User login
COVID-19 & Mental Health
On Thursday, April 23, 2020, MDedge Psychiatry hosted a Twitter conversation at #MDedgeChats on COVID-19 and mental health.
Two psychiatrists affiliated with Johns Hopkins University, Dinah Miller, MD (@shrinkrapdinah), and Elizabeth Ryznar, MD (@RyznarMD), hosted the conversation. Throughout the conversation several themes emerged. One is that COVID-19 illustrates the connections between housing and health, and another is that stigma tied to being COVID positive is leading to suicidality, particularly in Haiti. The discussants also talked about the importance of self-care.
Questions asked during the Twitter chat:
- How are your pre-pandemic patients doing during this crisis?
- How has COVID-19 affected inpatient and outpatient care for you?
- How are our most vulnerable populations being affected by COVID-19?
- How are you doing personally and professionally as medical professionals during the pandemic?
- What psychiatric manifestations are you seeing in your patients who have had COVID-19?
The following is an edited version of the discussion. For the full experience, visit our Twitter archive, you can still join the conversation.













Some experts are predicting that the magnitude of the mental health fallout from the COVID-19 pandemic will be profound. They also have concerns that physical distancing and increased unemployment forced by the pandemic will lead to a rise in suicide risk, particularly for at-risk populations.1
For psychiatric patients, COVID-19 is expected to leave behind higher levels of anxiety, depression, and insomnia.2
And for health care workers on the front lines, the mental health toll could lead to stress, burnout, and worse.
Clinicians are also dealing with shortages of PPE and medical equipment, worrying about their safety and that of their families, while trying to save lives amid great uncertainty about SARS-CoV-2, the coronavirus that causes COVID-19.
Most recently an emergency department physician in New York who was recovering from COVID-19 herself reportedly recently ended her own life, according to her father, who is a physician.
As Dr. Sarah Candler said in a previous twitter chat with MDedge Internal Medicine, “Good doctors take care of themselves, too.” Be kind to yourself during this global crisis.
The National Suicide Prevention Lifeline is always available at 1-800-273-TALK (8255).
Resources
- Mental health and the COVID-19 pandemic
- Brief examines the COVID-19 crisis’ implications for Americans’ mental health
- COVID-19: Helping health care workers on the front lines
- Overcoming COVID-related stress
- Confessions of an outpatient psychiatrist during the pandemic
- Psychiatric patients may be among the hardest hit
- Experts hasten to head off mental health crisis
- Podcast: Physician Suicide
1Lancet Psychiatry. 2020 Apr 21. doi: 10.1016/S2215-0366(20):30171-1.
2Brain, Behav Immun. 2020 Apr 27. doi: 10.10116/j.bbi.2020.04.069).
On Thursday, April 23, 2020, MDedge Psychiatry hosted a Twitter conversation at #MDedgeChats on COVID-19 and mental health.
Two psychiatrists affiliated with Johns Hopkins University, Dinah Miller, MD (@shrinkrapdinah), and Elizabeth Ryznar, MD (@RyznarMD), hosted the conversation. Throughout the conversation several themes emerged. One is that COVID-19 illustrates the connections between housing and health, and another is that stigma tied to being COVID positive is leading to suicidality, particularly in Haiti. The discussants also talked about the importance of self-care.
Questions asked during the Twitter chat:
- How are your pre-pandemic patients doing during this crisis?
- How has COVID-19 affected inpatient and outpatient care for you?
- How are our most vulnerable populations being affected by COVID-19?
- How are you doing personally and professionally as medical professionals during the pandemic?
- What psychiatric manifestations are you seeing in your patients who have had COVID-19?
The following is an edited version of the discussion. For the full experience, visit our Twitter archive, you can still join the conversation.













Some experts are predicting that the magnitude of the mental health fallout from the COVID-19 pandemic will be profound. They also have concerns that physical distancing and increased unemployment forced by the pandemic will lead to a rise in suicide risk, particularly for at-risk populations.1
For psychiatric patients, COVID-19 is expected to leave behind higher levels of anxiety, depression, and insomnia.2
And for health care workers on the front lines, the mental health toll could lead to stress, burnout, and worse.
Clinicians are also dealing with shortages of PPE and medical equipment, worrying about their safety and that of their families, while trying to save lives amid great uncertainty about SARS-CoV-2, the coronavirus that causes COVID-19.
Most recently an emergency department physician in New York who was recovering from COVID-19 herself reportedly recently ended her own life, according to her father, who is a physician.
As Dr. Sarah Candler said in a previous twitter chat with MDedge Internal Medicine, “Good doctors take care of themselves, too.” Be kind to yourself during this global crisis.
The National Suicide Prevention Lifeline is always available at 1-800-273-TALK (8255).
Resources
- Mental health and the COVID-19 pandemic
- Brief examines the COVID-19 crisis’ implications for Americans’ mental health
- COVID-19: Helping health care workers on the front lines
- Overcoming COVID-related stress
- Confessions of an outpatient psychiatrist during the pandemic
- Psychiatric patients may be among the hardest hit
- Experts hasten to head off mental health crisis
- Podcast: Physician Suicide
1Lancet Psychiatry. 2020 Apr 21. doi: 10.1016/S2215-0366(20):30171-1.
2Brain, Behav Immun. 2020 Apr 27. doi: 10.10116/j.bbi.2020.04.069).
On Thursday, April 23, 2020, MDedge Psychiatry hosted a Twitter conversation at #MDedgeChats on COVID-19 and mental health.
Two psychiatrists affiliated with Johns Hopkins University, Dinah Miller, MD (@shrinkrapdinah), and Elizabeth Ryznar, MD (@RyznarMD), hosted the conversation. Throughout the conversation several themes emerged. One is that COVID-19 illustrates the connections between housing and health, and another is that stigma tied to being COVID positive is leading to suicidality, particularly in Haiti. The discussants also talked about the importance of self-care.
Questions asked during the Twitter chat:
- How are your pre-pandemic patients doing during this crisis?
- How has COVID-19 affected inpatient and outpatient care for you?
- How are our most vulnerable populations being affected by COVID-19?
- How are you doing personally and professionally as medical professionals during the pandemic?
- What psychiatric manifestations are you seeing in your patients who have had COVID-19?
The following is an edited version of the discussion. For the full experience, visit our Twitter archive, you can still join the conversation.













Some experts are predicting that the magnitude of the mental health fallout from the COVID-19 pandemic will be profound. They also have concerns that physical distancing and increased unemployment forced by the pandemic will lead to a rise in suicide risk, particularly for at-risk populations.1
For psychiatric patients, COVID-19 is expected to leave behind higher levels of anxiety, depression, and insomnia.2
And for health care workers on the front lines, the mental health toll could lead to stress, burnout, and worse.
Clinicians are also dealing with shortages of PPE and medical equipment, worrying about their safety and that of their families, while trying to save lives amid great uncertainty about SARS-CoV-2, the coronavirus that causes COVID-19.
Most recently an emergency department physician in New York who was recovering from COVID-19 herself reportedly recently ended her own life, according to her father, who is a physician.
As Dr. Sarah Candler said in a previous twitter chat with MDedge Internal Medicine, “Good doctors take care of themselves, too.” Be kind to yourself during this global crisis.
The National Suicide Prevention Lifeline is always available at 1-800-273-TALK (8255).
Resources
- Mental health and the COVID-19 pandemic
- Brief examines the COVID-19 crisis’ implications for Americans’ mental health
- COVID-19: Helping health care workers on the front lines
- Overcoming COVID-related stress
- Confessions of an outpatient psychiatrist during the pandemic
- Psychiatric patients may be among the hardest hit
- Experts hasten to head off mental health crisis
- Podcast: Physician Suicide
1Lancet Psychiatry. 2020 Apr 21. doi: 10.1016/S2215-0366(20):30171-1.
2Brain, Behav Immun. 2020 Apr 27. doi: 10.10116/j.bbi.2020.04.069).
COVID-19 & Mental Health

Join us on Thursday, April 23, at 8:30 p.m. EST as we discuss how the COVID-19 pandemic is affecting the mental health of psychiatry patients and providers around the world.
Our special guests include two psychiatry educators with expertise in therapeutic psychotherapy and solutions on how to help our most vulnerable populations being affected by COVID-19, Dinah Miller, MD (@shrinkraphdinah), and Elizabeth Ryznar, MD (@RyznarMD). We hope you will participate in our Twitter chat this evening, at 8:30 p.m. EST on #MDedgeChats.
Public health emergencies can affect the well-being of individuals and communities causing possible feelings of insecurity, confusion, and emotional isolation. These effects may translate into a range of emotional reactions affecting current psychiatric conditions and creating new ones, according to the New England Journal of Medicine.
According to the Kaiser Family Foundation, “nearly 45% of adults across the country say that worry and stress related to the coronavirus pandemic are hurting their mental health.”
In this chat, we will discuss this topic and how COVID-19 is affecting your patients and practice. Join us tonight and feel free to share what you have experienced during this pandemic at 8:30 pm EST on #MDedgeChats.
Topics of Conversation
Question 1: How are pre-pandemic patients doing during the crisis?
Question 2: How has COVID-19 affected inpatient and outpatient care for you?
Question 3: How are our most vulnerable populations being affected by COVID-19?
Question 4: How are you doing personally and professionally as a medical professional and psychiatrist amidst this pandemic?
Question 5: What psychiatric manifestations are you seeing in your patients who have had COVID-19?
About Dr. Dinah Miller
Dr. Dinah Miller (@shrinkrapdinah) a psychiatrist with a private practice and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. Dr. Miller is also a columnist for and a member of the Editorial Advisory Board of Clinical Psychiatry News. She is the co-author of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016) and “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University, 2011).
About Dr. Elizabeth Ryznar
Dr. Elizabeth Ryznar (@RyznarMD) is a psychiatry clinician-educator research fellow and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. She completed her medical training at Harvard Medical School in Boston and her residency training at Northwestern University in Chicago. Dr. Ryznar is co-editor of the new book “Landmark Papers in Psychiatry,” published by Oxford University Press, and has several peer-reviewed articles.
Resources
- Mental health and the COVID-19 pandemic
- Brief examines the COVID-19 crisis’ implications for Americans’ mental health
- COVID-19: Helping health care workers on the front lines
- Overcoming COVID-related stress
- Confessions of an outpatient psychiatrist during the pandemic
- Psychiatric patients may be among the hardest hit
- Experts hasten to head off mental health crisis

Join us on Thursday, April 23, at 8:30 p.m. EST as we discuss how the COVID-19 pandemic is affecting the mental health of psychiatry patients and providers around the world.
Our special guests include two psychiatry educators with expertise in therapeutic psychotherapy and solutions on how to help our most vulnerable populations being affected by COVID-19, Dinah Miller, MD (@shrinkraphdinah), and Elizabeth Ryznar, MD (@RyznarMD). We hope you will participate in our Twitter chat this evening, at 8:30 p.m. EST on #MDedgeChats.
Public health emergencies can affect the well-being of individuals and communities causing possible feelings of insecurity, confusion, and emotional isolation. These effects may translate into a range of emotional reactions affecting current psychiatric conditions and creating new ones, according to the New England Journal of Medicine.
According to the Kaiser Family Foundation, “nearly 45% of adults across the country say that worry and stress related to the coronavirus pandemic are hurting their mental health.”
In this chat, we will discuss this topic and how COVID-19 is affecting your patients and practice. Join us tonight and feel free to share what you have experienced during this pandemic at 8:30 pm EST on #MDedgeChats.
Topics of Conversation
Question 1: How are pre-pandemic patients doing during the crisis?
Question 2: How has COVID-19 affected inpatient and outpatient care for you?
Question 3: How are our most vulnerable populations being affected by COVID-19?
Question 4: How are you doing personally and professionally as a medical professional and psychiatrist amidst this pandemic?
Question 5: What psychiatric manifestations are you seeing in your patients who have had COVID-19?
About Dr. Dinah Miller
Dr. Dinah Miller (@shrinkrapdinah) a psychiatrist with a private practice and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. Dr. Miller is also a columnist for and a member of the Editorial Advisory Board of Clinical Psychiatry News. She is the co-author of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016) and “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University, 2011).
About Dr. Elizabeth Ryznar
Dr. Elizabeth Ryznar (@RyznarMD) is a psychiatry clinician-educator research fellow and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. She completed her medical training at Harvard Medical School in Boston and her residency training at Northwestern University in Chicago. Dr. Ryznar is co-editor of the new book “Landmark Papers in Psychiatry,” published by Oxford University Press, and has several peer-reviewed articles.
Resources
- Mental health and the COVID-19 pandemic
- Brief examines the COVID-19 crisis’ implications for Americans’ mental health
- COVID-19: Helping health care workers on the front lines
- Overcoming COVID-related stress
- Confessions of an outpatient psychiatrist during the pandemic
- Psychiatric patients may be among the hardest hit
- Experts hasten to head off mental health crisis

Join us on Thursday, April 23, at 8:30 p.m. EST as we discuss how the COVID-19 pandemic is affecting the mental health of psychiatry patients and providers around the world.
Our special guests include two psychiatry educators with expertise in therapeutic psychotherapy and solutions on how to help our most vulnerable populations being affected by COVID-19, Dinah Miller, MD (@shrinkraphdinah), and Elizabeth Ryznar, MD (@RyznarMD). We hope you will participate in our Twitter chat this evening, at 8:30 p.m. EST on #MDedgeChats.
Public health emergencies can affect the well-being of individuals and communities causing possible feelings of insecurity, confusion, and emotional isolation. These effects may translate into a range of emotional reactions affecting current psychiatric conditions and creating new ones, according to the New England Journal of Medicine.
According to the Kaiser Family Foundation, “nearly 45% of adults across the country say that worry and stress related to the coronavirus pandemic are hurting their mental health.”
In this chat, we will discuss this topic and how COVID-19 is affecting your patients and practice. Join us tonight and feel free to share what you have experienced during this pandemic at 8:30 pm EST on #MDedgeChats.
Topics of Conversation
Question 1: How are pre-pandemic patients doing during the crisis?
Question 2: How has COVID-19 affected inpatient and outpatient care for you?
Question 3: How are our most vulnerable populations being affected by COVID-19?
Question 4: How are you doing personally and professionally as a medical professional and psychiatrist amidst this pandemic?
Question 5: What psychiatric manifestations are you seeing in your patients who have had COVID-19?
About Dr. Dinah Miller
Dr. Dinah Miller (@shrinkrapdinah) a psychiatrist with a private practice and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. Dr. Miller is also a columnist for and a member of the Editorial Advisory Board of Clinical Psychiatry News. She is the co-author of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016) and “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University, 2011).
About Dr. Elizabeth Ryznar
Dr. Elizabeth Ryznar (@RyznarMD) is a psychiatry clinician-educator research fellow and an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore. She completed her medical training at Harvard Medical School in Boston and her residency training at Northwestern University in Chicago. Dr. Ryznar is co-editor of the new book “Landmark Papers in Psychiatry,” published by Oxford University Press, and has several peer-reviewed articles.
Resources
- Mental health and the COVID-19 pandemic
- Brief examines the COVID-19 crisis’ implications for Americans’ mental health
- COVID-19: Helping health care workers on the front lines
- Overcoming COVID-related stress
- Confessions of an outpatient psychiatrist during the pandemic
- Psychiatric patients may be among the hardest hit
- Experts hasten to head off mental health crisis
Twitter Chat: Skin Cancer
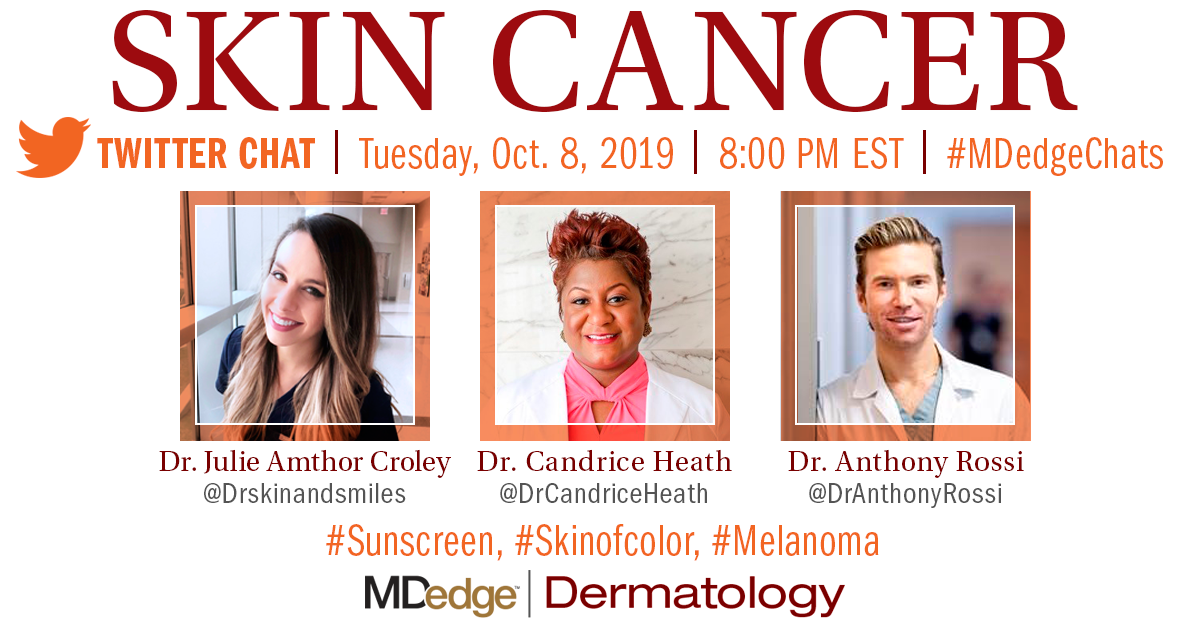
Join us on Tuesday, October 8, 2019, at 8:00 pm EST on Twitter at #MDedgeChats as we discuss skin cancer, and what’s new in sunscreen, skin of color, and melanoma.
Special guests include physicians with expertise in dermatology and skin cancer, Anthony Rossi, MD (@DrAnthonyRossi), Julie Amthor Croley, MD, 15k followers on IG (@Drskinandsmiles), and Candrice Heath, MD (@DrCandriceHeath). Background information about the chat can be found below.
What will the conversation cover?
Q1: What are the most common types of skin cancer?
Q2: What recent research findings can better inform patients about skin cancer risks?
Q3: What’s the difference between melanoma in fair skin vs. darker skin?
Q4: How does the risk of skin cancer differ in people with darker skin?
Q5: Why should sunscreen be used even in the fall and winter?

Follow us here: @MDedgeDerm | @MDedgeTweets | #MDedgeChats
About Dr. Rossi:
Dr. Anthony Rossi (@DrAnthonyRossi) is a board-certified dermatologist with fellowship training in Mohs micrographic surgery, cosmetic and laser surgery, and advanced cutaneous oncology at the Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College program, both in New York. He specializes in skin cancer surgery, cosmetic dermatologic surgery, and laser surgery.
His research includes quality of life in cancer survivors, the use of noninvasive imaging of the skin, and nonsurgical treatments of skin cancer. Additionally, Dr. Rossi is active in dermatologic organizations and advocacy for medicine.
Research and Publications by Dr. Rossi
About Dr. Heath:
Dr. Candrice Heath (@DrCandriceHeath) is Assistant Professor of Dermatology at the Lewis Katz School of Medicine at Temple University in Philadelphia, Pennsylvania with fellowship training in pediatric dermatology at Johns Hopkins University in Baltimore, Maryland. Dr. Heath is triple board certified in pediatrics, dermatology, and pediatric dermatology. She specializes in adult and pediatric dermatology, skin of color, acne, and eczema. Dr. Heath also enjoys educating primary care physicians on the front lines of health care and delivering easy to understand information to consumers.
Research and publications by Dr. Heath
Guest host of MDedge podcast: A sunscreen update with Dr. Vincent DeLeo.
About Dr. Croley:
Dr. Julie Amthor Croley (@Drskinandsmiles) also known as “Dr. Skin and Smiles” has 15,000 followers on Instagram, and is a Chief Dermatology Resident at the University of Texas Medical Branch in Galveston, Texas. She has a special interest in skin cancer and dermatological surgery and hopes to complete a fellowship in Mohs micrographic surgery after residency. In her free time, Dr. Croley enjoys spending time with her husband (an orthopedic surgeon), running and competing in marathons, and spending time on the beach.
Cutaneous melanoma is the most fatal form of skin cancer and is a considerable public health concern in the United States. Early detection and management of skin cancer can lead to decreased morbidity and mortality from skin cancer. As a result, the American Academy of Dermatology Association supports safe sun-protective practices and diligent self-screening for changing lesions.
Sunscreen use is an essential component of sun protection. New regulations from the US Food and Drug Administration (FDA) have left consumers concerned about the safety of sunscreens. According to a recent Cutis editorial from Vincent A. DeLeo, MD, “There is no question that, as physicians, we want to ‘first, do no harm,’ so we should all be interested in assuring our patients that our sunscreen recommendations are safe and we support the FDA proposal for additional data.”
Patients with skin of color experience disproportionately higher morbidity and mortality when diagnosed with melanoma. “Poor prognosis in patients with skin of color is multifactorial and may be due to poor use of sun protection, misconceptions about melanoma risk, atypical clinical presentation, impaired access to care, and delay in diagnosis,” according to a recent Cutis article.
Population-based skin cancer screening performed exclusively by dermatologists is not practical. Primary care physicians and other experts in melanoma and public health need to be involved in reducing melanoma mortality.
In this chat, we will provide expert recommendations on the diagnosis of skin cancer, preventive measures, and the latest research discussed among physicians.
- “Doctor, Do I Need a Skin Check?”
- Assessing the effectiveness of knowledge-based interventions in skin of color populations.
- Melanoma in US Hispanics
- Podcast: Sunscreen update from Dr. Vincent DeLeo
- Windshield and UV exposure
- Racial, ethnic minorities often don’t practice sun-protective behaviors.
- Sunscreen regulations and advice for your patients.
Join us on Tuesday, October 8, 2019, at 8:00 pm EST on Twitter at #MDedgeChats as we discuss skin cancer, and what’s new in sunscreen, skin of color, and melanoma.
Special guests include physicians with expertise in dermatology and skin cancer, Anthony Rossi, MD (@DrAnthonyRossi), Julie Amthor Croley, MD, 15k followers on IG (@Drskinandsmiles), and Candrice Heath, MD (@DrCandriceHeath). Background information about the chat can be found below.
What will the conversation cover?
Q1: What are the most common types of skin cancer?
Q2: What recent research findings can better inform patients about skin cancer risks?
Q3: What’s the difference between melanoma in fair skin vs. darker skin?
Q4: How does the risk of skin cancer differ in people with darker skin?
Q5: Why should sunscreen be used even in the fall and winter?

Follow us here: @MDedgeDerm | @MDedgeTweets | #MDedgeChats
About Dr. Rossi:
Dr. Anthony Rossi (@DrAnthonyRossi) is a board-certified dermatologist with fellowship training in Mohs micrographic surgery, cosmetic and laser surgery, and advanced cutaneous oncology at the Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College program, both in New York. He specializes in skin cancer surgery, cosmetic dermatologic surgery, and laser surgery.
His research includes quality of life in cancer survivors, the use of noninvasive imaging of the skin, and nonsurgical treatments of skin cancer. Additionally, Dr. Rossi is active in dermatologic organizations and advocacy for medicine.
Research and Publications by Dr. Rossi
About Dr. Heath:
Dr. Candrice Heath (@DrCandriceHeath) is Assistant Professor of Dermatology at the Lewis Katz School of Medicine at Temple University in Philadelphia, Pennsylvania with fellowship training in pediatric dermatology at Johns Hopkins University in Baltimore, Maryland. Dr. Heath is triple board certified in pediatrics, dermatology, and pediatric dermatology. She specializes in adult and pediatric dermatology, skin of color, acne, and eczema. Dr. Heath also enjoys educating primary care physicians on the front lines of health care and delivering easy to understand information to consumers.
Research and publications by Dr. Heath
Guest host of MDedge podcast: A sunscreen update with Dr. Vincent DeLeo.
About Dr. Croley:
Dr. Julie Amthor Croley (@Drskinandsmiles) also known as “Dr. Skin and Smiles” has 15,000 followers on Instagram, and is a Chief Dermatology Resident at the University of Texas Medical Branch in Galveston, Texas. She has a special interest in skin cancer and dermatological surgery and hopes to complete a fellowship in Mohs micrographic surgery after residency. In her free time, Dr. Croley enjoys spending time with her husband (an orthopedic surgeon), running and competing in marathons, and spending time on the beach.
Cutaneous melanoma is the most fatal form of skin cancer and is a considerable public health concern in the United States. Early detection and management of skin cancer can lead to decreased morbidity and mortality from skin cancer. As a result, the American Academy of Dermatology Association supports safe sun-protective practices and diligent self-screening for changing lesions.
Sunscreen use is an essential component of sun protection. New regulations from the US Food and Drug Administration (FDA) have left consumers concerned about the safety of sunscreens. According to a recent Cutis editorial from Vincent A. DeLeo, MD, “There is no question that, as physicians, we want to ‘first, do no harm,’ so we should all be interested in assuring our patients that our sunscreen recommendations are safe and we support the FDA proposal for additional data.”
Patients with skin of color experience disproportionately higher morbidity and mortality when diagnosed with melanoma. “Poor prognosis in patients with skin of color is multifactorial and may be due to poor use of sun protection, misconceptions about melanoma risk, atypical clinical presentation, impaired access to care, and delay in diagnosis,” according to a recent Cutis article.
Population-based skin cancer screening performed exclusively by dermatologists is not practical. Primary care physicians and other experts in melanoma and public health need to be involved in reducing melanoma mortality.
In this chat, we will provide expert recommendations on the diagnosis of skin cancer, preventive measures, and the latest research discussed among physicians.
- “Doctor, Do I Need a Skin Check?”
- Assessing the effectiveness of knowledge-based interventions in skin of color populations.
- Melanoma in US Hispanics
- Podcast: Sunscreen update from Dr. Vincent DeLeo
- Windshield and UV exposure
- Racial, ethnic minorities often don’t practice sun-protective behaviors.
- Sunscreen regulations and advice for your patients.
Join us on Tuesday, October 8, 2019, at 8:00 pm EST on Twitter at #MDedgeChats as we discuss skin cancer, and what’s new in sunscreen, skin of color, and melanoma.
Special guests include physicians with expertise in dermatology and skin cancer, Anthony Rossi, MD (@DrAnthonyRossi), Julie Amthor Croley, MD, 15k followers on IG (@Drskinandsmiles), and Candrice Heath, MD (@DrCandriceHeath). Background information about the chat can be found below.
What will the conversation cover?
Q1: What are the most common types of skin cancer?
Q2: What recent research findings can better inform patients about skin cancer risks?
Q3: What’s the difference between melanoma in fair skin vs. darker skin?
Q4: How does the risk of skin cancer differ in people with darker skin?
Q5: Why should sunscreen be used even in the fall and winter?

Follow us here: @MDedgeDerm | @MDedgeTweets | #MDedgeChats
About Dr. Rossi:
Dr. Anthony Rossi (@DrAnthonyRossi) is a board-certified dermatologist with fellowship training in Mohs micrographic surgery, cosmetic and laser surgery, and advanced cutaneous oncology at the Memorial Sloan Kettering Cancer Center and Weill Cornell Medical College program, both in New York. He specializes in skin cancer surgery, cosmetic dermatologic surgery, and laser surgery.
His research includes quality of life in cancer survivors, the use of noninvasive imaging of the skin, and nonsurgical treatments of skin cancer. Additionally, Dr. Rossi is active in dermatologic organizations and advocacy for medicine.
Research and Publications by Dr. Rossi
About Dr. Heath:
Dr. Candrice Heath (@DrCandriceHeath) is Assistant Professor of Dermatology at the Lewis Katz School of Medicine at Temple University in Philadelphia, Pennsylvania with fellowship training in pediatric dermatology at Johns Hopkins University in Baltimore, Maryland. Dr. Heath is triple board certified in pediatrics, dermatology, and pediatric dermatology. She specializes in adult and pediatric dermatology, skin of color, acne, and eczema. Dr. Heath also enjoys educating primary care physicians on the front lines of health care and delivering easy to understand information to consumers.
Research and publications by Dr. Heath
Guest host of MDedge podcast: A sunscreen update with Dr. Vincent DeLeo.
About Dr. Croley:
Dr. Julie Amthor Croley (@Drskinandsmiles) also known as “Dr. Skin and Smiles” has 15,000 followers on Instagram, and is a Chief Dermatology Resident at the University of Texas Medical Branch in Galveston, Texas. She has a special interest in skin cancer and dermatological surgery and hopes to complete a fellowship in Mohs micrographic surgery after residency. In her free time, Dr. Croley enjoys spending time with her husband (an orthopedic surgeon), running and competing in marathons, and spending time on the beach.
Cutaneous melanoma is the most fatal form of skin cancer and is a considerable public health concern in the United States. Early detection and management of skin cancer can lead to decreased morbidity and mortality from skin cancer. As a result, the American Academy of Dermatology Association supports safe sun-protective practices and diligent self-screening for changing lesions.
Sunscreen use is an essential component of sun protection. New regulations from the US Food and Drug Administration (FDA) have left consumers concerned about the safety of sunscreens. According to a recent Cutis editorial from Vincent A. DeLeo, MD, “There is no question that, as physicians, we want to ‘first, do no harm,’ so we should all be interested in assuring our patients that our sunscreen recommendations are safe and we support the FDA proposal for additional data.”
Patients with skin of color experience disproportionately higher morbidity and mortality when diagnosed with melanoma. “Poor prognosis in patients with skin of color is multifactorial and may be due to poor use of sun protection, misconceptions about melanoma risk, atypical clinical presentation, impaired access to care, and delay in diagnosis,” according to a recent Cutis article.
Population-based skin cancer screening performed exclusively by dermatologists is not practical. Primary care physicians and other experts in melanoma and public health need to be involved in reducing melanoma mortality.
In this chat, we will provide expert recommendations on the diagnosis of skin cancer, preventive measures, and the latest research discussed among physicians.
- “Doctor, Do I Need a Skin Check?”
- Assessing the effectiveness of knowledge-based interventions in skin of color populations.
- Melanoma in US Hispanics
- Podcast: Sunscreen update from Dr. Vincent DeLeo
- Windshield and UV exposure
- Racial, ethnic minorities often don’t practice sun-protective behaviors.
- Sunscreen regulations and advice for your patients.

