User login
Medication Adherence and Operating Room Efficiency for a Surgical Subspecialty
Inefficiencies in the operating room (OR) can occur before, during, and between cases and lead to multiple problems, including delays in the delivery of patient care. They also have a negative financial impact for the institution and cause frustration for surgeons, anesthesiologists, and other OR staff. Ultimately, delays lead to dissatisfaction among patients and health care providers. Operating room efficiency increasingly is becoming a marker of the quality of surgical care.
The Institute of Medicine (IOM) identified timeliness and efficiency as 2 of 6 areas for improvement for U.S. hospitals.1 Organizations such as the Centers for Medicare and Medicaid Services, Agency for Healthcare Research and Quality, IOM, Institute for Healthcare Improvement, The Joint Commission, Leapfrog Group, and National Quality Forum are beginning to monitor patient care workflow in order to improve quality while reducing costs.2
About 187 million Americans take at least 1 prescription drug.3 An estimated 20% to 50% of patients do not take their medications as prescribed and are said to be nonadherent with therapy.4,5 Nonadherence to medication also has been shown to result in increased health risks and costs of up to $290 billion.6 Patients who receive pharmacist services achieve better clinical outcomes for chronic diseases than national standards.7
Among patients with a chronic disease, poor adherence tends to result in poor outcomes and increased medical costs. Yet these are the patients who face the most risks in surgery and require the most preoperative care. Several studies have evaluated the frequency of medication nonadherence prior to surgery and its effect on surgery cancellations. These studies have examined a variety of factors related to patient preoperative education, medications, food intake, bowel prep, etc.
In a VA Puget Sound Health Care System study, 23% of patients undergoing ambulatory surgery were nonadherent to preoperative medication instructions.8 Studies have found that up to 7% of cancellations were impacted by medication nonadherence and preoperative education.9-13 Furthermore, studies using large-scale databases have found medically treatable conditions as a significant source of surgical delay.14 Had these conditions been treated a priori, delay in surgery would not have occurred. Unfortunately, it is not clear whether the delays were the result of missed preoperative checks or medication nonadherence.
Ensuring patient safety, including reducing medical errors and adverse events (AEs), is imperative in the surgical workflow. In 1999, the IOM estimated that medical error was a leading cause of death in the U.S. and resulted in up to 100,000 deaths annually.15
In a retrospective study of 15,000 cases, Gawande and colleagues found that 66% of all AEs were surgical and 54% of these were preventable.16 In addition to improving reporting systems, creating a culture of safety with all members of the health care team and building a partnership with patients during preoperative visits can ensure increased adherence and reduced medication AEs. In a neurosurgical cohort of patients, Bernstein and colleagues found that 85% of patients were subjected to at least 1 error; 10% of the errors were major, and 65% were deemed preventable.17
The purpose of this study is to evaluate whether redundancy built into the patient care protocols prior to surgery helps catch errors as demonstrated in time-out analyses.18 Decreasing these errors would lead to fewer surgical cancellations and medical workup delays. The authors hypothesize that a structured preoperative pharmacologic workup would result in decreased preoperative delay in the surgical workflow.
Methods
The study protocol was reviewed and determined to be a quality improvement/quality assurance initiative, which exempted it from institutional review board or other oversight committee review, at the Minneapolis VA Health Care System. The VA OR Efficiency Task Force identified medication adherence as a possible source of delay. A study therefore was undertaken to determine the adherence rate and how it impacted operative delays. Data were extracted from this study to test the stated hypothesis and compare with historic data.
Fifty consecutive patients undergoing neurosurgical procedures from May 2010 through July 2010 were retrospectively reviewed and evaluated. All patients had a preoperative consultation with a pharmacist and the neurosurgery coordinator who reviewed all medications with the patient and gave specific instructions on which medications should be continued or discontinued prior to the surgery date. This information was documented on the OR Medication Compliance Worksheet and included in the patient’s preoperative chart by the neurosurgery coordinator. On the day of surgery, all active medications on this chart were reviewed with the patient by the anesthesiologist and documented on the OR Medication Compliance Worksheet. The worksheet was then sent to the neurosurgery coordinator for secondary review and analysis.
To evaluate delays, the authors reviewed the patient anesthesiology records. Delays were defined as either cancellations of the case due to medication nonadherence, which would make it unsafe to proceed with surgery, or minor delays due to medication nonadherence, which required further preoperative assessment and workup before proceeding with surgery. Cancelled cases were defined as cases on the final copy of the published OR schedule that did not occur.
Medication Adherence Program
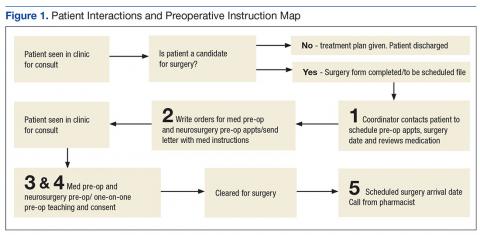
In order to ensure medication adherence prior to surgery there were 5 points of contact with a patient from the time the patient was scheduled for surgery and the date of the surgery (Figure 1):
- The coordinator reviewed medications with patient at time of scheduling
- A letter was sent with specific instructions about medications
- Preoperative medicine clearance
- Preoperative neurosurgery appointment
- Call from pharmacist 1 week before surgery
Results
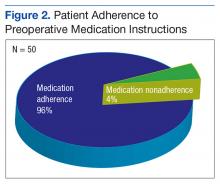
The authors reviewed 10 months of the neurosurgical service prior to initiation of the protocol. Of 317 analyzed cases, 30 were delayed/cancelled. Among these, 5 cases with the possibility of a 6th were cancelled due to medication issues. Following the initialization of the study, 50 patients underwent preoperative counseling with the pharmacist and the neurosurgery coordinator and had an OR Medication Compliance Worksheet created.
Review of the OR Medication Compliance Worksheet demonstrated that 2 patients were nonadherent with their medications.
Discussion
The OR is one of the most expensive areas in an acute care hospital.2 Cancellations or delays can have significant negative financial implications (about $1,500 per hour of lost revenue).19 In order to improve OR efficiency and reduce preoperative delays, the causes of preoperative delays must be determined.
Some delays and cancellations result from either preoperative or perioperative issues. Prolonged wait time and postponement may cause preoperative delays. Perioperative delays include delays in getting into the OR once the patient has arrived in the hospital as well as delays during the operation. These delays can be due to both human error and system deficiencies.20
One Toronto, Canada study looked at the different etiologies for delays in cranial and spinal procedures and found that equipment failure followed by physical transit into the OR were the top reasons for delays.21 These researchers also found that first cases each day sometimes had a higher incidence of delays than did subsequent cases because several ORs prepare to start simultaneously, which causes an increased demand on hospital support services (eg, registration desk, imaging department, nurses in the patient holding area, or transportation). The number of these support staff remains constant throughout the day, whereas the first-case patients all arrive at about the same time, causing a bottleneck in the early morning. The authors looked at 1 facet of the delay problem as an ongoing analysis for hospital efficiency improvement.
With the implementation of a simple 5-step process, medication adherence was > 90% and the impact of nonadherence on surgical procedure delays was eliminated during the trial period. In this sample, nonadherence did not impact surgery, which resulted in fewer delays and cancellations. The process emphasized repetition and communication, involving 5 reminders between the date of OR scheduling and the date of the actual surgery. The authors found that in this quality improvement study, redundancy in the workflow actually improved the efficiency of the patient’s hospital course.
Within the OR, there are many perspectives to consider for improving OR efficiency. For instance, Archer and colleagues present several distinct perspectives: that of the health care institution, the individual practitioner, the patient, and evidenced-based medicine.2 According to Strum and colleagues, OR inefficiency is the sum of under- and overutilized time and efficiency is highest when OR inefficiency is minimized.22 An OR is considered underutilized when it is staffed at regular wages but not used for surgery, setup, or cleanup. An OR is considered overutilized when the OR staff receives overtime wages, multiplied by the relative cost of overtime compared with straight time. Delayed or cancelled surgeries can result in idle operating room staff, while repeat or correlative studies (ie, electrocardiogram, drug levels) may overutilize support services.
Limitations
This study has obvious limitations due to its small scale. Because the protocol implementation resulted in few delays, a very large cohort would have been necessary to attain statistical power.
Conclusion
By improving OR efficiency and reducing preoperative delays, surgical capacity can be increased.
In this study, the authors demonstrate that with little addition of cost, medication nonadherence can be reduced or eliminated as an issue for surgical delays. With the implementation of the 5-step reminder process as well as the addition of a pharmacist consultation/visit, medication adherence was > 90% among preoperative patients in this small study. With the number of patients with complex medication regimens, increasing medication adherence in the preoperative period is not only important in reducing operative delays, but also an opportunity to ensure the patient is safe and optimally treated. ˜
1. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washing ton, DC: National Academy Press; 2001. https://www.nap.edu/catalog/10027/crossing-the-quality -chasm-a-new-health-system-for-the.
2. Archer T, Macario A. The drive for operating room efficiency will increase quality of patient care. Curr Opin Anaesthesiol. 2006;19(2):171-176.
3. Lundy J; Kaiser Family Foundation. Prescription drug trends. https://kaiserfamilyfoundation.files .wordpress.com/2013/01/3057-08.pdf. Published May 2010. Accessed January 26, 2017.
4. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-497.
5. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200-209.
6. National Priorities Partnership, NEHI. Improving patient medication adherence: a $100+ billion opportunity. http://adhereforhealth.org/wp-content/uploads/pdf/ImprovingPatientMedicationAdherence-NPP_Patient_Medication_Adherence_NQF.pdf. Published April 2011. Accessed January 26, 2017.
7. Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167(6):540-550.
8. Chew JD, Bradley KA, Flum DR, Cornia PB, Koepsell TD. The impact of low health literacy on surgical practice. Am J Surg. 2004;188(3):250-253.
9. van Klei WA, Moons KG, Rutten CL, et al. The effect of outpatient preoperative evaluation of hospital inpatients on cancellation of surgery and length of hospital stay. Anesth Analg. 2002;94(3):644-649.
10. Sanjay P, Dodds A, Miller E, Arumugam PJ, Woodward A. Cancelled elective operations: an observational study from a district general hospital. J Health Organ Manag. 2007;21(1):54-58.
11. Schofield WN, Rubin GL, Piza M, et al. Cancellation of operations on the day of intended surgery at a major Australian referral hospital. Med J Aust. 2005;182(12):612-615.
12. Zafar A, Mufti TS, Griffin S, Ahmed S, Ansari JA. Cancelled elective general surgical operations in Ayub Teaching Hospital. J Ayub Med Coll Abbottabad. 2007;19(3):64-66.
13. Knox M, Myers E, Hurley M. The impact of pre-operative assessment clinics on elective surgical case cancellations. Surgeon. 2009;7(2):76-78.
14. Phruetthiphat OA, Gao Y, Anthony CA, Pugely AJ, Warth LC, Callaghan JJ. Incidence of and preoperative risk factors for surgical delay in primary total hip arthroplasty: analysis from the American College of Surgeons National Surgical Quality Improvement Program. J Arthroplasty. 2016;31(11): 2432-2436.
15. Kohn LT, Corrigan JM, Donaldson MD, eds; Institute of Medicine; Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies; 2000. https://www.nap.edu/catalog/9728/to-err-is-human-building-a-safer-health-system.
16. Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126(1):66-75.
17. Bernstein M, Massicotte E, Etchells E. Error in neurosurgery: a prospective pilot study. Can J Neurol Sci. 2001;28(suppl 2):S60.
18. Altpeter T, Luckhardt K, Lewis JN, Harken AH, Polk HC Jr. Expanded surgical time out: a key to real-time data collection and quality improvement. J Am Coll Surg. 2007;204(4):527-532.
19. Dexter F, Marcon E, Epstein RH, Ledolter J. Validation of statistical methods to compare cancellation rates on the day of surgery. Anesth Analg. 2005;101(2):465-473.
20. Etchells E, O’Neill C, Bernstein M. Patient safety in surgery: error detection and prevention. World J Surg. 2003;27(8):936-941.
21. Wong J, Khu KJ, Kaderali Z, Bernstein M. Delays in the operating room: signs of an imperfect system. Can J Surg. 2010;53(3):189-195.
22. Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning: a minimal cost analysis model. Anesthesiology. 1999;90(4):1176-1185.
Inefficiencies in the operating room (OR) can occur before, during, and between cases and lead to multiple problems, including delays in the delivery of patient care. They also have a negative financial impact for the institution and cause frustration for surgeons, anesthesiologists, and other OR staff. Ultimately, delays lead to dissatisfaction among patients and health care providers. Operating room efficiency increasingly is becoming a marker of the quality of surgical care.
The Institute of Medicine (IOM) identified timeliness and efficiency as 2 of 6 areas for improvement for U.S. hospitals.1 Organizations such as the Centers for Medicare and Medicaid Services, Agency for Healthcare Research and Quality, IOM, Institute for Healthcare Improvement, The Joint Commission, Leapfrog Group, and National Quality Forum are beginning to monitor patient care workflow in order to improve quality while reducing costs.2
About 187 million Americans take at least 1 prescription drug.3 An estimated 20% to 50% of patients do not take their medications as prescribed and are said to be nonadherent with therapy.4,5 Nonadherence to medication also has been shown to result in increased health risks and costs of up to $290 billion.6 Patients who receive pharmacist services achieve better clinical outcomes for chronic diseases than national standards.7
Among patients with a chronic disease, poor adherence tends to result in poor outcomes and increased medical costs. Yet these are the patients who face the most risks in surgery and require the most preoperative care. Several studies have evaluated the frequency of medication nonadherence prior to surgery and its effect on surgery cancellations. These studies have examined a variety of factors related to patient preoperative education, medications, food intake, bowel prep, etc.
In a VA Puget Sound Health Care System study, 23% of patients undergoing ambulatory surgery were nonadherent to preoperative medication instructions.8 Studies have found that up to 7% of cancellations were impacted by medication nonadherence and preoperative education.9-13 Furthermore, studies using large-scale databases have found medically treatable conditions as a significant source of surgical delay.14 Had these conditions been treated a priori, delay in surgery would not have occurred. Unfortunately, it is not clear whether the delays were the result of missed preoperative checks or medication nonadherence.
Ensuring patient safety, including reducing medical errors and adverse events (AEs), is imperative in the surgical workflow. In 1999, the IOM estimated that medical error was a leading cause of death in the U.S. and resulted in up to 100,000 deaths annually.15
In a retrospective study of 15,000 cases, Gawande and colleagues found that 66% of all AEs were surgical and 54% of these were preventable.16 In addition to improving reporting systems, creating a culture of safety with all members of the health care team and building a partnership with patients during preoperative visits can ensure increased adherence and reduced medication AEs. In a neurosurgical cohort of patients, Bernstein and colleagues found that 85% of patients were subjected to at least 1 error; 10% of the errors were major, and 65% were deemed preventable.17
The purpose of this study is to evaluate whether redundancy built into the patient care protocols prior to surgery helps catch errors as demonstrated in time-out analyses.18 Decreasing these errors would lead to fewer surgical cancellations and medical workup delays. The authors hypothesize that a structured preoperative pharmacologic workup would result in decreased preoperative delay in the surgical workflow.
Methods
The study protocol was reviewed and determined to be a quality improvement/quality assurance initiative, which exempted it from institutional review board or other oversight committee review, at the Minneapolis VA Health Care System. The VA OR Efficiency Task Force identified medication adherence as a possible source of delay. A study therefore was undertaken to determine the adherence rate and how it impacted operative delays. Data were extracted from this study to test the stated hypothesis and compare with historic data.
Fifty consecutive patients undergoing neurosurgical procedures from May 2010 through July 2010 were retrospectively reviewed and evaluated. All patients had a preoperative consultation with a pharmacist and the neurosurgery coordinator who reviewed all medications with the patient and gave specific instructions on which medications should be continued or discontinued prior to the surgery date. This information was documented on the OR Medication Compliance Worksheet and included in the patient’s preoperative chart by the neurosurgery coordinator. On the day of surgery, all active medications on this chart were reviewed with the patient by the anesthesiologist and documented on the OR Medication Compliance Worksheet. The worksheet was then sent to the neurosurgery coordinator for secondary review and analysis.
To evaluate delays, the authors reviewed the patient anesthesiology records. Delays were defined as either cancellations of the case due to medication nonadherence, which would make it unsafe to proceed with surgery, or minor delays due to medication nonadherence, which required further preoperative assessment and workup before proceeding with surgery. Cancelled cases were defined as cases on the final copy of the published OR schedule that did not occur.
Medication Adherence Program
In order to ensure medication adherence prior to surgery there were 5 points of contact with a patient from the time the patient was scheduled for surgery and the date of the surgery (Figure 1):
- The coordinator reviewed medications with patient at time of scheduling
- A letter was sent with specific instructions about medications
- Preoperative medicine clearance
- Preoperative neurosurgery appointment
- Call from pharmacist 1 week before surgery
Results
The authors reviewed 10 months of the neurosurgical service prior to initiation of the protocol. Of 317 analyzed cases, 30 were delayed/cancelled. Among these, 5 cases with the possibility of a 6th were cancelled due to medication issues. Following the initialization of the study, 50 patients underwent preoperative counseling with the pharmacist and the neurosurgery coordinator and had an OR Medication Compliance Worksheet created.
Review of the OR Medication Compliance Worksheet demonstrated that 2 patients were nonadherent with their medications.
Discussion
The OR is one of the most expensive areas in an acute care hospital.2 Cancellations or delays can have significant negative financial implications (about $1,500 per hour of lost revenue).19 In order to improve OR efficiency and reduce preoperative delays, the causes of preoperative delays must be determined.
Some delays and cancellations result from either preoperative or perioperative issues. Prolonged wait time and postponement may cause preoperative delays. Perioperative delays include delays in getting into the OR once the patient has arrived in the hospital as well as delays during the operation. These delays can be due to both human error and system deficiencies.20
One Toronto, Canada study looked at the different etiologies for delays in cranial and spinal procedures and found that equipment failure followed by physical transit into the OR were the top reasons for delays.21 These researchers also found that first cases each day sometimes had a higher incidence of delays than did subsequent cases because several ORs prepare to start simultaneously, which causes an increased demand on hospital support services (eg, registration desk, imaging department, nurses in the patient holding area, or transportation). The number of these support staff remains constant throughout the day, whereas the first-case patients all arrive at about the same time, causing a bottleneck in the early morning. The authors looked at 1 facet of the delay problem as an ongoing analysis for hospital efficiency improvement.
With the implementation of a simple 5-step process, medication adherence was > 90% and the impact of nonadherence on surgical procedure delays was eliminated during the trial period. In this sample, nonadherence did not impact surgery, which resulted in fewer delays and cancellations. The process emphasized repetition and communication, involving 5 reminders between the date of OR scheduling and the date of the actual surgery. The authors found that in this quality improvement study, redundancy in the workflow actually improved the efficiency of the patient’s hospital course.
Within the OR, there are many perspectives to consider for improving OR efficiency. For instance, Archer and colleagues present several distinct perspectives: that of the health care institution, the individual practitioner, the patient, and evidenced-based medicine.2 According to Strum and colleagues, OR inefficiency is the sum of under- and overutilized time and efficiency is highest when OR inefficiency is minimized.22 An OR is considered underutilized when it is staffed at regular wages but not used for surgery, setup, or cleanup. An OR is considered overutilized when the OR staff receives overtime wages, multiplied by the relative cost of overtime compared with straight time. Delayed or cancelled surgeries can result in idle operating room staff, while repeat or correlative studies (ie, electrocardiogram, drug levels) may overutilize support services.
Limitations
This study has obvious limitations due to its small scale. Because the protocol implementation resulted in few delays, a very large cohort would have been necessary to attain statistical power.
Conclusion
By improving OR efficiency and reducing preoperative delays, surgical capacity can be increased.
In this study, the authors demonstrate that with little addition of cost, medication nonadherence can be reduced or eliminated as an issue for surgical delays. With the implementation of the 5-step reminder process as well as the addition of a pharmacist consultation/visit, medication adherence was > 90% among preoperative patients in this small study. With the number of patients with complex medication regimens, increasing medication adherence in the preoperative period is not only important in reducing operative delays, but also an opportunity to ensure the patient is safe and optimally treated. ˜
Inefficiencies in the operating room (OR) can occur before, during, and between cases and lead to multiple problems, including delays in the delivery of patient care. They also have a negative financial impact for the institution and cause frustration for surgeons, anesthesiologists, and other OR staff. Ultimately, delays lead to dissatisfaction among patients and health care providers. Operating room efficiency increasingly is becoming a marker of the quality of surgical care.
The Institute of Medicine (IOM) identified timeliness and efficiency as 2 of 6 areas for improvement for U.S. hospitals.1 Organizations such as the Centers for Medicare and Medicaid Services, Agency for Healthcare Research and Quality, IOM, Institute for Healthcare Improvement, The Joint Commission, Leapfrog Group, and National Quality Forum are beginning to monitor patient care workflow in order to improve quality while reducing costs.2
About 187 million Americans take at least 1 prescription drug.3 An estimated 20% to 50% of patients do not take their medications as prescribed and are said to be nonadherent with therapy.4,5 Nonadherence to medication also has been shown to result in increased health risks and costs of up to $290 billion.6 Patients who receive pharmacist services achieve better clinical outcomes for chronic diseases than national standards.7
Among patients with a chronic disease, poor adherence tends to result in poor outcomes and increased medical costs. Yet these are the patients who face the most risks in surgery and require the most preoperative care. Several studies have evaluated the frequency of medication nonadherence prior to surgery and its effect on surgery cancellations. These studies have examined a variety of factors related to patient preoperative education, medications, food intake, bowel prep, etc.
In a VA Puget Sound Health Care System study, 23% of patients undergoing ambulatory surgery were nonadherent to preoperative medication instructions.8 Studies have found that up to 7% of cancellations were impacted by medication nonadherence and preoperative education.9-13 Furthermore, studies using large-scale databases have found medically treatable conditions as a significant source of surgical delay.14 Had these conditions been treated a priori, delay in surgery would not have occurred. Unfortunately, it is not clear whether the delays were the result of missed preoperative checks or medication nonadherence.
Ensuring patient safety, including reducing medical errors and adverse events (AEs), is imperative in the surgical workflow. In 1999, the IOM estimated that medical error was a leading cause of death in the U.S. and resulted in up to 100,000 deaths annually.15
In a retrospective study of 15,000 cases, Gawande and colleagues found that 66% of all AEs were surgical and 54% of these were preventable.16 In addition to improving reporting systems, creating a culture of safety with all members of the health care team and building a partnership with patients during preoperative visits can ensure increased adherence and reduced medication AEs. In a neurosurgical cohort of patients, Bernstein and colleagues found that 85% of patients were subjected to at least 1 error; 10% of the errors were major, and 65% were deemed preventable.17
The purpose of this study is to evaluate whether redundancy built into the patient care protocols prior to surgery helps catch errors as demonstrated in time-out analyses.18 Decreasing these errors would lead to fewer surgical cancellations and medical workup delays. The authors hypothesize that a structured preoperative pharmacologic workup would result in decreased preoperative delay in the surgical workflow.
Methods
The study protocol was reviewed and determined to be a quality improvement/quality assurance initiative, which exempted it from institutional review board or other oversight committee review, at the Minneapolis VA Health Care System. The VA OR Efficiency Task Force identified medication adherence as a possible source of delay. A study therefore was undertaken to determine the adherence rate and how it impacted operative delays. Data were extracted from this study to test the stated hypothesis and compare with historic data.
Fifty consecutive patients undergoing neurosurgical procedures from May 2010 through July 2010 were retrospectively reviewed and evaluated. All patients had a preoperative consultation with a pharmacist and the neurosurgery coordinator who reviewed all medications with the patient and gave specific instructions on which medications should be continued or discontinued prior to the surgery date. This information was documented on the OR Medication Compliance Worksheet and included in the patient’s preoperative chart by the neurosurgery coordinator. On the day of surgery, all active medications on this chart were reviewed with the patient by the anesthesiologist and documented on the OR Medication Compliance Worksheet. The worksheet was then sent to the neurosurgery coordinator for secondary review and analysis.
To evaluate delays, the authors reviewed the patient anesthesiology records. Delays were defined as either cancellations of the case due to medication nonadherence, which would make it unsafe to proceed with surgery, or minor delays due to medication nonadherence, which required further preoperative assessment and workup before proceeding with surgery. Cancelled cases were defined as cases on the final copy of the published OR schedule that did not occur.
Medication Adherence Program
In order to ensure medication adherence prior to surgery there were 5 points of contact with a patient from the time the patient was scheduled for surgery and the date of the surgery (Figure 1):
- The coordinator reviewed medications with patient at time of scheduling
- A letter was sent with specific instructions about medications
- Preoperative medicine clearance
- Preoperative neurosurgery appointment
- Call from pharmacist 1 week before surgery
Results
The authors reviewed 10 months of the neurosurgical service prior to initiation of the protocol. Of 317 analyzed cases, 30 were delayed/cancelled. Among these, 5 cases with the possibility of a 6th were cancelled due to medication issues. Following the initialization of the study, 50 patients underwent preoperative counseling with the pharmacist and the neurosurgery coordinator and had an OR Medication Compliance Worksheet created.
Review of the OR Medication Compliance Worksheet demonstrated that 2 patients were nonadherent with their medications.
Discussion
The OR is one of the most expensive areas in an acute care hospital.2 Cancellations or delays can have significant negative financial implications (about $1,500 per hour of lost revenue).19 In order to improve OR efficiency and reduce preoperative delays, the causes of preoperative delays must be determined.
Some delays and cancellations result from either preoperative or perioperative issues. Prolonged wait time and postponement may cause preoperative delays. Perioperative delays include delays in getting into the OR once the patient has arrived in the hospital as well as delays during the operation. These delays can be due to both human error and system deficiencies.20
One Toronto, Canada study looked at the different etiologies for delays in cranial and spinal procedures and found that equipment failure followed by physical transit into the OR were the top reasons for delays.21 These researchers also found that first cases each day sometimes had a higher incidence of delays than did subsequent cases because several ORs prepare to start simultaneously, which causes an increased demand on hospital support services (eg, registration desk, imaging department, nurses in the patient holding area, or transportation). The number of these support staff remains constant throughout the day, whereas the first-case patients all arrive at about the same time, causing a bottleneck in the early morning. The authors looked at 1 facet of the delay problem as an ongoing analysis for hospital efficiency improvement.
With the implementation of a simple 5-step process, medication adherence was > 90% and the impact of nonadherence on surgical procedure delays was eliminated during the trial period. In this sample, nonadherence did not impact surgery, which resulted in fewer delays and cancellations. The process emphasized repetition and communication, involving 5 reminders between the date of OR scheduling and the date of the actual surgery. The authors found that in this quality improvement study, redundancy in the workflow actually improved the efficiency of the patient’s hospital course.
Within the OR, there are many perspectives to consider for improving OR efficiency. For instance, Archer and colleagues present several distinct perspectives: that of the health care institution, the individual practitioner, the patient, and evidenced-based medicine.2 According to Strum and colleagues, OR inefficiency is the sum of under- and overutilized time and efficiency is highest when OR inefficiency is minimized.22 An OR is considered underutilized when it is staffed at regular wages but not used for surgery, setup, or cleanup. An OR is considered overutilized when the OR staff receives overtime wages, multiplied by the relative cost of overtime compared with straight time. Delayed or cancelled surgeries can result in idle operating room staff, while repeat or correlative studies (ie, electrocardiogram, drug levels) may overutilize support services.
Limitations
This study has obvious limitations due to its small scale. Because the protocol implementation resulted in few delays, a very large cohort would have been necessary to attain statistical power.
Conclusion
By improving OR efficiency and reducing preoperative delays, surgical capacity can be increased.
In this study, the authors demonstrate that with little addition of cost, medication nonadherence can be reduced or eliminated as an issue for surgical delays. With the implementation of the 5-step reminder process as well as the addition of a pharmacist consultation/visit, medication adherence was > 90% among preoperative patients in this small study. With the number of patients with complex medication regimens, increasing medication adherence in the preoperative period is not only important in reducing operative delays, but also an opportunity to ensure the patient is safe and optimally treated. ˜
1. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washing ton, DC: National Academy Press; 2001. https://www.nap.edu/catalog/10027/crossing-the-quality -chasm-a-new-health-system-for-the.
2. Archer T, Macario A. The drive for operating room efficiency will increase quality of patient care. Curr Opin Anaesthesiol. 2006;19(2):171-176.
3. Lundy J; Kaiser Family Foundation. Prescription drug trends. https://kaiserfamilyfoundation.files .wordpress.com/2013/01/3057-08.pdf. Published May 2010. Accessed January 26, 2017.
4. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-497.
5. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200-209.
6. National Priorities Partnership, NEHI. Improving patient medication adherence: a $100+ billion opportunity. http://adhereforhealth.org/wp-content/uploads/pdf/ImprovingPatientMedicationAdherence-NPP_Patient_Medication_Adherence_NQF.pdf. Published April 2011. Accessed January 26, 2017.
7. Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167(6):540-550.
8. Chew JD, Bradley KA, Flum DR, Cornia PB, Koepsell TD. The impact of low health literacy on surgical practice. Am J Surg. 2004;188(3):250-253.
9. van Klei WA, Moons KG, Rutten CL, et al. The effect of outpatient preoperative evaluation of hospital inpatients on cancellation of surgery and length of hospital stay. Anesth Analg. 2002;94(3):644-649.
10. Sanjay P, Dodds A, Miller E, Arumugam PJ, Woodward A. Cancelled elective operations: an observational study from a district general hospital. J Health Organ Manag. 2007;21(1):54-58.
11. Schofield WN, Rubin GL, Piza M, et al. Cancellation of operations on the day of intended surgery at a major Australian referral hospital. Med J Aust. 2005;182(12):612-615.
12. Zafar A, Mufti TS, Griffin S, Ahmed S, Ansari JA. Cancelled elective general surgical operations in Ayub Teaching Hospital. J Ayub Med Coll Abbottabad. 2007;19(3):64-66.
13. Knox M, Myers E, Hurley M. The impact of pre-operative assessment clinics on elective surgical case cancellations. Surgeon. 2009;7(2):76-78.
14. Phruetthiphat OA, Gao Y, Anthony CA, Pugely AJ, Warth LC, Callaghan JJ. Incidence of and preoperative risk factors for surgical delay in primary total hip arthroplasty: analysis from the American College of Surgeons National Surgical Quality Improvement Program. J Arthroplasty. 2016;31(11): 2432-2436.
15. Kohn LT, Corrigan JM, Donaldson MD, eds; Institute of Medicine; Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies; 2000. https://www.nap.edu/catalog/9728/to-err-is-human-building-a-safer-health-system.
16. Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126(1):66-75.
17. Bernstein M, Massicotte E, Etchells E. Error in neurosurgery: a prospective pilot study. Can J Neurol Sci. 2001;28(suppl 2):S60.
18. Altpeter T, Luckhardt K, Lewis JN, Harken AH, Polk HC Jr. Expanded surgical time out: a key to real-time data collection and quality improvement. J Am Coll Surg. 2007;204(4):527-532.
19. Dexter F, Marcon E, Epstein RH, Ledolter J. Validation of statistical methods to compare cancellation rates on the day of surgery. Anesth Analg. 2005;101(2):465-473.
20. Etchells E, O’Neill C, Bernstein M. Patient safety in surgery: error detection and prevention. World J Surg. 2003;27(8):936-941.
21. Wong J, Khu KJ, Kaderali Z, Bernstein M. Delays in the operating room: signs of an imperfect system. Can J Surg. 2010;53(3):189-195.
22. Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning: a minimal cost analysis model. Anesthesiology. 1999;90(4):1176-1185.
1. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washing ton, DC: National Academy Press; 2001. https://www.nap.edu/catalog/10027/crossing-the-quality -chasm-a-new-health-system-for-the.
2. Archer T, Macario A. The drive for operating room efficiency will increase quality of patient care. Curr Opin Anaesthesiol. 2006;19(2):171-176.
3. Lundy J; Kaiser Family Foundation. Prescription drug trends. https://kaiserfamilyfoundation.files .wordpress.com/2013/01/3057-08.pdf. Published May 2010. Accessed January 26, 2017.
4. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-497.
5. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200-209.
6. National Priorities Partnership, NEHI. Improving patient medication adherence: a $100+ billion opportunity. http://adhereforhealth.org/wp-content/uploads/pdf/ImprovingPatientMedicationAdherence-NPP_Patient_Medication_Adherence_NQF.pdf. Published April 2011. Accessed January 26, 2017.
7. Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167(6):540-550.
8. Chew JD, Bradley KA, Flum DR, Cornia PB, Koepsell TD. The impact of low health literacy on surgical practice. Am J Surg. 2004;188(3):250-253.
9. van Klei WA, Moons KG, Rutten CL, et al. The effect of outpatient preoperative evaluation of hospital inpatients on cancellation of surgery and length of hospital stay. Anesth Analg. 2002;94(3):644-649.
10. Sanjay P, Dodds A, Miller E, Arumugam PJ, Woodward A. Cancelled elective operations: an observational study from a district general hospital. J Health Organ Manag. 2007;21(1):54-58.
11. Schofield WN, Rubin GL, Piza M, et al. Cancellation of operations on the day of intended surgery at a major Australian referral hospital. Med J Aust. 2005;182(12):612-615.
12. Zafar A, Mufti TS, Griffin S, Ahmed S, Ansari JA. Cancelled elective general surgical operations in Ayub Teaching Hospital. J Ayub Med Coll Abbottabad. 2007;19(3):64-66.
13. Knox M, Myers E, Hurley M. The impact of pre-operative assessment clinics on elective surgical case cancellations. Surgeon. 2009;7(2):76-78.
14. Phruetthiphat OA, Gao Y, Anthony CA, Pugely AJ, Warth LC, Callaghan JJ. Incidence of and preoperative risk factors for surgical delay in primary total hip arthroplasty: analysis from the American College of Surgeons National Surgical Quality Improvement Program. J Arthroplasty. 2016;31(11): 2432-2436.
15. Kohn LT, Corrigan JM, Donaldson MD, eds; Institute of Medicine; Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies; 2000. https://www.nap.edu/catalog/9728/to-err-is-human-building-a-safer-health-system.
16. Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126(1):66-75.
17. Bernstein M, Massicotte E, Etchells E. Error in neurosurgery: a prospective pilot study. Can J Neurol Sci. 2001;28(suppl 2):S60.
18. Altpeter T, Luckhardt K, Lewis JN, Harken AH, Polk HC Jr. Expanded surgical time out: a key to real-time data collection and quality improvement. J Am Coll Surg. 2007;204(4):527-532.
19. Dexter F, Marcon E, Epstein RH, Ledolter J. Validation of statistical methods to compare cancellation rates on the day of surgery. Anesth Analg. 2005;101(2):465-473.
20. Etchells E, O’Neill C, Bernstein M. Patient safety in surgery: error detection and prevention. World J Surg. 2003;27(8):936-941.
21. Wong J, Khu KJ, Kaderali Z, Bernstein M. Delays in the operating room: signs of an imperfect system. Can J Surg. 2010;53(3):189-195.
22. Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning: a minimal cost analysis model. Anesthesiology. 1999;90(4):1176-1185.