User login
Diabetes Basic Training Program: Empowering Veterans for Wellness
More than 37 million Americans (11.3%) have diabetes mellitus (DM), and 90% to 95% are diagnosed with type 2 DM, including nearly 1 in 4 veterans receiving Veterans Health Administration (VHA) care.1,2 DM is associated with serious negative health outcomes, including cardiovascular disease and subsequent complications as well as significant health care system utilization and cost.1,3
Group interventions have been identified as a possible method of improving DM outcomes. For example, shared medical appointments (SMAs) have been identified by the VHA as holding promise for improving care and efficiency for DM and other common health conditions.4 Although the precise structure and SMA process for managing DM has been noted to be heterogeneous, the appointment is typically led by an interdisciplinary health care team and includes individualized assessment including medication review and adjustment, group education, and troubleshooting challenges with management in a group format.5 Research suggests that DM SMAs are a worthwhile treatment approach.5 Several studies have found that SMAs were associated with decreased hemoglobin A1c (Hb A1c) levels and improvement in overall disease complications and severity.6
The high degree of SMA heterogeneity and lack of detailed description of structure and process of SMAs studied has made meta-analysis and other synthesis of the literature difficult.5 Consequently, there is inadequate empirically supported guidance for clinicians and health care organizations on how to best implement SMAs and similar group-based treatments. Edelman and colleagues recommended that future research should focus on more consistent and standardized intervention structures and real-world patient- and staff-centered outcomes to address gaps in the literature.5 They noted that a mental health professional was utilized in only a minority of SMAs studied.5 Additionally, we noted a paucity of studies examining patient satisfaction with SMAs.
Another group-based intervention found to be effective in improving DM outcomes is the 6-session Stanford Diabetes Self-Management Program (DSMP), a workshop led in part by trained peers with DM. The sessions focus on educating patients on DM care and self-management tools. The workshop encourages active practice in building DM self-management skills and confidence. DSMP participation has been associated with improvement in DM-related outcomes, including Hb A1c levels, amount of exercise, and medication adherence.7
While SMAs and DSMP have been shown to enhance clinical outcomes, they provide differing types of patient support. SMAs allow for frequent interaction with a health care professional (HCP) and less emphasis on behavioral health interventions. DSMPs include behavioral health professionals and peer leaders and emphasize higher levels of psychosocial support, but do not offer access to clinicians. It is possible that combining these interventions could result in better outcomes than what either could provide on their own.
In 2018, the Cincinnati Veterans Affairs Medical Center (VAMC) in Ohio offered Diabetes Basic Training, a structured DM intervention. Patients enrolled in the program participated in a 9-week intervention that included 3 SMAs and 6 DSMP sessions. During the SMAs, a clinical psychologist or psychology postdoctoral fellow skilled in motivational interviewing facilitated the group to enhance patient engagement and empowerment for improved self-management. In addition, patients participated in structured DSMP groups with an emphasis on action-planning, often surrounding nutrition, physical activity, and other health behavior change information reviewed during the SMAs.
Design and Referral
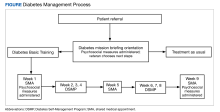
Self-management programs for chronic health conditions are often underutilized. Although HCPs may wish to connect veterans with available programs, time constraints may limit opportunities for detailed discussions with patients about specific aspects of each program. To simplify this process, a 2-hour orientation program was offered that explained individual and group DM self-management options (Figure). During this initial visit, patients met with an interdisciplinary care team (registered dietician, diabetes nurse practitioner, and behavioral health specialist) and were informed about Diabetes Basic Training, DM clinical care practices, and other related resources available at the Cincinnati VAMC (eg, cooking classes, food pantry). Patients received individualized referral recommendations and were urged to consult with their primary care practitioner to finalize their treatment plan.
Shared Medical Appointments
Diabetes Basic Training interventions had an average of 6 to 8 veterans participating in the weekly groups. The first, fifth, and final weeks were SMAs in which an interdisciplinary team collaboratively provided group-based health care for DM. The team consisted of a registered nurse, a prescriber (eg, nurse practitioner), a moderator (eg, psychologist), and a content expert (eg, nutritionist). Before each SMA began, the nurse checked-in patients in the SMA room and collected heart rate and blood pressure, and performed a diabetic foot check. Each SMA consisted of introductions, group-driven discussions (facilitated by an HCP) and troubleshooting DM self-management challenges. During group discussions, the prescriber initiated a 1-on-1 discussion with each patient in a private office regarding their recent laboratory results, medication regimen, and other aspects of DM care. The patient’s medications were refilled and/or adjusted as needed and other orders and referrals were submitted. If a patient had a medical question, the prescriber and moderator engaged the entire group so all individuals could benefit from generating and hearing answers. When discussion slowed, education was provided on topics generated by the group. Frequent topics included challenges managing DM, concerns, how DM impacted daily life and relationships, and sharing successes. As needed, HCPs spoke individually with patients following the SMA. Patients were sometimes asked, but never required, to do homework consistent with standard DM care (eg, recording what they eat or blood sugar levels). Each SMA session lasted about 2 hours.
Diabetes Self-Management Program
The second, third, fourth, sixth, seventh, and eighth weeks of the program were devoted to the DSMP. These sessions were delivered primarily by veteran peers who received appropriate training, observation, and certification. Each 2-hour educational program provided ample practice in many fundamental self-management skills, such as decision making, problem solving, and action planning. Patients were asked, but never required, to practice related skills during the sessions and to create weekly action plans to be completed between sessions that typically involved increasing exercise or improving diet. Patients were encouraged to follow up with HCPs at SMAs when they had questions requiring HCP expertise. If participants had more immediate concerns regarding their treatment plan and/or medications, they contacted their primary care practitioner prior to the next SMA.
As a part of participation in the program, psychosocial and health data and Hb A1c levels at baseline (the closest level to 90 days prior to start) and follow-up (the closest level to 90 days after the final session) were collected.8 In addition, Problem Areas in Diabetes (PAID), Patient Activation Measure (PAM)-13, and Diabetes Self-Management Questionnaire (DSMQ) were administered at 3 points: during the orientation, in the first week, and in the ninth week of the program.
PAID, a 20-item self-report questionnaire designed to capture
Observations
All measures were collected as part of traditional clinical care, and we present initial program evaluation data to demonstrate potential effectiveness of the clinic model. Paired samples t tests were used to examine differences between baseline and follow-up measures for the 24 veteran participants. The age of participants who completed the program ranged from 42 to 74 years (mean, 68 years); 29% of participants were Black veterans and 12% were female. Examination of clinical outcomes indicated that veterans reported significant increases in activation levels for managing their health increasing from a baseline mean (SD) 62.1 (12.3) to 68.4 (14.5) at follow up (t[23] = 2.15, P = .04). Hb A1c levels trended downward from a mean (SD) 8.6% (1.3) at baseline to 8.2% (1.2) at 90-day follow up (t[21] 1.05, P = .30). Similar nonsignificant trends in PAID scores were seen for pre- and postprogram reductions in emotional distress related to having DM from a mean (SD) 7.9 (5.0) at baseline to 6.3 (5.1) (t[18] = 11.51, P = .15), and enhanced self-management of glucose with a mean (SD) 6.5 (1.5) at baseline to 6.8 (1.3) at follow up (t[19] = 0.52, P = .61). The trends found in this study show promising outcomes for this pilot group-based DM treatment, though the small sample size (N = 24) limits statistical power. These findings support further exploration and expansion of interdisciplinary health programs supporting veteran self-management.
Discussion
DM is a condition of epidemic proportions that causes substantial negative health outcomes and costs at a national level. Current standards of DM care do not appear to be reversing these trends. Wider implementation of group-based treatment for DM could improve efficiency of care, increase access to quality care, and reduce burden on individual HCPs.
The VHA continues the transformation of its care system, which shifts toward a patient-centered, proactive focus on veteran well-being. This new whole health approach integrates conventional medical treatment with veteran self-empowerment in the pursuit of health goals based on individual veteran’s identified values.19 This approach emphasizes peer-led explorations of veterans’ aspirations, purpose, and individual mission, personalized health planning, and use of whole health coaches and well-being programs, with both allopathic and complementary and integrative clinical care centered around veterans’ identified goals and priorities.20
Including a program like Diabetes Basic Training as a part of whole health programming could offer several benefits. Diabetes Basic Training is unique in its integration of more traditional SMA structure with psychosocial interventions including values identification and motivational interviewing strategies to enhance patient engagement. Veterans can learn from each other’s experiences and concerns, leading to better DM management knowledge and skills. The group nature of the sessions enhances opportunities for emotional support and reduced isolation, as well as peer accountability for maintaining medication adherence.
By meeting with HCPs from multiple disciplines, veterans are exposed to different perspectives on self-management techniques, including behavioral approaches for overcoming barriers to behavior change. Clinicians have more time to engage with patients, building stronger relationships and trust. SMAs are cost-efficient and time efficient, allowing HCPs to see multiple patients at once, reducing wait times and increasing the number of patients treated in a given time frame.
The COVID-19 pandemic temporarily impacted the ongoing expansion of the program, when so many services were shifted from in-person to virtual classes. Due to staffing and other logistic issues, our pilot program was suspended during that time, but plans to resume the program by early 2024 are moving forward.
CONCLUSIONS
The Diabetes Basic Training program serves as a successful model for implementation within a VAMC. Although the number of veterans with complete data available for analysis was small, the trends exhibited in the preliminary outcome data are promising. We encourage other VAMCs to replicate this program with a larger participant base and evaluate its impact on veteran health outcomes. Next steps include comparing the clinical data from treatment as usual with outcomes from DM group participants. As the program resumes, we will reinitiate recruitment efforts to increase HCP referrals to this program.
1. National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes Statistics. Updated February 2023. Accessed January 22, 2024. https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics
2. US Department of Veterans Affairs, Office of Research and Development. VA research on diabetes. www.research.va.gov. Updated January 15, 2023. Accessed January 22, 2024. https://www.research.va.gov/topics/diabetes.cfm
3. Halter JB, Musi N, McFarland Horne F, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578-2589. doi:10.2337/db14-0020
4. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient and provider expertise to strengthen care management. Updated December 2010. Accessed January 22, 2024. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=1513366&FileName=VA244-14-R-0025-011.pdf
5. Edelman D, Gierisch JM, McDuffie JR, Oddone E, Williams JW Jr. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med. 2015;30(1):99-106. doi:10.1007/s11606-014-2978-7
6. Watts SA, Strauss GJ, Pascuzzi K, et al. Shared medical appointments for patients with diabetes: glycemic reduction in high-risk patients. J Am Assoc Nurse Pract. 2015;27(8):450-456. doi:10.1002/2327-6924.12200
7. Lorig K, Ritter PL, Turner RM, English K, Laurent DD, Greenberg J. Benefits of diabetes self-management for health plan members: a 6-month translation study. J Med Internet Res. 2016;18(6):e164. Published 2016 Jun 24. doi:10.2196/jmir.5568
8. Gilstrap LG, Chernew ME, Nguyen CA, et al. Association between clinical practice group adherence to quality measures and adverse outcomes among adult patients with diabetes. JAMA Netw Open. 2019;2(8):e199139. Published 2019 Aug 2. doi:10.1001/jamanetworkopen.2019.9139
9. Venkataraman K, Tan LS, Bautista DC, et al. Psychometric properties of the Problem Areas in Diabetes (PAID) instrument in Singapore. PLoS One. 2015;10(9):e0136759. Published 2015 Sep 3. doi:10.1371/journal.pone.0136759
10. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20(1):69-72. doi:10.1046/j.1464-5491.2003.00832.x
11. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918-1930. doi:10.1111/j.1475-6773.2005.00438.x
12. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005-1026. doi:10.1111/j.1475-6773.2004.00269.x
13. Ahn YH, Yi CH, Ham OK, Kim BJ. Psychometric properties of the Korean version of the “Patient Activation Measure 13” (PAM13-K) in patients with osteoarthritis. Eval Health Prof. 2015;38(2):255-264. doi:10.1177/0163278714540915
14. Brenk-Franz K, Hibbard JH, Herrmann WJ, et al. Validation of the German version of the patient activation measure 13 (PAM13-D) in an international multicentre study of primary care patients. PLoS One. 2013;8(9):e74786. Published 2013 Sep 30. doi:10.1371/journal.pone.0074786
15. Zill JM, Dwinger S, Kriston L, Rohenkohl A, Härter M, Dirmaier J. Psychometric evaluation of the German version of the Patient Activation Measure (PAM13). BMC Public Health. 2013;13:1027. Published 2013 Oct 30. doi:10.1186/1471-2458-13-1027
16. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual Life Outcomes. 2013;11:138. Published 2013 Aug 13. doi:10.1186/1477-7525-11-138
17. Schmitt A, Reimer A, Hermanns N, et al. assessing diabetes self-management with the Diabetes Self-Management Questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic control. PLoS One. 2016;11(3):e0150774. Published 2016 Mar 3. doi:10.1371/journal.pone.0150774
18. Bukhsh A, Lee SWH, Pusparajah P, Schmitt A, Khan TM. Psychometric properties of the Diabetes Self-Management Questionnaire (DSMQ) in Urdu. Health Qual Life Outcomes. 2017;15(1):200. Published 2017 Oct 12. doi:10.1186/s12955-017-0776-8
19. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12 Suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
20. Bokhour BG, Haun JN, Hyde J, Charns M, Kligler B. Transforming the Veterans Affairs to a whole health system of care: time for action and research. Med Care. 2020;58(4):295-300. doi:10.1097/MLR.0000000000001316
More than 37 million Americans (11.3%) have diabetes mellitus (DM), and 90% to 95% are diagnosed with type 2 DM, including nearly 1 in 4 veterans receiving Veterans Health Administration (VHA) care.1,2 DM is associated with serious negative health outcomes, including cardiovascular disease and subsequent complications as well as significant health care system utilization and cost.1,3
Group interventions have been identified as a possible method of improving DM outcomes. For example, shared medical appointments (SMAs) have been identified by the VHA as holding promise for improving care and efficiency for DM and other common health conditions.4 Although the precise structure and SMA process for managing DM has been noted to be heterogeneous, the appointment is typically led by an interdisciplinary health care team and includes individualized assessment including medication review and adjustment, group education, and troubleshooting challenges with management in a group format.5 Research suggests that DM SMAs are a worthwhile treatment approach.5 Several studies have found that SMAs were associated with decreased hemoglobin A1c (Hb A1c) levels and improvement in overall disease complications and severity.6
The high degree of SMA heterogeneity and lack of detailed description of structure and process of SMAs studied has made meta-analysis and other synthesis of the literature difficult.5 Consequently, there is inadequate empirically supported guidance for clinicians and health care organizations on how to best implement SMAs and similar group-based treatments. Edelman and colleagues recommended that future research should focus on more consistent and standardized intervention structures and real-world patient- and staff-centered outcomes to address gaps in the literature.5 They noted that a mental health professional was utilized in only a minority of SMAs studied.5 Additionally, we noted a paucity of studies examining patient satisfaction with SMAs.
Another group-based intervention found to be effective in improving DM outcomes is the 6-session Stanford Diabetes Self-Management Program (DSMP), a workshop led in part by trained peers with DM. The sessions focus on educating patients on DM care and self-management tools. The workshop encourages active practice in building DM self-management skills and confidence. DSMP participation has been associated with improvement in DM-related outcomes, including Hb A1c levels, amount of exercise, and medication adherence.7
While SMAs and DSMP have been shown to enhance clinical outcomes, they provide differing types of patient support. SMAs allow for frequent interaction with a health care professional (HCP) and less emphasis on behavioral health interventions. DSMPs include behavioral health professionals and peer leaders and emphasize higher levels of psychosocial support, but do not offer access to clinicians. It is possible that combining these interventions could result in better outcomes than what either could provide on their own.
In 2018, the Cincinnati Veterans Affairs Medical Center (VAMC) in Ohio offered Diabetes Basic Training, a structured DM intervention. Patients enrolled in the program participated in a 9-week intervention that included 3 SMAs and 6 DSMP sessions. During the SMAs, a clinical psychologist or psychology postdoctoral fellow skilled in motivational interviewing facilitated the group to enhance patient engagement and empowerment for improved self-management. In addition, patients participated in structured DSMP groups with an emphasis on action-planning, often surrounding nutrition, physical activity, and other health behavior change information reviewed during the SMAs.
Design and Referral
Self-management programs for chronic health conditions are often underutilized. Although HCPs may wish to connect veterans with available programs, time constraints may limit opportunities for detailed discussions with patients about specific aspects of each program. To simplify this process, a 2-hour orientation program was offered that explained individual and group DM self-management options (Figure). During this initial visit, patients met with an interdisciplinary care team (registered dietician, diabetes nurse practitioner, and behavioral health specialist) and were informed about Diabetes Basic Training, DM clinical care practices, and other related resources available at the Cincinnati VAMC (eg, cooking classes, food pantry). Patients received individualized referral recommendations and were urged to consult with their primary care practitioner to finalize their treatment plan.
Shared Medical Appointments
Diabetes Basic Training interventions had an average of 6 to 8 veterans participating in the weekly groups. The first, fifth, and final weeks were SMAs in which an interdisciplinary team collaboratively provided group-based health care for DM. The team consisted of a registered nurse, a prescriber (eg, nurse practitioner), a moderator (eg, psychologist), and a content expert (eg, nutritionist). Before each SMA began, the nurse checked-in patients in the SMA room and collected heart rate and blood pressure, and performed a diabetic foot check. Each SMA consisted of introductions, group-driven discussions (facilitated by an HCP) and troubleshooting DM self-management challenges. During group discussions, the prescriber initiated a 1-on-1 discussion with each patient in a private office regarding their recent laboratory results, medication regimen, and other aspects of DM care. The patient’s medications were refilled and/or adjusted as needed and other orders and referrals were submitted. If a patient had a medical question, the prescriber and moderator engaged the entire group so all individuals could benefit from generating and hearing answers. When discussion slowed, education was provided on topics generated by the group. Frequent topics included challenges managing DM, concerns, how DM impacted daily life and relationships, and sharing successes. As needed, HCPs spoke individually with patients following the SMA. Patients were sometimes asked, but never required, to do homework consistent with standard DM care (eg, recording what they eat or blood sugar levels). Each SMA session lasted about 2 hours.
Diabetes Self-Management Program
The second, third, fourth, sixth, seventh, and eighth weeks of the program were devoted to the DSMP. These sessions were delivered primarily by veteran peers who received appropriate training, observation, and certification. Each 2-hour educational program provided ample practice in many fundamental self-management skills, such as decision making, problem solving, and action planning. Patients were asked, but never required, to practice related skills during the sessions and to create weekly action plans to be completed between sessions that typically involved increasing exercise or improving diet. Patients were encouraged to follow up with HCPs at SMAs when they had questions requiring HCP expertise. If participants had more immediate concerns regarding their treatment plan and/or medications, they contacted their primary care practitioner prior to the next SMA.
As a part of participation in the program, psychosocial and health data and Hb A1c levels at baseline (the closest level to 90 days prior to start) and follow-up (the closest level to 90 days after the final session) were collected.8 In addition, Problem Areas in Diabetes (PAID), Patient Activation Measure (PAM)-13, and Diabetes Self-Management Questionnaire (DSMQ) were administered at 3 points: during the orientation, in the first week, and in the ninth week of the program.
PAID, a 20-item self-report questionnaire designed to capture
Observations
All measures were collected as part of traditional clinical care, and we present initial program evaluation data to demonstrate potential effectiveness of the clinic model. Paired samples t tests were used to examine differences between baseline and follow-up measures for the 24 veteran participants. The age of participants who completed the program ranged from 42 to 74 years (mean, 68 years); 29% of participants were Black veterans and 12% were female. Examination of clinical outcomes indicated that veterans reported significant increases in activation levels for managing their health increasing from a baseline mean (SD) 62.1 (12.3) to 68.4 (14.5) at follow up (t[23] = 2.15, P = .04). Hb A1c levels trended downward from a mean (SD) 8.6% (1.3) at baseline to 8.2% (1.2) at 90-day follow up (t[21] 1.05, P = .30). Similar nonsignificant trends in PAID scores were seen for pre- and postprogram reductions in emotional distress related to having DM from a mean (SD) 7.9 (5.0) at baseline to 6.3 (5.1) (t[18] = 11.51, P = .15), and enhanced self-management of glucose with a mean (SD) 6.5 (1.5) at baseline to 6.8 (1.3) at follow up (t[19] = 0.52, P = .61). The trends found in this study show promising outcomes for this pilot group-based DM treatment, though the small sample size (N = 24) limits statistical power. These findings support further exploration and expansion of interdisciplinary health programs supporting veteran self-management.
Discussion
DM is a condition of epidemic proportions that causes substantial negative health outcomes and costs at a national level. Current standards of DM care do not appear to be reversing these trends. Wider implementation of group-based treatment for DM could improve efficiency of care, increase access to quality care, and reduce burden on individual HCPs.
The VHA continues the transformation of its care system, which shifts toward a patient-centered, proactive focus on veteran well-being. This new whole health approach integrates conventional medical treatment with veteran self-empowerment in the pursuit of health goals based on individual veteran’s identified values.19 This approach emphasizes peer-led explorations of veterans’ aspirations, purpose, and individual mission, personalized health planning, and use of whole health coaches and well-being programs, with both allopathic and complementary and integrative clinical care centered around veterans’ identified goals and priorities.20
Including a program like Diabetes Basic Training as a part of whole health programming could offer several benefits. Diabetes Basic Training is unique in its integration of more traditional SMA structure with psychosocial interventions including values identification and motivational interviewing strategies to enhance patient engagement. Veterans can learn from each other’s experiences and concerns, leading to better DM management knowledge and skills. The group nature of the sessions enhances opportunities for emotional support and reduced isolation, as well as peer accountability for maintaining medication adherence.
By meeting with HCPs from multiple disciplines, veterans are exposed to different perspectives on self-management techniques, including behavioral approaches for overcoming barriers to behavior change. Clinicians have more time to engage with patients, building stronger relationships and trust. SMAs are cost-efficient and time efficient, allowing HCPs to see multiple patients at once, reducing wait times and increasing the number of patients treated in a given time frame.
The COVID-19 pandemic temporarily impacted the ongoing expansion of the program, when so many services were shifted from in-person to virtual classes. Due to staffing and other logistic issues, our pilot program was suspended during that time, but plans to resume the program by early 2024 are moving forward.
CONCLUSIONS
The Diabetes Basic Training program serves as a successful model for implementation within a VAMC. Although the number of veterans with complete data available for analysis was small, the trends exhibited in the preliminary outcome data are promising. We encourage other VAMCs to replicate this program with a larger participant base and evaluate its impact on veteran health outcomes. Next steps include comparing the clinical data from treatment as usual with outcomes from DM group participants. As the program resumes, we will reinitiate recruitment efforts to increase HCP referrals to this program.
More than 37 million Americans (11.3%) have diabetes mellitus (DM), and 90% to 95% are diagnosed with type 2 DM, including nearly 1 in 4 veterans receiving Veterans Health Administration (VHA) care.1,2 DM is associated with serious negative health outcomes, including cardiovascular disease and subsequent complications as well as significant health care system utilization and cost.1,3
Group interventions have been identified as a possible method of improving DM outcomes. For example, shared medical appointments (SMAs) have been identified by the VHA as holding promise for improving care and efficiency for DM and other common health conditions.4 Although the precise structure and SMA process for managing DM has been noted to be heterogeneous, the appointment is typically led by an interdisciplinary health care team and includes individualized assessment including medication review and adjustment, group education, and troubleshooting challenges with management in a group format.5 Research suggests that DM SMAs are a worthwhile treatment approach.5 Several studies have found that SMAs were associated with decreased hemoglobin A1c (Hb A1c) levels and improvement in overall disease complications and severity.6
The high degree of SMA heterogeneity and lack of detailed description of structure and process of SMAs studied has made meta-analysis and other synthesis of the literature difficult.5 Consequently, there is inadequate empirically supported guidance for clinicians and health care organizations on how to best implement SMAs and similar group-based treatments. Edelman and colleagues recommended that future research should focus on more consistent and standardized intervention structures and real-world patient- and staff-centered outcomes to address gaps in the literature.5 They noted that a mental health professional was utilized in only a minority of SMAs studied.5 Additionally, we noted a paucity of studies examining patient satisfaction with SMAs.
Another group-based intervention found to be effective in improving DM outcomes is the 6-session Stanford Diabetes Self-Management Program (DSMP), a workshop led in part by trained peers with DM. The sessions focus on educating patients on DM care and self-management tools. The workshop encourages active practice in building DM self-management skills and confidence. DSMP participation has been associated with improvement in DM-related outcomes, including Hb A1c levels, amount of exercise, and medication adherence.7
While SMAs and DSMP have been shown to enhance clinical outcomes, they provide differing types of patient support. SMAs allow for frequent interaction with a health care professional (HCP) and less emphasis on behavioral health interventions. DSMPs include behavioral health professionals and peer leaders and emphasize higher levels of psychosocial support, but do not offer access to clinicians. It is possible that combining these interventions could result in better outcomes than what either could provide on their own.
In 2018, the Cincinnati Veterans Affairs Medical Center (VAMC) in Ohio offered Diabetes Basic Training, a structured DM intervention. Patients enrolled in the program participated in a 9-week intervention that included 3 SMAs and 6 DSMP sessions. During the SMAs, a clinical psychologist or psychology postdoctoral fellow skilled in motivational interviewing facilitated the group to enhance patient engagement and empowerment for improved self-management. In addition, patients participated in structured DSMP groups with an emphasis on action-planning, often surrounding nutrition, physical activity, and other health behavior change information reviewed during the SMAs.
Design and Referral
Self-management programs for chronic health conditions are often underutilized. Although HCPs may wish to connect veterans with available programs, time constraints may limit opportunities for detailed discussions with patients about specific aspects of each program. To simplify this process, a 2-hour orientation program was offered that explained individual and group DM self-management options (Figure). During this initial visit, patients met with an interdisciplinary care team (registered dietician, diabetes nurse practitioner, and behavioral health specialist) and were informed about Diabetes Basic Training, DM clinical care practices, and other related resources available at the Cincinnati VAMC (eg, cooking classes, food pantry). Patients received individualized referral recommendations and were urged to consult with their primary care practitioner to finalize their treatment plan.
Shared Medical Appointments
Diabetes Basic Training interventions had an average of 6 to 8 veterans participating in the weekly groups. The first, fifth, and final weeks were SMAs in which an interdisciplinary team collaboratively provided group-based health care for DM. The team consisted of a registered nurse, a prescriber (eg, nurse practitioner), a moderator (eg, psychologist), and a content expert (eg, nutritionist). Before each SMA began, the nurse checked-in patients in the SMA room and collected heart rate and blood pressure, and performed a diabetic foot check. Each SMA consisted of introductions, group-driven discussions (facilitated by an HCP) and troubleshooting DM self-management challenges. During group discussions, the prescriber initiated a 1-on-1 discussion with each patient in a private office regarding their recent laboratory results, medication regimen, and other aspects of DM care. The patient’s medications were refilled and/or adjusted as needed and other orders and referrals were submitted. If a patient had a medical question, the prescriber and moderator engaged the entire group so all individuals could benefit from generating and hearing answers. When discussion slowed, education was provided on topics generated by the group. Frequent topics included challenges managing DM, concerns, how DM impacted daily life and relationships, and sharing successes. As needed, HCPs spoke individually with patients following the SMA. Patients were sometimes asked, but never required, to do homework consistent with standard DM care (eg, recording what they eat or blood sugar levels). Each SMA session lasted about 2 hours.
Diabetes Self-Management Program
The second, third, fourth, sixth, seventh, and eighth weeks of the program were devoted to the DSMP. These sessions were delivered primarily by veteran peers who received appropriate training, observation, and certification. Each 2-hour educational program provided ample practice in many fundamental self-management skills, such as decision making, problem solving, and action planning. Patients were asked, but never required, to practice related skills during the sessions and to create weekly action plans to be completed between sessions that typically involved increasing exercise or improving diet. Patients were encouraged to follow up with HCPs at SMAs when they had questions requiring HCP expertise. If participants had more immediate concerns regarding their treatment plan and/or medications, they contacted their primary care practitioner prior to the next SMA.
As a part of participation in the program, psychosocial and health data and Hb A1c levels at baseline (the closest level to 90 days prior to start) and follow-up (the closest level to 90 days after the final session) were collected.8 In addition, Problem Areas in Diabetes (PAID), Patient Activation Measure (PAM)-13, and Diabetes Self-Management Questionnaire (DSMQ) were administered at 3 points: during the orientation, in the first week, and in the ninth week of the program.
PAID, a 20-item self-report questionnaire designed to capture
Observations
All measures were collected as part of traditional clinical care, and we present initial program evaluation data to demonstrate potential effectiveness of the clinic model. Paired samples t tests were used to examine differences between baseline and follow-up measures for the 24 veteran participants. The age of participants who completed the program ranged from 42 to 74 years (mean, 68 years); 29% of participants were Black veterans and 12% were female. Examination of clinical outcomes indicated that veterans reported significant increases in activation levels for managing their health increasing from a baseline mean (SD) 62.1 (12.3) to 68.4 (14.5) at follow up (t[23] = 2.15, P = .04). Hb A1c levels trended downward from a mean (SD) 8.6% (1.3) at baseline to 8.2% (1.2) at 90-day follow up (t[21] 1.05, P = .30). Similar nonsignificant trends in PAID scores were seen for pre- and postprogram reductions in emotional distress related to having DM from a mean (SD) 7.9 (5.0) at baseline to 6.3 (5.1) (t[18] = 11.51, P = .15), and enhanced self-management of glucose with a mean (SD) 6.5 (1.5) at baseline to 6.8 (1.3) at follow up (t[19] = 0.52, P = .61). The trends found in this study show promising outcomes for this pilot group-based DM treatment, though the small sample size (N = 24) limits statistical power. These findings support further exploration and expansion of interdisciplinary health programs supporting veteran self-management.
Discussion
DM is a condition of epidemic proportions that causes substantial negative health outcomes and costs at a national level. Current standards of DM care do not appear to be reversing these trends. Wider implementation of group-based treatment for DM could improve efficiency of care, increase access to quality care, and reduce burden on individual HCPs.
The VHA continues the transformation of its care system, which shifts toward a patient-centered, proactive focus on veteran well-being. This new whole health approach integrates conventional medical treatment with veteran self-empowerment in the pursuit of health goals based on individual veteran’s identified values.19 This approach emphasizes peer-led explorations of veterans’ aspirations, purpose, and individual mission, personalized health planning, and use of whole health coaches and well-being programs, with both allopathic and complementary and integrative clinical care centered around veterans’ identified goals and priorities.20
Including a program like Diabetes Basic Training as a part of whole health programming could offer several benefits. Diabetes Basic Training is unique in its integration of more traditional SMA structure with psychosocial interventions including values identification and motivational interviewing strategies to enhance patient engagement. Veterans can learn from each other’s experiences and concerns, leading to better DM management knowledge and skills. The group nature of the sessions enhances opportunities for emotional support and reduced isolation, as well as peer accountability for maintaining medication adherence.
By meeting with HCPs from multiple disciplines, veterans are exposed to different perspectives on self-management techniques, including behavioral approaches for overcoming barriers to behavior change. Clinicians have more time to engage with patients, building stronger relationships and trust. SMAs are cost-efficient and time efficient, allowing HCPs to see multiple patients at once, reducing wait times and increasing the number of patients treated in a given time frame.
The COVID-19 pandemic temporarily impacted the ongoing expansion of the program, when so many services were shifted from in-person to virtual classes. Due to staffing and other logistic issues, our pilot program was suspended during that time, but plans to resume the program by early 2024 are moving forward.
CONCLUSIONS
The Diabetes Basic Training program serves as a successful model for implementation within a VAMC. Although the number of veterans with complete data available for analysis was small, the trends exhibited in the preliminary outcome data are promising. We encourage other VAMCs to replicate this program with a larger participant base and evaluate its impact on veteran health outcomes. Next steps include comparing the clinical data from treatment as usual with outcomes from DM group participants. As the program resumes, we will reinitiate recruitment efforts to increase HCP referrals to this program.
1. National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes Statistics. Updated February 2023. Accessed January 22, 2024. https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics
2. US Department of Veterans Affairs, Office of Research and Development. VA research on diabetes. www.research.va.gov. Updated January 15, 2023. Accessed January 22, 2024. https://www.research.va.gov/topics/diabetes.cfm
3. Halter JB, Musi N, McFarland Horne F, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578-2589. doi:10.2337/db14-0020
4. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient and provider expertise to strengthen care management. Updated December 2010. Accessed January 22, 2024. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=1513366&FileName=VA244-14-R-0025-011.pdf
5. Edelman D, Gierisch JM, McDuffie JR, Oddone E, Williams JW Jr. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med. 2015;30(1):99-106. doi:10.1007/s11606-014-2978-7
6. Watts SA, Strauss GJ, Pascuzzi K, et al. Shared medical appointments for patients with diabetes: glycemic reduction in high-risk patients. J Am Assoc Nurse Pract. 2015;27(8):450-456. doi:10.1002/2327-6924.12200
7. Lorig K, Ritter PL, Turner RM, English K, Laurent DD, Greenberg J. Benefits of diabetes self-management for health plan members: a 6-month translation study. J Med Internet Res. 2016;18(6):e164. Published 2016 Jun 24. doi:10.2196/jmir.5568
8. Gilstrap LG, Chernew ME, Nguyen CA, et al. Association between clinical practice group adherence to quality measures and adverse outcomes among adult patients with diabetes. JAMA Netw Open. 2019;2(8):e199139. Published 2019 Aug 2. doi:10.1001/jamanetworkopen.2019.9139
9. Venkataraman K, Tan LS, Bautista DC, et al. Psychometric properties of the Problem Areas in Diabetes (PAID) instrument in Singapore. PLoS One. 2015;10(9):e0136759. Published 2015 Sep 3. doi:10.1371/journal.pone.0136759
10. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20(1):69-72. doi:10.1046/j.1464-5491.2003.00832.x
11. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918-1930. doi:10.1111/j.1475-6773.2005.00438.x
12. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005-1026. doi:10.1111/j.1475-6773.2004.00269.x
13. Ahn YH, Yi CH, Ham OK, Kim BJ. Psychometric properties of the Korean version of the “Patient Activation Measure 13” (PAM13-K) in patients with osteoarthritis. Eval Health Prof. 2015;38(2):255-264. doi:10.1177/0163278714540915
14. Brenk-Franz K, Hibbard JH, Herrmann WJ, et al. Validation of the German version of the patient activation measure 13 (PAM13-D) in an international multicentre study of primary care patients. PLoS One. 2013;8(9):e74786. Published 2013 Sep 30. doi:10.1371/journal.pone.0074786
15. Zill JM, Dwinger S, Kriston L, Rohenkohl A, Härter M, Dirmaier J. Psychometric evaluation of the German version of the Patient Activation Measure (PAM13). BMC Public Health. 2013;13:1027. Published 2013 Oct 30. doi:10.1186/1471-2458-13-1027
16. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual Life Outcomes. 2013;11:138. Published 2013 Aug 13. doi:10.1186/1477-7525-11-138
17. Schmitt A, Reimer A, Hermanns N, et al. assessing diabetes self-management with the Diabetes Self-Management Questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic control. PLoS One. 2016;11(3):e0150774. Published 2016 Mar 3. doi:10.1371/journal.pone.0150774
18. Bukhsh A, Lee SWH, Pusparajah P, Schmitt A, Khan TM. Psychometric properties of the Diabetes Self-Management Questionnaire (DSMQ) in Urdu. Health Qual Life Outcomes. 2017;15(1):200. Published 2017 Oct 12. doi:10.1186/s12955-017-0776-8
19. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12 Suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
20. Bokhour BG, Haun JN, Hyde J, Charns M, Kligler B. Transforming the Veterans Affairs to a whole health system of care: time for action and research. Med Care. 2020;58(4):295-300. doi:10.1097/MLR.0000000000001316
1. National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes Statistics. Updated February 2023. Accessed January 22, 2024. https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics
2. US Department of Veterans Affairs, Office of Research and Development. VA research on diabetes. www.research.va.gov. Updated January 15, 2023. Accessed January 22, 2024. https://www.research.va.gov/topics/diabetes.cfm
3. Halter JB, Musi N, McFarland Horne F, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578-2589. doi:10.2337/db14-0020
4. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient and provider expertise to strengthen care management. Updated December 2010. Accessed January 22, 2024. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=1513366&FileName=VA244-14-R-0025-011.pdf
5. Edelman D, Gierisch JM, McDuffie JR, Oddone E, Williams JW Jr. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med. 2015;30(1):99-106. doi:10.1007/s11606-014-2978-7
6. Watts SA, Strauss GJ, Pascuzzi K, et al. Shared medical appointments for patients with diabetes: glycemic reduction in high-risk patients. J Am Assoc Nurse Pract. 2015;27(8):450-456. doi:10.1002/2327-6924.12200
7. Lorig K, Ritter PL, Turner RM, English K, Laurent DD, Greenberg J. Benefits of diabetes self-management for health plan members: a 6-month translation study. J Med Internet Res. 2016;18(6):e164. Published 2016 Jun 24. doi:10.2196/jmir.5568
8. Gilstrap LG, Chernew ME, Nguyen CA, et al. Association between clinical practice group adherence to quality measures and adverse outcomes among adult patients with diabetes. JAMA Netw Open. 2019;2(8):e199139. Published 2019 Aug 2. doi:10.1001/jamanetworkopen.2019.9139
9. Venkataraman K, Tan LS, Bautista DC, et al. Psychometric properties of the Problem Areas in Diabetes (PAID) instrument in Singapore. PLoS One. 2015;10(9):e0136759. Published 2015 Sep 3. doi:10.1371/journal.pone.0136759
10. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20(1):69-72. doi:10.1046/j.1464-5491.2003.00832.x
11. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918-1930. doi:10.1111/j.1475-6773.2005.00438.x
12. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005-1026. doi:10.1111/j.1475-6773.2004.00269.x
13. Ahn YH, Yi CH, Ham OK, Kim BJ. Psychometric properties of the Korean version of the “Patient Activation Measure 13” (PAM13-K) in patients with osteoarthritis. Eval Health Prof. 2015;38(2):255-264. doi:10.1177/0163278714540915
14. Brenk-Franz K, Hibbard JH, Herrmann WJ, et al. Validation of the German version of the patient activation measure 13 (PAM13-D) in an international multicentre study of primary care patients. PLoS One. 2013;8(9):e74786. Published 2013 Sep 30. doi:10.1371/journal.pone.0074786
15. Zill JM, Dwinger S, Kriston L, Rohenkohl A, Härter M, Dirmaier J. Psychometric evaluation of the German version of the Patient Activation Measure (PAM13). BMC Public Health. 2013;13:1027. Published 2013 Oct 30. doi:10.1186/1471-2458-13-1027
16. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual Life Outcomes. 2013;11:138. Published 2013 Aug 13. doi:10.1186/1477-7525-11-138
17. Schmitt A, Reimer A, Hermanns N, et al. assessing diabetes self-management with the Diabetes Self-Management Questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic control. PLoS One. 2016;11(3):e0150774. Published 2016 Mar 3. doi:10.1371/journal.pone.0150774
18. Bukhsh A, Lee SWH, Pusparajah P, Schmitt A, Khan TM. Psychometric properties of the Diabetes Self-Management Questionnaire (DSMQ) in Urdu. Health Qual Life Outcomes. 2017;15(1):200. Published 2017 Oct 12. doi:10.1186/s12955-017-0776-8
19. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12 Suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
20. Bokhour BG, Haun JN, Hyde J, Charns M, Kligler B. Transforming the Veterans Affairs to a whole health system of care: time for action and research. Med Care. 2020;58(4):295-300. doi:10.1097/MLR.0000000000001316