User login
For decades, clinicians used the normative findings reported by Friedman in 1954 to help manage labor.1 Recent observational research on labor progress, however, has identified a new set of norms for the 21st Century on assessing the progress of labor. These contemporary observations significantly influence how we manage labor. In this editorial, I outline the new standards, compared with the old, so you can effectively apply best obstetric practice.
PRACTICE CHANGER #1
Your patient may not be in the active phase of labor until she reaches a cervical dilation
of 6 cm
Friedman’s research identified two phases of the first stage of labor, the latent phase, where cervical dilation is slow, and the active phase, where cervical dilation is much faster. For clinicians managing labor, it is important to know the cervical dilation when most women are in the active phase of labor so that protraction and arrest disorders can be optimally diagnosed and treated.
Old norm: 4 cm; New norm: 6 cm
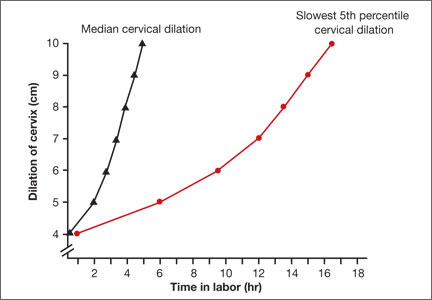
The standard Friedman partogram shows 4 cm as the cervical dilation where there is commonly a transition from the latent to the active phase. In a recent analysis of more than 62,000 labors, however, Zhang and colleagues reported the norms of 21st Century labor patterns.2 They found that most nulliparous women do not begin to dilate at a rate greater than 1 cm/hr (considered the active phase) until they reach a cervical dilation of 5 to 6 cm. The study data also show that there is no abrupt change in the rate of cervical dilation from the latent to the active phase. Rather, the increasing rate of cervical change is very gradual (FIGURE).
In 1998, Peisner and Rosen3 reported on the cervical dilation at which women entered the active phase, defined as a cervical change of more than 1.2 cm/hr in nulliparous women and more than 1.5 cm/hr in multiparous women. In this study, the percentages of women who entered the active phase at various degrees of cervical dilation were:
- ≤3 cm, 25%
- 4 cm, 25%
- 5 cm, 24%
- 6 cm, 15%
- ≥6 cm, 11%.
Based on these considerations, in contemporary practice it is best to use 6 cm of cervical dilation, not 4 cm, as the milestone in labor where a more rapid change in cervical dilation can be expected.
Related Article: Update on Obstetrics Jaimey M. Pauli, MD, and John T. Repke, MD (January 2013)
PRACTICE CHANGER #2
During the active phase of normal labor, the cervix may dilate as slowly as 0.5 cm/hr
It is important for obstetricians to know when labor is progressing too slowly, so that they can optimally manage protraction and arrest disorders of the first stage, thereby improving maternal and newborn outcomes. But, what is the slowest rate of cervical change we should expect in the active phase of the first stage of normal labor?
Old norm: as slow as 1.2 cm/hr; New norm: as slow as 0.5 cm/hr
Arbitrarily, an abnormally slow rate of cervical change during the active phase of labor can be defined as the rate of cervical change observed in the 5% of women with the slowest first stage of labor associated with a normal vaginal birth. Zhang and colleagues2 reported that the 5% of women with the slowest change during active labor had a rate of cervical dilation of:
- 0.45 to 0.70 cm/hr (nulliparous women) or
- 0.50 to 1.10 cm/hr (multiparous women).
Based on data from the mid-20th Century, Friedman reported that active labor was associated with a rate of cervical change of:
- >1.2 cm/hr in nulliparous and
- >1.5 cm/hr in multiparous women.
The data reported by Zhang and colleagues indicate that in the 21st Century, normal labor is associated with a much slower rate of cervical change, as slow as 0.5 cm/hr.
PRACTICE CHANGER #3
The normal second stage may last up to 3.6 hr in nulliparous women given an epidural anesthetic
Friedman1 reported that the second stage of normal labor was 3 hours or less in nulliparous women and 1 hour or less in multiparous women. Zhang and colleagues2 observed that in nulliparous women the second stage of normal labor was 3.6 hr or less with an epidural and 2.8 hr or less without an epidural anesthetic.
In multiparous women, the second stage of normal labor is less than 2.0 hr with an epidural and less than 1.3 hr without an epidural. These data suggest that we should reset our expectations of the length of a normal second stage in nulliparous women given an epidural from less than 3 hr to less than 3.6 hr.
Related Article: Develop and use a checklist for 3rd- and 4th-degree perineal lacerations
Robert L. Barbieri, MD (Editorial, August 2013)
ADJUST YOUR PRACTICE
Management of labor is a clinical art, requiring the integration of many diverse pieces of information, including the medical conditions affecting the parturient, the strength and frequency of uterine contractions, the physical characteristics of the birth canal, the size and position of the fetus, status of the membranes, and assessment of the fetal physiologic state. The bottom line of the Zhang report2 is that 21st Century labor has a pace that is slower than the pace reported by Friedman1 based on data from the mid-20th Century. Adjust your practice to integrate these new labor progress norms into your decision making.
INSTANT POLL
Do you favor the use of amniotomy and early oxytocin administration in the management of normal labor?
Tell us—at rbarbieri@frontlinemedcom.com
Please include your name and city and state.
- Friedman EA. The graphic analysis of labor. Am J Obstet Gynecol. 1954;68(6):1568–1575.
- Zhang J, Landy HJ, Branch DW, et al; Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116(6):1281–1287.
- Peisner DB, Rosen MG. Transition from latent to active labor. Obstet Gynecol. 1986;68(4):448–451.
For decades, clinicians used the normative findings reported by Friedman in 1954 to help manage labor.1 Recent observational research on labor progress, however, has identified a new set of norms for the 21st Century on assessing the progress of labor. These contemporary observations significantly influence how we manage labor. In this editorial, I outline the new standards, compared with the old, so you can effectively apply best obstetric practice.
PRACTICE CHANGER #1
Your patient may not be in the active phase of labor until she reaches a cervical dilation
of 6 cm
Friedman’s research identified two phases of the first stage of labor, the latent phase, where cervical dilation is slow, and the active phase, where cervical dilation is much faster. For clinicians managing labor, it is important to know the cervical dilation when most women are in the active phase of labor so that protraction and arrest disorders can be optimally diagnosed and treated.
Old norm: 4 cm; New norm: 6 cm
The standard Friedman partogram shows 4 cm as the cervical dilation where there is commonly a transition from the latent to the active phase. In a recent analysis of more than 62,000 labors, however, Zhang and colleagues reported the norms of 21st Century labor patterns.2 They found that most nulliparous women do not begin to dilate at a rate greater than 1 cm/hr (considered the active phase) until they reach a cervical dilation of 5 to 6 cm. The study data also show that there is no abrupt change in the rate of cervical dilation from the latent to the active phase. Rather, the increasing rate of cervical change is very gradual (FIGURE).
In 1998, Peisner and Rosen3 reported on the cervical dilation at which women entered the active phase, defined as a cervical change of more than 1.2 cm/hr in nulliparous women and more than 1.5 cm/hr in multiparous women. In this study, the percentages of women who entered the active phase at various degrees of cervical dilation were:
- ≤3 cm, 25%
- 4 cm, 25%
- 5 cm, 24%
- 6 cm, 15%
- ≥6 cm, 11%.
Based on these considerations, in contemporary practice it is best to use 6 cm of cervical dilation, not 4 cm, as the milestone in labor where a more rapid change in cervical dilation can be expected.
Related Article: Update on Obstetrics Jaimey M. Pauli, MD, and John T. Repke, MD (January 2013)
PRACTICE CHANGER #2
During the active phase of normal labor, the cervix may dilate as slowly as 0.5 cm/hr
It is important for obstetricians to know when labor is progressing too slowly, so that they can optimally manage protraction and arrest disorders of the first stage, thereby improving maternal and newborn outcomes. But, what is the slowest rate of cervical change we should expect in the active phase of the first stage of normal labor?
Old norm: as slow as 1.2 cm/hr; New norm: as slow as 0.5 cm/hr
Arbitrarily, an abnormally slow rate of cervical change during the active phase of labor can be defined as the rate of cervical change observed in the 5% of women with the slowest first stage of labor associated with a normal vaginal birth. Zhang and colleagues2 reported that the 5% of women with the slowest change during active labor had a rate of cervical dilation of:
- 0.45 to 0.70 cm/hr (nulliparous women) or
- 0.50 to 1.10 cm/hr (multiparous women).
Based on data from the mid-20th Century, Friedman reported that active labor was associated with a rate of cervical change of:
- >1.2 cm/hr in nulliparous and
- >1.5 cm/hr in multiparous women.
The data reported by Zhang and colleagues indicate that in the 21st Century, normal labor is associated with a much slower rate of cervical change, as slow as 0.5 cm/hr.
PRACTICE CHANGER #3
The normal second stage may last up to 3.6 hr in nulliparous women given an epidural anesthetic
Friedman1 reported that the second stage of normal labor was 3 hours or less in nulliparous women and 1 hour or less in multiparous women. Zhang and colleagues2 observed that in nulliparous women the second stage of normal labor was 3.6 hr or less with an epidural and 2.8 hr or less without an epidural anesthetic.
In multiparous women, the second stage of normal labor is less than 2.0 hr with an epidural and less than 1.3 hr without an epidural. These data suggest that we should reset our expectations of the length of a normal second stage in nulliparous women given an epidural from less than 3 hr to less than 3.6 hr.
Related Article: Develop and use a checklist for 3rd- and 4th-degree perineal lacerations
Robert L. Barbieri, MD (Editorial, August 2013)
ADJUST YOUR PRACTICE
Management of labor is a clinical art, requiring the integration of many diverse pieces of information, including the medical conditions affecting the parturient, the strength and frequency of uterine contractions, the physical characteristics of the birth canal, the size and position of the fetus, status of the membranes, and assessment of the fetal physiologic state. The bottom line of the Zhang report2 is that 21st Century labor has a pace that is slower than the pace reported by Friedman1 based on data from the mid-20th Century. Adjust your practice to integrate these new labor progress norms into your decision making.
INSTANT POLL
Do you favor the use of amniotomy and early oxytocin administration in the management of normal labor?
Tell us—at rbarbieri@frontlinemedcom.com
Please include your name and city and state.
For decades, clinicians used the normative findings reported by Friedman in 1954 to help manage labor.1 Recent observational research on labor progress, however, has identified a new set of norms for the 21st Century on assessing the progress of labor. These contemporary observations significantly influence how we manage labor. In this editorial, I outline the new standards, compared with the old, so you can effectively apply best obstetric practice.
PRACTICE CHANGER #1
Your patient may not be in the active phase of labor until she reaches a cervical dilation
of 6 cm
Friedman’s research identified two phases of the first stage of labor, the latent phase, where cervical dilation is slow, and the active phase, where cervical dilation is much faster. For clinicians managing labor, it is important to know the cervical dilation when most women are in the active phase of labor so that protraction and arrest disorders can be optimally diagnosed and treated.
Old norm: 4 cm; New norm: 6 cm
The standard Friedman partogram shows 4 cm as the cervical dilation where there is commonly a transition from the latent to the active phase. In a recent analysis of more than 62,000 labors, however, Zhang and colleagues reported the norms of 21st Century labor patterns.2 They found that most nulliparous women do not begin to dilate at a rate greater than 1 cm/hr (considered the active phase) until they reach a cervical dilation of 5 to 6 cm. The study data also show that there is no abrupt change in the rate of cervical dilation from the latent to the active phase. Rather, the increasing rate of cervical change is very gradual (FIGURE).
In 1998, Peisner and Rosen3 reported on the cervical dilation at which women entered the active phase, defined as a cervical change of more than 1.2 cm/hr in nulliparous women and more than 1.5 cm/hr in multiparous women. In this study, the percentages of women who entered the active phase at various degrees of cervical dilation were:
- ≤3 cm, 25%
- 4 cm, 25%
- 5 cm, 24%
- 6 cm, 15%
- ≥6 cm, 11%.
Based on these considerations, in contemporary practice it is best to use 6 cm of cervical dilation, not 4 cm, as the milestone in labor where a more rapid change in cervical dilation can be expected.
Related Article: Update on Obstetrics Jaimey M. Pauli, MD, and John T. Repke, MD (January 2013)
PRACTICE CHANGER #2
During the active phase of normal labor, the cervix may dilate as slowly as 0.5 cm/hr
It is important for obstetricians to know when labor is progressing too slowly, so that they can optimally manage protraction and arrest disorders of the first stage, thereby improving maternal and newborn outcomes. But, what is the slowest rate of cervical change we should expect in the active phase of the first stage of normal labor?
Old norm: as slow as 1.2 cm/hr; New norm: as slow as 0.5 cm/hr
Arbitrarily, an abnormally slow rate of cervical change during the active phase of labor can be defined as the rate of cervical change observed in the 5% of women with the slowest first stage of labor associated with a normal vaginal birth. Zhang and colleagues2 reported that the 5% of women with the slowest change during active labor had a rate of cervical dilation of:
- 0.45 to 0.70 cm/hr (nulliparous women) or
- 0.50 to 1.10 cm/hr (multiparous women).
Based on data from the mid-20th Century, Friedman reported that active labor was associated with a rate of cervical change of:
- >1.2 cm/hr in nulliparous and
- >1.5 cm/hr in multiparous women.
The data reported by Zhang and colleagues indicate that in the 21st Century, normal labor is associated with a much slower rate of cervical change, as slow as 0.5 cm/hr.
PRACTICE CHANGER #3
The normal second stage may last up to 3.6 hr in nulliparous women given an epidural anesthetic
Friedman1 reported that the second stage of normal labor was 3 hours or less in nulliparous women and 1 hour or less in multiparous women. Zhang and colleagues2 observed that in nulliparous women the second stage of normal labor was 3.6 hr or less with an epidural and 2.8 hr or less without an epidural anesthetic.
In multiparous women, the second stage of normal labor is less than 2.0 hr with an epidural and less than 1.3 hr without an epidural. These data suggest that we should reset our expectations of the length of a normal second stage in nulliparous women given an epidural from less than 3 hr to less than 3.6 hr.
Related Article: Develop and use a checklist for 3rd- and 4th-degree perineal lacerations
Robert L. Barbieri, MD (Editorial, August 2013)
ADJUST YOUR PRACTICE
Management of labor is a clinical art, requiring the integration of many diverse pieces of information, including the medical conditions affecting the parturient, the strength and frequency of uterine contractions, the physical characteristics of the birth canal, the size and position of the fetus, status of the membranes, and assessment of the fetal physiologic state. The bottom line of the Zhang report2 is that 21st Century labor has a pace that is slower than the pace reported by Friedman1 based on data from the mid-20th Century. Adjust your practice to integrate these new labor progress norms into your decision making.
INSTANT POLL
Do you favor the use of amniotomy and early oxytocin administration in the management of normal labor?
Tell us—at rbarbieri@frontlinemedcom.com
Please include your name and city and state.
- Friedman EA. The graphic analysis of labor. Am J Obstet Gynecol. 1954;68(6):1568–1575.
- Zhang J, Landy HJ, Branch DW, et al; Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116(6):1281–1287.
- Peisner DB, Rosen MG. Transition from latent to active labor. Obstet Gynecol. 1986;68(4):448–451.
- Friedman EA. The graphic analysis of labor. Am J Obstet Gynecol. 1954;68(6):1568–1575.
- Zhang J, Landy HJ, Branch DW, et al; Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116(6):1281–1287.
- Peisner DB, Rosen MG. Transition from latent to active labor. Obstet Gynecol. 1986;68(4):448–451.