the trial “was a truly academic trial, without any finances from industry or drug support from industry. So we actually had to get a grant to buy commercial drugs for the study on the commercial drug market, and that limited the duration of treatment in this trial.”
The primary endpoint of the trial was response rate—best response of PR or better by IMWG criteria.
Investigators considered a 30% or higher response rate promising.
Secondary endpoints included adverse events, time to next new anti-myeloma therapy or death, progressive disease under trial treatment, duration of response, progression-free survival, and time to progression.
Patients were eligible to enroll if they had been exposed to or could not tolerate an immunomodulatory drug, were refractory to their most recent PI-containing regimen, had a performance status of 3 or less, had creatinine clearance of 15 mL/minute or greater, had a platelet count of 50,000/μL or more, and had a hemoglobin level of 8.0 g/dL or higher.
Patients were excluded if they had uncontrolled, clinically significant, active concurrent disease, concomitant additional systemic cancer treatment, concomitant radiotherapy, or significant neuropathy of grades 3-4 or grade 2 with pain.
Patient population
Thirty-four patients enrolled on the trial. They were a median age of 67 (range, 42–82), 62% were male, 91% had a performance status of 0 or 1, and 76% had a prior autologous stem cell transplant.
They had a median of 5 prior systemic therapies (range, 2–10), and 38% had poor-risk cytogenetics.
The time from last dose of prior therapy to enrollment on the study was a median of 27 days.
“So [it was] a truly progressive, highly refractory myeloma population,” Dr Driessen emphasized.
All 34 patients were refractory to bortezomib. All patients were also exposed to lenalidomide, and 79% were refractory to it.
Forty-four percent were refractory to pomalidomide, and 6% were refractory to carfilzomib. One patient was refractory to all 4 agents.
“Very few patients were exposed to carfilzomib because it wasn’t available in Switzerland at that time,” Dr Driessen explained.
Efficacy
Patients received a median of 4.5 cycles of therapy (range, 1–6), and the best response of PR or greater was achieved by 22 patients (65%).
Five patients (15%) achieved a very good partial response (VGPR), 17 (50%) PR, 3 (9%) MR, and 4 (12%) stable disease.
Twenty-five patients (74%) achieved a clinical benefit (VGPR+PR+MR).
Ten of the 13 patients (77%) with poor-risk cytogenetics achieved a best response of PR or greater.
Patients had a median of 16 weeks (range, 13–24) time to a new anti-myeloma therapy or death, and 13 patients (38%) had confirmed progressive disease while on trial therapy.
In 32 patients, all but 4 had a decrease from baseline in serum M protein or serum free light chain concentration.
Efficacy by prior therapy
Twenty-two of 34 patients (65%) refractory to bortezomib had a best response of PR or greater.
For patients refractory to bortezomib and lenalidomide, 70% achieved a best response of PR or greater.
For patients refractory to bortezomib, lenalidomide, and pomalidomide, 60% achieved a best response of PR or greater.
And for patients who were refractory to bortezomib, lenalidomide, and carfilzomib, 50% achieved a best response of PR or greater.
Adverse events
“The hematologic toxicity was essentially what you would expect from this heavily pretreated population,” Dr Driessen said.
“We did, however, experience 4 deaths on the trial therapy from infectious complications of sepsis and neutropenia, and we don’t know whether this is a true signal or whether this is due to the low numbers. We did not mandate antibiotic prophylaxis on the trial.”
Grade 3 or higher adverse events (AEs) occurring in 2 or more patients were anemia (n=10), febrile neutropenia (n=4, including 1 grade 5), thrombocytopenia (n=15), lung infection (n=8), sepsis (n=3, all grade 5), fatigue (n=5), peripheral sensory neuropathy (n=3), hypertension (n=6), increased creatinine (n=4), hyperglycemia (n=6) hypokalemia (n=3), and hyponatremia (n=5).
Dr Driessen indicated that with a future generic version of bortezomib, nelfinavir plus bortezomib and dexamethasone “has the potential to become a fully generic, affordable, active therapy option for PI-refractory patients.”
The investigators believe the results of their study call for further development of nelfinavir as a sensitizing drug for PI-based treatments and as a promising new agent for MM therapy. ![]()

SAN DIEGO—An antiretroviral drug used to treat the human immunodeficiency virus (HIV) may find a role in the treatment of multiple myeloma (MM) patients who are proteasome inhibitor (PI)-refractory.
According to investigators, nelfinavir may sensitize refractory patients so that PI-based treatments become an option for them.
In a phase 2 study of 34 patients, nelfinavir in combination with bortezomib and dexamethasone produced an objective response rate of 65%, which investigators called an “exceptional” response in this heavily pretreated, mostly dual-refractory patient population.
Christoph Driessen, MD, PhD, of Kantonsspital St Gallen in Switzerland, discussed the findings of this study, known as SAKK 39/13, at the 2016 ASH Annual Meeting as abstract 487.
Dr Driessen explained that downregulation of IRE1/XBP1 produces PI resistance, and this downregulation occurs in PI-refractory MM patients.
High expression of IRE1/XBP1 correlates with bortezomib sensitivity, and pharmacologic upregulation of IRE1/XBP1 re-sensitizes myeloma cells to PI treatment.
Nelfinavir, which overcomes PI resistance in vitro, is approved for oral HIV therapy.
“It’s an old drug, it’s a generic drug,” Dr Driessen said, and it’s approved at a dose of 2 x 1250 mg daily.
So the SAKK investigators undertook a phase 1 trial of nelfinavir in MM patients.
In an exploratory extension cohort, they found that 5 of 6 MM patients double-refractory to bortezomib and lenalidomide experienced clinical benefit from nelfinavir at the recommended phase 2 dose (2 x 2500 mg daily) in addition to standard treatment with bortezomib and dexamethasone.
Three patients achieved a partial response (PR) and 3 a minor response (MR).
The investigators’ objective in the phase 2 study was to determine whether the addition of nelfinavir to approved bortezomib-dexamethasone therapy is sufficiently active to merit further investigation in a randomized trial.
Study design
Patients in this prospective, single-arm, multicenter, open-label trial received the following treatment:
- Nelfinavir at 2 x 2500 mg orally on days 1–14
- Bortezomib at 1.3 mg/m2 intravenously or subcutaneously on days 1, 4, 8, and 11
- Dexamethasone at 20 mg orally on days 1-2, 4-5, 8-9, and 11-12 of each 21-day cycle.
Trial therapy lasted for a maximum of 6 cycles (18 weeks).
Dr Driessen explained that the trial “was a truly academic trial, without any finances from industry or drug support from industry. So we actually had to get a grant to buy commercial drugs for the study on the commercial drug market, and that limited the duration of treatment in this trial.”
The primary endpoint of the trial was response rate—best response of PR or better by IMWG criteria.
Investigators considered a 30% or higher response rate promising.
Secondary endpoints included adverse events, time to next new anti-myeloma therapy or death, progressive disease under trial treatment, duration of response, progression-free survival, and time to progression.
Patients were eligible to enroll if they had been exposed to or could not tolerate an immunomodulatory drug, were refractory to their most recent PI-containing regimen, had a performance status of 3 or less, had creatinine clearance of 15 mL/minute or greater, had a platelet count of 50,000/μL or more, and had a hemoglobin level of 8.0 g/dL or higher.
Patients were excluded if they had uncontrolled, clinically significant, active concurrent disease, concomitant additional systemic cancer treatment, concomitant radiotherapy, or significant neuropathy of grades 3-4 or grade 2 with pain.
Patient population
Thirty-four patients enrolled on the trial. They were a median age of 67 (range, 42–82), 62% were male, 91% had a performance status of 0 or 1, and 76% had a prior autologous stem cell transplant.
They had a median of 5 prior systemic therapies (range, 2–10), and 38% had poor-risk cytogenetics.
The time from last dose of prior therapy to enrollment on the study was a median of 27 days.
“So [it was] a truly progressive, highly refractory myeloma population,” Dr Driessen emphasized.
All 34 patients were refractory to bortezomib. All patients were also exposed to lenalidomide, and 79% were refractory to it.
Forty-four percent were refractory to pomalidomide, and 6% were refractory to carfilzomib. One patient was refractory to all 4 agents.
“Very few patients were exposed to carfilzomib because it wasn’t available in Switzerland at that time,” Dr Driessen explained.
Efficacy
Patients received a median of 4.5 cycles of therapy (range, 1–6), and the best response of PR or greater was achieved by 22 patients (65%).
Five patients (15%) achieved a very good partial response (VGPR), 17 (50%) PR, 3 (9%) MR, and 4 (12%) stable disease.
Twenty-five patients (74%) achieved a clinical benefit (VGPR+PR+MR).
Ten of the 13 patients (77%) with poor-risk cytogenetics achieved a best response of PR or greater.
Patients had a median of 16 weeks (range, 13–24) time to a new anti-myeloma therapy or death, and 13 patients (38%) had confirmed progressive disease while on trial therapy.
In 32 patients, all but 4 had a decrease from baseline in serum M protein or serum free light chain concentration.
Efficacy by prior therapy
Twenty-two of 34 patients (65%) refractory to bortezomib had a best response of PR or greater.
For patients refractory to bortezomib and lenalidomide, 70% achieved a best response of PR or greater.
For patients refractory to bortezomib, lenalidomide, and pomalidomide, 60% achieved a best response of PR or greater.
And for patients who were refractory to bortezomib, lenalidomide, and carfilzomib, 50% achieved a best response of PR or greater.
Adverse events
“The hematologic toxicity was essentially what you would expect from this heavily pretreated population,” Dr Driessen said.
“We did, however, experience 4 deaths on the trial therapy from infectious complications of sepsis and neutropenia, and we don’t know whether this is a true signal or whether this is due to the low numbers. We did not mandate antibiotic prophylaxis on the trial.”
Grade 3 or higher adverse events (AEs) occurring in 2 or more patients were anemia (n=10), febrile neutropenia (n=4, including 1 grade 5), thrombocytopenia (n=15), lung infection (n=8), sepsis (n=3, all grade 5), fatigue (n=5), peripheral sensory neuropathy (n=3), hypertension (n=6), increased creatinine (n=4), hyperglycemia (n=6) hypokalemia (n=3), and hyponatremia (n=5).
Dr Driessen indicated that with a future generic version of bortezomib, nelfinavir plus bortezomib and dexamethasone “has the potential to become a fully generic, affordable, active therapy option for PI-refractory patients.”
The investigators believe the results of their study call for further development of nelfinavir as a sensitizing drug for PI-based treatments and as a promising new agent for MM therapy. ![]()

SAN DIEGO—An antiretroviral drug used to treat the human immunodeficiency virus (HIV) may find a role in the treatment of multiple myeloma (MM) patients who are proteasome inhibitor (PI)-refractory.
According to investigators, nelfinavir may sensitize refractory patients so that PI-based treatments become an option for them.
In a phase 2 study of 34 patients, nelfinavir in combination with bortezomib and dexamethasone produced an objective response rate of 65%, which investigators called an “exceptional” response in this heavily pretreated, mostly dual-refractory patient population.
Christoph Driessen, MD, PhD, of Kantonsspital St Gallen in Switzerland, discussed the findings of this study, known as SAKK 39/13, at the 2016 ASH Annual Meeting as abstract 487.
Dr Driessen explained that downregulation of IRE1/XBP1 produces PI resistance, and this downregulation occurs in PI-refractory MM patients.
High expression of IRE1/XBP1 correlates with bortezomib sensitivity, and pharmacologic upregulation of IRE1/XBP1 re-sensitizes myeloma cells to PI treatment.
Nelfinavir, which overcomes PI resistance in vitro, is approved for oral HIV therapy.
“It’s an old drug, it’s a generic drug,” Dr Driessen said, and it’s approved at a dose of 2 x 1250 mg daily.
So the SAKK investigators undertook a phase 1 trial of nelfinavir in MM patients.
In an exploratory extension cohort, they found that 5 of 6 MM patients double-refractory to bortezomib and lenalidomide experienced clinical benefit from nelfinavir at the recommended phase 2 dose (2 x 2500 mg daily) in addition to standard treatment with bortezomib and dexamethasone.
Three patients achieved a partial response (PR) and 3 a minor response (MR).
The investigators’ objective in the phase 2 study was to determine whether the addition of nelfinavir to approved bortezomib-dexamethasone therapy is sufficiently active to merit further investigation in a randomized trial.
Study design
Patients in this prospective, single-arm, multicenter, open-label trial received the following treatment:
- Nelfinavir at 2 x 2500 mg orally on days 1–14
- Bortezomib at 1.3 mg/m2 intravenously or subcutaneously on days 1, 4, 8, and 11
- Dexamethasone at 20 mg orally on days 1-2, 4-5, 8-9, and 11-12 of each 21-day cycle.
Trial therapy lasted for a maximum of 6 cycles (18 weeks).
Dr Driessen explained that the trial “was a truly academic trial, without any finances from industry or drug support from industry. So we actually had to get a grant to buy commercial drugs for the study on the commercial drug market, and that limited the duration of treatment in this trial.”
The primary endpoint of the trial was response rate—best response of PR or better by IMWG criteria.
Investigators considered a 30% or higher response rate promising.
Secondary endpoints included adverse events, time to next new anti-myeloma therapy or death, progressive disease under trial treatment, duration of response, progression-free survival, and time to progression.
Patients were eligible to enroll if they had been exposed to or could not tolerate an immunomodulatory drug, were refractory to their most recent PI-containing regimen, had a performance status of 3 or less, had creatinine clearance of 15 mL/minute or greater, had a platelet count of 50,000/μL or more, and had a hemoglobin level of 8.0 g/dL or higher.
Patients were excluded if they had uncontrolled, clinically significant, active concurrent disease, concomitant additional systemic cancer treatment, concomitant radiotherapy, or significant neuropathy of grades 3-4 or grade 2 with pain.
Patient population
Thirty-four patients enrolled on the trial. They were a median age of 67 (range, 42–82), 62% were male, 91% had a performance status of 0 or 1, and 76% had a prior autologous stem cell transplant.
They had a median of 5 prior systemic therapies (range, 2–10), and 38% had poor-risk cytogenetics.
The time from last dose of prior therapy to enrollment on the study was a median of 27 days.
“So [it was] a truly progressive, highly refractory myeloma population,” Dr Driessen emphasized.
All 34 patients were refractory to bortezomib. All patients were also exposed to lenalidomide, and 79% were refractory to it.
Forty-four percent were refractory to pomalidomide, and 6% were refractory to carfilzomib. One patient was refractory to all 4 agents.
“Very few patients were exposed to carfilzomib because it wasn’t available in Switzerland at that time,” Dr Driessen explained.
Efficacy
Patients received a median of 4.5 cycles of therapy (range, 1–6), and the best response of PR or greater was achieved by 22 patients (65%).
Five patients (15%) achieved a very good partial response (VGPR), 17 (50%) PR, 3 (9%) MR, and 4 (12%) stable disease.
Twenty-five patients (74%) achieved a clinical benefit (VGPR+PR+MR).
Ten of the 13 patients (77%) with poor-risk cytogenetics achieved a best response of PR or greater.
Patients had a median of 16 weeks (range, 13–24) time to a new anti-myeloma therapy or death, and 13 patients (38%) had confirmed progressive disease while on trial therapy.
In 32 patients, all but 4 had a decrease from baseline in serum M protein or serum free light chain concentration.
Efficacy by prior therapy
Twenty-two of 34 patients (65%) refractory to bortezomib had a best response of PR or greater.
For patients refractory to bortezomib and lenalidomide, 70% achieved a best response of PR or greater.
For patients refractory to bortezomib, lenalidomide, and pomalidomide, 60% achieved a best response of PR or greater.
And for patients who were refractory to bortezomib, lenalidomide, and carfilzomib, 50% achieved a best response of PR or greater.
Adverse events
“The hematologic toxicity was essentially what you would expect from this heavily pretreated population,” Dr Driessen said.
“We did, however, experience 4 deaths on the trial therapy from infectious complications of sepsis and neutropenia, and we don’t know whether this is a true signal or whether this is due to the low numbers. We did not mandate antibiotic prophylaxis on the trial.”
Grade 3 or higher adverse events (AEs) occurring in 2 or more patients were anemia (n=10), febrile neutropenia (n=4, including 1 grade 5), thrombocytopenia (n=15), lung infection (n=8), sepsis (n=3, all grade 5), fatigue (n=5), peripheral sensory neuropathy (n=3), hypertension (n=6), increased creatinine (n=4), hyperglycemia (n=6) hypokalemia (n=3), and hyponatremia (n=5).
Dr Driessen indicated that with a future generic version of bortezomib, nelfinavir plus bortezomib and dexamethasone “has the potential to become a fully generic, affordable, active therapy option for PI-refractory patients.”
The investigators believe the results of their study call for further development of nelfinavir as a sensitizing drug for PI-based treatments and as a promising new agent for MM therapy. ![]()
MM patients with t(11;14) benefit from venetoclax
SAN DIEGO—Venetoclax, the oral BCL-2 inhibitor approved by the US Food and Drug Administration to treat chronic lymphocytic leukemia (CLL) patients with 17p deletion, is also showing activity in multiple myeloma (MM) patients, particularly those with t(11;14).
Final results of a phase 1 study showed venetoclax to be safe as monotherapy in relapsed or refractory MM, producing a response rate of 40% in patients with the translocation and 21% overall.
Preliminary results of the study were presented at the 2015 ASH Annual Meeting, and final results were presented at the 2016 ASH Annual Meeting.
“So I think we have a drug that potentially can change the outcome of a lot of patients with myeloma,” Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota, said during the presentation of the findings at ASH (abstract 488*).
“[It] also opens the possibility of being combined with a variety of other therapeutics that we have in this disease today.”
Venetoclax induces cell death in MM cell lines, particularly those positive for t(11;14). The translocation correlates with higher ratios of BCL-2 to MCL-1 and BCL-2 to MCL-2L1 (BCL-XL) mRNA. BCL-2 and MCL-1 promote survival of MM cells.
Study design and enrollment
The phase 1, open-label, multicenter study was designed to determine the best tolerated dose of venetoclax.
Secondary and exploratory objectives included overall response rate (ORR), time to progression, duration of response, and predictive biomarkers.
Patients had to have previously treated MM with measurable disease, ECOG status of 0 or 1, and adequate organ function.
They were excluded if they had an active infection, a history of significant renal, neurologic, psychiatric, endocrine, immunologic, cardiovascular, or hepatic disease within 6 months of study entry, or a history of other active malignancies within 3 years of study entry.
The study called for a 2-week lead-in period of venetoclax with weekly dose escalation. Four different dose cohorts were evaluated—300 mg, 600 mg, 900 mg, and 1200 mg.
Thirty patients were enrolled during the lead-in period, and 36 additional patients enrolled at the maximum evaluated dose of 1200 mg in the safety expansion cohort, for a total of 66 patients.
Patients were treated on a 21-day cycle with daily venetoclax. They could also receive dexamethasone to continue on the study if they progressed while receiving the monotherapy.
Patient characteristics
Patient characteristics were “similar to what you would see in relapsed/refractory multiple myloma,” Dr Kumar said.
Median age was 63 (range, 31–79), and most (62%) were ISS stage II/III.
“I want to draw your attention to two features here,” Dr Kumar said.
“Thirty patients, or 46% of the patients, had 11;14 translocation, and that reflects the interest in this drug for this particular class of patients.”
Twelve patients (18%) had 17p deletion, 32 (48%) had 13q deletion, and 27 (41%) were hyperdiploid.
“What is most striking in this cohort of patients,” Dr Kumar added, “is the fact that the median number of prior lines of therapy was 5, with some as high as 15 prior lines of therapy.”
Seventy percent were refractory to bortezomib, 77% refractory to lenalidomide, and 61% refractory to both. Fifty-two patients (79%) were refractory to their last prior therapy.
Patient disposition
At the time of data cutoff on August 19, 2016, 11 patients (17%) were still active on the study.
The median time on study was 3.3 months (range, 0.2–27), median time on venetoclax monotherapy was 2.5 months (range, 0.2–25), and median time on venetoclax plus dexamethasone was 1.4 months (range, 1–13). Seventeen patients received the combination after disease progression.
Fifty-five patients (83%) discontinued treatment, 41 (62%) because of disease progression, 5 (8%) because of adverse events, 2 (3%) withdrew consent, 1 (2%) was lost to follow-up, and 6 (9%) for unspecified reasons.
The 5 adverse events leading to withdrawal included renal failure (n=2), worsening pulmonary disorder (n=1), paralyzing sciatica (n=1), and shortness of breath and pain (n=1).
“Eight patients died on study,” Dr Kumar said, “none thought to be related to the drug.”
Adverse events
The toxicity profile was primarily hematologic and gastrointestinal.
All patients experienced an adverse event of any grade, and 45 (68%) had a grade 3 or 4 event.
“I wanted to highlight that the majority of the gastrointestinal and non-hematologic toxicity we saw were grades 1 and 2,” Dr Kumar pointed out, “and could be managed symptomatically or with dose modifications.”
Grade 3-4 hematologic adverse events included thrombocytopenia (26%), neutropenia (21%), anemia (14%), leukopenia (14%), and lymphopenia (15%).
Grade 3-4 non-hematologic adverse events included nausea (3%), diarrhea (3%), fatigue (5%), back pain (8%), and vomiting (3%).
Serious adverse events occurring in 2% or more of patients included pneumonia (8%), sepsis (5%), pain, pyrexia, cough, and hypotension (3% each).
Two patients had dose-limiting toxicities of abdominal pain and nausea at the 600 mg dose.
No events of tumor lysis syndrome (TLS) were reported. Dr Kumar explained that this may have been the case because patients thought to be at high risk for TLS were mandated to be in the hospital and observed for early tumor lysis in the initial part of the study.
Response
The ORR was 21% in all patients, including a stringent complete response (sCR) of 3% and a CR of 4%.
“But what was really striking was the response rate that we observed in the 30 patients with translocation 11;14,” Dr Kumar said. “The overall response rate was 40%, with 14% of the patients having complete response or better [stringent CR] and 13% of the patients with very good partial response.”
The 36 patients without t(11;14) had a 6% ORR, 3% sCR, and 3% very good partial response.
“If you look at the response rates based on the type of therapy they were coming off or the drugs they were refractory to, the response rate is very similar across all these patient subgroups, irrespective of what groups of drugs they were refractory to,” he added.
Time to progression for all patients was about 2.5 months. For patients with the translocation, it was about 6.6 months.
“Responses were fairly durable among those who had a response,” Dr Kumar said, “considering these are patients with a median of 5 prior lines of therapy.”
Duration of response for patients with t(11;14) was close to 10 months.
Biomarker analysis
The underlying biology for the response was the BCL-2 to BCL-2L1 ratio, as the investigators had observed in the cell lines.
So they analyzed the BCL-2 gene expression ratio in 24 of the 30 patients with t(11;14).
The investigators used droplet digital PCR performed on CD138-selected bone marrow mononuclear cells collected at baseline.
Nine patients had a high ratio, and their ORR was 88%. Fifteen patients had a low ratio, and their ORR was 20%.
Median time to progression for patients with a high ratio was about 12 months. For those with a low ratio, it was about 9 months.
Median change in M protein for patients with t(11;14) was –53%, compared to +11% in the patients without the translocation.
The investigators recommend additional studies with venetoclax in MM, including those with alternative combination therapies.
Venetoclax is being developed by AbbVie, in partnership with Genentech and Roche. This study was sponsored by AbbVie. ![]()
*Data in the abstract differ from the presentation.
SAN DIEGO—Venetoclax, the oral BCL-2 inhibitor approved by the US Food and Drug Administration to treat chronic lymphocytic leukemia (CLL) patients with 17p deletion, is also showing activity in multiple myeloma (MM) patients, particularly those with t(11;14).
Final results of a phase 1 study showed venetoclax to be safe as monotherapy in relapsed or refractory MM, producing a response rate of 40% in patients with the translocation and 21% overall.
Preliminary results of the study were presented at the 2015 ASH Annual Meeting, and final results were presented at the 2016 ASH Annual Meeting.
“So I think we have a drug that potentially can change the outcome of a lot of patients with myeloma,” Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota, said during the presentation of the findings at ASH (abstract 488*).
“[It] also opens the possibility of being combined with a variety of other therapeutics that we have in this disease today.”
Venetoclax induces cell death in MM cell lines, particularly those positive for t(11;14). The translocation correlates with higher ratios of BCL-2 to MCL-1 and BCL-2 to MCL-2L1 (BCL-XL) mRNA. BCL-2 and MCL-1 promote survival of MM cells.
Study design and enrollment
The phase 1, open-label, multicenter study was designed to determine the best tolerated dose of venetoclax.
Secondary and exploratory objectives included overall response rate (ORR), time to progression, duration of response, and predictive biomarkers.
Patients had to have previously treated MM with measurable disease, ECOG status of 0 or 1, and adequate organ function.
They were excluded if they had an active infection, a history of significant renal, neurologic, psychiatric, endocrine, immunologic, cardiovascular, or hepatic disease within 6 months of study entry, or a history of other active malignancies within 3 years of study entry.
The study called for a 2-week lead-in period of venetoclax with weekly dose escalation. Four different dose cohorts were evaluated—300 mg, 600 mg, 900 mg, and 1200 mg.
Thirty patients were enrolled during the lead-in period, and 36 additional patients enrolled at the maximum evaluated dose of 1200 mg in the safety expansion cohort, for a total of 66 patients.
Patients were treated on a 21-day cycle with daily venetoclax. They could also receive dexamethasone to continue on the study if they progressed while receiving the monotherapy.
Patient characteristics
Patient characteristics were “similar to what you would see in relapsed/refractory multiple myloma,” Dr Kumar said.
Median age was 63 (range, 31–79), and most (62%) were ISS stage II/III.
“I want to draw your attention to two features here,” Dr Kumar said.
“Thirty patients, or 46% of the patients, had 11;14 translocation, and that reflects the interest in this drug for this particular class of patients.”
Twelve patients (18%) had 17p deletion, 32 (48%) had 13q deletion, and 27 (41%) were hyperdiploid.
“What is most striking in this cohort of patients,” Dr Kumar added, “is the fact that the median number of prior lines of therapy was 5, with some as high as 15 prior lines of therapy.”
Seventy percent were refractory to bortezomib, 77% refractory to lenalidomide, and 61% refractory to both. Fifty-two patients (79%) were refractory to their last prior therapy.
Patient disposition
At the time of data cutoff on August 19, 2016, 11 patients (17%) were still active on the study.
The median time on study was 3.3 months (range, 0.2–27), median time on venetoclax monotherapy was 2.5 months (range, 0.2–25), and median time on venetoclax plus dexamethasone was 1.4 months (range, 1–13). Seventeen patients received the combination after disease progression.
Fifty-five patients (83%) discontinued treatment, 41 (62%) because of disease progression, 5 (8%) because of adverse events, 2 (3%) withdrew consent, 1 (2%) was lost to follow-up, and 6 (9%) for unspecified reasons.
The 5 adverse events leading to withdrawal included renal failure (n=2), worsening pulmonary disorder (n=1), paralyzing sciatica (n=1), and shortness of breath and pain (n=1).
“Eight patients died on study,” Dr Kumar said, “none thought to be related to the drug.”
Adverse events
The toxicity profile was primarily hematologic and gastrointestinal.
All patients experienced an adverse event of any grade, and 45 (68%) had a grade 3 or 4 event.
“I wanted to highlight that the majority of the gastrointestinal and non-hematologic toxicity we saw were grades 1 and 2,” Dr Kumar pointed out, “and could be managed symptomatically or with dose modifications.”
Grade 3-4 hematologic adverse events included thrombocytopenia (26%), neutropenia (21%), anemia (14%), leukopenia (14%), and lymphopenia (15%).
Grade 3-4 non-hematologic adverse events included nausea (3%), diarrhea (3%), fatigue (5%), back pain (8%), and vomiting (3%).
Serious adverse events occurring in 2% or more of patients included pneumonia (8%), sepsis (5%), pain, pyrexia, cough, and hypotension (3% each).
Two patients had dose-limiting toxicities of abdominal pain and nausea at the 600 mg dose.
No events of tumor lysis syndrome (TLS) were reported. Dr Kumar explained that this may have been the case because patients thought to be at high risk for TLS were mandated to be in the hospital and observed for early tumor lysis in the initial part of the study.
Response
The ORR was 21% in all patients, including a stringent complete response (sCR) of 3% and a CR of 4%.
“But what was really striking was the response rate that we observed in the 30 patients with translocation 11;14,” Dr Kumar said. “The overall response rate was 40%, with 14% of the patients having complete response or better [stringent CR] and 13% of the patients with very good partial response.”
The 36 patients without t(11;14) had a 6% ORR, 3% sCR, and 3% very good partial response.
“If you look at the response rates based on the type of therapy they were coming off or the drugs they were refractory to, the response rate is very similar across all these patient subgroups, irrespective of what groups of drugs they were refractory to,” he added.
Time to progression for all patients was about 2.5 months. For patients with the translocation, it was about 6.6 months.
“Responses were fairly durable among those who had a response,” Dr Kumar said, “considering these are patients with a median of 5 prior lines of therapy.”
Duration of response for patients with t(11;14) was close to 10 months.
Biomarker analysis
The underlying biology for the response was the BCL-2 to BCL-2L1 ratio, as the investigators had observed in the cell lines.
So they analyzed the BCL-2 gene expression ratio in 24 of the 30 patients with t(11;14).
The investigators used droplet digital PCR performed on CD138-selected bone marrow mononuclear cells collected at baseline.
Nine patients had a high ratio, and their ORR was 88%. Fifteen patients had a low ratio, and their ORR was 20%.
Median time to progression for patients with a high ratio was about 12 months. For those with a low ratio, it was about 9 months.
Median change in M protein for patients with t(11;14) was –53%, compared to +11% in the patients without the translocation.
The investigators recommend additional studies with venetoclax in MM, including those with alternative combination therapies.
Venetoclax is being developed by AbbVie, in partnership with Genentech and Roche. This study was sponsored by AbbVie. ![]()
*Data in the abstract differ from the presentation.
SAN DIEGO—Venetoclax, the oral BCL-2 inhibitor approved by the US Food and Drug Administration to treat chronic lymphocytic leukemia (CLL) patients with 17p deletion, is also showing activity in multiple myeloma (MM) patients, particularly those with t(11;14).
Final results of a phase 1 study showed venetoclax to be safe as monotherapy in relapsed or refractory MM, producing a response rate of 40% in patients with the translocation and 21% overall.
Preliminary results of the study were presented at the 2015 ASH Annual Meeting, and final results were presented at the 2016 ASH Annual Meeting.
“So I think we have a drug that potentially can change the outcome of a lot of patients with myeloma,” Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota, said during the presentation of the findings at ASH (abstract 488*).
“[It] also opens the possibility of being combined with a variety of other therapeutics that we have in this disease today.”
Venetoclax induces cell death in MM cell lines, particularly those positive for t(11;14). The translocation correlates with higher ratios of BCL-2 to MCL-1 and BCL-2 to MCL-2L1 (BCL-XL) mRNA. BCL-2 and MCL-1 promote survival of MM cells.
Study design and enrollment
The phase 1, open-label, multicenter study was designed to determine the best tolerated dose of venetoclax.
Secondary and exploratory objectives included overall response rate (ORR), time to progression, duration of response, and predictive biomarkers.
Patients had to have previously treated MM with measurable disease, ECOG status of 0 or 1, and adequate organ function.
They were excluded if they had an active infection, a history of significant renal, neurologic, psychiatric, endocrine, immunologic, cardiovascular, or hepatic disease within 6 months of study entry, or a history of other active malignancies within 3 years of study entry.
The study called for a 2-week lead-in period of venetoclax with weekly dose escalation. Four different dose cohorts were evaluated—300 mg, 600 mg, 900 mg, and 1200 mg.
Thirty patients were enrolled during the lead-in period, and 36 additional patients enrolled at the maximum evaluated dose of 1200 mg in the safety expansion cohort, for a total of 66 patients.
Patients were treated on a 21-day cycle with daily venetoclax. They could also receive dexamethasone to continue on the study if they progressed while receiving the monotherapy.
Patient characteristics
Patient characteristics were “similar to what you would see in relapsed/refractory multiple myloma,” Dr Kumar said.
Median age was 63 (range, 31–79), and most (62%) were ISS stage II/III.
“I want to draw your attention to two features here,” Dr Kumar said.
“Thirty patients, or 46% of the patients, had 11;14 translocation, and that reflects the interest in this drug for this particular class of patients.”
Twelve patients (18%) had 17p deletion, 32 (48%) had 13q deletion, and 27 (41%) were hyperdiploid.
“What is most striking in this cohort of patients,” Dr Kumar added, “is the fact that the median number of prior lines of therapy was 5, with some as high as 15 prior lines of therapy.”
Seventy percent were refractory to bortezomib, 77% refractory to lenalidomide, and 61% refractory to both. Fifty-two patients (79%) were refractory to their last prior therapy.
Patient disposition
At the time of data cutoff on August 19, 2016, 11 patients (17%) were still active on the study.
The median time on study was 3.3 months (range, 0.2–27), median time on venetoclax monotherapy was 2.5 months (range, 0.2–25), and median time on venetoclax plus dexamethasone was 1.4 months (range, 1–13). Seventeen patients received the combination after disease progression.
Fifty-five patients (83%) discontinued treatment, 41 (62%) because of disease progression, 5 (8%) because of adverse events, 2 (3%) withdrew consent, 1 (2%) was lost to follow-up, and 6 (9%) for unspecified reasons.
The 5 adverse events leading to withdrawal included renal failure (n=2), worsening pulmonary disorder (n=1), paralyzing sciatica (n=1), and shortness of breath and pain (n=1).
“Eight patients died on study,” Dr Kumar said, “none thought to be related to the drug.”
Adverse events
The toxicity profile was primarily hematologic and gastrointestinal.
All patients experienced an adverse event of any grade, and 45 (68%) had a grade 3 or 4 event.
“I wanted to highlight that the majority of the gastrointestinal and non-hematologic toxicity we saw were grades 1 and 2,” Dr Kumar pointed out, “and could be managed symptomatically or with dose modifications.”
Grade 3-4 hematologic adverse events included thrombocytopenia (26%), neutropenia (21%), anemia (14%), leukopenia (14%), and lymphopenia (15%).
Grade 3-4 non-hematologic adverse events included nausea (3%), diarrhea (3%), fatigue (5%), back pain (8%), and vomiting (3%).
Serious adverse events occurring in 2% or more of patients included pneumonia (8%), sepsis (5%), pain, pyrexia, cough, and hypotension (3% each).
Two patients had dose-limiting toxicities of abdominal pain and nausea at the 600 mg dose.
No events of tumor lysis syndrome (TLS) were reported. Dr Kumar explained that this may have been the case because patients thought to be at high risk for TLS were mandated to be in the hospital and observed for early tumor lysis in the initial part of the study.
Response
The ORR was 21% in all patients, including a stringent complete response (sCR) of 3% and a CR of 4%.
“But what was really striking was the response rate that we observed in the 30 patients with translocation 11;14,” Dr Kumar said. “The overall response rate was 40%, with 14% of the patients having complete response or better [stringent CR] and 13% of the patients with very good partial response.”
The 36 patients without t(11;14) had a 6% ORR, 3% sCR, and 3% very good partial response.
“If you look at the response rates based on the type of therapy they were coming off or the drugs they were refractory to, the response rate is very similar across all these patient subgroups, irrespective of what groups of drugs they were refractory to,” he added.
Time to progression for all patients was about 2.5 months. For patients with the translocation, it was about 6.6 months.
“Responses were fairly durable among those who had a response,” Dr Kumar said, “considering these are patients with a median of 5 prior lines of therapy.”
Duration of response for patients with t(11;14) was close to 10 months.
Biomarker analysis
The underlying biology for the response was the BCL-2 to BCL-2L1 ratio, as the investigators had observed in the cell lines.
So they analyzed the BCL-2 gene expression ratio in 24 of the 30 patients with t(11;14).
The investigators used droplet digital PCR performed on CD138-selected bone marrow mononuclear cells collected at baseline.
Nine patients had a high ratio, and their ORR was 88%. Fifteen patients had a low ratio, and their ORR was 20%.
Median time to progression for patients with a high ratio was about 12 months. For those with a low ratio, it was about 9 months.
Median change in M protein for patients with t(11;14) was –53%, compared to +11% in the patients without the translocation.
The investigators recommend additional studies with venetoclax in MM, including those with alternative combination therapies.
Venetoclax is being developed by AbbVie, in partnership with Genentech and Roche. This study was sponsored by AbbVie. ![]()
*Data in the abstract differ from the presentation.
KTE-C19 feasible in most young, high-risk ALL patients, study suggests

Photo by Bill Branson
SAN DIEGO—Trial results suggest treatment with the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 is feasible for most young patients with high-risk B-cell acute lymphoblastic leukemia (ALL).
Nearly all ALL patients in this trial were able to receive their assigned dose of KTE-C19 after a preparative chemotherapy regimen.
The complete response (CR) rate in these patients was 62%, and the rate of severe cytokine release syndrome (CRS) was low.
Daniel W. Lee III, MD, of the University of Virginia in Charlottesville, presented these results at the 2016 ASH Annual Meeting (abstract 218).
Dr Lee noted that CAR T cells have shown promise in early studies, but morbidity related to high-grade CRS and/or neurotoxicity could limit wide applicability of this treatment in patients with high disease burden. Among those who achieve CR to CD19 CAR T-cell therapy, nearly half of patients relapse in the first year.
At ASH, Dr Lee reported results of a non-randomized clinical trial of KTE-C19, a CD19 CAR T-cell therapy under development by Kite Pharmaceuticals. The company did not sponsor this study, although investigators reported relationships with Kite and other companies. The trial was sponsored by the National Cancer Institute.
The trial included 53 children and young adults with relapsed/refractory ALL (n=51) or diffuse large B-cell lymphoma (n=2). The patients’ median age was 13 (range, 4-30), and most were male (n=41).
Of the ALL patients, 11 had primary refractory disease, 5 had Ph-positive ALL, 3 had Down syndrome, 6 had central nervous system (CNS) disease (2 with CNS3, 4 with CNS2), and 2 had MLL-rearranged ALL. The median ALL disease burden was 27%.
The first 21 patients received a low-dose fludarabine/cyclophosphamide preparative regimen, and the subsequent 32 patients received an alternative intensified preparative regimen in an attempt to mitigate severe CRS risk and improve response.
Possible intensive preparative regimens included higher-dose fludarabine/cyclophosphamide, fludarabine/high-dose cytarabine/G-CSF, and ifosfamide/etoposide.
All 53 patients had peripheral blood cells collected, and 52 were infused with CAR T cells. One patient did not receive an infusion due to progressive fungal pneumonia, and 2 patients received less than their assigned dose.
Therefore, Dr Lee said KTE-C19 was feasible in 94% of patients.
Efficacy
The median follow-up was 18.7 months.
Dr Lee said KTE-C19 “produced robust responses in very high-risk ALL patients.” He noted, however, that the CR rate was lower among patients with high disease burden.
The CR rate among the ALL patients was 62%. Of the 31 patients who achieved a CR, 28 had a minimal residual disease (MRD)-negative remission.
The rate of MRD-negative CR was 100% among the 11 patients with primary refractory ALL, 100% among the 6 patients with CNS disease, 60% among the 5 patients with Ph+ ALL, and 67% among the 3 with Down syndrome. Neither of the 2 patients with MLL-rearranged ALL responded.
“Attempts to increase response rate by modifying the preparative regimen have not yet been successful,” Dr Lee pointed out.
However, he noted superior response and overall survival rates among patients who received a fludarabine/cyclophosphamide preparative regimen.
“Median overall survival in all enrolled patients is 13.3 months with fludarabine/cyclophosphamide prep versus 5.5 months with other regimens,” he said.
The overall survival rate for the ALL patients was 28%, and the median overall survival was 11.2 months.
For patients who achieved an MRD-negative remission, the leukemia-free survival (LFS) rate was 56%. The median LFS was not reached.
Dr Lee noted that hematopoietic stem cell transplant (HSCT) after KTE-C19 correlated with decreased relapse rates and led to superior LFS.
Of the 28 patients who achieved MRD-negative CR, 21 went on to HSCT after KTE-C19. The median time to HSCT after CAR T-cell dose was 54 days. (Ten of the 28 patients had HSCT before receiving KTE-C19.)
Nineteen (91%) of the patients who proceeded to HSCT after KTE-C19 did not relapse, compared to 1 (14%) of the patients who did not have a post-CAR T transplant.
The median LFS was 4.9 months among the MRD responders who did not proceed to HSCT and undefined among MRD responders with a transplant after KTE-C19.
The probability of survival was 65% beginning at 18 months among patients who underwent HSCT and 14% beginning at 9.8 months among patients without a post-KTE-C19 transplant.
CD19 escape remains a challenge, Dr Lee said. The risk may be diminished, but not eradicated, with HSCT.
Toxicity
“There was a low rate of CRS, which was successfully managed with a grade-driven algorithm,” Dr Lee noted.
Five patients (10%) had grade 3 CRS, and 2 (4%) had grade 4 CRS.
Other grade 3/4 adverse events that were considered at least possibly related to therapy included fever (38% grade 3), febrile neutropenia (23% grade
3), hypotension (9% grade 3, 4% grade 4), LV systolic dysfunction (9% grade 3), prolonged QTc (2% grade 3), dysphasia (2% grade 3), cardiac arrest (2% grade 4), multi-organ failure (2% grade 3), hypoxia (2% grade 3, 2% grade 4), and pulmonary embolism (2% grade 3).
“There were no severe or permanent neurologic toxicities,” Dr Lee said. “Intensive neuropsychological testing in 13 patients revealed no consistent treatment-related neurocognitive decline, and several patients improved following therapy.”
In all, there were 46 cases of neurotoxicity, including visual hallucination (8 grade 1, 17%), headache (1 grade 3 [2%], 3 grade 2 [6%]), confusion (2 grade 1, 4%),
dysphasia (1 grade 3, 2%), delirium (1 grade 3, 2%), seizure (1 grade 2, 1 grade 1 [2% each]), ataxia (1 grade 2, 2%), tremor (1 grade 2, 2%), dysesthesia (1 grade 2, 2%), and dysarthria (1 grade 1, 2%). ![]()

Photo by Bill Branson
SAN DIEGO—Trial results suggest treatment with the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 is feasible for most young patients with high-risk B-cell acute lymphoblastic leukemia (ALL).
Nearly all ALL patients in this trial were able to receive their assigned dose of KTE-C19 after a preparative chemotherapy regimen.
The complete response (CR) rate in these patients was 62%, and the rate of severe cytokine release syndrome (CRS) was low.
Daniel W. Lee III, MD, of the University of Virginia in Charlottesville, presented these results at the 2016 ASH Annual Meeting (abstract 218).
Dr Lee noted that CAR T cells have shown promise in early studies, but morbidity related to high-grade CRS and/or neurotoxicity could limit wide applicability of this treatment in patients with high disease burden. Among those who achieve CR to CD19 CAR T-cell therapy, nearly half of patients relapse in the first year.
At ASH, Dr Lee reported results of a non-randomized clinical trial of KTE-C19, a CD19 CAR T-cell therapy under development by Kite Pharmaceuticals. The company did not sponsor this study, although investigators reported relationships with Kite and other companies. The trial was sponsored by the National Cancer Institute.
The trial included 53 children and young adults with relapsed/refractory ALL (n=51) or diffuse large B-cell lymphoma (n=2). The patients’ median age was 13 (range, 4-30), and most were male (n=41).
Of the ALL patients, 11 had primary refractory disease, 5 had Ph-positive ALL, 3 had Down syndrome, 6 had central nervous system (CNS) disease (2 with CNS3, 4 with CNS2), and 2 had MLL-rearranged ALL. The median ALL disease burden was 27%.
The first 21 patients received a low-dose fludarabine/cyclophosphamide preparative regimen, and the subsequent 32 patients received an alternative intensified preparative regimen in an attempt to mitigate severe CRS risk and improve response.
Possible intensive preparative regimens included higher-dose fludarabine/cyclophosphamide, fludarabine/high-dose cytarabine/G-CSF, and ifosfamide/etoposide.
All 53 patients had peripheral blood cells collected, and 52 were infused with CAR T cells. One patient did not receive an infusion due to progressive fungal pneumonia, and 2 patients received less than their assigned dose.
Therefore, Dr Lee said KTE-C19 was feasible in 94% of patients.
Efficacy
The median follow-up was 18.7 months.
Dr Lee said KTE-C19 “produced robust responses in very high-risk ALL patients.” He noted, however, that the CR rate was lower among patients with high disease burden.
The CR rate among the ALL patients was 62%. Of the 31 patients who achieved a CR, 28 had a minimal residual disease (MRD)-negative remission.
The rate of MRD-negative CR was 100% among the 11 patients with primary refractory ALL, 100% among the 6 patients with CNS disease, 60% among the 5 patients with Ph+ ALL, and 67% among the 3 with Down syndrome. Neither of the 2 patients with MLL-rearranged ALL responded.
“Attempts to increase response rate by modifying the preparative regimen have not yet been successful,” Dr Lee pointed out.
However, he noted superior response and overall survival rates among patients who received a fludarabine/cyclophosphamide preparative regimen.
“Median overall survival in all enrolled patients is 13.3 months with fludarabine/cyclophosphamide prep versus 5.5 months with other regimens,” he said.
The overall survival rate for the ALL patients was 28%, and the median overall survival was 11.2 months.
For patients who achieved an MRD-negative remission, the leukemia-free survival (LFS) rate was 56%. The median LFS was not reached.
Dr Lee noted that hematopoietic stem cell transplant (HSCT) after KTE-C19 correlated with decreased relapse rates and led to superior LFS.
Of the 28 patients who achieved MRD-negative CR, 21 went on to HSCT after KTE-C19. The median time to HSCT after CAR T-cell dose was 54 days. (Ten of the 28 patients had HSCT before receiving KTE-C19.)
Nineteen (91%) of the patients who proceeded to HSCT after KTE-C19 did not relapse, compared to 1 (14%) of the patients who did not have a post-CAR T transplant.
The median LFS was 4.9 months among the MRD responders who did not proceed to HSCT and undefined among MRD responders with a transplant after KTE-C19.
The probability of survival was 65% beginning at 18 months among patients who underwent HSCT and 14% beginning at 9.8 months among patients without a post-KTE-C19 transplant.
CD19 escape remains a challenge, Dr Lee said. The risk may be diminished, but not eradicated, with HSCT.
Toxicity
“There was a low rate of CRS, which was successfully managed with a grade-driven algorithm,” Dr Lee noted.
Five patients (10%) had grade 3 CRS, and 2 (4%) had grade 4 CRS.
Other grade 3/4 adverse events that were considered at least possibly related to therapy included fever (38% grade 3), febrile neutropenia (23% grade
3), hypotension (9% grade 3, 4% grade 4), LV systolic dysfunction (9% grade 3), prolonged QTc (2% grade 3), dysphasia (2% grade 3), cardiac arrest (2% grade 4), multi-organ failure (2% grade 3), hypoxia (2% grade 3, 2% grade 4), and pulmonary embolism (2% grade 3).
“There were no severe or permanent neurologic toxicities,” Dr Lee said. “Intensive neuropsychological testing in 13 patients revealed no consistent treatment-related neurocognitive decline, and several patients improved following therapy.”
In all, there were 46 cases of neurotoxicity, including visual hallucination (8 grade 1, 17%), headache (1 grade 3 [2%], 3 grade 2 [6%]), confusion (2 grade 1, 4%),
dysphasia (1 grade 3, 2%), delirium (1 grade 3, 2%), seizure (1 grade 2, 1 grade 1 [2% each]), ataxia (1 grade 2, 2%), tremor (1 grade 2, 2%), dysesthesia (1 grade 2, 2%), and dysarthria (1 grade 1, 2%). ![]()

Photo by Bill Branson
SAN DIEGO—Trial results suggest treatment with the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 is feasible for most young patients with high-risk B-cell acute lymphoblastic leukemia (ALL).
Nearly all ALL patients in this trial were able to receive their assigned dose of KTE-C19 after a preparative chemotherapy regimen.
The complete response (CR) rate in these patients was 62%, and the rate of severe cytokine release syndrome (CRS) was low.
Daniel W. Lee III, MD, of the University of Virginia in Charlottesville, presented these results at the 2016 ASH Annual Meeting (abstract 218).
Dr Lee noted that CAR T cells have shown promise in early studies, but morbidity related to high-grade CRS and/or neurotoxicity could limit wide applicability of this treatment in patients with high disease burden. Among those who achieve CR to CD19 CAR T-cell therapy, nearly half of patients relapse in the first year.
At ASH, Dr Lee reported results of a non-randomized clinical trial of KTE-C19, a CD19 CAR T-cell therapy under development by Kite Pharmaceuticals. The company did not sponsor this study, although investigators reported relationships with Kite and other companies. The trial was sponsored by the National Cancer Institute.
The trial included 53 children and young adults with relapsed/refractory ALL (n=51) or diffuse large B-cell lymphoma (n=2). The patients’ median age was 13 (range, 4-30), and most were male (n=41).
Of the ALL patients, 11 had primary refractory disease, 5 had Ph-positive ALL, 3 had Down syndrome, 6 had central nervous system (CNS) disease (2 with CNS3, 4 with CNS2), and 2 had MLL-rearranged ALL. The median ALL disease burden was 27%.
The first 21 patients received a low-dose fludarabine/cyclophosphamide preparative regimen, and the subsequent 32 patients received an alternative intensified preparative regimen in an attempt to mitigate severe CRS risk and improve response.
Possible intensive preparative regimens included higher-dose fludarabine/cyclophosphamide, fludarabine/high-dose cytarabine/G-CSF, and ifosfamide/etoposide.
All 53 patients had peripheral blood cells collected, and 52 were infused with CAR T cells. One patient did not receive an infusion due to progressive fungal pneumonia, and 2 patients received less than their assigned dose.
Therefore, Dr Lee said KTE-C19 was feasible in 94% of patients.
Efficacy
The median follow-up was 18.7 months.
Dr Lee said KTE-C19 “produced robust responses in very high-risk ALL patients.” He noted, however, that the CR rate was lower among patients with high disease burden.
The CR rate among the ALL patients was 62%. Of the 31 patients who achieved a CR, 28 had a minimal residual disease (MRD)-negative remission.
The rate of MRD-negative CR was 100% among the 11 patients with primary refractory ALL, 100% among the 6 patients with CNS disease, 60% among the 5 patients with Ph+ ALL, and 67% among the 3 with Down syndrome. Neither of the 2 patients with MLL-rearranged ALL responded.
“Attempts to increase response rate by modifying the preparative regimen have not yet been successful,” Dr Lee pointed out.
However, he noted superior response and overall survival rates among patients who received a fludarabine/cyclophosphamide preparative regimen.
“Median overall survival in all enrolled patients is 13.3 months with fludarabine/cyclophosphamide prep versus 5.5 months with other regimens,” he said.
The overall survival rate for the ALL patients was 28%, and the median overall survival was 11.2 months.
For patients who achieved an MRD-negative remission, the leukemia-free survival (LFS) rate was 56%. The median LFS was not reached.
Dr Lee noted that hematopoietic stem cell transplant (HSCT) after KTE-C19 correlated with decreased relapse rates and led to superior LFS.
Of the 28 patients who achieved MRD-negative CR, 21 went on to HSCT after KTE-C19. The median time to HSCT after CAR T-cell dose was 54 days. (Ten of the 28 patients had HSCT before receiving KTE-C19.)
Nineteen (91%) of the patients who proceeded to HSCT after KTE-C19 did not relapse, compared to 1 (14%) of the patients who did not have a post-CAR T transplant.
The median LFS was 4.9 months among the MRD responders who did not proceed to HSCT and undefined among MRD responders with a transplant after KTE-C19.
The probability of survival was 65% beginning at 18 months among patients who underwent HSCT and 14% beginning at 9.8 months among patients without a post-KTE-C19 transplant.
CD19 escape remains a challenge, Dr Lee said. The risk may be diminished, but not eradicated, with HSCT.
Toxicity
“There was a low rate of CRS, which was successfully managed with a grade-driven algorithm,” Dr Lee noted.
Five patients (10%) had grade 3 CRS, and 2 (4%) had grade 4 CRS.
Other grade 3/4 adverse events that were considered at least possibly related to therapy included fever (38% grade 3), febrile neutropenia (23% grade
3), hypotension (9% grade 3, 4% grade 4), LV systolic dysfunction (9% grade 3), prolonged QTc (2% grade 3), dysphasia (2% grade 3), cardiac arrest (2% grade 4), multi-organ failure (2% grade 3), hypoxia (2% grade 3, 2% grade 4), and pulmonary embolism (2% grade 3).
“There were no severe or permanent neurologic toxicities,” Dr Lee said. “Intensive neuropsychological testing in 13 patients revealed no consistent treatment-related neurocognitive decline, and several patients improved following therapy.”
In all, there were 46 cases of neurotoxicity, including visual hallucination (8 grade 1, 17%), headache (1 grade 3 [2%], 3 grade 2 [6%]), confusion (2 grade 1, 4%),
dysphasia (1 grade 3, 2%), delirium (1 grade 3, 2%), seizure (1 grade 2, 1 grade 1 [2% each]), ataxia (1 grade 2, 2%), tremor (1 grade 2, 2%), dysesthesia (1 grade 2, 2%), and dysarthria (1 grade 1, 2%).