User login
‘Med check’ appointments: How to minimize your malpractice risk
Medical malpractice claims can arise in any type of health care setting. The purpose of this article is to discuss the risk of medical malpractice suits in the context of brief “med checks,” which are 15- to 20-minute follow-up appointments for psychiatric outpatient medication management. Similar issues arise in brief new patient and transfer visits.
Malpractice hinges on ‘reasonableness’
Malpractice is an allegation of professional negligence.1 More specifically, it is an allegation that a clinician violated an existing duty by deviating from the standard of care, and that deviation caused damages.2 Medical malpractice claims involve questions about whether there was a deviation from the standard of care (whether the clinician failed to exercise a reasonable degree of skill and care given the context of the situation) and whether there was causation (whether a deviation caused a patient’s damages).3 These are fact-based determinations. Thus, the legal resolution of a malpractice claim is based on the facts of each specific case.
The advisability of 15-minute med checks and the associated limitation on a clinician’s ability to provide talk therapy are beyond the scope of this article. What is clear, however, is that not all brief med check appointments are created equal. Their safety and efficacy are dictated by the milieu in which they exist.
Practically speaking, although many factors need to be considered, the standard of care in a medical malpractice lawsuit is based on reasonableness.4-6 One strategy to proactively manage your malpractice risk is to consider—either for your existing job or before accepting a new position—whether your agency’s setup for brief med checks will allow you to practice reasonably. This article provides information to help you answer this question and describes a hypothetical case vignette to illustrate how certain factors might help lower the chances of facing a malpractice suit.
Established patients
In med check appointments for established patients, consider the patient population, the availability of pre- and postvisit support services, and contingency plans (Table).
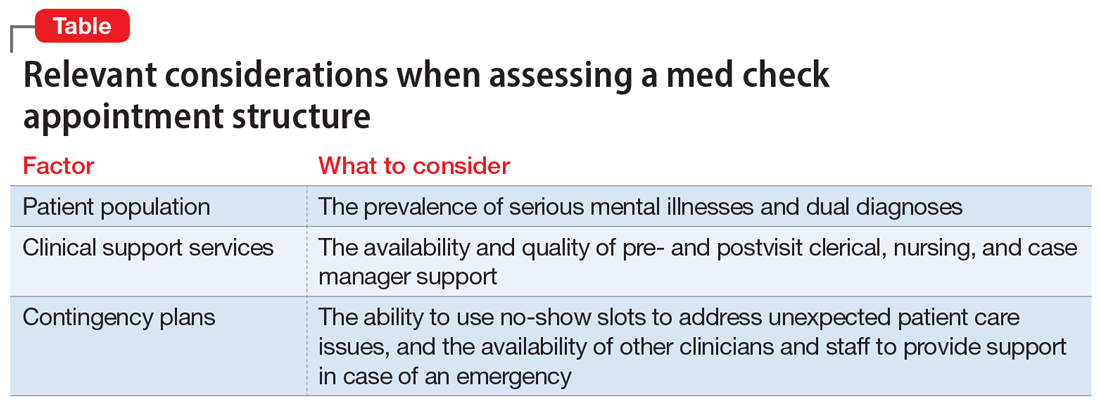
Different patient populations require different levels of treatment. Consider, for example, a patient with anxiety and trauma who is actively engaged with a therapist who works at the same agency as their psychiatrist, where the medication management appointments are solely for selective serotonin reuptake inhibitor refills. Compare that to a dual-diagnosis patient—with a psychotic and substance use disorder—who has had poor medication compliance and frequent rehospitalizations. The first patient is more likely to be reasonably managed in a 15-minute med check. The second patient would need significantly more pre- and postvisit support services. This consideration is relevant from a clinical perspective, and if a bad outcome occurs, from a malpractice perspective. Patient populations are not homogeneous; the reasonableness of a clinician’s actions during a brief med check visit depends on the specific patient.
Pre- and postvisit support services vary greatly from clinic to clinic. They range from clerical support (eg, calling a pharmacy to ensure that a patient’s medication is available for same-day pickup) to nursing support (eg, an injection nurse who is on site and can immediately provide a patient with a missed injection) to case manager support (eg, a case manager to facilitate coordination of care, such as by having a patient fill out record releases and then working to ensure that relevant hospital records are received prior to the next visit). The real-world availability of these services can determine the feasibility of safely conducting a 15-minute med check visit.
Continue to: Regardless of the patient population...
Regardless of the patient population, unexpected situations will arise. It could be a patient with posttraumatic stress disorder who was recently retraumatized and is in the midst of disclosing this new trauma at the end of a 15-minute visit. Or it could be a patient with dual diagnoses who comes to the agency intoxicated and manic, describing a plan to kill his neighbor with a shotgun. A clinician’s ability to meet the standard of care, and act reasonably within the confines of a brief med check structure, can thus depend on whether there are means of adequately managing such emergent situations.
Some clinics have fairly high no-show rates. Leaving no-show slots open for administrative time can provide a means of managing emergent situations. If, however, they are automatically rebooked with walk-ins, brief visits become more challenging. Thus, when assessing contingency plan logistics, consider the no-show rate, what happens when there are no-shows, how many other clinicians are available on a given day, and whether staff is available to provide support (eg, sitting with a patient while waiting for an ambulance).
New and transfer patients
Brief visits for new or transfer patients require the same assessment described above. However, there are additional considerations regarding previsit support services. Some clinics use clinical social workers to perform intake evaluations before a new patient sees the psychiatrist. A high-quality intake evaluation can allow a psychiatrist to focus, in a shorter amount of time, on a patient’s medication needs. An additional time saver is having support staff who will obtain relevant medical records before a patient’s first psychiatric visit. Such actions can greatly increase the efficacy of a new patient appointment for the prescribing clinician.
The reliability of and level of detail assessed in prior evaluations can be particularly relevant when considering a job providing coverage as locum tenens, when all patients will be new to you. Unfortunately, if you are not employed at a clinic, it can be hard to assess this ahead of time. If you know colleagues in the area where you are considering taking a locum position, ask for their opinions about the quality of work at the agency.
Case vignette
Mr. J is a 30-year-old man with schizoaffective disorder. For several years, he has been followed once every 4 weeks at the local clinic. During the first year of treatment, he had numerous hospitalizations due to medication noncompliance, psychotic episodes, and threats of violence against his mother. For the past year, he had been stable on the same dose of an oral antipsychotic medication (risperidone 2 mg twice a day). Then he stopped taking his medication, became increasingly psychotic, and, while holding a butcher knife, threatened to kill his mother. His mother called 911 and Mr. J was hospitalized.
Continue to: While in the hospital...
While in the hospital, Mr. J was restarted on risperidone 2 mg twice a day, and lithium 600 mg twice a day was added. As part of discharge planning, the hospital social worker set up an outpatient appointment with Dr. R, Mr. J’s treating psychiatrist at the clinic. That appointment was scheduled as a 15-minute med check. At the visit, Dr. R did not have or try to obtain a copy of the hospital discharge summary. Mr. J told Dr. R that he had been hospitalized because he had run out of his oral antipsychotic, and that it had been restarted during the hospitalization. Dr. R—who did not know about the recent incident involving a butcher knife or the subsequent medication changes—continued Mr. J’s risperidone, but did not continue his lithium because she did not know it had been added.
Dr. R scheduled a 4-week follow-up visit for Mr. J. Then she went on maternity leave. Because the agency was short-staffed, they hired Dr. C—a locum tenens—to see all of Dr. R’s established patients in 15-minute time slots.
At their first visit, Mr. J told Dr. C that he was gaining too much weight from his antipsychotic and wanted to know if it would be OK to decrease the dose. Dr. C reviewed Dr. R’s last office note but, due to limited time, did not review any other notes. Although Dr. C had 2 no-shows that day, the clinic had a policy that required Dr. C to see walk-ins whenever there was a no-show.
Dr. C did not know of Mr. J’s threats of violence or the medication changes associated with his recent hospitalization (they were not referenced in Dr. R’s last note). Dr. C decreased the dose of Mr. J’s risperidone from 2 mg twice a day to 0.5 mg twice a day. He did not do a violence risk assessment. Two weeks after the visit with Dr. C, Mr. J, who had become increasingly depressed and psychotic, killed his mother and died by suicide.
The estates of Mr. J and his mother filed a medical malpractice lawsuit against Dr. R and Dr. C. Both psychiatrists had a duty to Mr. J. Whether there was a duty to Mr. J’s mother would depend in part on the state’s duty to protect laws. Either way, the malpractice case would hinge on whether the psychiatrists’ conduct fell below the standard of care.
Continue to: In this case...
In this case, the critical issues were Dr. R’s failure to obtain and review the recent hospital records and Dr. C’s decision to decrease the antipsychotic dose. Of particular concern is Dr. C’s decision to decrease the antipsychotic dose without reviewing more information from past records, and the resultant failure to perform a violence risk assessment. These deviations cannot be blamed entirely on the brevity of the med check appointment. They could happen in a clinic that allotted longer time periods for follow-up visits, but they are, however, more likely to occur in a short med check appointment due to time constraints.
The likelihood of these errors could have been reduced by additional support services, as well as more time for Dr. C to see each patient who was new to him. For example, if there had been a support person available to obtain hospital records prior to the postdischarge appointment, Dr. R and Dr. C would have been more likely to be aware of the violent threat associated with Mr. J’s hospitalization. Additionally, if the busy clinicians had contingency plans to assess complicated patients, such as the ability to use no-show time to deal with difficult situations, Dr. C could have taken more time to review past records.
Bottom Line
When working in a setting that involves brief med check appointments, assess the agency structure, and whether it will allow you to practice reasonably. This will be relevant clinically and may reduce the risk of malpractice lawsuits. Reasonableness of a clinician’s actions is a fact-specific question and is influenced by multiple factors, including the patient population, the availability and quality of an agency’s support services, and contingency plans.
Related Resources
- Mossman D. Successfully navigating the 15-minute ‘med check.’ Current Psychiatry. 2010;9(6):40-43.
- Olfson M, Marcus SC. National trends in outpatient psychotherapy. Am J Psychiatry. 2010;167(12):1456-1463.
Drug Brand Names
Lithium • Eskalith, Lithobid
Risperidone • Risperdal
1. Malpractice. In: Garner BA, ed. Black’s Law Dictionary. 11th ed. Thomson West; 2019:1148.
2. Frierson RL, Joshi KG. Malpractice law and psychiatry: an overview. Focus. 2019;17:332-336. doi:10.1176/appi.focus.20190017
3. Negligence Based Claims. In: Boumil MM, Hattis PA, eds. Medical Liability in a Nutshell. 4th ed. West Academic Publishing; 2017:43-88
4. Peters PG. The quiet demise of deference to custom: malpractice law at the millennium. Washington and Lee Law Review. 2000;57(1):163-205. Accessed July 8, 2022. https://scholarlycommons.law.wlu.edu/wlulr/vol57/iss1/5
5. Simon RI. Standard-of-care testimony: best practices or reasonable care? J Am Acad Psychiatry Law. 2005;33(1):8-11. Accessed July 8, 2022. http://jaapl.org/content/33/1/8
6. Behrens SA. Call in Houdini: the time has come to be released from the geographic straightjacket known as the locality rule. Drake Law Review. 2008; 56(3):753-790. Accessed June 20, 2022. https://lawreviewdrake.files.wordpress.com/2015/06/lrvol56-3_behrens.pdf
Medical malpractice claims can arise in any type of health care setting. The purpose of this article is to discuss the risk of medical malpractice suits in the context of brief “med checks,” which are 15- to 20-minute follow-up appointments for psychiatric outpatient medication management. Similar issues arise in brief new patient and transfer visits.
Malpractice hinges on ‘reasonableness’
Malpractice is an allegation of professional negligence.1 More specifically, it is an allegation that a clinician violated an existing duty by deviating from the standard of care, and that deviation caused damages.2 Medical malpractice claims involve questions about whether there was a deviation from the standard of care (whether the clinician failed to exercise a reasonable degree of skill and care given the context of the situation) and whether there was causation (whether a deviation caused a patient’s damages).3 These are fact-based determinations. Thus, the legal resolution of a malpractice claim is based on the facts of each specific case.
The advisability of 15-minute med checks and the associated limitation on a clinician’s ability to provide talk therapy are beyond the scope of this article. What is clear, however, is that not all brief med check appointments are created equal. Their safety and efficacy are dictated by the milieu in which they exist.
Practically speaking, although many factors need to be considered, the standard of care in a medical malpractice lawsuit is based on reasonableness.4-6 One strategy to proactively manage your malpractice risk is to consider—either for your existing job or before accepting a new position—whether your agency’s setup for brief med checks will allow you to practice reasonably. This article provides information to help you answer this question and describes a hypothetical case vignette to illustrate how certain factors might help lower the chances of facing a malpractice suit.
Established patients
In med check appointments for established patients, consider the patient population, the availability of pre- and postvisit support services, and contingency plans (Table).
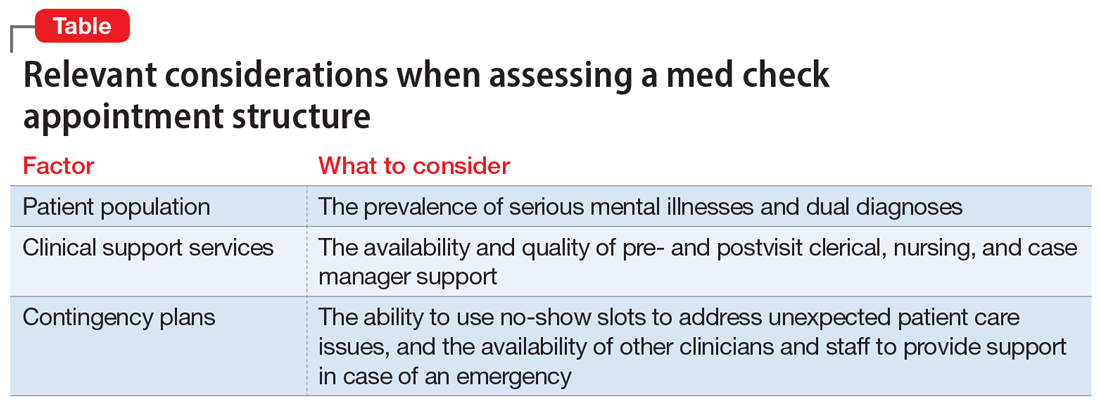
Different patient populations require different levels of treatment. Consider, for example, a patient with anxiety and trauma who is actively engaged with a therapist who works at the same agency as their psychiatrist, where the medication management appointments are solely for selective serotonin reuptake inhibitor refills. Compare that to a dual-diagnosis patient—with a psychotic and substance use disorder—who has had poor medication compliance and frequent rehospitalizations. The first patient is more likely to be reasonably managed in a 15-minute med check. The second patient would need significantly more pre- and postvisit support services. This consideration is relevant from a clinical perspective, and if a bad outcome occurs, from a malpractice perspective. Patient populations are not homogeneous; the reasonableness of a clinician’s actions during a brief med check visit depends on the specific patient.
Pre- and postvisit support services vary greatly from clinic to clinic. They range from clerical support (eg, calling a pharmacy to ensure that a patient’s medication is available for same-day pickup) to nursing support (eg, an injection nurse who is on site and can immediately provide a patient with a missed injection) to case manager support (eg, a case manager to facilitate coordination of care, such as by having a patient fill out record releases and then working to ensure that relevant hospital records are received prior to the next visit). The real-world availability of these services can determine the feasibility of safely conducting a 15-minute med check visit.
Continue to: Regardless of the patient population...
Regardless of the patient population, unexpected situations will arise. It could be a patient with posttraumatic stress disorder who was recently retraumatized and is in the midst of disclosing this new trauma at the end of a 15-minute visit. Or it could be a patient with dual diagnoses who comes to the agency intoxicated and manic, describing a plan to kill his neighbor with a shotgun. A clinician’s ability to meet the standard of care, and act reasonably within the confines of a brief med check structure, can thus depend on whether there are means of adequately managing such emergent situations.
Some clinics have fairly high no-show rates. Leaving no-show slots open for administrative time can provide a means of managing emergent situations. If, however, they are automatically rebooked with walk-ins, brief visits become more challenging. Thus, when assessing contingency plan logistics, consider the no-show rate, what happens when there are no-shows, how many other clinicians are available on a given day, and whether staff is available to provide support (eg, sitting with a patient while waiting for an ambulance).
New and transfer patients
Brief visits for new or transfer patients require the same assessment described above. However, there are additional considerations regarding previsit support services. Some clinics use clinical social workers to perform intake evaluations before a new patient sees the psychiatrist. A high-quality intake evaluation can allow a psychiatrist to focus, in a shorter amount of time, on a patient’s medication needs. An additional time saver is having support staff who will obtain relevant medical records before a patient’s first psychiatric visit. Such actions can greatly increase the efficacy of a new patient appointment for the prescribing clinician.
The reliability of and level of detail assessed in prior evaluations can be particularly relevant when considering a job providing coverage as locum tenens, when all patients will be new to you. Unfortunately, if you are not employed at a clinic, it can be hard to assess this ahead of time. If you know colleagues in the area where you are considering taking a locum position, ask for their opinions about the quality of work at the agency.
Case vignette
Mr. J is a 30-year-old man with schizoaffective disorder. For several years, he has been followed once every 4 weeks at the local clinic. During the first year of treatment, he had numerous hospitalizations due to medication noncompliance, psychotic episodes, and threats of violence against his mother. For the past year, he had been stable on the same dose of an oral antipsychotic medication (risperidone 2 mg twice a day). Then he stopped taking his medication, became increasingly psychotic, and, while holding a butcher knife, threatened to kill his mother. His mother called 911 and Mr. J was hospitalized.
Continue to: While in the hospital...
While in the hospital, Mr. J was restarted on risperidone 2 mg twice a day, and lithium 600 mg twice a day was added. As part of discharge planning, the hospital social worker set up an outpatient appointment with Dr. R, Mr. J’s treating psychiatrist at the clinic. That appointment was scheduled as a 15-minute med check. At the visit, Dr. R did not have or try to obtain a copy of the hospital discharge summary. Mr. J told Dr. R that he had been hospitalized because he had run out of his oral antipsychotic, and that it had been restarted during the hospitalization. Dr. R—who did not know about the recent incident involving a butcher knife or the subsequent medication changes—continued Mr. J’s risperidone, but did not continue his lithium because she did not know it had been added.
Dr. R scheduled a 4-week follow-up visit for Mr. J. Then she went on maternity leave. Because the agency was short-staffed, they hired Dr. C—a locum tenens—to see all of Dr. R’s established patients in 15-minute time slots.
At their first visit, Mr. J told Dr. C that he was gaining too much weight from his antipsychotic and wanted to know if it would be OK to decrease the dose. Dr. C reviewed Dr. R’s last office note but, due to limited time, did not review any other notes. Although Dr. C had 2 no-shows that day, the clinic had a policy that required Dr. C to see walk-ins whenever there was a no-show.
Dr. C did not know of Mr. J’s threats of violence or the medication changes associated with his recent hospitalization (they were not referenced in Dr. R’s last note). Dr. C decreased the dose of Mr. J’s risperidone from 2 mg twice a day to 0.5 mg twice a day. He did not do a violence risk assessment. Two weeks after the visit with Dr. C, Mr. J, who had become increasingly depressed and psychotic, killed his mother and died by suicide.
The estates of Mr. J and his mother filed a medical malpractice lawsuit against Dr. R and Dr. C. Both psychiatrists had a duty to Mr. J. Whether there was a duty to Mr. J’s mother would depend in part on the state’s duty to protect laws. Either way, the malpractice case would hinge on whether the psychiatrists’ conduct fell below the standard of care.
Continue to: In this case...
In this case, the critical issues were Dr. R’s failure to obtain and review the recent hospital records and Dr. C’s decision to decrease the antipsychotic dose. Of particular concern is Dr. C’s decision to decrease the antipsychotic dose without reviewing more information from past records, and the resultant failure to perform a violence risk assessment. These deviations cannot be blamed entirely on the brevity of the med check appointment. They could happen in a clinic that allotted longer time periods for follow-up visits, but they are, however, more likely to occur in a short med check appointment due to time constraints.
The likelihood of these errors could have been reduced by additional support services, as well as more time for Dr. C to see each patient who was new to him. For example, if there had been a support person available to obtain hospital records prior to the postdischarge appointment, Dr. R and Dr. C would have been more likely to be aware of the violent threat associated with Mr. J’s hospitalization. Additionally, if the busy clinicians had contingency plans to assess complicated patients, such as the ability to use no-show time to deal with difficult situations, Dr. C could have taken more time to review past records.
Bottom Line
When working in a setting that involves brief med check appointments, assess the agency structure, and whether it will allow you to practice reasonably. This will be relevant clinically and may reduce the risk of malpractice lawsuits. Reasonableness of a clinician’s actions is a fact-specific question and is influenced by multiple factors, including the patient population, the availability and quality of an agency’s support services, and contingency plans.
Related Resources
- Mossman D. Successfully navigating the 15-minute ‘med check.’ Current Psychiatry. 2010;9(6):40-43.
- Olfson M, Marcus SC. National trends in outpatient psychotherapy. Am J Psychiatry. 2010;167(12):1456-1463.
Drug Brand Names
Lithium • Eskalith, Lithobid
Risperidone • Risperdal
Medical malpractice claims can arise in any type of health care setting. The purpose of this article is to discuss the risk of medical malpractice suits in the context of brief “med checks,” which are 15- to 20-minute follow-up appointments for psychiatric outpatient medication management. Similar issues arise in brief new patient and transfer visits.
Malpractice hinges on ‘reasonableness’
Malpractice is an allegation of professional negligence.1 More specifically, it is an allegation that a clinician violated an existing duty by deviating from the standard of care, and that deviation caused damages.2 Medical malpractice claims involve questions about whether there was a deviation from the standard of care (whether the clinician failed to exercise a reasonable degree of skill and care given the context of the situation) and whether there was causation (whether a deviation caused a patient’s damages).3 These are fact-based determinations. Thus, the legal resolution of a malpractice claim is based on the facts of each specific case.
The advisability of 15-minute med checks and the associated limitation on a clinician’s ability to provide talk therapy are beyond the scope of this article. What is clear, however, is that not all brief med check appointments are created equal. Their safety and efficacy are dictated by the milieu in which they exist.
Practically speaking, although many factors need to be considered, the standard of care in a medical malpractice lawsuit is based on reasonableness.4-6 One strategy to proactively manage your malpractice risk is to consider—either for your existing job or before accepting a new position—whether your agency’s setup for brief med checks will allow you to practice reasonably. This article provides information to help you answer this question and describes a hypothetical case vignette to illustrate how certain factors might help lower the chances of facing a malpractice suit.
Established patients
In med check appointments for established patients, consider the patient population, the availability of pre- and postvisit support services, and contingency plans (Table).
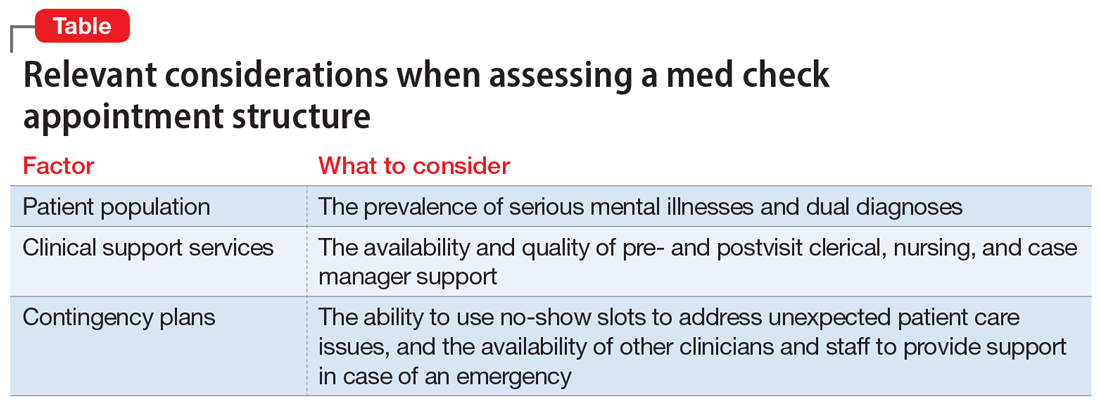
Different patient populations require different levels of treatment. Consider, for example, a patient with anxiety and trauma who is actively engaged with a therapist who works at the same agency as their psychiatrist, where the medication management appointments are solely for selective serotonin reuptake inhibitor refills. Compare that to a dual-diagnosis patient—with a psychotic and substance use disorder—who has had poor medication compliance and frequent rehospitalizations. The first patient is more likely to be reasonably managed in a 15-minute med check. The second patient would need significantly more pre- and postvisit support services. This consideration is relevant from a clinical perspective, and if a bad outcome occurs, from a malpractice perspective. Patient populations are not homogeneous; the reasonableness of a clinician’s actions during a brief med check visit depends on the specific patient.
Pre- and postvisit support services vary greatly from clinic to clinic. They range from clerical support (eg, calling a pharmacy to ensure that a patient’s medication is available for same-day pickup) to nursing support (eg, an injection nurse who is on site and can immediately provide a patient with a missed injection) to case manager support (eg, a case manager to facilitate coordination of care, such as by having a patient fill out record releases and then working to ensure that relevant hospital records are received prior to the next visit). The real-world availability of these services can determine the feasibility of safely conducting a 15-minute med check visit.
Continue to: Regardless of the patient population...
Regardless of the patient population, unexpected situations will arise. It could be a patient with posttraumatic stress disorder who was recently retraumatized and is in the midst of disclosing this new trauma at the end of a 15-minute visit. Or it could be a patient with dual diagnoses who comes to the agency intoxicated and manic, describing a plan to kill his neighbor with a shotgun. A clinician’s ability to meet the standard of care, and act reasonably within the confines of a brief med check structure, can thus depend on whether there are means of adequately managing such emergent situations.
Some clinics have fairly high no-show rates. Leaving no-show slots open for administrative time can provide a means of managing emergent situations. If, however, they are automatically rebooked with walk-ins, brief visits become more challenging. Thus, when assessing contingency plan logistics, consider the no-show rate, what happens when there are no-shows, how many other clinicians are available on a given day, and whether staff is available to provide support (eg, sitting with a patient while waiting for an ambulance).
New and transfer patients
Brief visits for new or transfer patients require the same assessment described above. However, there are additional considerations regarding previsit support services. Some clinics use clinical social workers to perform intake evaluations before a new patient sees the psychiatrist. A high-quality intake evaluation can allow a psychiatrist to focus, in a shorter amount of time, on a patient’s medication needs. An additional time saver is having support staff who will obtain relevant medical records before a patient’s first psychiatric visit. Such actions can greatly increase the efficacy of a new patient appointment for the prescribing clinician.
The reliability of and level of detail assessed in prior evaluations can be particularly relevant when considering a job providing coverage as locum tenens, when all patients will be new to you. Unfortunately, if you are not employed at a clinic, it can be hard to assess this ahead of time. If you know colleagues in the area where you are considering taking a locum position, ask for their opinions about the quality of work at the agency.
Case vignette
Mr. J is a 30-year-old man with schizoaffective disorder. For several years, he has been followed once every 4 weeks at the local clinic. During the first year of treatment, he had numerous hospitalizations due to medication noncompliance, psychotic episodes, and threats of violence against his mother. For the past year, he had been stable on the same dose of an oral antipsychotic medication (risperidone 2 mg twice a day). Then he stopped taking his medication, became increasingly psychotic, and, while holding a butcher knife, threatened to kill his mother. His mother called 911 and Mr. J was hospitalized.
Continue to: While in the hospital...
While in the hospital, Mr. J was restarted on risperidone 2 mg twice a day, and lithium 600 mg twice a day was added. As part of discharge planning, the hospital social worker set up an outpatient appointment with Dr. R, Mr. J’s treating psychiatrist at the clinic. That appointment was scheduled as a 15-minute med check. At the visit, Dr. R did not have or try to obtain a copy of the hospital discharge summary. Mr. J told Dr. R that he had been hospitalized because he had run out of his oral antipsychotic, and that it had been restarted during the hospitalization. Dr. R—who did not know about the recent incident involving a butcher knife or the subsequent medication changes—continued Mr. J’s risperidone, but did not continue his lithium because she did not know it had been added.
Dr. R scheduled a 4-week follow-up visit for Mr. J. Then she went on maternity leave. Because the agency was short-staffed, they hired Dr. C—a locum tenens—to see all of Dr. R’s established patients in 15-minute time slots.
At their first visit, Mr. J told Dr. C that he was gaining too much weight from his antipsychotic and wanted to know if it would be OK to decrease the dose. Dr. C reviewed Dr. R’s last office note but, due to limited time, did not review any other notes. Although Dr. C had 2 no-shows that day, the clinic had a policy that required Dr. C to see walk-ins whenever there was a no-show.
Dr. C did not know of Mr. J’s threats of violence or the medication changes associated with his recent hospitalization (they were not referenced in Dr. R’s last note). Dr. C decreased the dose of Mr. J’s risperidone from 2 mg twice a day to 0.5 mg twice a day. He did not do a violence risk assessment. Two weeks after the visit with Dr. C, Mr. J, who had become increasingly depressed and psychotic, killed his mother and died by suicide.
The estates of Mr. J and his mother filed a medical malpractice lawsuit against Dr. R and Dr. C. Both psychiatrists had a duty to Mr. J. Whether there was a duty to Mr. J’s mother would depend in part on the state’s duty to protect laws. Either way, the malpractice case would hinge on whether the psychiatrists’ conduct fell below the standard of care.
Continue to: In this case...
In this case, the critical issues were Dr. R’s failure to obtain and review the recent hospital records and Dr. C’s decision to decrease the antipsychotic dose. Of particular concern is Dr. C’s decision to decrease the antipsychotic dose without reviewing more information from past records, and the resultant failure to perform a violence risk assessment. These deviations cannot be blamed entirely on the brevity of the med check appointment. They could happen in a clinic that allotted longer time periods for follow-up visits, but they are, however, more likely to occur in a short med check appointment due to time constraints.
The likelihood of these errors could have been reduced by additional support services, as well as more time for Dr. C to see each patient who was new to him. For example, if there had been a support person available to obtain hospital records prior to the postdischarge appointment, Dr. R and Dr. C would have been more likely to be aware of the violent threat associated with Mr. J’s hospitalization. Additionally, if the busy clinicians had contingency plans to assess complicated patients, such as the ability to use no-show time to deal with difficult situations, Dr. C could have taken more time to review past records.
Bottom Line
When working in a setting that involves brief med check appointments, assess the agency structure, and whether it will allow you to practice reasonably. This will be relevant clinically and may reduce the risk of malpractice lawsuits. Reasonableness of a clinician’s actions is a fact-specific question and is influenced by multiple factors, including the patient population, the availability and quality of an agency’s support services, and contingency plans.
Related Resources
- Mossman D. Successfully navigating the 15-minute ‘med check.’ Current Psychiatry. 2010;9(6):40-43.
- Olfson M, Marcus SC. National trends in outpatient psychotherapy. Am J Psychiatry. 2010;167(12):1456-1463.
Drug Brand Names
Lithium • Eskalith, Lithobid
Risperidone • Risperdal
1. Malpractice. In: Garner BA, ed. Black’s Law Dictionary. 11th ed. Thomson West; 2019:1148.
2. Frierson RL, Joshi KG. Malpractice law and psychiatry: an overview. Focus. 2019;17:332-336. doi:10.1176/appi.focus.20190017
3. Negligence Based Claims. In: Boumil MM, Hattis PA, eds. Medical Liability in a Nutshell. 4th ed. West Academic Publishing; 2017:43-88
4. Peters PG. The quiet demise of deference to custom: malpractice law at the millennium. Washington and Lee Law Review. 2000;57(1):163-205. Accessed July 8, 2022. https://scholarlycommons.law.wlu.edu/wlulr/vol57/iss1/5
5. Simon RI. Standard-of-care testimony: best practices or reasonable care? J Am Acad Psychiatry Law. 2005;33(1):8-11. Accessed July 8, 2022. http://jaapl.org/content/33/1/8
6. Behrens SA. Call in Houdini: the time has come to be released from the geographic straightjacket known as the locality rule. Drake Law Review. 2008; 56(3):753-790. Accessed June 20, 2022. https://lawreviewdrake.files.wordpress.com/2015/06/lrvol56-3_behrens.pdf
1. Malpractice. In: Garner BA, ed. Black’s Law Dictionary. 11th ed. Thomson West; 2019:1148.
2. Frierson RL, Joshi KG. Malpractice law and psychiatry: an overview. Focus. 2019;17:332-336. doi:10.1176/appi.focus.20190017
3. Negligence Based Claims. In: Boumil MM, Hattis PA, eds. Medical Liability in a Nutshell. 4th ed. West Academic Publishing; 2017:43-88
4. Peters PG. The quiet demise of deference to custom: malpractice law at the millennium. Washington and Lee Law Review. 2000;57(1):163-205. Accessed July 8, 2022. https://scholarlycommons.law.wlu.edu/wlulr/vol57/iss1/5
5. Simon RI. Standard-of-care testimony: best practices or reasonable care? J Am Acad Psychiatry Law. 2005;33(1):8-11. Accessed July 8, 2022. http://jaapl.org/content/33/1/8
6. Behrens SA. Call in Houdini: the time has come to be released from the geographic straightjacket known as the locality rule. Drake Law Review. 2008; 56(3):753-790. Accessed June 20, 2022. https://lawreviewdrake.files.wordpress.com/2015/06/lrvol56-3_behrens.pdf
Evaluating suicidality
From paranoid fear to completed homicide
A crescendo of paranoid fear sharply increases the likelihood that a person will kill his (her) misperceived persecutor. Persecutory delusions are more likely to lead to homicide than any other psychiatric symptom.1 If people define a delusional situation as real, the situation is real in its consequences.
Based on my experience performing more than 100 insanity evaluations of paranoid persons charged with murder, I have identified 4 paranoid motives for homicide.
Self-defense. The most common paranoid motive for murder is the misperceived need to defend one’s self.
A steel worker believed that there was a conspiracy to kill him. His wife insisted that he go to a hospital emergency room for an evaluation. He then concluded that his wife was in on the conspiracy and stabbed her to death.
Defense of one’s manhood. Homosexual panic occurs in men who think of themselves as heterosexual.
A man with paranoid schizophrenia developed a delusion that his former high school football coach was having the entire team rape him at night. He shot the coach 6 times in front of 22 witnesses.
Defense of one’s children. A parent may kill to save her (his) children’s souls.
A deeply religious woman developed persecutory delusions that her 9-year-old son and 3-year-old daughter were going to be kidnapped and forced to make child pornography. To save her children’s souls, she stabbed her children more than 100 times.
Defense of the world. Homicide may be seen as a way to protect all humankind.
A woman developed a delusion that her father was Satan and would kill her. She believed that if she could kill her father (Satan) and his family she would save herself and bring about world peace. After killing her father, she thrust the sharp end of a tire iron into her grandmother’s umbilicus and vagina because those body parts were involved in “birthing Satan.”
Questioning to determine risk
I have found that, when evaluating a paranoid, delusional person for potential violence, it is better to present that person with a hypothetical question about encountering his perceived persecutor than with a generic question about homicidality.2 For example, a delusional person who reports that he was afraid of being killed by the Mafia could be asked, “If you were walking down an alley and encountered a man dressed like a Mafia hit man with a bulge in his jacket, what would you do?” One interviewee might reply, “The Mafia has so much power there is nothing I could do.” Another might answer, “As soon as I got close enough I would blow his head off with my .357 Magnum.” Although both people would be reporting honestly that they have no homicidal ideas, the latter has a much lower threshold for killing in misperceived self-defense.
Summing up
Persecutory delusions are more likely than any other psychiatric symptom to lead a psychotic person to commit homicide. The killing might be motivated by misperceived self-defense, defense of one’s manhood, defense of one’s children, or defense of the world.
A crescendo of paranoid fear sharply increases the likelihood that a person will kill his (her) misperceived persecutor. Persecutory delusions are more likely to lead to homicide than any other psychiatric symptom.1 If people define a delusional situation as real, the situation is real in its consequences.
Based on my experience performing more than 100 insanity evaluations of paranoid persons charged with murder, I have identified 4 paranoid motives for homicide.
Self-defense. The most common paranoid motive for murder is the misperceived need to defend one’s self.
A steel worker believed that there was a conspiracy to kill him. His wife insisted that he go to a hospital emergency room for an evaluation. He then concluded that his wife was in on the conspiracy and stabbed her to death.
Defense of one’s manhood. Homosexual panic occurs in men who think of themselves as heterosexual.
A man with paranoid schizophrenia developed a delusion that his former high school football coach was having the entire team rape him at night. He shot the coach 6 times in front of 22 witnesses.
Defense of one’s children. A parent may kill to save her (his) children’s souls.
A deeply religious woman developed persecutory delusions that her 9-year-old son and 3-year-old daughter were going to be kidnapped and forced to make child pornography. To save her children’s souls, she stabbed her children more than 100 times.
Defense of the world. Homicide may be seen as a way to protect all humankind.
A woman developed a delusion that her father was Satan and would kill her. She believed that if she could kill her father (Satan) and his family she would save herself and bring about world peace. After killing her father, she thrust the sharp end of a tire iron into her grandmother’s umbilicus and vagina because those body parts were involved in “birthing Satan.”
Questioning to determine risk
I have found that, when evaluating a paranoid, delusional person for potential violence, it is better to present that person with a hypothetical question about encountering his perceived persecutor than with a generic question about homicidality.2 For example, a delusional person who reports that he was afraid of being killed by the Mafia could be asked, “If you were walking down an alley and encountered a man dressed like a Mafia hit man with a bulge in his jacket, what would you do?” One interviewee might reply, “The Mafia has so much power there is nothing I could do.” Another might answer, “As soon as I got close enough I would blow his head off with my .357 Magnum.” Although both people would be reporting honestly that they have no homicidal ideas, the latter has a much lower threshold for killing in misperceived self-defense.
Summing up
Persecutory delusions are more likely than any other psychiatric symptom to lead a psychotic person to commit homicide. The killing might be motivated by misperceived self-defense, defense of one’s manhood, defense of one’s children, or defense of the world.
A crescendo of paranoid fear sharply increases the likelihood that a person will kill his (her) misperceived persecutor. Persecutory delusions are more likely to lead to homicide than any other psychiatric symptom.1 If people define a delusional situation as real, the situation is real in its consequences.
Based on my experience performing more than 100 insanity evaluations of paranoid persons charged with murder, I have identified 4 paranoid motives for homicide.
Self-defense. The most common paranoid motive for murder is the misperceived need to defend one’s self.
A steel worker believed that there was a conspiracy to kill him. His wife insisted that he go to a hospital emergency room for an evaluation. He then concluded that his wife was in on the conspiracy and stabbed her to death.
Defense of one’s manhood. Homosexual panic occurs in men who think of themselves as heterosexual.
A man with paranoid schizophrenia developed a delusion that his former high school football coach was having the entire team rape him at night. He shot the coach 6 times in front of 22 witnesses.
Defense of one’s children. A parent may kill to save her (his) children’s souls.
A deeply religious woman developed persecutory delusions that her 9-year-old son and 3-year-old daughter were going to be kidnapped and forced to make child pornography. To save her children’s souls, she stabbed her children more than 100 times.
Defense of the world. Homicide may be seen as a way to protect all humankind.
A woman developed a delusion that her father was Satan and would kill her. She believed that if she could kill her father (Satan) and his family she would save herself and bring about world peace. After killing her father, she thrust the sharp end of a tire iron into her grandmother’s umbilicus and vagina because those body parts were involved in “birthing Satan.”
Questioning to determine risk
I have found that, when evaluating a paranoid, delusional person for potential violence, it is better to present that person with a hypothetical question about encountering his perceived persecutor than with a generic question about homicidality.2 For example, a delusional person who reports that he was afraid of being killed by the Mafia could be asked, “If you were walking down an alley and encountered a man dressed like a Mafia hit man with a bulge in his jacket, what would you do?” One interviewee might reply, “The Mafia has so much power there is nothing I could do.” Another might answer, “As soon as I got close enough I would blow his head off with my .357 Magnum.” Although both people would be reporting honestly that they have no homicidal ideas, the latter has a much lower threshold for killing in misperceived self-defense.
Summing up
Persecutory delusions are more likely than any other psychiatric symptom to lead a psychotic person to commit homicide. The killing might be motivated by misperceived self-defense, defense of one’s manhood, defense of one’s children, or defense of the world.
Postpartum psychosis: Strategies to protect infant and mother from harm
In June 2001, Andrea Yates drowned her 5 children ages 6 months to 7 years in the bathtub of their home. She had delusions that her house was bugged and television cameras were monitoring her mothering skills. She came to believe that “the one and only Satan” was within her, and that her children would burn in hell if she did not save their souls while they were still innocent.
Her conviction of capital murder in her first trial was overturned on appeal. She was found not guilty by reason of insanity at her retrial in 2006 and committed to a Texas state mental hospital.1
Postpartum psychosis (PPP) presents dramatically days to weeks after delivery, with wide-ranging symptoms that can include dysphoric mania and delirium. Because untreated PPP has an estimated 4% risk of infanticide (murder of the infant in the first year of life),2 and a 5% risk of suicide,3 psychiatric hospitalization usually is required to protect the mother and her baby.
The diagnosis may be missed, however, because postpartum psychotic symptoms wax and wane and suspiciousness or poor insight cause some women—such as Andrea Yates—to hide their delusional thinking from their families. This article discusses the risk factors, prevention, and treatment of PPP, including a review of:
- infanticide and suicide risks in the postpartum period
- increased susceptibility to PPP in women with bipolar disorder and other psychiatric disorders
- hospitalization for support and safety of the mother and her infant.
Risks of infanticide and suicide
A number of motives exist for infanticide (Table 1).4 Psychiatric literature shows that mothers who kill their children often have experienced psychosis, suicidality, depression, and considerable life stress.5 Common factors include alcohol use, limited social support, and a personal history of abuse. Studies on infanticide found a significant increase in common psychiatric disorders and financial stress among the mothers. Neonaticide (murder of the infant in the first day of life) generally is not related to PPP because PPP usually does not begin until after the day of delivery.6
Among women who develop psychiatric illness, homicidal ideation is more frequent in those with a perinatal onset of psychopathology.7 Infanticidal ideas and behavior are associated with psychotic ideas about the infant.8 Suicide is the cause of up to 20% of postpartum deaths.9
Table 1
Motives for infanticide: Mental illness or something else?
| Motives | Examples |
|---|---|
| Likely related to postpartum psychosis or depression | |
| Altruistic | A depressed or psychotic mother may believe she is sending her baby to heaven to prevent suffering on earth |
| A suicidal mother may kill her infant along with herself rather than leave the child alone | |
| Acutely psychotic | A mother kills her baby for no comprehensible reason, such as in response to command hallucinations or the confusion of delirium |
| Rarely related to postpartum psychosis | |
| Fatal maltreatment | ‘Battered child’ syndrome is the most common cause of infanticide; death often occurs after chronic abuse or neglect |
| A minority of perpetrators are psychotic; a mother out of touch with reality may have difficulty providing for her infant’s needs | |
| Not likely related to postpartum psychosis | |
| Unwanted child | Parent does not want child because of inconvenience or out-of-wedlock birth |
| Spouse revenge | Murder of a child to cause emotional suffering for the other parent is the least frequent motive for infanticide |
| Source: Reference 4 | |
The bipolar connection
Many factors can elevate the risk of PPP, including sleep deprivation in susceptible women, the hormonal shifts after birth, and psychiatric comorbidity (Table 2). Nearly three-fourths (>72%) of mothers with PPP have bipolar disorder or schizoaffective disorder, whereas 12% have schizophrenia.10 Some authors consider PPP to be bipolar disorder until proven otherwise. Mothers with a history of bipolar disorder or PPP have a 100-fold increase in rates of psychiatric hospitalization in the postpartum period.11
Presentation. PPP is relatively rare, occurring at a rate of 1 to 3 cases per 1,000 births. Symptoms often have an abrupt onset, within days to weeks of delivery.10 In at least one-half of cases, symptoms begin by the third postpartum day,13 when many mothers have been discharged home and may be solely responsible for their infants.
Symptoms include confusion, bizarre behaviors, hallucinations (including rarer types such as tactile and olfactory), mood lability (ranging from euphoria to depression), decreased need for sleep or insomnia, restlessness, agitation, disorganized thinking, and bizarre delusions of relatively rapid onset.13 One mother might believe God wants her baby to be sacrificed as the second coming of the Messiah, a second may believe she has special powers, and a third that her baby is defective.
Table 2
Postpartum psychosis: Risk factors supported by evidence
| Sleep deprivation in susceptible women |
| Hormonal shifts after birth (primarily the rapid drop in estrogen) |
| Psychosocial stressors such as marital problems, older age, single motherhood, lower socioeconomic status |
| Bipolar disorder or schizoaffective disorder |
| Past history of postpartum psychosis |
| Family history of postpartum psychosis |
| Previous psychiatric hospitalization, especially during the prenatal period for a bipolar or psychotic condition |
| Menstruation or cessation of lactation |
Obstetric factors that can cause a small increase in relative risk:
|
| Source: For bibliographic citations |
Differential diagnosis
When evaluating a postpartum woman with psychotic symptoms, stay in contact with her obstetrician and the child’s pediatrician. Rule out delirium and organic causes of the mother’s symptoms (Box).11
Postpartum depression (PPD) occurs in approximately 10% to 15% of new mothers.14 Depressive symptoms occur within weeks to months after delivery and often coexist with anxious symptoms. Some women with severe depression may present with psychotic symptoms. A mother may experience insomnia, sometimes not being able to sleep when the baby is sleeping. She may lack interest in caring for her baby and experience difficulty bonding.
At times it can be difficult to distinguish PPD from PPP. When evaluating a mother who is referred for “postpartum depression,” consider PPP in the differential diagnosis. A woman with PPD or PPP may report depressed mood, but in PPP this symptom usually is related to rapid mood changes. Other clinical features that point toward PPP are abnormal hallucinations (such as olfactory or tactile), hypomanic or mixed mood symptoms, and confusion.
When evaluating a postpartum woman with psychotic symptoms, stay in contact with her obstetrician and the child’s pediatrician. Rule out delirium and organic causes of the mother’s symptoms, giving special consideration to metabolic, neurologic, cardiovascular, infectious, and substance- or medication-induced origins. The extensive differential diagnosis includes:
- thyroiditis
- tumor
- CNS infection
- head injury
- embolism
- eclampsia
- substance withdrawal
- medication-induced (such as corticosteroids)
- electrolyte anomalies
- anoxia
- vitamin B12 deficiency.11
Psychosis vs OCD. Psychotic thinking and behaviors also must be differentiated from obsessive thoughts and compulsions.10,16 Obsessive compulsive disorder (OCD) may be exacerbated or emerge for the first time during the perinatal period.17
In postpartum OCD, women may experience intrusive thoughts of accidental or purposeful harm to their baby. As opposed to women with PPP, mothers with OCD are not out of touch with reality and their thoughts are ego-dystonic.17 When these mothers have thoughts of their infants being harmed, they realize that these thoughts are not plans but fears and they try to avoid the thoughts.
Preventing PPP
Bipolar disorder is one of the most difficult disorders to treat during pregnancy because the serious risks of untreated illness must be balanced against the potential teratogenic risk of medications. Nevertheless, proactively managing bipolar disorder during pregnancy may reduce the risk of PPP.10
Closely monitor women with a history of bipolar disorder or PPP. During pregnancy, counsel them—and their partners—to:
- anticipate that depressive or psychotic symptoms could develop within days after delivery18
- seek treatment immediately if this occurs.
Postpartum medication. Whether or not a woman with bipolar disorder takes medication during pregnancy, consider treatment with mood stabilizers or atypical antipsychotics in the postpartum to prevent PPP (Table 3). Evidence is limited, but a search of PubMed found 1 study in which prophylactic lithium was given late in the third trimester or immediately after delivery to 21 women with a history of bipolar disorder or PPP. Only 2 patients had a psychotic recurrence while on prophylactic lithium; 1 unexplained stillbirth occurred.19
A retrospective study examined the course of women with bipolar disorder, some of whom were given prophylactic mood stabilizers immediately in the postpartum. One of 14 who received antimanic agents relapsed within the first 3 months postpartum, compared with 8 of 13 who were not so treated.18
Compared with antiepileptics, less information is available about the use of atypical antipsychotics in pregnancy and lactation. Antipsychotics’ potential advantage in women at risk for PPP is that these agents may help prevent or treat both manic and psychotic symptoms.
In a small, naturalistic, prospective study, 11 women at risk for PPP received olanzapine alone or with an antidepressant or mood stabilizer for at least 4 weeks after delivery. Two (18%) experienced a postpartum mood episode, compared with 8 (57%) of 14 other at-risk women who received antidepressants, mood stabilizers, or no medication.20
When you discuss breast-feeding, consider possible risks to the neonate as well as potential sleep interruption for the mother. If a mother has a supportive partner, the partner might be put in charge of night-time feedings in a routine combining breast-feeding and bottle-feeding. In some cases you may need to recommend cessation of lactation.21
Table 3
Treating postpartum psychosis: Consider 3 components
| Component | Recommendations |
|---|---|
| Hospitalization vs home care | Hospitalize in most cases because of emergent severe symptoms and fluctuating course; base decision on risk evaluation/safety issues for patient and infant After discharge, visiting nurses are useful to help monitor the mother’s condition at home |
| Psychoeducation | Educate patient, family, and social support network; address risks to mother and infant and risks in future pregnancies |
| Medication | When prescribing mood stabilizers and/or antipsychotics, consider:
|
Managing PPP
Early symptoms. Because of its severity and rapid evolution, PPP often presents as a psychiatric emergency. Monitor atrisk patients’ sleep patterns and mood for early signs of psychosis.22 Watch especially for hypomanic symptoms such as elevated or mixed mood and decreased judgment, which are common early in PPP.13
A mother with few signs of abnormal mood, good social support, and close follow-up may potentially be safely managed as an outpatient. Initial evaluation and management of PPP usually requires hospitalization, however, because of the risks of suicide, infanticide, and child maltreatment.23
Hospitalization. Mother-infant bonding is important, but safety is paramount if a mother is psychotic—especially if she is experiencing psychotic thoughts about her infant. If possible, the infant should remain with family members during the mother’s hospitalization. Supervised mother-infant visits are often arranged, as appropriate.
Mood-stabilizing medications, including antipsychotics, are mainstays of treatment.24 In some cases, conventional antipsychotics such as haloperidol may be useful because of a lower risk of weight gain or of sedation that could impair a mother’s ability to respond to her infant. Electroconvulsive therapy often yields rapid symptomatic improvement for mothers with postpartum mood or psychotic symptoms.25
Discharge planning. Assuming that the mother adheres to prescribed treatment, discharge may occur within 1 week. Plan discharge arrangements carefully (Table 4).28 A team approach can be very useful within the outpatient clinic. In the model of the Perinatal Psychiatry Clinic of Connections in suburban Cleveland, OH, the mother’s treatment team includes perinatal psychiatrists, nurses, counsellors, case managers (who do home visits), and peer counselors.
Outpatient civil commitment, in which patients are mandated to accept treatment, is an option in some jurisdictions and could help ensure that patients receive treatment consistently.
Table 4
Discharge planning for safety of mother and infant
| Notify child protective services (CPS) depending on the risk to the child. Case-by-case review is needed to assess whether the infant should be removed. CPS may put in place a plan for safety, short of removal. The plan may require that the woman continue psychiatric care |
| Meet with the patient and family to discuss her diagnosis, the risks, the importance of continued medication adherence, and the need for family or social supports to assist with child care |
| Consider engaging visiting nurses or doulas to provide help and support at home |
| Schedule frequent outpatient appointments for the mother after discharge |
| Consider family therapy after the mother has improved because of her risk for affective episodes outside the postpartum28 |
Related resources
- Altshuler L, Richards M, Yonkers K. Treating bipolar disorder during pregnancy. Current Psychiatry. 2003;2(7):14-26. www.CurrentPsychiatry.com.
- Gentile S. Infant safety with antipsychotic therapy in breastfeeding: a systematic review. J Clin Psychiatry. 2008;69(4):666-673.
- Miller LJ. Postpartum mood disorders. Washington, DC: American Psychiatric Publishing, Inc; 1999.
- Stowe ZN. The use of mood stabilizers during breastfeeding. J Clin Psychiatry. 2007;68(suppl 9):22-28.
- Toxicology Data Network (Toxnet). Literature on reproductive risks associated with psychotropics. National Library of Medicine. http://toxnet.nlm.nih.gov.
- Haloperidol • Haldol
- Lithium • various
- Olanzapine • Zyprexa
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
Dr. Resnick, a forensic psychiatrist and coauthor of this article, testified for the defense in both trials of Andrea Yates.
1. Resnick PJ. The Andrea Yates case: insanity on trial. Cleveland State Law Review. 2007;55(2):147-156.
2. Altshuler LL, Hendrick V, Cohen LS. Course of mood and anxiety disorders during pregnancy and the postpartum period. J Clin Psychiatry. 1998;59(suppl. 2):29-33.
3. Knops GG. Postpartum mood disorders. Postgrad Med. 1993;93:103-116.
4. Resnick PJ. Child murder by parents: a psychiatric review of filicide. Am J Psychiatry. 1969;126:73-82.
5. Friedman SH, Horwitz SM, Resnick PJ. Child murder by mothers: a critical analysis of the current state of knowledge and a research agenda. Am J Psychiatry. 2005;162:1578-1587.
6. Friedman SH, Resnick PJ. Neonaticide: phenomenology and considerations for prevention. Int J Law Psychiatry. In press.
7. Wisner K, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30:77-87.
8. Chandra PS, Venkatasubramanian G, Thomas T. Infanticidal ideas and infanticidal behaviour in Indian women with severe postpartum psychiatric disorders. J Nerv Ment Dis. 2002;190(7):457-461.
9. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
10. Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Women’s Health. 2006;15(4):352-368.
11. Attia E, Downey J, Oberman M. Postpartum psychoses. In: Miller LJ, ed. Postpartum mood disorders. Washington, DC: American Psychiatric Publishing Inc.; 1999:99-117.
12. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
13. Heron J, McGuinness M, Blackmore ER, et al. Early postpartum symptoms in puerperal psychosis. BJOG. 2008;115(3):348-353.
14. Meltzer-Brody S, Payne J, Rubinow D. Postpartum depression: what to tell patients who breast-feed. Current Psychiatry. 2008;7(5):87-95.
15. Jennings KD, Ross S, Popper S, et al. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54:21-28.
16. Wisner KL, Gracious BL, Piontek CM, et al. Postpartum disorders: phenomenology, treatment approaches, and relationship to infanticide. In: Spinelli MG, ed. Infanticide: psychosocial and legal perspectives on mothers who kill. Washington, DC: American Psychiatric Publishing, Inc.; 2003.
17. Fairbrother N, Abramowitz JS. New parenthood as a risk factors for the development of obsessional problems. Behav Res Ther. 2007;45(9):2155-2163.
18. Cohen LS, Sichel DA, Robertson LM, et al. Postpartum prophylaxis for women with bipolar disorder. Am J Psychiatry. 1995;152(11):1641-1645.
19. Stewart DE, Klompenhouwer JL, Kendell RE, et al. Prophylactic lithium in puerperal psychosis. Br J Psychiatry. 1991;158:393-397.
20. Sharma V, Smith A, Mazmanian D. Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord. 2006;8(4):400-404.
21. Pfuhlmann B, Stoeber G, Beckmann H. Postpartum psychoses: prognosis, risk factors, and treatment. Curr Psychiatry Rep. 2002;4(3):185-190.
22. Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5(2):98-105.
23. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
24. Connell M. The postpartum psychosis defense and feminism: more or less justice for women? Case Western Reserve Law Review. 2002;53:143.-
25. Forray A, Ostroff RB. The use of electroconvulsive therapy in postpartum affective disorders. J ECT. 2007;23(3):188-193.
26. Engqvist I, Nilsson A, Nilsson K, et al. Strategies in caring for women with postpartum psychosis—an interview study with psychiatric nurses. J Clin Nurs. 2007;16(7):1333-1342.
27. Robertson E, Lyons A. Living with puerperal psychosis: a qualitative analysis. Psychol Psychother. 2003;76(4):411-431.
28. Robertson E, Jones I, Haque S, et al. Risk of puerperal and non-puerperal recurrence of illness following bipolar affective puerperal (post-partum) psychosis. Br J Psychiatry. 2005;186:258-259.
In June 2001, Andrea Yates drowned her 5 children ages 6 months to 7 years in the bathtub of their home. She had delusions that her house was bugged and television cameras were monitoring her mothering skills. She came to believe that “the one and only Satan” was within her, and that her children would burn in hell if she did not save their souls while they were still innocent.
Her conviction of capital murder in her first trial was overturned on appeal. She was found not guilty by reason of insanity at her retrial in 2006 and committed to a Texas state mental hospital.1
Postpartum psychosis (PPP) presents dramatically days to weeks after delivery, with wide-ranging symptoms that can include dysphoric mania and delirium. Because untreated PPP has an estimated 4% risk of infanticide (murder of the infant in the first year of life),2 and a 5% risk of suicide,3 psychiatric hospitalization usually is required to protect the mother and her baby.
The diagnosis may be missed, however, because postpartum psychotic symptoms wax and wane and suspiciousness or poor insight cause some women—such as Andrea Yates—to hide their delusional thinking from their families. This article discusses the risk factors, prevention, and treatment of PPP, including a review of:
- infanticide and suicide risks in the postpartum period
- increased susceptibility to PPP in women with bipolar disorder and other psychiatric disorders
- hospitalization for support and safety of the mother and her infant.
Risks of infanticide and suicide
A number of motives exist for infanticide (Table 1).4 Psychiatric literature shows that mothers who kill their children often have experienced psychosis, suicidality, depression, and considerable life stress.5 Common factors include alcohol use, limited social support, and a personal history of abuse. Studies on infanticide found a significant increase in common psychiatric disorders and financial stress among the mothers. Neonaticide (murder of the infant in the first day of life) generally is not related to PPP because PPP usually does not begin until after the day of delivery.6
Among women who develop psychiatric illness, homicidal ideation is more frequent in those with a perinatal onset of psychopathology.7 Infanticidal ideas and behavior are associated with psychotic ideas about the infant.8 Suicide is the cause of up to 20% of postpartum deaths.9
Table 1
Motives for infanticide: Mental illness or something else?
| Motives | Examples |
|---|---|
| Likely related to postpartum psychosis or depression | |
| Altruistic | A depressed or psychotic mother may believe she is sending her baby to heaven to prevent suffering on earth |
| A suicidal mother may kill her infant along with herself rather than leave the child alone | |
| Acutely psychotic | A mother kills her baby for no comprehensible reason, such as in response to command hallucinations or the confusion of delirium |
| Rarely related to postpartum psychosis | |
| Fatal maltreatment | ‘Battered child’ syndrome is the most common cause of infanticide; death often occurs after chronic abuse or neglect |
| A minority of perpetrators are psychotic; a mother out of touch with reality may have difficulty providing for her infant’s needs | |
| Not likely related to postpartum psychosis | |
| Unwanted child | Parent does not want child because of inconvenience or out-of-wedlock birth |
| Spouse revenge | Murder of a child to cause emotional suffering for the other parent is the least frequent motive for infanticide |
| Source: Reference 4 | |
The bipolar connection
Many factors can elevate the risk of PPP, including sleep deprivation in susceptible women, the hormonal shifts after birth, and psychiatric comorbidity (Table 2). Nearly three-fourths (>72%) of mothers with PPP have bipolar disorder or schizoaffective disorder, whereas 12% have schizophrenia.10 Some authors consider PPP to be bipolar disorder until proven otherwise. Mothers with a history of bipolar disorder or PPP have a 100-fold increase in rates of psychiatric hospitalization in the postpartum period.11
Presentation. PPP is relatively rare, occurring at a rate of 1 to 3 cases per 1,000 births. Symptoms often have an abrupt onset, within days to weeks of delivery.10 In at least one-half of cases, symptoms begin by the third postpartum day,13 when many mothers have been discharged home and may be solely responsible for their infants.
Symptoms include confusion, bizarre behaviors, hallucinations (including rarer types such as tactile and olfactory), mood lability (ranging from euphoria to depression), decreased need for sleep or insomnia, restlessness, agitation, disorganized thinking, and bizarre delusions of relatively rapid onset.13 One mother might believe God wants her baby to be sacrificed as the second coming of the Messiah, a second may believe she has special powers, and a third that her baby is defective.
Table 2
Postpartum psychosis: Risk factors supported by evidence
| Sleep deprivation in susceptible women |
| Hormonal shifts after birth (primarily the rapid drop in estrogen) |
| Psychosocial stressors such as marital problems, older age, single motherhood, lower socioeconomic status |
| Bipolar disorder or schizoaffective disorder |
| Past history of postpartum psychosis |
| Family history of postpartum psychosis |
| Previous psychiatric hospitalization, especially during the prenatal period for a bipolar or psychotic condition |
| Menstruation or cessation of lactation |
Obstetric factors that can cause a small increase in relative risk:
|
| Source: For bibliographic citations |
Differential diagnosis
When evaluating a postpartum woman with psychotic symptoms, stay in contact with her obstetrician and the child’s pediatrician. Rule out delirium and organic causes of the mother’s symptoms (Box).11
Postpartum depression (PPD) occurs in approximately 10% to 15% of new mothers.14 Depressive symptoms occur within weeks to months after delivery and often coexist with anxious symptoms. Some women with severe depression may present with psychotic symptoms. A mother may experience insomnia, sometimes not being able to sleep when the baby is sleeping. She may lack interest in caring for her baby and experience difficulty bonding.
At times it can be difficult to distinguish PPD from PPP. When evaluating a mother who is referred for “postpartum depression,” consider PPP in the differential diagnosis. A woman with PPD or PPP may report depressed mood, but in PPP this symptom usually is related to rapid mood changes. Other clinical features that point toward PPP are abnormal hallucinations (such as olfactory or tactile), hypomanic or mixed mood symptoms, and confusion.
When evaluating a postpartum woman with psychotic symptoms, stay in contact with her obstetrician and the child’s pediatrician. Rule out delirium and organic causes of the mother’s symptoms, giving special consideration to metabolic, neurologic, cardiovascular, infectious, and substance- or medication-induced origins. The extensive differential diagnosis includes:
- thyroiditis
- tumor
- CNS infection
- head injury
- embolism
- eclampsia
- substance withdrawal
- medication-induced (such as corticosteroids)
- electrolyte anomalies
- anoxia
- vitamin B12 deficiency.11
Psychosis vs OCD. Psychotic thinking and behaviors also must be differentiated from obsessive thoughts and compulsions.10,16 Obsessive compulsive disorder (OCD) may be exacerbated or emerge for the first time during the perinatal period.17
In postpartum OCD, women may experience intrusive thoughts of accidental or purposeful harm to their baby. As opposed to women with PPP, mothers with OCD are not out of touch with reality and their thoughts are ego-dystonic.17 When these mothers have thoughts of their infants being harmed, they realize that these thoughts are not plans but fears and they try to avoid the thoughts.
Preventing PPP
Bipolar disorder is one of the most difficult disorders to treat during pregnancy because the serious risks of untreated illness must be balanced against the potential teratogenic risk of medications. Nevertheless, proactively managing bipolar disorder during pregnancy may reduce the risk of PPP.10
Closely monitor women with a history of bipolar disorder or PPP. During pregnancy, counsel them—and their partners—to:
- anticipate that depressive or psychotic symptoms could develop within days after delivery18
- seek treatment immediately if this occurs.
Postpartum medication. Whether or not a woman with bipolar disorder takes medication during pregnancy, consider treatment with mood stabilizers or atypical antipsychotics in the postpartum to prevent PPP (Table 3). Evidence is limited, but a search of PubMed found 1 study in which prophylactic lithium was given late in the third trimester or immediately after delivery to 21 women with a history of bipolar disorder or PPP. Only 2 patients had a psychotic recurrence while on prophylactic lithium; 1 unexplained stillbirth occurred.19
A retrospective study examined the course of women with bipolar disorder, some of whom were given prophylactic mood stabilizers immediately in the postpartum. One of 14 who received antimanic agents relapsed within the first 3 months postpartum, compared with 8 of 13 who were not so treated.18
Compared with antiepileptics, less information is available about the use of atypical antipsychotics in pregnancy and lactation. Antipsychotics’ potential advantage in women at risk for PPP is that these agents may help prevent or treat both manic and psychotic symptoms.
In a small, naturalistic, prospective study, 11 women at risk for PPP received olanzapine alone or with an antidepressant or mood stabilizer for at least 4 weeks after delivery. Two (18%) experienced a postpartum mood episode, compared with 8 (57%) of 14 other at-risk women who received antidepressants, mood stabilizers, or no medication.20
When you discuss breast-feeding, consider possible risks to the neonate as well as potential sleep interruption for the mother. If a mother has a supportive partner, the partner might be put in charge of night-time feedings in a routine combining breast-feeding and bottle-feeding. In some cases you may need to recommend cessation of lactation.21
Table 3
Treating postpartum psychosis: Consider 3 components
| Component | Recommendations |
|---|---|
| Hospitalization vs home care | Hospitalize in most cases because of emergent severe symptoms and fluctuating course; base decision on risk evaluation/safety issues for patient and infant After discharge, visiting nurses are useful to help monitor the mother’s condition at home |
| Psychoeducation | Educate patient, family, and social support network; address risks to mother and infant and risks in future pregnancies |
| Medication | When prescribing mood stabilizers and/or antipsychotics, consider:
|
Managing PPP
Early symptoms. Because of its severity and rapid evolution, PPP often presents as a psychiatric emergency. Monitor atrisk patients’ sleep patterns and mood for early signs of psychosis.22 Watch especially for hypomanic symptoms such as elevated or mixed mood and decreased judgment, which are common early in PPP.13
A mother with few signs of abnormal mood, good social support, and close follow-up may potentially be safely managed as an outpatient. Initial evaluation and management of PPP usually requires hospitalization, however, because of the risks of suicide, infanticide, and child maltreatment.23
Hospitalization. Mother-infant bonding is important, but safety is paramount if a mother is psychotic—especially if she is experiencing psychotic thoughts about her infant. If possible, the infant should remain with family members during the mother’s hospitalization. Supervised mother-infant visits are often arranged, as appropriate.
Mood-stabilizing medications, including antipsychotics, are mainstays of treatment.24 In some cases, conventional antipsychotics such as haloperidol may be useful because of a lower risk of weight gain or of sedation that could impair a mother’s ability to respond to her infant. Electroconvulsive therapy often yields rapid symptomatic improvement for mothers with postpartum mood or psychotic symptoms.25
Discharge planning. Assuming that the mother adheres to prescribed treatment, discharge may occur within 1 week. Plan discharge arrangements carefully (Table 4).28 A team approach can be very useful within the outpatient clinic. In the model of the Perinatal Psychiatry Clinic of Connections in suburban Cleveland, OH, the mother’s treatment team includes perinatal psychiatrists, nurses, counsellors, case managers (who do home visits), and peer counselors.
Outpatient civil commitment, in which patients are mandated to accept treatment, is an option in some jurisdictions and could help ensure that patients receive treatment consistently.
Table 4
Discharge planning for safety of mother and infant
| Notify child protective services (CPS) depending on the risk to the child. Case-by-case review is needed to assess whether the infant should be removed. CPS may put in place a plan for safety, short of removal. The plan may require that the woman continue psychiatric care |
| Meet with the patient and family to discuss her diagnosis, the risks, the importance of continued medication adherence, and the need for family or social supports to assist with child care |
| Consider engaging visiting nurses or doulas to provide help and support at home |
| Schedule frequent outpatient appointments for the mother after discharge |
| Consider family therapy after the mother has improved because of her risk for affective episodes outside the postpartum28 |
Related resources
- Altshuler L, Richards M, Yonkers K. Treating bipolar disorder during pregnancy. Current Psychiatry. 2003;2(7):14-26. www.CurrentPsychiatry.com.
- Gentile S. Infant safety with antipsychotic therapy in breastfeeding: a systematic review. J Clin Psychiatry. 2008;69(4):666-673.
- Miller LJ. Postpartum mood disorders. Washington, DC: American Psychiatric Publishing, Inc; 1999.
- Stowe ZN. The use of mood stabilizers during breastfeeding. J Clin Psychiatry. 2007;68(suppl 9):22-28.
- Toxicology Data Network (Toxnet). Literature on reproductive risks associated with psychotropics. National Library of Medicine. http://toxnet.nlm.nih.gov.
- Haloperidol • Haldol
- Lithium • various
- Olanzapine • Zyprexa
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
Dr. Resnick, a forensic psychiatrist and coauthor of this article, testified for the defense in both trials of Andrea Yates.
In June 2001, Andrea Yates drowned her 5 children ages 6 months to 7 years in the bathtub of their home. She had delusions that her house was bugged and television cameras were monitoring her mothering skills. She came to believe that “the one and only Satan” was within her, and that her children would burn in hell if she did not save their souls while they were still innocent.
Her conviction of capital murder in her first trial was overturned on appeal. She was found not guilty by reason of insanity at her retrial in 2006 and committed to a Texas state mental hospital.1
Postpartum psychosis (PPP) presents dramatically days to weeks after delivery, with wide-ranging symptoms that can include dysphoric mania and delirium. Because untreated PPP has an estimated 4% risk of infanticide (murder of the infant in the first year of life),2 and a 5% risk of suicide,3 psychiatric hospitalization usually is required to protect the mother and her baby.
The diagnosis may be missed, however, because postpartum psychotic symptoms wax and wane and suspiciousness or poor insight cause some women—such as Andrea Yates—to hide their delusional thinking from their families. This article discusses the risk factors, prevention, and treatment of PPP, including a review of:
- infanticide and suicide risks in the postpartum period
- increased susceptibility to PPP in women with bipolar disorder and other psychiatric disorders
- hospitalization for support and safety of the mother and her infant.
Risks of infanticide and suicide
A number of motives exist for infanticide (Table 1).4 Psychiatric literature shows that mothers who kill their children often have experienced psychosis, suicidality, depression, and considerable life stress.5 Common factors include alcohol use, limited social support, and a personal history of abuse. Studies on infanticide found a significant increase in common psychiatric disorders and financial stress among the mothers. Neonaticide (murder of the infant in the first day of life) generally is not related to PPP because PPP usually does not begin until after the day of delivery.6
Among women who develop psychiatric illness, homicidal ideation is more frequent in those with a perinatal onset of psychopathology.7 Infanticidal ideas and behavior are associated with psychotic ideas about the infant.8 Suicide is the cause of up to 20% of postpartum deaths.9
Table 1
Motives for infanticide: Mental illness or something else?
| Motives | Examples |
|---|---|
| Likely related to postpartum psychosis or depression | |
| Altruistic | A depressed or psychotic mother may believe she is sending her baby to heaven to prevent suffering on earth |
| A suicidal mother may kill her infant along with herself rather than leave the child alone | |
| Acutely psychotic | A mother kills her baby for no comprehensible reason, such as in response to command hallucinations or the confusion of delirium |
| Rarely related to postpartum psychosis | |
| Fatal maltreatment | ‘Battered child’ syndrome is the most common cause of infanticide; death often occurs after chronic abuse or neglect |
| A minority of perpetrators are psychotic; a mother out of touch with reality may have difficulty providing for her infant’s needs | |
| Not likely related to postpartum psychosis | |
| Unwanted child | Parent does not want child because of inconvenience or out-of-wedlock birth |
| Spouse revenge | Murder of a child to cause emotional suffering for the other parent is the least frequent motive for infanticide |
| Source: Reference 4 | |
The bipolar connection
Many factors can elevate the risk of PPP, including sleep deprivation in susceptible women, the hormonal shifts after birth, and psychiatric comorbidity (Table 2). Nearly three-fourths (>72%) of mothers with PPP have bipolar disorder or schizoaffective disorder, whereas 12% have schizophrenia.10 Some authors consider PPP to be bipolar disorder until proven otherwise. Mothers with a history of bipolar disorder or PPP have a 100-fold increase in rates of psychiatric hospitalization in the postpartum period.11
Presentation. PPP is relatively rare, occurring at a rate of 1 to 3 cases per 1,000 births. Symptoms often have an abrupt onset, within days to weeks of delivery.10 In at least one-half of cases, symptoms begin by the third postpartum day,13 when many mothers have been discharged home and may be solely responsible for their infants.
Symptoms include confusion, bizarre behaviors, hallucinations (including rarer types such as tactile and olfactory), mood lability (ranging from euphoria to depression), decreased need for sleep or insomnia, restlessness, agitation, disorganized thinking, and bizarre delusions of relatively rapid onset.13 One mother might believe God wants her baby to be sacrificed as the second coming of the Messiah, a second may believe she has special powers, and a third that her baby is defective.
Table 2
Postpartum psychosis: Risk factors supported by evidence
| Sleep deprivation in susceptible women |
| Hormonal shifts after birth (primarily the rapid drop in estrogen) |
| Psychosocial stressors such as marital problems, older age, single motherhood, lower socioeconomic status |
| Bipolar disorder or schizoaffective disorder |
| Past history of postpartum psychosis |
| Family history of postpartum psychosis |
| Previous psychiatric hospitalization, especially during the prenatal period for a bipolar or psychotic condition |
| Menstruation or cessation of lactation |
Obstetric factors that can cause a small increase in relative risk:
|
| Source: For bibliographic citations |
Differential diagnosis
When evaluating a postpartum woman with psychotic symptoms, stay in contact with her obstetrician and the child’s pediatrician. Rule out delirium and organic causes of the mother’s symptoms (Box).11
Postpartum depression (PPD) occurs in approximately 10% to 15% of new mothers.14 Depressive symptoms occur within weeks to months after delivery and often coexist with anxious symptoms. Some women with severe depression may present with psychotic symptoms. A mother may experience insomnia, sometimes not being able to sleep when the baby is sleeping. She may lack interest in caring for her baby and experience difficulty bonding.
At times it can be difficult to distinguish PPD from PPP. When evaluating a mother who is referred for “postpartum depression,” consider PPP in the differential diagnosis. A woman with PPD or PPP may report depressed mood, but in PPP this symptom usually is related to rapid mood changes. Other clinical features that point toward PPP are abnormal hallucinations (such as olfactory or tactile), hypomanic or mixed mood symptoms, and confusion.
When evaluating a postpartum woman with psychotic symptoms, stay in contact with her obstetrician and the child’s pediatrician. Rule out delirium and organic causes of the mother’s symptoms, giving special consideration to metabolic, neurologic, cardiovascular, infectious, and substance- or medication-induced origins. The extensive differential diagnosis includes:
- thyroiditis
- tumor
- CNS infection
- head injury
- embolism
- eclampsia
- substance withdrawal
- medication-induced (such as corticosteroids)
- electrolyte anomalies
- anoxia
- vitamin B12 deficiency.11
Psychosis vs OCD. Psychotic thinking and behaviors also must be differentiated from obsessive thoughts and compulsions.10,16 Obsessive compulsive disorder (OCD) may be exacerbated or emerge for the first time during the perinatal period.17
In postpartum OCD, women may experience intrusive thoughts of accidental or purposeful harm to their baby. As opposed to women with PPP, mothers with OCD are not out of touch with reality and their thoughts are ego-dystonic.17 When these mothers have thoughts of their infants being harmed, they realize that these thoughts are not plans but fears and they try to avoid the thoughts.
Preventing PPP
Bipolar disorder is one of the most difficult disorders to treat during pregnancy because the serious risks of untreated illness must be balanced against the potential teratogenic risk of medications. Nevertheless, proactively managing bipolar disorder during pregnancy may reduce the risk of PPP.10
Closely monitor women with a history of bipolar disorder or PPP. During pregnancy, counsel them—and their partners—to:
- anticipate that depressive or psychotic symptoms could develop within days after delivery18
- seek treatment immediately if this occurs.
Postpartum medication. Whether or not a woman with bipolar disorder takes medication during pregnancy, consider treatment with mood stabilizers or atypical antipsychotics in the postpartum to prevent PPP (Table 3). Evidence is limited, but a search of PubMed found 1 study in which prophylactic lithium was given late in the third trimester or immediately after delivery to 21 women with a history of bipolar disorder or PPP. Only 2 patients had a psychotic recurrence while on prophylactic lithium; 1 unexplained stillbirth occurred.19
A retrospective study examined the course of women with bipolar disorder, some of whom were given prophylactic mood stabilizers immediately in the postpartum. One of 14 who received antimanic agents relapsed within the first 3 months postpartum, compared with 8 of 13 who were not so treated.18
Compared with antiepileptics, less information is available about the use of atypical antipsychotics in pregnancy and lactation. Antipsychotics’ potential advantage in women at risk for PPP is that these agents may help prevent or treat both manic and psychotic symptoms.
In a small, naturalistic, prospective study, 11 women at risk for PPP received olanzapine alone or with an antidepressant or mood stabilizer for at least 4 weeks after delivery. Two (18%) experienced a postpartum mood episode, compared with 8 (57%) of 14 other at-risk women who received antidepressants, mood stabilizers, or no medication.20
When you discuss breast-feeding, consider possible risks to the neonate as well as potential sleep interruption for the mother. If a mother has a supportive partner, the partner might be put in charge of night-time feedings in a routine combining breast-feeding and bottle-feeding. In some cases you may need to recommend cessation of lactation.21
Table 3
Treating postpartum psychosis: Consider 3 components
| Component | Recommendations |
|---|---|
| Hospitalization vs home care | Hospitalize in most cases because of emergent severe symptoms and fluctuating course; base decision on risk evaluation/safety issues for patient and infant After discharge, visiting nurses are useful to help monitor the mother’s condition at home |
| Psychoeducation | Educate patient, family, and social support network; address risks to mother and infant and risks in future pregnancies |
| Medication | When prescribing mood stabilizers and/or antipsychotics, consider:
|
Managing PPP
Early symptoms. Because of its severity and rapid evolution, PPP often presents as a psychiatric emergency. Monitor atrisk patients’ sleep patterns and mood for early signs of psychosis.22 Watch especially for hypomanic symptoms such as elevated or mixed mood and decreased judgment, which are common early in PPP.13
A mother with few signs of abnormal mood, good social support, and close follow-up may potentially be safely managed as an outpatient. Initial evaluation and management of PPP usually requires hospitalization, however, because of the risks of suicide, infanticide, and child maltreatment.23
Hospitalization. Mother-infant bonding is important, but safety is paramount if a mother is psychotic—especially if she is experiencing psychotic thoughts about her infant. If possible, the infant should remain with family members during the mother’s hospitalization. Supervised mother-infant visits are often arranged, as appropriate.
Mood-stabilizing medications, including antipsychotics, are mainstays of treatment.24 In some cases, conventional antipsychotics such as haloperidol may be useful because of a lower risk of weight gain or of sedation that could impair a mother’s ability to respond to her infant. Electroconvulsive therapy often yields rapid symptomatic improvement for mothers with postpartum mood or psychotic symptoms.25
Discharge planning. Assuming that the mother adheres to prescribed treatment, discharge may occur within 1 week. Plan discharge arrangements carefully (Table 4).28 A team approach can be very useful within the outpatient clinic. In the model of the Perinatal Psychiatry Clinic of Connections in suburban Cleveland, OH, the mother’s treatment team includes perinatal psychiatrists, nurses, counsellors, case managers (who do home visits), and peer counselors.
Outpatient civil commitment, in which patients are mandated to accept treatment, is an option in some jurisdictions and could help ensure that patients receive treatment consistently.
Table 4
Discharge planning for safety of mother and infant
| Notify child protective services (CPS) depending on the risk to the child. Case-by-case review is needed to assess whether the infant should be removed. CPS may put in place a plan for safety, short of removal. The plan may require that the woman continue psychiatric care |
| Meet with the patient and family to discuss her diagnosis, the risks, the importance of continued medication adherence, and the need for family or social supports to assist with child care |
| Consider engaging visiting nurses or doulas to provide help and support at home |
| Schedule frequent outpatient appointments for the mother after discharge |
| Consider family therapy after the mother has improved because of her risk for affective episodes outside the postpartum28 |
Related resources
- Altshuler L, Richards M, Yonkers K. Treating bipolar disorder during pregnancy. Current Psychiatry. 2003;2(7):14-26. www.CurrentPsychiatry.com.
- Gentile S. Infant safety with antipsychotic therapy in breastfeeding: a systematic review. J Clin Psychiatry. 2008;69(4):666-673.
- Miller LJ. Postpartum mood disorders. Washington, DC: American Psychiatric Publishing, Inc; 1999.
- Stowe ZN. The use of mood stabilizers during breastfeeding. J Clin Psychiatry. 2007;68(suppl 9):22-28.
- Toxicology Data Network (Toxnet). Literature on reproductive risks associated with psychotropics. National Library of Medicine. http://toxnet.nlm.nih.gov.
- Haloperidol • Haldol
- Lithium • various
- Olanzapine • Zyprexa
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
Dr. Resnick, a forensic psychiatrist and coauthor of this article, testified for the defense in both trials of Andrea Yates.
1. Resnick PJ. The Andrea Yates case: insanity on trial. Cleveland State Law Review. 2007;55(2):147-156.
2. Altshuler LL, Hendrick V, Cohen LS. Course of mood and anxiety disorders during pregnancy and the postpartum period. J Clin Psychiatry. 1998;59(suppl. 2):29-33.
3. Knops GG. Postpartum mood disorders. Postgrad Med. 1993;93:103-116.
4. Resnick PJ. Child murder by parents: a psychiatric review of filicide. Am J Psychiatry. 1969;126:73-82.
5. Friedman SH, Horwitz SM, Resnick PJ. Child murder by mothers: a critical analysis of the current state of knowledge and a research agenda. Am J Psychiatry. 2005;162:1578-1587.
6. Friedman SH, Resnick PJ. Neonaticide: phenomenology and considerations for prevention. Int J Law Psychiatry. In press.
7. Wisner K, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30:77-87.
8. Chandra PS, Venkatasubramanian G, Thomas T. Infanticidal ideas and infanticidal behaviour in Indian women with severe postpartum psychiatric disorders. J Nerv Ment Dis. 2002;190(7):457-461.
9. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
10. Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Women’s Health. 2006;15(4):352-368.
11. Attia E, Downey J, Oberman M. Postpartum psychoses. In: Miller LJ, ed. Postpartum mood disorders. Washington, DC: American Psychiatric Publishing Inc.; 1999:99-117.
12. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
13. Heron J, McGuinness M, Blackmore ER, et al. Early postpartum symptoms in puerperal psychosis. BJOG. 2008;115(3):348-353.
14. Meltzer-Brody S, Payne J, Rubinow D. Postpartum depression: what to tell patients who breast-feed. Current Psychiatry. 2008;7(5):87-95.
15. Jennings KD, Ross S, Popper S, et al. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54:21-28.
16. Wisner KL, Gracious BL, Piontek CM, et al. Postpartum disorders: phenomenology, treatment approaches, and relationship to infanticide. In: Spinelli MG, ed. Infanticide: psychosocial and legal perspectives on mothers who kill. Washington, DC: American Psychiatric Publishing, Inc.; 2003.
17. Fairbrother N, Abramowitz JS. New parenthood as a risk factors for the development of obsessional problems. Behav Res Ther. 2007;45(9):2155-2163.
18. Cohen LS, Sichel DA, Robertson LM, et al. Postpartum prophylaxis for women with bipolar disorder. Am J Psychiatry. 1995;152(11):1641-1645.
19. Stewart DE, Klompenhouwer JL, Kendell RE, et al. Prophylactic lithium in puerperal psychosis. Br J Psychiatry. 1991;158:393-397.
20. Sharma V, Smith A, Mazmanian D. Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord. 2006;8(4):400-404.
21. Pfuhlmann B, Stoeber G, Beckmann H. Postpartum psychoses: prognosis, risk factors, and treatment. Curr Psychiatry Rep. 2002;4(3):185-190.
22. Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5(2):98-105.
23. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
24. Connell M. The postpartum psychosis defense and feminism: more or less justice for women? Case Western Reserve Law Review. 2002;53:143.-
25. Forray A, Ostroff RB. The use of electroconvulsive therapy in postpartum affective disorders. J ECT. 2007;23(3):188-193.
26. Engqvist I, Nilsson A, Nilsson K, et al. Strategies in caring for women with postpartum psychosis—an interview study with psychiatric nurses. J Clin Nurs. 2007;16(7):1333-1342.
27. Robertson E, Lyons A. Living with puerperal psychosis: a qualitative analysis. Psychol Psychother. 2003;76(4):411-431.
28. Robertson E, Jones I, Haque S, et al. Risk of puerperal and non-puerperal recurrence of illness following bipolar affective puerperal (post-partum) psychosis. Br J Psychiatry. 2005;186:258-259.
1. Resnick PJ. The Andrea Yates case: insanity on trial. Cleveland State Law Review. 2007;55(2):147-156.
2. Altshuler LL, Hendrick V, Cohen LS. Course of mood and anxiety disorders during pregnancy and the postpartum period. J Clin Psychiatry. 1998;59(suppl. 2):29-33.
3. Knops GG. Postpartum mood disorders. Postgrad Med. 1993;93:103-116.
4. Resnick PJ. Child murder by parents: a psychiatric review of filicide. Am J Psychiatry. 1969;126:73-82.
5. Friedman SH, Horwitz SM, Resnick PJ. Child murder by mothers: a critical analysis of the current state of knowledge and a research agenda. Am J Psychiatry. 2005;162:1578-1587.
6. Friedman SH, Resnick PJ. Neonaticide: phenomenology and considerations for prevention. Int J Law Psychiatry. In press.
7. Wisner K, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30:77-87.
8. Chandra PS, Venkatasubramanian G, Thomas T. Infanticidal ideas and infanticidal behaviour in Indian women with severe postpartum psychiatric disorders. J Nerv Ment Dis. 2002;190(7):457-461.
9. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
10. Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Women’s Health. 2006;15(4):352-368.
11. Attia E, Downey J, Oberman M. Postpartum psychoses. In: Miller LJ, ed. Postpartum mood disorders. Washington, DC: American Psychiatric Publishing Inc.; 1999:99-117.
12. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
13. Heron J, McGuinness M, Blackmore ER, et al. Early postpartum symptoms in puerperal psychosis. BJOG. 2008;115(3):348-353.
14. Meltzer-Brody S, Payne J, Rubinow D. Postpartum depression: what to tell patients who breast-feed. Current Psychiatry. 2008;7(5):87-95.
15. Jennings KD, Ross S, Popper S, et al. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54:21-28.
16. Wisner KL, Gracious BL, Piontek CM, et al. Postpartum disorders: phenomenology, treatment approaches, and relationship to infanticide. In: Spinelli MG, ed. Infanticide: psychosocial and legal perspectives on mothers who kill. Washington, DC: American Psychiatric Publishing, Inc.; 2003.
17. Fairbrother N, Abramowitz JS. New parenthood as a risk factors for the development of obsessional problems. Behav Res Ther. 2007;45(9):2155-2163.
18. Cohen LS, Sichel DA, Robertson LM, et al. Postpartum prophylaxis for women with bipolar disorder. Am J Psychiatry. 1995;152(11):1641-1645.
19. Stewart DE, Klompenhouwer JL, Kendell RE, et al. Prophylactic lithium in puerperal psychosis. Br J Psychiatry. 1991;158:393-397.
20. Sharma V, Smith A, Mazmanian D. Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord. 2006;8(4):400-404.
21. Pfuhlmann B, Stoeber G, Beckmann H. Postpartum psychoses: prognosis, risk factors, and treatment. Curr Psychiatry Rep. 2002;4(3):185-190.
22. Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5(2):98-105.
23. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
24. Connell M. The postpartum psychosis defense and feminism: more or less justice for women? Case Western Reserve Law Review. 2002;53:143.-
25. Forray A, Ostroff RB. The use of electroconvulsive therapy in postpartum affective disorders. J ECT. 2007;23(3):188-193.
26. Engqvist I, Nilsson A, Nilsson K, et al. Strategies in caring for women with postpartum psychosis—an interview study with psychiatric nurses. J Clin Nurs. 2007;16(7):1333-1342.
27. Robertson E, Lyons A. Living with puerperal psychosis: a qualitative analysis. Psychol Psychother. 2003;76(4):411-431.
28. Robertson E, Jones I, Haque S, et al. Risk of puerperal and non-puerperal recurrence of illness following bipolar affective puerperal (post-partum) psychosis. Br J Psychiatry. 2005;186:258-259.
Deposition dos and don’ts: How to answer 8 tricky questions
During your deposition in a malpractice suit, would you know how to answer if the plaintiff’s counsel asked you: “Doctor, are you saying it was impossible to foresee Mr. Jones’ suicide?”
Ninety percent of malpractice cases are settled before trial, and the deposition often is the turning point.1-3 Your answer to tricky questions such as this could favorably affect a critical stage of litigation—or spur the plaintiff’s attorney to pursue the case more vigorously. Even if a case is settled in the plaintiff’s favor before trial, the deposition’s effectiveness may determine whether the settlement is $300,000 or $1 million.
Don’t go to a deposition unprepared. This article offers guidelines to help you anticipate many different scenarios and includes examples of honest, skillful answers to 8 difficult questions (Box 1).3-7
Digging for pay dirt
Discovery begins after a formal complaint alleges malpractice. The parties to a lawsuit gather information through written interrogatories, requests for documents, and witness depositions—out-of-court testimony to be used later in court or for discovery purposes.8 Discovery’s rationale is to reduce surprises at trial and encourage pretrial settlement. The witness being deposed is the “deponent,” and testimony is given under oath.9
A discovery deposition is designed to gather information, with almost all questions asked by opposing counsel. If you are sued for malpractice, this is the type of deposition you probably will encounter.
Rules of engagement. The plaintiff’s attorney initiates the discovery deposition. Ground rules vary by jurisdiction, but in general the Rules of Civil Procedure give deposing counsel substantial latitude in the questions that can be asked.10 The deponent and defending counsel, opposing counsel, and transcriptionist typically attend the deposition. To help you prepare appropriately, confirm with your defense counsel if other attorneys or the plaintiff will be present.
Not-so-hidden agendas. The plaintiff’s attorney’s primary goal is to gather as much information as possible about your side’s case4 (Table 1). No matter how accurate the medical records may be, they require interpretation and follow-up questioning of key players to get the full story. Opposing counsel also wants to:
- “lock down” your testimony for use at trial (testimony captured at a deposition can be used to impeach a witness who gives inconsistent testimony at trial)9
- “size up” your potential impact on a jury by assessing your strengths and weaknesses as a witness.11
The impression you make may influence the opposing attorney’s decision about how far to pursue the case. Plaintiffs’ attorney Bruce Fagel once told an interviewer that defense attorneys, too, may consider settling a case “if their client shows such arrogance in our deposition that they’re afraid to let him appear in front of a jury.”12
- The Impossible Dream
- The Hypothetical
- Invitation to Speculate
- Did I Say That?
- The Authoritative Treatise
- The Tyranny of Yes or No
- Convoluted Compounds
- Give Me More
Choosing a site. Most depositions take place in a conference room in one of the attorney’s law offices or at a neutral site. Avoid the temptation to schedule the de-position in your office, even though meeting there might seem more expedient and comfortable for you.9 Scheduling the deposition at your site:
- might make you feel it is “just another day at the office” and dissuade you from preparing sufficiently or taking the deposition seriously
- allows opposing counsel to scrutinize diplomas, books, journals, and other materials in your office.
Questioning you about these materials during the deposition is not off limits for the plaintiff’s attorney. You might find it difficult to explain why a book on your bookshelf is not “authoritative.”
Table 1
5 goals of the plaintiff’s attorney at a deposition
| Lock down testimony for trial |
| Scrutinize defendant’s qualifications |
| Size up defendant’s effectiveness as a witness |
| Probe defendant for bias, arrogance, or hostility |
| Learn as much as possible (‘fishing’) |
Prepare, prepare, prepare
Your emotional stress will probably wax and wane during the lengthy litigation process.13,14 Knowing what to expect and being well-prepared for the deposition may relieve some anxiety.
Review the case. At least twice, carefully review the entire database—including medical records and other fact witness discovery depositions. Perform 1 of these reviews just before the deposition.3 Having the details fresh in mind will help you if opposing counsel mischaracterizes information when questioning you.
Meet with your attorney. Insist on at least 2 predeposition conferences with defense counsel.
At the first conference, volunteer all pertinent information about the case as well as any noteworthy medical inconsistencies.2 Find out what documents to bring to the deposition, who will be present, and the expected duration. You might wish to prepare mentally by inquiring about the style and personality of opposing counsel.
Defense counsel does not control how long a deposition lasts but might be able to give a rough estimate. Plan accordingly, and allow for sufficient scheduling flexibility. Depositions typically last half a day, but they can last more than 1 day.
At a later predeposition conference, defense counsel might walk you through a mock deposition that involves difficult or anticipated questions. This is a good opportunity to master your anxiety and improve your effectiveness as a witness.
You also may wish to go over your curriculum vitae with defense counsel and check it for mistakes or other content that might raise problematic questions during the deposition (Table 2). Make sure your c.v. is up-to-date, and refresh your memory if it lists lectures given or articles written—no matter how long ago—on topics related to the litigation.
Table 2
Malpractice: How to prepare for your deposition
| Thoroughly review case records |
| Master the case (memorize key names, dates, facts) |
Meet with defense counsel at least twice to:
|
| Double-check your curriculum vitae for accuracy and updating |
| Come to the deposition well-rested |
On deposition day
Don’t open Pandora’s box. Keep your answers to deposition questions brief and clear. Opposing counsel may ask broad questions, hoping to encourage rambling answers that reveal new facts. Answering questions briefly provides the least information to opposing counsel and is best under most circumstances.
One exception may involve scenarios in which the defense attorney instructs you, for various reasons, to provide information beyond the question asked. For example, when a case is close to settling, your attorney might instruct you to lay out all evidence that supports your professional judgment and clinical decisions in the case. Do not use this approach, however, unless your attorney specifically instructs you to do so.
You are under no obligation to make op-posing counsel’s job easier. In a discovery deposition, volunteering information may:
- open up new areas for questioning
- equip the deposing attorney with more ammunition
- eliminate opportunities for your attorney to use surprise as a strategy, should the case go to trial.
Consider, for example, a scenario in which you and a hospital are sued in regard to an inpatient suicide case. At deposition, you might be asked whether you can identify written evidence anywhere in the patient’s chart that the decedent was checked every 15 minutes.
The correct answer would be “no,” even though you know 15-minute checks are documented in a log kept at the nursing station in this hospital. You might be tempted to reveal this information, but leave the timing of its disclosure to the defense attorney. Your attorney’s strategy may be to reveal this critical piece of information at trial, when the plaintiff’s attorney has less opportunity to strategize ways to discredit the evidence.
Keep your cool. Attorneys have different styles of questioning, depending on their personalities. Some may be excessively polite or friendly to get you to let down your guard—only to set you up for a devastating blow at the deposition’s end (or save this for trial). Other attorneys might employ a “bullying” style that seeks to intimidate. In responding to questions, always remain composed and resist the urge to counterattack.
In all circumstances, strive for humility and dignified confidence. Opposing counsel gains the advantage when defendants lose composure or become angry, defensive, or arrogant. Indeed, experienced plaintiff’s attorneys may be testing for precisely this reaction in the hope that a defendant will “demonstrate his arrogance” during the deposition or later on the witness stand.12
In working as expert witnesses in malpractice cases, we have observed many instances in which a defendant psychiatrist’s arrogant or hostile remarks at deposition played a key role in causing the case to be prematurely settled in the plaintiff’s favor.
Avoid making jokes or sarcastic comments. Even a well-timed, self-deprecating joke may backfire should opposing counsel take the opportunity to point out that the case is a “serious matter.”
Listen carefully to each question during the deposition. Pause for a moment to consider the question and allow time for other attorneys to object.5 Your attorney’s objection may suggest the best way for you to respond to the question. Refrain from answering any questions when defense counsel advises you to do so (Table 3).
Don’t answer questions you don’t understand. Rather, ask for clarification. Avoid using adjectives and superlatives such as “never” and “always,” which may be used to distort or mischaracterize your testimony at trial.
Don’t guess. No rule prevents opposing counsel from asking a witness to speculate, but generally avoid doing so. You are required to tell the truth—not to speculate or volunteer guesses. The best way to cause a jury to disbelieve your testimony is to make inaccurate or unfounded statements, which opposing counsel will surely point out at trial.
Don’t be tempted to “plumb the depths” of your memory for a forgotten piece of information, however. If asked, for example, if a patient displayed a specific symptom during an appointment 4 years ago, the true answer is likely to be “not that I recall,” rather than “no.” Qualify similar answers with statements such as “to the best of my recollection,” or “not that I recall at this time.”
If opposing counsel asks questions based on a particular document, request to see the document. Review it carefully for:
- who signed and/or authored it
- when it was prepared and dated
- whether it is a draft copy
- whether it contains confidential information relating to patients other than the plaintiff
- whether it is attorney-client privileged
- and—most importantly—whether opposing counsel has quoted portions of the document out of context.
Procedural pitfalls. Throughout the deposition, the attorneys may periodically tell the court reporter they wish to have a discussion “off the record.” Nothing is off the record for you, however. If you make a statement when the court reporter has been told to stop, opposing counsel can summarize on the record everything you said during that time.
At the beginning or end of the deposition, one of the attorneys may ask if you wish to retain or waive the right to read and sign the deposition transcript. Seek your counsel’s advice, but defendants usually choose to retain this right. Typically, you will have 30 days to read the transcript and correct any errors. Keep in mind, though, that substantive changes that go beyond typos are likely to be the subject of intense cross-examination should the case go to trial.9
Depositions are sometimes videotaped, usually because a witness will not be available at the time of trial. Because the jury will hear and see you, approach a videotaped deposition as if it were an actual trial. Dress appropriately, speak clearly, and look directly into the camera. Don’t feel embarrassed about making sure you are videotaped with the best possible lighting, camera angle, and background.
Table 3
Deposition dos and don’ts
| Always tell the truth |
| Actively listen to questions, and pause before answering |
| Keep your cool; never lose composure |
| Answer only the question asked |
| Stop speaking and listen carefully if your attorney makes an objection |
| Avoid long narratives, and don’t volunteer information |
| Don’t speculate or guess |
| Avoid absolutes such as ‘never’ or ‘always’ |
| Avoid jokes, sarcasm, and edgy comments |
| Ask for breaks if needed to keep from becoming inattentive |
| Carefully examine documents, reports, etc. before answering opposing counsel’s questions about them |
| Ask for clarification of confusing questions |
| Remember that nothing is ‘off the record’ |
| Don’t waive your right to read and sign the deposition transcript |
Keep your guard up
Don’t allow yourself to be distracted if op-posing counsel jumps from open-ended questions to clarification questions to “pinning down” questions. Using an erratic approach could be part of opposing counsel’s strategy. Answer only the question asked, and give the shortest correct answer to each question.
Opposing counsel may ask a question in a way that suggests substantial confusion or misunderstanding. If this confusion does not affect your testimony, you don’t need to clear up matters for opposing counsel. If, for example, opposing counsel asserts that one of your statements was contradictory, an appropriate response may be simply, “No, it wasn’t.” It is opposing counsel’s job to explicate further details.11
Opposing counsel may approach the deposition with a particular demeanor—such as friendly or eager to learn—in an attempt to get you to let down your guard and speak more freely (Box 2).
Particularly in a full-day deposition, the greatest likelihood of making mistakes begins around 4 pm. Indeed, some attorneys may reserve especially important questions for this time period, hoping that the witness will be less guarded. Be sure to start the day well rested, and ask for breaks if fatigue be-gins to affect your concentration.
Be alert to a pattern of questioning designed to elicit only “yes” answers. This technique—commonly used by salespersons—makes it difficult to say “no” in response to an ambiguous question.
Point out errors if opposing counsel misquotes earlier testimony or states facts incorrectly. These mistakes may be innocent or a deliberate attempt to distort your testimony.
‘Mr./Ms. Friendly.’ Some attorneys look for an opportunity before the deposition begins to show that they are ‘friendly’ and not to be feared. Remember that discussions with opposing counsel without defense counsel present are not appropriate.
‘Eager Student.’ Opposing counsel may play the ‘eager student’ to massage your ego and pave the way for long narratives and volunteered information.
‘Counselor Clueless.’ Opposing counsel may appear so ignorant of certain facts that you can scarcely resist jumping in to educate him or her.
Silent treatment. After you give a brief, honest answer, opposing counsel may sit silently as if expecting a more substantive response. Resist the temptation to fill the silence.
Related resources
- Professional Risk Management Services, Inc. The Psychiatrists’ Program. www.psychprogram.com.
- Simon R, Sadoff R. Psychiatric malpractice: cases and comments for clinicians. Washington DC: American Psychiatric Press, Inc; 1992.
Drug brand name
- Olanzapine • Zyprexa
1. Babitsky S, Mangraviti J. The discovery process. In: How to become a dangerous expert witness: advanced techniques and strategies. Falmouth, MA: Seak Inc;2005; 4-9:113-39.
2. Clark A, Fox P. The defendant physician’s deposition: fighting back—at last! Mo Med 2002;99(10):524-5.
3. Rice B. Malpractice: how to survive a deposition. Med Econ 2005;82:45-8.
4. Babitsky S, Mangraviti J. How to excel during depositions: techniques for experts that work. Falmouth, MA: Seak Inc; 1998.
5. Gutheil T. The psychiatrist as expert witness. Washington DC: American Psychiatric Publishing, Inc; 1998.
6. Babitsky S, Mangraviti J. How to excel during cross-examination: techniques for experts that work. Falmouth, MA: Seak Inc; 1997.
7. Hirsch C, Morris R, Moritz A. Handbook of legal medicine. 5th ed. St. Louis, MO: CV Mosby Co; 1979.
8. Black H. Black’s law dictionary. 8th ed. St. Paul, MN: West Publishing; 2004;440-
9. Babitsky S, Mangraviti J. Depositions: the comprehensive guide for expert witnesses. Falmouth, MA: Seak Inc; 2007.
10. Cornell Law School. Federal Rules of Civil Procedure. Depositions and discovery. Rule 26(5) B(1). Available at: http://www.law.cornell.edu/rules/frcp/Rule26.htm. Accessed January 18, 2008.
11. Culley C, Spisak L. So you’re being sued: do’s and don’ts for the defendant. Cleve Clin J Med 2002;69(10):752-60.
12. Rice B. How I pick the doctors I’ll sue. Med Econ 2004;81:54.-
13. Charles S. Coping with a medical malpractice suit. West J Med 2001;174:55-8.
14. Charles S. Malpractice distress: Help yourself and others survive. Current Psychiatry 2007;6(2):23-35.
During your deposition in a malpractice suit, would you know how to answer if the plaintiff’s counsel asked you: “Doctor, are you saying it was impossible to foresee Mr. Jones’ suicide?”
Ninety percent of malpractice cases are settled before trial, and the deposition often is the turning point.1-3 Your answer to tricky questions such as this could favorably affect a critical stage of litigation—or spur the plaintiff’s attorney to pursue the case more vigorously. Even if a case is settled in the plaintiff’s favor before trial, the deposition’s effectiveness may determine whether the settlement is $300,000 or $1 million.
Don’t go to a deposition unprepared. This article offers guidelines to help you anticipate many different scenarios and includes examples of honest, skillful answers to 8 difficult questions (Box 1).3-7
Digging for pay dirt
Discovery begins after a formal complaint alleges malpractice. The parties to a lawsuit gather information through written interrogatories, requests for documents, and witness depositions—out-of-court testimony to be used later in court or for discovery purposes.8 Discovery’s rationale is to reduce surprises at trial and encourage pretrial settlement. The witness being deposed is the “deponent,” and testimony is given under oath.9
A discovery deposition is designed to gather information, with almost all questions asked by opposing counsel. If you are sued for malpractice, this is the type of deposition you probably will encounter.
Rules of engagement. The plaintiff’s attorney initiates the discovery deposition. Ground rules vary by jurisdiction, but in general the Rules of Civil Procedure give deposing counsel substantial latitude in the questions that can be asked.10 The deponent and defending counsel, opposing counsel, and transcriptionist typically attend the deposition. To help you prepare appropriately, confirm with your defense counsel if other attorneys or the plaintiff will be present.
Not-so-hidden agendas. The plaintiff’s attorney’s primary goal is to gather as much information as possible about your side’s case4 (Table 1). No matter how accurate the medical records may be, they require interpretation and follow-up questioning of key players to get the full story. Opposing counsel also wants to:
- “lock down” your testimony for use at trial (testimony captured at a deposition can be used to impeach a witness who gives inconsistent testimony at trial)9
- “size up” your potential impact on a jury by assessing your strengths and weaknesses as a witness.11
The impression you make may influence the opposing attorney’s decision about how far to pursue the case. Plaintiffs’ attorney Bruce Fagel once told an interviewer that defense attorneys, too, may consider settling a case “if their client shows such arrogance in our deposition that they’re afraid to let him appear in front of a jury.”12
- The Impossible Dream
- The Hypothetical
- Invitation to Speculate
- Did I Say That?
- The Authoritative Treatise
- The Tyranny of Yes or No
- Convoluted Compounds
- Give Me More
Choosing a site. Most depositions take place in a conference room in one of the attorney’s law offices or at a neutral site. Avoid the temptation to schedule the de-position in your office, even though meeting there might seem more expedient and comfortable for you.9 Scheduling the deposition at your site:
- might make you feel it is “just another day at the office” and dissuade you from preparing sufficiently or taking the deposition seriously
- allows opposing counsel to scrutinize diplomas, books, journals, and other materials in your office.
Questioning you about these materials during the deposition is not off limits for the plaintiff’s attorney. You might find it difficult to explain why a book on your bookshelf is not “authoritative.”
Table 1
5 goals of the plaintiff’s attorney at a deposition
| Lock down testimony for trial |
| Scrutinize defendant’s qualifications |
| Size up defendant’s effectiveness as a witness |
| Probe defendant for bias, arrogance, or hostility |
| Learn as much as possible (‘fishing’) |
Prepare, prepare, prepare
Your emotional stress will probably wax and wane during the lengthy litigation process.13,14 Knowing what to expect and being well-prepared for the deposition may relieve some anxiety.
Review the case. At least twice, carefully review the entire database—including medical records and other fact witness discovery depositions. Perform 1 of these reviews just before the deposition.3 Having the details fresh in mind will help you if opposing counsel mischaracterizes information when questioning you.
Meet with your attorney. Insist on at least 2 predeposition conferences with defense counsel.
At the first conference, volunteer all pertinent information about the case as well as any noteworthy medical inconsistencies.2 Find out what documents to bring to the deposition, who will be present, and the expected duration. You might wish to prepare mentally by inquiring about the style and personality of opposing counsel.
Defense counsel does not control how long a deposition lasts but might be able to give a rough estimate. Plan accordingly, and allow for sufficient scheduling flexibility. Depositions typically last half a day, but they can last more than 1 day.
At a later predeposition conference, defense counsel might walk you through a mock deposition that involves difficult or anticipated questions. This is a good opportunity to master your anxiety and improve your effectiveness as a witness.
You also may wish to go over your curriculum vitae with defense counsel and check it for mistakes or other content that might raise problematic questions during the deposition (Table 2). Make sure your c.v. is up-to-date, and refresh your memory if it lists lectures given or articles written—no matter how long ago—on topics related to the litigation.
Table 2
Malpractice: How to prepare for your deposition
| Thoroughly review case records |
| Master the case (memorize key names, dates, facts) |
Meet with defense counsel at least twice to:
|
| Double-check your curriculum vitae for accuracy and updating |
| Come to the deposition well-rested |
On deposition day
Don’t open Pandora’s box. Keep your answers to deposition questions brief and clear. Opposing counsel may ask broad questions, hoping to encourage rambling answers that reveal new facts. Answering questions briefly provides the least information to opposing counsel and is best under most circumstances.
One exception may involve scenarios in which the defense attorney instructs you, for various reasons, to provide information beyond the question asked. For example, when a case is close to settling, your attorney might instruct you to lay out all evidence that supports your professional judgment and clinical decisions in the case. Do not use this approach, however, unless your attorney specifically instructs you to do so.
You are under no obligation to make op-posing counsel’s job easier. In a discovery deposition, volunteering information may:
- open up new areas for questioning
- equip the deposing attorney with more ammunition
- eliminate opportunities for your attorney to use surprise as a strategy, should the case go to trial.
Consider, for example, a scenario in which you and a hospital are sued in regard to an inpatient suicide case. At deposition, you might be asked whether you can identify written evidence anywhere in the patient’s chart that the decedent was checked every 15 minutes.
The correct answer would be “no,” even though you know 15-minute checks are documented in a log kept at the nursing station in this hospital. You might be tempted to reveal this information, but leave the timing of its disclosure to the defense attorney. Your attorney’s strategy may be to reveal this critical piece of information at trial, when the plaintiff’s attorney has less opportunity to strategize ways to discredit the evidence.
Keep your cool. Attorneys have different styles of questioning, depending on their personalities. Some may be excessively polite or friendly to get you to let down your guard—only to set you up for a devastating blow at the deposition’s end (or save this for trial). Other attorneys might employ a “bullying” style that seeks to intimidate. In responding to questions, always remain composed and resist the urge to counterattack.
In all circumstances, strive for humility and dignified confidence. Opposing counsel gains the advantage when defendants lose composure or become angry, defensive, or arrogant. Indeed, experienced plaintiff’s attorneys may be testing for precisely this reaction in the hope that a defendant will “demonstrate his arrogance” during the deposition or later on the witness stand.12
In working as expert witnesses in malpractice cases, we have observed many instances in which a defendant psychiatrist’s arrogant or hostile remarks at deposition played a key role in causing the case to be prematurely settled in the plaintiff’s favor.
Avoid making jokes or sarcastic comments. Even a well-timed, self-deprecating joke may backfire should opposing counsel take the opportunity to point out that the case is a “serious matter.”
Listen carefully to each question during the deposition. Pause for a moment to consider the question and allow time for other attorneys to object.5 Your attorney’s objection may suggest the best way for you to respond to the question. Refrain from answering any questions when defense counsel advises you to do so (Table 3).
Don’t answer questions you don’t understand. Rather, ask for clarification. Avoid using adjectives and superlatives such as “never” and “always,” which may be used to distort or mischaracterize your testimony at trial.
Don’t guess. No rule prevents opposing counsel from asking a witness to speculate, but generally avoid doing so. You are required to tell the truth—not to speculate or volunteer guesses. The best way to cause a jury to disbelieve your testimony is to make inaccurate or unfounded statements, which opposing counsel will surely point out at trial.
Don’t be tempted to “plumb the depths” of your memory for a forgotten piece of information, however. If asked, for example, if a patient displayed a specific symptom during an appointment 4 years ago, the true answer is likely to be “not that I recall,” rather than “no.” Qualify similar answers with statements such as “to the best of my recollection,” or “not that I recall at this time.”
If opposing counsel asks questions based on a particular document, request to see the document. Review it carefully for:
- who signed and/or authored it
- when it was prepared and dated
- whether it is a draft copy
- whether it contains confidential information relating to patients other than the plaintiff
- whether it is attorney-client privileged
- and—most importantly—whether opposing counsel has quoted portions of the document out of context.
Procedural pitfalls. Throughout the deposition, the attorneys may periodically tell the court reporter they wish to have a discussion “off the record.” Nothing is off the record for you, however. If you make a statement when the court reporter has been told to stop, opposing counsel can summarize on the record everything you said during that time.
At the beginning or end of the deposition, one of the attorneys may ask if you wish to retain or waive the right to read and sign the deposition transcript. Seek your counsel’s advice, but defendants usually choose to retain this right. Typically, you will have 30 days to read the transcript and correct any errors. Keep in mind, though, that substantive changes that go beyond typos are likely to be the subject of intense cross-examination should the case go to trial.9
Depositions are sometimes videotaped, usually because a witness will not be available at the time of trial. Because the jury will hear and see you, approach a videotaped deposition as if it were an actual trial. Dress appropriately, speak clearly, and look directly into the camera. Don’t feel embarrassed about making sure you are videotaped with the best possible lighting, camera angle, and background.
Table 3
Deposition dos and don’ts
| Always tell the truth |
| Actively listen to questions, and pause before answering |
| Keep your cool; never lose composure |
| Answer only the question asked |
| Stop speaking and listen carefully if your attorney makes an objection |
| Avoid long narratives, and don’t volunteer information |
| Don’t speculate or guess |
| Avoid absolutes such as ‘never’ or ‘always’ |
| Avoid jokes, sarcasm, and edgy comments |
| Ask for breaks if needed to keep from becoming inattentive |
| Carefully examine documents, reports, etc. before answering opposing counsel’s questions about them |
| Ask for clarification of confusing questions |
| Remember that nothing is ‘off the record’ |
| Don’t waive your right to read and sign the deposition transcript |
Keep your guard up
Don’t allow yourself to be distracted if op-posing counsel jumps from open-ended questions to clarification questions to “pinning down” questions. Using an erratic approach could be part of opposing counsel’s strategy. Answer only the question asked, and give the shortest correct answer to each question.
Opposing counsel may ask a question in a way that suggests substantial confusion or misunderstanding. If this confusion does not affect your testimony, you don’t need to clear up matters for opposing counsel. If, for example, opposing counsel asserts that one of your statements was contradictory, an appropriate response may be simply, “No, it wasn’t.” It is opposing counsel’s job to explicate further details.11
Opposing counsel may approach the deposition with a particular demeanor—such as friendly or eager to learn—in an attempt to get you to let down your guard and speak more freely (Box 2).
Particularly in a full-day deposition, the greatest likelihood of making mistakes begins around 4 pm. Indeed, some attorneys may reserve especially important questions for this time period, hoping that the witness will be less guarded. Be sure to start the day well rested, and ask for breaks if fatigue be-gins to affect your concentration.
Be alert to a pattern of questioning designed to elicit only “yes” answers. This technique—commonly used by salespersons—makes it difficult to say “no” in response to an ambiguous question.
Point out errors if opposing counsel misquotes earlier testimony or states facts incorrectly. These mistakes may be innocent or a deliberate attempt to distort your testimony.
‘Mr./Ms. Friendly.’ Some attorneys look for an opportunity before the deposition begins to show that they are ‘friendly’ and not to be feared. Remember that discussions with opposing counsel without defense counsel present are not appropriate.
‘Eager Student.’ Opposing counsel may play the ‘eager student’ to massage your ego and pave the way for long narratives and volunteered information.
‘Counselor Clueless.’ Opposing counsel may appear so ignorant of certain facts that you can scarcely resist jumping in to educate him or her.
Silent treatment. After you give a brief, honest answer, opposing counsel may sit silently as if expecting a more substantive response. Resist the temptation to fill the silence.
Related resources
- Professional Risk Management Services, Inc. The Psychiatrists’ Program. www.psychprogram.com.
- Simon R, Sadoff R. Psychiatric malpractice: cases and comments for clinicians. Washington DC: American Psychiatric Press, Inc; 1992.
Drug brand name
- Olanzapine • Zyprexa
During your deposition in a malpractice suit, would you know how to answer if the plaintiff’s counsel asked you: “Doctor, are you saying it was impossible to foresee Mr. Jones’ suicide?”
Ninety percent of malpractice cases are settled before trial, and the deposition often is the turning point.1-3 Your answer to tricky questions such as this could favorably affect a critical stage of litigation—or spur the plaintiff’s attorney to pursue the case more vigorously. Even if a case is settled in the plaintiff’s favor before trial, the deposition’s effectiveness may determine whether the settlement is $300,000 or $1 million.
Don’t go to a deposition unprepared. This article offers guidelines to help you anticipate many different scenarios and includes examples of honest, skillful answers to 8 difficult questions (Box 1).3-7
Digging for pay dirt
Discovery begins after a formal complaint alleges malpractice. The parties to a lawsuit gather information through written interrogatories, requests for documents, and witness depositions—out-of-court testimony to be used later in court or for discovery purposes.8 Discovery’s rationale is to reduce surprises at trial and encourage pretrial settlement. The witness being deposed is the “deponent,” and testimony is given under oath.9
A discovery deposition is designed to gather information, with almost all questions asked by opposing counsel. If you are sued for malpractice, this is the type of deposition you probably will encounter.
Rules of engagement. The plaintiff’s attorney initiates the discovery deposition. Ground rules vary by jurisdiction, but in general the Rules of Civil Procedure give deposing counsel substantial latitude in the questions that can be asked.10 The deponent and defending counsel, opposing counsel, and transcriptionist typically attend the deposition. To help you prepare appropriately, confirm with your defense counsel if other attorneys or the plaintiff will be present.
Not-so-hidden agendas. The plaintiff’s attorney’s primary goal is to gather as much information as possible about your side’s case4 (Table 1). No matter how accurate the medical records may be, they require interpretation and follow-up questioning of key players to get the full story. Opposing counsel also wants to:
- “lock down” your testimony for use at trial (testimony captured at a deposition can be used to impeach a witness who gives inconsistent testimony at trial)9
- “size up” your potential impact on a jury by assessing your strengths and weaknesses as a witness.11
The impression you make may influence the opposing attorney’s decision about how far to pursue the case. Plaintiffs’ attorney Bruce Fagel once told an interviewer that defense attorneys, too, may consider settling a case “if their client shows such arrogance in our deposition that they’re afraid to let him appear in front of a jury.”12
- The Impossible Dream
- The Hypothetical
- Invitation to Speculate
- Did I Say That?
- The Authoritative Treatise
- The Tyranny of Yes or No
- Convoluted Compounds
- Give Me More
Choosing a site. Most depositions take place in a conference room in one of the attorney’s law offices or at a neutral site. Avoid the temptation to schedule the de-position in your office, even though meeting there might seem more expedient and comfortable for you.9 Scheduling the deposition at your site:
- might make you feel it is “just another day at the office” and dissuade you from preparing sufficiently or taking the deposition seriously
- allows opposing counsel to scrutinize diplomas, books, journals, and other materials in your office.
Questioning you about these materials during the deposition is not off limits for the plaintiff’s attorney. You might find it difficult to explain why a book on your bookshelf is not “authoritative.”
Table 1
5 goals of the plaintiff’s attorney at a deposition
| Lock down testimony for trial |
| Scrutinize defendant’s qualifications |
| Size up defendant’s effectiveness as a witness |
| Probe defendant for bias, arrogance, or hostility |
| Learn as much as possible (‘fishing’) |
Prepare, prepare, prepare
Your emotional stress will probably wax and wane during the lengthy litigation process.13,14 Knowing what to expect and being well-prepared for the deposition may relieve some anxiety.
Review the case. At least twice, carefully review the entire database—including medical records and other fact witness discovery depositions. Perform 1 of these reviews just before the deposition.3 Having the details fresh in mind will help you if opposing counsel mischaracterizes information when questioning you.
Meet with your attorney. Insist on at least 2 predeposition conferences with defense counsel.
At the first conference, volunteer all pertinent information about the case as well as any noteworthy medical inconsistencies.2 Find out what documents to bring to the deposition, who will be present, and the expected duration. You might wish to prepare mentally by inquiring about the style and personality of opposing counsel.
Defense counsel does not control how long a deposition lasts but might be able to give a rough estimate. Plan accordingly, and allow for sufficient scheduling flexibility. Depositions typically last half a day, but they can last more than 1 day.
At a later predeposition conference, defense counsel might walk you through a mock deposition that involves difficult or anticipated questions. This is a good opportunity to master your anxiety and improve your effectiveness as a witness.
You also may wish to go over your curriculum vitae with defense counsel and check it for mistakes or other content that might raise problematic questions during the deposition (Table 2). Make sure your c.v. is up-to-date, and refresh your memory if it lists lectures given or articles written—no matter how long ago—on topics related to the litigation.
Table 2
Malpractice: How to prepare for your deposition
| Thoroughly review case records |
| Master the case (memorize key names, dates, facts) |
Meet with defense counsel at least twice to:
|
| Double-check your curriculum vitae for accuracy and updating |
| Come to the deposition well-rested |
On deposition day
Don’t open Pandora’s box. Keep your answers to deposition questions brief and clear. Opposing counsel may ask broad questions, hoping to encourage rambling answers that reveal new facts. Answering questions briefly provides the least information to opposing counsel and is best under most circumstances.
One exception may involve scenarios in which the defense attorney instructs you, for various reasons, to provide information beyond the question asked. For example, when a case is close to settling, your attorney might instruct you to lay out all evidence that supports your professional judgment and clinical decisions in the case. Do not use this approach, however, unless your attorney specifically instructs you to do so.
You are under no obligation to make op-posing counsel’s job easier. In a discovery deposition, volunteering information may:
- open up new areas for questioning
- equip the deposing attorney with more ammunition
- eliminate opportunities for your attorney to use surprise as a strategy, should the case go to trial.
Consider, for example, a scenario in which you and a hospital are sued in regard to an inpatient suicide case. At deposition, you might be asked whether you can identify written evidence anywhere in the patient’s chart that the decedent was checked every 15 minutes.
The correct answer would be “no,” even though you know 15-minute checks are documented in a log kept at the nursing station in this hospital. You might be tempted to reveal this information, but leave the timing of its disclosure to the defense attorney. Your attorney’s strategy may be to reveal this critical piece of information at trial, when the plaintiff’s attorney has less opportunity to strategize ways to discredit the evidence.
Keep your cool. Attorneys have different styles of questioning, depending on their personalities. Some may be excessively polite or friendly to get you to let down your guard—only to set you up for a devastating blow at the deposition’s end (or save this for trial). Other attorneys might employ a “bullying” style that seeks to intimidate. In responding to questions, always remain composed and resist the urge to counterattack.
In all circumstances, strive for humility and dignified confidence. Opposing counsel gains the advantage when defendants lose composure or become angry, defensive, or arrogant. Indeed, experienced plaintiff’s attorneys may be testing for precisely this reaction in the hope that a defendant will “demonstrate his arrogance” during the deposition or later on the witness stand.12
In working as expert witnesses in malpractice cases, we have observed many instances in which a defendant psychiatrist’s arrogant or hostile remarks at deposition played a key role in causing the case to be prematurely settled in the plaintiff’s favor.
Avoid making jokes or sarcastic comments. Even a well-timed, self-deprecating joke may backfire should opposing counsel take the opportunity to point out that the case is a “serious matter.”
Listen carefully to each question during the deposition. Pause for a moment to consider the question and allow time for other attorneys to object.5 Your attorney’s objection may suggest the best way for you to respond to the question. Refrain from answering any questions when defense counsel advises you to do so (Table 3).
Don’t answer questions you don’t understand. Rather, ask for clarification. Avoid using adjectives and superlatives such as “never” and “always,” which may be used to distort or mischaracterize your testimony at trial.
Don’t guess. No rule prevents opposing counsel from asking a witness to speculate, but generally avoid doing so. You are required to tell the truth—not to speculate or volunteer guesses. The best way to cause a jury to disbelieve your testimony is to make inaccurate or unfounded statements, which opposing counsel will surely point out at trial.
Don’t be tempted to “plumb the depths” of your memory for a forgotten piece of information, however. If asked, for example, if a patient displayed a specific symptom during an appointment 4 years ago, the true answer is likely to be “not that I recall,” rather than “no.” Qualify similar answers with statements such as “to the best of my recollection,” or “not that I recall at this time.”
If opposing counsel asks questions based on a particular document, request to see the document. Review it carefully for:
- who signed and/or authored it
- when it was prepared and dated
- whether it is a draft copy
- whether it contains confidential information relating to patients other than the plaintiff
- whether it is attorney-client privileged
- and—most importantly—whether opposing counsel has quoted portions of the document out of context.
Procedural pitfalls. Throughout the deposition, the attorneys may periodically tell the court reporter they wish to have a discussion “off the record.” Nothing is off the record for you, however. If you make a statement when the court reporter has been told to stop, opposing counsel can summarize on the record everything you said during that time.
At the beginning or end of the deposition, one of the attorneys may ask if you wish to retain or waive the right to read and sign the deposition transcript. Seek your counsel’s advice, but defendants usually choose to retain this right. Typically, you will have 30 days to read the transcript and correct any errors. Keep in mind, though, that substantive changes that go beyond typos are likely to be the subject of intense cross-examination should the case go to trial.9
Depositions are sometimes videotaped, usually because a witness will not be available at the time of trial. Because the jury will hear and see you, approach a videotaped deposition as if it were an actual trial. Dress appropriately, speak clearly, and look directly into the camera. Don’t feel embarrassed about making sure you are videotaped with the best possible lighting, camera angle, and background.
Table 3
Deposition dos and don’ts
| Always tell the truth |
| Actively listen to questions, and pause before answering |
| Keep your cool; never lose composure |
| Answer only the question asked |
| Stop speaking and listen carefully if your attorney makes an objection |
| Avoid long narratives, and don’t volunteer information |
| Don’t speculate or guess |
| Avoid absolutes such as ‘never’ or ‘always’ |
| Avoid jokes, sarcasm, and edgy comments |
| Ask for breaks if needed to keep from becoming inattentive |
| Carefully examine documents, reports, etc. before answering opposing counsel’s questions about them |
| Ask for clarification of confusing questions |
| Remember that nothing is ‘off the record’ |
| Don’t waive your right to read and sign the deposition transcript |
Keep your guard up
Don’t allow yourself to be distracted if op-posing counsel jumps from open-ended questions to clarification questions to “pinning down” questions. Using an erratic approach could be part of opposing counsel’s strategy. Answer only the question asked, and give the shortest correct answer to each question.
Opposing counsel may ask a question in a way that suggests substantial confusion or misunderstanding. If this confusion does not affect your testimony, you don’t need to clear up matters for opposing counsel. If, for example, opposing counsel asserts that one of your statements was contradictory, an appropriate response may be simply, “No, it wasn’t.” It is opposing counsel’s job to explicate further details.11
Opposing counsel may approach the deposition with a particular demeanor—such as friendly or eager to learn—in an attempt to get you to let down your guard and speak more freely (Box 2).
Particularly in a full-day deposition, the greatest likelihood of making mistakes begins around 4 pm. Indeed, some attorneys may reserve especially important questions for this time period, hoping that the witness will be less guarded. Be sure to start the day well rested, and ask for breaks if fatigue be-gins to affect your concentration.
Be alert to a pattern of questioning designed to elicit only “yes” answers. This technique—commonly used by salespersons—makes it difficult to say “no” in response to an ambiguous question.
Point out errors if opposing counsel misquotes earlier testimony or states facts incorrectly. These mistakes may be innocent or a deliberate attempt to distort your testimony.
‘Mr./Ms. Friendly.’ Some attorneys look for an opportunity before the deposition begins to show that they are ‘friendly’ and not to be feared. Remember that discussions with opposing counsel without defense counsel present are not appropriate.
‘Eager Student.’ Opposing counsel may play the ‘eager student’ to massage your ego and pave the way for long narratives and volunteered information.
‘Counselor Clueless.’ Opposing counsel may appear so ignorant of certain facts that you can scarcely resist jumping in to educate him or her.
Silent treatment. After you give a brief, honest answer, opposing counsel may sit silently as if expecting a more substantive response. Resist the temptation to fill the silence.
Related resources
- Professional Risk Management Services, Inc. The Psychiatrists’ Program. www.psychprogram.com.
- Simon R, Sadoff R. Psychiatric malpractice: cases and comments for clinicians. Washington DC: American Psychiatric Press, Inc; 1992.
Drug brand name
- Olanzapine • Zyprexa
1. Babitsky S, Mangraviti J. The discovery process. In: How to become a dangerous expert witness: advanced techniques and strategies. Falmouth, MA: Seak Inc;2005; 4-9:113-39.
2. Clark A, Fox P. The defendant physician’s deposition: fighting back—at last! Mo Med 2002;99(10):524-5.
3. Rice B. Malpractice: how to survive a deposition. Med Econ 2005;82:45-8.
4. Babitsky S, Mangraviti J. How to excel during depositions: techniques for experts that work. Falmouth, MA: Seak Inc; 1998.
5. Gutheil T. The psychiatrist as expert witness. Washington DC: American Psychiatric Publishing, Inc; 1998.
6. Babitsky S, Mangraviti J. How to excel during cross-examination: techniques for experts that work. Falmouth, MA: Seak Inc; 1997.
7. Hirsch C, Morris R, Moritz A. Handbook of legal medicine. 5th ed. St. Louis, MO: CV Mosby Co; 1979.
8. Black H. Black’s law dictionary. 8th ed. St. Paul, MN: West Publishing; 2004;440-
9. Babitsky S, Mangraviti J. Depositions: the comprehensive guide for expert witnesses. Falmouth, MA: Seak Inc; 2007.
10. Cornell Law School. Federal Rules of Civil Procedure. Depositions and discovery. Rule 26(5) B(1). Available at: http://www.law.cornell.edu/rules/frcp/Rule26.htm. Accessed January 18, 2008.
11. Culley C, Spisak L. So you’re being sued: do’s and don’ts for the defendant. Cleve Clin J Med 2002;69(10):752-60.
12. Rice B. How I pick the doctors I’ll sue. Med Econ 2004;81:54.-
13. Charles S. Coping with a medical malpractice suit. West J Med 2001;174:55-8.
14. Charles S. Malpractice distress: Help yourself and others survive. Current Psychiatry 2007;6(2):23-35.
1. Babitsky S, Mangraviti J. The discovery process. In: How to become a dangerous expert witness: advanced techniques and strategies. Falmouth, MA: Seak Inc;2005; 4-9:113-39.
2. Clark A, Fox P. The defendant physician’s deposition: fighting back—at last! Mo Med 2002;99(10):524-5.
3. Rice B. Malpractice: how to survive a deposition. Med Econ 2005;82:45-8.
4. Babitsky S, Mangraviti J. How to excel during depositions: techniques for experts that work. Falmouth, MA: Seak Inc; 1998.
5. Gutheil T. The psychiatrist as expert witness. Washington DC: American Psychiatric Publishing, Inc; 1998.
6. Babitsky S, Mangraviti J. How to excel during cross-examination: techniques for experts that work. Falmouth, MA: Seak Inc; 1997.
7. Hirsch C, Morris R, Moritz A. Handbook of legal medicine. 5th ed. St. Louis, MO: CV Mosby Co; 1979.
8. Black H. Black’s law dictionary. 8th ed. St. Paul, MN: West Publishing; 2004;440-
9. Babitsky S, Mangraviti J. Depositions: the comprehensive guide for expert witnesses. Falmouth, MA: Seak Inc; 2007.
10. Cornell Law School. Federal Rules of Civil Procedure. Depositions and discovery. Rule 26(5) B(1). Available at: http://www.law.cornell.edu/rules/frcp/Rule26.htm. Accessed January 18, 2008.
11. Culley C, Spisak L. So you’re being sued: do’s and don’ts for the defendant. Cleve Clin J Med 2002;69(10):752-60.
12. Rice B. How I pick the doctors I’ll sue. Med Econ 2004;81:54.-
13. Charles S. Coping with a medical malpractice suit. West J Med 2001;174:55-8.
14. Charles S. Malpractice distress: Help yourself and others survive. Current Psychiatry 2007;6(2):23-35.
Stalking intervention: Know the 5 stalker types, safety strategies for victims
A patient, a colleague, or perhaps you have been stalked. The chances of a woman being stalked are an estimated 1 in 14; for men, it is 1 in 50.1 Fearful stalking victims may restrict their lives, change jobs, and curtail social activities to protect themselves from unwanted attention, physical assault, or even murder. They may develop anxiety, depression, or posttraumatic stress disorder (PTSD).2,3
Historical, clinical, and behavioral factors increase a stalker’s risk for committing violence (Table 1).2-7 As a psychiatrist, you may be asked to consult with local law enforcement and stalking victims to assess and manage victims’ risk. To best protect them, be aware of:
- 5 types of stalkers and their typical response to management strategies
- legal and safety issues to consider before taking actions that might endanger stalking victims
- strategies to help victims protect themselves
- interventions for victims and stalkers.
Table 1
Factors that increase the risk of violence
| Factor type | Features |
|---|---|
| Historical | Ex-intimate partner |
| Previous violence | |
| Criminal record (especially violent crimes) | |
| Previous threats (especially specific or face-to-face) | |
| Clinical | “Rejected” or “predatory” stalker type |
| Substance use | |
| Narcissism, entitlement | |
| Personality disorder with anger or behavioral instability | |
| Depression with suicidal ideas | |
| Behavioral | Access to weapons |
| Proximity to victim | |
| Victim in a new relationship | |
| Has already taken actions on plans/threats | |
| Researching the victim | |
| Unconcerned with negative consequences | |
| Risk factors for homicide or serious physical harm: | |
| |
| Source: References 2-7 | |
Stalker types
Mullen et al8 developed a clinically oriented, validated stalker classification system to identify an individual stalker’s type, risks, and probable responses to management interventions (Table 2).
Rejected stalkers—the most common and dangerous type—pursue the victim, often a former intimate partner, after a relationship ends. They often acknowledge a complex and volatile mix of desire for reconciliation and revenge. These stalkers likely have a history of criminal assault.
Rejected stalkers appear to respond best to a combination of coordinated legal sanctions and mental health intervention. Because they are most likely to be violent, rejected stalkers need intensive probation or parole supervision.5
Intimacy-seeking stalkers want an intimate relationship with a victim they believe is their “true love” and tend to imbue their victims with special desirability, excellence, and other qualities consistent with their belief of romanticized love. Most have erotomanic delusions, and the rest have morbid infatuations with the victim. Intimacy-seeking stalkers typically are unperturbed by legal sanctions, viewing them as the price to pay for “true love.” They often require court-mandated psychiatric treatment.
Incompetent stalkers know the victim is disinterested but forge ahead in hopes that their behavior will lead to a relationship. Their stalking can be viewed as crude or “incompetent” attempts to court the victim. Incompetent stalkers often are intellectually limited; they feel entitled to a partner but because of underdeveloped social skills are unable to build upon lesser forms of social interaction. Unlike intimacy-seekers, incompetent stalkers do not endow the victim with unique qualities.
In addition to needing legal sanctions and possible mental health treatment, incompetent stalkers often require social skills training. Otherwise, they are likely to continue their pattern of stalking with other victims.
Resentful stalkers who suffer from mental illness generally require court-ordered psychiatric treatment but are difficult to engage in therapy. Legal sanctions may inflame this type of stalker.
Predatory stalkers prepare for a sexual assault. They stalk to discover the victim’s vulnerabilities and seldom give warnings, so the victim is often unaware of the danger.
Predatory stalkers frequently suffer from paraphilias and have prior convictions for sexual offenses. They must be secured in a correctional or forensic setting to address their paraphilias and propensity for violence.
Table 2
Identifying types of stalkers
| Type | Traits and behaviors |
|---|---|
| Rejected | Pursues former intimate partner |
| Desires reconciliation and/or revenge | |
| Criminal assault history | |
| Personality disorders predominate | |
| Intimacy-seeking | Desires relationship with “true love” |
| Oblivious to victim response | |
| Most have erotomanic delusions | |
| Endows victim with unique qualities | |
| Incompetent | Acknowledges victim’s disinterest |
| Hopes behavior leads to intimacy | |
| Does not endow victim with unique qualities | |
| Low IQ, socially inept, entitled | |
| Resentful | Feels persecuted and desires retribution |
| Intends to frighten or distress | |
| Specific or general grievance | |
| Paranoid diagnoses | |
| Predatory | Preparing for sexual attack |
| Stalks to study and observe | |
| Paraphilias, prior sexual offenses are common | |
| No warnings before attack | |
| Source: Reference 8 | |
Managing victims’ risk
Effectively managing a victim’s stalking risk is a dynamic process. It is critical to use professional judgment in a flexible manner and to work as a team with professionals from other agencies (Box).9-12
Intervention dilemma. Before taking any action, consider that taking direct measures against the stalker to reduce stalking may increase the risk of violence.10 A law enforcement intervention may provoke a stalker by challenging or humiliating him or her. Therefore, there is no single best approach to risk management. Consider the significance of individual-specific nuances, and solicit input from different disciplines. In some cases, no direct action may be preferable.
Protective orders. Obtaining a protective order may or may not be helpful. Most domestic violence research indicates that such orders protect abused women.13 This is important because stalking by a former intimate partner often occurs in relationships characterized by domestic violence.14 In addition to potentially preventing stalking behavior, a protective order may provide legal evidence of the course of stalking, as well as document a “fearful victim,” which is required by law to obtain a criminal conviction.
No conclusive studies have investigated the effectiveness of protective orders specifically related to stalkers, so consider the stalker’s reaction to previous orders.15 Counsel a victim who obtains a protective order against a former intimate partner to avoid developing a false sense of security. Rejected stalkers who have considerable emotional investment in the relationship may not be deterred by the threat of criminal sanctions. Furthermore, stalkers who are psychotic may misperceive and disregard criminal injunctions. In rare cases, a protective order may escalate stalking and violence.15
Dramatic moments. Advise a victim to remain vigilant during “dramatic moments” when violence risk may be especially heightened.15 These include:
- arrests
- issuance of protective orders
- court hearings
- custody hearings
- anniversary dates
- family-oriented holidays.
Encourage a victim who is especially concerned about an impending dramatic moment to prepare by:
- arranging to be out of town on that date
- notifying law enforcement and victim advocates.
A multidisciplinary approach is the most effective way to reduce stalking violence risk. In addition to mental health professionals, an effective team usually includes law enforcement and criminal justice personnel, attorneys, security specialists/private investigators, victim advocates, and the victim and his or her social network.
The victim can increase the chances that officials will view his or her case as a priority by establishing rapport with the senior police official and district attorney assigned to the case.10,11 Such rapport also allows the victim to learn about the laws and resources available for managing stalking risk.
A multidisciplinary team can assess and manage risk, provide education, and support victims. One well-established anti-stalking team—the San Diego Stalking Strike Force—meets monthly to evaluate cases.12 Members also are on-call for emergencies. By exchanging information monthly, the case manager and parole agent enhance stalker supervision.
In court, advocacy is critical. The consultant psychiatrist or victim advocate can educate the court that stalking is not a “lovers’ spat” (in the case of the rejected stalker) or mere nuisance behavior (in the case of other stalker types). The victim and psychiatrist may need to mobilize resources and promote collaboration among professionals in communities that do not have advocates or anti-stalking services.
Treating victims’ symptoms
As a result of the risks they face, stalking victims often suffer significant “social damage.” To cope with being stalked, many victims must make substantial life changes, such as relocating or finding new employment. They may need to restrict outings, adapt security measures, and take time off from work.16 This social damage and anxiety may predispose them to substance abuse.17
Stalking victims also experience emotional distress.3,18 They commonly report symptoms of anxiety disorders, in particular PTSD, and one-quarter experience depression and suicidal ruminations.19 Victims who perceive their stalking as severe report elevated levels of helplessness, anxiety, PTSD, and depression.20
Few studies focus on the duration of victims’ symptoms or their successful treatment.21 Mullen8 has recommended a comprehensive approach that includes education, supportive counseling, psychotherapy, and pharmacotherapy. In particular, cognitive-oriented therapy can target common issues such as anxiety leading to feelings of loss of control and associated avoidance. Pharmacotherapy for anxiety or depressive symptoms follows recommended treatment guidelines.
Because the stalking and associated stress may have an adverse impact on the victim’s personal relationships, partner and family therapy may be necessary. Support organizations for stalking victims, such as Survivors of Stalking, can provide education, safety information, and emotional support.
Improving victims’ safety
Coach a victim to take responsibility for his or her safety by becoming familiar with local stalking laws, resources, and law enforcement policies.13,22 Emphasize that a victim must be assertive to ensure that safety measures are in place (Table 3).3,8,10,15,18
As soon as unwanted pursuit is apparent, the victim should unequivocally tell the stalker that no relationship is wanted.8 This message must be firm, reasonable, and as clear as possible. The victim should not attempt to deliver the message gently or let the stalker “down easy.” Otherwise, the stalker may believe the victim is ambivalent about the decision and will continue or redouble his or her efforts.
After delivering this message, the victim should not engage in any further discussion or initiate contact with the stalker. The victim must avoid all contact to minimize the effects of “intermittent positive reinforcement.”15
The victim should document and preserve evidence by recording the dates and times of each unwanted contact, including vandalism, in an “incident log” or journal. Encourage him or her to photograph and note the date of any property damage. This documentation will help establish a clear course of illegal conduct and can prove invaluable to police and prosecution efforts.
The victim should preserve any evidence—including gifts, mementos, and other materials—by placing it in a plastic bag labeled with the date, time, and place it was received. Encourage the victim to:
- resist the urge to discard evidence that may evoke feelings of fear, shame, or disgust
- avoid handling evidence, and store it in a secure location.
- establish a post office box to prevent someone from stealing mail containing personal information
- shred personal mail instead of placing it in the trash.
It is essential for the victim to form a network of trusted social contacts who will provide a “safety net.” Informing family, friends, co-workers, and neighbors about stalking and its potentially serious consequences may reduce the risk that they might inadvertently disclose a victim’s personal information to the stalker.8 The victim can distribute a photo of the stalker to members of the safety network, as well as co-workers, with instructions to call the victim if the stalker is spotted.
Security experts often advise victims not to adhere to their usual, predictable routines by, for example, taking different daily travel routes or being prepared to go out of town at short notice.2 Victims should also make contingency plans in case their social supports are unavailable in an emergency. Victim advocacy agents can give information about services and locations of local “safe houses” or domestic violence shelters.
Table 3
Victim safety strategies
|
| Source: References 3,8,10,15,18 |
Treating stalkers
Failing to treat a mentally ill stalker may result in continued risk to the victim. For example, an intimacy-seeking stalker with erotomanic delusions who is confined without treatment likely will be released with no significant reduction in risk. No reliable outcome data exist on treatment for stalkers, however, so you must rely on empirically derived clinical data.
If you work with stalkers, you must be familiar with your state’s duty-to-protect statutes and relevant case law related to stalking so you can discuss legal obligations with the stalker before beginning treatment.
Most stalkers will be difficult to engage in treatment because they have been compelled by a court order to seek therapy. Initially you are likely to encounter the stalker’s striking lack of insight into the nature and consequences of this behavior. The stalker may seek validation for his or her actions while demonstrating little interest in ending the obsessional behavior. Expect well-entrenched defenses of denial, rationalization, and minimization.
A comprehensive description of treatment for stalkers is beyond the scope of this article. However, clinicians with experience treating stalkers recommend the following interventions:4
- thorough psychiatric assessment and diagnosis
- treatment of Axis I or II pathology
- cognitive-behavioral therapy to focus on the stalker’s misperceptions
- motivational interviewing techniques to help the stalker appreciate the need for intervention
- victim empathy development
- social skills enhancement
- periodic risk assessments.
- Stalking Resource Center, National Center for Victims of Crime. www.ncvc.org/src.
- Pinals DA, ed. Stalking: a psychiatric perspective. New York: Oxford University Press; 2007.
- The Antistalking Web Site resources. www.antistalking.com/resource.htm.
- U.S. Department of Justice anti-stalking resources. www.usdoj.gov/ovw/stalking.htm.
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Basile KC, Swahn MH, Chen J, Saltzman LE. Stalking in the United States: recent national prevalence estimates. Am J Prev Med 2006;31(2):172-5.
2. McEwan T, Mullen PE, Purcell R. Identifying risk factors in stalking: a review of current research. Int J Law Psychiatry 2007;30:1-9.
3. Spitzberg BH, Cupach WR. The state of the art of stalking: taking stock of the emerging literature. Aggression and Violent Behavior 2007;12:64-86.
4. Mullen P, Mackenzie R, Ogloff JR, et al. Assessing and managing the risks in the stalking situation. J Am Acad Psychiatry Law 2006;34:439-50.
5. Mohandie K, Meloy JR, McGowan MG, Williams J. The RECON typology of stalking: reliability and validity based upon a large sample of North American stalkers. J Forensic Sci 2006;51(1):147-55.
6. James DV, Farnham FR. Stalking and serious violence. J Am Acad Psychiatry Law 2003;31(4):432-9.
7. McFarlane J, Campbell JC, Watson K. Intimate partner stalking and femicide: urgent implications for women’s safety. Behav Sci Law 2002;20(1-2):51-68.
8. Mullen PE, Pathé M, Purcell R. Stalkers and their victims. Cambridge, UK: Cambridge University Press; 2000.
9. Binder RL. Commentary: the importance of professional judgment in evaluation of stalking and threatening situations. J Am Acad Psychiatry Law 2006;34(4):451-4.
10. White S, Cawood J. Threat management of stalking cases. In: Meloy JR, ed. The psychology of stalking: clinical and forensic perspectives. San Diego, CA: Academic Press; 1998:295-314.
11. Orion D. I know you really love me: a psychiatrist’s journal of erotomania, stalking, and obsessive love. New York: Macmillan; 1997.
12. Maxey W. The San Diego stalking strike force: a multi-disciplinary approach to assessing and managing stalking and threat cases. Journal of Threat Assessment 2002;2(1):43-53.
13. McFarlane J, Malecha A, Gist J, et al. Protection orders and intimate partner violence: an 18-month study of 150 black, Hispanic, and white women. Am J Public Health 2004;94(4):613-8.
14. Melton HC. Predicting the occurrence of stalking in relationships characterized by domestic violence. J Interpers Violence 2007;22(1):3-25.
15. Meloy JR. The clinical risk management of stalking: “someone is watching over me….” Am J Psychother 1997;51(2):174-84.
16. Purcell R, Pathé M, Mullen PE. When do repeated intrusions become stalking? J Forensic Psychiatry Psychol 2004;15(4):571-3.
17. Pathé M. Surviving stalking. Cambridge, UK: Cambridge University Press; 2002.
18. Kamphuis JH, Emmelkamp PMG. Traumatic distress among support-seeking female victims of stalking. Am J Psychiatry 2001;158:795-8.
19. Pathé M, Mullen PE. The impact of stalkers on their victims. Br J Psychiatry 1997;170:12-7.
20. Turmanis SA, Brown RI. The stalking and harassment behavior scale: measuring the incidence, nature, and severity of stalking and relational harassment and their psychological effects. Psychol Psychother 2006;79(Pt 2):183-98.
21. Ashmore R, Jones J, Jackson A, Smoyak S. A survey of mental health nurses’ experiences of stalking. J Psychiatr Ment Health Nurs 2006;13:562-9.
22. De Becker G. The gift of fear: survival signals that protect us from violence. New York: Dell Publishing; 1997.
A patient, a colleague, or perhaps you have been stalked. The chances of a woman being stalked are an estimated 1 in 14; for men, it is 1 in 50.1 Fearful stalking victims may restrict their lives, change jobs, and curtail social activities to protect themselves from unwanted attention, physical assault, or even murder. They may develop anxiety, depression, or posttraumatic stress disorder (PTSD).2,3
Historical, clinical, and behavioral factors increase a stalker’s risk for committing violence (Table 1).2-7 As a psychiatrist, you may be asked to consult with local law enforcement and stalking victims to assess and manage victims’ risk. To best protect them, be aware of:
- 5 types of stalkers and their typical response to management strategies
- legal and safety issues to consider before taking actions that might endanger stalking victims
- strategies to help victims protect themselves
- interventions for victims and stalkers.
Table 1
Factors that increase the risk of violence
| Factor type | Features |
|---|---|
| Historical | Ex-intimate partner |
| Previous violence | |
| Criminal record (especially violent crimes) | |
| Previous threats (especially specific or face-to-face) | |
| Clinical | “Rejected” or “predatory” stalker type |
| Substance use | |
| Narcissism, entitlement | |
| Personality disorder with anger or behavioral instability | |
| Depression with suicidal ideas | |
| Behavioral | Access to weapons |
| Proximity to victim | |
| Victim in a new relationship | |
| Has already taken actions on plans/threats | |
| Researching the victim | |
| Unconcerned with negative consequences | |
| Risk factors for homicide or serious physical harm: | |
| |
| Source: References 2-7 | |
Stalker types
Mullen et al8 developed a clinically oriented, validated stalker classification system to identify an individual stalker’s type, risks, and probable responses to management interventions (Table 2).
Rejected stalkers—the most common and dangerous type—pursue the victim, often a former intimate partner, after a relationship ends. They often acknowledge a complex and volatile mix of desire for reconciliation and revenge. These stalkers likely have a history of criminal assault.
Rejected stalkers appear to respond best to a combination of coordinated legal sanctions and mental health intervention. Because they are most likely to be violent, rejected stalkers need intensive probation or parole supervision.5
Intimacy-seeking stalkers want an intimate relationship with a victim they believe is their “true love” and tend to imbue their victims with special desirability, excellence, and other qualities consistent with their belief of romanticized love. Most have erotomanic delusions, and the rest have morbid infatuations with the victim. Intimacy-seeking stalkers typically are unperturbed by legal sanctions, viewing them as the price to pay for “true love.” They often require court-mandated psychiatric treatment.
Incompetent stalkers know the victim is disinterested but forge ahead in hopes that their behavior will lead to a relationship. Their stalking can be viewed as crude or “incompetent” attempts to court the victim. Incompetent stalkers often are intellectually limited; they feel entitled to a partner but because of underdeveloped social skills are unable to build upon lesser forms of social interaction. Unlike intimacy-seekers, incompetent stalkers do not endow the victim with unique qualities.
In addition to needing legal sanctions and possible mental health treatment, incompetent stalkers often require social skills training. Otherwise, they are likely to continue their pattern of stalking with other victims.
Resentful stalkers who suffer from mental illness generally require court-ordered psychiatric treatment but are difficult to engage in therapy. Legal sanctions may inflame this type of stalker.
Predatory stalkers prepare for a sexual assault. They stalk to discover the victim’s vulnerabilities and seldom give warnings, so the victim is often unaware of the danger.
Predatory stalkers frequently suffer from paraphilias and have prior convictions for sexual offenses. They must be secured in a correctional or forensic setting to address their paraphilias and propensity for violence.
Table 2
Identifying types of stalkers
| Type | Traits and behaviors |
|---|---|
| Rejected | Pursues former intimate partner |
| Desires reconciliation and/or revenge | |
| Criminal assault history | |
| Personality disorders predominate | |
| Intimacy-seeking | Desires relationship with “true love” |
| Oblivious to victim response | |
| Most have erotomanic delusions | |
| Endows victim with unique qualities | |
| Incompetent | Acknowledges victim’s disinterest |
| Hopes behavior leads to intimacy | |
| Does not endow victim with unique qualities | |
| Low IQ, socially inept, entitled | |
| Resentful | Feels persecuted and desires retribution |
| Intends to frighten or distress | |
| Specific or general grievance | |
| Paranoid diagnoses | |
| Predatory | Preparing for sexual attack |
| Stalks to study and observe | |
| Paraphilias, prior sexual offenses are common | |
| No warnings before attack | |
| Source: Reference 8 | |
Managing victims’ risk
Effectively managing a victim’s stalking risk is a dynamic process. It is critical to use professional judgment in a flexible manner and to work as a team with professionals from other agencies (Box).9-12
Intervention dilemma. Before taking any action, consider that taking direct measures against the stalker to reduce stalking may increase the risk of violence.10 A law enforcement intervention may provoke a stalker by challenging or humiliating him or her. Therefore, there is no single best approach to risk management. Consider the significance of individual-specific nuances, and solicit input from different disciplines. In some cases, no direct action may be preferable.
Protective orders. Obtaining a protective order may or may not be helpful. Most domestic violence research indicates that such orders protect abused women.13 This is important because stalking by a former intimate partner often occurs in relationships characterized by domestic violence.14 In addition to potentially preventing stalking behavior, a protective order may provide legal evidence of the course of stalking, as well as document a “fearful victim,” which is required by law to obtain a criminal conviction.
No conclusive studies have investigated the effectiveness of protective orders specifically related to stalkers, so consider the stalker’s reaction to previous orders.15 Counsel a victim who obtains a protective order against a former intimate partner to avoid developing a false sense of security. Rejected stalkers who have considerable emotional investment in the relationship may not be deterred by the threat of criminal sanctions. Furthermore, stalkers who are psychotic may misperceive and disregard criminal injunctions. In rare cases, a protective order may escalate stalking and violence.15
Dramatic moments. Advise a victim to remain vigilant during “dramatic moments” when violence risk may be especially heightened.15 These include:
- arrests
- issuance of protective orders
- court hearings
- custody hearings
- anniversary dates
- family-oriented holidays.
Encourage a victim who is especially concerned about an impending dramatic moment to prepare by:
- arranging to be out of town on that date
- notifying law enforcement and victim advocates.
A multidisciplinary approach is the most effective way to reduce stalking violence risk. In addition to mental health professionals, an effective team usually includes law enforcement and criminal justice personnel, attorneys, security specialists/private investigators, victim advocates, and the victim and his or her social network.
The victim can increase the chances that officials will view his or her case as a priority by establishing rapport with the senior police official and district attorney assigned to the case.10,11 Such rapport also allows the victim to learn about the laws and resources available for managing stalking risk.
A multidisciplinary team can assess and manage risk, provide education, and support victims. One well-established anti-stalking team—the San Diego Stalking Strike Force—meets monthly to evaluate cases.12 Members also are on-call for emergencies. By exchanging information monthly, the case manager and parole agent enhance stalker supervision.
In court, advocacy is critical. The consultant psychiatrist or victim advocate can educate the court that stalking is not a “lovers’ spat” (in the case of the rejected stalker) or mere nuisance behavior (in the case of other stalker types). The victim and psychiatrist may need to mobilize resources and promote collaboration among professionals in communities that do not have advocates or anti-stalking services.
Treating victims’ symptoms
As a result of the risks they face, stalking victims often suffer significant “social damage.” To cope with being stalked, many victims must make substantial life changes, such as relocating or finding new employment. They may need to restrict outings, adapt security measures, and take time off from work.16 This social damage and anxiety may predispose them to substance abuse.17
Stalking victims also experience emotional distress.3,18 They commonly report symptoms of anxiety disorders, in particular PTSD, and one-quarter experience depression and suicidal ruminations.19 Victims who perceive their stalking as severe report elevated levels of helplessness, anxiety, PTSD, and depression.20
Few studies focus on the duration of victims’ symptoms or their successful treatment.21 Mullen8 has recommended a comprehensive approach that includes education, supportive counseling, psychotherapy, and pharmacotherapy. In particular, cognitive-oriented therapy can target common issues such as anxiety leading to feelings of loss of control and associated avoidance. Pharmacotherapy for anxiety or depressive symptoms follows recommended treatment guidelines.
Because the stalking and associated stress may have an adverse impact on the victim’s personal relationships, partner and family therapy may be necessary. Support organizations for stalking victims, such as Survivors of Stalking, can provide education, safety information, and emotional support.
Improving victims’ safety
Coach a victim to take responsibility for his or her safety by becoming familiar with local stalking laws, resources, and law enforcement policies.13,22 Emphasize that a victim must be assertive to ensure that safety measures are in place (Table 3).3,8,10,15,18
As soon as unwanted pursuit is apparent, the victim should unequivocally tell the stalker that no relationship is wanted.8 This message must be firm, reasonable, and as clear as possible. The victim should not attempt to deliver the message gently or let the stalker “down easy.” Otherwise, the stalker may believe the victim is ambivalent about the decision and will continue or redouble his or her efforts.
After delivering this message, the victim should not engage in any further discussion or initiate contact with the stalker. The victim must avoid all contact to minimize the effects of “intermittent positive reinforcement.”15
The victim should document and preserve evidence by recording the dates and times of each unwanted contact, including vandalism, in an “incident log” or journal. Encourage him or her to photograph and note the date of any property damage. This documentation will help establish a clear course of illegal conduct and can prove invaluable to police and prosecution efforts.
The victim should preserve any evidence—including gifts, mementos, and other materials—by placing it in a plastic bag labeled with the date, time, and place it was received. Encourage the victim to:
- resist the urge to discard evidence that may evoke feelings of fear, shame, or disgust
- avoid handling evidence, and store it in a secure location.
- establish a post office box to prevent someone from stealing mail containing personal information
- shred personal mail instead of placing it in the trash.
It is essential for the victim to form a network of trusted social contacts who will provide a “safety net.” Informing family, friends, co-workers, and neighbors about stalking and its potentially serious consequences may reduce the risk that they might inadvertently disclose a victim’s personal information to the stalker.8 The victim can distribute a photo of the stalker to members of the safety network, as well as co-workers, with instructions to call the victim if the stalker is spotted.
Security experts often advise victims not to adhere to their usual, predictable routines by, for example, taking different daily travel routes or being prepared to go out of town at short notice.2 Victims should also make contingency plans in case their social supports are unavailable in an emergency. Victim advocacy agents can give information about services and locations of local “safe houses” or domestic violence shelters.
Table 3
Victim safety strategies
|
| Source: References 3,8,10,15,18 |
Treating stalkers
Failing to treat a mentally ill stalker may result in continued risk to the victim. For example, an intimacy-seeking stalker with erotomanic delusions who is confined without treatment likely will be released with no significant reduction in risk. No reliable outcome data exist on treatment for stalkers, however, so you must rely on empirically derived clinical data.
If you work with stalkers, you must be familiar with your state’s duty-to-protect statutes and relevant case law related to stalking so you can discuss legal obligations with the stalker before beginning treatment.
Most stalkers will be difficult to engage in treatment because they have been compelled by a court order to seek therapy. Initially you are likely to encounter the stalker’s striking lack of insight into the nature and consequences of this behavior. The stalker may seek validation for his or her actions while demonstrating little interest in ending the obsessional behavior. Expect well-entrenched defenses of denial, rationalization, and minimization.
A comprehensive description of treatment for stalkers is beyond the scope of this article. However, clinicians with experience treating stalkers recommend the following interventions:4
- thorough psychiatric assessment and diagnosis
- treatment of Axis I or II pathology
- cognitive-behavioral therapy to focus on the stalker’s misperceptions
- motivational interviewing techniques to help the stalker appreciate the need for intervention
- victim empathy development
- social skills enhancement
- periodic risk assessments.
- Stalking Resource Center, National Center for Victims of Crime. www.ncvc.org/src.
- Pinals DA, ed. Stalking: a psychiatric perspective. New York: Oxford University Press; 2007.
- The Antistalking Web Site resources. www.antistalking.com/resource.htm.
- U.S. Department of Justice anti-stalking resources. www.usdoj.gov/ovw/stalking.htm.
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
A patient, a colleague, or perhaps you have been stalked. The chances of a woman being stalked are an estimated 1 in 14; for men, it is 1 in 50.1 Fearful stalking victims may restrict their lives, change jobs, and curtail social activities to protect themselves from unwanted attention, physical assault, or even murder. They may develop anxiety, depression, or posttraumatic stress disorder (PTSD).2,3
Historical, clinical, and behavioral factors increase a stalker’s risk for committing violence (Table 1).2-7 As a psychiatrist, you may be asked to consult with local law enforcement and stalking victims to assess and manage victims’ risk. To best protect them, be aware of:
- 5 types of stalkers and their typical response to management strategies
- legal and safety issues to consider before taking actions that might endanger stalking victims
- strategies to help victims protect themselves
- interventions for victims and stalkers.
Table 1
Factors that increase the risk of violence
| Factor type | Features |
|---|---|
| Historical | Ex-intimate partner |
| Previous violence | |
| Criminal record (especially violent crimes) | |
| Previous threats (especially specific or face-to-face) | |
| Clinical | “Rejected” or “predatory” stalker type |
| Substance use | |
| Narcissism, entitlement | |
| Personality disorder with anger or behavioral instability | |
| Depression with suicidal ideas | |
| Behavioral | Access to weapons |
| Proximity to victim | |
| Victim in a new relationship | |
| Has already taken actions on plans/threats | |
| Researching the victim | |
| Unconcerned with negative consequences | |
| Risk factors for homicide or serious physical harm: | |
| |
| Source: References 2-7 | |
Stalker types
Mullen et al8 developed a clinically oriented, validated stalker classification system to identify an individual stalker’s type, risks, and probable responses to management interventions (Table 2).
Rejected stalkers—the most common and dangerous type—pursue the victim, often a former intimate partner, after a relationship ends. They often acknowledge a complex and volatile mix of desire for reconciliation and revenge. These stalkers likely have a history of criminal assault.
Rejected stalkers appear to respond best to a combination of coordinated legal sanctions and mental health intervention. Because they are most likely to be violent, rejected stalkers need intensive probation or parole supervision.5
Intimacy-seeking stalkers want an intimate relationship with a victim they believe is their “true love” and tend to imbue their victims with special desirability, excellence, and other qualities consistent with their belief of romanticized love. Most have erotomanic delusions, and the rest have morbid infatuations with the victim. Intimacy-seeking stalkers typically are unperturbed by legal sanctions, viewing them as the price to pay for “true love.” They often require court-mandated psychiatric treatment.
Incompetent stalkers know the victim is disinterested but forge ahead in hopes that their behavior will lead to a relationship. Their stalking can be viewed as crude or “incompetent” attempts to court the victim. Incompetent stalkers often are intellectually limited; they feel entitled to a partner but because of underdeveloped social skills are unable to build upon lesser forms of social interaction. Unlike intimacy-seekers, incompetent stalkers do not endow the victim with unique qualities.
In addition to needing legal sanctions and possible mental health treatment, incompetent stalkers often require social skills training. Otherwise, they are likely to continue their pattern of stalking with other victims.
Resentful stalkers who suffer from mental illness generally require court-ordered psychiatric treatment but are difficult to engage in therapy. Legal sanctions may inflame this type of stalker.
Predatory stalkers prepare for a sexual assault. They stalk to discover the victim’s vulnerabilities and seldom give warnings, so the victim is often unaware of the danger.
Predatory stalkers frequently suffer from paraphilias and have prior convictions for sexual offenses. They must be secured in a correctional or forensic setting to address their paraphilias and propensity for violence.
Table 2
Identifying types of stalkers
| Type | Traits and behaviors |
|---|---|
| Rejected | Pursues former intimate partner |
| Desires reconciliation and/or revenge | |
| Criminal assault history | |
| Personality disorders predominate | |
| Intimacy-seeking | Desires relationship with “true love” |
| Oblivious to victim response | |
| Most have erotomanic delusions | |
| Endows victim with unique qualities | |
| Incompetent | Acknowledges victim’s disinterest |
| Hopes behavior leads to intimacy | |
| Does not endow victim with unique qualities | |
| Low IQ, socially inept, entitled | |
| Resentful | Feels persecuted and desires retribution |
| Intends to frighten or distress | |
| Specific or general grievance | |
| Paranoid diagnoses | |
| Predatory | Preparing for sexual attack |
| Stalks to study and observe | |
| Paraphilias, prior sexual offenses are common | |
| No warnings before attack | |
| Source: Reference 8 | |
Managing victims’ risk
Effectively managing a victim’s stalking risk is a dynamic process. It is critical to use professional judgment in a flexible manner and to work as a team with professionals from other agencies (Box).9-12
Intervention dilemma. Before taking any action, consider that taking direct measures against the stalker to reduce stalking may increase the risk of violence.10 A law enforcement intervention may provoke a stalker by challenging or humiliating him or her. Therefore, there is no single best approach to risk management. Consider the significance of individual-specific nuances, and solicit input from different disciplines. In some cases, no direct action may be preferable.
Protective orders. Obtaining a protective order may or may not be helpful. Most domestic violence research indicates that such orders protect abused women.13 This is important because stalking by a former intimate partner often occurs in relationships characterized by domestic violence.14 In addition to potentially preventing stalking behavior, a protective order may provide legal evidence of the course of stalking, as well as document a “fearful victim,” which is required by law to obtain a criminal conviction.
No conclusive studies have investigated the effectiveness of protective orders specifically related to stalkers, so consider the stalker’s reaction to previous orders.15 Counsel a victim who obtains a protective order against a former intimate partner to avoid developing a false sense of security. Rejected stalkers who have considerable emotional investment in the relationship may not be deterred by the threat of criminal sanctions. Furthermore, stalkers who are psychotic may misperceive and disregard criminal injunctions. In rare cases, a protective order may escalate stalking and violence.15
Dramatic moments. Advise a victim to remain vigilant during “dramatic moments” when violence risk may be especially heightened.15 These include:
- arrests
- issuance of protective orders
- court hearings
- custody hearings
- anniversary dates
- family-oriented holidays.
Encourage a victim who is especially concerned about an impending dramatic moment to prepare by:
- arranging to be out of town on that date
- notifying law enforcement and victim advocates.
A multidisciplinary approach is the most effective way to reduce stalking violence risk. In addition to mental health professionals, an effective team usually includes law enforcement and criminal justice personnel, attorneys, security specialists/private investigators, victim advocates, and the victim and his or her social network.
The victim can increase the chances that officials will view his or her case as a priority by establishing rapport with the senior police official and district attorney assigned to the case.10,11 Such rapport also allows the victim to learn about the laws and resources available for managing stalking risk.
A multidisciplinary team can assess and manage risk, provide education, and support victims. One well-established anti-stalking team—the San Diego Stalking Strike Force—meets monthly to evaluate cases.12 Members also are on-call for emergencies. By exchanging information monthly, the case manager and parole agent enhance stalker supervision.
In court, advocacy is critical. The consultant psychiatrist or victim advocate can educate the court that stalking is not a “lovers’ spat” (in the case of the rejected stalker) or mere nuisance behavior (in the case of other stalker types). The victim and psychiatrist may need to mobilize resources and promote collaboration among professionals in communities that do not have advocates or anti-stalking services.
Treating victims’ symptoms
As a result of the risks they face, stalking victims often suffer significant “social damage.” To cope with being stalked, many victims must make substantial life changes, such as relocating or finding new employment. They may need to restrict outings, adapt security measures, and take time off from work.16 This social damage and anxiety may predispose them to substance abuse.17
Stalking victims also experience emotional distress.3,18 They commonly report symptoms of anxiety disorders, in particular PTSD, and one-quarter experience depression and suicidal ruminations.19 Victims who perceive their stalking as severe report elevated levels of helplessness, anxiety, PTSD, and depression.20
Few studies focus on the duration of victims’ symptoms or their successful treatment.21 Mullen8 has recommended a comprehensive approach that includes education, supportive counseling, psychotherapy, and pharmacotherapy. In particular, cognitive-oriented therapy can target common issues such as anxiety leading to feelings of loss of control and associated avoidance. Pharmacotherapy for anxiety or depressive symptoms follows recommended treatment guidelines.
Because the stalking and associated stress may have an adverse impact on the victim’s personal relationships, partner and family therapy may be necessary. Support organizations for stalking victims, such as Survivors of Stalking, can provide education, safety information, and emotional support.
Improving victims’ safety
Coach a victim to take responsibility for his or her safety by becoming familiar with local stalking laws, resources, and law enforcement policies.13,22 Emphasize that a victim must be assertive to ensure that safety measures are in place (Table 3).3,8,10,15,18
As soon as unwanted pursuit is apparent, the victim should unequivocally tell the stalker that no relationship is wanted.8 This message must be firm, reasonable, and as clear as possible. The victim should not attempt to deliver the message gently or let the stalker “down easy.” Otherwise, the stalker may believe the victim is ambivalent about the decision and will continue or redouble his or her efforts.
After delivering this message, the victim should not engage in any further discussion or initiate contact with the stalker. The victim must avoid all contact to minimize the effects of “intermittent positive reinforcement.”15
The victim should document and preserve evidence by recording the dates and times of each unwanted contact, including vandalism, in an “incident log” or journal. Encourage him or her to photograph and note the date of any property damage. This documentation will help establish a clear course of illegal conduct and can prove invaluable to police and prosecution efforts.
The victim should preserve any evidence—including gifts, mementos, and other materials—by placing it in a plastic bag labeled with the date, time, and place it was received. Encourage the victim to:
- resist the urge to discard evidence that may evoke feelings of fear, shame, or disgust
- avoid handling evidence, and store it in a secure location.
- establish a post office box to prevent someone from stealing mail containing personal information
- shred personal mail instead of placing it in the trash.
It is essential for the victim to form a network of trusted social contacts who will provide a “safety net.” Informing family, friends, co-workers, and neighbors about stalking and its potentially serious consequences may reduce the risk that they might inadvertently disclose a victim’s personal information to the stalker.8 The victim can distribute a photo of the stalker to members of the safety network, as well as co-workers, with instructions to call the victim if the stalker is spotted.
Security experts often advise victims not to adhere to their usual, predictable routines by, for example, taking different daily travel routes or being prepared to go out of town at short notice.2 Victims should also make contingency plans in case their social supports are unavailable in an emergency. Victim advocacy agents can give information about services and locations of local “safe houses” or domestic violence shelters.
Table 3
Victim safety strategies
|
| Source: References 3,8,10,15,18 |
Treating stalkers
Failing to treat a mentally ill stalker may result in continued risk to the victim. For example, an intimacy-seeking stalker with erotomanic delusions who is confined without treatment likely will be released with no significant reduction in risk. No reliable outcome data exist on treatment for stalkers, however, so you must rely on empirically derived clinical data.
If you work with stalkers, you must be familiar with your state’s duty-to-protect statutes and relevant case law related to stalking so you can discuss legal obligations with the stalker before beginning treatment.
Most stalkers will be difficult to engage in treatment because they have been compelled by a court order to seek therapy. Initially you are likely to encounter the stalker’s striking lack of insight into the nature and consequences of this behavior. The stalker may seek validation for his or her actions while demonstrating little interest in ending the obsessional behavior. Expect well-entrenched defenses of denial, rationalization, and minimization.
A comprehensive description of treatment for stalkers is beyond the scope of this article. However, clinicians with experience treating stalkers recommend the following interventions:4
- thorough psychiatric assessment and diagnosis
- treatment of Axis I or II pathology
- cognitive-behavioral therapy to focus on the stalker’s misperceptions
- motivational interviewing techniques to help the stalker appreciate the need for intervention
- victim empathy development
- social skills enhancement
- periodic risk assessments.
- Stalking Resource Center, National Center for Victims of Crime. www.ncvc.org/src.
- Pinals DA, ed. Stalking: a psychiatric perspective. New York: Oxford University Press; 2007.
- The Antistalking Web Site resources. www.antistalking.com/resource.htm.
- U.S. Department of Justice anti-stalking resources. www.usdoj.gov/ovw/stalking.htm.
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Basile KC, Swahn MH, Chen J, Saltzman LE. Stalking in the United States: recent national prevalence estimates. Am J Prev Med 2006;31(2):172-5.
2. McEwan T, Mullen PE, Purcell R. Identifying risk factors in stalking: a review of current research. Int J Law Psychiatry 2007;30:1-9.
3. Spitzberg BH, Cupach WR. The state of the art of stalking: taking stock of the emerging literature. Aggression and Violent Behavior 2007;12:64-86.
4. Mullen P, Mackenzie R, Ogloff JR, et al. Assessing and managing the risks in the stalking situation. J Am Acad Psychiatry Law 2006;34:439-50.
5. Mohandie K, Meloy JR, McGowan MG, Williams J. The RECON typology of stalking: reliability and validity based upon a large sample of North American stalkers. J Forensic Sci 2006;51(1):147-55.
6. James DV, Farnham FR. Stalking and serious violence. J Am Acad Psychiatry Law 2003;31(4):432-9.
7. McFarlane J, Campbell JC, Watson K. Intimate partner stalking and femicide: urgent implications for women’s safety. Behav Sci Law 2002;20(1-2):51-68.
8. Mullen PE, Pathé M, Purcell R. Stalkers and their victims. Cambridge, UK: Cambridge University Press; 2000.
9. Binder RL. Commentary: the importance of professional judgment in evaluation of stalking and threatening situations. J Am Acad Psychiatry Law 2006;34(4):451-4.
10. White S, Cawood J. Threat management of stalking cases. In: Meloy JR, ed. The psychology of stalking: clinical and forensic perspectives. San Diego, CA: Academic Press; 1998:295-314.
11. Orion D. I know you really love me: a psychiatrist’s journal of erotomania, stalking, and obsessive love. New York: Macmillan; 1997.
12. Maxey W. The San Diego stalking strike force: a multi-disciplinary approach to assessing and managing stalking and threat cases. Journal of Threat Assessment 2002;2(1):43-53.
13. McFarlane J, Malecha A, Gist J, et al. Protection orders and intimate partner violence: an 18-month study of 150 black, Hispanic, and white women. Am J Public Health 2004;94(4):613-8.
14. Melton HC. Predicting the occurrence of stalking in relationships characterized by domestic violence. J Interpers Violence 2007;22(1):3-25.
15. Meloy JR. The clinical risk management of stalking: “someone is watching over me….” Am J Psychother 1997;51(2):174-84.
16. Purcell R, Pathé M, Mullen PE. When do repeated intrusions become stalking? J Forensic Psychiatry Psychol 2004;15(4):571-3.
17. Pathé M. Surviving stalking. Cambridge, UK: Cambridge University Press; 2002.
18. Kamphuis JH, Emmelkamp PMG. Traumatic distress among support-seeking female victims of stalking. Am J Psychiatry 2001;158:795-8.
19. Pathé M, Mullen PE. The impact of stalkers on their victims. Br J Psychiatry 1997;170:12-7.
20. Turmanis SA, Brown RI. The stalking and harassment behavior scale: measuring the incidence, nature, and severity of stalking and relational harassment and their psychological effects. Psychol Psychother 2006;79(Pt 2):183-98.
21. Ashmore R, Jones J, Jackson A, Smoyak S. A survey of mental health nurses’ experiences of stalking. J Psychiatr Ment Health Nurs 2006;13:562-9.
22. De Becker G. The gift of fear: survival signals that protect us from violence. New York: Dell Publishing; 1997.
1. Basile KC, Swahn MH, Chen J, Saltzman LE. Stalking in the United States: recent national prevalence estimates. Am J Prev Med 2006;31(2):172-5.
2. McEwan T, Mullen PE, Purcell R. Identifying risk factors in stalking: a review of current research. Int J Law Psychiatry 2007;30:1-9.
3. Spitzberg BH, Cupach WR. The state of the art of stalking: taking stock of the emerging literature. Aggression and Violent Behavior 2007;12:64-86.
4. Mullen P, Mackenzie R, Ogloff JR, et al. Assessing and managing the risks in the stalking situation. J Am Acad Psychiatry Law 2006;34:439-50.
5. Mohandie K, Meloy JR, McGowan MG, Williams J. The RECON typology of stalking: reliability and validity based upon a large sample of North American stalkers. J Forensic Sci 2006;51(1):147-55.
6. James DV, Farnham FR. Stalking and serious violence. J Am Acad Psychiatry Law 2003;31(4):432-9.
7. McFarlane J, Campbell JC, Watson K. Intimate partner stalking and femicide: urgent implications for women’s safety. Behav Sci Law 2002;20(1-2):51-68.
8. Mullen PE, Pathé M, Purcell R. Stalkers and their victims. Cambridge, UK: Cambridge University Press; 2000.
9. Binder RL. Commentary: the importance of professional judgment in evaluation of stalking and threatening situations. J Am Acad Psychiatry Law 2006;34(4):451-4.
10. White S, Cawood J. Threat management of stalking cases. In: Meloy JR, ed. The psychology of stalking: clinical and forensic perspectives. San Diego, CA: Academic Press; 1998:295-314.
11. Orion D. I know you really love me: a psychiatrist’s journal of erotomania, stalking, and obsessive love. New York: Macmillan; 1997.
12. Maxey W. The San Diego stalking strike force: a multi-disciplinary approach to assessing and managing stalking and threat cases. Journal of Threat Assessment 2002;2(1):43-53.
13. McFarlane J, Malecha A, Gist J, et al. Protection orders and intimate partner violence: an 18-month study of 150 black, Hispanic, and white women. Am J Public Health 2004;94(4):613-8.
14. Melton HC. Predicting the occurrence of stalking in relationships characterized by domestic violence. J Interpers Violence 2007;22(1):3-25.
15. Meloy JR. The clinical risk management of stalking: “someone is watching over me….” Am J Psychother 1997;51(2):174-84.
16. Purcell R, Pathé M, Mullen PE. When do repeated intrusions become stalking? J Forensic Psychiatry Psychol 2004;15(4):571-3.
17. Pathé M. Surviving stalking. Cambridge, UK: Cambridge University Press; 2002.
18. Kamphuis JH, Emmelkamp PMG. Traumatic distress among support-seeking female victims of stalking. Am J Psychiatry 2001;158:795-8.
19. Pathé M, Mullen PE. The impact of stalkers on their victims. Br J Psychiatry 1997;170:12-7.
20. Turmanis SA, Brown RI. The stalking and harassment behavior scale: measuring the incidence, nature, and severity of stalking and relational harassment and their psychological effects. Psychol Psychother 2006;79(Pt 2):183-98.
21. Ashmore R, Jones J, Jackson A, Smoyak S. A survey of mental health nurses’ experiences of stalking. J Psychiatr Ment Health Nurs 2006;13:562-9.
22. De Becker G. The gift of fear: survival signals that protect us from violence. New York: Dell Publishing; 1997.
Faking it: How to detect malingered psychosis
Reputed Cosa Nostra boss Vincent “The Chin” Gigante deceived “the most respected minds in forensic psychiatry” for years by malingering schizophrenia.1 Ultimately, he admitted to maintaining his charade from 1990 to 1997 during evaluations of his competency to stand trial for racketeering.
A lesson from this case—said a psychiatrist who concluded Gigante was malingering—is, “When feigning is a consideration, we must be more critical and less accepting of our impressions when we conduct and interpret a psychiatric examination…than might be the case in a typical clinical situation.”2
Even in typical clinical situations, however, psychiatrists may be reluctant to diagnose malingering3 for fear of being sued, assaulted—or wrong. An inaccurate diagnosis of malingering may unjustly stigmatize a patient and deny him needed care.4
Because psychiatrists need a systematized approach to detect malingering,5 we offer specific clinical factors and approaches to help you recognize malingered psychosis.
What is Malingering?
No other syndrome is as easy to define yet so difficult to diagnose as malingering. Reliably diagnosing malingered mental illness is complex, requiring the psychiatrist to consider collateral data beyond the patient interview.
Malingering is the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives.6 In practice, malingering commonly must be differentiated from factitious disorder, which also involves intentional production of symptoms. In factitious disorders, the patient’s motivation is to assume the sick role, which can be thought of as an internal or psychological incentive.
Three categories of malingering include:
- pure malingering (feigning a nonexistent disorder)
- partial malingering (consciously exaggerating real symptoms)
- false imputation (ascribing real symptoms to a cause the individual knows is unrelated to the symptoms).7
Motivations. Individuals usually malinger to avoid pain (such as difficult situations or punishment) or to seek pleasure (such as to obtain compensation or medications) (Table 1). In correctional settings, for example, inmates may malinger mental illness to do “easier time” or to obtain drugs. On the other hand, malingering in prison also may be an adaptive response by a mentally ill inmate to relatively sparse and difficult-to-obtain mental health resources.8
Table 1
Common motives of malingerers
| Motives | Examples |
|---|---|
| To avoid pain | To avoid: |
| Arrest | |
| Criminal prosecution | |
| Conscription into the military | |
| To seek pleasure | To obtain: |
| Controlled substances | |
| Free room and board | |
| Workers’ compensation or disability benefits for alleged psychological injury |
Interview Style
When you suspect a patient is malingering, keep your suspicions to yourself and conduct an objective evaluation. Patients are likely to become defensive if you show annoyance or incredulity, and putting them on guard decreases your ability to uncover evidence of malingering.9
Begin by asking open-ended questions, which allow patients to report symptoms in their own words. To avoid hinting at correct responses, carefully phrase initial inquiries about symptoms. Later in the interview, you can proceed to more-detailed questions of specific symptoms, as discussed below.
If possible, review collateral data before the interview, when it is most helpful. Consider information that would support or refute the alleged symptoms, such as treatment and insurance records, police reports, and interviews of close friends or family.
The patient interview may be prolonged because fatigue may diminish a malingerer’s ability to maintain fake symptoms. In very difficult cases, consider monitoring during inpatient assessment because feigned psychosis is extremely difficult to maintain 24 hours a day.
Watch for individuals who endorse rare or improbable symptoms. Rare symptoms—by definition—occur very infrequently, and even severely disturbed patients almost never report improbable symptoms.10 Consider asking malingerers about improbable symptoms to see if they will endorse them. For example:
- “When people talk to you, do you see the words they speak spelled out?”11
- “Have you ever believed that automobiles are members of an organized religion?”12
Watch closely for internal or external inconsistency in the suspected malingerer’s presentation (Table 2).
Table 2
Clues to identify malingering during patient evaluation
| Internal inconsistencies | Example |
| In subject’s report of symptoms | Gives a clear and articulate explanation of being confused |
| In subject’s own reported history | Gives conflicting versions |
| External inconsistencies | Example |
| Between reported and observed symptoms | Alleges having active auditory and visual hallucinations yet shows no evidence of being distracted |
| Between reported and observed level of functioning | Behaves in disorganized or confused manner around psychiatrist, yet plays excellent chess on ward with other patients |
| Between reported symptoms and nature of genuine symptoms | Reports seeing visual hallucinations in black and white, whereas genuine visual hallucinations are seen in color |
| Between reported symptoms and psychological test results | Alleges genuine psychotic symptoms, yet testing suggests faking or exaggeration |
Malingered Psychotic Symptoms
Detecting malingered mental illness is considered an advanced psychiatric skill, partly because you must understand thoroughly how genuine psychotic symptoms manifest.
Hallucinations. If a patient alleges atypical hallucinations, ask about them in detail. Hallucinations are usually (88%) associated with delusions.13 Genuine hallucinations are typically intermittent rather than continuous.
Continue to: Auditory hallucinations
Auditory hallucinations are usually clear, not vague (7%) or inaudible. Both male and female voices are commonly heard (75%), and voices are usually perceived as originating outside the head (88%).14 In schizophrenia, the major themes are persecutory or instructive.15
Command auditory hallucinations are easy to fabricate. Persons experiencing genuine command hallucinations:
- do not always obey the voices, especially if doing so would be dangerous16
- usually present with noncommand hallucinations (85%) and delusions (75%) as well17
Thus, view with suspicion someone who alleges an isolated command hallucination without other psychotic symptoms.
Genuine schizophrenic hallucinations tend to diminish when patients are involved in activities. Thus, to deal with their hallucinations, persons with schizophrenia typically cope by:
- engaging in activities (working, listening to a radio, watching TV)
- changing posture (lying down, walking)
- seeking interpersonal contact
- taking medications.
If you suspect a person of malingered auditory hallucinations, ask what he or she does to make the voices go away or diminish in intensity. Patients with genuine schizophrenia often can stop their auditory hallucinations while in remission but not during acute illness.
Malingerers may report auditory hallucinations of stilted or implausible language. For example, we have evaluated:
- an individual charged with attempted rape who alleged that voices said, “Go commit a sex offense.”
- a bank robber who alleged that voices kept screaming, “Stick up, stick up, stick up!”
Both examples contain language that is very questionable for genuine hallucinations, while providing the patient with “psychotic justification” for an illegal act that has a rational alternative motive.
Visual hallucinations are experienced by an estimated 24% to 30% of psychotic individuals but are reported much more often by malingerers (46%) than by persons with genuine psychosis (4%).18
Genuine visual hallucinations are usually of normalsized people and are seen in color.14 On rare occasions, genuine visual hallucinations of small people (Lilliputian hallucinations) may be associated with alcohol use, organic disease, or toxic psychosis (such as anticholinergic toxicity) but are rarely seen by persons with schizophrenia.
Psychotic visual hallucinations do not typically change if the eyes are closed or open, whereas drug-induced hallucinations are more readily seen with eyes closed or in the dark. Unformed hallucinations—such as flashes of light, shadows, or moving objects—are typically associated with neurologic disease and substance use.19
Suspect malingering if the patient reports dramatic or atypical visual hallucinations. For example, one defendant charged with bank robbery calmly reported seeing “a 30-foot tall, red giant smashing down the walls” of the interview room. When he was asked detailed questions, he frequently replied, “I don’t know.” He eventually admitted to malingering.
Delusions. Genuine delusions vary in content, theme, degree of systemization, and relevance to the person’s life. The complexity and sophistication of delusional systems usually reflect the individual’s intelligence. Persecutory delusions are more likely to be acted upon than are other types of delusions.20
Malingerers may claim that a delusion began or disappeared suddenly. In reality, systematized delusions usually take weeks to develop and much longer to disappear. Typically, the delusion will become somewhat less relevant, and the individual will gradually relinquish its importance over time after adequate treatment. In general, the more bizarre the delusion’s content, the more disorganized the individual’s thinking is likely to be (Table 3).
With genuine delusions, the individual’s behavior usually conforms to the delusions’ content. For example, Russell Weston—who suffered from schizophrenia—made a deadly assault on the U.S. Capitol in 1998 because he held a delusional belief that cannibalism was destroying Washington, DC. Before he shot and killed two U.S. Capitol security officers, he had gone to the Central Intelligence Agency several years before and voiced the same delusional concerns.
Suspect malingering if a patient alleges persecutory delusions without engaging in corresponding paranoid behaviors. One exception is the person with long-standing schizophrenia who has grown accustomed to the delusion and whose behavior is no longer consistent with it.
Table 3
Uncommon psychosis presentations that suggest malingering
| Hallucinations |
|
| Delusions |
|
Where Malingerers Trip Up
Malingerers may have inadequate or incomplete knowledge of the mental illness they are faking. Indeed, malingerers are like actors who can portray a role only as well as they understand it. They often overact their part or mistakenly believe the more bizarre their behavior, the more convincing they will be. Conversely, “successful” malingerers are more likely to endorse fewer symptoms and avoid endorsing overly bizarre or unusual symptoms.21
Continue to: Numerous clinical factors suggest malingering...
Numerous clinical factors suggest malingering (Table 4). Malingerers are more likely to eagerly “thrust forward” their illness, whereas patients with genuine schizophrenia are often reluctant to discuss their symptoms.22
Malingerers may attempt to take control of the interview and behave in an intimidating or hostile manner. They may accuse the psychiatrist of inferring that they are faking. Such behavior is rare in genuinely psychotic individuals. Although DSM-IV-TR states that antisocial personality disorder should arouse suspicions of malingering, some studies have failed to show a relationship. One study has associated psychopathic traits with malingering.23
Malingerers often believe that faking intellectual deficits, in addition to psychotic symptoms, will make them more believable. For example, a man who had completed several years of college alleged that he did not know the colors of the American flag.
Malingerers are more likely to give vague or hedging answers to straightforward questions. For example, when asked whether an alleged voice was male or female, one malingerer replied, “It was probably a man’s voice.” Malingerers may also answer, “I don’t know” to detailed questions about psychotic symptoms. Whereas a person with genuine psychotic symptoms could easily give an answer, the malingerer may have never experienced the symptoms and consequently “doesn’t know” the correct answer.
Psychotic symptoms such as derailment, neologisms, loose associations, and word salad are rarely simulated. This is because it is much more difficult for a malingerer to successfully imitate psychotic thought processes than psychotic thought content. Similarly, it is unusual for a malingerer to fake schizophrenia’s subtle signs, such as negative symptoms.
Table 4
Clinical factors that suggest malingering
| Absence of active or subtle signs of psychosis |
| Marked inconsistencies, contradictions |
Patient endorses improbable psychiatric symptoms
|
Patient is evasive or uncooperative
|
| Psychological testing indicates malingering (SIRS, M-FAST, MMPI-2) |
| SIRS: Structured Interview of Reported Symptoms |
| M-FAST: Miller Forensic Assessment of Symptoms Test |
| MMPI-2: Minnesota Multiphasic Personality Inventory, Revised |
Psychological Testing
Although many psychometric tests are available for detecting malingered psychosis, few have been validated. Among the more reliable are:
- Structured Interview of Reported Symptoms (SIRS)
- Minnesota Multiphasic Personality Inventory, Revised (MMPI-2)
- Miller Forensic Assessment of Symptoms Test (M-FAST).11
SIRS includes questions about rare symptoms, uncommon symptom pairing, atypical symptoms, and other indices involving excessive symptom reporting. It takes 30 to 60 minutes to administer. Tested in inpatient, forensic, and correctional populations, the SIRS has shown consistently high accuracy in detecting malingered psychiatric illness.24
Two MMPI-2 scales—F-scale and F-K Index—are the most frequently used test for evaluating suspected malingering. When using the MMPI-2 in this manner, consult the literature for appropriate cutoff scores (see Related resources). Although the MMPI-2 is the most validated psychometric method to detect malingering, a malingerer with high intelligence and previous knowledge of the test could evade detection.25
M-FAST was developed to provide a brief, reliable screen for malingered mental illness. This test takes 10 to 15 minutes to administer and measures rare symptom combinations, excessive reporting, and atypical symptoms.11 It has shown good validity and high correlation with the SIRS and MMPI-2.26,27
Confronting the Malingerer
If a thorough investigation indicates that a patient is malingering psychosis, you may decide to confront the evaluee. Avoid direct accusations of lying,10 and give the suspected malingerer every opportunity to save face. For example, it is preferable to say, “You haven’t told me the whole truth.”
A thoughtful approach that asks the evaluee to clarify inconsistencies is more likely to be productive and safer for the examiner. When confronting individuals with a history of violence and aggression, have adequate security personnel with you.
- Structured Interview of Reported Symptoms (SIRS). Available for purchase from Psychological Assessment Resources at www3.parinc.com (enter “SIRS” in search field).
- Graham JR. MMPI-2: Assessing personality and psychopathology. New York: Oxford Press; 2000. (Source of cutoff scores to use MMPI-2 scales [F-scale and F-K Index] to evaluate suspected malingering).
- Psychological Assessment Resources, Inc. Miller Forensic Assessment of Symptoms Test (M-FAST). Available at: www3.parinc.com (enter “M-FAST” in search field).
1. Newman A. Analyze this: Vincent Gigante, not crazy after all those years. New York Times, April 13, 2003.
2. Brodie JD. Personal communication, 2005.
3. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv 1996;47:998-1000.
4. Kropp PR, Rogers R. Understanding malingering: motivation, method, and detection. In: Lewis M, Saarini C (eds). Lying and deception. New York: Guilford Press; 1993.
5. Kucharski LT, et al. Clinical symptom presentation in suspected malingerers: an empirical investigation. Bull Am Acad Psychiatry Law. 1998;26:579-85.
6. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American Psychiatric Association; 2000.
7. Resnick PJ. Malingering of posttraumatic stress disorders. In: Rogers R (ed). Clinical assessment of malingering and deception (2nd ed.). New York: Guilford Press; 1997;130-52.
8. Kupers TA. Malingering in correctional settings. Correctional Ment Health Rep. 2004;5(6):81-95.
9. Sadock BJ, Sadock VA. Kaplan & Sadock’s synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003;898.-
10. Thompson JW, LeBourgeois HW, Black FW. Malingering. In: Simon R, Gold L (eds). Textbook of forensic psychiatry. Washington, DC: American Psychiatric Publishing; 2004.
11. Miller HA. M.-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
12. Rogers R. Assessment of malingering within a forensic context. In Weisstub DW (ed.). Law and psychiatry: international perspectives. New York: Plenum Press; 1987;3:209-37.
13. Lewinsohn PM. An empirical test of several popular notions about hallucinations in schizophrenic patients. In: Keup W (ed.). Origin and mechanisms of hallucinations. New York: Plenum Press; 1970;401-3.
14. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry 1971;24:76-80.
15. Small IF, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Sys 1966;27:349-53.
16. Kasper ME, Rogers R, Adams PA. Dangerousness and command hallucinations: an investigation of psychotic inpatients. Bull Am Acad Psychiatry Law 1996;24:219-24.
17. Thompson JS, Stuart GL, Holden CE. Command hallucinations and legal insanity. Forensic Rep 1992;5:29-43.
18. Cornell DG, Hawk GL. Clinical presentation of malingerers diagnosed by experienced forensic psychologists. Law Hum Behav 1989;13:375-83.
19. Cummings JL, Miller BL. Visual hallucinations: clinical occurrence and use in differential diagnosis. West J Med 1987;146:46-51.
20. Wessely S, Buchanan A, Reed A, et al. Acting on delusions: I. Prevalence. Br J Psychiatry 1993;163:69-76.
21. Edens JF, Guy LS, Otto RK, et al. Factors differentiating successful versus unsuccessful malingerers. J Pers Assess 2001;77(2):333-8.
22. Ritson B, Forest A. The simulation of psychosis: a contemporary presentation. Br J Psychol 1970;43:31-7.
23. Edens JF, Buffington JK, Tomicic TL. An investigation of the relationship between psychopathic traits and malingering on the Psychopathic Personality Inventory. Assessment 2000;7:281-96.
24. Rogers R. Structured interviews and dissimulation. In: Rogers R (ed). Clinical assessment of malingering and deception. New York: Guilford Press; 1997.
25. Pelfrey WV. The relationship between malingerers’ intelligence and MMPI-2 knowledge and their ability to avoid detection. Int J Offender Ther Comp Criminol. 2004;48(6):649-63.
26. Jackson RL, Rogers R, Sewell KW. Forensic applications of the Miller Forensic Assessment of Symptoms Test (MFAST): screening for feigned disorders in competency to stand trial evaluations. Law Human Behav 2005;29(2):199-210.
27. Miller HA. Examining the use of the M-FAST with criminal defendants incompetent to stand trial. Int J Offender Ther Comp Criminol 2004;48(3):268-80.
Reputed Cosa Nostra boss Vincent “The Chin” Gigante deceived “the most respected minds in forensic psychiatry” for years by malingering schizophrenia.1 Ultimately, he admitted to maintaining his charade from 1990 to 1997 during evaluations of his competency to stand trial for racketeering.
A lesson from this case—said a psychiatrist who concluded Gigante was malingering—is, “When feigning is a consideration, we must be more critical and less accepting of our impressions when we conduct and interpret a psychiatric examination…than might be the case in a typical clinical situation.”2
Even in typical clinical situations, however, psychiatrists may be reluctant to diagnose malingering3 for fear of being sued, assaulted—or wrong. An inaccurate diagnosis of malingering may unjustly stigmatize a patient and deny him needed care.4
Because psychiatrists need a systematized approach to detect malingering,5 we offer specific clinical factors and approaches to help you recognize malingered psychosis.
What is Malingering?
No other syndrome is as easy to define yet so difficult to diagnose as malingering. Reliably diagnosing malingered mental illness is complex, requiring the psychiatrist to consider collateral data beyond the patient interview.
Malingering is the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives.6 In practice, malingering commonly must be differentiated from factitious disorder, which also involves intentional production of symptoms. In factitious disorders, the patient’s motivation is to assume the sick role, which can be thought of as an internal or psychological incentive.
Three categories of malingering include:
- pure malingering (feigning a nonexistent disorder)
- partial malingering (consciously exaggerating real symptoms)
- false imputation (ascribing real symptoms to a cause the individual knows is unrelated to the symptoms).7
Motivations. Individuals usually malinger to avoid pain (such as difficult situations or punishment) or to seek pleasure (such as to obtain compensation or medications) (Table 1). In correctional settings, for example, inmates may malinger mental illness to do “easier time” or to obtain drugs. On the other hand, malingering in prison also may be an adaptive response by a mentally ill inmate to relatively sparse and difficult-to-obtain mental health resources.8
Table 1
Common motives of malingerers
| Motives | Examples |
|---|---|
| To avoid pain | To avoid: |
| Arrest | |
| Criminal prosecution | |
| Conscription into the military | |
| To seek pleasure | To obtain: |
| Controlled substances | |
| Free room and board | |
| Workers’ compensation or disability benefits for alleged psychological injury |
Interview Style
When you suspect a patient is malingering, keep your suspicions to yourself and conduct an objective evaluation. Patients are likely to become defensive if you show annoyance or incredulity, and putting them on guard decreases your ability to uncover evidence of malingering.9
Begin by asking open-ended questions, which allow patients to report symptoms in their own words. To avoid hinting at correct responses, carefully phrase initial inquiries about symptoms. Later in the interview, you can proceed to more-detailed questions of specific symptoms, as discussed below.
If possible, review collateral data before the interview, when it is most helpful. Consider information that would support or refute the alleged symptoms, such as treatment and insurance records, police reports, and interviews of close friends or family.
The patient interview may be prolonged because fatigue may diminish a malingerer’s ability to maintain fake symptoms. In very difficult cases, consider monitoring during inpatient assessment because feigned psychosis is extremely difficult to maintain 24 hours a day.
Watch for individuals who endorse rare or improbable symptoms. Rare symptoms—by definition—occur very infrequently, and even severely disturbed patients almost never report improbable symptoms.10 Consider asking malingerers about improbable symptoms to see if they will endorse them. For example:
- “When people talk to you, do you see the words they speak spelled out?”11
- “Have you ever believed that automobiles are members of an organized religion?”12
Watch closely for internal or external inconsistency in the suspected malingerer’s presentation (Table 2).
Table 2
Clues to identify malingering during patient evaluation
| Internal inconsistencies | Example |
| In subject’s report of symptoms | Gives a clear and articulate explanation of being confused |
| In subject’s own reported history | Gives conflicting versions |
| External inconsistencies | Example |
| Between reported and observed symptoms | Alleges having active auditory and visual hallucinations yet shows no evidence of being distracted |
| Between reported and observed level of functioning | Behaves in disorganized or confused manner around psychiatrist, yet plays excellent chess on ward with other patients |
| Between reported symptoms and nature of genuine symptoms | Reports seeing visual hallucinations in black and white, whereas genuine visual hallucinations are seen in color |
| Between reported symptoms and psychological test results | Alleges genuine psychotic symptoms, yet testing suggests faking or exaggeration |
Malingered Psychotic Symptoms
Detecting malingered mental illness is considered an advanced psychiatric skill, partly because you must understand thoroughly how genuine psychotic symptoms manifest.
Hallucinations. If a patient alleges atypical hallucinations, ask about them in detail. Hallucinations are usually (88%) associated with delusions.13 Genuine hallucinations are typically intermittent rather than continuous.
Continue to: Auditory hallucinations
Auditory hallucinations are usually clear, not vague (7%) or inaudible. Both male and female voices are commonly heard (75%), and voices are usually perceived as originating outside the head (88%).14 In schizophrenia, the major themes are persecutory or instructive.15
Command auditory hallucinations are easy to fabricate. Persons experiencing genuine command hallucinations:
- do not always obey the voices, especially if doing so would be dangerous16
- usually present with noncommand hallucinations (85%) and delusions (75%) as well17
Thus, view with suspicion someone who alleges an isolated command hallucination without other psychotic symptoms.
Genuine schizophrenic hallucinations tend to diminish when patients are involved in activities. Thus, to deal with their hallucinations, persons with schizophrenia typically cope by:
- engaging in activities (working, listening to a radio, watching TV)
- changing posture (lying down, walking)
- seeking interpersonal contact
- taking medications.
If you suspect a person of malingered auditory hallucinations, ask what he or she does to make the voices go away or diminish in intensity. Patients with genuine schizophrenia often can stop their auditory hallucinations while in remission but not during acute illness.
Malingerers may report auditory hallucinations of stilted or implausible language. For example, we have evaluated:
- an individual charged with attempted rape who alleged that voices said, “Go commit a sex offense.”
- a bank robber who alleged that voices kept screaming, “Stick up, stick up, stick up!”
Both examples contain language that is very questionable for genuine hallucinations, while providing the patient with “psychotic justification” for an illegal act that has a rational alternative motive.
Visual hallucinations are experienced by an estimated 24% to 30% of psychotic individuals but are reported much more often by malingerers (46%) than by persons with genuine psychosis (4%).18
Genuine visual hallucinations are usually of normalsized people and are seen in color.14 On rare occasions, genuine visual hallucinations of small people (Lilliputian hallucinations) may be associated with alcohol use, organic disease, or toxic psychosis (such as anticholinergic toxicity) but are rarely seen by persons with schizophrenia.
Psychotic visual hallucinations do not typically change if the eyes are closed or open, whereas drug-induced hallucinations are more readily seen with eyes closed or in the dark. Unformed hallucinations—such as flashes of light, shadows, or moving objects—are typically associated with neurologic disease and substance use.19
Suspect malingering if the patient reports dramatic or atypical visual hallucinations. For example, one defendant charged with bank robbery calmly reported seeing “a 30-foot tall, red giant smashing down the walls” of the interview room. When he was asked detailed questions, he frequently replied, “I don’t know.” He eventually admitted to malingering.
Delusions. Genuine delusions vary in content, theme, degree of systemization, and relevance to the person’s life. The complexity and sophistication of delusional systems usually reflect the individual’s intelligence. Persecutory delusions are more likely to be acted upon than are other types of delusions.20
Malingerers may claim that a delusion began or disappeared suddenly. In reality, systematized delusions usually take weeks to develop and much longer to disappear. Typically, the delusion will become somewhat less relevant, and the individual will gradually relinquish its importance over time after adequate treatment. In general, the more bizarre the delusion’s content, the more disorganized the individual’s thinking is likely to be (Table 3).
With genuine delusions, the individual’s behavior usually conforms to the delusions’ content. For example, Russell Weston—who suffered from schizophrenia—made a deadly assault on the U.S. Capitol in 1998 because he held a delusional belief that cannibalism was destroying Washington, DC. Before he shot and killed two U.S. Capitol security officers, he had gone to the Central Intelligence Agency several years before and voiced the same delusional concerns.
Suspect malingering if a patient alleges persecutory delusions without engaging in corresponding paranoid behaviors. One exception is the person with long-standing schizophrenia who has grown accustomed to the delusion and whose behavior is no longer consistent with it.
Table 3
Uncommon psychosis presentations that suggest malingering
| Hallucinations |
|
| Delusions |
|
Where Malingerers Trip Up
Malingerers may have inadequate or incomplete knowledge of the mental illness they are faking. Indeed, malingerers are like actors who can portray a role only as well as they understand it. They often overact their part or mistakenly believe the more bizarre their behavior, the more convincing they will be. Conversely, “successful” malingerers are more likely to endorse fewer symptoms and avoid endorsing overly bizarre or unusual symptoms.21
Continue to: Numerous clinical factors suggest malingering...
Numerous clinical factors suggest malingering (Table 4). Malingerers are more likely to eagerly “thrust forward” their illness, whereas patients with genuine schizophrenia are often reluctant to discuss their symptoms.22
Malingerers may attempt to take control of the interview and behave in an intimidating or hostile manner. They may accuse the psychiatrist of inferring that they are faking. Such behavior is rare in genuinely psychotic individuals. Although DSM-IV-TR states that antisocial personality disorder should arouse suspicions of malingering, some studies have failed to show a relationship. One study has associated psychopathic traits with malingering.23
Malingerers often believe that faking intellectual deficits, in addition to psychotic symptoms, will make them more believable. For example, a man who had completed several years of college alleged that he did not know the colors of the American flag.
Malingerers are more likely to give vague or hedging answers to straightforward questions. For example, when asked whether an alleged voice was male or female, one malingerer replied, “It was probably a man’s voice.” Malingerers may also answer, “I don’t know” to detailed questions about psychotic symptoms. Whereas a person with genuine psychotic symptoms could easily give an answer, the malingerer may have never experienced the symptoms and consequently “doesn’t know” the correct answer.
Psychotic symptoms such as derailment, neologisms, loose associations, and word salad are rarely simulated. This is because it is much more difficult for a malingerer to successfully imitate psychotic thought processes than psychotic thought content. Similarly, it is unusual for a malingerer to fake schizophrenia’s subtle signs, such as negative symptoms.
Table 4
Clinical factors that suggest malingering
| Absence of active or subtle signs of psychosis |
| Marked inconsistencies, contradictions |
Patient endorses improbable psychiatric symptoms
|
Patient is evasive or uncooperative
|
| Psychological testing indicates malingering (SIRS, M-FAST, MMPI-2) |
| SIRS: Structured Interview of Reported Symptoms |
| M-FAST: Miller Forensic Assessment of Symptoms Test |
| MMPI-2: Minnesota Multiphasic Personality Inventory, Revised |
Psychological Testing
Although many psychometric tests are available for detecting malingered psychosis, few have been validated. Among the more reliable are:
- Structured Interview of Reported Symptoms (SIRS)
- Minnesota Multiphasic Personality Inventory, Revised (MMPI-2)
- Miller Forensic Assessment of Symptoms Test (M-FAST).11
SIRS includes questions about rare symptoms, uncommon symptom pairing, atypical symptoms, and other indices involving excessive symptom reporting. It takes 30 to 60 minutes to administer. Tested in inpatient, forensic, and correctional populations, the SIRS has shown consistently high accuracy in detecting malingered psychiatric illness.24
Two MMPI-2 scales—F-scale and F-K Index—are the most frequently used test for evaluating suspected malingering. When using the MMPI-2 in this manner, consult the literature for appropriate cutoff scores (see Related resources). Although the MMPI-2 is the most validated psychometric method to detect malingering, a malingerer with high intelligence and previous knowledge of the test could evade detection.25
M-FAST was developed to provide a brief, reliable screen for malingered mental illness. This test takes 10 to 15 minutes to administer and measures rare symptom combinations, excessive reporting, and atypical symptoms.11 It has shown good validity and high correlation with the SIRS and MMPI-2.26,27
Confronting the Malingerer
If a thorough investigation indicates that a patient is malingering psychosis, you may decide to confront the evaluee. Avoid direct accusations of lying,10 and give the suspected malingerer every opportunity to save face. For example, it is preferable to say, “You haven’t told me the whole truth.”
A thoughtful approach that asks the evaluee to clarify inconsistencies is more likely to be productive and safer for the examiner. When confronting individuals with a history of violence and aggression, have adequate security personnel with you.
- Structured Interview of Reported Symptoms (SIRS). Available for purchase from Psychological Assessment Resources at www3.parinc.com (enter “SIRS” in search field).
- Graham JR. MMPI-2: Assessing personality and psychopathology. New York: Oxford Press; 2000. (Source of cutoff scores to use MMPI-2 scales [F-scale and F-K Index] to evaluate suspected malingering).
- Psychological Assessment Resources, Inc. Miller Forensic Assessment of Symptoms Test (M-FAST). Available at: www3.parinc.com (enter “M-FAST” in search field).
Reputed Cosa Nostra boss Vincent “The Chin” Gigante deceived “the most respected minds in forensic psychiatry” for years by malingering schizophrenia.1 Ultimately, he admitted to maintaining his charade from 1990 to 1997 during evaluations of his competency to stand trial for racketeering.
A lesson from this case—said a psychiatrist who concluded Gigante was malingering—is, “When feigning is a consideration, we must be more critical and less accepting of our impressions when we conduct and interpret a psychiatric examination…than might be the case in a typical clinical situation.”2
Even in typical clinical situations, however, psychiatrists may be reluctant to diagnose malingering3 for fear of being sued, assaulted—or wrong. An inaccurate diagnosis of malingering may unjustly stigmatize a patient and deny him needed care.4
Because psychiatrists need a systematized approach to detect malingering,5 we offer specific clinical factors and approaches to help you recognize malingered psychosis.
What is Malingering?
No other syndrome is as easy to define yet so difficult to diagnose as malingering. Reliably diagnosing malingered mental illness is complex, requiring the psychiatrist to consider collateral data beyond the patient interview.
Malingering is the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives.6 In practice, malingering commonly must be differentiated from factitious disorder, which also involves intentional production of symptoms. In factitious disorders, the patient’s motivation is to assume the sick role, which can be thought of as an internal or psychological incentive.
Three categories of malingering include:
- pure malingering (feigning a nonexistent disorder)
- partial malingering (consciously exaggerating real symptoms)
- false imputation (ascribing real symptoms to a cause the individual knows is unrelated to the symptoms).7
Motivations. Individuals usually malinger to avoid pain (such as difficult situations or punishment) or to seek pleasure (such as to obtain compensation or medications) (Table 1). In correctional settings, for example, inmates may malinger mental illness to do “easier time” or to obtain drugs. On the other hand, malingering in prison also may be an adaptive response by a mentally ill inmate to relatively sparse and difficult-to-obtain mental health resources.8
Table 1
Common motives of malingerers
| Motives | Examples |
|---|---|
| To avoid pain | To avoid: |
| Arrest | |
| Criminal prosecution | |
| Conscription into the military | |
| To seek pleasure | To obtain: |
| Controlled substances | |
| Free room and board | |
| Workers’ compensation or disability benefits for alleged psychological injury |
Interview Style
When you suspect a patient is malingering, keep your suspicions to yourself and conduct an objective evaluation. Patients are likely to become defensive if you show annoyance or incredulity, and putting them on guard decreases your ability to uncover evidence of malingering.9
Begin by asking open-ended questions, which allow patients to report symptoms in their own words. To avoid hinting at correct responses, carefully phrase initial inquiries about symptoms. Later in the interview, you can proceed to more-detailed questions of specific symptoms, as discussed below.
If possible, review collateral data before the interview, when it is most helpful. Consider information that would support or refute the alleged symptoms, such as treatment and insurance records, police reports, and interviews of close friends or family.
The patient interview may be prolonged because fatigue may diminish a malingerer’s ability to maintain fake symptoms. In very difficult cases, consider monitoring during inpatient assessment because feigned psychosis is extremely difficult to maintain 24 hours a day.
Watch for individuals who endorse rare or improbable symptoms. Rare symptoms—by definition—occur very infrequently, and even severely disturbed patients almost never report improbable symptoms.10 Consider asking malingerers about improbable symptoms to see if they will endorse them. For example:
- “When people talk to you, do you see the words they speak spelled out?”11
- “Have you ever believed that automobiles are members of an organized religion?”12
Watch closely for internal or external inconsistency in the suspected malingerer’s presentation (Table 2).
Table 2
Clues to identify malingering during patient evaluation
| Internal inconsistencies | Example |
| In subject’s report of symptoms | Gives a clear and articulate explanation of being confused |
| In subject’s own reported history | Gives conflicting versions |
| External inconsistencies | Example |
| Between reported and observed symptoms | Alleges having active auditory and visual hallucinations yet shows no evidence of being distracted |
| Between reported and observed level of functioning | Behaves in disorganized or confused manner around psychiatrist, yet plays excellent chess on ward with other patients |
| Between reported symptoms and nature of genuine symptoms | Reports seeing visual hallucinations in black and white, whereas genuine visual hallucinations are seen in color |
| Between reported symptoms and psychological test results | Alleges genuine psychotic symptoms, yet testing suggests faking or exaggeration |
Malingered Psychotic Symptoms
Detecting malingered mental illness is considered an advanced psychiatric skill, partly because you must understand thoroughly how genuine psychotic symptoms manifest.
Hallucinations. If a patient alleges atypical hallucinations, ask about them in detail. Hallucinations are usually (88%) associated with delusions.13 Genuine hallucinations are typically intermittent rather than continuous.
Continue to: Auditory hallucinations
Auditory hallucinations are usually clear, not vague (7%) or inaudible. Both male and female voices are commonly heard (75%), and voices are usually perceived as originating outside the head (88%).14 In schizophrenia, the major themes are persecutory or instructive.15
Command auditory hallucinations are easy to fabricate. Persons experiencing genuine command hallucinations:
- do not always obey the voices, especially if doing so would be dangerous16
- usually present with noncommand hallucinations (85%) and delusions (75%) as well17
Thus, view with suspicion someone who alleges an isolated command hallucination without other psychotic symptoms.
Genuine schizophrenic hallucinations tend to diminish when patients are involved in activities. Thus, to deal with their hallucinations, persons with schizophrenia typically cope by:
- engaging in activities (working, listening to a radio, watching TV)
- changing posture (lying down, walking)
- seeking interpersonal contact
- taking medications.
If you suspect a person of malingered auditory hallucinations, ask what he or she does to make the voices go away or diminish in intensity. Patients with genuine schizophrenia often can stop their auditory hallucinations while in remission but not during acute illness.
Malingerers may report auditory hallucinations of stilted or implausible language. For example, we have evaluated:
- an individual charged with attempted rape who alleged that voices said, “Go commit a sex offense.”
- a bank robber who alleged that voices kept screaming, “Stick up, stick up, stick up!”
Both examples contain language that is very questionable for genuine hallucinations, while providing the patient with “psychotic justification” for an illegal act that has a rational alternative motive.
Visual hallucinations are experienced by an estimated 24% to 30% of psychotic individuals but are reported much more often by malingerers (46%) than by persons with genuine psychosis (4%).18
Genuine visual hallucinations are usually of normalsized people and are seen in color.14 On rare occasions, genuine visual hallucinations of small people (Lilliputian hallucinations) may be associated with alcohol use, organic disease, or toxic psychosis (such as anticholinergic toxicity) but are rarely seen by persons with schizophrenia.
Psychotic visual hallucinations do not typically change if the eyes are closed or open, whereas drug-induced hallucinations are more readily seen with eyes closed or in the dark. Unformed hallucinations—such as flashes of light, shadows, or moving objects—are typically associated with neurologic disease and substance use.19
Suspect malingering if the patient reports dramatic or atypical visual hallucinations. For example, one defendant charged with bank robbery calmly reported seeing “a 30-foot tall, red giant smashing down the walls” of the interview room. When he was asked detailed questions, he frequently replied, “I don’t know.” He eventually admitted to malingering.
Delusions. Genuine delusions vary in content, theme, degree of systemization, and relevance to the person’s life. The complexity and sophistication of delusional systems usually reflect the individual’s intelligence. Persecutory delusions are more likely to be acted upon than are other types of delusions.20
Malingerers may claim that a delusion began or disappeared suddenly. In reality, systematized delusions usually take weeks to develop and much longer to disappear. Typically, the delusion will become somewhat less relevant, and the individual will gradually relinquish its importance over time after adequate treatment. In general, the more bizarre the delusion’s content, the more disorganized the individual’s thinking is likely to be (Table 3).
With genuine delusions, the individual’s behavior usually conforms to the delusions’ content. For example, Russell Weston—who suffered from schizophrenia—made a deadly assault on the U.S. Capitol in 1998 because he held a delusional belief that cannibalism was destroying Washington, DC. Before he shot and killed two U.S. Capitol security officers, he had gone to the Central Intelligence Agency several years before and voiced the same delusional concerns.
Suspect malingering if a patient alleges persecutory delusions without engaging in corresponding paranoid behaviors. One exception is the person with long-standing schizophrenia who has grown accustomed to the delusion and whose behavior is no longer consistent with it.
Table 3
Uncommon psychosis presentations that suggest malingering
| Hallucinations |
|
| Delusions |
|
Where Malingerers Trip Up
Malingerers may have inadequate or incomplete knowledge of the mental illness they are faking. Indeed, malingerers are like actors who can portray a role only as well as they understand it. They often overact their part or mistakenly believe the more bizarre their behavior, the more convincing they will be. Conversely, “successful” malingerers are more likely to endorse fewer symptoms and avoid endorsing overly bizarre or unusual symptoms.21
Continue to: Numerous clinical factors suggest malingering...
Numerous clinical factors suggest malingering (Table 4). Malingerers are more likely to eagerly “thrust forward” their illness, whereas patients with genuine schizophrenia are often reluctant to discuss their symptoms.22
Malingerers may attempt to take control of the interview and behave in an intimidating or hostile manner. They may accuse the psychiatrist of inferring that they are faking. Such behavior is rare in genuinely psychotic individuals. Although DSM-IV-TR states that antisocial personality disorder should arouse suspicions of malingering, some studies have failed to show a relationship. One study has associated psychopathic traits with malingering.23
Malingerers often believe that faking intellectual deficits, in addition to psychotic symptoms, will make them more believable. For example, a man who had completed several years of college alleged that he did not know the colors of the American flag.
Malingerers are more likely to give vague or hedging answers to straightforward questions. For example, when asked whether an alleged voice was male or female, one malingerer replied, “It was probably a man’s voice.” Malingerers may also answer, “I don’t know” to detailed questions about psychotic symptoms. Whereas a person with genuine psychotic symptoms could easily give an answer, the malingerer may have never experienced the symptoms and consequently “doesn’t know” the correct answer.
Psychotic symptoms such as derailment, neologisms, loose associations, and word salad are rarely simulated. This is because it is much more difficult for a malingerer to successfully imitate psychotic thought processes than psychotic thought content. Similarly, it is unusual for a malingerer to fake schizophrenia’s subtle signs, such as negative symptoms.
Table 4
Clinical factors that suggest malingering
| Absence of active or subtle signs of psychosis |
| Marked inconsistencies, contradictions |
Patient endorses improbable psychiatric symptoms
|
Patient is evasive or uncooperative
|
| Psychological testing indicates malingering (SIRS, M-FAST, MMPI-2) |
| SIRS: Structured Interview of Reported Symptoms |
| M-FAST: Miller Forensic Assessment of Symptoms Test |
| MMPI-2: Minnesota Multiphasic Personality Inventory, Revised |
Psychological Testing
Although many psychometric tests are available for detecting malingered psychosis, few have been validated. Among the more reliable are:
- Structured Interview of Reported Symptoms (SIRS)
- Minnesota Multiphasic Personality Inventory, Revised (MMPI-2)
- Miller Forensic Assessment of Symptoms Test (M-FAST).11
SIRS includes questions about rare symptoms, uncommon symptom pairing, atypical symptoms, and other indices involving excessive symptom reporting. It takes 30 to 60 minutes to administer. Tested in inpatient, forensic, and correctional populations, the SIRS has shown consistently high accuracy in detecting malingered psychiatric illness.24
Two MMPI-2 scales—F-scale and F-K Index—are the most frequently used test for evaluating suspected malingering. When using the MMPI-2 in this manner, consult the literature for appropriate cutoff scores (see Related resources). Although the MMPI-2 is the most validated psychometric method to detect malingering, a malingerer with high intelligence and previous knowledge of the test could evade detection.25
M-FAST was developed to provide a brief, reliable screen for malingered mental illness. This test takes 10 to 15 minutes to administer and measures rare symptom combinations, excessive reporting, and atypical symptoms.11 It has shown good validity and high correlation with the SIRS and MMPI-2.26,27
Confronting the Malingerer
If a thorough investigation indicates that a patient is malingering psychosis, you may decide to confront the evaluee. Avoid direct accusations of lying,10 and give the suspected malingerer every opportunity to save face. For example, it is preferable to say, “You haven’t told me the whole truth.”
A thoughtful approach that asks the evaluee to clarify inconsistencies is more likely to be productive and safer for the examiner. When confronting individuals with a history of violence and aggression, have adequate security personnel with you.
- Structured Interview of Reported Symptoms (SIRS). Available for purchase from Psychological Assessment Resources at www3.parinc.com (enter “SIRS” in search field).
- Graham JR. MMPI-2: Assessing personality and psychopathology. New York: Oxford Press; 2000. (Source of cutoff scores to use MMPI-2 scales [F-scale and F-K Index] to evaluate suspected malingering).
- Psychological Assessment Resources, Inc. Miller Forensic Assessment of Symptoms Test (M-FAST). Available at: www3.parinc.com (enter “M-FAST” in search field).
1. Newman A. Analyze this: Vincent Gigante, not crazy after all those years. New York Times, April 13, 2003.
2. Brodie JD. Personal communication, 2005.
3. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv 1996;47:998-1000.
4. Kropp PR, Rogers R. Understanding malingering: motivation, method, and detection. In: Lewis M, Saarini C (eds). Lying and deception. New York: Guilford Press; 1993.
5. Kucharski LT, et al. Clinical symptom presentation in suspected malingerers: an empirical investigation. Bull Am Acad Psychiatry Law. 1998;26:579-85.
6. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American Psychiatric Association; 2000.
7. Resnick PJ. Malingering of posttraumatic stress disorders. In: Rogers R (ed). Clinical assessment of malingering and deception (2nd ed.). New York: Guilford Press; 1997;130-52.
8. Kupers TA. Malingering in correctional settings. Correctional Ment Health Rep. 2004;5(6):81-95.
9. Sadock BJ, Sadock VA. Kaplan & Sadock’s synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003;898.-
10. Thompson JW, LeBourgeois HW, Black FW. Malingering. In: Simon R, Gold L (eds). Textbook of forensic psychiatry. Washington, DC: American Psychiatric Publishing; 2004.
11. Miller HA. M.-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
12. Rogers R. Assessment of malingering within a forensic context. In Weisstub DW (ed.). Law and psychiatry: international perspectives. New York: Plenum Press; 1987;3:209-37.
13. Lewinsohn PM. An empirical test of several popular notions about hallucinations in schizophrenic patients. In: Keup W (ed.). Origin and mechanisms of hallucinations. New York: Plenum Press; 1970;401-3.
14. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry 1971;24:76-80.
15. Small IF, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Sys 1966;27:349-53.
16. Kasper ME, Rogers R, Adams PA. Dangerousness and command hallucinations: an investigation of psychotic inpatients. Bull Am Acad Psychiatry Law 1996;24:219-24.
17. Thompson JS, Stuart GL, Holden CE. Command hallucinations and legal insanity. Forensic Rep 1992;5:29-43.
18. Cornell DG, Hawk GL. Clinical presentation of malingerers diagnosed by experienced forensic psychologists. Law Hum Behav 1989;13:375-83.
19. Cummings JL, Miller BL. Visual hallucinations: clinical occurrence and use in differential diagnosis. West J Med 1987;146:46-51.
20. Wessely S, Buchanan A, Reed A, et al. Acting on delusions: I. Prevalence. Br J Psychiatry 1993;163:69-76.
21. Edens JF, Guy LS, Otto RK, et al. Factors differentiating successful versus unsuccessful malingerers. J Pers Assess 2001;77(2):333-8.
22. Ritson B, Forest A. The simulation of psychosis: a contemporary presentation. Br J Psychol 1970;43:31-7.
23. Edens JF, Buffington JK, Tomicic TL. An investigation of the relationship between psychopathic traits and malingering on the Psychopathic Personality Inventory. Assessment 2000;7:281-96.
24. Rogers R. Structured interviews and dissimulation. In: Rogers R (ed). Clinical assessment of malingering and deception. New York: Guilford Press; 1997.
25. Pelfrey WV. The relationship between malingerers’ intelligence and MMPI-2 knowledge and their ability to avoid detection. Int J Offender Ther Comp Criminol. 2004;48(6):649-63.
26. Jackson RL, Rogers R, Sewell KW. Forensic applications of the Miller Forensic Assessment of Symptoms Test (MFAST): screening for feigned disorders in competency to stand trial evaluations. Law Human Behav 2005;29(2):199-210.
27. Miller HA. Examining the use of the M-FAST with criminal defendants incompetent to stand trial. Int J Offender Ther Comp Criminol 2004;48(3):268-80.
1. Newman A. Analyze this: Vincent Gigante, not crazy after all those years. New York Times, April 13, 2003.
2. Brodie JD. Personal communication, 2005.
3. Yates BD, Nordquist CR, Schultz-Ross RA. Feigned psychiatric symptoms in the emergency room. Psychiatr Serv 1996;47:998-1000.
4. Kropp PR, Rogers R. Understanding malingering: motivation, method, and detection. In: Lewis M, Saarini C (eds). Lying and deception. New York: Guilford Press; 1993.
5. Kucharski LT, et al. Clinical symptom presentation in suspected malingerers: an empirical investigation. Bull Am Acad Psychiatry Law. 1998;26:579-85.
6. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American Psychiatric Association; 2000.
7. Resnick PJ. Malingering of posttraumatic stress disorders. In: Rogers R (ed). Clinical assessment of malingering and deception (2nd ed.). New York: Guilford Press; 1997;130-52.
8. Kupers TA. Malingering in correctional settings. Correctional Ment Health Rep. 2004;5(6):81-95.
9. Sadock BJ, Sadock VA. Kaplan & Sadock’s synopsis of psychiatry, 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003;898.-
10. Thompson JW, LeBourgeois HW, Black FW. Malingering. In: Simon R, Gold L (eds). Textbook of forensic psychiatry. Washington, DC: American Psychiatric Publishing; 2004.
11. Miller HA. M.-FAST interview booklet. Lutz, FL: Psychological Assessment Resources; 2001.
12. Rogers R. Assessment of malingering within a forensic context. In Weisstub DW (ed.). Law and psychiatry: international perspectives. New York: Plenum Press; 1987;3:209-37.
13. Lewinsohn PM. An empirical test of several popular notions about hallucinations in schizophrenic patients. In: Keup W (ed.). Origin and mechanisms of hallucinations. New York: Plenum Press; 1970;401-3.
14. Goodwin DW, Anderson P, Rosenthal R. Clinical significance of hallucinations in psychiatric disorders: a study of 116 hallucinatory patients. Arch Gen Psychiatry 1971;24:76-80.
15. Small IF, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Sys 1966;27:349-53.
16. Kasper ME, Rogers R, Adams PA. Dangerousness and command hallucinations: an investigation of psychotic inpatients. Bull Am Acad Psychiatry Law 1996;24:219-24.
17. Thompson JS, Stuart GL, Holden CE. Command hallucinations and legal insanity. Forensic Rep 1992;5:29-43.
18. Cornell DG, Hawk GL. Clinical presentation of malingerers diagnosed by experienced forensic psychologists. Law Hum Behav 1989;13:375-83.
19. Cummings JL, Miller BL. Visual hallucinations: clinical occurrence and use in differential diagnosis. West J Med 1987;146:46-51.
20. Wessely S, Buchanan A, Reed A, et al. Acting on delusions: I. Prevalence. Br J Psychiatry 1993;163:69-76.
21. Edens JF, Guy LS, Otto RK, et al. Factors differentiating successful versus unsuccessful malingerers. J Pers Assess 2001;77(2):333-8.
22. Ritson B, Forest A. The simulation of psychosis: a contemporary presentation. Br J Psychol 1970;43:31-7.
23. Edens JF, Buffington JK, Tomicic TL. An investigation of the relationship between psychopathic traits and malingering on the Psychopathic Personality Inventory. Assessment 2000;7:281-96.
24. Rogers R. Structured interviews and dissimulation. In: Rogers R (ed). Clinical assessment of malingering and deception. New York: Guilford Press; 1997.
25. Pelfrey WV. The relationship between malingerers’ intelligence and MMPI-2 knowledge and their ability to avoid detection. Int J Offender Ther Comp Criminol. 2004;48(6):649-63.
26. Jackson RL, Rogers R, Sewell KW. Forensic applications of the Miller Forensic Assessment of Symptoms Test (MFAST): screening for feigned disorders in competency to stand trial evaluations. Law Human Behav 2005;29(2):199-210.
27. Miller HA. Examining the use of the M-FAST with criminal defendants incompetent to stand trial. Int J Offender Ther Comp Criminol 2004;48(3):268-80.

