User login
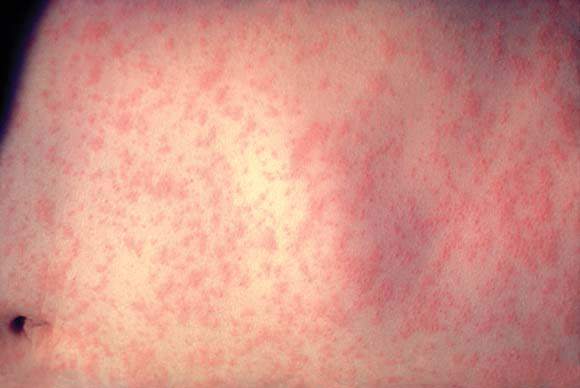
Of the almost 9 million children and adolescents aged 17 years and younger estimated to be measles susceptible in the United States, those 3 years and younger show the highest levels of risk for infection, according to the results of a study published in the American Journal of Epidemiology.
Robert A. Bednarczyk, MD, and his colleagues at Emory University, Atlanta, developed a model based on age-specific measles vaccination data from the National Immunization Survey–Teen collected between 2008 and 2013 (18 cumulative birth cohorts) to estimate the number of U.S. children (birth–age 12 years ) and adolescents (aged 13-17 years) susceptible to measles infection (Am J Epidemiol. 2016 Jul 15;184[2]:148-56).
The model was developed using the survey data in conjunction with assumptions designed to account for several potentially confounding variables. These included the effectiveness of the vaccine used, whether infants were protected by maternally derived, vaccine-induced antibodies, and any loss of immunity attributable to treatment for cancer during childhood. The model also allowed for an examination of susceptibility by different age groupings, as well as by state. Additionally, the study authors were able to estimate the impact of decreased measles-containing vaccine effectiveness on susceptibility to infection in adolescents.
Results from the model indicated that 12.5% of the over 69 million of U.S. children and adolescents in the 18 birth cohorts are susceptible to measles infection. Those with the highest percentage of susceptibility were children 3 years of age and younger (24.7%), compared with 9.0% of children and adolescents aged 4-17 years. Geographic differences in susceptibility also were apparent. In addition to the District of Columbia, 10 states had adolescent susceptibility levels of at least 6%, and 14 states each had over 20,000 susceptible adolescents.
Using the model to simulate a 1% decrease in vaccine effectiveness for both the first (93%-92%) and second (97%-96%) measles-containing vaccine doses, the study authors reported the addition of almost 1 million children and adolescents (13.4%) to the measles-susceptible category. This finding indicates that very small changes in vaccine effectiveness can have a substantial impact on susceptibility through a slow accumulation of additional susceptible children and adolescents each year, culminating in a steady decline in the proportion of children and adolescents immune to measles.
Regarding their overall findings, Dr. Bednarczyk and his colleagues stated, “the overall level of immunity to measles is generally at or higher than the operational threshold of 92%. This is compatible with the experience to date that, despite substantial numbers of importations, endemic measles transmission has not been reestablished.”
As for broader implications, the investigators said that “These estimates underscore the need to help public health professionals plan for future immunization programs and potential measles outbreaks, and to maintain appropriate levels of immunity in the population to prevent widespread transmission of this highly infectious disease.”
Of the almost 9 million children and adolescents aged 17 years and younger estimated to be measles susceptible in the United States, those 3 years and younger show the highest levels of risk for infection, according to the results of a study published in the American Journal of Epidemiology.
Robert A. Bednarczyk, MD, and his colleagues at Emory University, Atlanta, developed a model based on age-specific measles vaccination data from the National Immunization Survey–Teen collected between 2008 and 2013 (18 cumulative birth cohorts) to estimate the number of U.S. children (birth–age 12 years ) and adolescents (aged 13-17 years) susceptible to measles infection (Am J Epidemiol. 2016 Jul 15;184[2]:148-56).
The model was developed using the survey data in conjunction with assumptions designed to account for several potentially confounding variables. These included the effectiveness of the vaccine used, whether infants were protected by maternally derived, vaccine-induced antibodies, and any loss of immunity attributable to treatment for cancer during childhood. The model also allowed for an examination of susceptibility by different age groupings, as well as by state. Additionally, the study authors were able to estimate the impact of decreased measles-containing vaccine effectiveness on susceptibility to infection in adolescents.
Results from the model indicated that 12.5% of the over 69 million of U.S. children and adolescents in the 18 birth cohorts are susceptible to measles infection. Those with the highest percentage of susceptibility were children 3 years of age and younger (24.7%), compared with 9.0% of children and adolescents aged 4-17 years. Geographic differences in susceptibility also were apparent. In addition to the District of Columbia, 10 states had adolescent susceptibility levels of at least 6%, and 14 states each had over 20,000 susceptible adolescents.
Using the model to simulate a 1% decrease in vaccine effectiveness for both the first (93%-92%) and second (97%-96%) measles-containing vaccine doses, the study authors reported the addition of almost 1 million children and adolescents (13.4%) to the measles-susceptible category. This finding indicates that very small changes in vaccine effectiveness can have a substantial impact on susceptibility through a slow accumulation of additional susceptible children and adolescents each year, culminating in a steady decline in the proportion of children and adolescents immune to measles.
Regarding their overall findings, Dr. Bednarczyk and his colleagues stated, “the overall level of immunity to measles is generally at or higher than the operational threshold of 92%. This is compatible with the experience to date that, despite substantial numbers of importations, endemic measles transmission has not been reestablished.”
As for broader implications, the investigators said that “These estimates underscore the need to help public health professionals plan for future immunization programs and potential measles outbreaks, and to maintain appropriate levels of immunity in the population to prevent widespread transmission of this highly infectious disease.”
Of the almost 9 million children and adolescents aged 17 years and younger estimated to be measles susceptible in the United States, those 3 years and younger show the highest levels of risk for infection, according to the results of a study published in the American Journal of Epidemiology.
Robert A. Bednarczyk, MD, and his colleagues at Emory University, Atlanta, developed a model based on age-specific measles vaccination data from the National Immunization Survey–Teen collected between 2008 and 2013 (18 cumulative birth cohorts) to estimate the number of U.S. children (birth–age 12 years ) and adolescents (aged 13-17 years) susceptible to measles infection (Am J Epidemiol. 2016 Jul 15;184[2]:148-56).
The model was developed using the survey data in conjunction with assumptions designed to account for several potentially confounding variables. These included the effectiveness of the vaccine used, whether infants were protected by maternally derived, vaccine-induced antibodies, and any loss of immunity attributable to treatment for cancer during childhood. The model also allowed for an examination of susceptibility by different age groupings, as well as by state. Additionally, the study authors were able to estimate the impact of decreased measles-containing vaccine effectiveness on susceptibility to infection in adolescents.
Results from the model indicated that 12.5% of the over 69 million of U.S. children and adolescents in the 18 birth cohorts are susceptible to measles infection. Those with the highest percentage of susceptibility were children 3 years of age and younger (24.7%), compared with 9.0% of children and adolescents aged 4-17 years. Geographic differences in susceptibility also were apparent. In addition to the District of Columbia, 10 states had adolescent susceptibility levels of at least 6%, and 14 states each had over 20,000 susceptible adolescents.
Using the model to simulate a 1% decrease in vaccine effectiveness for both the first (93%-92%) and second (97%-96%) measles-containing vaccine doses, the study authors reported the addition of almost 1 million children and adolescents (13.4%) to the measles-susceptible category. This finding indicates that very small changes in vaccine effectiveness can have a substantial impact on susceptibility through a slow accumulation of additional susceptible children and adolescents each year, culminating in a steady decline in the proportion of children and adolescents immune to measles.
Regarding their overall findings, Dr. Bednarczyk and his colleagues stated, “the overall level of immunity to measles is generally at or higher than the operational threshold of 92%. This is compatible with the experience to date that, despite substantial numbers of importations, endemic measles transmission has not been reestablished.”
As for broader implications, the investigators said that “These estimates underscore the need to help public health professionals plan for future immunization programs and potential measles outbreaks, and to maintain appropriate levels of immunity in the population to prevent widespread transmission of this highly infectious disease.”
Key clinical point: U.S. children younger than 3 years of age have a high estimated susceptibility to measles infection.
Major finding: An estimated 12.5% of U.S. children and adolescents 17 years and younger are susceptible to measles infection, with differences in susceptibility levels detected for specific age ranges and states. Small decreases in vaccine effectiveness can have a large impact on susceptibility levels.
Data sources: National Immunization Survey–Teen collected between 2008 and 2013.
Disclosures: The study was conducted without grant support. All authors reported no conflicts of interest.