User login
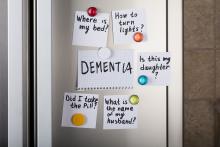
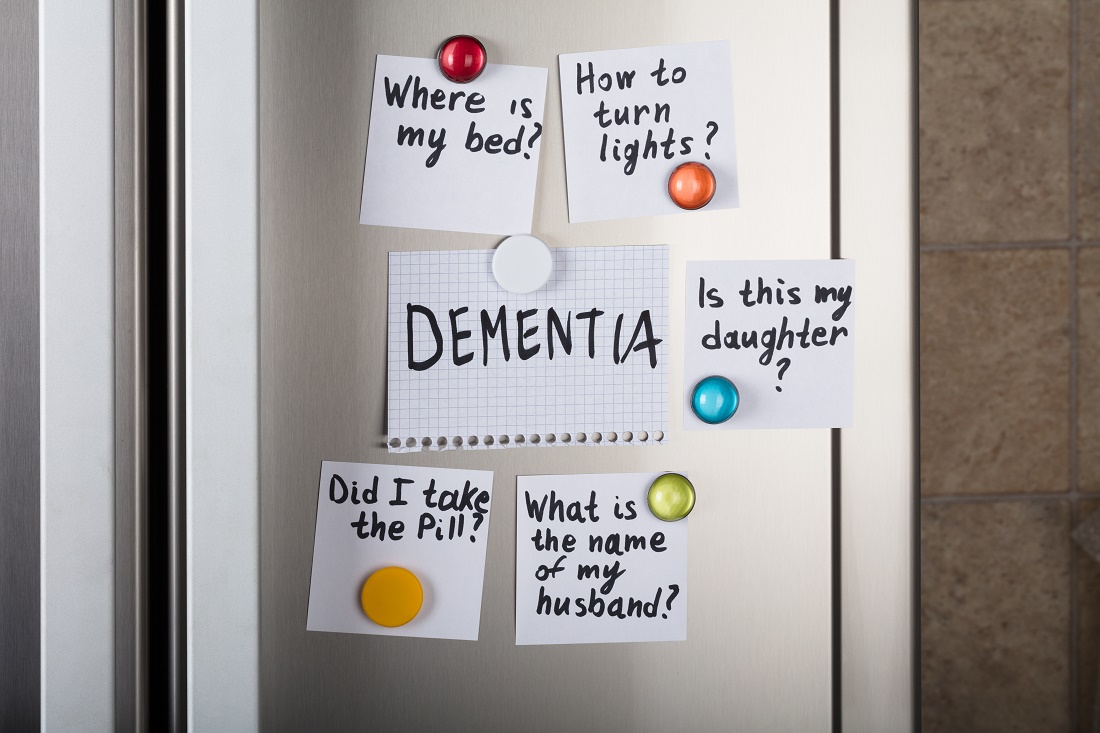
Cannabinoids promising for improving appetite, behavior in dementia
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
Traumatic brain injury tied to long-term sleep problems
Veterans who have suffered a traumatic brain injury (TBI) are significantly more likely to develop insomnia and other sleep problems years later compared to their counterparts who have not suffered a brain injury, a new study shows.
Results of a large longitudinal study show that those with TBI were about 40% more likely to develop insomnia, sleep apnea, excessive daytime sleepiness, or another sleep disorder in later years, after adjusting for demographics and medical and psychiatric conditions.
Interestingly, the association with sleep disorders was strongest among those with mild TBI versus a more severe brain injury.
The study showed that the risk for sleep disorders increased up to 14 years after a brain injury, an indicator that “clinicians should really pay attention to sleep disorders in TBI patients both in the short term and the long term,” study investigator Yue Leng, MD, PhD, assistant professor, department of psychiatry and behavioral sciences, University of California, San Francisco, told this news organization.
The study was published online March 3 in Neurology.
First long-term look
TBI is common among veterans, who may have sleep complaints or psychiatric symptoms, but previous studies into the consequences of TBI have examined the short- vs. long-term impact, said Dr. Leng.
To examine the longitudinal association between TBI and sleep disorders, the investigators examined data on 98,709 Veterans Health Administration patients diagnosed with TBI and an age-matched group of the same number of veterans who had not received such a diagnosis. The mean age of the participants was 49 years at baseline, and 11.7% were women. Of the TBI cases, 49.6% were mild.
Researchers used an exposure survey and diagnostic codes to establish TBI and its severity.
Patients with TBI were more likely to be male and were much more likely to have a psychiatric condition, such as a mood disorder (22.4% vs. 9.3%), anxiety (10.5% vs. 4.4%), posttraumatic stress disorder (19.5% vs. 4.4%), or substance abuse (11.4% vs. 5.2%). They were also more likely to smoke or use tobacco (13.5% vs. 8.7%).
Researchers assessed a number of sleep disorders, including insomnia, hypersomnia disorders, narcolepsy, sleep-related breathing disorders, and sleep-related movement disorders.
During a follow-up period that averaged 5 years but ranged up to 14 years, 23.4% of veterans with TBI and 15.8% of those without TBI developed a sleep disorder.
After adjusting for age, sex, race, education, and income, those who had suffered a TBI were 50% more likely to develop any sleep disorder, compared with those who had not had a TBI (hazard ratio, 1.50; 95% confidence interval, 1.47-1.53.)
After controlling for medical conditions that included diabetes, hypertension, myocardial infarction, and cerebrovascular disease, as well as psychiatric disorders such as mood disorders, anxiety, PTSD, substance use disorder, and tobacco use, the HR for developing a sleep disorder was 1.41 (95% CI, 1.37-1.44).
The association with TBI was stronger for some sleep disorders. Adjusted HRs were 1.50 (95% CI, 1.45-1.55) for insomnia, 1.50 (95% CI, 1.39-1.61) for hypersomnia, 1.33 (95% CI, 1.16-1.52) for sleep-related movement disorders, and 1.28 (95% CI, 1.24-1.32) for sleep apnea.
It’s unclear what causes postinjury sleep problems, but it could be that TBI induces structural brain damage, or it could affect melatonin secretion or wake-promoting neurons.
Damage to arousal-promoting neurons could help explain the reason the link between TBI and sleep disorders was strongest for insomnia and hypersomnia, although the exact mechanism is unclear, said Dr. Leng.
Greater risk with mild TBI
Overall, the association was stronger for mild TBI than for moderate to severe TBI. This, said Dr. Leng, might be because of differences in the brain injury mechanism.
Mild TBI often involves repetitive concussive or subconcussive injuries, such as sports injuries or blast injury among active-duty military personnel. This type of injury is more likely to cause diffuse axonal injury and inflammation, whereas moderate or severe TBI is often attributable to a direct blow with more focal but severe damage, explained Dr. Leng.
She noted that veterans with mild TBI were more likely to have a psychiatric condition, but because the study controlled for such conditions, this doesn’t fully explain the stronger association between mild TBI and sleep disorders.
Further studies are needed to sort out the exact mechanisms, she said.
The association between TBI and risk for sleep disorders was reduced somewhat but was still moderate in an analysis that excluded patients who developed a sleep disorder within 2 years of a brain injury.
This analysis, said Dr. Leng, helped ensure that the sleep disorder developed after the brain injury.
The researchers could not examine the trajectory of sleep problems, so it’s not clear whether sleep problems worsen or get better over time, said Dr. Leng.
Because PTSD also leads to sleep problems, the researchers thought that having both PTSD and TBI might increase the risk for sleep problems. “But actually we found the association was pretty similar in those with, and without, PTSD, so that was kind of contrary to our hypothesis,” she said.
The new results underline the need for more screening for sleep disorders among patients with TBI, both in the short term and the long term, said Dr. Leng. “Clinicians should ask TBI patients about their sleep, and they should follow that up,” she said.
She added that long-term sleep disorders can affect a patient’s health and can lead to psychiatric problems and neurodegenerative diseases.
Depending on the type of sleep disorder, there are a number of possible treatments. For example, for patients with sleep apnea, continuous positive airway pressure treatment may be considered.
‘Outstanding’ research
Commenting for this news organization, Frank Conidi, MD, director, Florida Center for Headache and Sports Neurology; CEO, Brainsport, Team Neurologist, the Florida Panthers of the National Hockey League; and past president, Florida Society of Neurology, said the study is “by far” the largest to investigate the correlation between sleep disorders and head trauma.
The design and outcome measures “were well thought out,” and the researchers “did an outstanding job in sorting through and analyzing the data,” said Dr. Conidi.
He added that he was particularly impressed with how the researchers addressed PTSD, which is highly prevalent among veterans with head trauma and is known to affect sleep.
The new results “solidify what those of us who see individuals with TBI have observed over the years: that there is a higher incidence of all types of sleep disorders” in individuals with a TBI, said Dr. Conidi.
However, he questioned the study’s use of guidelines to classify the various types of head trauma. These guidelines, he said, “are based on loss of consciousness, which we have started to move away from when classifying TBI.”
In addition, Dr. Conidi said he “would have loved to have seen” some correlation with neuroimaging studies, such as those used to assess subdural hematoma, epidural hematoma, subarachnoid hemorrhage, and diffuse axonal injury, but that this “could be an impetus for future studies.”
In “a perfect world,” all patients with a TBI would undergo a polysomnography study in a sleep laboratory, but insurance companies now rarely cover such studies and have attempted to have clinicians shift to home sleep studies, said Dr. Conidi. “These are marginal at best for screening for sleep disorders,” he noted.
At his centers, every TBI patient is screened for sleep disorders and, whenever possible, undergoes formal evaluation in the sleep lab, he added.
The study was supported by the U.S. Army Medical Research and Material Command and the U.S. Department of Veterans Affairs. Dr. Leng and Dr. Conidi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Veterans who have suffered a traumatic brain injury (TBI) are significantly more likely to develop insomnia and other sleep problems years later compared to their counterparts who have not suffered a brain injury, a new study shows.
Results of a large longitudinal study show that those with TBI were about 40% more likely to develop insomnia, sleep apnea, excessive daytime sleepiness, or another sleep disorder in later years, after adjusting for demographics and medical and psychiatric conditions.
Interestingly, the association with sleep disorders was strongest among those with mild TBI versus a more severe brain injury.
The study showed that the risk for sleep disorders increased up to 14 years after a brain injury, an indicator that “clinicians should really pay attention to sleep disorders in TBI patients both in the short term and the long term,” study investigator Yue Leng, MD, PhD, assistant professor, department of psychiatry and behavioral sciences, University of California, San Francisco, told this news organization.
The study was published online March 3 in Neurology.
First long-term look
TBI is common among veterans, who may have sleep complaints or psychiatric symptoms, but previous studies into the consequences of TBI have examined the short- vs. long-term impact, said Dr. Leng.
To examine the longitudinal association between TBI and sleep disorders, the investigators examined data on 98,709 Veterans Health Administration patients diagnosed with TBI and an age-matched group of the same number of veterans who had not received such a diagnosis. The mean age of the participants was 49 years at baseline, and 11.7% were women. Of the TBI cases, 49.6% were mild.
Researchers used an exposure survey and diagnostic codes to establish TBI and its severity.
Patients with TBI were more likely to be male and were much more likely to have a psychiatric condition, such as a mood disorder (22.4% vs. 9.3%), anxiety (10.5% vs. 4.4%), posttraumatic stress disorder (19.5% vs. 4.4%), or substance abuse (11.4% vs. 5.2%). They were also more likely to smoke or use tobacco (13.5% vs. 8.7%).
Researchers assessed a number of sleep disorders, including insomnia, hypersomnia disorders, narcolepsy, sleep-related breathing disorders, and sleep-related movement disorders.
During a follow-up period that averaged 5 years but ranged up to 14 years, 23.4% of veterans with TBI and 15.8% of those without TBI developed a sleep disorder.
After adjusting for age, sex, race, education, and income, those who had suffered a TBI were 50% more likely to develop any sleep disorder, compared with those who had not had a TBI (hazard ratio, 1.50; 95% confidence interval, 1.47-1.53.)
After controlling for medical conditions that included diabetes, hypertension, myocardial infarction, and cerebrovascular disease, as well as psychiatric disorders such as mood disorders, anxiety, PTSD, substance use disorder, and tobacco use, the HR for developing a sleep disorder was 1.41 (95% CI, 1.37-1.44).
The association with TBI was stronger for some sleep disorders. Adjusted HRs were 1.50 (95% CI, 1.45-1.55) for insomnia, 1.50 (95% CI, 1.39-1.61) for hypersomnia, 1.33 (95% CI, 1.16-1.52) for sleep-related movement disorders, and 1.28 (95% CI, 1.24-1.32) for sleep apnea.
It’s unclear what causes postinjury sleep problems, but it could be that TBI induces structural brain damage, or it could affect melatonin secretion or wake-promoting neurons.
Damage to arousal-promoting neurons could help explain the reason the link between TBI and sleep disorders was strongest for insomnia and hypersomnia, although the exact mechanism is unclear, said Dr. Leng.
Greater risk with mild TBI
Overall, the association was stronger for mild TBI than for moderate to severe TBI. This, said Dr. Leng, might be because of differences in the brain injury mechanism.
Mild TBI often involves repetitive concussive or subconcussive injuries, such as sports injuries or blast injury among active-duty military personnel. This type of injury is more likely to cause diffuse axonal injury and inflammation, whereas moderate or severe TBI is often attributable to a direct blow with more focal but severe damage, explained Dr. Leng.
She noted that veterans with mild TBI were more likely to have a psychiatric condition, but because the study controlled for such conditions, this doesn’t fully explain the stronger association between mild TBI and sleep disorders.
Further studies are needed to sort out the exact mechanisms, she said.
The association between TBI and risk for sleep disorders was reduced somewhat but was still moderate in an analysis that excluded patients who developed a sleep disorder within 2 years of a brain injury.
This analysis, said Dr. Leng, helped ensure that the sleep disorder developed after the brain injury.
The researchers could not examine the trajectory of sleep problems, so it’s not clear whether sleep problems worsen or get better over time, said Dr. Leng.
Because PTSD also leads to sleep problems, the researchers thought that having both PTSD and TBI might increase the risk for sleep problems. “But actually we found the association was pretty similar in those with, and without, PTSD, so that was kind of contrary to our hypothesis,” she said.
The new results underline the need for more screening for sleep disorders among patients with TBI, both in the short term and the long term, said Dr. Leng. “Clinicians should ask TBI patients about their sleep, and they should follow that up,” she said.
She added that long-term sleep disorders can affect a patient’s health and can lead to psychiatric problems and neurodegenerative diseases.
Depending on the type of sleep disorder, there are a number of possible treatments. For example, for patients with sleep apnea, continuous positive airway pressure treatment may be considered.
‘Outstanding’ research
Commenting for this news organization, Frank Conidi, MD, director, Florida Center for Headache and Sports Neurology; CEO, Brainsport, Team Neurologist, the Florida Panthers of the National Hockey League; and past president, Florida Society of Neurology, said the study is “by far” the largest to investigate the correlation between sleep disorders and head trauma.
The design and outcome measures “were well thought out,” and the researchers “did an outstanding job in sorting through and analyzing the data,” said Dr. Conidi.
He added that he was particularly impressed with how the researchers addressed PTSD, which is highly prevalent among veterans with head trauma and is known to affect sleep.
The new results “solidify what those of us who see individuals with TBI have observed over the years: that there is a higher incidence of all types of sleep disorders” in individuals with a TBI, said Dr. Conidi.
However, he questioned the study’s use of guidelines to classify the various types of head trauma. These guidelines, he said, “are based on loss of consciousness, which we have started to move away from when classifying TBI.”
In addition, Dr. Conidi said he “would have loved to have seen” some correlation with neuroimaging studies, such as those used to assess subdural hematoma, epidural hematoma, subarachnoid hemorrhage, and diffuse axonal injury, but that this “could be an impetus for future studies.”
In “a perfect world,” all patients with a TBI would undergo a polysomnography study in a sleep laboratory, but insurance companies now rarely cover such studies and have attempted to have clinicians shift to home sleep studies, said Dr. Conidi. “These are marginal at best for screening for sleep disorders,” he noted.
At his centers, every TBI patient is screened for sleep disorders and, whenever possible, undergoes formal evaluation in the sleep lab, he added.
The study was supported by the U.S. Army Medical Research and Material Command and the U.S. Department of Veterans Affairs. Dr. Leng and Dr. Conidi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Veterans who have suffered a traumatic brain injury (TBI) are significantly more likely to develop insomnia and other sleep problems years later compared to their counterparts who have not suffered a brain injury, a new study shows.
Results of a large longitudinal study show that those with TBI were about 40% more likely to develop insomnia, sleep apnea, excessive daytime sleepiness, or another sleep disorder in later years, after adjusting for demographics and medical and psychiatric conditions.
Interestingly, the association with sleep disorders was strongest among those with mild TBI versus a more severe brain injury.
The study showed that the risk for sleep disorders increased up to 14 years after a brain injury, an indicator that “clinicians should really pay attention to sleep disorders in TBI patients both in the short term and the long term,” study investigator Yue Leng, MD, PhD, assistant professor, department of psychiatry and behavioral sciences, University of California, San Francisco, told this news organization.
The study was published online March 3 in Neurology.
First long-term look
TBI is common among veterans, who may have sleep complaints or psychiatric symptoms, but previous studies into the consequences of TBI have examined the short- vs. long-term impact, said Dr. Leng.
To examine the longitudinal association between TBI and sleep disorders, the investigators examined data on 98,709 Veterans Health Administration patients diagnosed with TBI and an age-matched group of the same number of veterans who had not received such a diagnosis. The mean age of the participants was 49 years at baseline, and 11.7% were women. Of the TBI cases, 49.6% were mild.
Researchers used an exposure survey and diagnostic codes to establish TBI and its severity.
Patients with TBI were more likely to be male and were much more likely to have a psychiatric condition, such as a mood disorder (22.4% vs. 9.3%), anxiety (10.5% vs. 4.4%), posttraumatic stress disorder (19.5% vs. 4.4%), or substance abuse (11.4% vs. 5.2%). They were also more likely to smoke or use tobacco (13.5% vs. 8.7%).
Researchers assessed a number of sleep disorders, including insomnia, hypersomnia disorders, narcolepsy, sleep-related breathing disorders, and sleep-related movement disorders.
During a follow-up period that averaged 5 years but ranged up to 14 years, 23.4% of veterans with TBI and 15.8% of those without TBI developed a sleep disorder.
After adjusting for age, sex, race, education, and income, those who had suffered a TBI were 50% more likely to develop any sleep disorder, compared with those who had not had a TBI (hazard ratio, 1.50; 95% confidence interval, 1.47-1.53.)
After controlling for medical conditions that included diabetes, hypertension, myocardial infarction, and cerebrovascular disease, as well as psychiatric disorders such as mood disorders, anxiety, PTSD, substance use disorder, and tobacco use, the HR for developing a sleep disorder was 1.41 (95% CI, 1.37-1.44).
The association with TBI was stronger for some sleep disorders. Adjusted HRs were 1.50 (95% CI, 1.45-1.55) for insomnia, 1.50 (95% CI, 1.39-1.61) for hypersomnia, 1.33 (95% CI, 1.16-1.52) for sleep-related movement disorders, and 1.28 (95% CI, 1.24-1.32) for sleep apnea.
It’s unclear what causes postinjury sleep problems, but it could be that TBI induces structural brain damage, or it could affect melatonin secretion or wake-promoting neurons.
Damage to arousal-promoting neurons could help explain the reason the link between TBI and sleep disorders was strongest for insomnia and hypersomnia, although the exact mechanism is unclear, said Dr. Leng.
Greater risk with mild TBI
Overall, the association was stronger for mild TBI than for moderate to severe TBI. This, said Dr. Leng, might be because of differences in the brain injury mechanism.
Mild TBI often involves repetitive concussive or subconcussive injuries, such as sports injuries or blast injury among active-duty military personnel. This type of injury is more likely to cause diffuse axonal injury and inflammation, whereas moderate or severe TBI is often attributable to a direct blow with more focal but severe damage, explained Dr. Leng.
She noted that veterans with mild TBI were more likely to have a psychiatric condition, but because the study controlled for such conditions, this doesn’t fully explain the stronger association between mild TBI and sleep disorders.
Further studies are needed to sort out the exact mechanisms, she said.
The association between TBI and risk for sleep disorders was reduced somewhat but was still moderate in an analysis that excluded patients who developed a sleep disorder within 2 years of a brain injury.
This analysis, said Dr. Leng, helped ensure that the sleep disorder developed after the brain injury.
The researchers could not examine the trajectory of sleep problems, so it’s not clear whether sleep problems worsen or get better over time, said Dr. Leng.
Because PTSD also leads to sleep problems, the researchers thought that having both PTSD and TBI might increase the risk for sleep problems. “But actually we found the association was pretty similar in those with, and without, PTSD, so that was kind of contrary to our hypothesis,” she said.
The new results underline the need for more screening for sleep disorders among patients with TBI, both in the short term and the long term, said Dr. Leng. “Clinicians should ask TBI patients about their sleep, and they should follow that up,” she said.
She added that long-term sleep disorders can affect a patient’s health and can lead to psychiatric problems and neurodegenerative diseases.
Depending on the type of sleep disorder, there are a number of possible treatments. For example, for patients with sleep apnea, continuous positive airway pressure treatment may be considered.
‘Outstanding’ research
Commenting for this news organization, Frank Conidi, MD, director, Florida Center for Headache and Sports Neurology; CEO, Brainsport, Team Neurologist, the Florida Panthers of the National Hockey League; and past president, Florida Society of Neurology, said the study is “by far” the largest to investigate the correlation between sleep disorders and head trauma.
The design and outcome measures “were well thought out,” and the researchers “did an outstanding job in sorting through and analyzing the data,” said Dr. Conidi.
He added that he was particularly impressed with how the researchers addressed PTSD, which is highly prevalent among veterans with head trauma and is known to affect sleep.
The new results “solidify what those of us who see individuals with TBI have observed over the years: that there is a higher incidence of all types of sleep disorders” in individuals with a TBI, said Dr. Conidi.
However, he questioned the study’s use of guidelines to classify the various types of head trauma. These guidelines, he said, “are based on loss of consciousness, which we have started to move away from when classifying TBI.”
In addition, Dr. Conidi said he “would have loved to have seen” some correlation with neuroimaging studies, such as those used to assess subdural hematoma, epidural hematoma, subarachnoid hemorrhage, and diffuse axonal injury, but that this “could be an impetus for future studies.”
In “a perfect world,” all patients with a TBI would undergo a polysomnography study in a sleep laboratory, but insurance companies now rarely cover such studies and have attempted to have clinicians shift to home sleep studies, said Dr. Conidi. “These are marginal at best for screening for sleep disorders,” he noted.
At his centers, every TBI patient is screened for sleep disorders and, whenever possible, undergoes formal evaluation in the sleep lab, he added.
The study was supported by the U.S. Army Medical Research and Material Command and the U.S. Department of Veterans Affairs. Dr. Leng and Dr. Conidi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sleep apnea and cognitive impairment are common bedfellows
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
FROM AAN 2021
‘Landmark’ schizophrenia drug in the wings?
A novel therapy that combines a muscarinic receptor agonist with an anticholinergic agent is associated with a greater reduction in psychosis symptoms, compared with placebo, new research shows.
In a randomized, phase 2 trial composed of nearly 200 participants, xanomeline-trospium (KarXT) was generally well tolerated and had none of the common side effects linked to current antipsychotics, including weight gain and extrapyramidal symptoms such as dystonia, parkinsonism, and tardive dyskinesia.
“The results showing robust therapeutic efficacy of a non–dopamine targeting antipsychotic drug is an important milestone in the advance of the therapeutics of schizophrenia and other psychotic disorders,” coinvestigator Jeffrey A. Lieberman, MD, professor and chairman in the department of psychiatry, Columbia University, New York, said in an interview.
If approved, the new agent will be a “landmark” drug, Dr. Lieberman added.
The study was published in the Feb. 25, 2021, issue of the New England Journal of Medicine.
Long journey
The journey to develop an effective schizophrenia drug that reduces psychosis symptoms without onerous side effects has been a long one full of excitement and disappointment.
First-generation antipsychotics, dating back to the 1950s, targeted the postsynaptic dopamine-2 (D2) receptor. At the time, it was a “breakthrough” similar in scope to insulin for diabetes or antibiotics for infections, said Dr. Lieberman.
That was followed by development of numerous “me too” drugs with the same mechanism of action. However, these drugs had significant side effects, especially neurologic adverse events such as parkinsonism.
In 1989, second-generation antipsychotics were introduced, beginning with clozapine. They still targeted the D2 receptor but were “kinder and gentler,” Dr. Lieberman noted. “They didn’t bind to [the receptor] with such affinity that it shut things down completely, so had fewer neurologic side effects.”
However, these agents had other adverse consequences, such as weight gain and other metabolic effects including hyperglycemia and hyperlipidemia.
Many have poor functional status and quality of life despite lifelong treatment with current antipsychotic agents.
“The pharmaceutical industry, biotech industry, and academic psychiatric community have been desperately trying to find novel strategies for antipsychotic drug development and asking, ‘Is D2 the only holy grail or are there other ways of treating psychotic symptoms of schizophrenia?’ ” Dr. Lieberman said.
Enter KarXT – a novel combination of xanomeline with trospium.
An ‘ingenious’ combination
Xanomeline, an oral muscarinic cholinergic receptor agonist, does not have direct effects on the dopamine receptor. Evidence suggests the muscarinic cholinergic system is involved in the pathophysiology of schizophrenia.
However, there may be dose-dependent adverse events with the medication, such as nausea, vomiting, diarrhea, sweating, and hypersalivation from stimulation of peripheral muscarinic cholinergic receptors.
That’s where trospium chloride, an oral panmuscarinic receptor antagonist approved for treating overactive bladder, comes in. It does not reach detectable levels in the cerebrospinal fluid and should avoid adverse central nervous system effects.
Dr. Lieberman said the idea of the drug combination is “ingenious.”
The new phase 2, multisite study included adult patients with a validated diagnosis of schizophrenia who were hospitalized with an acute exacerbation of psychosis, and who were free of antipsychotic medication for at least 2 weeks.
Participants were required to have a baseline Positive and Negative Syndrome Scale (PANSS) total score of 80 points or more.
In addition to seven positive symptom items, including delusions, hallucinations, and conceptual disorganization, the PANSS has seven negative symptom items. These include restricted emotional expression, paucity of speech, and diminished interest, social drive, and activity. Each item is scored from 1 to 7, with higher scores indicating more severe symptoms.
Patients also had to have a score on the Clinical Global Impression–Severity (CGI-S) scale of 4 or higher. Scores on the CGI-S range from 1 to 7, with higher scores indicating greater severity of illness.
The modified intention-to-treat analysis included patients randomly assigned to receive oral xanomeline-trospium (n = 83) or placebo (n = 87).
The dosing schedule was flexible, starting with 50 mg of xanomeline and 20 mg of trospium twice daily. The schedule increased to a maximum of 125 mg of xanomeline and 30 mg of trospium twice daily, with the option of lowering the dose if there were unacceptable side effects.
Mean scores at baseline for the treatment and placebo groups were 97.7 versus 96.6 for the PANSS total score, 26.4 versus 26.3 for the positive subscore, 22.6 versus 22.8 for the negative subscore, and 5.0 versus 4.9 in the CGI-S scale.
‘Impressively robust’ effect size
The primary endpoint was change in the PANSS total score at 5 weeks. Results showed a change of –17.4 points in the treatment group and –5.9 points in the placebo group (least-squares mean difference, –11.6 points; 95% confidence interval, –16.1 to –7.1; P < .001).
The effect size, which was almost 0.8 (0.75), was “impressively robust,” said Dr. Lieberman, adding that a moderate effect size in this patient population might be in the order of 0.4 or 0.5.
“That gives hope that this drug may not just be as effective as other antipsychotics, albeit acting in a novel way and in a way that has a less of side effect burden, but that it may actually have some elements of superior efficacy,” he said.
There were significant benefits on some secondary outcomes, including change in the PANSS positive symptom subscore (–5.6 points in the treatment group vs. –2.4 points in the placebo group; least-squares mean difference, –3.2 points; 95% CI, –4.8 to –1.7; P < .001).
The active treatment also came out on top for CGI-S scores (P < .001), and PANSS negative symptom subscore (P < .001).
Because participants were hospitalized with an acute exacerbation of positive symptoms at time of study, it is difficult to determine “definitive efficacy” for negative symptoms, Dr. Lieberman noted. Negative symptoms may have improved simply because positive symptoms got better, he said.
Although the study included adults only, “there is nothing in the KarXT clinical profile that suggests it would be problematic for younger people,” Dr. Lieberman noted. This could include teenagers with first-episode psychosis.
Safety profile
Adverse events (AEs) were reported in 54% of the treatment group and 43% of the placebo group. AEs that were more common in the active treatment group included constipation (17% vs. 3%), nausea (17% vs. 4%), dry mouth (9% vs. 1%), dyspepsia (9% vs. 4%), and vomiting (9% vs. 4%). All AEs were rated as mild or moderate in severity and none resulted in discontinuation of treatment.
Rates of nausea, vomiting, and dry mouth were highest early in the trial and lower at the end, whereas constipation remained constant throughout the study.
Persistent constipation could affect the drug’s “utility” in elderly patients with cognitive issues but may be more of a “minor nuisance,” compared with other antipsychotics for those with schizophrenia, said Dr. Lieberman. He added that constipation might be mitigated with an over-the-counter treatment such as Metamucil. Importantly, there was no difference between groups in extrapyramidal symptoms.
In addition, participants receiving the active treatment did not have greater weight gain, which was about 3% versus 4% in the placebo group. The mean change in weight was 1.5 kg (3.3 lb) and 1.1 kg (2.4 lb), respectively.
Dr. Lieberman praised the manufacturer for undertaking the study.
“In an era when Big Pharma has retreated to a considerable degree from psychotropic drug development, it’s commendable that some companies have stayed the course and are succeeding in drug development,” he said.
Exciting mechanism
Commenting on the findings in an interview, Thomas Sedlak, MD, PhD, director of the Schizophrenia and Psychosis Consult Clinic and assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, called some aspects of the study “exciting.”
What’s especially important is that the novel agent “acts by a different mechanism than what we have been using for maybe 60 years,” said Dr. Sedlak, who was not involved with the research.
“There has been a lot of research in the last few decades into drugs that might act by alternate mechanisms of action, but nothing’s really gotten to market for schizophrenia,” he noted.
Another interesting aspect of the study is that it examined a combination drug that aims to maximize effects on the brain while minimizing periphery effects, Dr. Sedlak said.
In addition, he called the PANSS results “respectable.”
“It’s interesting that you get a big change in PANSS total score, but it’s not as big in the positive symptom score as you might have expected, and it’s not a huge drop in negative symptoms either,” said Dr. Sedlak.
It’s possible, he said, that the drug is targeting PANSS elements not captured in the main positive or negative symptom items; for example, anxiety, depression, guilt, attention, impulse control, disorientation, and judgment.
Dr. Sedlak noted that, while the new results are exciting, the enthusiasm may not be long-lasting. “When a new drug comes out, there’s often a lot of excitement about it, but once you start using it, expectations may deflate..
“More flexible ratios” of the two components of the drug might be useful to treat individual patients, he added.
In addition, using the components by themselves might be preferable for some clinicians. “I think a lot of physicians prefer using two separate drugs so they can alter the dose of each one independently and not be stuck with the ratio the manufacturer is providing,” Dr. Sedlak said.
However, he acknowledged that studying different choices of ratios would require much larger trials.
The study was supported by Karuna Therapeutics and the Wellcome Trust. Dr. Lieberman reported serving on an advisory board for Karuna Therapeutics and Intra-Cellular Therapies. Dr. Sedlak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A novel therapy that combines a muscarinic receptor agonist with an anticholinergic agent is associated with a greater reduction in psychosis symptoms, compared with placebo, new research shows.
In a randomized, phase 2 trial composed of nearly 200 participants, xanomeline-trospium (KarXT) was generally well tolerated and had none of the common side effects linked to current antipsychotics, including weight gain and extrapyramidal symptoms such as dystonia, parkinsonism, and tardive dyskinesia.
“The results showing robust therapeutic efficacy of a non–dopamine targeting antipsychotic drug is an important milestone in the advance of the therapeutics of schizophrenia and other psychotic disorders,” coinvestigator Jeffrey A. Lieberman, MD, professor and chairman in the department of psychiatry, Columbia University, New York, said in an interview.
If approved, the new agent will be a “landmark” drug, Dr. Lieberman added.
The study was published in the Feb. 25, 2021, issue of the New England Journal of Medicine.
Long journey
The journey to develop an effective schizophrenia drug that reduces psychosis symptoms without onerous side effects has been a long one full of excitement and disappointment.
First-generation antipsychotics, dating back to the 1950s, targeted the postsynaptic dopamine-2 (D2) receptor. At the time, it was a “breakthrough” similar in scope to insulin for diabetes or antibiotics for infections, said Dr. Lieberman.
That was followed by development of numerous “me too” drugs with the same mechanism of action. However, these drugs had significant side effects, especially neurologic adverse events such as parkinsonism.
In 1989, second-generation antipsychotics were introduced, beginning with clozapine. They still targeted the D2 receptor but were “kinder and gentler,” Dr. Lieberman noted. “They didn’t bind to [the receptor] with such affinity that it shut things down completely, so had fewer neurologic side effects.”
However, these agents had other adverse consequences, such as weight gain and other metabolic effects including hyperglycemia and hyperlipidemia.
Many have poor functional status and quality of life despite lifelong treatment with current antipsychotic agents.
“The pharmaceutical industry, biotech industry, and academic psychiatric community have been desperately trying to find novel strategies for antipsychotic drug development and asking, ‘Is D2 the only holy grail or are there other ways of treating psychotic symptoms of schizophrenia?’ ” Dr. Lieberman said.
Enter KarXT – a novel combination of xanomeline with trospium.
An ‘ingenious’ combination
Xanomeline, an oral muscarinic cholinergic receptor agonist, does not have direct effects on the dopamine receptor. Evidence suggests the muscarinic cholinergic system is involved in the pathophysiology of schizophrenia.
However, there may be dose-dependent adverse events with the medication, such as nausea, vomiting, diarrhea, sweating, and hypersalivation from stimulation of peripheral muscarinic cholinergic receptors.
That’s where trospium chloride, an oral panmuscarinic receptor antagonist approved for treating overactive bladder, comes in. It does not reach detectable levels in the cerebrospinal fluid and should avoid adverse central nervous system effects.
Dr. Lieberman said the idea of the drug combination is “ingenious.”
The new phase 2, multisite study included adult patients with a validated diagnosis of schizophrenia who were hospitalized with an acute exacerbation of psychosis, and who were free of antipsychotic medication for at least 2 weeks.
Participants were required to have a baseline Positive and Negative Syndrome Scale (PANSS) total score of 80 points or more.
In addition to seven positive symptom items, including delusions, hallucinations, and conceptual disorganization, the PANSS has seven negative symptom items. These include restricted emotional expression, paucity of speech, and diminished interest, social drive, and activity. Each item is scored from 1 to 7, with higher scores indicating more severe symptoms.
Patients also had to have a score on the Clinical Global Impression–Severity (CGI-S) scale of 4 or higher. Scores on the CGI-S range from 1 to 7, with higher scores indicating greater severity of illness.
The modified intention-to-treat analysis included patients randomly assigned to receive oral xanomeline-trospium (n = 83) or placebo (n = 87).
The dosing schedule was flexible, starting with 50 mg of xanomeline and 20 mg of trospium twice daily. The schedule increased to a maximum of 125 mg of xanomeline and 30 mg of trospium twice daily, with the option of lowering the dose if there were unacceptable side effects.
Mean scores at baseline for the treatment and placebo groups were 97.7 versus 96.6 for the PANSS total score, 26.4 versus 26.3 for the positive subscore, 22.6 versus 22.8 for the negative subscore, and 5.0 versus 4.9 in the CGI-S scale.
‘Impressively robust’ effect size
The primary endpoint was change in the PANSS total score at 5 weeks. Results showed a change of –17.4 points in the treatment group and –5.9 points in the placebo group (least-squares mean difference, –11.6 points; 95% confidence interval, –16.1 to –7.1; P < .001).
The effect size, which was almost 0.8 (0.75), was “impressively robust,” said Dr. Lieberman, adding that a moderate effect size in this patient population might be in the order of 0.4 or 0.5.
“That gives hope that this drug may not just be as effective as other antipsychotics, albeit acting in a novel way and in a way that has a less of side effect burden, but that it may actually have some elements of superior efficacy,” he said.
There were significant benefits on some secondary outcomes, including change in the PANSS positive symptom subscore (–5.6 points in the treatment group vs. –2.4 points in the placebo group; least-squares mean difference, –3.2 points; 95% CI, –4.8 to –1.7; P < .001).
The active treatment also came out on top for CGI-S scores (P < .001), and PANSS negative symptom subscore (P < .001).
Because participants were hospitalized with an acute exacerbation of positive symptoms at time of study, it is difficult to determine “definitive efficacy” for negative symptoms, Dr. Lieberman noted. Negative symptoms may have improved simply because positive symptoms got better, he said.
Although the study included adults only, “there is nothing in the KarXT clinical profile that suggests it would be problematic for younger people,” Dr. Lieberman noted. This could include teenagers with first-episode psychosis.
Safety profile
Adverse events (AEs) were reported in 54% of the treatment group and 43% of the placebo group. AEs that were more common in the active treatment group included constipation (17% vs. 3%), nausea (17% vs. 4%), dry mouth (9% vs. 1%), dyspepsia (9% vs. 4%), and vomiting (9% vs. 4%). All AEs were rated as mild or moderate in severity and none resulted in discontinuation of treatment.
Rates of nausea, vomiting, and dry mouth were highest early in the trial and lower at the end, whereas constipation remained constant throughout the study.
Persistent constipation could affect the drug’s “utility” in elderly patients with cognitive issues but may be more of a “minor nuisance,” compared with other antipsychotics for those with schizophrenia, said Dr. Lieberman. He added that constipation might be mitigated with an over-the-counter treatment such as Metamucil. Importantly, there was no difference between groups in extrapyramidal symptoms.
In addition, participants receiving the active treatment did not have greater weight gain, which was about 3% versus 4% in the placebo group. The mean change in weight was 1.5 kg (3.3 lb) and 1.1 kg (2.4 lb), respectively.
Dr. Lieberman praised the manufacturer for undertaking the study.
“In an era when Big Pharma has retreated to a considerable degree from psychotropic drug development, it’s commendable that some companies have stayed the course and are succeeding in drug development,” he said.
Exciting mechanism
Commenting on the findings in an interview, Thomas Sedlak, MD, PhD, director of the Schizophrenia and Psychosis Consult Clinic and assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, called some aspects of the study “exciting.”
What’s especially important is that the novel agent “acts by a different mechanism than what we have been using for maybe 60 years,” said Dr. Sedlak, who was not involved with the research.
“There has been a lot of research in the last few decades into drugs that might act by alternate mechanisms of action, but nothing’s really gotten to market for schizophrenia,” he noted.
Another interesting aspect of the study is that it examined a combination drug that aims to maximize effects on the brain while minimizing periphery effects, Dr. Sedlak said.
In addition, he called the PANSS results “respectable.”
“It’s interesting that you get a big change in PANSS total score, but it’s not as big in the positive symptom score as you might have expected, and it’s not a huge drop in negative symptoms either,” said Dr. Sedlak.
It’s possible, he said, that the drug is targeting PANSS elements not captured in the main positive or negative symptom items; for example, anxiety, depression, guilt, attention, impulse control, disorientation, and judgment.
Dr. Sedlak noted that, while the new results are exciting, the enthusiasm may not be long-lasting. “When a new drug comes out, there’s often a lot of excitement about it, but once you start using it, expectations may deflate..
“More flexible ratios” of the two components of the drug might be useful to treat individual patients, he added.
In addition, using the components by themselves might be preferable for some clinicians. “I think a lot of physicians prefer using two separate drugs so they can alter the dose of each one independently and not be stuck with the ratio the manufacturer is providing,” Dr. Sedlak said.
However, he acknowledged that studying different choices of ratios would require much larger trials.
The study was supported by Karuna Therapeutics and the Wellcome Trust. Dr. Lieberman reported serving on an advisory board for Karuna Therapeutics and Intra-Cellular Therapies. Dr. Sedlak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A novel therapy that combines a muscarinic receptor agonist with an anticholinergic agent is associated with a greater reduction in psychosis symptoms, compared with placebo, new research shows.
In a randomized, phase 2 trial composed of nearly 200 participants, xanomeline-trospium (KarXT) was generally well tolerated and had none of the common side effects linked to current antipsychotics, including weight gain and extrapyramidal symptoms such as dystonia, parkinsonism, and tardive dyskinesia.
“The results showing robust therapeutic efficacy of a non–dopamine targeting antipsychotic drug is an important milestone in the advance of the therapeutics of schizophrenia and other psychotic disorders,” coinvestigator Jeffrey A. Lieberman, MD, professor and chairman in the department of psychiatry, Columbia University, New York, said in an interview.
If approved, the new agent will be a “landmark” drug, Dr. Lieberman added.
The study was published in the Feb. 25, 2021, issue of the New England Journal of Medicine.
Long journey
The journey to develop an effective schizophrenia drug that reduces psychosis symptoms without onerous side effects has been a long one full of excitement and disappointment.
First-generation antipsychotics, dating back to the 1950s, targeted the postsynaptic dopamine-2 (D2) receptor. At the time, it was a “breakthrough” similar in scope to insulin for diabetes or antibiotics for infections, said Dr. Lieberman.
That was followed by development of numerous “me too” drugs with the same mechanism of action. However, these drugs had significant side effects, especially neurologic adverse events such as parkinsonism.
In 1989, second-generation antipsychotics were introduced, beginning with clozapine. They still targeted the D2 receptor but were “kinder and gentler,” Dr. Lieberman noted. “They didn’t bind to [the receptor] with such affinity that it shut things down completely, so had fewer neurologic side effects.”
However, these agents had other adverse consequences, such as weight gain and other metabolic effects including hyperglycemia and hyperlipidemia.
Many have poor functional status and quality of life despite lifelong treatment with current antipsychotic agents.
“The pharmaceutical industry, biotech industry, and academic psychiatric community have been desperately trying to find novel strategies for antipsychotic drug development and asking, ‘Is D2 the only holy grail or are there other ways of treating psychotic symptoms of schizophrenia?’ ” Dr. Lieberman said.
Enter KarXT – a novel combination of xanomeline with trospium.
An ‘ingenious’ combination
Xanomeline, an oral muscarinic cholinergic receptor agonist, does not have direct effects on the dopamine receptor. Evidence suggests the muscarinic cholinergic system is involved in the pathophysiology of schizophrenia.
However, there may be dose-dependent adverse events with the medication, such as nausea, vomiting, diarrhea, sweating, and hypersalivation from stimulation of peripheral muscarinic cholinergic receptors.
That’s where trospium chloride, an oral panmuscarinic receptor antagonist approved for treating overactive bladder, comes in. It does not reach detectable levels in the cerebrospinal fluid and should avoid adverse central nervous system effects.
Dr. Lieberman said the idea of the drug combination is “ingenious.”
The new phase 2, multisite study included adult patients with a validated diagnosis of schizophrenia who were hospitalized with an acute exacerbation of psychosis, and who were free of antipsychotic medication for at least 2 weeks.
Participants were required to have a baseline Positive and Negative Syndrome Scale (PANSS) total score of 80 points or more.
In addition to seven positive symptom items, including delusions, hallucinations, and conceptual disorganization, the PANSS has seven negative symptom items. These include restricted emotional expression, paucity of speech, and diminished interest, social drive, and activity. Each item is scored from 1 to 7, with higher scores indicating more severe symptoms.
Patients also had to have a score on the Clinical Global Impression–Severity (CGI-S) scale of 4 or higher. Scores on the CGI-S range from 1 to 7, with higher scores indicating greater severity of illness.
The modified intention-to-treat analysis included patients randomly assigned to receive oral xanomeline-trospium (n = 83) or placebo (n = 87).
The dosing schedule was flexible, starting with 50 mg of xanomeline and 20 mg of trospium twice daily. The schedule increased to a maximum of 125 mg of xanomeline and 30 mg of trospium twice daily, with the option of lowering the dose if there were unacceptable side effects.
Mean scores at baseline for the treatment and placebo groups were 97.7 versus 96.6 for the PANSS total score, 26.4 versus 26.3 for the positive subscore, 22.6 versus 22.8 for the negative subscore, and 5.0 versus 4.9 in the CGI-S scale.
‘Impressively robust’ effect size
The primary endpoint was change in the PANSS total score at 5 weeks. Results showed a change of –17.4 points in the treatment group and –5.9 points in the placebo group (least-squares mean difference, –11.6 points; 95% confidence interval, –16.1 to –7.1; P < .001).
The effect size, which was almost 0.8 (0.75), was “impressively robust,” said Dr. Lieberman, adding that a moderate effect size in this patient population might be in the order of 0.4 or 0.5.
“That gives hope that this drug may not just be as effective as other antipsychotics, albeit acting in a novel way and in a way that has a less of side effect burden, but that it may actually have some elements of superior efficacy,” he said.
There were significant benefits on some secondary outcomes, including change in the PANSS positive symptom subscore (–5.6 points in the treatment group vs. –2.4 points in the placebo group; least-squares mean difference, –3.2 points; 95% CI, –4.8 to –1.7; P < .001).
The active treatment also came out on top for CGI-S scores (P < .001), and PANSS negative symptom subscore (P < .001).
Because participants were hospitalized with an acute exacerbation of positive symptoms at time of study, it is difficult to determine “definitive efficacy” for negative symptoms, Dr. Lieberman noted. Negative symptoms may have improved simply because positive symptoms got better, he said.
Although the study included adults only, “there is nothing in the KarXT clinical profile that suggests it would be problematic for younger people,” Dr. Lieberman noted. This could include teenagers with first-episode psychosis.
Safety profile
Adverse events (AEs) were reported in 54% of the treatment group and 43% of the placebo group. AEs that were more common in the active treatment group included constipation (17% vs. 3%), nausea (17% vs. 4%), dry mouth (9% vs. 1%), dyspepsia (9% vs. 4%), and vomiting (9% vs. 4%). All AEs were rated as mild or moderate in severity and none resulted in discontinuation of treatment.
Rates of nausea, vomiting, and dry mouth were highest early in the trial and lower at the end, whereas constipation remained constant throughout the study.
Persistent constipation could affect the drug’s “utility” in elderly patients with cognitive issues but may be more of a “minor nuisance,” compared with other antipsychotics for those with schizophrenia, said Dr. Lieberman. He added that constipation might be mitigated with an over-the-counter treatment such as Metamucil. Importantly, there was no difference between groups in extrapyramidal symptoms.
In addition, participants receiving the active treatment did not have greater weight gain, which was about 3% versus 4% in the placebo group. The mean change in weight was 1.5 kg (3.3 lb) and 1.1 kg (2.4 lb), respectively.
Dr. Lieberman praised the manufacturer for undertaking the study.
“In an era when Big Pharma has retreated to a considerable degree from psychotropic drug development, it’s commendable that some companies have stayed the course and are succeeding in drug development,” he said.
Exciting mechanism
Commenting on the findings in an interview, Thomas Sedlak, MD, PhD, director of the Schizophrenia and Psychosis Consult Clinic and assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, called some aspects of the study “exciting.”
What’s especially important is that the novel agent “acts by a different mechanism than what we have been using for maybe 60 years,” said Dr. Sedlak, who was not involved with the research.
“There has been a lot of research in the last few decades into drugs that might act by alternate mechanisms of action, but nothing’s really gotten to market for schizophrenia,” he noted.
Another interesting aspect of the study is that it examined a combination drug that aims to maximize effects on the brain while minimizing periphery effects, Dr. Sedlak said.
In addition, he called the PANSS results “respectable.”
“It’s interesting that you get a big change in PANSS total score, but it’s not as big in the positive symptom score as you might have expected, and it’s not a huge drop in negative symptoms either,” said Dr. Sedlak.
It’s possible, he said, that the drug is targeting PANSS elements not captured in the main positive or negative symptom items; for example, anxiety, depression, guilt, attention, impulse control, disorientation, and judgment.
Dr. Sedlak noted that, while the new results are exciting, the enthusiasm may not be long-lasting. “When a new drug comes out, there’s often a lot of excitement about it, but once you start using it, expectations may deflate..
“More flexible ratios” of the two components of the drug might be useful to treat individual patients, he added.
In addition, using the components by themselves might be preferable for some clinicians. “I think a lot of physicians prefer using two separate drugs so they can alter the dose of each one independently and not be stuck with the ratio the manufacturer is providing,” Dr. Sedlak said.
However, he acknowledged that studying different choices of ratios would require much larger trials.
The study was supported by Karuna Therapeutics and the Wellcome Trust. Dr. Lieberman reported serving on an advisory board for Karuna Therapeutics and Intra-Cellular Therapies. Dr. Sedlak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Loss of smell lingers post COVID-19
The findings illustrate that olfactory problems are common not only during the acute COVID-19 phase but also “in the long run” and that these problems should be “taken into consideration” when following up these patients, study investigator Johannes Frasnelli, MD, professor, department of anatomy, Université du Québec à Trois-Rivières, said in an interview.
Loss of the sense of smell can affect quality of life because it affects eating and drinking, and may even be dangerous, said Dr. Frasnelli. “If your sense of smell is impaired, you may unknowingly eat spoiled food, or you may not smell smoke or gas in your home,” he said. In addition, Dr. Frasnelli noted that an impaired sense of smell is associated with higher rates of depression. The findings will be presented at the annual meeting of the American Academy of Neurology in April.
‘Striking’ finding
Research shows that about 60% of patients with COVID-19 lose their sense of smell to some degree during the acute phase of the disease. “But we wanted to go further and look at the longer-term effects of loss of smell and taste,” said Dr. Frasnelli.
The analysis included 813 health care workers in the province of Quebec. For all the patients, SARS-CoV-2 infection was confirmed through testing with a nasopharyngeal viral swab.
Participants completed a 64-item online questionnaire that asked about three senses: olfactory; gustatory, which includes tastes such as sweet, sour, bitter, salty, savory and umami; and trigeminal, which includes sensations such as spiciness of hot peppers and “coolness” of mint.
They were asked to rate these on a scale of 0 (no perception) to 10 (very strong perception) before the infection, during the infection, and currently. They were also asked about other symptoms, including fatigue.
Most respondents had been infected in the first wave of the virus in March and April of 2020 and responded to the questionnaire an average of 5 months later.
The vast majority of respondents (84.1%) were women, which Dr. Frasnelli said was not surprising because women predominate in the health care field.
The analysis showed that average smell ratings were 8.98 before infection, 2.85 during the acute phase, and 7.41 when respondents answered the questionnaire. The sense of taste was less affected and recovered faster than did the sense of smell. Results for taste were 9.20 before infection, 3.59 during the acute phase, and 8.05 after COVID-19.
Among 580 respondents who indicated a compromised sense of smell during the acute phase, the average smell rating when answering the questionnaire was 6.89, compared to 9.03 before the infection. More than half (51.2%) reported not regaining full olfactory function.
The fact that the sense of smell had not returned to normal for half the participants so long after being infected is “novel and quite striking,” said Dr. Frasnelli.
However, he noted, this doesn’t necessarily mean all those with a compromised sense of smell “have huge problems.” In some cases, he said, the problem “is more subtle.”
Not a CNS problem?
Respondents also completed a chemosensory dysfunction home test (CD-HT). They were asked to prepare common household food items, such as peanut butter, sugar, salt, and vinegar, in a particular way – for example, to add sugar or salt to water – and provide feedback on how they smell and taste.
For this CD-HT analysis, 18.4% of respondents reported having persistent loss of smell. This, Dr. Frasnelli said, adds to evidence from self-reported responses and suggests that in some cases, the problem is more than senses not returning to normal.
“From the questionnaires, roughly 50% said their sense of smell is still not back to normal, and when we look at the CD home test, we see that almost 20% of subjects indeed have pretty strong impairment of their sense of smell,” he said.
The results showed no sex differences, although Dr. Frasnelli noted that most of the sample were women. “It’s tricky to look at the data with regard to sex because it’s a bit skewed,” he said.
Male respondents were older than female participants, but there was no difference in impairment between age groups. Dr. Frasnelli said this was “quite interesting,” inasmuch as older people usually lose some sense of smell.
The researchers have not yet examined whether the results differ by type of health care worker.
They also have not examined in detail whether infection severity affects the risk for extended olfactory impairment. Although some research suggests that the problem with smell is more common in less severe cases, Dr. Frasnelli noted this could be because loss of smell is not a huge problem for patients battling grave health problems.
As for other symptoms, many respondents reported lingering fatigue; some reported debilitating fatigue, said Dr. Frasnelli. However, he cautioned that this is difficult to interpret, because the participants were health care workers, many of whom returned to work during the pandemic and perhaps had not fully rested.
He also noted that he and his colleagues have not “made the link” between impaired smell and the degree of fatigue.
The COVID-19 virus appears to attack supporting sustentacular cells in the olfactory epithelium, not nerve cells.
“Right now, it seems that the smell problem is not a central nervous system problem but a peripheral problem,” said Dr. Frasnelli. “But we don’t know for sure; it may be that the virus somehow gets into the brain and some symptoms are caused by the effects of the infection on the brain.”
The researchers will extend their research with another questionnaire to assess senses 10-12 months after COVID-19.
Limitations of the study include the subjective nature of the smell and taste ratings and the single time point at which data were collected.
Confirmatory findings
Commenting on the research in an interview, Thomas Hummel, MD, professor, smell and taste clinic, department of otorhinolaryngology, Technische Universität Dresden (Germany), said the new results regarding loss of smell after COVID-19 are “very congruent” with what he and his colleagues have observed.
Research shows that up to one in five of those infected with SARS-CoV-2 experience olfactory loss. “While the numbers may vary a bit from study to study or lab to lab, I think 5% to 20% of post–COVID-19 patients exhibit long-term olfactory loss,” Dr. Hummel said.
His group has observed that “many more are not back to normal,” which conforms with what Dr. Frasnelli’s study reveals, said Dr. Hummel.
Also commenting on the research, Kenneth L. Tyler, MD, professor of neurology, University of Colorado at Denver, Aurora, and a fellow of the American Academy of Neurology, said the study was relatively large and the results “interesting.”
Although it “provides more evidence there’s a subset of patients with symptoms even well past the acute phase” of COVID-19, the results are “mostly confirmatory” and include “nothing super surprising,” Dr. Tyler said in an interview.
However, the investigators did attempt to make the study “a little more quantitative” and “to confirm the self-reporting with their validated CD home test,” he said.
Dr. Tyler wondered how representative the sample was and whether the study drew more participants with impaired senses. “If I had a loss of smell or taste, maybe I would be more likely to respond to such a survey,” he said.
He also noted the difficulty of separating loss of smell from loss of taste.
“If you lose your sense of smell, things don’t taste right, so it can be confounding as to how to separate out those two,” he noted.
The study was supported by the Foundation of the Université du Québec à Trois-Rivières and the Province of Quebec. Dr. Frasnelli has received royalties from Styriabooks in Austria for a book on olfaction published in 2019 and has received honoraria for speaking engagements. Dr. Hummel and Dr. Tyler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The findings illustrate that olfactory problems are common not only during the acute COVID-19 phase but also “in the long run” and that these problems should be “taken into consideration” when following up these patients, study investigator Johannes Frasnelli, MD, professor, department of anatomy, Université du Québec à Trois-Rivières, said in an interview.
Loss of the sense of smell can affect quality of life because it affects eating and drinking, and may even be dangerous, said Dr. Frasnelli. “If your sense of smell is impaired, you may unknowingly eat spoiled food, or you may not smell smoke or gas in your home,” he said. In addition, Dr. Frasnelli noted that an impaired sense of smell is associated with higher rates of depression. The findings will be presented at the annual meeting of the American Academy of Neurology in April.
‘Striking’ finding
Research shows that about 60% of patients with COVID-19 lose their sense of smell to some degree during the acute phase of the disease. “But we wanted to go further and look at the longer-term effects of loss of smell and taste,” said Dr. Frasnelli.
The analysis included 813 health care workers in the province of Quebec. For all the patients, SARS-CoV-2 infection was confirmed through testing with a nasopharyngeal viral swab.
Participants completed a 64-item online questionnaire that asked about three senses: olfactory; gustatory, which includes tastes such as sweet, sour, bitter, salty, savory and umami; and trigeminal, which includes sensations such as spiciness of hot peppers and “coolness” of mint.
They were asked to rate these on a scale of 0 (no perception) to 10 (very strong perception) before the infection, during the infection, and currently. They were also asked about other symptoms, including fatigue.
Most respondents had been infected in the first wave of the virus in March and April of 2020 and responded to the questionnaire an average of 5 months later.
The vast majority of respondents (84.1%) were women, which Dr. Frasnelli said was not surprising because women predominate in the health care field.
The analysis showed that average smell ratings were 8.98 before infection, 2.85 during the acute phase, and 7.41 when respondents answered the questionnaire. The sense of taste was less affected and recovered faster than did the sense of smell. Results for taste were 9.20 before infection, 3.59 during the acute phase, and 8.05 after COVID-19.
Among 580 respondents who indicated a compromised sense of smell during the acute phase, the average smell rating when answering the questionnaire was 6.89, compared to 9.03 before the infection. More than half (51.2%) reported not regaining full olfactory function.
The fact that the sense of smell had not returned to normal for half the participants so long after being infected is “novel and quite striking,” said Dr. Frasnelli.
However, he noted, this doesn’t necessarily mean all those with a compromised sense of smell “have huge problems.” In some cases, he said, the problem “is more subtle.”
Not a CNS problem?
Respondents also completed a chemosensory dysfunction home test (CD-HT). They were asked to prepare common household food items, such as peanut butter, sugar, salt, and vinegar, in a particular way – for example, to add sugar or salt to water – and provide feedback on how they smell and taste.
For this CD-HT analysis, 18.4% of respondents reported having persistent loss of smell. This, Dr. Frasnelli said, adds to evidence from self-reported responses and suggests that in some cases, the problem is more than senses not returning to normal.
“From the questionnaires, roughly 50% said their sense of smell is still not back to normal, and when we look at the CD home test, we see that almost 20% of subjects indeed have pretty strong impairment of their sense of smell,” he said.
The results showed no sex differences, although Dr. Frasnelli noted that most of the sample were women. “It’s tricky to look at the data with regard to sex because it’s a bit skewed,” he said.
Male respondents were older than female participants, but there was no difference in impairment between age groups. Dr. Frasnelli said this was “quite interesting,” inasmuch as older people usually lose some sense of smell.
The researchers have not yet examined whether the results differ by type of health care worker.
They also have not examined in detail whether infection severity affects the risk for extended olfactory impairment. Although some research suggests that the problem with smell is more common in less severe cases, Dr. Frasnelli noted this could be because loss of smell is not a huge problem for patients battling grave health problems.
As for other symptoms, many respondents reported lingering fatigue; some reported debilitating fatigue, said Dr. Frasnelli. However, he cautioned that this is difficult to interpret, because the participants were health care workers, many of whom returned to work during the pandemic and perhaps had not fully rested.
He also noted that he and his colleagues have not “made the link” between impaired smell and the degree of fatigue.
The COVID-19 virus appears to attack supporting sustentacular cells in the olfactory epithelium, not nerve cells.
“Right now, it seems that the smell problem is not a central nervous system problem but a peripheral problem,” said Dr. Frasnelli. “But we don’t know for sure; it may be that the virus somehow gets into the brain and some symptoms are caused by the effects of the infection on the brain.”
The researchers will extend their research with another questionnaire to assess senses 10-12 months after COVID-19.
Limitations of the study include the subjective nature of the smell and taste ratings and the single time point at which data were collected.
Confirmatory findings
Commenting on the research in an interview, Thomas Hummel, MD, professor, smell and taste clinic, department of otorhinolaryngology, Technische Universität Dresden (Germany), said the new results regarding loss of smell after COVID-19 are “very congruent” with what he and his colleagues have observed.
Research shows that up to one in five of those infected with SARS-CoV-2 experience olfactory loss. “While the numbers may vary a bit from study to study or lab to lab, I think 5% to 20% of post–COVID-19 patients exhibit long-term olfactory loss,” Dr. Hummel said.
His group has observed that “many more are not back to normal,” which conforms with what Dr. Frasnelli’s study reveals, said Dr. Hummel.
Also commenting on the research, Kenneth L. Tyler, MD, professor of neurology, University of Colorado at Denver, Aurora, and a fellow of the American Academy of Neurology, said the study was relatively large and the results “interesting.”
Although it “provides more evidence there’s a subset of patients with symptoms even well past the acute phase” of COVID-19, the results are “mostly confirmatory” and include “nothing super surprising,” Dr. Tyler said in an interview.
However, the investigators did attempt to make the study “a little more quantitative” and “to confirm the self-reporting with their validated CD home test,” he said.
Dr. Tyler wondered how representative the sample was and whether the study drew more participants with impaired senses. “If I had a loss of smell or taste, maybe I would be more likely to respond to such a survey,” he said.
He also noted the difficulty of separating loss of smell from loss of taste.
“If you lose your sense of smell, things don’t taste right, so it can be confounding as to how to separate out those two,” he noted.
The study was supported by the Foundation of the Université du Québec à Trois-Rivières and the Province of Quebec. Dr. Frasnelli has received royalties from Styriabooks in Austria for a book on olfaction published in 2019 and has received honoraria for speaking engagements. Dr. Hummel and Dr. Tyler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The findings illustrate that olfactory problems are common not only during the acute COVID-19 phase but also “in the long run” and that these problems should be “taken into consideration” when following up these patients, study investigator Johannes Frasnelli, MD, professor, department of anatomy, Université du Québec à Trois-Rivières, said in an interview.
Loss of the sense of smell can affect quality of life because it affects eating and drinking, and may even be dangerous, said Dr. Frasnelli. “If your sense of smell is impaired, you may unknowingly eat spoiled food, or you may not smell smoke or gas in your home,” he said. In addition, Dr. Frasnelli noted that an impaired sense of smell is associated with higher rates of depression. The findings will be presented at the annual meeting of the American Academy of Neurology in April.
‘Striking’ finding
Research shows that about 60% of patients with COVID-19 lose their sense of smell to some degree during the acute phase of the disease. “But we wanted to go further and look at the longer-term effects of loss of smell and taste,” said Dr. Frasnelli.
The analysis included 813 health care workers in the province of Quebec. For all the patients, SARS-CoV-2 infection was confirmed through testing with a nasopharyngeal viral swab.
Participants completed a 64-item online questionnaire that asked about three senses: olfactory; gustatory, which includes tastes such as sweet, sour, bitter, salty, savory and umami; and trigeminal, which includes sensations such as spiciness of hot peppers and “coolness” of mint.
They were asked to rate these on a scale of 0 (no perception) to 10 (very strong perception) before the infection, during the infection, and currently. They were also asked about other symptoms, including fatigue.
Most respondents had been infected in the first wave of the virus in March and April of 2020 and responded to the questionnaire an average of 5 months later.
The vast majority of respondents (84.1%) were women, which Dr. Frasnelli said was not surprising because women predominate in the health care field.
The analysis showed that average smell ratings were 8.98 before infection, 2.85 during the acute phase, and 7.41 when respondents answered the questionnaire. The sense of taste was less affected and recovered faster than did the sense of smell. Results for taste were 9.20 before infection, 3.59 during the acute phase, and 8.05 after COVID-19.
Among 580 respondents who indicated a compromised sense of smell during the acute phase, the average smell rating when answering the questionnaire was 6.89, compared to 9.03 before the infection. More than half (51.2%) reported not regaining full olfactory function.
The fact that the sense of smell had not returned to normal for half the participants so long after being infected is “novel and quite striking,” said Dr. Frasnelli.
However, he noted, this doesn’t necessarily mean all those with a compromised sense of smell “have huge problems.” In some cases, he said, the problem “is more subtle.”
Not a CNS problem?
Respondents also completed a chemosensory dysfunction home test (CD-HT). They were asked to prepare common household food items, such as peanut butter, sugar, salt, and vinegar, in a particular way – for example, to add sugar or salt to water – and provide feedback on how they smell and taste.
For this CD-HT analysis, 18.4% of respondents reported having persistent loss of smell. This, Dr. Frasnelli said, adds to evidence from self-reported responses and suggests that in some cases, the problem is more than senses not returning to normal.
“From the questionnaires, roughly 50% said their sense of smell is still not back to normal, and when we look at the CD home test, we see that almost 20% of subjects indeed have pretty strong impairment of their sense of smell,” he said.
The results showed no sex differences, although Dr. Frasnelli noted that most of the sample were women. “It’s tricky to look at the data with regard to sex because it’s a bit skewed,” he said.
Male respondents were older than female participants, but there was no difference in impairment between age groups. Dr. Frasnelli said this was “quite interesting,” inasmuch as older people usually lose some sense of smell.
The researchers have not yet examined whether the results differ by type of health care worker.
They also have not examined in detail whether infection severity affects the risk for extended olfactory impairment. Although some research suggests that the problem with smell is more common in less severe cases, Dr. Frasnelli noted this could be because loss of smell is not a huge problem for patients battling grave health problems.
As for other symptoms, many respondents reported lingering fatigue; some reported debilitating fatigue, said Dr. Frasnelli. However, he cautioned that this is difficult to interpret, because the participants were health care workers, many of whom returned to work during the pandemic and perhaps had not fully rested.
He also noted that he and his colleagues have not “made the link” between impaired smell and the degree of fatigue.
The COVID-19 virus appears to attack supporting sustentacular cells in the olfactory epithelium, not nerve cells.
“Right now, it seems that the smell problem is not a central nervous system problem but a peripheral problem,” said Dr. Frasnelli. “But we don’t know for sure; it may be that the virus somehow gets into the brain and some symptoms are caused by the effects of the infection on the brain.”
The researchers will extend their research with another questionnaire to assess senses 10-12 months after COVID-19.
Limitations of the study include the subjective nature of the smell and taste ratings and the single time point at which data were collected.
Confirmatory findings
Commenting on the research in an interview, Thomas Hummel, MD, professor, smell and taste clinic, department of otorhinolaryngology, Technische Universität Dresden (Germany), said the new results regarding loss of smell after COVID-19 are “very congruent” with what he and his colleagues have observed.
Research shows that up to one in five of those infected with SARS-CoV-2 experience olfactory loss. “While the numbers may vary a bit from study to study or lab to lab, I think 5% to 20% of post–COVID-19 patients exhibit long-term olfactory loss,” Dr. Hummel said.
His group has observed that “many more are not back to normal,” which conforms with what Dr. Frasnelli’s study reveals, said Dr. Hummel.
Also commenting on the research, Kenneth L. Tyler, MD, professor of neurology, University of Colorado at Denver, Aurora, and a fellow of the American Academy of Neurology, said the study was relatively large and the results “interesting.”
Although it “provides more evidence there’s a subset of patients with symptoms even well past the acute phase” of COVID-19, the results are “mostly confirmatory” and include “nothing super surprising,” Dr. Tyler said in an interview.
However, the investigators did attempt to make the study “a little more quantitative” and “to confirm the self-reporting with their validated CD home test,” he said.
Dr. Tyler wondered how representative the sample was and whether the study drew more participants with impaired senses. “If I had a loss of smell or taste, maybe I would be more likely to respond to such a survey,” he said.
He also noted the difficulty of separating loss of smell from loss of taste.
“If you lose your sense of smell, things don’t taste right, so it can be confounding as to how to separate out those two,” he noted.
The study was supported by the Foundation of the Université du Québec à Trois-Rivières and the Province of Quebec. Dr. Frasnelli has received royalties from Styriabooks in Austria for a book on olfaction published in 2019 and has received honoraria for speaking engagements. Dr. Hummel and Dr. Tyler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
National spike in methamphetamine overdose deaths
The national rate of methamphetamine overdose deaths shot up significantly between 2011 and 2018, particularly among non-Hispanic American Indian and Alaska Native communities, new research shows.
Rates rose for both men and women but more so among men, the study found. The spike in these deaths underscores the need for culturally tailored prevention and treatment strategies, the study authors said.
“While much attention is focused on the opioid crisis, a methamphetamine crisis has been quietly, but actively, gaining steam – particularly among American Indians and Alaska Natives, who are disproportionately affected by a number of health conditions,” senior investigator Nora D. Volkow, MD, director of the National Institute on Drug Abuse, said in a press release.
The study was published online Jan. 20 in JAMA Psychiatry.
Highly toxic
Methamphetamine is highly toxic. Its use is associated with pulmonary and cardiovascular pathology and frequently co-occurs with other substance use and mental disorders.
In addition, there are currently no Food and Drug Administration–approved medications to reverse methamphetamine overdose or treat methamphetamine use disorder.
However, In addition, a recent clinical trial reported significant therapeutic benefits with the combination of naltrexone with bupropion in patients with methamphetamine use disorder.
For the study, the investigators used deidentified public health surveillance data from the Centers for Disease Control and Prevention’s National Vital Statistics System files for multiple causes of death.
The researchers used the psychostimulant category to estimate death rates from methamphetamine. The authors noted that up to 90% of psychostimulant-involved death certificates mentioned methamphetamine.
Researchers stratified age-adjusted overdose death rates during 2011-2018 by sex and race/ethnicity and limited the analysis to those aged 25-54 years. Approximately 80% of methamphetamine users are between the ages of 25 and 54 years.
During the study period, rates for methamphetamine-involved deaths increased from 1.8 to 10.1 per 100,000 among men (average annual percentage change, 29.1; 95% confidence interval, 25.5-32.8; P < .001) and from 0.8 to 4.5 per 100,000 among women (AAPC, 28.1; 95% CI, 25.1-31.2; P < .001).
Need for tailored interventions
For both men and women, those in non-Hispanic American Indian or Alaska Native communities had the highest rates. These increased from 5.6 to 26.4 per 100,000 among men and from 3.6 to 15.6 per 100,000 among women.
While American Indian and Alaska Native individuals experience sociostructural disadvantages, their cultural strengths “can be leveraged to improve addiction outcomes,” the investigators wrote.
Non-Hispanic Whites had the second highest rates. These rose from 2.2 to 12.6 per 100,000 among men (AAPC, 29.8; 95% CI, 24.3-35.4; P < .001) and from 1.1 to 6.2 per 100,000 among women (AAPC, 29.1; 95% CI, 25.2-33.2; P < .001).
Rates among Hispanic individuals increased from 1.4 to 6.6 per 100,000 for men and from 0.5 to 2.0 per 100,000 for women. Among non-Hispanic Asian individuals, rates increased to 3.4 per 100,000 for men and to 1.1 per 100,000 for women. Non-Hispanic Black individuals had low rates. Within each racial/ethnic group, rates were higher among men versus women.
Methamphetamine death rates may be underestimated because some overdose death certificates do not report specific drugs involved, the authors noted.
Identifying populations that have a higher rate of methamphetamine overdose is a crucial step toward curbing the underlying methamphetamine crisis,” study author Beth Han, MD, PhD, of NIDA, said in a press release.
“By focusing on the unique needs of individuals and developing culturally tailored interventions, we can begin to move away from one-size-fits-all approaches and toward more effective, tailored interventions,” she said.
The study was sponsored by NIDA.
A version of this article first appeared on Medscape.com.
The national rate of methamphetamine overdose deaths shot up significantly between 2011 and 2018, particularly among non-Hispanic American Indian and Alaska Native communities, new research shows.
Rates rose for both men and women but more so among men, the study found. The spike in these deaths underscores the need for culturally tailored prevention and treatment strategies, the study authors said.
“While much attention is focused on the opioid crisis, a methamphetamine crisis has been quietly, but actively, gaining steam – particularly among American Indians and Alaska Natives, who are disproportionately affected by a number of health conditions,” senior investigator Nora D. Volkow, MD, director of the National Institute on Drug Abuse, said in a press release.
The study was published online Jan. 20 in JAMA Psychiatry.
Highly toxic
Methamphetamine is highly toxic. Its use is associated with pulmonary and cardiovascular pathology and frequently co-occurs with other substance use and mental disorders.
In addition, there are currently no Food and Drug Administration–approved medications to reverse methamphetamine overdose or treat methamphetamine use disorder.
However, In addition, a recent clinical trial reported significant therapeutic benefits with the combination of naltrexone with bupropion in patients with methamphetamine use disorder.
For the study, the investigators used deidentified public health surveillance data from the Centers for Disease Control and Prevention’s National Vital Statistics System files for multiple causes of death.
The researchers used the psychostimulant category to estimate death rates from methamphetamine. The authors noted that up to 90% of psychostimulant-involved death certificates mentioned methamphetamine.
Researchers stratified age-adjusted overdose death rates during 2011-2018 by sex and race/ethnicity and limited the analysis to those aged 25-54 years. Approximately 80% of methamphetamine users are between the ages of 25 and 54 years.
During the study period, rates for methamphetamine-involved deaths increased from 1.8 to 10.1 per 100,000 among men (average annual percentage change, 29.1; 95% confidence interval, 25.5-32.8; P < .001) and from 0.8 to 4.5 per 100,000 among women (AAPC, 28.1; 95% CI, 25.1-31.2; P < .001).
Need for tailored interventions
For both men and women, those in non-Hispanic American Indian or Alaska Native communities had the highest rates. These increased from 5.6 to 26.4 per 100,000 among men and from 3.6 to 15.6 per 100,000 among women.
While American Indian and Alaska Native individuals experience sociostructural disadvantages, their cultural strengths “can be leveraged to improve addiction outcomes,” the investigators wrote.
Non-Hispanic Whites had the second highest rates. These rose from 2.2 to 12.6 per 100,000 among men (AAPC, 29.8; 95% CI, 24.3-35.4; P < .001) and from 1.1 to 6.2 per 100,000 among women (AAPC, 29.1; 95% CI, 25.2-33.2; P < .001).
Rates among Hispanic individuals increased from 1.4 to 6.6 per 100,000 for men and from 0.5 to 2.0 per 100,000 for women. Among non-Hispanic Asian individuals, rates increased to 3.4 per 100,000 for men and to 1.1 per 100,000 for women. Non-Hispanic Black individuals had low rates. Within each racial/ethnic group, rates were higher among men versus women.
Methamphetamine death rates may be underestimated because some overdose death certificates do not report specific drugs involved, the authors noted.
Identifying populations that have a higher rate of methamphetamine overdose is a crucial step toward curbing the underlying methamphetamine crisis,” study author Beth Han, MD, PhD, of NIDA, said in a press release.
“By focusing on the unique needs of individuals and developing culturally tailored interventions, we can begin to move away from one-size-fits-all approaches and toward more effective, tailored interventions,” she said.
The study was sponsored by NIDA.
A version of this article first appeared on Medscape.com.
The national rate of methamphetamine overdose deaths shot up significantly between 2011 and 2018, particularly among non-Hispanic American Indian and Alaska Native communities, new research shows.
Rates rose for both men and women but more so among men, the study found. The spike in these deaths underscores the need for culturally tailored prevention and treatment strategies, the study authors said.
“While much attention is focused on the opioid crisis, a methamphetamine crisis has been quietly, but actively, gaining steam – particularly among American Indians and Alaska Natives, who are disproportionately affected by a number of health conditions,” senior investigator Nora D. Volkow, MD, director of the National Institute on Drug Abuse, said in a press release.
The study was published online Jan. 20 in JAMA Psychiatry.
Highly toxic
Methamphetamine is highly toxic. Its use is associated with pulmonary and cardiovascular pathology and frequently co-occurs with other substance use and mental disorders.
In addition, there are currently no Food and Drug Administration–approved medications to reverse methamphetamine overdose or treat methamphetamine use disorder.
However, In addition, a recent clinical trial reported significant therapeutic benefits with the combination of naltrexone with bupropion in patients with methamphetamine use disorder.
For the study, the investigators used deidentified public health surveillance data from the Centers for Disease Control and Prevention’s National Vital Statistics System files for multiple causes of death.
The researchers used the psychostimulant category to estimate death rates from methamphetamine. The authors noted that up to 90% of psychostimulant-involved death certificates mentioned methamphetamine.
Researchers stratified age-adjusted overdose death rates during 2011-2018 by sex and race/ethnicity and limited the analysis to those aged 25-54 years. Approximately 80% of methamphetamine users are between the ages of 25 and 54 years.
During the study period, rates for methamphetamine-involved deaths increased from 1.8 to 10.1 per 100,000 among men (average annual percentage change, 29.1; 95% confidence interval, 25.5-32.8; P < .001) and from 0.8 to 4.5 per 100,000 among women (AAPC, 28.1; 95% CI, 25.1-31.2; P < .001).
Need for tailored interventions
For both men and women, those in non-Hispanic American Indian or Alaska Native communities had the highest rates. These increased from 5.6 to 26.4 per 100,000 among men and from 3.6 to 15.6 per 100,000 among women.
While American Indian and Alaska Native individuals experience sociostructural disadvantages, their cultural strengths “can be leveraged to improve addiction outcomes,” the investigators wrote.
Non-Hispanic Whites had the second highest rates. These rose from 2.2 to 12.6 per 100,000 among men (AAPC, 29.8; 95% CI, 24.3-35.4; P < .001) and from 1.1 to 6.2 per 100,000 among women (AAPC, 29.1; 95% CI, 25.2-33.2; P < .001).
Rates among Hispanic individuals increased from 1.4 to 6.6 per 100,000 for men and from 0.5 to 2.0 per 100,000 for women. Among non-Hispanic Asian individuals, rates increased to 3.4 per 100,000 for men and to 1.1 per 100,000 for women. Non-Hispanic Black individuals had low rates. Within each racial/ethnic group, rates were higher among men versus women.
Methamphetamine death rates may be underestimated because some overdose death certificates do not report specific drugs involved, the authors noted.
Identifying populations that have a higher rate of methamphetamine overdose is a crucial step toward curbing the underlying methamphetamine crisis,” study author Beth Han, MD, PhD, of NIDA, said in a press release.
“By focusing on the unique needs of individuals and developing culturally tailored interventions, we can begin to move away from one-size-fits-all approaches and toward more effective, tailored interventions,” she said.
The study was sponsored by NIDA.
A version of this article first appeared on Medscape.com.
Bedside EEG test aids prognosis in patients with brain injury
results of a new study suggest. The study showed that the use of a paradigm that measures the strength of responses to speech improved the accuracy of prognosis for these patients, compared with prognoses made solely on the basis of standard clinical characteristics.
“What we found is really compelling evidence” of the usefulness of the test, lead study author Rodika Sokoliuk, PhD, a postdoctoral researcher at the Center for Human Brain Health, University of Birmingham (England), said in an interview.
The passive measure of comprehension, which doesn’t require any other response from the patient, can reduce uncertainty at a critical phase of decision-making in the ICU, said Dr. Sokoliuk.
The study was published online Dec. 23, 2020, in Annals of Neurology.
Useful information at a time of ‘considerable prognostic uncertainty’
Accurate, early prognostication is vital for efficient stratification of patients after a TBI, the authors wrote. This can often be achieved from patient behavior and CT at admission, but some patients continue to fail to obey commands after washout of sedation.
These patients pose a significant challenge for neurologic prognostication, they noted. In these cases, clinicians and families must decide whether to “wait and see” or consider treatment withdrawal.
The authors noted that a lack of command following early in the postsedation period is associated with poor outcome, including vegetative state/unresponsive wakefulness syndrome (VS/UWS). This, they said, represents a “window of opportunity” for cessation of life-sustaining therapy at a time of considerable prognostic uncertainty.
Recent research shows that a significant proportion of unresponsive patients retain a level of cognition, and even consciousness, that isn’t evident from their external behavior – the so-called cognitive-motor dissociation.
The new study included 28 adult patients who had experienced a TBI and were admitted to the ICU of the Queen Elizabeth Hospital in Birmingham, England. The patients had a Glasgow Coma Scale motor score less than 6 (i.e., they were incapable of obeying commands). They had been sedation free for 2-7 days.
For the paradigm, researchers constructed 288 English words using the male voice of the Apple synthesizer. The words required the same amount of time to be generated (320 ms) and were monosyllabic, so the rhythms of the sounds were the same.
The words were presented in a specific order: an adjective, then a noun, then a verb, then a noun. Two words – for example, an adjective and noun – “would build a meaningful phrase,” and four words would build a sentence, said Dr. Sokoliuk.
The researchers built 72 of these four-word sentences. A trial comprised 12 of these sentences, resulting in a total of 864 four-word sentences.
Dr. Sokoliuk likened the paradigm to a rap song with a specific beat that is continually repeated. “Basically, we play 12 of these four-word sentences in a row, without any gaps,” she said.
Each sentence was played to patients, in random order, a minimum of eight and a maximum of nine times per patient throughout the experiment. The patients’ brain activity was recorded on EEG.
Dr. Sokoliuk noted that brain activity in healthy people synchronizes only with the rhythm of phrases and sentences when listeners consciously comprehend the speech. The researchers assessed the level of comprehension in the unresponsive patients by measuring the strength of this synchronicity or brain pattern.
After exclusions, 17 patients were available for outcome assessment 3 months post EEG, and 16 patients were available 6 months post EEG.
The analysis showed that outcome significantly correlated with the strength of patients’ acute cortical tracking of phrases and sentences (r > 0.6; P < .007), quantified by intertrial phase coherence.
Linear regressions revealed that the strength of this comprehension response (beta, 0.603; P = .006) significantly improved the accuracy of prognoses relative to clinical characteristics alone, such as the Glasgow Coma Scale or CT grade.
Previous studies showed that, if there is no understanding of the language used or if the subject is asleep, the brain doesn’t have the “signature” of tracking phrases and sentences, so it doesn’t have the synchronicity or the pattern of individuals with normal cognition, said Dr. Sokoliuk.
“You need a certain level of consciousness, and you need to understand the language, so your brain can actually track sentences or phrases,” she said.
Dr. Sokoliuk explained that the paradigm shows that patients are understanding the sentences and are not just hearing them.
“It’s not showing us that they only hear it, because there are no obvious gaps between the sentences; if there were gaps between sentences, it would probably only show that they hear it. It could be both, that they hear and understand it, but we wouldn’t know.”
A receiver operating characteristics analysis indicated 100% sensitivity and 80% specificity for a distinction between bad outcome (death, VS/UWS) and good outcome at 6 months.
“We could actually define a threshold of the tracking,” said Dr. Sokoliuk. “Patients who had phrases and sentences tracking below this threshold had worse outcome than those whose tracking value was above this threshold.”
The study illustrates that some posttraumatic patients who remain in an unresponsive state despite being sedation free may nevertheless comprehend speech.
The EEG paradigm approach, the authors said, may significantly reduce prognostic uncertainty in a critical phase of medical decision-making. It could also help clinicians make more appropriate decisions about whether or not to continue life-sustaining therapy and ensure more appropriate distribution of limited rehabilitation resources to patients most likely to benefit.
Dr. Sokoliuk stressed that the paradigm could be used at the bedside soon after a brain injury. “The critical thing is, we can actually use it during the acute phase, which is very important for clinical decisions about life-sustaining methods, therapy, and long-term care.”
A prognostic tool
The simple approach promises to be more accessible than fMRI, said Dr. Sokoliuk. “Putting an unresponsive coma patient in a scanner is very difficult and also much more expensive,” she said.
The next step, said Dr. Sokoliuk, is to repeat the study with a larger sample. “The number in the current study was quite small, and we can’t say if the sensitivity of the paradigm is strong enough to use it as a standard prognostic tool.”
To use it in clinical setting, “we really have to have robust measures,” she added.
She aims to conduct a collaborative study involving several institutions and more patients.
The research team plans to eventually build “an open-access toolbox” that would include the auditory streams to be played during EEG recordings and a program to analyze the data, said Dr. Sokoliuk. “Then, in the end, you would get a threshold or a value of tracking for phrases and sentences, and this could then classify a patient to be in a good-outcome or in bad-outcome group.”
She stressed this is a prognostic tool, not a diagnostic tool, and it should not be used in isolation. “It’s important to know that no clinician should only use this paradigm to prognosticate a patient; our paradigm should be part of a bigger battery of tests.”
But it could go a long way toward helping families as well as physicians. “If they know that the patient would be better in 3 months’ time, it’s easier for them to decide what should come next,” she said.
And it’s heartening to know that when families talk to their unresponsive loved one, the patient understands them, she added.
Promising basic research
Commenting on the study in an interview, Christine Blume, PhD, of the Center for Chronobiology, University of Basel (Switzerland), whose research interests include cognitive processing of patients with disorders of consciousness, described it as “very elegant and appealing” and the paradigm it used as “really promising.”
“However, we do, of course, not yet know about the prognostic value on a single-subject level, as the authors performed only group analyses,” said Dr. Blume. “This will require more extensive and perhaps even multicenter studies.”
It would also require developing a “solution” that “allows clinicians with limited time resources and perhaps lacking expert knowledge on the paradigm and the necessary analyses to apply the paradigm at bedside,” said Dr. Blume.
She agreed that a passive paradigm that helps determine whether a patient consciously understands speech, without the need for further processing, “has the potential to really improve the diagnostic process and uncover covert consciousness.”
One should bear in mind, though, that the paradigm “makes one essential assumption: that patients can understand speech,” said Dr. Blume. “For example, an aphasic patient might not understand but still be conscious.”
In this context, she added, “it’s essential to note that while the presence of a response suggests consciousness, the absence of a response does not suggest the absence of consciousness.”
Dr. Blume cautioned that the approach used in the study “is still at the stage of basic research.” Although the paradigm is promising, “I do not think it is ‘around the corner,’ ” she said.
The study was funded by the Medical Research Council. It was further supported by the National Institute for Health Research Surgical Reconstruction and Microbiology Research Center. Dr. Sokoliuk and Dr. Blume have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
results of a new study suggest. The study showed that the use of a paradigm that measures the strength of responses to speech improved the accuracy of prognosis for these patients, compared with prognoses made solely on the basis of standard clinical characteristics.
“What we found is really compelling evidence” of the usefulness of the test, lead study author Rodika Sokoliuk, PhD, a postdoctoral researcher at the Center for Human Brain Health, University of Birmingham (England), said in an interview.
The passive measure of comprehension, which doesn’t require any other response from the patient, can reduce uncertainty at a critical phase of decision-making in the ICU, said Dr. Sokoliuk.
The study was published online Dec. 23, 2020, in Annals of Neurology.
Useful information at a time of ‘considerable prognostic uncertainty’
Accurate, early prognostication is vital for efficient stratification of patients after a TBI, the authors wrote. This can often be achieved from patient behavior and CT at admission, but some patients continue to fail to obey commands after washout of sedation.
These patients pose a significant challenge for neurologic prognostication, they noted. In these cases, clinicians and families must decide whether to “wait and see” or consider treatment withdrawal.
The authors noted that a lack of command following early in the postsedation period is associated with poor outcome, including vegetative state/unresponsive wakefulness syndrome (VS/UWS). This, they said, represents a “window of opportunity” for cessation of life-sustaining therapy at a time of considerable prognostic uncertainty.
Recent research shows that a significant proportion of unresponsive patients retain a level of cognition, and even consciousness, that isn’t evident from their external behavior – the so-called cognitive-motor dissociation.
The new study included 28 adult patients who had experienced a TBI and were admitted to the ICU of the Queen Elizabeth Hospital in Birmingham, England. The patients had a Glasgow Coma Scale motor score less than 6 (i.e., they were incapable of obeying commands). They had been sedation free for 2-7 days.
For the paradigm, researchers constructed 288 English words using the male voice of the Apple synthesizer. The words required the same amount of time to be generated (320 ms) and were monosyllabic, so the rhythms of the sounds were the same.
The words were presented in a specific order: an adjective, then a noun, then a verb, then a noun. Two words – for example, an adjective and noun – “would build a meaningful phrase,” and four words would build a sentence, said Dr. Sokoliuk.
The researchers built 72 of these four-word sentences. A trial comprised 12 of these sentences, resulting in a total of 864 four-word sentences.
Dr. Sokoliuk likened the paradigm to a rap song with a specific beat that is continually repeated. “Basically, we play 12 of these four-word sentences in a row, without any gaps,” she said.
Each sentence was played to patients, in random order, a minimum of eight and a maximum of nine times per patient throughout the experiment. The patients’ brain activity was recorded on EEG.
Dr. Sokoliuk noted that brain activity in healthy people synchronizes only with the rhythm of phrases and sentences when listeners consciously comprehend the speech. The researchers assessed the level of comprehension in the unresponsive patients by measuring the strength of this synchronicity or brain pattern.
After exclusions, 17 patients were available for outcome assessment 3 months post EEG, and 16 patients were available 6 months post EEG.
The analysis showed that outcome significantly correlated with the strength of patients’ acute cortical tracking of phrases and sentences (r > 0.6; P < .007), quantified by intertrial phase coherence.
Linear regressions revealed that the strength of this comprehension response (beta, 0.603; P = .006) significantly improved the accuracy of prognoses relative to clinical characteristics alone, such as the Glasgow Coma Scale or CT grade.
Previous studies showed that, if there is no understanding of the language used or if the subject is asleep, the brain doesn’t have the “signature” of tracking phrases and sentences, so it doesn’t have the synchronicity or the pattern of individuals with normal cognition, said Dr. Sokoliuk.
“You need a certain level of consciousness, and you need to understand the language, so your brain can actually track sentences or phrases,” she said.
Dr. Sokoliuk explained that the paradigm shows that patients are understanding the sentences and are not just hearing them.
“It’s not showing us that they only hear it, because there are no obvious gaps between the sentences; if there were gaps between sentences, it would probably only show that they hear it. It could be both, that they hear and understand it, but we wouldn’t know.”
A receiver operating characteristics analysis indicated 100% sensitivity and 80% specificity for a distinction between bad outcome (death, VS/UWS) and good outcome at 6 months.
“We could actually define a threshold of the tracking,” said Dr. Sokoliuk. “Patients who had phrases and sentences tracking below this threshold had worse outcome than those whose tracking value was above this threshold.”
The study illustrates that some posttraumatic patients who remain in an unresponsive state despite being sedation free may nevertheless comprehend speech.
The EEG paradigm approach, the authors said, may significantly reduce prognostic uncertainty in a critical phase of medical decision-making. It could also help clinicians make more appropriate decisions about whether or not to continue life-sustaining therapy and ensure more appropriate distribution of limited rehabilitation resources to patients most likely to benefit.
Dr. Sokoliuk stressed that the paradigm could be used at the bedside soon after a brain injury. “The critical thing is, we can actually use it during the acute phase, which is very important for clinical decisions about life-sustaining methods, therapy, and long-term care.”
A prognostic tool
The simple approach promises to be more accessible than fMRI, said Dr. Sokoliuk. “Putting an unresponsive coma patient in a scanner is very difficult and also much more expensive,” she said.
The next step, said Dr. Sokoliuk, is to repeat the study with a larger sample. “The number in the current study was quite small, and we can’t say if the sensitivity of the paradigm is strong enough to use it as a standard prognostic tool.”
To use it in clinical setting, “we really have to have robust measures,” she added.
She aims to conduct a collaborative study involving several institutions and more patients.
The research team plans to eventually build “an open-access toolbox” that would include the auditory streams to be played during EEG recordings and a program to analyze the data, said Dr. Sokoliuk. “Then, in the end, you would get a threshold or a value of tracking for phrases and sentences, and this could then classify a patient to be in a good-outcome or in bad-outcome group.”
She stressed this is a prognostic tool, not a diagnostic tool, and it should not be used in isolation. “It’s important to know that no clinician should only use this paradigm to prognosticate a patient; our paradigm should be part of a bigger battery of tests.”
But it could go a long way toward helping families as well as physicians. “If they know that the patient would be better in 3 months’ time, it’s easier for them to decide what should come next,” she said.
And it’s heartening to know that when families talk to their unresponsive loved one, the patient understands them, she added.
Promising basic research
Commenting on the study in an interview, Christine Blume, PhD, of the Center for Chronobiology, University of Basel (Switzerland), whose research interests include cognitive processing of patients with disorders of consciousness, described it as “very elegant and appealing” and the paradigm it used as “really promising.”
“However, we do, of course, not yet know about the prognostic value on a single-subject level, as the authors performed only group analyses,” said Dr. Blume. “This will require more extensive and perhaps even multicenter studies.”
It would also require developing a “solution” that “allows clinicians with limited time resources and perhaps lacking expert knowledge on the paradigm and the necessary analyses to apply the paradigm at bedside,” said Dr. Blume.
She agreed that a passive paradigm that helps determine whether a patient consciously understands speech, without the need for further processing, “has the potential to really improve the diagnostic process and uncover covert consciousness.”
One should bear in mind, though, that the paradigm “makes one essential assumption: that patients can understand speech,” said Dr. Blume. “For example, an aphasic patient might not understand but still be conscious.”
In this context, she added, “it’s essential to note that while the presence of a response suggests consciousness, the absence of a response does not suggest the absence of consciousness.”
Dr. Blume cautioned that the approach used in the study “is still at the stage of basic research.” Although the paradigm is promising, “I do not think it is ‘around the corner,’ ” she said.
The study was funded by the Medical Research Council. It was further supported by the National Institute for Health Research Surgical Reconstruction and Microbiology Research Center. Dr. Sokoliuk and Dr. Blume have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
results of a new study suggest. The study showed that the use of a paradigm that measures the strength of responses to speech improved the accuracy of prognosis for these patients, compared with prognoses made solely on the basis of standard clinical characteristics.
“What we found is really compelling evidence” of the usefulness of the test, lead study author Rodika Sokoliuk, PhD, a postdoctoral researcher at the Center for Human Brain Health, University of Birmingham (England), said in an interview.
The passive measure of comprehension, which doesn’t require any other response from the patient, can reduce uncertainty at a critical phase of decision-making in the ICU, said Dr. Sokoliuk.
The study was published online Dec. 23, 2020, in Annals of Neurology.
Useful information at a time of ‘considerable prognostic uncertainty’
Accurate, early prognostication is vital for efficient stratification of patients after a TBI, the authors wrote. This can often be achieved from patient behavior and CT at admission, but some patients continue to fail to obey commands after washout of sedation.
These patients pose a significant challenge for neurologic prognostication, they noted. In these cases, clinicians and families must decide whether to “wait and see” or consider treatment withdrawal.
The authors noted that a lack of command following early in the postsedation period is associated with poor outcome, including vegetative state/unresponsive wakefulness syndrome (VS/UWS). This, they said, represents a “window of opportunity” for cessation of life-sustaining therapy at a time of considerable prognostic uncertainty.
Recent research shows that a significant proportion of unresponsive patients retain a level of cognition, and even consciousness, that isn’t evident from their external behavior – the so-called cognitive-motor dissociation.
The new study included 28 adult patients who had experienced a TBI and were admitted to the ICU of the Queen Elizabeth Hospital in Birmingham, England. The patients had a Glasgow Coma Scale motor score less than 6 (i.e., they were incapable of obeying commands). They had been sedation free for 2-7 days.
For the paradigm, researchers constructed 288 English words using the male voice of the Apple synthesizer. The words required the same amount of time to be generated (320 ms) and were monosyllabic, so the rhythms of the sounds were the same.
The words were presented in a specific order: an adjective, then a noun, then a verb, then a noun. Two words – for example, an adjective and noun – “would build a meaningful phrase,” and four words would build a sentence, said Dr. Sokoliuk.
The researchers built 72 of these four-word sentences. A trial comprised 12 of these sentences, resulting in a total of 864 four-word sentences.
Dr. Sokoliuk likened the paradigm to a rap song with a specific beat that is continually repeated. “Basically, we play 12 of these four-word sentences in a row, without any gaps,” she said.
Each sentence was played to patients, in random order, a minimum of eight and a maximum of nine times per patient throughout the experiment. The patients’ brain activity was recorded on EEG.
Dr. Sokoliuk noted that brain activity in healthy people synchronizes only with the rhythm of phrases and sentences when listeners consciously comprehend the speech. The researchers assessed the level of comprehension in the unresponsive patients by measuring the strength of this synchronicity or brain pattern.
After exclusions, 17 patients were available for outcome assessment 3 months post EEG, and 16 patients were available 6 months post EEG.
The analysis showed that outcome significantly correlated with the strength of patients’ acute cortical tracking of phrases and sentences (r > 0.6; P < .007), quantified by intertrial phase coherence.
Linear regressions revealed that the strength of this comprehension response (beta, 0.603; P = .006) significantly improved the accuracy of prognoses relative to clinical characteristics alone, such as the Glasgow Coma Scale or CT grade.
Previous studies showed that, if there is no understanding of the language used or if the subject is asleep, the brain doesn’t have the “signature” of tracking phrases and sentences, so it doesn’t have the synchronicity or the pattern of individuals with normal cognition, said Dr. Sokoliuk.
“You need a certain level of consciousness, and you need to understand the language, so your brain can actually track sentences or phrases,” she said.
Dr. Sokoliuk explained that the paradigm shows that patients are understanding the sentences and are not just hearing them.
“It’s not showing us that they only hear it, because there are no obvious gaps between the sentences; if there were gaps between sentences, it would probably only show that they hear it. It could be both, that they hear and understand it, but we wouldn’t know.”
A receiver operating characteristics analysis indicated 100% sensitivity and 80% specificity for a distinction between bad outcome (death, VS/UWS) and good outcome at 6 months.
“We could actually define a threshold of the tracking,” said Dr. Sokoliuk. “Patients who had phrases and sentences tracking below this threshold had worse outcome than those whose tracking value was above this threshold.”
The study illustrates that some posttraumatic patients who remain in an unresponsive state despite being sedation free may nevertheless comprehend speech.
The EEG paradigm approach, the authors said, may significantly reduce prognostic uncertainty in a critical phase of medical decision-making. It could also help clinicians make more appropriate decisions about whether or not to continue life-sustaining therapy and ensure more appropriate distribution of limited rehabilitation resources to patients most likely to benefit.
Dr. Sokoliuk stressed that the paradigm could be used at the bedside soon after a brain injury. “The critical thing is, we can actually use it during the acute phase, which is very important for clinical decisions about life-sustaining methods, therapy, and long-term care.”
A prognostic tool
The simple approach promises to be more accessible than fMRI, said Dr. Sokoliuk. “Putting an unresponsive coma patient in a scanner is very difficult and also much more expensive,” she said.
The next step, said Dr. Sokoliuk, is to repeat the study with a larger sample. “The number in the current study was quite small, and we can’t say if the sensitivity of the paradigm is strong enough to use it as a standard prognostic tool.”
To use it in clinical setting, “we really have to have robust measures,” she added.
She aims to conduct a collaborative study involving several institutions and more patients.
The research team plans to eventually build “an open-access toolbox” that would include the auditory streams to be played during EEG recordings and a program to analyze the data, said Dr. Sokoliuk. “Then, in the end, you would get a threshold or a value of tracking for phrases and sentences, and this could then classify a patient to be in a good-outcome or in bad-outcome group.”
She stressed this is a prognostic tool, not a diagnostic tool, and it should not be used in isolation. “It’s important to know that no clinician should only use this paradigm to prognosticate a patient; our paradigm should be part of a bigger battery of tests.”
But it could go a long way toward helping families as well as physicians. “If they know that the patient would be better in 3 months’ time, it’s easier for them to decide what should come next,” she said.
And it’s heartening to know that when families talk to their unresponsive loved one, the patient understands them, she added.
Promising basic research
Commenting on the study in an interview, Christine Blume, PhD, of the Center for Chronobiology, University of Basel (Switzerland), whose research interests include cognitive processing of patients with disorders of consciousness, described it as “very elegant and appealing” and the paradigm it used as “really promising.”
“However, we do, of course, not yet know about the prognostic value on a single-subject level, as the authors performed only group analyses,” said Dr. Blume. “This will require more extensive and perhaps even multicenter studies.”
It would also require developing a “solution” that “allows clinicians with limited time resources and perhaps lacking expert knowledge on the paradigm and the necessary analyses to apply the paradigm at bedside,” said Dr. Blume.
She agreed that a passive paradigm that helps determine whether a patient consciously understands speech, without the need for further processing, “has the potential to really improve the diagnostic process and uncover covert consciousness.”
One should bear in mind, though, that the paradigm “makes one essential assumption: that patients can understand speech,” said Dr. Blume. “For example, an aphasic patient might not understand but still be conscious.”
In this context, she added, “it’s essential to note that while the presence of a response suggests consciousness, the absence of a response does not suggest the absence of consciousness.”
Dr. Blume cautioned that the approach used in the study “is still at the stage of basic research.” Although the paradigm is promising, “I do not think it is ‘around the corner,’ ” she said.
The study was funded by the Medical Research Council. It was further supported by the National Institute for Health Research Surgical Reconstruction and Microbiology Research Center. Dr. Sokoliuk and Dr. Blume have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF NEUROLOGY
Heavy drinking by teens may affect white-matter integrity
Heavy alcohol use in adolescence is linked to disruptions in white-matter integrity, new research suggests.
In a case-control study of more than 400 participants, the association was more pronounced in younger adolescents and in the anterior and middle corpus callosum, which serve the interhemispheric integration of frontal networking and communication.
The results provide clinicians with yet another reason to ask adolescents about their alcohol use, said investigator Adolf Pfefferbaum, MD, Center for Health Sciences, SRI International, Menlo Park, Calif., and professor emeritus at Stanford (Calif.) University.
However, when questioning adolescents about their alcohol use, “sometimes it’s better to ask: ‘How much alcohol do you drink?’ ” instead of just asking if they drink, Dr. Pfefferbaum said in an interview. That’s because they may be more willing to answer the first question honestly.
It’s also important for clinicians to nonjudgmentally tell teens there is evidence “that heavy drinking is bad for their brain,” he added.
The findings were published online Dec. 30, 2020, in JAMA Psychiatry.
Fractional anisotropy
Adolescence is a critical period of physiological and social maturation accompanied by significant structural, functional, and neurochemical brain changes, the investigators noted.
Diffusion tensor imaging (DTI) produces a measure called fractional anisotropy (FA), which characterizes some of these brain changes by measuring molecular water diffusion in the brain.
“FA is a measure of the integrity of brain white matter; so, the part of the brain that connects neurons with each other,” Dr. Pfefferbaum said. He added that FA decreases in diseases such as multiple sclerosis (MS), reflecting “some kind of pathology.”
Affected fiber systems include the corpus callosum, superior longitudinal fasciculus, internal and external capsule, brain stem, and cortical projection fibers. Disruption of these neural systems may degrade neural signal transmission and affect certain cognitive functions, possibly resulting in enhanced impulsivity, poor inhibitory control, and restricted working memory capacity, the researchers wrote.
FA follows an inverted U-shaped pattern. “The natural trajectory is to increase from infancy up to middle adolescence and then, as we get older, from about age 25 to 30 years, starts to go down. Our brains are starting to show signs of aging a bit by then,” said Dr. Pfefferbaum.
The current analysis assessed 451 adolescents (228 boys and 223 girls) from the NCANDA study, for whom researchers had four years of longitudinal DTI data. All were aged 12- 21 years at baseline.
The NCANDA cohort was recruited across five U.S. sites. Participants are assessed yearly on psychobiologic measures, including brain maturation. The cohort, which did not have any significant substance abuse upon entry, is balanced in terms of gender and ethnicity.
The investigators quantified the developmental change of white-matter (WM) integrity within each individual as the slope of FA over visits. They also examined altered developmental trajectories associated with drinking onset during adolescence and the differential alcohol associations by age with specific regional WM fiber tracts.
Researchers assessed drinking on a scale of 1-4, based on the youth-adjusted Cahalan score. The scale considers quantity and frequency to classify drinking levels based on past-year self-reported patterns.
Altered trajectory
Results showed that 291 participants (37.2%) remained at no to low drinking levels (youth-adjusted Cahalan score, 0) throughout the time points examined, and 160 (20.5%) were classified as heavy drinkers for at least two consecutive visits (youth-adjusted Cahalan score >1).
Among the no to low drinkers, 48.4% were boys with a mean age of 16.5 years and 51.2% were girls with a mean age of 16.5 years. About two thirds of the group (66%) were White.
Among heavy drinkers, 53.8% were boys with a mean age of 20.1 years and 46.3% were girls with a mean age of 20.5 years. In this group, 88.8% were White.
The investigators did not analyze moderate drinkers or those who initiated heavy drinking for only one visit.
The findings also showed that heavy drinkers exhibited significant reduction of whole-brain FA. The slopes of the 78 heavy drinkers were significantly more negative than the 78 matched no to low drinkers (mean, –0.0013 vs. 0.0001; P = .008).
“The concept of the slopes is really important here because it’s the trajectory that seems to be the most sensitive measure,” Dr. Pfefferbaum said. “Probably what’s happening is the exposure to alcohol is interfering with the normal myelination and normal development of the adolescent’s white matter.”
The no to low drinkers had relatively stable FA measures across all visits.
A reduction in FA was significantly linked to heavy drinking. An analysis of 63 youth who transitioned from being a no to low drinker to a heavy drinker showed that before the transition, they had significantly increased FA over visits (95% CI of slope, 0.0011-0.0024; P < .001). In addition, their corresponding slopes were not different from other no to low drinkers of the same age range.
However, this group’s FA declined significantly after they reported heavy drinking, resulting in slopes significantly below zero (95% CI of slope, –0.0036 to –0.0014; P < .001) and that were lower than the no to low participants of the same age range.
and further illustrates that heavy drinking in adolescence affects WM integrity, Dr. Pfefferbaum said.
Potential markers
None of the slope measures correlated with number of visits or use of tobacco or cannabis. The association of alcohol with the slope measures was more apparent in the younger cohort (<19 years).
“The effects were seen more readily in younger adolescents because they are the ones who are still progressing along this normal developmental trajectory,” Dr. Pfefferbaum noted. “In a sense, the younger you are when you’re exposed to alcohol, probably the more vulnerable you are.”
Previous studies have suggested that damage in WM tracts is associated with heightened neural reactivity to alcohol cues in adults with alcohol use disorder. Given this evidence, the greater WM degradation at younger versus older ages might help explain why adolescents who initiate early drinking are more likely to develop addiction later in life, the investigators wrote.
Of the five major fiber tracts, only the commissural fibers (corpus callosum) showed a significant association with alcohol. The researchers noted that WM volume shrinkage and callosal demyelination are two of the most prominent markers in adult alcoholism and are potential markers in adolescent alcohol abuse.
Upon further extending the analysis to the four subregions of the corpus callosum, the investigators found that only the anterior and middle callosal regions (genu and body) showed significant age-alcohol interactions.
This could be a result of the timing of fiber myelination in these regions of the brain, compared with others, Dr. Pfefferbaum said.
He noted that these fibers connect the left and right part of the anterior regions of the brain, especially the frontal lobes, which are particularly vulnerable to the effects of alcohol. “It may well be that we have this interaction of the developmental time and the sensitivity of the frontal parts of the brain.”
Cognitive effects?
Although the researchers did not find any sex effects, Dr. Pfefferbaum stressed that this doesn’t mean they do not exist. “We just may not have the power to see them,” he said.
The study did not look specifically at binge drinkers, defined as consuming five drinks in 2 hours for men and four drinks in 2 hours for women. Dr. Pfefferbaum noted that it is difficult to get “good quantification” of binge drinking. “We don’t have a fine enough grain analysis to separate that out,” he said.
Asked whether the altered FA trajectory in heavy drinkers affects cognition, Dr. Pfefferbaum said “those studies are still in progress,” with results hopefully available within about a year.
Dr. Pfefferbaum said he and his colleagues are continuing to follow these adolescents and hope to see if the altered FA trajectory in heavy drinkers returns to normal, adding: “The real question now is: If they stop heavy drinking, will they get back on track?”
This study is believed to be the first to suggest in vivo differential vulnerability in WM microstructure with respect to age, the authors note.
In addition to asking teens about their alcohol use, the clinician’s role should be to “counsel and refer,” said Dr. Pfefferbaum. He also suggested accessing resources from the National Institute on Alcohol Abuse and Alcoholism.
Important data, but several limitations
In an interview, Oscar G. Bukstein, MD, MPH, medical director of outpatient psychiatry service at Boston Children’s Hospital, and professor of psychiatry at Harvard Medical School, also in Boston, said the findings provide further evidence that alcohol affects the maturing brain.
This study, and others that have examined cannabis use, “show that you have a dynamically growing brain with certain sections, particularly in this case the anterior and middle corpus callosum, that mature later [and] that are more likely to be affected by early alcohol use,” said Dr. Bukstein, who was not involved with the research.
He stressed the importance of determining the mechanism involved and noted some study limitations. For example, the DTI technology used may “already be out of date,” he said.
Using older technology may have prevented finding an impact of heavy drinking on parts of the brain other than the anterior and middle corpus callosum, Dr. Bukstein noted.
Newer technology might provide “a finer-grain nonlinear voxel-wise analysis,” although using more updated scanning techniques may not have detected additional differences in study groups, he added.
Dr. Bukstein also noted that there were limitations: The study did not have “gradations,” but only looked at heavy drinking and no to low drinking. “You’d like to find out about kids who are somewhere in the middle.” It also didn’t determine a “cutoff” where deleterious effects of alcohol on the brain begin, Dr. Bukstein added.
Additionally, the study didn’t look at brain development outcomes in children with conditions such as depression and ADHD that are known to lead to substance use – something a larger study may have been able to do, he said.
Dr. Bukstein noted that a newer and much larger study, the Adolescent Brain Cognitive Development study, has begun assessing kids for risk factors such as substance use, starting at age 10 years.
The study was funded by grants from NIAAA and by the National Institute on Drug Abuse, the National Institute of Mental Health, the National Institute of Child Health and Human Development, and the Stanford Institute for Human-Centered Artificial Intelligence–AWS Cloud Credits for Research. Dr. Pfefferbaum reported receiving an NIAAA grant during the conduct of the study. Dr. Bukstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Heavy alcohol use in adolescence is linked to disruptions in white-matter integrity, new research suggests.
In a case-control study of more than 400 participants, the association was more pronounced in younger adolescents and in the anterior and middle corpus callosum, which serve the interhemispheric integration of frontal networking and communication.
The results provide clinicians with yet another reason to ask adolescents about their alcohol use, said investigator Adolf Pfefferbaum, MD, Center for Health Sciences, SRI International, Menlo Park, Calif., and professor emeritus at Stanford (Calif.) University.
However, when questioning adolescents about their alcohol use, “sometimes it’s better to ask: ‘How much alcohol do you drink?’ ” instead of just asking if they drink, Dr. Pfefferbaum said in an interview. That’s because they may be more willing to answer the first question honestly.
It’s also important for clinicians to nonjudgmentally tell teens there is evidence “that heavy drinking is bad for their brain,” he added.
The findings were published online Dec. 30, 2020, in JAMA Psychiatry.
Fractional anisotropy
Adolescence is a critical period of physiological and social maturation accompanied by significant structural, functional, and neurochemical brain changes, the investigators noted.
Diffusion tensor imaging (DTI) produces a measure called fractional anisotropy (FA), which characterizes some of these brain changes by measuring molecular water diffusion in the brain.
“FA is a measure of the integrity of brain white matter; so, the part of the brain that connects neurons with each other,” Dr. Pfefferbaum said. He added that FA decreases in diseases such as multiple sclerosis (MS), reflecting “some kind of pathology.”
Affected fiber systems include the corpus callosum, superior longitudinal fasciculus, internal and external capsule, brain stem, and cortical projection fibers. Disruption of these neural systems may degrade neural signal transmission and affect certain cognitive functions, possibly resulting in enhanced impulsivity, poor inhibitory control, and restricted working memory capacity, the researchers wrote.
FA follows an inverted U-shaped pattern. “The natural trajectory is to increase from infancy up to middle adolescence and then, as we get older, from about age 25 to 30 years, starts to go down. Our brains are starting to show signs of aging a bit by then,” said Dr. Pfefferbaum.
The current analysis assessed 451 adolescents (228 boys and 223 girls) from the NCANDA study, for whom researchers had four years of longitudinal DTI data. All were aged 12- 21 years at baseline.
The NCANDA cohort was recruited across five U.S. sites. Participants are assessed yearly on psychobiologic measures, including brain maturation. The cohort, which did not have any significant substance abuse upon entry, is balanced in terms of gender and ethnicity.
The investigators quantified the developmental change of white-matter (WM) integrity within each individual as the slope of FA over visits. They also examined altered developmental trajectories associated with drinking onset during adolescence and the differential alcohol associations by age with specific regional WM fiber tracts.
Researchers assessed drinking on a scale of 1-4, based on the youth-adjusted Cahalan score. The scale considers quantity and frequency to classify drinking levels based on past-year self-reported patterns.
Altered trajectory
Results showed that 291 participants (37.2%) remained at no to low drinking levels (youth-adjusted Cahalan score, 0) throughout the time points examined, and 160 (20.5%) were classified as heavy drinkers for at least two consecutive visits (youth-adjusted Cahalan score >1).
Among the no to low drinkers, 48.4% were boys with a mean age of 16.5 years and 51.2% were girls with a mean age of 16.5 years. About two thirds of the group (66%) were White.
Among heavy drinkers, 53.8% were boys with a mean age of 20.1 years and 46.3% were girls with a mean age of 20.5 years. In this group, 88.8% were White.
The investigators did not analyze moderate drinkers or those who initiated heavy drinking for only one visit.
The findings also showed that heavy drinkers exhibited significant reduction of whole-brain FA. The slopes of the 78 heavy drinkers were significantly more negative than the 78 matched no to low drinkers (mean, –0.0013 vs. 0.0001; P = .008).
“The concept of the slopes is really important here because it’s the trajectory that seems to be the most sensitive measure,” Dr. Pfefferbaum said. “Probably what’s happening is the exposure to alcohol is interfering with the normal myelination and normal development of the adolescent’s white matter.”
The no to low drinkers had relatively stable FA measures across all visits.
A reduction in FA was significantly linked to heavy drinking. An analysis of 63 youth who transitioned from being a no to low drinker to a heavy drinker showed that before the transition, they had significantly increased FA over visits (95% CI of slope, 0.0011-0.0024; P < .001). In addition, their corresponding slopes were not different from other no to low drinkers of the same age range.
However, this group’s FA declined significantly after they reported heavy drinking, resulting in slopes significantly below zero (95% CI of slope, –0.0036 to –0.0014; P < .001) and that were lower than the no to low participants of the same age range.
and further illustrates that heavy drinking in adolescence affects WM integrity, Dr. Pfefferbaum said.
Potential markers
None of the slope measures correlated with number of visits or use of tobacco or cannabis. The association of alcohol with the slope measures was more apparent in the younger cohort (<19 years).
“The effects were seen more readily in younger adolescents because they are the ones who are still progressing along this normal developmental trajectory,” Dr. Pfefferbaum noted. “In a sense, the younger you are when you’re exposed to alcohol, probably the more vulnerable you are.”
Previous studies have suggested that damage in WM tracts is associated with heightened neural reactivity to alcohol cues in adults with alcohol use disorder. Given this evidence, the greater WM degradation at younger versus older ages might help explain why adolescents who initiate early drinking are more likely to develop addiction later in life, the investigators wrote.
Of the five major fiber tracts, only the commissural fibers (corpus callosum) showed a significant association with alcohol. The researchers noted that WM volume shrinkage and callosal demyelination are two of the most prominent markers in adult alcoholism and are potential markers in adolescent alcohol abuse.
Upon further extending the analysis to the four subregions of the corpus callosum, the investigators found that only the anterior and middle callosal regions (genu and body) showed significant age-alcohol interactions.
This could be a result of the timing of fiber myelination in these regions of the brain, compared with others, Dr. Pfefferbaum said.
He noted that these fibers connect the left and right part of the anterior regions of the brain, especially the frontal lobes, which are particularly vulnerable to the effects of alcohol. “It may well be that we have this interaction of the developmental time and the sensitivity of the frontal parts of the brain.”
Cognitive effects?
Although the researchers did not find any sex effects, Dr. Pfefferbaum stressed that this doesn’t mean they do not exist. “We just may not have the power to see them,” he said.
The study did not look specifically at binge drinkers, defined as consuming five drinks in 2 hours for men and four drinks in 2 hours for women. Dr. Pfefferbaum noted that it is difficult to get “good quantification” of binge drinking. “We don’t have a fine enough grain analysis to separate that out,” he said.
Asked whether the altered FA trajectory in heavy drinkers affects cognition, Dr. Pfefferbaum said “those studies are still in progress,” with results hopefully available within about a year.
Dr. Pfefferbaum said he and his colleagues are continuing to follow these adolescents and hope to see if the altered FA trajectory in heavy drinkers returns to normal, adding: “The real question now is: If they stop heavy drinking, will they get back on track?”
This study is believed to be the first to suggest in vivo differential vulnerability in WM microstructure with respect to age, the authors note.
In addition to asking teens about their alcohol use, the clinician’s role should be to “counsel and refer,” said Dr. Pfefferbaum. He also suggested accessing resources from the National Institute on Alcohol Abuse and Alcoholism.
Important data, but several limitations
In an interview, Oscar G. Bukstein, MD, MPH, medical director of outpatient psychiatry service at Boston Children’s Hospital, and professor of psychiatry at Harvard Medical School, also in Boston, said the findings provide further evidence that alcohol affects the maturing brain.
This study, and others that have examined cannabis use, “show that you have a dynamically growing brain with certain sections, particularly in this case the anterior and middle corpus callosum, that mature later [and] that are more likely to be affected by early alcohol use,” said Dr. Bukstein, who was not involved with the research.
He stressed the importance of determining the mechanism involved and noted some study limitations. For example, the DTI technology used may “already be out of date,” he said.
Using older technology may have prevented finding an impact of heavy drinking on parts of the brain other than the anterior and middle corpus callosum, Dr. Bukstein noted.
Newer technology might provide “a finer-grain nonlinear voxel-wise analysis,” although using more updated scanning techniques may not have detected additional differences in study groups, he added.
Dr. Bukstein also noted that there were limitations: The study did not have “gradations,” but only looked at heavy drinking and no to low drinking. “You’d like to find out about kids who are somewhere in the middle.” It also didn’t determine a “cutoff” where deleterious effects of alcohol on the brain begin, Dr. Bukstein added.
Additionally, the study didn’t look at brain development outcomes in children with conditions such as depression and ADHD that are known to lead to substance use – something a larger study may have been able to do, he said.
Dr. Bukstein noted that a newer and much larger study, the Adolescent Brain Cognitive Development study, has begun assessing kids for risk factors such as substance use, starting at age 10 years.
The study was funded by grants from NIAAA and by the National Institute on Drug Abuse, the National Institute of Mental Health, the National Institute of Child Health and Human Development, and the Stanford Institute for Human-Centered Artificial Intelligence–AWS Cloud Credits for Research. Dr. Pfefferbaum reported receiving an NIAAA grant during the conduct of the study. Dr. Bukstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Heavy alcohol use in adolescence is linked to disruptions in white-matter integrity, new research suggests.
In a case-control study of more than 400 participants, the association was more pronounced in younger adolescents and in the anterior and middle corpus callosum, which serve the interhemispheric integration of frontal networking and communication.
The results provide clinicians with yet another reason to ask adolescents about their alcohol use, said investigator Adolf Pfefferbaum, MD, Center for Health Sciences, SRI International, Menlo Park, Calif., and professor emeritus at Stanford (Calif.) University.
However, when questioning adolescents about their alcohol use, “sometimes it’s better to ask: ‘How much alcohol do you drink?’ ” instead of just asking if they drink, Dr. Pfefferbaum said in an interview. That’s because they may be more willing to answer the first question honestly.
It’s also important for clinicians to nonjudgmentally tell teens there is evidence “that heavy drinking is bad for their brain,” he added.
The findings were published online Dec. 30, 2020, in JAMA Psychiatry.
Fractional anisotropy
Adolescence is a critical period of physiological and social maturation accompanied by significant structural, functional, and neurochemical brain changes, the investigators noted.
Diffusion tensor imaging (DTI) produces a measure called fractional anisotropy (FA), which characterizes some of these brain changes by measuring molecular water diffusion in the brain.
“FA is a measure of the integrity of brain white matter; so, the part of the brain that connects neurons with each other,” Dr. Pfefferbaum said. He added that FA decreases in diseases such as multiple sclerosis (MS), reflecting “some kind of pathology.”
Affected fiber systems include the corpus callosum, superior longitudinal fasciculus, internal and external capsule, brain stem, and cortical projection fibers. Disruption of these neural systems may degrade neural signal transmission and affect certain cognitive functions, possibly resulting in enhanced impulsivity, poor inhibitory control, and restricted working memory capacity, the researchers wrote.
FA follows an inverted U-shaped pattern. “The natural trajectory is to increase from infancy up to middle adolescence and then, as we get older, from about age 25 to 30 years, starts to go down. Our brains are starting to show signs of aging a bit by then,” said Dr. Pfefferbaum.
The current analysis assessed 451 adolescents (228 boys and 223 girls) from the NCANDA study, for whom researchers had four years of longitudinal DTI data. All were aged 12- 21 years at baseline.
The NCANDA cohort was recruited across five U.S. sites. Participants are assessed yearly on psychobiologic measures, including brain maturation. The cohort, which did not have any significant substance abuse upon entry, is balanced in terms of gender and ethnicity.
The investigators quantified the developmental change of white-matter (WM) integrity within each individual as the slope of FA over visits. They also examined altered developmental trajectories associated with drinking onset during adolescence and the differential alcohol associations by age with specific regional WM fiber tracts.
Researchers assessed drinking on a scale of 1-4, based on the youth-adjusted Cahalan score. The scale considers quantity and frequency to classify drinking levels based on past-year self-reported patterns.
Altered trajectory
Results showed that 291 participants (37.2%) remained at no to low drinking levels (youth-adjusted Cahalan score, 0) throughout the time points examined, and 160 (20.5%) were classified as heavy drinkers for at least two consecutive visits (youth-adjusted Cahalan score >1).
Among the no to low drinkers, 48.4% were boys with a mean age of 16.5 years and 51.2% were girls with a mean age of 16.5 years. About two thirds of the group (66%) were White.
Among heavy drinkers, 53.8% were boys with a mean age of 20.1 years and 46.3% were girls with a mean age of 20.5 years. In this group, 88.8% were White.
The investigators did not analyze moderate drinkers or those who initiated heavy drinking for only one visit.
The findings also showed that heavy drinkers exhibited significant reduction of whole-brain FA. The slopes of the 78 heavy drinkers were significantly more negative than the 78 matched no to low drinkers (mean, –0.0013 vs. 0.0001; P = .008).
“The concept of the slopes is really important here because it’s the trajectory that seems to be the most sensitive measure,” Dr. Pfefferbaum said. “Probably what’s happening is the exposure to alcohol is interfering with the normal myelination and normal development of the adolescent’s white matter.”
The no to low drinkers had relatively stable FA measures across all visits.
A reduction in FA was significantly linked to heavy drinking. An analysis of 63 youth who transitioned from being a no to low drinker to a heavy drinker showed that before the transition, they had significantly increased FA over visits (95% CI of slope, 0.0011-0.0024; P < .001). In addition, their corresponding slopes were not different from other no to low drinkers of the same age range.
However, this group’s FA declined significantly after they reported heavy drinking, resulting in slopes significantly below zero (95% CI of slope, –0.0036 to –0.0014; P < .001) and that were lower than the no to low participants of the same age range.
and further illustrates that heavy drinking in adolescence affects WM integrity, Dr. Pfefferbaum said.
Potential markers
None of the slope measures correlated with number of visits or use of tobacco or cannabis. The association of alcohol with the slope measures was more apparent in the younger cohort (<19 years).
“The effects were seen more readily in younger adolescents because they are the ones who are still progressing along this normal developmental trajectory,” Dr. Pfefferbaum noted. “In a sense, the younger you are when you’re exposed to alcohol, probably the more vulnerable you are.”
Previous studies have suggested that damage in WM tracts is associated with heightened neural reactivity to alcohol cues in adults with alcohol use disorder. Given this evidence, the greater WM degradation at younger versus older ages might help explain why adolescents who initiate early drinking are more likely to develop addiction later in life, the investigators wrote.
Of the five major fiber tracts, only the commissural fibers (corpus callosum) showed a significant association with alcohol. The researchers noted that WM volume shrinkage and callosal demyelination are two of the most prominent markers in adult alcoholism and are potential markers in adolescent alcohol abuse.
Upon further extending the analysis to the four subregions of the corpus callosum, the investigators found that only the anterior and middle callosal regions (genu and body) showed significant age-alcohol interactions.
This could be a result of the timing of fiber myelination in these regions of the brain, compared with others, Dr. Pfefferbaum said.
He noted that these fibers connect the left and right part of the anterior regions of the brain, especially the frontal lobes, which are particularly vulnerable to the effects of alcohol. “It may well be that we have this interaction of the developmental time and the sensitivity of the frontal parts of the brain.”
Cognitive effects?
Although the researchers did not find any sex effects, Dr. Pfefferbaum stressed that this doesn’t mean they do not exist. “We just may not have the power to see them,” he said.
The study did not look specifically at binge drinkers, defined as consuming five drinks in 2 hours for men and four drinks in 2 hours for women. Dr. Pfefferbaum noted that it is difficult to get “good quantification” of binge drinking. “We don’t have a fine enough grain analysis to separate that out,” he said.
Asked whether the altered FA trajectory in heavy drinkers affects cognition, Dr. Pfefferbaum said “those studies are still in progress,” with results hopefully available within about a year.
Dr. Pfefferbaum said he and his colleagues are continuing to follow these adolescents and hope to see if the altered FA trajectory in heavy drinkers returns to normal, adding: “The real question now is: If they stop heavy drinking, will they get back on track?”
This study is believed to be the first to suggest in vivo differential vulnerability in WM microstructure with respect to age, the authors note.
In addition to asking teens about their alcohol use, the clinician’s role should be to “counsel and refer,” said Dr. Pfefferbaum. He also suggested accessing resources from the National Institute on Alcohol Abuse and Alcoholism.
Important data, but several limitations
In an interview, Oscar G. Bukstein, MD, MPH, medical director of outpatient psychiatry service at Boston Children’s Hospital, and professor of psychiatry at Harvard Medical School, also in Boston, said the findings provide further evidence that alcohol affects the maturing brain.
This study, and others that have examined cannabis use, “show that you have a dynamically growing brain with certain sections, particularly in this case the anterior and middle corpus callosum, that mature later [and] that are more likely to be affected by early alcohol use,” said Dr. Bukstein, who was not involved with the research.
He stressed the importance of determining the mechanism involved and noted some study limitations. For example, the DTI technology used may “already be out of date,” he said.
Using older technology may have prevented finding an impact of heavy drinking on parts of the brain other than the anterior and middle corpus callosum, Dr. Bukstein noted.
Newer technology might provide “a finer-grain nonlinear voxel-wise analysis,” although using more updated scanning techniques may not have detected additional differences in study groups, he added.
Dr. Bukstein also noted that there were limitations: The study did not have “gradations,” but only looked at heavy drinking and no to low drinking. “You’d like to find out about kids who are somewhere in the middle.” It also didn’t determine a “cutoff” where deleterious effects of alcohol on the brain begin, Dr. Bukstein added.
Additionally, the study didn’t look at brain development outcomes in children with conditions such as depression and ADHD that are known to lead to substance use – something a larger study may have been able to do, he said.
Dr. Bukstein noted that a newer and much larger study, the Adolescent Brain Cognitive Development study, has begun assessing kids for risk factors such as substance use, starting at age 10 years.
The study was funded by grants from NIAAA and by the National Institute on Drug Abuse, the National Institute of Mental Health, the National Institute of Child Health and Human Development, and the Stanford Institute for Human-Centered Artificial Intelligence–AWS Cloud Credits for Research. Dr. Pfefferbaum reported receiving an NIAAA grant during the conduct of the study. Dr. Bukstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Encouraging results for new epilepsy drug
Post hoc analyses from an open-label study showed that seizure frequency was significantly reduced and the seizure-freedom rate was significantly improved among 240 adult participants who received cenobamate. The patients’ use of concomitant antiseizure medications was also reduced, with no effect on efficacy.
These results are “fascinating” and “very, very exciting,” said lead author William E. Rosenfeld, MD, director, Comprehensive Epilepsy Care Center for Children and Adults, St. Louis, Mo. Although responder rates were impressive, at 50% or greater and 75% or greater, “what patients really want is to have seizure freedom, or at least a 90% reduction in seizures,” Dr. Rosenfeld said.
The findings were presented at the annual meeting of the American Epilepsy Society, held online this year.
Adverse events
Cenobamate reduces seizures by inhibiting sodium current or affecting the GABAA channel, or potentially through a combination of these two mechanisms, said Dr. Rosenfeld. The drug was approved by the U.S. Food and Drug Administration in November 2019 for the treatment of uncontrolled partial-onset seizures in adults, which represent about 60% of all epileptic seizures. It has been on the market since May 2020.
During the drug’s development, three cases of drug reaction with eosinophilia and systemic symptoms (DRESS) occurred. This condition typically involves a skin rash, fever, swollen lymph nodes, and characteristic blood abnormalities, including a high level of eosinophils. However, an open-label study, published earlier this year in Epilepsia, that assessed safety and pharmacokinetics in 1,347 patients aged 18-70 years who received stable doses of one to three antiseizure medications showed that, with “slow and low titration” of cenobamate, there were no cases of DRESS, Dr. Rosenfeld said.
In that safety study, investigators administered increasing daily doses of cenobamate at 12.5, 25, 50, 100, 150, and 200 mg/day at 2-week intervals. If necessary, the dose could be increased to 400 mg/day via 50-mg/day increments every other week.
The researchers presented post hoc analyses regarding 240 patients from 10 U.S. sites who participated in the safety study. Dr. Rosenfeld noted, “These are all good epilepsy centers, and they all kept seizure records.” Of these participants, 177 continued taking the drug as they had at their last visit for a mean of more than 30 months; for some, it was up to 44 months.
“So we had a 73.8% retention rate over the course of the open label, which is the maintenance phase of the study,” Dr. Rosenfeld said.
Among the entire group of 240 patients, 25.8% had been seizure free for more than 12 months at their last visit. Of the 177 who continued to take cenobamate, 33.9% were seizure free for an average of 23.5 months.
“We have never seen those kinds of numbers in the past,” said Dr. Rosenfeld, adding, “it’s so important for patients to get seizure freedom.” These promising results may be related to the fact that the drug works on more than one mechanism of seizure, he speculated.
For some patients, the drug will “make a big difference” by providing them with the best quality of life and allow them to resume normal activities, Dr. Rosenfeld noted. In addition, the drug was well tolerated. The most common adverse events were dizziness/diplopia and sleepiness/drowsiness.
Concomitant drug reductions
Another post hoc analysis of the 240 patients showed that many patients were able to reduce use of other antiseizure medications. At study outset, about 41% were taking lacosamide, 35.7% were taking levetiracetam, and 27.7% were taking lamotrigine. Among patients who continued to take cenobamate, 22.7% of concomitant baseline antiseizure medications were discontinued. Carbamazepine was discontinued by 31.3%, oxcarbazepine by 26.7%, lacosamide by 23.4%, eslicarbazepine by 23.1%, clobazam by 26.7%, lamotrigine by 14.6%, and levetiracetam by 20.3%.
“We found that the patients who stayed in the study the longest had greater reductions in their concomitant antiepileptic mediation,” said Dr. Rosenfeld. Lowering concomitant medications did not reduce efficacy at a target dose of 200 mg/day.
The investigators hope to test the drug in children and in patients with different seizure types.
Promising, with caveats
Commenting on the research, Jong Woo Lee, MD, PhD, associate professor of neurology, the Edward B. Bromfield Epilepsy Program, Brigham and Women’s Hospital, Boston, said cenobamate “has certainly given new hope” to some of his patients. He noted that a few of these patients had been experiencing daily or nearly daily seizures and had been taking three or more medications for many years.
“The chances of another medication being effective for these patients is very low,” said Dr. Lee, who was not involved with the research. “But several of these patients responded to cenobamate, and some of them achieved complete seizure freedom.”
However, as with all new promising medications, there are some caveats. “The concern is for long-term efficacy for more than 5 years and, of course, unforeseen side effects,” Dr. Lee said.
The studies were funded by SK Life Science. Dr. Rosenfeld has been a consultant for SK Life Science. Dr. Lee has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Post hoc analyses from an open-label study showed that seizure frequency was significantly reduced and the seizure-freedom rate was significantly improved among 240 adult participants who received cenobamate. The patients’ use of concomitant antiseizure medications was also reduced, with no effect on efficacy.
These results are “fascinating” and “very, very exciting,” said lead author William E. Rosenfeld, MD, director, Comprehensive Epilepsy Care Center for Children and Adults, St. Louis, Mo. Although responder rates were impressive, at 50% or greater and 75% or greater, “what patients really want is to have seizure freedom, or at least a 90% reduction in seizures,” Dr. Rosenfeld said.
The findings were presented at the annual meeting of the American Epilepsy Society, held online this year.
Adverse events
Cenobamate reduces seizures by inhibiting sodium current or affecting the GABAA channel, or potentially through a combination of these two mechanisms, said Dr. Rosenfeld. The drug was approved by the U.S. Food and Drug Administration in November 2019 for the treatment of uncontrolled partial-onset seizures in adults, which represent about 60% of all epileptic seizures. It has been on the market since May 2020.
During the drug’s development, three cases of drug reaction with eosinophilia and systemic symptoms (DRESS) occurred. This condition typically involves a skin rash, fever, swollen lymph nodes, and characteristic blood abnormalities, including a high level of eosinophils. However, an open-label study, published earlier this year in Epilepsia, that assessed safety and pharmacokinetics in 1,347 patients aged 18-70 years who received stable doses of one to three antiseizure medications showed that, with “slow and low titration” of cenobamate, there were no cases of DRESS, Dr. Rosenfeld said.
In that safety study, investigators administered increasing daily doses of cenobamate at 12.5, 25, 50, 100, 150, and 200 mg/day at 2-week intervals. If necessary, the dose could be increased to 400 mg/day via 50-mg/day increments every other week.
The researchers presented post hoc analyses regarding 240 patients from 10 U.S. sites who participated in the safety study. Dr. Rosenfeld noted, “These are all good epilepsy centers, and they all kept seizure records.” Of these participants, 177 continued taking the drug as they had at their last visit for a mean of more than 30 months; for some, it was up to 44 months.
“So we had a 73.8% retention rate over the course of the open label, which is the maintenance phase of the study,” Dr. Rosenfeld said.
Among the entire group of 240 patients, 25.8% had been seizure free for more than 12 months at their last visit. Of the 177 who continued to take cenobamate, 33.9% were seizure free for an average of 23.5 months.
“We have never seen those kinds of numbers in the past,” said Dr. Rosenfeld, adding, “it’s so important for patients to get seizure freedom.” These promising results may be related to the fact that the drug works on more than one mechanism of seizure, he speculated.
For some patients, the drug will “make a big difference” by providing them with the best quality of life and allow them to resume normal activities, Dr. Rosenfeld noted. In addition, the drug was well tolerated. The most common adverse events were dizziness/diplopia and sleepiness/drowsiness.
Concomitant drug reductions
Another post hoc analysis of the 240 patients showed that many patients were able to reduce use of other antiseizure medications. At study outset, about 41% were taking lacosamide, 35.7% were taking levetiracetam, and 27.7% were taking lamotrigine. Among patients who continued to take cenobamate, 22.7% of concomitant baseline antiseizure medications were discontinued. Carbamazepine was discontinued by 31.3%, oxcarbazepine by 26.7%, lacosamide by 23.4%, eslicarbazepine by 23.1%, clobazam by 26.7%, lamotrigine by 14.6%, and levetiracetam by 20.3%.
“We found that the patients who stayed in the study the longest had greater reductions in their concomitant antiepileptic mediation,” said Dr. Rosenfeld. Lowering concomitant medications did not reduce efficacy at a target dose of 200 mg/day.
The investigators hope to test the drug in children and in patients with different seizure types.
Promising, with caveats
Commenting on the research, Jong Woo Lee, MD, PhD, associate professor of neurology, the Edward B. Bromfield Epilepsy Program, Brigham and Women’s Hospital, Boston, said cenobamate “has certainly given new hope” to some of his patients. He noted that a few of these patients had been experiencing daily or nearly daily seizures and had been taking three or more medications for many years.
“The chances of another medication being effective for these patients is very low,” said Dr. Lee, who was not involved with the research. “But several of these patients responded to cenobamate, and some of them achieved complete seizure freedom.”
However, as with all new promising medications, there are some caveats. “The concern is for long-term efficacy for more than 5 years and, of course, unforeseen side effects,” Dr. Lee said.
The studies were funded by SK Life Science. Dr. Rosenfeld has been a consultant for SK Life Science. Dr. Lee has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Post hoc analyses from an open-label study showed that seizure frequency was significantly reduced and the seizure-freedom rate was significantly improved among 240 adult participants who received cenobamate. The patients’ use of concomitant antiseizure medications was also reduced, with no effect on efficacy.
These results are “fascinating” and “very, very exciting,” said lead author William E. Rosenfeld, MD, director, Comprehensive Epilepsy Care Center for Children and Adults, St. Louis, Mo. Although responder rates were impressive, at 50% or greater and 75% or greater, “what patients really want is to have seizure freedom, or at least a 90% reduction in seizures,” Dr. Rosenfeld said.
The findings were presented at the annual meeting of the American Epilepsy Society, held online this year.
Adverse events
Cenobamate reduces seizures by inhibiting sodium current or affecting the GABAA channel, or potentially through a combination of these two mechanisms, said Dr. Rosenfeld. The drug was approved by the U.S. Food and Drug Administration in November 2019 for the treatment of uncontrolled partial-onset seizures in adults, which represent about 60% of all epileptic seizures. It has been on the market since May 2020.
During the drug’s development, three cases of drug reaction with eosinophilia and systemic symptoms (DRESS) occurred. This condition typically involves a skin rash, fever, swollen lymph nodes, and characteristic blood abnormalities, including a high level of eosinophils. However, an open-label study, published earlier this year in Epilepsia, that assessed safety and pharmacokinetics in 1,347 patients aged 18-70 years who received stable doses of one to three antiseizure medications showed that, with “slow and low titration” of cenobamate, there were no cases of DRESS, Dr. Rosenfeld said.
In that safety study, investigators administered increasing daily doses of cenobamate at 12.5, 25, 50, 100, 150, and 200 mg/day at 2-week intervals. If necessary, the dose could be increased to 400 mg/day via 50-mg/day increments every other week.
The researchers presented post hoc analyses regarding 240 patients from 10 U.S. sites who participated in the safety study. Dr. Rosenfeld noted, “These are all good epilepsy centers, and they all kept seizure records.” Of these participants, 177 continued taking the drug as they had at their last visit for a mean of more than 30 months; for some, it was up to 44 months.
“So we had a 73.8% retention rate over the course of the open label, which is the maintenance phase of the study,” Dr. Rosenfeld said.
Among the entire group of 240 patients, 25.8% had been seizure free for more than 12 months at their last visit. Of the 177 who continued to take cenobamate, 33.9% were seizure free for an average of 23.5 months.
“We have never seen those kinds of numbers in the past,” said Dr. Rosenfeld, adding, “it’s so important for patients to get seizure freedom.” These promising results may be related to the fact that the drug works on more than one mechanism of seizure, he speculated.
For some patients, the drug will “make a big difference” by providing them with the best quality of life and allow them to resume normal activities, Dr. Rosenfeld noted. In addition, the drug was well tolerated. The most common adverse events were dizziness/diplopia and sleepiness/drowsiness.
Concomitant drug reductions
Another post hoc analysis of the 240 patients showed that many patients were able to reduce use of other antiseizure medications. At study outset, about 41% were taking lacosamide, 35.7% were taking levetiracetam, and 27.7% were taking lamotrigine. Among patients who continued to take cenobamate, 22.7% of concomitant baseline antiseizure medications were discontinued. Carbamazepine was discontinued by 31.3%, oxcarbazepine by 26.7%, lacosamide by 23.4%, eslicarbazepine by 23.1%, clobazam by 26.7%, lamotrigine by 14.6%, and levetiracetam by 20.3%.
“We found that the patients who stayed in the study the longest had greater reductions in their concomitant antiepileptic mediation,” said Dr. Rosenfeld. Lowering concomitant medications did not reduce efficacy at a target dose of 200 mg/day.
The investigators hope to test the drug in children and in patients with different seizure types.
Promising, with caveats
Commenting on the research, Jong Woo Lee, MD, PhD, associate professor of neurology, the Edward B. Bromfield Epilepsy Program, Brigham and Women’s Hospital, Boston, said cenobamate “has certainly given new hope” to some of his patients. He noted that a few of these patients had been experiencing daily or nearly daily seizures and had been taking three or more medications for many years.
“The chances of another medication being effective for these patients is very low,” said Dr. Lee, who was not involved with the research. “But several of these patients responded to cenobamate, and some of them achieved complete seizure freedom.”
However, as with all new promising medications, there are some caveats. “The concern is for long-term efficacy for more than 5 years and, of course, unforeseen side effects,” Dr. Lee said.
The studies were funded by SK Life Science. Dr. Rosenfeld has been a consultant for SK Life Science. Dr. Lee has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AES 2020
Wearable device clears a first ‘milestone’ in seizure detection
The new findings have the potential to revolutionize the management of patients with epilepsy, according to the researchers. “We have set a first benchmark for automatic detection of a variety of epileptic seizures using wearable sensors and deep-learning algorithms. In other words, we have shown for the first time that it’s possible to do this,” said study investigator Jianbin Tang, MA, data science project lead, IBM Research Australia, Victoria.
The findings were presented at the American Epilepsy Society’s annual meeting, held online this year because of the COVID-19 pandemic.
Accurate monitoring of seizures is important for assessing risk, injury prevention, and treatment response evaluation. Currently, video EEG is the gold standard for seizure detection, but it requires a hospital stay, is often costly, and can be stigmatizing, said Mr. Tang.
An advance in detecting seizure types
Recent advances in non-EEG wearable devices show promise in detecting generalized onset tonic-clonic and focal to bilateral tonic-clonic seizures, but it’s not clear if they have the ability to detect other seizure types. “We hope to fill this gap by expanding wearable seizure detection to additional seizure types,” said Mr. Tang.
Seizure tracking outside the hospital setting largely “relies on manually annotated family and patient reports, which often can be unreliable due to missed seizures and problems recalling seizures,” he said.
The study included 75 children (44% were female; mean age was 11.1 years) admitted to a long-term EEG monitoring unit at a single center for a 24-hour stay. Patients wore the detector on the ankle or wrist. The device continuously collected data on functions such as sweating, heart rate, movement, and temperature.
With part of the dataset, researchers trained deep-learning algorithms to automatically detect seizure segments. They then validated the performance of the detection algorithms on the remainder of the dataset.
The analysis was based on data from 722 epileptic seizures of all types including focal and generalized, motor and nonmotor. Seizures occurred throughout the day and during the night while patients were awake or asleep.
When a seizure is detected, the system triggers a real-time alert and will store the information about the detected seizure in a repository, said Mr. Tang.
The signals were initially stored in the wristband and then securely uploaded to the Cloud. From there, the signal files were downloaded by the investigators for analysis and interpretation. All data were entirely anonymized and de-identified. Researchers used Area Under Curve–Receiver Operating Characteristic (AUC-ROC) to assess performance.
“Our best performing detection models reach an AUC-ROC of 67.59%, which represents a decent performance level,” said Mr. Tang. “There certainly is room for performance improvement and we are already working on this,” he added.
The device performed “better than chance,” which is a “standard technical term” in the field of machine learning and is “the first hurdle any machine-learning model needs to take to be considered useful.” The investigators noted that such automatic seizure detection “is feasible across a broad spectrum of epileptic seizure types,” said Mr. Tang. “This is a first and has not been shown before.”
The study suggests that the noninvasive wearable device could be used at home, at school, and in other everyday settings outside the clinic. “This could one day provide patients, caregivers, and clinicians with reliable seizure reports,” said Mr. Tang.
He said he believes the device might be especially useful in detecting frequent or subtle seizures, which are easy to miss. Patients requiring medication evaluation and rescue medication and those at risk of status epilepticus may be good candidates.
The researchers don’t expect wearable technology to totally replace EEG but see it as “a useful complementary tool to track seizures continuously at times or in settings where EEG monitoring is not available,” said Mr. Tang.
‘Important milestone’
Commenting on the research, Benjamin H. Brinkmann, PhD, associate professor of neurology at the Mayo Clinic in Rochester, Minn., said the investigators “have done very good work applying state of the art machine learning techniques” to the “important problem” of accurately detecting seizures.
Dr. Brinkmann is part of the Epilepsy Foundation–sponsored “My Seizure Gauge” project that’s evaluating various wearable devices, including the Empatica E4 wristband and the Fitbit Charge 3, to determine what measurements are needed for reliable seizure forecasting.
“Previously, no one knew whether seizure prediction was possible with these devices, and the fact that this group was able to achieve ‘better-than-chance’ prediction accuracy is an important milestone.”
However, he emphasized that there is still a great deal of work to be done to determine, for example, if seizure prediction with these devices can be accurate enough to be clinically useful. “For example, if the system generates too many false-positive predictions, patients won’t use it.”
In addition, the findings need to be replicated and recordings extended to 6 months or more to determine whether they are helpful to patients long term and in the home environment, said Dr. Brinkmann.
The investigators and Dr. Brinkmann have disclosed having no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The new findings have the potential to revolutionize the management of patients with epilepsy, according to the researchers. “We have set a first benchmark for automatic detection of a variety of epileptic seizures using wearable sensors and deep-learning algorithms. In other words, we have shown for the first time that it’s possible to do this,” said study investigator Jianbin Tang, MA, data science project lead, IBM Research Australia, Victoria.
The findings were presented at the American Epilepsy Society’s annual meeting, held online this year because of the COVID-19 pandemic.
Accurate monitoring of seizures is important for assessing risk, injury prevention, and treatment response evaluation. Currently, video EEG is the gold standard for seizure detection, but it requires a hospital stay, is often costly, and can be stigmatizing, said Mr. Tang.
An advance in detecting seizure types
Recent advances in non-EEG wearable devices show promise in detecting generalized onset tonic-clonic and focal to bilateral tonic-clonic seizures, but it’s not clear if they have the ability to detect other seizure types. “We hope to fill this gap by expanding wearable seizure detection to additional seizure types,” said Mr. Tang.
Seizure tracking outside the hospital setting largely “relies on manually annotated family and patient reports, which often can be unreliable due to missed seizures and problems recalling seizures,” he said.
The study included 75 children (44% were female; mean age was 11.1 years) admitted to a long-term EEG monitoring unit at a single center for a 24-hour stay. Patients wore the detector on the ankle or wrist. The device continuously collected data on functions such as sweating, heart rate, movement, and temperature.
With part of the dataset, researchers trained deep-learning algorithms to automatically detect seizure segments. They then validated the performance of the detection algorithms on the remainder of the dataset.
The analysis was based on data from 722 epileptic seizures of all types including focal and generalized, motor and nonmotor. Seizures occurred throughout the day and during the night while patients were awake or asleep.
When a seizure is detected, the system triggers a real-time alert and will store the information about the detected seizure in a repository, said Mr. Tang.
The signals were initially stored in the wristband and then securely uploaded to the Cloud. From there, the signal files were downloaded by the investigators for analysis and interpretation. All data were entirely anonymized and de-identified. Researchers used Area Under Curve–Receiver Operating Characteristic (AUC-ROC) to assess performance.
“Our best performing detection models reach an AUC-ROC of 67.59%, which represents a decent performance level,” said Mr. Tang. “There certainly is room for performance improvement and we are already working on this,” he added.
The device performed “better than chance,” which is a “standard technical term” in the field of machine learning and is “the first hurdle any machine-learning model needs to take to be considered useful.” The investigators noted that such automatic seizure detection “is feasible across a broad spectrum of epileptic seizure types,” said Mr. Tang. “This is a first and has not been shown before.”
The study suggests that the noninvasive wearable device could be used at home, at school, and in other everyday settings outside the clinic. “This could one day provide patients, caregivers, and clinicians with reliable seizure reports,” said Mr. Tang.
He said he believes the device might be especially useful in detecting frequent or subtle seizures, which are easy to miss. Patients requiring medication evaluation and rescue medication and those at risk of status epilepticus may be good candidates.
The researchers don’t expect wearable technology to totally replace EEG but see it as “a useful complementary tool to track seizures continuously at times or in settings where EEG monitoring is not available,” said Mr. Tang.
‘Important milestone’
Commenting on the research, Benjamin H. Brinkmann, PhD, associate professor of neurology at the Mayo Clinic in Rochester, Minn., said the investigators “have done very good work applying state of the art machine learning techniques” to the “important problem” of accurately detecting seizures.
Dr. Brinkmann is part of the Epilepsy Foundation–sponsored “My Seizure Gauge” project that’s evaluating various wearable devices, including the Empatica E4 wristband and the Fitbit Charge 3, to determine what measurements are needed for reliable seizure forecasting.
“Previously, no one knew whether seizure prediction was possible with these devices, and the fact that this group was able to achieve ‘better-than-chance’ prediction accuracy is an important milestone.”
However, he emphasized that there is still a great deal of work to be done to determine, for example, if seizure prediction with these devices can be accurate enough to be clinically useful. “For example, if the system generates too many false-positive predictions, patients won’t use it.”
In addition, the findings need to be replicated and recordings extended to 6 months or more to determine whether they are helpful to patients long term and in the home environment, said Dr. Brinkmann.
The investigators and Dr. Brinkmann have disclosed having no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The new findings have the potential to revolutionize the management of patients with epilepsy, according to the researchers. “We have set a first benchmark for automatic detection of a variety of epileptic seizures using wearable sensors and deep-learning algorithms. In other words, we have shown for the first time that it’s possible to do this,” said study investigator Jianbin Tang, MA, data science project lead, IBM Research Australia, Victoria.
The findings were presented at the American Epilepsy Society’s annual meeting, held online this year because of the COVID-19 pandemic.
Accurate monitoring of seizures is important for assessing risk, injury prevention, and treatment response evaluation. Currently, video EEG is the gold standard for seizure detection, but it requires a hospital stay, is often costly, and can be stigmatizing, said Mr. Tang.
An advance in detecting seizure types
Recent advances in non-EEG wearable devices show promise in detecting generalized onset tonic-clonic and focal to bilateral tonic-clonic seizures, but it’s not clear if they have the ability to detect other seizure types. “We hope to fill this gap by expanding wearable seizure detection to additional seizure types,” said Mr. Tang.
Seizure tracking outside the hospital setting largely “relies on manually annotated family and patient reports, which often can be unreliable due to missed seizures and problems recalling seizures,” he said.
The study included 75 children (44% were female; mean age was 11.1 years) admitted to a long-term EEG monitoring unit at a single center for a 24-hour stay. Patients wore the detector on the ankle or wrist. The device continuously collected data on functions such as sweating, heart rate, movement, and temperature.
With part of the dataset, researchers trained deep-learning algorithms to automatically detect seizure segments. They then validated the performance of the detection algorithms on the remainder of the dataset.
The analysis was based on data from 722 epileptic seizures of all types including focal and generalized, motor and nonmotor. Seizures occurred throughout the day and during the night while patients were awake or asleep.
When a seizure is detected, the system triggers a real-time alert and will store the information about the detected seizure in a repository, said Mr. Tang.
The signals were initially stored in the wristband and then securely uploaded to the Cloud. From there, the signal files were downloaded by the investigators for analysis and interpretation. All data were entirely anonymized and de-identified. Researchers used Area Under Curve–Receiver Operating Characteristic (AUC-ROC) to assess performance.
“Our best performing detection models reach an AUC-ROC of 67.59%, which represents a decent performance level,” said Mr. Tang. “There certainly is room for performance improvement and we are already working on this,” he added.
The device performed “better than chance,” which is a “standard technical term” in the field of machine learning and is “the first hurdle any machine-learning model needs to take to be considered useful.” The investigators noted that such automatic seizure detection “is feasible across a broad spectrum of epileptic seizure types,” said Mr. Tang. “This is a first and has not been shown before.”
The study suggests that the noninvasive wearable device could be used at home, at school, and in other everyday settings outside the clinic. “This could one day provide patients, caregivers, and clinicians with reliable seizure reports,” said Mr. Tang.
He said he believes the device might be especially useful in detecting frequent or subtle seizures, which are easy to miss. Patients requiring medication evaluation and rescue medication and those at risk of status epilepticus may be good candidates.
The researchers don’t expect wearable technology to totally replace EEG but see it as “a useful complementary tool to track seizures continuously at times or in settings where EEG monitoring is not available,” said Mr. Tang.
‘Important milestone’
Commenting on the research, Benjamin H. Brinkmann, PhD, associate professor of neurology at the Mayo Clinic in Rochester, Minn., said the investigators “have done very good work applying state of the art machine learning techniques” to the “important problem” of accurately detecting seizures.
Dr. Brinkmann is part of the Epilepsy Foundation–sponsored “My Seizure Gauge” project that’s evaluating various wearable devices, including the Empatica E4 wristband and the Fitbit Charge 3, to determine what measurements are needed for reliable seizure forecasting.
“Previously, no one knew whether seizure prediction was possible with these devices, and the fact that this group was able to achieve ‘better-than-chance’ prediction accuracy is an important milestone.”
However, he emphasized that there is still a great deal of work to be done to determine, for example, if seizure prediction with these devices can be accurate enough to be clinically useful. “For example, if the system generates too many false-positive predictions, patients won’t use it.”
In addition, the findings need to be replicated and recordings extended to 6 months or more to determine whether they are helpful to patients long term and in the home environment, said Dr. Brinkmann.
The investigators and Dr. Brinkmann have disclosed having no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM AES 2020