User login
Editor’s Note: This is the first installment of a six-part series that will review key concepts and articles that ob.gyns. can use to prepare for the American Board of Obstetrics and Gynecology Maintenance of Certification examination. The series is adapted from Ob/Gyn Board Master (obgynboardmaster.com), an online board review course created by Erudyte Inc. The series will cover key topics across the specialty, as well as general test-taking and study tips. This month’s edition of the Board Exam Corner focuses on urinary incontinence.
The literature
The American College of Obstetricians and Gynecologists and the American Urogynecologic Society recently published an updated Practice Bulletin regarding the diagnosis and management of urinary incontinence. Practice Bulletin No. 155 was also a maintenance of certification (MOC) assignment for 2016. The contents of this article are critical as urinary incontinence is a prevalent and treatable condition, and it will likely be part of this year’s board examination. This month’s Board Corner will review the key elements of the updated guidelines.
Let’s begin with a possible medical board question: An 80-year old patient has urinary leakage as a result of severe arthritis and poor vision, and is unable to reach the bathroom in time. What is the diagnosis?
A. Mixed urinary incontinence
B. Extraurethral incontinence
C. Functional incontinence
D. Postural incontinence
E. Ectopic ureter
The answer is C.
Functional incontinence occurs because of cognitive or mobility impairments in the presence of an intact lower urinary tract. The patient in the vignette has “restricted mobility” and a physical impairment that leads to urinary incontinence.
A is incorrect because mixed incontinence is an involuntary loss of urine associated with urgency and with physical exertion.
B and E are incorrect because extraurethral incontinence is urine leakage through channels other than the urethral meatus (e.g., vesicovaginal fistula or ectopic ureter).
D is incorrect because postural incontinence is the involuntary loss of urine associated with change in body positions (e.g., from sitting to standing).
The key points to remember are:
• Urinary incontinence is a prevalent condition that is treatable despite what many women believe.
• There are several types of incontinence but the main types are stress, urgency, and mixed incontinence.
• Basic office evaluation includes urinalysis and postvoid residual, but not urodynamics or cystoscopy.
• Treatment of stress incontinence includes weight loss, fluid management, pelvic floor muscle exercises (with or without assistance from a physical therapist), and suburethral sling or bulking agent injections.
• Treatment of urgency urinary incontinence includes bladder training, fluid management, decreasing caffeine, antimuscarinic and beta-3 agonists, and third-line treatments (botulinum toxin A injection, sacral neuromodulation, or tibial nerve stimulation).
• The mnemonic DIAPPERS is useful in remembering all of the reversible, nongenitourinary (i.e., functional) causes of incontinence. 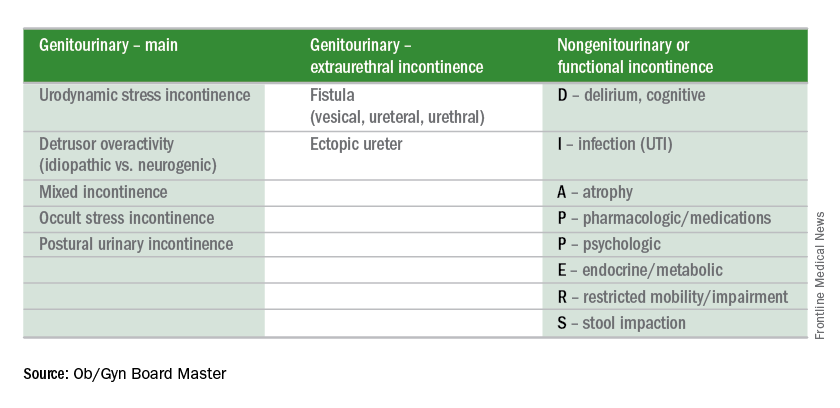
Test-taking tip of the month
If you finish the test early, take the time to go back to any question for which you made an educated guess. Reread the question carefully. Don’t change your answer unless there is a very good reason for doing so because your first impression is usually the right one. Don’t change an answer just because you have a gut feeling. However, there are good reasons to change your answers when you go back. For instance, consider changing your answer if rereading the question helped you to better understand what is being asked, if you reconsidered and conceptualized a better answer, if you remembered a new piece of information, or if you learned something from a later question that will help you better answer the earlier question.
Reference
Obstet Gynecol. 2015 Nov;126(5): e66-81.
Dr. Sam Siddighi is editor-in-chief of the Ob/Gyn Board Master and director of female pelvic medicine and reconstructive surgery and director of grand rounds at Loma Linda University Health in California. Ob.Gyn. News and Ob/Gyn Board Master are owned by the same parent company, Frontline Medical Communications.
Editor’s Note: This is the first installment of a six-part series that will review key concepts and articles that ob.gyns. can use to prepare for the American Board of Obstetrics and Gynecology Maintenance of Certification examination. The series is adapted from Ob/Gyn Board Master (obgynboardmaster.com), an online board review course created by Erudyte Inc. The series will cover key topics across the specialty, as well as general test-taking and study tips. This month’s edition of the Board Exam Corner focuses on urinary incontinence.
The literature
The American College of Obstetricians and Gynecologists and the American Urogynecologic Society recently published an updated Practice Bulletin regarding the diagnosis and management of urinary incontinence. Practice Bulletin No. 155 was also a maintenance of certification (MOC) assignment for 2016. The contents of this article are critical as urinary incontinence is a prevalent and treatable condition, and it will likely be part of this year’s board examination. This month’s Board Corner will review the key elements of the updated guidelines.
Let’s begin with a possible medical board question: An 80-year old patient has urinary leakage as a result of severe arthritis and poor vision, and is unable to reach the bathroom in time. What is the diagnosis?
A. Mixed urinary incontinence
B. Extraurethral incontinence
C. Functional incontinence
D. Postural incontinence
E. Ectopic ureter
The answer is C.
Functional incontinence occurs because of cognitive or mobility impairments in the presence of an intact lower urinary tract. The patient in the vignette has “restricted mobility” and a physical impairment that leads to urinary incontinence.
A is incorrect because mixed incontinence is an involuntary loss of urine associated with urgency and with physical exertion.
B and E are incorrect because extraurethral incontinence is urine leakage through channels other than the urethral meatus (e.g., vesicovaginal fistula or ectopic ureter).
D is incorrect because postural incontinence is the involuntary loss of urine associated with change in body positions (e.g., from sitting to standing).
The key points to remember are:
• Urinary incontinence is a prevalent condition that is treatable despite what many women believe.
• There are several types of incontinence but the main types are stress, urgency, and mixed incontinence.
• Basic office evaluation includes urinalysis and postvoid residual, but not urodynamics or cystoscopy.
• Treatment of stress incontinence includes weight loss, fluid management, pelvic floor muscle exercises (with or without assistance from a physical therapist), and suburethral sling or bulking agent injections.
• Treatment of urgency urinary incontinence includes bladder training, fluid management, decreasing caffeine, antimuscarinic and beta-3 agonists, and third-line treatments (botulinum toxin A injection, sacral neuromodulation, or tibial nerve stimulation).
• The mnemonic DIAPPERS is useful in remembering all of the reversible, nongenitourinary (i.e., functional) causes of incontinence. 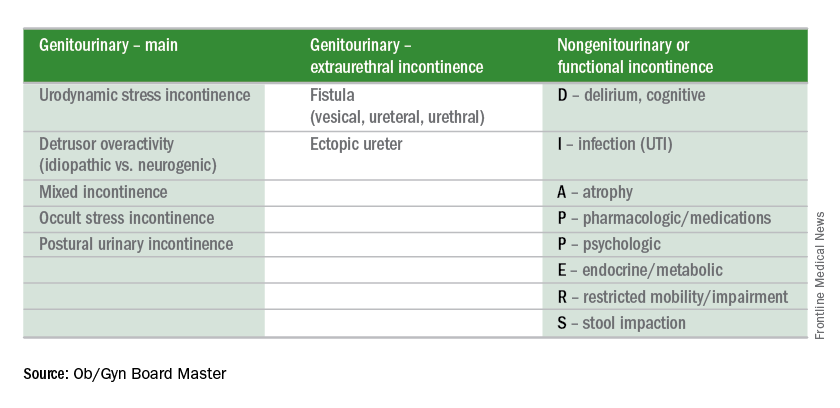
Test-taking tip of the month
If you finish the test early, take the time to go back to any question for which you made an educated guess. Reread the question carefully. Don’t change your answer unless there is a very good reason for doing so because your first impression is usually the right one. Don’t change an answer just because you have a gut feeling. However, there are good reasons to change your answers when you go back. For instance, consider changing your answer if rereading the question helped you to better understand what is being asked, if you reconsidered and conceptualized a better answer, if you remembered a new piece of information, or if you learned something from a later question that will help you better answer the earlier question.
Reference
Obstet Gynecol. 2015 Nov;126(5): e66-81.
Dr. Sam Siddighi is editor-in-chief of the Ob/Gyn Board Master and director of female pelvic medicine and reconstructive surgery and director of grand rounds at Loma Linda University Health in California. Ob.Gyn. News and Ob/Gyn Board Master are owned by the same parent company, Frontline Medical Communications.
Editor’s Note: This is the first installment of a six-part series that will review key concepts and articles that ob.gyns. can use to prepare for the American Board of Obstetrics and Gynecology Maintenance of Certification examination. The series is adapted from Ob/Gyn Board Master (obgynboardmaster.com), an online board review course created by Erudyte Inc. The series will cover key topics across the specialty, as well as general test-taking and study tips. This month’s edition of the Board Exam Corner focuses on urinary incontinence.
The literature
The American College of Obstetricians and Gynecologists and the American Urogynecologic Society recently published an updated Practice Bulletin regarding the diagnosis and management of urinary incontinence. Practice Bulletin No. 155 was also a maintenance of certification (MOC) assignment for 2016. The contents of this article are critical as urinary incontinence is a prevalent and treatable condition, and it will likely be part of this year’s board examination. This month’s Board Corner will review the key elements of the updated guidelines.
Let’s begin with a possible medical board question: An 80-year old patient has urinary leakage as a result of severe arthritis and poor vision, and is unable to reach the bathroom in time. What is the diagnosis?
A. Mixed urinary incontinence
B. Extraurethral incontinence
C. Functional incontinence
D. Postural incontinence
E. Ectopic ureter
The answer is C.
Functional incontinence occurs because of cognitive or mobility impairments in the presence of an intact lower urinary tract. The patient in the vignette has “restricted mobility” and a physical impairment that leads to urinary incontinence.
A is incorrect because mixed incontinence is an involuntary loss of urine associated with urgency and with physical exertion.
B and E are incorrect because extraurethral incontinence is urine leakage through channels other than the urethral meatus (e.g., vesicovaginal fistula or ectopic ureter).
D is incorrect because postural incontinence is the involuntary loss of urine associated with change in body positions (e.g., from sitting to standing).
The key points to remember are:
• Urinary incontinence is a prevalent condition that is treatable despite what many women believe.
• There are several types of incontinence but the main types are stress, urgency, and mixed incontinence.
• Basic office evaluation includes urinalysis and postvoid residual, but not urodynamics or cystoscopy.
• Treatment of stress incontinence includes weight loss, fluid management, pelvic floor muscle exercises (with or without assistance from a physical therapist), and suburethral sling or bulking agent injections.
• Treatment of urgency urinary incontinence includes bladder training, fluid management, decreasing caffeine, antimuscarinic and beta-3 agonists, and third-line treatments (botulinum toxin A injection, sacral neuromodulation, or tibial nerve stimulation).
• The mnemonic DIAPPERS is useful in remembering all of the reversible, nongenitourinary (i.e., functional) causes of incontinence. 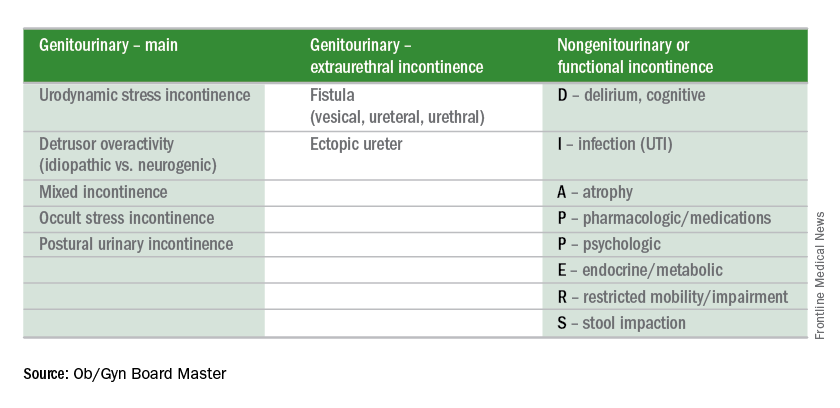
Test-taking tip of the month
If you finish the test early, take the time to go back to any question for which you made an educated guess. Reread the question carefully. Don’t change your answer unless there is a very good reason for doing so because your first impression is usually the right one. Don’t change an answer just because you have a gut feeling. However, there are good reasons to change your answers when you go back. For instance, consider changing your answer if rereading the question helped you to better understand what is being asked, if you reconsidered and conceptualized a better answer, if you remembered a new piece of information, or if you learned something from a later question that will help you better answer the earlier question.
Reference
Obstet Gynecol. 2015 Nov;126(5): e66-81.
Dr. Sam Siddighi is editor-in-chief of the Ob/Gyn Board Master and director of female pelvic medicine and reconstructive surgery and director of grand rounds at Loma Linda University Health in California. Ob.Gyn. News and Ob/Gyn Board Master are owned by the same parent company, Frontline Medical Communications.

