User login
A Transdisciplinary Program for Care of Veterans With Neurocognitive Disorders
Dementia is a devastating condition resulting in major functional, emotional, and financial impact on patients, their caregivers, and families. Approximately 6.5 million Americans are living with Alzheimer disease (AD), the most common of many causes of dementia.1 The prevalence of AD could increase to 12.7 million Americans by 2050 as the population ages.1 Studies suggest that dementia, also known as major neurocognitive disorder, is common and underdiagnosed among US veterans, a population with a mean age of 65 years.2 During cognitive screening, memory impairment is present in approximately 20% of veterans aged ≥ 75 years who have not been diagnosed with a neurocognitive disorder.3 In addition, veterans might be particularly vulnerable to dementia at an earlier age than the general population because of vascular risk factors and traumatic brain injuries.4 These concerns highlight the need for effective dementia care programs at US Department of Veterans Affairs (VA) facilities.
The US health care system often does not adequately address the needs of patients with dementia and their caregivers.5 Dementia care requires specialized medical care among collaborating professionals and caregiver and psychosocial interventions and services. However, the US health care system is fragmented with different clinicians and services siloed into separate practices and most dementia care occurring in primary care settings.6 Primary care professionals (PCPs) often are uncomfortable diagnosing and managing dementia because of time constraints, lack of expertise and training, and inability to deal with the range of care needs.7 PCPs do not identify approximately 42% of their patients with dementia and, when recognized, do not adhere to dementia care guidelines and address caregiver needs.8-10 Research indicates that caregiver support improves dementia care by teaching behavioral management skills and caregiver coping strategies, allowing patients to stay at home and delay institutionalization.6,11,12 Clinicians underuse available resources and do not incorporate them in their patient care.10 These community services benefit patients and caregivers and significantly improve the overall quality of care.6
Memory clinics have emerged to address these deficiencies when managing dementia.13 The most effective memory clinics maximize the use of specialists with different expertise in dementia care, particularly integrated programs where disciplines function together rather than independently.1,5,14 Systematic reviews and meta-analyses have documented the effectiveness of collaborative care management programs.11,12,15 Integration of dementia care management is associated with earlier diagnosis and interventions, decreased functional and cognitive symptom severity, decreased or delayed institutionalization, improved quality of life for patients and caregivers, enhanced overall quality of care and cost-effectiveness, and better integration of community services.11,12,14-19 In these programs, designating a dementia care manager (DCM) as the patient’s advocate facilitates the integrated structure, increases the quality of care, helps caregivers, facilitates adherence to dementia practice guidelines, and prevents behavioral and psychological symptoms of dementia (BPSD).1,6,11,12,20,21
The best interprofessional model for dementia care might be the transdisciplinary model that includes a DCM. To meet the specific demands of dementia care, there must be a high level of interprofessional collaboration rather than multiple health care professionals (HCPs) delivering care in isolation—an approach that is time consuming and often difficult to implement.22 Whereas multidisciplinary care refers to delivery of parallel services and interdisciplinary care implies a joint formulation, transdisciplinary care aims to maximize integration of HCPs and their specific expertise and contributions through interactions and discussions that deliver focused input to the lead physician. The transdisciplinary model addresses needs that often are missed and can minimize disparities in the quality of dementia care.23 A DCM is an integral part of our program, facilitating understanding and implementation of the final care plan and providing long-term follow-up and care. We outline a conference-centered transdisciplinary dementia care model with a social worker as DCM (SW-DCM) at our VA medical center.
Program Description
In 2020, the VA Greater Los Angeles Healthcare System (VAGLAHS) in California established a multispecialty clinic dedicated to evaluation and treatment of veterans with memory and neurocognitive disorders and to provide support for their caregivers and families. With the agreement of leadership in mental health, neurology, and geriatrics services on the importance of collaboration for dementia care, the psychiatry and neurology services created a joint Memory and Neurobehavior Clinic, which completed its first 2 years of operation as a full-day program. In recent months, the clinic has scheduled 24 veterans per day, approximately 50% new evaluations and 50% follow-up patients, with wait times of < 2 months. There is a mean of 12 intake or lead physicians who could attend sessions in the morning, afternoon, or both. The general clinic flow consists of a 2-hour intake evaluation of new referrals by the lead physician followed by a clinic conference with transdisciplinary discussion. The DCM then follows up with the veteran/caregiver presenting a final care plan individualized to the veterans, caregivers, and families.
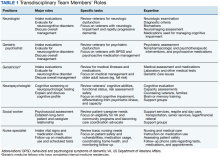
The Memory and Neurobehavior team includes behavioral neurologists, geriatric psychiatrists, neuropsychologists, geriatric fellows, advanced clinical nurses, and social workers who function as the DCM (Table 1).
Procedures
Before the office visit, the coordinating geriatric psychiatrist triages veterans to neurology, psychiatry, or geriatric physicians based on the clinical presentation, history of neurologic signs or symptoms, BPSD or psychiatric history, functional decline, or comorbid medical illnesses. Although veterans often have overlapping concerns, the triage process aims to coordinate the intake evaluations with the most indicated and available specialist with the intention to notify the other specialists during the transdisciplinary conference.
Referrals to the program occur from many sources, notably from primary care (70.8%), mental health (16.7%), and specialty clinics (12.5%). The clinic also receives referrals from the affiliated Veterans Cognitive Assessment and Management Program, which provides dementia evaluation and support via telehealth screening. This VAGLAHS program services a diverse population of veterans: 87% male; 43% aged > 65 years (75% in our clinic); 51% non-Hispanic White; 19% non-Hispanic African American; 16% Hispanic; 4% Asian; and 1% Native American. This population receives care at regional VA medical centers and community-based outpatient clinics over a wide geographic service area.
The initial standardized assessments by intake or lead physicians includes mental status screening with the Montreal Cognitive Assessment (with certified clinicians), the Neurobehavioral Status Examination for a more detailed assessment of cognitive domains, the Columbia-Suicide Severity Rating Scale, the Patient Health Questionnaire for depression screening, and assessment for impairments in instrumental or basic activities of daily living. This initial evaluation aims to apply clinical guidelines and diagnostic criteria for the differential diagnosis of neurocognitive disorders, determine eligibility for cognitive-enhancing medications and techniques, assess for BPSD and the need for nonpharmacologic or pharmacologic interventions, determine functional status, and evaluate the need for supervision, safety concerns, and evidence of neglect or abuse.
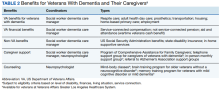
As part of its mission, the clinic is charged with implementing the VA Dementia System of Care (DSOC). The stated goals of the DSOC are to provide individualized person-centered dementia care to help veterans experiencing dementia and their caregivers maintain a positive and optimal quality of life and create an environment where VA medical center staff understand the health care needs of veterans with dementia and their caregivers’ role. As part of this initiative, the clinic includes (1) coordination of care through a SW-DCM; (2)
Transdisciplinary Conference
Clinic conferences are held after the veterans are seen. Staff gather to discuss the patient and review management. All team members are present, as well as the head of the clinical clerical staff who can facilitate appointments, make lobby and wait times more bearable for our patients and caregivers, and help manage emergencies. Although this is an in-person conference, the COVID-19 pandemic has allowed us to include staff who screen at remote sites via videoconferencing, similar to other VA programs.24 The Memory and Neurobehavior Clinic has two ≤ 90-minute conferences daily. The lead physicians and their senior attendings present the new intake evaluations (4-6 at each conference session) with a preliminary formulation and questions for discussion. The moderator solicits contributions from the different disciplines, going from one to the next and recording their responses for each veteran. Further specialists are available for consultation through the conference mechanism if necessary. The final assessment is reviewed, a diagnosis is established, and a tailored, individualized care plan for adjusting or optimizing the veteran’s care is presented to the lead physician who makes the final determination. At the close of the conference, the team’s discussion is recorded along with the lead physician’s original detailed intake evaluation. Currently, the records go into the Computerized Patient Record System, but we are making plans to transition to Cerner as it is implemented.
During the discussion, team members review several areas of consideration. If there is neuroimaging, neurologists review the images projected on a large computer screen. Team members also will assess for the need to obtain biomarker studies, such as blood, cerebrospinal fluid, or positron emission tomography. Psychiatrists could review management of BPSD and use of psychotropic agents, and neuropsychologists might consider the need for more precise cognitive testing and whether a capacity assessment is indicated. Social work might bring up the need for a durable power of attorney as well as applicable caregiver and community resources. Geriatric medicine and nursing could provide input into medical management and care and the ability of veterans and caregivers to follow the prescribed regimen. Further areas of discussion include driving safety and restrictions on driving (as required in California) and the presence of guns in the home. Finally, brief education is provided in short 10-to-15-minute lectures covering pertinent topics so staff remain up-to-date in this changing field.
Postconference Continuity
After the conference, the SW-DCM continues to provide support throughout the disease course, helping veterans and their caregivers understand and follow through on the team’s recommendations. The SW-DCM, who is experienced and trained in case management, forms an ongoing relationship with the veterans and their caregivers and remains an advocate for their care. The SW-DCM communicates the final plan by phone and, when necessary, requests the lead physician to call to clarify any poorly understood or technical aspects of the care plan. About 50% of our veterans—primarily those who do not have a neurocognitive disorder or have mild cognitive impairment—return to their PCPs with our care plan consultation; about 25% are already enrolled in geriatric and other programs with long-term follow-up. The assigned SW-DCM follows up with the remaining veterans and caregivers regularly by phone, facilitates communication with other team members, and endeavors to assure postvisit continuity of care and support during advancing stages of the disease. In addition, the SW-DCM can provide supportive counseling and psychotherapy for stressed caregivers, refer to support groups and cognitive rehabilitation programs, and help develop long-term goals and consideration for supervised living environments. The nurse specialist participates with follow-up calls regarding medications and scheduled tests and appointments, clearing up confusion about instructions, avoiding medication errors, and providing education in dementia care. Both social worker and nurse are present throughout the week, reachable by phone, and, in turn, able to contact the clinic physicians for veterans’ needs.
Discussion
Because of the heterogenous medical and psychosocial needs of veterans with dementia and their caregivers, a transdisciplinary team with a dedicated DCM might offer the most effective and efficient model for dementia care. We present a transdisciplinary program that incorporates dementia specialists in a single evaluation by maximizing their time through a conference-centered program. Our program involves neurologists, psychiatrists, geriatricians, psychologists, nurses, and social workers collaborating and communicating to enact effective dementia care. It further meets the goals of the VA-DSOC in implementing individualized patient and caregiver care.
This transdisciplinary model addresses a number of issues, starting with the differential diagnosis of underlying neurologic conditions. Within the transdisciplinary team, the neurologist can provide specific insights into any neurologic findings and illnesses, such as Alzheimer disease and other neurodegenerative dementias, vascular dementia syndromes, normal pressure hydrocephalus, Creutzfeldt-Jakob disease, neurosyphilis, and others. Most veterans with dementia experience BPSD at some point during of their illness. The psychiatrists on the transdisciplinary team can maximize management of BPSD with nonpharmacologic interventions and the fewest and least aversive psychoactive medications. Our program also addresses the need for more precise cognitive evaluation. Neuropsychologists are present and available for administrating neuropsychologic tests and interpreting cognitive performance and any earlier neuropsychologic testing. This model also cares for the caregivers and assesses their needs. The social worker—as well as other members of the team—can provide caregivers with strategies for coping with disruptive and other behaviors related to dementia, counsel them on how to manage the veteran’s functional decline, and aid in establishing a safe living space. Because the social worker serves as a DCM, these coping and adjustment questions occupy significant clinical attention between appointments. This transdisciplinary model places the patient’s illness in the context of their functional status, diagnoses, and medications. The team geriatrician and the nurse specialist are indispensable resources. The clinic conference provides a teaching venue for staff and trainees and a mechanism to discuss new developments in dementia care, such as the increasing need to assess individuals with mild cognitive impairment.25 This model depends on the DCM’s invaluable role in ensuring implementation of the dementia care plan and continuity of care.
Conclusions
We describe effective dementia care with a transdisciplinary team in a conference setting and with the participation of a dedicated DCM.5 To date, this program appears to be an efficient, sustainable application of the limited resources allocated to dementia care. Nevertheless, we are collecting data to compare with performance measures, track use, and assess the programs effects on continuity of care. We look forward to presenting metrics from our program that show improvement in the health care for veterans experiencing a devastating and increasingly common disorder.
1. 2022 Alzheimer’s disease facts and figures. Alzheimers Dement. 2022;18(4):700-789. doi:10.1002/alz.12638
2. National Center for Veterans Analysis and Statistics. Profile of veterans: 2016. Accessed October 12, 2022. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2016.pdf
3. Chodosh J, Sultzer DL, Lee ML, et al. Memory impairment among primary care veterans. Aging Ment Health. 2007;11(4):444-450. doi:10.1080/13607860601086272
4. Kennedy E, Panahi S, Stewart IJ, et al. Traumatic brain injury and early onset dementia in post 9-11 veterans. Brain Inj. 2022;36(5):620-627. doi:10.1080/02699052.2022.20338465. Heintz H, Monette P, Epstein-Lubow G, Smith L, Rowlett S, Forester BP. Emerging collaborative care models for dementia care in the primary care setting: a narrative review. Am J Geriatr Psychiatry. 2020;28(3):320-330. doi:10.1016/j.jagp.2019.07.015
6. Reuben DB, Evertson LC, Wenger NS, et al. The University of California at Los Angeles Alzheimer’s and Dementia Care program for comprehensive, coordinated, patient-centered care: preliminary data. J Am Geriatr Soc. 2013;61(12):2214-2218. doi:10.1111/jgs.12562
7. Apesoa-Varano EC, Barker JC, Hinton L. Curing and caring: the work of primary care physicians with dementia patients. Qual Health Res. 2011;21(11):1469-1483. doi:10.1177/1049732311412788
8. Creavin ST, Noel-Storr AH, Langdon RJ, et al. Clinical judgement by primary care physicians for the diagnosis of all-cause dementia or cognitive impairment in symptomatic people. Cochrane Database Syst Rev. 2022;6:CD012558. doi:10.1002/14651858.CD012558.pub2
9. Sivananthan SN, Puyat JH, McGrail KM. Variations in self-reported practice of physicians providing clinical care to individuals with dementia: a systematic review. J Am Geriatr Soc. 2013;61(8):1277-1285. doi:10.1111/jgs.12368
10. Rosen CS, Chow HC, Greenbaum MA, et al. How well are clinicians following dementia practice guidelines? Alzheimer Dis Assoc Disord. 2002;16(1):15-23. doi:10.1097/00002093-200201000-00003
11. Reilly S, Miranda-Castillo C, Malouf R, et al. Case management approaches to home support for people with dementia. Cochrane Database Syst Rev. 2015;1:CD008345. doi:10.1002/14651858.CD008345.pub2
12. Tam-Tham H, Cepoiu-Martin M, Ronksley PE, Maxwell CJ, Hemmelgarn BR. Dementia case management and risk of long-term care placement: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2013;28(9):889-902. doi:10.1002/gps.3906
13. Jolley D, Benbow SM, Grizzell M. Memory clinics. Postgrad Med J. 2006;82(965):199-206. doi:10.1136/pgmj.2005.040592
14. Muhlichen F, Michalowsky B, Radke A, et al. Tasks and activities of an effective collaborative dementia care management program in German primary care. J Alzheimers Dis. 2022;87(4):1615-1625. doi:10.3233/JAD-215656
15. Somme D, Trouve H, Drame M, Gagnon D, Couturier Y, Saint-Jean O. Analysis of case management programs for patients with dementia: a systematic review. Alzheimers Dement. 2012;8(5):426-436. doi:10.1016/j.jalz.2011.06.004
16. Ramakers IH, Verhey FR. Development of memory clinics in the Netherlands: 1998 to 2009. Aging Ment Health. 2011;15(1):34-39. doi:10.1080/13607863.2010.519321
17. LaMantia MA, Alder CA, Callahan CM, et al. The aging brain care medical home: preliminary data. J Am Geriatr Soc. 2015;63(6):1209-1213. doi:10.1111/jgs.13447
18. Rubinsztein JS, van Rensburg MJ, Al-Salihy Z, et al. A memory clinic v. traditional community mental health team service: comparison of costs and quality. BJPsych Bull. 2015;39(1):6-11. doi:10.1192/pb.bp.113.044263
19. Lee L, Hillier LM, Harvey D. Integrating community services into primary care: improving the quality of dementia care. Neurodegener Dis Manag. 2014;4(1):11-21. doi:10.2217/nmt.13.72
20. Bass DM, Judge KS, Snow AL, et al. Caregiver outcomes of partners in dementia care: effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc. 2013;61(8):1377-1386. doi:10.1111/jgs.12362
21. Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148-2157. doi:10.1001/jama.295.18.2148
22. Leggett A, Connell C, Dubin L, et al. Dementia care across a tertiary care health system: what exists now and what needs to change. J Am Med Dir Assoc. 2019;20(10):1307-12 e1. doi:10.1016/j.jamda.2019.04.006
23. Brown AF, Vassar SD, Connor KI, Vickrey BG. Collaborative care management reduces disparities in dementia care quality for caregivers with less education. J Am Geriatr Soc. 2013;61(2):243-251. doi:10.1111/jgs.12079
24. Powers BB, Homer MC, Morone N, Edmonds N, Rossi MI. Creation of an interprofessional teledementia clinic for rural veterans: preliminary data. J Am Geriatr Soc. 2017;65(5):1092-1099. doi:10.1111/jgs.14839
25. Galvin JE, Aisen P, Langbaum JB, et al. Early stages of Alzheimer’s Disease: evolving the care team for optimal patient management. Front Neurol. 2020;11:592302. doi:10.3389/fneur.2020.592302
Dementia is a devastating condition resulting in major functional, emotional, and financial impact on patients, their caregivers, and families. Approximately 6.5 million Americans are living with Alzheimer disease (AD), the most common of many causes of dementia.1 The prevalence of AD could increase to 12.7 million Americans by 2050 as the population ages.1 Studies suggest that dementia, also known as major neurocognitive disorder, is common and underdiagnosed among US veterans, a population with a mean age of 65 years.2 During cognitive screening, memory impairment is present in approximately 20% of veterans aged ≥ 75 years who have not been diagnosed with a neurocognitive disorder.3 In addition, veterans might be particularly vulnerable to dementia at an earlier age than the general population because of vascular risk factors and traumatic brain injuries.4 These concerns highlight the need for effective dementia care programs at US Department of Veterans Affairs (VA) facilities.
The US health care system often does not adequately address the needs of patients with dementia and their caregivers.5 Dementia care requires specialized medical care among collaborating professionals and caregiver and psychosocial interventions and services. However, the US health care system is fragmented with different clinicians and services siloed into separate practices and most dementia care occurring in primary care settings.6 Primary care professionals (PCPs) often are uncomfortable diagnosing and managing dementia because of time constraints, lack of expertise and training, and inability to deal with the range of care needs.7 PCPs do not identify approximately 42% of their patients with dementia and, when recognized, do not adhere to dementia care guidelines and address caregiver needs.8-10 Research indicates that caregiver support improves dementia care by teaching behavioral management skills and caregiver coping strategies, allowing patients to stay at home and delay institutionalization.6,11,12 Clinicians underuse available resources and do not incorporate them in their patient care.10 These community services benefit patients and caregivers and significantly improve the overall quality of care.6
Memory clinics have emerged to address these deficiencies when managing dementia.13 The most effective memory clinics maximize the use of specialists with different expertise in dementia care, particularly integrated programs where disciplines function together rather than independently.1,5,14 Systematic reviews and meta-analyses have documented the effectiveness of collaborative care management programs.11,12,15 Integration of dementia care management is associated with earlier diagnosis and interventions, decreased functional and cognitive symptom severity, decreased or delayed institutionalization, improved quality of life for patients and caregivers, enhanced overall quality of care and cost-effectiveness, and better integration of community services.11,12,14-19 In these programs, designating a dementia care manager (DCM) as the patient’s advocate facilitates the integrated structure, increases the quality of care, helps caregivers, facilitates adherence to dementia practice guidelines, and prevents behavioral and psychological symptoms of dementia (BPSD).1,6,11,12,20,21
The best interprofessional model for dementia care might be the transdisciplinary model that includes a DCM. To meet the specific demands of dementia care, there must be a high level of interprofessional collaboration rather than multiple health care professionals (HCPs) delivering care in isolation—an approach that is time consuming and often difficult to implement.22 Whereas multidisciplinary care refers to delivery of parallel services and interdisciplinary care implies a joint formulation, transdisciplinary care aims to maximize integration of HCPs and their specific expertise and contributions through interactions and discussions that deliver focused input to the lead physician. The transdisciplinary model addresses needs that often are missed and can minimize disparities in the quality of dementia care.23 A DCM is an integral part of our program, facilitating understanding and implementation of the final care plan and providing long-term follow-up and care. We outline a conference-centered transdisciplinary dementia care model with a social worker as DCM (SW-DCM) at our VA medical center.
Program Description
In 2020, the VA Greater Los Angeles Healthcare System (VAGLAHS) in California established a multispecialty clinic dedicated to evaluation and treatment of veterans with memory and neurocognitive disorders and to provide support for their caregivers and families. With the agreement of leadership in mental health, neurology, and geriatrics services on the importance of collaboration for dementia care, the psychiatry and neurology services created a joint Memory and Neurobehavior Clinic, which completed its first 2 years of operation as a full-day program. In recent months, the clinic has scheduled 24 veterans per day, approximately 50% new evaluations and 50% follow-up patients, with wait times of < 2 months. There is a mean of 12 intake or lead physicians who could attend sessions in the morning, afternoon, or both. The general clinic flow consists of a 2-hour intake evaluation of new referrals by the lead physician followed by a clinic conference with transdisciplinary discussion. The DCM then follows up with the veteran/caregiver presenting a final care plan individualized to the veterans, caregivers, and families.
The Memory and Neurobehavior team includes behavioral neurologists, geriatric psychiatrists, neuropsychologists, geriatric fellows, advanced clinical nurses, and social workers who function as the DCM (Table 1).
Procedures
Before the office visit, the coordinating geriatric psychiatrist triages veterans to neurology, psychiatry, or geriatric physicians based on the clinical presentation, history of neurologic signs or symptoms, BPSD or psychiatric history, functional decline, or comorbid medical illnesses. Although veterans often have overlapping concerns, the triage process aims to coordinate the intake evaluations with the most indicated and available specialist with the intention to notify the other specialists during the transdisciplinary conference.
Referrals to the program occur from many sources, notably from primary care (70.8%), mental health (16.7%), and specialty clinics (12.5%). The clinic also receives referrals from the affiliated Veterans Cognitive Assessment and Management Program, which provides dementia evaluation and support via telehealth screening. This VAGLAHS program services a diverse population of veterans: 87% male; 43% aged > 65 years (75% in our clinic); 51% non-Hispanic White; 19% non-Hispanic African American; 16% Hispanic; 4% Asian; and 1% Native American. This population receives care at regional VA medical centers and community-based outpatient clinics over a wide geographic service area.
The initial standardized assessments by intake or lead physicians includes mental status screening with the Montreal Cognitive Assessment (with certified clinicians), the Neurobehavioral Status Examination for a more detailed assessment of cognitive domains, the Columbia-Suicide Severity Rating Scale, the Patient Health Questionnaire for depression screening, and assessment for impairments in instrumental or basic activities of daily living. This initial evaluation aims to apply clinical guidelines and diagnostic criteria for the differential diagnosis of neurocognitive disorders, determine eligibility for cognitive-enhancing medications and techniques, assess for BPSD and the need for nonpharmacologic or pharmacologic interventions, determine functional status, and evaluate the need for supervision, safety concerns, and evidence of neglect or abuse.
As part of its mission, the clinic is charged with implementing the VA Dementia System of Care (DSOC). The stated goals of the DSOC are to provide individualized person-centered dementia care to help veterans experiencing dementia and their caregivers maintain a positive and optimal quality of life and create an environment where VA medical center staff understand the health care needs of veterans with dementia and their caregivers’ role. As part of this initiative, the clinic includes (1) coordination of care through a SW-DCM; (2)
Transdisciplinary Conference
Clinic conferences are held after the veterans are seen. Staff gather to discuss the patient and review management. All team members are present, as well as the head of the clinical clerical staff who can facilitate appointments, make lobby and wait times more bearable for our patients and caregivers, and help manage emergencies. Although this is an in-person conference, the COVID-19 pandemic has allowed us to include staff who screen at remote sites via videoconferencing, similar to other VA programs.24 The Memory and Neurobehavior Clinic has two ≤ 90-minute conferences daily. The lead physicians and their senior attendings present the new intake evaluations (4-6 at each conference session) with a preliminary formulation and questions for discussion. The moderator solicits contributions from the different disciplines, going from one to the next and recording their responses for each veteran. Further specialists are available for consultation through the conference mechanism if necessary. The final assessment is reviewed, a diagnosis is established, and a tailored, individualized care plan for adjusting or optimizing the veteran’s care is presented to the lead physician who makes the final determination. At the close of the conference, the team’s discussion is recorded along with the lead physician’s original detailed intake evaluation. Currently, the records go into the Computerized Patient Record System, but we are making plans to transition to Cerner as it is implemented.
During the discussion, team members review several areas of consideration. If there is neuroimaging, neurologists review the images projected on a large computer screen. Team members also will assess for the need to obtain biomarker studies, such as blood, cerebrospinal fluid, or positron emission tomography. Psychiatrists could review management of BPSD and use of psychotropic agents, and neuropsychologists might consider the need for more precise cognitive testing and whether a capacity assessment is indicated. Social work might bring up the need for a durable power of attorney as well as applicable caregiver and community resources. Geriatric medicine and nursing could provide input into medical management and care and the ability of veterans and caregivers to follow the prescribed regimen. Further areas of discussion include driving safety and restrictions on driving (as required in California) and the presence of guns in the home. Finally, brief education is provided in short 10-to-15-minute lectures covering pertinent topics so staff remain up-to-date in this changing field.
Postconference Continuity
After the conference, the SW-DCM continues to provide support throughout the disease course, helping veterans and their caregivers understand and follow through on the team’s recommendations. The SW-DCM, who is experienced and trained in case management, forms an ongoing relationship with the veterans and their caregivers and remains an advocate for their care. The SW-DCM communicates the final plan by phone and, when necessary, requests the lead physician to call to clarify any poorly understood or technical aspects of the care plan. About 50% of our veterans—primarily those who do not have a neurocognitive disorder or have mild cognitive impairment—return to their PCPs with our care plan consultation; about 25% are already enrolled in geriatric and other programs with long-term follow-up. The assigned SW-DCM follows up with the remaining veterans and caregivers regularly by phone, facilitates communication with other team members, and endeavors to assure postvisit continuity of care and support during advancing stages of the disease. In addition, the SW-DCM can provide supportive counseling and psychotherapy for stressed caregivers, refer to support groups and cognitive rehabilitation programs, and help develop long-term goals and consideration for supervised living environments. The nurse specialist participates with follow-up calls regarding medications and scheduled tests and appointments, clearing up confusion about instructions, avoiding medication errors, and providing education in dementia care. Both social worker and nurse are present throughout the week, reachable by phone, and, in turn, able to contact the clinic physicians for veterans’ needs.
Discussion
Because of the heterogenous medical and psychosocial needs of veterans with dementia and their caregivers, a transdisciplinary team with a dedicated DCM might offer the most effective and efficient model for dementia care. We present a transdisciplinary program that incorporates dementia specialists in a single evaluation by maximizing their time through a conference-centered program. Our program involves neurologists, psychiatrists, geriatricians, psychologists, nurses, and social workers collaborating and communicating to enact effective dementia care. It further meets the goals of the VA-DSOC in implementing individualized patient and caregiver care.
This transdisciplinary model addresses a number of issues, starting with the differential diagnosis of underlying neurologic conditions. Within the transdisciplinary team, the neurologist can provide specific insights into any neurologic findings and illnesses, such as Alzheimer disease and other neurodegenerative dementias, vascular dementia syndromes, normal pressure hydrocephalus, Creutzfeldt-Jakob disease, neurosyphilis, and others. Most veterans with dementia experience BPSD at some point during of their illness. The psychiatrists on the transdisciplinary team can maximize management of BPSD with nonpharmacologic interventions and the fewest and least aversive psychoactive medications. Our program also addresses the need for more precise cognitive evaluation. Neuropsychologists are present and available for administrating neuropsychologic tests and interpreting cognitive performance and any earlier neuropsychologic testing. This model also cares for the caregivers and assesses their needs. The social worker—as well as other members of the team—can provide caregivers with strategies for coping with disruptive and other behaviors related to dementia, counsel them on how to manage the veteran’s functional decline, and aid in establishing a safe living space. Because the social worker serves as a DCM, these coping and adjustment questions occupy significant clinical attention between appointments. This transdisciplinary model places the patient’s illness in the context of their functional status, diagnoses, and medications. The team geriatrician and the nurse specialist are indispensable resources. The clinic conference provides a teaching venue for staff and trainees and a mechanism to discuss new developments in dementia care, such as the increasing need to assess individuals with mild cognitive impairment.25 This model depends on the DCM’s invaluable role in ensuring implementation of the dementia care plan and continuity of care.
Conclusions
We describe effective dementia care with a transdisciplinary team in a conference setting and with the participation of a dedicated DCM.5 To date, this program appears to be an efficient, sustainable application of the limited resources allocated to dementia care. Nevertheless, we are collecting data to compare with performance measures, track use, and assess the programs effects on continuity of care. We look forward to presenting metrics from our program that show improvement in the health care for veterans experiencing a devastating and increasingly common disorder.
Dementia is a devastating condition resulting in major functional, emotional, and financial impact on patients, their caregivers, and families. Approximately 6.5 million Americans are living with Alzheimer disease (AD), the most common of many causes of dementia.1 The prevalence of AD could increase to 12.7 million Americans by 2050 as the population ages.1 Studies suggest that dementia, also known as major neurocognitive disorder, is common and underdiagnosed among US veterans, a population with a mean age of 65 years.2 During cognitive screening, memory impairment is present in approximately 20% of veterans aged ≥ 75 years who have not been diagnosed with a neurocognitive disorder.3 In addition, veterans might be particularly vulnerable to dementia at an earlier age than the general population because of vascular risk factors and traumatic brain injuries.4 These concerns highlight the need for effective dementia care programs at US Department of Veterans Affairs (VA) facilities.
The US health care system often does not adequately address the needs of patients with dementia and their caregivers.5 Dementia care requires specialized medical care among collaborating professionals and caregiver and psychosocial interventions and services. However, the US health care system is fragmented with different clinicians and services siloed into separate practices and most dementia care occurring in primary care settings.6 Primary care professionals (PCPs) often are uncomfortable diagnosing and managing dementia because of time constraints, lack of expertise and training, and inability to deal with the range of care needs.7 PCPs do not identify approximately 42% of their patients with dementia and, when recognized, do not adhere to dementia care guidelines and address caregiver needs.8-10 Research indicates that caregiver support improves dementia care by teaching behavioral management skills and caregiver coping strategies, allowing patients to stay at home and delay institutionalization.6,11,12 Clinicians underuse available resources and do not incorporate them in their patient care.10 These community services benefit patients and caregivers and significantly improve the overall quality of care.6
Memory clinics have emerged to address these deficiencies when managing dementia.13 The most effective memory clinics maximize the use of specialists with different expertise in dementia care, particularly integrated programs where disciplines function together rather than independently.1,5,14 Systematic reviews and meta-analyses have documented the effectiveness of collaborative care management programs.11,12,15 Integration of dementia care management is associated with earlier diagnosis and interventions, decreased functional and cognitive symptom severity, decreased or delayed institutionalization, improved quality of life for patients and caregivers, enhanced overall quality of care and cost-effectiveness, and better integration of community services.11,12,14-19 In these programs, designating a dementia care manager (DCM) as the patient’s advocate facilitates the integrated structure, increases the quality of care, helps caregivers, facilitates adherence to dementia practice guidelines, and prevents behavioral and psychological symptoms of dementia (BPSD).1,6,11,12,20,21
The best interprofessional model for dementia care might be the transdisciplinary model that includes a DCM. To meet the specific demands of dementia care, there must be a high level of interprofessional collaboration rather than multiple health care professionals (HCPs) delivering care in isolation—an approach that is time consuming and often difficult to implement.22 Whereas multidisciplinary care refers to delivery of parallel services and interdisciplinary care implies a joint formulation, transdisciplinary care aims to maximize integration of HCPs and their specific expertise and contributions through interactions and discussions that deliver focused input to the lead physician. The transdisciplinary model addresses needs that often are missed and can minimize disparities in the quality of dementia care.23 A DCM is an integral part of our program, facilitating understanding and implementation of the final care plan and providing long-term follow-up and care. We outline a conference-centered transdisciplinary dementia care model with a social worker as DCM (SW-DCM) at our VA medical center.
Program Description
In 2020, the VA Greater Los Angeles Healthcare System (VAGLAHS) in California established a multispecialty clinic dedicated to evaluation and treatment of veterans with memory and neurocognitive disorders and to provide support for their caregivers and families. With the agreement of leadership in mental health, neurology, and geriatrics services on the importance of collaboration for dementia care, the psychiatry and neurology services created a joint Memory and Neurobehavior Clinic, which completed its first 2 years of operation as a full-day program. In recent months, the clinic has scheduled 24 veterans per day, approximately 50% new evaluations and 50% follow-up patients, with wait times of < 2 months. There is a mean of 12 intake or lead physicians who could attend sessions in the morning, afternoon, or both. The general clinic flow consists of a 2-hour intake evaluation of new referrals by the lead physician followed by a clinic conference with transdisciplinary discussion. The DCM then follows up with the veteran/caregiver presenting a final care plan individualized to the veterans, caregivers, and families.
The Memory and Neurobehavior team includes behavioral neurologists, geriatric psychiatrists, neuropsychologists, geriatric fellows, advanced clinical nurses, and social workers who function as the DCM (Table 1).
Procedures
Before the office visit, the coordinating geriatric psychiatrist triages veterans to neurology, psychiatry, or geriatric physicians based on the clinical presentation, history of neurologic signs or symptoms, BPSD or psychiatric history, functional decline, or comorbid medical illnesses. Although veterans often have overlapping concerns, the triage process aims to coordinate the intake evaluations with the most indicated and available specialist with the intention to notify the other specialists during the transdisciplinary conference.
Referrals to the program occur from many sources, notably from primary care (70.8%), mental health (16.7%), and specialty clinics (12.5%). The clinic also receives referrals from the affiliated Veterans Cognitive Assessment and Management Program, which provides dementia evaluation and support via telehealth screening. This VAGLAHS program services a diverse population of veterans: 87% male; 43% aged > 65 years (75% in our clinic); 51% non-Hispanic White; 19% non-Hispanic African American; 16% Hispanic; 4% Asian; and 1% Native American. This population receives care at regional VA medical centers and community-based outpatient clinics over a wide geographic service area.
The initial standardized assessments by intake or lead physicians includes mental status screening with the Montreal Cognitive Assessment (with certified clinicians), the Neurobehavioral Status Examination for a more detailed assessment of cognitive domains, the Columbia-Suicide Severity Rating Scale, the Patient Health Questionnaire for depression screening, and assessment for impairments in instrumental or basic activities of daily living. This initial evaluation aims to apply clinical guidelines and diagnostic criteria for the differential diagnosis of neurocognitive disorders, determine eligibility for cognitive-enhancing medications and techniques, assess for BPSD and the need for nonpharmacologic or pharmacologic interventions, determine functional status, and evaluate the need for supervision, safety concerns, and evidence of neglect or abuse.
As part of its mission, the clinic is charged with implementing the VA Dementia System of Care (DSOC). The stated goals of the DSOC are to provide individualized person-centered dementia care to help veterans experiencing dementia and their caregivers maintain a positive and optimal quality of life and create an environment where VA medical center staff understand the health care needs of veterans with dementia and their caregivers’ role. As part of this initiative, the clinic includes (1) coordination of care through a SW-DCM; (2)
Transdisciplinary Conference
Clinic conferences are held after the veterans are seen. Staff gather to discuss the patient and review management. All team members are present, as well as the head of the clinical clerical staff who can facilitate appointments, make lobby and wait times more bearable for our patients and caregivers, and help manage emergencies. Although this is an in-person conference, the COVID-19 pandemic has allowed us to include staff who screen at remote sites via videoconferencing, similar to other VA programs.24 The Memory and Neurobehavior Clinic has two ≤ 90-minute conferences daily. The lead physicians and their senior attendings present the new intake evaluations (4-6 at each conference session) with a preliminary formulation and questions for discussion. The moderator solicits contributions from the different disciplines, going from one to the next and recording their responses for each veteran. Further specialists are available for consultation through the conference mechanism if necessary. The final assessment is reviewed, a diagnosis is established, and a tailored, individualized care plan for adjusting or optimizing the veteran’s care is presented to the lead physician who makes the final determination. At the close of the conference, the team’s discussion is recorded along with the lead physician’s original detailed intake evaluation. Currently, the records go into the Computerized Patient Record System, but we are making plans to transition to Cerner as it is implemented.
During the discussion, team members review several areas of consideration. If there is neuroimaging, neurologists review the images projected on a large computer screen. Team members also will assess for the need to obtain biomarker studies, such as blood, cerebrospinal fluid, or positron emission tomography. Psychiatrists could review management of BPSD and use of psychotropic agents, and neuropsychologists might consider the need for more precise cognitive testing and whether a capacity assessment is indicated. Social work might bring up the need for a durable power of attorney as well as applicable caregiver and community resources. Geriatric medicine and nursing could provide input into medical management and care and the ability of veterans and caregivers to follow the prescribed regimen. Further areas of discussion include driving safety and restrictions on driving (as required in California) and the presence of guns in the home. Finally, brief education is provided in short 10-to-15-minute lectures covering pertinent topics so staff remain up-to-date in this changing field.
Postconference Continuity
After the conference, the SW-DCM continues to provide support throughout the disease course, helping veterans and their caregivers understand and follow through on the team’s recommendations. The SW-DCM, who is experienced and trained in case management, forms an ongoing relationship with the veterans and their caregivers and remains an advocate for their care. The SW-DCM communicates the final plan by phone and, when necessary, requests the lead physician to call to clarify any poorly understood or technical aspects of the care plan. About 50% of our veterans—primarily those who do not have a neurocognitive disorder or have mild cognitive impairment—return to their PCPs with our care plan consultation; about 25% are already enrolled in geriatric and other programs with long-term follow-up. The assigned SW-DCM follows up with the remaining veterans and caregivers regularly by phone, facilitates communication with other team members, and endeavors to assure postvisit continuity of care and support during advancing stages of the disease. In addition, the SW-DCM can provide supportive counseling and psychotherapy for stressed caregivers, refer to support groups and cognitive rehabilitation programs, and help develop long-term goals and consideration for supervised living environments. The nurse specialist participates with follow-up calls regarding medications and scheduled tests and appointments, clearing up confusion about instructions, avoiding medication errors, and providing education in dementia care. Both social worker and nurse are present throughout the week, reachable by phone, and, in turn, able to contact the clinic physicians for veterans’ needs.
Discussion
Because of the heterogenous medical and psychosocial needs of veterans with dementia and their caregivers, a transdisciplinary team with a dedicated DCM might offer the most effective and efficient model for dementia care. We present a transdisciplinary program that incorporates dementia specialists in a single evaluation by maximizing their time through a conference-centered program. Our program involves neurologists, psychiatrists, geriatricians, psychologists, nurses, and social workers collaborating and communicating to enact effective dementia care. It further meets the goals of the VA-DSOC in implementing individualized patient and caregiver care.
This transdisciplinary model addresses a number of issues, starting with the differential diagnosis of underlying neurologic conditions. Within the transdisciplinary team, the neurologist can provide specific insights into any neurologic findings and illnesses, such as Alzheimer disease and other neurodegenerative dementias, vascular dementia syndromes, normal pressure hydrocephalus, Creutzfeldt-Jakob disease, neurosyphilis, and others. Most veterans with dementia experience BPSD at some point during of their illness. The psychiatrists on the transdisciplinary team can maximize management of BPSD with nonpharmacologic interventions and the fewest and least aversive psychoactive medications. Our program also addresses the need for more precise cognitive evaluation. Neuropsychologists are present and available for administrating neuropsychologic tests and interpreting cognitive performance and any earlier neuropsychologic testing. This model also cares for the caregivers and assesses their needs. The social worker—as well as other members of the team—can provide caregivers with strategies for coping with disruptive and other behaviors related to dementia, counsel them on how to manage the veteran’s functional decline, and aid in establishing a safe living space. Because the social worker serves as a DCM, these coping and adjustment questions occupy significant clinical attention between appointments. This transdisciplinary model places the patient’s illness in the context of their functional status, diagnoses, and medications. The team geriatrician and the nurse specialist are indispensable resources. The clinic conference provides a teaching venue for staff and trainees and a mechanism to discuss new developments in dementia care, such as the increasing need to assess individuals with mild cognitive impairment.25 This model depends on the DCM’s invaluable role in ensuring implementation of the dementia care plan and continuity of care.
Conclusions
We describe effective dementia care with a transdisciplinary team in a conference setting and with the participation of a dedicated DCM.5 To date, this program appears to be an efficient, sustainable application of the limited resources allocated to dementia care. Nevertheless, we are collecting data to compare with performance measures, track use, and assess the programs effects on continuity of care. We look forward to presenting metrics from our program that show improvement in the health care for veterans experiencing a devastating and increasingly common disorder.
1. 2022 Alzheimer’s disease facts and figures. Alzheimers Dement. 2022;18(4):700-789. doi:10.1002/alz.12638
2. National Center for Veterans Analysis and Statistics. Profile of veterans: 2016. Accessed October 12, 2022. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2016.pdf
3. Chodosh J, Sultzer DL, Lee ML, et al. Memory impairment among primary care veterans. Aging Ment Health. 2007;11(4):444-450. doi:10.1080/13607860601086272
4. Kennedy E, Panahi S, Stewart IJ, et al. Traumatic brain injury and early onset dementia in post 9-11 veterans. Brain Inj. 2022;36(5):620-627. doi:10.1080/02699052.2022.20338465. Heintz H, Monette P, Epstein-Lubow G, Smith L, Rowlett S, Forester BP. Emerging collaborative care models for dementia care in the primary care setting: a narrative review. Am J Geriatr Psychiatry. 2020;28(3):320-330. doi:10.1016/j.jagp.2019.07.015
6. Reuben DB, Evertson LC, Wenger NS, et al. The University of California at Los Angeles Alzheimer’s and Dementia Care program for comprehensive, coordinated, patient-centered care: preliminary data. J Am Geriatr Soc. 2013;61(12):2214-2218. doi:10.1111/jgs.12562
7. Apesoa-Varano EC, Barker JC, Hinton L. Curing and caring: the work of primary care physicians with dementia patients. Qual Health Res. 2011;21(11):1469-1483. doi:10.1177/1049732311412788
8. Creavin ST, Noel-Storr AH, Langdon RJ, et al. Clinical judgement by primary care physicians for the diagnosis of all-cause dementia or cognitive impairment in symptomatic people. Cochrane Database Syst Rev. 2022;6:CD012558. doi:10.1002/14651858.CD012558.pub2
9. Sivananthan SN, Puyat JH, McGrail KM. Variations in self-reported practice of physicians providing clinical care to individuals with dementia: a systematic review. J Am Geriatr Soc. 2013;61(8):1277-1285. doi:10.1111/jgs.12368
10. Rosen CS, Chow HC, Greenbaum MA, et al. How well are clinicians following dementia practice guidelines? Alzheimer Dis Assoc Disord. 2002;16(1):15-23. doi:10.1097/00002093-200201000-00003
11. Reilly S, Miranda-Castillo C, Malouf R, et al. Case management approaches to home support for people with dementia. Cochrane Database Syst Rev. 2015;1:CD008345. doi:10.1002/14651858.CD008345.pub2
12. Tam-Tham H, Cepoiu-Martin M, Ronksley PE, Maxwell CJ, Hemmelgarn BR. Dementia case management and risk of long-term care placement: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2013;28(9):889-902. doi:10.1002/gps.3906
13. Jolley D, Benbow SM, Grizzell M. Memory clinics. Postgrad Med J. 2006;82(965):199-206. doi:10.1136/pgmj.2005.040592
14. Muhlichen F, Michalowsky B, Radke A, et al. Tasks and activities of an effective collaborative dementia care management program in German primary care. J Alzheimers Dis. 2022;87(4):1615-1625. doi:10.3233/JAD-215656
15. Somme D, Trouve H, Drame M, Gagnon D, Couturier Y, Saint-Jean O. Analysis of case management programs for patients with dementia: a systematic review. Alzheimers Dement. 2012;8(5):426-436. doi:10.1016/j.jalz.2011.06.004
16. Ramakers IH, Verhey FR. Development of memory clinics in the Netherlands: 1998 to 2009. Aging Ment Health. 2011;15(1):34-39. doi:10.1080/13607863.2010.519321
17. LaMantia MA, Alder CA, Callahan CM, et al. The aging brain care medical home: preliminary data. J Am Geriatr Soc. 2015;63(6):1209-1213. doi:10.1111/jgs.13447
18. Rubinsztein JS, van Rensburg MJ, Al-Salihy Z, et al. A memory clinic v. traditional community mental health team service: comparison of costs and quality. BJPsych Bull. 2015;39(1):6-11. doi:10.1192/pb.bp.113.044263
19. Lee L, Hillier LM, Harvey D. Integrating community services into primary care: improving the quality of dementia care. Neurodegener Dis Manag. 2014;4(1):11-21. doi:10.2217/nmt.13.72
20. Bass DM, Judge KS, Snow AL, et al. Caregiver outcomes of partners in dementia care: effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc. 2013;61(8):1377-1386. doi:10.1111/jgs.12362
21. Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148-2157. doi:10.1001/jama.295.18.2148
22. Leggett A, Connell C, Dubin L, et al. Dementia care across a tertiary care health system: what exists now and what needs to change. J Am Med Dir Assoc. 2019;20(10):1307-12 e1. doi:10.1016/j.jamda.2019.04.006
23. Brown AF, Vassar SD, Connor KI, Vickrey BG. Collaborative care management reduces disparities in dementia care quality for caregivers with less education. J Am Geriatr Soc. 2013;61(2):243-251. doi:10.1111/jgs.12079
24. Powers BB, Homer MC, Morone N, Edmonds N, Rossi MI. Creation of an interprofessional teledementia clinic for rural veterans: preliminary data. J Am Geriatr Soc. 2017;65(5):1092-1099. doi:10.1111/jgs.14839
25. Galvin JE, Aisen P, Langbaum JB, et al. Early stages of Alzheimer’s Disease: evolving the care team for optimal patient management. Front Neurol. 2020;11:592302. doi:10.3389/fneur.2020.592302
1. 2022 Alzheimer’s disease facts and figures. Alzheimers Dement. 2022;18(4):700-789. doi:10.1002/alz.12638
2. National Center for Veterans Analysis and Statistics. Profile of veterans: 2016. Accessed October 12, 2022. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2016.pdf
3. Chodosh J, Sultzer DL, Lee ML, et al. Memory impairment among primary care veterans. Aging Ment Health. 2007;11(4):444-450. doi:10.1080/13607860601086272
4. Kennedy E, Panahi S, Stewart IJ, et al. Traumatic brain injury and early onset dementia in post 9-11 veterans. Brain Inj. 2022;36(5):620-627. doi:10.1080/02699052.2022.20338465. Heintz H, Monette P, Epstein-Lubow G, Smith L, Rowlett S, Forester BP. Emerging collaborative care models for dementia care in the primary care setting: a narrative review. Am J Geriatr Psychiatry. 2020;28(3):320-330. doi:10.1016/j.jagp.2019.07.015
6. Reuben DB, Evertson LC, Wenger NS, et al. The University of California at Los Angeles Alzheimer’s and Dementia Care program for comprehensive, coordinated, patient-centered care: preliminary data. J Am Geriatr Soc. 2013;61(12):2214-2218. doi:10.1111/jgs.12562
7. Apesoa-Varano EC, Barker JC, Hinton L. Curing and caring: the work of primary care physicians with dementia patients. Qual Health Res. 2011;21(11):1469-1483. doi:10.1177/1049732311412788
8. Creavin ST, Noel-Storr AH, Langdon RJ, et al. Clinical judgement by primary care physicians for the diagnosis of all-cause dementia or cognitive impairment in symptomatic people. Cochrane Database Syst Rev. 2022;6:CD012558. doi:10.1002/14651858.CD012558.pub2
9. Sivananthan SN, Puyat JH, McGrail KM. Variations in self-reported practice of physicians providing clinical care to individuals with dementia: a systematic review. J Am Geriatr Soc. 2013;61(8):1277-1285. doi:10.1111/jgs.12368
10. Rosen CS, Chow HC, Greenbaum MA, et al. How well are clinicians following dementia practice guidelines? Alzheimer Dis Assoc Disord. 2002;16(1):15-23. doi:10.1097/00002093-200201000-00003
11. Reilly S, Miranda-Castillo C, Malouf R, et al. Case management approaches to home support for people with dementia. Cochrane Database Syst Rev. 2015;1:CD008345. doi:10.1002/14651858.CD008345.pub2
12. Tam-Tham H, Cepoiu-Martin M, Ronksley PE, Maxwell CJ, Hemmelgarn BR. Dementia case management and risk of long-term care placement: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2013;28(9):889-902. doi:10.1002/gps.3906
13. Jolley D, Benbow SM, Grizzell M. Memory clinics. Postgrad Med J. 2006;82(965):199-206. doi:10.1136/pgmj.2005.040592
14. Muhlichen F, Michalowsky B, Radke A, et al. Tasks and activities of an effective collaborative dementia care management program in German primary care. J Alzheimers Dis. 2022;87(4):1615-1625. doi:10.3233/JAD-215656
15. Somme D, Trouve H, Drame M, Gagnon D, Couturier Y, Saint-Jean O. Analysis of case management programs for patients with dementia: a systematic review. Alzheimers Dement. 2012;8(5):426-436. doi:10.1016/j.jalz.2011.06.004
16. Ramakers IH, Verhey FR. Development of memory clinics in the Netherlands: 1998 to 2009. Aging Ment Health. 2011;15(1):34-39. doi:10.1080/13607863.2010.519321
17. LaMantia MA, Alder CA, Callahan CM, et al. The aging brain care medical home: preliminary data. J Am Geriatr Soc. 2015;63(6):1209-1213. doi:10.1111/jgs.13447
18. Rubinsztein JS, van Rensburg MJ, Al-Salihy Z, et al. A memory clinic v. traditional community mental health team service: comparison of costs and quality. BJPsych Bull. 2015;39(1):6-11. doi:10.1192/pb.bp.113.044263
19. Lee L, Hillier LM, Harvey D. Integrating community services into primary care: improving the quality of dementia care. Neurodegener Dis Manag. 2014;4(1):11-21. doi:10.2217/nmt.13.72
20. Bass DM, Judge KS, Snow AL, et al. Caregiver outcomes of partners in dementia care: effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc. 2013;61(8):1377-1386. doi:10.1111/jgs.12362
21. Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148-2157. doi:10.1001/jama.295.18.2148
22. Leggett A, Connell C, Dubin L, et al. Dementia care across a tertiary care health system: what exists now and what needs to change. J Am Med Dir Assoc. 2019;20(10):1307-12 e1. doi:10.1016/j.jamda.2019.04.006
23. Brown AF, Vassar SD, Connor KI, Vickrey BG. Collaborative care management reduces disparities in dementia care quality for caregivers with less education. J Am Geriatr Soc. 2013;61(2):243-251. doi:10.1111/jgs.12079
24. Powers BB, Homer MC, Morone N, Edmonds N, Rossi MI. Creation of an interprofessional teledementia clinic for rural veterans: preliminary data. J Am Geriatr Soc. 2017;65(5):1092-1099. doi:10.1111/jgs.14839
25. Galvin JE, Aisen P, Langbaum JB, et al. Early stages of Alzheimer’s Disease: evolving the care team for optimal patient management. Front Neurol. 2020;11:592302. doi:10.3389/fneur.2020.592302