User login
Weakness with left elbow flexion • left anterior shoulder pain • Dx?
THE CASE
A 41-year-old, right-hand dominant man sought care at our facility one day after trying to pull his boat out of the water. He’d tried to lift the boat with his hands while his forearms were fully supinated and his elbows were flexed to about 90°. He then felt a sharp burning sensation in his left anterior shoulder and was unable to lift the boat. The patient denied feeling a popping sensation at the time of the injury. He had mild pain at night, but was able to sleep. He said that he had mild diminished strength with elbow flexion, but denied having any numbness, tingling, or discoloration of his skin.
The patient said he did weightlifting and strength training of his upper and lower extremities 4 times/week. He was in good general health, was not taking any medications or supplements, and denied smoking or using illicit drugs. His surgical history was significant for a Bankart repair 8 years ago.
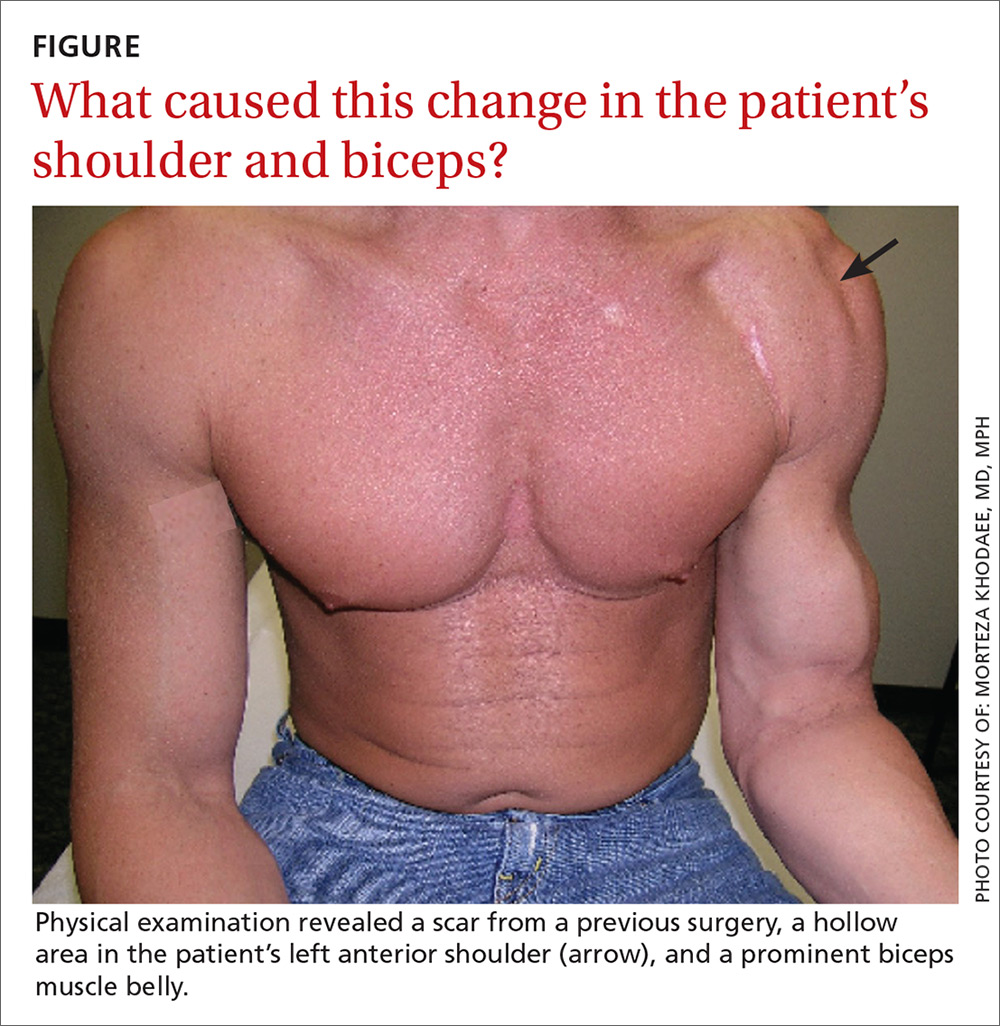
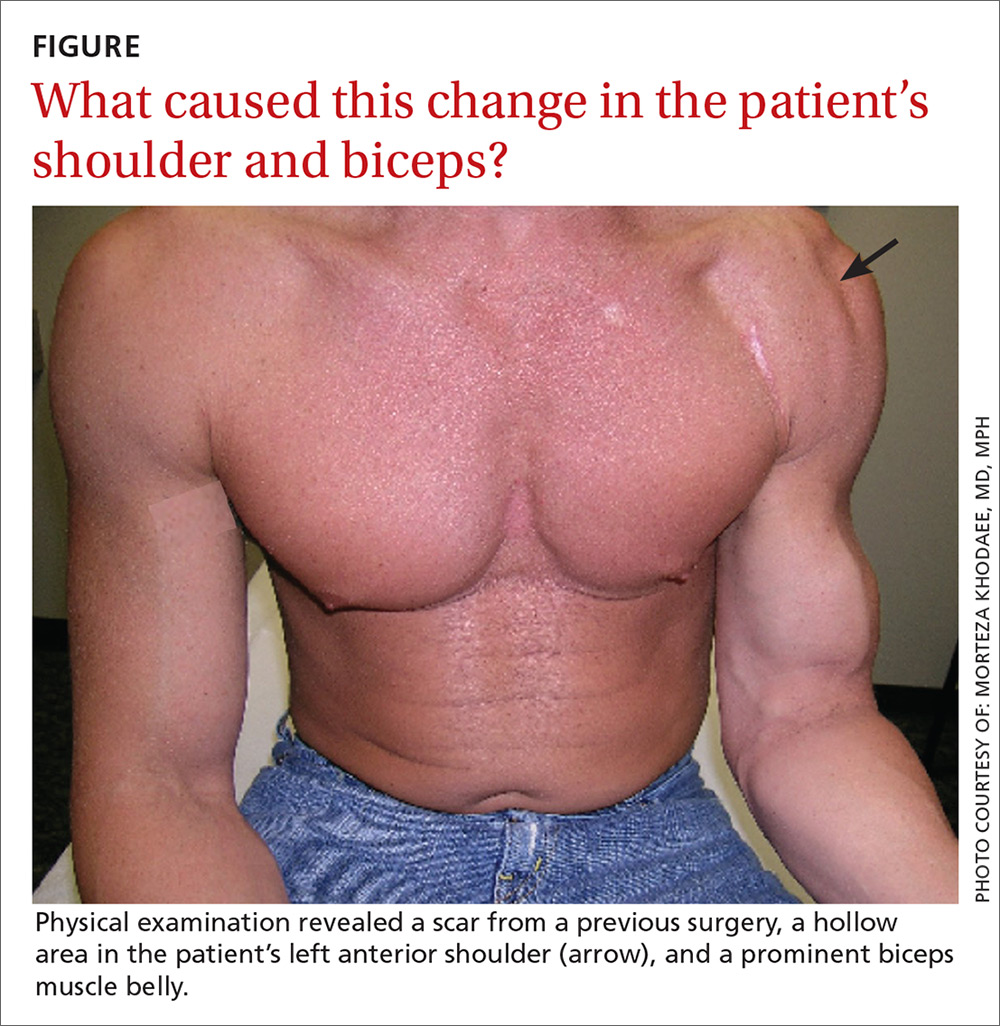
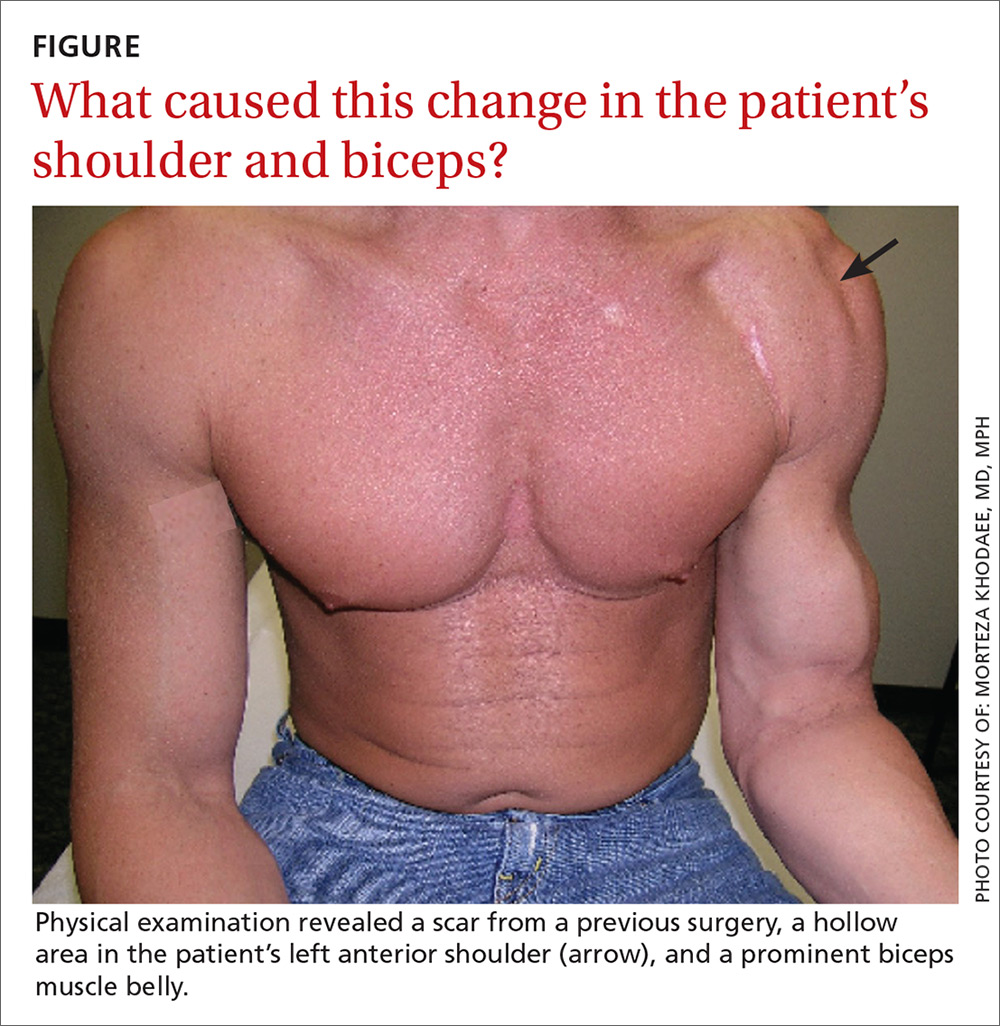
On physical examination, the patient had a scar from the previous surgery, a hollow area in his left anterior shoulder, and a prominent biceps muscle belly (FIGURE). His shoulder range of motion was normal. Left shoulder Neer, Hawkins-Kennedy, drop-arm, cross-arm, empty can, and apprehension tests were negative. A left Speed’s test (resisted elbow flexion when elbow is flexed 20° to 30° with the forearm in supination and the arm in about 60° of flexion) was positive for mild anterior shoulder pain. So, too, was a Yergason’s test (resisted forearm supination and elbow flexion when forearm is pronated and elbow is flexed to 90°). The patient’s elbow flexion strength was 4 out of 5, and his supination strength was 5 out of 5. Neurovascular and sensory examinations of his upper extremities, including radial and ulnar pulses, were normal.
THE DIAGNOSIS
A diagnostic musculoskeletal ultrasound revealed an empty tendon sheath of the long head of the biceps in the bicipital groove and a retracted echogenic stump with associated hematoma at the proximal musculotendinous junction. Based on the patient’s history, physical examination, and ultrasound, a diagnosis of an acute rupture of the left long head of the biceps brachii tendon was made.
DISCUSSION
Diagnosis of acute rupture is often made clinically based on a visually apparent defect proximally and a bulbous mass distally (“Popeye deformity”).1 Ultrasound and magnetic resonance imaging (MRI) may aid in the diagnosis by demonstrating an absence of the long head in the bicipital groove or at its insertion.
The biceps brachii tendon functions in flexion and supination of the forearm. The long head of the biceps also plays a stabilizing role in the glenohumeral joint during elbow flexion and supination.2 Injury to the biceps most often occurs in middle-aged men following a traumatic sudden eccentric bicipital contraction event, during which most patients describe a snapping or popping sensation.3,4
Rupture of the proximal biceps tendon represents about 90% of all biceps ruptures, which almost exclusively involve the long head of the biceps.3,5,6 Risk factors for tendon rupture include obesity, smoking, steroid injection in or around the tendon, and previous tendinopathy.7-10
Functional limitations. It is generally thought that functional limitations following a proximal biceps rupture are relatively minimal, due to the work of other flexors and supinators, including the brachialis and brachioradialis. However, because strength and endurance of the muscle can decrease by about 25%, physical laborers and high-demand athletes may notice a degree of residual weakness with supination and elbow flexion.11,12
Surgery is suitable for some, but not all
Surgical repair is recommended for acute ruptures in patients with high physical demands and for whom a slight loss of flexion and supination strength would not be well tolerated.13 Tenotomy and tenodesis are the main techniques used to surgically repair a rupture of the long head of the biceps brachii tendon. Although there is no consensus on which technique is superior, it seems that there is less cosmetic deformity and better post-surgery biomechanical strength with tenodesis compared with tenotomy.14 However, tenodesis is associated with a higher likelihood of bicipital pain,14 and recent case reports have suggested it is associated with an increased risk of humeral fracture.15 Therefore, each patient should be treated on an individual case basis, taking into account age, activity level, and physical demand.14
For most patients, treatment remains conservative with typically excellent outcomes. Nonoperative management includes gentle range-of-motion exercises for the prevention of contractures of the elbow and shoulder. Such exercises can be started almost immediately after injury. In one study, nonoperative management was recommended for patients with sedentary work, injury in the non-dominant arm, and acceptable cosmetic deformity. Researchers noted that patients who opt for a nonsurgical treatment generally do well with a home exercise program and rarely have stiffness.1
If the patient is a young athlete, if cosmetic deformity is unacceptable, or if the injury is in the dominant arm of a laborer, then the patient may want to consider tenodesis.1 Tangari et al found that in high-demand athletes, biceps tenodesis resulted in excellent functional and cosmetic results with no clinically significant decrease in strength after an average follow-up of 7.6 years.13 In a case s
Our patient elected to proceed with a tenodesis procedure. Two months after the surgery, he had fully recovered.
THE TAKEAWAY
Rupture of the biceps brachii tendon is relatively uncommon. In the vast majority of cases, it happens in the long head of the dominant arm of middle-aged men. Diagnosis is mainly clinical; however, ultrasound and MRI can confirm the diagnosis when there is doubt. Nonoperative management is appropriate for the majority of patients. Young athletes, patients who are concerned with cosmetic appearance, and labor workers with injury to their dominant arm should be referred to an orthopedic surgeon for possible surgery.
1. Geaney LE, Mazzocca AD. Biceps brachii tendon ruptures: a review of diagnosis and treatment of proximal and distal biceps tendon ruptures. Phys Sportsmed. 2010;38:117-125.
2. Payne LZ, Deng XH, Craig EV, et al. The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25:801-808.
3. Jayamoorthy T, Field JR, Costi JJ, et al. Biceps tenodesis: a biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13:160-164.
4. Mazzocca AD, Spang JT, Arciero RA. Distal biceps rupture. Orthop Clin North Am. 2008;39:237-249, vii.
5. Carter AN, Erickson SM. Proximal biceps tendon rupture: primarily an injury of middle age. Phys Sportsmed. 1999;27:95-101.
6. Elser F, Braun S, Dewing CB, et al. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581-592.
7. Kelly MP, Perkinson SG, Ablove RH, et al. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43:2012-2017.
8. Schneider A, Bennett JM, O’Connor DP, et al. Bilateral ruptures of the distal biceps brachii tendon. J Shoulder Elbow Surg. 2009;18:804-807.
9. Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999;8:644-654.
10. The Physician and Sportsmedicine. Complete rupture of large tendons. Risk factors, signs, and definitive treatment. Available at: https://orthony.com/directory/uploads/flik_complete-rupture-of-large-tendons.pdf. Accessed December 8, 2017.
11. Pearl ML, Bessos K, Wong K. Strength deficits related to distal biceps tendon rupture and repair. A case report. Am J Sports Med. 1998;26:295-296.
12. Deutch SR, Gelineck J, Johannsen HV, et al. Permanent disabilities in the displaced muscle from rupture of the long head tendon of the biceps. Scand J Med Sci Sports. 2005;15:159-162.
13. Tangari M, Carbone S, Gallo M, et al. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20:409-413.
14. Hsu AR, Ghodadra NS, Provencher MT, et al. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326-332.
15. Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7-e11.
THE CASE
A 41-year-old, right-hand dominant man sought care at our facility one day after trying to pull his boat out of the water. He’d tried to lift the boat with his hands while his forearms were fully supinated and his elbows were flexed to about 90°. He then felt a sharp burning sensation in his left anterior shoulder and was unable to lift the boat. The patient denied feeling a popping sensation at the time of the injury. He had mild pain at night, but was able to sleep. He said that he had mild diminished strength with elbow flexion, but denied having any numbness, tingling, or discoloration of his skin.
The patient said he did weightlifting and strength training of his upper and lower extremities 4 times/week. He was in good general health, was not taking any medications or supplements, and denied smoking or using illicit drugs. His surgical history was significant for a Bankart repair 8 years ago.
On physical examination, the patient had a scar from the previous surgery, a hollow area in his left anterior shoulder, and a prominent biceps muscle belly (FIGURE). His shoulder range of motion was normal. Left shoulder Neer, Hawkins-Kennedy, drop-arm, cross-arm, empty can, and apprehension tests were negative. A left Speed’s test (resisted elbow flexion when elbow is flexed 20° to 30° with the forearm in supination and the arm in about 60° of flexion) was positive for mild anterior shoulder pain. So, too, was a Yergason’s test (resisted forearm supination and elbow flexion when forearm is pronated and elbow is flexed to 90°). The patient’s elbow flexion strength was 4 out of 5, and his supination strength was 5 out of 5. Neurovascular and sensory examinations of his upper extremities, including radial and ulnar pulses, were normal.
THE DIAGNOSIS
A diagnostic musculoskeletal ultrasound revealed an empty tendon sheath of the long head of the biceps in the bicipital groove and a retracted echogenic stump with associated hematoma at the proximal musculotendinous junction. Based on the patient’s history, physical examination, and ultrasound, a diagnosis of an acute rupture of the left long head of the biceps brachii tendon was made.
DISCUSSION
Diagnosis of acute rupture is often made clinically based on a visually apparent defect proximally and a bulbous mass distally (“Popeye deformity”).1 Ultrasound and magnetic resonance imaging (MRI) may aid in the diagnosis by demonstrating an absence of the long head in the bicipital groove or at its insertion.
The biceps brachii tendon functions in flexion and supination of the forearm. The long head of the biceps also plays a stabilizing role in the glenohumeral joint during elbow flexion and supination.2 Injury to the biceps most often occurs in middle-aged men following a traumatic sudden eccentric bicipital contraction event, during which most patients describe a snapping or popping sensation.3,4
Rupture of the proximal biceps tendon represents about 90% of all biceps ruptures, which almost exclusively involve the long head of the biceps.3,5,6 Risk factors for tendon rupture include obesity, smoking, steroid injection in or around the tendon, and previous tendinopathy.7-10
Functional limitations. It is generally thought that functional limitations following a proximal biceps rupture are relatively minimal, due to the work of other flexors and supinators, including the brachialis and brachioradialis. However, because strength and endurance of the muscle can decrease by about 25%, physical laborers and high-demand athletes may notice a degree of residual weakness with supination and elbow flexion.11,12
Surgery is suitable for some, but not all
Surgical repair is recommended for acute ruptures in patients with high physical demands and for whom a slight loss of flexion and supination strength would not be well tolerated.13 Tenotomy and tenodesis are the main techniques used to surgically repair a rupture of the long head of the biceps brachii tendon. Although there is no consensus on which technique is superior, it seems that there is less cosmetic deformity and better post-surgery biomechanical strength with tenodesis compared with tenotomy.14 However, tenodesis is associated with a higher likelihood of bicipital pain,14 and recent case reports have suggested it is associated with an increased risk of humeral fracture.15 Therefore, each patient should be treated on an individual case basis, taking into account age, activity level, and physical demand.14
For most patients, treatment remains conservative with typically excellent outcomes. Nonoperative management includes gentle range-of-motion exercises for the prevention of contractures of the elbow and shoulder. Such exercises can be started almost immediately after injury. In one study, nonoperative management was recommended for patients with sedentary work, injury in the non-dominant arm, and acceptable cosmetic deformity. Researchers noted that patients who opt for a nonsurgical treatment generally do well with a home exercise program and rarely have stiffness.1
If the patient is a young athlete, if cosmetic deformity is unacceptable, or if the injury is in the dominant arm of a laborer, then the patient may want to consider tenodesis.1 Tangari et al found that in high-demand athletes, biceps tenodesis resulted in excellent functional and cosmetic results with no clinically significant decrease in strength after an average follow-up of 7.6 years.13 In a case s
Our patient elected to proceed with a tenodesis procedure. Two months after the surgery, he had fully recovered.
THE TAKEAWAY
Rupture of the biceps brachii tendon is relatively uncommon. In the vast majority of cases, it happens in the long head of the dominant arm of middle-aged men. Diagnosis is mainly clinical; however, ultrasound and MRI can confirm the diagnosis when there is doubt. Nonoperative management is appropriate for the majority of patients. Young athletes, patients who are concerned with cosmetic appearance, and labor workers with injury to their dominant arm should be referred to an orthopedic surgeon for possible surgery.
THE CASE
A 41-year-old, right-hand dominant man sought care at our facility one day after trying to pull his boat out of the water. He’d tried to lift the boat with his hands while his forearms were fully supinated and his elbows were flexed to about 90°. He then felt a sharp burning sensation in his left anterior shoulder and was unable to lift the boat. The patient denied feeling a popping sensation at the time of the injury. He had mild pain at night, but was able to sleep. He said that he had mild diminished strength with elbow flexion, but denied having any numbness, tingling, or discoloration of his skin.
The patient said he did weightlifting and strength training of his upper and lower extremities 4 times/week. He was in good general health, was not taking any medications or supplements, and denied smoking or using illicit drugs. His surgical history was significant for a Bankart repair 8 years ago.
On physical examination, the patient had a scar from the previous surgery, a hollow area in his left anterior shoulder, and a prominent biceps muscle belly (FIGURE). His shoulder range of motion was normal. Left shoulder Neer, Hawkins-Kennedy, drop-arm, cross-arm, empty can, and apprehension tests were negative. A left Speed’s test (resisted elbow flexion when elbow is flexed 20° to 30° with the forearm in supination and the arm in about 60° of flexion) was positive for mild anterior shoulder pain. So, too, was a Yergason’s test (resisted forearm supination and elbow flexion when forearm is pronated and elbow is flexed to 90°). The patient’s elbow flexion strength was 4 out of 5, and his supination strength was 5 out of 5. Neurovascular and sensory examinations of his upper extremities, including radial and ulnar pulses, were normal.
THE DIAGNOSIS
A diagnostic musculoskeletal ultrasound revealed an empty tendon sheath of the long head of the biceps in the bicipital groove and a retracted echogenic stump with associated hematoma at the proximal musculotendinous junction. Based on the patient’s history, physical examination, and ultrasound, a diagnosis of an acute rupture of the left long head of the biceps brachii tendon was made.
DISCUSSION
Diagnosis of acute rupture is often made clinically based on a visually apparent defect proximally and a bulbous mass distally (“Popeye deformity”).1 Ultrasound and magnetic resonance imaging (MRI) may aid in the diagnosis by demonstrating an absence of the long head in the bicipital groove or at its insertion.
The biceps brachii tendon functions in flexion and supination of the forearm. The long head of the biceps also plays a stabilizing role in the glenohumeral joint during elbow flexion and supination.2 Injury to the biceps most often occurs in middle-aged men following a traumatic sudden eccentric bicipital contraction event, during which most patients describe a snapping or popping sensation.3,4
Rupture of the proximal biceps tendon represents about 90% of all biceps ruptures, which almost exclusively involve the long head of the biceps.3,5,6 Risk factors for tendon rupture include obesity, smoking, steroid injection in or around the tendon, and previous tendinopathy.7-10
Functional limitations. It is generally thought that functional limitations following a proximal biceps rupture are relatively minimal, due to the work of other flexors and supinators, including the brachialis and brachioradialis. However, because strength and endurance of the muscle can decrease by about 25%, physical laborers and high-demand athletes may notice a degree of residual weakness with supination and elbow flexion.11,12
Surgery is suitable for some, but not all
Surgical repair is recommended for acute ruptures in patients with high physical demands and for whom a slight loss of flexion and supination strength would not be well tolerated.13 Tenotomy and tenodesis are the main techniques used to surgically repair a rupture of the long head of the biceps brachii tendon. Although there is no consensus on which technique is superior, it seems that there is less cosmetic deformity and better post-surgery biomechanical strength with tenodesis compared with tenotomy.14 However, tenodesis is associated with a higher likelihood of bicipital pain,14 and recent case reports have suggested it is associated with an increased risk of humeral fracture.15 Therefore, each patient should be treated on an individual case basis, taking into account age, activity level, and physical demand.14
For most patients, treatment remains conservative with typically excellent outcomes. Nonoperative management includes gentle range-of-motion exercises for the prevention of contractures of the elbow and shoulder. Such exercises can be started almost immediately after injury. In one study, nonoperative management was recommended for patients with sedentary work, injury in the non-dominant arm, and acceptable cosmetic deformity. Researchers noted that patients who opt for a nonsurgical treatment generally do well with a home exercise program and rarely have stiffness.1
If the patient is a young athlete, if cosmetic deformity is unacceptable, or if the injury is in the dominant arm of a laborer, then the patient may want to consider tenodesis.1 Tangari et al found that in high-demand athletes, biceps tenodesis resulted in excellent functional and cosmetic results with no clinically significant decrease in strength after an average follow-up of 7.6 years.13 In a case s
Our patient elected to proceed with a tenodesis procedure. Two months after the surgery, he had fully recovered.
THE TAKEAWAY
Rupture of the biceps brachii tendon is relatively uncommon. In the vast majority of cases, it happens in the long head of the dominant arm of middle-aged men. Diagnosis is mainly clinical; however, ultrasound and MRI can confirm the diagnosis when there is doubt. Nonoperative management is appropriate for the majority of patients. Young athletes, patients who are concerned with cosmetic appearance, and labor workers with injury to their dominant arm should be referred to an orthopedic surgeon for possible surgery.
1. Geaney LE, Mazzocca AD. Biceps brachii tendon ruptures: a review of diagnosis and treatment of proximal and distal biceps tendon ruptures. Phys Sportsmed. 2010;38:117-125.
2. Payne LZ, Deng XH, Craig EV, et al. The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25:801-808.
3. Jayamoorthy T, Field JR, Costi JJ, et al. Biceps tenodesis: a biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13:160-164.
4. Mazzocca AD, Spang JT, Arciero RA. Distal biceps rupture. Orthop Clin North Am. 2008;39:237-249, vii.
5. Carter AN, Erickson SM. Proximal biceps tendon rupture: primarily an injury of middle age. Phys Sportsmed. 1999;27:95-101.
6. Elser F, Braun S, Dewing CB, et al. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581-592.
7. Kelly MP, Perkinson SG, Ablove RH, et al. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43:2012-2017.
8. Schneider A, Bennett JM, O’Connor DP, et al. Bilateral ruptures of the distal biceps brachii tendon. J Shoulder Elbow Surg. 2009;18:804-807.
9. Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999;8:644-654.
10. The Physician and Sportsmedicine. Complete rupture of large tendons. Risk factors, signs, and definitive treatment. Available at: https://orthony.com/directory/uploads/flik_complete-rupture-of-large-tendons.pdf. Accessed December 8, 2017.
11. Pearl ML, Bessos K, Wong K. Strength deficits related to distal biceps tendon rupture and repair. A case report. Am J Sports Med. 1998;26:295-296.
12. Deutch SR, Gelineck J, Johannsen HV, et al. Permanent disabilities in the displaced muscle from rupture of the long head tendon of the biceps. Scand J Med Sci Sports. 2005;15:159-162.
13. Tangari M, Carbone S, Gallo M, et al. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20:409-413.
14. Hsu AR, Ghodadra NS, Provencher MT, et al. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326-332.
15. Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7-e11.
1. Geaney LE, Mazzocca AD. Biceps brachii tendon ruptures: a review of diagnosis and treatment of proximal and distal biceps tendon ruptures. Phys Sportsmed. 2010;38:117-125.
2. Payne LZ, Deng XH, Craig EV, et al. The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25:801-808.
3. Jayamoorthy T, Field JR, Costi JJ, et al. Biceps tenodesis: a biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13:160-164.
4. Mazzocca AD, Spang JT, Arciero RA. Distal biceps rupture. Orthop Clin North Am. 2008;39:237-249, vii.
5. Carter AN, Erickson SM. Proximal biceps tendon rupture: primarily an injury of middle age. Phys Sportsmed. 1999;27:95-101.
6. Elser F, Braun S, Dewing CB, et al. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581-592.
7. Kelly MP, Perkinson SG, Ablove RH, et al. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43:2012-2017.
8. Schneider A, Bennett JM, O’Connor DP, et al. Bilateral ruptures of the distal biceps brachii tendon. J Shoulder Elbow Surg. 2009;18:804-807.
9. Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999;8:644-654.
10. The Physician and Sportsmedicine. Complete rupture of large tendons. Risk factors, signs, and definitive treatment. Available at: https://orthony.com/directory/uploads/flik_complete-rupture-of-large-tendons.pdf. Accessed December 8, 2017.
11. Pearl ML, Bessos K, Wong K. Strength deficits related to distal biceps tendon rupture and repair. A case report. Am J Sports Med. 1998;26:295-296.
12. Deutch SR, Gelineck J, Johannsen HV, et al. Permanent disabilities in the displaced muscle from rupture of the long head tendon of the biceps. Scand J Med Sci Sports. 2005;15:159-162.
13. Tangari M, Carbone S, Gallo M, et al. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20:409-413.
14. Hsu AR, Ghodadra NS, Provencher MT, et al. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326-332.
15. Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7-e11.
