User login
Late Oral Complications After Head/Neck Radiation 'Underreported'
PHOENIX – Late oral effects of head and neck cancer therapy are "multiple, underreported, and underappreciated."
That is the perspective of Joel Epstein, D.M.D., who has worked extensively with head and neck cancer patients experiencing severe dental and other oral problems following radiation therapy.
"The acute complications of head and neck cancer therapy are pretty well known, but the late complications are underappreciated," Dr. Epstein, director of oral medicine at City of Hope National Medical Center, Duarte, Calif., told attendees at the symposium.
As head and neck cancer treatments have advanced and patients are living longer, the spectrum of treatment complications has shifted, he explained. In a 5-year, prospective longitudinal study of 122 patients with oral carcinoma, dry mouth, sticky saliva, speech changes, dental problems, and sleep disturbance were reported by all patients except those treated only with surgery. These complications persisted at 1 and 5 years and affected quality of life (Head Neck 2008;30:461-70).
According to Dr. Epstein, the data illustrate the need for better collaboration between oncologists and dentists. "While people discuss the concept of multidisciplinary [and] interdisciplinary teams for the benefit of our patients, it is unfortunate that dentistry developed separately from physicians and surgeons. So while we need to interact, we’re not really well prepared to do so, particularly in the community," he said.
Clinically, it’s important to evaluate oral care, including brushing, flossing, fluoride, and tobacco abstinence, at all head and neck cancer treatment follow-up visits. Patients should be assessed for xerostomia, speech, swallowing, mucosal sensitivity, and taste. Head and neck and oral exams should include assessments for saliva (wet mucosa), exposed bone, infection, and new lesions or recurrent cancer, and a dental exam (for plaque, caries, and periodontal health), Dr. Epstein recommended.
Dry mouth, in particular, can lead to a host of other chronic problems related to swallowing, eating, sleeping, and dental health. When the 50-item Vanderbilt Head and Neck Symptom Survey was administered to a total of 70 patients, 67 reported having dry mouth at more than 6 months’ follow up (Head Neck 2011 Aug. 24 [doi:10.1002/hed.21816]).
The majority reported that dry mouth makes chewing/swallowing difficult (65) and that it affects their ability to sleep (67) and talk (64). With regard to eating and swallowing, similar majorities reported trouble eating solids (67) and drinking liquids (68), with food getting stuck in their mouth (66) and throat (67).
And, of concern, the same numbers of patients reported the sensation of choking or strangling on solids (66) and liquids (68). "The impact on function from the lack of saliva and the change in quality of saliva are issues we need to be more ready and willing to address," Dr. Epstein commented.
Taste and smell may also be profoundly altered. In the Vanderbilt survey, most patients reported altered taste (68), a decreased desire to eat (68), altered food choices (66), and a decrease in food eaten (66). A change in sense of smell was reported by 69 patients.
Such alterations often result in changes in diet, including decreased consumption of high-fiber food and of vitamins and other nutrients, along with increased consumption of fats, caffeine, and sugar. All of these factors increase the risk for dietary deficiencies, as well as dental caries.
Yet, altered taste sensation is not something patients might think to mention. "Half of patients experience altered taste sensation. But if they think you’re not interested or you don’t ask, you may not know," Dr. Epstein commented.
Periodontal health is often compromised by hyposalivation, which can lead to inflammation, bone/attachment loss, oral infection, and necrosis. Dental demineralization and cavitation may develop as early as 2-3 months after cancer treatment and progress rapidly, leading to fractures of the gum line, tooth loss, and necrosis.
Demineralization appears as a change to white, which may not be recognized as a problem because of the belief that white teeth are healthy. However, recognition at this stage is critical in order to prevent further dental damage, he said.
"The white change near the gum line and the tips of the teeth represent demineralization, and [in] time reversal can be accomplished prior to structural breakdown. Once cavitation has occurred, fillings are needed and prevention must be instituted or the cavities will recur and progress," Dr. Epstein said in an interview.
In the Vanderbilt survey, reported dental problems included difficulty chewing because of teeth/dentures (54 of the 70 patients); tooth sensitivity to hot, cold, or sweet foods (52); teeth feeling looser (51); teeth cracking/chipping (50); and trouble with dentures (24).
Oral candidiasis is another common problem, affecting approximately 39% of head and neck cancer patients during treatment and 33% afterward. One common clinical mistake is prescribing these patients antifungals that contain sugar, such as nystatin. "Nystatin is very high in sugar, and one of the [most commonly] used antifungals. The message is to avoid sugar-sweetened products in dry mouth patients and utilize alternatives," Dr. Epstein said in the interview.
Mucosal sensitivity and pain is also frequent. In a meta-analysis of 22 studies published between 1990 and 2008, the prevalence of trismus was 25.4% in patients who received conventional radiotherapy and 5% for the few intensity-modulated radiation therapy studies that were included, suggesting that the newer radiation modality might diminish the problem (Support. Care Cancer 2010;18:1033-8).
Data suggest that the radiation effect on mandibular movement correlates with the radiation dose to the mastication muscles, with a steep dose-response curve. Onset is typically 2-6 months post treatment and is ongoing. Concurrent chemotherapy may increase the incidence and/or severity of mandibular immobility (Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999;88:365-73).
In the Vanderbilt survey, most patients reported burning in the throat or mouth (69); sensitivity to hot, spicy, or acid food (67); sensitivity to dryness (69); and changes in food intake because of mucosal sensitivity (67); most patients also reported that mucosal sensitivity prevents tooth brushing (63). "Mucosal sensitivity is a quality of life issue," Dr. Epstein said.
The Vanderbilt survey was particularly illuminating, Dr. Epstein commented. Studies that utilize claims data probably underrepresent the problem of long-term oral complications because dental and medical insurance are separate and the data are not easily combined, he added.
"Late oral effects are best diagnosed [and] managed in a multidisciplinary team with close communication between medical and dental providers. ... We really need to come together."
The Multinational Association of Supportive Care in Cancer is developing tools to improve communication between dentistry and medicine. These could be available for beta testing as early as this fall.
Dr. Epstein said he had no relevant financial disclosures.
PHOENIX – Late oral effects of head and neck cancer therapy are "multiple, underreported, and underappreciated."
That is the perspective of Joel Epstein, D.M.D., who has worked extensively with head and neck cancer patients experiencing severe dental and other oral problems following radiation therapy.
"The acute complications of head and neck cancer therapy are pretty well known, but the late complications are underappreciated," Dr. Epstein, director of oral medicine at City of Hope National Medical Center, Duarte, Calif., told attendees at the symposium.
As head and neck cancer treatments have advanced and patients are living longer, the spectrum of treatment complications has shifted, he explained. In a 5-year, prospective longitudinal study of 122 patients with oral carcinoma, dry mouth, sticky saliva, speech changes, dental problems, and sleep disturbance were reported by all patients except those treated only with surgery. These complications persisted at 1 and 5 years and affected quality of life (Head Neck 2008;30:461-70).
According to Dr. Epstein, the data illustrate the need for better collaboration between oncologists and dentists. "While people discuss the concept of multidisciplinary [and] interdisciplinary teams for the benefit of our patients, it is unfortunate that dentistry developed separately from physicians and surgeons. So while we need to interact, we’re not really well prepared to do so, particularly in the community," he said.
Clinically, it’s important to evaluate oral care, including brushing, flossing, fluoride, and tobacco abstinence, at all head and neck cancer treatment follow-up visits. Patients should be assessed for xerostomia, speech, swallowing, mucosal sensitivity, and taste. Head and neck and oral exams should include assessments for saliva (wet mucosa), exposed bone, infection, and new lesions or recurrent cancer, and a dental exam (for plaque, caries, and periodontal health), Dr. Epstein recommended.
Dry mouth, in particular, can lead to a host of other chronic problems related to swallowing, eating, sleeping, and dental health. When the 50-item Vanderbilt Head and Neck Symptom Survey was administered to a total of 70 patients, 67 reported having dry mouth at more than 6 months’ follow up (Head Neck 2011 Aug. 24 [doi:10.1002/hed.21816]).
The majority reported that dry mouth makes chewing/swallowing difficult (65) and that it affects their ability to sleep (67) and talk (64). With regard to eating and swallowing, similar majorities reported trouble eating solids (67) and drinking liquids (68), with food getting stuck in their mouth (66) and throat (67).
And, of concern, the same numbers of patients reported the sensation of choking or strangling on solids (66) and liquids (68). "The impact on function from the lack of saliva and the change in quality of saliva are issues we need to be more ready and willing to address," Dr. Epstein commented.
Taste and smell may also be profoundly altered. In the Vanderbilt survey, most patients reported altered taste (68), a decreased desire to eat (68), altered food choices (66), and a decrease in food eaten (66). A change in sense of smell was reported by 69 patients.
Such alterations often result in changes in diet, including decreased consumption of high-fiber food and of vitamins and other nutrients, along with increased consumption of fats, caffeine, and sugar. All of these factors increase the risk for dietary deficiencies, as well as dental caries.
Yet, altered taste sensation is not something patients might think to mention. "Half of patients experience altered taste sensation. But if they think you’re not interested or you don’t ask, you may not know," Dr. Epstein commented.
Periodontal health is often compromised by hyposalivation, which can lead to inflammation, bone/attachment loss, oral infection, and necrosis. Dental demineralization and cavitation may develop as early as 2-3 months after cancer treatment and progress rapidly, leading to fractures of the gum line, tooth loss, and necrosis.
Demineralization appears as a change to white, which may not be recognized as a problem because of the belief that white teeth are healthy. However, recognition at this stage is critical in order to prevent further dental damage, he said.
"The white change near the gum line and the tips of the teeth represent demineralization, and [in] time reversal can be accomplished prior to structural breakdown. Once cavitation has occurred, fillings are needed and prevention must be instituted or the cavities will recur and progress," Dr. Epstein said in an interview.
In the Vanderbilt survey, reported dental problems included difficulty chewing because of teeth/dentures (54 of the 70 patients); tooth sensitivity to hot, cold, or sweet foods (52); teeth feeling looser (51); teeth cracking/chipping (50); and trouble with dentures (24).
Oral candidiasis is another common problem, affecting approximately 39% of head and neck cancer patients during treatment and 33% afterward. One common clinical mistake is prescribing these patients antifungals that contain sugar, such as nystatin. "Nystatin is very high in sugar, and one of the [most commonly] used antifungals. The message is to avoid sugar-sweetened products in dry mouth patients and utilize alternatives," Dr. Epstein said in the interview.
Mucosal sensitivity and pain is also frequent. In a meta-analysis of 22 studies published between 1990 and 2008, the prevalence of trismus was 25.4% in patients who received conventional radiotherapy and 5% for the few intensity-modulated radiation therapy studies that were included, suggesting that the newer radiation modality might diminish the problem (Support. Care Cancer 2010;18:1033-8).
Data suggest that the radiation effect on mandibular movement correlates with the radiation dose to the mastication muscles, with a steep dose-response curve. Onset is typically 2-6 months post treatment and is ongoing. Concurrent chemotherapy may increase the incidence and/or severity of mandibular immobility (Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999;88:365-73).
In the Vanderbilt survey, most patients reported burning in the throat or mouth (69); sensitivity to hot, spicy, or acid food (67); sensitivity to dryness (69); and changes in food intake because of mucosal sensitivity (67); most patients also reported that mucosal sensitivity prevents tooth brushing (63). "Mucosal sensitivity is a quality of life issue," Dr. Epstein said.
The Vanderbilt survey was particularly illuminating, Dr. Epstein commented. Studies that utilize claims data probably underrepresent the problem of long-term oral complications because dental and medical insurance are separate and the data are not easily combined, he added.
"Late oral effects are best diagnosed [and] managed in a multidisciplinary team with close communication between medical and dental providers. ... We really need to come together."
The Multinational Association of Supportive Care in Cancer is developing tools to improve communication between dentistry and medicine. These could be available for beta testing as early as this fall.
Dr. Epstein said he had no relevant financial disclosures.
PHOENIX – Late oral effects of head and neck cancer therapy are "multiple, underreported, and underappreciated."
That is the perspective of Joel Epstein, D.M.D., who has worked extensively with head and neck cancer patients experiencing severe dental and other oral problems following radiation therapy.
"The acute complications of head and neck cancer therapy are pretty well known, but the late complications are underappreciated," Dr. Epstein, director of oral medicine at City of Hope National Medical Center, Duarte, Calif., told attendees at the symposium.
As head and neck cancer treatments have advanced and patients are living longer, the spectrum of treatment complications has shifted, he explained. In a 5-year, prospective longitudinal study of 122 patients with oral carcinoma, dry mouth, sticky saliva, speech changes, dental problems, and sleep disturbance were reported by all patients except those treated only with surgery. These complications persisted at 1 and 5 years and affected quality of life (Head Neck 2008;30:461-70).
According to Dr. Epstein, the data illustrate the need for better collaboration between oncologists and dentists. "While people discuss the concept of multidisciplinary [and] interdisciplinary teams for the benefit of our patients, it is unfortunate that dentistry developed separately from physicians and surgeons. So while we need to interact, we’re not really well prepared to do so, particularly in the community," he said.
Clinically, it’s important to evaluate oral care, including brushing, flossing, fluoride, and tobacco abstinence, at all head and neck cancer treatment follow-up visits. Patients should be assessed for xerostomia, speech, swallowing, mucosal sensitivity, and taste. Head and neck and oral exams should include assessments for saliva (wet mucosa), exposed bone, infection, and new lesions or recurrent cancer, and a dental exam (for plaque, caries, and periodontal health), Dr. Epstein recommended.
Dry mouth, in particular, can lead to a host of other chronic problems related to swallowing, eating, sleeping, and dental health. When the 50-item Vanderbilt Head and Neck Symptom Survey was administered to a total of 70 patients, 67 reported having dry mouth at more than 6 months’ follow up (Head Neck 2011 Aug. 24 [doi:10.1002/hed.21816]).
The majority reported that dry mouth makes chewing/swallowing difficult (65) and that it affects their ability to sleep (67) and talk (64). With regard to eating and swallowing, similar majorities reported trouble eating solids (67) and drinking liquids (68), with food getting stuck in their mouth (66) and throat (67).
And, of concern, the same numbers of patients reported the sensation of choking or strangling on solids (66) and liquids (68). "The impact on function from the lack of saliva and the change in quality of saliva are issues we need to be more ready and willing to address," Dr. Epstein commented.
Taste and smell may also be profoundly altered. In the Vanderbilt survey, most patients reported altered taste (68), a decreased desire to eat (68), altered food choices (66), and a decrease in food eaten (66). A change in sense of smell was reported by 69 patients.
Such alterations often result in changes in diet, including decreased consumption of high-fiber food and of vitamins and other nutrients, along with increased consumption of fats, caffeine, and sugar. All of these factors increase the risk for dietary deficiencies, as well as dental caries.
Yet, altered taste sensation is not something patients might think to mention. "Half of patients experience altered taste sensation. But if they think you’re not interested or you don’t ask, you may not know," Dr. Epstein commented.
Periodontal health is often compromised by hyposalivation, which can lead to inflammation, bone/attachment loss, oral infection, and necrosis. Dental demineralization and cavitation may develop as early as 2-3 months after cancer treatment and progress rapidly, leading to fractures of the gum line, tooth loss, and necrosis.
Demineralization appears as a change to white, which may not be recognized as a problem because of the belief that white teeth are healthy. However, recognition at this stage is critical in order to prevent further dental damage, he said.
"The white change near the gum line and the tips of the teeth represent demineralization, and [in] time reversal can be accomplished prior to structural breakdown. Once cavitation has occurred, fillings are needed and prevention must be instituted or the cavities will recur and progress," Dr. Epstein said in an interview.
In the Vanderbilt survey, reported dental problems included difficulty chewing because of teeth/dentures (54 of the 70 patients); tooth sensitivity to hot, cold, or sweet foods (52); teeth feeling looser (51); teeth cracking/chipping (50); and trouble with dentures (24).
Oral candidiasis is another common problem, affecting approximately 39% of head and neck cancer patients during treatment and 33% afterward. One common clinical mistake is prescribing these patients antifungals that contain sugar, such as nystatin. "Nystatin is very high in sugar, and one of the [most commonly] used antifungals. The message is to avoid sugar-sweetened products in dry mouth patients and utilize alternatives," Dr. Epstein said in the interview.
Mucosal sensitivity and pain is also frequent. In a meta-analysis of 22 studies published between 1990 and 2008, the prevalence of trismus was 25.4% in patients who received conventional radiotherapy and 5% for the few intensity-modulated radiation therapy studies that were included, suggesting that the newer radiation modality might diminish the problem (Support. Care Cancer 2010;18:1033-8).
Data suggest that the radiation effect on mandibular movement correlates with the radiation dose to the mastication muscles, with a steep dose-response curve. Onset is typically 2-6 months post treatment and is ongoing. Concurrent chemotherapy may increase the incidence and/or severity of mandibular immobility (Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999;88:365-73).
In the Vanderbilt survey, most patients reported burning in the throat or mouth (69); sensitivity to hot, spicy, or acid food (67); sensitivity to dryness (69); and changes in food intake because of mucosal sensitivity (67); most patients also reported that mucosal sensitivity prevents tooth brushing (63). "Mucosal sensitivity is a quality of life issue," Dr. Epstein said.
The Vanderbilt survey was particularly illuminating, Dr. Epstein commented. Studies that utilize claims data probably underrepresent the problem of long-term oral complications because dental and medical insurance are separate and the data are not easily combined, he added.
"Late oral effects are best diagnosed [and] managed in a multidisciplinary team with close communication between medical and dental providers. ... We really need to come together."
The Multinational Association of Supportive Care in Cancer is developing tools to improve communication between dentistry and medicine. These could be available for beta testing as early as this fall.
Dr. Epstein said he had no relevant financial disclosures.
EXPERT OPINION FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
CD4 Counts Predict Chemo Response in Laryngeal Cancer
PHOENIX – Pretreatment CD4 levels predicted response to induction chemotherapy among 97 patients with advanced laryngeal cancer, but not for 66 patients with advanced oropharyngeal cancer, according to a retrospective analysis of data from two clinical trials.
The two groups of head and neck cancer patients were enrolled in two identical prospective, phase II trials of induction chemotherapy and organ preservation, in which tumor response after one cycle of cisplatin and 5-fluorouracil was used to select those who would undergo surgery or definitive chemoradiation (J. Clin. Oncol. 2006;24:593-8 in laryngeal cancer; J. Clin. Oncol. 2008;26:3138-46 in oropharyngeal cancer).
Several lymphocyte subsets were measured before treatment via routine flow cytometry in peripheral blood in the laryngeal cancer patients, but only CD4 (helper cell) levels were significantly associated with chemotherapy response. Both absolute CD4 counts and CD4 percentages were higher among induction chemotherapy responders than nonresponders (P = .006 and P = .04, respectively).
Investigators also saw a trend for responders to have an increased percentage of CD3 cells (P = .13), decreased percentage of CD8 cells (P = .11), and higher CD4/CD8 ratios.
"Host immune parameters are important factors in treatment outcome, and may be useful in identifying subsets of patients with cancers that are responsive to organ-preserving therapy," said Dr. Gregory T. Wolf, who presented the data at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
"It is likely that immunobiology of head and neck cancers differ significantly by tumor site and predisposing factors," added Dr. Wolf, a professor in the department of otolaryngology at the University of Michigan, Ann Arbor.
The median length of follow-up in the two studies was 7.9 years for the patients with laryngeal cancer and 6.6 years for those with cancer of the oropharynx. Disease-free survival was 86% at 3 years and 82% at 5 years for laryngeal cancer, and 78% at 3 years and 76% at 4 years for oropharyngeal cancer. The proportions responding to induction chemotherapy were 75% in the laryngeal cancer trial and 82% in the oropharyngeal cancer study.
In an interview, Dr. Wolf said that having two identical treatment trials provided an opportunity to determine whether correlations of pretreatment CD4 levels with chemoresponse differed by tumor site. When the laryngeal and oropharyngeal cancer patient groups were combined, higher CD4 levels were still associated with response, but this was primarily because of the strong correlation among the larynx cancer patients.
Statistical regression testing determined that for patients with oropharyngeal cancer, CD8 cells were more closely associated with chemotherapy response, but the relationship was not as strong as the strong correlation of CD4 levels among laryngeal cancer patients.
There was a trend toward improved survival by both CD4 percentage (P = .36) and absolute CD4 count (P = .15) in the laryngeal cohort, but not in the oropharyngeal cohort. None of the other lymphocyte subsets predicted survival in either group, Dr. Wolf said.
Results for the oropharyngeal cancer patients were further stratified by human papillomavirus status, and were combined with the laryngeal cancer group. Both lower CD4/CD8 ratio and higher CD8 levels were consistent with better prognosis among patients who were HPV positive (P = .02 and P = .06, respectively).
"We combined the results to get the largest sample size and [to see] if the relationship was independent of tumor site, since the biology of these cancers is so different. It was remarkable that the prediction differed by tumor site, with CD4 cells being predictive for larynx and CD8 cells predictive for oropharynx," Dr. Wolf explained in an interview. This finding likely reflects the major biological differences between these cancers, and is why it was important to also include HPV status, he added.
Dr. Wolf is a consultant for IRX Therapeutics, Inc.
PHOENIX – Pretreatment CD4 levels predicted response to induction chemotherapy among 97 patients with advanced laryngeal cancer, but not for 66 patients with advanced oropharyngeal cancer, according to a retrospective analysis of data from two clinical trials.
The two groups of head and neck cancer patients were enrolled in two identical prospective, phase II trials of induction chemotherapy and organ preservation, in which tumor response after one cycle of cisplatin and 5-fluorouracil was used to select those who would undergo surgery or definitive chemoradiation (J. Clin. Oncol. 2006;24:593-8 in laryngeal cancer; J. Clin. Oncol. 2008;26:3138-46 in oropharyngeal cancer).
Several lymphocyte subsets were measured before treatment via routine flow cytometry in peripheral blood in the laryngeal cancer patients, but only CD4 (helper cell) levels were significantly associated with chemotherapy response. Both absolute CD4 counts and CD4 percentages were higher among induction chemotherapy responders than nonresponders (P = .006 and P = .04, respectively).
Investigators also saw a trend for responders to have an increased percentage of CD3 cells (P = .13), decreased percentage of CD8 cells (P = .11), and higher CD4/CD8 ratios.
"Host immune parameters are important factors in treatment outcome, and may be useful in identifying subsets of patients with cancers that are responsive to organ-preserving therapy," said Dr. Gregory T. Wolf, who presented the data at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
"It is likely that immunobiology of head and neck cancers differ significantly by tumor site and predisposing factors," added Dr. Wolf, a professor in the department of otolaryngology at the University of Michigan, Ann Arbor.
The median length of follow-up in the two studies was 7.9 years for the patients with laryngeal cancer and 6.6 years for those with cancer of the oropharynx. Disease-free survival was 86% at 3 years and 82% at 5 years for laryngeal cancer, and 78% at 3 years and 76% at 4 years for oropharyngeal cancer. The proportions responding to induction chemotherapy were 75% in the laryngeal cancer trial and 82% in the oropharyngeal cancer study.
In an interview, Dr. Wolf said that having two identical treatment trials provided an opportunity to determine whether correlations of pretreatment CD4 levels with chemoresponse differed by tumor site. When the laryngeal and oropharyngeal cancer patient groups were combined, higher CD4 levels were still associated with response, but this was primarily because of the strong correlation among the larynx cancer patients.
Statistical regression testing determined that for patients with oropharyngeal cancer, CD8 cells were more closely associated with chemotherapy response, but the relationship was not as strong as the strong correlation of CD4 levels among laryngeal cancer patients.
There was a trend toward improved survival by both CD4 percentage (P = .36) and absolute CD4 count (P = .15) in the laryngeal cohort, but not in the oropharyngeal cohort. None of the other lymphocyte subsets predicted survival in either group, Dr. Wolf said.
Results for the oropharyngeal cancer patients were further stratified by human papillomavirus status, and were combined with the laryngeal cancer group. Both lower CD4/CD8 ratio and higher CD8 levels were consistent with better prognosis among patients who were HPV positive (P = .02 and P = .06, respectively).
"We combined the results to get the largest sample size and [to see] if the relationship was independent of tumor site, since the biology of these cancers is so different. It was remarkable that the prediction differed by tumor site, with CD4 cells being predictive for larynx and CD8 cells predictive for oropharynx," Dr. Wolf explained in an interview. This finding likely reflects the major biological differences between these cancers, and is why it was important to also include HPV status, he added.
Dr. Wolf is a consultant for IRX Therapeutics, Inc.
PHOENIX – Pretreatment CD4 levels predicted response to induction chemotherapy among 97 patients with advanced laryngeal cancer, but not for 66 patients with advanced oropharyngeal cancer, according to a retrospective analysis of data from two clinical trials.
The two groups of head and neck cancer patients were enrolled in two identical prospective, phase II trials of induction chemotherapy and organ preservation, in which tumor response after one cycle of cisplatin and 5-fluorouracil was used to select those who would undergo surgery or definitive chemoradiation (J. Clin. Oncol. 2006;24:593-8 in laryngeal cancer; J. Clin. Oncol. 2008;26:3138-46 in oropharyngeal cancer).
Several lymphocyte subsets were measured before treatment via routine flow cytometry in peripheral blood in the laryngeal cancer patients, but only CD4 (helper cell) levels were significantly associated with chemotherapy response. Both absolute CD4 counts and CD4 percentages were higher among induction chemotherapy responders than nonresponders (P = .006 and P = .04, respectively).
Investigators also saw a trend for responders to have an increased percentage of CD3 cells (P = .13), decreased percentage of CD8 cells (P = .11), and higher CD4/CD8 ratios.
"Host immune parameters are important factors in treatment outcome, and may be useful in identifying subsets of patients with cancers that are responsive to organ-preserving therapy," said Dr. Gregory T. Wolf, who presented the data at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
"It is likely that immunobiology of head and neck cancers differ significantly by tumor site and predisposing factors," added Dr. Wolf, a professor in the department of otolaryngology at the University of Michigan, Ann Arbor.
The median length of follow-up in the two studies was 7.9 years for the patients with laryngeal cancer and 6.6 years for those with cancer of the oropharynx. Disease-free survival was 86% at 3 years and 82% at 5 years for laryngeal cancer, and 78% at 3 years and 76% at 4 years for oropharyngeal cancer. The proportions responding to induction chemotherapy were 75% in the laryngeal cancer trial and 82% in the oropharyngeal cancer study.
In an interview, Dr. Wolf said that having two identical treatment trials provided an opportunity to determine whether correlations of pretreatment CD4 levels with chemoresponse differed by tumor site. When the laryngeal and oropharyngeal cancer patient groups were combined, higher CD4 levels were still associated with response, but this was primarily because of the strong correlation among the larynx cancer patients.
Statistical regression testing determined that for patients with oropharyngeal cancer, CD8 cells were more closely associated with chemotherapy response, but the relationship was not as strong as the strong correlation of CD4 levels among laryngeal cancer patients.
There was a trend toward improved survival by both CD4 percentage (P = .36) and absolute CD4 count (P = .15) in the laryngeal cohort, but not in the oropharyngeal cohort. None of the other lymphocyte subsets predicted survival in either group, Dr. Wolf said.
Results for the oropharyngeal cancer patients were further stratified by human papillomavirus status, and were combined with the laryngeal cancer group. Both lower CD4/CD8 ratio and higher CD8 levels were consistent with better prognosis among patients who were HPV positive (P = .02 and P = .06, respectively).
"We combined the results to get the largest sample size and [to see] if the relationship was independent of tumor site, since the biology of these cancers is so different. It was remarkable that the prediction differed by tumor site, with CD4 cells being predictive for larynx and CD8 cells predictive for oropharynx," Dr. Wolf explained in an interview. This finding likely reflects the major biological differences between these cancers, and is why it was important to also include HPV status, he added.
Dr. Wolf is a consultant for IRX Therapeutics, Inc.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: Among laryngeal cancer patients, both absolute and percent CD4 counts were significantly higher among responders to induction chemotherapy than in nonresponders (P = .006 and P = .04, respectively).
Data Source: The data come from a retrospective analysis of head and neck cancer patients who were enrolled in two identical prospective, phase II trials of induction chemotherapy and organ preservation.
Disclosures: Dr. Wolf is a consultant for IRX Therapeutics.
Infrared Imaging Eyes Mucositis After Head & Neck Radiation
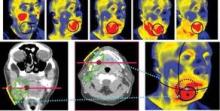
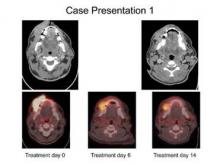
PHOENIX – Thermal imaging was able to detect small and early changes in the temperature of mucosal surfaces – a possible predictor of the development of mucositis – among 34 patients who were treated with chemoradiotherapy for locally advanced squamous cell carcinoma of the head and neck.
"Detection of these early changes using sensitive thermal imaging technology would allow identification of patients who will require more intensive supportive care," said Dr. Ezra Cohen, who presented the pilot study at the head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
Radiotherapy-associated mucositis manifests initially as erythematous areas in the treatment field, which are accompanied by an intense inflammatory response histologically. Thus, Dr. Cohen and his associates had hypothesized that patients destined to display severe mucocutaneous toxicity would demonstrate greater alterations in thermal intensity early in therapy, compared with identically treated counterparts who do not subsequently develop the toxicity.
The researchers further hypothesized that they could measure those changes with infrared thermal imaging, a noninvasive technique that allows visualization and quantification of changes in skin or mucosal surface temperature.
The 34 patients (28 male, mean age 58 years) in the pilot study were treated with identical chemoradiotherapy regimens of 5-fluorouracil and hydroxyurea with a median radiation dose of 74 Gy for cancers of the oral cavity or oropharynx.
Using a portable device developed at Argonne National Laboratory in Illinois, the investigators conducted noninvasive baseline and weekly thermal imaging. The device detects infrared light naturally emitted from the skin or mucosal surface and generates an electrical signal, which is amplified and converted into digital data flow that is visualized in color on a monitor.
Grade 3 mucositis based on the National Cancer Institute’s Common Terminology Criteria for Adverse Events v3.0 was observed in 53% of the patients, and dermatitis in 21%. All patients displayed an increase in temperature within the radiation field.
Investigators charted a statistically significant positive association between an early rise in temperature in oral mucous membranes when compared with a reference area and mucositis grade (P = .03). For every 1 C increase in temperature, compared with the reference (temperature near the medial angle of one eye), there was a 0.157 increase in average subsequent mucositis grade, reported Dr. Cohen, codirector of the head and neck cancer program at the University of Chicago.
Mucositis and its clinical sequelae are consistently reported as the most clinically significant acute toxicity in the treatment of locally advanced squamous cell carcinoma of the head and neck with chemoradiotherapy, according to Dr. Cohen, who also chaired the meeting. Patient to patient variability in mucositis is related to radiotherapy dosing, fractionation, and volumes, but there also appear to be individual differences in "normal tissue tolerance," even among patients on the same treatment regimen, he said.
"Larger studies with greater dynamic ranges in mucositis scoring are warranted to evaluate whether this tool can help predict which patients would be in need of early intervention to prevent acute complications," he said.
The study was funded by the National Institutes of Health and the University of Chicago Comprehensive Cancer Center. Dr. Cohen and his associates said they had no relevant financial disclosures.
PHOENIX – Thermal imaging was able to detect small and early changes in the temperature of mucosal surfaces – a possible predictor of the development of mucositis – among 34 patients who were treated with chemoradiotherapy for locally advanced squamous cell carcinoma of the head and neck.
"Detection of these early changes using sensitive thermal imaging technology would allow identification of patients who will require more intensive supportive care," said Dr. Ezra Cohen, who presented the pilot study at the head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
Radiotherapy-associated mucositis manifests initially as erythematous areas in the treatment field, which are accompanied by an intense inflammatory response histologically. Thus, Dr. Cohen and his associates had hypothesized that patients destined to display severe mucocutaneous toxicity would demonstrate greater alterations in thermal intensity early in therapy, compared with identically treated counterparts who do not subsequently develop the toxicity.
The researchers further hypothesized that they could measure those changes with infrared thermal imaging, a noninvasive technique that allows visualization and quantification of changes in skin or mucosal surface temperature.
The 34 patients (28 male, mean age 58 years) in the pilot study were treated with identical chemoradiotherapy regimens of 5-fluorouracil and hydroxyurea with a median radiation dose of 74 Gy for cancers of the oral cavity or oropharynx.
Using a portable device developed at Argonne National Laboratory in Illinois, the investigators conducted noninvasive baseline and weekly thermal imaging. The device detects infrared light naturally emitted from the skin or mucosal surface and generates an electrical signal, which is amplified and converted into digital data flow that is visualized in color on a monitor.
Grade 3 mucositis based on the National Cancer Institute’s Common Terminology Criteria for Adverse Events v3.0 was observed in 53% of the patients, and dermatitis in 21%. All patients displayed an increase in temperature within the radiation field.
Investigators charted a statistically significant positive association between an early rise in temperature in oral mucous membranes when compared with a reference area and mucositis grade (P = .03). For every 1 C increase in temperature, compared with the reference (temperature near the medial angle of one eye), there was a 0.157 increase in average subsequent mucositis grade, reported Dr. Cohen, codirector of the head and neck cancer program at the University of Chicago.
Mucositis and its clinical sequelae are consistently reported as the most clinically significant acute toxicity in the treatment of locally advanced squamous cell carcinoma of the head and neck with chemoradiotherapy, according to Dr. Cohen, who also chaired the meeting. Patient to patient variability in mucositis is related to radiotherapy dosing, fractionation, and volumes, but there also appear to be individual differences in "normal tissue tolerance," even among patients on the same treatment regimen, he said.
"Larger studies with greater dynamic ranges in mucositis scoring are warranted to evaluate whether this tool can help predict which patients would be in need of early intervention to prevent acute complications," he said.
The study was funded by the National Institutes of Health and the University of Chicago Comprehensive Cancer Center. Dr. Cohen and his associates said they had no relevant financial disclosures.
PHOENIX – Thermal imaging was able to detect small and early changes in the temperature of mucosal surfaces – a possible predictor of the development of mucositis – among 34 patients who were treated with chemoradiotherapy for locally advanced squamous cell carcinoma of the head and neck.
"Detection of these early changes using sensitive thermal imaging technology would allow identification of patients who will require more intensive supportive care," said Dr. Ezra Cohen, who presented the pilot study at the head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
Radiotherapy-associated mucositis manifests initially as erythematous areas in the treatment field, which are accompanied by an intense inflammatory response histologically. Thus, Dr. Cohen and his associates had hypothesized that patients destined to display severe mucocutaneous toxicity would demonstrate greater alterations in thermal intensity early in therapy, compared with identically treated counterparts who do not subsequently develop the toxicity.
The researchers further hypothesized that they could measure those changes with infrared thermal imaging, a noninvasive technique that allows visualization and quantification of changes in skin or mucosal surface temperature.
The 34 patients (28 male, mean age 58 years) in the pilot study were treated with identical chemoradiotherapy regimens of 5-fluorouracil and hydroxyurea with a median radiation dose of 74 Gy for cancers of the oral cavity or oropharynx.
Using a portable device developed at Argonne National Laboratory in Illinois, the investigators conducted noninvasive baseline and weekly thermal imaging. The device detects infrared light naturally emitted from the skin or mucosal surface and generates an electrical signal, which is amplified and converted into digital data flow that is visualized in color on a monitor.
Grade 3 mucositis based on the National Cancer Institute’s Common Terminology Criteria for Adverse Events v3.0 was observed in 53% of the patients, and dermatitis in 21%. All patients displayed an increase in temperature within the radiation field.
Investigators charted a statistically significant positive association between an early rise in temperature in oral mucous membranes when compared with a reference area and mucositis grade (P = .03). For every 1 C increase in temperature, compared with the reference (temperature near the medial angle of one eye), there was a 0.157 increase in average subsequent mucositis grade, reported Dr. Cohen, codirector of the head and neck cancer program at the University of Chicago.
Mucositis and its clinical sequelae are consistently reported as the most clinically significant acute toxicity in the treatment of locally advanced squamous cell carcinoma of the head and neck with chemoradiotherapy, according to Dr. Cohen, who also chaired the meeting. Patient to patient variability in mucositis is related to radiotherapy dosing, fractionation, and volumes, but there also appear to be individual differences in "normal tissue tolerance," even among patients on the same treatment regimen, he said.
"Larger studies with greater dynamic ranges in mucositis scoring are warranted to evaluate whether this tool can help predict which patients would be in need of early intervention to prevent acute complications," he said.
The study was funded by the National Institutes of Health and the University of Chicago Comprehensive Cancer Center. Dr. Cohen and his associates said they had no relevant financial disclosures.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: For every 1 C increase in temperature, compared with the reference (temperature near the medial angle of one eye), there was a 0.157 increase in average subsequent mucositis.
Data Source: Data come from a pilot study of functional infrared imaging in 34 patients with locally advanced head and neck cancer who were treated with chemoradiotherapy.
Disclosures: The study was funded by the National Institutes of Health and the University of Chicago Comprehensive Cancer Center. Dr. Cohen and his associates said they had no relevant financial disclosures.
Jaw Complications Persist With Head & Neck Cancer Treatment
PHOENIX – An analysis of Medicare data for more than 1,800 head and neck cancer patients suggests that jaw complications following radiation treatment may be more common than recognized.
Moreover, intensity-modulated radiation therapy (IMRT) was not associated with significantly lower rates of jaw complications, compared with older radiation techniques, although there was a slight trend in that direction and the interval to developing jaw complications was longer following IMRT, reported Dr. Beth M. Beadle at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
In the literature, osteoradionecrosis (ORN), the most severe jaw manifestation resulting from head/neck radiation, was reported on average in 11.8% of patients in 10 studies (total, 3,312 irradiated patients) from the 1930s through the 1960s, said Dr. Beadle, a radiation oncologist at the University of Texas M.D. Anderson Cancer Center, Houston.
With improved technologies, the rate dropped to 5.4%, as documented in 21 studies involving a total of 11,077 patients conducted from the 1970s through the early 1990s. Since 1997, 25 retrospective and prospective studies involving 9,632 patients overall have reported an overall average ORN rate of 3.0%, she said.
For the current study, data were taken from the SEER (Surveillance, Epidemiology, and End Results) database for Medicare beneficiaries. Patients who were diagnosed with oral cancers in 1999-2007 were identified using SEER, ICD-9, and CPT codes. Primary tumor sites included those of the lip, tongue, floor of mouth, gum, tonsil, oropharynx, and other oral cavity and pharynx.
Of 1,848 patients overall, 16.1% (297) had at least one osteoradionecrosis code within 90 days of radiation therapy completion. Of those, 256 patients had ICD-9 diagnostic codes that included those for osteonecrosis of jaw (733.45), osteomyelitis of jaw (526.4), and other diseases of the jaws, including inflammatory conditions, alveolitis, and periradicular pathology (all 526.x).
Some 41 patients (3.8% of the total) had CPT procedure codes, including drainage of abscess (41800), alveolectomy (41830), operations on facial bones or joints with concurrent ORN diagnosis (76.3), or hyperbaric oxygen therapy (99183), and 30 patients (1.6% of the total) had both a diagnostic and a procedural ORN code, Dr. Beadle said.
The percentage of patients who required intervention for ORN (3.8%) is more consistent with the overall ORN rates from the literature, suggesting that most previous studies have captured only the more severe osteoradionecrosis, which is usually defined as that requiring a procedure, she explained.
In univariate analysis, female sex, not receiving chemotherapy, and a lower number of comorbidities on the Charlson Comorbidity Index were the only factors significantly associated with all jaw complications.
Receipt of IMRT was not a significant predictor, although there was a trend. Patients who received IMRT differed significantly from non-IMRT patients in several ways, however, including their younger age and their greater likelihood to be male, to have advanced-stage disease, to have received definitive vs. adjuvant treatment, to have received chemotherapy, and to have fewer comorbidities.
Although IMRT per se did not predict jaw complications, there was a longer time interval between treatment and the development of jaw complications among the patients who received IMRT (462 days vs. 386 days for the non-IMRT patient).
In response to questions from the audience, Dr. Beadle said that it wasn’t clear why jaw complications would be more common among patients who did not receive chemotherapy, but it might be that those patients received higher doses of radiation. As for the sex difference, she suggested it may be that women have better follow-up care, or it might relate to either osteoporosis or use of bisphosphonates. Her group is investigating those possibilities.
Dr. Beadle stated that she has no disclosures.
PHOENIX – An analysis of Medicare data for more than 1,800 head and neck cancer patients suggests that jaw complications following radiation treatment may be more common than recognized.
Moreover, intensity-modulated radiation therapy (IMRT) was not associated with significantly lower rates of jaw complications, compared with older radiation techniques, although there was a slight trend in that direction and the interval to developing jaw complications was longer following IMRT, reported Dr. Beth M. Beadle at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
In the literature, osteoradionecrosis (ORN), the most severe jaw manifestation resulting from head/neck radiation, was reported on average in 11.8% of patients in 10 studies (total, 3,312 irradiated patients) from the 1930s through the 1960s, said Dr. Beadle, a radiation oncologist at the University of Texas M.D. Anderson Cancer Center, Houston.
With improved technologies, the rate dropped to 5.4%, as documented in 21 studies involving a total of 11,077 patients conducted from the 1970s through the early 1990s. Since 1997, 25 retrospective and prospective studies involving 9,632 patients overall have reported an overall average ORN rate of 3.0%, she said.
For the current study, data were taken from the SEER (Surveillance, Epidemiology, and End Results) database for Medicare beneficiaries. Patients who were diagnosed with oral cancers in 1999-2007 were identified using SEER, ICD-9, and CPT codes. Primary tumor sites included those of the lip, tongue, floor of mouth, gum, tonsil, oropharynx, and other oral cavity and pharynx.
Of 1,848 patients overall, 16.1% (297) had at least one osteoradionecrosis code within 90 days of radiation therapy completion. Of those, 256 patients had ICD-9 diagnostic codes that included those for osteonecrosis of jaw (733.45), osteomyelitis of jaw (526.4), and other diseases of the jaws, including inflammatory conditions, alveolitis, and periradicular pathology (all 526.x).
Some 41 patients (3.8% of the total) had CPT procedure codes, including drainage of abscess (41800), alveolectomy (41830), operations on facial bones or joints with concurrent ORN diagnosis (76.3), or hyperbaric oxygen therapy (99183), and 30 patients (1.6% of the total) had both a diagnostic and a procedural ORN code, Dr. Beadle said.
The percentage of patients who required intervention for ORN (3.8%) is more consistent with the overall ORN rates from the literature, suggesting that most previous studies have captured only the more severe osteoradionecrosis, which is usually defined as that requiring a procedure, she explained.
In univariate analysis, female sex, not receiving chemotherapy, and a lower number of comorbidities on the Charlson Comorbidity Index were the only factors significantly associated with all jaw complications.
Receipt of IMRT was not a significant predictor, although there was a trend. Patients who received IMRT differed significantly from non-IMRT patients in several ways, however, including their younger age and their greater likelihood to be male, to have advanced-stage disease, to have received definitive vs. adjuvant treatment, to have received chemotherapy, and to have fewer comorbidities.
Although IMRT per se did not predict jaw complications, there was a longer time interval between treatment and the development of jaw complications among the patients who received IMRT (462 days vs. 386 days for the non-IMRT patient).
In response to questions from the audience, Dr. Beadle said that it wasn’t clear why jaw complications would be more common among patients who did not receive chemotherapy, but it might be that those patients received higher doses of radiation. As for the sex difference, she suggested it may be that women have better follow-up care, or it might relate to either osteoporosis or use of bisphosphonates. Her group is investigating those possibilities.
Dr. Beadle stated that she has no disclosures.
PHOENIX – An analysis of Medicare data for more than 1,800 head and neck cancer patients suggests that jaw complications following radiation treatment may be more common than recognized.
Moreover, intensity-modulated radiation therapy (IMRT) was not associated with significantly lower rates of jaw complications, compared with older radiation techniques, although there was a slight trend in that direction and the interval to developing jaw complications was longer following IMRT, reported Dr. Beth M. Beadle at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
In the literature, osteoradionecrosis (ORN), the most severe jaw manifestation resulting from head/neck radiation, was reported on average in 11.8% of patients in 10 studies (total, 3,312 irradiated patients) from the 1930s through the 1960s, said Dr. Beadle, a radiation oncologist at the University of Texas M.D. Anderson Cancer Center, Houston.
With improved technologies, the rate dropped to 5.4%, as documented in 21 studies involving a total of 11,077 patients conducted from the 1970s through the early 1990s. Since 1997, 25 retrospective and prospective studies involving 9,632 patients overall have reported an overall average ORN rate of 3.0%, she said.
For the current study, data were taken from the SEER (Surveillance, Epidemiology, and End Results) database for Medicare beneficiaries. Patients who were diagnosed with oral cancers in 1999-2007 were identified using SEER, ICD-9, and CPT codes. Primary tumor sites included those of the lip, tongue, floor of mouth, gum, tonsil, oropharynx, and other oral cavity and pharynx.
Of 1,848 patients overall, 16.1% (297) had at least one osteoradionecrosis code within 90 days of radiation therapy completion. Of those, 256 patients had ICD-9 diagnostic codes that included those for osteonecrosis of jaw (733.45), osteomyelitis of jaw (526.4), and other diseases of the jaws, including inflammatory conditions, alveolitis, and periradicular pathology (all 526.x).
Some 41 patients (3.8% of the total) had CPT procedure codes, including drainage of abscess (41800), alveolectomy (41830), operations on facial bones or joints with concurrent ORN diagnosis (76.3), or hyperbaric oxygen therapy (99183), and 30 patients (1.6% of the total) had both a diagnostic and a procedural ORN code, Dr. Beadle said.
The percentage of patients who required intervention for ORN (3.8%) is more consistent with the overall ORN rates from the literature, suggesting that most previous studies have captured only the more severe osteoradionecrosis, which is usually defined as that requiring a procedure, she explained.
In univariate analysis, female sex, not receiving chemotherapy, and a lower number of comorbidities on the Charlson Comorbidity Index were the only factors significantly associated with all jaw complications.
Receipt of IMRT was not a significant predictor, although there was a trend. Patients who received IMRT differed significantly from non-IMRT patients in several ways, however, including their younger age and their greater likelihood to be male, to have advanced-stage disease, to have received definitive vs. adjuvant treatment, to have received chemotherapy, and to have fewer comorbidities.
Although IMRT per se did not predict jaw complications, there was a longer time interval between treatment and the development of jaw complications among the patients who received IMRT (462 days vs. 386 days for the non-IMRT patient).
In response to questions from the audience, Dr. Beadle said that it wasn’t clear why jaw complications would be more common among patients who did not receive chemotherapy, but it might be that those patients received higher doses of radiation. As for the sex difference, she suggested it may be that women have better follow-up care, or it might relate to either osteoporosis or use of bisphosphonates. Her group is investigating those possibilities.
Dr. Beadle stated that she has no disclosures.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: Of a total 1,848 patients with oral cancers, 16% (297) had at least one osteoradionecrosis code within 90 days of radiation therapy completion.
Data source: Data were taken from the SEER database for Medicare beneficiaries.
Disclosures: Dr. Beadle reported having no financial disclosures.
Toxicity Drives Costly Head and Neck Cancer Readmissions
PHOENIX – Unplanned hospitalizations due to toxicities associated with head and neck cancer treatment were a source of substantial cost in a retrospective chart review of 141 patients treated at a single cancer center during 2007-2011.
Much of the increased cost was among patients who underwent docetaxel plus cisplatin and fluorouracil induction chemotherapy (TPF) plus chemoradiotherapy.
"In recent years, induction chemotherapy has been increasingly incorporated into multimodality regimens for selected patients with locally advanced primary squamous cell carcinoma of the head and neck (HNSCC) ... Although efficacious (N. Engl. J. Med. 2007;357:1705-15), TPF has the potential for toxicities [that] may lead to unplanned admissions during treatment. Concurrent use of chemotherapy with radiation is well documented to intensify therapeutic effect and toxicity," Dr. Regan D. Rostorfer and his associates said in a poster.
Symptoms leading to the unplanned readmissions during induction chemotherapy (27 readmissions, 18 patients) included dehydration (in 13 of the 27 readmissions), infection (8), diarrhea (6), nausea/vomiting (5), pain (4), and mucositis (3).
A range of strategies can be used to avoid readmissions and thereby reduce these costs, including careful patient selection, use of prophylactic antimicrobials, standardized use of growth factor support, post-treatment support with outpatient intravenous fluids, integration of home health care services, early gastrostomy-tube placement, use of long-acting antiemetics during treatment, and frequent outpatient office visits during treatment, Dr. Rostorfer and his associates said.
"A number of initiatives are ongoing at our center in efforts to decrease readmission rates during combined modality treatment. Further studies are planned to assess the impact of these measures on readmission rates, and impact on costs of care," the investigators said in their poster.
In an interview, Dr. Rostorfer said the study was initially intended to simply to gather statistics about readmission for head/neck cancer treatment-related toxicity, since there were no published data on it.
"We decided to look at data from our own institution, simply to see how frequently patients were readmitted, and the reason for readmission. More recently, costs have become an issue at almost every hospital in the country, so we decided to look at the excess costs associated with these unplanned admissions, as well.
The investigators reviewed charts for 91 randomly assigned patients with locally advanced primary HNSCC who received treatment with concurrent chemoradiotherapy, and for another 50 patients who received induction TPF chemotherapy followed by chemoradiation. The oropharynx was the most common cancer site, in 24 of the induction group (48%) and 59 of the concurrent group (65%).
A total of 19 induction patients (38%) required unplanned readmission, with 8 requiring more than one. Median length of stay for those total 27 unplanned stays was 6 days (range 1-25). In the concurrent group, 47 patients required unplanned readmission (52%), with 19 requiring more than one. That group had a total 77 unplanned readmissions, with a median stay of 7.8 days (1-65).
Total costs of admissions in the induction group were $3,368,583 for the planned admissions and $1,777,136 for the unplanned admissions. The median cost per planned hospital stay – elective admission for chemotherapy – was $32,276. In contrast, the cost per unplanned hospital stay was $42,390. For the concurrent group, which did not have planned hospitalizations, the cost per unplanned stay was $69,460, said Dr. Rostorfer, medical oncology and hematology chief fellow at MD Anderson Cancer Center Orlando, and his associates.
"Obviously this was a small, retrospective review, but the numbers can be quite alarming. We have begun to implement measures to reduce the numbers of readmission, so hopefully to reduce the cost associated with care. We will see the difference it makes."
Dr. Rostorfer stated that he has no disclosures.
PHOENIX – Unplanned hospitalizations due to toxicities associated with head and neck cancer treatment were a source of substantial cost in a retrospective chart review of 141 patients treated at a single cancer center during 2007-2011.
Much of the increased cost was among patients who underwent docetaxel plus cisplatin and fluorouracil induction chemotherapy (TPF) plus chemoradiotherapy.
"In recent years, induction chemotherapy has been increasingly incorporated into multimodality regimens for selected patients with locally advanced primary squamous cell carcinoma of the head and neck (HNSCC) ... Although efficacious (N. Engl. J. Med. 2007;357:1705-15), TPF has the potential for toxicities [that] may lead to unplanned admissions during treatment. Concurrent use of chemotherapy with radiation is well documented to intensify therapeutic effect and toxicity," Dr. Regan D. Rostorfer and his associates said in a poster.
Symptoms leading to the unplanned readmissions during induction chemotherapy (27 readmissions, 18 patients) included dehydration (in 13 of the 27 readmissions), infection (8), diarrhea (6), nausea/vomiting (5), pain (4), and mucositis (3).
A range of strategies can be used to avoid readmissions and thereby reduce these costs, including careful patient selection, use of prophylactic antimicrobials, standardized use of growth factor support, post-treatment support with outpatient intravenous fluids, integration of home health care services, early gastrostomy-tube placement, use of long-acting antiemetics during treatment, and frequent outpatient office visits during treatment, Dr. Rostorfer and his associates said.
"A number of initiatives are ongoing at our center in efforts to decrease readmission rates during combined modality treatment. Further studies are planned to assess the impact of these measures on readmission rates, and impact on costs of care," the investigators said in their poster.
In an interview, Dr. Rostorfer said the study was initially intended to simply to gather statistics about readmission for head/neck cancer treatment-related toxicity, since there were no published data on it.
"We decided to look at data from our own institution, simply to see how frequently patients were readmitted, and the reason for readmission. More recently, costs have become an issue at almost every hospital in the country, so we decided to look at the excess costs associated with these unplanned admissions, as well.
The investigators reviewed charts for 91 randomly assigned patients with locally advanced primary HNSCC who received treatment with concurrent chemoradiotherapy, and for another 50 patients who received induction TPF chemotherapy followed by chemoradiation. The oropharynx was the most common cancer site, in 24 of the induction group (48%) and 59 of the concurrent group (65%).
A total of 19 induction patients (38%) required unplanned readmission, with 8 requiring more than one. Median length of stay for those total 27 unplanned stays was 6 days (range 1-25). In the concurrent group, 47 patients required unplanned readmission (52%), with 19 requiring more than one. That group had a total 77 unplanned readmissions, with a median stay of 7.8 days (1-65).
Total costs of admissions in the induction group were $3,368,583 for the planned admissions and $1,777,136 for the unplanned admissions. The median cost per planned hospital stay – elective admission for chemotherapy – was $32,276. In contrast, the cost per unplanned hospital stay was $42,390. For the concurrent group, which did not have planned hospitalizations, the cost per unplanned stay was $69,460, said Dr. Rostorfer, medical oncology and hematology chief fellow at MD Anderson Cancer Center Orlando, and his associates.
"Obviously this was a small, retrospective review, but the numbers can be quite alarming. We have begun to implement measures to reduce the numbers of readmission, so hopefully to reduce the cost associated with care. We will see the difference it makes."
Dr. Rostorfer stated that he has no disclosures.
PHOENIX – Unplanned hospitalizations due to toxicities associated with head and neck cancer treatment were a source of substantial cost in a retrospective chart review of 141 patients treated at a single cancer center during 2007-2011.
Much of the increased cost was among patients who underwent docetaxel plus cisplatin and fluorouracil induction chemotherapy (TPF) plus chemoradiotherapy.
"In recent years, induction chemotherapy has been increasingly incorporated into multimodality regimens for selected patients with locally advanced primary squamous cell carcinoma of the head and neck (HNSCC) ... Although efficacious (N. Engl. J. Med. 2007;357:1705-15), TPF has the potential for toxicities [that] may lead to unplanned admissions during treatment. Concurrent use of chemotherapy with radiation is well documented to intensify therapeutic effect and toxicity," Dr. Regan D. Rostorfer and his associates said in a poster.
Symptoms leading to the unplanned readmissions during induction chemotherapy (27 readmissions, 18 patients) included dehydration (in 13 of the 27 readmissions), infection (8), diarrhea (6), nausea/vomiting (5), pain (4), and mucositis (3).
A range of strategies can be used to avoid readmissions and thereby reduce these costs, including careful patient selection, use of prophylactic antimicrobials, standardized use of growth factor support, post-treatment support with outpatient intravenous fluids, integration of home health care services, early gastrostomy-tube placement, use of long-acting antiemetics during treatment, and frequent outpatient office visits during treatment, Dr. Rostorfer and his associates said.
"A number of initiatives are ongoing at our center in efforts to decrease readmission rates during combined modality treatment. Further studies are planned to assess the impact of these measures on readmission rates, and impact on costs of care," the investigators said in their poster.
In an interview, Dr. Rostorfer said the study was initially intended to simply to gather statistics about readmission for head/neck cancer treatment-related toxicity, since there were no published data on it.
"We decided to look at data from our own institution, simply to see how frequently patients were readmitted, and the reason for readmission. More recently, costs have become an issue at almost every hospital in the country, so we decided to look at the excess costs associated with these unplanned admissions, as well.
The investigators reviewed charts for 91 randomly assigned patients with locally advanced primary HNSCC who received treatment with concurrent chemoradiotherapy, and for another 50 patients who received induction TPF chemotherapy followed by chemoradiation. The oropharynx was the most common cancer site, in 24 of the induction group (48%) and 59 of the concurrent group (65%).
A total of 19 induction patients (38%) required unplanned readmission, with 8 requiring more than one. Median length of stay for those total 27 unplanned stays was 6 days (range 1-25). In the concurrent group, 47 patients required unplanned readmission (52%), with 19 requiring more than one. That group had a total 77 unplanned readmissions, with a median stay of 7.8 days (1-65).
Total costs of admissions in the induction group were $3,368,583 for the planned admissions and $1,777,136 for the unplanned admissions. The median cost per planned hospital stay – elective admission for chemotherapy – was $32,276. In contrast, the cost per unplanned hospital stay was $42,390. For the concurrent group, which did not have planned hospitalizations, the cost per unplanned stay was $69,460, said Dr. Rostorfer, medical oncology and hematology chief fellow at MD Anderson Cancer Center Orlando, and his associates.
"Obviously this was a small, retrospective review, but the numbers can be quite alarming. We have begun to implement measures to reduce the numbers of readmission, so hopefully to reduce the cost associated with care. We will see the difference it makes."
Dr. Rostorfer stated that he has no disclosures.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: Total costs of all admissions for the induction group were $3,368,583 for the planned admissions and $1,777,136 for the unplanned admissions. The median cost per planned hospital stay, that is, the elective admission for chemotherapy, was $32,276. In contrast, the cost per unplanned hospital stay was $42,390. For the concurrent group, the cost per unplanned stay was $69,460.
Data Source: The findings come from a retrospective chart review of 141 patients with locally advanced head and neck cancer seen at a single center.
Disclosures: Dr. Rostorfer reported having no financial disclosures.
IMRT Provides Better QOL in Head and Neck Cancers
PHOENIX – Intensity-modulated radiotherapy is more expensive than 3-D–conformal radiotherapy is and has not been shown to improve standard outcomes in patients with head and neck cancer. But it results in better quality of life.
These findings from two studies presented at the Multidisciplinary Head and Neck Cancer Symposium raise the question: Does improved quality of life justify the greater expense of intensity modulated radiotherapy (IMRT), which has been rapidly adopted for the treatment of head and neck cancer?
Because IMRT spares surrounding tissues, it reduces the likelihood of developing xerostomia, noted Dr. Nathan C. Sheets, who presented data on billing charges associated with IMRT, compared with 3-D–conformal radiotherapy (CRT). IMRT is reimbursed at a substantially higher level than CRT, however, and it is unclear how to assess this cost relative to other aspects of care in this population, said Dr. Sheets, a radiation oncology resident at the University of North Carolina, Chapel Hill.
A separate study presented by Dr. Allen M. Chen compared quality of life in patients who received IMRT vs. CRT. "There’s very little data to suggest IMRT is better than non-IMRT using traditional end points. But the question is: How do you define ‘better’?" said Dr. Chen, director of the radiation oncology residency training program at the University of California, Davis in Sacramento.
"IMRT might not particularly involve better cure rates, but it could make a difference in terms of other end points, such as quality of life, which we all know is very important to patients," he said.
Gap Ranges from $5,000 to $6,000
The cost study analyzed data for 184 patients who had received definitive radiation therapy for head and neck squamous cell cancer at the University of North Carolina at Chapel Hill during 2000-2009 and for whom billing records were available.
The median year of treatment was 2004 for 89 patients treated with CRT, and 2007 for 95 IMRT patients, reflecting the shift to use of IMRT over time. The majority of patients – 87% of CRT and 94% of IMRT – received concurrent chemotherapy. More IMRT patients received positron emission tomography (PET) scans at any point (69% vs. 37%).
Over 36 months’ follow-up, locoregional control was nearly identical for the two patient groups (P = .73). Mean total costs, from the time of diagnosis through the first year of follow-up, were considerably higher for IMRT, at $50,502 vs. $38,977 for CRT. Outpatient costs accounted for the bulk of the difference ($35,418 IMRT vs. $22,696 CRT), whereas inpatient costs were similar, Dr. Sheets reported.
Multivariate analysis showed that factors associated with increased cost of radiotherapy included IMRT, recurrent disease, comorbidities, non-white race, and use of positron-emission scanning. After adjustment for inflation, each of these factors, including IMRT, independently increased the total cost by approximately $5,000-$6000. (Treatment failure was much more expensive, contributing about $14,274 to the total cost.)
Dr. Sheets ended his presentation with the question, "Do the benefits of IMRT outweigh the costs?"
QOL Improves Over 2 Years’ Follow-up
Dr. Chen’s quality of life study addressed that question. The study used the University of Washington Quality of Life instrument (UW-QOL), a previously validated, self-administered questionnaire given to patients returning for follow-up after completion of radiation therapy for head and neck cancer. The University of California, Davis, routinely uses the measure in clinical practice.
Scores on the UW-QOL were retrospectively reviewed for 155 patients with squamous cell carcinomas of the head and neck requiring bilateral neck irradiation for locally advanced disease. Only patients who were clinically without evidence of recurrent disease and with at least 2 years of follow-up were included in the analysis. Definitive radiation therapy was given to 82 patients (53%), while 73 (47%) underwent postoperative treatment.
IMRT was used in 84 patients (54%), with inclusion of the low neck in an extended field. The remaining 71 patients (46%) were treated with 3-D–CRT using opposed lateral fields matched to a low anterior neck field. Concurrent chemotherapy was administered with radiation therapy for 73 patients (47%).
The mean global quality of life scores for the IMRT patients were 67.5 at 1 year and 80.1 at 2 years, compared with 55.4 and 57.0, respectively, for the CRT patients (P less than .001). At 1 year after completion of radiation therapy, the proportion of patients who rated their global quality of life as "very good" or "outstanding" 51% of the IMRT patients, compared with 41% of those treated with CRT (P = .11).
Those numbers became statistically significant at 2 years, with "very good" or "outstanding" quality of life reported by 73% of the IMRT patients and 49% of the CRT group (P less than .001). At last follow-up, 80% of patients treated by IMRT reported that their health-related quality of life was "much better" or "somewhat better," compared with the month before developing cancer, compared with 61% among patients treated by 3-D–CRT (P less than .001).
On multivariate analysis accounting for gender, age, radiation intent (definitive vs. postoperative), radiation dose, T stage, primary site, use of concurrent chemotherapy, and neck dissection, the use of IMRT was the only variable independently associated with improved quality of life (P = .01).
In 1- and 2-year analyses of factors contributing to the difference in UW-QOL score, only "saliva" was found to be significantly different between IMRT and CRT (P less than .001) for both time points. Other examined factors that did not affect the score included pain, appearance, activity, recreation, chewing, swallowing, speech, mood, and anxiety.
"Treatments for dry mouth are fairly primitive and ineffective at present, so preventing dry mouth is so critical. It’s a huge problem. Imagine not being able to make any saliva. And, there are health consequences with respect to things like oral hygiene and dental caries. There’s a cost associated with chronic dry mouth," Dr. Chen said in the interview.
Increased Cost Not That Big
The increase in cost with IMRT isn’t that big, Dr. Bhisham Chera, the principal investigator for the cost study and a radiation oncologist at the University of North Carolina said in an interview.
"On average, it was about $5,000-$6,000 more total," he said. "It is more expensive, but what was shocking to me is that it wasn’t much more expensive as some therapies – like newer chemotherapy drugs, compared to older ones, where there’s a hundred thousand dollar difference in cost and the survival improvement is only a few months."
"We think the incremental increase in cost is justified because of the improvement in dry mouth. If you really compare it to other therapies such as using transperineal prostatectomy vs. robotic prostatectomy or cisplatin vs. cetuximab chemotherapy, the cost difference is vastly greater," he added. "Here, the incremental difference is not that much. It is more expensive, but it’s not astronomically more expensive."
Dr. Sheets, Dr. Chen, and Dr. Chera all stated that they had no disclosures.
PHOENIX – Intensity-modulated radiotherapy is more expensive than 3-D–conformal radiotherapy is and has not been shown to improve standard outcomes in patients with head and neck cancer. But it results in better quality of life.
These findings from two studies presented at the Multidisciplinary Head and Neck Cancer Symposium raise the question: Does improved quality of life justify the greater expense of intensity modulated radiotherapy (IMRT), which has been rapidly adopted for the treatment of head and neck cancer?
Because IMRT spares surrounding tissues, it reduces the likelihood of developing xerostomia, noted Dr. Nathan C. Sheets, who presented data on billing charges associated with IMRT, compared with 3-D–conformal radiotherapy (CRT). IMRT is reimbursed at a substantially higher level than CRT, however, and it is unclear how to assess this cost relative to other aspects of care in this population, said Dr. Sheets, a radiation oncology resident at the University of North Carolina, Chapel Hill.
A separate study presented by Dr. Allen M. Chen compared quality of life in patients who received IMRT vs. CRT. "There’s very little data to suggest IMRT is better than non-IMRT using traditional end points. But the question is: How do you define ‘better’?" said Dr. Chen, director of the radiation oncology residency training program at the University of California, Davis in Sacramento.
"IMRT might not particularly involve better cure rates, but it could make a difference in terms of other end points, such as quality of life, which we all know is very important to patients," he said.
Gap Ranges from $5,000 to $6,000
The cost study analyzed data for 184 patients who had received definitive radiation therapy for head and neck squamous cell cancer at the University of North Carolina at Chapel Hill during 2000-2009 and for whom billing records were available.
The median year of treatment was 2004 for 89 patients treated with CRT, and 2007 for 95 IMRT patients, reflecting the shift to use of IMRT over time. The majority of patients – 87% of CRT and 94% of IMRT – received concurrent chemotherapy. More IMRT patients received positron emission tomography (PET) scans at any point (69% vs. 37%).
Over 36 months’ follow-up, locoregional control was nearly identical for the two patient groups (P = .73). Mean total costs, from the time of diagnosis through the first year of follow-up, were considerably higher for IMRT, at $50,502 vs. $38,977 for CRT. Outpatient costs accounted for the bulk of the difference ($35,418 IMRT vs. $22,696 CRT), whereas inpatient costs were similar, Dr. Sheets reported.
Multivariate analysis showed that factors associated with increased cost of radiotherapy included IMRT, recurrent disease, comorbidities, non-white race, and use of positron-emission scanning. After adjustment for inflation, each of these factors, including IMRT, independently increased the total cost by approximately $5,000-$6000. (Treatment failure was much more expensive, contributing about $14,274 to the total cost.)
Dr. Sheets ended his presentation with the question, "Do the benefits of IMRT outweigh the costs?"
QOL Improves Over 2 Years’ Follow-up
Dr. Chen’s quality of life study addressed that question. The study used the University of Washington Quality of Life instrument (UW-QOL), a previously validated, self-administered questionnaire given to patients returning for follow-up after completion of radiation therapy for head and neck cancer. The University of California, Davis, routinely uses the measure in clinical practice.
Scores on the UW-QOL were retrospectively reviewed for 155 patients with squamous cell carcinomas of the head and neck requiring bilateral neck irradiation for locally advanced disease. Only patients who were clinically without evidence of recurrent disease and with at least 2 years of follow-up were included in the analysis. Definitive radiation therapy was given to 82 patients (53%), while 73 (47%) underwent postoperative treatment.
IMRT was used in 84 patients (54%), with inclusion of the low neck in an extended field. The remaining 71 patients (46%) were treated with 3-D–CRT using opposed lateral fields matched to a low anterior neck field. Concurrent chemotherapy was administered with radiation therapy for 73 patients (47%).
The mean global quality of life scores for the IMRT patients were 67.5 at 1 year and 80.1 at 2 years, compared with 55.4 and 57.0, respectively, for the CRT patients (P less than .001). At 1 year after completion of radiation therapy, the proportion of patients who rated their global quality of life as "very good" or "outstanding" 51% of the IMRT patients, compared with 41% of those treated with CRT (P = .11).
Those numbers became statistically significant at 2 years, with "very good" or "outstanding" quality of life reported by 73% of the IMRT patients and 49% of the CRT group (P less than .001). At last follow-up, 80% of patients treated by IMRT reported that their health-related quality of life was "much better" or "somewhat better," compared with the month before developing cancer, compared with 61% among patients treated by 3-D–CRT (P less than .001).
On multivariate analysis accounting for gender, age, radiation intent (definitive vs. postoperative), radiation dose, T stage, primary site, use of concurrent chemotherapy, and neck dissection, the use of IMRT was the only variable independently associated with improved quality of life (P = .01).
In 1- and 2-year analyses of factors contributing to the difference in UW-QOL score, only "saliva" was found to be significantly different between IMRT and CRT (P less than .001) for both time points. Other examined factors that did not affect the score included pain, appearance, activity, recreation, chewing, swallowing, speech, mood, and anxiety.
"Treatments for dry mouth are fairly primitive and ineffective at present, so preventing dry mouth is so critical. It’s a huge problem. Imagine not being able to make any saliva. And, there are health consequences with respect to things like oral hygiene and dental caries. There’s a cost associated with chronic dry mouth," Dr. Chen said in the interview.
Increased Cost Not That Big
The increase in cost with IMRT isn’t that big, Dr. Bhisham Chera, the principal investigator for the cost study and a radiation oncologist at the University of North Carolina said in an interview.
"On average, it was about $5,000-$6,000 more total," he said. "It is more expensive, but what was shocking to me is that it wasn’t much more expensive as some therapies – like newer chemotherapy drugs, compared to older ones, where there’s a hundred thousand dollar difference in cost and the survival improvement is only a few months."
"We think the incremental increase in cost is justified because of the improvement in dry mouth. If you really compare it to other therapies such as using transperineal prostatectomy vs. robotic prostatectomy or cisplatin vs. cetuximab chemotherapy, the cost difference is vastly greater," he added. "Here, the incremental difference is not that much. It is more expensive, but it’s not astronomically more expensive."
Dr. Sheets, Dr. Chen, and Dr. Chera all stated that they had no disclosures.
PHOENIX – Intensity-modulated radiotherapy is more expensive than 3-D–conformal radiotherapy is and has not been shown to improve standard outcomes in patients with head and neck cancer. But it results in better quality of life.
These findings from two studies presented at the Multidisciplinary Head and Neck Cancer Symposium raise the question: Does improved quality of life justify the greater expense of intensity modulated radiotherapy (IMRT), which has been rapidly adopted for the treatment of head and neck cancer?
Because IMRT spares surrounding tissues, it reduces the likelihood of developing xerostomia, noted Dr. Nathan C. Sheets, who presented data on billing charges associated with IMRT, compared with 3-D–conformal radiotherapy (CRT). IMRT is reimbursed at a substantially higher level than CRT, however, and it is unclear how to assess this cost relative to other aspects of care in this population, said Dr. Sheets, a radiation oncology resident at the University of North Carolina, Chapel Hill.
A separate study presented by Dr. Allen M. Chen compared quality of life in patients who received IMRT vs. CRT. "There’s very little data to suggest IMRT is better than non-IMRT using traditional end points. But the question is: How do you define ‘better’?" said Dr. Chen, director of the radiation oncology residency training program at the University of California, Davis in Sacramento.
"IMRT might not particularly involve better cure rates, but it could make a difference in terms of other end points, such as quality of life, which we all know is very important to patients," he said.
Gap Ranges from $5,000 to $6,000
The cost study analyzed data for 184 patients who had received definitive radiation therapy for head and neck squamous cell cancer at the University of North Carolina at Chapel Hill during 2000-2009 and for whom billing records were available.
The median year of treatment was 2004 for 89 patients treated with CRT, and 2007 for 95 IMRT patients, reflecting the shift to use of IMRT over time. The majority of patients – 87% of CRT and 94% of IMRT – received concurrent chemotherapy. More IMRT patients received positron emission tomography (PET) scans at any point (69% vs. 37%).
Over 36 months’ follow-up, locoregional control was nearly identical for the two patient groups (P = .73). Mean total costs, from the time of diagnosis through the first year of follow-up, were considerably higher for IMRT, at $50,502 vs. $38,977 for CRT. Outpatient costs accounted for the bulk of the difference ($35,418 IMRT vs. $22,696 CRT), whereas inpatient costs were similar, Dr. Sheets reported.
Multivariate analysis showed that factors associated with increased cost of radiotherapy included IMRT, recurrent disease, comorbidities, non-white race, and use of positron-emission scanning. After adjustment for inflation, each of these factors, including IMRT, independently increased the total cost by approximately $5,000-$6000. (Treatment failure was much more expensive, contributing about $14,274 to the total cost.)
Dr. Sheets ended his presentation with the question, "Do the benefits of IMRT outweigh the costs?"
QOL Improves Over 2 Years’ Follow-up
Dr. Chen’s quality of life study addressed that question. The study used the University of Washington Quality of Life instrument (UW-QOL), a previously validated, self-administered questionnaire given to patients returning for follow-up after completion of radiation therapy for head and neck cancer. The University of California, Davis, routinely uses the measure in clinical practice.
Scores on the UW-QOL were retrospectively reviewed for 155 patients with squamous cell carcinomas of the head and neck requiring bilateral neck irradiation for locally advanced disease. Only patients who were clinically without evidence of recurrent disease and with at least 2 years of follow-up were included in the analysis. Definitive radiation therapy was given to 82 patients (53%), while 73 (47%) underwent postoperative treatment.
IMRT was used in 84 patients (54%), with inclusion of the low neck in an extended field. The remaining 71 patients (46%) were treated with 3-D–CRT using opposed lateral fields matched to a low anterior neck field. Concurrent chemotherapy was administered with radiation therapy for 73 patients (47%).
The mean global quality of life scores for the IMRT patients were 67.5 at 1 year and 80.1 at 2 years, compared with 55.4 and 57.0, respectively, for the CRT patients (P less than .001). At 1 year after completion of radiation therapy, the proportion of patients who rated their global quality of life as "very good" or "outstanding" 51% of the IMRT patients, compared with 41% of those treated with CRT (P = .11).
Those numbers became statistically significant at 2 years, with "very good" or "outstanding" quality of life reported by 73% of the IMRT patients and 49% of the CRT group (P less than .001). At last follow-up, 80% of patients treated by IMRT reported that their health-related quality of life was "much better" or "somewhat better," compared with the month before developing cancer, compared with 61% among patients treated by 3-D–CRT (P less than .001).
On multivariate analysis accounting for gender, age, radiation intent (definitive vs. postoperative), radiation dose, T stage, primary site, use of concurrent chemotherapy, and neck dissection, the use of IMRT was the only variable independently associated with improved quality of life (P = .01).
In 1- and 2-year analyses of factors contributing to the difference in UW-QOL score, only "saliva" was found to be significantly different between IMRT and CRT (P less than .001) for both time points. Other examined factors that did not affect the score included pain, appearance, activity, recreation, chewing, swallowing, speech, mood, and anxiety.
"Treatments for dry mouth are fairly primitive and ineffective at present, so preventing dry mouth is so critical. It’s a huge problem. Imagine not being able to make any saliva. And, there are health consequences with respect to things like oral hygiene and dental caries. There’s a cost associated with chronic dry mouth," Dr. Chen said in the interview.
Increased Cost Not That Big
The increase in cost with IMRT isn’t that big, Dr. Bhisham Chera, the principal investigator for the cost study and a radiation oncologist at the University of North Carolina said in an interview.
"On average, it was about $5,000-$6,000 more total," he said. "It is more expensive, but what was shocking to me is that it wasn’t much more expensive as some therapies – like newer chemotherapy drugs, compared to older ones, where there’s a hundred thousand dollar difference in cost and the survival improvement is only a few months."
"We think the incremental increase in cost is justified because of the improvement in dry mouth. If you really compare it to other therapies such as using transperineal prostatectomy vs. robotic prostatectomy or cisplatin vs. cetuximab chemotherapy, the cost difference is vastly greater," he added. "Here, the incremental difference is not that much. It is more expensive, but it’s not astronomically more expensive."
Dr. Sheets, Dr. Chen, and Dr. Chera all stated that they had no disclosures.
A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: IMRT was about $5,000-$6,000 more expensive than was 3-D–CRT. But 73% of IMRT patients reported very good or outstanding quality of life at 2 years vs. 49% of CRT patients (P less than .001).
Data Source: Investigators presented separate retrospective studies comparing IMRT with 3D-CRT in head and neck cancers at their institutions.
Disclosures: Dr. Sheets, Dr. Chen, and Dr. Chera all stated that they had no disclosures.
Cisplatin Aids Survival of High-Risk Head and Neck Cancer
PHOENIX – Adding chemotherapy to radiotherapy improved 10-year survival of resectable head and neck carcinomas among high-risk patients who had microscopically involved resection margins and/or extracapsular spread of disease – but not in high-risk patients who only had tumor in multiple lymph nodes.
The findings come from a long-term update and unplanned subset analysis of 410 evaluable patients from the RTOG (Radiation Therapy Oncology Group) 9501 phase III study, which previously showed no overall survival advantage from the addition of cisplatin chemotherapy to radiation.
The new data are "good news," according to lead author Dr. Jay Cooper, director of Maimonides Cancer Center in Brooklyn, N.Y.
"We now can eradicate some advanced head and neck tumors that we couldn’t before by adding chemotherapy to radiation therapy. At the same time, we can spare other patients who would not do better with the addition of chemotherapy from its side effects," he said at a head and neck cancer symposium sponsored by the American Society for Radiation Therapy.
The RTOG 9501 study randomized 459 patients with high-risk, resected head and neck cancers to receive either radiation therapy of 60 Gy in 6 weeks (RT), or identical radiotherapy plus cisplatin at 100 mg/m2 IV on days 1, 22, and 43 (RT+CT).
When reported at a median follow-up of 45.9 months, the locoregional control rate was significantly higher in the combined-therapy group than in the group given radiotherapy alone (hazard ratio for locoregional recurrence, 0.61); disease-free survival was significantly longer with combined therapy (HR for disease or death, 0.78), but overall survival was not (HR for death, 0.84). Moreover, four patients who received combination therapy died as a result of treatment (N. Engl. J. Med. 2004;350:1937-44).
In the current updated analysis conducted 10 years post treatment, none of the primary outcomes differed significantly between the two groups. The evaluable population comprised 208 patients who received RT and 202 given RT+CT. For patients treated by RT vs. RT+CT, the rates were, respectively, 28.8% vs. 22.3% (P = .10) for locoregional failure, 19.1% vs. 20.1% (P = .25) for disease-free survival, and 27.0% vs. 29.1% (P = .31) for overall survival.
In a subset analysis that had not been performed previously, however, statistically significant differences appeared within the 242 patients who had microscopically involved resection margins and/or extracapsular spread of disease. In this group, 115 patients received RT and 127 were given RT+CT. Locoregional failure occurred in 33.1% of the CT group vs. 21.0% of those treated with RT+CT (P = .02). The disease-free survival rate was 12.3% vs. 18.4% (P = .05), and the overall survival rate was 19.6% vs. 27.1% (P = .07), with both end points favoring RT+CT.
That left 168 patients who did not have involved margins or extracapsular extension and were included in the trial solely because they had multiple involved nodes. In this group, 93 received RT and 75 RT+CT, with no significant difference in long-term outcomes.
There was a trend in improved cause-specific survival with RT+CT for patients whose death resulted from head and neck cancer, but more deaths not due to the study cancer were observed in patients treated with concurrent cisplatin. This is a hypothesis-generating finding that needs to be investigated in future trials, Dr. Cooper noted.
In an interview, he explained that the rationale for looking specifically at the patients with microscopically involved resection margins and/or extracapsular spread came from a previous analysis of the raw data from the RTOG trial combined with those of a concurrently published study conducted by the EORTC (European Organisation for Research and Treatment of Cancer).
Although the design of the EORTC 22931 study was similar, the outcome was different. Of a total 167 patients who had been randomized to RT or RT+CT, the rate of progression-free survival at a median follow-up of 60 months was significantly higher in the combined-therapy group than in the group given radiotherapy alone (P = .04) (N. Engl. J. Med. 2004;350:1945-52).
When the data from RTOG and EORTC were combined, it became clear that the main reason for the difference in outcome was in the different entry criteria for the two trials, and that extracapsular extension (ECE) and/or microscopically involved surgical margins were the only risk factors for which the impact of adjuvant chemotherapy-enhanced radiation therapy was significant in both trials (Head Neck 2005;27:843-50).
"What we learned from that analysis is that the patients who got on one of the trials but wouldn’t have qualified for the other trial were not getting much benefit from the study regimen, whereas those who qualified for either study – due to having involved margins and/or extracapsular extension – did better with chemotherapy on all three measures.
"These results were highly significant. But more importantly, the data suggested a subgroup where the big bang for the buck was," Dr. Cooper said in the interview.
The findings don’t mean that the patients who did not benefit are not "high risk," Dr. Cooper said. "Would they benefit from other chemotherapy? We don’t know. Would they benefit from different drugs or different regimens? Maybe. But we can now fairly comfortably say that in both the short and long run, if patients are high risk only because of involved lymph nodes, don’t treat them with this combination, and spare them the toxicity."
Dr. Cooper stated that he has no disclosures, as did nine coauthors. One additional coauthor is an employee of Lilly USA.
PHOENIX – Adding chemotherapy to radiotherapy improved 10-year survival of resectable head and neck carcinomas among high-risk patients who had microscopically involved resection margins and/or extracapsular spread of disease – but not in high-risk patients who only had tumor in multiple lymph nodes.
The findings come from a long-term update and unplanned subset analysis of 410 evaluable patients from the RTOG (Radiation Therapy Oncology Group) 9501 phase III study, which previously showed no overall survival advantage from the addition of cisplatin chemotherapy to radiation.
The new data are "good news," according to lead author Dr. Jay Cooper, director of Maimonides Cancer Center in Brooklyn, N.Y.
"We now can eradicate some advanced head and neck tumors that we couldn’t before by adding chemotherapy to radiation therapy. At the same time, we can spare other patients who would not do better with the addition of chemotherapy from its side effects," he said at a head and neck cancer symposium sponsored by the American Society for Radiation Therapy.
The RTOG 9501 study randomized 459 patients with high-risk, resected head and neck cancers to receive either radiation therapy of 60 Gy in 6 weeks (RT), or identical radiotherapy plus cisplatin at 100 mg/m2 IV on days 1, 22, and 43 (RT+CT).
When reported at a median follow-up of 45.9 months, the locoregional control rate was significantly higher in the combined-therapy group than in the group given radiotherapy alone (hazard ratio for locoregional recurrence, 0.61); disease-free survival was significantly longer with combined therapy (HR for disease or death, 0.78), but overall survival was not (HR for death, 0.84). Moreover, four patients who received combination therapy died as a result of treatment (N. Engl. J. Med. 2004;350:1937-44).
In the current updated analysis conducted 10 years post treatment, none of the primary outcomes differed significantly between the two groups. The evaluable population comprised 208 patients who received RT and 202 given RT+CT. For patients treated by RT vs. RT+CT, the rates were, respectively, 28.8% vs. 22.3% (P = .10) for locoregional failure, 19.1% vs. 20.1% (P = .25) for disease-free survival, and 27.0% vs. 29.1% (P = .31) for overall survival.
In a subset analysis that had not been performed previously, however, statistically significant differences appeared within the 242 patients who had microscopically involved resection margins and/or extracapsular spread of disease. In this group, 115 patients received RT and 127 were given RT+CT. Locoregional failure occurred in 33.1% of the CT group vs. 21.0% of those treated with RT+CT (P = .02). The disease-free survival rate was 12.3% vs. 18.4% (P = .05), and the overall survival rate was 19.6% vs. 27.1% (P = .07), with both end points favoring RT+CT.
That left 168 patients who did not have involved margins or extracapsular extension and were included in the trial solely because they had multiple involved nodes. In this group, 93 received RT and 75 RT+CT, with no significant difference in long-term outcomes.
There was a trend in improved cause-specific survival with RT+CT for patients whose death resulted from head and neck cancer, but more deaths not due to the study cancer were observed in patients treated with concurrent cisplatin. This is a hypothesis-generating finding that needs to be investigated in future trials, Dr. Cooper noted.
In an interview, he explained that the rationale for looking specifically at the patients with microscopically involved resection margins and/or extracapsular spread came from a previous analysis of the raw data from the RTOG trial combined with those of a concurrently published study conducted by the EORTC (European Organisation for Research and Treatment of Cancer).
Although the design of the EORTC 22931 study was similar, the outcome was different. Of a total 167 patients who had been randomized to RT or RT+CT, the rate of progression-free survival at a median follow-up of 60 months was significantly higher in the combined-therapy group than in the group given radiotherapy alone (P = .04) (N. Engl. J. Med. 2004;350:1945-52).
When the data from RTOG and EORTC were combined, it became clear that the main reason for the difference in outcome was in the different entry criteria for the two trials, and that extracapsular extension (ECE) and/or microscopically involved surgical margins were the only risk factors for which the impact of adjuvant chemotherapy-enhanced radiation therapy was significant in both trials (Head Neck 2005;27:843-50).
"What we learned from that analysis is that the patients who got on one of the trials but wouldn’t have qualified for the other trial were not getting much benefit from the study regimen, whereas those who qualified for either study – due to having involved margins and/or extracapsular extension – did better with chemotherapy on all three measures.
"These results were highly significant. But more importantly, the data suggested a subgroup where the big bang for the buck was," Dr. Cooper said in the interview.
The findings don’t mean that the patients who did not benefit are not "high risk," Dr. Cooper said. "Would they benefit from other chemotherapy? We don’t know. Would they benefit from different drugs or different regimens? Maybe. But we can now fairly comfortably say that in both the short and long run, if patients are high risk only because of involved lymph nodes, don’t treat them with this combination, and spare them the toxicity."
Dr. Cooper stated that he has no disclosures, as did nine coauthors. One additional coauthor is an employee of Lilly USA.
PHOENIX – Adding chemotherapy to radiotherapy improved 10-year survival of resectable head and neck carcinomas among high-risk patients who had microscopically involved resection margins and/or extracapsular spread of disease – but not in high-risk patients who only had tumor in multiple lymph nodes.
The findings come from a long-term update and unplanned subset analysis of 410 evaluable patients from the RTOG (Radiation Therapy Oncology Group) 9501 phase III study, which previously showed no overall survival advantage from the addition of cisplatin chemotherapy to radiation.
The new data are "good news," according to lead author Dr. Jay Cooper, director of Maimonides Cancer Center in Brooklyn, N.Y.
"We now can eradicate some advanced head and neck tumors that we couldn’t before by adding chemotherapy to radiation therapy. At the same time, we can spare other patients who would not do better with the addition of chemotherapy from its side effects," he said at a head and neck cancer symposium sponsored by the American Society for Radiation Therapy.
The RTOG 9501 study randomized 459 patients with high-risk, resected head and neck cancers to receive either radiation therapy of 60 Gy in 6 weeks (RT), or identical radiotherapy plus cisplatin at 100 mg/m2 IV on days 1, 22, and 43 (RT+CT).
When reported at a median follow-up of 45.9 months, the locoregional control rate was significantly higher in the combined-therapy group than in the group given radiotherapy alone (hazard ratio for locoregional recurrence, 0.61); disease-free survival was significantly longer with combined therapy (HR for disease or death, 0.78), but overall survival was not (HR for death, 0.84). Moreover, four patients who received combination therapy died as a result of treatment (N. Engl. J. Med. 2004;350:1937-44).
In the current updated analysis conducted 10 years post treatment, none of the primary outcomes differed significantly between the two groups. The evaluable population comprised 208 patients who received RT and 202 given RT+CT. For patients treated by RT vs. RT+CT, the rates were, respectively, 28.8% vs. 22.3% (P = .10) for locoregional failure, 19.1% vs. 20.1% (P = .25) for disease-free survival, and 27.0% vs. 29.1% (P = .31) for overall survival.
In a subset analysis that had not been performed previously, however, statistically significant differences appeared within the 242 patients who had microscopically involved resection margins and/or extracapsular spread of disease. In this group, 115 patients received RT and 127 were given RT+CT. Locoregional failure occurred in 33.1% of the CT group vs. 21.0% of those treated with RT+CT (P = .02). The disease-free survival rate was 12.3% vs. 18.4% (P = .05), and the overall survival rate was 19.6% vs. 27.1% (P = .07), with both end points favoring RT+CT.
That left 168 patients who did not have involved margins or extracapsular extension and were included in the trial solely because they had multiple involved nodes. In this group, 93 received RT and 75 RT+CT, with no significant difference in long-term outcomes.
There was a trend in improved cause-specific survival with RT+CT for patients whose death resulted from head and neck cancer, but more deaths not due to the study cancer were observed in patients treated with concurrent cisplatin. This is a hypothesis-generating finding that needs to be investigated in future trials, Dr. Cooper noted.
In an interview, he explained that the rationale for looking specifically at the patients with microscopically involved resection margins and/or extracapsular spread came from a previous analysis of the raw data from the RTOG trial combined with those of a concurrently published study conducted by the EORTC (European Organisation for Research and Treatment of Cancer).
Although the design of the EORTC 22931 study was similar, the outcome was different. Of a total 167 patients who had been randomized to RT or RT+CT, the rate of progression-free survival at a median follow-up of 60 months was significantly higher in the combined-therapy group than in the group given radiotherapy alone (P = .04) (N. Engl. J. Med. 2004;350:1945-52).
When the data from RTOG and EORTC were combined, it became clear that the main reason for the difference in outcome was in the different entry criteria for the two trials, and that extracapsular extension (ECE) and/or microscopically involved surgical margins were the only risk factors for which the impact of adjuvant chemotherapy-enhanced radiation therapy was significant in both trials (Head Neck 2005;27:843-50).
"What we learned from that analysis is that the patients who got on one of the trials but wouldn’t have qualified for the other trial were not getting much benefit from the study regimen, whereas those who qualified for either study – due to having involved margins and/or extracapsular extension – did better with chemotherapy on all three measures.
"These results were highly significant. But more importantly, the data suggested a subgroup where the big bang for the buck was," Dr. Cooper said in the interview.
The findings don’t mean that the patients who did not benefit are not "high risk," Dr. Cooper said. "Would they benefit from other chemotherapy? We don’t know. Would they benefit from different drugs or different regimens? Maybe. But we can now fairly comfortably say that in both the short and long run, if patients are high risk only because of involved lymph nodes, don’t treat them with this combination, and spare them the toxicity."
Dr. Cooper stated that he has no disclosures, as did nine coauthors. One additional coauthor is an employee of Lilly USA.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONOSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: At 10 years post treatment, the overall survival rate was higher when cisplatin was added to adjuvant radiotherapy in patients who had microscopically involved resection margins and/or extracapsular spread of disease (27.1% vs. 19.6% with RT alone; P = .07).
Data Source: The data come from an unplanned analysis of 410 patients in the randomized phase III RTOG 9501.
Disclosures: Dr. Cooper stated that he has no disclosures, as did nine coauthors. One additional coauthor is an employee of Lilly USA.
PET/CT Detects Early Recurrence of Head and Neck Cancer
PHOENIX – Routine use of positron emission tomography/computed tomography scans can detect locoregional recurrences of squamous cell carcinoma of the head and neck before they became clinically apparent, according to a retrospective chart review of 234 patients who had been treated with chemoradiation between 2006 and 2010.
The finding suggests that routine use of positron emission tomography/computed tomography (PET/CT) may improve the outcome of salvage therapy, said Dr. Yasir Rudha, who reported the study at the Multidisciplinary Head and Neck Symposium sponsored by the American Society for Radiation Oncology.
PET/CT was associated with a high false positive rate, which should be considered when ordering radiological exams and biopsies, but a negative posttherapy PET scan appears to be an excellent predictor of freedom from future locoregional recurrence, said Dr. Rudha of St. John Hospital/Van Elslander Cancer Center, Grosse Pointe Woods, Mich.
The technology is relatively new, and its use for routine follow-up in patients with head and neck cancer is still controversial, he acknowledged. "Only a few publications have reported the value of PET examination at a fixed time interval after the end of treatment," he said. "PET scan is often ordered in our hospital as a routine surveillance tool following successful completion of treatment."
The review of charts for all 234 patients identified 45 who had achieved clinical no-evidence-of-disease status at the time of posttreatment imaging. In this group, PET/CT scanning at 6-9 weeks identified 15 patients with abnormalities that required further evaluation. Of those, eight patients (53%) were proven to have malignancies based on biopsy findings: six showed occult persistent disease at the primary site, and two were diagnosed with regional lymph node recurrence and colon cancer, respectively.
In the remaining seven cases, imaging findings were shown to represent false positive results with unnecessary work-up and/or biopsy evaluation. All patients who had negative PET/CT scans remained free from locoregional relapse at the time of last follow-up.
Thus, Dr. Rudha said the true positive rate for routine PET/CT surveillance in head and neck cancer patients was estimated as 8/15, or 53%, and the false positive rate as 7/15, or 46%.
"With malignancies found in 53% of abnormal scans in this study, our research proves that PET/CT scans are valuable as routine follow-up and as a surveillance method for head and neck cancer patients ... However, since the rate of false positives was 46%, caution should be shown when ordering biopsies after abnormal scans to prevent excessive unnecessary biopsies," he said.
During a press briefing, Dr. Rudha said that the 46% false positive rate was lower than what he and his colleagues expected. "Actually we expected the false positive ratio to be about 90%," he said.
In an interview, he said that at his institution patients with positive PET/CT scans at 6-9 weeks postsurgery are followed in a variety of ways, depending primarily on the PET standard uptake volume (SUV). If low, the patient might undergo another PET scan at about 3 months. But if SUV is high, the patient would likely be referred for another test such as magnetic resonance imaging, ultrasound, or biopsy at the site of recurrence.
However, if the postsurgery PET/CT scan is negative, "according to this research, it gives a great indication that the patient is free from disease and the treatment is successful."
Dr. Rudha and his coauthors stated that they had no disclosures.
PET/CT is being evaluated in a variety of different situations. We’re still looking at programs that are combining PET/CT imaging with functional DCI/MRI imaging in part to help oncologists find the tumor volume and define how to plan our treatments in regard to what the target volumes are both on the ipsilateral and contralateral side of the neck.
 |
|
In the posttreatment setting, it’s been absolutely critical for us in terms of determining who should go on to further evaluation or who could be watched carefully. For instance, a University of Maryland group has shown quite nicely that in patients who have a clinical complete response and a complete response by PET imaging, almost all those patients do not need a neck dissection (Head Neck 2010;32:46-52). ... That’s a significant savings in health care costs, whereas in the past, almost all of those patients 10-15 years ago would have gone on to a neck dissection.
The current study also offers important data. I believe 6 weeks is too early. We recommend a minimum of 8 weeks, preferably 12 weeks posttreatment, to allow inflammation to subside. That may help reduce the false positive rate. I think use of PET/CT continues to evolve, and hopefully additional functional imaging studies will help us nail down which patients need to go on to further treatment or biopsy.
Dr. David Raben is professor of radiation oncology at the University of Colorado, Denver. He had no disclosures
PET/CT is being evaluated in a variety of different situations. We’re still looking at programs that are combining PET/CT imaging with functional DCI/MRI imaging in part to help oncologists find the tumor volume and define how to plan our treatments in regard to what the target volumes are both on the ipsilateral and contralateral side of the neck.
 |
|
In the posttreatment setting, it’s been absolutely critical for us in terms of determining who should go on to further evaluation or who could be watched carefully. For instance, a University of Maryland group has shown quite nicely that in patients who have a clinical complete response and a complete response by PET imaging, almost all those patients do not need a neck dissection (Head Neck 2010;32:46-52). ... That’s a significant savings in health care costs, whereas in the past, almost all of those patients 10-15 years ago would have gone on to a neck dissection.
The current study also offers important data. I believe 6 weeks is too early. We recommend a minimum of 8 weeks, preferably 12 weeks posttreatment, to allow inflammation to subside. That may help reduce the false positive rate. I think use of PET/CT continues to evolve, and hopefully additional functional imaging studies will help us nail down which patients need to go on to further treatment or biopsy.
Dr. David Raben is professor of radiation oncology at the University of Colorado, Denver. He had no disclosures
PET/CT is being evaluated in a variety of different situations. We’re still looking at programs that are combining PET/CT imaging with functional DCI/MRI imaging in part to help oncologists find the tumor volume and define how to plan our treatments in regard to what the target volumes are both on the ipsilateral and contralateral side of the neck.
 |
|
In the posttreatment setting, it’s been absolutely critical for us in terms of determining who should go on to further evaluation or who could be watched carefully. For instance, a University of Maryland group has shown quite nicely that in patients who have a clinical complete response and a complete response by PET imaging, almost all those patients do not need a neck dissection (Head Neck 2010;32:46-52). ... That’s a significant savings in health care costs, whereas in the past, almost all of those patients 10-15 years ago would have gone on to a neck dissection.
The current study also offers important data. I believe 6 weeks is too early. We recommend a minimum of 8 weeks, preferably 12 weeks posttreatment, to allow inflammation to subside. That may help reduce the false positive rate. I think use of PET/CT continues to evolve, and hopefully additional functional imaging studies will help us nail down which patients need to go on to further treatment or biopsy.
Dr. David Raben is professor of radiation oncology at the University of Colorado, Denver. He had no disclosures
PHOENIX – Routine use of positron emission tomography/computed tomography scans can detect locoregional recurrences of squamous cell carcinoma of the head and neck before they became clinically apparent, according to a retrospective chart review of 234 patients who had been treated with chemoradiation between 2006 and 2010.
The finding suggests that routine use of positron emission tomography/computed tomography (PET/CT) may improve the outcome of salvage therapy, said Dr. Yasir Rudha, who reported the study at the Multidisciplinary Head and Neck Symposium sponsored by the American Society for Radiation Oncology.
PET/CT was associated with a high false positive rate, which should be considered when ordering radiological exams and biopsies, but a negative posttherapy PET scan appears to be an excellent predictor of freedom from future locoregional recurrence, said Dr. Rudha of St. John Hospital/Van Elslander Cancer Center, Grosse Pointe Woods, Mich.
The technology is relatively new, and its use for routine follow-up in patients with head and neck cancer is still controversial, he acknowledged. "Only a few publications have reported the value of PET examination at a fixed time interval after the end of treatment," he said. "PET scan is often ordered in our hospital as a routine surveillance tool following successful completion of treatment."
The review of charts for all 234 patients identified 45 who had achieved clinical no-evidence-of-disease status at the time of posttreatment imaging. In this group, PET/CT scanning at 6-9 weeks identified 15 patients with abnormalities that required further evaluation. Of those, eight patients (53%) were proven to have malignancies based on biopsy findings: six showed occult persistent disease at the primary site, and two were diagnosed with regional lymph node recurrence and colon cancer, respectively.
In the remaining seven cases, imaging findings were shown to represent false positive results with unnecessary work-up and/or biopsy evaluation. All patients who had negative PET/CT scans remained free from locoregional relapse at the time of last follow-up.
Thus, Dr. Rudha said the true positive rate for routine PET/CT surveillance in head and neck cancer patients was estimated as 8/15, or 53%, and the false positive rate as 7/15, or 46%.
"With malignancies found in 53% of abnormal scans in this study, our research proves that PET/CT scans are valuable as routine follow-up and as a surveillance method for head and neck cancer patients ... However, since the rate of false positives was 46%, caution should be shown when ordering biopsies after abnormal scans to prevent excessive unnecessary biopsies," he said.
During a press briefing, Dr. Rudha said that the 46% false positive rate was lower than what he and his colleagues expected. "Actually we expected the false positive ratio to be about 90%," he said.
In an interview, he said that at his institution patients with positive PET/CT scans at 6-9 weeks postsurgery are followed in a variety of ways, depending primarily on the PET standard uptake volume (SUV). If low, the patient might undergo another PET scan at about 3 months. But if SUV is high, the patient would likely be referred for another test such as magnetic resonance imaging, ultrasound, or biopsy at the site of recurrence.
However, if the postsurgery PET/CT scan is negative, "according to this research, it gives a great indication that the patient is free from disease and the treatment is successful."
Dr. Rudha and his coauthors stated that they had no disclosures.
PHOENIX – Routine use of positron emission tomography/computed tomography scans can detect locoregional recurrences of squamous cell carcinoma of the head and neck before they became clinically apparent, according to a retrospective chart review of 234 patients who had been treated with chemoradiation between 2006 and 2010.
The finding suggests that routine use of positron emission tomography/computed tomography (PET/CT) may improve the outcome of salvage therapy, said Dr. Yasir Rudha, who reported the study at the Multidisciplinary Head and Neck Symposium sponsored by the American Society for Radiation Oncology.
PET/CT was associated with a high false positive rate, which should be considered when ordering radiological exams and biopsies, but a negative posttherapy PET scan appears to be an excellent predictor of freedom from future locoregional recurrence, said Dr. Rudha of St. John Hospital/Van Elslander Cancer Center, Grosse Pointe Woods, Mich.
The technology is relatively new, and its use for routine follow-up in patients with head and neck cancer is still controversial, he acknowledged. "Only a few publications have reported the value of PET examination at a fixed time interval after the end of treatment," he said. "PET scan is often ordered in our hospital as a routine surveillance tool following successful completion of treatment."
The review of charts for all 234 patients identified 45 who had achieved clinical no-evidence-of-disease status at the time of posttreatment imaging. In this group, PET/CT scanning at 6-9 weeks identified 15 patients with abnormalities that required further evaluation. Of those, eight patients (53%) were proven to have malignancies based on biopsy findings: six showed occult persistent disease at the primary site, and two were diagnosed with regional lymph node recurrence and colon cancer, respectively.
In the remaining seven cases, imaging findings were shown to represent false positive results with unnecessary work-up and/or biopsy evaluation. All patients who had negative PET/CT scans remained free from locoregional relapse at the time of last follow-up.
Thus, Dr. Rudha said the true positive rate for routine PET/CT surveillance in head and neck cancer patients was estimated as 8/15, or 53%, and the false positive rate as 7/15, or 46%.
"With malignancies found in 53% of abnormal scans in this study, our research proves that PET/CT scans are valuable as routine follow-up and as a surveillance method for head and neck cancer patients ... However, since the rate of false positives was 46%, caution should be shown when ordering biopsies after abnormal scans to prevent excessive unnecessary biopsies," he said.
During a press briefing, Dr. Rudha said that the 46% false positive rate was lower than what he and his colleagues expected. "Actually we expected the false positive ratio to be about 90%," he said.
In an interview, he said that at his institution patients with positive PET/CT scans at 6-9 weeks postsurgery are followed in a variety of ways, depending primarily on the PET standard uptake volume (SUV). If low, the patient might undergo another PET scan at about 3 months. But if SUV is high, the patient would likely be referred for another test such as magnetic resonance imaging, ultrasound, or biopsy at the site of recurrence.
However, if the postsurgery PET/CT scan is negative, "according to this research, it gives a great indication that the patient is free from disease and the treatment is successful."
Dr. Rudha and his coauthors stated that they had no disclosures.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: The true positive rate for routine PET/CT surveillance in head and neck cancer patients was estimated as 8/15, or 53%, and the false positive rate as 7/15, or 46%.
Data Source: The data come from 45 patients with no evidence of disease after treatment with chemoradiation between 2006 and 2010.
Disclosures: Dr. Rudha and his coauthors reported having no disclosures.
Erlotinib Dose Doubled for Smokers With Head/Neck Cancer
PHOENIX – Giving smokers a higher, short-course dose of erlotinib before definitive surgery for squamous cell carcinoma of the head and neck resulted in favorable responses for the first patients evaluated in a small pilot study.
Investigators gave 300 mg of erlotinib (Tarceva) to smokers daily and 150 mg daily to nonsmokers who had a waiting period of more than 14 days before scheduled surgery for head and neck cancer. Seven of the 10 patients evaluated so far had partial responses and 3 had stable disease, according to a poster presented at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
The study was based on recent data in non–small cell lung cancer (NSCLC) patients showing that smokers metabolize erlotinib, an epidermal growth factor receptor (EGFR) inhibitor, twice as quickly as do nonsmokers (J. Clin. Oncol. 2009;27:1220-6), said lead author Dr. Mercedes Porosnicu of Wake Forest Baptist Medical Center in Winston Salem, N.C. That study established the maximum tolerated dose of erlotinib at 300 mg daily in NSCLC patients who smoke.
Dr. Poroniscu’s presentation included the case study of a smoker with a very large oral cavity tumor protruding through his lips. He was described as being in significant pain and unable to eat or chew. The first CT scan showed a tumor of at least 8 cm and there was "significant metabolic activity" on PET scan.
"At 6 days of erlotinib treatment, his tumor was obviously smaller and he could chew, eat, and talk. Metabolic activity on PET scan dropped to 44% compared to initial tumor metabolic activity," Dr. Porosnicu said. "At the end of 14 days’ treatment, his tumor was at least 20% smaller, and he had gained 5 pounds. His surgery wasn’t delayed, and the only treatment-related toxicity was a minimal skin rash."
A total of 12 patients have been treated to date, for an average of 18.2 days, she reported. Nine were smokers and three were nonsmokers. All patients, smokers and nonsmokers, tolerated the erlotinib dose well with no serious adverse events and no delays in the scheduled time of surgical intervention. There were no grade 3 or 4 toxicities.
Of 10 evaluable patients (including 8 smokers who received 300 mg), 7 (including 5 smokers) showed a partial response, as defined by at least a 20% reduction in maximum tumor diameter. The other three patients (all smokers) showed stable disease. Two of the 12 treated patients received shorter duration treatment but nonetheless displayed good responses.
Interestingly, all four treated female patients (including one smoker) had good responses, independent of the erlotinib dose received, Dr. Porosnicu said.
Early 18[F]-FDG PET scans taken 4-6 days after the start of neoadjuvant erlotinib showed a decrease in metabolic activity of 2% in maximum standardized uptake value (SUVmax) to 98.75% in patients with stable disease and a decrease to 48.06% in patients with partial response.
"Early changes in the PET scan uptake should be further investigated as a marker predictive of response to EGFR inhibition. This pilot trial will continue to enroll patients," Dr. Porosnicu said.
Erlotinib is approved for indications in non–small cell lung cancer and pancreatic cancer. Head and neck cancer would be an off-label use.
Dr. Porosnicu disclosed that she received financial support for this study from Astellas Pharma.
PHOENIX – Giving smokers a higher, short-course dose of erlotinib before definitive surgery for squamous cell carcinoma of the head and neck resulted in favorable responses for the first patients evaluated in a small pilot study.
Investigators gave 300 mg of erlotinib (Tarceva) to smokers daily and 150 mg daily to nonsmokers who had a waiting period of more than 14 days before scheduled surgery for head and neck cancer. Seven of the 10 patients evaluated so far had partial responses and 3 had stable disease, according to a poster presented at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
The study was based on recent data in non–small cell lung cancer (NSCLC) patients showing that smokers metabolize erlotinib, an epidermal growth factor receptor (EGFR) inhibitor, twice as quickly as do nonsmokers (J. Clin. Oncol. 2009;27:1220-6), said lead author Dr. Mercedes Porosnicu of Wake Forest Baptist Medical Center in Winston Salem, N.C. That study established the maximum tolerated dose of erlotinib at 300 mg daily in NSCLC patients who smoke.
Dr. Poroniscu’s presentation included the case study of a smoker with a very large oral cavity tumor protruding through his lips. He was described as being in significant pain and unable to eat or chew. The first CT scan showed a tumor of at least 8 cm and there was "significant metabolic activity" on PET scan.
"At 6 days of erlotinib treatment, his tumor was obviously smaller and he could chew, eat, and talk. Metabolic activity on PET scan dropped to 44% compared to initial tumor metabolic activity," Dr. Porosnicu said. "At the end of 14 days’ treatment, his tumor was at least 20% smaller, and he had gained 5 pounds. His surgery wasn’t delayed, and the only treatment-related toxicity was a minimal skin rash."
A total of 12 patients have been treated to date, for an average of 18.2 days, she reported. Nine were smokers and three were nonsmokers. All patients, smokers and nonsmokers, tolerated the erlotinib dose well with no serious adverse events and no delays in the scheduled time of surgical intervention. There were no grade 3 or 4 toxicities.
Of 10 evaluable patients (including 8 smokers who received 300 mg), 7 (including 5 smokers) showed a partial response, as defined by at least a 20% reduction in maximum tumor diameter. The other three patients (all smokers) showed stable disease. Two of the 12 treated patients received shorter duration treatment but nonetheless displayed good responses.
Interestingly, all four treated female patients (including one smoker) had good responses, independent of the erlotinib dose received, Dr. Porosnicu said.
Early 18[F]-FDG PET scans taken 4-6 days after the start of neoadjuvant erlotinib showed a decrease in metabolic activity of 2% in maximum standardized uptake value (SUVmax) to 98.75% in patients with stable disease and a decrease to 48.06% in patients with partial response.
"Early changes in the PET scan uptake should be further investigated as a marker predictive of response to EGFR inhibition. This pilot trial will continue to enroll patients," Dr. Porosnicu said.
Erlotinib is approved for indications in non–small cell lung cancer and pancreatic cancer. Head and neck cancer would be an off-label use.
Dr. Porosnicu disclosed that she received financial support for this study from Astellas Pharma.
PHOENIX – Giving smokers a higher, short-course dose of erlotinib before definitive surgery for squamous cell carcinoma of the head and neck resulted in favorable responses for the first patients evaluated in a small pilot study.
Investigators gave 300 mg of erlotinib (Tarceva) to smokers daily and 150 mg daily to nonsmokers who had a waiting period of more than 14 days before scheduled surgery for head and neck cancer. Seven of the 10 patients evaluated so far had partial responses and 3 had stable disease, according to a poster presented at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
The study was based on recent data in non–small cell lung cancer (NSCLC) patients showing that smokers metabolize erlotinib, an epidermal growth factor receptor (EGFR) inhibitor, twice as quickly as do nonsmokers (J. Clin. Oncol. 2009;27:1220-6), said lead author Dr. Mercedes Porosnicu of Wake Forest Baptist Medical Center in Winston Salem, N.C. That study established the maximum tolerated dose of erlotinib at 300 mg daily in NSCLC patients who smoke.
Dr. Poroniscu’s presentation included the case study of a smoker with a very large oral cavity tumor protruding through his lips. He was described as being in significant pain and unable to eat or chew. The first CT scan showed a tumor of at least 8 cm and there was "significant metabolic activity" on PET scan.
"At 6 days of erlotinib treatment, his tumor was obviously smaller and he could chew, eat, and talk. Metabolic activity on PET scan dropped to 44% compared to initial tumor metabolic activity," Dr. Porosnicu said. "At the end of 14 days’ treatment, his tumor was at least 20% smaller, and he had gained 5 pounds. His surgery wasn’t delayed, and the only treatment-related toxicity was a minimal skin rash."
A total of 12 patients have been treated to date, for an average of 18.2 days, she reported. Nine were smokers and three were nonsmokers. All patients, smokers and nonsmokers, tolerated the erlotinib dose well with no serious adverse events and no delays in the scheduled time of surgical intervention. There were no grade 3 or 4 toxicities.
Of 10 evaluable patients (including 8 smokers who received 300 mg), 7 (including 5 smokers) showed a partial response, as defined by at least a 20% reduction in maximum tumor diameter. The other three patients (all smokers) showed stable disease. Two of the 12 treated patients received shorter duration treatment but nonetheless displayed good responses.
Interestingly, all four treated female patients (including one smoker) had good responses, independent of the erlotinib dose received, Dr. Porosnicu said.
Early 18[F]-FDG PET scans taken 4-6 days after the start of neoadjuvant erlotinib showed a decrease in metabolic activity of 2% in maximum standardized uptake value (SUVmax) to 98.75% in patients with stable disease and a decrease to 48.06% in patients with partial response.
"Early changes in the PET scan uptake should be further investigated as a marker predictive of response to EGFR inhibition. This pilot trial will continue to enroll patients," Dr. Porosnicu said.
Erlotinib is approved for indications in non–small cell lung cancer and pancreatic cancer. Head and neck cancer would be an off-label use.
Dr. Porosnicu disclosed that she received financial support for this study from Astellas Pharma.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: Of 10 evaluable head and neck cancer patients, 7 (including 5 smokers) showed a partial response, as defined by at least a 20% reduction in maximum tumor diameter.
Data Source: In this small, ongoing pilot study smokers received 300 mg and nonsmokers 150 mg daily of neoadjuvant erlotinib.
Disclosures: Dr. Porosnicu disclosed that she received financial support for this study from Astellas Pharma.
Head/Neck Cancer Treatments Less Effective in HIV Patients
PHOENIX – Definitive radiation therapy with or without chemotherapy was less tolerated and less effective in HIV-positive patients with head and neck squamous cell carcinoma than in HIV-negative patients in a single-institution retrospective study of 71 HIV-positive patients.
"Head and neck squamous cell carcinoma with coexisting HIV remains a challenging clinical problem. ... Due to the advances in highly active antiretroviral therapy (HAART) – which prolongs HIV patients’ survival – the likelihood to develop HIV-related malignancy increases. It is of paramount importance to establish better-tolerated treatment strategies and regimens to improve tolerance, toxicity, and outcomes in this growing patient population," said Dr. Waleed Mourad, a radiation oncologist at Beth Israel Medical Center, New York.
The 71 HIV-positive patients with HNSCC were treated January 1997 through 2010. They had a median age of 34 years at the time of HIV diagnosis (range 25-50 years) with a median 11 years’ duration of seropositivity (6-20 years). Their median age at the time of radiation therapy was 51 years (32-72 years). All but one patient had squamous cell carcinoma, with the other having submandibular salivary duct carcinoma. That patient was treated with definitive surgery and received adjuvant radiation therapy without chemotherapy, Dr. Mourad noted.
Approximately one-third of the patients had cancer of the oropharynx (32%) and larynx (35%), and another 13% had cancer of the oral cavity. Other cancers among the patients included those located in the hypopharynx, nasopharynx, occult primary, and nasal cavity. American Joint Committee on Cancer 7th edition stages I-II, III and IVa/b were 22%, 27%, 51% respectively.
All patients were treated definitively with radiation therapy, with or without chemotherapy (cisplatin, carboplatin, or cetuximab). A total of 50 patients (70%) were on HAART during treatment, with a median CD4 count of 290 (range, 203-1,142). A median dose of 70 Gy (66-70) was delivered to the gross disease; high-risk neck 60-63 Gy; low-risk neck; and lateral retropharyngeal nodes 54 Gy. All fractions were given at the rate of 1.8-2 Gy/fraction. The median duration of treatment was 52 (49-64) days. A total of 12 patients (17%) underwent planned neck dissection for N3 disease.
In all, local control was achieved in 69% (49) and locoregional failure occurred in 31% (22). By site, local control rates were 70% (16) for the oropharynx, 76% (19) for the larynx, 78% (7) for the oral cavity, 0% (of 5) for hypopharynx, 67% (2) for the nasopharynx, 100% (3) for occult primary, 50% (1) for the nasal cavity, and 100% (1) for the submandibular duct.
Thus, locoregional failure rates ranged from 100% (all five patients with hypopharyngeal cancer) to 0 (for the three patients with occult primary cancer and the one with submandibular duct cancer). Seven patients developed second primary cancers, Dr. Mourad reported.
After a median follow up of 47 months (7-140), there were no fatalities related to radiation or chemotherapy. Treatment breaks in excess of 10, 7, and 5 days occurred in 6%, 13%, and 14% of patients, respectively. Acute dysphagia and odynophagia grades 1, 2, and 3 occurred in 31%, 52%, and 17%, respectively. All of the patients experienced dysgeusia, dysphagia, and xerostomia of grades 1-3. Acute desquamation of the skin of grades 1, 2, and 3 occurred in 66%, 20%, and 14%.
One patient was hospitalized for grade 4 mucositis, dysphagia, and fever. Another developed osteoradionecrosis during concurrent chemoradiotherapy. Late dysphagia of grades 1-4 occurred in 46%, 28%, 15%, and 11%. Xerostomia of grades 1-3 occurred in 45%, 32%, and 23%, respectively, he said.
At 4 years, locoregional control was 69% and overall survival 55%. In an interview, Dr. Mourad noted that at his institution, the comparable rates for non-HIV patients were 85%-90% and 75%-85%, respectively.
The median CD4 count prior to chemotherapy was 370, and viral load was undetectable. The CD4 count dropped as chemoradiotherapy progressed to a nadir at 11 weeks, at which point it began to rise again and viral load decreased.
There was a statistically significant relationship between locoregional control and the duration of radiation therapy (P less than .001), and positive trends with weight loss of greater than 10% and absence of second malignancy. However, multivariate analysis did not show any statistically significant relationship because of the relatively small sample size with diverse subsites, Dr. Mourad noted.
"We believe that our data provide important information regarding treatment outcomes for newly diagnosed head and neck cancer with HIV. This is particularly important given the growing population of patients who live with HIV long term because of effective antiretroviral maintenance treatments," Dr. Mourad said in an interview.
Dr. Mourad and his nine coauthors declared that they had no financial disclosures.
PHOENIX – Definitive radiation therapy with or without chemotherapy was less tolerated and less effective in HIV-positive patients with head and neck squamous cell carcinoma than in HIV-negative patients in a single-institution retrospective study of 71 HIV-positive patients.
"Head and neck squamous cell carcinoma with coexisting HIV remains a challenging clinical problem. ... Due to the advances in highly active antiretroviral therapy (HAART) – which prolongs HIV patients’ survival – the likelihood to develop HIV-related malignancy increases. It is of paramount importance to establish better-tolerated treatment strategies and regimens to improve tolerance, toxicity, and outcomes in this growing patient population," said Dr. Waleed Mourad, a radiation oncologist at Beth Israel Medical Center, New York.
The 71 HIV-positive patients with HNSCC were treated January 1997 through 2010. They had a median age of 34 years at the time of HIV diagnosis (range 25-50 years) with a median 11 years’ duration of seropositivity (6-20 years). Their median age at the time of radiation therapy was 51 years (32-72 years). All but one patient had squamous cell carcinoma, with the other having submandibular salivary duct carcinoma. That patient was treated with definitive surgery and received adjuvant radiation therapy without chemotherapy, Dr. Mourad noted.
Approximately one-third of the patients had cancer of the oropharynx (32%) and larynx (35%), and another 13% had cancer of the oral cavity. Other cancers among the patients included those located in the hypopharynx, nasopharynx, occult primary, and nasal cavity. American Joint Committee on Cancer 7th edition stages I-II, III and IVa/b were 22%, 27%, 51% respectively.
All patients were treated definitively with radiation therapy, with or without chemotherapy (cisplatin, carboplatin, or cetuximab). A total of 50 patients (70%) were on HAART during treatment, with a median CD4 count of 290 (range, 203-1,142). A median dose of 70 Gy (66-70) was delivered to the gross disease; high-risk neck 60-63 Gy; low-risk neck; and lateral retropharyngeal nodes 54 Gy. All fractions were given at the rate of 1.8-2 Gy/fraction. The median duration of treatment was 52 (49-64) days. A total of 12 patients (17%) underwent planned neck dissection for N3 disease.
In all, local control was achieved in 69% (49) and locoregional failure occurred in 31% (22). By site, local control rates were 70% (16) for the oropharynx, 76% (19) for the larynx, 78% (7) for the oral cavity, 0% (of 5) for hypopharynx, 67% (2) for the nasopharynx, 100% (3) for occult primary, 50% (1) for the nasal cavity, and 100% (1) for the submandibular duct.
Thus, locoregional failure rates ranged from 100% (all five patients with hypopharyngeal cancer) to 0 (for the three patients with occult primary cancer and the one with submandibular duct cancer). Seven patients developed second primary cancers, Dr. Mourad reported.
After a median follow up of 47 months (7-140), there were no fatalities related to radiation or chemotherapy. Treatment breaks in excess of 10, 7, and 5 days occurred in 6%, 13%, and 14% of patients, respectively. Acute dysphagia and odynophagia grades 1, 2, and 3 occurred in 31%, 52%, and 17%, respectively. All of the patients experienced dysgeusia, dysphagia, and xerostomia of grades 1-3. Acute desquamation of the skin of grades 1, 2, and 3 occurred in 66%, 20%, and 14%.
One patient was hospitalized for grade 4 mucositis, dysphagia, and fever. Another developed osteoradionecrosis during concurrent chemoradiotherapy. Late dysphagia of grades 1-4 occurred in 46%, 28%, 15%, and 11%. Xerostomia of grades 1-3 occurred in 45%, 32%, and 23%, respectively, he said.
At 4 years, locoregional control was 69% and overall survival 55%. In an interview, Dr. Mourad noted that at his institution, the comparable rates for non-HIV patients were 85%-90% and 75%-85%, respectively.
The median CD4 count prior to chemotherapy was 370, and viral load was undetectable. The CD4 count dropped as chemoradiotherapy progressed to a nadir at 11 weeks, at which point it began to rise again and viral load decreased.
There was a statistically significant relationship between locoregional control and the duration of radiation therapy (P less than .001), and positive trends with weight loss of greater than 10% and absence of second malignancy. However, multivariate analysis did not show any statistically significant relationship because of the relatively small sample size with diverse subsites, Dr. Mourad noted.
"We believe that our data provide important information regarding treatment outcomes for newly diagnosed head and neck cancer with HIV. This is particularly important given the growing population of patients who live with HIV long term because of effective antiretroviral maintenance treatments," Dr. Mourad said in an interview.
Dr. Mourad and his nine coauthors declared that they had no financial disclosures.
PHOENIX – Definitive radiation therapy with or without chemotherapy was less tolerated and less effective in HIV-positive patients with head and neck squamous cell carcinoma than in HIV-negative patients in a single-institution retrospective study of 71 HIV-positive patients.
"Head and neck squamous cell carcinoma with coexisting HIV remains a challenging clinical problem. ... Due to the advances in highly active antiretroviral therapy (HAART) – which prolongs HIV patients’ survival – the likelihood to develop HIV-related malignancy increases. It is of paramount importance to establish better-tolerated treatment strategies and regimens to improve tolerance, toxicity, and outcomes in this growing patient population," said Dr. Waleed Mourad, a radiation oncologist at Beth Israel Medical Center, New York.
The 71 HIV-positive patients with HNSCC were treated January 1997 through 2010. They had a median age of 34 years at the time of HIV diagnosis (range 25-50 years) with a median 11 years’ duration of seropositivity (6-20 years). Their median age at the time of radiation therapy was 51 years (32-72 years). All but one patient had squamous cell carcinoma, with the other having submandibular salivary duct carcinoma. That patient was treated with definitive surgery and received adjuvant radiation therapy without chemotherapy, Dr. Mourad noted.
Approximately one-third of the patients had cancer of the oropharynx (32%) and larynx (35%), and another 13% had cancer of the oral cavity. Other cancers among the patients included those located in the hypopharynx, nasopharynx, occult primary, and nasal cavity. American Joint Committee on Cancer 7th edition stages I-II, III and IVa/b were 22%, 27%, 51% respectively.
All patients were treated definitively with radiation therapy, with or without chemotherapy (cisplatin, carboplatin, or cetuximab). A total of 50 patients (70%) were on HAART during treatment, with a median CD4 count of 290 (range, 203-1,142). A median dose of 70 Gy (66-70) was delivered to the gross disease; high-risk neck 60-63 Gy; low-risk neck; and lateral retropharyngeal nodes 54 Gy. All fractions were given at the rate of 1.8-2 Gy/fraction. The median duration of treatment was 52 (49-64) days. A total of 12 patients (17%) underwent planned neck dissection for N3 disease.
In all, local control was achieved in 69% (49) and locoregional failure occurred in 31% (22). By site, local control rates were 70% (16) for the oropharynx, 76% (19) for the larynx, 78% (7) for the oral cavity, 0% (of 5) for hypopharynx, 67% (2) for the nasopharynx, 100% (3) for occult primary, 50% (1) for the nasal cavity, and 100% (1) for the submandibular duct.
Thus, locoregional failure rates ranged from 100% (all five patients with hypopharyngeal cancer) to 0 (for the three patients with occult primary cancer and the one with submandibular duct cancer). Seven patients developed second primary cancers, Dr. Mourad reported.
After a median follow up of 47 months (7-140), there were no fatalities related to radiation or chemotherapy. Treatment breaks in excess of 10, 7, and 5 days occurred in 6%, 13%, and 14% of patients, respectively. Acute dysphagia and odynophagia grades 1, 2, and 3 occurred in 31%, 52%, and 17%, respectively. All of the patients experienced dysgeusia, dysphagia, and xerostomia of grades 1-3. Acute desquamation of the skin of grades 1, 2, and 3 occurred in 66%, 20%, and 14%.
One patient was hospitalized for grade 4 mucositis, dysphagia, and fever. Another developed osteoradionecrosis during concurrent chemoradiotherapy. Late dysphagia of grades 1-4 occurred in 46%, 28%, 15%, and 11%. Xerostomia of grades 1-3 occurred in 45%, 32%, and 23%, respectively, he said.
At 4 years, locoregional control was 69% and overall survival 55%. In an interview, Dr. Mourad noted that at his institution, the comparable rates for non-HIV patients were 85%-90% and 75%-85%, respectively.
The median CD4 count prior to chemotherapy was 370, and viral load was undetectable. The CD4 count dropped as chemoradiotherapy progressed to a nadir at 11 weeks, at which point it began to rise again and viral load decreased.
There was a statistically significant relationship between locoregional control and the duration of radiation therapy (P less than .001), and positive trends with weight loss of greater than 10% and absence of second malignancy. However, multivariate analysis did not show any statistically significant relationship because of the relatively small sample size with diverse subsites, Dr. Mourad noted.
"We believe that our data provide important information regarding treatment outcomes for newly diagnosed head and neck cancer with HIV. This is particularly important given the growing population of patients who live with HIV long term because of effective antiretroviral maintenance treatments," Dr. Mourad said in an interview.
Dr. Mourad and his nine coauthors declared that they had no financial disclosures.
FROM A HEAD AND NECK CANCER SYMPOSIUM BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: At 4 years, locoregional control was 69% and overall survival 55%.
Data Source: The findings come from a single-institution retrospective study of 71 HIV-positive patients with head and neck squamous cell carcinoma.
Disclosures: Dr. Mourad and his nine coauthors declared that they had no financial disclosures.