User login
Asthma management: How the guidelines compare
CASE
Erica S*, age 22, has intermittent asthma and presents to your clinic to discuss refills of her albuterol inhaler. Two years ago, she was hospitalized for a severe asthma exacerbation because she was unable to afford medications. Since then, her asthma has generally been well controlled, and she needs to use albuterol only 1 or 2 times per month. Ms. S says she has no morning chest tightness or nocturnal coughing, but she does experience increased wheezing and shortness of breath with activity.
What would you recommend? Would your recommendation differ if she had persistent asthma?
* The patient’s name has been changed to protect her identity .
As of 2020, more than 20 million adults and 4 million children younger than 18 years of age in the United States were living with asthma.1 In 2019 alone, there were more than 1.8 million asthma-related emergency department visits for adults, and more than 790,000 asthma-related emergency department visits for children. Asthma caused more than 4000 deaths in the United States in 2020.1 Given the scale of the burden of asthma, it is not surprising that approximately 60% of all asthma visits occur in primary care settings,2 making it essential that primary care physicians stay abreast of recent developments in asthma diagnosis and management.
Since 1991, the major guidance on best practices for asthma management in the United States has been provided by the National Heart, Lung, and Blood Institute (NHLBI)’s National Asthma Education and Prevention Program (NAEPP). Its last major update on asthma was released in 2007 as the Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma (EPR-3).3 Since that time, there has been significant progress in our understanding of asthma as a complex spectrum of phenotypes, which has advanced our knowledge of pathophysiology and helped refine treatment. In contrast to the NAEPP, the Global Initiative for Asthma (GINA) has published annual updates on asthma management incorporating up-to-date information.4 In response to the continuously evolving body of knowledge on asthma, the NAEPP Coordinating Committee Expert Panel Working Group published the 2020 Focused Updates to the Asthma Management Guidelines.5
Given the vast resources available on asthma, our purpose in this article is not to provide a comprehensive review of the stepwise approach to asthma management, but instead to summarize the major points presented in the 2020 Focused Updates and how these compare and contrast with the latest guidance from GINA.
A heterogeneous disease
Asthma is a chronic respiratory disease characterized by both variable symptoms and airflow limitation that change over time, often in response to external triggers such as exercise, allergens, and viral respiratory infections. Common symptoms include wheezing, cough, chest tightness, and shortness of breath. Despite the common symptomatology, asthma is a heterogeneous disease with several recognizable phenotypes including allergic, nonallergic, and asthma with persistent airflow limitation.
Continue to: The airflow limitation...
The airflow limitation in asthma occurs through both airway hyperresponsiveness to external stimuli and chronic airway inflammation. Airway constriction is regulated by nerves to the smooth muscles of the airway. Beta-2 nerve receptors have long been the target of asthma therapy with both short-acting beta-2 agonists (SABAs) as rescue treatment and long-acting beta-2 agonists (LABAs) as maintenance therapy.3,4 However, there is increasing evidence that cholinergic nerves also have a role in airway regulation in asthma, and long-acting muscarinic antagonists (LAMAs) have recently shown benefit as add-on therapy in some types of asthma.4-6 Inhaled corticosteroids (ICSs) have long held an important role in reducing airway inflammation, especially in the setting of allergic or eosinophilic inflammation.3-5
Spirometry is essential to asthma Dx—but what about FeNO?
The mainstay of asthma diagnosis is confirming both a history of variable respiratory symptoms and variable expiratory airflow limitation exhibited by spirometry. Obstruction is defined as a reduced forced expiratory volume in 1 second (FEV1) and as a decreased ratio of FEV1 over forced vital capacity (FVC) based on predicted values. An increase of at least 12% in FEV1 post bronchodilator use indicates asthma for adolescents and adults.
More recently, studies have examined the role of fractional exhaled nitric oxide (FeNO) in the diagnosis of asthma. The 2020 Focused Updates report states that FeNO may be useful when the diagnosis of asthma is uncertain using initial history, physical exam, and spirometry findings, or when spirometry cannot be performed reliably.5 Levels of FeNO > 50 ppb make eosinophilic inflammation and treatment response to an ICS more likely. FeNO levels < 25 ppb make inflammatory asthma less likely and should prompt a search for an alternate diagnosis.5 For patients with FeNO of 25 to 50 ppb, more detailed clinical context is needed. In contrast, the 2022 GINA updates conclude that FeNO is not yet an established diagnostic tool for asthma.4
Management
When to start and adjust an ICS
ICSs continue to be the primary controller treatment for patients with asthma. However, the NAEPP and GINA have provided different guidance on how to initiate step therapy (TABLE3-5). NAEPP focuses on severity classification, while GINA recommends treatment initiation based on presenting symptoms. Since both guidelines recommend early follow-up and adjustment of therapy according to level of control, this difference becomes less apparent in ongoing care.
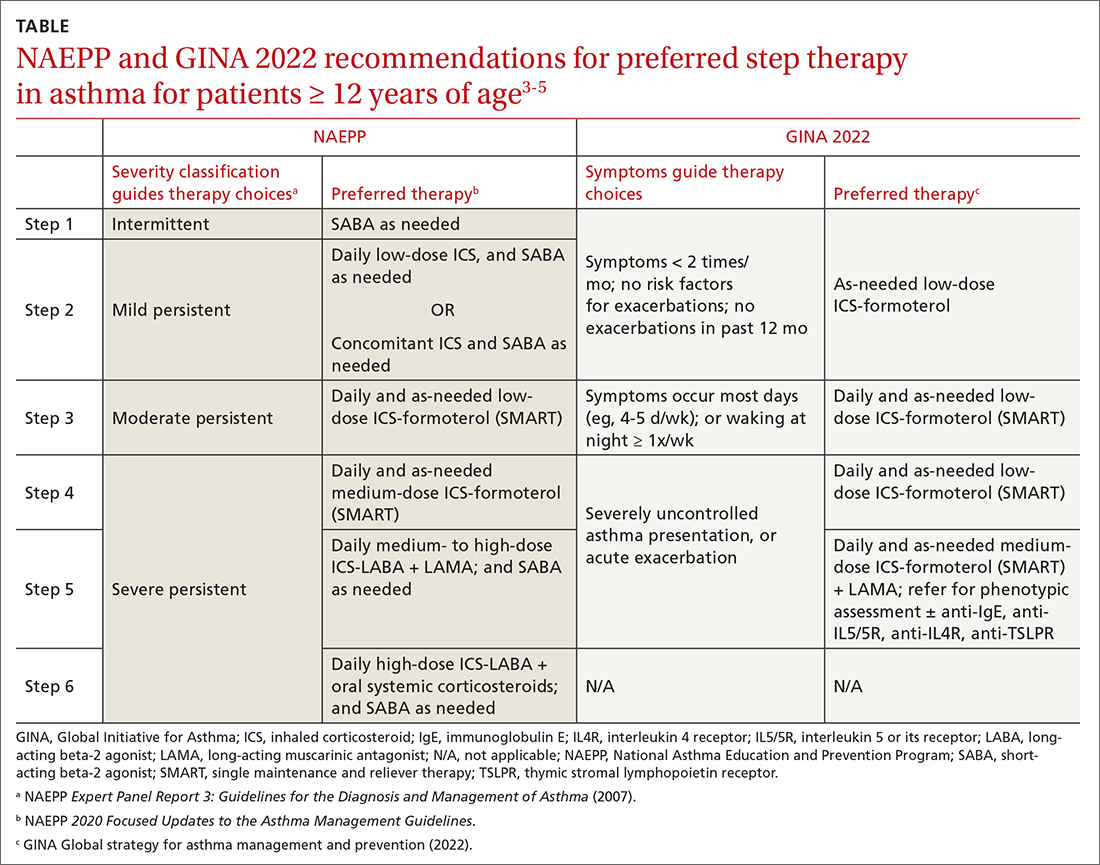
A more fundamental difference is seen in the recommended therapies for each step (TABLE3-5). Whereas the 2020 Focused Updates prefers a SABA as needed in step 1, GINA favors a low-dose combination of ICS-formoterol as needed. The GINA recommendation is driven by supportive evidence for early initiation of low-dose ICS in any patient with asthma for greater improvement in lung function. This also addresses concerns that overuse of as-needed SABAs may increase the risk for severe exacerbations. Evidence also indicates that the risk for asthma-related death and urgent asthma-related health care increases when a patient takes a SABA as needed as monotherapy compared with ICS therapy, even with good symptom control.7,8
Continue to: Dosing of an ICS
Dosing of an ICS is based on step therapy regardless of the guideline used and is given at a total daily amount—low, medium, and high—for each age group. When initiating an ICS, consider differences between available treatment options (eg, cost, administration technique, likely patient adherence, patient preferences) and employ shared decision-making strategies. Dosing may need to be limited depending on the commercially available product, especially when used in combination with a LABA. However, as GINA emphasizes, a low-dose ICS provides the most clinical benefit. A high-dose ICS is needed by very few patients and is associated with greater risk for local and systemic adverse effects, such as adrenal suppression. With these considerations, both guidelines recommend using the lowest effective ICS dose and stepping up and down according to the patient’s comfort level.
Give an ICS time to work. Although an ICS can begin to reduce inflammation within days of initiation, the full benefit may be evident only after 2 to 3 months.4 Once the patient’s asthma is well controlled for 3 months, stepping down the dose can be considered and approached carefully. Complete cessation of ICSs is associated with significantly higher risk for exacerbations. Therefore, a general recommendation is to step down an ICS by 50% or reduce ICS-LABA from twice-daily administration to once daily. Risk for exacerbation after step-down therapy is heightened if the patient has a history of exacerbation or an emergency department visit in the past 12 months, a low baseline FEV1, or a loss of control during a dose reduction (ie, airway hyperresponsiveness and sputum eosinophilia).
Weigh the utility of FeNO measurement. The 2020 Focused Updates also recommend considering FeNO measurement to guide treatment choice and monitoring, although this is based on overall low certainty of evidence.5 GINA affirms the mixed evidence for FeNO, stating that while a few studies have shown significantly reduced exacerbations among children, adolescents, and pregnant women with FeNO-guided treatment, other studies have shown no significant difference in exacerbations.4,9-15 At this time, the role for FeNO in asthma management remains inconclusive, and access to it is limited across primary care settings.
When assessing response to ICS therapy (and before stepping up therapy), consider patient adherence, inhaler technique, whether allergen exposure is persistent, and possible comorbidities. Inhaler technique can be especially challenging, as each inhaler varies in appearance and operation. Employ patient education strategies (eg, videos, demonstration, teach-back methods). If stepping up therapy is indicated, adding a LABA is recommended over increasing the ICS dose. Since asthma is variable, stepping up therapy can be tried and reassessed in 2 to 3 months.
SMART is preferred
Single maintenance and reliever therapy (SMART) with ICS-formoterol, used as needed, is the preferred therapy for steps 3 and 4 in both GINA recommendations and the 2020 Focused Updates (TABLE3-5). GINA also prefers SMART for step 5. The recommended SMART combination that has been studied contains budesonide (or beclomethasone, not available in combination in the United States) for the ICS and formoterol for the LABA in a single inhaler that is used both daily for control and as needed for rescue therapy.
Continue to: Other ICS-formoterol...
Other ICS-formoterol or ICS-LABA combinations can be considered for controller therapy, especially those described in the NAEPP and GINA alternative step therapy recommendations. However, SMART has been more effective than other combinations in reducing exacerbations and provides similar or better levels of control at lower average ICS doses (compared with ICS-LABA with SABA or ICS with SABA) for adolescent and adult patients.3,4 As patients use greater amounts of ICS-formoterol during episodes of increased symptoms, this additional ICS may augment the anti-inflammatory effects. SMART may also improve adherence, especially among those who confuse multiple inhalers.
SMART is also recommended for use in children. Specifically, from the 2020 Focused Updates, any patient ≥ 4 years of age with a severe exacerbation in the past year is a good SMART candidate. Also consider SMART before higher-dose ICS-LABA and SABA as needed. Additional benefits in this younger patient population are fewer medical visits or less systemic corticosteroid use with improved control and quality of life.
Caveats. Patients who have a difficult time recognizing symptoms may not be good candidates for SMART, due to the potential for taking higher or lower ICS doses than necessary.
SMART specifically refers to formoterol combinations that produce bronchodilation within 1 to 3 minutes.16 For example, the SMART strategy is not recommended for patients using ICS-salmeterol as controller therapy.
Although guideline supported, SMART options are not approved by the US Food and Drug Administration for use as reliever therapy.
Continue to: With the single combination...
With the single combination inhaler, consider the dosing limits of formoterol. The maximum daily amount of formoterol for adolescents and adults is 54 μg (12 puffs) delivered with the budesonide-formoterol metered dose inhaler. When using SMART as reliever therapy, the low-dose ICS-formoterol recommendation remains. However, depending on insurance coverage, a 1-month supply of ICS-formoterol may not be sufficient for additional reliever therapy use.
The role of LAMAs as add-on therapy
Bronchiolar smooth muscle tone is mediated by complex mechanisms that include cholinergic stimulation at muscarinic (M3) receptors.17 LAMAs, a mainstay in the management of chronic obstructive pulmonary disease (COPD), are likely to be effective in reducing asthma exacerbations and the need for oral steroids. When patients have not achieved control at step 4 of asthma therapy, both the 2020 Focused Updates and GINA now recommend considering a LAMA (eg, tiotropium) as add-on therapy for patients > 12 years of age already taking medium-dose ICS-LABA for modest improvements in lung function and reductions in severe exacerbations. GINA recommendations also now include a LAMA as add-on treatment for those ages 6 to 11 years, as some evidence supports the use in school-aged children.18 It is important to note that LAMAs should not replace a LABA for treatment, as the ICS-LABA combination is likely more effective than ICS-LAMA.
Addressing asthma-COPD overlap
Asthma and COPD are frequently and frustratingly intertwined without clear demarcation. This tends to occur as patients age and chronic lung changes appear from longstanding asthma. However, it is important to distinguish between these conditions, because there are clearly delineated treatments for each that can improve outcomes.
The priority in addressing asthma-COPD overlap (ACO) is to evaluate symptoms and determine if asthma or COPD is predominant.19 This includes establishing patient age at which symptoms began, variation and triggers of symptoms, and history of exposures to smoke/environmental respiratory toxins. Age 40 years is often used as the tipping point at which symptom onset favors a diagnosis of COPD. Serial spirometry may also be used to evaluate lung function over time and persistence of disease. If a firm diagnosis is evasive, consider a referral to a pulmonary specialist for further testing.
Choosing to use an ICS or LAMA depends on which underlying disorder is more likely. While early COPD management includes LAMA + LABA, the addition of an ICS is reserved for more severe disease. High-dose ICSs, particularly fluticasone, should be limited in COPD due to an increased risk for pneumonia. For asthma or ACO, the addition of an ICS is critical and prioritized to reduce airway inflammation and risk for exacerbations and death. While a LAMA is likely useful earlier in ACO, it is not used until step 5 of asthma therapy. Given the complexities of ACO treatment, further research is needed to provide adequate guidance.
CASE
For Ms. S, you would be wise to use an ICS-formoterol combination for as-needed symptom relief. If symptoms were more persistent, you could consider recommending the ICS-formoterol inhaler as SMART therapy, with regular doses taken twice daily and extra doses taken as needed.
CORRESPONDENCE
Tanner Nissly, DO, University of Minnesota School of Medicine, Department of Family Medicine and Community Health, 2426 West Broadway Avenue, Minneapolis, MN 55411; nissl003@umn.edu
1. CDC. Most recent national asthma data. Accessed October 24, 2022. www.cdc.gov/asthma/most_recent_national_asthma_data.htm
2. Akinbami LJ, Santo L, Williams S, et al. Characteristics of asthma visits to physician offices in the United States: 2012–2015 National Ambulatory Medical Care Survey. Natl Health Stat Report. 2019;128:1-20.
3. NHLBI. National Asthma Education and Prevention Program expert panel report 3: guidelines for the diagnosis and management of asthma. NIH Publication 07-4051. 2007. Accessed October 24, 2022. www.nhlbi.nih.gov/sites/default/files/media/docs/EPR-3_Asthma_Full_Report_2007.pdf
4. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. 2022. Accessed October 24, 2022. https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf
5. NHLBI. 2020 Focused updates to the asthma management guidelines. Accessed October 24, 2022. www.nhlbi.nih.gov/health-topics/all-publications-and-resources/2020-focused-updates-asthma-management-guidelines
6. Lazarus SC, Krishnan JA, King TS, et al. Mometasone or tiotropium in mild asthma with a low sputum eosinophil level. N Engl J Med. 2019;380:2009-2019. doi: 10.1056/NEJMoa1814917
7. Suissa S, Ernst P, Benayoun S, et al. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med. 2000;343:332-336. doi: 10.1056/NEJM200008033430504
8. Suissa S, Ernst P, Kezouh A. Regular use of inhaled corticosteroids and the long term prevention of hospitalisation for asthma. Thorax. 2002;57:880-884. doi: 10.1136/thorax.57.10.880
9. Szefler SJ, Mitchell H, Sorkness CA, et al. Management of asthma based on exhaled nitric oxide in addition to guideline-based treatment for inner-city adolescents and young adults: a randomised controlled trial. Lancet. 2008;372:1065-1072. doi: 10.1016/S0140-6736(08)61448-8
10. Calhoun WJ, Ameredes BT, King TS, et al. Comparison of physician-, biomarker-, and symptom-based strategies for adjustment of inhaled corticosteroid therapy in adults with asthma: the BASALT randomized controlled trial. JAMA. 2012;308:987-997. doi: 10.1001/2012.jama.10893
11. Garg Y, Kakria N, Katoch CDS, et al. Exhaled nitric oxide as a guiding tool for bronchial asthma: a randomised controlled trial. Med J Armed Forces India. 2020;76:17-22. doi: 10.1016/j.mjafi.2018.02.001
12. Honkoop PJ, Loijmans RJ, Termeer EH, et al. Symptom- and fraction of exhaled nitric oxide-driven strategies for asthma control: a cluster-randomized trial in primary care. J Allergy Clin Immunol. 2015;135:682-8.e11. doi: 10.1016/j.jaci.2014.07.016
13. Peirsman EJ, Carvelli TJ, Hage PY, et al. Exhaled nitric oxide in childhood allergic asthma management: a randomised controlled trial. Pediatr Pulmonol. 2014;49:624-631. doi: 10.1002/ppul.22873
14. Powell H, Murphy VE, Taylor DR, et al. Management of asthma in pregnancy guided by measurement of fraction of exhaled nitric oxide: a double-blind, randomised controlled trial. Lancet. 2011;378:983-990. doi: 10.1016/S0140-6736(11)60971-9
15. Shaw DE, Berry MA, Thomas M, et al. The use of exhaled nitric oxide to guide asthma management: a randomized controlled trial. Am J Respir Crit Care Med. 2007;176:231-237. doi: 10.1164/rccm.200610-1427OC
16. Stam J, Souren M, Zweers P. The onset of action of formoterol, a new beta 2 adrenoceptor agonist. Int J Clin Pharmacol Ther Toxicol. 1993;31:23-26.
17. Evgenov OV, Liang Y, Jiang Y, et al. Pulmonary pharmacology and inhaled anesthetics. In: Gropper MA, Miller RD, Evgenov O, et al, eds. Miller’s Anesthesia. 8th ed. Elsevier; 2020:540-571.
18. Rodrigo GJ, Neffen H. Efficacy and safety of tiotropium in school-age children with moderate-to-severe symptomatic asthma: a systematic review. Pediatr Allergy Immunol. 2017;28:573-578. doi: 10.1111/pai.12759
19. Global Initiative for Asthma (GINA). Asthma, COPD, and asthma-COPD overlap syndrome (ACOS). 2015. Accessed October 24, 2022. https://goldcopd.org/wp-content/uploads/2016/04/GOLD_ACOS_2015.pdf
CASE
Erica S*, age 22, has intermittent asthma and presents to your clinic to discuss refills of her albuterol inhaler. Two years ago, she was hospitalized for a severe asthma exacerbation because she was unable to afford medications. Since then, her asthma has generally been well controlled, and she needs to use albuterol only 1 or 2 times per month. Ms. S says she has no morning chest tightness or nocturnal coughing, but she does experience increased wheezing and shortness of breath with activity.
What would you recommend? Would your recommendation differ if she had persistent asthma?
* The patient’s name has been changed to protect her identity .
As of 2020, more than 20 million adults and 4 million children younger than 18 years of age in the United States were living with asthma.1 In 2019 alone, there were more than 1.8 million asthma-related emergency department visits for adults, and more than 790,000 asthma-related emergency department visits for children. Asthma caused more than 4000 deaths in the United States in 2020.1 Given the scale of the burden of asthma, it is not surprising that approximately 60% of all asthma visits occur in primary care settings,2 making it essential that primary care physicians stay abreast of recent developments in asthma diagnosis and management.
Since 1991, the major guidance on best practices for asthma management in the United States has been provided by the National Heart, Lung, and Blood Institute (NHLBI)’s National Asthma Education and Prevention Program (NAEPP). Its last major update on asthma was released in 2007 as the Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma (EPR-3).3 Since that time, there has been significant progress in our understanding of asthma as a complex spectrum of phenotypes, which has advanced our knowledge of pathophysiology and helped refine treatment. In contrast to the NAEPP, the Global Initiative for Asthma (GINA) has published annual updates on asthma management incorporating up-to-date information.4 In response to the continuously evolving body of knowledge on asthma, the NAEPP Coordinating Committee Expert Panel Working Group published the 2020 Focused Updates to the Asthma Management Guidelines.5
Given the vast resources available on asthma, our purpose in this article is not to provide a comprehensive review of the stepwise approach to asthma management, but instead to summarize the major points presented in the 2020 Focused Updates and how these compare and contrast with the latest guidance from GINA.
A heterogeneous disease
Asthma is a chronic respiratory disease characterized by both variable symptoms and airflow limitation that change over time, often in response to external triggers such as exercise, allergens, and viral respiratory infections. Common symptoms include wheezing, cough, chest tightness, and shortness of breath. Despite the common symptomatology, asthma is a heterogeneous disease with several recognizable phenotypes including allergic, nonallergic, and asthma with persistent airflow limitation.
Continue to: The airflow limitation...
The airflow limitation in asthma occurs through both airway hyperresponsiveness to external stimuli and chronic airway inflammation. Airway constriction is regulated by nerves to the smooth muscles of the airway. Beta-2 nerve receptors have long been the target of asthma therapy with both short-acting beta-2 agonists (SABAs) as rescue treatment and long-acting beta-2 agonists (LABAs) as maintenance therapy.3,4 However, there is increasing evidence that cholinergic nerves also have a role in airway regulation in asthma, and long-acting muscarinic antagonists (LAMAs) have recently shown benefit as add-on therapy in some types of asthma.4-6 Inhaled corticosteroids (ICSs) have long held an important role in reducing airway inflammation, especially in the setting of allergic or eosinophilic inflammation.3-5
Spirometry is essential to asthma Dx—but what about FeNO?
The mainstay of asthma diagnosis is confirming both a history of variable respiratory symptoms and variable expiratory airflow limitation exhibited by spirometry. Obstruction is defined as a reduced forced expiratory volume in 1 second (FEV1) and as a decreased ratio of FEV1 over forced vital capacity (FVC) based on predicted values. An increase of at least 12% in FEV1 post bronchodilator use indicates asthma for adolescents and adults.
More recently, studies have examined the role of fractional exhaled nitric oxide (FeNO) in the diagnosis of asthma. The 2020 Focused Updates report states that FeNO may be useful when the diagnosis of asthma is uncertain using initial history, physical exam, and spirometry findings, or when spirometry cannot be performed reliably.5 Levels of FeNO > 50 ppb make eosinophilic inflammation and treatment response to an ICS more likely. FeNO levels < 25 ppb make inflammatory asthma less likely and should prompt a search for an alternate diagnosis.5 For patients with FeNO of 25 to 50 ppb, more detailed clinical context is needed. In contrast, the 2022 GINA updates conclude that FeNO is not yet an established diagnostic tool for asthma.4
Management
When to start and adjust an ICS
ICSs continue to be the primary controller treatment for patients with asthma. However, the NAEPP and GINA have provided different guidance on how to initiate step therapy (TABLE3-5). NAEPP focuses on severity classification, while GINA recommends treatment initiation based on presenting symptoms. Since both guidelines recommend early follow-up and adjustment of therapy according to level of control, this difference becomes less apparent in ongoing care.
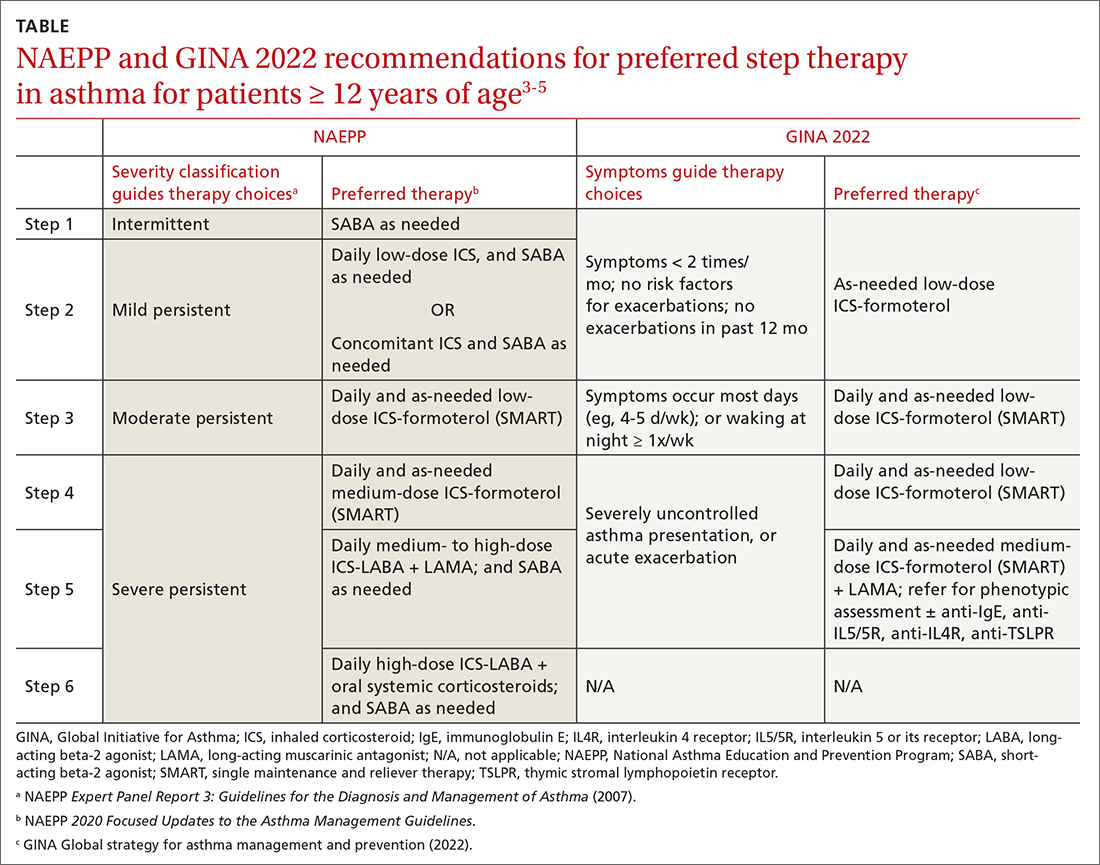
A more fundamental difference is seen in the recommended therapies for each step (TABLE3-5). Whereas the 2020 Focused Updates prefers a SABA as needed in step 1, GINA favors a low-dose combination of ICS-formoterol as needed. The GINA recommendation is driven by supportive evidence for early initiation of low-dose ICS in any patient with asthma for greater improvement in lung function. This also addresses concerns that overuse of as-needed SABAs may increase the risk for severe exacerbations. Evidence also indicates that the risk for asthma-related death and urgent asthma-related health care increases when a patient takes a SABA as needed as monotherapy compared with ICS therapy, even with good symptom control.7,8
Continue to: Dosing of an ICS
Dosing of an ICS is based on step therapy regardless of the guideline used and is given at a total daily amount—low, medium, and high—for each age group. When initiating an ICS, consider differences between available treatment options (eg, cost, administration technique, likely patient adherence, patient preferences) and employ shared decision-making strategies. Dosing may need to be limited depending on the commercially available product, especially when used in combination with a LABA. However, as GINA emphasizes, a low-dose ICS provides the most clinical benefit. A high-dose ICS is needed by very few patients and is associated with greater risk for local and systemic adverse effects, such as adrenal suppression. With these considerations, both guidelines recommend using the lowest effective ICS dose and stepping up and down according to the patient’s comfort level.
Give an ICS time to work. Although an ICS can begin to reduce inflammation within days of initiation, the full benefit may be evident only after 2 to 3 months.4 Once the patient’s asthma is well controlled for 3 months, stepping down the dose can be considered and approached carefully. Complete cessation of ICSs is associated with significantly higher risk for exacerbations. Therefore, a general recommendation is to step down an ICS by 50% or reduce ICS-LABA from twice-daily administration to once daily. Risk for exacerbation after step-down therapy is heightened if the patient has a history of exacerbation or an emergency department visit in the past 12 months, a low baseline FEV1, or a loss of control during a dose reduction (ie, airway hyperresponsiveness and sputum eosinophilia).
Weigh the utility of FeNO measurement. The 2020 Focused Updates also recommend considering FeNO measurement to guide treatment choice and monitoring, although this is based on overall low certainty of evidence.5 GINA affirms the mixed evidence for FeNO, stating that while a few studies have shown significantly reduced exacerbations among children, adolescents, and pregnant women with FeNO-guided treatment, other studies have shown no significant difference in exacerbations.4,9-15 At this time, the role for FeNO in asthma management remains inconclusive, and access to it is limited across primary care settings.
When assessing response to ICS therapy (and before stepping up therapy), consider patient adherence, inhaler technique, whether allergen exposure is persistent, and possible comorbidities. Inhaler technique can be especially challenging, as each inhaler varies in appearance and operation. Employ patient education strategies (eg, videos, demonstration, teach-back methods). If stepping up therapy is indicated, adding a LABA is recommended over increasing the ICS dose. Since asthma is variable, stepping up therapy can be tried and reassessed in 2 to 3 months.
SMART is preferred
Single maintenance and reliever therapy (SMART) with ICS-formoterol, used as needed, is the preferred therapy for steps 3 and 4 in both GINA recommendations and the 2020 Focused Updates (TABLE3-5). GINA also prefers SMART for step 5. The recommended SMART combination that has been studied contains budesonide (or beclomethasone, not available in combination in the United States) for the ICS and formoterol for the LABA in a single inhaler that is used both daily for control and as needed for rescue therapy.
Continue to: Other ICS-formoterol...
Other ICS-formoterol or ICS-LABA combinations can be considered for controller therapy, especially those described in the NAEPP and GINA alternative step therapy recommendations. However, SMART has been more effective than other combinations in reducing exacerbations and provides similar or better levels of control at lower average ICS doses (compared with ICS-LABA with SABA or ICS with SABA) for adolescent and adult patients.3,4 As patients use greater amounts of ICS-formoterol during episodes of increased symptoms, this additional ICS may augment the anti-inflammatory effects. SMART may also improve adherence, especially among those who confuse multiple inhalers.
SMART is also recommended for use in children. Specifically, from the 2020 Focused Updates, any patient ≥ 4 years of age with a severe exacerbation in the past year is a good SMART candidate. Also consider SMART before higher-dose ICS-LABA and SABA as needed. Additional benefits in this younger patient population are fewer medical visits or less systemic corticosteroid use with improved control and quality of life.
Caveats. Patients who have a difficult time recognizing symptoms may not be good candidates for SMART, due to the potential for taking higher or lower ICS doses than necessary.
SMART specifically refers to formoterol combinations that produce bronchodilation within 1 to 3 minutes.16 For example, the SMART strategy is not recommended for patients using ICS-salmeterol as controller therapy.
Although guideline supported, SMART options are not approved by the US Food and Drug Administration for use as reliever therapy.
Continue to: With the single combination...
With the single combination inhaler, consider the dosing limits of formoterol. The maximum daily amount of formoterol for adolescents and adults is 54 μg (12 puffs) delivered with the budesonide-formoterol metered dose inhaler. When using SMART as reliever therapy, the low-dose ICS-formoterol recommendation remains. However, depending on insurance coverage, a 1-month supply of ICS-formoterol may not be sufficient for additional reliever therapy use.
The role of LAMAs as add-on therapy
Bronchiolar smooth muscle tone is mediated by complex mechanisms that include cholinergic stimulation at muscarinic (M3) receptors.17 LAMAs, a mainstay in the management of chronic obstructive pulmonary disease (COPD), are likely to be effective in reducing asthma exacerbations and the need for oral steroids. When patients have not achieved control at step 4 of asthma therapy, both the 2020 Focused Updates and GINA now recommend considering a LAMA (eg, tiotropium) as add-on therapy for patients > 12 years of age already taking medium-dose ICS-LABA for modest improvements in lung function and reductions in severe exacerbations. GINA recommendations also now include a LAMA as add-on treatment for those ages 6 to 11 years, as some evidence supports the use in school-aged children.18 It is important to note that LAMAs should not replace a LABA for treatment, as the ICS-LABA combination is likely more effective than ICS-LAMA.
Addressing asthma-COPD overlap
Asthma and COPD are frequently and frustratingly intertwined without clear demarcation. This tends to occur as patients age and chronic lung changes appear from longstanding asthma. However, it is important to distinguish between these conditions, because there are clearly delineated treatments for each that can improve outcomes.
The priority in addressing asthma-COPD overlap (ACO) is to evaluate symptoms and determine if asthma or COPD is predominant.19 This includes establishing patient age at which symptoms began, variation and triggers of symptoms, and history of exposures to smoke/environmental respiratory toxins. Age 40 years is often used as the tipping point at which symptom onset favors a diagnosis of COPD. Serial spirometry may also be used to evaluate lung function over time and persistence of disease. If a firm diagnosis is evasive, consider a referral to a pulmonary specialist for further testing.
Choosing to use an ICS or LAMA depends on which underlying disorder is more likely. While early COPD management includes LAMA + LABA, the addition of an ICS is reserved for more severe disease. High-dose ICSs, particularly fluticasone, should be limited in COPD due to an increased risk for pneumonia. For asthma or ACO, the addition of an ICS is critical and prioritized to reduce airway inflammation and risk for exacerbations and death. While a LAMA is likely useful earlier in ACO, it is not used until step 5 of asthma therapy. Given the complexities of ACO treatment, further research is needed to provide adequate guidance.
CASE
For Ms. S, you would be wise to use an ICS-formoterol combination for as-needed symptom relief. If symptoms were more persistent, you could consider recommending the ICS-formoterol inhaler as SMART therapy, with regular doses taken twice daily and extra doses taken as needed.
CORRESPONDENCE
Tanner Nissly, DO, University of Minnesota School of Medicine, Department of Family Medicine and Community Health, 2426 West Broadway Avenue, Minneapolis, MN 55411; nissl003@umn.edu
CASE
Erica S*, age 22, has intermittent asthma and presents to your clinic to discuss refills of her albuterol inhaler. Two years ago, she was hospitalized for a severe asthma exacerbation because she was unable to afford medications. Since then, her asthma has generally been well controlled, and she needs to use albuterol only 1 or 2 times per month. Ms. S says she has no morning chest tightness or nocturnal coughing, but she does experience increased wheezing and shortness of breath with activity.
What would you recommend? Would your recommendation differ if she had persistent asthma?
* The patient’s name has been changed to protect her identity .
As of 2020, more than 20 million adults and 4 million children younger than 18 years of age in the United States were living with asthma.1 In 2019 alone, there were more than 1.8 million asthma-related emergency department visits for adults, and more than 790,000 asthma-related emergency department visits for children. Asthma caused more than 4000 deaths in the United States in 2020.1 Given the scale of the burden of asthma, it is not surprising that approximately 60% of all asthma visits occur in primary care settings,2 making it essential that primary care physicians stay abreast of recent developments in asthma diagnosis and management.
Since 1991, the major guidance on best practices for asthma management in the United States has been provided by the National Heart, Lung, and Blood Institute (NHLBI)’s National Asthma Education and Prevention Program (NAEPP). Its last major update on asthma was released in 2007 as the Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma (EPR-3).3 Since that time, there has been significant progress in our understanding of asthma as a complex spectrum of phenotypes, which has advanced our knowledge of pathophysiology and helped refine treatment. In contrast to the NAEPP, the Global Initiative for Asthma (GINA) has published annual updates on asthma management incorporating up-to-date information.4 In response to the continuously evolving body of knowledge on asthma, the NAEPP Coordinating Committee Expert Panel Working Group published the 2020 Focused Updates to the Asthma Management Guidelines.5
Given the vast resources available on asthma, our purpose in this article is not to provide a comprehensive review of the stepwise approach to asthma management, but instead to summarize the major points presented in the 2020 Focused Updates and how these compare and contrast with the latest guidance from GINA.
A heterogeneous disease
Asthma is a chronic respiratory disease characterized by both variable symptoms and airflow limitation that change over time, often in response to external triggers such as exercise, allergens, and viral respiratory infections. Common symptoms include wheezing, cough, chest tightness, and shortness of breath. Despite the common symptomatology, asthma is a heterogeneous disease with several recognizable phenotypes including allergic, nonallergic, and asthma with persistent airflow limitation.
Continue to: The airflow limitation...
The airflow limitation in asthma occurs through both airway hyperresponsiveness to external stimuli and chronic airway inflammation. Airway constriction is regulated by nerves to the smooth muscles of the airway. Beta-2 nerve receptors have long been the target of asthma therapy with both short-acting beta-2 agonists (SABAs) as rescue treatment and long-acting beta-2 agonists (LABAs) as maintenance therapy.3,4 However, there is increasing evidence that cholinergic nerves also have a role in airway regulation in asthma, and long-acting muscarinic antagonists (LAMAs) have recently shown benefit as add-on therapy in some types of asthma.4-6 Inhaled corticosteroids (ICSs) have long held an important role in reducing airway inflammation, especially in the setting of allergic or eosinophilic inflammation.3-5
Spirometry is essential to asthma Dx—but what about FeNO?
The mainstay of asthma diagnosis is confirming both a history of variable respiratory symptoms and variable expiratory airflow limitation exhibited by spirometry. Obstruction is defined as a reduced forced expiratory volume in 1 second (FEV1) and as a decreased ratio of FEV1 over forced vital capacity (FVC) based on predicted values. An increase of at least 12% in FEV1 post bronchodilator use indicates asthma for adolescents and adults.
More recently, studies have examined the role of fractional exhaled nitric oxide (FeNO) in the diagnosis of asthma. The 2020 Focused Updates report states that FeNO may be useful when the diagnosis of asthma is uncertain using initial history, physical exam, and spirometry findings, or when spirometry cannot be performed reliably.5 Levels of FeNO > 50 ppb make eosinophilic inflammation and treatment response to an ICS more likely. FeNO levels < 25 ppb make inflammatory asthma less likely and should prompt a search for an alternate diagnosis.5 For patients with FeNO of 25 to 50 ppb, more detailed clinical context is needed. In contrast, the 2022 GINA updates conclude that FeNO is not yet an established diagnostic tool for asthma.4
Management
When to start and adjust an ICS
ICSs continue to be the primary controller treatment for patients with asthma. However, the NAEPP and GINA have provided different guidance on how to initiate step therapy (TABLE3-5). NAEPP focuses on severity classification, while GINA recommends treatment initiation based on presenting symptoms. Since both guidelines recommend early follow-up and adjustment of therapy according to level of control, this difference becomes less apparent in ongoing care.
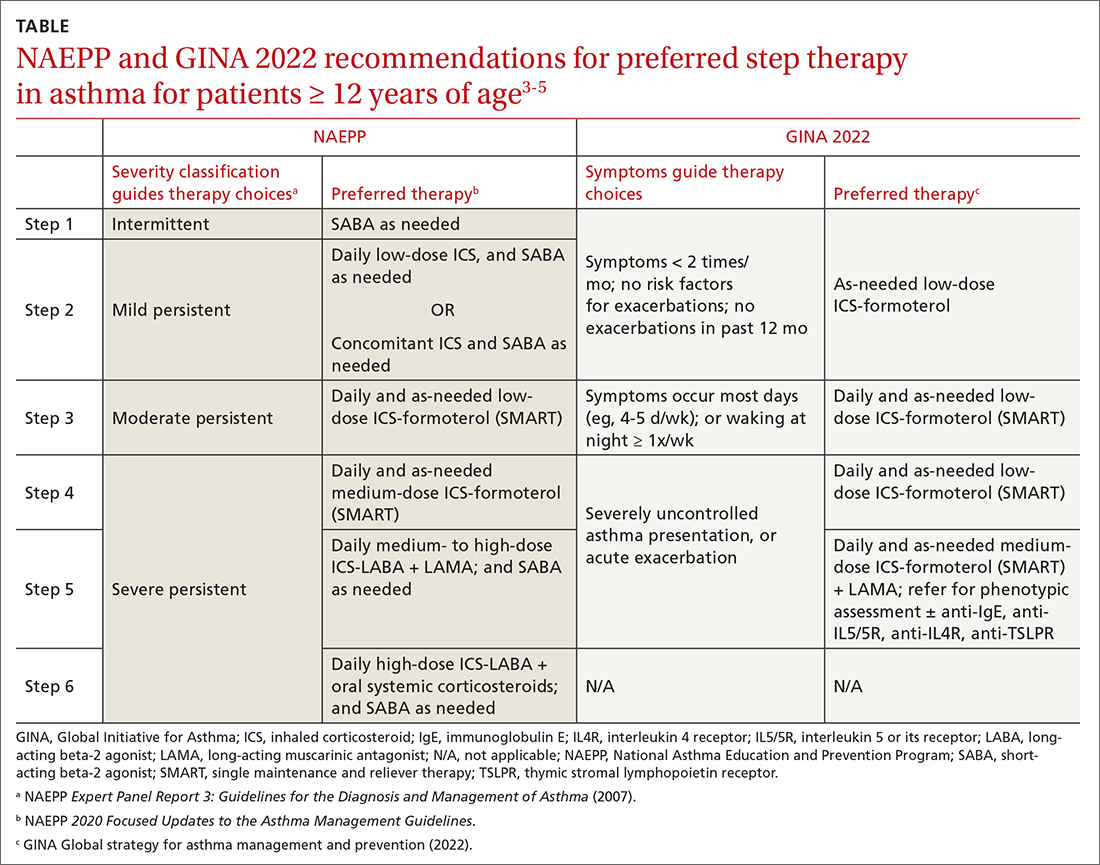
A more fundamental difference is seen in the recommended therapies for each step (TABLE3-5). Whereas the 2020 Focused Updates prefers a SABA as needed in step 1, GINA favors a low-dose combination of ICS-formoterol as needed. The GINA recommendation is driven by supportive evidence for early initiation of low-dose ICS in any patient with asthma for greater improvement in lung function. This also addresses concerns that overuse of as-needed SABAs may increase the risk for severe exacerbations. Evidence also indicates that the risk for asthma-related death and urgent asthma-related health care increases when a patient takes a SABA as needed as monotherapy compared with ICS therapy, even with good symptom control.7,8
Continue to: Dosing of an ICS
Dosing of an ICS is based on step therapy regardless of the guideline used and is given at a total daily amount—low, medium, and high—for each age group. When initiating an ICS, consider differences between available treatment options (eg, cost, administration technique, likely patient adherence, patient preferences) and employ shared decision-making strategies. Dosing may need to be limited depending on the commercially available product, especially when used in combination with a LABA. However, as GINA emphasizes, a low-dose ICS provides the most clinical benefit. A high-dose ICS is needed by very few patients and is associated with greater risk for local and systemic adverse effects, such as adrenal suppression. With these considerations, both guidelines recommend using the lowest effective ICS dose and stepping up and down according to the patient’s comfort level.
Give an ICS time to work. Although an ICS can begin to reduce inflammation within days of initiation, the full benefit may be evident only after 2 to 3 months.4 Once the patient’s asthma is well controlled for 3 months, stepping down the dose can be considered and approached carefully. Complete cessation of ICSs is associated with significantly higher risk for exacerbations. Therefore, a general recommendation is to step down an ICS by 50% or reduce ICS-LABA from twice-daily administration to once daily. Risk for exacerbation after step-down therapy is heightened if the patient has a history of exacerbation or an emergency department visit in the past 12 months, a low baseline FEV1, or a loss of control during a dose reduction (ie, airway hyperresponsiveness and sputum eosinophilia).
Weigh the utility of FeNO measurement. The 2020 Focused Updates also recommend considering FeNO measurement to guide treatment choice and monitoring, although this is based on overall low certainty of evidence.5 GINA affirms the mixed evidence for FeNO, stating that while a few studies have shown significantly reduced exacerbations among children, adolescents, and pregnant women with FeNO-guided treatment, other studies have shown no significant difference in exacerbations.4,9-15 At this time, the role for FeNO in asthma management remains inconclusive, and access to it is limited across primary care settings.
When assessing response to ICS therapy (and before stepping up therapy), consider patient adherence, inhaler technique, whether allergen exposure is persistent, and possible comorbidities. Inhaler technique can be especially challenging, as each inhaler varies in appearance and operation. Employ patient education strategies (eg, videos, demonstration, teach-back methods). If stepping up therapy is indicated, adding a LABA is recommended over increasing the ICS dose. Since asthma is variable, stepping up therapy can be tried and reassessed in 2 to 3 months.
SMART is preferred
Single maintenance and reliever therapy (SMART) with ICS-formoterol, used as needed, is the preferred therapy for steps 3 and 4 in both GINA recommendations and the 2020 Focused Updates (TABLE3-5). GINA also prefers SMART for step 5. The recommended SMART combination that has been studied contains budesonide (or beclomethasone, not available in combination in the United States) for the ICS and formoterol for the LABA in a single inhaler that is used both daily for control and as needed for rescue therapy.
Continue to: Other ICS-formoterol...
Other ICS-formoterol or ICS-LABA combinations can be considered for controller therapy, especially those described in the NAEPP and GINA alternative step therapy recommendations. However, SMART has been more effective than other combinations in reducing exacerbations and provides similar or better levels of control at lower average ICS doses (compared with ICS-LABA with SABA or ICS with SABA) for adolescent and adult patients.3,4 As patients use greater amounts of ICS-formoterol during episodes of increased symptoms, this additional ICS may augment the anti-inflammatory effects. SMART may also improve adherence, especially among those who confuse multiple inhalers.
SMART is also recommended for use in children. Specifically, from the 2020 Focused Updates, any patient ≥ 4 years of age with a severe exacerbation in the past year is a good SMART candidate. Also consider SMART before higher-dose ICS-LABA and SABA as needed. Additional benefits in this younger patient population are fewer medical visits or less systemic corticosteroid use with improved control and quality of life.
Caveats. Patients who have a difficult time recognizing symptoms may not be good candidates for SMART, due to the potential for taking higher or lower ICS doses than necessary.
SMART specifically refers to formoterol combinations that produce bronchodilation within 1 to 3 minutes.16 For example, the SMART strategy is not recommended for patients using ICS-salmeterol as controller therapy.
Although guideline supported, SMART options are not approved by the US Food and Drug Administration for use as reliever therapy.
Continue to: With the single combination...
With the single combination inhaler, consider the dosing limits of formoterol. The maximum daily amount of formoterol for adolescents and adults is 54 μg (12 puffs) delivered with the budesonide-formoterol metered dose inhaler. When using SMART as reliever therapy, the low-dose ICS-formoterol recommendation remains. However, depending on insurance coverage, a 1-month supply of ICS-formoterol may not be sufficient for additional reliever therapy use.
The role of LAMAs as add-on therapy
Bronchiolar smooth muscle tone is mediated by complex mechanisms that include cholinergic stimulation at muscarinic (M3) receptors.17 LAMAs, a mainstay in the management of chronic obstructive pulmonary disease (COPD), are likely to be effective in reducing asthma exacerbations and the need for oral steroids. When patients have not achieved control at step 4 of asthma therapy, both the 2020 Focused Updates and GINA now recommend considering a LAMA (eg, tiotropium) as add-on therapy for patients > 12 years of age already taking medium-dose ICS-LABA for modest improvements in lung function and reductions in severe exacerbations. GINA recommendations also now include a LAMA as add-on treatment for those ages 6 to 11 years, as some evidence supports the use in school-aged children.18 It is important to note that LAMAs should not replace a LABA for treatment, as the ICS-LABA combination is likely more effective than ICS-LAMA.
Addressing asthma-COPD overlap
Asthma and COPD are frequently and frustratingly intertwined without clear demarcation. This tends to occur as patients age and chronic lung changes appear from longstanding asthma. However, it is important to distinguish between these conditions, because there are clearly delineated treatments for each that can improve outcomes.
The priority in addressing asthma-COPD overlap (ACO) is to evaluate symptoms and determine if asthma or COPD is predominant.19 This includes establishing patient age at which symptoms began, variation and triggers of symptoms, and history of exposures to smoke/environmental respiratory toxins. Age 40 years is often used as the tipping point at which symptom onset favors a diagnosis of COPD. Serial spirometry may also be used to evaluate lung function over time and persistence of disease. If a firm diagnosis is evasive, consider a referral to a pulmonary specialist for further testing.
Choosing to use an ICS or LAMA depends on which underlying disorder is more likely. While early COPD management includes LAMA + LABA, the addition of an ICS is reserved for more severe disease. High-dose ICSs, particularly fluticasone, should be limited in COPD due to an increased risk for pneumonia. For asthma or ACO, the addition of an ICS is critical and prioritized to reduce airway inflammation and risk for exacerbations and death. While a LAMA is likely useful earlier in ACO, it is not used until step 5 of asthma therapy. Given the complexities of ACO treatment, further research is needed to provide adequate guidance.
CASE
For Ms. S, you would be wise to use an ICS-formoterol combination for as-needed symptom relief. If symptoms were more persistent, you could consider recommending the ICS-formoterol inhaler as SMART therapy, with regular doses taken twice daily and extra doses taken as needed.
CORRESPONDENCE
Tanner Nissly, DO, University of Minnesota School of Medicine, Department of Family Medicine and Community Health, 2426 West Broadway Avenue, Minneapolis, MN 55411; nissl003@umn.edu
1. CDC. Most recent national asthma data. Accessed October 24, 2022. www.cdc.gov/asthma/most_recent_national_asthma_data.htm
2. Akinbami LJ, Santo L, Williams S, et al. Characteristics of asthma visits to physician offices in the United States: 2012–2015 National Ambulatory Medical Care Survey. Natl Health Stat Report. 2019;128:1-20.
3. NHLBI. National Asthma Education and Prevention Program expert panel report 3: guidelines for the diagnosis and management of asthma. NIH Publication 07-4051. 2007. Accessed October 24, 2022. www.nhlbi.nih.gov/sites/default/files/media/docs/EPR-3_Asthma_Full_Report_2007.pdf
4. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. 2022. Accessed October 24, 2022. https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf
5. NHLBI. 2020 Focused updates to the asthma management guidelines. Accessed October 24, 2022. www.nhlbi.nih.gov/health-topics/all-publications-and-resources/2020-focused-updates-asthma-management-guidelines
6. Lazarus SC, Krishnan JA, King TS, et al. Mometasone or tiotropium in mild asthma with a low sputum eosinophil level. N Engl J Med. 2019;380:2009-2019. doi: 10.1056/NEJMoa1814917
7. Suissa S, Ernst P, Benayoun S, et al. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med. 2000;343:332-336. doi: 10.1056/NEJM200008033430504
8. Suissa S, Ernst P, Kezouh A. Regular use of inhaled corticosteroids and the long term prevention of hospitalisation for asthma. Thorax. 2002;57:880-884. doi: 10.1136/thorax.57.10.880
9. Szefler SJ, Mitchell H, Sorkness CA, et al. Management of asthma based on exhaled nitric oxide in addition to guideline-based treatment for inner-city adolescents and young adults: a randomised controlled trial. Lancet. 2008;372:1065-1072. doi: 10.1016/S0140-6736(08)61448-8
10. Calhoun WJ, Ameredes BT, King TS, et al. Comparison of physician-, biomarker-, and symptom-based strategies for adjustment of inhaled corticosteroid therapy in adults with asthma: the BASALT randomized controlled trial. JAMA. 2012;308:987-997. doi: 10.1001/2012.jama.10893
11. Garg Y, Kakria N, Katoch CDS, et al. Exhaled nitric oxide as a guiding tool for bronchial asthma: a randomised controlled trial. Med J Armed Forces India. 2020;76:17-22. doi: 10.1016/j.mjafi.2018.02.001
12. Honkoop PJ, Loijmans RJ, Termeer EH, et al. Symptom- and fraction of exhaled nitric oxide-driven strategies for asthma control: a cluster-randomized trial in primary care. J Allergy Clin Immunol. 2015;135:682-8.e11. doi: 10.1016/j.jaci.2014.07.016
13. Peirsman EJ, Carvelli TJ, Hage PY, et al. Exhaled nitric oxide in childhood allergic asthma management: a randomised controlled trial. Pediatr Pulmonol. 2014;49:624-631. doi: 10.1002/ppul.22873
14. Powell H, Murphy VE, Taylor DR, et al. Management of asthma in pregnancy guided by measurement of fraction of exhaled nitric oxide: a double-blind, randomised controlled trial. Lancet. 2011;378:983-990. doi: 10.1016/S0140-6736(11)60971-9
15. Shaw DE, Berry MA, Thomas M, et al. The use of exhaled nitric oxide to guide asthma management: a randomized controlled trial. Am J Respir Crit Care Med. 2007;176:231-237. doi: 10.1164/rccm.200610-1427OC
16. Stam J, Souren M, Zweers P. The onset of action of formoterol, a new beta 2 adrenoceptor agonist. Int J Clin Pharmacol Ther Toxicol. 1993;31:23-26.
17. Evgenov OV, Liang Y, Jiang Y, et al. Pulmonary pharmacology and inhaled anesthetics. In: Gropper MA, Miller RD, Evgenov O, et al, eds. Miller’s Anesthesia. 8th ed. Elsevier; 2020:540-571.
18. Rodrigo GJ, Neffen H. Efficacy and safety of tiotropium in school-age children with moderate-to-severe symptomatic asthma: a systematic review. Pediatr Allergy Immunol. 2017;28:573-578. doi: 10.1111/pai.12759
19. Global Initiative for Asthma (GINA). Asthma, COPD, and asthma-COPD overlap syndrome (ACOS). 2015. Accessed October 24, 2022. https://goldcopd.org/wp-content/uploads/2016/04/GOLD_ACOS_2015.pdf
1. CDC. Most recent national asthma data. Accessed October 24, 2022. www.cdc.gov/asthma/most_recent_national_asthma_data.htm
2. Akinbami LJ, Santo L, Williams S, et al. Characteristics of asthma visits to physician offices in the United States: 2012–2015 National Ambulatory Medical Care Survey. Natl Health Stat Report. 2019;128:1-20.
3. NHLBI. National Asthma Education and Prevention Program expert panel report 3: guidelines for the diagnosis and management of asthma. NIH Publication 07-4051. 2007. Accessed October 24, 2022. www.nhlbi.nih.gov/sites/default/files/media/docs/EPR-3_Asthma_Full_Report_2007.pdf
4. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. 2022. Accessed October 24, 2022. https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf
5. NHLBI. 2020 Focused updates to the asthma management guidelines. Accessed October 24, 2022. www.nhlbi.nih.gov/health-topics/all-publications-and-resources/2020-focused-updates-asthma-management-guidelines
6. Lazarus SC, Krishnan JA, King TS, et al. Mometasone or tiotropium in mild asthma with a low sputum eosinophil level. N Engl J Med. 2019;380:2009-2019. doi: 10.1056/NEJMoa1814917
7. Suissa S, Ernst P, Benayoun S, et al. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med. 2000;343:332-336. doi: 10.1056/NEJM200008033430504
8. Suissa S, Ernst P, Kezouh A. Regular use of inhaled corticosteroids and the long term prevention of hospitalisation for asthma. Thorax. 2002;57:880-884. doi: 10.1136/thorax.57.10.880
9. Szefler SJ, Mitchell H, Sorkness CA, et al. Management of asthma based on exhaled nitric oxide in addition to guideline-based treatment for inner-city adolescents and young adults: a randomised controlled trial. Lancet. 2008;372:1065-1072. doi: 10.1016/S0140-6736(08)61448-8
10. Calhoun WJ, Ameredes BT, King TS, et al. Comparison of physician-, biomarker-, and symptom-based strategies for adjustment of inhaled corticosteroid therapy in adults with asthma: the BASALT randomized controlled trial. JAMA. 2012;308:987-997. doi: 10.1001/2012.jama.10893
11. Garg Y, Kakria N, Katoch CDS, et al. Exhaled nitric oxide as a guiding tool for bronchial asthma: a randomised controlled trial. Med J Armed Forces India. 2020;76:17-22. doi: 10.1016/j.mjafi.2018.02.001
12. Honkoop PJ, Loijmans RJ, Termeer EH, et al. Symptom- and fraction of exhaled nitric oxide-driven strategies for asthma control: a cluster-randomized trial in primary care. J Allergy Clin Immunol. 2015;135:682-8.e11. doi: 10.1016/j.jaci.2014.07.016
13. Peirsman EJ, Carvelli TJ, Hage PY, et al. Exhaled nitric oxide in childhood allergic asthma management: a randomised controlled trial. Pediatr Pulmonol. 2014;49:624-631. doi: 10.1002/ppul.22873
14. Powell H, Murphy VE, Taylor DR, et al. Management of asthma in pregnancy guided by measurement of fraction of exhaled nitric oxide: a double-blind, randomised controlled trial. Lancet. 2011;378:983-990. doi: 10.1016/S0140-6736(11)60971-9
15. Shaw DE, Berry MA, Thomas M, et al. The use of exhaled nitric oxide to guide asthma management: a randomized controlled trial. Am J Respir Crit Care Med. 2007;176:231-237. doi: 10.1164/rccm.200610-1427OC
16. Stam J, Souren M, Zweers P. The onset of action of formoterol, a new beta 2 adrenoceptor agonist. Int J Clin Pharmacol Ther Toxicol. 1993;31:23-26.
17. Evgenov OV, Liang Y, Jiang Y, et al. Pulmonary pharmacology and inhaled anesthetics. In: Gropper MA, Miller RD, Evgenov O, et al, eds. Miller’s Anesthesia. 8th ed. Elsevier; 2020:540-571.
18. Rodrigo GJ, Neffen H. Efficacy and safety of tiotropium in school-age children with moderate-to-severe symptomatic asthma: a systematic review. Pediatr Allergy Immunol. 2017;28:573-578. doi: 10.1111/pai.12759
19. Global Initiative for Asthma (GINA). Asthma, COPD, and asthma-COPD overlap syndrome (ACOS). 2015. Accessed October 24, 2022. https://goldcopd.org/wp-content/uploads/2016/04/GOLD_ACOS_2015.pdf
PRACTICE RECOMMENDATIONS
› Consider early initiation of intermittent inhaled corticosteroid (ICS)- formoterol over a short-acting beta-2 agonist for reliever therapy. A
› Start prescribing single maintenance and reliever therapy (SMART) with ICS-formoterol to reduce exacerbation rates and simplify application. A
› Consider FeNO assessment when the diagnosis of asthma remains unclear despite history and spirometry findings. B
› Consider adding a longacting antimuscarinic agent to a medium- or high-dose ICS-LABA (long-acting beta-2 agonist) combination in uncontrolled asthma. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Treating UTIs in reproductive-age women—Proceed with caution
Nitrofurantoin and sulfonamides may cause major birth defects and should be used with caution—if at all—in women of reproductive age.1
Strength of Recommendation
B: Population-based case-control study
1. Crider KS, Cleves MA, Reefhuis J, et al. Antibacterial medication use during pregnancy and risk of birth defects: National Birth Defects Prevention Study. Arch Pediatr Adolesc Med. 2009;163:978-985.
Illustrative case
A 24-year-old woman comes to your clinic because of frequent urination for the past 2 to 3 days. She is not taking any medication, but does take a daily prenatal vitamin because she and her husband are trying to conceive. After your examination, you order a urinalysis and perform a urine pregnancy test. The urinalysis shows bacteriuria ≥100,000 cfu/ml, and the pregnancy test is positive.
What will you prescribe to treat her urinary tract infection?
Antibacterial agents are among the most commonly used medications during pregnancy because treatment of infections is critical to both maternal and fetal well-being.1 Urinary tract infections (UTIs) are the most common medical complication during pregnancy, with Escherichia coli contributing to roughly 90% of the infections.2 Screening for and treating asymptomatic bacteriuria is also recommended during pregnancy to prevent pyelonephritis and increased maternal and fetal morbidity.3 In addition, UTIs are common in reproductive-age women who may not know they are pregnant or who become pregnant during treatment with antibiotics. And nitrofurantoin and sulfonamides are commonly prescribed antibiotics for the treatment of UTIs, both in pregnant women and women of reproductive age.
Prior warnings only address near-term pregnancy
Prior to the study detailed in this PURL, no clinical trials had reported a teratogenic risk associated with either nitrofurantoin (current pregnancy category B) or sulfonamide (current pregnancy category C).4 It is recommended, however, that both of these antibacterials be avoided in pregnant women who are near term because of the risk of hemolytic disease in patients with glucose-6-phosphate dehydrogenase deficiency associated with nitrofurantoin and the risk of kernicterus in neonates exposed to sulfamethoxazole.5
But a rise in E coli resistance to penicillins (resistance to amoxicillin, for example, can be as high as 30-40%6) has led to greater use of nitrofurantoin. The drug has been viewed as a safe and effective alternative treatment for UTIs associated with E coli.7 Indeed, nitrofurantoin has been considered to be the preferred antibiotic for bacteriuria suppression, as both ampicillin and cephalosporins can interfere with the normal gastrointestinal flora. Thus, nitrofurantoin is used extensively in pregnant women. Sulfonamides are also prescribed for pregnant women, although not as frequently.7,8
STUDY SUMMARY: First trimester use linked to many defects
The study by Crider et al1 was based on the National Birth Defects Prevention Study, an ongoing, population-based case control study of an estimated annual birth population of roughly 482,000, including cases identified by birth defects surveillance registries in 10 states.9 The researchers identified pregnancies affected by any of 30 types of birth defects from 1997 to 2003 (n=13,155). The controls (n=4941) were randomly selected from similar geographic locations, and matched for race/ethnicity, age, and prepregnancy body mass index. Exposure to antibacterials from 1 month prepregnancy through the end of the first trimester was recorded.
Crider et al interviewed all the participants up to 24 months after delivery to obtain their exposure history to penicillins, erythromycins, nitrofurantoin, sulfonamides, cephalosporins, quinolones, tetracyclines, other miscellaneous beta-lactams, aminoglycosides, antimycobacterial agents, and other antibiotics. (Exposure to antivirals, antifungals, and antiparasitic agents was not addressed.) Women who didn’t know whether they had been exposed to these agents or could not remember the timing of exposure were excluded.
Overall, antibacterial use ranged from 2% to 5.8%, and peaked in the third month of pregnancy. Penicillins were the most commonly used antibiotics. Odds ratios obtained for birth defects were adjusted for confounders such as maternal age, race, education level, prepregnancy body mass index, time from estimated date of delivery to the interview, use of folic acid or multivitamins from 1 month prior to pregnancy through the first month, and periconceptional smoking and/or alcohol use.
Nitrofurantoin was associated with anophthalmia or microphthalmos (adjusted odds ratio [AOR]=3.7; 95% confidence interval [CI], 1.1-12.2), hypoplastic left heart syndrome (AOR=4.2; 95% CI, 1.9-9.1), atrial septal defects (AOR=1.9; 95% CI, 1.1-3.4), and cleft lip with cleft palate (AOR=2.1; 95% CI, 1.2-3.9).
Sulfonamides were associated with anencephaly (AOR=3.4; 95% CI, 1.3-8.8), hypoplastic left heart syndrome (AOR=3.2; 95% CI, 1.3-7.6), coarctation of the aorta (AOR=2.7; 95% CI, 1.3-5.6), choanal atresia (AOR=8.0; 95% CI, 2.7-23.5), transverse limb deficiency (AOR=2.5; 95% CI, 1.0-5.9), and diaphragmatic hernia (AOR=2.4; 95% CI, 1.1-5.4).
Some links between other antibiotics and birth defects were also found. For example, erythromycins were associated with anencephaly and transverse limb deficiency, penicillins with intercalary limb deficiency, and cephalosporins with atrial septal defects. The authors noted, however, that these agents, which are commonly prescribed for pregnant women, were not associated with many birth defects—and that because of limited sample sizes for these drug classes, the associations may be spurious.
WHAT'S NEW: A large-scale study provides evidence of risk
Previous case studies and meta-analysis have shown no link between the use of nitrofurantoin and congenital abnormalities.8 Similarly, sulfonamides have not appeared to pose significant teratogenic risk. This is the first large-scale study evaluating the risk of birth defects associated with antibiotic use during pregnancy, and therefore provides evidence of risk not previously available.
CAVEATS: Study design raises questions of recall bias
The retrospective case-control methodology used in this study leaves open the possibility of recall bias, misclassification bias, and confounding bias. The length of time from actual exposure to data collection could affect the accuracy of participants’ memories. The data gathered were not cross-verified against medical records, and other issues, such as the possible effect of medications for other infections (eg, antivirals and antifungals), could not be measured. However, women who did not know or were unsure of their medication exposure history were excluded from the analysis, which should reduce the risk of this potential bias.
The investigators also controlled for several important sources of potential confounding bias, and the reporting rates were similar among participants in both the case and control groups. These measures provide some assurance that the outcomes are valid.
It would be unethical (and extraordinarily expensive) to conduct a prospective randomized controlled trial to confirm these findings. Case-control methodology is the most practical way to assess for the risk of birth defects, and our literature review suggests that this is the most rigorous study to date. In our view, the potential harm from continuing to use these antibiotics for pregnant women and women who may become pregnant far outweighs the risk that these findings may be erroneous.
That said, a final caveat is the fact that even a several-fold increase in the risk of a rare major birth defect such as those reported in this study is still a rare risk. There may be clinical situations in which the benefits of using nitrofurantoin or sulfonamides in women who are or may become pregnant outweigh the potential risks.
CHALLENGES TO IMPLEMENTATION: Finding an alternative treatment
The main challenge to implementing this new recommendation lies in choosing alternative antibiotics with which to treat UTIs in reproductive-age women and bacteriuria in pregnancy. Obtaining a pregnancy test in sexually active patients of reproductive age who are not using a reliable form of contraception seems like a prudent first step.
If the pregnancy test is positive, cephalexin should be a good initial choice until the results of culture and sensitivities are available. In the event of Enterococcus infection (for which cephalosporins are not active) or other organisms resistant to cephalosporins, the sensitivity results should provide guidance.3
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant was a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Crider KS, Cleves MA, Reefhuis J, et al. Antibacterial medication use during pregnancy and risk of birth defects: National Birth Defects Prevention Study. Arch Pediatr Adolesc Med. 2009;163:978-985.
2. Gilstrap LC, 3rd, Ramin SM. Urinary tract infections during pregnancy. Obstet Gynecol. 2001;28:581-591.
3. Macejko AM, Schaeffer AJ. Asymptomatic bacteriuria and symptomatic urinary tract infections during pregnancy. Urol Clin North Am. 2007;34:35-42.
4. Thomson Reuters (Healthcare). Micromedex® Healthcare Series Intranet. 5.1.
5. Czeizel AE, Rockenbauer M, Olsen J. Use of antibiotics during pregnancy. Eur J Obstet Gynecol Reprod Biol. 1998;81:1-8.
6. ABXguide. Urinary tract infections in pregnancy. Available at: http://prod.hopkins-abxguide.org/diagnosis/genitourinary/urinary_tract_infections_in_pregnancy.html?contentInstanceId=255490. Accessed February 15, 2010.
7. Huang ES, Stafford RS. National patterns in the treatment of urinary tract infections in women by ambulatory care physicians. Arch Intern Med. 2002;162:41-47.
8. Shrim A, Garcia-Bournissen F, Koren G. Pharmaceutical agents and pregnancy in urology practice. Urol Clin North Am. 2007;34:27-33.
9. Yoon PW, Rasmussen SA, Lynberg MC, et al. The National Birth Defects Prevention Study. Public Health Rep. 2001;116(suppl 1):32-40.
Nitrofurantoin and sulfonamides may cause major birth defects and should be used with caution—if at all—in women of reproductive age.1
Strength of Recommendation
B: Population-based case-control study
1. Crider KS, Cleves MA, Reefhuis J, et al. Antibacterial medication use during pregnancy and risk of birth defects: National Birth Defects Prevention Study. Arch Pediatr Adolesc Med. 2009;163:978-985.
Illustrative case
A 24-year-old woman comes to your clinic because of frequent urination for the past 2 to 3 days. She is not taking any medication, but does take a daily prenatal vitamin because she and her husband are trying to conceive. After your examination, you order a urinalysis and perform a urine pregnancy test. The urinalysis shows bacteriuria ≥100,000 cfu/ml, and the pregnancy test is positive.
What will you prescribe to treat her urinary tract infection?
Antibacterial agents are among the most commonly used medications during pregnancy because treatment of infections is critical to both maternal and fetal well-being.1 Urinary tract infections (UTIs) are the most common medical complication during pregnancy, with Escherichia coli contributing to roughly 90% of the infections.2 Screening for and treating asymptomatic bacteriuria is also recommended during pregnancy to prevent pyelonephritis and increased maternal and fetal morbidity.3 In addition, UTIs are common in reproductive-age women who may not know they are pregnant or who become pregnant during treatment with antibiotics. And nitrofurantoin and sulfonamides are commonly prescribed antibiotics for the treatment of UTIs, both in pregnant women and women of reproductive age.
Prior warnings only address near-term pregnancy
Prior to the study detailed in this PURL, no clinical trials had reported a teratogenic risk associated with either nitrofurantoin (current pregnancy category B) or sulfonamide (current pregnancy category C).4 It is recommended, however, that both of these antibacterials be avoided in pregnant women who are near term because of the risk of hemolytic disease in patients with glucose-6-phosphate dehydrogenase deficiency associated with nitrofurantoin and the risk of kernicterus in neonates exposed to sulfamethoxazole.5
But a rise in E coli resistance to penicillins (resistance to amoxicillin, for example, can be as high as 30-40%6) has led to greater use of nitrofurantoin. The drug has been viewed as a safe and effective alternative treatment for UTIs associated with E coli.7 Indeed, nitrofurantoin has been considered to be the preferred antibiotic for bacteriuria suppression, as both ampicillin and cephalosporins can interfere with the normal gastrointestinal flora. Thus, nitrofurantoin is used extensively in pregnant women. Sulfonamides are also prescribed for pregnant women, although not as frequently.7,8
STUDY SUMMARY: First trimester use linked to many defects
The study by Crider et al1 was based on the National Birth Defects Prevention Study, an ongoing, population-based case control study of an estimated annual birth population of roughly 482,000, including cases identified by birth defects surveillance registries in 10 states.9 The researchers identified pregnancies affected by any of 30 types of birth defects from 1997 to 2003 (n=13,155). The controls (n=4941) were randomly selected from similar geographic locations, and matched for race/ethnicity, age, and prepregnancy body mass index. Exposure to antibacterials from 1 month prepregnancy through the end of the first trimester was recorded.
Crider et al interviewed all the participants up to 24 months after delivery to obtain their exposure history to penicillins, erythromycins, nitrofurantoin, sulfonamides, cephalosporins, quinolones, tetracyclines, other miscellaneous beta-lactams, aminoglycosides, antimycobacterial agents, and other antibiotics. (Exposure to antivirals, antifungals, and antiparasitic agents was not addressed.) Women who didn’t know whether they had been exposed to these agents or could not remember the timing of exposure were excluded.
Overall, antibacterial use ranged from 2% to 5.8%, and peaked in the third month of pregnancy. Penicillins were the most commonly used antibiotics. Odds ratios obtained for birth defects were adjusted for confounders such as maternal age, race, education level, prepregnancy body mass index, time from estimated date of delivery to the interview, use of folic acid or multivitamins from 1 month prior to pregnancy through the first month, and periconceptional smoking and/or alcohol use.
Nitrofurantoin was associated with anophthalmia or microphthalmos (adjusted odds ratio [AOR]=3.7; 95% confidence interval [CI], 1.1-12.2), hypoplastic left heart syndrome (AOR=4.2; 95% CI, 1.9-9.1), atrial septal defects (AOR=1.9; 95% CI, 1.1-3.4), and cleft lip with cleft palate (AOR=2.1; 95% CI, 1.2-3.9).
Sulfonamides were associated with anencephaly (AOR=3.4; 95% CI, 1.3-8.8), hypoplastic left heart syndrome (AOR=3.2; 95% CI, 1.3-7.6), coarctation of the aorta (AOR=2.7; 95% CI, 1.3-5.6), choanal atresia (AOR=8.0; 95% CI, 2.7-23.5), transverse limb deficiency (AOR=2.5; 95% CI, 1.0-5.9), and diaphragmatic hernia (AOR=2.4; 95% CI, 1.1-5.4).
Some links between other antibiotics and birth defects were also found. For example, erythromycins were associated with anencephaly and transverse limb deficiency, penicillins with intercalary limb deficiency, and cephalosporins with atrial septal defects. The authors noted, however, that these agents, which are commonly prescribed for pregnant women, were not associated with many birth defects—and that because of limited sample sizes for these drug classes, the associations may be spurious.
WHAT'S NEW: A large-scale study provides evidence of risk
Previous case studies and meta-analysis have shown no link between the use of nitrofurantoin and congenital abnormalities.8 Similarly, sulfonamides have not appeared to pose significant teratogenic risk. This is the first large-scale study evaluating the risk of birth defects associated with antibiotic use during pregnancy, and therefore provides evidence of risk not previously available.
CAVEATS: Study design raises questions of recall bias
The retrospective case-control methodology used in this study leaves open the possibility of recall bias, misclassification bias, and confounding bias. The length of time from actual exposure to data collection could affect the accuracy of participants’ memories. The data gathered were not cross-verified against medical records, and other issues, such as the possible effect of medications for other infections (eg, antivirals and antifungals), could not be measured. However, women who did not know or were unsure of their medication exposure history were excluded from the analysis, which should reduce the risk of this potential bias.
The investigators also controlled for several important sources of potential confounding bias, and the reporting rates were similar among participants in both the case and control groups. These measures provide some assurance that the outcomes are valid.
It would be unethical (and extraordinarily expensive) to conduct a prospective randomized controlled trial to confirm these findings. Case-control methodology is the most practical way to assess for the risk of birth defects, and our literature review suggests that this is the most rigorous study to date. In our view, the potential harm from continuing to use these antibiotics for pregnant women and women who may become pregnant far outweighs the risk that these findings may be erroneous.
That said, a final caveat is the fact that even a several-fold increase in the risk of a rare major birth defect such as those reported in this study is still a rare risk. There may be clinical situations in which the benefits of using nitrofurantoin or sulfonamides in women who are or may become pregnant outweigh the potential risks.
CHALLENGES TO IMPLEMENTATION: Finding an alternative treatment
The main challenge to implementing this new recommendation lies in choosing alternative antibiotics with which to treat UTIs in reproductive-age women and bacteriuria in pregnancy. Obtaining a pregnancy test in sexually active patients of reproductive age who are not using a reliable form of contraception seems like a prudent first step.
If the pregnancy test is positive, cephalexin should be a good initial choice until the results of culture and sensitivities are available. In the event of Enterococcus infection (for which cephalosporins are not active) or other organisms resistant to cephalosporins, the sensitivity results should provide guidance.3
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant was a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
Nitrofurantoin and sulfonamides may cause major birth defects and should be used with caution—if at all—in women of reproductive age.1
Strength of Recommendation
B: Population-based case-control study
1. Crider KS, Cleves MA, Reefhuis J, et al. Antibacterial medication use during pregnancy and risk of birth defects: National Birth Defects Prevention Study. Arch Pediatr Adolesc Med. 2009;163:978-985.
Illustrative case
A 24-year-old woman comes to your clinic because of frequent urination for the past 2 to 3 days. She is not taking any medication, but does take a daily prenatal vitamin because she and her husband are trying to conceive. After your examination, you order a urinalysis and perform a urine pregnancy test. The urinalysis shows bacteriuria ≥100,000 cfu/ml, and the pregnancy test is positive.
What will you prescribe to treat her urinary tract infection?
Antibacterial agents are among the most commonly used medications during pregnancy because treatment of infections is critical to both maternal and fetal well-being.1 Urinary tract infections (UTIs) are the most common medical complication during pregnancy, with Escherichia coli contributing to roughly 90% of the infections.2 Screening for and treating asymptomatic bacteriuria is also recommended during pregnancy to prevent pyelonephritis and increased maternal and fetal morbidity.3 In addition, UTIs are common in reproductive-age women who may not know they are pregnant or who become pregnant during treatment with antibiotics. And nitrofurantoin and sulfonamides are commonly prescribed antibiotics for the treatment of UTIs, both in pregnant women and women of reproductive age.
Prior warnings only address near-term pregnancy
Prior to the study detailed in this PURL, no clinical trials had reported a teratogenic risk associated with either nitrofurantoin (current pregnancy category B) or sulfonamide (current pregnancy category C).4 It is recommended, however, that both of these antibacterials be avoided in pregnant women who are near term because of the risk of hemolytic disease in patients with glucose-6-phosphate dehydrogenase deficiency associated with nitrofurantoin and the risk of kernicterus in neonates exposed to sulfamethoxazole.5
But a rise in E coli resistance to penicillins (resistance to amoxicillin, for example, can be as high as 30-40%6) has led to greater use of nitrofurantoin. The drug has been viewed as a safe and effective alternative treatment for UTIs associated with E coli.7 Indeed, nitrofurantoin has been considered to be the preferred antibiotic for bacteriuria suppression, as both ampicillin and cephalosporins can interfere with the normal gastrointestinal flora. Thus, nitrofurantoin is used extensively in pregnant women. Sulfonamides are also prescribed for pregnant women, although not as frequently.7,8
STUDY SUMMARY: First trimester use linked to many defects
The study by Crider et al1 was based on the National Birth Defects Prevention Study, an ongoing, population-based case control study of an estimated annual birth population of roughly 482,000, including cases identified by birth defects surveillance registries in 10 states.9 The researchers identified pregnancies affected by any of 30 types of birth defects from 1997 to 2003 (n=13,155). The controls (n=4941) were randomly selected from similar geographic locations, and matched for race/ethnicity, age, and prepregnancy body mass index. Exposure to antibacterials from 1 month prepregnancy through the end of the first trimester was recorded.
Crider et al interviewed all the participants up to 24 months after delivery to obtain their exposure history to penicillins, erythromycins, nitrofurantoin, sulfonamides, cephalosporins, quinolones, tetracyclines, other miscellaneous beta-lactams, aminoglycosides, antimycobacterial agents, and other antibiotics. (Exposure to antivirals, antifungals, and antiparasitic agents was not addressed.) Women who didn’t know whether they had been exposed to these agents or could not remember the timing of exposure were excluded.
Overall, antibacterial use ranged from 2% to 5.8%, and peaked in the third month of pregnancy. Penicillins were the most commonly used antibiotics. Odds ratios obtained for birth defects were adjusted for confounders such as maternal age, race, education level, prepregnancy body mass index, time from estimated date of delivery to the interview, use of folic acid or multivitamins from 1 month prior to pregnancy through the first month, and periconceptional smoking and/or alcohol use.
Nitrofurantoin was associated with anophthalmia or microphthalmos (adjusted odds ratio [AOR]=3.7; 95% confidence interval [CI], 1.1-12.2), hypoplastic left heart syndrome (AOR=4.2; 95% CI, 1.9-9.1), atrial septal defects (AOR=1.9; 95% CI, 1.1-3.4), and cleft lip with cleft palate (AOR=2.1; 95% CI, 1.2-3.9).
Sulfonamides were associated with anencephaly (AOR=3.4; 95% CI, 1.3-8.8), hypoplastic left heart syndrome (AOR=3.2; 95% CI, 1.3-7.6), coarctation of the aorta (AOR=2.7; 95% CI, 1.3-5.6), choanal atresia (AOR=8.0; 95% CI, 2.7-23.5), transverse limb deficiency (AOR=2.5; 95% CI, 1.0-5.9), and diaphragmatic hernia (AOR=2.4; 95% CI, 1.1-5.4).
Some links between other antibiotics and birth defects were also found. For example, erythromycins were associated with anencephaly and transverse limb deficiency, penicillins with intercalary limb deficiency, and cephalosporins with atrial septal defects. The authors noted, however, that these agents, which are commonly prescribed for pregnant women, were not associated with many birth defects—and that because of limited sample sizes for these drug classes, the associations may be spurious.
WHAT'S NEW: A large-scale study provides evidence of risk
Previous case studies and meta-analysis have shown no link between the use of nitrofurantoin and congenital abnormalities.8 Similarly, sulfonamides have not appeared to pose significant teratogenic risk. This is the first large-scale study evaluating the risk of birth defects associated with antibiotic use during pregnancy, and therefore provides evidence of risk not previously available.
CAVEATS: Study design raises questions of recall bias
The retrospective case-control methodology used in this study leaves open the possibility of recall bias, misclassification bias, and confounding bias. The length of time from actual exposure to data collection could affect the accuracy of participants’ memories. The data gathered were not cross-verified against medical records, and other issues, such as the possible effect of medications for other infections (eg, antivirals and antifungals), could not be measured. However, women who did not know or were unsure of their medication exposure history were excluded from the analysis, which should reduce the risk of this potential bias.
The investigators also controlled for several important sources of potential confounding bias, and the reporting rates were similar among participants in both the case and control groups. These measures provide some assurance that the outcomes are valid.
It would be unethical (and extraordinarily expensive) to conduct a prospective randomized controlled trial to confirm these findings. Case-control methodology is the most practical way to assess for the risk of birth defects, and our literature review suggests that this is the most rigorous study to date. In our view, the potential harm from continuing to use these antibiotics for pregnant women and women who may become pregnant far outweighs the risk that these findings may be erroneous.
That said, a final caveat is the fact that even a several-fold increase in the risk of a rare major birth defect such as those reported in this study is still a rare risk. There may be clinical situations in which the benefits of using nitrofurantoin or sulfonamides in women who are or may become pregnant outweigh the potential risks.
CHALLENGES TO IMPLEMENTATION: Finding an alternative treatment
The main challenge to implementing this new recommendation lies in choosing alternative antibiotics with which to treat UTIs in reproductive-age women and bacteriuria in pregnancy. Obtaining a pregnancy test in sexually active patients of reproductive age who are not using a reliable form of contraception seems like a prudent first step.
If the pregnancy test is positive, cephalexin should be a good initial choice until the results of culture and sensitivities are available. In the event of Enterococcus infection (for which cephalosporins are not active) or other organisms resistant to cephalosporins, the sensitivity results should provide guidance.3
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant was a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Crider KS, Cleves MA, Reefhuis J, et al. Antibacterial medication use during pregnancy and risk of birth defects: National Birth Defects Prevention Study. Arch Pediatr Adolesc Med. 2009;163:978-985.
2. Gilstrap LC, 3rd, Ramin SM. Urinary tract infections during pregnancy. Obstet Gynecol. 2001;28:581-591.
3. Macejko AM, Schaeffer AJ. Asymptomatic bacteriuria and symptomatic urinary tract infections during pregnancy. Urol Clin North Am. 2007;34:35-42.
4. Thomson Reuters (Healthcare). Micromedex® Healthcare Series Intranet. 5.1.
5. Czeizel AE, Rockenbauer M, Olsen J. Use of antibiotics during pregnancy. Eur J Obstet Gynecol Reprod Biol. 1998;81:1-8.
6. ABXguide. Urinary tract infections in pregnancy. Available at: http://prod.hopkins-abxguide.org/diagnosis/genitourinary/urinary_tract_infections_in_pregnancy.html?contentInstanceId=255490. Accessed February 15, 2010.
7. Huang ES, Stafford RS. National patterns in the treatment of urinary tract infections in women by ambulatory care physicians. Arch Intern Med. 2002;162:41-47.
8. Shrim A, Garcia-Bournissen F, Koren G. Pharmaceutical agents and pregnancy in urology practice. Urol Clin North Am. 2007;34:27-33.
9. Yoon PW, Rasmussen SA, Lynberg MC, et al. The National Birth Defects Prevention Study. Public Health Rep. 2001;116(suppl 1):32-40.
1. Crider KS, Cleves MA, Reefhuis J, et al. Antibacterial medication use during pregnancy and risk of birth defects: National Birth Defects Prevention Study. Arch Pediatr Adolesc Med. 2009;163:978-985.
2. Gilstrap LC, 3rd, Ramin SM. Urinary tract infections during pregnancy. Obstet Gynecol. 2001;28:581-591.
3. Macejko AM, Schaeffer AJ. Asymptomatic bacteriuria and symptomatic urinary tract infections during pregnancy. Urol Clin North Am. 2007;34:35-42.
4. Thomson Reuters (Healthcare). Micromedex® Healthcare Series Intranet. 5.1.
5. Czeizel AE, Rockenbauer M, Olsen J. Use of antibiotics during pregnancy. Eur J Obstet Gynecol Reprod Biol. 1998;81:1-8.
6. ABXguide. Urinary tract infections in pregnancy. Available at: http://prod.hopkins-abxguide.org/diagnosis/genitourinary/urinary_tract_infections_in_pregnancy.html?contentInstanceId=255490. Accessed February 15, 2010.
7. Huang ES, Stafford RS. National patterns in the treatment of urinary tract infections in women by ambulatory care physicians. Arch Intern Med. 2002;162:41-47.
8. Shrim A, Garcia-Bournissen F, Koren G. Pharmaceutical agents and pregnancy in urology practice. Urol Clin North Am. 2007;34:27-33.
9. Yoon PW, Rasmussen SA, Lynberg MC, et al. The National Birth Defects Prevention Study. Public Health Rep. 2001;116(suppl 1):32-40.
Copyright © 2010 The Family Physicians Inquiries Network.
All rights reserved.