User login
Watch for failure to thrive in children with eosinophilic esophagitis
Be on the lookout for failure to thrive among pediatric patients with eosinophilic esophagitis, according to a letter to the editor of Annals of Allergy, Asthma & Immunology by Dr. Brenda Paquet of Sainte-Justine University Hospital Center in Montreal, and her colleagues.
These investigators reviewed charts for all children referred to their allergy clinic with a diagnosis of eosinophilic esophagitis (EoE) from 2004 to 2012. In addition to a standard clinical evaluation, patients had undergone a series of food and respiratory skin prick tests and food patch testing. Dr. Paquet and her associates also reviewed anthropometric measurements for the children and applied failure to thrive (FTT) criteria to all growth parameters available from birth.
Of 62 patients referred to the clinic, 15 (24%) met at least one of the six criteria for FTT, and more than half (n = 8) met at least two criteria. The most frequent FTT criterion met was a weight deceleration crossing two major percentile lines.
FTT should be assessed through different growth characteristics, such as weight, length, growth velocity, and body mass index, Dr Paquet and her associates wrote. “Because no single clinical feature can accurately predict it, it is important to maintain a high level of suspicion for FTT in children with a confirmed or suspected diagnosis of EoE, and inversely, EoE should be included in the differential diagnosis of FTT.” Although FTT usually resolves, it can persist in some children despite medical treatment, “highlighting the need for research and new therapies.”
Read the article in Annals of Allergy, Asthma & Immunology (2016 Jan. doi: 10.1016/j.anai.2015.09.015).
Be on the lookout for failure to thrive among pediatric patients with eosinophilic esophagitis, according to a letter to the editor of Annals of Allergy, Asthma & Immunology by Dr. Brenda Paquet of Sainte-Justine University Hospital Center in Montreal, and her colleagues.
These investigators reviewed charts for all children referred to their allergy clinic with a diagnosis of eosinophilic esophagitis (EoE) from 2004 to 2012. In addition to a standard clinical evaluation, patients had undergone a series of food and respiratory skin prick tests and food patch testing. Dr. Paquet and her associates also reviewed anthropometric measurements for the children and applied failure to thrive (FTT) criteria to all growth parameters available from birth.
Of 62 patients referred to the clinic, 15 (24%) met at least one of the six criteria for FTT, and more than half (n = 8) met at least two criteria. The most frequent FTT criterion met was a weight deceleration crossing two major percentile lines.
FTT should be assessed through different growth characteristics, such as weight, length, growth velocity, and body mass index, Dr Paquet and her associates wrote. “Because no single clinical feature can accurately predict it, it is important to maintain a high level of suspicion for FTT in children with a confirmed or suspected diagnosis of EoE, and inversely, EoE should be included in the differential diagnosis of FTT.” Although FTT usually resolves, it can persist in some children despite medical treatment, “highlighting the need for research and new therapies.”
Read the article in Annals of Allergy, Asthma & Immunology (2016 Jan. doi: 10.1016/j.anai.2015.09.015).
Be on the lookout for failure to thrive among pediatric patients with eosinophilic esophagitis, according to a letter to the editor of Annals of Allergy, Asthma & Immunology by Dr. Brenda Paquet of Sainte-Justine University Hospital Center in Montreal, and her colleagues.
These investigators reviewed charts for all children referred to their allergy clinic with a diagnosis of eosinophilic esophagitis (EoE) from 2004 to 2012. In addition to a standard clinical evaluation, patients had undergone a series of food and respiratory skin prick tests and food patch testing. Dr. Paquet and her associates also reviewed anthropometric measurements for the children and applied failure to thrive (FTT) criteria to all growth parameters available from birth.
Of 62 patients referred to the clinic, 15 (24%) met at least one of the six criteria for FTT, and more than half (n = 8) met at least two criteria. The most frequent FTT criterion met was a weight deceleration crossing two major percentile lines.
FTT should be assessed through different growth characteristics, such as weight, length, growth velocity, and body mass index, Dr Paquet and her associates wrote. “Because no single clinical feature can accurately predict it, it is important to maintain a high level of suspicion for FTT in children with a confirmed or suspected diagnosis of EoE, and inversely, EoE should be included in the differential diagnosis of FTT.” Although FTT usually resolves, it can persist in some children despite medical treatment, “highlighting the need for research and new therapies.”
Read the article in Annals of Allergy, Asthma & Immunology (2016 Jan. doi: 10.1016/j.anai.2015.09.015).
FROM ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
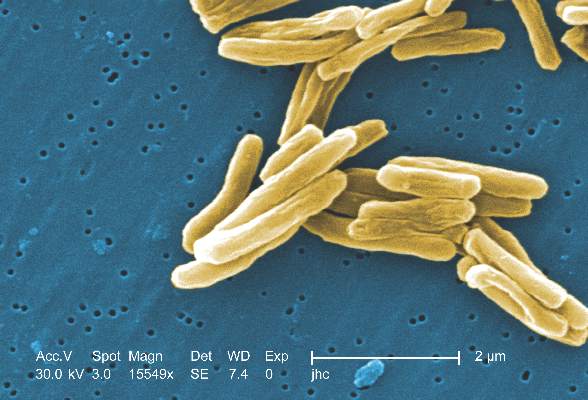
TB declines among foreign-born in U.S.
Tuberculosis rates among foreign-born people living in the United States have fallen by nearly 20%, according to a Centers for Disease Control and Prevention report in PLOS One.
From 2007 to 2011, there was an overall decline of 1,456 TB cases (–19.3%) among all foreign-born people in the United States, wrote Dr. Brian Baker of the CDC’s division of tuberculosis elimination, and colleagues. The largest relative declines in case counts were among those who emigrated within the past 3 years from Mexico (–56.1%, –270 cases); the Philippines (–52.5%, –180 cases), and India (–39.8%, –101 cases).
Factors contributing to the declines varied by country of origin.
Among recent entrants born in Mexico, 80.7% of the case count decline was attributable to a decrease in people from that country coming to the United States, while declines among recent entrants from the Philippines, India, Vietnam, and China were almost exclusively (95.5%-100%) the result of decreases in TB case rates.
TB rates also declined among foreign-born individuals who have been in the United States for 3 years or more, the investigators noted. There was an 8.9% decline in this population (–443 cases) that resulted entirely from a decrease in the TB case rate.
Strategies such as investment in overseas TB control, as well as expanded testing of high-risk subgroups living in the United States, “will be necessary to achieve further declines in TB morbidity among foreign-born persons,” the authors wrote.
Read the article in PLOS One (2016 Feb 10. doi: 10.1371/journal.pone.0147353)
Tuberculosis rates among foreign-born people living in the United States have fallen by nearly 20%, according to a Centers for Disease Control and Prevention report in PLOS One.
From 2007 to 2011, there was an overall decline of 1,456 TB cases (–19.3%) among all foreign-born people in the United States, wrote Dr. Brian Baker of the CDC’s division of tuberculosis elimination, and colleagues. The largest relative declines in case counts were among those who emigrated within the past 3 years from Mexico (–56.1%, –270 cases); the Philippines (–52.5%, –180 cases), and India (–39.8%, –101 cases).
Factors contributing to the declines varied by country of origin.
Among recent entrants born in Mexico, 80.7% of the case count decline was attributable to a decrease in people from that country coming to the United States, while declines among recent entrants from the Philippines, India, Vietnam, and China were almost exclusively (95.5%-100%) the result of decreases in TB case rates.
TB rates also declined among foreign-born individuals who have been in the United States for 3 years or more, the investigators noted. There was an 8.9% decline in this population (–443 cases) that resulted entirely from a decrease in the TB case rate.
Strategies such as investment in overseas TB control, as well as expanded testing of high-risk subgroups living in the United States, “will be necessary to achieve further declines in TB morbidity among foreign-born persons,” the authors wrote.
Read the article in PLOS One (2016 Feb 10. doi: 10.1371/journal.pone.0147353)
Tuberculosis rates among foreign-born people living in the United States have fallen by nearly 20%, according to a Centers for Disease Control and Prevention report in PLOS One.
From 2007 to 2011, there was an overall decline of 1,456 TB cases (–19.3%) among all foreign-born people in the United States, wrote Dr. Brian Baker of the CDC’s division of tuberculosis elimination, and colleagues. The largest relative declines in case counts were among those who emigrated within the past 3 years from Mexico (–56.1%, –270 cases); the Philippines (–52.5%, –180 cases), and India (–39.8%, –101 cases).
Factors contributing to the declines varied by country of origin.
Among recent entrants born in Mexico, 80.7% of the case count decline was attributable to a decrease in people from that country coming to the United States, while declines among recent entrants from the Philippines, India, Vietnam, and China were almost exclusively (95.5%-100%) the result of decreases in TB case rates.
TB rates also declined among foreign-born individuals who have been in the United States for 3 years or more, the investigators noted. There was an 8.9% decline in this population (–443 cases) that resulted entirely from a decrease in the TB case rate.
Strategies such as investment in overseas TB control, as well as expanded testing of high-risk subgroups living in the United States, “will be necessary to achieve further declines in TB morbidity among foreign-born persons,” the authors wrote.
Read the article in PLOS One (2016 Feb 10. doi: 10.1371/journal.pone.0147353)
FROM PLOS ONE
Comorbid personality, mood disorders tied to suicide attempts
The risk of suicide attempts is twice as likely among people with comorbid personality and mood disorders, an analysis of 597 participants in three prospective cohort studies shows.
In the analysis, Dr. Pekka Jylhä and associates found that having any personality disorder (PD) diagnosis increased the lifetime suicide attempt rate by 90% and suicide attempts during the follow-up periods by 102%.
Overall, 219 (36.7%) subjects had 718 lifetime suicide attempts, and 88 (14.7%) patients had 242 suicide attempts during the prospective follow-up periods of up to 5 years. During major depressive episodes, the presence of any PD increased the rate of a new suicide attempt by 39%. Having a cluster C disorder nearly doubled (90% increase) the rate of suicide attempts. Having an avoidant (n = 108) or dependent (n = 26) PD increased the rate of suicide attempts by 165% (95% confidence interval,104.2%-244.7%), reported Dr. Jylhä of Finland’s National Institute of Health and Welfare and the University of Helsinki.
The excess risk of suicide attempts “is mostly due to the fact that patients with comorbid PDs spend more time in depressive episodes than those without comorbid PDs,” the authors wrote. “This putative causal pathway has important clinical implications because major depressive episodes are treatable. However, direct risk-modifying effects of PDs are also likely to exist.”
Read the article in the Journal of Affective Disorders (2016 Jan 15;190:632-9).
The risk of suicide attempts is twice as likely among people with comorbid personality and mood disorders, an analysis of 597 participants in three prospective cohort studies shows.
In the analysis, Dr. Pekka Jylhä and associates found that having any personality disorder (PD) diagnosis increased the lifetime suicide attempt rate by 90% and suicide attempts during the follow-up periods by 102%.
Overall, 219 (36.7%) subjects had 718 lifetime suicide attempts, and 88 (14.7%) patients had 242 suicide attempts during the prospective follow-up periods of up to 5 years. During major depressive episodes, the presence of any PD increased the rate of a new suicide attempt by 39%. Having a cluster C disorder nearly doubled (90% increase) the rate of suicide attempts. Having an avoidant (n = 108) or dependent (n = 26) PD increased the rate of suicide attempts by 165% (95% confidence interval,104.2%-244.7%), reported Dr. Jylhä of Finland’s National Institute of Health and Welfare and the University of Helsinki.
The excess risk of suicide attempts “is mostly due to the fact that patients with comorbid PDs spend more time in depressive episodes than those without comorbid PDs,” the authors wrote. “This putative causal pathway has important clinical implications because major depressive episodes are treatable. However, direct risk-modifying effects of PDs are also likely to exist.”
Read the article in the Journal of Affective Disorders (2016 Jan 15;190:632-9).
The risk of suicide attempts is twice as likely among people with comorbid personality and mood disorders, an analysis of 597 participants in three prospective cohort studies shows.
In the analysis, Dr. Pekka Jylhä and associates found that having any personality disorder (PD) diagnosis increased the lifetime suicide attempt rate by 90% and suicide attempts during the follow-up periods by 102%.
Overall, 219 (36.7%) subjects had 718 lifetime suicide attempts, and 88 (14.7%) patients had 242 suicide attempts during the prospective follow-up periods of up to 5 years. During major depressive episodes, the presence of any PD increased the rate of a new suicide attempt by 39%. Having a cluster C disorder nearly doubled (90% increase) the rate of suicide attempts. Having an avoidant (n = 108) or dependent (n = 26) PD increased the rate of suicide attempts by 165% (95% confidence interval,104.2%-244.7%), reported Dr. Jylhä of Finland’s National Institute of Health and Welfare and the University of Helsinki.
The excess risk of suicide attempts “is mostly due to the fact that patients with comorbid PDs spend more time in depressive episodes than those without comorbid PDs,” the authors wrote. “This putative causal pathway has important clinical implications because major depressive episodes are treatable. However, direct risk-modifying effects of PDs are also likely to exist.”
Read the article in the Journal of Affective Disorders (2016 Jan 15;190:632-9).
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Prospective study supports hepatitis A vaccine schedule
Current vaccine recommendations for hepatitis A were endorsed by the findings of a prospective, randomized study of 183 Alaskan Native adolescents followed from infancy to age 15-16 years.
Study participants were randomly assigned to receive two doses of hepatitis A vaccine on three different schedules: at ages 6 and 12 months (group 1); at 12 and 18 months (group 2); or at 15 and 21 months (group 3). Each group was randomized according to maternal anti-HAV status.
Serum samples were collected from study participants at eight sampling time points from 1 month after the second vaccine until age 15-16 years. Those with anti-HAV levels of at least 20 mIU/mL were considered to be seropositive.
Seropositivity was high through age 10 years in all three groups – 100% in groups 2 and 3, and more than 90% in group 1. After age 10 years, however, seropositivity decreased. At age 15-16 years, 50%-75% of those on the 6 and 12 months’ schedule were seropositive as were 67%-87% of the other two groups whose mothers were anti-HAV-positive. Among those who were seropositive at age 15-16 years, 84% are predicted to remain so for at least another 30 years.
The findings that seropositivity was less frequent among those starting vaccination at age 6 months and among those whose mothers were antibody positive and who started vaccination at age 12 months or 15 months support current vaccine recommendations, Dr. Philip Spradling of the Centers for Disease Control and Prevention and his colleagues wrote.
Read the article in Hepatology (2015 Dec 5. doi: 10.1002/hep.28375).
Current vaccine recommendations for hepatitis A were endorsed by the findings of a prospective, randomized study of 183 Alaskan Native adolescents followed from infancy to age 15-16 years.
Study participants were randomly assigned to receive two doses of hepatitis A vaccine on three different schedules: at ages 6 and 12 months (group 1); at 12 and 18 months (group 2); or at 15 and 21 months (group 3). Each group was randomized according to maternal anti-HAV status.
Serum samples were collected from study participants at eight sampling time points from 1 month after the second vaccine until age 15-16 years. Those with anti-HAV levels of at least 20 mIU/mL were considered to be seropositive.
Seropositivity was high through age 10 years in all three groups – 100% in groups 2 and 3, and more than 90% in group 1. After age 10 years, however, seropositivity decreased. At age 15-16 years, 50%-75% of those on the 6 and 12 months’ schedule were seropositive as were 67%-87% of the other two groups whose mothers were anti-HAV-positive. Among those who were seropositive at age 15-16 years, 84% are predicted to remain so for at least another 30 years.
The findings that seropositivity was less frequent among those starting vaccination at age 6 months and among those whose mothers were antibody positive and who started vaccination at age 12 months or 15 months support current vaccine recommendations, Dr. Philip Spradling of the Centers for Disease Control and Prevention and his colleagues wrote.
Read the article in Hepatology (2015 Dec 5. doi: 10.1002/hep.28375).
Current vaccine recommendations for hepatitis A were endorsed by the findings of a prospective, randomized study of 183 Alaskan Native adolescents followed from infancy to age 15-16 years.
Study participants were randomly assigned to receive two doses of hepatitis A vaccine on three different schedules: at ages 6 and 12 months (group 1); at 12 and 18 months (group 2); or at 15 and 21 months (group 3). Each group was randomized according to maternal anti-HAV status.
Serum samples were collected from study participants at eight sampling time points from 1 month after the second vaccine until age 15-16 years. Those with anti-HAV levels of at least 20 mIU/mL were considered to be seropositive.
Seropositivity was high through age 10 years in all three groups – 100% in groups 2 and 3, and more than 90% in group 1. After age 10 years, however, seropositivity decreased. At age 15-16 years, 50%-75% of those on the 6 and 12 months’ schedule were seropositive as were 67%-87% of the other two groups whose mothers were anti-HAV-positive. Among those who were seropositive at age 15-16 years, 84% are predicted to remain so for at least another 30 years.
The findings that seropositivity was less frequent among those starting vaccination at age 6 months and among those whose mothers were antibody positive and who started vaccination at age 12 months or 15 months support current vaccine recommendations, Dr. Philip Spradling of the Centers for Disease Control and Prevention and his colleagues wrote.
Read the article in Hepatology (2015 Dec 5. doi: 10.1002/hep.28375).
FROM HEPATOLOGY
Cortical atrophy, lesion burden in MS linked to Epstein-Barr virus
Humoral response to Epstein-Barr virus (EBV) antigens is associated with more advanced cortical atrophy, accumulation of chronic T1 black holes, and focal white matter lesions in patients with multiple sclerosis, Dr. Robert Zivadinov of the State University of New York, Buffalo, and his colleagues reported in Neurology.
Researchers enrolled 846 participants for the study, including 539 patients with MS (369 with relapsing-remitting MS, 135 with secondary progressive MS, and 35 with primary progressive MS); 66 patients with clinically isolated syndrome (CIS); 63 patients with other neurologic diseases (OND); and 178 healthy controls. They used 3T MRI to scan participants’ brains and evaluated serum samples for IgG antibodies against EBV viral capsid antigen (VCA) and EBV nuclear antigen-1 (EBNA-1), dividing the group into quartiles based on their responses.
More than 30% of patients with MS and CIS presented with the highest quartile of anti–EBV-VCA and anti–EBNA-1 status, compared with 10% or fewer of healthy controls (P less than .001). The figures were 9 (14.3%) and 7 (12.3%) for patients with OND. Patients with MS with the highest quartile of anti–EBV-VCA showed significantly increased T2 lesion volume (P = .001), T1 lesion number (P = .002), and T1 lesion volume (P = .04), as well as decreased gray matter (P = .041) and cortical volumes (P = .043), compared with patients with MS in lower quartiles.
“The results provide evidence for further research aimed at modulating the response of patients with MS to these viruses via drug and vaccine strategies,” the authors wrote.
Read the article in Neurology (2016;3:e190. doi: 10.1212/NXI.0000000000000190).
Humoral response to Epstein-Barr virus (EBV) antigens is associated with more advanced cortical atrophy, accumulation of chronic T1 black holes, and focal white matter lesions in patients with multiple sclerosis, Dr. Robert Zivadinov of the State University of New York, Buffalo, and his colleagues reported in Neurology.
Researchers enrolled 846 participants for the study, including 539 patients with MS (369 with relapsing-remitting MS, 135 with secondary progressive MS, and 35 with primary progressive MS); 66 patients with clinically isolated syndrome (CIS); 63 patients with other neurologic diseases (OND); and 178 healthy controls. They used 3T MRI to scan participants’ brains and evaluated serum samples for IgG antibodies against EBV viral capsid antigen (VCA) and EBV nuclear antigen-1 (EBNA-1), dividing the group into quartiles based on their responses.
More than 30% of patients with MS and CIS presented with the highest quartile of anti–EBV-VCA and anti–EBNA-1 status, compared with 10% or fewer of healthy controls (P less than .001). The figures were 9 (14.3%) and 7 (12.3%) for patients with OND. Patients with MS with the highest quartile of anti–EBV-VCA showed significantly increased T2 lesion volume (P = .001), T1 lesion number (P = .002), and T1 lesion volume (P = .04), as well as decreased gray matter (P = .041) and cortical volumes (P = .043), compared with patients with MS in lower quartiles.
“The results provide evidence for further research aimed at modulating the response of patients with MS to these viruses via drug and vaccine strategies,” the authors wrote.
Read the article in Neurology (2016;3:e190. doi: 10.1212/NXI.0000000000000190).
Humoral response to Epstein-Barr virus (EBV) antigens is associated with more advanced cortical atrophy, accumulation of chronic T1 black holes, and focal white matter lesions in patients with multiple sclerosis, Dr. Robert Zivadinov of the State University of New York, Buffalo, and his colleagues reported in Neurology.
Researchers enrolled 846 participants for the study, including 539 patients with MS (369 with relapsing-remitting MS, 135 with secondary progressive MS, and 35 with primary progressive MS); 66 patients with clinically isolated syndrome (CIS); 63 patients with other neurologic diseases (OND); and 178 healthy controls. They used 3T MRI to scan participants’ brains and evaluated serum samples for IgG antibodies against EBV viral capsid antigen (VCA) and EBV nuclear antigen-1 (EBNA-1), dividing the group into quartiles based on their responses.
More than 30% of patients with MS and CIS presented with the highest quartile of anti–EBV-VCA and anti–EBNA-1 status, compared with 10% or fewer of healthy controls (P less than .001). The figures were 9 (14.3%) and 7 (12.3%) for patients with OND. Patients with MS with the highest quartile of anti–EBV-VCA showed significantly increased T2 lesion volume (P = .001), T1 lesion number (P = .002), and T1 lesion volume (P = .04), as well as decreased gray matter (P = .041) and cortical volumes (P = .043), compared with patients with MS in lower quartiles.
“The results provide evidence for further research aimed at modulating the response of patients with MS to these viruses via drug and vaccine strategies,” the authors wrote.
Read the article in Neurology (2016;3:e190. doi: 10.1212/NXI.0000000000000190).
FROM NEUROLOGY
New case of MS possibly related to tocilizumab
Canadian researchers have reported the first case of a patient developing multiple sclerosis (MS) while taking tocilizumab for rheumatoid arthritis.
A 48-year-old woman with a 20-year history of rheumatoid arthritis was seen for right hemisensory symptoms that began as numbness and pain on her right foot that spread to her trunk, arm, and face over a week, Dr. Philippe Beauchemin and Dr. Robert Carruthers of the University of British Columbia, Vancouver, noted in Multiple Sclerosis Journal. She had received many treatments for rheumatoid arthritis, including hydroxychloroquine, etanercept, and adalimumab. She also was on methotrexate, vitamin D, naproxen, and dexlansoprazole. MRI showed 20 lesions consistent with the diagnosis of MS. Doctors immediately discontinued tocilizumab and methotrexate. Three months later, another MRI showed two new lesions confirming MS diagnosis.
“There is absolutely no proof of a causal relationship between tocilizumab and MS in this patient, but it is also not excluded that tocilizumab might have caused secondary autoimmunity in CNS,” the authors wrote. The drug is in efficacy trials for patients with neuromyelitis optica spectrum disorder.
Two scenarios could explain this potential relationship, according to an accompanying commentary by Dr. Manuel Comabella of the Multiple Sclerosis Center of Catalonia, Vall d’Hebron University Hospital, Barcelona. The patient may have developed demyelinating lesions as a consequence of previous exposure to anti-TNF agents, and MS was later precipitated by treatment with tocilizumab; or that the drug itself can trigger a demyelinating disorder. “IL-6 may have immunosuppressive properties … that when absent by the effect of anti-IL6 agents, predisposes the individual to demyelinating conditions.”
Read the article in Multiple Sclerosis Journal (doi: 10:1177/1352458515623862).
Canadian researchers have reported the first case of a patient developing multiple sclerosis (MS) while taking tocilizumab for rheumatoid arthritis.
A 48-year-old woman with a 20-year history of rheumatoid arthritis was seen for right hemisensory symptoms that began as numbness and pain on her right foot that spread to her trunk, arm, and face over a week, Dr. Philippe Beauchemin and Dr. Robert Carruthers of the University of British Columbia, Vancouver, noted in Multiple Sclerosis Journal. She had received many treatments for rheumatoid arthritis, including hydroxychloroquine, etanercept, and adalimumab. She also was on methotrexate, vitamin D, naproxen, and dexlansoprazole. MRI showed 20 lesions consistent with the diagnosis of MS. Doctors immediately discontinued tocilizumab and methotrexate. Three months later, another MRI showed two new lesions confirming MS diagnosis.
“There is absolutely no proof of a causal relationship between tocilizumab and MS in this patient, but it is also not excluded that tocilizumab might have caused secondary autoimmunity in CNS,” the authors wrote. The drug is in efficacy trials for patients with neuromyelitis optica spectrum disorder.
Two scenarios could explain this potential relationship, according to an accompanying commentary by Dr. Manuel Comabella of the Multiple Sclerosis Center of Catalonia, Vall d’Hebron University Hospital, Barcelona. The patient may have developed demyelinating lesions as a consequence of previous exposure to anti-TNF agents, and MS was later precipitated by treatment with tocilizumab; or that the drug itself can trigger a demyelinating disorder. “IL-6 may have immunosuppressive properties … that when absent by the effect of anti-IL6 agents, predisposes the individual to demyelinating conditions.”
Read the article in Multiple Sclerosis Journal (doi: 10:1177/1352458515623862).
Canadian researchers have reported the first case of a patient developing multiple sclerosis (MS) while taking tocilizumab for rheumatoid arthritis.
A 48-year-old woman with a 20-year history of rheumatoid arthritis was seen for right hemisensory symptoms that began as numbness and pain on her right foot that spread to her trunk, arm, and face over a week, Dr. Philippe Beauchemin and Dr. Robert Carruthers of the University of British Columbia, Vancouver, noted in Multiple Sclerosis Journal. She had received many treatments for rheumatoid arthritis, including hydroxychloroquine, etanercept, and adalimumab. She also was on methotrexate, vitamin D, naproxen, and dexlansoprazole. MRI showed 20 lesions consistent with the diagnosis of MS. Doctors immediately discontinued tocilizumab and methotrexate. Three months later, another MRI showed two new lesions confirming MS diagnosis.
“There is absolutely no proof of a causal relationship between tocilizumab and MS in this patient, but it is also not excluded that tocilizumab might have caused secondary autoimmunity in CNS,” the authors wrote. The drug is in efficacy trials for patients with neuromyelitis optica spectrum disorder.
Two scenarios could explain this potential relationship, according to an accompanying commentary by Dr. Manuel Comabella of the Multiple Sclerosis Center of Catalonia, Vall d’Hebron University Hospital, Barcelona. The patient may have developed demyelinating lesions as a consequence of previous exposure to anti-TNF agents, and MS was later precipitated by treatment with tocilizumab; or that the drug itself can trigger a demyelinating disorder. “IL-6 may have immunosuppressive properties … that when absent by the effect of anti-IL6 agents, predisposes the individual to demyelinating conditions.”
Read the article in Multiple Sclerosis Journal (doi: 10:1177/1352458515623862).
FROM MULTIPLE SCLEROSIS JOURNAL
Smartphones feasible modality for collecting data in bipolar disorders
Smartphone surveys of mood and social stress might be useful in identifying mental changes in bipolar disorder patients, according to a pilot feasibility study by Stefani Schwartz of the department of psychiatry at Pennsylvania State University, Hershey, and her associates.
Ten bipolar disorder patients and 10 healthy controls recruited for the study were given smartphones and asked to complete surveys of mood and social stress twice a day at random for 14 days. The surveys included a visual analog scale to record ratings of mood, energy, speed of thoughts, and impulsivity, in which participants could choose any point along a scale of 0-100 by moving a sliding marker; and a Likert scale to measure social stress. For this part, participants revealed whether they were with others and whether they would rather be alone.
Completion rates were similar among the groups: a median of 95% in the bipolar disorder group and 88% in the healthy control group (P = 0.68). Median scores of the 14-day mean mood and energy in the bipolar disorder group were significantly lower in the bipolar disorder group, while speed of thoughts, impulsivity, and social stress were not significantly different between the groups. Median scores of the 14-day range for mood, speed of thoughts, and impulsivity did differ from the healthy controls, while energy and social stress did not differ significantly.
Prolonged monitoring might be required to detect prodromal symptoms of an impending major episode among patients with bipolar disorder, the authors wrote. Also, the findings are preliminary in light of many factors, including the small sample. Nevertheless, the techniques used in this study “could be investigated in subjects in different treatment settings to explore the sensitivity of detection of changes in symptoms,” the investigators wrote.
Read the article in the Journal of Affective Disorders (http://dx.doi.org/10.1016/j.jad.2015.11.013).
Smartphone surveys of mood and social stress might be useful in identifying mental changes in bipolar disorder patients, according to a pilot feasibility study by Stefani Schwartz of the department of psychiatry at Pennsylvania State University, Hershey, and her associates.
Ten bipolar disorder patients and 10 healthy controls recruited for the study were given smartphones and asked to complete surveys of mood and social stress twice a day at random for 14 days. The surveys included a visual analog scale to record ratings of mood, energy, speed of thoughts, and impulsivity, in which participants could choose any point along a scale of 0-100 by moving a sliding marker; and a Likert scale to measure social stress. For this part, participants revealed whether they were with others and whether they would rather be alone.
Completion rates were similar among the groups: a median of 95% in the bipolar disorder group and 88% in the healthy control group (P = 0.68). Median scores of the 14-day mean mood and energy in the bipolar disorder group were significantly lower in the bipolar disorder group, while speed of thoughts, impulsivity, and social stress were not significantly different between the groups. Median scores of the 14-day range for mood, speed of thoughts, and impulsivity did differ from the healthy controls, while energy and social stress did not differ significantly.
Prolonged monitoring might be required to detect prodromal symptoms of an impending major episode among patients with bipolar disorder, the authors wrote. Also, the findings are preliminary in light of many factors, including the small sample. Nevertheless, the techniques used in this study “could be investigated in subjects in different treatment settings to explore the sensitivity of detection of changes in symptoms,” the investigators wrote.
Read the article in the Journal of Affective Disorders (http://dx.doi.org/10.1016/j.jad.2015.11.013).
Smartphone surveys of mood and social stress might be useful in identifying mental changes in bipolar disorder patients, according to a pilot feasibility study by Stefani Schwartz of the department of psychiatry at Pennsylvania State University, Hershey, and her associates.
Ten bipolar disorder patients and 10 healthy controls recruited for the study were given smartphones and asked to complete surveys of mood and social stress twice a day at random for 14 days. The surveys included a visual analog scale to record ratings of mood, energy, speed of thoughts, and impulsivity, in which participants could choose any point along a scale of 0-100 by moving a sliding marker; and a Likert scale to measure social stress. For this part, participants revealed whether they were with others and whether they would rather be alone.
Completion rates were similar among the groups: a median of 95% in the bipolar disorder group and 88% in the healthy control group (P = 0.68). Median scores of the 14-day mean mood and energy in the bipolar disorder group were significantly lower in the bipolar disorder group, while speed of thoughts, impulsivity, and social stress were not significantly different between the groups. Median scores of the 14-day range for mood, speed of thoughts, and impulsivity did differ from the healthy controls, while energy and social stress did not differ significantly.
Prolonged monitoring might be required to detect prodromal symptoms of an impending major episode among patients with bipolar disorder, the authors wrote. Also, the findings are preliminary in light of many factors, including the small sample. Nevertheless, the techniques used in this study “could be investigated in subjects in different treatment settings to explore the sensitivity of detection of changes in symptoms,” the investigators wrote.
Read the article in the Journal of Affective Disorders (http://dx.doi.org/10.1016/j.jad.2015.11.013).
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Positive music produces more negative emotions in bipolar
Patients with bipolar disorder might experience more complex negative emotions in response to positive music than typical adults, even when in a euthymic state, Dr. Sabine Choppin of the University of Rennes 1 (France) and colleagues reported.
Researchers recruited 21 patients with bipolar disorder in a euthymic phase and 21 matched healthy controls for the study. First, participants rated their emotional reactivity on two self-report scales: the Emotion Reactivity Scale (ERS) and the Multidimensional Assessment of Thymic States Scale (MAThyS). Next, they used headphones to listen to a series of 12 instrumental music excerpts lasting 45 seconds each with their eyes closed. After each musical selection, they were asked to rate how strongly they had experienced each of the nine emotional categories on the Geneva Emotional Music Scale: joy, sadness, tension, wonder, peacefulness, power, tenderness, nostalgia, and transcendence.
Statistical analyses showed that patients in the bipolar disorder group had a mean score of 41.2 on the ERS, compared with a mean score of 22.9 among healthy controls. In addition, bipolar disorder patients reported experiencing more tension and sadness than did healthy controls when listening to positive musical excerpts that had been classified as inducing joy and wonder.
“This finding tallies with the negative emotional bias displayed by depressed patients, who tend to experience more negative emotions than healthy controls,” the authors wrote. “Bipolar patients struggle so much to regulate their own positive emotions that it creates a chronic source of distress, which could be experienced as a negative emotion.”
Read the article in the Journal of Affective Disorders (2016 Feb;191:15-23. doi: 10.1016/j.jad.2015.10.063).
Patients with bipolar disorder might experience more complex negative emotions in response to positive music than typical adults, even when in a euthymic state, Dr. Sabine Choppin of the University of Rennes 1 (France) and colleagues reported.
Researchers recruited 21 patients with bipolar disorder in a euthymic phase and 21 matched healthy controls for the study. First, participants rated their emotional reactivity on two self-report scales: the Emotion Reactivity Scale (ERS) and the Multidimensional Assessment of Thymic States Scale (MAThyS). Next, they used headphones to listen to a series of 12 instrumental music excerpts lasting 45 seconds each with their eyes closed. After each musical selection, they were asked to rate how strongly they had experienced each of the nine emotional categories on the Geneva Emotional Music Scale: joy, sadness, tension, wonder, peacefulness, power, tenderness, nostalgia, and transcendence.
Statistical analyses showed that patients in the bipolar disorder group had a mean score of 41.2 on the ERS, compared with a mean score of 22.9 among healthy controls. In addition, bipolar disorder patients reported experiencing more tension and sadness than did healthy controls when listening to positive musical excerpts that had been classified as inducing joy and wonder.
“This finding tallies with the negative emotional bias displayed by depressed patients, who tend to experience more negative emotions than healthy controls,” the authors wrote. “Bipolar patients struggle so much to regulate their own positive emotions that it creates a chronic source of distress, which could be experienced as a negative emotion.”
Read the article in the Journal of Affective Disorders (2016 Feb;191:15-23. doi: 10.1016/j.jad.2015.10.063).
Patients with bipolar disorder might experience more complex negative emotions in response to positive music than typical adults, even when in a euthymic state, Dr. Sabine Choppin of the University of Rennes 1 (France) and colleagues reported.
Researchers recruited 21 patients with bipolar disorder in a euthymic phase and 21 matched healthy controls for the study. First, participants rated their emotional reactivity on two self-report scales: the Emotion Reactivity Scale (ERS) and the Multidimensional Assessment of Thymic States Scale (MAThyS). Next, they used headphones to listen to a series of 12 instrumental music excerpts lasting 45 seconds each with their eyes closed. After each musical selection, they were asked to rate how strongly they had experienced each of the nine emotional categories on the Geneva Emotional Music Scale: joy, sadness, tension, wonder, peacefulness, power, tenderness, nostalgia, and transcendence.
Statistical analyses showed that patients in the bipolar disorder group had a mean score of 41.2 on the ERS, compared with a mean score of 22.9 among healthy controls. In addition, bipolar disorder patients reported experiencing more tension and sadness than did healthy controls when listening to positive musical excerpts that had been classified as inducing joy and wonder.
“This finding tallies with the negative emotional bias displayed by depressed patients, who tend to experience more negative emotions than healthy controls,” the authors wrote. “Bipolar patients struggle so much to regulate their own positive emotions that it creates a chronic source of distress, which could be experienced as a negative emotion.”
Read the article in the Journal of Affective Disorders (2016 Feb;191:15-23. doi: 10.1016/j.jad.2015.10.063).
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Genetic differences may help predict progression of PsC to PsA
Dermatology researchers have uncovered differences in the genetic architecture of psoriatic arthritis (PsA) and cutaneous psoriasis (PsC).
Dr. Philip E. Stuart of the University of Michigan, Ann Arbor, and his colleagues from 32 institutions in the United States, Europe, and Canada, carried out a genome-wide association study (GWAS) of 1,430 patients with psoriatic arthritis and 1,417 healthy controls. They then combined results of their GWAS with five published studies of psoriasis associations (three GWASs and two targeted studies), comprising 3,061 psoriatic arthritis patients, 3,110 cutaneous-only psoriasis patients, and 9,273 psoriasis vulgaris patients, and 13,670 healthy controls of European descent.
The work, published in the American Journal of Human Genetics, identified five regions of significance in the PsA GWAS. These were all in known risk regions for PsA, with the strongest signals near HLA-B, IL12B, TRAF3IP2, TNIP1, and TYK2.
Looking across all studies, researchers detected 10 regions associated with PsA and 11 with PsC at genome-wide significance. Several of these association signals (IFNLR1, IFIH1, NFKBIA for PsA, and TJFRSF9, LCE3C/B, TRAF3IP2, IL23A, and NFKBIA for PsC) had not previously achieved such significance. Researchers also identified a genetic variant associated with psoriasis vulgaris (PsV) near CDKAL1, and other variants that were more strongly associated with either PsA or PsC.
“These results provide insights into the pathogenic similarities and differences between PsC and PsA,” the authors wrote. Identifying the causative variants driving the observed associations “will aid prediction and therapy of psoriasis and its cutaneous and joint manifestations.”
Read the article in the American Journal of Human Genetics (2015 Dec 3;97:816-36).
Dermatology researchers have uncovered differences in the genetic architecture of psoriatic arthritis (PsA) and cutaneous psoriasis (PsC).
Dr. Philip E. Stuart of the University of Michigan, Ann Arbor, and his colleagues from 32 institutions in the United States, Europe, and Canada, carried out a genome-wide association study (GWAS) of 1,430 patients with psoriatic arthritis and 1,417 healthy controls. They then combined results of their GWAS with five published studies of psoriasis associations (three GWASs and two targeted studies), comprising 3,061 psoriatic arthritis patients, 3,110 cutaneous-only psoriasis patients, and 9,273 psoriasis vulgaris patients, and 13,670 healthy controls of European descent.
The work, published in the American Journal of Human Genetics, identified five regions of significance in the PsA GWAS. These were all in known risk regions for PsA, with the strongest signals near HLA-B, IL12B, TRAF3IP2, TNIP1, and TYK2.
Looking across all studies, researchers detected 10 regions associated with PsA and 11 with PsC at genome-wide significance. Several of these association signals (IFNLR1, IFIH1, NFKBIA for PsA, and TJFRSF9, LCE3C/B, TRAF3IP2, IL23A, and NFKBIA for PsC) had not previously achieved such significance. Researchers also identified a genetic variant associated with psoriasis vulgaris (PsV) near CDKAL1, and other variants that were more strongly associated with either PsA or PsC.
“These results provide insights into the pathogenic similarities and differences between PsC and PsA,” the authors wrote. Identifying the causative variants driving the observed associations “will aid prediction and therapy of psoriasis and its cutaneous and joint manifestations.”
Read the article in the American Journal of Human Genetics (2015 Dec 3;97:816-36).
Dermatology researchers have uncovered differences in the genetic architecture of psoriatic arthritis (PsA) and cutaneous psoriasis (PsC).
Dr. Philip E. Stuart of the University of Michigan, Ann Arbor, and his colleagues from 32 institutions in the United States, Europe, and Canada, carried out a genome-wide association study (GWAS) of 1,430 patients with psoriatic arthritis and 1,417 healthy controls. They then combined results of their GWAS with five published studies of psoriasis associations (three GWASs and two targeted studies), comprising 3,061 psoriatic arthritis patients, 3,110 cutaneous-only psoriasis patients, and 9,273 psoriasis vulgaris patients, and 13,670 healthy controls of European descent.
The work, published in the American Journal of Human Genetics, identified five regions of significance in the PsA GWAS. These were all in known risk regions for PsA, with the strongest signals near HLA-B, IL12B, TRAF3IP2, TNIP1, and TYK2.
Looking across all studies, researchers detected 10 regions associated with PsA and 11 with PsC at genome-wide significance. Several of these association signals (IFNLR1, IFIH1, NFKBIA for PsA, and TJFRSF9, LCE3C/B, TRAF3IP2, IL23A, and NFKBIA for PsC) had not previously achieved such significance. Researchers also identified a genetic variant associated with psoriasis vulgaris (PsV) near CDKAL1, and other variants that were more strongly associated with either PsA or PsC.
“These results provide insights into the pathogenic similarities and differences between PsC and PsA,” the authors wrote. Identifying the causative variants driving the observed associations “will aid prediction and therapy of psoriasis and its cutaneous and joint manifestations.”
Read the article in the American Journal of Human Genetics (2015 Dec 3;97:816-36).
FROM AMERICAN JOURNAL OF HUMAN GENETICS
USPSTF continues to urge syphilis screening in high-risk groups
Men who have sex with men and people living with HIV are at the highest risk for contracting syphilis and should be screened for the infection, according to a draft recommendation from the U.S. Preventive Services Task Force.
The draft recommendation, released on Dec. 14, is consistent with the advice that the task force offered to clinicians in 2004. The recommendation applies to asymptomatic, nonpregnant adolescents and adults.
Clinicians also should consider other factors associated with increased rates of syphilis, including male sex combined with age younger than 29 years, race/ethnicity, geography, incarceration, and sex work, the task force wrote in the draft recommendation.
In 2013, prevalence rates of primary and secondary syphilis were 16.8 cases per 100,000 for blacks, 8.6 cases per 100,000 for Native Hawaiians/Pacific Islanders, 6.3 cases per 100,000 for Hispanics, 4.6 cases per 100,000 for American Indians/Alaska Natives, 3.0 cases per 100,000 for whites, and 2.5 cases per 100,000 for Asians. Geographically, the southern United States has the largest proportion of syphilis cases at 40%, while the case rate is highest in the West (6.8 cases per 100,000). There is also an increased prevalence of syphilis in metropolitan areas.
Syphilis rates in the United States have been increasing. In 2014, there were 19,999 cases of the earliest stages of syphilis, the highest number since 1994, according to the USPSTF.
“Overall, the USPSTF found convincing evidence that screening for syphilis infection in asymptomatic, nonpregnant persons who are at increased risk for infection provides substantial benefit. Accurate screening tests are available to identify syphilis infection in populations at increased risk,” the task force wrote. “Effective treatment with antibiotics can prevent progression to late-stage disease, with small associated harms, providing an overall substantial health benefit.”
The draft recommendation statement and draft evidence review are available at www.uspreventiveservicestaskforce.org. Public comments may be submitted online through Jan. 18.
The draft recommendation complements a 2009 statement in which the task force recommended screening for syphilis infection in all pregnant women.
Men who have sex with men and people living with HIV are at the highest risk for contracting syphilis and should be screened for the infection, according to a draft recommendation from the U.S. Preventive Services Task Force.
The draft recommendation, released on Dec. 14, is consistent with the advice that the task force offered to clinicians in 2004. The recommendation applies to asymptomatic, nonpregnant adolescents and adults.
Clinicians also should consider other factors associated with increased rates of syphilis, including male sex combined with age younger than 29 years, race/ethnicity, geography, incarceration, and sex work, the task force wrote in the draft recommendation.
In 2013, prevalence rates of primary and secondary syphilis were 16.8 cases per 100,000 for blacks, 8.6 cases per 100,000 for Native Hawaiians/Pacific Islanders, 6.3 cases per 100,000 for Hispanics, 4.6 cases per 100,000 for American Indians/Alaska Natives, 3.0 cases per 100,000 for whites, and 2.5 cases per 100,000 for Asians. Geographically, the southern United States has the largest proportion of syphilis cases at 40%, while the case rate is highest in the West (6.8 cases per 100,000). There is also an increased prevalence of syphilis in metropolitan areas.
Syphilis rates in the United States have been increasing. In 2014, there were 19,999 cases of the earliest stages of syphilis, the highest number since 1994, according to the USPSTF.
“Overall, the USPSTF found convincing evidence that screening for syphilis infection in asymptomatic, nonpregnant persons who are at increased risk for infection provides substantial benefit. Accurate screening tests are available to identify syphilis infection in populations at increased risk,” the task force wrote. “Effective treatment with antibiotics can prevent progression to late-stage disease, with small associated harms, providing an overall substantial health benefit.”
The draft recommendation statement and draft evidence review are available at www.uspreventiveservicestaskforce.org. Public comments may be submitted online through Jan. 18.
The draft recommendation complements a 2009 statement in which the task force recommended screening for syphilis infection in all pregnant women.
Men who have sex with men and people living with HIV are at the highest risk for contracting syphilis and should be screened for the infection, according to a draft recommendation from the U.S. Preventive Services Task Force.
The draft recommendation, released on Dec. 14, is consistent with the advice that the task force offered to clinicians in 2004. The recommendation applies to asymptomatic, nonpregnant adolescents and adults.
Clinicians also should consider other factors associated with increased rates of syphilis, including male sex combined with age younger than 29 years, race/ethnicity, geography, incarceration, and sex work, the task force wrote in the draft recommendation.
In 2013, prevalence rates of primary and secondary syphilis were 16.8 cases per 100,000 for blacks, 8.6 cases per 100,000 for Native Hawaiians/Pacific Islanders, 6.3 cases per 100,000 for Hispanics, 4.6 cases per 100,000 for American Indians/Alaska Natives, 3.0 cases per 100,000 for whites, and 2.5 cases per 100,000 for Asians. Geographically, the southern United States has the largest proportion of syphilis cases at 40%, while the case rate is highest in the West (6.8 cases per 100,000). There is also an increased prevalence of syphilis in metropolitan areas.
Syphilis rates in the United States have been increasing. In 2014, there were 19,999 cases of the earliest stages of syphilis, the highest number since 1994, according to the USPSTF.
“Overall, the USPSTF found convincing evidence that screening for syphilis infection in asymptomatic, nonpregnant persons who are at increased risk for infection provides substantial benefit. Accurate screening tests are available to identify syphilis infection in populations at increased risk,” the task force wrote. “Effective treatment with antibiotics can prevent progression to late-stage disease, with small associated harms, providing an overall substantial health benefit.”
The draft recommendation statement and draft evidence review are available at www.uspreventiveservicestaskforce.org. Public comments may be submitted online through Jan. 18.
The draft recommendation complements a 2009 statement in which the task force recommended screening for syphilis infection in all pregnant women.