User login
There are a lack of research on, and strategies for dealing with, an insufficient response to antipsychotics. Treatment often is guided by what is described in published case reports or anecdotal evidence, rather than the findings of systematic studies.
We propose that a patient be considered “difficult-to-treat” or “treatment-resistant” after experiencing limited or negative responses to 3 different antipsychotics—with ≥1 being a second-generation antipsychotic (SGA)—that the patient has taken for at least 6 to 8 weeks at the maximum recommended dosage. Furthermore, switching to clozapine is an important strategy; do not consider it solely a last resort.
These 6 ‘D’s can remind you of other problems to consider when evaluating a treatment-resistant patient.
Diagnosis. Is the diagnosis, including the presence of comorbid conditions, accurate? Are significant psychosocial stressors undermining treatment response? Treat any comorbid conditions and consider instituting adjunctive psychosocial interventions, including cognitive-behavioral therapy.
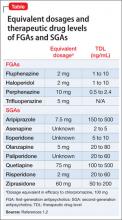
Dosage. Have the patient try the maximum recommended dosage if he (she) can tolerate it. Equivalent dosages of antipsychotics are shown in the Table,1,2 and can guide off-label use of higher dosages. Research does not support use of chlorpromazine equivalents >1,000 mg/d, and usually should not be employed. If using a higher than normal dosage, perform an ECG before the increase.3
Beneficial and adverse effects should be monitored carefully. Reduce the dosage after 3 months if the risk-benefit ratio does not justify the higher dosage.3
Duration. Try a treatment for at least 6 weeks at the maximum tolerated
dosage—even extending it to 12 weeks—before considering abandoning it because of insufficient response.
Drug interactions. Use a drug interaction tool to ensure drug-drug interactions are not reducing antipsychotic levels. A recent increase in smoking or decrease in caffeine intake can reduce the blood level of olanzapine and clozapine.4 Ultra-rapid metabolizers of cytochrome P450 isoenzymes may have a lower blood level of antipsychotic.
Consider pharmacogenetic testing in patients in whom you observe an unexpected lack of efficacy or adverse effects at customary dosages.
Double up. You might need to add another medication to the antipsychotic. Symptoms might help determine which medication to add:
- a combination of an SGA and a first-generation antipsychotic may be more effective than antipsychotic monotherapy5
- for prominent negative symptoms, consider using 2 SGAs of different potency together. Use caution when prescribing ziprasidone with another antipsychotic because this could prolong the QTc interval
- if a mood stabilizer is appropriate, consider lamotrigine because of its possible potentiating effect on SGAs6
- benzodiazepines can be used to reduce agitation or anxiety but are ineffective for psychosis.7
Drug levels. Measurement of the blood level of the drug is most useful when administering clozapine; focus on the clozapine, not on the norclozapine level that also is reported. Ensure a clozapine level of 350 to 600 ng/mL.
Therapeutic levels have been established for most antipsychotics (Table).1,2 Occasionally, knowing these levels can be helpful in evaluating patients for potential problems with absorption and metabolism of the drug, and with nonadherence.
Disclosures
Drs. Faden and Pinninti report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Mago receives grant/research support from Bristol-Myers Squibb, Forest Institute, Genomind, and Shire.
1. Gardner DM, Murphy AL, O’Donnell H, et al. International consensus study of antipsychotic dosing. Am J Psychiatry. 2010;167(6):686-693.
2. Hiemke C, Baumann P, Bergemann N, et al. AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: update 2011. Pharmacopsychiatry. 2011;44(6):195-235.
3. Royal College of Psychiatrists. Consensus statement on high-dose antipsychotic medication. http://www.rcpsych.ac.uk/files/pdfversion/CR138.pdf. Published May 2006. Accessed March 26, 2013.
4. Pinninti NR, Mago R, de Leon J. Coffee, cigarettes and meds: what are the metabolic effects? Psychiatric Times. 2005;22(6):20-23.
5. Correll CU, Rummel-Kluge C, Corves C, et al. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35(2):443-457.
6. Citrome L. Treatment-resistant schizophrenia: what can we do about it? Current Psychiatry. 2011;10(6):52-58.
7. Volz A, Khorsand V, Gillies D, et al. Benzodiazepines for schizophrenia. Cochrane Database Syst Rev. 2007;(1): CD006391.
There are a lack of research on, and strategies for dealing with, an insufficient response to antipsychotics. Treatment often is guided by what is described in published case reports or anecdotal evidence, rather than the findings of systematic studies.
We propose that a patient be considered “difficult-to-treat” or “treatment-resistant” after experiencing limited or negative responses to 3 different antipsychotics—with ≥1 being a second-generation antipsychotic (SGA)—that the patient has taken for at least 6 to 8 weeks at the maximum recommended dosage. Furthermore, switching to clozapine is an important strategy; do not consider it solely a last resort.
These 6 ‘D’s can remind you of other problems to consider when evaluating a treatment-resistant patient.
Diagnosis. Is the diagnosis, including the presence of comorbid conditions, accurate? Are significant psychosocial stressors undermining treatment response? Treat any comorbid conditions and consider instituting adjunctive psychosocial interventions, including cognitive-behavioral therapy.
Dosage. Have the patient try the maximum recommended dosage if he (she) can tolerate it. Equivalent dosages of antipsychotics are shown in the Table,1,2 and can guide off-label use of higher dosages. Research does not support use of chlorpromazine equivalents >1,000 mg/d, and usually should not be employed. If using a higher than normal dosage, perform an ECG before the increase.3
Beneficial and adverse effects should be monitored carefully. Reduce the dosage after 3 months if the risk-benefit ratio does not justify the higher dosage.3
Duration. Try a treatment for at least 6 weeks at the maximum tolerated
dosage—even extending it to 12 weeks—before considering abandoning it because of insufficient response.
Drug interactions. Use a drug interaction tool to ensure drug-drug interactions are not reducing antipsychotic levels. A recent increase in smoking or decrease in caffeine intake can reduce the blood level of olanzapine and clozapine.4 Ultra-rapid metabolizers of cytochrome P450 isoenzymes may have a lower blood level of antipsychotic.
Consider pharmacogenetic testing in patients in whom you observe an unexpected lack of efficacy or adverse effects at customary dosages.
Double up. You might need to add another medication to the antipsychotic. Symptoms might help determine which medication to add:
- a combination of an SGA and a first-generation antipsychotic may be more effective than antipsychotic monotherapy5
- for prominent negative symptoms, consider using 2 SGAs of different potency together. Use caution when prescribing ziprasidone with another antipsychotic because this could prolong the QTc interval
- if a mood stabilizer is appropriate, consider lamotrigine because of its possible potentiating effect on SGAs6
- benzodiazepines can be used to reduce agitation or anxiety but are ineffective for psychosis.7
Drug levels. Measurement of the blood level of the drug is most useful when administering clozapine; focus on the clozapine, not on the norclozapine level that also is reported. Ensure a clozapine level of 350 to 600 ng/mL.
Therapeutic levels have been established for most antipsychotics (Table).1,2 Occasionally, knowing these levels can be helpful in evaluating patients for potential problems with absorption and metabolism of the drug, and with nonadherence.
Disclosures
Drs. Faden and Pinninti report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Mago receives grant/research support from Bristol-Myers Squibb, Forest Institute, Genomind, and Shire.
There are a lack of research on, and strategies for dealing with, an insufficient response to antipsychotics. Treatment often is guided by what is described in published case reports or anecdotal evidence, rather than the findings of systematic studies.
We propose that a patient be considered “difficult-to-treat” or “treatment-resistant” after experiencing limited or negative responses to 3 different antipsychotics—with ≥1 being a second-generation antipsychotic (SGA)—that the patient has taken for at least 6 to 8 weeks at the maximum recommended dosage. Furthermore, switching to clozapine is an important strategy; do not consider it solely a last resort.
These 6 ‘D’s can remind you of other problems to consider when evaluating a treatment-resistant patient.
Diagnosis. Is the diagnosis, including the presence of comorbid conditions, accurate? Are significant psychosocial stressors undermining treatment response? Treat any comorbid conditions and consider instituting adjunctive psychosocial interventions, including cognitive-behavioral therapy.
Dosage. Have the patient try the maximum recommended dosage if he (she) can tolerate it. Equivalent dosages of antipsychotics are shown in the Table,1,2 and can guide off-label use of higher dosages. Research does not support use of chlorpromazine equivalents >1,000 mg/d, and usually should not be employed. If using a higher than normal dosage, perform an ECG before the increase.3
Beneficial and adverse effects should be monitored carefully. Reduce the dosage after 3 months if the risk-benefit ratio does not justify the higher dosage.3
Duration. Try a treatment for at least 6 weeks at the maximum tolerated
dosage—even extending it to 12 weeks—before considering abandoning it because of insufficient response.
Drug interactions. Use a drug interaction tool to ensure drug-drug interactions are not reducing antipsychotic levels. A recent increase in smoking or decrease in caffeine intake can reduce the blood level of olanzapine and clozapine.4 Ultra-rapid metabolizers of cytochrome P450 isoenzymes may have a lower blood level of antipsychotic.
Consider pharmacogenetic testing in patients in whom you observe an unexpected lack of efficacy or adverse effects at customary dosages.
Double up. You might need to add another medication to the antipsychotic. Symptoms might help determine which medication to add:
- a combination of an SGA and a first-generation antipsychotic may be more effective than antipsychotic monotherapy5
- for prominent negative symptoms, consider using 2 SGAs of different potency together. Use caution when prescribing ziprasidone with another antipsychotic because this could prolong the QTc interval
- if a mood stabilizer is appropriate, consider lamotrigine because of its possible potentiating effect on SGAs6
- benzodiazepines can be used to reduce agitation or anxiety but are ineffective for psychosis.7
Drug levels. Measurement of the blood level of the drug is most useful when administering clozapine; focus on the clozapine, not on the norclozapine level that also is reported. Ensure a clozapine level of 350 to 600 ng/mL.
Therapeutic levels have been established for most antipsychotics (Table).1,2 Occasionally, knowing these levels can be helpful in evaluating patients for potential problems with absorption and metabolism of the drug, and with nonadherence.
Disclosures
Drs. Faden and Pinninti report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Mago receives grant/research support from Bristol-Myers Squibb, Forest Institute, Genomind, and Shire.
1. Gardner DM, Murphy AL, O’Donnell H, et al. International consensus study of antipsychotic dosing. Am J Psychiatry. 2010;167(6):686-693.
2. Hiemke C, Baumann P, Bergemann N, et al. AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: update 2011. Pharmacopsychiatry. 2011;44(6):195-235.
3. Royal College of Psychiatrists. Consensus statement on high-dose antipsychotic medication. http://www.rcpsych.ac.uk/files/pdfversion/CR138.pdf. Published May 2006. Accessed March 26, 2013.
4. Pinninti NR, Mago R, de Leon J. Coffee, cigarettes and meds: what are the metabolic effects? Psychiatric Times. 2005;22(6):20-23.
5. Correll CU, Rummel-Kluge C, Corves C, et al. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35(2):443-457.
6. Citrome L. Treatment-resistant schizophrenia: what can we do about it? Current Psychiatry. 2011;10(6):52-58.
7. Volz A, Khorsand V, Gillies D, et al. Benzodiazepines for schizophrenia. Cochrane Database Syst Rev. 2007;(1): CD006391.
1. Gardner DM, Murphy AL, O’Donnell H, et al. International consensus study of antipsychotic dosing. Am J Psychiatry. 2010;167(6):686-693.
2. Hiemke C, Baumann P, Bergemann N, et al. AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: update 2011. Pharmacopsychiatry. 2011;44(6):195-235.
3. Royal College of Psychiatrists. Consensus statement on high-dose antipsychotic medication. http://www.rcpsych.ac.uk/files/pdfversion/CR138.pdf. Published May 2006. Accessed March 26, 2013.
4. Pinninti NR, Mago R, de Leon J. Coffee, cigarettes and meds: what are the metabolic effects? Psychiatric Times. 2005;22(6):20-23.
5. Correll CU, Rummel-Kluge C, Corves C, et al. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35(2):443-457.
6. Citrome L. Treatment-resistant schizophrenia: what can we do about it? Current Psychiatry. 2011;10(6):52-58.
7. Volz A, Khorsand V, Gillies D, et al. Benzodiazepines for schizophrenia. Cochrane Database Syst Rev. 2007;(1): CD006391.