User login
QDoes postmenopausal use of unopposed estrogen increase the risk of breast cancer?
<huc>A</huc>Yes, if the estrogen is oral estradiol and it is used for 5 years or longer. When Lyytinen and colleagues studied different estrogen doses, constituents, and routes of administration in a cohort representing the entire postmenopausal population of Finland, they found an additional 2 to 3 cases of breast cancer for every 1,000 women when oral estradiol was used for 5 years or more. When it was used for a shorter time, or when the estrogen was oral estriol or a vaginal formulation, there was no increase in risk.
Expert Commentary
Statistical modeling cannot adequately account for the multiple variables involved in complex conditions such as breast cancer. For example, the GAIL model, which is used to predict an individual’s chance of having breast cancer, will only correctly score 59% of women with cancer; 41% of women with cancer will have a lower score estimate than their cancer-free cohorts. In short, “current breast cancer risk prediction models perform well for populations but poorly for individuals.”1
Breast cancer is not a single disease
Estrogen-related breast cancer is preceded histologically by atypical epithelial hyperplasia that progresses to invasive disease in some but not all women. Women who develop breast cancer while taking estrogen are more likely to have immature duct epithelium that is predominantly estrogen receptor-alpha (ERα). They are also likely to be genetically susceptible to modified physiologic cell growth and estrogen-metabolizing pathways in response to various environmental carcinogens or oncogenic promoters. In this context, exogenous estrogen may be a promoter, but not an instigator, of breast cancer.
A deficiency of vitamin D also plays a role. Vitamin D has potent antiproliferative effects that include the differentiation of breast tissue, enhanced apoptosis, and inhibition of cancer cell growth.
Untreated women with breast cancer have higher tissue levels of estrogen, which are correlated with increased breast-tissue enzymatic activity (aromatase, sulfatase, and 17β-OH dehydrogenase), especially in women with a genetic predisposition to increased or aberrant breast-tissue estrogen synthesis and metabolism. Other inherent factors include gene mutation involving cell-cycle growth (BRCA1, BRCA2, p53), and the ratio and expression of estrogen receptors; estrogen-therapy-associated breast cancer is more prevalent in women with a predominant ERα/ERβ ratio.
Mammographic density reflects the breast’s hormonal environment, the influence of background genetics, and the effect of various types, dosages, and routes of exogenous estrogen.
Not all estrogen is bioavailable
About 95% of orally administered estradiol is metabolized to estrone, estrone sulfate, and estradiol glucoronide. The bioconversion of these pro-hormones to more potent estradiol is dependent on the estrogen-metabolizing enzymes noted previously, the dose of estrogen, and the route of administration. Only 5% of orally administered estradiol is bioavailable. Because of the hepatic first-pass effect, 1 mg of oral 17β-estradiol and 25 μg of transdermal estrogen yield equivalent levels of free serum estradiol.
Variability in these and unknown factors account for the differing results of population-based studies and meta-analyses. It also may explain why, in a randomly selected group of Finnish women, only 2 to 3 extra cases of breast cancer for every 1,000 women were detected after 10 years of estrogen therapy, and at a dose twice that currently recommended.
Timing is critical, too
In the estrogen-alone arm of the Women’s Health Initiative, women aged 50 to 59 years—who are most likely to be treated with estrogen in everyday clinical practice—derived cardiovascular protection (hazard ratio [HR], 0.56), reduced colorectal cancer incidence, and a reduction in breast cancer (HR, 0.72). In contrast, most of the women in the study by Lyytinen and colleagues were over age 60. Other important risk factors not noted in their study include parity (pregnancy induces differentiation and maturation of breast ductal epithelium), pretreatment mammographic density, and vitamin D status.
Clinical recommendations
- Conduct a full clinical evaluation before initiating estrogen therapy
- Assess mammographic density before and after initiation of estrogen therapy. If density increases, stop therapy or reduce the dosage and repeat mammography in 3 to 6 months
- Measure high-sensitivity serum estradiol in women at high risk. Values in excess of 10 pg/dL may reflect an increased risk of breast cancer in untreated women—although no particular level of concern has been definitively identified
- Individualize dose and length of therapy according to age and indication.
Arbitrary restriction of estrogen therapy to 5 years is not biologically rational or clinically justifiable.
1. Elmore JG, Fletcher SW. The risk of cancer risk predisposition: “What is my risk of getting breast cancer?” J Natl Cancer Inst. 2006;98:1673-1675.
<huc>A</huc>Yes, if the estrogen is oral estradiol and it is used for 5 years or longer. When Lyytinen and colleagues studied different estrogen doses, constituents, and routes of administration in a cohort representing the entire postmenopausal population of Finland, they found an additional 2 to 3 cases of breast cancer for every 1,000 women when oral estradiol was used for 5 years or more. When it was used for a shorter time, or when the estrogen was oral estriol or a vaginal formulation, there was no increase in risk.
Expert Commentary
Statistical modeling cannot adequately account for the multiple variables involved in complex conditions such as breast cancer. For example, the GAIL model, which is used to predict an individual’s chance of having breast cancer, will only correctly score 59% of women with cancer; 41% of women with cancer will have a lower score estimate than their cancer-free cohorts. In short, “current breast cancer risk prediction models perform well for populations but poorly for individuals.”1
Breast cancer is not a single disease
Estrogen-related breast cancer is preceded histologically by atypical epithelial hyperplasia that progresses to invasive disease in some but not all women. Women who develop breast cancer while taking estrogen are more likely to have immature duct epithelium that is predominantly estrogen receptor-alpha (ERα). They are also likely to be genetically susceptible to modified physiologic cell growth and estrogen-metabolizing pathways in response to various environmental carcinogens or oncogenic promoters. In this context, exogenous estrogen may be a promoter, but not an instigator, of breast cancer.
A deficiency of vitamin D also plays a role. Vitamin D has potent antiproliferative effects that include the differentiation of breast tissue, enhanced apoptosis, and inhibition of cancer cell growth.
Untreated women with breast cancer have higher tissue levels of estrogen, which are correlated with increased breast-tissue enzymatic activity (aromatase, sulfatase, and 17β-OH dehydrogenase), especially in women with a genetic predisposition to increased or aberrant breast-tissue estrogen synthesis and metabolism. Other inherent factors include gene mutation involving cell-cycle growth (BRCA1, BRCA2, p53), and the ratio and expression of estrogen receptors; estrogen-therapy-associated breast cancer is more prevalent in women with a predominant ERα/ERβ ratio.
Mammographic density reflects the breast’s hormonal environment, the influence of background genetics, and the effect of various types, dosages, and routes of exogenous estrogen.
Not all estrogen is bioavailable
About 95% of orally administered estradiol is metabolized to estrone, estrone sulfate, and estradiol glucoronide. The bioconversion of these pro-hormones to more potent estradiol is dependent on the estrogen-metabolizing enzymes noted previously, the dose of estrogen, and the route of administration. Only 5% of orally administered estradiol is bioavailable. Because of the hepatic first-pass effect, 1 mg of oral 17β-estradiol and 25 μg of transdermal estrogen yield equivalent levels of free serum estradiol.
Variability in these and unknown factors account for the differing results of population-based studies and meta-analyses. It also may explain why, in a randomly selected group of Finnish women, only 2 to 3 extra cases of breast cancer for every 1,000 women were detected after 10 years of estrogen therapy, and at a dose twice that currently recommended.
Timing is critical, too
In the estrogen-alone arm of the Women’s Health Initiative, women aged 50 to 59 years—who are most likely to be treated with estrogen in everyday clinical practice—derived cardiovascular protection (hazard ratio [HR], 0.56), reduced colorectal cancer incidence, and a reduction in breast cancer (HR, 0.72). In contrast, most of the women in the study by Lyytinen and colleagues were over age 60. Other important risk factors not noted in their study include parity (pregnancy induces differentiation and maturation of breast ductal epithelium), pretreatment mammographic density, and vitamin D status.
Clinical recommendations
- Conduct a full clinical evaluation before initiating estrogen therapy
- Assess mammographic density before and after initiation of estrogen therapy. If density increases, stop therapy or reduce the dosage and repeat mammography in 3 to 6 months
- Measure high-sensitivity serum estradiol in women at high risk. Values in excess of 10 pg/dL may reflect an increased risk of breast cancer in untreated women—although no particular level of concern has been definitively identified
- Individualize dose and length of therapy according to age and indication.
Arbitrary restriction of estrogen therapy to 5 years is not biologically rational or clinically justifiable.
<huc>A</huc>Yes, if the estrogen is oral estradiol and it is used for 5 years or longer. When Lyytinen and colleagues studied different estrogen doses, constituents, and routes of administration in a cohort representing the entire postmenopausal population of Finland, they found an additional 2 to 3 cases of breast cancer for every 1,000 women when oral estradiol was used for 5 years or more. When it was used for a shorter time, or when the estrogen was oral estriol or a vaginal formulation, there was no increase in risk.
Expert Commentary
Statistical modeling cannot adequately account for the multiple variables involved in complex conditions such as breast cancer. For example, the GAIL model, which is used to predict an individual’s chance of having breast cancer, will only correctly score 59% of women with cancer; 41% of women with cancer will have a lower score estimate than their cancer-free cohorts. In short, “current breast cancer risk prediction models perform well for populations but poorly for individuals.”1
Breast cancer is not a single disease
Estrogen-related breast cancer is preceded histologically by atypical epithelial hyperplasia that progresses to invasive disease in some but not all women. Women who develop breast cancer while taking estrogen are more likely to have immature duct epithelium that is predominantly estrogen receptor-alpha (ERα). They are also likely to be genetically susceptible to modified physiologic cell growth and estrogen-metabolizing pathways in response to various environmental carcinogens or oncogenic promoters. In this context, exogenous estrogen may be a promoter, but not an instigator, of breast cancer.
A deficiency of vitamin D also plays a role. Vitamin D has potent antiproliferative effects that include the differentiation of breast tissue, enhanced apoptosis, and inhibition of cancer cell growth.
Untreated women with breast cancer have higher tissue levels of estrogen, which are correlated with increased breast-tissue enzymatic activity (aromatase, sulfatase, and 17β-OH dehydrogenase), especially in women with a genetic predisposition to increased or aberrant breast-tissue estrogen synthesis and metabolism. Other inherent factors include gene mutation involving cell-cycle growth (BRCA1, BRCA2, p53), and the ratio and expression of estrogen receptors; estrogen-therapy-associated breast cancer is more prevalent in women with a predominant ERα/ERβ ratio.
Mammographic density reflects the breast’s hormonal environment, the influence of background genetics, and the effect of various types, dosages, and routes of exogenous estrogen.
Not all estrogen is bioavailable
About 95% of orally administered estradiol is metabolized to estrone, estrone sulfate, and estradiol glucoronide. The bioconversion of these pro-hormones to more potent estradiol is dependent on the estrogen-metabolizing enzymes noted previously, the dose of estrogen, and the route of administration. Only 5% of orally administered estradiol is bioavailable. Because of the hepatic first-pass effect, 1 mg of oral 17β-estradiol and 25 μg of transdermal estrogen yield equivalent levels of free serum estradiol.
Variability in these and unknown factors account for the differing results of population-based studies and meta-analyses. It also may explain why, in a randomly selected group of Finnish women, only 2 to 3 extra cases of breast cancer for every 1,000 women were detected after 10 years of estrogen therapy, and at a dose twice that currently recommended.
Timing is critical, too
In the estrogen-alone arm of the Women’s Health Initiative, women aged 50 to 59 years—who are most likely to be treated with estrogen in everyday clinical practice—derived cardiovascular protection (hazard ratio [HR], 0.56), reduced colorectal cancer incidence, and a reduction in breast cancer (HR, 0.72). In contrast, most of the women in the study by Lyytinen and colleagues were over age 60. Other important risk factors not noted in their study include parity (pregnancy induces differentiation and maturation of breast ductal epithelium), pretreatment mammographic density, and vitamin D status.
Clinical recommendations
- Conduct a full clinical evaluation before initiating estrogen therapy
- Assess mammographic density before and after initiation of estrogen therapy. If density increases, stop therapy or reduce the dosage and repeat mammography in 3 to 6 months
- Measure high-sensitivity serum estradiol in women at high risk. Values in excess of 10 pg/dL may reflect an increased risk of breast cancer in untreated women—although no particular level of concern has been definitively identified
- Individualize dose and length of therapy according to age and indication.
Arbitrary restriction of estrogen therapy to 5 years is not biologically rational or clinically justifiable.
1. Elmore JG, Fletcher SW. The risk of cancer risk predisposition: “What is my risk of getting breast cancer?” J Natl Cancer Inst. 2006;98:1673-1675.
1. Elmore JG, Fletcher SW. The risk of cancer risk predisposition: “What is my risk of getting breast cancer?” J Natl Cancer Inst. 2006;98:1673-1675.
New estrogen guidelines: 2 experts give opposing views
The decision by the US Food and Drug Administration (FDA) to put warning labels on all estrogen and estrogen-progestin products prescribed for postmenopausal women is startling—especially when you consider that barely a year ago, estrogen was viewed as a remedy or preventive for all kinds of ills.
This reversal in the official status of estrogen has created shock waves among Ob/Gyns still struggling to answer patients’ questions and counsel them appropriately.
The FDA’s role has been anything but passive; early this year, it issued several recommendations on the use of estrogen and estrogenprogestin hormone replacement therapy (HRT) by postmenopausal women. The FDA:
- acknowledged that estrogen and estrogen-progestin formulations remain the most effective treatment for hot flashes and night sweats caused by menopause, but counseled doctors to prescribe the lowest possible dose for the shortest duration.
- advised against using HRT to prevent cardiovascular disease.
- urged clinicians to consider approved non-estrogen agents when prescribing HRT to prevent menopause-induced osteoporosis, reserving estrogen for cases in which the risk of osteoporosis is greater than the risks associated with the therapy. (See related article “New options in osteoporosis therapy: combination and sequential treatment”.)
- recommended that, until more data become available, all estrogens—with or without a progestin—be presumed to carry risks similar to those observed for conjugated equine estrogen (CEE) and medroxyprogesterone acetate (MPA) in the Women’s Health Initiative (WHI).
The best advice came from FDA Commissioner Mark McClellan, MD, PhD, who encouraged women to consult their physicians about the clinical implications of the WHI findings.
Although concrete data on the risks and benefits of estrogen have never been so substantial, considerable disagreement remains over how to proceed from here. To provide our readers with additional perspective and insight, OBG Management asked 2 international experts, Dr. Morris Notelovitz and Dr. Susan Love, to offer their views on the WHI findings and other aspects of postmenopausal estrogen use.
—Robert L. Barbieri, MD
Editor-in-Chief
Beware of widespread preventive therapies
The recent FDA decision to require warning labels on all estrogen and estrogen-progestin products prescribed for postmenopausal women is a vindication for all of us who have been worried about the widespread use of these drugs for prevention. (Note that this article is not about symptom relief; short-term use of hormone therapy for this indication is a different discussion.)
Although many women and doctors were shocked by the data from the long-overdue randomized, controlled trials on the use of HRT for prevention, there were many others who cheered—not because of the findings, but because at last we were doing the kind of studies that would tell us whether the commonly held hypothesis about these drugs was true.
Those who are holding on to the fact that the WHI’s estrogen-alone study has not yet been halted as evidence that progestin is the culprit should note that an increase in heart attacks and strokes has been seen in this cohort as well. The breast cancer risk may be less without the progestin, but many studies suggest that it certainly is not zero. Plus, the smaller size of the study means it would take longer to reach the same stopping goals. The risk-benefit ratio is likely to be similar to that for estrogen-progestin for most endpoints.
An abundance of observational data
Prior to the Heart and Estrogen-progestin Replacement Study (HERS) and WHI trials, only 1 long-term randomized, controlled trial had explored postmenopausal HRT, and it was too small to yield definitive data.1-3 The rest of the many studies looking at the benefits and risks of hormone therapy for prevention were based on observation. Indeed, the overwhelming majority of them demonstrated that HRT decreased heart disease.4,5 But these studies were still observational. Observational studies cannot prove cause and effect.
As we now know all too well, women who took postmenopausal HRT were, in general, of a higher socioeconomic level, better educated, and healthier than the women who did not.6 It was not a matter of hormones making women healthy, but rather, healthy women taking hormones.
Women who can generate as little as 5 pg/mL of their own estrogen have almost no fractures; these data suggest that we probably do not have to “replace” hormones in most women.
—Dr. Love
In itself this is not surprising. Confounding is common in observational studies and is one of the reasons this research is better at driving hypotheses than proving cause and effect. Somehow, however, the number and consistency of these studies clouded our collective judgment and caused us to get ahead of the data. It is not the first time we have let this happen, and I am sure it will not be the last.
In breast cancer, for example, the use of high-dose chemotherapy with stem-cell rescue became the standard of care before there were any randomized data demonstrating its value. When the randomized studies did finally come in, many clinicians were surprised to find that this aggressive regimen was no better than standard therapy and had worse side effects.7 Now, the use of this therapy has virtually ceased.
It would behoove us to follow this lead in the use of hormones for prevention. In a recent analysis at the National Cancer Institute meeting on HRT, Deborah Grady could find no subgroup, including women with an osteoporotic fracture, where the benefits outweighed the risk.8
Exercise prescriptions should replace hormones, and weight should be monitored rather than bone density in a woman in her 50s.
—Dr. Love
Risks of rushing to substitute
What should we do? Many clinicians may wish to quickly find something else to give women—be it selective estrogen receptor modulators, bisphosphonates, or bio-identical hormones. In my view, that misses the point. This new data on postmenopausal hormone therapy should cause us to question the hypothesis upon which its use was based.
Perhaps we do not have to treat postmenopausal women with anything. Rather than equate menopause with ovarian failure or estrogen deficiency, perhaps we can regard it as the natural progression of a woman’s life. New studies indicate that postmenopausal women who are able to generate as little as 5 pg or more of their own estrogen per milliliter of serum have almost no fractures; these data suggest that we probably do not have to “replace” hormones in the majority of women.9
In addition, the data suggest that age is a more potent predictor of fracture risk than bone density.10 Many experts are suggesting that osteopenia should not be treated and that bone density should not be measured until age 65.
Deaths from heart disease are at all-time lows due mostly to improved treatment techniques rather than prevention.11
Lifestyle changes are still the best prevention
I would suggest that the warning label on the estrogen and estrogen-progestin formulations be viewed as a caution against the whole concept of widespread use of drugs in healthy women for prevention. Lifestyle changes remain the best way to maintain quality of life and prevent the diseases of aging. Weight control, exercise, diet, and not smoking are still the safest approaches to a healthy life.
Rather than continue this debate, we should put our energies into devising strategies to help women achieve healthy lifestyle goals. Exercise prescriptions should be the replacement for hormones, and weight should be monitored rather than bone density in a woman in her 50s. Advice about smoking cessation needs to take the place of discussions of breast self-exam.
My hope is that this warning will serve as a wake-up call for all who care for women.
Dr. Love reports no financial arrangements or affiliations with any of the companies that manufacture products mentioned in this article or their competitors.
REFERENCES
1. Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA. 1998;280:605-613.
2. Writing Group for the Women’s Health Initiative Randomized Controlled Trial Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
3. Nachtigall LE, Nachtigall R, Nachtigall RD, Beckman EM. Estrogen replacement therapy II: A prospective study in the relationship to carcinoma and cardiovascular and metabolic problems. Obstet Gynecol. 1979;54(1):74-79.
4. Stampfer MJ, Colditz GA. Estrogen replacement therapy and coronary heart disease: A quantitative assessment of the epidemiologic evidence. Prev Med. 1991;20:47-63.
5. Grodstein E, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use: The risk of cardiovascular disease. N Engl J Med. 1996;335:453-461.
6. Barrett-Connor E. Postmenopausal estrogen and prevention bias. Ann Intern Med. 1991;115:455-456.
7. Peters W, Rosner G, Vredenburgh J, et al. A prospective, randomized comparison of two doses of combination alkylating agents as consolidation after CAF in high-risk primary breast cancer involving ten or more axillary lymph nodes: Preliminary results of CALBG9082/SWOG9114/NCIC MA-13. Proc Am Soc Clin Oncol. 1999;18:1a.-Abstract.
8. Grady D. Postmenopausal hormone therapy: balancing the risks and benefits. Presented at: National Institutes of Health Scientific Workshop on Menopausal Hormone Therapy; October 23, 2002; Bethesda, Md.
9. Cummings SR, Browner WS, Bauer D, et al. Study of Osteoporotic Fractures Research Group. Endogenous hormones and the risk of hip and vertebral fractures among older women. N Engl J Med. 1998;339:733-738.
10. Kanis JA, Johnell O, et al. Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone. 2000;27:585-590.
11. Kolata G. Gains on heart disease leave more survivors, and questions. New York Times. January 19, 2003;sect 1:1.-
Estrogen is a valid option when prescribed correctly
Women are living longer, but not necessarily better. Increases in longevity are partially offset by a greater prevalence of chronic conditions such as osteoporosis, cardiovascular disease, cognitive dysfunction, and breast cancer—all of which impact a woman’s quality of life. HRT is a logical outgrowth of this increased longevity.
Unfortunately, while it represents an attempt to improve the health and well-being of postmenopausal women, HRT is based upon a faulty premise: that all women are biologically equal and react similarly to the menopausal transition. Equally erroneous are 2 corollaries: that all menopausal women will respond to the same dose of HRT and that all estrogen formulations are comparable.
As has become clear, this generic approach to menopause is inappropriate. The convenient but simplistic strategy of treating all women at and beyond menopause with a standard dose of the same estrogen-progestin formulation is ill-founded. Estrogen offers the postmenopausal patient numerous benefits and needs to remain an important part of the Ob/Gyn’s options. However, it can no longer be prescribed in the “traditional” manner.
The trouble with tradition
Here are 2 problems with the conventional approach:
- Every woman synthesizes estrogen differently, depending on the endocrinology of her nonreproductive organs in the premenopausal, perimenopausal, and postmenopausal periods; the pathogenesis of conditions such as cardiovascular disease and their relationship to estrogen and androgen synthesis and metabolism; and the pharmacokinetic and pharmacodynamic variance between HRT formulations.1,2
- Women are encouraged to have annual examinations, yet a review of the type and dose of HRT rarely takes place at these exams.
New strategy: Replenish hormones to age 65, maintain thereafter
Women need “individualized and adjusted hormone therapy.” This is relevant for patients 35 to 65 years of age and is based on our ability to tailor the type and route of hormone therapy to approximate the hormonal milieu of women at a given age. The term “HRT”—which I define as the attempt to replicate a premenopausal woman’s hormonal milieu—should be restricted to women who are between the ages of 35 and 45 who need hormone therapy. After that, hormone replenishment should be practiced until age 65. Based on the pharmacokinetics of estrogen, HRT is best achieved by non-oral estradiol; hormone replenishment relies on the bioconversion of estradiol to estrone after oral estrogen and the “normal” postmenopausal estrone:estradiol ratio. Hormone maintenance refers to women who have been stabilized on a prior hormonal regimen. They should be left on their current medication as long as there is still an indication for hormone therapy.
The type, dose, and route of this therapy should be regularly reviewed and adjusted, if necessary, as a woman’s needs change over time.
Estrogen synthesis and metabolism. Only 2 bioavailable estrogens are synthesized in postmenopausal women: estradiol and estrone. Both are derived from the aromatization of androgens in adipose tissue and muscle and are further metabolized by the liver. The aromatization of androgens to estrogens occurs in tissues such as breast, bone, and coronary artery, and the local concentration far exceeds that measured in the peripheral circulation. The estrogen synthesized locally and the metabolites produced by the liver can have protective effects (increased bone density) or potentially harmful effects (breast cancer), even though serum estradiol may be within a “normal” range (i.e., less than 20 pg per deciliter).
The synthesis and metabolism of estrogen are genetically controlled. For example, the genes determine whether a woman has a high risk of breast cancer. Therefore, clinicians should select the dose and route of estrogen administration that would optimize the benefit and limit the risk of hormone therapy. This will be different in each woman. (Although most postmenopausal women can safely take hormones, some may have an endogenous abnormality that precludes the therapy.)
Fraction of dose may relieve symptoms. The estrogen threshold for the relief of hot flashes—HRT’s main indication—also varies among women. One half to one quarter of the “standard” dose (0.625 mg per day of CEE)—the amount prescribed in the WHI3—has been shown to be effective.
The long trajectory of ‘menopausal’ diseases
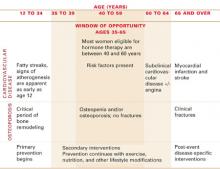
The pathogenesis of osteoporosis and cardiovascular disease—conditions for which longterm HRT has been advocated—commences with the first menstrual period (FIGURE). Thus, primary prevention should begin in early adulthood. This includes diet and lifestyle modifications and exercise. Normal ovarian function is essential, as anovulatory hypoestrogenic disorders predispose young women to a greater risk of these conditions later in life.
Endogenous estrogen’s protective effect is based on the presence of estrogen—and androgen—receptors in bone (e.g., osteoblasts, osteoclasts) and in the coronary artery (e.g., endothelium, smooth muscle) and liver. As estrogen levels decline, bone remodeling accelerates and bone mineral is lost; the process of atherothrombosis also accelerates. Given the multifactorial nature of these conditions, estrogen therapy plays an important role in stabilizing bone loss and halting the progression of atheromatosis, both at menopause and at other times when a lack of estrogen is a relevant causative factor. When bone loss is due to hyperthyroidism or when cardiovascular disease is associated with dyslipidemia, hypertension or diabetes, disease-specific treatment is needed.
Individualizing HRT to condition and severity
As for HRT, the dosage and type need to be judged according to each clinical situation and degree of abnormality. For example, a lower dose of estrogen is required when a woman has osteopenia than when she has osteoporosis. Transdermal estrogen is the best option for a woman with elevated serum triglycerides or C-reactive protein (a cardiac inflammatory biomarker). Women with low levels of high-density–lipoprotein cholesterol will benefit from oral estrogen.
Measurement is central to this approach. Without a mammogram, breast density (a sign of local estrogen biosynthesis) cannot be documented or quantified. A bone-density test (with bone markers) is needed to assess bone health; a fasting lipid profile (including glucose) and possibly a C-reactive protein assay are the only means of assessing the patient’s cardiovascular disease risk status.
Prescribe lowest dose and monitor. Clinicians should prescribe the lowest estrogen dose and then monitor therapy. This entails measuring baseline serum estradiol and conducting meaningful posttreatment monitoring, best achieved with 17ß-estradiol-based products (oral or transdermal). A total serum estradiol value of 40 to 80 pg per milliliter has been found effective in controlling bone loss, coronary artery vasoreactivity, and cognition. The late initiation of hormone therapy is not recommended, since estrogen may disrupt the fibrin capsule of arterial intimal plaques and precipitate thrombosis with vascular luminal occlusion and myocardial infarction or stroke.
Not all hormones are the same
Not all estrogens or progestins are equal in their formulation, pharmacologic properties, or function. As noted previously, nonpregnant women synthesize only 2 bioavailable estrogens: estradiol and estrone. Pharmacologic preparations of 17ß-estradiol have properties similar to those of endogenous estrogen. Depending on the dose and route of administration, they can, to a certain degree, replicate a premenopausal or postmenopausal estrogen milieu. CEE, the preparation used in the WHI, contains 10 estrogens and 200 metabolites, with varying degrees of estrogenic and antiestrogenic activity. Thus, it is not possible to monitor posttreatment estradiol values.
It is significant that only the estrogenprogestin arm of the WHI was suspended. This suggests that MPA, the progestin in the combination therapy used in the trial, may be responsible for the unwanted results. There are a number of pharmacologic differences between MPA, natural progesterone, and the 19-nor-testosterone–derived progestins (e.g., norethindrone acetate [NETA]). In addition, the half-life of MPA (24 hours) greatly exceeds that of progesterone (12 hours) and NETA (6 to 8 hours), thus potentially downregulating estrogen receptors in vital blood vessels that may already be compromised.
Putting the WHI in perspective
The WHI was planned as a primary cardiovascular-disease–prevention trial. Of the women enrolled in the study, 45.3% were 60 to 69 years of age, and 21.3% were 70 to 79. Thus, given the pathogenesis of cardiovascular disease, most subjects had some degree of coronary artery disease at the start of the study. Yet only 37 hormone-group subjects versus 30 placebo-group subjects per 10,000 women annually experienced an adverse clinical cardiovascular event. Except for year 5, the ratio of such adverse events in the hormone group decreased over time, compared with women in the placebo group. The HRT:placebo ratios of these events for years 1 through 6 were 1.78, 1.15, 1.06, 0.99, 2.38, and 0.78, respectively. (The unexpected jump in the event ratio in year 5 was due to an unexplained paucity of events in the placebo group and not an increase in the group of subjects treated with hormone therapy.)
The WHI definition of “healthy postmenopausal woman” ignored the heterogeneity of the climacteric by assuming that all women were biologically equal and that age had not added its toll in organ damage. In a parallel observational arm of the WHI, C-reactive protein independently predicted vascular events among healthy postmenopausal women, but this was related to baseline levels of the inflammatory biomarkers and not to the hormone-therapy–related increase in C-reactive protein. The same is true for the stated increased risk of HRT-related breast cancer: 35 versus 30 events annually per 10,000 women on HRT and placebo, respectively. What differentiated the 35 who developed breast cancer from the 9,965 who did not?
Clinical challenge: Not to withhold HRT, but to identify women at risk
As clinicians, we must strive not to deny HRT to women who could safely benefit from it, but to develop cost-effective strategies to differentiate healthy women from those with metabolic dysfunction (e.g., premammographic breast cancer) and asymptomatic latent disease (e.g., silent atherogenesis). “Normal” women will benefit from selective HRT; the latter require medications specific to their underlying disorder.
In the aftermath of the WHI, the scope of the HRT problem has been overblown. When the absolute-risk numbers for HRT-related cardiovascular disease and breast cancer are extrapolated to the nation, the perceived size of the problem—which is only a mathematical projection and estimate—can assume troubling proportions. But physicians in clinical practice have only 1 responsibility: ensuring the health and well-being of their patients, 1 at a time. Thus, the question of HRT must be resolved between the physician and the patient. This takes time—time to talk with, examine, and test the patient; time to think through the problem; and time to prescribe and educate the patient regarding her therapeutic needs. This is time well spent.
FIGURE Female life span: Window of opportunity for hormone therapy*
Dr. Notelovitz reports no financial arrangements or affiliations with any of the companies that manufacture products mentioned in this article or their competitors.
1. Utian WH, Shoup D, Bachmann G, et al. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril. 2001;75:1065-1079.
2. Notelovitz M, Lenihan JP, McDermott M, et al. Initial 17ß-estradiol dose for treating vasomotor symptoms. Obstet Gynecol. 2000;95:726-731.
3. Writing Group for the Women’s Health Initiative Randomized Controlled Trial. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
The decision by the US Food and Drug Administration (FDA) to put warning labels on all estrogen and estrogen-progestin products prescribed for postmenopausal women is startling—especially when you consider that barely a year ago, estrogen was viewed as a remedy or preventive for all kinds of ills.
This reversal in the official status of estrogen has created shock waves among Ob/Gyns still struggling to answer patients’ questions and counsel them appropriately.
The FDA’s role has been anything but passive; early this year, it issued several recommendations on the use of estrogen and estrogenprogestin hormone replacement therapy (HRT) by postmenopausal women. The FDA:
- acknowledged that estrogen and estrogen-progestin formulations remain the most effective treatment for hot flashes and night sweats caused by menopause, but counseled doctors to prescribe the lowest possible dose for the shortest duration.
- advised against using HRT to prevent cardiovascular disease.
- urged clinicians to consider approved non-estrogen agents when prescribing HRT to prevent menopause-induced osteoporosis, reserving estrogen for cases in which the risk of osteoporosis is greater than the risks associated with the therapy. (See related article “New options in osteoporosis therapy: combination and sequential treatment”.)
- recommended that, until more data become available, all estrogens—with or without a progestin—be presumed to carry risks similar to those observed for conjugated equine estrogen (CEE) and medroxyprogesterone acetate (MPA) in the Women’s Health Initiative (WHI).
The best advice came from FDA Commissioner Mark McClellan, MD, PhD, who encouraged women to consult their physicians about the clinical implications of the WHI findings.
Although concrete data on the risks and benefits of estrogen have never been so substantial, considerable disagreement remains over how to proceed from here. To provide our readers with additional perspective and insight, OBG Management asked 2 international experts, Dr. Morris Notelovitz and Dr. Susan Love, to offer their views on the WHI findings and other aspects of postmenopausal estrogen use.
—Robert L. Barbieri, MD
Editor-in-Chief
Beware of widespread preventive therapies
The recent FDA decision to require warning labels on all estrogen and estrogen-progestin products prescribed for postmenopausal women is a vindication for all of us who have been worried about the widespread use of these drugs for prevention. (Note that this article is not about symptom relief; short-term use of hormone therapy for this indication is a different discussion.)
Although many women and doctors were shocked by the data from the long-overdue randomized, controlled trials on the use of HRT for prevention, there were many others who cheered—not because of the findings, but because at last we were doing the kind of studies that would tell us whether the commonly held hypothesis about these drugs was true.
Those who are holding on to the fact that the WHI’s estrogen-alone study has not yet been halted as evidence that progestin is the culprit should note that an increase in heart attacks and strokes has been seen in this cohort as well. The breast cancer risk may be less without the progestin, but many studies suggest that it certainly is not zero. Plus, the smaller size of the study means it would take longer to reach the same stopping goals. The risk-benefit ratio is likely to be similar to that for estrogen-progestin for most endpoints.
An abundance of observational data
Prior to the Heart and Estrogen-progestin Replacement Study (HERS) and WHI trials, only 1 long-term randomized, controlled trial had explored postmenopausal HRT, and it was too small to yield definitive data.1-3 The rest of the many studies looking at the benefits and risks of hormone therapy for prevention were based on observation. Indeed, the overwhelming majority of them demonstrated that HRT decreased heart disease.4,5 But these studies were still observational. Observational studies cannot prove cause and effect.
As we now know all too well, women who took postmenopausal HRT were, in general, of a higher socioeconomic level, better educated, and healthier than the women who did not.6 It was not a matter of hormones making women healthy, but rather, healthy women taking hormones.
Women who can generate as little as 5 pg/mL of their own estrogen have almost no fractures; these data suggest that we probably do not have to “replace” hormones in most women.
—Dr. Love
In itself this is not surprising. Confounding is common in observational studies and is one of the reasons this research is better at driving hypotheses than proving cause and effect. Somehow, however, the number and consistency of these studies clouded our collective judgment and caused us to get ahead of the data. It is not the first time we have let this happen, and I am sure it will not be the last.
In breast cancer, for example, the use of high-dose chemotherapy with stem-cell rescue became the standard of care before there were any randomized data demonstrating its value. When the randomized studies did finally come in, many clinicians were surprised to find that this aggressive regimen was no better than standard therapy and had worse side effects.7 Now, the use of this therapy has virtually ceased.
It would behoove us to follow this lead in the use of hormones for prevention. In a recent analysis at the National Cancer Institute meeting on HRT, Deborah Grady could find no subgroup, including women with an osteoporotic fracture, where the benefits outweighed the risk.8
Exercise prescriptions should replace hormones, and weight should be monitored rather than bone density in a woman in her 50s.
—Dr. Love
Risks of rushing to substitute
What should we do? Many clinicians may wish to quickly find something else to give women—be it selective estrogen receptor modulators, bisphosphonates, or bio-identical hormones. In my view, that misses the point. This new data on postmenopausal hormone therapy should cause us to question the hypothesis upon which its use was based.
Perhaps we do not have to treat postmenopausal women with anything. Rather than equate menopause with ovarian failure or estrogen deficiency, perhaps we can regard it as the natural progression of a woman’s life. New studies indicate that postmenopausal women who are able to generate as little as 5 pg or more of their own estrogen per milliliter of serum have almost no fractures; these data suggest that we probably do not have to “replace” hormones in the majority of women.9
In addition, the data suggest that age is a more potent predictor of fracture risk than bone density.10 Many experts are suggesting that osteopenia should not be treated and that bone density should not be measured until age 65.
Deaths from heart disease are at all-time lows due mostly to improved treatment techniques rather than prevention.11
Lifestyle changes are still the best prevention
I would suggest that the warning label on the estrogen and estrogen-progestin formulations be viewed as a caution against the whole concept of widespread use of drugs in healthy women for prevention. Lifestyle changes remain the best way to maintain quality of life and prevent the diseases of aging. Weight control, exercise, diet, and not smoking are still the safest approaches to a healthy life.
Rather than continue this debate, we should put our energies into devising strategies to help women achieve healthy lifestyle goals. Exercise prescriptions should be the replacement for hormones, and weight should be monitored rather than bone density in a woman in her 50s. Advice about smoking cessation needs to take the place of discussions of breast self-exam.
My hope is that this warning will serve as a wake-up call for all who care for women.
Dr. Love reports no financial arrangements or affiliations with any of the companies that manufacture products mentioned in this article or their competitors.
REFERENCES
1. Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA. 1998;280:605-613.
2. Writing Group for the Women’s Health Initiative Randomized Controlled Trial Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
3. Nachtigall LE, Nachtigall R, Nachtigall RD, Beckman EM. Estrogen replacement therapy II: A prospective study in the relationship to carcinoma and cardiovascular and metabolic problems. Obstet Gynecol. 1979;54(1):74-79.
4. Stampfer MJ, Colditz GA. Estrogen replacement therapy and coronary heart disease: A quantitative assessment of the epidemiologic evidence. Prev Med. 1991;20:47-63.
5. Grodstein E, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use: The risk of cardiovascular disease. N Engl J Med. 1996;335:453-461.
6. Barrett-Connor E. Postmenopausal estrogen and prevention bias. Ann Intern Med. 1991;115:455-456.
7. Peters W, Rosner G, Vredenburgh J, et al. A prospective, randomized comparison of two doses of combination alkylating agents as consolidation after CAF in high-risk primary breast cancer involving ten or more axillary lymph nodes: Preliminary results of CALBG9082/SWOG9114/NCIC MA-13. Proc Am Soc Clin Oncol. 1999;18:1a.-Abstract.
8. Grady D. Postmenopausal hormone therapy: balancing the risks and benefits. Presented at: National Institutes of Health Scientific Workshop on Menopausal Hormone Therapy; October 23, 2002; Bethesda, Md.
9. Cummings SR, Browner WS, Bauer D, et al. Study of Osteoporotic Fractures Research Group. Endogenous hormones and the risk of hip and vertebral fractures among older women. N Engl J Med. 1998;339:733-738.
10. Kanis JA, Johnell O, et al. Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone. 2000;27:585-590.
11. Kolata G. Gains on heart disease leave more survivors, and questions. New York Times. January 19, 2003;sect 1:1.-
Estrogen is a valid option when prescribed correctly
Women are living longer, but not necessarily better. Increases in longevity are partially offset by a greater prevalence of chronic conditions such as osteoporosis, cardiovascular disease, cognitive dysfunction, and breast cancer—all of which impact a woman’s quality of life. HRT is a logical outgrowth of this increased longevity.
Unfortunately, while it represents an attempt to improve the health and well-being of postmenopausal women, HRT is based upon a faulty premise: that all women are biologically equal and react similarly to the menopausal transition. Equally erroneous are 2 corollaries: that all menopausal women will respond to the same dose of HRT and that all estrogen formulations are comparable.
As has become clear, this generic approach to menopause is inappropriate. The convenient but simplistic strategy of treating all women at and beyond menopause with a standard dose of the same estrogen-progestin formulation is ill-founded. Estrogen offers the postmenopausal patient numerous benefits and needs to remain an important part of the Ob/Gyn’s options. However, it can no longer be prescribed in the “traditional” manner.
The trouble with tradition
Here are 2 problems with the conventional approach:
- Every woman synthesizes estrogen differently, depending on the endocrinology of her nonreproductive organs in the premenopausal, perimenopausal, and postmenopausal periods; the pathogenesis of conditions such as cardiovascular disease and their relationship to estrogen and androgen synthesis and metabolism; and the pharmacokinetic and pharmacodynamic variance between HRT formulations.1,2
- Women are encouraged to have annual examinations, yet a review of the type and dose of HRT rarely takes place at these exams.
New strategy: Replenish hormones to age 65, maintain thereafter
Women need “individualized and adjusted hormone therapy.” This is relevant for patients 35 to 65 years of age and is based on our ability to tailor the type and route of hormone therapy to approximate the hormonal milieu of women at a given age. The term “HRT”—which I define as the attempt to replicate a premenopausal woman’s hormonal milieu—should be restricted to women who are between the ages of 35 and 45 who need hormone therapy. After that, hormone replenishment should be practiced until age 65. Based on the pharmacokinetics of estrogen, HRT is best achieved by non-oral estradiol; hormone replenishment relies on the bioconversion of estradiol to estrone after oral estrogen and the “normal” postmenopausal estrone:estradiol ratio. Hormone maintenance refers to women who have been stabilized on a prior hormonal regimen. They should be left on their current medication as long as there is still an indication for hormone therapy.
The type, dose, and route of this therapy should be regularly reviewed and adjusted, if necessary, as a woman’s needs change over time.
Estrogen synthesis and metabolism. Only 2 bioavailable estrogens are synthesized in postmenopausal women: estradiol and estrone. Both are derived from the aromatization of androgens in adipose tissue and muscle and are further metabolized by the liver. The aromatization of androgens to estrogens occurs in tissues such as breast, bone, and coronary artery, and the local concentration far exceeds that measured in the peripheral circulation. The estrogen synthesized locally and the metabolites produced by the liver can have protective effects (increased bone density) or potentially harmful effects (breast cancer), even though serum estradiol may be within a “normal” range (i.e., less than 20 pg per deciliter).
The synthesis and metabolism of estrogen are genetically controlled. For example, the genes determine whether a woman has a high risk of breast cancer. Therefore, clinicians should select the dose and route of estrogen administration that would optimize the benefit and limit the risk of hormone therapy. This will be different in each woman. (Although most postmenopausal women can safely take hormones, some may have an endogenous abnormality that precludes the therapy.)
Fraction of dose may relieve symptoms. The estrogen threshold for the relief of hot flashes—HRT’s main indication—also varies among women. One half to one quarter of the “standard” dose (0.625 mg per day of CEE)—the amount prescribed in the WHI3—has been shown to be effective.
The long trajectory of ‘menopausal’ diseases
The pathogenesis of osteoporosis and cardiovascular disease—conditions for which longterm HRT has been advocated—commences with the first menstrual period (FIGURE). Thus, primary prevention should begin in early adulthood. This includes diet and lifestyle modifications and exercise. Normal ovarian function is essential, as anovulatory hypoestrogenic disorders predispose young women to a greater risk of these conditions later in life.
Endogenous estrogen’s protective effect is based on the presence of estrogen—and androgen—receptors in bone (e.g., osteoblasts, osteoclasts) and in the coronary artery (e.g., endothelium, smooth muscle) and liver. As estrogen levels decline, bone remodeling accelerates and bone mineral is lost; the process of atherothrombosis also accelerates. Given the multifactorial nature of these conditions, estrogen therapy plays an important role in stabilizing bone loss and halting the progression of atheromatosis, both at menopause and at other times when a lack of estrogen is a relevant causative factor. When bone loss is due to hyperthyroidism or when cardiovascular disease is associated with dyslipidemia, hypertension or diabetes, disease-specific treatment is needed.
Individualizing HRT to condition and severity
As for HRT, the dosage and type need to be judged according to each clinical situation and degree of abnormality. For example, a lower dose of estrogen is required when a woman has osteopenia than when she has osteoporosis. Transdermal estrogen is the best option for a woman with elevated serum triglycerides or C-reactive protein (a cardiac inflammatory biomarker). Women with low levels of high-density–lipoprotein cholesterol will benefit from oral estrogen.
Measurement is central to this approach. Without a mammogram, breast density (a sign of local estrogen biosynthesis) cannot be documented or quantified. A bone-density test (with bone markers) is needed to assess bone health; a fasting lipid profile (including glucose) and possibly a C-reactive protein assay are the only means of assessing the patient’s cardiovascular disease risk status.
Prescribe lowest dose and monitor. Clinicians should prescribe the lowest estrogen dose and then monitor therapy. This entails measuring baseline serum estradiol and conducting meaningful posttreatment monitoring, best achieved with 17ß-estradiol-based products (oral or transdermal). A total serum estradiol value of 40 to 80 pg per milliliter has been found effective in controlling bone loss, coronary artery vasoreactivity, and cognition. The late initiation of hormone therapy is not recommended, since estrogen may disrupt the fibrin capsule of arterial intimal plaques and precipitate thrombosis with vascular luminal occlusion and myocardial infarction or stroke.
Not all hormones are the same
Not all estrogens or progestins are equal in their formulation, pharmacologic properties, or function. As noted previously, nonpregnant women synthesize only 2 bioavailable estrogens: estradiol and estrone. Pharmacologic preparations of 17ß-estradiol have properties similar to those of endogenous estrogen. Depending on the dose and route of administration, they can, to a certain degree, replicate a premenopausal or postmenopausal estrogen milieu. CEE, the preparation used in the WHI, contains 10 estrogens and 200 metabolites, with varying degrees of estrogenic and antiestrogenic activity. Thus, it is not possible to monitor posttreatment estradiol values.
It is significant that only the estrogenprogestin arm of the WHI was suspended. This suggests that MPA, the progestin in the combination therapy used in the trial, may be responsible for the unwanted results. There are a number of pharmacologic differences between MPA, natural progesterone, and the 19-nor-testosterone–derived progestins (e.g., norethindrone acetate [NETA]). In addition, the half-life of MPA (24 hours) greatly exceeds that of progesterone (12 hours) and NETA (6 to 8 hours), thus potentially downregulating estrogen receptors in vital blood vessels that may already be compromised.
Putting the WHI in perspective
The WHI was planned as a primary cardiovascular-disease–prevention trial. Of the women enrolled in the study, 45.3% were 60 to 69 years of age, and 21.3% were 70 to 79. Thus, given the pathogenesis of cardiovascular disease, most subjects had some degree of coronary artery disease at the start of the study. Yet only 37 hormone-group subjects versus 30 placebo-group subjects per 10,000 women annually experienced an adverse clinical cardiovascular event. Except for year 5, the ratio of such adverse events in the hormone group decreased over time, compared with women in the placebo group. The HRT:placebo ratios of these events for years 1 through 6 were 1.78, 1.15, 1.06, 0.99, 2.38, and 0.78, respectively. (The unexpected jump in the event ratio in year 5 was due to an unexplained paucity of events in the placebo group and not an increase in the group of subjects treated with hormone therapy.)
The WHI definition of “healthy postmenopausal woman” ignored the heterogeneity of the climacteric by assuming that all women were biologically equal and that age had not added its toll in organ damage. In a parallel observational arm of the WHI, C-reactive protein independently predicted vascular events among healthy postmenopausal women, but this was related to baseline levels of the inflammatory biomarkers and not to the hormone-therapy–related increase in C-reactive protein. The same is true for the stated increased risk of HRT-related breast cancer: 35 versus 30 events annually per 10,000 women on HRT and placebo, respectively. What differentiated the 35 who developed breast cancer from the 9,965 who did not?
Clinical challenge: Not to withhold HRT, but to identify women at risk
As clinicians, we must strive not to deny HRT to women who could safely benefit from it, but to develop cost-effective strategies to differentiate healthy women from those with metabolic dysfunction (e.g., premammographic breast cancer) and asymptomatic latent disease (e.g., silent atherogenesis). “Normal” women will benefit from selective HRT; the latter require medications specific to their underlying disorder.
In the aftermath of the WHI, the scope of the HRT problem has been overblown. When the absolute-risk numbers for HRT-related cardiovascular disease and breast cancer are extrapolated to the nation, the perceived size of the problem—which is only a mathematical projection and estimate—can assume troubling proportions. But physicians in clinical practice have only 1 responsibility: ensuring the health and well-being of their patients, 1 at a time. Thus, the question of HRT must be resolved between the physician and the patient. This takes time—time to talk with, examine, and test the patient; time to think through the problem; and time to prescribe and educate the patient regarding her therapeutic needs. This is time well spent.
FIGURE Female life span: Window of opportunity for hormone therapy*
Dr. Notelovitz reports no financial arrangements or affiliations with any of the companies that manufacture products mentioned in this article or their competitors.
The decision by the US Food and Drug Administration (FDA) to put warning labels on all estrogen and estrogen-progestin products prescribed for postmenopausal women is startling—especially when you consider that barely a year ago, estrogen was viewed as a remedy or preventive for all kinds of ills.
This reversal in the official status of estrogen has created shock waves among Ob/Gyns still struggling to answer patients’ questions and counsel them appropriately.
The FDA’s role has been anything but passive; early this year, it issued several recommendations on the use of estrogen and estrogenprogestin hormone replacement therapy (HRT) by postmenopausal women. The FDA:
- acknowledged that estrogen and estrogen-progestin formulations remain the most effective treatment for hot flashes and night sweats caused by menopause, but counseled doctors to prescribe the lowest possible dose for the shortest duration.
- advised against using HRT to prevent cardiovascular disease.
- urged clinicians to consider approved non-estrogen agents when prescribing HRT to prevent menopause-induced osteoporosis, reserving estrogen for cases in which the risk of osteoporosis is greater than the risks associated with the therapy. (See related article “New options in osteoporosis therapy: combination and sequential treatment”.)
- recommended that, until more data become available, all estrogens—with or without a progestin—be presumed to carry risks similar to those observed for conjugated equine estrogen (CEE) and medroxyprogesterone acetate (MPA) in the Women’s Health Initiative (WHI).
The best advice came from FDA Commissioner Mark McClellan, MD, PhD, who encouraged women to consult their physicians about the clinical implications of the WHI findings.
Although concrete data on the risks and benefits of estrogen have never been so substantial, considerable disagreement remains over how to proceed from here. To provide our readers with additional perspective and insight, OBG Management asked 2 international experts, Dr. Morris Notelovitz and Dr. Susan Love, to offer their views on the WHI findings and other aspects of postmenopausal estrogen use.
—Robert L. Barbieri, MD
Editor-in-Chief
Beware of widespread preventive therapies
The recent FDA decision to require warning labels on all estrogen and estrogen-progestin products prescribed for postmenopausal women is a vindication for all of us who have been worried about the widespread use of these drugs for prevention. (Note that this article is not about symptom relief; short-term use of hormone therapy for this indication is a different discussion.)
Although many women and doctors were shocked by the data from the long-overdue randomized, controlled trials on the use of HRT for prevention, there were many others who cheered—not because of the findings, but because at last we were doing the kind of studies that would tell us whether the commonly held hypothesis about these drugs was true.
Those who are holding on to the fact that the WHI’s estrogen-alone study has not yet been halted as evidence that progestin is the culprit should note that an increase in heart attacks and strokes has been seen in this cohort as well. The breast cancer risk may be less without the progestin, but many studies suggest that it certainly is not zero. Plus, the smaller size of the study means it would take longer to reach the same stopping goals. The risk-benefit ratio is likely to be similar to that for estrogen-progestin for most endpoints.
An abundance of observational data
Prior to the Heart and Estrogen-progestin Replacement Study (HERS) and WHI trials, only 1 long-term randomized, controlled trial had explored postmenopausal HRT, and it was too small to yield definitive data.1-3 The rest of the many studies looking at the benefits and risks of hormone therapy for prevention were based on observation. Indeed, the overwhelming majority of them demonstrated that HRT decreased heart disease.4,5 But these studies were still observational. Observational studies cannot prove cause and effect.
As we now know all too well, women who took postmenopausal HRT were, in general, of a higher socioeconomic level, better educated, and healthier than the women who did not.6 It was not a matter of hormones making women healthy, but rather, healthy women taking hormones.
Women who can generate as little as 5 pg/mL of their own estrogen have almost no fractures; these data suggest that we probably do not have to “replace” hormones in most women.
—Dr. Love
In itself this is not surprising. Confounding is common in observational studies and is one of the reasons this research is better at driving hypotheses than proving cause and effect. Somehow, however, the number and consistency of these studies clouded our collective judgment and caused us to get ahead of the data. It is not the first time we have let this happen, and I am sure it will not be the last.
In breast cancer, for example, the use of high-dose chemotherapy with stem-cell rescue became the standard of care before there were any randomized data demonstrating its value. When the randomized studies did finally come in, many clinicians were surprised to find that this aggressive regimen was no better than standard therapy and had worse side effects.7 Now, the use of this therapy has virtually ceased.
It would behoove us to follow this lead in the use of hormones for prevention. In a recent analysis at the National Cancer Institute meeting on HRT, Deborah Grady could find no subgroup, including women with an osteoporotic fracture, where the benefits outweighed the risk.8
Exercise prescriptions should replace hormones, and weight should be monitored rather than bone density in a woman in her 50s.
—Dr. Love
Risks of rushing to substitute
What should we do? Many clinicians may wish to quickly find something else to give women—be it selective estrogen receptor modulators, bisphosphonates, or bio-identical hormones. In my view, that misses the point. This new data on postmenopausal hormone therapy should cause us to question the hypothesis upon which its use was based.
Perhaps we do not have to treat postmenopausal women with anything. Rather than equate menopause with ovarian failure or estrogen deficiency, perhaps we can regard it as the natural progression of a woman’s life. New studies indicate that postmenopausal women who are able to generate as little as 5 pg or more of their own estrogen per milliliter of serum have almost no fractures; these data suggest that we probably do not have to “replace” hormones in the majority of women.9
In addition, the data suggest that age is a more potent predictor of fracture risk than bone density.10 Many experts are suggesting that osteopenia should not be treated and that bone density should not be measured until age 65.
Deaths from heart disease are at all-time lows due mostly to improved treatment techniques rather than prevention.11
Lifestyle changes are still the best prevention
I would suggest that the warning label on the estrogen and estrogen-progestin formulations be viewed as a caution against the whole concept of widespread use of drugs in healthy women for prevention. Lifestyle changes remain the best way to maintain quality of life and prevent the diseases of aging. Weight control, exercise, diet, and not smoking are still the safest approaches to a healthy life.
Rather than continue this debate, we should put our energies into devising strategies to help women achieve healthy lifestyle goals. Exercise prescriptions should be the replacement for hormones, and weight should be monitored rather than bone density in a woman in her 50s. Advice about smoking cessation needs to take the place of discussions of breast self-exam.
My hope is that this warning will serve as a wake-up call for all who care for women.
Dr. Love reports no financial arrangements or affiliations with any of the companies that manufacture products mentioned in this article or their competitors.
REFERENCES
1. Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA. 1998;280:605-613.
2. Writing Group for the Women’s Health Initiative Randomized Controlled Trial Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
3. Nachtigall LE, Nachtigall R, Nachtigall RD, Beckman EM. Estrogen replacement therapy II: A prospective study in the relationship to carcinoma and cardiovascular and metabolic problems. Obstet Gynecol. 1979;54(1):74-79.
4. Stampfer MJ, Colditz GA. Estrogen replacement therapy and coronary heart disease: A quantitative assessment of the epidemiologic evidence. Prev Med. 1991;20:47-63.
5. Grodstein E, Stampfer MJ, Manson JE, et al. Postmenopausal estrogen and progestin use: The risk of cardiovascular disease. N Engl J Med. 1996;335:453-461.
6. Barrett-Connor E. Postmenopausal estrogen and prevention bias. Ann Intern Med. 1991;115:455-456.
7. Peters W, Rosner G, Vredenburgh J, et al. A prospective, randomized comparison of two doses of combination alkylating agents as consolidation after CAF in high-risk primary breast cancer involving ten or more axillary lymph nodes: Preliminary results of CALBG9082/SWOG9114/NCIC MA-13. Proc Am Soc Clin Oncol. 1999;18:1a.-Abstract.
8. Grady D. Postmenopausal hormone therapy: balancing the risks and benefits. Presented at: National Institutes of Health Scientific Workshop on Menopausal Hormone Therapy; October 23, 2002; Bethesda, Md.
9. Cummings SR, Browner WS, Bauer D, et al. Study of Osteoporotic Fractures Research Group. Endogenous hormones and the risk of hip and vertebral fractures among older women. N Engl J Med. 1998;339:733-738.
10. Kanis JA, Johnell O, et al. Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone. 2000;27:585-590.
11. Kolata G. Gains on heart disease leave more survivors, and questions. New York Times. January 19, 2003;sect 1:1.-
Estrogen is a valid option when prescribed correctly
Women are living longer, but not necessarily better. Increases in longevity are partially offset by a greater prevalence of chronic conditions such as osteoporosis, cardiovascular disease, cognitive dysfunction, and breast cancer—all of which impact a woman’s quality of life. HRT is a logical outgrowth of this increased longevity.
Unfortunately, while it represents an attempt to improve the health and well-being of postmenopausal women, HRT is based upon a faulty premise: that all women are biologically equal and react similarly to the menopausal transition. Equally erroneous are 2 corollaries: that all menopausal women will respond to the same dose of HRT and that all estrogen formulations are comparable.
As has become clear, this generic approach to menopause is inappropriate. The convenient but simplistic strategy of treating all women at and beyond menopause with a standard dose of the same estrogen-progestin formulation is ill-founded. Estrogen offers the postmenopausal patient numerous benefits and needs to remain an important part of the Ob/Gyn’s options. However, it can no longer be prescribed in the “traditional” manner.
The trouble with tradition
Here are 2 problems with the conventional approach:
- Every woman synthesizes estrogen differently, depending on the endocrinology of her nonreproductive organs in the premenopausal, perimenopausal, and postmenopausal periods; the pathogenesis of conditions such as cardiovascular disease and their relationship to estrogen and androgen synthesis and metabolism; and the pharmacokinetic and pharmacodynamic variance between HRT formulations.1,2
- Women are encouraged to have annual examinations, yet a review of the type and dose of HRT rarely takes place at these exams.
New strategy: Replenish hormones to age 65, maintain thereafter
Women need “individualized and adjusted hormone therapy.” This is relevant for patients 35 to 65 years of age and is based on our ability to tailor the type and route of hormone therapy to approximate the hormonal milieu of women at a given age. The term “HRT”—which I define as the attempt to replicate a premenopausal woman’s hormonal milieu—should be restricted to women who are between the ages of 35 and 45 who need hormone therapy. After that, hormone replenishment should be practiced until age 65. Based on the pharmacokinetics of estrogen, HRT is best achieved by non-oral estradiol; hormone replenishment relies on the bioconversion of estradiol to estrone after oral estrogen and the “normal” postmenopausal estrone:estradiol ratio. Hormone maintenance refers to women who have been stabilized on a prior hormonal regimen. They should be left on their current medication as long as there is still an indication for hormone therapy.
The type, dose, and route of this therapy should be regularly reviewed and adjusted, if necessary, as a woman’s needs change over time.
Estrogen synthesis and metabolism. Only 2 bioavailable estrogens are synthesized in postmenopausal women: estradiol and estrone. Both are derived from the aromatization of androgens in adipose tissue and muscle and are further metabolized by the liver. The aromatization of androgens to estrogens occurs in tissues such as breast, bone, and coronary artery, and the local concentration far exceeds that measured in the peripheral circulation. The estrogen synthesized locally and the metabolites produced by the liver can have protective effects (increased bone density) or potentially harmful effects (breast cancer), even though serum estradiol may be within a “normal” range (i.e., less than 20 pg per deciliter).
The synthesis and metabolism of estrogen are genetically controlled. For example, the genes determine whether a woman has a high risk of breast cancer. Therefore, clinicians should select the dose and route of estrogen administration that would optimize the benefit and limit the risk of hormone therapy. This will be different in each woman. (Although most postmenopausal women can safely take hormones, some may have an endogenous abnormality that precludes the therapy.)
Fraction of dose may relieve symptoms. The estrogen threshold for the relief of hot flashes—HRT’s main indication—also varies among women. One half to one quarter of the “standard” dose (0.625 mg per day of CEE)—the amount prescribed in the WHI3—has been shown to be effective.
The long trajectory of ‘menopausal’ diseases
The pathogenesis of osteoporosis and cardiovascular disease—conditions for which longterm HRT has been advocated—commences with the first menstrual period (FIGURE). Thus, primary prevention should begin in early adulthood. This includes diet and lifestyle modifications and exercise. Normal ovarian function is essential, as anovulatory hypoestrogenic disorders predispose young women to a greater risk of these conditions later in life.
Endogenous estrogen’s protective effect is based on the presence of estrogen—and androgen—receptors in bone (e.g., osteoblasts, osteoclasts) and in the coronary artery (e.g., endothelium, smooth muscle) and liver. As estrogen levels decline, bone remodeling accelerates and bone mineral is lost; the process of atherothrombosis also accelerates. Given the multifactorial nature of these conditions, estrogen therapy plays an important role in stabilizing bone loss and halting the progression of atheromatosis, both at menopause and at other times when a lack of estrogen is a relevant causative factor. When bone loss is due to hyperthyroidism or when cardiovascular disease is associated with dyslipidemia, hypertension or diabetes, disease-specific treatment is needed.
Individualizing HRT to condition and severity
As for HRT, the dosage and type need to be judged according to each clinical situation and degree of abnormality. For example, a lower dose of estrogen is required when a woman has osteopenia than when she has osteoporosis. Transdermal estrogen is the best option for a woman with elevated serum triglycerides or C-reactive protein (a cardiac inflammatory biomarker). Women with low levels of high-density–lipoprotein cholesterol will benefit from oral estrogen.
Measurement is central to this approach. Without a mammogram, breast density (a sign of local estrogen biosynthesis) cannot be documented or quantified. A bone-density test (with bone markers) is needed to assess bone health; a fasting lipid profile (including glucose) and possibly a C-reactive protein assay are the only means of assessing the patient’s cardiovascular disease risk status.
Prescribe lowest dose and monitor. Clinicians should prescribe the lowest estrogen dose and then monitor therapy. This entails measuring baseline serum estradiol and conducting meaningful posttreatment monitoring, best achieved with 17ß-estradiol-based products (oral or transdermal). A total serum estradiol value of 40 to 80 pg per milliliter has been found effective in controlling bone loss, coronary artery vasoreactivity, and cognition. The late initiation of hormone therapy is not recommended, since estrogen may disrupt the fibrin capsule of arterial intimal plaques and precipitate thrombosis with vascular luminal occlusion and myocardial infarction or stroke.
Not all hormones are the same
Not all estrogens or progestins are equal in their formulation, pharmacologic properties, or function. As noted previously, nonpregnant women synthesize only 2 bioavailable estrogens: estradiol and estrone. Pharmacologic preparations of 17ß-estradiol have properties similar to those of endogenous estrogen. Depending on the dose and route of administration, they can, to a certain degree, replicate a premenopausal or postmenopausal estrogen milieu. CEE, the preparation used in the WHI, contains 10 estrogens and 200 metabolites, with varying degrees of estrogenic and antiestrogenic activity. Thus, it is not possible to monitor posttreatment estradiol values.
It is significant that only the estrogenprogestin arm of the WHI was suspended. This suggests that MPA, the progestin in the combination therapy used in the trial, may be responsible for the unwanted results. There are a number of pharmacologic differences between MPA, natural progesterone, and the 19-nor-testosterone–derived progestins (e.g., norethindrone acetate [NETA]). In addition, the half-life of MPA (24 hours) greatly exceeds that of progesterone (12 hours) and NETA (6 to 8 hours), thus potentially downregulating estrogen receptors in vital blood vessels that may already be compromised.
Putting the WHI in perspective
The WHI was planned as a primary cardiovascular-disease–prevention trial. Of the women enrolled in the study, 45.3% were 60 to 69 years of age, and 21.3% were 70 to 79. Thus, given the pathogenesis of cardiovascular disease, most subjects had some degree of coronary artery disease at the start of the study. Yet only 37 hormone-group subjects versus 30 placebo-group subjects per 10,000 women annually experienced an adverse clinical cardiovascular event. Except for year 5, the ratio of such adverse events in the hormone group decreased over time, compared with women in the placebo group. The HRT:placebo ratios of these events for years 1 through 6 were 1.78, 1.15, 1.06, 0.99, 2.38, and 0.78, respectively. (The unexpected jump in the event ratio in year 5 was due to an unexplained paucity of events in the placebo group and not an increase in the group of subjects treated with hormone therapy.)
The WHI definition of “healthy postmenopausal woman” ignored the heterogeneity of the climacteric by assuming that all women were biologically equal and that age had not added its toll in organ damage. In a parallel observational arm of the WHI, C-reactive protein independently predicted vascular events among healthy postmenopausal women, but this was related to baseline levels of the inflammatory biomarkers and not to the hormone-therapy–related increase in C-reactive protein. The same is true for the stated increased risk of HRT-related breast cancer: 35 versus 30 events annually per 10,000 women on HRT and placebo, respectively. What differentiated the 35 who developed breast cancer from the 9,965 who did not?
Clinical challenge: Not to withhold HRT, but to identify women at risk
As clinicians, we must strive not to deny HRT to women who could safely benefit from it, but to develop cost-effective strategies to differentiate healthy women from those with metabolic dysfunction (e.g., premammographic breast cancer) and asymptomatic latent disease (e.g., silent atherogenesis). “Normal” women will benefit from selective HRT; the latter require medications specific to their underlying disorder.
In the aftermath of the WHI, the scope of the HRT problem has been overblown. When the absolute-risk numbers for HRT-related cardiovascular disease and breast cancer are extrapolated to the nation, the perceived size of the problem—which is only a mathematical projection and estimate—can assume troubling proportions. But physicians in clinical practice have only 1 responsibility: ensuring the health and well-being of their patients, 1 at a time. Thus, the question of HRT must be resolved between the physician and the patient. This takes time—time to talk with, examine, and test the patient; time to think through the problem; and time to prescribe and educate the patient regarding her therapeutic needs. This is time well spent.
FIGURE Female life span: Window of opportunity for hormone therapy*
Dr. Notelovitz reports no financial arrangements or affiliations with any of the companies that manufacture products mentioned in this article or their competitors.
1. Utian WH, Shoup D, Bachmann G, et al. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril. 2001;75:1065-1079.
2. Notelovitz M, Lenihan JP, McDermott M, et al. Initial 17ß-estradiol dose for treating vasomotor symptoms. Obstet Gynecol. 2000;95:726-731.
3. Writing Group for the Women’s Health Initiative Randomized Controlled Trial. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
1. Utian WH, Shoup D, Bachmann G, et al. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril. 2001;75:1065-1079.
2. Notelovitz M, Lenihan JP, McDermott M, et al. Initial 17ß-estradiol dose for treating vasomotor symptoms. Obstet Gynecol. 2000;95:726-731.
3. Writing Group for the Women’s Health Initiative Randomized Controlled Trial. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.