User login
Six PAD diagnostic tests vary widely in patients with diabetes
Six different clinical tests used to identify peripheral arterial disease (PAD) were found to be significantly different in their ability to detect PAD in a population of 50 patients with diabetes, according to a report published online in Primary Care Diabetes.
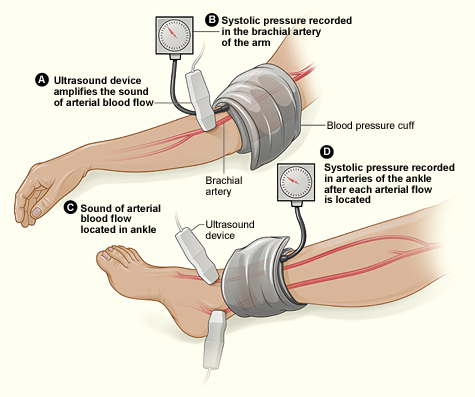
This study assessed the same group of participants with each of the following six tests: Doppler Waveform, toe-brachial pressure index (TBPI), ankle-brachial pressure index (ABPI), posterior tibial artery pulse (ATP), transcutaneous oxygen pressure (TCPO), and pulse palpation. The right and left foot were assessed in each participant, yeilding100 limbs for analysis, according to Yvonne Midolo Azzopardi, MD, of the University of Malta in Msida and her colleagues.
The highest percent of participants who were found to have PAD was 93%, as detected by Doppler Waveform, followed by TBPI (72%), ABPI (57%), ATP (35%), TCPO (30%), and pulse palpation (23%). The difference between these percentages was significant at P less than .0005.
“The reported observations suggest that use of only one screening tool in isolation could yield high false results since it is clear that these tests do not concur with each other to a large extent,” the authors stated.
Dr. Azzopardi and her colleagues pointed out that the use of more specialized tools, such as duplex scanning, could be compared with these six modalities to detect PAD but that such methods were unlikely to be routinely available to primary care physicians who are at the front lines of making the determination of PAD in patients with diabetes.
“The authors advocate for urgent, more robust studies utilizing a gold standard modality for the diagnosis of PAD in order to provide evidence regarding which noninvasive screening modalities would yield the most valid results. This would significantly reduce the proportion of patients with diabetes who would be falsely identified as having no PAD and subsequently denied beneficial and effective secondary risk factor control,” Dr. Azzopardi and her colleagues concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Azzopardi YM et al. 2018. Prim Care Diabetes.. doi: 10.1016/j.pcd.2018.08.005.
Six different clinical tests used to identify peripheral arterial disease (PAD) were found to be significantly different in their ability to detect PAD in a population of 50 patients with diabetes, according to a report published online in Primary Care Diabetes.
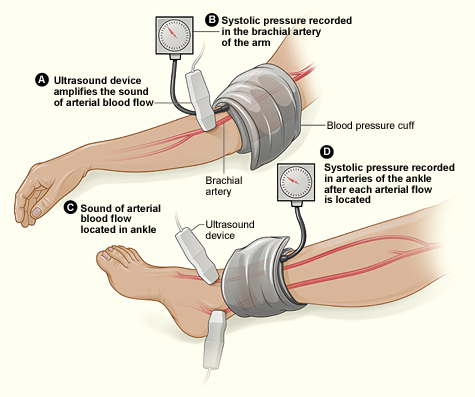
This study assessed the same group of participants with each of the following six tests: Doppler Waveform, toe-brachial pressure index (TBPI), ankle-brachial pressure index (ABPI), posterior tibial artery pulse (ATP), transcutaneous oxygen pressure (TCPO), and pulse palpation. The right and left foot were assessed in each participant, yeilding100 limbs for analysis, according to Yvonne Midolo Azzopardi, MD, of the University of Malta in Msida and her colleagues.
The highest percent of participants who were found to have PAD was 93%, as detected by Doppler Waveform, followed by TBPI (72%), ABPI (57%), ATP (35%), TCPO (30%), and pulse palpation (23%). The difference between these percentages was significant at P less than .0005.
“The reported observations suggest that use of only one screening tool in isolation could yield high false results since it is clear that these tests do not concur with each other to a large extent,” the authors stated.
Dr. Azzopardi and her colleagues pointed out that the use of more specialized tools, such as duplex scanning, could be compared with these six modalities to detect PAD but that such methods were unlikely to be routinely available to primary care physicians who are at the front lines of making the determination of PAD in patients with diabetes.
“The authors advocate for urgent, more robust studies utilizing a gold standard modality for the diagnosis of PAD in order to provide evidence regarding which noninvasive screening modalities would yield the most valid results. This would significantly reduce the proportion of patients with diabetes who would be falsely identified as having no PAD and subsequently denied beneficial and effective secondary risk factor control,” Dr. Azzopardi and her colleagues concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Azzopardi YM et al. 2018. Prim Care Diabetes.. doi: 10.1016/j.pcd.2018.08.005.
Six different clinical tests used to identify peripheral arterial disease (PAD) were found to be significantly different in their ability to detect PAD in a population of 50 patients with diabetes, according to a report published online in Primary Care Diabetes.
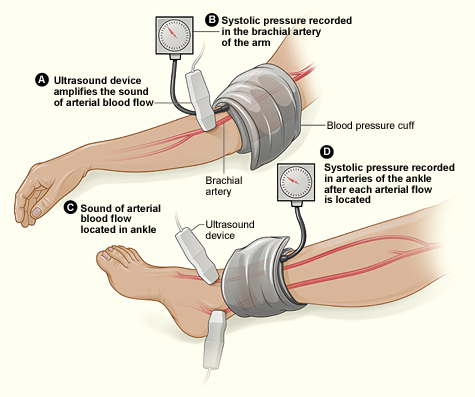
This study assessed the same group of participants with each of the following six tests: Doppler Waveform, toe-brachial pressure index (TBPI), ankle-brachial pressure index (ABPI), posterior tibial artery pulse (ATP), transcutaneous oxygen pressure (TCPO), and pulse palpation. The right and left foot were assessed in each participant, yeilding100 limbs for analysis, according to Yvonne Midolo Azzopardi, MD, of the University of Malta in Msida and her colleagues.
The highest percent of participants who were found to have PAD was 93%, as detected by Doppler Waveform, followed by TBPI (72%), ABPI (57%), ATP (35%), TCPO (30%), and pulse palpation (23%). The difference between these percentages was significant at P less than .0005.
“The reported observations suggest that use of only one screening tool in isolation could yield high false results since it is clear that these tests do not concur with each other to a large extent,” the authors stated.
Dr. Azzopardi and her colleagues pointed out that the use of more specialized tools, such as duplex scanning, could be compared with these six modalities to detect PAD but that such methods were unlikely to be routinely available to primary care physicians who are at the front lines of making the determination of PAD in patients with diabetes.
“The authors advocate for urgent, more robust studies utilizing a gold standard modality for the diagnosis of PAD in order to provide evidence regarding which noninvasive screening modalities would yield the most valid results. This would significantly reduce the proportion of patients with diabetes who would be falsely identified as having no PAD and subsequently denied beneficial and effective secondary risk factor control,” Dr. Azzopardi and her colleagues concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Azzopardi YM et al. 2018. Prim Care Diabetes.. doi: 10.1016/j.pcd.2018.08.005.
FROM PRIMARY CARE DIABETES
Key clinical point: Six different tests used to identify PAD differed significantly in their ability to detect the disease.
Major finding: Detection ranged from 93% to 23% in the same group of patients.
Study details: Both legs of 50 patients with diabetes were assessed for PAD using six screening modalities.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Azzopardi YM et al. 2018. Prim Care Diabetes. doi: 10.1016/j.pcd.2018.08.005.
Obesity tied to improved inpatient survival of patients with PAD
The obesity paradox appears alive and well in the treatment of peripheral arterial disease (PAD), according to the results of a 10-year, 5.6-million patient database study.
The researchers found that coding for obesity is associated with lower in-hospital mortality in PAD patients relative to those who were normal weight or overweight. This obesity survival paradox was independent of age, sex, and comorbidities and was seen in all obesity classes, according to Karsten Keller, MD, of the University Medical Center Mainz (Germany), and his colleagues.
In total, 5,611,827 inpatients aged 18 years or older with PAD were treated between 2005 and 2015 in Germany, 5,611,484 of whom (64.8% men) were eligible for analysis. Among these, 500,027 (8.9%) were coded with obesity and 16,620 (0.3%) were coded as underweight; 5,094,837 (90.8%) were in neither classification (considered healthy/overweight) and served as the reference group for comparison, according to Dr. Keller and his colleagues.
Obese PAD patients were younger, more frequently women, and had less cancer but were diagnosed more often with cardiovascular disease risk factors such as diabetes and hypertension, compared with the reference group. In addition, there were higher levels of coronary artery disease, heart failure, renal insufficiency, and chronic obstructive pulmonary disease (COPD) in obese patients.
Obese patients had lower mortality (3.2% vs. 5.1%; P less than .001), compared with the reference group, and showed a reduced risk of in-hospital mortality (odds ratio, 0.617; P less than .001). Univariate logistic regression analyses showed the association of obesity and reduced in-hospital mortality was consistent and significant, even with adjustment for age, sex, and comorbidities.
In contrast, underweight patients were significantly more likely to die than those in the reference group (6% vs. 5.1%; P less than .001), according to the researchers. Underweight was associated with an increased risk for in-hospital mortality (OR, 1.18; P less than .001), and this was consistent throughout univariate analysis.
Underweight PAD patients also had significantly higher frequencies of cancer and COPD, but lower rates of diabetes mellitus, hypertension, coronary artery disease, and heart failure, compared with the reference group. Both obese and underweight PAD patients stayed longer in the hospital than the PAD patients who were not coded as underweight or obese.
Obese PAD patients had slight but significantly higher rates of MI (3.9% vs. 3.4%; P less than .001) and venous thromboembolic events, and more often had to undergo amputation surgery (8.3% vs. 8.1%; P less than .001), including a higher relative number of minor amputations (6.3% vs. 5.5%; P less than .001). However, major amputation rates were significantly lower in obese patients (2.6% vs. 3.2%; P less than .001), with univariate analysis showing a significant association between obesity and a lower risk of major amputation (OR, 0.82; P less than .001), which remained stable after multivariate adjustment.
Limitations of the study reported by the researchers included a lower than expected percent obesity in the 10-year database, compared with current rates, and the inability to follow tobacco use or to determine the socioeconomic status of the patients.
“Obesity is associated with lower in-hospital mortality in PAD patients relative to those with normal weight/overweight. ... Therefore, greater concern should be directed to the thinner patients with PAD who are particularly at increased risk of mortality,” the researchers concluded.
This study was supported by the German Federal Ministry of Education and Research; the authors reported that they had no disclosures.
SOURCE: Keller K et al. Clin Nutr. 2018 Oct 3. doi: 10.1016/j.clnu.2018.09.031.
The obesity paradox appears alive and well in the treatment of peripheral arterial disease (PAD), according to the results of a 10-year, 5.6-million patient database study.
The researchers found that coding for obesity is associated with lower in-hospital mortality in PAD patients relative to those who were normal weight or overweight. This obesity survival paradox was independent of age, sex, and comorbidities and was seen in all obesity classes, according to Karsten Keller, MD, of the University Medical Center Mainz (Germany), and his colleagues.
In total, 5,611,827 inpatients aged 18 years or older with PAD were treated between 2005 and 2015 in Germany, 5,611,484 of whom (64.8% men) were eligible for analysis. Among these, 500,027 (8.9%) were coded with obesity and 16,620 (0.3%) were coded as underweight; 5,094,837 (90.8%) were in neither classification (considered healthy/overweight) and served as the reference group for comparison, according to Dr. Keller and his colleagues.
Obese PAD patients were younger, more frequently women, and had less cancer but were diagnosed more often with cardiovascular disease risk factors such as diabetes and hypertension, compared with the reference group. In addition, there were higher levels of coronary artery disease, heart failure, renal insufficiency, and chronic obstructive pulmonary disease (COPD) in obese patients.
Obese patients had lower mortality (3.2% vs. 5.1%; P less than .001), compared with the reference group, and showed a reduced risk of in-hospital mortality (odds ratio, 0.617; P less than .001). Univariate logistic regression analyses showed the association of obesity and reduced in-hospital mortality was consistent and significant, even with adjustment for age, sex, and comorbidities.
In contrast, underweight patients were significantly more likely to die than those in the reference group (6% vs. 5.1%; P less than .001), according to the researchers. Underweight was associated with an increased risk for in-hospital mortality (OR, 1.18; P less than .001), and this was consistent throughout univariate analysis.
Underweight PAD patients also had significantly higher frequencies of cancer and COPD, but lower rates of diabetes mellitus, hypertension, coronary artery disease, and heart failure, compared with the reference group. Both obese and underweight PAD patients stayed longer in the hospital than the PAD patients who were not coded as underweight or obese.
Obese PAD patients had slight but significantly higher rates of MI (3.9% vs. 3.4%; P less than .001) and venous thromboembolic events, and more often had to undergo amputation surgery (8.3% vs. 8.1%; P less than .001), including a higher relative number of minor amputations (6.3% vs. 5.5%; P less than .001). However, major amputation rates were significantly lower in obese patients (2.6% vs. 3.2%; P less than .001), with univariate analysis showing a significant association between obesity and a lower risk of major amputation (OR, 0.82; P less than .001), which remained stable after multivariate adjustment.
Limitations of the study reported by the researchers included a lower than expected percent obesity in the 10-year database, compared with current rates, and the inability to follow tobacco use or to determine the socioeconomic status of the patients.
“Obesity is associated with lower in-hospital mortality in PAD patients relative to those with normal weight/overweight. ... Therefore, greater concern should be directed to the thinner patients with PAD who are particularly at increased risk of mortality,” the researchers concluded.
This study was supported by the German Federal Ministry of Education and Research; the authors reported that they had no disclosures.
SOURCE: Keller K et al. Clin Nutr. 2018 Oct 3. doi: 10.1016/j.clnu.2018.09.031.
The obesity paradox appears alive and well in the treatment of peripheral arterial disease (PAD), according to the results of a 10-year, 5.6-million patient database study.
The researchers found that coding for obesity is associated with lower in-hospital mortality in PAD patients relative to those who were normal weight or overweight. This obesity survival paradox was independent of age, sex, and comorbidities and was seen in all obesity classes, according to Karsten Keller, MD, of the University Medical Center Mainz (Germany), and his colleagues.
In total, 5,611,827 inpatients aged 18 years or older with PAD were treated between 2005 and 2015 in Germany, 5,611,484 of whom (64.8% men) were eligible for analysis. Among these, 500,027 (8.9%) were coded with obesity and 16,620 (0.3%) were coded as underweight; 5,094,837 (90.8%) were in neither classification (considered healthy/overweight) and served as the reference group for comparison, according to Dr. Keller and his colleagues.
Obese PAD patients were younger, more frequently women, and had less cancer but were diagnosed more often with cardiovascular disease risk factors such as diabetes and hypertension, compared with the reference group. In addition, there were higher levels of coronary artery disease, heart failure, renal insufficiency, and chronic obstructive pulmonary disease (COPD) in obese patients.
Obese patients had lower mortality (3.2% vs. 5.1%; P less than .001), compared with the reference group, and showed a reduced risk of in-hospital mortality (odds ratio, 0.617; P less than .001). Univariate logistic regression analyses showed the association of obesity and reduced in-hospital mortality was consistent and significant, even with adjustment for age, sex, and comorbidities.
In contrast, underweight patients were significantly more likely to die than those in the reference group (6% vs. 5.1%; P less than .001), according to the researchers. Underweight was associated with an increased risk for in-hospital mortality (OR, 1.18; P less than .001), and this was consistent throughout univariate analysis.
Underweight PAD patients also had significantly higher frequencies of cancer and COPD, but lower rates of diabetes mellitus, hypertension, coronary artery disease, and heart failure, compared with the reference group. Both obese and underweight PAD patients stayed longer in the hospital than the PAD patients who were not coded as underweight or obese.
Obese PAD patients had slight but significantly higher rates of MI (3.9% vs. 3.4%; P less than .001) and venous thromboembolic events, and more often had to undergo amputation surgery (8.3% vs. 8.1%; P less than .001), including a higher relative number of minor amputations (6.3% vs. 5.5%; P less than .001). However, major amputation rates were significantly lower in obese patients (2.6% vs. 3.2%; P less than .001), with univariate analysis showing a significant association between obesity and a lower risk of major amputation (OR, 0.82; P less than .001), which remained stable after multivariate adjustment.
Limitations of the study reported by the researchers included a lower than expected percent obesity in the 10-year database, compared with current rates, and the inability to follow tobacco use or to determine the socioeconomic status of the patients.
“Obesity is associated with lower in-hospital mortality in PAD patients relative to those with normal weight/overweight. ... Therefore, greater concern should be directed to the thinner patients with PAD who are particularly at increased risk of mortality,” the researchers concluded.
This study was supported by the German Federal Ministry of Education and Research; the authors reported that they had no disclosures.
SOURCE: Keller K et al. Clin Nutr. 2018 Oct 3. doi: 10.1016/j.clnu.2018.09.031.
FROM CLINICAL NUTRITION
Key clinical point: Obesity is associated with lower in-hospital mortality in patients with peripheral arterial disease relative to those who were healthy weight or overweight.
Major finding: Obese patients had a lower mortality (3.2% vs. 5.1%; P less than .001), compared with the reference group.
Study details: A database study of 5,611,484 inpatients diagnosed with peripheral arterial disease.
Disclosures: This study was supported by the German Federal Ministry of Education and Research; the authors reported that they had no disclosures.
Source: Keller K et al. Clin Nutr. 2018 Oct 3. doi: 10.1016/j.clnu.2018.09.031.
Lower-limb atherosclerosis predicts long-term mortality in patients with PAD
The location and extent of lower limb atherosclerosis predicts long-term mortality in patients with peripheral arterial disease (PAD), according to the results of a retrospective cohort study performed in England.
Comprehensive infrainguinal arterial imaging that used duplex ultrasound to determine the overall and site-specific burden of atherosclerotic disease predicted long-term outcomes in this patient group, according to a report published online in the European Journal of Vascular and Endovascular Surgery.
“Not only does such imaging provide anatomical information to guide intervention, but it may also provide information to further risk-stratify patients with regard to long-term cardiovascular risk,” wrote Paul J.W. Tern, MD, of Addenbrooke’s Hospital, Cambridge, England, and his colleagues.
A retrospective cohort study was performed on a consecutive series of 678 patients undergoing a lower limb arterial duplex scan during October 2009–June 2011 at Addenbrooke’s Hospital. Patients had a median age of 74 years and were followed for a median of 70 months.
A total of 307 patients died, which was the primary end point. Independent predictors of all-cause mortality included total Bollinger score (odds ratio, 1.11; P less than .001), femoropopliteal Bollinger score (OR, 1.34; P = .05); and crural Bollinger score (OR, 1.03; P = .03). The Bollinger score has been found to be a validated tool when used to determine overall lower limb atherosclerotic burden, the authors stated.
Dr. Tern and his colleagues also found that mortality was significantly associated with age, a history of ischemic heart disease, a history of congestive cardiac failure, and chronic renal failure (chronic kidney disease), although statin and antiplatelet therapy were found to be protective.
“This study has shown that infrainguinal atherosclerotic site and burden are independent predictors of poor outcome in patients; it is straightforward to determine and as such could be used to further risk stratify patients and influence the intensity of cardiovascular risk modification,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Tern PJW et al. Eur J Vasc Endovasc Surg. 2018 Oct 1. doi: 10.1016/j.ejvs.2018.07.020.
The location and extent of lower limb atherosclerosis predicts long-term mortality in patients with peripheral arterial disease (PAD), according to the results of a retrospective cohort study performed in England.
Comprehensive infrainguinal arterial imaging that used duplex ultrasound to determine the overall and site-specific burden of atherosclerotic disease predicted long-term outcomes in this patient group, according to a report published online in the European Journal of Vascular and Endovascular Surgery.
“Not only does such imaging provide anatomical information to guide intervention, but it may also provide information to further risk-stratify patients with regard to long-term cardiovascular risk,” wrote Paul J.W. Tern, MD, of Addenbrooke’s Hospital, Cambridge, England, and his colleagues.
A retrospective cohort study was performed on a consecutive series of 678 patients undergoing a lower limb arterial duplex scan during October 2009–June 2011 at Addenbrooke’s Hospital. Patients had a median age of 74 years and were followed for a median of 70 months.
A total of 307 patients died, which was the primary end point. Independent predictors of all-cause mortality included total Bollinger score (odds ratio, 1.11; P less than .001), femoropopliteal Bollinger score (OR, 1.34; P = .05); and crural Bollinger score (OR, 1.03; P = .03). The Bollinger score has been found to be a validated tool when used to determine overall lower limb atherosclerotic burden, the authors stated.
Dr. Tern and his colleagues also found that mortality was significantly associated with age, a history of ischemic heart disease, a history of congestive cardiac failure, and chronic renal failure (chronic kidney disease), although statin and antiplatelet therapy were found to be protective.
“This study has shown that infrainguinal atherosclerotic site and burden are independent predictors of poor outcome in patients; it is straightforward to determine and as such could be used to further risk stratify patients and influence the intensity of cardiovascular risk modification,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Tern PJW et al. Eur J Vasc Endovasc Surg. 2018 Oct 1. doi: 10.1016/j.ejvs.2018.07.020.
The location and extent of lower limb atherosclerosis predicts long-term mortality in patients with peripheral arterial disease (PAD), according to the results of a retrospective cohort study performed in England.
Comprehensive infrainguinal arterial imaging that used duplex ultrasound to determine the overall and site-specific burden of atherosclerotic disease predicted long-term outcomes in this patient group, according to a report published online in the European Journal of Vascular and Endovascular Surgery.
“Not only does such imaging provide anatomical information to guide intervention, but it may also provide information to further risk-stratify patients with regard to long-term cardiovascular risk,” wrote Paul J.W. Tern, MD, of Addenbrooke’s Hospital, Cambridge, England, and his colleagues.
A retrospective cohort study was performed on a consecutive series of 678 patients undergoing a lower limb arterial duplex scan during October 2009–June 2011 at Addenbrooke’s Hospital. Patients had a median age of 74 years and were followed for a median of 70 months.
A total of 307 patients died, which was the primary end point. Independent predictors of all-cause mortality included total Bollinger score (odds ratio, 1.11; P less than .001), femoropopliteal Bollinger score (OR, 1.34; P = .05); and crural Bollinger score (OR, 1.03; P = .03). The Bollinger score has been found to be a validated tool when used to determine overall lower limb atherosclerotic burden, the authors stated.
Dr. Tern and his colleagues also found that mortality was significantly associated with age, a history of ischemic heart disease, a history of congestive cardiac failure, and chronic renal failure (chronic kidney disease), although statin and antiplatelet therapy were found to be protective.
“This study has shown that infrainguinal atherosclerotic site and burden are independent predictors of poor outcome in patients; it is straightforward to determine and as such could be used to further risk stratify patients and influence the intensity of cardiovascular risk modification,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Tern PJW et al. Eur J Vasc Endovasc Surg. 2018 Oct 1. doi: 10.1016/j.ejvs.2018.07.020.
FROM THE EUROPEAN JOURNAL OF VASCULAR AND ENDOVASCULAR SURGERY
Key clinical point: Duplex utrasound imaging can predict long-term PAD mortality.
Major finding: Mortality risk was predicted by total (odds ratio, 1.11), femoropopliteal (OR, 1.34), and crural (OR, 1.03) Bollinger scores.
Study details: A retrospective cohort study of 678 patients.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Tern PJW et al. Eur J Vasc Endovasc Surg. 2018 Oct 1. doi: 10.1016/j.ejvs.2018.07.020.
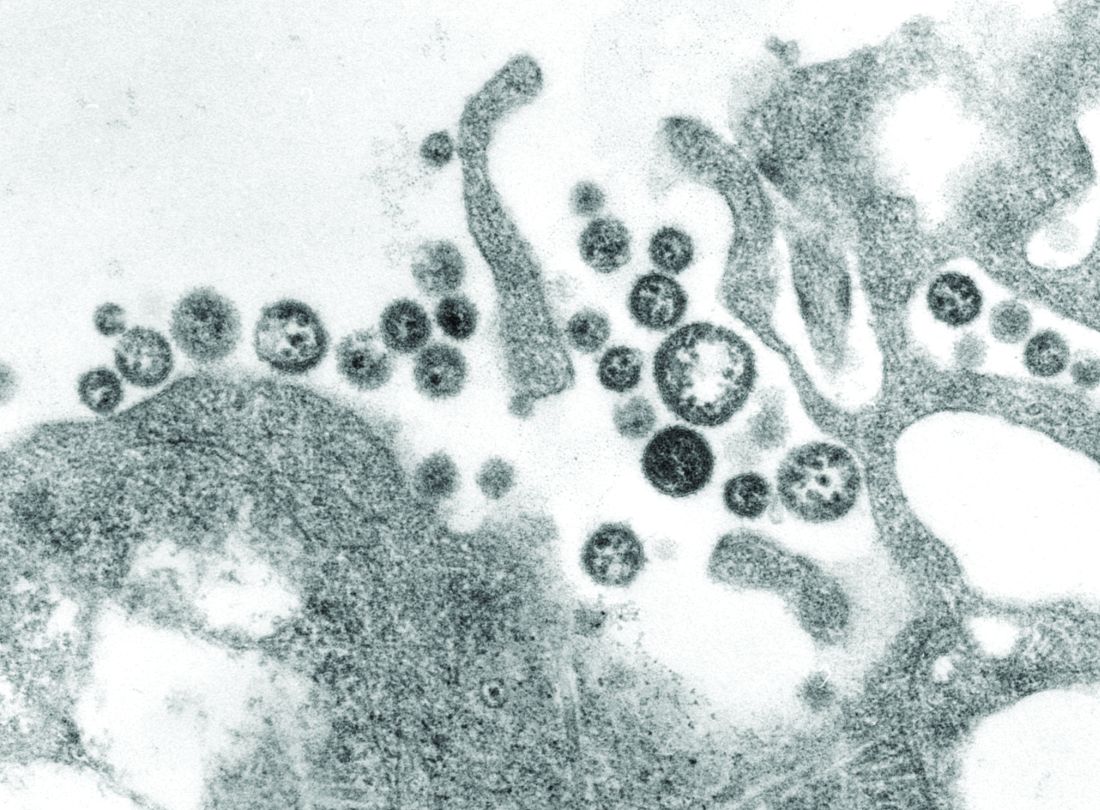
Novel recombinant vaccine protects animals from Lassa fever
An inactivated recombinant Lassa virus (LASV) and rabies vaccine candidate was developed that protects both mice and guinea pigs from Lassa fever. The vaccine also elicits a lasting humoral response against both LASV and rabies virus in both animal models. The novel vaccine, which uses a rabies virus–derived vector, expresses a codon-optimized LASV glycoprotein, according to Tiago Abreu Mota, a doctoral student at Jefferson University, Philadelphia, and his colleagues.
Lassa fever, a World Health Organization priority disease with a biosafety level of 4, is a hemorrhagic fever caused by the Lassa virus, which has no approved vaccine or potent antiviral treatment, according to the report published online in Nature Communications. So the development of a vaccine would be an important step in protecting the West African population from this deadly disease, which infects an estimated 100,000-300,000 people annually. As many as 80% of Lassa fever exposures are mildly symptomatic and thus go unreported; however, the case fatality rate of full-blown Lassa fever has been reported to reach as high as 50%, according to Mr. Mota and his colleagues.
An advantage to the new vaccine is that it is inactivated and thus could potentially be used in pregnant women and immunosuppressed patients, both of which are major risk groups for Lassa fever, according to the researchers. The vaccine could also protect against rabies, which is another major health concern in the regions affected by the Lassa virus.
In terms of mechanism of action, the vaccine did not induce virus-neutralizing antibodies, but rather appeared to trigger cell-mediated protection through activating natural killer cells to promote significantly more killing of virus-infected cells than nontriggered NK cells (P less than .01), as seen through in vitro testing.
The ability to assay for this form of vaccine effectiveness was a key development, according to the researchers. “The neutralizing antibody has been something of a gold standard in vaccine development. High levels are usually a good indication that the immune reaction is strong enough to deflect viral disease. In the case of Lassa virus, however, neutralizing antibodies have not been very good surrogates, since they are produced in much lower quantities. ... The new surrogate of protection will aid in the development of a more potent vaccine against Lassa virus,” according to a press release by Jefferson University.
This work was supported by various grants from the National Institutes of Health. Mr. Mota and two of his colleagues are inventors on a U.S. provisional patent application for a recombinant Lassa-rabies vaccine.
SOURCE: Mota TA et al. Nat Commun. 2018;9:4223. doi: 10.1038/s41467-018-06741-w.
An inactivated recombinant Lassa virus (LASV) and rabies vaccine candidate was developed that protects both mice and guinea pigs from Lassa fever. The vaccine also elicits a lasting humoral response against both LASV and rabies virus in both animal models. The novel vaccine, which uses a rabies virus–derived vector, expresses a codon-optimized LASV glycoprotein, according to Tiago Abreu Mota, a doctoral student at Jefferson University, Philadelphia, and his colleagues.
Lassa fever, a World Health Organization priority disease with a biosafety level of 4, is a hemorrhagic fever caused by the Lassa virus, which has no approved vaccine or potent antiviral treatment, according to the report published online in Nature Communications. So the development of a vaccine would be an important step in protecting the West African population from this deadly disease, which infects an estimated 100,000-300,000 people annually. As many as 80% of Lassa fever exposures are mildly symptomatic and thus go unreported; however, the case fatality rate of full-blown Lassa fever has been reported to reach as high as 50%, according to Mr. Mota and his colleagues.
An advantage to the new vaccine is that it is inactivated and thus could potentially be used in pregnant women and immunosuppressed patients, both of which are major risk groups for Lassa fever, according to the researchers. The vaccine could also protect against rabies, which is another major health concern in the regions affected by the Lassa virus.
In terms of mechanism of action, the vaccine did not induce virus-neutralizing antibodies, but rather appeared to trigger cell-mediated protection through activating natural killer cells to promote significantly more killing of virus-infected cells than nontriggered NK cells (P less than .01), as seen through in vitro testing.
The ability to assay for this form of vaccine effectiveness was a key development, according to the researchers. “The neutralizing antibody has been something of a gold standard in vaccine development. High levels are usually a good indication that the immune reaction is strong enough to deflect viral disease. In the case of Lassa virus, however, neutralizing antibodies have not been very good surrogates, since they are produced in much lower quantities. ... The new surrogate of protection will aid in the development of a more potent vaccine against Lassa virus,” according to a press release by Jefferson University.
This work was supported by various grants from the National Institutes of Health. Mr. Mota and two of his colleagues are inventors on a U.S. provisional patent application for a recombinant Lassa-rabies vaccine.
SOURCE: Mota TA et al. Nat Commun. 2018;9:4223. doi: 10.1038/s41467-018-06741-w.
An inactivated recombinant Lassa virus (LASV) and rabies vaccine candidate was developed that protects both mice and guinea pigs from Lassa fever. The vaccine also elicits a lasting humoral response against both LASV and rabies virus in both animal models. The novel vaccine, which uses a rabies virus–derived vector, expresses a codon-optimized LASV glycoprotein, according to Tiago Abreu Mota, a doctoral student at Jefferson University, Philadelphia, and his colleagues.
Lassa fever, a World Health Organization priority disease with a biosafety level of 4, is a hemorrhagic fever caused by the Lassa virus, which has no approved vaccine or potent antiviral treatment, according to the report published online in Nature Communications. So the development of a vaccine would be an important step in protecting the West African population from this deadly disease, which infects an estimated 100,000-300,000 people annually. As many as 80% of Lassa fever exposures are mildly symptomatic and thus go unreported; however, the case fatality rate of full-blown Lassa fever has been reported to reach as high as 50%, according to Mr. Mota and his colleagues.
An advantage to the new vaccine is that it is inactivated and thus could potentially be used in pregnant women and immunosuppressed patients, both of which are major risk groups for Lassa fever, according to the researchers. The vaccine could also protect against rabies, which is another major health concern in the regions affected by the Lassa virus.
In terms of mechanism of action, the vaccine did not induce virus-neutralizing antibodies, but rather appeared to trigger cell-mediated protection through activating natural killer cells to promote significantly more killing of virus-infected cells than nontriggered NK cells (P less than .01), as seen through in vitro testing.
The ability to assay for this form of vaccine effectiveness was a key development, according to the researchers. “The neutralizing antibody has been something of a gold standard in vaccine development. High levels are usually a good indication that the immune reaction is strong enough to deflect viral disease. In the case of Lassa virus, however, neutralizing antibodies have not been very good surrogates, since they are produced in much lower quantities. ... The new surrogate of protection will aid in the development of a more potent vaccine against Lassa virus,” according to a press release by Jefferson University.
This work was supported by various grants from the National Institutes of Health. Mr. Mota and two of his colleagues are inventors on a U.S. provisional patent application for a recombinant Lassa-rabies vaccine.
SOURCE: Mota TA et al. Nat Commun. 2018;9:4223. doi: 10.1038/s41467-018-06741-w.
FROM NATURE COMMUNICATIONS
Key clinical point: A novel recombinant Lassa virus vaccine protected guinea pigs and mice against Lassa fever.
Major finding: A novel recombinant Lassa virus vaccine elicited strong humeral antibody response in guinea pigs and mice against Lassa and rabies viruses.
Study details: Animal models and an in vitro cellular system were used to assay for the effectiveness of a novel Lassa fever vaccine.
Disclosures: This work was supported by grants from the National Institutes of Health. Mr. Mota and two of his colleagues are inventors on a U.S. provisional patent application for a recombinant Lassa-rabies vaccine.
Source: Mota TA et al. Nat Commun. 2018;9:4223. doi: 10.1038/s41467-018-06741-w.
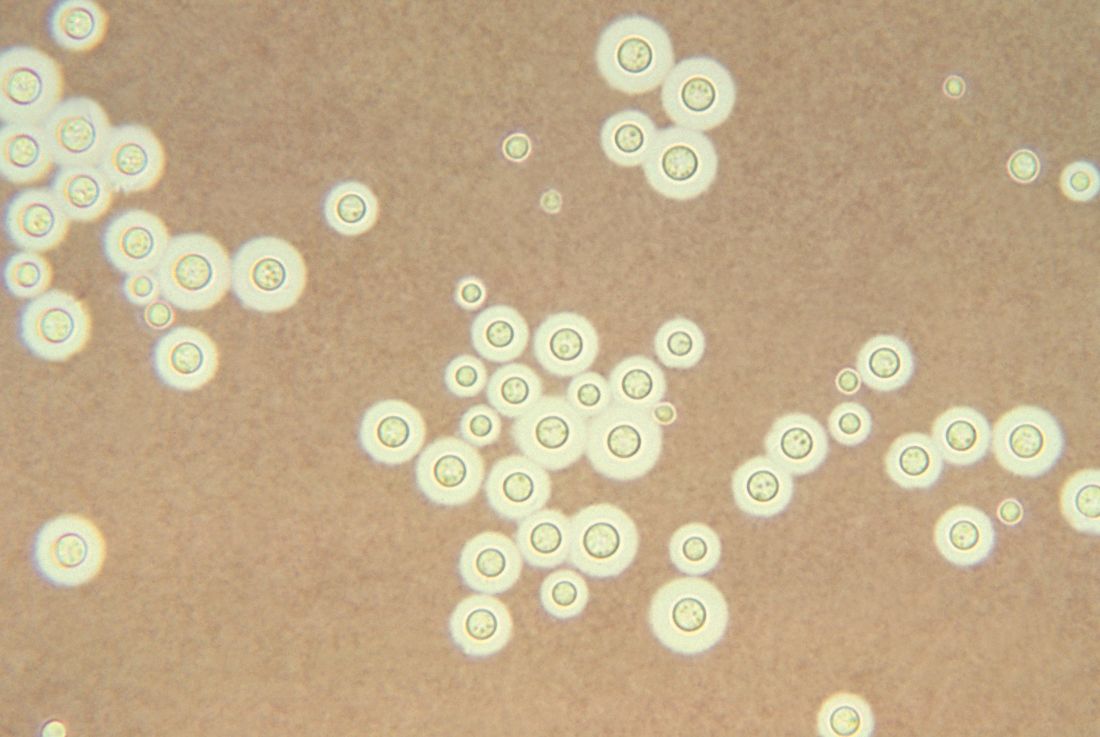
Treating cryptococcal meningitis in patients with HIV
One-week treatment with amphotericin B deoxycholate (AmBd)– and flucytosine (5FC)–based therapy, followed by fluconazole (FLU) on days 8 through 14, is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis, according to the authors of a review of the available literature in the Cochrane Database of Systemic Reviews.
The review is an update of one previous previously published in 2011. The authors found 13 eligible studies that enrolled 2,426 participants and compared 21 interventions. They performed a network meta-analysis using multivariate meta-regression, modeled treatment differences (RR and 95% confidence interval), and determined treatment rankings for 2-week and 10-week mortality outcomes using surface under the cumulative ranking curve, which represents the probability that a treatment will present the best outcome with no uncertainty and was used to develop a hierarchy of treatments for HIV-associated cryptococcal meningitis.
In addition, certainty of the evidence was assessed using the GRADE approach, according to Mark W. Tenforde, MD, of the University of Washington School of Public Health, Seattle, and his colleagues.
They found “reduced 10-week mortality with shortened [AmBd and 5FC] induction therapy, compared to the current gold standard of 2 weeks of AmBd and 5FC, based on moderate-certainty evidence.” They also found no mortality benefit of combination 2 weeks AmBd and FLU, compared with AmBd alone.
“In resource-limited settings, 1-week AmBd- and 5FC-based therapy is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis,” they wrote. “An all-oral regimen of 2 weeks 5FC and FLU may be an alternative in settings where AmBd is unavailable or intravenous therapy cannot be safely administered.” These results indicated the need to expand access to 5FC in resource-limited settings in which HIV-associated cryptococcal meningitis is most common.
They also reported finding no mortality benefit of 2 weeks of combination AmBd and FLU, compared with AmBd alone.
“Given the absence of data from studies in children, and limited data from high-income countries, our findings provide limited guidance for treatment in these patients and settings,” Dr. Tenforde and his colleagues stated.
The authors reported that they had no relevant conflicts of interest.
SOURCE: Tenforde MW et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018 Jul 25;7:CD005647. doi: 10.1002/14651858.CD005647.
One-week treatment with amphotericin B deoxycholate (AmBd)– and flucytosine (5FC)–based therapy, followed by fluconazole (FLU) on days 8 through 14, is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis, according to the authors of a review of the available literature in the Cochrane Database of Systemic Reviews.
The review is an update of one previous previously published in 2011. The authors found 13 eligible studies that enrolled 2,426 participants and compared 21 interventions. They performed a network meta-analysis using multivariate meta-regression, modeled treatment differences (RR and 95% confidence interval), and determined treatment rankings for 2-week and 10-week mortality outcomes using surface under the cumulative ranking curve, which represents the probability that a treatment will present the best outcome with no uncertainty and was used to develop a hierarchy of treatments for HIV-associated cryptococcal meningitis.
In addition, certainty of the evidence was assessed using the GRADE approach, according to Mark W. Tenforde, MD, of the University of Washington School of Public Health, Seattle, and his colleagues.
They found “reduced 10-week mortality with shortened [AmBd and 5FC] induction therapy, compared to the current gold standard of 2 weeks of AmBd and 5FC, based on moderate-certainty evidence.” They also found no mortality benefit of combination 2 weeks AmBd and FLU, compared with AmBd alone.
“In resource-limited settings, 1-week AmBd- and 5FC-based therapy is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis,” they wrote. “An all-oral regimen of 2 weeks 5FC and FLU may be an alternative in settings where AmBd is unavailable or intravenous therapy cannot be safely administered.” These results indicated the need to expand access to 5FC in resource-limited settings in which HIV-associated cryptococcal meningitis is most common.
They also reported finding no mortality benefit of 2 weeks of combination AmBd and FLU, compared with AmBd alone.
“Given the absence of data from studies in children, and limited data from high-income countries, our findings provide limited guidance for treatment in these patients and settings,” Dr. Tenforde and his colleagues stated.
The authors reported that they had no relevant conflicts of interest.
SOURCE: Tenforde MW et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018 Jul 25;7:CD005647. doi: 10.1002/14651858.CD005647.
One-week treatment with amphotericin B deoxycholate (AmBd)– and flucytosine (5FC)–based therapy, followed by fluconazole (FLU) on days 8 through 14, is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis, according to the authors of a review of the available literature in the Cochrane Database of Systemic Reviews.
The review is an update of one previous previously published in 2011. The authors found 13 eligible studies that enrolled 2,426 participants and compared 21 interventions. They performed a network meta-analysis using multivariate meta-regression, modeled treatment differences (RR and 95% confidence interval), and determined treatment rankings for 2-week and 10-week mortality outcomes using surface under the cumulative ranking curve, which represents the probability that a treatment will present the best outcome with no uncertainty and was used to develop a hierarchy of treatments for HIV-associated cryptococcal meningitis.
In addition, certainty of the evidence was assessed using the GRADE approach, according to Mark W. Tenforde, MD, of the University of Washington School of Public Health, Seattle, and his colleagues.
They found “reduced 10-week mortality with shortened [AmBd and 5FC] induction therapy, compared to the current gold standard of 2 weeks of AmBd and 5FC, based on moderate-certainty evidence.” They also found no mortality benefit of combination 2 weeks AmBd and FLU, compared with AmBd alone.
“In resource-limited settings, 1-week AmBd- and 5FC-based therapy is probably superior to other regimens for treatment of HIV-associated cryptococcal meningitis,” they wrote. “An all-oral regimen of 2 weeks 5FC and FLU may be an alternative in settings where AmBd is unavailable or intravenous therapy cannot be safely administered.” These results indicated the need to expand access to 5FC in resource-limited settings in which HIV-associated cryptococcal meningitis is most common.
They also reported finding no mortality benefit of 2 weeks of combination AmBd and FLU, compared with AmBd alone.
“Given the absence of data from studies in children, and limited data from high-income countries, our findings provide limited guidance for treatment in these patients and settings,” Dr. Tenforde and his colleagues stated.
The authors reported that they had no relevant conflicts of interest.
SOURCE: Tenforde MW et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018 Jul 25;7:CD005647. doi: 10.1002/14651858.CD005647.
FROM COCHRANE DATABASE OF SYSTEMIC REVIEWS
Key clinical point: Shorter drug treatment beat the gold standard for HIV-associated cryptococcal meningitis according to a literature review.
Major finding:
Study details: Updated review of articles, registries, and clinical trials during Jan. 1, 1980–July 9, 2018.
Disclosures: The authors reported that they had no relevant conflicts of interest.
Source: Tenforde MW et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018 Jul 25;7:CD005647. doi: 10.1002/14651858.CD005647.
Sex workers: High rates of HIV, low rates of treatment
The HIV pandemic among sex workers remains underaddressed and underresourced, with “glaring gaps” in comprehensive measures of HIV prevalence and incidence, and in prevention and treatment, according to the results of an updated literature review published in the Lancet.
Kate Shannon, PhD, director of the gender and sexual health initiative at the University of British Columbia, Vancouver, and her colleagues updated a 2013 literature search for the Lancet series on HIV and sex workers to include reports and manuscripts published from Jan. 1, 2006, to Sept. 6, 2017.
They found that In particular, 4 years after their previous Lancet series on HIV and sex workers, this updated analysis showed that the global HIV burden among female sex workers was still similar to the previously determined 11.8% and “unacceptably high” at 10.4%, (95% confidence interval, 9.5-11.5).
Although there has been some improvement in the assessment of HIV in transgender women since the previous analysis, according to Dr. Shannon and her colleagues, small sample sizes and conflation of transgender women and men who have sex with men (MSM) continue to limit the volume of transgender-specific HIV data, particularly in Africa.
Access to HIV prevention and treatment also remains a considerable problem for sex workers, according to the authors. In particular, “qualitative data in sub-Saharan Africa suggest that profound structural barriers of stigma and discrimination impede progress in the HIV care continuum,” with studies confirming that “successful HIV treatment trajectories are impeded by violence and displacement” because of policing, they wrote.
They pointed out that things may well become worse, with evidence-based progress on full decriminalization grounded in health and human rights – which was a key recommendation in their earlier Lancet Series – having stalled in all but South Africa. In fact, they reported that several countries had even rolled back rights further for sex workers.
“HIV prevention and treatment tools are available but, without comprehensive HIV epidemiology, a lack of denominators and failure to address structural determinants (including decriminalisation of sex work) means that progress in achieving health and rights for all sex workers will fall short,” the researchers concluded.
The authors reported that they had no competing interests.
SOURCE: Shannon K et al. Lancet. 2018 Aug 25;392:698-710.
The HIV pandemic among sex workers remains underaddressed and underresourced, with “glaring gaps” in comprehensive measures of HIV prevalence and incidence, and in prevention and treatment, according to the results of an updated literature review published in the Lancet.
Kate Shannon, PhD, director of the gender and sexual health initiative at the University of British Columbia, Vancouver, and her colleagues updated a 2013 literature search for the Lancet series on HIV and sex workers to include reports and manuscripts published from Jan. 1, 2006, to Sept. 6, 2017.
They found that In particular, 4 years after their previous Lancet series on HIV and sex workers, this updated analysis showed that the global HIV burden among female sex workers was still similar to the previously determined 11.8% and “unacceptably high” at 10.4%, (95% confidence interval, 9.5-11.5).
Although there has been some improvement in the assessment of HIV in transgender women since the previous analysis, according to Dr. Shannon and her colleagues, small sample sizes and conflation of transgender women and men who have sex with men (MSM) continue to limit the volume of transgender-specific HIV data, particularly in Africa.
Access to HIV prevention and treatment also remains a considerable problem for sex workers, according to the authors. In particular, “qualitative data in sub-Saharan Africa suggest that profound structural barriers of stigma and discrimination impede progress in the HIV care continuum,” with studies confirming that “successful HIV treatment trajectories are impeded by violence and displacement” because of policing, they wrote.
They pointed out that things may well become worse, with evidence-based progress on full decriminalization grounded in health and human rights – which was a key recommendation in their earlier Lancet Series – having stalled in all but South Africa. In fact, they reported that several countries had even rolled back rights further for sex workers.
“HIV prevention and treatment tools are available but, without comprehensive HIV epidemiology, a lack of denominators and failure to address structural determinants (including decriminalisation of sex work) means that progress in achieving health and rights for all sex workers will fall short,” the researchers concluded.
The authors reported that they had no competing interests.
SOURCE: Shannon K et al. Lancet. 2018 Aug 25;392:698-710.
The HIV pandemic among sex workers remains underaddressed and underresourced, with “glaring gaps” in comprehensive measures of HIV prevalence and incidence, and in prevention and treatment, according to the results of an updated literature review published in the Lancet.
Kate Shannon, PhD, director of the gender and sexual health initiative at the University of British Columbia, Vancouver, and her colleagues updated a 2013 literature search for the Lancet series on HIV and sex workers to include reports and manuscripts published from Jan. 1, 2006, to Sept. 6, 2017.
They found that In particular, 4 years after their previous Lancet series on HIV and sex workers, this updated analysis showed that the global HIV burden among female sex workers was still similar to the previously determined 11.8% and “unacceptably high” at 10.4%, (95% confidence interval, 9.5-11.5).
Although there has been some improvement in the assessment of HIV in transgender women since the previous analysis, according to Dr. Shannon and her colleagues, small sample sizes and conflation of transgender women and men who have sex with men (MSM) continue to limit the volume of transgender-specific HIV data, particularly in Africa.
Access to HIV prevention and treatment also remains a considerable problem for sex workers, according to the authors. In particular, “qualitative data in sub-Saharan Africa suggest that profound structural barriers of stigma and discrimination impede progress in the HIV care continuum,” with studies confirming that “successful HIV treatment trajectories are impeded by violence and displacement” because of policing, they wrote.
They pointed out that things may well become worse, with evidence-based progress on full decriminalization grounded in health and human rights – which was a key recommendation in their earlier Lancet Series – having stalled in all but South Africa. In fact, they reported that several countries had even rolled back rights further for sex workers.
“HIV prevention and treatment tools are available but, without comprehensive HIV epidemiology, a lack of denominators and failure to address structural determinants (including decriminalisation of sex work) means that progress in achieving health and rights for all sex workers will fall short,” the researchers concluded.
The authors reported that they had no competing interests.
SOURCE: Shannon K et al. Lancet. 2018 Aug 25;392:698-710.
FROM THE LANCET
Key clinical point: The HIV pandemic among sex workers remains underaddressed and underresourced, with “glaring gaps” in assessment, treatment.
Major finding: The global HIV burden among female sex workers shows that HIV prevalence was “unacceptably high” at 10.4%.
Study details: Researchers updated a 2013 literature review with reports published from Jan. 1, 2006, to Sept. 6, 2017.
Disclosures: The authors reported that they had no competing interests.
Source: Shannon K et al. Lancet. 2018 Aug 25;392:698-710.
Automated algorithm improves HIV/HCV screening in the ED
More patients had newly diagnosed HIV and hepatitis C virus (HCV) infection during an automated-laboratory-order HIV/HCV screening algorithm than with a nurse-order HIV/HCV screening algorithm, according to the results of a retrospective before/after comparison study of the two electronic health record (EHR)–based protocols.
The results of nurse-order HIV/HCV screening in the 5-month period of March 1, 2016, through July 31, 2016, were compared to the subsequently adopted automated-laboratory-order system results from March 1, 2017, through July 31, 2017, according to Douglas A.E. White, MD, and his colleagues at Highland Hospital Emergency Department, Oakland, Calif.
Via the EHR, nurses were instructed to offer screening to all adults aged 18-75 years unless they were known to be HIV- or HCV-positive, unable to verbally consent (e.g., language barriers, intoxication), or medically unstable. Exclusion was at the discretion of the triage nurse. Using a drop-down menu, nurses could choose “accepts” or “declines” for HIV and HCV testing, according to patient response. Choosing “accepts” automatically ordered the test, according to the report (Ann Emerg Med. 2018 Oct;72[4]:438-48).
Automated-laboratory-order HIV/HCV screening was integrated into clinical care. With this protocol, the EHR-automated annual HIV/hepatitis C virus screening was performed on adult patients aged 18-75 years who had laboratory tests ordered. The EHR was configured to automatically order an HIV or HCV test for age-eligible patients who had any test ordered that required laboratory processing of whole blood (excluding point-of-care tests such as for lactate or glucose level) or a urine or urethral swab for chlamydia or gonorrhea testing, according to the researchers.
There were 20,975 and 19,887 unique, age-eligible patients during the nurse-order HIV/HCV virus screening algorithm and automated-laboratory-order HIV/HCV screening algorithm study periods, respectively. A total of 4,121 patients (19.6%) were screened for HIV and 2,968 (14.2%) patients were screened for HCV during the nurse-order period vs. 6,736 (33.9%) patients screened for HIV and 6,972 (35.1%) screened for HCV during the automated-laboratory-order period.
Overall, HIV screening increased from 19.6% to 33.9% and HCV screening, from 14.2% to 35.1% using the automated vs. the nurse-ordered EHR-based algorithm.
“An automated electronic health record algorithm that links nontargeted opt-out HIV and hepatitis C virus screening to physician laboratory ordering more effectively screens ED patients, provides results before discharge, minimizes repeated screening, and diagnoses more new infections than an algorithm that relies on nursing staff to offer screening. Because most EDs in the United States now use EHR systems, this model can be easily replicated and should be considered the standard for future programs,” the researchers concluded.
This work was supported, in part, by grant funding through the FOCUS program, Gilead Sciences, which also has provided funding to various of the authors of the study.
SOURCE: White DAE et al. Ann Emerg Med. 2018 Oct;72[4]:438-48.
More patients had newly diagnosed HIV and hepatitis C virus (HCV) infection during an automated-laboratory-order HIV/HCV screening algorithm than with a nurse-order HIV/HCV screening algorithm, according to the results of a retrospective before/after comparison study of the two electronic health record (EHR)–based protocols.
The results of nurse-order HIV/HCV screening in the 5-month period of March 1, 2016, through July 31, 2016, were compared to the subsequently adopted automated-laboratory-order system results from March 1, 2017, through July 31, 2017, according to Douglas A.E. White, MD, and his colleagues at Highland Hospital Emergency Department, Oakland, Calif.
Via the EHR, nurses were instructed to offer screening to all adults aged 18-75 years unless they were known to be HIV- or HCV-positive, unable to verbally consent (e.g., language barriers, intoxication), or medically unstable. Exclusion was at the discretion of the triage nurse. Using a drop-down menu, nurses could choose “accepts” or “declines” for HIV and HCV testing, according to patient response. Choosing “accepts” automatically ordered the test, according to the report (Ann Emerg Med. 2018 Oct;72[4]:438-48).
Automated-laboratory-order HIV/HCV screening was integrated into clinical care. With this protocol, the EHR-automated annual HIV/hepatitis C virus screening was performed on adult patients aged 18-75 years who had laboratory tests ordered. The EHR was configured to automatically order an HIV or HCV test for age-eligible patients who had any test ordered that required laboratory processing of whole blood (excluding point-of-care tests such as for lactate or glucose level) or a urine or urethral swab for chlamydia or gonorrhea testing, according to the researchers.
There were 20,975 and 19,887 unique, age-eligible patients during the nurse-order HIV/HCV virus screening algorithm and automated-laboratory-order HIV/HCV screening algorithm study periods, respectively. A total of 4,121 patients (19.6%) were screened for HIV and 2,968 (14.2%) patients were screened for HCV during the nurse-order period vs. 6,736 (33.9%) patients screened for HIV and 6,972 (35.1%) screened for HCV during the automated-laboratory-order period.
Overall, HIV screening increased from 19.6% to 33.9% and HCV screening, from 14.2% to 35.1% using the automated vs. the nurse-ordered EHR-based algorithm.
“An automated electronic health record algorithm that links nontargeted opt-out HIV and hepatitis C virus screening to physician laboratory ordering more effectively screens ED patients, provides results before discharge, minimizes repeated screening, and diagnoses more new infections than an algorithm that relies on nursing staff to offer screening. Because most EDs in the United States now use EHR systems, this model can be easily replicated and should be considered the standard for future programs,” the researchers concluded.
This work was supported, in part, by grant funding through the FOCUS program, Gilead Sciences, which also has provided funding to various of the authors of the study.
SOURCE: White DAE et al. Ann Emerg Med. 2018 Oct;72[4]:438-48.
More patients had newly diagnosed HIV and hepatitis C virus (HCV) infection during an automated-laboratory-order HIV/HCV screening algorithm than with a nurse-order HIV/HCV screening algorithm, according to the results of a retrospective before/after comparison study of the two electronic health record (EHR)–based protocols.
The results of nurse-order HIV/HCV screening in the 5-month period of March 1, 2016, through July 31, 2016, were compared to the subsequently adopted automated-laboratory-order system results from March 1, 2017, through July 31, 2017, according to Douglas A.E. White, MD, and his colleagues at Highland Hospital Emergency Department, Oakland, Calif.
Via the EHR, nurses were instructed to offer screening to all adults aged 18-75 years unless they were known to be HIV- or HCV-positive, unable to verbally consent (e.g., language barriers, intoxication), or medically unstable. Exclusion was at the discretion of the triage nurse. Using a drop-down menu, nurses could choose “accepts” or “declines” for HIV and HCV testing, according to patient response. Choosing “accepts” automatically ordered the test, according to the report (Ann Emerg Med. 2018 Oct;72[4]:438-48).
Automated-laboratory-order HIV/HCV screening was integrated into clinical care. With this protocol, the EHR-automated annual HIV/hepatitis C virus screening was performed on adult patients aged 18-75 years who had laboratory tests ordered. The EHR was configured to automatically order an HIV or HCV test for age-eligible patients who had any test ordered that required laboratory processing of whole blood (excluding point-of-care tests such as for lactate or glucose level) or a urine or urethral swab for chlamydia or gonorrhea testing, according to the researchers.
There were 20,975 and 19,887 unique, age-eligible patients during the nurse-order HIV/HCV virus screening algorithm and automated-laboratory-order HIV/HCV screening algorithm study periods, respectively. A total of 4,121 patients (19.6%) were screened for HIV and 2,968 (14.2%) patients were screened for HCV during the nurse-order period vs. 6,736 (33.9%) patients screened for HIV and 6,972 (35.1%) screened for HCV during the automated-laboratory-order period.
Overall, HIV screening increased from 19.6% to 33.9% and HCV screening, from 14.2% to 35.1% using the automated vs. the nurse-ordered EHR-based algorithm.
“An automated electronic health record algorithm that links nontargeted opt-out HIV and hepatitis C virus screening to physician laboratory ordering more effectively screens ED patients, provides results before discharge, minimizes repeated screening, and diagnoses more new infections than an algorithm that relies on nursing staff to offer screening. Because most EDs in the United States now use EHR systems, this model can be easily replicated and should be considered the standard for future programs,” the researchers concluded.
This work was supported, in part, by grant funding through the FOCUS program, Gilead Sciences, which also has provided funding to various of the authors of the study.
SOURCE: White DAE et al. Ann Emerg Med. 2018 Oct;72[4]:438-48.
FROM ANNALS OF EMERGENCY MEDICINE
Key clinical point:
Major finding: HIV screening increased from 19.6% to 33.9%; HCV screening, from 14.2% to 35.1%, with use of an automated vs. nurse-ordered EHR-based algorithm.
Study details: There were 20,975 and 19,887eligible patients assessed during the nurse-order HIV/HCV screening and the automated–laboratory-order screening periods, respectively.
Disclosures: This work was supported, in part, by grant funding through the FOCUS program, Gilead Sciences, which also has provided funding to various of the authors of the study.
Source: White DAE et al. Ann Emerg Med. 2018 Oct;72[4]:438-48.
Myeloperoxidase elevated in HCV-related liver cancer
Myeloperoxidase (MPO) expression was significantly higher in hepatitis C virus (HCV)–related hepatocellular carcinoma (HCC) cases when compared with cirrhotic patients, according to a study of 59 patients with HCV-related liver disease.
HCV is the main cause of liver disease, wrote Mohamed Abdel-Hamed, MD, of Minia University in Egypt, and his colleagues. In addition, HCV is associated with significant oxidative stress, which has been identified as a significant metabolic pathway culminating in hepatic cirrhosis, liver failure, and liver cancer. Thus the researchers studied the role of MPO, an oxidative enzyme released at sites of inflammation, in the possible etiology of HCV-related liver cancer.
The patients were divided into two groups, 25 with HCC and 34 with chronic liver diseases with cirrhosis. All patients were examined immunohistochemically to demonstrate the expression of myeloperoxidase, according to the report published in Meta Gene.
Subjects with HCC showed markedly increased MPO expression when compared with MPO expression in hepatocytes of subjects with liver cirrhosis, who mostly showed a mild degree of expression. In addition, no mild expression of MPO was detected in the subjects with HCC. These findings were highly statistically significant (P less than .0001), according to Dr. Abdel-Hamed and his colleagues.
“The present study showed that marked expression of MPO plays an important role in the pathogenesis of HCV-associated HCC,” the authors stated. “This study could provide valuable, predictive parameters that can be used clinically in the prognosis of HCC patients.”
The authors did not report any disclosures.
SOURCE: Abdel-Hamid M et al. Meta Gene. 2018 Dec;18:1-8.
Myeloperoxidase (MPO) expression was significantly higher in hepatitis C virus (HCV)–related hepatocellular carcinoma (HCC) cases when compared with cirrhotic patients, according to a study of 59 patients with HCV-related liver disease.
HCV is the main cause of liver disease, wrote Mohamed Abdel-Hamed, MD, of Minia University in Egypt, and his colleagues. In addition, HCV is associated with significant oxidative stress, which has been identified as a significant metabolic pathway culminating in hepatic cirrhosis, liver failure, and liver cancer. Thus the researchers studied the role of MPO, an oxidative enzyme released at sites of inflammation, in the possible etiology of HCV-related liver cancer.
The patients were divided into two groups, 25 with HCC and 34 with chronic liver diseases with cirrhosis. All patients were examined immunohistochemically to demonstrate the expression of myeloperoxidase, according to the report published in Meta Gene.
Subjects with HCC showed markedly increased MPO expression when compared with MPO expression in hepatocytes of subjects with liver cirrhosis, who mostly showed a mild degree of expression. In addition, no mild expression of MPO was detected in the subjects with HCC. These findings were highly statistically significant (P less than .0001), according to Dr. Abdel-Hamed and his colleagues.
“The present study showed that marked expression of MPO plays an important role in the pathogenesis of HCV-associated HCC,” the authors stated. “This study could provide valuable, predictive parameters that can be used clinically in the prognosis of HCC patients.”
The authors did not report any disclosures.
SOURCE: Abdel-Hamid M et al. Meta Gene. 2018 Dec;18:1-8.
Myeloperoxidase (MPO) expression was significantly higher in hepatitis C virus (HCV)–related hepatocellular carcinoma (HCC) cases when compared with cirrhotic patients, according to a study of 59 patients with HCV-related liver disease.
HCV is the main cause of liver disease, wrote Mohamed Abdel-Hamed, MD, of Minia University in Egypt, and his colleagues. In addition, HCV is associated with significant oxidative stress, which has been identified as a significant metabolic pathway culminating in hepatic cirrhosis, liver failure, and liver cancer. Thus the researchers studied the role of MPO, an oxidative enzyme released at sites of inflammation, in the possible etiology of HCV-related liver cancer.
The patients were divided into two groups, 25 with HCC and 34 with chronic liver diseases with cirrhosis. All patients were examined immunohistochemically to demonstrate the expression of myeloperoxidase, according to the report published in Meta Gene.
Subjects with HCC showed markedly increased MPO expression when compared with MPO expression in hepatocytes of subjects with liver cirrhosis, who mostly showed a mild degree of expression. In addition, no mild expression of MPO was detected in the subjects with HCC. These findings were highly statistically significant (P less than .0001), according to Dr. Abdel-Hamed and his colleagues.
“The present study showed that marked expression of MPO plays an important role in the pathogenesis of HCV-associated HCC,” the authors stated. “This study could provide valuable, predictive parameters that can be used clinically in the prognosis of HCC patients.”
The authors did not report any disclosures.
SOURCE: Abdel-Hamid M et al. Meta Gene. 2018 Dec;18:1-8.
FROM META GENE
Key clinical point:
Major finding: Hepatocellular carcinoma subjects showed a marked increase of myeloperoxidase expression when compared with subjects with liver cirrhosis (P less than .0001).
Study details: An immunohistochemical analysis of 59 patients infected with hepatitis C virus.
Disclosures: The authors did not report any disclosures.
Source: Abdel-Hamid M et al. Meta Gene. 2018 Dec;18:1-8.
Resident participation in surgery is safe for patients, study shows
Despite concerns that resident involvement in operations might pose a risk to the patient, the inclusion of general surgery residents in high-risk surgery cases does not negatively impact outcomes, according to a database study of more than 25,000 patients.
Adrienne N. Cobb, MD, of Loyola University Medical Center, Maywood, Ill., and her colleagues used the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database (2005-2012) to identify all patients undergoing any of six high-risk procedures on an elective basis.
Dr. Cobb and her colleagues compared outcomes for 25,363 patients who had procedures with and without resident participation: 4,018 and 21,345 patients, respectively. They also evaluated selected outcomes by postgraduate year (PGY). Junior residents were considered as PGY 1-2, senior residents were considered PGY 3, 4, and 5, and participants were considered fellows if they were PGY 6 or higher, according to their report published in the Journal of Surgical Research.
The six procedures assessed were esophagectomy (1,233 patients), open abdominal aortic aneurysm repair (162), laparoscopic paraesophageal resection with Nissen fundoplication (2,316), pancreaticoduodenectomy (Whipple, 10,309), abdominoperineal resection (2,003), and hepatectomy (9,329).
The primary outcome of the study was 30-day mortality with the exposure being resident involvement. Secondary outcomes that had complications included superficial and deep surgical site infection, wound disruption, bleeding requiring transfusion, return to the operating room, pneumonia, unplanned reintubation, pulmonary embolism, acute renal failure, stroke, MI, sepsis, urinary tract infection (UTI), and deep vein thrombosis, operative time, and length of stay.
In both univariate and multivariate analysis, there were no significant differences in mortality between patients who did or did not have procedures in which resident participation at any level of training was involved.
Overall, resident participation did increase the odds of a prolonged operative time (odds ratio, 1.5; 95% confidence interval, 1.1-2.1). Only abdominal perineal resection showed an increased odds risk of having a prolonged operation when residents were involved (OR, 4.3; 95% CI, 1.1-4.8). With regard to these results, the authors commented: “We assert that the additional time spent with trainees in the OR is integral to the production of confident and competent surgeons and does not lead to poorer outcomes for patients. It may, however, lead to increasing costs for the hospital and the patient.”
When risk-adjusted odds were calculated for all the other secondary outcomes and postoperative outcomes tested, UTI was the only one to show a negative impact when residents were involved (OR, 2.3; 95% CI, 1.1-4.8).
The study limitations include the age of the data and the limited number of procedures evaluated, and thus might not be generalizable to a more modern era and other procedures, according to the authors.
“Apart from UTI rates, resident participation did not significantly increase patient morbidity or mortality. Residents should continue to be given active and engaging roles in the OR, even in the most challenging cases,” Dr. Cobb and her colleagues concluded.
The study was funded by the National Institutes of Health. The authors reported that they had no disclosures.
SOURCE: Cobb AN et al. J Surg Res. 2018 Dec; 232:308-17.
Despite concerns that resident involvement in operations might pose a risk to the patient, the inclusion of general surgery residents in high-risk surgery cases does not negatively impact outcomes, according to a database study of more than 25,000 patients.
Adrienne N. Cobb, MD, of Loyola University Medical Center, Maywood, Ill., and her colleagues used the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database (2005-2012) to identify all patients undergoing any of six high-risk procedures on an elective basis.
Dr. Cobb and her colleagues compared outcomes for 25,363 patients who had procedures with and without resident participation: 4,018 and 21,345 patients, respectively. They also evaluated selected outcomes by postgraduate year (PGY). Junior residents were considered as PGY 1-2, senior residents were considered PGY 3, 4, and 5, and participants were considered fellows if they were PGY 6 or higher, according to their report published in the Journal of Surgical Research.
The six procedures assessed were esophagectomy (1,233 patients), open abdominal aortic aneurysm repair (162), laparoscopic paraesophageal resection with Nissen fundoplication (2,316), pancreaticoduodenectomy (Whipple, 10,309), abdominoperineal resection (2,003), and hepatectomy (9,329).
The primary outcome of the study was 30-day mortality with the exposure being resident involvement. Secondary outcomes that had complications included superficial and deep surgical site infection, wound disruption, bleeding requiring transfusion, return to the operating room, pneumonia, unplanned reintubation, pulmonary embolism, acute renal failure, stroke, MI, sepsis, urinary tract infection (UTI), and deep vein thrombosis, operative time, and length of stay.
In both univariate and multivariate analysis, there were no significant differences in mortality between patients who did or did not have procedures in which resident participation at any level of training was involved.
Overall, resident participation did increase the odds of a prolonged operative time (odds ratio, 1.5; 95% confidence interval, 1.1-2.1). Only abdominal perineal resection showed an increased odds risk of having a prolonged operation when residents were involved (OR, 4.3; 95% CI, 1.1-4.8). With regard to these results, the authors commented: “We assert that the additional time spent with trainees in the OR is integral to the production of confident and competent surgeons and does not lead to poorer outcomes for patients. It may, however, lead to increasing costs for the hospital and the patient.”
When risk-adjusted odds were calculated for all the other secondary outcomes and postoperative outcomes tested, UTI was the only one to show a negative impact when residents were involved (OR, 2.3; 95% CI, 1.1-4.8).
The study limitations include the age of the data and the limited number of procedures evaluated, and thus might not be generalizable to a more modern era and other procedures, according to the authors.
“Apart from UTI rates, resident participation did not significantly increase patient morbidity or mortality. Residents should continue to be given active and engaging roles in the OR, even in the most challenging cases,” Dr. Cobb and her colleagues concluded.
The study was funded by the National Institutes of Health. The authors reported that they had no disclosures.
SOURCE: Cobb AN et al. J Surg Res. 2018 Dec; 232:308-17.
Despite concerns that resident involvement in operations might pose a risk to the patient, the inclusion of general surgery residents in high-risk surgery cases does not negatively impact outcomes, according to a database study of more than 25,000 patients.
Adrienne N. Cobb, MD, of Loyola University Medical Center, Maywood, Ill., and her colleagues used the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database (2005-2012) to identify all patients undergoing any of six high-risk procedures on an elective basis.
Dr. Cobb and her colleagues compared outcomes for 25,363 patients who had procedures with and without resident participation: 4,018 and 21,345 patients, respectively. They also evaluated selected outcomes by postgraduate year (PGY). Junior residents were considered as PGY 1-2, senior residents were considered PGY 3, 4, and 5, and participants were considered fellows if they were PGY 6 or higher, according to their report published in the Journal of Surgical Research.
The six procedures assessed were esophagectomy (1,233 patients), open abdominal aortic aneurysm repair (162), laparoscopic paraesophageal resection with Nissen fundoplication (2,316), pancreaticoduodenectomy (Whipple, 10,309), abdominoperineal resection (2,003), and hepatectomy (9,329).
The primary outcome of the study was 30-day mortality with the exposure being resident involvement. Secondary outcomes that had complications included superficial and deep surgical site infection, wound disruption, bleeding requiring transfusion, return to the operating room, pneumonia, unplanned reintubation, pulmonary embolism, acute renal failure, stroke, MI, sepsis, urinary tract infection (UTI), and deep vein thrombosis, operative time, and length of stay.
In both univariate and multivariate analysis, there were no significant differences in mortality between patients who did or did not have procedures in which resident participation at any level of training was involved.
Overall, resident participation did increase the odds of a prolonged operative time (odds ratio, 1.5; 95% confidence interval, 1.1-2.1). Only abdominal perineal resection showed an increased odds risk of having a prolonged operation when residents were involved (OR, 4.3; 95% CI, 1.1-4.8). With regard to these results, the authors commented: “We assert that the additional time spent with trainees in the OR is integral to the production of confident and competent surgeons and does not lead to poorer outcomes for patients. It may, however, lead to increasing costs for the hospital and the patient.”
When risk-adjusted odds were calculated for all the other secondary outcomes and postoperative outcomes tested, UTI was the only one to show a negative impact when residents were involved (OR, 2.3; 95% CI, 1.1-4.8).
The study limitations include the age of the data and the limited number of procedures evaluated, and thus might not be generalizable to a more modern era and other procedures, according to the authors.
“Apart from UTI rates, resident participation did not significantly increase patient morbidity or mortality. Residents should continue to be given active and engaging roles in the OR, even in the most challenging cases,” Dr. Cobb and her colleagues concluded.
The study was funded by the National Institutes of Health. The authors reported that they had no disclosures.
SOURCE: Cobb AN et al. J Surg Res. 2018 Dec; 232:308-17.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: Resident participation in surgery during training was safe for the patients involved.
Major finding: UTI was the only secondary outcome to show a negative impact when residents were involved in surgery (OR, 2.3; 95% CI, 1.1-4.8).
Study details: A retrospective database analysis of six complex procedures involving more than 25,000 surgeries during 2005-2012.
Disclosures: The authors reported that they had no disclosures.
Source: Cobb AN et al. J Surg Res 2018 Dec;232:308-17.
Transition to noninjected drug use lowers risk of HCV infection
A protective effect was seen with regard to hepatitis C virus (HCV) transmission among individuals who “reversed transitioned” to noninjected drug use and in persons who used noninjected drugs in addition to injecting, according to an interview study of 846 drug users.
Data were collected between January 2007 and December 2017 as part of a long-running study of persons entering Mount Sinai Beth Israel drug detoxification and methadone maintenance programs, reported Don C. Des Jarlais, MD, of the Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
Among the 846 individuals studied, men comprised 79%; 41% were white, 15% African American, and 40% Hispanic, with a mean age of 35 years. They were all currently persons who injected drugs (PWID), according to the report published in Drug and Alcohol Dependence.
A total of 97 persons (11%) “reverse transitioned” back to noninjected drug use, according to the researchers; this reverse transitioning was strongly associated with lower HCV positivity, compared with those who continued injecting (30% vs. 47%, respectively; P less than .005).
There was a substantial difference in the HCV prevalence between PWID who reported noninjected use of heroin (43%) versus PWID who did not report noninjected use of heroin (53%) (P = .005).
Distributive needle sharing was common in HCV seropositives who were injecting cocaine in the 6 months prior to the interview: 28% of the HCV seropositives injecting cocaine reported distributive sharing versus 14% of the HCV seropositives not injecting cocaine (P = .001).
“Harm reduction for PWID has been largely defined in terms of ‘safer injection,’ using sterile injection equipment, proper preparation of the injecting site, etc. We would like to suggest that harm reduction for PWID be broadened to include reverse transitions back to exclusive noninjecting use and frequent substitution of noninjecting for injecting use,” the investigators suggested.
The study was funded by the U.S. National Institute on Drug Abuse. The authors reported that they had no conflicts of interest.
SOURCE: Des Jarlais DC et al. Drug Alcohol Depend. 2018 Sep 12. doi: 10.1016/j.drugalcdep.2018.07.034.
A protective effect was seen with regard to hepatitis C virus (HCV) transmission among individuals who “reversed transitioned” to noninjected drug use and in persons who used noninjected drugs in addition to injecting, according to an interview study of 846 drug users.
Data were collected between January 2007 and December 2017 as part of a long-running study of persons entering Mount Sinai Beth Israel drug detoxification and methadone maintenance programs, reported Don C. Des Jarlais, MD, of the Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
Among the 846 individuals studied, men comprised 79%; 41% were white, 15% African American, and 40% Hispanic, with a mean age of 35 years. They were all currently persons who injected drugs (PWID), according to the report published in Drug and Alcohol Dependence.
A total of 97 persons (11%) “reverse transitioned” back to noninjected drug use, according to the researchers; this reverse transitioning was strongly associated with lower HCV positivity, compared with those who continued injecting (30% vs. 47%, respectively; P less than .005).
There was a substantial difference in the HCV prevalence between PWID who reported noninjected use of heroin (43%) versus PWID who did not report noninjected use of heroin (53%) (P = .005).
Distributive needle sharing was common in HCV seropositives who were injecting cocaine in the 6 months prior to the interview: 28% of the HCV seropositives injecting cocaine reported distributive sharing versus 14% of the HCV seropositives not injecting cocaine (P = .001).
“Harm reduction for PWID has been largely defined in terms of ‘safer injection,’ using sterile injection equipment, proper preparation of the injecting site, etc. We would like to suggest that harm reduction for PWID be broadened to include reverse transitions back to exclusive noninjecting use and frequent substitution of noninjecting for injecting use,” the investigators suggested.
The study was funded by the U.S. National Institute on Drug Abuse. The authors reported that they had no conflicts of interest.
SOURCE: Des Jarlais DC et al. Drug Alcohol Depend. 2018 Sep 12. doi: 10.1016/j.drugalcdep.2018.07.034.
A protective effect was seen with regard to hepatitis C virus (HCV) transmission among individuals who “reversed transitioned” to noninjected drug use and in persons who used noninjected drugs in addition to injecting, according to an interview study of 846 drug users.
Data were collected between January 2007 and December 2017 as part of a long-running study of persons entering Mount Sinai Beth Israel drug detoxification and methadone maintenance programs, reported Don C. Des Jarlais, MD, of the Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
Among the 846 individuals studied, men comprised 79%; 41% were white, 15% African American, and 40% Hispanic, with a mean age of 35 years. They were all currently persons who injected drugs (PWID), according to the report published in Drug and Alcohol Dependence.
A total of 97 persons (11%) “reverse transitioned” back to noninjected drug use, according to the researchers; this reverse transitioning was strongly associated with lower HCV positivity, compared with those who continued injecting (30% vs. 47%, respectively; P less than .005).
There was a substantial difference in the HCV prevalence between PWID who reported noninjected use of heroin (43%) versus PWID who did not report noninjected use of heroin (53%) (P = .005).
Distributive needle sharing was common in HCV seropositives who were injecting cocaine in the 6 months prior to the interview: 28% of the HCV seropositives injecting cocaine reported distributive sharing versus 14% of the HCV seropositives not injecting cocaine (P = .001).
“Harm reduction for PWID has been largely defined in terms of ‘safer injection,’ using sterile injection equipment, proper preparation of the injecting site, etc. We would like to suggest that harm reduction for PWID be broadened to include reverse transitions back to exclusive noninjecting use and frequent substitution of noninjecting for injecting use,” the investigators suggested.
The study was funded by the U.S. National Institute on Drug Abuse. The authors reported that they had no conflicts of interest.
SOURCE: Des Jarlais DC et al. Drug Alcohol Depend. 2018 Sep 12. doi: 10.1016/j.drugalcdep.2018.07.034.
FROM DRUG AND ALCOHOL DEPENDENCE
Key clinical point: Encouraging reverse transitioning to noninjected drug use could help persons who injected drugs lower their risk of hepatitis C virus infection.
Major finding: Reverse transitioning was strongly associated with lower hepatitis C virus positivity, compared with continued drug injection (P less than .005).
Study details: An interview study of 846 drug users.
Disclosures: The study was funded by the U.S. National Institute on Drug Abuse. The authors reported that they had no conflicts of interest.
Source: Des Jarlais DC et al. Drug Alcohol Depend. 2018 Sep 12. doi: 10.1016/j.drugalcdep.2018.07.034.