User login
Patients with PD-L1–positive tumors had better response to immune checkpoint inhibitor
SAN DIEGO – Preliminary findings from two studies presented at the annual meeting of the American Association for Cancer Research suggest that cancer patients whose tumors contained the protein PD-L1 responded favorably to treatment with the investigational checkpoint inhibitor MK-3475.
A highly selective anti–PD-1 immunotherapy being developed by Merck, MK-3475 is designed to restore the natural ability of the immune system to recognize and target cancer cells by selectively achieving dual ligand blockade (PD-L1 and PD-L2) of the PD-1 protein.
Both studies are analyses from the ongoing phase 1B KEYNOTE-001 study. In the first analysis, researchers led by Dr. Adil I. Daud evaluated tumor samples from 195 patients with late-stage melanoma who received MK-3475 at three different doses: 10 mg/kg every 2 weeks, 10 mg/kg every 3 weeks, or 2 mg/kg every 3 weeks. Some of the patients had received prior treatment with ipilimumab.
Dr. Daud, codirector of the University of California, San Francisco, melanoma center and director of melanoma clinical research at the UCSF Helen Diller Family Comprehensive Cancer Center, and his associates measured the amount of PD-L1 in the tumor samples and considered them PD-L1 positive if at least 1 cell/100 tumors cells stained by immunohistochemistry contained the protein. They also used multiplex flow cytometry to assess absolute CD4 and CD8 T-cell counts and the percentage of activated CD4 and CD8 T-cell counts in peripheral blood.
All study participants had a new tumor biopsy within 2 months before the first dose of MK-3475. Their mean age was 63 years, 76% were male, and 76% had BRAF wild-type tumors. Of the 125 evaluable tumor samples, 89 (71%) were PD-L1 positive and 36 were PD-L1 negative. Disease did not progress for about 50 weeks among patients with PD-L1–positive tumors, compared with about 12 weeks among those with PD-L1–negative tumors. Among the entire study population, the overall response rate was 40%, "which is high for immunotherapy," Dr. Daud said during a press briefing.
Based on cut point of at least 1 cell/100 tumors cells, the response rate among patients with PD-L1–positive tumors was 49%, compared with 13% among patients with PD-L1–negative tumors (P = .0007). At 6 months, 57% of patients with PD-L1–positive tumors had no disease progression, compared with 35% of those whose tumors were PD-L1 negative (P = 0.0051).
Between baseline and week 6, the researchers observed a significant median increase in the percentage of CD8-positive CD4-positive T cells (14.6% vs. 15.7%, respectively) though no significant change in the absolute numbers of circulating T cells was observed.
"Given the high prevalence of PD-L1–positive tumors, the clinical utility of PD-L1 expression in melanoma is not clear at this point, because unselected patients have such a high level of response," Dr. Daud said. Changes in T-cell subtype distribution as a pharmacodynamic marker "supports the proposed MK-3475 mechanism of action."
He characterized the study as "a good foundation to build on, and we think that ongoing studies looking at larger clinical trials will help clarify the role of PD-L1 expression in terms of correlating with response of patients treated with MK-3475. Clinical development of MK-3475, both as monotherapy and as part of combination strategies, is ongoing in multiple solid tumors and hematologic malignancies."
In the second study, Dr. Leena Gandhi presented extended data from an earlier trial of 38 patients with non–small cell lung cancer who were treated with MK-3475. That trial found that higher levels of PD-L1 expression "appeared to correlate with an increased response to MK-3475," Dr. Gandhi, a thoracic oncologist at the Dana-Farber Cancer Institute, Boston, said during a press briefing. The purpose of the current analysis, which included 146 patients, was to determine an optimal cut point for defining whether a tumor is likely to respond to MK-3475 therapy or not. The patients received the agent at three different doses: 2 mg/kg every 3 weeks, 10 mg/kg every 3 weeks, or 10 mg/kg every 2 weeks. Tumors were assessed by imaging every 9 weeks and by RECIST 1.1 (Response Evaluation Criteria in Solid Tumors).
Dr. Gandhi and her associates found that PD-L1 levels of greater than 50% as measured by immunohistochemistry was the best cut-off point for determining whether a tumor is likely to respond to MK-3475. Six months after starting treatment, 41% of patients with tumors that contained high levels of PD-L1 prior to treatment had no disease progression, compared with 17% of those whose tumors contained low levels of PD-L1 (hazard ratio, 0.53; P = .004). This finding is "based on very small numbers of patients with long-term follow-up, so we expect that the final progression-free survival differences may change over time with additional patients," Dr. Gandhi noted.
As for overall survival, 72% of patients with tumors that contained high levels of PD-L1 were alive at 6 months, compared with 53% of those whose tumors contained low levels of PD-L1. This difference trended toward statistical significance (HR, 0.65; P = .134) and may also change as data from additional patients are realized, she said.
Dr. Gandhi noted that data from two ongoing studies will be used to "further explore the relationship between tumor PD-L1 expression and MK-3475 activity in NSCLC patients."
In an interview, Dr. Patricia M. LoRusso, director of the Center for Translational Therapeutics at Wayne State University’s Karmanos Cancer Institute, Detroit, characterized the MK-3475 biomarker as "maturing, but I still think it’s under investigation. I still think we have a ways to go in identifying the best predictive biomarker. I don’t think it’s 100% foolproof by any means."
Both studies were funded by Merck. Dr. Daud disclosed that he has served on the advisory board of Merck and GlaxoSmithKline. Dr. Gandhi said that she had no relevant financial conflicts to disclose.
Dr. LoRusso disclosed that she has received research funding from Agios Pharmaceuticals.
SAN DIEGO – Preliminary findings from two studies presented at the annual meeting of the American Association for Cancer Research suggest that cancer patients whose tumors contained the protein PD-L1 responded favorably to treatment with the investigational checkpoint inhibitor MK-3475.
A highly selective anti–PD-1 immunotherapy being developed by Merck, MK-3475 is designed to restore the natural ability of the immune system to recognize and target cancer cells by selectively achieving dual ligand blockade (PD-L1 and PD-L2) of the PD-1 protein.
Both studies are analyses from the ongoing phase 1B KEYNOTE-001 study. In the first analysis, researchers led by Dr. Adil I. Daud evaluated tumor samples from 195 patients with late-stage melanoma who received MK-3475 at three different doses: 10 mg/kg every 2 weeks, 10 mg/kg every 3 weeks, or 2 mg/kg every 3 weeks. Some of the patients had received prior treatment with ipilimumab.
Dr. Daud, codirector of the University of California, San Francisco, melanoma center and director of melanoma clinical research at the UCSF Helen Diller Family Comprehensive Cancer Center, and his associates measured the amount of PD-L1 in the tumor samples and considered them PD-L1 positive if at least 1 cell/100 tumors cells stained by immunohistochemistry contained the protein. They also used multiplex flow cytometry to assess absolute CD4 and CD8 T-cell counts and the percentage of activated CD4 and CD8 T-cell counts in peripheral blood.
All study participants had a new tumor biopsy within 2 months before the first dose of MK-3475. Their mean age was 63 years, 76% were male, and 76% had BRAF wild-type tumors. Of the 125 evaluable tumor samples, 89 (71%) were PD-L1 positive and 36 were PD-L1 negative. Disease did not progress for about 50 weeks among patients with PD-L1–positive tumors, compared with about 12 weeks among those with PD-L1–negative tumors. Among the entire study population, the overall response rate was 40%, "which is high for immunotherapy," Dr. Daud said during a press briefing.
Based on cut point of at least 1 cell/100 tumors cells, the response rate among patients with PD-L1–positive tumors was 49%, compared with 13% among patients with PD-L1–negative tumors (P = .0007). At 6 months, 57% of patients with PD-L1–positive tumors had no disease progression, compared with 35% of those whose tumors were PD-L1 negative (P = 0.0051).
Between baseline and week 6, the researchers observed a significant median increase in the percentage of CD8-positive CD4-positive T cells (14.6% vs. 15.7%, respectively) though no significant change in the absolute numbers of circulating T cells was observed.
"Given the high prevalence of PD-L1–positive tumors, the clinical utility of PD-L1 expression in melanoma is not clear at this point, because unselected patients have such a high level of response," Dr. Daud said. Changes in T-cell subtype distribution as a pharmacodynamic marker "supports the proposed MK-3475 mechanism of action."
He characterized the study as "a good foundation to build on, and we think that ongoing studies looking at larger clinical trials will help clarify the role of PD-L1 expression in terms of correlating with response of patients treated with MK-3475. Clinical development of MK-3475, both as monotherapy and as part of combination strategies, is ongoing in multiple solid tumors and hematologic malignancies."
In the second study, Dr. Leena Gandhi presented extended data from an earlier trial of 38 patients with non–small cell lung cancer who were treated with MK-3475. That trial found that higher levels of PD-L1 expression "appeared to correlate with an increased response to MK-3475," Dr. Gandhi, a thoracic oncologist at the Dana-Farber Cancer Institute, Boston, said during a press briefing. The purpose of the current analysis, which included 146 patients, was to determine an optimal cut point for defining whether a tumor is likely to respond to MK-3475 therapy or not. The patients received the agent at three different doses: 2 mg/kg every 3 weeks, 10 mg/kg every 3 weeks, or 10 mg/kg every 2 weeks. Tumors were assessed by imaging every 9 weeks and by RECIST 1.1 (Response Evaluation Criteria in Solid Tumors).
Dr. Gandhi and her associates found that PD-L1 levels of greater than 50% as measured by immunohistochemistry was the best cut-off point for determining whether a tumor is likely to respond to MK-3475. Six months after starting treatment, 41% of patients with tumors that contained high levels of PD-L1 prior to treatment had no disease progression, compared with 17% of those whose tumors contained low levels of PD-L1 (hazard ratio, 0.53; P = .004). This finding is "based on very small numbers of patients with long-term follow-up, so we expect that the final progression-free survival differences may change over time with additional patients," Dr. Gandhi noted.
As for overall survival, 72% of patients with tumors that contained high levels of PD-L1 were alive at 6 months, compared with 53% of those whose tumors contained low levels of PD-L1. This difference trended toward statistical significance (HR, 0.65; P = .134) and may also change as data from additional patients are realized, she said.
Dr. Gandhi noted that data from two ongoing studies will be used to "further explore the relationship between tumor PD-L1 expression and MK-3475 activity in NSCLC patients."
In an interview, Dr. Patricia M. LoRusso, director of the Center for Translational Therapeutics at Wayne State University’s Karmanos Cancer Institute, Detroit, characterized the MK-3475 biomarker as "maturing, but I still think it’s under investigation. I still think we have a ways to go in identifying the best predictive biomarker. I don’t think it’s 100% foolproof by any means."
Both studies were funded by Merck. Dr. Daud disclosed that he has served on the advisory board of Merck and GlaxoSmithKline. Dr. Gandhi said that she had no relevant financial conflicts to disclose.
Dr. LoRusso disclosed that she has received research funding from Agios Pharmaceuticals.
SAN DIEGO – Preliminary findings from two studies presented at the annual meeting of the American Association for Cancer Research suggest that cancer patients whose tumors contained the protein PD-L1 responded favorably to treatment with the investigational checkpoint inhibitor MK-3475.
A highly selective anti–PD-1 immunotherapy being developed by Merck, MK-3475 is designed to restore the natural ability of the immune system to recognize and target cancer cells by selectively achieving dual ligand blockade (PD-L1 and PD-L2) of the PD-1 protein.
Both studies are analyses from the ongoing phase 1B KEYNOTE-001 study. In the first analysis, researchers led by Dr. Adil I. Daud evaluated tumor samples from 195 patients with late-stage melanoma who received MK-3475 at three different doses: 10 mg/kg every 2 weeks, 10 mg/kg every 3 weeks, or 2 mg/kg every 3 weeks. Some of the patients had received prior treatment with ipilimumab.
Dr. Daud, codirector of the University of California, San Francisco, melanoma center and director of melanoma clinical research at the UCSF Helen Diller Family Comprehensive Cancer Center, and his associates measured the amount of PD-L1 in the tumor samples and considered them PD-L1 positive if at least 1 cell/100 tumors cells stained by immunohistochemistry contained the protein. They also used multiplex flow cytometry to assess absolute CD4 and CD8 T-cell counts and the percentage of activated CD4 and CD8 T-cell counts in peripheral blood.
All study participants had a new tumor biopsy within 2 months before the first dose of MK-3475. Their mean age was 63 years, 76% were male, and 76% had BRAF wild-type tumors. Of the 125 evaluable tumor samples, 89 (71%) were PD-L1 positive and 36 were PD-L1 negative. Disease did not progress for about 50 weeks among patients with PD-L1–positive tumors, compared with about 12 weeks among those with PD-L1–negative tumors. Among the entire study population, the overall response rate was 40%, "which is high for immunotherapy," Dr. Daud said during a press briefing.
Based on cut point of at least 1 cell/100 tumors cells, the response rate among patients with PD-L1–positive tumors was 49%, compared with 13% among patients with PD-L1–negative tumors (P = .0007). At 6 months, 57% of patients with PD-L1–positive tumors had no disease progression, compared with 35% of those whose tumors were PD-L1 negative (P = 0.0051).
Between baseline and week 6, the researchers observed a significant median increase in the percentage of CD8-positive CD4-positive T cells (14.6% vs. 15.7%, respectively) though no significant change in the absolute numbers of circulating T cells was observed.
"Given the high prevalence of PD-L1–positive tumors, the clinical utility of PD-L1 expression in melanoma is not clear at this point, because unselected patients have such a high level of response," Dr. Daud said. Changes in T-cell subtype distribution as a pharmacodynamic marker "supports the proposed MK-3475 mechanism of action."
He characterized the study as "a good foundation to build on, and we think that ongoing studies looking at larger clinical trials will help clarify the role of PD-L1 expression in terms of correlating with response of patients treated with MK-3475. Clinical development of MK-3475, both as monotherapy and as part of combination strategies, is ongoing in multiple solid tumors and hematologic malignancies."
In the second study, Dr. Leena Gandhi presented extended data from an earlier trial of 38 patients with non–small cell lung cancer who were treated with MK-3475. That trial found that higher levels of PD-L1 expression "appeared to correlate with an increased response to MK-3475," Dr. Gandhi, a thoracic oncologist at the Dana-Farber Cancer Institute, Boston, said during a press briefing. The purpose of the current analysis, which included 146 patients, was to determine an optimal cut point for defining whether a tumor is likely to respond to MK-3475 therapy or not. The patients received the agent at three different doses: 2 mg/kg every 3 weeks, 10 mg/kg every 3 weeks, or 10 mg/kg every 2 weeks. Tumors were assessed by imaging every 9 weeks and by RECIST 1.1 (Response Evaluation Criteria in Solid Tumors).
Dr. Gandhi and her associates found that PD-L1 levels of greater than 50% as measured by immunohistochemistry was the best cut-off point for determining whether a tumor is likely to respond to MK-3475. Six months after starting treatment, 41% of patients with tumors that contained high levels of PD-L1 prior to treatment had no disease progression, compared with 17% of those whose tumors contained low levels of PD-L1 (hazard ratio, 0.53; P = .004). This finding is "based on very small numbers of patients with long-term follow-up, so we expect that the final progression-free survival differences may change over time with additional patients," Dr. Gandhi noted.
As for overall survival, 72% of patients with tumors that contained high levels of PD-L1 were alive at 6 months, compared with 53% of those whose tumors contained low levels of PD-L1. This difference trended toward statistical significance (HR, 0.65; P = .134) and may also change as data from additional patients are realized, she said.
Dr. Gandhi noted that data from two ongoing studies will be used to "further explore the relationship between tumor PD-L1 expression and MK-3475 activity in NSCLC patients."
In an interview, Dr. Patricia M. LoRusso, director of the Center for Translational Therapeutics at Wayne State University’s Karmanos Cancer Institute, Detroit, characterized the MK-3475 biomarker as "maturing, but I still think it’s under investigation. I still think we have a ways to go in identifying the best predictive biomarker. I don’t think it’s 100% foolproof by any means."
Both studies were funded by Merck. Dr. Daud disclosed that he has served on the advisory board of Merck and GlaxoSmithKline. Dr. Gandhi said that she had no relevant financial conflicts to disclose.
Dr. LoRusso disclosed that she has received research funding from Agios Pharmaceuticals.
AT THE AACR ANNUAL MEETING
Major finding: Overall response to MK-3475 among melanoma patients with PD-L1–positive tumors was 49%, compared with 13% among patients with PD-L1–negative tumors (P = .0007). In a separate study, 41% of NSCLC patients with tumors that contained high levels of PD-L1 prior to treatment had no disease progression, compared with 17% of those whose tumors contained low levels of PD-L1 (P = .004).
Data source: Two studies of 341 patients from the ongoing phase 1B KEYNOTE-001 study.
Disclosures: The studies were funded by Merck. Dr. Daud disclosed that he has served on the advisory board of Merck and GlaxoSmithKline. Dr. Gandhi said that she had no relevant financial conflicts to disclose.
How autophagy helps cancer cells evade death
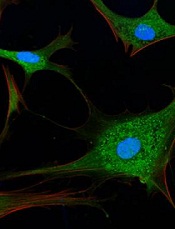
Credit: Sarah Pfau
SAN DIEGO—New research suggests that autophagy may allow cancer cells to recover and divide, rather than die, when faced with chemotherapy.
“What we showed is that if this mechanism doesn’t work right—for example, if autophagy is too high or if the target regulated by autophagy isn’t around—cancer cells may be able to rescue themselves from death caused by chemotherapies,” said study author Andrew Thorburn, PhD, of the University of Colorado Denver.
He and his colleagues believe this finding has important implications. It demonstrates a mechanism whereby autophagy controls cell death, and it further reinforces the clinical potential of inhibiting autophagy to sensitize cancer cells to chemotherapy.
Dr Thorburn and his colleagues recounted their research in Cell Reports and presented it in an education session at the AACR Annual Meeting 2014.
The researchers had set out to examine how autophagy affects canonical death receptor-induced mitochondrial outer membrane permeabilization (MOMP) and apoptosis. They found that MOMP occurs at variable times in cells, and it’s delayed by autophagy.
Furthermore, autophagy leads to inefficient MOMP. This causes some cells to die via a slower process than typical apoptosis, which allows them to eventually recover and divide.
Specifically, the researchers found that, as a cancer cell begins to die, mitochondrial cell walls break down. And the cell’s mitochondria release proteins via MOMP.
But then, high autophagy allows the cell to encapsulate and “digest” these released proteins before MOMP can keep the cell well and truly dead. The cell recovers and goes on to divide.
“The implication here is that if you inhibit autophagy, you’d make this less likely to happen; ie, when you kill cancer cells, they would stay dead,” Dr Thorburn said.
He and his colleagues also found that autophagy depends on the target PUMA to regulate cell death. When PUMA is absent, it doesn’t matter if autophagy is inhibited. Without the communicating action of PUMA, cancer cells evade apoptosis and continue to survive.
The researchers said this suggests autophagy can control apoptosis via a regulator that makes MOMP faster and more efficient, thus ensuring the rapid completion of apoptosis.
“Autophagy is complex and, as yet, not fully understood,” Dr Thorburn said. “But now that we see a molecular mechanism whereby cell fate can be determined by autophagy, we hope to discover patient populations that could benefit from drugs that inhibit this action.” ![]()
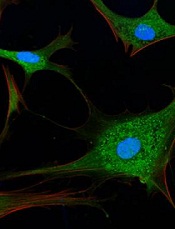
Credit: Sarah Pfau
SAN DIEGO—New research suggests that autophagy may allow cancer cells to recover and divide, rather than die, when faced with chemotherapy.
“What we showed is that if this mechanism doesn’t work right—for example, if autophagy is too high or if the target regulated by autophagy isn’t around—cancer cells may be able to rescue themselves from death caused by chemotherapies,” said study author Andrew Thorburn, PhD, of the University of Colorado Denver.
He and his colleagues believe this finding has important implications. It demonstrates a mechanism whereby autophagy controls cell death, and it further reinforces the clinical potential of inhibiting autophagy to sensitize cancer cells to chemotherapy.
Dr Thorburn and his colleagues recounted their research in Cell Reports and presented it in an education session at the AACR Annual Meeting 2014.
The researchers had set out to examine how autophagy affects canonical death receptor-induced mitochondrial outer membrane permeabilization (MOMP) and apoptosis. They found that MOMP occurs at variable times in cells, and it’s delayed by autophagy.
Furthermore, autophagy leads to inefficient MOMP. This causes some cells to die via a slower process than typical apoptosis, which allows them to eventually recover and divide.
Specifically, the researchers found that, as a cancer cell begins to die, mitochondrial cell walls break down. And the cell’s mitochondria release proteins via MOMP.
But then, high autophagy allows the cell to encapsulate and “digest” these released proteins before MOMP can keep the cell well and truly dead. The cell recovers and goes on to divide.
“The implication here is that if you inhibit autophagy, you’d make this less likely to happen; ie, when you kill cancer cells, they would stay dead,” Dr Thorburn said.
He and his colleagues also found that autophagy depends on the target PUMA to regulate cell death. When PUMA is absent, it doesn’t matter if autophagy is inhibited. Without the communicating action of PUMA, cancer cells evade apoptosis and continue to survive.
The researchers said this suggests autophagy can control apoptosis via a regulator that makes MOMP faster and more efficient, thus ensuring the rapid completion of apoptosis.
“Autophagy is complex and, as yet, not fully understood,” Dr Thorburn said. “But now that we see a molecular mechanism whereby cell fate can be determined by autophagy, we hope to discover patient populations that could benefit from drugs that inhibit this action.” ![]()
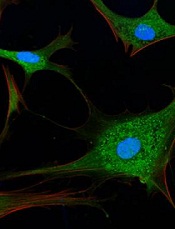
Credit: Sarah Pfau
SAN DIEGO—New research suggests that autophagy may allow cancer cells to recover and divide, rather than die, when faced with chemotherapy.
“What we showed is that if this mechanism doesn’t work right—for example, if autophagy is too high or if the target regulated by autophagy isn’t around—cancer cells may be able to rescue themselves from death caused by chemotherapies,” said study author Andrew Thorburn, PhD, of the University of Colorado Denver.
He and his colleagues believe this finding has important implications. It demonstrates a mechanism whereby autophagy controls cell death, and it further reinforces the clinical potential of inhibiting autophagy to sensitize cancer cells to chemotherapy.
Dr Thorburn and his colleagues recounted their research in Cell Reports and presented it in an education session at the AACR Annual Meeting 2014.
The researchers had set out to examine how autophagy affects canonical death receptor-induced mitochondrial outer membrane permeabilization (MOMP) and apoptosis. They found that MOMP occurs at variable times in cells, and it’s delayed by autophagy.
Furthermore, autophagy leads to inefficient MOMP. This causes some cells to die via a slower process than typical apoptosis, which allows them to eventually recover and divide.
Specifically, the researchers found that, as a cancer cell begins to die, mitochondrial cell walls break down. And the cell’s mitochondria release proteins via MOMP.
But then, high autophagy allows the cell to encapsulate and “digest” these released proteins before MOMP can keep the cell well and truly dead. The cell recovers and goes on to divide.
“The implication here is that if you inhibit autophagy, you’d make this less likely to happen; ie, when you kill cancer cells, they would stay dead,” Dr Thorburn said.
He and his colleagues also found that autophagy depends on the target PUMA to regulate cell death. When PUMA is absent, it doesn’t matter if autophagy is inhibited. Without the communicating action of PUMA, cancer cells evade apoptosis and continue to survive.
The researchers said this suggests autophagy can control apoptosis via a regulator that makes MOMP faster and more efficient, thus ensuring the rapid completion of apoptosis.
“Autophagy is complex and, as yet, not fully understood,” Dr Thorburn said. “But now that we see a molecular mechanism whereby cell fate can be determined by autophagy, we hope to discover patient populations that could benefit from drugs that inhibit this action.” ![]()


