User login
The 84-year-old state boxing champ: Bipolar disorder, or something else?
CASE Agitated, uncooperative, and irritable
Mr. X, age 84, presents to the emergency department with agitation, mania-like symptoms, and mood-congruent psychotic symptoms that started 2 weeks ago. Mr. X, who is accompanied by his wife, has no psychiatric history.
On examination, Mr. X is easily agitated and uncooperative. His speech is fast, but not pressured, with increased volume and tone. He states, “My mood is fantastic” with mood-congruent affect. His thought process reveals circumstantiality and loose association. Mr. X’s thought content includes flight of ideas and delusions of grandeur; he claims to be a state boxing champion and a psychologist. He also claims that he will run for Congress in the near future. He reports that he’s started knocking on his neighbors’ doors, pitched the idea to buy their house, and convinced them to vote for him as their congressman. He denies any suicidal or homicidal ideations. There is no evidence of perceptual disturbance. Mr. X undergoes a Mini-Mental State Examination (MMSE) and scores 26/30, which suggests no cognitive impairment. However, his insight and judgment are poor.
Mr. X’s physical examination is unremarkable. His laboratory workup includes a complete blood count, comprehensive metabolic panel, urinalysis, thyroid function test, vitamin B12 and folate levels, urine drug screen, and blood alcohol level. All results are within normal limits. He has no history of alcohol or recreational drug use as evident by the laboratory results and collateral information from his wife. Further, a non-contrast CT scan of his head shows no abnormality.
Approximately 1 month ago, Mr. X was diagnosed with restless leg syndrome (RLS). Mr. X’s medication regimen consists of gabapentin, 300 mg 3 times daily, prescribed years ago by his neurologist for neuropathic pain; and ropinirole, 3 mg/d, for RLS. His neurologist had prescribed him ropinirole, which was started at 1 mg/d and titrated to 3 mg/d within a 1-week span. Two weeks after Mr. X started this medication regimen, his wife reports that she noticed changes in his behavior, including severe agitation, irritability, delusions of grandeur, decreased need for sleep, and racing of thoughts.
[polldaddy:10417490]
The authors’ observations
Mr. X was diagnosed with medication (ropinirole)-induced bipolar and related disorder with mood-congruent psychotic features.
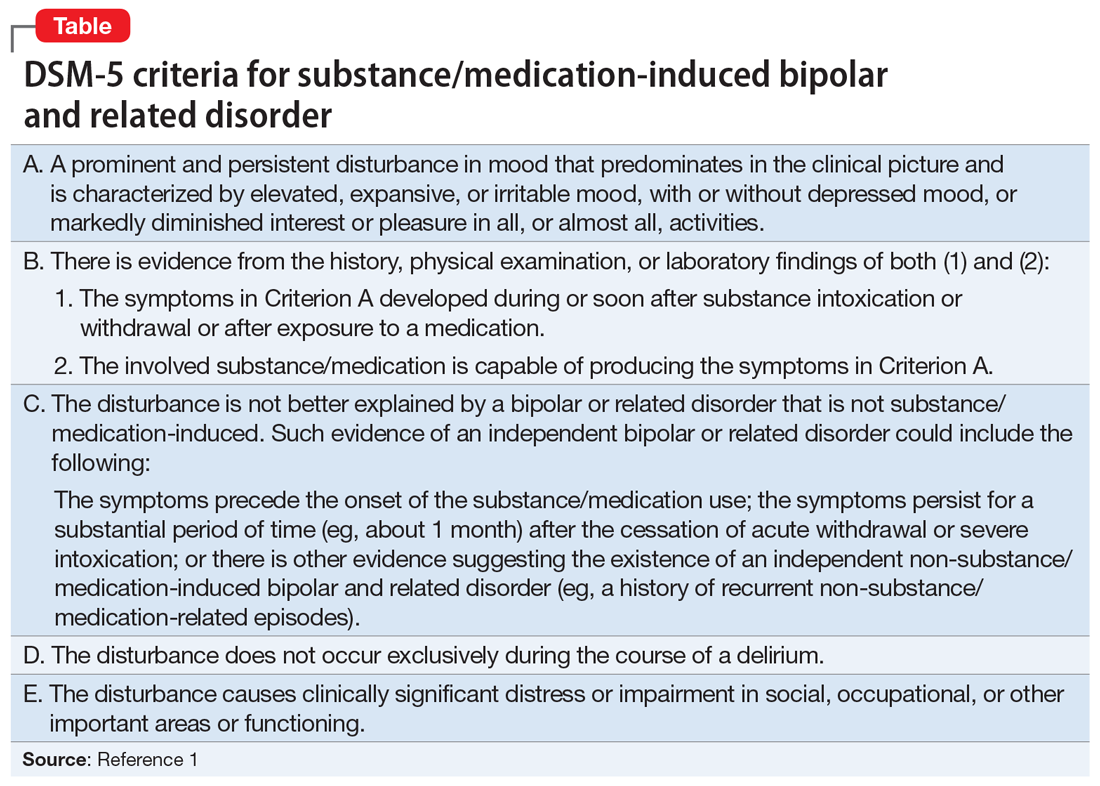
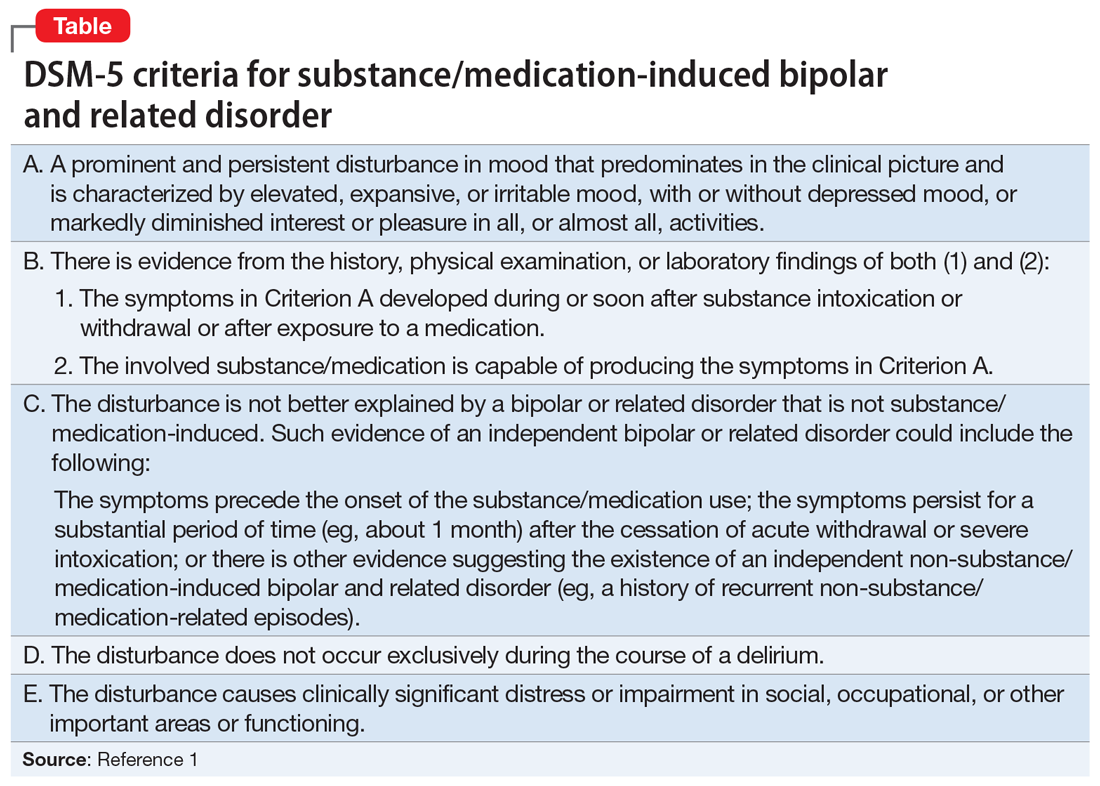
To determine this diagnosis, we initially considered Mr. X’s age and medical conditions, including stroke and space-occupying lesions of the brain. However, the laboratory and neuroimaging studies, which included a CT scan of the head and MRI of the brain, were negative. Next, because Mr. X had sudden onset manic symptoms after ropinirole was initiated, we considered the possibility of a substance/medication-induced bipolar and related disorder. Further, ropinirole is capable of producing the symptoms in criterion A of DSM-5 criteria for substance/medication-induced bipolar and related disorder. Mr. X met all DSM-5 criteria for substance/medication-induced bipolar and related disorder (Table1).
[polldaddy:10417494]
TREATMENT Medication adjustments and improvement
The admitting clinician discontinues ropinirole and initiates divalproex sodium, 500 mg twice a day. By Day 4, Mr. X shows significant improvement, including no irritable mood and regression of delusions of grandeur, and his sleep cycle returns to normal. At this time, the divalproex sodium is also discontinued.
Continue to: The authors' observations
The authors’ observations
Dopamine agonist agents are a standard treatment in the management of Parkinson’s disease and RLS.2-5 Ropinirole, a dopamine receptor agonist, has a high affinity for dopamine D2 and D3 receptor subtypes.4 Published reports have linked dopamine agonists to mania with psychotic features.6,7 In a study by Stoner et al,8 of 95 patients treated with ropinirole, 13 patients developed psychotic features that necessitated the use of antipsychotic medications or a lower dose of ropinirole.
The recommended starting dose for ropinirole is 0.25 mg/d. The dose can be increased to 0.5 mg in the next 2 days, and to 1 mg/d at the end of the first week.9 The mean effective daily dose is 2 mg/d, and maximum recommended dose is 4 mg/d.9 For Mr. X, ropinirole was quickly titrated to 3 mg/d over 1 week, which resulted in mania and psychosis. We suggest that when treating geriatric patients, clinicians should consider prescribing the lowest effective dose of psychotropic medications, such as ropinirole, to prevent adverse effects. Higher doses of dopamine agonists, especially in geriatric patients, increase the risk of common adverse effects, such as nausea (25% to 50%), headache (7% to 22%), fatigue (1% to 19%), dizziness (6% to 18%), and vomiting (5% to 11%).10 When prescribing dopamine agonists, clinicians should educate patients and their caregivers about the rare but potential risk of medication-induced mania and psychosis.
Mr. X’s case emphasizes the importance of a comprehensive psychiatric evaluation and medical workup to rule out a wide differential diagnosis when approaching new-onset mania and psychosis in geriatric patients.11 Our case contributes to the evidence that dopamine agonist medications are associated with mania and psychotic symptoms.
OUTCOME A return to baseline
On Day 12, Mr. X is discharged home in a stable condition. Two weeks later, at an outpatient follow-up visit, Mr. X is asymptomatic and has returned to his baseline functioning.
Bottom Line
When approaching new-onset mania and psychosis in geriatric patients, a comprehensive psychiatric evaluation and medical workup are necessary to rule out a wide differential diagnosis. Ropinirole use can lead to mania and psychotic symptoms, especially in geriatric patients. As should be done with all other dopaminergic agents, increase the dose of ropinirole with caution, and be vigilant for the emergence of signs of mania and/or psychosis.
Continue to: Related Resources
Related Resources
- Adabie A, Jackson JC, Torrence CL. Older-age bipolar disorder: A case series. Current Psychiatry. 2019;18(2):24-29.
- Chen P, Dols A, Rej S, et al. Update on the epidemiology, diagnosis, and treatment of mania in older-age bipolar disorder. Curr Psychiatry Rep. 2017;19(8):46.
Drug Brand Names
Divalproex sodium • Depakote
Gabapentin • Neurontin
Ropinirole • Requip
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Singh A, Althoff R, Martineau RJ, et al. Pramipexole, ropinirole, and mania in Parkinson’s disease. Am J Psychiatry. 2005;162(4):814-815.
3. Weiss HD, Pontone GM. Dopamine receptor agonist drugs and impulse control disorders. JAMA Intern Med. 2014;174(12):1935-1937.
4 Shill HA, Stacy M. Update on ropinirole in the treatment of Parkinson’s disease. Neuropsychiatr Dis Treat. 2009;5:33-36.
5. Borovac JA. Side effects of a dopamine agonist therapy for Parkinson’s disease: a mini-review of clinical pharmacology. Yale J Biol Med. 2016;89(1):37-47.
6. Yüksel RN, Elyas Kaya Z, Dilbaz N, et al. Cabergoline-induced manic episode: case report. Ther Adv Psychopharmacol. 2016;6(3):229-231.
7. Perea E, Robbins BV, Hutto B. Psychosis related to ropinirole. Am J Psychiatry. 2006;163(3):547-548.
8. Stoner SC, Dahmen MM, Makos M, et al. An exploratory retrospective evaluation of ropinirole-associated psychotic symptoms in an outpatient population treated for restless legs syndrome or Parkinson’s disease. Ann Pharmacother. 2009;43(9):1426-1432.
9. Trenkwalder C, Hening WA, Montagna P, et al. Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice. Mov Disord. 2008;23(16):2267-2302.
10. Garcia-Borreguero D, Kohnen R, Silber MH, et al. The long-term treatment of restless legs syndrome/Willis-Ekbom disease: evidence-based guidelines and clinical consensus best practice guidance: a report from the International Restless Legs Syndrome Study Group. Sleep Med. 2013;14(7):675-684.
11. Dols A, Beekman A. Older age bipolar disorder. Psychiatr Clin North Am. 2018;41(1):95-110.
CASE Agitated, uncooperative, and irritable
Mr. X, age 84, presents to the emergency department with agitation, mania-like symptoms, and mood-congruent psychotic symptoms that started 2 weeks ago. Mr. X, who is accompanied by his wife, has no psychiatric history.
On examination, Mr. X is easily agitated and uncooperative. His speech is fast, but not pressured, with increased volume and tone. He states, “My mood is fantastic” with mood-congruent affect. His thought process reveals circumstantiality and loose association. Mr. X’s thought content includes flight of ideas and delusions of grandeur; he claims to be a state boxing champion and a psychologist. He also claims that he will run for Congress in the near future. He reports that he’s started knocking on his neighbors’ doors, pitched the idea to buy their house, and convinced them to vote for him as their congressman. He denies any suicidal or homicidal ideations. There is no evidence of perceptual disturbance. Mr. X undergoes a Mini-Mental State Examination (MMSE) and scores 26/30, which suggests no cognitive impairment. However, his insight and judgment are poor.
Mr. X’s physical examination is unremarkable. His laboratory workup includes a complete blood count, comprehensive metabolic panel, urinalysis, thyroid function test, vitamin B12 and folate levels, urine drug screen, and blood alcohol level. All results are within normal limits. He has no history of alcohol or recreational drug use as evident by the laboratory results and collateral information from his wife. Further, a non-contrast CT scan of his head shows no abnormality.
Approximately 1 month ago, Mr. X was diagnosed with restless leg syndrome (RLS). Mr. X’s medication regimen consists of gabapentin, 300 mg 3 times daily, prescribed years ago by his neurologist for neuropathic pain; and ropinirole, 3 mg/d, for RLS. His neurologist had prescribed him ropinirole, which was started at 1 mg/d and titrated to 3 mg/d within a 1-week span. Two weeks after Mr. X started this medication regimen, his wife reports that she noticed changes in his behavior, including severe agitation, irritability, delusions of grandeur, decreased need for sleep, and racing of thoughts.
[polldaddy:10417490]
The authors’ observations
Mr. X was diagnosed with medication (ropinirole)-induced bipolar and related disorder with mood-congruent psychotic features.
To determine this diagnosis, we initially considered Mr. X’s age and medical conditions, including stroke and space-occupying lesions of the brain. However, the laboratory and neuroimaging studies, which included a CT scan of the head and MRI of the brain, were negative. Next, because Mr. X had sudden onset manic symptoms after ropinirole was initiated, we considered the possibility of a substance/medication-induced bipolar and related disorder. Further, ropinirole is capable of producing the symptoms in criterion A of DSM-5 criteria for substance/medication-induced bipolar and related disorder. Mr. X met all DSM-5 criteria for substance/medication-induced bipolar and related disorder (Table1).
[polldaddy:10417494]
TREATMENT Medication adjustments and improvement
The admitting clinician discontinues ropinirole and initiates divalproex sodium, 500 mg twice a day. By Day 4, Mr. X shows significant improvement, including no irritable mood and regression of delusions of grandeur, and his sleep cycle returns to normal. At this time, the divalproex sodium is also discontinued.
Continue to: The authors' observations
The authors’ observations
Dopamine agonist agents are a standard treatment in the management of Parkinson’s disease and RLS.2-5 Ropinirole, a dopamine receptor agonist, has a high affinity for dopamine D2 and D3 receptor subtypes.4 Published reports have linked dopamine agonists to mania with psychotic features.6,7 In a study by Stoner et al,8 of 95 patients treated with ropinirole, 13 patients developed psychotic features that necessitated the use of antipsychotic medications or a lower dose of ropinirole.
The recommended starting dose for ropinirole is 0.25 mg/d. The dose can be increased to 0.5 mg in the next 2 days, and to 1 mg/d at the end of the first week.9 The mean effective daily dose is 2 mg/d, and maximum recommended dose is 4 mg/d.9 For Mr. X, ropinirole was quickly titrated to 3 mg/d over 1 week, which resulted in mania and psychosis. We suggest that when treating geriatric patients, clinicians should consider prescribing the lowest effective dose of psychotropic medications, such as ropinirole, to prevent adverse effects. Higher doses of dopamine agonists, especially in geriatric patients, increase the risk of common adverse effects, such as nausea (25% to 50%), headache (7% to 22%), fatigue (1% to 19%), dizziness (6% to 18%), and vomiting (5% to 11%).10 When prescribing dopamine agonists, clinicians should educate patients and their caregivers about the rare but potential risk of medication-induced mania and psychosis.
Mr. X’s case emphasizes the importance of a comprehensive psychiatric evaluation and medical workup to rule out a wide differential diagnosis when approaching new-onset mania and psychosis in geriatric patients.11 Our case contributes to the evidence that dopamine agonist medications are associated with mania and psychotic symptoms.
OUTCOME A return to baseline
On Day 12, Mr. X is discharged home in a stable condition. Two weeks later, at an outpatient follow-up visit, Mr. X is asymptomatic and has returned to his baseline functioning.
Bottom Line
When approaching new-onset mania and psychosis in geriatric patients, a comprehensive psychiatric evaluation and medical workup are necessary to rule out a wide differential diagnosis. Ropinirole use can lead to mania and psychotic symptoms, especially in geriatric patients. As should be done with all other dopaminergic agents, increase the dose of ropinirole with caution, and be vigilant for the emergence of signs of mania and/or psychosis.
Continue to: Related Resources
Related Resources
- Adabie A, Jackson JC, Torrence CL. Older-age bipolar disorder: A case series. Current Psychiatry. 2019;18(2):24-29.
- Chen P, Dols A, Rej S, et al. Update on the epidemiology, diagnosis, and treatment of mania in older-age bipolar disorder. Curr Psychiatry Rep. 2017;19(8):46.
Drug Brand Names
Divalproex sodium • Depakote
Gabapentin • Neurontin
Ropinirole • Requip
CASE Agitated, uncooperative, and irritable
Mr. X, age 84, presents to the emergency department with agitation, mania-like symptoms, and mood-congruent psychotic symptoms that started 2 weeks ago. Mr. X, who is accompanied by his wife, has no psychiatric history.
On examination, Mr. X is easily agitated and uncooperative. His speech is fast, but not pressured, with increased volume and tone. He states, “My mood is fantastic” with mood-congruent affect. His thought process reveals circumstantiality and loose association. Mr. X’s thought content includes flight of ideas and delusions of grandeur; he claims to be a state boxing champion and a psychologist. He also claims that he will run for Congress in the near future. He reports that he’s started knocking on his neighbors’ doors, pitched the idea to buy their house, and convinced them to vote for him as their congressman. He denies any suicidal or homicidal ideations. There is no evidence of perceptual disturbance. Mr. X undergoes a Mini-Mental State Examination (MMSE) and scores 26/30, which suggests no cognitive impairment. However, his insight and judgment are poor.
Mr. X’s physical examination is unremarkable. His laboratory workup includes a complete blood count, comprehensive metabolic panel, urinalysis, thyroid function test, vitamin B12 and folate levels, urine drug screen, and blood alcohol level. All results are within normal limits. He has no history of alcohol or recreational drug use as evident by the laboratory results and collateral information from his wife. Further, a non-contrast CT scan of his head shows no abnormality.
Approximately 1 month ago, Mr. X was diagnosed with restless leg syndrome (RLS). Mr. X’s medication regimen consists of gabapentin, 300 mg 3 times daily, prescribed years ago by his neurologist for neuropathic pain; and ropinirole, 3 mg/d, for RLS. His neurologist had prescribed him ropinirole, which was started at 1 mg/d and titrated to 3 mg/d within a 1-week span. Two weeks after Mr. X started this medication regimen, his wife reports that she noticed changes in his behavior, including severe agitation, irritability, delusions of grandeur, decreased need for sleep, and racing of thoughts.
[polldaddy:10417490]
The authors’ observations
Mr. X was diagnosed with medication (ropinirole)-induced bipolar and related disorder with mood-congruent psychotic features.
To determine this diagnosis, we initially considered Mr. X’s age and medical conditions, including stroke and space-occupying lesions of the brain. However, the laboratory and neuroimaging studies, which included a CT scan of the head and MRI of the brain, were negative. Next, because Mr. X had sudden onset manic symptoms after ropinirole was initiated, we considered the possibility of a substance/medication-induced bipolar and related disorder. Further, ropinirole is capable of producing the symptoms in criterion A of DSM-5 criteria for substance/medication-induced bipolar and related disorder. Mr. X met all DSM-5 criteria for substance/medication-induced bipolar and related disorder (Table1).
[polldaddy:10417494]
TREATMENT Medication adjustments and improvement
The admitting clinician discontinues ropinirole and initiates divalproex sodium, 500 mg twice a day. By Day 4, Mr. X shows significant improvement, including no irritable mood and regression of delusions of grandeur, and his sleep cycle returns to normal. At this time, the divalproex sodium is also discontinued.
Continue to: The authors' observations
The authors’ observations
Dopamine agonist agents are a standard treatment in the management of Parkinson’s disease and RLS.2-5 Ropinirole, a dopamine receptor agonist, has a high affinity for dopamine D2 and D3 receptor subtypes.4 Published reports have linked dopamine agonists to mania with psychotic features.6,7 In a study by Stoner et al,8 of 95 patients treated with ropinirole, 13 patients developed psychotic features that necessitated the use of antipsychotic medications or a lower dose of ropinirole.
The recommended starting dose for ropinirole is 0.25 mg/d. The dose can be increased to 0.5 mg in the next 2 days, and to 1 mg/d at the end of the first week.9 The mean effective daily dose is 2 mg/d, and maximum recommended dose is 4 mg/d.9 For Mr. X, ropinirole was quickly titrated to 3 mg/d over 1 week, which resulted in mania and psychosis. We suggest that when treating geriatric patients, clinicians should consider prescribing the lowest effective dose of psychotropic medications, such as ropinirole, to prevent adverse effects. Higher doses of dopamine agonists, especially in geriatric patients, increase the risk of common adverse effects, such as nausea (25% to 50%), headache (7% to 22%), fatigue (1% to 19%), dizziness (6% to 18%), and vomiting (5% to 11%).10 When prescribing dopamine agonists, clinicians should educate patients and their caregivers about the rare but potential risk of medication-induced mania and psychosis.
Mr. X’s case emphasizes the importance of a comprehensive psychiatric evaluation and medical workup to rule out a wide differential diagnosis when approaching new-onset mania and psychosis in geriatric patients.11 Our case contributes to the evidence that dopamine agonist medications are associated with mania and psychotic symptoms.
OUTCOME A return to baseline
On Day 12, Mr. X is discharged home in a stable condition. Two weeks later, at an outpatient follow-up visit, Mr. X is asymptomatic and has returned to his baseline functioning.
Bottom Line
When approaching new-onset mania and psychosis in geriatric patients, a comprehensive psychiatric evaluation and medical workup are necessary to rule out a wide differential diagnosis. Ropinirole use can lead to mania and psychotic symptoms, especially in geriatric patients. As should be done with all other dopaminergic agents, increase the dose of ropinirole with caution, and be vigilant for the emergence of signs of mania and/or psychosis.
Continue to: Related Resources
Related Resources
- Adabie A, Jackson JC, Torrence CL. Older-age bipolar disorder: A case series. Current Psychiatry. 2019;18(2):24-29.
- Chen P, Dols A, Rej S, et al. Update on the epidemiology, diagnosis, and treatment of mania in older-age bipolar disorder. Curr Psychiatry Rep. 2017;19(8):46.
Drug Brand Names
Divalproex sodium • Depakote
Gabapentin • Neurontin
Ropinirole • Requip
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Singh A, Althoff R, Martineau RJ, et al. Pramipexole, ropinirole, and mania in Parkinson’s disease. Am J Psychiatry. 2005;162(4):814-815.
3. Weiss HD, Pontone GM. Dopamine receptor agonist drugs and impulse control disorders. JAMA Intern Med. 2014;174(12):1935-1937.
4 Shill HA, Stacy M. Update on ropinirole in the treatment of Parkinson’s disease. Neuropsychiatr Dis Treat. 2009;5:33-36.
5. Borovac JA. Side effects of a dopamine agonist therapy for Parkinson’s disease: a mini-review of clinical pharmacology. Yale J Biol Med. 2016;89(1):37-47.
6. Yüksel RN, Elyas Kaya Z, Dilbaz N, et al. Cabergoline-induced manic episode: case report. Ther Adv Psychopharmacol. 2016;6(3):229-231.
7. Perea E, Robbins BV, Hutto B. Psychosis related to ropinirole. Am J Psychiatry. 2006;163(3):547-548.
8. Stoner SC, Dahmen MM, Makos M, et al. An exploratory retrospective evaluation of ropinirole-associated psychotic symptoms in an outpatient population treated for restless legs syndrome or Parkinson’s disease. Ann Pharmacother. 2009;43(9):1426-1432.
9. Trenkwalder C, Hening WA, Montagna P, et al. Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice. Mov Disord. 2008;23(16):2267-2302.
10. Garcia-Borreguero D, Kohnen R, Silber MH, et al. The long-term treatment of restless legs syndrome/Willis-Ekbom disease: evidence-based guidelines and clinical consensus best practice guidance: a report from the International Restless Legs Syndrome Study Group. Sleep Med. 2013;14(7):675-684.
11. Dols A, Beekman A. Older age bipolar disorder. Psychiatr Clin North Am. 2018;41(1):95-110.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Singh A, Althoff R, Martineau RJ, et al. Pramipexole, ropinirole, and mania in Parkinson’s disease. Am J Psychiatry. 2005;162(4):814-815.
3. Weiss HD, Pontone GM. Dopamine receptor agonist drugs and impulse control disorders. JAMA Intern Med. 2014;174(12):1935-1937.
4 Shill HA, Stacy M. Update on ropinirole in the treatment of Parkinson’s disease. Neuropsychiatr Dis Treat. 2009;5:33-36.
5. Borovac JA. Side effects of a dopamine agonist therapy for Parkinson’s disease: a mini-review of clinical pharmacology. Yale J Biol Med. 2016;89(1):37-47.
6. Yüksel RN, Elyas Kaya Z, Dilbaz N, et al. Cabergoline-induced manic episode: case report. Ther Adv Psychopharmacol. 2016;6(3):229-231.
7. Perea E, Robbins BV, Hutto B. Psychosis related to ropinirole. Am J Psychiatry. 2006;163(3):547-548.
8. Stoner SC, Dahmen MM, Makos M, et al. An exploratory retrospective evaluation of ropinirole-associated psychotic symptoms in an outpatient population treated for restless legs syndrome or Parkinson’s disease. Ann Pharmacother. 2009;43(9):1426-1432.
9. Trenkwalder C, Hening WA, Montagna P, et al. Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice. Mov Disord. 2008;23(16):2267-2302.
10. Garcia-Borreguero D, Kohnen R, Silber MH, et al. The long-term treatment of restless legs syndrome/Willis-Ekbom disease: evidence-based guidelines and clinical consensus best practice guidance: a report from the International Restless Legs Syndrome Study Group. Sleep Med. 2013;14(7):675-684.
11. Dols A, Beekman A. Older age bipolar disorder. Psychiatr Clin North Am. 2018;41(1):95-110.
Dehydration in terminal illness: Which path forward?
CASE 1
A 94-year-old white woman, who had been in excellent health (other than pernicious anemia, treated with monthly cyanocobalamin injections), suddenly developed gastrointestinal distress 2 weeks earlier. A work-up performed by her physician revealed advanced pancreatic cancer.
Over the next 2 weeks, she experienced pain and nausea. A left-sided fistula developed externally at her flank that drained feces and induced considerable discomfort. An indwelling drain was placed, which provided some relief, but the patient’s dyspepsia, pain, and nausea escalated.
One month into her disease course, an oncologist reported on her potential treatment options and prognosis. Her life expectancy was about 3 months without treatment. This could be extended by 1 to 2 months with extensive surgical and chemotherapeutic interventions, but would further diminish her quality of life. The patient declined further treatment.
Her clinical status declined, and her quality of life significantly deteriorated. At 3 months, she felt life had lost meaning and was not worth living. She began asking for a morphine overdose, stating a desire to end her life.
After several discussions with the oncologist, one of the patient’s adult children suggested that her mother stop eating and drinking in order to diminish discomfort and hasten her demise. This plan was adopted, and the patient declined food and drank only enough to swish for oral comfort.
CASE 2
An 83-year-old woman with advanced Parkinson’s disease had become increasingly disabled. Her gait and motor skills were dramatically and progressively compromised. Pharmacotherapy yielded only transient improvement and considerable adverse effects of choreiform hyperkinesia and hallucinations, which were troublesome and embarrassing. Her social, physical, and personal well-being declined to the point that she was placed in a nursing home.
Despite this help, worsening parkinsonism progressively diminished her physical capacity. She became largely bedridden and developed decubitus ulcerations, especially at the coccyx, which produced severe pain and distress.
Continue to: The confluence of pain...
The confluence of pain, bedfastness, constipation, and social isolation yielded a loss of interest and joy in life. The patient required assistance with almost every aspect of daily life, including eating. As the illness progressed, she prayed at night that God would “take her.” Each morning, she spoke of disappointment upon reawakening. She overtly expressed her lack of desire to live to her family. Medical interventions were increasingly ineffective.
After repeated family and physician discussions had focused on her death wishes, one adult daughter recommended her mother stop eating and drinking; her food intake was already minimal. Although she did not endorse this plan verbally, the patient’s oral intake significantly diminished. Within 2 weeks, her physical state had declined, and she died one night during sleep.
Adequate hydration is stressed in physician education and practice. A conventional expectation to normalize fluid balance is important to restore health and improve well-being. In addition to being good medical practice, it can also show patients (and their families) that we care about their well-being.1-3
Treating dehydration in individuals with terminal illness is controversial from both medical and ethical standpoints. While the natural tendency of physicians is to restore full hydration to their patients, in select cases of imminent death, being fully hydrated may prolong discomfort.1,2 Emphasis in this population should be consistently placed on improving comfort care and quality of life, rather than prolonging life or delaying death.3-5
Continue to: A multifactorial, patient-based decision
A multifactorial, patient-based decision
Years ago, before the advent of hospitalizing people with terminal illnesses, dying at home amongst loved ones was believed to be peaceful. Nevertheless, questions arise about the practical vs ethical approach to caring for patients with terminal illness.2 Sometimes it is difficult to find a balance between potential health care benefits and the burdens induced by medical, legal, moral, and/or social pressures. Our medical communities and the general population uphold preserving dignity at the end of life, which is supported by organizations such as Compassion & Choices (a nonprofit group that seeks to improve and expand options for end of life care; https://www.compassionandchoices.org).
Allowing for voluntary, patient-determined dehydration in those with terminal illness can offer greater comfort than maintaining the physiologic degrees of fluid balance. There are 3 key considerations to bear in mind:
- Hydration is usually a standard part of quality medical care.1
- Selectively allowing dehydration in patients who are dying can facilitate comfort.1-5
- Dehydration may be a deliberate strategy to hasten death.6
When is dehydration appropriate?
Hydration is not favored whenever doing so may increase discomfort and prolong pain without meaningful life.3 In people with terminal illness, hydration may reduce quality of life.7
The data support dehydration in certain patients. A randomized controlled trial involving 129 patients receiving hospice care compared parenteral hydration with placebo, documenting that rehydration did not improve symptoms or quality of life; there was no significant difference between patients who were hydrated and those who were dehydrated.7 In fact, dehydration may even yield greater patient comfort.8
Case reports, retrospective chart reviews, and testimonials from health care professionals have reported that being less hydrated can diminish nausea, vomiting, diarrhea, ascites, edema, and urinary or bowel incontinence, with less skin breakdown.8 Hydration, on the other hand, may exacerbate dyspnea, coughing, and choking, increasing the need for suctioning.
Continue to: A component of palliative care
A component of palliative care. When death is imminent, palliation becomes key. Pain may be more manageable with less fluids, an important goal for this population.6,8 Dehydration is associated with an accumulation of opioids throughout body fluid volumes, which may decrease pain, consciousness, and/or agony.2 Pharmacotherapies might also have greater efficacy in a dehydrated patient.9 In addition, tissue shrinkage might mitigate pain from tumors, especially those in confined spaces.8
Hospice care and palliative medicine confirm that routine hydration is not always advisable; allowing for dehydration is a conventional practice, especially in older adults with terminal illness.7 However, do not deny access to liquids if a patient wants them, and never force unwanted fluids by any route.8 Facilitate oral care in the form of swishing fluids, elective drinking, or providing mouth lubrication for any patients selectively allowed to become dehydrated.3,8
The role of the physician in decision-making
Patients with terminal illness sometimes do not want fluids and may actively decline food and drink.10 This can be emotionally distressing for family members and/or caregivers to witness. Physicians can address this concern by compassionately explaining: “I know you are concerned that your relative is not eating or drinking, but there is no indication that hydration or parenteral feeding will improve function or quality of life.”10 This can generate a discussion between physicians and families by acknowledging concerns, relieving distress, and leading to what is ultimately best for the patient.
Implications for practice: Individualized autonomy
Physicians must identify patients who wish to die by purposely becoming dehydrated and uphold the important physician obligation to hydrate those with a recoverable illness. Allowing for a moderate degree of dehydration might provide greater comfort in select people with terminal illness. Some individuals for whom life has lost meaning may choose dehydration as a means to hasten their departure.4-6 Allowing individualized autonomy over life and death choices is part of a physician’s obligation to their patients. It can be difficult for caregivers, but it is medically indicated to comply with a patient’s desire for comfort when death is imminent.
Providing palliation as a priority over treatment is sometimes challenging, but comfort care takes preference and is always coordinated with the person’s own wishes. Facilitating dehydration removes assisted-suicide issues or requests and thus affords everyone involved more emotional comfort. An advantage of this method is that a decisional patient maintains full control over the direction of their choices and helps preserve dignity during the end of life.
CORRESPONDENCE
Steven Lippmann, MD, Department of Psychiatry, University of Louisville School of Medicine, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu
1. Burge FI. Dehydration and provision of fluids in palliative care. What is the evidence? Can Fam Physician. 1996;42:2383-2388.
2. Printz LA. Is withholding hydration a valid comfort measure in the terminally ill? Geriatrics. 1988;43:84-88.
3. Lippmann S. Palliative dehydration. Prim Care Companion CNS Disord. 2015;17: doi: 10.4088/PCC.15101797.
4. Bernat JL, Gert B, Mogielnicki RP. Patient refusal of hydration and nutrition: an alternative to physician-assisted suicide or voluntary active euthanasia. Arch Intern Med. 1993;153:2723-2728.
5. Sullivan RJ. Accepting death without artificial nutrition or hydration. J Gen Intern Med.1993;8:220-224.
6. Miller FG, Meier DE. Voluntary death: a comparison of terminal dehydration and physician-assisted suicide. Ann Intern Med. 1998;128:559-562.
7. Bruera E, Hui D, Dalal S, et al. Parenteral hydration in patients with advanced cancer: a multicenter, double-blind, placebo-controlled randomized trial. J Clin Oncol. 2013;31:111-118.
8. Forrow L, Smith HS. Pain management in end of life: palliative care. In: Warfield CA, Bajwa ZH, ed. Principles and Practice of Pain Management. 2nd ed. New York, NY: McGraw-Hill; 2004.
9. Zerwekh JV. The dehydration question. Nursing. 1983;13:47-51.
10. Bailey F, Harman S. Palliative care: The last hours and days of life. www.uptodate.com. September, 2016. Accessed on September 11, 2018.
CASE 1
A 94-year-old white woman, who had been in excellent health (other than pernicious anemia, treated with monthly cyanocobalamin injections), suddenly developed gastrointestinal distress 2 weeks earlier. A work-up performed by her physician revealed advanced pancreatic cancer.
Over the next 2 weeks, she experienced pain and nausea. A left-sided fistula developed externally at her flank that drained feces and induced considerable discomfort. An indwelling drain was placed, which provided some relief, but the patient’s dyspepsia, pain, and nausea escalated.
One month into her disease course, an oncologist reported on her potential treatment options and prognosis. Her life expectancy was about 3 months without treatment. This could be extended by 1 to 2 months with extensive surgical and chemotherapeutic interventions, but would further diminish her quality of life. The patient declined further treatment.
Her clinical status declined, and her quality of life significantly deteriorated. At 3 months, she felt life had lost meaning and was not worth living. She began asking for a morphine overdose, stating a desire to end her life.
After several discussions with the oncologist, one of the patient’s adult children suggested that her mother stop eating and drinking in order to diminish discomfort and hasten her demise. This plan was adopted, and the patient declined food and drank only enough to swish for oral comfort.
CASE 2
An 83-year-old woman with advanced Parkinson’s disease had become increasingly disabled. Her gait and motor skills were dramatically and progressively compromised. Pharmacotherapy yielded only transient improvement and considerable adverse effects of choreiform hyperkinesia and hallucinations, which were troublesome and embarrassing. Her social, physical, and personal well-being declined to the point that she was placed in a nursing home.
Despite this help, worsening parkinsonism progressively diminished her physical capacity. She became largely bedridden and developed decubitus ulcerations, especially at the coccyx, which produced severe pain and distress.
Continue to: The confluence of pain...
The confluence of pain, bedfastness, constipation, and social isolation yielded a loss of interest and joy in life. The patient required assistance with almost every aspect of daily life, including eating. As the illness progressed, she prayed at night that God would “take her.” Each morning, she spoke of disappointment upon reawakening. She overtly expressed her lack of desire to live to her family. Medical interventions were increasingly ineffective.
After repeated family and physician discussions had focused on her death wishes, one adult daughter recommended her mother stop eating and drinking; her food intake was already minimal. Although she did not endorse this plan verbally, the patient’s oral intake significantly diminished. Within 2 weeks, her physical state had declined, and she died one night during sleep.
Adequate hydration is stressed in physician education and practice. A conventional expectation to normalize fluid balance is important to restore health and improve well-being. In addition to being good medical practice, it can also show patients (and their families) that we care about their well-being.1-3
Treating dehydration in individuals with terminal illness is controversial from both medical and ethical standpoints. While the natural tendency of physicians is to restore full hydration to their patients, in select cases of imminent death, being fully hydrated may prolong discomfort.1,2 Emphasis in this population should be consistently placed on improving comfort care and quality of life, rather than prolonging life or delaying death.3-5
Continue to: A multifactorial, patient-based decision
A multifactorial, patient-based decision
Years ago, before the advent of hospitalizing people with terminal illnesses, dying at home amongst loved ones was believed to be peaceful. Nevertheless, questions arise about the practical vs ethical approach to caring for patients with terminal illness.2 Sometimes it is difficult to find a balance between potential health care benefits and the burdens induced by medical, legal, moral, and/or social pressures. Our medical communities and the general population uphold preserving dignity at the end of life, which is supported by organizations such as Compassion & Choices (a nonprofit group that seeks to improve and expand options for end of life care; https://www.compassionandchoices.org).
Allowing for voluntary, patient-determined dehydration in those with terminal illness can offer greater comfort than maintaining the physiologic degrees of fluid balance. There are 3 key considerations to bear in mind:
- Hydration is usually a standard part of quality medical care.1
- Selectively allowing dehydration in patients who are dying can facilitate comfort.1-5
- Dehydration may be a deliberate strategy to hasten death.6
When is dehydration appropriate?
Hydration is not favored whenever doing so may increase discomfort and prolong pain without meaningful life.3 In people with terminal illness, hydration may reduce quality of life.7
The data support dehydration in certain patients. A randomized controlled trial involving 129 patients receiving hospice care compared parenteral hydration with placebo, documenting that rehydration did not improve symptoms or quality of life; there was no significant difference between patients who were hydrated and those who were dehydrated.7 In fact, dehydration may even yield greater patient comfort.8
Case reports, retrospective chart reviews, and testimonials from health care professionals have reported that being less hydrated can diminish nausea, vomiting, diarrhea, ascites, edema, and urinary or bowel incontinence, with less skin breakdown.8 Hydration, on the other hand, may exacerbate dyspnea, coughing, and choking, increasing the need for suctioning.
Continue to: A component of palliative care
A component of palliative care. When death is imminent, palliation becomes key. Pain may be more manageable with less fluids, an important goal for this population.6,8 Dehydration is associated with an accumulation of opioids throughout body fluid volumes, which may decrease pain, consciousness, and/or agony.2 Pharmacotherapies might also have greater efficacy in a dehydrated patient.9 In addition, tissue shrinkage might mitigate pain from tumors, especially those in confined spaces.8
Hospice care and palliative medicine confirm that routine hydration is not always advisable; allowing for dehydration is a conventional practice, especially in older adults with terminal illness.7 However, do not deny access to liquids if a patient wants them, and never force unwanted fluids by any route.8 Facilitate oral care in the form of swishing fluids, elective drinking, or providing mouth lubrication for any patients selectively allowed to become dehydrated.3,8
The role of the physician in decision-making
Patients with terminal illness sometimes do not want fluids and may actively decline food and drink.10 This can be emotionally distressing for family members and/or caregivers to witness. Physicians can address this concern by compassionately explaining: “I know you are concerned that your relative is not eating or drinking, but there is no indication that hydration or parenteral feeding will improve function or quality of life.”10 This can generate a discussion between physicians and families by acknowledging concerns, relieving distress, and leading to what is ultimately best for the patient.
Implications for practice: Individualized autonomy
Physicians must identify patients who wish to die by purposely becoming dehydrated and uphold the important physician obligation to hydrate those with a recoverable illness. Allowing for a moderate degree of dehydration might provide greater comfort in select people with terminal illness. Some individuals for whom life has lost meaning may choose dehydration as a means to hasten their departure.4-6 Allowing individualized autonomy over life and death choices is part of a physician’s obligation to their patients. It can be difficult for caregivers, but it is medically indicated to comply with a patient’s desire for comfort when death is imminent.
Providing palliation as a priority over treatment is sometimes challenging, but comfort care takes preference and is always coordinated with the person’s own wishes. Facilitating dehydration removes assisted-suicide issues or requests and thus affords everyone involved more emotional comfort. An advantage of this method is that a decisional patient maintains full control over the direction of their choices and helps preserve dignity during the end of life.
CORRESPONDENCE
Steven Lippmann, MD, Department of Psychiatry, University of Louisville School of Medicine, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu
CASE 1
A 94-year-old white woman, who had been in excellent health (other than pernicious anemia, treated with monthly cyanocobalamin injections), suddenly developed gastrointestinal distress 2 weeks earlier. A work-up performed by her physician revealed advanced pancreatic cancer.
Over the next 2 weeks, she experienced pain and nausea. A left-sided fistula developed externally at her flank that drained feces and induced considerable discomfort. An indwelling drain was placed, which provided some relief, but the patient’s dyspepsia, pain, and nausea escalated.
One month into her disease course, an oncologist reported on her potential treatment options and prognosis. Her life expectancy was about 3 months without treatment. This could be extended by 1 to 2 months with extensive surgical and chemotherapeutic interventions, but would further diminish her quality of life. The patient declined further treatment.
Her clinical status declined, and her quality of life significantly deteriorated. At 3 months, she felt life had lost meaning and was not worth living. She began asking for a morphine overdose, stating a desire to end her life.
After several discussions with the oncologist, one of the patient’s adult children suggested that her mother stop eating and drinking in order to diminish discomfort and hasten her demise. This plan was adopted, and the patient declined food and drank only enough to swish for oral comfort.
CASE 2
An 83-year-old woman with advanced Parkinson’s disease had become increasingly disabled. Her gait and motor skills were dramatically and progressively compromised. Pharmacotherapy yielded only transient improvement and considerable adverse effects of choreiform hyperkinesia and hallucinations, which were troublesome and embarrassing. Her social, physical, and personal well-being declined to the point that she was placed in a nursing home.
Despite this help, worsening parkinsonism progressively diminished her physical capacity. She became largely bedridden and developed decubitus ulcerations, especially at the coccyx, which produced severe pain and distress.
Continue to: The confluence of pain...
The confluence of pain, bedfastness, constipation, and social isolation yielded a loss of interest and joy in life. The patient required assistance with almost every aspect of daily life, including eating. As the illness progressed, she prayed at night that God would “take her.” Each morning, she spoke of disappointment upon reawakening. She overtly expressed her lack of desire to live to her family. Medical interventions were increasingly ineffective.
After repeated family and physician discussions had focused on her death wishes, one adult daughter recommended her mother stop eating and drinking; her food intake was already minimal. Although she did not endorse this plan verbally, the patient’s oral intake significantly diminished. Within 2 weeks, her physical state had declined, and she died one night during sleep.
Adequate hydration is stressed in physician education and practice. A conventional expectation to normalize fluid balance is important to restore health and improve well-being. In addition to being good medical practice, it can also show patients (and their families) that we care about their well-being.1-3
Treating dehydration in individuals with terminal illness is controversial from both medical and ethical standpoints. While the natural tendency of physicians is to restore full hydration to their patients, in select cases of imminent death, being fully hydrated may prolong discomfort.1,2 Emphasis in this population should be consistently placed on improving comfort care and quality of life, rather than prolonging life or delaying death.3-5
Continue to: A multifactorial, patient-based decision
A multifactorial, patient-based decision
Years ago, before the advent of hospitalizing people with terminal illnesses, dying at home amongst loved ones was believed to be peaceful. Nevertheless, questions arise about the practical vs ethical approach to caring for patients with terminal illness.2 Sometimes it is difficult to find a balance between potential health care benefits and the burdens induced by medical, legal, moral, and/or social pressures. Our medical communities and the general population uphold preserving dignity at the end of life, which is supported by organizations such as Compassion & Choices (a nonprofit group that seeks to improve and expand options for end of life care; https://www.compassionandchoices.org).
Allowing for voluntary, patient-determined dehydration in those with terminal illness can offer greater comfort than maintaining the physiologic degrees of fluid balance. There are 3 key considerations to bear in mind:
- Hydration is usually a standard part of quality medical care.1
- Selectively allowing dehydration in patients who are dying can facilitate comfort.1-5
- Dehydration may be a deliberate strategy to hasten death.6
When is dehydration appropriate?
Hydration is not favored whenever doing so may increase discomfort and prolong pain without meaningful life.3 In people with terminal illness, hydration may reduce quality of life.7
The data support dehydration in certain patients. A randomized controlled trial involving 129 patients receiving hospice care compared parenteral hydration with placebo, documenting that rehydration did not improve symptoms or quality of life; there was no significant difference between patients who were hydrated and those who were dehydrated.7 In fact, dehydration may even yield greater patient comfort.8
Case reports, retrospective chart reviews, and testimonials from health care professionals have reported that being less hydrated can diminish nausea, vomiting, diarrhea, ascites, edema, and urinary or bowel incontinence, with less skin breakdown.8 Hydration, on the other hand, may exacerbate dyspnea, coughing, and choking, increasing the need for suctioning.
Continue to: A component of palliative care
A component of palliative care. When death is imminent, palliation becomes key. Pain may be more manageable with less fluids, an important goal for this population.6,8 Dehydration is associated with an accumulation of opioids throughout body fluid volumes, which may decrease pain, consciousness, and/or agony.2 Pharmacotherapies might also have greater efficacy in a dehydrated patient.9 In addition, tissue shrinkage might mitigate pain from tumors, especially those in confined spaces.8
Hospice care and palliative medicine confirm that routine hydration is not always advisable; allowing for dehydration is a conventional practice, especially in older adults with terminal illness.7 However, do not deny access to liquids if a patient wants them, and never force unwanted fluids by any route.8 Facilitate oral care in the form of swishing fluids, elective drinking, or providing mouth lubrication for any patients selectively allowed to become dehydrated.3,8
The role of the physician in decision-making
Patients with terminal illness sometimes do not want fluids and may actively decline food and drink.10 This can be emotionally distressing for family members and/or caregivers to witness. Physicians can address this concern by compassionately explaining: “I know you are concerned that your relative is not eating or drinking, but there is no indication that hydration or parenteral feeding will improve function or quality of life.”10 This can generate a discussion between physicians and families by acknowledging concerns, relieving distress, and leading to what is ultimately best for the patient.
Implications for practice: Individualized autonomy
Physicians must identify patients who wish to die by purposely becoming dehydrated and uphold the important physician obligation to hydrate those with a recoverable illness. Allowing for a moderate degree of dehydration might provide greater comfort in select people with terminal illness. Some individuals for whom life has lost meaning may choose dehydration as a means to hasten their departure.4-6 Allowing individualized autonomy over life and death choices is part of a physician’s obligation to their patients. It can be difficult for caregivers, but it is medically indicated to comply with a patient’s desire for comfort when death is imminent.
Providing palliation as a priority over treatment is sometimes challenging, but comfort care takes preference and is always coordinated with the person’s own wishes. Facilitating dehydration removes assisted-suicide issues or requests and thus affords everyone involved more emotional comfort. An advantage of this method is that a decisional patient maintains full control over the direction of their choices and helps preserve dignity during the end of life.
CORRESPONDENCE
Steven Lippmann, MD, Department of Psychiatry, University of Louisville School of Medicine, 401 East Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu
1. Burge FI. Dehydration and provision of fluids in palliative care. What is the evidence? Can Fam Physician. 1996;42:2383-2388.
2. Printz LA. Is withholding hydration a valid comfort measure in the terminally ill? Geriatrics. 1988;43:84-88.
3. Lippmann S. Palliative dehydration. Prim Care Companion CNS Disord. 2015;17: doi: 10.4088/PCC.15101797.
4. Bernat JL, Gert B, Mogielnicki RP. Patient refusal of hydration and nutrition: an alternative to physician-assisted suicide or voluntary active euthanasia. Arch Intern Med. 1993;153:2723-2728.
5. Sullivan RJ. Accepting death without artificial nutrition or hydration. J Gen Intern Med.1993;8:220-224.
6. Miller FG, Meier DE. Voluntary death: a comparison of terminal dehydration and physician-assisted suicide. Ann Intern Med. 1998;128:559-562.
7. Bruera E, Hui D, Dalal S, et al. Parenteral hydration in patients with advanced cancer: a multicenter, double-blind, placebo-controlled randomized trial. J Clin Oncol. 2013;31:111-118.
8. Forrow L, Smith HS. Pain management in end of life: palliative care. In: Warfield CA, Bajwa ZH, ed. Principles and Practice of Pain Management. 2nd ed. New York, NY: McGraw-Hill; 2004.
9. Zerwekh JV. The dehydration question. Nursing. 1983;13:47-51.
10. Bailey F, Harman S. Palliative care: The last hours and days of life. www.uptodate.com. September, 2016. Accessed on September 11, 2018.
1. Burge FI. Dehydration and provision of fluids in palliative care. What is the evidence? Can Fam Physician. 1996;42:2383-2388.
2. Printz LA. Is withholding hydration a valid comfort measure in the terminally ill? Geriatrics. 1988;43:84-88.
3. Lippmann S. Palliative dehydration. Prim Care Companion CNS Disord. 2015;17: doi: 10.4088/PCC.15101797.
4. Bernat JL, Gert B, Mogielnicki RP. Patient refusal of hydration and nutrition: an alternative to physician-assisted suicide or voluntary active euthanasia. Arch Intern Med. 1993;153:2723-2728.
5. Sullivan RJ. Accepting death without artificial nutrition or hydration. J Gen Intern Med.1993;8:220-224.
6. Miller FG, Meier DE. Voluntary death: a comparison of terminal dehydration and physician-assisted suicide. Ann Intern Med. 1998;128:559-562.
7. Bruera E, Hui D, Dalal S, et al. Parenteral hydration in patients with advanced cancer: a multicenter, double-blind, placebo-controlled randomized trial. J Clin Oncol. 2013;31:111-118.
8. Forrow L, Smith HS. Pain management in end of life: palliative care. In: Warfield CA, Bajwa ZH, ed. Principles and Practice of Pain Management. 2nd ed. New York, NY: McGraw-Hill; 2004.
9. Zerwekh JV. The dehydration question. Nursing. 1983;13:47-51.
10. Bailey F, Harman S. Palliative care: The last hours and days of life. www.uptodate.com. September, 2016. Accessed on September 11, 2018.
E-cigarettes: How “safe” are they?
› Inform patients that e-cigarette vapors contain toxic substances, including the heavy metals lead, cadmium, and nickel. A
› Educate all patients—particularly young people and those who are pregnant or lactating—about the potential health risks of e-cigarettes. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Electronic cigarettes (e-cigarettes) have become increasingly popular over the last decade. Although they are perceived by many to be safer than traditional cigarettes, many of the devices still contain nicotine, and inhaling their vapors exposes users to toxic substances, including lead, cadmium, and nickel—heavy metals that are associated with significant health problems.1 (For more on how e-cigarettes work, see “Cigarettes vs e-cigarettes: How does the experience (and cost) compare?”)
In addition, many people use e-cigarettes as a means to stop smoking, but few who do so achieve abstinence.2,3 They frequently end up utilizing both, increasing their health risks by exposing themselves to the dangers of 2 products instead of one.1
Further complicating the issue is that the manufacture and distribution of e-cigarettes has not been well regulated. Without regulation, there is no way to know with certainty how much nicotine the devices contain and what else is in them.
Things, however, are changing. The Food and Drug Administration (FDA) recently announced that e-cigarettes and other tobacco products like cigars and hookahs will now be regulated in the same way the government regulates tobacco cigarettes and smokeless tobacco.4 The rule will not take effect immediately because companies requested time to comply, but once it is enacted, packaging will be required to list what the products contain, among other changes.
Keeping up on the latest information on e-cigarettes is now—and will continue to be—important as family physicians are increasingly asked about them. What follows is a review of what we know about their potential risks.
A nicotine system developed by a pharmacist
E-cigarettes, or electronic nicotine delivery systems, were patented in 2003 by a Chinese pharmacist.5 Since their introduction to North America and Europe in 2007, the devices have become known by over 400 different brand names.6 Consumption among adults doubled by 2012, and by 2014, about 4% of US adults used e-cigarettes every day or some days.7 Many of them are dual users of tobacco and electronic cigarettes. In fact, Jenkins and colleagues reports in this issue of JFP (see "E-cigarettes: Who's using them and why?") that over half of cigarette smokers (52%) in their study use e-cigarettes, usually to either lower their cigarette consumption or aid in smoking cessation. (Throughout this article, we will use “cigarettes” and “smoking” to refer to the use of traditional tobacco cigarettes.)
In addition to concern over an increase in use among the general population, there is significant concern about the increase in e-cigarette use among US middle and high school students.1,8,9 In 2015, e-cigarettes were the most commonly used smoking product among middle and high school students, with 620,000 middle school students and nearly 2.4 million high school students using the battery-powered devices in the past 30 days.10
Many factors have contributed to the growing popularity of e-cigarettes.
- Perceived safety. With tobacco’s dangers so thoroughly documented, many advertising campaigns tout e-cigarettes as less dangerous than conventional cigarettes in terms of their ability to cause cardiac and lung diseases and low birth weights. This is largely because e-cigarettes do not produce the combustion products of tar, ash, or carbon monoxide. In addition, many consumers are mistakenly less fearful about the nicotine added to many e-cigarettes.
- Expectation that it helps smokers quit. Many smokers view e-cigarettes as an aid to smoking cessation.6 In fact, testimonials of efficacy in tobacco cessation abound in promotional materials and on the Web, and e-cigarettes are recommended by some physicians as a means to quit or lessen smoking of tobacco cigarettes.11
- Wide availability and opportunities for use. The use of electronic nicotine delivery devices is sometimes permitted in places where smoking of conventional cigarettes is banned, although rules vary widely in different parts of the country. In addition, e-cigarettes are readily available for purchase on the Internet without age verification.
- Extensive advertising. There are increasing concerns that advertising campaigns unduly target adolescents, young adults, and women.12-155 In addition to advertising, the media and social influences play significant roles in young people’s experimentation with “vaping,” the term for inhaling electronic cigarette aerosols.14,15
- Regulation, legislation remain controversial. Currently, e-cigarettes are not required to be tested before marketing,16 but that may change with the FDA’s new regulations. The British National Public Health body, Public Health England, has documented public health benefits of e-cigarettes when used as a way to quit smoking, and provides evidence that the devices are less dangerous than traditional cigarettes.17 But this issue and public policy are the subject of ongoing debate. In 2015, the United Kingdom made it illegal to sell e-cigarettes or e-liquids to people younger than 18 years of age and urged child-proof packaging.
What’s “in” an e-cigarette—and are the ingredients toxic?
Because e-cigarettes are relatively new to the global marketplace, little research exists regarding the long-term effects and safety of their use, especially among habitual users.
Vapor/refills. E-liquids may contain a variety of substances because they have been largely unregulated, but they generally include some combination of nicotine, propylene glycol, glycerin, and flavorings. In fact, up to 7000 flavors are available,6 including such kid-friendly flavors as chocolate, cherry crush, and bubble gum.
When the refills do contain nicotine, users generally derive less of the substance from the electronic devices than they do from a conventional cigarette. Researchers found that individual puffs from an e-cigarette contained 0 to 35 µg nicotine per puff.1,18 Assuming an amount at the high end of the spectrum (30 µg nicotine), it would take about 30 puffs of an e-cigarette to derive the same amount of nicotine (1 mg) typically delivered by a conventional cigarette.
The chemical make-up of the vapor and the biologic effects on animal models have been investigated using 42 different liquid refills.19,20 All contained potentially harmful compounds, but the levels were within exposure limits authorized by the FDA. These potentially dangerous chemicals include the known toxins formaldehyde, acrolein, and hydrocarbons.20
An inflammatory response to the inhalation of the vapors was demonstrated in mouse lungs; exposure to e-cigarette aerosols reduced lung glutathione—an important enzyme in maintaining oxidation-reduction balance—to a degree similar to that of cigarette smoke exposure.20 Less of the enzyme facilitates increased pulmonary inflammation.
In addition, human lung cells release pro-inflammatory cytokines when exposed to e-cigarette aerosols.20 Other health risks include:
Harm to indoor air quality/secondhand exposure. Even though e-cigarettes do not emit smoke, bystanders are exposed to the aerosol or vapor exhaled by the user, and researchers have found varying levels of such substances as formaldehyde, acetaldehyde, isoprene, acetic acid, acetone, propanol, propylene glycol, and nicotine in the air. However, it is unclear at this time whether the ultra-fine particles in the e-cigarette vapor have health effects commensurate with the emissions of conventional cigarettes.1,21,22
Cartridge refill ingestion by children. Accidental nicotine poisonings, particularly among children drawn to the colors, flavors, and scents of the e-liquids, have been problematic. In 2014, for example, over 3500 exposures occurred and more than half of those were in children younger than 6 years of age. (Exposure is defined as contact with the substance in some way including ingestion, inhalation, absorption by the skin/eyes, etc; not all exposures are poisonings or overdoses).23 Although incidence has tapered off somewhat, the American Association of Poison Control Centers reports that there were 623 exposures across all age groups between January 1, 2016 and April 30, 2016.23
Environmental impact of discarded e-cigarettes. Discarded e-cigarettes filling our landfills is a new and emerging public health concern. Their batteries, as do all batteries, pollute the land and water and have the potential to leach lead into the environment.24 Similarly, incompletely used liquid cartridges and refills may contain nicotine and heavy metals, which add to these risks.24
Explosions. Fires and explosions have been documented with e-cigarette use, mostly due to malfunctioning lithium-ion batteries.25 Thermal injuries to the face and hands can be significant.
Heavy metals. The presence of lead, cadmium, and nickel in inhaled e-cigarette vapor is another area of significant concern, particularly for younger people who might have long-term exposure.1 All 3 heavy metals are known to be toxic to humans, and safe levels of inhalation have not been established.
Inhalation and/or ingestion of lead, in particular, can cause severe neurologic damage, especially to the developing brains of children.26 Lead also results in hematologic dysfunction. Because of the risks associated with inhalation of this heavy metal, the substance was removed from gasoline years ago.
Inhaled cadmium induces kidney, liver, bone, and respiratory tract pathology27 and can cause organ failure, hypertension, anemias, fractures, osteoporosis, and/or osteomalacia.28 And inhaling nickel produces an inflammatory pulmonary reaction.29
Pregnancy/lactation. Since no clear evidence exists on the safety of e-cigarette use during pregnancy, women should avoid exposure to these vapors during the entire perinatal period. Similarly, the effects of e-cigarettes on infants who are breastfeeding are not established. Pregnant and breastfeeding women should not replace cigarettes with e-cigarettes.30,31 For pregnant women who smoke, the US Preventive Services Task Force (USPSTF) advises using only behavioral methods to stop cigarette use.32 And until more information becomes available, exposing infants and young children to e-cigarette vapor during breastfeeding is not recommended.
On the flip side, without tobacco, tar, ash, or carbon monoxide, e-cigarettes may have some advantages when compared with the use of traditional cigarettes, but that has not been substantiated.
Cigarettes vs e-cigarettes: How does the experience (and cost) compare?
If you were to ask a smoker to describe how cigarette smoking compares to using e-cigarettes, he or she would probably tell you that while the process of drawing on an e-cigarette is similar to that of a conventional cigarette, the experience in terms of reaching that state of relaxation or getting that “smoker’s high” is not.
In fact, a recent national survey of current and former smokers found that more than three-quarters of current smokers (77%) rated e-cigarettes less satisfying than conventional cigarettes and stopped using them.1 “Being less harmful” was the most highly rated reason for continuing to use the devices among people who switched from conventional to e-cigarettes.
How do they work? E-cigarettes do not burn anything and users do not light them. E-cigarettes work in much the same way as a smoke or fog machine. They use battery power (usually a rechargeable lithium battery) to heat a solution—usually containing nicotine, flavorings, and other chemicals—to the point that it turns into vapor. Much of whatever substances are in the vapor enter the bloodstream through the buccal mucosa, rather than the lungs.
Devices typically have an on/off button or switch, an atomizer containing a heating coil, a battery, and an LED light, which is designed to simulate a burning cigarette. A sensor detects when a user takes a drag and activates the atomizer and light. Some of the devices can be charged with a USB cord.
Because e-cigarettes don’t burn anything, they don’t have any smoke. They also don’t have any tar, ash, carbon monoxide, or odor (except perhaps a faint, short-lived scent matching the flavor liquid chosen). But the issues of second-hand exposure and effects on air quality are still being investigated.
With over 500 brands available, devices generally fall into one of 3 categories:2
- Cigalikes: About the same size and shape of a conventional cigarette, these cigarette look-alikes may come pre-filled with about a day’s worth of liquid and then may be discarded, or they may be non-disposable and have a replaceable cartridge.
- eGo’s: Also known as "vape pens," these devices tend to be longer and wider than cigalikes, have a more powerful battery, and usually are refillable or have a replaceable cartridge.
- Mods: Short for “modules,” these “vaporizers” tend to be the largest and most expensive type of e-cigarette. They may be refilled with e-liquid or accept replaceable cartridges and have even more powerful batteries.
What do they cost? A pack of cigarettes (containing 20 cigarettes) costs anywhere from $5 to $14, depending on where one lives.3 The price of e-cigarette devices starts at about $8 and can climb higher than $100. A 5-pack of flavor cartridges or a refill tank of e-liquid (which may last as long as about 150 cigarettes) costs about $10 to $15.4
To put this in perspective, a pack-a-day smoker in New York might spend about $5000 a year on cigarettes ($14 per pack x 365 days in a year), whereas someone who uses an e-cigarette device ($10) plus a refill tank per week ($14 x 52 weeks per year) will spend about $740 a year. (The actual cost will be higher because atomizers or devices as a whole must be replaced periodically, with some lasting only days and others lasting weeks or months, depending largely on how often one uses them. Although the cost of atomizers ranges widely, many can be found for $3-$5.)
Of course, the difference between cigarettes and e-cigarettes will be less dramatic in states where cigarettes are cheaper.
References
1. Pechacek TF, Nayak P, Gregory KR, et al. The potential that electronic delivery systems can be a disruptive technology: results from a national survey. Nicotine Tob Res. 2016. Available at: http://ntr.oxfordjournals.org/content/early/2016/05/03/ntr.ntw102.abstract. Accessed May 13, 2016.
2. Center for Environmental Health. A smoking gun: cancer-causing chemicals in e-cigarettes. Available at: http://www.ceh.org/wp-content/uploads/CEH-2015-report_A-Smoking-Gun_-Cancer-Causing-Chemicals-in-E-Cigarettes_alt.pdf. Accessed May 11, 2016.
3. Holmes H. The price of being an American. What a pack of cigarettes costs, in every state. August 28, 2015. Available at: http://www.theawl.com/2015/08/what-a-pack-of-cigarettes-costs-in-every-state. Accessed May 11, 2016.
4. Blu. How much do e-cigs cost? E-cig & vapor cigarette prices. Available at: http://www.blucigs.com/much-e-cigs-cost/. Accessed May 13, 2016.
Don’t substitute one form of nicotine for another
The USPSTF has not determined the benefit-to-harm ratio of using e-cigarettes as a smoking cessation aid, but recommends prescribing behavioral techniques and/or pharmacologic alternatives instead.32 Because the devices have been promoted as an aid to smoking cessation, intention to quit using tobacco products is a reason often stated for utilizing e-cigarettes.2,33,34 Indeed, use of e-cigarettes is much more likely among those who already utilize tobacco products.35-37
At least one study reports that e-cigarettes have efficacy similar to nicotine patches in achieving smoking abstinence among smokers who want to quit.38 Former smokers who used e-cigarettes to quit smoking reported fewer withdrawal symptoms than those who used nicotine skin patches.39 In addition, former smokers were more likely to endorse e-cigarettes than nicotine patches as a tobacco cigarette cessation aid. Significant reduction in tobacco smoke exposure has been demonstrated in dual users of tobacco and electronic cigarettes;40,41 however, both of these nicotine delivery systems sustain nicotine addiction.
Despite many ongoing studies to determine if e-cigarettes are useful as a smoking cessation aid, the results vary widely and are inconclusive at this time.42
E-cigarettes do not increase long-term tobacco abstinence
Contrary to popular belief, research shows that e-cigarette use among smokers is not associated with long-term tobacco abstinence.1 E-cigarette users, however, may make more attempts to quit smoking compared with smokers not using them.43 In addition, even though there is some evidence that e-cigarettes help smokers reduce the number of cigarettes smoked per day, simply reducing the daily number of cigarettes does not equate with safety.44 Smoking just one to 4 cigarettes per day poses 3 times the risk of myocardial infarction and lung cancer compared with not smoking.44 And since many individuals continue to use traditional and electronic cigarettes, they end up in double jeopardy of toxicity through exposure to the dangers of both.
A gateway to other substances of abuse?
There is also fear that nicotine exposure via e-cigarettes, especially in young people, serves as a “gateway” to tobacco consumption and other substance abuses, and increases the risk for nicotine addiction.34 Such nicotine-induced effects are a result of changes in brain chemistry, and have been documented in humans and animals.34
These concerns about negative health consequences, combined with the fact that e-cigarettes are undocumented as a smoking cessation aid, add urgency to the need for legislative and regulatory actions that hopefully can curb all nicotine exposures, particularly for our nation’s youth. In the meantime, it is important for physicians to advise patients—and the public—about the risks of e-cigarettes and the importance of quitting all forms of nicotine inhalation because nicotine—regardless of how it is delivered—is still an addictive drug.
CORRESPONDENCE
Steven Lippmann, MD, University of Louisville School of Medicine, 401 E. Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu.
1. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129:1972-1986.
2. Vickerman KA, Carpenter KM, Altman T, et al. Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine Tob Res. 2013;15:1787-1791.
3. Grana R, Popova L, Ling P. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Int Med. 2014;174:812-813.
4. U.S. Food and Drug Administration. Vaporizers, e-cigarettes, and other electronic nicotine delivery systems (ENDS). Available at: http://www.fda.gov/TobaccoProducts/Labeling/ProductsIngredientsComponents/ucm456610.htm. Accessed May 12, 2016.
5. Grana R, Benowitz N, Glantz SA. Background paper on E-cigarettes (electronic nicotine delivery systems). Center for Tobacco Control Research and Education, University of California, San Francisco, a WHO Collaborating Center on Tobacco Control. Prepared for World Health Organization Tobacco Free Initiative. December 2013. Available at: http://pvw.escholarship.org/uc/item/13p2b72n. Accessed March 31, 2014.
6. Zhu SH, Sun JY, Bonnevie E, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23:iii3-iii9.
7. Electronic Cigarette Use Among Adults: United States, 2014. NCHStats: A blog of the National Center for Health Statistics. Available at: http://nchstats.com/2015/10/28/electronic-cigarette-use-among-adults-united-states-2014/. Accessed April 22, 2016.
8. Centers for Disease Control and Prevention. E-cigarette use more than doubles among U.S. middle and high school students from 2011-2012. Available at: http://www.cdc.gov/media/releases/2013/p0905-ecigarette-use.html. Accessed April 22, 2016.
9. Centers for Disease Control and Prevention. Notes from the field: electronic cigarette use among middle and high school students — United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 2013;62:729-730.
10. Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011-2015. MMWR Morb Mortal Wkly Rpt. 2016;65:361-367.
11. Kandra KL, Ranney LM, Lee JG, et al. Physicians’ attitudes and use of e-cigarettes as cessation devices, North Carolina, 2013. PloS One. 2014;9:e103462.
12. Schraufnagel DE. Electronic cigarettes: vulnerability of youth. Pediatr Allergy Immunol Pulmonol. 2015;28:2-6.
13. White J, Li J, Newcombe R, et al. Tripling use of electronic cigarettes among New Zealand adolescents between 2012 and 2014. J Adolesc Health. 2015;56:522-528.
14. Duke JC, Lee YO, Kim AE, et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134:29-36.
15. Huang J, Kornfield R, Szczypka G, et al. A cross-sectional examination of marketing of electronic cigarettes on Twitter. Tob Control. 2014;23:iii26-iii30.
16. Rojewski AM, Coleman N, Toll BA. Position Statement: Emerging policy issues regarding electronic nicotine delivery systems: a need for regulation. Society of Behavioral Medicine. 2016. Available at: http://www.sbm.org/UserFiles/file/e-cig-statement_v2_lores.pdf. Accessed April 22, 2016.
17. McNeill A, Brose LS, Calder R, et al. E-cigarettes: an evidence update. A report commissioned by Public Health England. 2015. Available at: https://www.gov.uk/government/publications/e-cigarettes-an-evidence-update. Accessed April 22, 2016.
18. Goniewicz ML, Kuma T, Gawron M, et al. Nicotine levels in electronic cigarettes. Nicotine Tob Res. 2013;15:158-166.
19. Varlet V, Farsalinos K, Augsburger M, et al. Toxicity assessment of refill liquids for electronic cigarettes. Int J Environ Res Public Health. 2015;12:4796-4815.
20. Lerner CA, Sundar IK, Yao H, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One. 2015;10:e0116732.
21. Schober W, Szendrei K, Matzen W, et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217:628-637.
22. Schripp T, Markewitz D, Uhde E, et al. Does e-cigarette consumption cause passive vaping? Indoor Air. 2013;23:25-31.
23. The American Association of Poison Control Centers. E-cigarettes and liquid nicotine. Available at: http://www.aapcc.org/alerts/e-cigarettes/. Accessed May 12, 2016.
24. Krause MJ, Townsend TG. Hazardous waste status of discarded electronic cigarettes. Waste Manag. 2015;39:57-62.
25. U.S. Fire Administration. Electronic cigarette fires and explosions. October 2014. Available at: https://www.usfa.fema.gov/downloads/pdf/publications/electronic_cigarettes.pdf. Accessed May 17, 2016.
26. Skerfving S, Löfmark L, Lundh T, et al. Late effects of low blood lead concentrations in children on school performance and cognitive functions. Neurotoxicology. 2015;49:114-120.
27. Bernhoft RA. Cadmium toxicity and treatment. Scientific World Journal. 2013;394652.
28. Agency for Toxic Substances and Disease Registry. Case studies in environmental medicine (CSEM) Cadmium Toxicity. Available at: http://www.atsdr.cdc.gov/csem/cadmium/docs/cadmium.pdf. Accessed April 22, 2016.
29. Das KK, Buchner V. Effect of nickel exposure on peripheral tissues: role of oxidative stress in toxicity and possible protection by ascorbic acid. Rev Environ Health. 2007;22:157-173.
30. England LJ, Bunnell RE, Pechacek TF, et al. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am J Prev Med. 2015;49:286-293.
31. Suter MA, Mastrobattista J, Sachs M, et al. Is there evidence for potential harm of electronic cigarette use in pregnancy? Birth defects research. Birth Defects Res A Clin Mol Teratol. 2015;103:186-195.
32. U.S. Preventive Services Task Force. Draft Recommendation Statement. Tobacco smoking cessation in adults and pregnant women: behavioral and pharmacotherapy interventions. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement147/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions1. Accessed March 22, 2016.
33. Peters EN, Harrell PT, Hendricks PS, et al. Electronic cigarettes in adults in outpatient substance use treatment: awareness, perceptions, use, and reasons for use. Am J Addict. 2015;24:233-239.
34. Kandel ER, Kandel DB. A molecular basis for nicotine as a gateway drug. N Engl J Med. 2014;371:932-943.
35. King BA, Patel R, Nguyen KH, et al. Trends in awareness and use of electronic cigarettes among US Adults, 2010-2013. Nicotine Tob Res. 2015;17:219-227.
36. McMillen RC, Gottlieb MA, Shaefer RM, et al. Trends in electronic cigarette use among U.S. adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;1195-1202.
37. Lee S, Grana RA, Glantz SA. Electronic cigarette use among Korean adolescents: a cross-sectional study of market penetration, dual use, and relationship to quit attempts and former smoking. J Adolesc Health. 2014;54:684-690.
38. Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382:1629-1637.
39. Nelson VA, Goniewicz ML, Beard E, et al. Comparison of the characteristics of long-term users of electronic cigarettes versus nicotine replacement therapy: a cross-sectional survey of English ex-smokers and current smokers. Drug Alcohol Depend. 2015;153:300-305.
40. Caponnetto P, Campagna D, Cibella F, et al. Efficiency and safety of an electronic cigarette (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One. 2013;8:e66317.
41. Polosa R, Caponnetto P, Morjaria JB, et al. Effect of an electronic nicotine delivery device (e-Cigarette) on smoking reduction and cessation: a prospective 6-month pilot study. BMC Public Health. 2011;11:786.
42. Malas M, van der Tempel J, Schwartz R, et al. Electronic cigarettes for smoking cessation: a systematic review. Nicotine Tob Res. 2016. [Epub ahead of print].
43. Brose LS, Hitchman SC, Brown J, et al. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction. 2015;110:1160-1168.
44. Bjartveit K, Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tob Control. 2005;14:315-320.
› Inform patients that e-cigarette vapors contain toxic substances, including the heavy metals lead, cadmium, and nickel. A
› Educate all patients—particularly young people and those who are pregnant or lactating—about the potential health risks of e-cigarettes. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Electronic cigarettes (e-cigarettes) have become increasingly popular over the last decade. Although they are perceived by many to be safer than traditional cigarettes, many of the devices still contain nicotine, and inhaling their vapors exposes users to toxic substances, including lead, cadmium, and nickel—heavy metals that are associated with significant health problems.1 (For more on how e-cigarettes work, see “Cigarettes vs e-cigarettes: How does the experience (and cost) compare?”)
In addition, many people use e-cigarettes as a means to stop smoking, but few who do so achieve abstinence.2,3 They frequently end up utilizing both, increasing their health risks by exposing themselves to the dangers of 2 products instead of one.1
Further complicating the issue is that the manufacture and distribution of e-cigarettes has not been well regulated. Without regulation, there is no way to know with certainty how much nicotine the devices contain and what else is in them.
Things, however, are changing. The Food and Drug Administration (FDA) recently announced that e-cigarettes and other tobacco products like cigars and hookahs will now be regulated in the same way the government regulates tobacco cigarettes and smokeless tobacco.4 The rule will not take effect immediately because companies requested time to comply, but once it is enacted, packaging will be required to list what the products contain, among other changes.
Keeping up on the latest information on e-cigarettes is now—and will continue to be—important as family physicians are increasingly asked about them. What follows is a review of what we know about their potential risks.
A nicotine system developed by a pharmacist
E-cigarettes, or electronic nicotine delivery systems, were patented in 2003 by a Chinese pharmacist.5 Since their introduction to North America and Europe in 2007, the devices have become known by over 400 different brand names.6 Consumption among adults doubled by 2012, and by 2014, about 4% of US adults used e-cigarettes every day or some days.7 Many of them are dual users of tobacco and electronic cigarettes. In fact, Jenkins and colleagues reports in this issue of JFP (see "E-cigarettes: Who's using them and why?") that over half of cigarette smokers (52%) in their study use e-cigarettes, usually to either lower their cigarette consumption or aid in smoking cessation. (Throughout this article, we will use “cigarettes” and “smoking” to refer to the use of traditional tobacco cigarettes.)
In addition to concern over an increase in use among the general population, there is significant concern about the increase in e-cigarette use among US middle and high school students.1,8,9 In 2015, e-cigarettes were the most commonly used smoking product among middle and high school students, with 620,000 middle school students and nearly 2.4 million high school students using the battery-powered devices in the past 30 days.10
Many factors have contributed to the growing popularity of e-cigarettes.
- Perceived safety. With tobacco’s dangers so thoroughly documented, many advertising campaigns tout e-cigarettes as less dangerous than conventional cigarettes in terms of their ability to cause cardiac and lung diseases and low birth weights. This is largely because e-cigarettes do not produce the combustion products of tar, ash, or carbon monoxide. In addition, many consumers are mistakenly less fearful about the nicotine added to many e-cigarettes.
- Expectation that it helps smokers quit. Many smokers view e-cigarettes as an aid to smoking cessation.6 In fact, testimonials of efficacy in tobacco cessation abound in promotional materials and on the Web, and e-cigarettes are recommended by some physicians as a means to quit or lessen smoking of tobacco cigarettes.11
- Wide availability and opportunities for use. The use of electronic nicotine delivery devices is sometimes permitted in places where smoking of conventional cigarettes is banned, although rules vary widely in different parts of the country. In addition, e-cigarettes are readily available for purchase on the Internet without age verification.
- Extensive advertising. There are increasing concerns that advertising campaigns unduly target adolescents, young adults, and women.12-155 In addition to advertising, the media and social influences play significant roles in young people’s experimentation with “vaping,” the term for inhaling electronic cigarette aerosols.14,15
- Regulation, legislation remain controversial. Currently, e-cigarettes are not required to be tested before marketing,16 but that may change with the FDA’s new regulations. The British National Public Health body, Public Health England, has documented public health benefits of e-cigarettes when used as a way to quit smoking, and provides evidence that the devices are less dangerous than traditional cigarettes.17 But this issue and public policy are the subject of ongoing debate. In 2015, the United Kingdom made it illegal to sell e-cigarettes or e-liquids to people younger than 18 years of age and urged child-proof packaging.
What’s “in” an e-cigarette—and are the ingredients toxic?
Because e-cigarettes are relatively new to the global marketplace, little research exists regarding the long-term effects and safety of their use, especially among habitual users.
Vapor/refills. E-liquids may contain a variety of substances because they have been largely unregulated, but they generally include some combination of nicotine, propylene glycol, glycerin, and flavorings. In fact, up to 7000 flavors are available,6 including such kid-friendly flavors as chocolate, cherry crush, and bubble gum.
When the refills do contain nicotine, users generally derive less of the substance from the electronic devices than they do from a conventional cigarette. Researchers found that individual puffs from an e-cigarette contained 0 to 35 µg nicotine per puff.1,18 Assuming an amount at the high end of the spectrum (30 µg nicotine), it would take about 30 puffs of an e-cigarette to derive the same amount of nicotine (1 mg) typically delivered by a conventional cigarette.
The chemical make-up of the vapor and the biologic effects on animal models have been investigated using 42 different liquid refills.19,20 All contained potentially harmful compounds, but the levels were within exposure limits authorized by the FDA. These potentially dangerous chemicals include the known toxins formaldehyde, acrolein, and hydrocarbons.20
An inflammatory response to the inhalation of the vapors was demonstrated in mouse lungs; exposure to e-cigarette aerosols reduced lung glutathione—an important enzyme in maintaining oxidation-reduction balance—to a degree similar to that of cigarette smoke exposure.20 Less of the enzyme facilitates increased pulmonary inflammation.
In addition, human lung cells release pro-inflammatory cytokines when exposed to e-cigarette aerosols.20 Other health risks include:
Harm to indoor air quality/secondhand exposure. Even though e-cigarettes do not emit smoke, bystanders are exposed to the aerosol or vapor exhaled by the user, and researchers have found varying levels of such substances as formaldehyde, acetaldehyde, isoprene, acetic acid, acetone, propanol, propylene glycol, and nicotine in the air. However, it is unclear at this time whether the ultra-fine particles in the e-cigarette vapor have health effects commensurate with the emissions of conventional cigarettes.1,21,22
Cartridge refill ingestion by children. Accidental nicotine poisonings, particularly among children drawn to the colors, flavors, and scents of the e-liquids, have been problematic. In 2014, for example, over 3500 exposures occurred and more than half of those were in children younger than 6 years of age. (Exposure is defined as contact with the substance in some way including ingestion, inhalation, absorption by the skin/eyes, etc; not all exposures are poisonings or overdoses).23 Although incidence has tapered off somewhat, the American Association of Poison Control Centers reports that there were 623 exposures across all age groups between January 1, 2016 and April 30, 2016.23
Environmental impact of discarded e-cigarettes. Discarded e-cigarettes filling our landfills is a new and emerging public health concern. Their batteries, as do all batteries, pollute the land and water and have the potential to leach lead into the environment.24 Similarly, incompletely used liquid cartridges and refills may contain nicotine and heavy metals, which add to these risks.24
Explosions. Fires and explosions have been documented with e-cigarette use, mostly due to malfunctioning lithium-ion batteries.25 Thermal injuries to the face and hands can be significant.
Heavy metals. The presence of lead, cadmium, and nickel in inhaled e-cigarette vapor is another area of significant concern, particularly for younger people who might have long-term exposure.1 All 3 heavy metals are known to be toxic to humans, and safe levels of inhalation have not been established.
Inhalation and/or ingestion of lead, in particular, can cause severe neurologic damage, especially to the developing brains of children.26 Lead also results in hematologic dysfunction. Because of the risks associated with inhalation of this heavy metal, the substance was removed from gasoline years ago.
Inhaled cadmium induces kidney, liver, bone, and respiratory tract pathology27 and can cause organ failure, hypertension, anemias, fractures, osteoporosis, and/or osteomalacia.28 And inhaling nickel produces an inflammatory pulmonary reaction.29
Pregnancy/lactation. Since no clear evidence exists on the safety of e-cigarette use during pregnancy, women should avoid exposure to these vapors during the entire perinatal period. Similarly, the effects of e-cigarettes on infants who are breastfeeding are not established. Pregnant and breastfeeding women should not replace cigarettes with e-cigarettes.30,31 For pregnant women who smoke, the US Preventive Services Task Force (USPSTF) advises using only behavioral methods to stop cigarette use.32 And until more information becomes available, exposing infants and young children to e-cigarette vapor during breastfeeding is not recommended.
On the flip side, without tobacco, tar, ash, or carbon monoxide, e-cigarettes may have some advantages when compared with the use of traditional cigarettes, but that has not been substantiated.
Cigarettes vs e-cigarettes: How does the experience (and cost) compare?
If you were to ask a smoker to describe how cigarette smoking compares to using e-cigarettes, he or she would probably tell you that while the process of drawing on an e-cigarette is similar to that of a conventional cigarette, the experience in terms of reaching that state of relaxation or getting that “smoker’s high” is not.
In fact, a recent national survey of current and former smokers found that more than three-quarters of current smokers (77%) rated e-cigarettes less satisfying than conventional cigarettes and stopped using them.1 “Being less harmful” was the most highly rated reason for continuing to use the devices among people who switched from conventional to e-cigarettes.
How do they work? E-cigarettes do not burn anything and users do not light them. E-cigarettes work in much the same way as a smoke or fog machine. They use battery power (usually a rechargeable lithium battery) to heat a solution—usually containing nicotine, flavorings, and other chemicals—to the point that it turns into vapor. Much of whatever substances are in the vapor enter the bloodstream through the buccal mucosa, rather than the lungs.
Devices typically have an on/off button or switch, an atomizer containing a heating coil, a battery, and an LED light, which is designed to simulate a burning cigarette. A sensor detects when a user takes a drag and activates the atomizer and light. Some of the devices can be charged with a USB cord.
Because e-cigarettes don’t burn anything, they don’t have any smoke. They also don’t have any tar, ash, carbon monoxide, or odor (except perhaps a faint, short-lived scent matching the flavor liquid chosen). But the issues of second-hand exposure and effects on air quality are still being investigated.
With over 500 brands available, devices generally fall into one of 3 categories:2
- Cigalikes: About the same size and shape of a conventional cigarette, these cigarette look-alikes may come pre-filled with about a day’s worth of liquid and then may be discarded, or they may be non-disposable and have a replaceable cartridge.
- eGo’s: Also known as "vape pens," these devices tend to be longer and wider than cigalikes, have a more powerful battery, and usually are refillable or have a replaceable cartridge.
- Mods: Short for “modules,” these “vaporizers” tend to be the largest and most expensive type of e-cigarette. They may be refilled with e-liquid or accept replaceable cartridges and have even more powerful batteries.
What do they cost? A pack of cigarettes (containing 20 cigarettes) costs anywhere from $5 to $14, depending on where one lives.3 The price of e-cigarette devices starts at about $8 and can climb higher than $100. A 5-pack of flavor cartridges or a refill tank of e-liquid (which may last as long as about 150 cigarettes) costs about $10 to $15.4
To put this in perspective, a pack-a-day smoker in New York might spend about $5000 a year on cigarettes ($14 per pack x 365 days in a year), whereas someone who uses an e-cigarette device ($10) plus a refill tank per week ($14 x 52 weeks per year) will spend about $740 a year. (The actual cost will be higher because atomizers or devices as a whole must be replaced periodically, with some lasting only days and others lasting weeks or months, depending largely on how often one uses them. Although the cost of atomizers ranges widely, many can be found for $3-$5.)
Of course, the difference between cigarettes and e-cigarettes will be less dramatic in states where cigarettes are cheaper.
References
1. Pechacek TF, Nayak P, Gregory KR, et al. The potential that electronic delivery systems can be a disruptive technology: results from a national survey. Nicotine Tob Res. 2016. Available at: http://ntr.oxfordjournals.org/content/early/2016/05/03/ntr.ntw102.abstract. Accessed May 13, 2016.
2. Center for Environmental Health. A smoking gun: cancer-causing chemicals in e-cigarettes. Available at: http://www.ceh.org/wp-content/uploads/CEH-2015-report_A-Smoking-Gun_-Cancer-Causing-Chemicals-in-E-Cigarettes_alt.pdf. Accessed May 11, 2016.
3. Holmes H. The price of being an American. What a pack of cigarettes costs, in every state. August 28, 2015. Available at: http://www.theawl.com/2015/08/what-a-pack-of-cigarettes-costs-in-every-state. Accessed May 11, 2016.
4. Blu. How much do e-cigs cost? E-cig & vapor cigarette prices. Available at: http://www.blucigs.com/much-e-cigs-cost/. Accessed May 13, 2016.
Don’t substitute one form of nicotine for another
The USPSTF has not determined the benefit-to-harm ratio of using e-cigarettes as a smoking cessation aid, but recommends prescribing behavioral techniques and/or pharmacologic alternatives instead.32 Because the devices have been promoted as an aid to smoking cessation, intention to quit using tobacco products is a reason often stated for utilizing e-cigarettes.2,33,34 Indeed, use of e-cigarettes is much more likely among those who already utilize tobacco products.35-37
At least one study reports that e-cigarettes have efficacy similar to nicotine patches in achieving smoking abstinence among smokers who want to quit.38 Former smokers who used e-cigarettes to quit smoking reported fewer withdrawal symptoms than those who used nicotine skin patches.39 In addition, former smokers were more likely to endorse e-cigarettes than nicotine patches as a tobacco cigarette cessation aid. Significant reduction in tobacco smoke exposure has been demonstrated in dual users of tobacco and electronic cigarettes;40,41 however, both of these nicotine delivery systems sustain nicotine addiction.
Despite many ongoing studies to determine if e-cigarettes are useful as a smoking cessation aid, the results vary widely and are inconclusive at this time.42
E-cigarettes do not increase long-term tobacco abstinence
Contrary to popular belief, research shows that e-cigarette use among smokers is not associated with long-term tobacco abstinence.1 E-cigarette users, however, may make more attempts to quit smoking compared with smokers not using them.43 In addition, even though there is some evidence that e-cigarettes help smokers reduce the number of cigarettes smoked per day, simply reducing the daily number of cigarettes does not equate with safety.44 Smoking just one to 4 cigarettes per day poses 3 times the risk of myocardial infarction and lung cancer compared with not smoking.44 And since many individuals continue to use traditional and electronic cigarettes, they end up in double jeopardy of toxicity through exposure to the dangers of both.
A gateway to other substances of abuse?
There is also fear that nicotine exposure via e-cigarettes, especially in young people, serves as a “gateway” to tobacco consumption and other substance abuses, and increases the risk for nicotine addiction.34 Such nicotine-induced effects are a result of changes in brain chemistry, and have been documented in humans and animals.34
These concerns about negative health consequences, combined with the fact that e-cigarettes are undocumented as a smoking cessation aid, add urgency to the need for legislative and regulatory actions that hopefully can curb all nicotine exposures, particularly for our nation’s youth. In the meantime, it is important for physicians to advise patients—and the public—about the risks of e-cigarettes and the importance of quitting all forms of nicotine inhalation because nicotine—regardless of how it is delivered—is still an addictive drug.
CORRESPONDENCE
Steven Lippmann, MD, University of Louisville School of Medicine, 401 E. Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu.
› Inform patients that e-cigarette vapors contain toxic substances, including the heavy metals lead, cadmium, and nickel. A
› Educate all patients—particularly young people and those who are pregnant or lactating—about the potential health risks of e-cigarettes. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Electronic cigarettes (e-cigarettes) have become increasingly popular over the last decade. Although they are perceived by many to be safer than traditional cigarettes, many of the devices still contain nicotine, and inhaling their vapors exposes users to toxic substances, including lead, cadmium, and nickel—heavy metals that are associated with significant health problems.1 (For more on how e-cigarettes work, see “Cigarettes vs e-cigarettes: How does the experience (and cost) compare?”)
In addition, many people use e-cigarettes as a means to stop smoking, but few who do so achieve abstinence.2,3 They frequently end up utilizing both, increasing their health risks by exposing themselves to the dangers of 2 products instead of one.1
Further complicating the issue is that the manufacture and distribution of e-cigarettes has not been well regulated. Without regulation, there is no way to know with certainty how much nicotine the devices contain and what else is in them.
Things, however, are changing. The Food and Drug Administration (FDA) recently announced that e-cigarettes and other tobacco products like cigars and hookahs will now be regulated in the same way the government regulates tobacco cigarettes and smokeless tobacco.4 The rule will not take effect immediately because companies requested time to comply, but once it is enacted, packaging will be required to list what the products contain, among other changes.
Keeping up on the latest information on e-cigarettes is now—and will continue to be—important as family physicians are increasingly asked about them. What follows is a review of what we know about their potential risks.
A nicotine system developed by a pharmacist
E-cigarettes, or electronic nicotine delivery systems, were patented in 2003 by a Chinese pharmacist.5 Since their introduction to North America and Europe in 2007, the devices have become known by over 400 different brand names.6 Consumption among adults doubled by 2012, and by 2014, about 4% of US adults used e-cigarettes every day or some days.7 Many of them are dual users of tobacco and electronic cigarettes. In fact, Jenkins and colleagues reports in this issue of JFP (see "E-cigarettes: Who's using them and why?") that over half of cigarette smokers (52%) in their study use e-cigarettes, usually to either lower their cigarette consumption or aid in smoking cessation. (Throughout this article, we will use “cigarettes” and “smoking” to refer to the use of traditional tobacco cigarettes.)
In addition to concern over an increase in use among the general population, there is significant concern about the increase in e-cigarette use among US middle and high school students.1,8,9 In 2015, e-cigarettes were the most commonly used smoking product among middle and high school students, with 620,000 middle school students and nearly 2.4 million high school students using the battery-powered devices in the past 30 days.10
Many factors have contributed to the growing popularity of e-cigarettes.
- Perceived safety. With tobacco’s dangers so thoroughly documented, many advertising campaigns tout e-cigarettes as less dangerous than conventional cigarettes in terms of their ability to cause cardiac and lung diseases and low birth weights. This is largely because e-cigarettes do not produce the combustion products of tar, ash, or carbon monoxide. In addition, many consumers are mistakenly less fearful about the nicotine added to many e-cigarettes.
- Expectation that it helps smokers quit. Many smokers view e-cigarettes as an aid to smoking cessation.6 In fact, testimonials of efficacy in tobacco cessation abound in promotional materials and on the Web, and e-cigarettes are recommended by some physicians as a means to quit or lessen smoking of tobacco cigarettes.11
- Wide availability and opportunities for use. The use of electronic nicotine delivery devices is sometimes permitted in places where smoking of conventional cigarettes is banned, although rules vary widely in different parts of the country. In addition, e-cigarettes are readily available for purchase on the Internet without age verification.
- Extensive advertising. There are increasing concerns that advertising campaigns unduly target adolescents, young adults, and women.12-155 In addition to advertising, the media and social influences play significant roles in young people’s experimentation with “vaping,” the term for inhaling electronic cigarette aerosols.14,15
- Regulation, legislation remain controversial. Currently, e-cigarettes are not required to be tested before marketing,16 but that may change with the FDA’s new regulations. The British National Public Health body, Public Health England, has documented public health benefits of e-cigarettes when used as a way to quit smoking, and provides evidence that the devices are less dangerous than traditional cigarettes.17 But this issue and public policy are the subject of ongoing debate. In 2015, the United Kingdom made it illegal to sell e-cigarettes or e-liquids to people younger than 18 years of age and urged child-proof packaging.
What’s “in” an e-cigarette—and are the ingredients toxic?
Because e-cigarettes are relatively new to the global marketplace, little research exists regarding the long-term effects and safety of their use, especially among habitual users.
Vapor/refills. E-liquids may contain a variety of substances because they have been largely unregulated, but they generally include some combination of nicotine, propylene glycol, glycerin, and flavorings. In fact, up to 7000 flavors are available,6 including such kid-friendly flavors as chocolate, cherry crush, and bubble gum.
When the refills do contain nicotine, users generally derive less of the substance from the electronic devices than they do from a conventional cigarette. Researchers found that individual puffs from an e-cigarette contained 0 to 35 µg nicotine per puff.1,18 Assuming an amount at the high end of the spectrum (30 µg nicotine), it would take about 30 puffs of an e-cigarette to derive the same amount of nicotine (1 mg) typically delivered by a conventional cigarette.
The chemical make-up of the vapor and the biologic effects on animal models have been investigated using 42 different liquid refills.19,20 All contained potentially harmful compounds, but the levels were within exposure limits authorized by the FDA. These potentially dangerous chemicals include the known toxins formaldehyde, acrolein, and hydrocarbons.20
An inflammatory response to the inhalation of the vapors was demonstrated in mouse lungs; exposure to e-cigarette aerosols reduced lung glutathione—an important enzyme in maintaining oxidation-reduction balance—to a degree similar to that of cigarette smoke exposure.20 Less of the enzyme facilitates increased pulmonary inflammation.
In addition, human lung cells release pro-inflammatory cytokines when exposed to e-cigarette aerosols.20 Other health risks include:
Harm to indoor air quality/secondhand exposure. Even though e-cigarettes do not emit smoke, bystanders are exposed to the aerosol or vapor exhaled by the user, and researchers have found varying levels of such substances as formaldehyde, acetaldehyde, isoprene, acetic acid, acetone, propanol, propylene glycol, and nicotine in the air. However, it is unclear at this time whether the ultra-fine particles in the e-cigarette vapor have health effects commensurate with the emissions of conventional cigarettes.1,21,22
Cartridge refill ingestion by children. Accidental nicotine poisonings, particularly among children drawn to the colors, flavors, and scents of the e-liquids, have been problematic. In 2014, for example, over 3500 exposures occurred and more than half of those were in children younger than 6 years of age. (Exposure is defined as contact with the substance in some way including ingestion, inhalation, absorption by the skin/eyes, etc; not all exposures are poisonings or overdoses).23 Although incidence has tapered off somewhat, the American Association of Poison Control Centers reports that there were 623 exposures across all age groups between January 1, 2016 and April 30, 2016.23
Environmental impact of discarded e-cigarettes. Discarded e-cigarettes filling our landfills is a new and emerging public health concern. Their batteries, as do all batteries, pollute the land and water and have the potential to leach lead into the environment.24 Similarly, incompletely used liquid cartridges and refills may contain nicotine and heavy metals, which add to these risks.24
Explosions. Fires and explosions have been documented with e-cigarette use, mostly due to malfunctioning lithium-ion batteries.25 Thermal injuries to the face and hands can be significant.
Heavy metals. The presence of lead, cadmium, and nickel in inhaled e-cigarette vapor is another area of significant concern, particularly for younger people who might have long-term exposure.1 All 3 heavy metals are known to be toxic to humans, and safe levels of inhalation have not been established.
Inhalation and/or ingestion of lead, in particular, can cause severe neurologic damage, especially to the developing brains of children.26 Lead also results in hematologic dysfunction. Because of the risks associated with inhalation of this heavy metal, the substance was removed from gasoline years ago.
Inhaled cadmium induces kidney, liver, bone, and respiratory tract pathology27 and can cause organ failure, hypertension, anemias, fractures, osteoporosis, and/or osteomalacia.28 And inhaling nickel produces an inflammatory pulmonary reaction.29
Pregnancy/lactation. Since no clear evidence exists on the safety of e-cigarette use during pregnancy, women should avoid exposure to these vapors during the entire perinatal period. Similarly, the effects of e-cigarettes on infants who are breastfeeding are not established. Pregnant and breastfeeding women should not replace cigarettes with e-cigarettes.30,31 For pregnant women who smoke, the US Preventive Services Task Force (USPSTF) advises using only behavioral methods to stop cigarette use.32 And until more information becomes available, exposing infants and young children to e-cigarette vapor during breastfeeding is not recommended.
On the flip side, without tobacco, tar, ash, or carbon monoxide, e-cigarettes may have some advantages when compared with the use of traditional cigarettes, but that has not been substantiated.
Cigarettes vs e-cigarettes: How does the experience (and cost) compare?
If you were to ask a smoker to describe how cigarette smoking compares to using e-cigarettes, he or she would probably tell you that while the process of drawing on an e-cigarette is similar to that of a conventional cigarette, the experience in terms of reaching that state of relaxation or getting that “smoker’s high” is not.
In fact, a recent national survey of current and former smokers found that more than three-quarters of current smokers (77%) rated e-cigarettes less satisfying than conventional cigarettes and stopped using them.1 “Being less harmful” was the most highly rated reason for continuing to use the devices among people who switched from conventional to e-cigarettes.
How do they work? E-cigarettes do not burn anything and users do not light them. E-cigarettes work in much the same way as a smoke or fog machine. They use battery power (usually a rechargeable lithium battery) to heat a solution—usually containing nicotine, flavorings, and other chemicals—to the point that it turns into vapor. Much of whatever substances are in the vapor enter the bloodstream through the buccal mucosa, rather than the lungs.
Devices typically have an on/off button or switch, an atomizer containing a heating coil, a battery, and an LED light, which is designed to simulate a burning cigarette. A sensor detects when a user takes a drag and activates the atomizer and light. Some of the devices can be charged with a USB cord.
Because e-cigarettes don’t burn anything, they don’t have any smoke. They also don’t have any tar, ash, carbon monoxide, or odor (except perhaps a faint, short-lived scent matching the flavor liquid chosen). But the issues of second-hand exposure and effects on air quality are still being investigated.
With over 500 brands available, devices generally fall into one of 3 categories:2
- Cigalikes: About the same size and shape of a conventional cigarette, these cigarette look-alikes may come pre-filled with about a day’s worth of liquid and then may be discarded, or they may be non-disposable and have a replaceable cartridge.
- eGo’s: Also known as "vape pens," these devices tend to be longer and wider than cigalikes, have a more powerful battery, and usually are refillable or have a replaceable cartridge.
- Mods: Short for “modules,” these “vaporizers” tend to be the largest and most expensive type of e-cigarette. They may be refilled with e-liquid or accept replaceable cartridges and have even more powerful batteries.
What do they cost? A pack of cigarettes (containing 20 cigarettes) costs anywhere from $5 to $14, depending on where one lives.3 The price of e-cigarette devices starts at about $8 and can climb higher than $100. A 5-pack of flavor cartridges or a refill tank of e-liquid (which may last as long as about 150 cigarettes) costs about $10 to $15.4
To put this in perspective, a pack-a-day smoker in New York might spend about $5000 a year on cigarettes ($14 per pack x 365 days in a year), whereas someone who uses an e-cigarette device ($10) plus a refill tank per week ($14 x 52 weeks per year) will spend about $740 a year. (The actual cost will be higher because atomizers or devices as a whole must be replaced periodically, with some lasting only days and others lasting weeks or months, depending largely on how often one uses them. Although the cost of atomizers ranges widely, many can be found for $3-$5.)
Of course, the difference between cigarettes and e-cigarettes will be less dramatic in states where cigarettes are cheaper.
References
1. Pechacek TF, Nayak P, Gregory KR, et al. The potential that electronic delivery systems can be a disruptive technology: results from a national survey. Nicotine Tob Res. 2016. Available at: http://ntr.oxfordjournals.org/content/early/2016/05/03/ntr.ntw102.abstract. Accessed May 13, 2016.
2. Center for Environmental Health. A smoking gun: cancer-causing chemicals in e-cigarettes. Available at: http://www.ceh.org/wp-content/uploads/CEH-2015-report_A-Smoking-Gun_-Cancer-Causing-Chemicals-in-E-Cigarettes_alt.pdf. Accessed May 11, 2016.
3. Holmes H. The price of being an American. What a pack of cigarettes costs, in every state. August 28, 2015. Available at: http://www.theawl.com/2015/08/what-a-pack-of-cigarettes-costs-in-every-state. Accessed May 11, 2016.
4. Blu. How much do e-cigs cost? E-cig & vapor cigarette prices. Available at: http://www.blucigs.com/much-e-cigs-cost/. Accessed May 13, 2016.
Don’t substitute one form of nicotine for another
The USPSTF has not determined the benefit-to-harm ratio of using e-cigarettes as a smoking cessation aid, but recommends prescribing behavioral techniques and/or pharmacologic alternatives instead.32 Because the devices have been promoted as an aid to smoking cessation, intention to quit using tobacco products is a reason often stated for utilizing e-cigarettes.2,33,34 Indeed, use of e-cigarettes is much more likely among those who already utilize tobacco products.35-37
At least one study reports that e-cigarettes have efficacy similar to nicotine patches in achieving smoking abstinence among smokers who want to quit.38 Former smokers who used e-cigarettes to quit smoking reported fewer withdrawal symptoms than those who used nicotine skin patches.39 In addition, former smokers were more likely to endorse e-cigarettes than nicotine patches as a tobacco cigarette cessation aid. Significant reduction in tobacco smoke exposure has been demonstrated in dual users of tobacco and electronic cigarettes;40,41 however, both of these nicotine delivery systems sustain nicotine addiction.
Despite many ongoing studies to determine if e-cigarettes are useful as a smoking cessation aid, the results vary widely and are inconclusive at this time.42
E-cigarettes do not increase long-term tobacco abstinence
Contrary to popular belief, research shows that e-cigarette use among smokers is not associated with long-term tobacco abstinence.1 E-cigarette users, however, may make more attempts to quit smoking compared with smokers not using them.43 In addition, even though there is some evidence that e-cigarettes help smokers reduce the number of cigarettes smoked per day, simply reducing the daily number of cigarettes does not equate with safety.44 Smoking just one to 4 cigarettes per day poses 3 times the risk of myocardial infarction and lung cancer compared with not smoking.44 And since many individuals continue to use traditional and electronic cigarettes, they end up in double jeopardy of toxicity through exposure to the dangers of both.
A gateway to other substances of abuse?
There is also fear that nicotine exposure via e-cigarettes, especially in young people, serves as a “gateway” to tobacco consumption and other substance abuses, and increases the risk for nicotine addiction.34 Such nicotine-induced effects are a result of changes in brain chemistry, and have been documented in humans and animals.34
These concerns about negative health consequences, combined with the fact that e-cigarettes are undocumented as a smoking cessation aid, add urgency to the need for legislative and regulatory actions that hopefully can curb all nicotine exposures, particularly for our nation’s youth. In the meantime, it is important for physicians to advise patients—and the public—about the risks of e-cigarettes and the importance of quitting all forms of nicotine inhalation because nicotine—regardless of how it is delivered—is still an addictive drug.
CORRESPONDENCE
Steven Lippmann, MD, University of Louisville School of Medicine, 401 E. Chestnut Street, Suite 610, Louisville, KY 40202; sblipp01@louisville.edu.
1. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129:1972-1986.
2. Vickerman KA, Carpenter KM, Altman T, et al. Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine Tob Res. 2013;15:1787-1791.
3. Grana R, Popova L, Ling P. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Int Med. 2014;174:812-813.
4. U.S. Food and Drug Administration. Vaporizers, e-cigarettes, and other electronic nicotine delivery systems (ENDS). Available at: http://www.fda.gov/TobaccoProducts/Labeling/ProductsIngredientsComponents/ucm456610.htm. Accessed May 12, 2016.
5. Grana R, Benowitz N, Glantz SA. Background paper on E-cigarettes (electronic nicotine delivery systems). Center for Tobacco Control Research and Education, University of California, San Francisco, a WHO Collaborating Center on Tobacco Control. Prepared for World Health Organization Tobacco Free Initiative. December 2013. Available at: http://pvw.escholarship.org/uc/item/13p2b72n. Accessed March 31, 2014.
6. Zhu SH, Sun JY, Bonnevie E, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23:iii3-iii9.
7. Electronic Cigarette Use Among Adults: United States, 2014. NCHStats: A blog of the National Center for Health Statistics. Available at: http://nchstats.com/2015/10/28/electronic-cigarette-use-among-adults-united-states-2014/. Accessed April 22, 2016.
8. Centers for Disease Control and Prevention. E-cigarette use more than doubles among U.S. middle and high school students from 2011-2012. Available at: http://www.cdc.gov/media/releases/2013/p0905-ecigarette-use.html. Accessed April 22, 2016.
9. Centers for Disease Control and Prevention. Notes from the field: electronic cigarette use among middle and high school students — United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 2013;62:729-730.
10. Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011-2015. MMWR Morb Mortal Wkly Rpt. 2016;65:361-367.
11. Kandra KL, Ranney LM, Lee JG, et al. Physicians’ attitudes and use of e-cigarettes as cessation devices, North Carolina, 2013. PloS One. 2014;9:e103462.
12. Schraufnagel DE. Electronic cigarettes: vulnerability of youth. Pediatr Allergy Immunol Pulmonol. 2015;28:2-6.
13. White J, Li J, Newcombe R, et al. Tripling use of electronic cigarettes among New Zealand adolescents between 2012 and 2014. J Adolesc Health. 2015;56:522-528.
14. Duke JC, Lee YO, Kim AE, et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134:29-36.
15. Huang J, Kornfield R, Szczypka G, et al. A cross-sectional examination of marketing of electronic cigarettes on Twitter. Tob Control. 2014;23:iii26-iii30.
16. Rojewski AM, Coleman N, Toll BA. Position Statement: Emerging policy issues regarding electronic nicotine delivery systems: a need for regulation. Society of Behavioral Medicine. 2016. Available at: http://www.sbm.org/UserFiles/file/e-cig-statement_v2_lores.pdf. Accessed April 22, 2016.
17. McNeill A, Brose LS, Calder R, et al. E-cigarettes: an evidence update. A report commissioned by Public Health England. 2015. Available at: https://www.gov.uk/government/publications/e-cigarettes-an-evidence-update. Accessed April 22, 2016.
18. Goniewicz ML, Kuma T, Gawron M, et al. Nicotine levels in electronic cigarettes. Nicotine Tob Res. 2013;15:158-166.
19. Varlet V, Farsalinos K, Augsburger M, et al. Toxicity assessment of refill liquids for electronic cigarettes. Int J Environ Res Public Health. 2015;12:4796-4815.
20. Lerner CA, Sundar IK, Yao H, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One. 2015;10:e0116732.
21. Schober W, Szendrei K, Matzen W, et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217:628-637.
22. Schripp T, Markewitz D, Uhde E, et al. Does e-cigarette consumption cause passive vaping? Indoor Air. 2013;23:25-31.
23. The American Association of Poison Control Centers. E-cigarettes and liquid nicotine. Available at: http://www.aapcc.org/alerts/e-cigarettes/. Accessed May 12, 2016.
24. Krause MJ, Townsend TG. Hazardous waste status of discarded electronic cigarettes. Waste Manag. 2015;39:57-62.
25. U.S. Fire Administration. Electronic cigarette fires and explosions. October 2014. Available at: https://www.usfa.fema.gov/downloads/pdf/publications/electronic_cigarettes.pdf. Accessed May 17, 2016.
26. Skerfving S, Löfmark L, Lundh T, et al. Late effects of low blood lead concentrations in children on school performance and cognitive functions. Neurotoxicology. 2015;49:114-120.
27. Bernhoft RA. Cadmium toxicity and treatment. Scientific World Journal. 2013;394652.
28. Agency for Toxic Substances and Disease Registry. Case studies in environmental medicine (CSEM) Cadmium Toxicity. Available at: http://www.atsdr.cdc.gov/csem/cadmium/docs/cadmium.pdf. Accessed April 22, 2016.
29. Das KK, Buchner V. Effect of nickel exposure on peripheral tissues: role of oxidative stress in toxicity and possible protection by ascorbic acid. Rev Environ Health. 2007;22:157-173.
30. England LJ, Bunnell RE, Pechacek TF, et al. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am J Prev Med. 2015;49:286-293.
31. Suter MA, Mastrobattista J, Sachs M, et al. Is there evidence for potential harm of electronic cigarette use in pregnancy? Birth defects research. Birth Defects Res A Clin Mol Teratol. 2015;103:186-195.
32. U.S. Preventive Services Task Force. Draft Recommendation Statement. Tobacco smoking cessation in adults and pregnant women: behavioral and pharmacotherapy interventions. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement147/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions1. Accessed March 22, 2016.
33. Peters EN, Harrell PT, Hendricks PS, et al. Electronic cigarettes in adults in outpatient substance use treatment: awareness, perceptions, use, and reasons for use. Am J Addict. 2015;24:233-239.
34. Kandel ER, Kandel DB. A molecular basis for nicotine as a gateway drug. N Engl J Med. 2014;371:932-943.
35. King BA, Patel R, Nguyen KH, et al. Trends in awareness and use of electronic cigarettes among US Adults, 2010-2013. Nicotine Tob Res. 2015;17:219-227.
36. McMillen RC, Gottlieb MA, Shaefer RM, et al. Trends in electronic cigarette use among U.S. adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;1195-1202.
37. Lee S, Grana RA, Glantz SA. Electronic cigarette use among Korean adolescents: a cross-sectional study of market penetration, dual use, and relationship to quit attempts and former smoking. J Adolesc Health. 2014;54:684-690.
38. Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382:1629-1637.
39. Nelson VA, Goniewicz ML, Beard E, et al. Comparison of the characteristics of long-term users of electronic cigarettes versus nicotine replacement therapy: a cross-sectional survey of English ex-smokers and current smokers. Drug Alcohol Depend. 2015;153:300-305.
40. Caponnetto P, Campagna D, Cibella F, et al. Efficiency and safety of an electronic cigarette (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One. 2013;8:e66317.
41. Polosa R, Caponnetto P, Morjaria JB, et al. Effect of an electronic nicotine delivery device (e-Cigarette) on smoking reduction and cessation: a prospective 6-month pilot study. BMC Public Health. 2011;11:786.
42. Malas M, van der Tempel J, Schwartz R, et al. Electronic cigarettes for smoking cessation: a systematic review. Nicotine Tob Res. 2016. [Epub ahead of print].
43. Brose LS, Hitchman SC, Brown J, et al. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction. 2015;110:1160-1168.
44. Bjartveit K, Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tob Control. 2005;14:315-320.
1. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129:1972-1986.
2. Vickerman KA, Carpenter KM, Altman T, et al. Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine Tob Res. 2013;15:1787-1791.
3. Grana R, Popova L, Ling P. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Int Med. 2014;174:812-813.
4. U.S. Food and Drug Administration. Vaporizers, e-cigarettes, and other electronic nicotine delivery systems (ENDS). Available at: http://www.fda.gov/TobaccoProducts/Labeling/ProductsIngredientsComponents/ucm456610.htm. Accessed May 12, 2016.
5. Grana R, Benowitz N, Glantz SA. Background paper on E-cigarettes (electronic nicotine delivery systems). Center for Tobacco Control Research and Education, University of California, San Francisco, a WHO Collaborating Center on Tobacco Control. Prepared for World Health Organization Tobacco Free Initiative. December 2013. Available at: http://pvw.escholarship.org/uc/item/13p2b72n. Accessed March 31, 2014.
6. Zhu SH, Sun JY, Bonnevie E, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23:iii3-iii9.
7. Electronic Cigarette Use Among Adults: United States, 2014. NCHStats: A blog of the National Center for Health Statistics. Available at: http://nchstats.com/2015/10/28/electronic-cigarette-use-among-adults-united-states-2014/. Accessed April 22, 2016.
8. Centers for Disease Control and Prevention. E-cigarette use more than doubles among U.S. middle and high school students from 2011-2012. Available at: http://www.cdc.gov/media/releases/2013/p0905-ecigarette-use.html. Accessed April 22, 2016.
9. Centers for Disease Control and Prevention. Notes from the field: electronic cigarette use among middle and high school students — United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 2013;62:729-730.
10. Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011-2015. MMWR Morb Mortal Wkly Rpt. 2016;65:361-367.
11. Kandra KL, Ranney LM, Lee JG, et al. Physicians’ attitudes and use of e-cigarettes as cessation devices, North Carolina, 2013. PloS One. 2014;9:e103462.
12. Schraufnagel DE. Electronic cigarettes: vulnerability of youth. Pediatr Allergy Immunol Pulmonol. 2015;28:2-6.
13. White J, Li J, Newcombe R, et al. Tripling use of electronic cigarettes among New Zealand adolescents between 2012 and 2014. J Adolesc Health. 2015;56:522-528.
14. Duke JC, Lee YO, Kim AE, et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134:29-36.
15. Huang J, Kornfield R, Szczypka G, et al. A cross-sectional examination of marketing of electronic cigarettes on Twitter. Tob Control. 2014;23:iii26-iii30.
16. Rojewski AM, Coleman N, Toll BA. Position Statement: Emerging policy issues regarding electronic nicotine delivery systems: a need for regulation. Society of Behavioral Medicine. 2016. Available at: http://www.sbm.org/UserFiles/file/e-cig-statement_v2_lores.pdf. Accessed April 22, 2016.
17. McNeill A, Brose LS, Calder R, et al. E-cigarettes: an evidence update. A report commissioned by Public Health England. 2015. Available at: https://www.gov.uk/government/publications/e-cigarettes-an-evidence-update. Accessed April 22, 2016.
18. Goniewicz ML, Kuma T, Gawron M, et al. Nicotine levels in electronic cigarettes. Nicotine Tob Res. 2013;15:158-166.
19. Varlet V, Farsalinos K, Augsburger M, et al. Toxicity assessment of refill liquids for electronic cigarettes. Int J Environ Res Public Health. 2015;12:4796-4815.
20. Lerner CA, Sundar IK, Yao H, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One. 2015;10:e0116732.
21. Schober W, Szendrei K, Matzen W, et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217:628-637.
22. Schripp T, Markewitz D, Uhde E, et al. Does e-cigarette consumption cause passive vaping? Indoor Air. 2013;23:25-31.
23. The American Association of Poison Control Centers. E-cigarettes and liquid nicotine. Available at: http://www.aapcc.org/alerts/e-cigarettes/. Accessed May 12, 2016.
24. Krause MJ, Townsend TG. Hazardous waste status of discarded electronic cigarettes. Waste Manag. 2015;39:57-62.
25. U.S. Fire Administration. Electronic cigarette fires and explosions. October 2014. Available at: https://www.usfa.fema.gov/downloads/pdf/publications/electronic_cigarettes.pdf. Accessed May 17, 2016.
26. Skerfving S, Löfmark L, Lundh T, et al. Late effects of low blood lead concentrations in children on school performance and cognitive functions. Neurotoxicology. 2015;49:114-120.
27. Bernhoft RA. Cadmium toxicity and treatment. Scientific World Journal. 2013;394652.
28. Agency for Toxic Substances and Disease Registry. Case studies in environmental medicine (CSEM) Cadmium Toxicity. Available at: http://www.atsdr.cdc.gov/csem/cadmium/docs/cadmium.pdf. Accessed April 22, 2016.
29. Das KK, Buchner V. Effect of nickel exposure on peripheral tissues: role of oxidative stress in toxicity and possible protection by ascorbic acid. Rev Environ Health. 2007;22:157-173.
30. England LJ, Bunnell RE, Pechacek TF, et al. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am J Prev Med. 2015;49:286-293.
31. Suter MA, Mastrobattista J, Sachs M, et al. Is there evidence for potential harm of electronic cigarette use in pregnancy? Birth defects research. Birth Defects Res A Clin Mol Teratol. 2015;103:186-195.
32. U.S. Preventive Services Task Force. Draft Recommendation Statement. Tobacco smoking cessation in adults and pregnant women: behavioral and pharmacotherapy interventions. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement147/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions1. Accessed March 22, 2016.
33. Peters EN, Harrell PT, Hendricks PS, et al. Electronic cigarettes in adults in outpatient substance use treatment: awareness, perceptions, use, and reasons for use. Am J Addict. 2015;24:233-239.
34. Kandel ER, Kandel DB. A molecular basis for nicotine as a gateway drug. N Engl J Med. 2014;371:932-943.
35. King BA, Patel R, Nguyen KH, et al. Trends in awareness and use of electronic cigarettes among US Adults, 2010-2013. Nicotine Tob Res. 2015;17:219-227.
36. McMillen RC, Gottlieb MA, Shaefer RM, et al. Trends in electronic cigarette use among U.S. adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;1195-1202.
37. Lee S, Grana RA, Glantz SA. Electronic cigarette use among Korean adolescents: a cross-sectional study of market penetration, dual use, and relationship to quit attempts and former smoking. J Adolesc Health. 2014;54:684-690.
38. Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382:1629-1637.
39. Nelson VA, Goniewicz ML, Beard E, et al. Comparison of the characteristics of long-term users of electronic cigarettes versus nicotine replacement therapy: a cross-sectional survey of English ex-smokers and current smokers. Drug Alcohol Depend. 2015;153:300-305.
40. Caponnetto P, Campagna D, Cibella F, et al. Efficiency and safety of an electronic cigarette (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One. 2013;8:e66317.
41. Polosa R, Caponnetto P, Morjaria JB, et al. Effect of an electronic nicotine delivery device (e-Cigarette) on smoking reduction and cessation: a prospective 6-month pilot study. BMC Public Health. 2011;11:786.
42. Malas M, van der Tempel J, Schwartz R, et al. Electronic cigarettes for smoking cessation: a systematic review. Nicotine Tob Res. 2016. [Epub ahead of print].
43. Brose LS, Hitchman SC, Brown J, et al. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction. 2015;110:1160-1168.
44. Bjartveit K, Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tob Control. 2005;14:315-320.
From The Journal of Family Practice | 2016;65(6):380-385.