User login
The Centers for Disease Control and Prevention (CDC) has published its 2015 immunization schedules for adults and for children and adolescents.1,2 There are very few changes from 2014 recommendations; most are alterations in the footnotes to clarify complex and confusing catch-up schedules. The 2 substantive changes have been discussed in previous Practice Alerts:
- the addition of the 13-valent pneumococcal conjugate vaccine (PCV13) to the 23-valent pneumococcal polysaccharide vaccine (PPSV23) in the routine older-adult recommendations;3
- a stated preference for live attenuated influenza vaccine (LAIV) for children ages 2 through 8 years.4
The LAIV statement came under criticism at the recent meeting of the Advisory Committee on Immunization Practices (ACIP). A prospective case-control study conducted at 5 sites in the US Flu Vaccine Effectiveness Network looked at the effectiveness of LAIV and inactivated influenza vaccine (IIV) against medically-attended influenza in 3 flu seasons: 2011-2012, 2012-2013, and 2013-2014.5 The results differed by age.
In patients ages 9 to 18 years, the vaccines were equally effective in all 3 seasons, with effectiveness ranging between 32% and 67% depending on the year and the vaccine. In children ages 2 to 8 years, LAIV appeared to be more effective than IIV in the 2011-2012 and 2012-2013 seasons, with odds ratios of .54 and .74, respectively (although not statistically significant). In the 2013-2014 season, however, IIV was the more effective vaccine, with a statistically significant odds ratio of 5.17.
In the immediate past season, the predominant influenza strain circulating was H1N1 pdm09, against which the LAIV appeared to be minimally, if at all, effective. These results were replicated in a study conducted by the LAIV producer, MedImmune, and in a study conducted by the United States Air Force.5 Based on the predominant circulating strains in the 2014-2015 flu season, ACIP has not changed its preference for LAIV for ages 2 through 8 years.
Typhoid fever vaccines
Late last year, ACIP updated its recommendations on the use of typhoid vaccines. They had last been reviewed with the recommendations in 1994, and surprisingly few changes were needed. Roughly 400 cases of typhoid fever occur in the United States each year, mostly in travelers returning from India, Bangladesh, or Pakistan. Each year, worldwide, there are an estimated 20 million cases of typhoid and 200,000 related deaths.6
ACIP recommends typhoid vaccine for travelers to areas within Asia, Africa, and Latin America that present a risk of exposure to Salmonella typhi. Country-specific recommendations can be found on the CDC travel Web site (http://wwwnc.cdc.gov/travel). Others for whom the vaccine is recommended: those who have a household contact with S. typhi or who have had other intimate exposure to a chronic S. typhi carrier (eg, someone who has excreted S. typhi in stool or urine for a year or more); and microbiologists and lab workers who might be exposed to S. typhi.
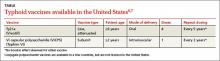
Two typhoid vaccines are available and neither is listed as preferred. One is a live vaccine (Ty21a) taken orally in 4 doses, one dose every other day over 7 days. The other is a killed vaccine (Vi capsular polysaccharide vaccine [ViCPS]), given intramuscularly in a single dose (TABLE).6,7 Ty21a is approved for individuals ages 6 years and older; ViCPS for ages 2 years and older.
Anticipated changes this year
HPV vaccine
Two human papillomavirus (HPV) vaccines are available in the United States: Gardasil, a quadrivalent vaccine (HPV4) that protects against types 6, 11, 16, and 18, and Cervarix, a bivalent product (HPV2) protecting against types 16 and 18. Both vaccines contain antigens of HPV subtypes 16 and 18, which cause 70% of cervical cancers in the United States and the rest of the world. The HPV4 is soon to be replaced with a 9-valent product that will contain antigens for types 6, 11, 16, 18, 31, 33, 45, 52, and 58, which are responsible for 90% of cervical cancers worldwide.8
Many countries now allow a 2-dose schedule for both HPV2 and HPV4. For girls younger than 15 years, the World Health Organization recommends a 2-dose schedule for HPV vaccines, 6 to 12 months apart.9 A 3-dose schedule is still recommended for those ages 15 years or older and for those who are immunocompromised.
ACIP will assess studies on the effectiveness of 2-dose schedules of HPV2, HPV4, and HPV9, and will make recommendations within the next year. Although the manufacturers of the HPV vaccines have not applied to the US Food and Drug Administration (FDA) for approval of a 2-dose schedule, ACIP will still consider the possibility of recommending it. The current 3-dose schedule is seen as a barrier to HPV vaccination and one reason why the rate of vaccination in girls in the United States remains at a disappointing 37.6% for 3 doses, 47.7% for at least 2 doses, and 57.3% for 1 dose.10
ACIP will attempt to address multiple issues in the next year regarding HPV vaccination: HPV9 use in men and women, including the possibility of catch-up schedules for those who have received HPV4 or HPV2; the possibility of using a 2-dose schedule for all HPV vaccines; and ways to increase uptake of this cancer-preventing vaccine.
Meningococcus type B
With the widespread use of quadrivalent meningococcal vaccines (MCV4), meningococcal meningitis has declined markedly in all age groups. The incidence of disease caused by meningococcal serotype B, which MCV4 does not protect against, has also declined from 0.3 to less than 0.1 cases per 100,000 between 1994 and 2013.11 The highest incidence occurs in infants under the age of 1 year, at 1.5/100,000, with 67% of cases attributable to serotype B. A slight bump in risk is seen with those ages 19 to 22 years (0.2/100,000) compared with other adolescents and adults.
While serotype B accounts for a larger proportion of all meningococcal disease than it did before, it is still relatively rare. In the United States between 2010 and 2012, annual cases totaled 48 to 56.11 Groups that are at higher risk of infection include those with complement deficiencies or asplenia (functional or anatomical), microbiologists and lab personnel who work with the organism, and those who have close contact with infected individuals.
In the past few years, well-publicized outbreaks of meningococcus B have occurred on some university campuses. Princeton had 9 cases, and the University of California at Santa Barbara had 4.11 This led to the use of meningococcal B vaccine as an outbreak control measure, with permission from the FDA before the vaccine was licensed. While these outbreaks created an impression of increased risks on college campuses, college students are actually at lower risk of type B meningococcal disease than others of the same age.11
This year, 2 meningococcal B vaccines will be available in the United States. The first, rLP2086, Trumenba (Pfizer) is a 3-dose series that was licensed in late 2014. The second, 4CMenB, Bexsero (Novartis) is a 2-dose series that received FDA approval in January 2015. Both are licensed for individuals ages 10 to 25 years. Formulating a recommendation for the use of these vaccines will be challenging because of several factors: the multiple dose schedules, the low rate of meningococcal B disease, and the age group for whom the vaccines are licensed.
1. Centers for Disease Control and Prevention. Recommended adult immunization schedule: United States - 2015. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf. Accessed February 11, 2015.
2. Centers for Disease Control and Prevention. Birth – 18 years & “Catch-up” immunization schedules. United States, 2015. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html. Accessed January 27, 2015.
3. Campos-Outcalt D. Pneumococcal vaccines for older adults: getting the timing right. J Fam Pract. 2014;63:730-733.
4. Campos-Outcalt D. The 2014-2015 influenza season: what you need to know. J Fam Pract. 2014;63:532-533.
5. Flannery B. Update on effectiveness of live-attenuated versus inactivated influenza vaccine in children and adolescents aged 2-18 years. Presented at: Advisory Committee on Immunization Practices; October 29, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/flu-03-flannery.pdf. Accessed January 27, 2015.
6. Jackson BR. Typhoid and typhoid vaccines. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/Typhoid-02-Jackson.pdf. Accessed January 27, 2015.
7. Centers for Disease Control and Prevention. Typhoid immunization—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1994:43:1-7.
8. Luxembourg A. 9-valent HPV vaccine program key results--Part III. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/HPV-02-Luxembourg.pdf. Accessed January 27, 2015.
9. Markowitz L. 2-dose HPV vaccination schedules. Presented at: Advisory Committee on Immunization Practices; June 25, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-06/HPV-04-Markowitz.pdf. Accessed January 27, 2015.
10. Stokley S, Jeyarajah J, Yankey D, et al; Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; Centers for Disease Control and Prevention (CDC). Human papillomavirus vaccination coverage among adolescents, 2007-2013, and postlicensure safety monitoring, 2006-2014—United States. MMWR Morb Mortal Wkly Rep. 2014;63:620-624.
11. MacNeil J. Epidemiology of serogroup B meningococcal disease, United States. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/mening-02-MacNeil.pdf. Accessed January 27, 2015.
The Centers for Disease Control and Prevention (CDC) has published its 2015 immunization schedules for adults and for children and adolescents.1,2 There are very few changes from 2014 recommendations; most are alterations in the footnotes to clarify complex and confusing catch-up schedules. The 2 substantive changes have been discussed in previous Practice Alerts:
- the addition of the 13-valent pneumococcal conjugate vaccine (PCV13) to the 23-valent pneumococcal polysaccharide vaccine (PPSV23) in the routine older-adult recommendations;3
- a stated preference for live attenuated influenza vaccine (LAIV) for children ages 2 through 8 years.4
The LAIV statement came under criticism at the recent meeting of the Advisory Committee on Immunization Practices (ACIP). A prospective case-control study conducted at 5 sites in the US Flu Vaccine Effectiveness Network looked at the effectiveness of LAIV and inactivated influenza vaccine (IIV) against medically-attended influenza in 3 flu seasons: 2011-2012, 2012-2013, and 2013-2014.5 The results differed by age.
In patients ages 9 to 18 years, the vaccines were equally effective in all 3 seasons, with effectiveness ranging between 32% and 67% depending on the year and the vaccine. In children ages 2 to 8 years, LAIV appeared to be more effective than IIV in the 2011-2012 and 2012-2013 seasons, with odds ratios of .54 and .74, respectively (although not statistically significant). In the 2013-2014 season, however, IIV was the more effective vaccine, with a statistically significant odds ratio of 5.17.
In the immediate past season, the predominant influenza strain circulating was H1N1 pdm09, against which the LAIV appeared to be minimally, if at all, effective. These results were replicated in a study conducted by the LAIV producer, MedImmune, and in a study conducted by the United States Air Force.5 Based on the predominant circulating strains in the 2014-2015 flu season, ACIP has not changed its preference for LAIV for ages 2 through 8 years.
Typhoid fever vaccines
Late last year, ACIP updated its recommendations on the use of typhoid vaccines. They had last been reviewed with the recommendations in 1994, and surprisingly few changes were needed. Roughly 400 cases of typhoid fever occur in the United States each year, mostly in travelers returning from India, Bangladesh, or Pakistan. Each year, worldwide, there are an estimated 20 million cases of typhoid and 200,000 related deaths.6
ACIP recommends typhoid vaccine for travelers to areas within Asia, Africa, and Latin America that present a risk of exposure to Salmonella typhi. Country-specific recommendations can be found on the CDC travel Web site (http://wwwnc.cdc.gov/travel). Others for whom the vaccine is recommended: those who have a household contact with S. typhi or who have had other intimate exposure to a chronic S. typhi carrier (eg, someone who has excreted S. typhi in stool or urine for a year or more); and microbiologists and lab workers who might be exposed to S. typhi.
Two typhoid vaccines are available and neither is listed as preferred. One is a live vaccine (Ty21a) taken orally in 4 doses, one dose every other day over 7 days. The other is a killed vaccine (Vi capsular polysaccharide vaccine [ViCPS]), given intramuscularly in a single dose (TABLE).6,7 Ty21a is approved for individuals ages 6 years and older; ViCPS for ages 2 years and older.
Anticipated changes this year
HPV vaccine
Two human papillomavirus (HPV) vaccines are available in the United States: Gardasil, a quadrivalent vaccine (HPV4) that protects against types 6, 11, 16, and 18, and Cervarix, a bivalent product (HPV2) protecting against types 16 and 18. Both vaccines contain antigens of HPV subtypes 16 and 18, which cause 70% of cervical cancers in the United States and the rest of the world. The HPV4 is soon to be replaced with a 9-valent product that will contain antigens for types 6, 11, 16, 18, 31, 33, 45, 52, and 58, which are responsible for 90% of cervical cancers worldwide.8
Many countries now allow a 2-dose schedule for both HPV2 and HPV4. For girls younger than 15 years, the World Health Organization recommends a 2-dose schedule for HPV vaccines, 6 to 12 months apart.9 A 3-dose schedule is still recommended for those ages 15 years or older and for those who are immunocompromised.
ACIP will assess studies on the effectiveness of 2-dose schedules of HPV2, HPV4, and HPV9, and will make recommendations within the next year. Although the manufacturers of the HPV vaccines have not applied to the US Food and Drug Administration (FDA) for approval of a 2-dose schedule, ACIP will still consider the possibility of recommending it. The current 3-dose schedule is seen as a barrier to HPV vaccination and one reason why the rate of vaccination in girls in the United States remains at a disappointing 37.6% for 3 doses, 47.7% for at least 2 doses, and 57.3% for 1 dose.10
ACIP will attempt to address multiple issues in the next year regarding HPV vaccination: HPV9 use in men and women, including the possibility of catch-up schedules for those who have received HPV4 or HPV2; the possibility of using a 2-dose schedule for all HPV vaccines; and ways to increase uptake of this cancer-preventing vaccine.
Meningococcus type B
With the widespread use of quadrivalent meningococcal vaccines (MCV4), meningococcal meningitis has declined markedly in all age groups. The incidence of disease caused by meningococcal serotype B, which MCV4 does not protect against, has also declined from 0.3 to less than 0.1 cases per 100,000 between 1994 and 2013.11 The highest incidence occurs in infants under the age of 1 year, at 1.5/100,000, with 67% of cases attributable to serotype B. A slight bump in risk is seen with those ages 19 to 22 years (0.2/100,000) compared with other adolescents and adults.
While serotype B accounts for a larger proportion of all meningococcal disease than it did before, it is still relatively rare. In the United States between 2010 and 2012, annual cases totaled 48 to 56.11 Groups that are at higher risk of infection include those with complement deficiencies or asplenia (functional or anatomical), microbiologists and lab personnel who work with the organism, and those who have close contact with infected individuals.
In the past few years, well-publicized outbreaks of meningococcus B have occurred on some university campuses. Princeton had 9 cases, and the University of California at Santa Barbara had 4.11 This led to the use of meningococcal B vaccine as an outbreak control measure, with permission from the FDA before the vaccine was licensed. While these outbreaks created an impression of increased risks on college campuses, college students are actually at lower risk of type B meningococcal disease than others of the same age.11
This year, 2 meningococcal B vaccines will be available in the United States. The first, rLP2086, Trumenba (Pfizer) is a 3-dose series that was licensed in late 2014. The second, 4CMenB, Bexsero (Novartis) is a 2-dose series that received FDA approval in January 2015. Both are licensed for individuals ages 10 to 25 years. Formulating a recommendation for the use of these vaccines will be challenging because of several factors: the multiple dose schedules, the low rate of meningococcal B disease, and the age group for whom the vaccines are licensed.
The Centers for Disease Control and Prevention (CDC) has published its 2015 immunization schedules for adults and for children and adolescents.1,2 There are very few changes from 2014 recommendations; most are alterations in the footnotes to clarify complex and confusing catch-up schedules. The 2 substantive changes have been discussed in previous Practice Alerts:
- the addition of the 13-valent pneumococcal conjugate vaccine (PCV13) to the 23-valent pneumococcal polysaccharide vaccine (PPSV23) in the routine older-adult recommendations;3
- a stated preference for live attenuated influenza vaccine (LAIV) for children ages 2 through 8 years.4
The LAIV statement came under criticism at the recent meeting of the Advisory Committee on Immunization Practices (ACIP). A prospective case-control study conducted at 5 sites in the US Flu Vaccine Effectiveness Network looked at the effectiveness of LAIV and inactivated influenza vaccine (IIV) against medically-attended influenza in 3 flu seasons: 2011-2012, 2012-2013, and 2013-2014.5 The results differed by age.
In patients ages 9 to 18 years, the vaccines were equally effective in all 3 seasons, with effectiveness ranging between 32% and 67% depending on the year and the vaccine. In children ages 2 to 8 years, LAIV appeared to be more effective than IIV in the 2011-2012 and 2012-2013 seasons, with odds ratios of .54 and .74, respectively (although not statistically significant). In the 2013-2014 season, however, IIV was the more effective vaccine, with a statistically significant odds ratio of 5.17.
In the immediate past season, the predominant influenza strain circulating was H1N1 pdm09, against which the LAIV appeared to be minimally, if at all, effective. These results were replicated in a study conducted by the LAIV producer, MedImmune, and in a study conducted by the United States Air Force.5 Based on the predominant circulating strains in the 2014-2015 flu season, ACIP has not changed its preference for LAIV for ages 2 through 8 years.
Typhoid fever vaccines
Late last year, ACIP updated its recommendations on the use of typhoid vaccines. They had last been reviewed with the recommendations in 1994, and surprisingly few changes were needed. Roughly 400 cases of typhoid fever occur in the United States each year, mostly in travelers returning from India, Bangladesh, or Pakistan. Each year, worldwide, there are an estimated 20 million cases of typhoid and 200,000 related deaths.6
ACIP recommends typhoid vaccine for travelers to areas within Asia, Africa, and Latin America that present a risk of exposure to Salmonella typhi. Country-specific recommendations can be found on the CDC travel Web site (http://wwwnc.cdc.gov/travel). Others for whom the vaccine is recommended: those who have a household contact with S. typhi or who have had other intimate exposure to a chronic S. typhi carrier (eg, someone who has excreted S. typhi in stool or urine for a year or more); and microbiologists and lab workers who might be exposed to S. typhi.
Two typhoid vaccines are available and neither is listed as preferred. One is a live vaccine (Ty21a) taken orally in 4 doses, one dose every other day over 7 days. The other is a killed vaccine (Vi capsular polysaccharide vaccine [ViCPS]), given intramuscularly in a single dose (TABLE).6,7 Ty21a is approved for individuals ages 6 years and older; ViCPS for ages 2 years and older.
Anticipated changes this year
HPV vaccine
Two human papillomavirus (HPV) vaccines are available in the United States: Gardasil, a quadrivalent vaccine (HPV4) that protects against types 6, 11, 16, and 18, and Cervarix, a bivalent product (HPV2) protecting against types 16 and 18. Both vaccines contain antigens of HPV subtypes 16 and 18, which cause 70% of cervical cancers in the United States and the rest of the world. The HPV4 is soon to be replaced with a 9-valent product that will contain antigens for types 6, 11, 16, 18, 31, 33, 45, 52, and 58, which are responsible for 90% of cervical cancers worldwide.8
Many countries now allow a 2-dose schedule for both HPV2 and HPV4. For girls younger than 15 years, the World Health Organization recommends a 2-dose schedule for HPV vaccines, 6 to 12 months apart.9 A 3-dose schedule is still recommended for those ages 15 years or older and for those who are immunocompromised.
ACIP will assess studies on the effectiveness of 2-dose schedules of HPV2, HPV4, and HPV9, and will make recommendations within the next year. Although the manufacturers of the HPV vaccines have not applied to the US Food and Drug Administration (FDA) for approval of a 2-dose schedule, ACIP will still consider the possibility of recommending it. The current 3-dose schedule is seen as a barrier to HPV vaccination and one reason why the rate of vaccination in girls in the United States remains at a disappointing 37.6% for 3 doses, 47.7% for at least 2 doses, and 57.3% for 1 dose.10
ACIP will attempt to address multiple issues in the next year regarding HPV vaccination: HPV9 use in men and women, including the possibility of catch-up schedules for those who have received HPV4 or HPV2; the possibility of using a 2-dose schedule for all HPV vaccines; and ways to increase uptake of this cancer-preventing vaccine.
Meningococcus type B
With the widespread use of quadrivalent meningococcal vaccines (MCV4), meningococcal meningitis has declined markedly in all age groups. The incidence of disease caused by meningococcal serotype B, which MCV4 does not protect against, has also declined from 0.3 to less than 0.1 cases per 100,000 between 1994 and 2013.11 The highest incidence occurs in infants under the age of 1 year, at 1.5/100,000, with 67% of cases attributable to serotype B. A slight bump in risk is seen with those ages 19 to 22 years (0.2/100,000) compared with other adolescents and adults.
While serotype B accounts for a larger proportion of all meningococcal disease than it did before, it is still relatively rare. In the United States between 2010 and 2012, annual cases totaled 48 to 56.11 Groups that are at higher risk of infection include those with complement deficiencies or asplenia (functional or anatomical), microbiologists and lab personnel who work with the organism, and those who have close contact with infected individuals.
In the past few years, well-publicized outbreaks of meningococcus B have occurred on some university campuses. Princeton had 9 cases, and the University of California at Santa Barbara had 4.11 This led to the use of meningococcal B vaccine as an outbreak control measure, with permission from the FDA before the vaccine was licensed. While these outbreaks created an impression of increased risks on college campuses, college students are actually at lower risk of type B meningococcal disease than others of the same age.11
This year, 2 meningococcal B vaccines will be available in the United States. The first, rLP2086, Trumenba (Pfizer) is a 3-dose series that was licensed in late 2014. The second, 4CMenB, Bexsero (Novartis) is a 2-dose series that received FDA approval in January 2015. Both are licensed for individuals ages 10 to 25 years. Formulating a recommendation for the use of these vaccines will be challenging because of several factors: the multiple dose schedules, the low rate of meningococcal B disease, and the age group for whom the vaccines are licensed.
1. Centers for Disease Control and Prevention. Recommended adult immunization schedule: United States - 2015. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf. Accessed February 11, 2015.
2. Centers for Disease Control and Prevention. Birth – 18 years & “Catch-up” immunization schedules. United States, 2015. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html. Accessed January 27, 2015.
3. Campos-Outcalt D. Pneumococcal vaccines for older adults: getting the timing right. J Fam Pract. 2014;63:730-733.
4. Campos-Outcalt D. The 2014-2015 influenza season: what you need to know. J Fam Pract. 2014;63:532-533.
5. Flannery B. Update on effectiveness of live-attenuated versus inactivated influenza vaccine in children and adolescents aged 2-18 years. Presented at: Advisory Committee on Immunization Practices; October 29, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/flu-03-flannery.pdf. Accessed January 27, 2015.
6. Jackson BR. Typhoid and typhoid vaccines. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/Typhoid-02-Jackson.pdf. Accessed January 27, 2015.
7. Centers for Disease Control and Prevention. Typhoid immunization—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1994:43:1-7.
8. Luxembourg A. 9-valent HPV vaccine program key results--Part III. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/HPV-02-Luxembourg.pdf. Accessed January 27, 2015.
9. Markowitz L. 2-dose HPV vaccination schedules. Presented at: Advisory Committee on Immunization Practices; June 25, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-06/HPV-04-Markowitz.pdf. Accessed January 27, 2015.
10. Stokley S, Jeyarajah J, Yankey D, et al; Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; Centers for Disease Control and Prevention (CDC). Human papillomavirus vaccination coverage among adolescents, 2007-2013, and postlicensure safety monitoring, 2006-2014—United States. MMWR Morb Mortal Wkly Rep. 2014;63:620-624.
11. MacNeil J. Epidemiology of serogroup B meningococcal disease, United States. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/mening-02-MacNeil.pdf. Accessed January 27, 2015.
1. Centers for Disease Control and Prevention. Recommended adult immunization schedule: United States - 2015. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf. Accessed February 11, 2015.
2. Centers for Disease Control and Prevention. Birth – 18 years & “Catch-up” immunization schedules. United States, 2015. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html. Accessed January 27, 2015.
3. Campos-Outcalt D. Pneumococcal vaccines for older adults: getting the timing right. J Fam Pract. 2014;63:730-733.
4. Campos-Outcalt D. The 2014-2015 influenza season: what you need to know. J Fam Pract. 2014;63:532-533.
5. Flannery B. Update on effectiveness of live-attenuated versus inactivated influenza vaccine in children and adolescents aged 2-18 years. Presented at: Advisory Committee on Immunization Practices; October 29, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/flu-03-flannery.pdf. Accessed January 27, 2015.
6. Jackson BR. Typhoid and typhoid vaccines. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/Typhoid-02-Jackson.pdf. Accessed January 27, 2015.
7. Centers for Disease Control and Prevention. Typhoid immunization—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1994:43:1-7.
8. Luxembourg A. 9-valent HPV vaccine program key results--Part III. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/HPV-02-Luxembourg.pdf. Accessed January 27, 2015.
9. Markowitz L. 2-dose HPV vaccination schedules. Presented at: Advisory Committee on Immunization Practices; June 25, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-06/HPV-04-Markowitz.pdf. Accessed January 27, 2015.
10. Stokley S, Jeyarajah J, Yankey D, et al; Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; Centers for Disease Control and Prevention (CDC). Human papillomavirus vaccination coverage among adolescents, 2007-2013, and postlicensure safety monitoring, 2006-2014—United States. MMWR Morb Mortal Wkly Rep. 2014;63:620-624.
11. MacNeil J. Epidemiology of serogroup B meningococcal disease, United States. Presented at: Advisory Committee on Immunization Practices; October 30, 2014; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2014-10/mening-02-MacNeil.pdf. Accessed January 27, 2015.