User login
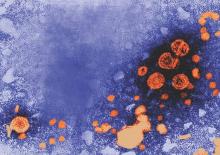
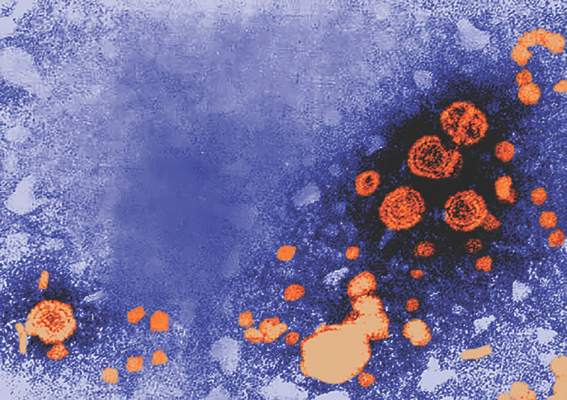
The antiviral drug tenofovir disoproxil fumarate (TDF) can be used by expectant mothers infected with the hepatitis B virus to decrease HBV DNA levels and, therefore, significantly decrease the risk of passing the virus onto their children, according to a new study.
“A small but growing body of evidence has suggested that antiviral treatment may reduce the risk of mother-to-child transmission among mothers with an HBV DNA level of more than 6 log10 copies per milliliter, although quality studies are lacking and the existing studies have shown conflicting results,” wrote Dr. Calvin Q. Pan of New York University and coauthors in a study published in the New England Journal of Medicine (2016;374[24]:2324-34. doi: 10.1056/NEJMoa1508660).
An international research team recruited pregnant women in China – all of whom were positive for hepatitis B e antigen and had a viral load of at least 200,000 IU/mL – from March 2012 through June 2013. A total of 200 women were selected for inclusion and randomized into either a control cohort, or a cohort taking TDF; 100 mothers with 88 infants ultimately completed the study in the control group, while 97 mothers with 92 children completed the study in the TDF cohort.
Women on TDF were given a 300-mg dose orally every day, beginning 30-32 weeks into their pregnancy and continuing through 4 weeks after giving birth. Follow-up examinations were conducted at 4, 12, 24, and 28 weeks post partum, and the primary outcome was determining transmission of HBV from mother to child, with transmission defined as an infant having an HBV DNA level higher than 20 IU/mL. Patients in the control group were given “usual care without antiviral therapy.”
Mothers on TDF had lower HBV DNA levels at delivery, with 68% (66/97) dropping to under 200,000 IU/mL levels versus just 2% (2/100) in the control group having levels under that threshold (P less than .001). At 28-week follow-up examinations, intent-to-treat analysis showed that 5% (5/97) of infants born to mothers on TDF were found to have HBV DNA levels higher than 20 IU/mL, compared with 18% of infants born to mothers in the control group (P = .007). In per-protocol analysis, none of the infants whose mothers were taking TDF had contracted the disease; on the other hand, 7% (6/88) of those in the control group had (P = .01). Rates of birth defects and HBV serologic outcomes were not significantly different between the two cohorts.
“TDF [may] be useful for preventing mother-to-child transmission, which is a critical step toward the global eradication of HBV and a reduction in the incidence of liver cancer,” Dr. Pan and his colleagues said, adding that “the postpartum cessation of TDF requires close monitoring” in order to further understand the drug’s longer-term effects.
The study was funded by Gilead Sciences. Dr. Pan reported grant support from Gilead Sciences during the conduct of the study; grant support from Merck, grant support and personal fees from Gilead Sciences and Bristol-Myers Squibb; and personal fees from Johnson and Johnson and AbbVie outside the submitted work.
The antiviral drug tenofovir disoproxil fumarate (TDF) can be used by expectant mothers infected with the hepatitis B virus to decrease HBV DNA levels and, therefore, significantly decrease the risk of passing the virus onto their children, according to a new study.
“A small but growing body of evidence has suggested that antiviral treatment may reduce the risk of mother-to-child transmission among mothers with an HBV DNA level of more than 6 log10 copies per milliliter, although quality studies are lacking and the existing studies have shown conflicting results,” wrote Dr. Calvin Q. Pan of New York University and coauthors in a study published in the New England Journal of Medicine (2016;374[24]:2324-34. doi: 10.1056/NEJMoa1508660).
An international research team recruited pregnant women in China – all of whom were positive for hepatitis B e antigen and had a viral load of at least 200,000 IU/mL – from March 2012 through June 2013. A total of 200 women were selected for inclusion and randomized into either a control cohort, or a cohort taking TDF; 100 mothers with 88 infants ultimately completed the study in the control group, while 97 mothers with 92 children completed the study in the TDF cohort.
Women on TDF were given a 300-mg dose orally every day, beginning 30-32 weeks into their pregnancy and continuing through 4 weeks after giving birth. Follow-up examinations were conducted at 4, 12, 24, and 28 weeks post partum, and the primary outcome was determining transmission of HBV from mother to child, with transmission defined as an infant having an HBV DNA level higher than 20 IU/mL. Patients in the control group were given “usual care without antiviral therapy.”
Mothers on TDF had lower HBV DNA levels at delivery, with 68% (66/97) dropping to under 200,000 IU/mL levels versus just 2% (2/100) in the control group having levels under that threshold (P less than .001). At 28-week follow-up examinations, intent-to-treat analysis showed that 5% (5/97) of infants born to mothers on TDF were found to have HBV DNA levels higher than 20 IU/mL, compared with 18% of infants born to mothers in the control group (P = .007). In per-protocol analysis, none of the infants whose mothers were taking TDF had contracted the disease; on the other hand, 7% (6/88) of those in the control group had (P = .01). Rates of birth defects and HBV serologic outcomes were not significantly different between the two cohorts.
“TDF [may] be useful for preventing mother-to-child transmission, which is a critical step toward the global eradication of HBV and a reduction in the incidence of liver cancer,” Dr. Pan and his colleagues said, adding that “the postpartum cessation of TDF requires close monitoring” in order to further understand the drug’s longer-term effects.
The study was funded by Gilead Sciences. Dr. Pan reported grant support from Gilead Sciences during the conduct of the study; grant support from Merck, grant support and personal fees from Gilead Sciences and Bristol-Myers Squibb; and personal fees from Johnson and Johnson and AbbVie outside the submitted work.
The antiviral drug tenofovir disoproxil fumarate (TDF) can be used by expectant mothers infected with the hepatitis B virus to decrease HBV DNA levels and, therefore, significantly decrease the risk of passing the virus onto their children, according to a new study.
“A small but growing body of evidence has suggested that antiviral treatment may reduce the risk of mother-to-child transmission among mothers with an HBV DNA level of more than 6 log10 copies per milliliter, although quality studies are lacking and the existing studies have shown conflicting results,” wrote Dr. Calvin Q. Pan of New York University and coauthors in a study published in the New England Journal of Medicine (2016;374[24]:2324-34. doi: 10.1056/NEJMoa1508660).
An international research team recruited pregnant women in China – all of whom were positive for hepatitis B e antigen and had a viral load of at least 200,000 IU/mL – from March 2012 through June 2013. A total of 200 women were selected for inclusion and randomized into either a control cohort, or a cohort taking TDF; 100 mothers with 88 infants ultimately completed the study in the control group, while 97 mothers with 92 children completed the study in the TDF cohort.
Women on TDF were given a 300-mg dose orally every day, beginning 30-32 weeks into their pregnancy and continuing through 4 weeks after giving birth. Follow-up examinations were conducted at 4, 12, 24, and 28 weeks post partum, and the primary outcome was determining transmission of HBV from mother to child, with transmission defined as an infant having an HBV DNA level higher than 20 IU/mL. Patients in the control group were given “usual care without antiviral therapy.”
Mothers on TDF had lower HBV DNA levels at delivery, with 68% (66/97) dropping to under 200,000 IU/mL levels versus just 2% (2/100) in the control group having levels under that threshold (P less than .001). At 28-week follow-up examinations, intent-to-treat analysis showed that 5% (5/97) of infants born to mothers on TDF were found to have HBV DNA levels higher than 20 IU/mL, compared with 18% of infants born to mothers in the control group (P = .007). In per-protocol analysis, none of the infants whose mothers were taking TDF had contracted the disease; on the other hand, 7% (6/88) of those in the control group had (P = .01). Rates of birth defects and HBV serologic outcomes were not significantly different between the two cohorts.
“TDF [may] be useful for preventing mother-to-child transmission, which is a critical step toward the global eradication of HBV and a reduction in the incidence of liver cancer,” Dr. Pan and his colleagues said, adding that “the postpartum cessation of TDF requires close monitoring” in order to further understand the drug’s longer-term effects.
The study was funded by Gilead Sciences. Dr. Pan reported grant support from Gilead Sciences during the conduct of the study; grant support from Merck, grant support and personal fees from Gilead Sciences and Bristol-Myers Squibb; and personal fees from Johnson and Johnson and AbbVie outside the submitted work.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: A 300-mg daily dose of tenofovir disoproxil fumarate significantly reduced the risk of pregnant mothers with HBV infection transmitting the disease to their children.
Major finding: In an intent-to-treat analysis, only 5% of children born to mothers taking TDF during pregnancy were found to have contracted the disease, versus 18% in the control group (P = .007); similarly, in the per-protocol analysis, 0% of children born to mothers taking TDF had HBV vs. 7% in the control group (P = .01).
Data source: A multicenter, open label, randomized, parallel-group study of 197 HBV-positive pregnant women from March 2012 through June 2013.
Disclosures: The study was funded by Gilead Sciences. Dr. Pan reported grant support from Gilead Sciences during the conduct of the study; grant support from Merck, grant support and personal fees from Gilead Sciences and Bristol-Myers Squibb; and personal fees from Johnson and Johnson and AbbVie outside the submitted work.