User login
What is the most effective beta-blocker for heart failure?
Three beta-blockers—carvedilol, metoprolol, and bisoprolol—reduce mortality in chronic heart failure caused by left ventricular systolic dysfunction, when used in addition to diuretics and angiotensin converting enzyme (ACE) inhibitors (strength of recommendation [SOR]: A, based on large randomized placebo-controlled trials). No differences in mortality or patient tolerance have been demonstrated in studies comparing carvedilol and metoprolol (SOR: B, based on small head-to-head trials).
Evidence summary
The Table shows the 5 largest trials of beta-blockers in systolic dysfunction, including patients with both ischemic and nonischemic heart disease. In all trials, the majority of subjects were taking diuretics and either an ACE inhibitor or angiotensin receptor blocker.
The Carvedilol Prospective Randomized Cumulative Survival2 (COPERNICUS) trial, Metoprolol CR/XL Randomized Intervention Trial in Heart Failure3 (MERIT-HF), and Cardiac Insufficiency Bisoprolol Study II4 (CIBIS-II) all showed similar reductions in mortality in moderately ill patients with heart failure.
In contrast, the Beta-Blocker Evaluation of Survival Trial5 (BEST) demonstrated no effect with bucindolol. This suggests there may be differences in effectiveness among beta-blockers in reducing mortality in heart failure, and that it would be unwise to assume that protection is a class effect. We found no meta-analysis that pooled data on individual drugs for comparison purposes.
The US Carvedilol trial1 demonstrated a larger reduction in mortality than that seen in other beta-blocker trials. However, it had several methodologic problems: it was a composite of 4 smaller studies that used exercise tolerance as the primary endpoint; median duration of data collection on subjects was only 6 months; it included many minimally symptomatic patients; the actual number of deaths was small (producing a wide confidence interval); and subjects who did not survive the run-in phase were excluded from analysis.6
Three randomized controlled trials have compared carvedilol and metoprolol head-to-head. The largest7 included 150 subjects with ejection fractions below 35% who were randomized to 1 of the 2 drugs and followed for more than 3 years. Symptom scores and quality of life assessments were similar in the 2 groups. A trend toward lower mortality in the carvedilol group did not reach statistical significance. Peak oxygen uptake during exercise was greater in the metoprolol group. The carvedilol group had a statistically greater improvement in ejection fraction (+10.9 ± 11.0 vs +7.2 ± 7.7 at rest). The Carvedilol or Metoprolol European Trial (COMET), a larger head-to-head trial of carvedilol and metoprolol (N=3029), is ongoing.8
No large studies of older beta-blockers adequately assess mortality in heart failure. One study of propranolol (N=158) showed a 27% reduction in mortality in mild heart failure in the setting of ischemic heart disease.9 A study of atenolol versus placebo in subjects with ejection fraction ≤25% from various causes (N=100) was halted early when atenolol produced a 50% reduction in worsening heart failure and a 71% reduction in cardiac hospitalizations.10 A trend toward improved survival was noted but did not reach statistical significance.
TABLE
Selected trials of beta-blockers for systolic dysfunction
| Study | Drug | N | Mortality reduction (%) | 95% CI (%) | Statistically significant? | NNT | Mean duration of follow-up (months) |
|---|---|---|---|---|---|---|---|
| US Carvedilol1 | Carvedilol | 1094 | (65) | 39–80 | Yes | 22 | 6.5 |
| COPERNICUS2 | Carvedilol | 2289 | (35) | 19–48 | Yes | 14 | 10.4 |
| MERIT-HF3 | Metoprolol | 3991 | (34) | 19–46 | Yes | 26 | 12 |
| CIBIS II4 | Bisoprolol | 2647 | (34) | 19–47 | Yes | 18 | 15.6 |
| BEST5 | Bucindolol | 2708 | (9) | –0.2–22 | No | — | 24 |
| CI, confidence interval; NNT, number needed to treat | |||||||
Recommendations from others
We found no guidelines that specifically endorsed one beta-blocker over another for heart failure.
Fred Grover, Jr, MD
University of Colorado Health Sciences Center, Denver
To provide the best care, we must go beyond the conventional ACE inhibitor and diuretic therapy for congestive heart failure patients. Adding 1 of the 3 beta-blockers (carvedilol, metoprolol, or bisoprolol), as recommended above, will further improve the survival rates and decrease hospitalization rates.
Remember these pearls when using beta-blockers in congestive heart failure:
- Do not start therapy until the patient’s fluid status has been stable for at least 1 month
- Avoid using in patients with bronchospastic disease, symptomatic bradycardia, or advanced heart blockage
- Start with low doses and titrate up slowly as tolerated every 2 weeks to the recommended target range of the beta-blocker chosen
- Decrease the dose if significant bradycardia or atrioventricular block occurs
- Let your patients know that it may take several months of beta-blocker therapy to obtain the protective benefits.
If you encounter difficulties with titration or don’t feel comfortable initiating beta-blocker therapy, consult your cardiologist for help.
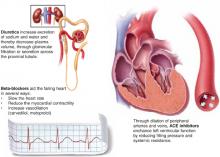
Chronic heart failure
Complementary actions of diuretics, ACE inhibitors, and beta blockers
Evidence shows that the combination of diuretics, ACE inhibitors, and 1 of 3 beta-blockers—carvedilol, metoprolol, bisoprolol—is more effective than just diuretics plus ACE inhibitors. The clinical effect of their combined actions is reduced workload on the failing heart.
1. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 1996;334:1349-1355.
2. Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651-1658.
3. Effect of metoprolol CR/XL in chronic heart failure: Metotprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999;353:2001-2007.
4. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet 1999;353:9-13.
5. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N Engl J Med 2001;344:1659-1667.
6. Hart SM. Influence of beta-blockers on mortality in chronic heart failure. Ann Pharmacother 2000;34:1440-1451.
7. Metra M, Giubbini Raffaele, Nodari E, Boldi E, Modena MG, Dei Cas L. Differential effects of beta-blockers in patients with heart failure: A prospective, randomized, double-blind comparison of the long-term effects of metoprolol versus carvedilol. Circulation 2000;102:546-551.
8. Poole-Wilson PA, Cleland JG, Di Lenarda A, et al. Rationale and design of the carvedilol or metoprolol European trail in patients with chronic heart failure: COMET. Eur J Heart Fail 2002;4:321-329.
9. Aronow WS, Ahn C, Kronzon AI. Effect of propranolol versus no propanolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction ≥40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol 1997;80:207-209.
10. Sturm B, Pacher R, Strametz-Juranek J, et al. Effect of beta 1 blockade with atenolol on progression of heart failure in patients pretreated with high-dose enalapril. Eur J Heart Fail 2000;2:407-412.
Three beta-blockers—carvedilol, metoprolol, and bisoprolol—reduce mortality in chronic heart failure caused by left ventricular systolic dysfunction, when used in addition to diuretics and angiotensin converting enzyme (ACE) inhibitors (strength of recommendation [SOR]: A, based on large randomized placebo-controlled trials). No differences in mortality or patient tolerance have been demonstrated in studies comparing carvedilol and metoprolol (SOR: B, based on small head-to-head trials).
Evidence summary
The Table shows the 5 largest trials of beta-blockers in systolic dysfunction, including patients with both ischemic and nonischemic heart disease. In all trials, the majority of subjects were taking diuretics and either an ACE inhibitor or angiotensin receptor blocker.
The Carvedilol Prospective Randomized Cumulative Survival2 (COPERNICUS) trial, Metoprolol CR/XL Randomized Intervention Trial in Heart Failure3 (MERIT-HF), and Cardiac Insufficiency Bisoprolol Study II4 (CIBIS-II) all showed similar reductions in mortality in moderately ill patients with heart failure.
In contrast, the Beta-Blocker Evaluation of Survival Trial5 (BEST) demonstrated no effect with bucindolol. This suggests there may be differences in effectiveness among beta-blockers in reducing mortality in heart failure, and that it would be unwise to assume that protection is a class effect. We found no meta-analysis that pooled data on individual drugs for comparison purposes.
The US Carvedilol trial1 demonstrated a larger reduction in mortality than that seen in other beta-blocker trials. However, it had several methodologic problems: it was a composite of 4 smaller studies that used exercise tolerance as the primary endpoint; median duration of data collection on subjects was only 6 months; it included many minimally symptomatic patients; the actual number of deaths was small (producing a wide confidence interval); and subjects who did not survive the run-in phase were excluded from analysis.6
Three randomized controlled trials have compared carvedilol and metoprolol head-to-head. The largest7 included 150 subjects with ejection fractions below 35% who were randomized to 1 of the 2 drugs and followed for more than 3 years. Symptom scores and quality of life assessments were similar in the 2 groups. A trend toward lower mortality in the carvedilol group did not reach statistical significance. Peak oxygen uptake during exercise was greater in the metoprolol group. The carvedilol group had a statistically greater improvement in ejection fraction (+10.9 ± 11.0 vs +7.2 ± 7.7 at rest). The Carvedilol or Metoprolol European Trial (COMET), a larger head-to-head trial of carvedilol and metoprolol (N=3029), is ongoing.8
No large studies of older beta-blockers adequately assess mortality in heart failure. One study of propranolol (N=158) showed a 27% reduction in mortality in mild heart failure in the setting of ischemic heart disease.9 A study of atenolol versus placebo in subjects with ejection fraction ≤25% from various causes (N=100) was halted early when atenolol produced a 50% reduction in worsening heart failure and a 71% reduction in cardiac hospitalizations.10 A trend toward improved survival was noted but did not reach statistical significance.
TABLE
Selected trials of beta-blockers for systolic dysfunction
| Study | Drug | N | Mortality reduction (%) | 95% CI (%) | Statistically significant? | NNT | Mean duration of follow-up (months) |
|---|---|---|---|---|---|---|---|
| US Carvedilol1 | Carvedilol | 1094 | (65) | 39–80 | Yes | 22 | 6.5 |
| COPERNICUS2 | Carvedilol | 2289 | (35) | 19–48 | Yes | 14 | 10.4 |
| MERIT-HF3 | Metoprolol | 3991 | (34) | 19–46 | Yes | 26 | 12 |
| CIBIS II4 | Bisoprolol | 2647 | (34) | 19–47 | Yes | 18 | 15.6 |
| BEST5 | Bucindolol | 2708 | (9) | –0.2–22 | No | — | 24 |
| CI, confidence interval; NNT, number needed to treat | |||||||
Recommendations from others
We found no guidelines that specifically endorsed one beta-blocker over another for heart failure.
Fred Grover, Jr, MD
University of Colorado Health Sciences Center, Denver
To provide the best care, we must go beyond the conventional ACE inhibitor and diuretic therapy for congestive heart failure patients. Adding 1 of the 3 beta-blockers (carvedilol, metoprolol, or bisoprolol), as recommended above, will further improve the survival rates and decrease hospitalization rates.
Remember these pearls when using beta-blockers in congestive heart failure:
- Do not start therapy until the patient’s fluid status has been stable for at least 1 month
- Avoid using in patients with bronchospastic disease, symptomatic bradycardia, or advanced heart blockage
- Start with low doses and titrate up slowly as tolerated every 2 weeks to the recommended target range of the beta-blocker chosen
- Decrease the dose if significant bradycardia or atrioventricular block occurs
- Let your patients know that it may take several months of beta-blocker therapy to obtain the protective benefits.
If you encounter difficulties with titration or don’t feel comfortable initiating beta-blocker therapy, consult your cardiologist for help.
Chronic heart failure
Complementary actions of diuretics, ACE inhibitors, and beta blockers
Evidence shows that the combination of diuretics, ACE inhibitors, and 1 of 3 beta-blockers—carvedilol, metoprolol, bisoprolol—is more effective than just diuretics plus ACE inhibitors. The clinical effect of their combined actions is reduced workload on the failing heart.
Three beta-blockers—carvedilol, metoprolol, and bisoprolol—reduce mortality in chronic heart failure caused by left ventricular systolic dysfunction, when used in addition to diuretics and angiotensin converting enzyme (ACE) inhibitors (strength of recommendation [SOR]: A, based on large randomized placebo-controlled trials). No differences in mortality or patient tolerance have been demonstrated in studies comparing carvedilol and metoprolol (SOR: B, based on small head-to-head trials).
Evidence summary
The Table shows the 5 largest trials of beta-blockers in systolic dysfunction, including patients with both ischemic and nonischemic heart disease. In all trials, the majority of subjects were taking diuretics and either an ACE inhibitor or angiotensin receptor blocker.
The Carvedilol Prospective Randomized Cumulative Survival2 (COPERNICUS) trial, Metoprolol CR/XL Randomized Intervention Trial in Heart Failure3 (MERIT-HF), and Cardiac Insufficiency Bisoprolol Study II4 (CIBIS-II) all showed similar reductions in mortality in moderately ill patients with heart failure.
In contrast, the Beta-Blocker Evaluation of Survival Trial5 (BEST) demonstrated no effect with bucindolol. This suggests there may be differences in effectiveness among beta-blockers in reducing mortality in heart failure, and that it would be unwise to assume that protection is a class effect. We found no meta-analysis that pooled data on individual drugs for comparison purposes.
The US Carvedilol trial1 demonstrated a larger reduction in mortality than that seen in other beta-blocker trials. However, it had several methodologic problems: it was a composite of 4 smaller studies that used exercise tolerance as the primary endpoint; median duration of data collection on subjects was only 6 months; it included many minimally symptomatic patients; the actual number of deaths was small (producing a wide confidence interval); and subjects who did not survive the run-in phase were excluded from analysis.6
Three randomized controlled trials have compared carvedilol and metoprolol head-to-head. The largest7 included 150 subjects with ejection fractions below 35% who were randomized to 1 of the 2 drugs and followed for more than 3 years. Symptom scores and quality of life assessments were similar in the 2 groups. A trend toward lower mortality in the carvedilol group did not reach statistical significance. Peak oxygen uptake during exercise was greater in the metoprolol group. The carvedilol group had a statistically greater improvement in ejection fraction (+10.9 ± 11.0 vs +7.2 ± 7.7 at rest). The Carvedilol or Metoprolol European Trial (COMET), a larger head-to-head trial of carvedilol and metoprolol (N=3029), is ongoing.8
No large studies of older beta-blockers adequately assess mortality in heart failure. One study of propranolol (N=158) showed a 27% reduction in mortality in mild heart failure in the setting of ischemic heart disease.9 A study of atenolol versus placebo in subjects with ejection fraction ≤25% from various causes (N=100) was halted early when atenolol produced a 50% reduction in worsening heart failure and a 71% reduction in cardiac hospitalizations.10 A trend toward improved survival was noted but did not reach statistical significance.
TABLE
Selected trials of beta-blockers for systolic dysfunction
| Study | Drug | N | Mortality reduction (%) | 95% CI (%) | Statistically significant? | NNT | Mean duration of follow-up (months) |
|---|---|---|---|---|---|---|---|
| US Carvedilol1 | Carvedilol | 1094 | (65) | 39–80 | Yes | 22 | 6.5 |
| COPERNICUS2 | Carvedilol | 2289 | (35) | 19–48 | Yes | 14 | 10.4 |
| MERIT-HF3 | Metoprolol | 3991 | (34) | 19–46 | Yes | 26 | 12 |
| CIBIS II4 | Bisoprolol | 2647 | (34) | 19–47 | Yes | 18 | 15.6 |
| BEST5 | Bucindolol | 2708 | (9) | –0.2–22 | No | — | 24 |
| CI, confidence interval; NNT, number needed to treat | |||||||
Recommendations from others
We found no guidelines that specifically endorsed one beta-blocker over another for heart failure.
Fred Grover, Jr, MD
University of Colorado Health Sciences Center, Denver
To provide the best care, we must go beyond the conventional ACE inhibitor and diuretic therapy for congestive heart failure patients. Adding 1 of the 3 beta-blockers (carvedilol, metoprolol, or bisoprolol), as recommended above, will further improve the survival rates and decrease hospitalization rates.
Remember these pearls when using beta-blockers in congestive heart failure:
- Do not start therapy until the patient’s fluid status has been stable for at least 1 month
- Avoid using in patients with bronchospastic disease, symptomatic bradycardia, or advanced heart blockage
- Start with low doses and titrate up slowly as tolerated every 2 weeks to the recommended target range of the beta-blocker chosen
- Decrease the dose if significant bradycardia or atrioventricular block occurs
- Let your patients know that it may take several months of beta-blocker therapy to obtain the protective benefits.
If you encounter difficulties with titration or don’t feel comfortable initiating beta-blocker therapy, consult your cardiologist for help.
Chronic heart failure
Complementary actions of diuretics, ACE inhibitors, and beta blockers
Evidence shows that the combination of diuretics, ACE inhibitors, and 1 of 3 beta-blockers—carvedilol, metoprolol, bisoprolol—is more effective than just diuretics plus ACE inhibitors. The clinical effect of their combined actions is reduced workload on the failing heart.
1. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 1996;334:1349-1355.
2. Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651-1658.
3. Effect of metoprolol CR/XL in chronic heart failure: Metotprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999;353:2001-2007.
4. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet 1999;353:9-13.
5. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N Engl J Med 2001;344:1659-1667.
6. Hart SM. Influence of beta-blockers on mortality in chronic heart failure. Ann Pharmacother 2000;34:1440-1451.
7. Metra M, Giubbini Raffaele, Nodari E, Boldi E, Modena MG, Dei Cas L. Differential effects of beta-blockers in patients with heart failure: A prospective, randomized, double-blind comparison of the long-term effects of metoprolol versus carvedilol. Circulation 2000;102:546-551.
8. Poole-Wilson PA, Cleland JG, Di Lenarda A, et al. Rationale and design of the carvedilol or metoprolol European trail in patients with chronic heart failure: COMET. Eur J Heart Fail 2002;4:321-329.
9. Aronow WS, Ahn C, Kronzon AI. Effect of propranolol versus no propanolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction ≥40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol 1997;80:207-209.
10. Sturm B, Pacher R, Strametz-Juranek J, et al. Effect of beta 1 blockade with atenolol on progression of heart failure in patients pretreated with high-dose enalapril. Eur J Heart Fail 2000;2:407-412.
1. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 1996;334:1349-1355.
2. Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651-1658.
3. Effect of metoprolol CR/XL in chronic heart failure: Metotprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999;353:2001-2007.
4. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet 1999;353:9-13.
5. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N Engl J Med 2001;344:1659-1667.
6. Hart SM. Influence of beta-blockers on mortality in chronic heart failure. Ann Pharmacother 2000;34:1440-1451.
7. Metra M, Giubbini Raffaele, Nodari E, Boldi E, Modena MG, Dei Cas L. Differential effects of beta-blockers in patients with heart failure: A prospective, randomized, double-blind comparison of the long-term effects of metoprolol versus carvedilol. Circulation 2000;102:546-551.
8. Poole-Wilson PA, Cleland JG, Di Lenarda A, et al. Rationale and design of the carvedilol or metoprolol European trail in patients with chronic heart failure: COMET. Eur J Heart Fail 2002;4:321-329.
9. Aronow WS, Ahn C, Kronzon AI. Effect of propranolol versus no propanolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction ≥40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol 1997;80:207-209.
10. Sturm B, Pacher R, Strametz-Juranek J, et al. Effect of beta 1 blockade with atenolol on progression of heart failure in patients pretreated with high-dose enalapril. Eur J Heart Fail 2000;2:407-412.
Evidence-based answers from the Family Physicians Inquiries Network
How accurate is the clinical diagnosis of pneumonia?
No element or combination of elements from the clinical history and physical examination are sufficiently sensitive or specific to confirm or exclude acute community-acquired pneumonia (CAP). A chest x-ray is recommended to make the diagnosis (Grade of Recommendation: A, based on well-designed cohort studies). No studies specifically demonstrate improved patient outcomes through use of chest x-ray in adults; however, accurate diagnosis is expected to reduce the number of unnecessary antibiotic prescriptions (Grade of Recommendation: D, based on expert opinion).
Evidence summary
Metlay and colleagues1 found only 4 high-quality, prospective cohort trials evaluating the sensitivity and specificity of the clinical history and physical examination in pneumonia. In each of the 4 studies, the reference standard for the diagnosis of pneumonia was a new infiltrate on chest radiograph. Subjects were community-dwelling adults with acute cough who were seen in ambulatory settings, and who had an average pneumonia prevalence of 7% (range, 3%–38%).1 Although no study specifically addressed the interobserver reliability of the history and physical examination findings in pneumonia, other studies of chest findings typically found variable reproducibility. In a study by Spiteri and associates,2 24 physicians examined 24 patients with a variety of respiratory conditions: only 4 had pneumonia on chest x-ray. The most reliable findings (dullness to percussion and wheezing) had only fair agreement among examiners (kappa approximately 0.5).
Nine symptoms (cough, dyspnea, sputum production, subjective fever, chills, night sweats, myalgias, sore throat, and rhinorrhea) and 3 items in the past medical history (asthma, immunosuppression, and dementia) were associated with pneumonia. For most elements of history, both the positive and negative likelihood ratios (LR+, LR−) were in the indeterminate range of 0.5 to 2.0. No single feature was sufficient to either rule in or rule out the diagnosis.1
Regarding the physical examination, tachypnea, tachycardia, and fever had LR+s between 1.5 and 2.4 in an ambulatory setting. In one study, the absence of any vital sign abnormalities reduced the likelihood of pneumonia substantially (LR− = 0.18), but did not rule out the diagnosis completely.1 Egophony had an LR+ of 5.3. Other physical findings (rhonchi, crackles, decreased breath sounds, dullness to percussion, and bronchial breath sounds) yielded LR+s from 1.5 to 3.5, respectively. Most individual findings were insufficient to diagnose pneumonia. For example, if the baseline prevalence of pneumonia was 5%, the presence of crackles raised the probability to 10% and their absence decreased the probability to 3%.
The sensitivity and specificity of clinical diagnosis varied with the prevalence of pneumonia. In a general practice setting, 20 of 402 patients with cough were diagnosed with pneumonia by chest x-ray.3 Physicians correctly diagnosed 7 patients clinically, and incorrectly diagnosed pneumonia in 22 additional patients.3 At a Veterans Administration hospital, a prospective cohort of 52 men with acute cough and change in sputum production underwent sequential blinded examination by 3 physicians. Rales and bronchial breath sounds were common, and chest x-ray confirmed pneumonia in 28 patients. Sensitivity of clinical diagnosis ranged from 47% to 69%, and specificity from 58% to 75%.4
Several researchers improved diagnostic accuracy by combining multiple elements from the history and physical examination. For example, according to Metlay and colleagues,1 Heckerling et al calculated the probability of pneumonia if up to 5 predictors were present. However, if the prevalence of pneumonia in a primary care population is 5%, the presence of all 5 predictors raises the probability of pneumonia only to 53%.1 The absence of 4 of the 5 findings (fever >37.8°C, heart rate >100 beats per minute, decreased breath sounds, crackles) reduces the risk of pneumonia to 1%, thus eliminating the need for radiography or antibiotics in most situations. If the patient also has asthma, the risk drops even further.
Recommendations from others
The Infectious Diseases Society of North America states that a chest x-ray is necessary for accurate diagnosis. In otherwise healthy adults with acute cough illness, antibiotic therapy is indicated only for pneumonia. A normal chest x-ray obviates the need for antibiotics.5,6
John W. Ely, MD, MSPH
University of Iowa Iowa City
john-ely@uiowa.ed.
The immediate question for clinicians is “Can you treat pneumonia based on clinical findings alone?” Apparently, the answer is “no” unless the radiograph would be unacceptably difficult to obtain (eg, certain nursing home or homebound patients). Can the patient have pneumonia even if the chest radiograph is negative? Subtle early pneumonias sometimes blossom on chest film after a day or two. The diagnosis of pneumonia can be just as much a subjective “call” for the radiologist as “a few crackles” can be for the clinician, so the bottom line is: If you suspect pneumonia, order a chest film.
1. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA 1997;278:1440-5.
2. Spiteri MA, Cook DG, Clarke SW. Reliability of eliciting physical signs in examination of the chest. Lancet 1988;1:873-5.
3. Melbye H, Straume B, Aasebo U, Dale K. Diagnosis of pneumonia in adults in general practice. Relative importance of typical symptoms and abnormal chest signs evaluated against a radiographic reference standard. Scand J Prim Health Care 1992;10:226-33.
4. Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination: relevant or relic? Arch Intern Med 1999;159:1082-7.
5. Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med 2001;134:521-9.
6. Bartlett JG, Dowell SF, Mandell LA, et al. Practice guidelines for the management of community-acquired pneumonia in adults.Infectious Diseases Society of America. Clin Infect Dis 2000;31:347-82.
No element or combination of elements from the clinical history and physical examination are sufficiently sensitive or specific to confirm or exclude acute community-acquired pneumonia (CAP). A chest x-ray is recommended to make the diagnosis (Grade of Recommendation: A, based on well-designed cohort studies). No studies specifically demonstrate improved patient outcomes through use of chest x-ray in adults; however, accurate diagnosis is expected to reduce the number of unnecessary antibiotic prescriptions (Grade of Recommendation: D, based on expert opinion).
Evidence summary
Metlay and colleagues1 found only 4 high-quality, prospective cohort trials evaluating the sensitivity and specificity of the clinical history and physical examination in pneumonia. In each of the 4 studies, the reference standard for the diagnosis of pneumonia was a new infiltrate on chest radiograph. Subjects were community-dwelling adults with acute cough who were seen in ambulatory settings, and who had an average pneumonia prevalence of 7% (range, 3%–38%).1 Although no study specifically addressed the interobserver reliability of the history and physical examination findings in pneumonia, other studies of chest findings typically found variable reproducibility. In a study by Spiteri and associates,2 24 physicians examined 24 patients with a variety of respiratory conditions: only 4 had pneumonia on chest x-ray. The most reliable findings (dullness to percussion and wheezing) had only fair agreement among examiners (kappa approximately 0.5).
Nine symptoms (cough, dyspnea, sputum production, subjective fever, chills, night sweats, myalgias, sore throat, and rhinorrhea) and 3 items in the past medical history (asthma, immunosuppression, and dementia) were associated with pneumonia. For most elements of history, both the positive and negative likelihood ratios (LR+, LR−) were in the indeterminate range of 0.5 to 2.0. No single feature was sufficient to either rule in or rule out the diagnosis.1
Regarding the physical examination, tachypnea, tachycardia, and fever had LR+s between 1.5 and 2.4 in an ambulatory setting. In one study, the absence of any vital sign abnormalities reduced the likelihood of pneumonia substantially (LR− = 0.18), but did not rule out the diagnosis completely.1 Egophony had an LR+ of 5.3. Other physical findings (rhonchi, crackles, decreased breath sounds, dullness to percussion, and bronchial breath sounds) yielded LR+s from 1.5 to 3.5, respectively. Most individual findings were insufficient to diagnose pneumonia. For example, if the baseline prevalence of pneumonia was 5%, the presence of crackles raised the probability to 10% and their absence decreased the probability to 3%.
The sensitivity and specificity of clinical diagnosis varied with the prevalence of pneumonia. In a general practice setting, 20 of 402 patients with cough were diagnosed with pneumonia by chest x-ray.3 Physicians correctly diagnosed 7 patients clinically, and incorrectly diagnosed pneumonia in 22 additional patients.3 At a Veterans Administration hospital, a prospective cohort of 52 men with acute cough and change in sputum production underwent sequential blinded examination by 3 physicians. Rales and bronchial breath sounds were common, and chest x-ray confirmed pneumonia in 28 patients. Sensitivity of clinical diagnosis ranged from 47% to 69%, and specificity from 58% to 75%.4
Several researchers improved diagnostic accuracy by combining multiple elements from the history and physical examination. For example, according to Metlay and colleagues,1 Heckerling et al calculated the probability of pneumonia if up to 5 predictors were present. However, if the prevalence of pneumonia in a primary care population is 5%, the presence of all 5 predictors raises the probability of pneumonia only to 53%.1 The absence of 4 of the 5 findings (fever >37.8°C, heart rate >100 beats per minute, decreased breath sounds, crackles) reduces the risk of pneumonia to 1%, thus eliminating the need for radiography or antibiotics in most situations. If the patient also has asthma, the risk drops even further.
Recommendations from others
The Infectious Diseases Society of North America states that a chest x-ray is necessary for accurate diagnosis. In otherwise healthy adults with acute cough illness, antibiotic therapy is indicated only for pneumonia. A normal chest x-ray obviates the need for antibiotics.5,6
John W. Ely, MD, MSPH
University of Iowa Iowa City
john-ely@uiowa.ed.
The immediate question for clinicians is “Can you treat pneumonia based on clinical findings alone?” Apparently, the answer is “no” unless the radiograph would be unacceptably difficult to obtain (eg, certain nursing home or homebound patients). Can the patient have pneumonia even if the chest radiograph is negative? Subtle early pneumonias sometimes blossom on chest film after a day or two. The diagnosis of pneumonia can be just as much a subjective “call” for the radiologist as “a few crackles” can be for the clinician, so the bottom line is: If you suspect pneumonia, order a chest film.
No element or combination of elements from the clinical history and physical examination are sufficiently sensitive or specific to confirm or exclude acute community-acquired pneumonia (CAP). A chest x-ray is recommended to make the diagnosis (Grade of Recommendation: A, based on well-designed cohort studies). No studies specifically demonstrate improved patient outcomes through use of chest x-ray in adults; however, accurate diagnosis is expected to reduce the number of unnecessary antibiotic prescriptions (Grade of Recommendation: D, based on expert opinion).
Evidence summary
Metlay and colleagues1 found only 4 high-quality, prospective cohort trials evaluating the sensitivity and specificity of the clinical history and physical examination in pneumonia. In each of the 4 studies, the reference standard for the diagnosis of pneumonia was a new infiltrate on chest radiograph. Subjects were community-dwelling adults with acute cough who were seen in ambulatory settings, and who had an average pneumonia prevalence of 7% (range, 3%–38%).1 Although no study specifically addressed the interobserver reliability of the history and physical examination findings in pneumonia, other studies of chest findings typically found variable reproducibility. In a study by Spiteri and associates,2 24 physicians examined 24 patients with a variety of respiratory conditions: only 4 had pneumonia on chest x-ray. The most reliable findings (dullness to percussion and wheezing) had only fair agreement among examiners (kappa approximately 0.5).
Nine symptoms (cough, dyspnea, sputum production, subjective fever, chills, night sweats, myalgias, sore throat, and rhinorrhea) and 3 items in the past medical history (asthma, immunosuppression, and dementia) were associated with pneumonia. For most elements of history, both the positive and negative likelihood ratios (LR+, LR−) were in the indeterminate range of 0.5 to 2.0. No single feature was sufficient to either rule in or rule out the diagnosis.1
Regarding the physical examination, tachypnea, tachycardia, and fever had LR+s between 1.5 and 2.4 in an ambulatory setting. In one study, the absence of any vital sign abnormalities reduced the likelihood of pneumonia substantially (LR− = 0.18), but did not rule out the diagnosis completely.1 Egophony had an LR+ of 5.3. Other physical findings (rhonchi, crackles, decreased breath sounds, dullness to percussion, and bronchial breath sounds) yielded LR+s from 1.5 to 3.5, respectively. Most individual findings were insufficient to diagnose pneumonia. For example, if the baseline prevalence of pneumonia was 5%, the presence of crackles raised the probability to 10% and their absence decreased the probability to 3%.
The sensitivity and specificity of clinical diagnosis varied with the prevalence of pneumonia. In a general practice setting, 20 of 402 patients with cough were diagnosed with pneumonia by chest x-ray.3 Physicians correctly diagnosed 7 patients clinically, and incorrectly diagnosed pneumonia in 22 additional patients.3 At a Veterans Administration hospital, a prospective cohort of 52 men with acute cough and change in sputum production underwent sequential blinded examination by 3 physicians. Rales and bronchial breath sounds were common, and chest x-ray confirmed pneumonia in 28 patients. Sensitivity of clinical diagnosis ranged from 47% to 69%, and specificity from 58% to 75%.4
Several researchers improved diagnostic accuracy by combining multiple elements from the history and physical examination. For example, according to Metlay and colleagues,1 Heckerling et al calculated the probability of pneumonia if up to 5 predictors were present. However, if the prevalence of pneumonia in a primary care population is 5%, the presence of all 5 predictors raises the probability of pneumonia only to 53%.1 The absence of 4 of the 5 findings (fever >37.8°C, heart rate >100 beats per minute, decreased breath sounds, crackles) reduces the risk of pneumonia to 1%, thus eliminating the need for radiography or antibiotics in most situations. If the patient also has asthma, the risk drops even further.
Recommendations from others
The Infectious Diseases Society of North America states that a chest x-ray is necessary for accurate diagnosis. In otherwise healthy adults with acute cough illness, antibiotic therapy is indicated only for pneumonia. A normal chest x-ray obviates the need for antibiotics.5,6
John W. Ely, MD, MSPH
University of Iowa Iowa City
john-ely@uiowa.ed.
The immediate question for clinicians is “Can you treat pneumonia based on clinical findings alone?” Apparently, the answer is “no” unless the radiograph would be unacceptably difficult to obtain (eg, certain nursing home or homebound patients). Can the patient have pneumonia even if the chest radiograph is negative? Subtle early pneumonias sometimes blossom on chest film after a day or two. The diagnosis of pneumonia can be just as much a subjective “call” for the radiologist as “a few crackles” can be for the clinician, so the bottom line is: If you suspect pneumonia, order a chest film.
1. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA 1997;278:1440-5.
2. Spiteri MA, Cook DG, Clarke SW. Reliability of eliciting physical signs in examination of the chest. Lancet 1988;1:873-5.
3. Melbye H, Straume B, Aasebo U, Dale K. Diagnosis of pneumonia in adults in general practice. Relative importance of typical symptoms and abnormal chest signs evaluated against a radiographic reference standard. Scand J Prim Health Care 1992;10:226-33.
4. Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination: relevant or relic? Arch Intern Med 1999;159:1082-7.
5. Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med 2001;134:521-9.
6. Bartlett JG, Dowell SF, Mandell LA, et al. Practice guidelines for the management of community-acquired pneumonia in adults.Infectious Diseases Society of America. Clin Infect Dis 2000;31:347-82.
1. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA 1997;278:1440-5.
2. Spiteri MA, Cook DG, Clarke SW. Reliability of eliciting physical signs in examination of the chest. Lancet 1988;1:873-5.
3. Melbye H, Straume B, Aasebo U, Dale K. Diagnosis of pneumonia in adults in general practice. Relative importance of typical symptoms and abnormal chest signs evaluated against a radiographic reference standard. Scand J Prim Health Care 1992;10:226-33.
4. Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination: relevant or relic? Arch Intern Med 1999;159:1082-7.
5. Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med 2001;134:521-9.
6. Bartlett JG, Dowell SF, Mandell LA, et al. Practice guidelines for the management of community-acquired pneumonia in adults.Infectious Diseases Society of America. Clin Infect Dis 2000;31:347-82.
Evidence-based answers from the Family Physicians Inquiries Network