User login
Topical honey for diabetic foot ulcers
A 79-year-old man with type 2 diabetes mellitus developed heel and forefoot ulcers, for which he received currently recommended therapy,1-5 including an off-loading orthotic, systemic antibiotics selected by infectious disease consultants, and topical therapies directed by a wound care expert.
After 14 months of care costing more than $390,000—which was the cost of 5 hospitalizations and 4 surgeries—the ulcers measured 8 x 5 cm and 3 x 3 cm. Deep tissue cultures grew methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), and Pseudomonas.
During this time the patient lost 2 toes but refused below-the-knee amputation. He was informed by 2 different surgical teams that without this surgery he would likely die. This opinion was based on the patient’s recurrent episodes of heel osteomyelitis and multiple medical complications, including acute renal failure from culture-specific antibiotics.
The patient was eventually discharged to his home at his request, after consulting with his family and the hospital’s ethics committee. He lost a third toe before consenting to a trial of topical honey.
Course of treatment with honey
Once-daily, thick applications of ordinary honey purchased at a supermarket were smeared on gauze 4x4s and placed on the wounds, which were then wrapped. Oral antibiotics and saline dressings were discontinued, but otherwise treatment was unchanged. Since the patient’s family purchased and applied the honey, the cost of this therapy was merely that of the dressings. Dressing changes were painless and the serum glucose remained in excellent control.
Granulation tissue appeared within 2 weeks; in 6 to 12 months the ulcers resolved (see FIGURES 1-6). Two years later, the ulcers have not recurred; the patient ambulates with a walker and reports improved quality-of-life.
FIGURE 1
After 3 weeks
Forefoot ulcer after 3 weeks of honey therapy.
FIGURE 2
After 3 months
Forefoot ulcer after 3 months of honey therapy.
FIGURE 3
After 12 months
Forefoot ulcer after 12 months of honey therapy.
FIGURE 4
After 3 weeks
Heel ulcer after 3 weeks of honey therapy.
FIGURE 5
After 3 months
Heel ulcer after 3 months of honey therapy.
FIGURE 6
After 6 months
Heel ulcer after 6 months of honey therapy.
Honey as wound treatment in the medical literature
Honey has been used to treat wounds for millennia,6 but the medical evidence supporting its use is limited. While there are many case reports of honey’s effectiveness, 7 controlled trials demonstrating effectiveness for treating burns and wounds are limited by poor quality and the use of nonstandard controls,7 while another trial found minimal benefit when “a very thin smear” was used.8 Concerns about wound infection from Clostridium spores9 appear unfounded, as no such complication has been described in more than 500 reports in the literature,10 and honey has repeatedly been shown to suppress bacterial growth.11
Gamma-irradiated “medical” honey is available, which has also been selected for its potent antibacterial properties, although most of the cases in the medical literature have used raw honey. A burning or stinging sensation has been described with honey’s topical use.
As rates of diabetes increase, it is important to identify effective strategies to reduce amputation rates, both to improve quality of life12 and to decrease cost.13 Given honey’s potential for improved outcomes, cost savings, and decreasing antibiotic use and resistance, we advocate publicly funded randomized controlled trials to determine its efficacy. Meanwhile, we encourage others to consider topical honey therapy for patients with refractory diabetic foot ulcers.
Acknowledgments
The authors gratefully acknowledge Guido Majno, MD, for his scholarship and generous assistance.
CORRESPONDING AUTHOR:
Jennifer J. Eddy, MD, Assistant Professor of Family Medicine, University of Wisconsin Medical School, 617 W. Clairemont Avenue, Eau Claire WI 54703. E-mail: jjemdg@sbcglobal.net
1. Consensus Development Conference on Diabetic Foot Wound Care: 7-8 April 1999, Boston, Massachusetts. Diabetes Care 1999;22:1354-1360.
2. Boulton AJM, Kisner RS, Vileikyte L. Clinical practice. Neuropathic diabetic foot ulcers. N Engl J Med 2004;351:48-55.
3. Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet 2003;361:1545-1551.
4. Watkins PJ. ABC of diabetes: the diabetic foot. BMJ 2003;326:977-980.
5. Frykberg RG. Diabetic foot ulcers: Pathogenesis and management. Am Fam Phys 2002;66:1655-1662.
6. Majno G. The Healing Hand: Man and Wound in the Ancient World. Cambridge, Mass: Harvard University Press;1975.
7. Moore OA, Smith LA, Campbell F, Seers K, McQuay HJ, Moore RA. Systematic review of the use of honey as a wound dressing. BMC Comp & Alt Med 2001;1(1):2.-
8. Wood B, Rademaker M, Molan PC. Manuka honey, a low cost ulcer dressing. NZ Med J 1997;110:107.-
9. Postmes T. Honey for wounds, ulcers, and skin graft preservation (letter). Lancet 1993;34:756-757.
10. Molan PC. Clinical usage of honey as a wound dressing: an update. J Wound Care 2004;13(9):353-356.
11. Molan PC. Potential of honey in the treatment of wounds and burns. Am J Clin Dermatology 2001;2(1):13-19.
12. Lindholm C. Quality of life in chronic leg ulcer patients. Acta Derm Venereol 1993;73:440-443.
13. Ollendorf AD, Kotsanos JG, Wishner WJ, et al. Potential economic benefits of lower-extremity amputation prevention strategies in diabetes. Diabetes Care 1998;21:1240-1245.
A 79-year-old man with type 2 diabetes mellitus developed heel and forefoot ulcers, for which he received currently recommended therapy,1-5 including an off-loading orthotic, systemic antibiotics selected by infectious disease consultants, and topical therapies directed by a wound care expert.
After 14 months of care costing more than $390,000—which was the cost of 5 hospitalizations and 4 surgeries—the ulcers measured 8 x 5 cm and 3 x 3 cm. Deep tissue cultures grew methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), and Pseudomonas.
During this time the patient lost 2 toes but refused below-the-knee amputation. He was informed by 2 different surgical teams that without this surgery he would likely die. This opinion was based on the patient’s recurrent episodes of heel osteomyelitis and multiple medical complications, including acute renal failure from culture-specific antibiotics.
The patient was eventually discharged to his home at his request, after consulting with his family and the hospital’s ethics committee. He lost a third toe before consenting to a trial of topical honey.
Course of treatment with honey
Once-daily, thick applications of ordinary honey purchased at a supermarket were smeared on gauze 4x4s and placed on the wounds, which were then wrapped. Oral antibiotics and saline dressings were discontinued, but otherwise treatment was unchanged. Since the patient’s family purchased and applied the honey, the cost of this therapy was merely that of the dressings. Dressing changes were painless and the serum glucose remained in excellent control.
Granulation tissue appeared within 2 weeks; in 6 to 12 months the ulcers resolved (see FIGURES 1-6). Two years later, the ulcers have not recurred; the patient ambulates with a walker and reports improved quality-of-life.
FIGURE 1
After 3 weeks
Forefoot ulcer after 3 weeks of honey therapy.
FIGURE 2
After 3 months
Forefoot ulcer after 3 months of honey therapy.
FIGURE 3
After 12 months
Forefoot ulcer after 12 months of honey therapy.
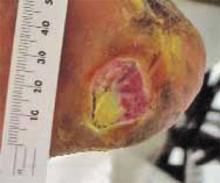
FIGURE 4
After 3 weeks
Heel ulcer after 3 weeks of honey therapy.
FIGURE 5
After 3 months
Heel ulcer after 3 months of honey therapy.
FIGURE 6
After 6 months
Heel ulcer after 6 months of honey therapy.
Honey as wound treatment in the medical literature
Honey has been used to treat wounds for millennia,6 but the medical evidence supporting its use is limited. While there are many case reports of honey’s effectiveness, 7 controlled trials demonstrating effectiveness for treating burns and wounds are limited by poor quality and the use of nonstandard controls,7 while another trial found minimal benefit when “a very thin smear” was used.8 Concerns about wound infection from Clostridium spores9 appear unfounded, as no such complication has been described in more than 500 reports in the literature,10 and honey has repeatedly been shown to suppress bacterial growth.11
Gamma-irradiated “medical” honey is available, which has also been selected for its potent antibacterial properties, although most of the cases in the medical literature have used raw honey. A burning or stinging sensation has been described with honey’s topical use.
As rates of diabetes increase, it is important to identify effective strategies to reduce amputation rates, both to improve quality of life12 and to decrease cost.13 Given honey’s potential for improved outcomes, cost savings, and decreasing antibiotic use and resistance, we advocate publicly funded randomized controlled trials to determine its efficacy. Meanwhile, we encourage others to consider topical honey therapy for patients with refractory diabetic foot ulcers.
Acknowledgments
The authors gratefully acknowledge Guido Majno, MD, for his scholarship and generous assistance.
CORRESPONDING AUTHOR:
Jennifer J. Eddy, MD, Assistant Professor of Family Medicine, University of Wisconsin Medical School, 617 W. Clairemont Avenue, Eau Claire WI 54703. E-mail: jjemdg@sbcglobal.net
A 79-year-old man with type 2 diabetes mellitus developed heel and forefoot ulcers, for which he received currently recommended therapy,1-5 including an off-loading orthotic, systemic antibiotics selected by infectious disease consultants, and topical therapies directed by a wound care expert.
After 14 months of care costing more than $390,000—which was the cost of 5 hospitalizations and 4 surgeries—the ulcers measured 8 x 5 cm and 3 x 3 cm. Deep tissue cultures grew methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), and Pseudomonas.
During this time the patient lost 2 toes but refused below-the-knee amputation. He was informed by 2 different surgical teams that without this surgery he would likely die. This opinion was based on the patient’s recurrent episodes of heel osteomyelitis and multiple medical complications, including acute renal failure from culture-specific antibiotics.
The patient was eventually discharged to his home at his request, after consulting with his family and the hospital’s ethics committee. He lost a third toe before consenting to a trial of topical honey.
Course of treatment with honey
Once-daily, thick applications of ordinary honey purchased at a supermarket were smeared on gauze 4x4s and placed on the wounds, which were then wrapped. Oral antibiotics and saline dressings were discontinued, but otherwise treatment was unchanged. Since the patient’s family purchased and applied the honey, the cost of this therapy was merely that of the dressings. Dressing changes were painless and the serum glucose remained in excellent control.
Granulation tissue appeared within 2 weeks; in 6 to 12 months the ulcers resolved (see FIGURES 1-6). Two years later, the ulcers have not recurred; the patient ambulates with a walker and reports improved quality-of-life.
FIGURE 1
After 3 weeks
Forefoot ulcer after 3 weeks of honey therapy.
FIGURE 2
After 3 months
Forefoot ulcer after 3 months of honey therapy.
FIGURE 3
After 12 months
Forefoot ulcer after 12 months of honey therapy.
FIGURE 4
After 3 weeks
Heel ulcer after 3 weeks of honey therapy.
FIGURE 5
After 3 months
Heel ulcer after 3 months of honey therapy.
FIGURE 6
After 6 months
Heel ulcer after 6 months of honey therapy.
Honey as wound treatment in the medical literature
Honey has been used to treat wounds for millennia,6 but the medical evidence supporting its use is limited. While there are many case reports of honey’s effectiveness, 7 controlled trials demonstrating effectiveness for treating burns and wounds are limited by poor quality and the use of nonstandard controls,7 while another trial found minimal benefit when “a very thin smear” was used.8 Concerns about wound infection from Clostridium spores9 appear unfounded, as no such complication has been described in more than 500 reports in the literature,10 and honey has repeatedly been shown to suppress bacterial growth.11
Gamma-irradiated “medical” honey is available, which has also been selected for its potent antibacterial properties, although most of the cases in the medical literature have used raw honey. A burning or stinging sensation has been described with honey’s topical use.
As rates of diabetes increase, it is important to identify effective strategies to reduce amputation rates, both to improve quality of life12 and to decrease cost.13 Given honey’s potential for improved outcomes, cost savings, and decreasing antibiotic use and resistance, we advocate publicly funded randomized controlled trials to determine its efficacy. Meanwhile, we encourage others to consider topical honey therapy for patients with refractory diabetic foot ulcers.
Acknowledgments
The authors gratefully acknowledge Guido Majno, MD, for his scholarship and generous assistance.
CORRESPONDING AUTHOR:
Jennifer J. Eddy, MD, Assistant Professor of Family Medicine, University of Wisconsin Medical School, 617 W. Clairemont Avenue, Eau Claire WI 54703. E-mail: jjemdg@sbcglobal.net
1. Consensus Development Conference on Diabetic Foot Wound Care: 7-8 April 1999, Boston, Massachusetts. Diabetes Care 1999;22:1354-1360.
2. Boulton AJM, Kisner RS, Vileikyte L. Clinical practice. Neuropathic diabetic foot ulcers. N Engl J Med 2004;351:48-55.
3. Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet 2003;361:1545-1551.
4. Watkins PJ. ABC of diabetes: the diabetic foot. BMJ 2003;326:977-980.
5. Frykberg RG. Diabetic foot ulcers: Pathogenesis and management. Am Fam Phys 2002;66:1655-1662.
6. Majno G. The Healing Hand: Man and Wound in the Ancient World. Cambridge, Mass: Harvard University Press;1975.
7. Moore OA, Smith LA, Campbell F, Seers K, McQuay HJ, Moore RA. Systematic review of the use of honey as a wound dressing. BMC Comp & Alt Med 2001;1(1):2.-
8. Wood B, Rademaker M, Molan PC. Manuka honey, a low cost ulcer dressing. NZ Med J 1997;110:107.-
9. Postmes T. Honey for wounds, ulcers, and skin graft preservation (letter). Lancet 1993;34:756-757.
10. Molan PC. Clinical usage of honey as a wound dressing: an update. J Wound Care 2004;13(9):353-356.
11. Molan PC. Potential of honey in the treatment of wounds and burns. Am J Clin Dermatology 2001;2(1):13-19.
12. Lindholm C. Quality of life in chronic leg ulcer patients. Acta Derm Venereol 1993;73:440-443.
13. Ollendorf AD, Kotsanos JG, Wishner WJ, et al. Potential economic benefits of lower-extremity amputation prevention strategies in diabetes. Diabetes Care 1998;21:1240-1245.
1. Consensus Development Conference on Diabetic Foot Wound Care: 7-8 April 1999, Boston, Massachusetts. Diabetes Care 1999;22:1354-1360.
2. Boulton AJM, Kisner RS, Vileikyte L. Clinical practice. Neuropathic diabetic foot ulcers. N Engl J Med 2004;351:48-55.
3. Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet 2003;361:1545-1551.
4. Watkins PJ. ABC of diabetes: the diabetic foot. BMJ 2003;326:977-980.
5. Frykberg RG. Diabetic foot ulcers: Pathogenesis and management. Am Fam Phys 2002;66:1655-1662.
6. Majno G. The Healing Hand: Man and Wound in the Ancient World. Cambridge, Mass: Harvard University Press;1975.
7. Moore OA, Smith LA, Campbell F, Seers K, McQuay HJ, Moore RA. Systematic review of the use of honey as a wound dressing. BMC Comp & Alt Med 2001;1(1):2.-
8. Wood B, Rademaker M, Molan PC. Manuka honey, a low cost ulcer dressing. NZ Med J 1997;110:107.-
9. Postmes T. Honey for wounds, ulcers, and skin graft preservation (letter). Lancet 1993;34:756-757.
10. Molan PC. Clinical usage of honey as a wound dressing: an update. J Wound Care 2004;13(9):353-356.
11. Molan PC. Potential of honey in the treatment of wounds and burns. Am J Clin Dermatology 2001;2(1):13-19.
12. Lindholm C. Quality of life in chronic leg ulcer patients. Acta Derm Venereol 1993;73:440-443.
13. Ollendorf AD, Kotsanos JG, Wishner WJ, et al. Potential economic benefits of lower-extremity amputation prevention strategies in diabetes. Diabetes Care 1998;21:1240-1245.