User login
The AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies took place September 20-23, 2014, in Philadelphia, Pennsylvania.
Targeting drug resistance earlier

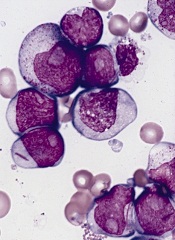
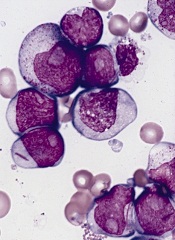
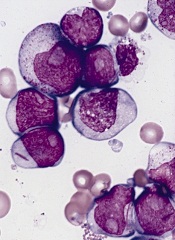
Credit: PNAS
PHILADELPHIA—A combination treatment strategy that takes tumor evolution into account could help us avoid drug resistance in hematologic malignancies, researchers say.
Preclinical experiments suggest we can prevent resistance by starting secondary treatment prior to relapse.
For example, a patient receiving dasatinib for acute lymphoblastic leukemia (ALL) could benefit from receiving crizotinib or foretinib during the early stages of clonal evolution.
The researchers described this strategy in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“Our goal is to identify vulnerabilities in cancer across stages of tumor evolution while it is developing resistance to initial treatment, to help guide the design of drug combination strategies,” said Douglas Lauffenburger, PhD, of the Koch Institute for Integrative Cancer Research at MIT in Boston.
“There may be many stages in a tumor evolution while under treatment that may make them vulnerable to already existing therapies. Rather than waiting for the tumor to become resistant to the first treatment and then thinking about a second-line drug to use, we can capitalize on opportunities that exploit vulnerabilities at different early stages, as the tumor is evolving to become resistant to the first drug.”
Dr Lauffenburger and his colleagues used a combination of computational and experimental approaches to identify drugs likely to be effective against a murine ALL cell line as the cells evolve.
To develop drug combinations based on the characteristics of evolving tumors, the researchers used escalating doses of imatinib, dasatinib, nilotinib, foretinib, and crizotinib on ALL cells.
As some cells exhibited resistance to a particular drug, the team treated the resistant cells with other drugs to check for cross-resistance. They found that resistant cells surviving at low multiples of the original drug dose actually demonstrated sensitization to certain other drugs, with the sensitization abrogated at higher doses.
Specifically, cell populations that were resistant to dasatinib at 1x and 2x IC90 became even more sensitive to crizotinib and foretinib. However, the sensitivity was lost at IC90 4x and above.
“Instead of only looking for the most resistant population of ALL cells at the end of this selection process, we monitored for drug sensitivity of the cells at each stage of the dose escalation,” Dr Lauffenburger explained.
“This led us to discover the vulnerabilities of a tumor at different stages of clonal evolution, a phenomenon we would have missed if we only analyzed for drug sensitivity at the last stage of this process, which is equivalent to when a patient has relapsed.” ![]()

Credit: PNAS
PHILADELPHIA—A combination treatment strategy that takes tumor evolution into account could help us avoid drug resistance in hematologic malignancies, researchers say.
Preclinical experiments suggest we can prevent resistance by starting secondary treatment prior to relapse.
For example, a patient receiving dasatinib for acute lymphoblastic leukemia (ALL) could benefit from receiving crizotinib or foretinib during the early stages of clonal evolution.
The researchers described this strategy in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“Our goal is to identify vulnerabilities in cancer across stages of tumor evolution while it is developing resistance to initial treatment, to help guide the design of drug combination strategies,” said Douglas Lauffenburger, PhD, of the Koch Institute for Integrative Cancer Research at MIT in Boston.
“There may be many stages in a tumor evolution while under treatment that may make them vulnerable to already existing therapies. Rather than waiting for the tumor to become resistant to the first treatment and then thinking about a second-line drug to use, we can capitalize on opportunities that exploit vulnerabilities at different early stages, as the tumor is evolving to become resistant to the first drug.”
Dr Lauffenburger and his colleagues used a combination of computational and experimental approaches to identify drugs likely to be effective against a murine ALL cell line as the cells evolve.
To develop drug combinations based on the characteristics of evolving tumors, the researchers used escalating doses of imatinib, dasatinib, nilotinib, foretinib, and crizotinib on ALL cells.
As some cells exhibited resistance to a particular drug, the team treated the resistant cells with other drugs to check for cross-resistance. They found that resistant cells surviving at low multiples of the original drug dose actually demonstrated sensitization to certain other drugs, with the sensitization abrogated at higher doses.
Specifically, cell populations that were resistant to dasatinib at 1x and 2x IC90 became even more sensitive to crizotinib and foretinib. However, the sensitivity was lost at IC90 4x and above.
“Instead of only looking for the most resistant population of ALL cells at the end of this selection process, we monitored for drug sensitivity of the cells at each stage of the dose escalation,” Dr Lauffenburger explained.
“This led us to discover the vulnerabilities of a tumor at different stages of clonal evolution, a phenomenon we would have missed if we only analyzed for drug sensitivity at the last stage of this process, which is equivalent to when a patient has relapsed.” ![]()

Credit: PNAS
PHILADELPHIA—A combination treatment strategy that takes tumor evolution into account could help us avoid drug resistance in hematologic malignancies, researchers say.
Preclinical experiments suggest we can prevent resistance by starting secondary treatment prior to relapse.
For example, a patient receiving dasatinib for acute lymphoblastic leukemia (ALL) could benefit from receiving crizotinib or foretinib during the early stages of clonal evolution.
The researchers described this strategy in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“Our goal is to identify vulnerabilities in cancer across stages of tumor evolution while it is developing resistance to initial treatment, to help guide the design of drug combination strategies,” said Douglas Lauffenburger, PhD, of the Koch Institute for Integrative Cancer Research at MIT in Boston.
“There may be many stages in a tumor evolution while under treatment that may make them vulnerable to already existing therapies. Rather than waiting for the tumor to become resistant to the first treatment and then thinking about a second-line drug to use, we can capitalize on opportunities that exploit vulnerabilities at different early stages, as the tumor is evolving to become resistant to the first drug.”
Dr Lauffenburger and his colleagues used a combination of computational and experimental approaches to identify drugs likely to be effective against a murine ALL cell line as the cells evolve.
To develop drug combinations based on the characteristics of evolving tumors, the researchers used escalating doses of imatinib, dasatinib, nilotinib, foretinib, and crizotinib on ALL cells.
As some cells exhibited resistance to a particular drug, the team treated the resistant cells with other drugs to check for cross-resistance. They found that resistant cells surviving at low multiples of the original drug dose actually demonstrated sensitization to certain other drugs, with the sensitization abrogated at higher doses.
Specifically, cell populations that were resistant to dasatinib at 1x and 2x IC90 became even more sensitive to crizotinib and foretinib. However, the sensitivity was lost at IC90 4x and above.
“Instead of only looking for the most resistant population of ALL cells at the end of this selection process, we monitored for drug sensitivity of the cells at each stage of the dose escalation,” Dr Lauffenburger explained.
“This led us to discover the vulnerabilities of a tumor at different stages of clonal evolution, a phenomenon we would have missed if we only analyzed for drug sensitivity at the last stage of this process, which is equivalent to when a patient has relapsed.” ![]()
Drug could treat a range of blood cancers

PHILADELPHIA—A drug that targets the ribosome may be active in a broad range of hematologic malignancies, researchers say.
The drug, CX-5461, inhibits the protein RNA polymerase I (Pol I), which is consistently upregulated in hematologic and other cancers.
CX-5461 significantly prolonged survival in mouse models of refractory acute myeloid leukemia (AML) and multiple myeloma (MM). It also synergized with everolimus to extend survival in mice with B-cell lymphoma.
Furthermore, the drug did not elicit severe adverse effects.
“We were excited to find that therapeutic doses of CX-5461 had little effect on normal cells in our experiments,” said Ross D. Hannan, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia,
“Prior to these studies, few people would have guessed that such a therapeutic window could be obtained by targeting a so-called house-keeping protein that is essential to all cells for survival.”
Dr Hannan and his colleagues presented these findings in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The researchers previously showed that cancer cells are much more dependent on ribosome biogenesis than normal cells. And blocking the accelerated reading of ribosomal genes in mice—using CX5461—can cause lymphoma and leukemia cells to die, while sparing normal cells.
With their latest research, the group expanded upon these findings by testing CX-5461 in MLL-driven AML, V*κ-Myc-driven MM, and Eμ-Myc lymphoma.
They found that CX-5461 improved overall survival in MLL/ENL Nras leukemic mice, compared to placebo and standard therapy. The median survival was 17 days for vehicle-treated mice, 21 days for mice treated with cytarabine and doxorubicin, and 36 days for mice that received CX-5461 (P<0.0001 for vehicle vs CX-5461).
CX-5461 treated MLL-driven AML by inducing apoptosis, delaying cell-cycle progression, and promoting differentiation.
The researchers also found the therapeutic benefit of CX-5461 is not p53-dependent, which contradicts their previous findings. Human AML cell lines and primary patient samples were sensitive to CX-5461 independent of p53 status.
And MLL/ENL Nras p53-/- leukemic mice had significantly prolonged survival when treated with CX-5461, compared to vehicle-treated controls. The median survival was 11 days and 24 days, respectively (P<0.0001).
Likewise, CX-5461 significantly prolonged survival in mice bearing V*κ-Myc MM. The median survival was 103.5 days for controls and 175 days for mice that received CX-5461 (P<0.0001).
Finally, the researchers showed that CX-5461 synergizes with everolimus to treat Eμ-Myc lymphoma. The median survival was 15 days in control mice, 18 days in mice that received everolimus, 32 days in mice treated with CX-5461, and 54 days in mice that received both drugs (P<0.0001 for CX-5461 vs the combination).
“These results provide further rationale for the first-in-human phase 1 clinical trial that we initiated in July 2013 testing CX-5461 for patients with advanced hematological malignancies, including AML and multiple myeloma,” Dr Hannan said.
His group’s preclinical research was funded by the National Health and Medical Research Council, Australia; the Leukaemia Foundation of Australia; and Cancer Council Victoria, Melbourne, Australia. Senhwa Biosciences, the makers of CX-5461, provided the drug. ![]()

PHILADELPHIA—A drug that targets the ribosome may be active in a broad range of hematologic malignancies, researchers say.
The drug, CX-5461, inhibits the protein RNA polymerase I (Pol I), which is consistently upregulated in hematologic and other cancers.
CX-5461 significantly prolonged survival in mouse models of refractory acute myeloid leukemia (AML) and multiple myeloma (MM). It also synergized with everolimus to extend survival in mice with B-cell lymphoma.
Furthermore, the drug did not elicit severe adverse effects.
“We were excited to find that therapeutic doses of CX-5461 had little effect on normal cells in our experiments,” said Ross D. Hannan, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia,
“Prior to these studies, few people would have guessed that such a therapeutic window could be obtained by targeting a so-called house-keeping protein that is essential to all cells for survival.”
Dr Hannan and his colleagues presented these findings in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The researchers previously showed that cancer cells are much more dependent on ribosome biogenesis than normal cells. And blocking the accelerated reading of ribosomal genes in mice—using CX5461—can cause lymphoma and leukemia cells to die, while sparing normal cells.
With their latest research, the group expanded upon these findings by testing CX-5461 in MLL-driven AML, V*κ-Myc-driven MM, and Eμ-Myc lymphoma.
They found that CX-5461 improved overall survival in MLL/ENL Nras leukemic mice, compared to placebo and standard therapy. The median survival was 17 days for vehicle-treated mice, 21 days for mice treated with cytarabine and doxorubicin, and 36 days for mice that received CX-5461 (P<0.0001 for vehicle vs CX-5461).
CX-5461 treated MLL-driven AML by inducing apoptosis, delaying cell-cycle progression, and promoting differentiation.
The researchers also found the therapeutic benefit of CX-5461 is not p53-dependent, which contradicts their previous findings. Human AML cell lines and primary patient samples were sensitive to CX-5461 independent of p53 status.
And MLL/ENL Nras p53-/- leukemic mice had significantly prolonged survival when treated with CX-5461, compared to vehicle-treated controls. The median survival was 11 days and 24 days, respectively (P<0.0001).
Likewise, CX-5461 significantly prolonged survival in mice bearing V*κ-Myc MM. The median survival was 103.5 days for controls and 175 days for mice that received CX-5461 (P<0.0001).
Finally, the researchers showed that CX-5461 synergizes with everolimus to treat Eμ-Myc lymphoma. The median survival was 15 days in control mice, 18 days in mice that received everolimus, 32 days in mice treated with CX-5461, and 54 days in mice that received both drugs (P<0.0001 for CX-5461 vs the combination).
“These results provide further rationale for the first-in-human phase 1 clinical trial that we initiated in July 2013 testing CX-5461 for patients with advanced hematological malignancies, including AML and multiple myeloma,” Dr Hannan said.
His group’s preclinical research was funded by the National Health and Medical Research Council, Australia; the Leukaemia Foundation of Australia; and Cancer Council Victoria, Melbourne, Australia. Senhwa Biosciences, the makers of CX-5461, provided the drug. ![]()

PHILADELPHIA—A drug that targets the ribosome may be active in a broad range of hematologic malignancies, researchers say.
The drug, CX-5461, inhibits the protein RNA polymerase I (Pol I), which is consistently upregulated in hematologic and other cancers.
CX-5461 significantly prolonged survival in mouse models of refractory acute myeloid leukemia (AML) and multiple myeloma (MM). It also synergized with everolimus to extend survival in mice with B-cell lymphoma.
Furthermore, the drug did not elicit severe adverse effects.
“We were excited to find that therapeutic doses of CX-5461 had little effect on normal cells in our experiments,” said Ross D. Hannan, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia,
“Prior to these studies, few people would have guessed that such a therapeutic window could be obtained by targeting a so-called house-keeping protein that is essential to all cells for survival.”
Dr Hannan and his colleagues presented these findings in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The researchers previously showed that cancer cells are much more dependent on ribosome biogenesis than normal cells. And blocking the accelerated reading of ribosomal genes in mice—using CX5461—can cause lymphoma and leukemia cells to die, while sparing normal cells.
With their latest research, the group expanded upon these findings by testing CX-5461 in MLL-driven AML, V*κ-Myc-driven MM, and Eμ-Myc lymphoma.
They found that CX-5461 improved overall survival in MLL/ENL Nras leukemic mice, compared to placebo and standard therapy. The median survival was 17 days for vehicle-treated mice, 21 days for mice treated with cytarabine and doxorubicin, and 36 days for mice that received CX-5461 (P<0.0001 for vehicle vs CX-5461).
CX-5461 treated MLL-driven AML by inducing apoptosis, delaying cell-cycle progression, and promoting differentiation.
The researchers also found the therapeutic benefit of CX-5461 is not p53-dependent, which contradicts their previous findings. Human AML cell lines and primary patient samples were sensitive to CX-5461 independent of p53 status.
And MLL/ENL Nras p53-/- leukemic mice had significantly prolonged survival when treated with CX-5461, compared to vehicle-treated controls. The median survival was 11 days and 24 days, respectively (P<0.0001).
Likewise, CX-5461 significantly prolonged survival in mice bearing V*κ-Myc MM. The median survival was 103.5 days for controls and 175 days for mice that received CX-5461 (P<0.0001).
Finally, the researchers showed that CX-5461 synergizes with everolimus to treat Eμ-Myc lymphoma. The median survival was 15 days in control mice, 18 days in mice that received everolimus, 32 days in mice treated with CX-5461, and 54 days in mice that received both drugs (P<0.0001 for CX-5461 vs the combination).
“These results provide further rationale for the first-in-human phase 1 clinical trial that we initiated in July 2013 testing CX-5461 for patients with advanced hematological malignancies, including AML and multiple myeloma,” Dr Hannan said.
His group’s preclinical research was funded by the National Health and Medical Research Council, Australia; the Leukaemia Foundation of Australia; and Cancer Council Victoria, Melbourne, Australia. Senhwa Biosciences, the makers of CX-5461, provided the drug. ![]()
Method can detect drivers of AML
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.” ![]()
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.” ![]()
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.” ![]()
Murine studies support use of TKIs in ALL subtype

PHILADELPHIA—Experiments in mice reinforce the idea that tyrosine kinase inhibitors (TKIs) can treat patients with Ph-like acute lymphoblastic leukemia (ALL).
Investigators recently identified genomic alterations in Ph-like ALL that suggest these patients might respond to TKIs, and tests in a small number of patients supported this theory.
Now, preclinical results show that kinase fusions in Ph-like ALL activate signaling pathways differently, and this affects sensitivity to TKIs.
Kathryn Roberts, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues presented these results at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We recently described a subtype of B-cell acute lymphoblastic leukemia with very poor outcome that is characterized by genetic alterations involving tyrosine kinases, termed Ph-like ALL,” Dr Roberts said. “We wanted to examine whether these alterations contribute to the development of Ph-like ALL and determine if they could be targeted with tyrosine kinase inhibitors.”
“We showed, for the first time, that the kinase alterations we tested contribute to the development of Ph-like ALL, and that Ph-like ALL can be treated effectively with tyrosine kinase inhibitors in animal models. These findings provide a strong rationale for treating Ph-like ALL patients with targeted therapies to improve their survival.”
Dr Roberts and her colleagues first introduced kinase alterations—RCSD1-ABL2, SSBP2-CSF1R, or PAX5-JAK2—in IL-7-dependent, Arf-/- mouse pre-B cells expressing IK6.
They found that each fusion conferred cytokine-independent growth in vitro. And mice that received transplants of pre-B cells expressing RCSD1-ABL2 or SSBP2-CSF1R developed ALL with a pre-B immunophenotype.
The investigators then assessed the activation of kinase signaling pathways and TKI sensitivity in Arf-/- pre-B cells and human leukemic cells harvested from xenografted mice expressing ETV6-ABL1, RANBP2-ABL1, PAG1-ABL2, RCSD1-ABL2, SSBP2-CSF1R, IGH-EPOR, ATF7IP-JAK2, and PAX5-JAK2.
In both cell types, signaling pathway activation and TKI sensitivity differed according to the kinase fusion.
Cells expressing ABL1-class kinase fusions (ABL1, ABL2, CSF1R, and PDGFRB) exhibited pSTAT5 activation that was inhibited by imatinib or dasatinib. But in cells expressing ATF7IP-JAK2, PAX5-JAK2, or IGH-EPOR, pSTAT5 activation was only inhibited by ruxolitinib.
Finally, the investigators tested dasatinib in xenograft models of ETV6-ABL1, RCSD1-ABL2, PAG1-ABL2, or SSBP2-CSF1R ALL.
They found that treated mice had significantly lower leukemic burdens and splenic weights than control mice. And STAT5 phosphorylation was attenuated in cells from treated mice.
“Our studies show that different FDA-approved TKIs such as imatinib, dasatinib, ruxolitinib, or crizotinib could potentially be used to treat Ph-like ALL patients, depending on the type of kinase alterations their tumors bear,” Dr Roberts said.
“We were able to gain a better understanding of the genetics underlying Ph-like ALL, and our studies could help identify patients who will not respond optimally to current therapy. By knowing the exact genetic alteration upfront, we may be able to implement different therapeutic strategies to improve the survival rate of future patients with ALL.” ![]()

PHILADELPHIA—Experiments in mice reinforce the idea that tyrosine kinase inhibitors (TKIs) can treat patients with Ph-like acute lymphoblastic leukemia (ALL).
Investigators recently identified genomic alterations in Ph-like ALL that suggest these patients might respond to TKIs, and tests in a small number of patients supported this theory.
Now, preclinical results show that kinase fusions in Ph-like ALL activate signaling pathways differently, and this affects sensitivity to TKIs.
Kathryn Roberts, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues presented these results at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We recently described a subtype of B-cell acute lymphoblastic leukemia with very poor outcome that is characterized by genetic alterations involving tyrosine kinases, termed Ph-like ALL,” Dr Roberts said. “We wanted to examine whether these alterations contribute to the development of Ph-like ALL and determine if they could be targeted with tyrosine kinase inhibitors.”
“We showed, for the first time, that the kinase alterations we tested contribute to the development of Ph-like ALL, and that Ph-like ALL can be treated effectively with tyrosine kinase inhibitors in animal models. These findings provide a strong rationale for treating Ph-like ALL patients with targeted therapies to improve their survival.”
Dr Roberts and her colleagues first introduced kinase alterations—RCSD1-ABL2, SSBP2-CSF1R, or PAX5-JAK2—in IL-7-dependent, Arf-/- mouse pre-B cells expressing IK6.
They found that each fusion conferred cytokine-independent growth in vitro. And mice that received transplants of pre-B cells expressing RCSD1-ABL2 or SSBP2-CSF1R developed ALL with a pre-B immunophenotype.
The investigators then assessed the activation of kinase signaling pathways and TKI sensitivity in Arf-/- pre-B cells and human leukemic cells harvested from xenografted mice expressing ETV6-ABL1, RANBP2-ABL1, PAG1-ABL2, RCSD1-ABL2, SSBP2-CSF1R, IGH-EPOR, ATF7IP-JAK2, and PAX5-JAK2.
In both cell types, signaling pathway activation and TKI sensitivity differed according to the kinase fusion.
Cells expressing ABL1-class kinase fusions (ABL1, ABL2, CSF1R, and PDGFRB) exhibited pSTAT5 activation that was inhibited by imatinib or dasatinib. But in cells expressing ATF7IP-JAK2, PAX5-JAK2, or IGH-EPOR, pSTAT5 activation was only inhibited by ruxolitinib.
Finally, the investigators tested dasatinib in xenograft models of ETV6-ABL1, RCSD1-ABL2, PAG1-ABL2, or SSBP2-CSF1R ALL.
They found that treated mice had significantly lower leukemic burdens and splenic weights than control mice. And STAT5 phosphorylation was attenuated in cells from treated mice.
“Our studies show that different FDA-approved TKIs such as imatinib, dasatinib, ruxolitinib, or crizotinib could potentially be used to treat Ph-like ALL patients, depending on the type of kinase alterations their tumors bear,” Dr Roberts said.
“We were able to gain a better understanding of the genetics underlying Ph-like ALL, and our studies could help identify patients who will not respond optimally to current therapy. By knowing the exact genetic alteration upfront, we may be able to implement different therapeutic strategies to improve the survival rate of future patients with ALL.” ![]()

PHILADELPHIA—Experiments in mice reinforce the idea that tyrosine kinase inhibitors (TKIs) can treat patients with Ph-like acute lymphoblastic leukemia (ALL).
Investigators recently identified genomic alterations in Ph-like ALL that suggest these patients might respond to TKIs, and tests in a small number of patients supported this theory.
Now, preclinical results show that kinase fusions in Ph-like ALL activate signaling pathways differently, and this affects sensitivity to TKIs.
Kathryn Roberts, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues presented these results at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We recently described a subtype of B-cell acute lymphoblastic leukemia with very poor outcome that is characterized by genetic alterations involving tyrosine kinases, termed Ph-like ALL,” Dr Roberts said. “We wanted to examine whether these alterations contribute to the development of Ph-like ALL and determine if they could be targeted with tyrosine kinase inhibitors.”
“We showed, for the first time, that the kinase alterations we tested contribute to the development of Ph-like ALL, and that Ph-like ALL can be treated effectively with tyrosine kinase inhibitors in animal models. These findings provide a strong rationale for treating Ph-like ALL patients with targeted therapies to improve their survival.”
Dr Roberts and her colleagues first introduced kinase alterations—RCSD1-ABL2, SSBP2-CSF1R, or PAX5-JAK2—in IL-7-dependent, Arf-/- mouse pre-B cells expressing IK6.
They found that each fusion conferred cytokine-independent growth in vitro. And mice that received transplants of pre-B cells expressing RCSD1-ABL2 or SSBP2-CSF1R developed ALL with a pre-B immunophenotype.
The investigators then assessed the activation of kinase signaling pathways and TKI sensitivity in Arf-/- pre-B cells and human leukemic cells harvested from xenografted mice expressing ETV6-ABL1, RANBP2-ABL1, PAG1-ABL2, RCSD1-ABL2, SSBP2-CSF1R, IGH-EPOR, ATF7IP-JAK2, and PAX5-JAK2.
In both cell types, signaling pathway activation and TKI sensitivity differed according to the kinase fusion.
Cells expressing ABL1-class kinase fusions (ABL1, ABL2, CSF1R, and PDGFRB) exhibited pSTAT5 activation that was inhibited by imatinib or dasatinib. But in cells expressing ATF7IP-JAK2, PAX5-JAK2, or IGH-EPOR, pSTAT5 activation was only inhibited by ruxolitinib.
Finally, the investigators tested dasatinib in xenograft models of ETV6-ABL1, RCSD1-ABL2, PAG1-ABL2, or SSBP2-CSF1R ALL.
They found that treated mice had significantly lower leukemic burdens and splenic weights than control mice. And STAT5 phosphorylation was attenuated in cells from treated mice.
“Our studies show that different FDA-approved TKIs such as imatinib, dasatinib, ruxolitinib, or crizotinib could potentially be used to treat Ph-like ALL patients, depending on the type of kinase alterations their tumors bear,” Dr Roberts said.
“We were able to gain a better understanding of the genetics underlying Ph-like ALL, and our studies could help identify patients who will not respond optimally to current therapy. By knowing the exact genetic alteration upfront, we may be able to implement different therapeutic strategies to improve the survival rate of future patients with ALL.” ![]()
ETBs prove effective against lymphoma and myeloma

Credit: Rhoda Baer
PHILADELPHIA—A pair of engineered toxin bodies (ETBs) can successfully treat Burkitt lymphoma and multiple myeloma, according to preclinical research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The ETBs, known as MT-4007 and MT-4007-D, work by targeting CD38.
They greatly reduced tumor burden and improved survival in mouse models. And they were well-tolerated, even at the highest doses administered.
“In this study, we found that the growth of human cancer cells in mice was substantially decreased, or the cells were even eliminated, following treatment with our investigational CD38-targeted therapy,” said Erin K. Willert, PhD, of Molecular Templates Inc., in Georgetown, Texas.
Dr Willert and her colleagues explained that ETBs are derived from the ribosome-inactivating alpha subunit of Shiga-like toxin 1 (SLT-1A). They have been engineered to contain a target binding domain fused to a modified SLT-1A protein, which allows for delivery to a cell surface target—in this case, CD38.
Upon binding to a CD38-expressing cell, the ETB enters the cell, routes to the cytosol, halts protein synthesis, and kills the cell.
The researchers first tested MT-4007 and MT-4007-D in a range of human cell lines. The agents exhibited cytotoxicity in CD38+ Burkitt lymphoma and multiple myeloma cell lines (H929, Daudi, ST486, and Raji). But neither agent proved cytotoxic in CD38- cell lines (U266, SKBR3, and HCC1954).
The team then moved on to test MT-4007 in a mouse model of Burkitt lymphoma. Following injection with Daudi-Luc cells, mice received no treatment or MT-4007 at 0.05 mg/kg, 0.5 mg/kg, or 2 mg/kg on days 3, 5, 8, 10, and 12.
Treated mice exhibited significantly reduced tumor burden compared to controls. The mean tumor burden for mice that received MT-4007 at 0.05 mg/kg was 29% of the control tumor burden (P<0.0001). It was 0.4% for mice that received 0.50 mg/kg (P<0.0001) and 0.02% for mice that received 2 mg/kg (P<0.0001).
In a model of multiple myeloma, MT-4007-D provided a dose-dependent delay in tumor growth. After receiving injections of H929 cells, mice received no treatment or MT-4007-D at 0.5 mg/kg, 2 mg/kg, or 3 mg/kg on days 1, 3, 5, 8, 10, and 12.
The researchers assessed efficacy by measuring the time to endpoint, which was a tumor volume of 2000 mm3. The median time to endpoint was 22.3 days in controls, 21.2 days in the 0.5 mg/kg arm (not significant), 24.5 days in the 2 mg/kg arm (P=0.004), and 26.2 days in the 3 mg/kg arm (P=0.04).
The team assessed safety using body weight. They found that all treated groups of mice maintained a stable weight, suggesting MT-4007-D is well-tolerated.
The researchers also noted that, in a previous dose-finding study, the maximum-tolerated dose of MT-4007 was not reached at the highest dose administered to mice (2 mg/kg), which suggests MT-4007 is well tolerated as well.
Finally, Dr Willert and her colleagues found that MT-4007 extends survival in models of Burkitt lymphoma. The team euthanized mice if they had a greater than 20% loss in body weight or symptoms such as hind limb paralysis.
In the control group, all 10 mice died, and the median survival was 34 days. In the 0.5 mg/kg treatment group, 5 mice died, and the median survival was 59.5 days (P=0.0002).
One mouse died in the 0.5 mg/kg group (P<0.0001), and none of the mice died in the 2 mg/kg group (P<0.0001). The median survival was undefined for both groups.
Dr Willert said these results suggest the ETBs should be moved forward to clinical trials in CD38+ B-cell malignancies such as multiple myeloma. And because the ETBs work differently from other treatments, they might prove effective in relapsed or refractory patients.
However, more preclinical research is needed before the ETBs can be tested in patients. MT-4007-D is under investigation in preclinical studies now.
This research was funded by Molecular Templates Inc., makers of MT-4007 and MT-4007-D. ![]()

Credit: Rhoda Baer
PHILADELPHIA—A pair of engineered toxin bodies (ETBs) can successfully treat Burkitt lymphoma and multiple myeloma, according to preclinical research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The ETBs, known as MT-4007 and MT-4007-D, work by targeting CD38.
They greatly reduced tumor burden and improved survival in mouse models. And they were well-tolerated, even at the highest doses administered.
“In this study, we found that the growth of human cancer cells in mice was substantially decreased, or the cells were even eliminated, following treatment with our investigational CD38-targeted therapy,” said Erin K. Willert, PhD, of Molecular Templates Inc., in Georgetown, Texas.
Dr Willert and her colleagues explained that ETBs are derived from the ribosome-inactivating alpha subunit of Shiga-like toxin 1 (SLT-1A). They have been engineered to contain a target binding domain fused to a modified SLT-1A protein, which allows for delivery to a cell surface target—in this case, CD38.
Upon binding to a CD38-expressing cell, the ETB enters the cell, routes to the cytosol, halts protein synthesis, and kills the cell.
The researchers first tested MT-4007 and MT-4007-D in a range of human cell lines. The agents exhibited cytotoxicity in CD38+ Burkitt lymphoma and multiple myeloma cell lines (H929, Daudi, ST486, and Raji). But neither agent proved cytotoxic in CD38- cell lines (U266, SKBR3, and HCC1954).
The team then moved on to test MT-4007 in a mouse model of Burkitt lymphoma. Following injection with Daudi-Luc cells, mice received no treatment or MT-4007 at 0.05 mg/kg, 0.5 mg/kg, or 2 mg/kg on days 3, 5, 8, 10, and 12.
Treated mice exhibited significantly reduced tumor burden compared to controls. The mean tumor burden for mice that received MT-4007 at 0.05 mg/kg was 29% of the control tumor burden (P<0.0001). It was 0.4% for mice that received 0.50 mg/kg (P<0.0001) and 0.02% for mice that received 2 mg/kg (P<0.0001).
In a model of multiple myeloma, MT-4007-D provided a dose-dependent delay in tumor growth. After receiving injections of H929 cells, mice received no treatment or MT-4007-D at 0.5 mg/kg, 2 mg/kg, or 3 mg/kg on days 1, 3, 5, 8, 10, and 12.
The researchers assessed efficacy by measuring the time to endpoint, which was a tumor volume of 2000 mm3. The median time to endpoint was 22.3 days in controls, 21.2 days in the 0.5 mg/kg arm (not significant), 24.5 days in the 2 mg/kg arm (P=0.004), and 26.2 days in the 3 mg/kg arm (P=0.04).
The team assessed safety using body weight. They found that all treated groups of mice maintained a stable weight, suggesting MT-4007-D is well-tolerated.
The researchers also noted that, in a previous dose-finding study, the maximum-tolerated dose of MT-4007 was not reached at the highest dose administered to mice (2 mg/kg), which suggests MT-4007 is well tolerated as well.
Finally, Dr Willert and her colleagues found that MT-4007 extends survival in models of Burkitt lymphoma. The team euthanized mice if they had a greater than 20% loss in body weight or symptoms such as hind limb paralysis.
In the control group, all 10 mice died, and the median survival was 34 days. In the 0.5 mg/kg treatment group, 5 mice died, and the median survival was 59.5 days (P=0.0002).
One mouse died in the 0.5 mg/kg group (P<0.0001), and none of the mice died in the 2 mg/kg group (P<0.0001). The median survival was undefined for both groups.
Dr Willert said these results suggest the ETBs should be moved forward to clinical trials in CD38+ B-cell malignancies such as multiple myeloma. And because the ETBs work differently from other treatments, they might prove effective in relapsed or refractory patients.
However, more preclinical research is needed before the ETBs can be tested in patients. MT-4007-D is under investigation in preclinical studies now.
This research was funded by Molecular Templates Inc., makers of MT-4007 and MT-4007-D. ![]()

Credit: Rhoda Baer
PHILADELPHIA—A pair of engineered toxin bodies (ETBs) can successfully treat Burkitt lymphoma and multiple myeloma, according to preclinical research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The ETBs, known as MT-4007 and MT-4007-D, work by targeting CD38.
They greatly reduced tumor burden and improved survival in mouse models. And they were well-tolerated, even at the highest doses administered.
“In this study, we found that the growth of human cancer cells in mice was substantially decreased, or the cells were even eliminated, following treatment with our investigational CD38-targeted therapy,” said Erin K. Willert, PhD, of Molecular Templates Inc., in Georgetown, Texas.
Dr Willert and her colleagues explained that ETBs are derived from the ribosome-inactivating alpha subunit of Shiga-like toxin 1 (SLT-1A). They have been engineered to contain a target binding domain fused to a modified SLT-1A protein, which allows for delivery to a cell surface target—in this case, CD38.
Upon binding to a CD38-expressing cell, the ETB enters the cell, routes to the cytosol, halts protein synthesis, and kills the cell.
The researchers first tested MT-4007 and MT-4007-D in a range of human cell lines. The agents exhibited cytotoxicity in CD38+ Burkitt lymphoma and multiple myeloma cell lines (H929, Daudi, ST486, and Raji). But neither agent proved cytotoxic in CD38- cell lines (U266, SKBR3, and HCC1954).
The team then moved on to test MT-4007 in a mouse model of Burkitt lymphoma. Following injection with Daudi-Luc cells, mice received no treatment or MT-4007 at 0.05 mg/kg, 0.5 mg/kg, or 2 mg/kg on days 3, 5, 8, 10, and 12.
Treated mice exhibited significantly reduced tumor burden compared to controls. The mean tumor burden for mice that received MT-4007 at 0.05 mg/kg was 29% of the control tumor burden (P<0.0001). It was 0.4% for mice that received 0.50 mg/kg (P<0.0001) and 0.02% for mice that received 2 mg/kg (P<0.0001).
In a model of multiple myeloma, MT-4007-D provided a dose-dependent delay in tumor growth. After receiving injections of H929 cells, mice received no treatment or MT-4007-D at 0.5 mg/kg, 2 mg/kg, or 3 mg/kg on days 1, 3, 5, 8, 10, and 12.
The researchers assessed efficacy by measuring the time to endpoint, which was a tumor volume of 2000 mm3. The median time to endpoint was 22.3 days in controls, 21.2 days in the 0.5 mg/kg arm (not significant), 24.5 days in the 2 mg/kg arm (P=0.004), and 26.2 days in the 3 mg/kg arm (P=0.04).
The team assessed safety using body weight. They found that all treated groups of mice maintained a stable weight, suggesting MT-4007-D is well-tolerated.
The researchers also noted that, in a previous dose-finding study, the maximum-tolerated dose of MT-4007 was not reached at the highest dose administered to mice (2 mg/kg), which suggests MT-4007 is well tolerated as well.
Finally, Dr Willert and her colleagues found that MT-4007 extends survival in models of Burkitt lymphoma. The team euthanized mice if they had a greater than 20% loss in body weight or symptoms such as hind limb paralysis.
In the control group, all 10 mice died, and the median survival was 34 days. In the 0.5 mg/kg treatment group, 5 mice died, and the median survival was 59.5 days (P=0.0002).
One mouse died in the 0.5 mg/kg group (P<0.0001), and none of the mice died in the 2 mg/kg group (P<0.0001). The median survival was undefined for both groups.
Dr Willert said these results suggest the ETBs should be moved forward to clinical trials in CD38+ B-cell malignancies such as multiple myeloma. And because the ETBs work differently from other treatments, they might prove effective in relapsed or refractory patients.
However, more preclinical research is needed before the ETBs can be tested in patients. MT-4007-D is under investigation in preclinical studies now.
This research was funded by Molecular Templates Inc., makers of MT-4007 and MT-4007-D. ![]()
Drugs demonstrate inconsistent synergy in CLL, MCL

PHILADELPHIA—The Bcl-2 inhibitor ABT-199 and the Bruton tyrosine kinase inhibitor ibrutinib can have a synergistic effect against mantle cell lymphoma (MCL) and chronic lymphocytic leukemia (CLL), preclinical data suggest.
In one set of experiments with MCL and CLL samples, the drugs induced apoptosis at a much higher rate when used together than when used alone.
However, in other experiments with CLL samples, ABT-199 and ibrutinib did not consistently display synergistic cytoxicity.
The researchers said this indicates substantial patient heterogeneity in response to the combination that may be due to variations in the genetic landscape.
Michael J. Weber, PhD, of the University of Virginia School of Medicine in Charlottesville, and his colleagues presented this research at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We took an empirical but systematic approach to identify combinations of drugs that might improve the ability of ibrutinib to kill cancer cells,” Dr Weber said. “The combination of ibrutinib and ABT-199 was, by far, the most effective in our assays, and we are in the very earliest stages of planning a clinical trial to test this combination in the clinic.”
In previous studies, Dr Weber and his colleagues found that ibrutinib synergized with both ABT-199 and the proteasome inhibitor carfilzomib to kill MCL cell lines. In this study, the team assessed the effects of exposure to these 2 combinations on samples from patients with MCL or CLL.
The researchers found that apoptosis occurred in 23% of cells exposed to ABT-199 and ibrutinib in combination, compared to 3.8% of cells exposed to ibrutinib and 3% exposed to ABT-199.
The combination of ibrutinib and carfilzomib also increased apoptosis in MCL and CLL cells compared to either agent alone, though to a lesser degree than the ABT-199 combination. Apoptosis occurred in 5.5% of cells exposed to ibrutinib and carfilzomib, 3.8% exposed to ibrutinib, and 1.7% exposed to carfilzomib.
The researchers observed minimal apoptosis in normal T cells, both with the single agents and the combinations.
Further analysis showed that ibrutinib and ABT-199 worked synergistically to cause apoptosis in leukemic cells from 5 of 9 patients with CLL.
According to Dr Weber, the variable response to this combination points to the importance of understanding how these combinations work, so we can match the treatments with the most appropriate patients.
“Ibrutinib and ABT-199 target different pathways involved in promoting cancer cell survival and growth,” Dr Weber said.
“This is very intriguing because, in most instances where cancer cells are resistant to a particular molecularly targeted drug, we find that cancer cells adapt and find new ways to reactivate the pathway being targeted by the drug and that combinations of drugs targeting this pathway in different ways can improve outcomes. Here, we found that targeting a pathway outside the primary pathway was effective.”
This study was funded by the University of Virginia Cancer Center. Dr Weber declared no conflicts of interest. ![]()

PHILADELPHIA—The Bcl-2 inhibitor ABT-199 and the Bruton tyrosine kinase inhibitor ibrutinib can have a synergistic effect against mantle cell lymphoma (MCL) and chronic lymphocytic leukemia (CLL), preclinical data suggest.
In one set of experiments with MCL and CLL samples, the drugs induced apoptosis at a much higher rate when used together than when used alone.
However, in other experiments with CLL samples, ABT-199 and ibrutinib did not consistently display synergistic cytoxicity.
The researchers said this indicates substantial patient heterogeneity in response to the combination that may be due to variations in the genetic landscape.
Michael J. Weber, PhD, of the University of Virginia School of Medicine in Charlottesville, and his colleagues presented this research at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We took an empirical but systematic approach to identify combinations of drugs that might improve the ability of ibrutinib to kill cancer cells,” Dr Weber said. “The combination of ibrutinib and ABT-199 was, by far, the most effective in our assays, and we are in the very earliest stages of planning a clinical trial to test this combination in the clinic.”
In previous studies, Dr Weber and his colleagues found that ibrutinib synergized with both ABT-199 and the proteasome inhibitor carfilzomib to kill MCL cell lines. In this study, the team assessed the effects of exposure to these 2 combinations on samples from patients with MCL or CLL.
The researchers found that apoptosis occurred in 23% of cells exposed to ABT-199 and ibrutinib in combination, compared to 3.8% of cells exposed to ibrutinib and 3% exposed to ABT-199.
The combination of ibrutinib and carfilzomib also increased apoptosis in MCL and CLL cells compared to either agent alone, though to a lesser degree than the ABT-199 combination. Apoptosis occurred in 5.5% of cells exposed to ibrutinib and carfilzomib, 3.8% exposed to ibrutinib, and 1.7% exposed to carfilzomib.
The researchers observed minimal apoptosis in normal T cells, both with the single agents and the combinations.
Further analysis showed that ibrutinib and ABT-199 worked synergistically to cause apoptosis in leukemic cells from 5 of 9 patients with CLL.
According to Dr Weber, the variable response to this combination points to the importance of understanding how these combinations work, so we can match the treatments with the most appropriate patients.
“Ibrutinib and ABT-199 target different pathways involved in promoting cancer cell survival and growth,” Dr Weber said.
“This is very intriguing because, in most instances where cancer cells are resistant to a particular molecularly targeted drug, we find that cancer cells adapt and find new ways to reactivate the pathway being targeted by the drug and that combinations of drugs targeting this pathway in different ways can improve outcomes. Here, we found that targeting a pathway outside the primary pathway was effective.”
This study was funded by the University of Virginia Cancer Center. Dr Weber declared no conflicts of interest. ![]()

PHILADELPHIA—The Bcl-2 inhibitor ABT-199 and the Bruton tyrosine kinase inhibitor ibrutinib can have a synergistic effect against mantle cell lymphoma (MCL) and chronic lymphocytic leukemia (CLL), preclinical data suggest.
In one set of experiments with MCL and CLL samples, the drugs induced apoptosis at a much higher rate when used together than when used alone.
However, in other experiments with CLL samples, ABT-199 and ibrutinib did not consistently display synergistic cytoxicity.
The researchers said this indicates substantial patient heterogeneity in response to the combination that may be due to variations in the genetic landscape.
Michael J. Weber, PhD, of the University of Virginia School of Medicine in Charlottesville, and his colleagues presented this research at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We took an empirical but systematic approach to identify combinations of drugs that might improve the ability of ibrutinib to kill cancer cells,” Dr Weber said. “The combination of ibrutinib and ABT-199 was, by far, the most effective in our assays, and we are in the very earliest stages of planning a clinical trial to test this combination in the clinic.”
In previous studies, Dr Weber and his colleagues found that ibrutinib synergized with both ABT-199 and the proteasome inhibitor carfilzomib to kill MCL cell lines. In this study, the team assessed the effects of exposure to these 2 combinations on samples from patients with MCL or CLL.
The researchers found that apoptosis occurred in 23% of cells exposed to ABT-199 and ibrutinib in combination, compared to 3.8% of cells exposed to ibrutinib and 3% exposed to ABT-199.
The combination of ibrutinib and carfilzomib also increased apoptosis in MCL and CLL cells compared to either agent alone, though to a lesser degree than the ABT-199 combination. Apoptosis occurred in 5.5% of cells exposed to ibrutinib and carfilzomib, 3.8% exposed to ibrutinib, and 1.7% exposed to carfilzomib.
The researchers observed minimal apoptosis in normal T cells, both with the single agents and the combinations.
Further analysis showed that ibrutinib and ABT-199 worked synergistically to cause apoptosis in leukemic cells from 5 of 9 patients with CLL.
According to Dr Weber, the variable response to this combination points to the importance of understanding how these combinations work, so we can match the treatments with the most appropriate patients.
“Ibrutinib and ABT-199 target different pathways involved in promoting cancer cell survival and growth,” Dr Weber said.
“This is very intriguing because, in most instances where cancer cells are resistant to a particular molecularly targeted drug, we find that cancer cells adapt and find new ways to reactivate the pathway being targeted by the drug and that combinations of drugs targeting this pathway in different ways can improve outcomes. Here, we found that targeting a pathway outside the primary pathway was effective.”
This study was funded by the University of Virginia Cancer Center. Dr Weber declared no conflicts of interest. ![]()