User login
One practice’s experience with obesity treatment
WASHINGTON – “We have heard about a lot of really interesting new things in therapy, but the reality is that they are just not economically viable at present,” said David Feldshon, MD, of Minnesota Gastroenterology (MNGI), speaking about his experience with offering obesity treatment in his practice.
One problem that Dr. Feldshon and MNGI faced was that they could never get enough patients into their weight loss program, a meal-replacement program priced at about $200 a month. Part of this program, Optifast, a commercially available low-calorie diet and behavior modification program, cost about $360 a month. Most patients found the cost to be prohibitive according to Dr. Feldshon. The program that MNGI offered was fairly competitive when compared with a number of other commercial diet programs like Nutrisystem and Medifast, which cost $300 and $329 a month, respectively.
Because of the economic pressure these programs can exert on patients, Dr. Feldshon spoke to the difficulty of recruiting patients with major metabolic and digestive disorders. “I work in the liver clinic, so I see people with NASH, NAFLD, cirrhosis, near-cirrhosis, diabetes. These are people that would really benefit from this type of program, and I could not get a single patient to sign up.”
For Dr. Feldshon’s program, patients were required to come to MNGI once a week, which led to higher dropout rates. This is troubling because it is important that patients meet with doctors and other patients as part of a weight loss program. But the inconvenience for patients and doctors is not just in physically attending meetings, but in the medical billing. The Affordable Care Act and Medicare cover obesity screening and counseling, but this is only for primary care physicians, nurse practitioners, physician assistants, or clinical nurse specialists. These limits may not extend into private insurance, but they remain a barrier for those covered by Medicare, according to Dr. Feldshon.
Another effective but ultimately expensive option is weight loss drugs. The cost of drugs can vary wildly. Even well-established drugs like phentermine can cost anywhere from $5 to $35 out of pocket a month, according to Dr. Feldshon. Some drugs, like Saxenda, can cost as much as $1,414 per month if paid for out of pocket. While Saxenda is effective, there is a catch in the prescribing and billing for this drug: “The moment you go above 2.4 mg per day, the insurance company says, ‘Aha! He’s treating obesity,’ and they stop covering it.” One drug that Dr. Feldshon recommends is topiramate because it is a multiuse drug. “Often, the insurance company can’t figure out why you’re prescribing it, so they’ll okay it,” said Dr. Feldshon.
One of the most effective nonsurgical methods of weight loss is intragastric balloon. From 2016 to 2017, MNGI used gastric balloons in 22 patients, resulting in 11.4% total body weight loss in these patients. Unfortunately, it was a “financial loser,” according to Dr. Feldshon. The global case rate charge for one balloon is $8,200. MNGI then incurred $2,000 per balloon, $3,000 in hospital charges, $750 for the medical weight loss program, $1,350 for office personnel and visits, and a calculated opportunity cost of $3,140 resulting in a net loss of $2,040 per balloon. The most important factor in this calculation is the opportunity cost, which includes travel to and from the hospital and phone encounters with patients, which took away Dr. Feldshon’s ability to conduct colonoscopies and GI consults.
In an attempt to make balloons cost effective, Dr. Feldshon committed to doing these procedures on his day off, which reduced the opportunity cost to $0. This made the balloon procedure profitable, at $1,100 per balloon, but the volume was too low to make it worthwhile.
Despite the challenges his group faced with treating obesity, Dr. Feldshon offered some cost-saving solutions to help keep costs down for both patients and doctors. He suggested avoiding manufacturer weight loss programs. Identify an internal program that is reasonably priced or an external program like Weight Watchers. Physicians can utilize video conferencing for weekly meetings; this helps patients interact with doctors, and products like AdobeConnect cost physicians only about $50 a month. Patients can use free online journaling products like MyFitnessPal to track diet and exercise. Physicians can also recommend using generic and over-the-counter drugs and consider enlisting the help of a life coach or dietitian.
“All obese patients benefit from weight loss but we should be targeting those with metabolic syndrome, diabetes, heart disease, hypercholesterolemia, hyperlipidemia, and increased abdominal girth,” said Dr. Feldshon.
Dr. Feldshon has served on advisory committees and review panels and has worked with United Health Group as well as Prime Therapeutics.
AGA Resource
AGA has created an Obesity Practice Guide to provide gastroenterologists with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management, including a model for how to operationalize business issues.
The increase in the proportion of people who are overweight and obese presents gastroenterologists with new challenges and opportunities. Our internal medicine background, experience in nutrition, and role as endoscopists puts us in a unique position to manage obesity. In addition, many GI conditions are directly affected by obesity, including NASH, GERD, pancreatic diseases, and colon cancer. Good nutrition will always be the cornerstone of healthy weight, but nutritional advice alone results in modest (2%-3%) total weight loss. This can be augmented with medications, meal replacement, endobariatrics, and combinations of these.
Having said this, there are significant challenges to managing obesity as a gastroenterologist, and these stem almost entirely from the fact that there is poor coverage for these therapeutic options, as emphasized by Dr. Feldshon. However, it is still important to bring weight loss interventions into our clinical practice – for many reasons.
First, unlike other obesity management programs, we are typically not managing obesity in isolation. Usually, we are managing obesity in the setting of a disease state such as NASH. When we manage patients with NASH and stage 3 fibrosis, the patients’ decision making on how much to invest to prevent further progression is different; they’re more likely to take on some costs. Second, the degree of coverage for medications is improving. Similarly, although endobariatrics is not currently covered, with time it likely will be under certain criteria.
We need to build the clinical experience necessary to manage obesity and do so now, or other specialties will have become the main providers of weight loss interventions. This will become a lost opportunity for both medical and endobariatric management of these patients by us.
So despite the challenges raised by Dr. Feldshon, I would suggest that a practicing gastroenterologist interested in weight loss management focus on patients with obesity-related diseases first and expand their focus incrementally.
Wahajat Mehal, MD, DPhil, is a hepatologist and director of the Yale Weight Loss Program at Yale University, New Haven, Conn. He is an associate editor for GI & Hepatology News.
The increase in the proportion of people who are overweight and obese presents gastroenterologists with new challenges and opportunities. Our internal medicine background, experience in nutrition, and role as endoscopists puts us in a unique position to manage obesity. In addition, many GI conditions are directly affected by obesity, including NASH, GERD, pancreatic diseases, and colon cancer. Good nutrition will always be the cornerstone of healthy weight, but nutritional advice alone results in modest (2%-3%) total weight loss. This can be augmented with medications, meal replacement, endobariatrics, and combinations of these.
Having said this, there are significant challenges to managing obesity as a gastroenterologist, and these stem almost entirely from the fact that there is poor coverage for these therapeutic options, as emphasized by Dr. Feldshon. However, it is still important to bring weight loss interventions into our clinical practice – for many reasons.
First, unlike other obesity management programs, we are typically not managing obesity in isolation. Usually, we are managing obesity in the setting of a disease state such as NASH. When we manage patients with NASH and stage 3 fibrosis, the patients’ decision making on how much to invest to prevent further progression is different; they’re more likely to take on some costs. Second, the degree of coverage for medications is improving. Similarly, although endobariatrics is not currently covered, with time it likely will be under certain criteria.
We need to build the clinical experience necessary to manage obesity and do so now, or other specialties will have become the main providers of weight loss interventions. This will become a lost opportunity for both medical and endobariatric management of these patients by us.
So despite the challenges raised by Dr. Feldshon, I would suggest that a practicing gastroenterologist interested in weight loss management focus on patients with obesity-related diseases first and expand their focus incrementally.
Wahajat Mehal, MD, DPhil, is a hepatologist and director of the Yale Weight Loss Program at Yale University, New Haven, Conn. He is an associate editor for GI & Hepatology News.
The increase in the proportion of people who are overweight and obese presents gastroenterologists with new challenges and opportunities. Our internal medicine background, experience in nutrition, and role as endoscopists puts us in a unique position to manage obesity. In addition, many GI conditions are directly affected by obesity, including NASH, GERD, pancreatic diseases, and colon cancer. Good nutrition will always be the cornerstone of healthy weight, but nutritional advice alone results in modest (2%-3%) total weight loss. This can be augmented with medications, meal replacement, endobariatrics, and combinations of these.
Having said this, there are significant challenges to managing obesity as a gastroenterologist, and these stem almost entirely from the fact that there is poor coverage for these therapeutic options, as emphasized by Dr. Feldshon. However, it is still important to bring weight loss interventions into our clinical practice – for many reasons.
First, unlike other obesity management programs, we are typically not managing obesity in isolation. Usually, we are managing obesity in the setting of a disease state such as NASH. When we manage patients with NASH and stage 3 fibrosis, the patients’ decision making on how much to invest to prevent further progression is different; they’re more likely to take on some costs. Second, the degree of coverage for medications is improving. Similarly, although endobariatrics is not currently covered, with time it likely will be under certain criteria.
We need to build the clinical experience necessary to manage obesity and do so now, or other specialties will have become the main providers of weight loss interventions. This will become a lost opportunity for both medical and endobariatric management of these patients by us.
So despite the challenges raised by Dr. Feldshon, I would suggest that a practicing gastroenterologist interested in weight loss management focus on patients with obesity-related diseases first and expand their focus incrementally.
Wahajat Mehal, MD, DPhil, is a hepatologist and director of the Yale Weight Loss Program at Yale University, New Haven, Conn. He is an associate editor for GI & Hepatology News.
WASHINGTON – “We have heard about a lot of really interesting new things in therapy, but the reality is that they are just not economically viable at present,” said David Feldshon, MD, of Minnesota Gastroenterology (MNGI), speaking about his experience with offering obesity treatment in his practice.
One problem that Dr. Feldshon and MNGI faced was that they could never get enough patients into their weight loss program, a meal-replacement program priced at about $200 a month. Part of this program, Optifast, a commercially available low-calorie diet and behavior modification program, cost about $360 a month. Most patients found the cost to be prohibitive according to Dr. Feldshon. The program that MNGI offered was fairly competitive when compared with a number of other commercial diet programs like Nutrisystem and Medifast, which cost $300 and $329 a month, respectively.
Because of the economic pressure these programs can exert on patients, Dr. Feldshon spoke to the difficulty of recruiting patients with major metabolic and digestive disorders. “I work in the liver clinic, so I see people with NASH, NAFLD, cirrhosis, near-cirrhosis, diabetes. These are people that would really benefit from this type of program, and I could not get a single patient to sign up.”
For Dr. Feldshon’s program, patients were required to come to MNGI once a week, which led to higher dropout rates. This is troubling because it is important that patients meet with doctors and other patients as part of a weight loss program. But the inconvenience for patients and doctors is not just in physically attending meetings, but in the medical billing. The Affordable Care Act and Medicare cover obesity screening and counseling, but this is only for primary care physicians, nurse practitioners, physician assistants, or clinical nurse specialists. These limits may not extend into private insurance, but they remain a barrier for those covered by Medicare, according to Dr. Feldshon.
Another effective but ultimately expensive option is weight loss drugs. The cost of drugs can vary wildly. Even well-established drugs like phentermine can cost anywhere from $5 to $35 out of pocket a month, according to Dr. Feldshon. Some drugs, like Saxenda, can cost as much as $1,414 per month if paid for out of pocket. While Saxenda is effective, there is a catch in the prescribing and billing for this drug: “The moment you go above 2.4 mg per day, the insurance company says, ‘Aha! He’s treating obesity,’ and they stop covering it.” One drug that Dr. Feldshon recommends is topiramate because it is a multiuse drug. “Often, the insurance company can’t figure out why you’re prescribing it, so they’ll okay it,” said Dr. Feldshon.
One of the most effective nonsurgical methods of weight loss is intragastric balloon. From 2016 to 2017, MNGI used gastric balloons in 22 patients, resulting in 11.4% total body weight loss in these patients. Unfortunately, it was a “financial loser,” according to Dr. Feldshon. The global case rate charge for one balloon is $8,200. MNGI then incurred $2,000 per balloon, $3,000 in hospital charges, $750 for the medical weight loss program, $1,350 for office personnel and visits, and a calculated opportunity cost of $3,140 resulting in a net loss of $2,040 per balloon. The most important factor in this calculation is the opportunity cost, which includes travel to and from the hospital and phone encounters with patients, which took away Dr. Feldshon’s ability to conduct colonoscopies and GI consults.
In an attempt to make balloons cost effective, Dr. Feldshon committed to doing these procedures on his day off, which reduced the opportunity cost to $0. This made the balloon procedure profitable, at $1,100 per balloon, but the volume was too low to make it worthwhile.
Despite the challenges his group faced with treating obesity, Dr. Feldshon offered some cost-saving solutions to help keep costs down for both patients and doctors. He suggested avoiding manufacturer weight loss programs. Identify an internal program that is reasonably priced or an external program like Weight Watchers. Physicians can utilize video conferencing for weekly meetings; this helps patients interact with doctors, and products like AdobeConnect cost physicians only about $50 a month. Patients can use free online journaling products like MyFitnessPal to track diet and exercise. Physicians can also recommend using generic and over-the-counter drugs and consider enlisting the help of a life coach or dietitian.
“All obese patients benefit from weight loss but we should be targeting those with metabolic syndrome, diabetes, heart disease, hypercholesterolemia, hyperlipidemia, and increased abdominal girth,” said Dr. Feldshon.
Dr. Feldshon has served on advisory committees and review panels and has worked with United Health Group as well as Prime Therapeutics.
AGA Resource
AGA has created an Obesity Practice Guide to provide gastroenterologists with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management, including a model for how to operationalize business issues.
WASHINGTON – “We have heard about a lot of really interesting new things in therapy, but the reality is that they are just not economically viable at present,” said David Feldshon, MD, of Minnesota Gastroenterology (MNGI), speaking about his experience with offering obesity treatment in his practice.
One problem that Dr. Feldshon and MNGI faced was that they could never get enough patients into their weight loss program, a meal-replacement program priced at about $200 a month. Part of this program, Optifast, a commercially available low-calorie diet and behavior modification program, cost about $360 a month. Most patients found the cost to be prohibitive according to Dr. Feldshon. The program that MNGI offered was fairly competitive when compared with a number of other commercial diet programs like Nutrisystem and Medifast, which cost $300 and $329 a month, respectively.
Because of the economic pressure these programs can exert on patients, Dr. Feldshon spoke to the difficulty of recruiting patients with major metabolic and digestive disorders. “I work in the liver clinic, so I see people with NASH, NAFLD, cirrhosis, near-cirrhosis, diabetes. These are people that would really benefit from this type of program, and I could not get a single patient to sign up.”
For Dr. Feldshon’s program, patients were required to come to MNGI once a week, which led to higher dropout rates. This is troubling because it is important that patients meet with doctors and other patients as part of a weight loss program. But the inconvenience for patients and doctors is not just in physically attending meetings, but in the medical billing. The Affordable Care Act and Medicare cover obesity screening and counseling, but this is only for primary care physicians, nurse practitioners, physician assistants, or clinical nurse specialists. These limits may not extend into private insurance, but they remain a barrier for those covered by Medicare, according to Dr. Feldshon.
Another effective but ultimately expensive option is weight loss drugs. The cost of drugs can vary wildly. Even well-established drugs like phentermine can cost anywhere from $5 to $35 out of pocket a month, according to Dr. Feldshon. Some drugs, like Saxenda, can cost as much as $1,414 per month if paid for out of pocket. While Saxenda is effective, there is a catch in the prescribing and billing for this drug: “The moment you go above 2.4 mg per day, the insurance company says, ‘Aha! He’s treating obesity,’ and they stop covering it.” One drug that Dr. Feldshon recommends is topiramate because it is a multiuse drug. “Often, the insurance company can’t figure out why you’re prescribing it, so they’ll okay it,” said Dr. Feldshon.
One of the most effective nonsurgical methods of weight loss is intragastric balloon. From 2016 to 2017, MNGI used gastric balloons in 22 patients, resulting in 11.4% total body weight loss in these patients. Unfortunately, it was a “financial loser,” according to Dr. Feldshon. The global case rate charge for one balloon is $8,200. MNGI then incurred $2,000 per balloon, $3,000 in hospital charges, $750 for the medical weight loss program, $1,350 for office personnel and visits, and a calculated opportunity cost of $3,140 resulting in a net loss of $2,040 per balloon. The most important factor in this calculation is the opportunity cost, which includes travel to and from the hospital and phone encounters with patients, which took away Dr. Feldshon’s ability to conduct colonoscopies and GI consults.
In an attempt to make balloons cost effective, Dr. Feldshon committed to doing these procedures on his day off, which reduced the opportunity cost to $0. This made the balloon procedure profitable, at $1,100 per balloon, but the volume was too low to make it worthwhile.
Despite the challenges his group faced with treating obesity, Dr. Feldshon offered some cost-saving solutions to help keep costs down for both patients and doctors. He suggested avoiding manufacturer weight loss programs. Identify an internal program that is reasonably priced or an external program like Weight Watchers. Physicians can utilize video conferencing for weekly meetings; this helps patients interact with doctors, and products like AdobeConnect cost physicians only about $50 a month. Patients can use free online journaling products like MyFitnessPal to track diet and exercise. Physicians can also recommend using generic and over-the-counter drugs and consider enlisting the help of a life coach or dietitian.
“All obese patients benefit from weight loss but we should be targeting those with metabolic syndrome, diabetes, heart disease, hypercholesterolemia, hyperlipidemia, and increased abdominal girth,” said Dr. Feldshon.
Dr. Feldshon has served on advisory committees and review panels and has worked with United Health Group as well as Prime Therapeutics.
AGA Resource
AGA has created an Obesity Practice Guide to provide gastroenterologists with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management, including a model for how to operationalize business issues.
EXPERT ANALYSIS FROM DDW 2018
Cost is high for Japanese encephalitis vaccinations
Vaccination costs surrounding Japanese encephalitis is high, according to an economic analysis presented at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
The analytic horizon for this research was 6 years, but productivity losses were evaluated over average life expectancy.
The researchers analyzed their data from two analytic perspectives: societal and traveler perspective. Factors analyzed included vaccine per dose, vaccine administration cost, and vaccine adverse events costs per vaccine.
The researchers assessed the risk to travelers based upon disease incidence among different groups. The highest-risk travelers (Group 1) – those who planned to spend a month or more in JE-endemic areas – had an incidence rate of 0.53/1 million travelers. Group 2 travelers – those who planned to stay less than a month and more than a fifth of their time outdoors – had an incidence rate of 0.25/1 million. Group 3 travelers, at lowest risk, had the lowest incidence rate at 0.04/1 million.
The calculated societal perspective cost per outcome averted was quite high for each risk group. For Group 1, the cost was $596 million per case averted. This cost rose to $1.3 billion for each case of long-term sequelae averted, and rose even higher to avert death, to $1.8 billion per death averted. These costs nearly doubled for Group 2, and in Group 3, the cost ballooned to $7.9 billion to avert one case of JE, $17 billion per prevention of long-term sequelae, and $23 billion per death averted.
The individual costs for JE vaccination are $292 per dose, with an administration fee of $46. Short-term treatment of JE costs nearly $30,000, and long-term treatment of JE also comes with a large bill of $8,437.
These costs are not simply monetary but are also felt in lost economic productivity. The cost of complete short-term recovery is nearly $60,000. Over an individual’s lifetime, this number rose to more than $1.5 million based on total loss of productivity.
Of the 67% of patients who survive JE, 32% recover completely while 68% deal with long-term sequelae. Of those, 28% experience mild symptoms while the remaining 72% have severe sequelae.
JE vaccine effectiveness does not appear to be an issue, with a 0.91 proportion of neutralizing antibodies seen after 1 year. With booster doses, vaccine effectiveness is 0.96.
There are limitations to this study, such as results being affected by the uncertainty of JE incidence. “The single most important variable is incidence,” stated Dr. Meltzer.
Vaccination costs surrounding Japanese encephalitis is high, according to an economic analysis presented at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
The analytic horizon for this research was 6 years, but productivity losses were evaluated over average life expectancy.
The researchers analyzed their data from two analytic perspectives: societal and traveler perspective. Factors analyzed included vaccine per dose, vaccine administration cost, and vaccine adverse events costs per vaccine.
The researchers assessed the risk to travelers based upon disease incidence among different groups. The highest-risk travelers (Group 1) – those who planned to spend a month or more in JE-endemic areas – had an incidence rate of 0.53/1 million travelers. Group 2 travelers – those who planned to stay less than a month and more than a fifth of their time outdoors – had an incidence rate of 0.25/1 million. Group 3 travelers, at lowest risk, had the lowest incidence rate at 0.04/1 million.
The calculated societal perspective cost per outcome averted was quite high for each risk group. For Group 1, the cost was $596 million per case averted. This cost rose to $1.3 billion for each case of long-term sequelae averted, and rose even higher to avert death, to $1.8 billion per death averted. These costs nearly doubled for Group 2, and in Group 3, the cost ballooned to $7.9 billion to avert one case of JE, $17 billion per prevention of long-term sequelae, and $23 billion per death averted.
The individual costs for JE vaccination are $292 per dose, with an administration fee of $46. Short-term treatment of JE costs nearly $30,000, and long-term treatment of JE also comes with a large bill of $8,437.
These costs are not simply monetary but are also felt in lost economic productivity. The cost of complete short-term recovery is nearly $60,000. Over an individual’s lifetime, this number rose to more than $1.5 million based on total loss of productivity.
Of the 67% of patients who survive JE, 32% recover completely while 68% deal with long-term sequelae. Of those, 28% experience mild symptoms while the remaining 72% have severe sequelae.
JE vaccine effectiveness does not appear to be an issue, with a 0.91 proportion of neutralizing antibodies seen after 1 year. With booster doses, vaccine effectiveness is 0.96.
There are limitations to this study, such as results being affected by the uncertainty of JE incidence. “The single most important variable is incidence,” stated Dr. Meltzer.
Vaccination costs surrounding Japanese encephalitis is high, according to an economic analysis presented at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
The analytic horizon for this research was 6 years, but productivity losses were evaluated over average life expectancy.
The researchers analyzed their data from two analytic perspectives: societal and traveler perspective. Factors analyzed included vaccine per dose, vaccine administration cost, and vaccine adverse events costs per vaccine.
The researchers assessed the risk to travelers based upon disease incidence among different groups. The highest-risk travelers (Group 1) – those who planned to spend a month or more in JE-endemic areas – had an incidence rate of 0.53/1 million travelers. Group 2 travelers – those who planned to stay less than a month and more than a fifth of their time outdoors – had an incidence rate of 0.25/1 million. Group 3 travelers, at lowest risk, had the lowest incidence rate at 0.04/1 million.
The calculated societal perspective cost per outcome averted was quite high for each risk group. For Group 1, the cost was $596 million per case averted. This cost rose to $1.3 billion for each case of long-term sequelae averted, and rose even higher to avert death, to $1.8 billion per death averted. These costs nearly doubled for Group 2, and in Group 3, the cost ballooned to $7.9 billion to avert one case of JE, $17 billion per prevention of long-term sequelae, and $23 billion per death averted.
The individual costs for JE vaccination are $292 per dose, with an administration fee of $46. Short-term treatment of JE costs nearly $30,000, and long-term treatment of JE also comes with a large bill of $8,437.
These costs are not simply monetary but are also felt in lost economic productivity. The cost of complete short-term recovery is nearly $60,000. Over an individual’s lifetime, this number rose to more than $1.5 million based on total loss of productivity.
Of the 67% of patients who survive JE, 32% recover completely while 68% deal with long-term sequelae. Of those, 28% experience mild symptoms while the remaining 72% have severe sequelae.
JE vaccine effectiveness does not appear to be an issue, with a 0.91 proportion of neutralizing antibodies seen after 1 year. With booster doses, vaccine effectiveness is 0.96.
There are limitations to this study, such as results being affected by the uncertainty of JE incidence. “The single most important variable is incidence,” stated Dr. Meltzer.
REPORTING FROM AN ACIP MEETING
Disparities found in access to medication treatment for OUDs
The number of Medicaid enrollees receiving medication treatment with methadone and buprenorphine rose from 2002 to 2009 because of the availability of buprenorphine. A cause for concern, however, is that medication treatment increased at a much higher rate in counties with lower poverty rates – and lower concentrations of black and Hispanic residents.
“Concerted efforts are needed to ensure that [medication treatment] benefits are equitably distributed across society and reach disadvantaged individuals who may be at higher risk of experiencing opioid use disorders,” wrote Bradley D. Stein, MD, PhD, and his colleagues. The report was published in Substance Abuse.
Dr. Stein, of Rand Corporation, and his colleagues set out to assess the changes in medication treatment use over time and how medication treatment was being used at the county level – in addition to the associations between poverty, race/ethnicity, and urbanicity. The research team analyzed Medicaid claims from 2002 to 2009 from 14 states, representing 53% of the U.S. population and 47% of 2009 Medicaid enrollees. The states selected in the analysis, chosen to represent regional and population diversity, were California, Connecticut, Florida, Georgia, Illinois, Louisiana, Massachusetts, Maryland, New York, Pennsylvania, Rhode Island, Texas, Vermont, and Wisconsin. The researchers looked at medication treatment use among 18- to 64-year-old Medicaid enrollees, excluding people who were eligible for both Medicare and Medicaid.
The variables for who received medication treatment and data on county characteristics were well defined. Individuals who had received either methadone or buprenorphine were identified as receiving medication treatment. Some patients (3% or less) used both methadone or buprenorphine but were categorized as methadone users in the analysis to better elucidate the role of buprenorphine in medication treatment. Counties were classified as low poverty if the percentage of the county population was below the median (less than 13.5%) of the counties in the 14 states in the analysis and the federal poverty line.
The racial/ethnic makeup of a county was determined to be low percentage of black people if the percentage of the black population was below the median (less than 5.6%) in all counties. Similarly, a county was considered low percentage of Hispanic residents if the proportion of the Hispanic population was below the median of less than 4.2%, reported Dr. Stein, who also is affiliated with the University of Pittsburgh.
The analysis showed that from 2002 to 2009, the proportion of Medicaid users receiving methadone increased by 20% (42,235 to 50,587), accounting for a fraction of the 62% increase in Medicaid enrollment (42,263 to 68,278). The real driver in increased medication treatment rates was the adoption of buprenorphine, which soared from 75 in 2002 to 19,691 in 2009. In 2009, 29% of Medicaid enrollees received medication treatment with buprenorphine. The growth of medication treatment varied by the characteristics of a county’s population. In 2002, urban counties had substantially higher rates of primarily methadone therapy than did rural counties (P less than.001). But no significant differences were found across the county based the concentration of black residents or poverty. Communities that did not have low concentrations of Hispanic residents experienced higher rates of medication treatment, regardless of poverty (P less than .01 for low poverty and not low poverty)
Those trends changed by 2009. Compared with individuals living in all other types of counties, those living in counties with a lower proportion of black residents and a low poverty rate were much more likely to receive medication treatment. A similar pattern was seen among populations with a lower proportion of Hispanic residents and a low poverty rate, compared with communities with high numbers of Hispanics and not low poverty rate.
Dr. Stein and his colleagues cited several limitations. First, because the study analyzed Medicaid enrollees, it is not known how the findings might translate to uninsured or commercially insured patients. Another limitation is that the study data analyzed patients until 2009, making it difficult to generalize the findings to the population today. Finally, the researchers used a population-based approach.
Nevertheless, they said, the study advances understanding of the impact of buprenorphine on medication treatment among patients who receive Medicaid.
“At a time of intensive policymaker and regulatory efforts to increase [medication treatment] availability, of suffering from these disorders,” Dr. Stein and his colleagues wrote.
The study was supported by a grant from the National Institute on Drug Abuse. The authors disclosed no relevant conflicts of interest.
SOURCE: Stein BD et al. Subst Abuse. 2018 Jun 22. doi: 10.1080/08897077.2018.1449166.
The number of Medicaid enrollees receiving medication treatment with methadone and buprenorphine rose from 2002 to 2009 because of the availability of buprenorphine. A cause for concern, however, is that medication treatment increased at a much higher rate in counties with lower poverty rates – and lower concentrations of black and Hispanic residents.
“Concerted efforts are needed to ensure that [medication treatment] benefits are equitably distributed across society and reach disadvantaged individuals who may be at higher risk of experiencing opioid use disorders,” wrote Bradley D. Stein, MD, PhD, and his colleagues. The report was published in Substance Abuse.
Dr. Stein, of Rand Corporation, and his colleagues set out to assess the changes in medication treatment use over time and how medication treatment was being used at the county level – in addition to the associations between poverty, race/ethnicity, and urbanicity. The research team analyzed Medicaid claims from 2002 to 2009 from 14 states, representing 53% of the U.S. population and 47% of 2009 Medicaid enrollees. The states selected in the analysis, chosen to represent regional and population diversity, were California, Connecticut, Florida, Georgia, Illinois, Louisiana, Massachusetts, Maryland, New York, Pennsylvania, Rhode Island, Texas, Vermont, and Wisconsin. The researchers looked at medication treatment use among 18- to 64-year-old Medicaid enrollees, excluding people who were eligible for both Medicare and Medicaid.
The variables for who received medication treatment and data on county characteristics were well defined. Individuals who had received either methadone or buprenorphine were identified as receiving medication treatment. Some patients (3% or less) used both methadone or buprenorphine but were categorized as methadone users in the analysis to better elucidate the role of buprenorphine in medication treatment. Counties were classified as low poverty if the percentage of the county population was below the median (less than 13.5%) of the counties in the 14 states in the analysis and the federal poverty line.
The racial/ethnic makeup of a county was determined to be low percentage of black people if the percentage of the black population was below the median (less than 5.6%) in all counties. Similarly, a county was considered low percentage of Hispanic residents if the proportion of the Hispanic population was below the median of less than 4.2%, reported Dr. Stein, who also is affiliated with the University of Pittsburgh.
The analysis showed that from 2002 to 2009, the proportion of Medicaid users receiving methadone increased by 20% (42,235 to 50,587), accounting for a fraction of the 62% increase in Medicaid enrollment (42,263 to 68,278). The real driver in increased medication treatment rates was the adoption of buprenorphine, which soared from 75 in 2002 to 19,691 in 2009. In 2009, 29% of Medicaid enrollees received medication treatment with buprenorphine. The growth of medication treatment varied by the characteristics of a county’s population. In 2002, urban counties had substantially higher rates of primarily methadone therapy than did rural counties (P less than.001). But no significant differences were found across the county based the concentration of black residents or poverty. Communities that did not have low concentrations of Hispanic residents experienced higher rates of medication treatment, regardless of poverty (P less than .01 for low poverty and not low poverty)
Those trends changed by 2009. Compared with individuals living in all other types of counties, those living in counties with a lower proportion of black residents and a low poverty rate were much more likely to receive medication treatment. A similar pattern was seen among populations with a lower proportion of Hispanic residents and a low poverty rate, compared with communities with high numbers of Hispanics and not low poverty rate.
Dr. Stein and his colleagues cited several limitations. First, because the study analyzed Medicaid enrollees, it is not known how the findings might translate to uninsured or commercially insured patients. Another limitation is that the study data analyzed patients until 2009, making it difficult to generalize the findings to the population today. Finally, the researchers used a population-based approach.
Nevertheless, they said, the study advances understanding of the impact of buprenorphine on medication treatment among patients who receive Medicaid.
“At a time of intensive policymaker and regulatory efforts to increase [medication treatment] availability, of suffering from these disorders,” Dr. Stein and his colleagues wrote.
The study was supported by a grant from the National Institute on Drug Abuse. The authors disclosed no relevant conflicts of interest.
SOURCE: Stein BD et al. Subst Abuse. 2018 Jun 22. doi: 10.1080/08897077.2018.1449166.
The number of Medicaid enrollees receiving medication treatment with methadone and buprenorphine rose from 2002 to 2009 because of the availability of buprenorphine. A cause for concern, however, is that medication treatment increased at a much higher rate in counties with lower poverty rates – and lower concentrations of black and Hispanic residents.
“Concerted efforts are needed to ensure that [medication treatment] benefits are equitably distributed across society and reach disadvantaged individuals who may be at higher risk of experiencing opioid use disorders,” wrote Bradley D. Stein, MD, PhD, and his colleagues. The report was published in Substance Abuse.
Dr. Stein, of Rand Corporation, and his colleagues set out to assess the changes in medication treatment use over time and how medication treatment was being used at the county level – in addition to the associations between poverty, race/ethnicity, and urbanicity. The research team analyzed Medicaid claims from 2002 to 2009 from 14 states, representing 53% of the U.S. population and 47% of 2009 Medicaid enrollees. The states selected in the analysis, chosen to represent regional and population diversity, were California, Connecticut, Florida, Georgia, Illinois, Louisiana, Massachusetts, Maryland, New York, Pennsylvania, Rhode Island, Texas, Vermont, and Wisconsin. The researchers looked at medication treatment use among 18- to 64-year-old Medicaid enrollees, excluding people who were eligible for both Medicare and Medicaid.
The variables for who received medication treatment and data on county characteristics were well defined. Individuals who had received either methadone or buprenorphine were identified as receiving medication treatment. Some patients (3% or less) used both methadone or buprenorphine but were categorized as methadone users in the analysis to better elucidate the role of buprenorphine in medication treatment. Counties were classified as low poverty if the percentage of the county population was below the median (less than 13.5%) of the counties in the 14 states in the analysis and the federal poverty line.
The racial/ethnic makeup of a county was determined to be low percentage of black people if the percentage of the black population was below the median (less than 5.6%) in all counties. Similarly, a county was considered low percentage of Hispanic residents if the proportion of the Hispanic population was below the median of less than 4.2%, reported Dr. Stein, who also is affiliated with the University of Pittsburgh.
The analysis showed that from 2002 to 2009, the proportion of Medicaid users receiving methadone increased by 20% (42,235 to 50,587), accounting for a fraction of the 62% increase in Medicaid enrollment (42,263 to 68,278). The real driver in increased medication treatment rates was the adoption of buprenorphine, which soared from 75 in 2002 to 19,691 in 2009. In 2009, 29% of Medicaid enrollees received medication treatment with buprenorphine. The growth of medication treatment varied by the characteristics of a county’s population. In 2002, urban counties had substantially higher rates of primarily methadone therapy than did rural counties (P less than.001). But no significant differences were found across the county based the concentration of black residents or poverty. Communities that did not have low concentrations of Hispanic residents experienced higher rates of medication treatment, regardless of poverty (P less than .01 for low poverty and not low poverty)
Those trends changed by 2009. Compared with individuals living in all other types of counties, those living in counties with a lower proportion of black residents and a low poverty rate were much more likely to receive medication treatment. A similar pattern was seen among populations with a lower proportion of Hispanic residents and a low poverty rate, compared with communities with high numbers of Hispanics and not low poverty rate.
Dr. Stein and his colleagues cited several limitations. First, because the study analyzed Medicaid enrollees, it is not known how the findings might translate to uninsured or commercially insured patients. Another limitation is that the study data analyzed patients until 2009, making it difficult to generalize the findings to the population today. Finally, the researchers used a population-based approach.
Nevertheless, they said, the study advances understanding of the impact of buprenorphine on medication treatment among patients who receive Medicaid.
“At a time of intensive policymaker and regulatory efforts to increase [medication treatment] availability, of suffering from these disorders,” Dr. Stein and his colleagues wrote.
The study was supported by a grant from the National Institute on Drug Abuse. The authors disclosed no relevant conflicts of interest.
SOURCE: Stein BD et al. Subst Abuse. 2018 Jun 22. doi: 10.1080/08897077.2018.1449166.
FROM SUBSTANCE ABUSE
Key clinical point: Medication treatment access for opioid use disorders varies greatly among Medicaid enrollees.
Major finding: Residents of counties with a lower proportion of black residents and a low poverty rate are much more likely to receive medication treatment.
Study details: An analysis of Medicaid claims from 2002 to 2009 from 14 states representing 53% of the U.S. population and 47% of 2009 Medicaid enrollees.
Disclosures: This study was supported by a grant from the National Institute on Drug Abuse. The authors disclosed no relevant conflicts of interest.
Source: Stein BD et al. Subst Abuse. 2018 Jun 22. doi: 10.1080/08897077.2018.1449166.
FDA approves topical anticholinergic for primary axillary hyperhidrosis
The in adults and children aged 9 years and older.
Glycopyrronium, which is formulated in a cloth wipe, will be marketed as Qbrexza and is expected to be available in October, according to the approval announcement June 29, which was made by Dermira, the manufacturer. The instructions for use section in the prescribing information states that patients are advised to use one cloth to apply the medication to both axillae, wiping the cloth across each underarm. Each cloth, intended for single use, is pre-moistened with 2.4% glycopyrronium solution.
Glycopyrronium blocks sweat production “by inhibiting the interaction between acetylcholine and the cholinergic receptors responsible for sweat gland activation,” the company said in a February press release.
The approval was based on the results of two phase 3 clinical studies, ATMOS-1 and ATMOS-2, which were multicenter, randomized, double-blind, vehicle-controlled, 4-week studies in patients 9 years of age or older with primary axillary hyperhidrosis for 6 months or longer. Study subjects had production of at least 50 mg of underarm sweat over 5 minutes, and scores of four or higher on the 11-point Axillary Sweating Daily Diary (ASDD) or the Children’s ASDD (ASDD-C) – an instrument developed by the company in consultation with the FDA – and scores of three or four on the four-grade Hyperhidrosis Disease Severity Scale (HDSS). In total, 463 patients were randomized to receive glycopyrronium and 234 to vehicle. Forty four of these patients were aged 9-16 years, with 25 receiving glycopyrronium and 19 receiving vehicle.
According to the February release, the ASDD/ASDD-C severity scale responder rates were about 60% in the pediatric and adult groups treated with glycopyrronium, compared with 13.0% and 28.8% for children and adults, respectively, in the vehicle group. At week 4, the median absolute change in sweat production was a reduction of 64.2 mg in children and a reduction of 80.6 mg among adults treated with glycopyrronium, compared with reductions of 53.7 mg and 62 mg among those in the vehicle group, respectively.
In the glycopyrronium-treated group, almost 80% of the pediatric patients and 74.3% of the adults experienced at least a 50% reduction in sweat production at week 4, compared with almost 55% and 53%, respectively, in the vehicle group.
Among pediatric patients, the mean decrease from baseline in the Children’s Dermatology Quality of Life Index was 8.1 in glycopyrronium-treated patients, compared with 1.9 in the vehicle group. In adults, scores on the Dermatology Life Quality Index measure were reduced by 8.4 and 4.7 in glycopyrronium- and vehicle-treated adult patients, respectively.
Nearly 57% of adults and 44% of pediatric patients treated with glycopyrronium experienced treatment-emergent adverse events, compared with 34.3% of adults and 10.5% of the pediatric patients in the vehicle group. The majority were related to anticholinergic activity and were mild, and rarely led to drug discontinuation, according to the company.
The press release announcing the approval stated that the most common adverse effects observed after application of glycopyrronium were dry mouth, mydriasis, sore throat, headache, urinary hesitation, blurred vision, dry nose, dry throat, dry eye, dry skin and constipation. Erythema, burning/stinging, and pruritus were the most common skin reactions.
The product is contraindicated in patients with glaucoma, paralytic ileus, and other medical conditions that can be exacerbated by its anticholinergic effects, according to the prescribing information. Patients should be advised that they should wash their hands thoroughly after application, and that it can cause temporary dilation of the pupils and blurred vision if glycopyrronium comes into contact with their eyes.
The in adults and children aged 9 years and older.
Glycopyrronium, which is formulated in a cloth wipe, will be marketed as Qbrexza and is expected to be available in October, according to the approval announcement June 29, which was made by Dermira, the manufacturer. The instructions for use section in the prescribing information states that patients are advised to use one cloth to apply the medication to both axillae, wiping the cloth across each underarm. Each cloth, intended for single use, is pre-moistened with 2.4% glycopyrronium solution.
Glycopyrronium blocks sweat production “by inhibiting the interaction between acetylcholine and the cholinergic receptors responsible for sweat gland activation,” the company said in a February press release.
The approval was based on the results of two phase 3 clinical studies, ATMOS-1 and ATMOS-2, which were multicenter, randomized, double-blind, vehicle-controlled, 4-week studies in patients 9 years of age or older with primary axillary hyperhidrosis for 6 months or longer. Study subjects had production of at least 50 mg of underarm sweat over 5 minutes, and scores of four or higher on the 11-point Axillary Sweating Daily Diary (ASDD) or the Children’s ASDD (ASDD-C) – an instrument developed by the company in consultation with the FDA – and scores of three or four on the four-grade Hyperhidrosis Disease Severity Scale (HDSS). In total, 463 patients were randomized to receive glycopyrronium and 234 to vehicle. Forty four of these patients were aged 9-16 years, with 25 receiving glycopyrronium and 19 receiving vehicle.
According to the February release, the ASDD/ASDD-C severity scale responder rates were about 60% in the pediatric and adult groups treated with glycopyrronium, compared with 13.0% and 28.8% for children and adults, respectively, in the vehicle group. At week 4, the median absolute change in sweat production was a reduction of 64.2 mg in children and a reduction of 80.6 mg among adults treated with glycopyrronium, compared with reductions of 53.7 mg and 62 mg among those in the vehicle group, respectively.
In the glycopyrronium-treated group, almost 80% of the pediatric patients and 74.3% of the adults experienced at least a 50% reduction in sweat production at week 4, compared with almost 55% and 53%, respectively, in the vehicle group.
Among pediatric patients, the mean decrease from baseline in the Children’s Dermatology Quality of Life Index was 8.1 in glycopyrronium-treated patients, compared with 1.9 in the vehicle group. In adults, scores on the Dermatology Life Quality Index measure were reduced by 8.4 and 4.7 in glycopyrronium- and vehicle-treated adult patients, respectively.
Nearly 57% of adults and 44% of pediatric patients treated with glycopyrronium experienced treatment-emergent adverse events, compared with 34.3% of adults and 10.5% of the pediatric patients in the vehicle group. The majority were related to anticholinergic activity and were mild, and rarely led to drug discontinuation, according to the company.
The press release announcing the approval stated that the most common adverse effects observed after application of glycopyrronium were dry mouth, mydriasis, sore throat, headache, urinary hesitation, blurred vision, dry nose, dry throat, dry eye, dry skin and constipation. Erythema, burning/stinging, and pruritus were the most common skin reactions.
The product is contraindicated in patients with glaucoma, paralytic ileus, and other medical conditions that can be exacerbated by its anticholinergic effects, according to the prescribing information. Patients should be advised that they should wash their hands thoroughly after application, and that it can cause temporary dilation of the pupils and blurred vision if glycopyrronium comes into contact with their eyes.
The in adults and children aged 9 years and older.
Glycopyrronium, which is formulated in a cloth wipe, will be marketed as Qbrexza and is expected to be available in October, according to the approval announcement June 29, which was made by Dermira, the manufacturer. The instructions for use section in the prescribing information states that patients are advised to use one cloth to apply the medication to both axillae, wiping the cloth across each underarm. Each cloth, intended for single use, is pre-moistened with 2.4% glycopyrronium solution.
Glycopyrronium blocks sweat production “by inhibiting the interaction between acetylcholine and the cholinergic receptors responsible for sweat gland activation,” the company said in a February press release.
The approval was based on the results of two phase 3 clinical studies, ATMOS-1 and ATMOS-2, which were multicenter, randomized, double-blind, vehicle-controlled, 4-week studies in patients 9 years of age or older with primary axillary hyperhidrosis for 6 months or longer. Study subjects had production of at least 50 mg of underarm sweat over 5 minutes, and scores of four or higher on the 11-point Axillary Sweating Daily Diary (ASDD) or the Children’s ASDD (ASDD-C) – an instrument developed by the company in consultation with the FDA – and scores of three or four on the four-grade Hyperhidrosis Disease Severity Scale (HDSS). In total, 463 patients were randomized to receive glycopyrronium and 234 to vehicle. Forty four of these patients were aged 9-16 years, with 25 receiving glycopyrronium and 19 receiving vehicle.
According to the February release, the ASDD/ASDD-C severity scale responder rates were about 60% in the pediatric and adult groups treated with glycopyrronium, compared with 13.0% and 28.8% for children and adults, respectively, in the vehicle group. At week 4, the median absolute change in sweat production was a reduction of 64.2 mg in children and a reduction of 80.6 mg among adults treated with glycopyrronium, compared with reductions of 53.7 mg and 62 mg among those in the vehicle group, respectively.
In the glycopyrronium-treated group, almost 80% of the pediatric patients and 74.3% of the adults experienced at least a 50% reduction in sweat production at week 4, compared with almost 55% and 53%, respectively, in the vehicle group.
Among pediatric patients, the mean decrease from baseline in the Children’s Dermatology Quality of Life Index was 8.1 in glycopyrronium-treated patients, compared with 1.9 in the vehicle group. In adults, scores on the Dermatology Life Quality Index measure were reduced by 8.4 and 4.7 in glycopyrronium- and vehicle-treated adult patients, respectively.
Nearly 57% of adults and 44% of pediatric patients treated with glycopyrronium experienced treatment-emergent adverse events, compared with 34.3% of adults and 10.5% of the pediatric patients in the vehicle group. The majority were related to anticholinergic activity and were mild, and rarely led to drug discontinuation, according to the company.
The press release announcing the approval stated that the most common adverse effects observed after application of glycopyrronium were dry mouth, mydriasis, sore throat, headache, urinary hesitation, blurred vision, dry nose, dry throat, dry eye, dry skin and constipation. Erythema, burning/stinging, and pruritus were the most common skin reactions.
The product is contraindicated in patients with glaucoma, paralytic ileus, and other medical conditions that can be exacerbated by its anticholinergic effects, according to the prescribing information. Patients should be advised that they should wash their hands thoroughly after application, and that it can cause temporary dilation of the pupils and blurred vision if glycopyrronium comes into contact with their eyes.
Screen sooner and more often for those with family history of CRC
WASHINGTON – The number of first- and second-degree relatives with colorectal cancer can increase an individual’s risk for CRC, which could require screening to be done more frequently.
“There have been multiple guidelines reported as to what should be done for these individuals,” Harminder Singh, MD, of the University of Manitoba and his associates stated. “However, for the most part, they have not systematically analyzed the data.” He went on to say that, “more importantly, there’s been no recent AGA [American Gastroenterological Association] or Canadian Association of Gastroenterology statement, which led the development of this guideline.”
To address this issue, Dr. Singh and his colleagues conducted a systematic review of 10 literature searches to answer the following five questions concerning colorectal risk and screening practices: What is the effect of a family history of CRC on an individual’s risk of CRC? What is the effect of a family history of adenoma on an individual’s risk of CRC? At what age should CRC screening begin? Which screening tests are optimal? What are the optimal testing intervals for people with a family history of CRC or adenoma?
These questions were developed via an iterative online platform and then further developed and voted on by a team of specialists. GRADE (Grading of Recommendation Assessment, Development and Evaluation) was used to assess the quality of evidence to support these questions.
Similarly, individuals with two or more first-degree relatives with CRC had a two- to fourfold increased risk of developing CRC, compared with the general population. The review also found that, of the 20 recommendation statements from the review panel, there was consensus about 19 of them.
Colorectal cancer screening is recommended for all individuals with a family history of CRC or documented adenoma. Similarly, colonoscopy is recommended as the preferred test for individuals at the highest risk– those with one or more affected first-degree relatives. Fecal immunochemistry tests are considered a viable alternative except in patients with two or more first-degree relatives.
If a patient is considered to have an elevated risk of CRC because of family history, then screening should begin when they are aged 10 years younger than when that first-degree relative was diagnosed, and a 5-year screening interval should be followed after that.
Dr. Singh pointed out that the age of the affected first-degree relative should be considered when weighing an individual’s related risk of developing CRC. For example, having an first-degree relative who is diagnosed after the age of 75 is not likely to elevate an individual’s risk of developing CRC. Individuals with one or more second-degree relatives with CRC or nonadvanced adenoma do not appear to have an elevated risk of developing CRC and should be screened according to average-risk guidelines.
Dr. Singh reported receiving funding for from Merck Canada.
SOURCE: Leddin D. Gastroenterology. 2018 Jun. doi: 10.1016/S0016-5085(18)31083-7.
WASHINGTON – The number of first- and second-degree relatives with colorectal cancer can increase an individual’s risk for CRC, which could require screening to be done more frequently.
“There have been multiple guidelines reported as to what should be done for these individuals,” Harminder Singh, MD, of the University of Manitoba and his associates stated. “However, for the most part, they have not systematically analyzed the data.” He went on to say that, “more importantly, there’s been no recent AGA [American Gastroenterological Association] or Canadian Association of Gastroenterology statement, which led the development of this guideline.”
To address this issue, Dr. Singh and his colleagues conducted a systematic review of 10 literature searches to answer the following five questions concerning colorectal risk and screening practices: What is the effect of a family history of CRC on an individual’s risk of CRC? What is the effect of a family history of adenoma on an individual’s risk of CRC? At what age should CRC screening begin? Which screening tests are optimal? What are the optimal testing intervals for people with a family history of CRC or adenoma?
These questions were developed via an iterative online platform and then further developed and voted on by a team of specialists. GRADE (Grading of Recommendation Assessment, Development and Evaluation) was used to assess the quality of evidence to support these questions.
Similarly, individuals with two or more first-degree relatives with CRC had a two- to fourfold increased risk of developing CRC, compared with the general population. The review also found that, of the 20 recommendation statements from the review panel, there was consensus about 19 of them.
Colorectal cancer screening is recommended for all individuals with a family history of CRC or documented adenoma. Similarly, colonoscopy is recommended as the preferred test for individuals at the highest risk– those with one or more affected first-degree relatives. Fecal immunochemistry tests are considered a viable alternative except in patients with two or more first-degree relatives.
If a patient is considered to have an elevated risk of CRC because of family history, then screening should begin when they are aged 10 years younger than when that first-degree relative was diagnosed, and a 5-year screening interval should be followed after that.
Dr. Singh pointed out that the age of the affected first-degree relative should be considered when weighing an individual’s related risk of developing CRC. For example, having an first-degree relative who is diagnosed after the age of 75 is not likely to elevate an individual’s risk of developing CRC. Individuals with one or more second-degree relatives with CRC or nonadvanced adenoma do not appear to have an elevated risk of developing CRC and should be screened according to average-risk guidelines.
Dr. Singh reported receiving funding for from Merck Canada.
SOURCE: Leddin D. Gastroenterology. 2018 Jun. doi: 10.1016/S0016-5085(18)31083-7.
WASHINGTON – The number of first- and second-degree relatives with colorectal cancer can increase an individual’s risk for CRC, which could require screening to be done more frequently.
“There have been multiple guidelines reported as to what should be done for these individuals,” Harminder Singh, MD, of the University of Manitoba and his associates stated. “However, for the most part, they have not systematically analyzed the data.” He went on to say that, “more importantly, there’s been no recent AGA [American Gastroenterological Association] or Canadian Association of Gastroenterology statement, which led the development of this guideline.”
To address this issue, Dr. Singh and his colleagues conducted a systematic review of 10 literature searches to answer the following five questions concerning colorectal risk and screening practices: What is the effect of a family history of CRC on an individual’s risk of CRC? What is the effect of a family history of adenoma on an individual’s risk of CRC? At what age should CRC screening begin? Which screening tests are optimal? What are the optimal testing intervals for people with a family history of CRC or adenoma?
These questions were developed via an iterative online platform and then further developed and voted on by a team of specialists. GRADE (Grading of Recommendation Assessment, Development and Evaluation) was used to assess the quality of evidence to support these questions.
Similarly, individuals with two or more first-degree relatives with CRC had a two- to fourfold increased risk of developing CRC, compared with the general population. The review also found that, of the 20 recommendation statements from the review panel, there was consensus about 19 of them.
Colorectal cancer screening is recommended for all individuals with a family history of CRC or documented adenoma. Similarly, colonoscopy is recommended as the preferred test for individuals at the highest risk– those with one or more affected first-degree relatives. Fecal immunochemistry tests are considered a viable alternative except in patients with two or more first-degree relatives.
If a patient is considered to have an elevated risk of CRC because of family history, then screening should begin when they are aged 10 years younger than when that first-degree relative was diagnosed, and a 5-year screening interval should be followed after that.
Dr. Singh pointed out that the age of the affected first-degree relative should be considered when weighing an individual’s related risk of developing CRC. For example, having an first-degree relative who is diagnosed after the age of 75 is not likely to elevate an individual’s risk of developing CRC. Individuals with one or more second-degree relatives with CRC or nonadvanced adenoma do not appear to have an elevated risk of developing CRC and should be screened according to average-risk guidelines.
Dr. Singh reported receiving funding for from Merck Canada.
SOURCE: Leddin D. Gastroenterology. 2018 Jun. doi: 10.1016/S0016-5085(18)31083-7.
REPORTING FROM DDW 2018
Key clinical point: Patients with 1 or more first-degree relative with CRC should be screened more often.
Major finding: Patients with one or more first-degree relatives with CRC or adenoma had a twofold greater risk of developing CRC, compared with those without a family history of these diseases.
Study details: A systematic review of 10 literature searches assessing risk of CRC in those with a family history of CRC.
Disclosures: Dr. Singh has received funding from Merck Canada.
Source: Leddin D. Gastroenterology. 2018 Jun. doi: 10.1016/S0016-5085(18)31083-7.
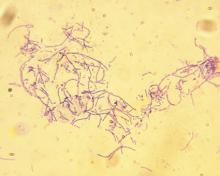
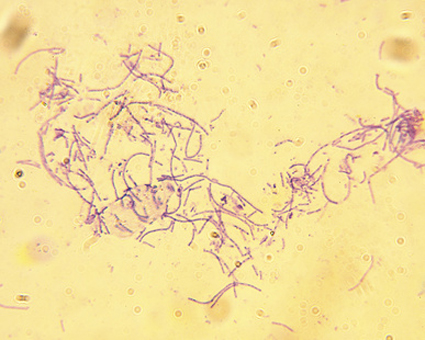
Anthrax vaccine recommendations updated in the event of a wide-area release
at their meeting.
The recommendations to the committee sought to optimize the use of Anthrax Vaccine Adsorbed (AVA) in post-exposure prophylaxis (PEP) in the event of a wide-area release of Bacillus anthracis spores. In this event, a mass vaccination effort would be undertaken, requiring expedited administration of AVA. ACIP now recommends that the intramuscular administration may be used over the traditional subcutaneous approach if there are any operational or logistical challenges that delay effective vaccination. Another recommendation from ACIP would allow two full doses or three half doses of AVA to be used to expand vaccine coverage for PEP in the event there is an inadequate vaccine supply. The committee also recommended that AbxPEP, an antimicrobial, be stopped 42 days after the first dose of AVA or 2 weeks after the last dose.
William A. Bower, MD, of the division of high-consequence pathogens and pathology at the Centers for Disease Control and Prevention, and the anthrax work group looked at three nonhuman primate studies and eight human immunogenicity and adverse event studies during the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE). All of the animal studies were used to predict human survival by vaccinating the nonhuman primates with AVA, then challenging them with B. anthracis. Using animal studies to predict human survival is common practice under the “animal rule.”
When Dr. Bower and the work group assessed the studies comparing intramuscular administration with subcutaneous administration of AVA, they rated the overall evidence as GRADE 2. However, they rated the adverse events data as GRADE 1.
Dr. Bower and his colleagues also reviewed dose-sparing studies to identify the feasibility of allowing two full doses or three half doses of AVA to be used to expand vaccine coverage for PEP in the event there is an inadequate vaccine supply. For these studies, the anthrax work group gave a GRADE score of 2.
The overall evidence score for microbial duration for PEP was judged to be GRADE 2.
“These forthcoming recommendations will be used by the CDC to inform state and local health departments to better prepare for an emergency response to a wide-area release of Bacillus anthracis spores,” said Dr. Bower.
The committee’s recommendations must be approved by the CDC’s director before they are considered official recommendations.
Dr. Bower did not report any relevant financial conflicts of interest.
at their meeting.
The recommendations to the committee sought to optimize the use of Anthrax Vaccine Adsorbed (AVA) in post-exposure prophylaxis (PEP) in the event of a wide-area release of Bacillus anthracis spores. In this event, a mass vaccination effort would be undertaken, requiring expedited administration of AVA. ACIP now recommends that the intramuscular administration may be used over the traditional subcutaneous approach if there are any operational or logistical challenges that delay effective vaccination. Another recommendation from ACIP would allow two full doses or three half doses of AVA to be used to expand vaccine coverage for PEP in the event there is an inadequate vaccine supply. The committee also recommended that AbxPEP, an antimicrobial, be stopped 42 days after the first dose of AVA or 2 weeks after the last dose.
William A. Bower, MD, of the division of high-consequence pathogens and pathology at the Centers for Disease Control and Prevention, and the anthrax work group looked at three nonhuman primate studies and eight human immunogenicity and adverse event studies during the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE). All of the animal studies were used to predict human survival by vaccinating the nonhuman primates with AVA, then challenging them with B. anthracis. Using animal studies to predict human survival is common practice under the “animal rule.”
When Dr. Bower and the work group assessed the studies comparing intramuscular administration with subcutaneous administration of AVA, they rated the overall evidence as GRADE 2. However, they rated the adverse events data as GRADE 1.
Dr. Bower and his colleagues also reviewed dose-sparing studies to identify the feasibility of allowing two full doses or three half doses of AVA to be used to expand vaccine coverage for PEP in the event there is an inadequate vaccine supply. For these studies, the anthrax work group gave a GRADE score of 2.
The overall evidence score for microbial duration for PEP was judged to be GRADE 2.
“These forthcoming recommendations will be used by the CDC to inform state and local health departments to better prepare for an emergency response to a wide-area release of Bacillus anthracis spores,” said Dr. Bower.
The committee’s recommendations must be approved by the CDC’s director before they are considered official recommendations.
Dr. Bower did not report any relevant financial conflicts of interest.
at their meeting.
The recommendations to the committee sought to optimize the use of Anthrax Vaccine Adsorbed (AVA) in post-exposure prophylaxis (PEP) in the event of a wide-area release of Bacillus anthracis spores. In this event, a mass vaccination effort would be undertaken, requiring expedited administration of AVA. ACIP now recommends that the intramuscular administration may be used over the traditional subcutaneous approach if there are any operational or logistical challenges that delay effective vaccination. Another recommendation from ACIP would allow two full doses or three half doses of AVA to be used to expand vaccine coverage for PEP in the event there is an inadequate vaccine supply. The committee also recommended that AbxPEP, an antimicrobial, be stopped 42 days after the first dose of AVA or 2 weeks after the last dose.
William A. Bower, MD, of the division of high-consequence pathogens and pathology at the Centers for Disease Control and Prevention, and the anthrax work group looked at three nonhuman primate studies and eight human immunogenicity and adverse event studies during the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE). All of the animal studies were used to predict human survival by vaccinating the nonhuman primates with AVA, then challenging them with B. anthracis. Using animal studies to predict human survival is common practice under the “animal rule.”
When Dr. Bower and the work group assessed the studies comparing intramuscular administration with subcutaneous administration of AVA, they rated the overall evidence as GRADE 2. However, they rated the adverse events data as GRADE 1.
Dr. Bower and his colleagues also reviewed dose-sparing studies to identify the feasibility of allowing two full doses or three half doses of AVA to be used to expand vaccine coverage for PEP in the event there is an inadequate vaccine supply. For these studies, the anthrax work group gave a GRADE score of 2.
The overall evidence score for microbial duration for PEP was judged to be GRADE 2.
“These forthcoming recommendations will be used by the CDC to inform state and local health departments to better prepare for an emergency response to a wide-area release of Bacillus anthracis spores,” said Dr. Bower.
The committee’s recommendations must be approved by the CDC’s director before they are considered official recommendations.
Dr. Bower did not report any relevant financial conflicts of interest.
REPORTING FROM AN ACIP MEETING
Bullae associated with pediatric human parvovirus B19 infection
reported Shoko Yoshii, MD, and his associates at the National Center for Child Health and Development in Tokyo.
In a case study, a 2-year-old boy was admitted to an ED with swelling of both lower limbs. In the 2 weeks previous, he had had a fever that lasted 3 days followed by erythema on the cheeks and limbs. A physical examination reveled edematous erythema on his lower limbs with a predominance of them on the left leg. Doctors analyzed his laboratory results and found that the boy’s white blood cell count was in the normal range, with C-reactive protein level of 3.2 mg/L. The boy was treated with cefazolin for suspected bacterial cellulitis, but this did little; erythema and edema progressed on the left leg and multiple bullae developed 2 days after admission. Within a week, the bullae spontaneously ruptured and resolved.
Parvovirus B19 infection was suspected, and parvovirus B19 IgM was positive on the first day of admission. The boy ultimately recovered and has had no further episodes within 1 year of follow-up.Bullae or vesicles are considered rare manifestations of parvovirus B19 infection, which more typically presents with a “slapped-cheek” appearance and lacy exanthema, sometimes called erythema infectiosum. In adults with parvovirus infection, bullae or vesicles develop at the same time as papular purpuric gloves-and-socks syndrome.
This case did not follow this pattern, with lesions appearing on the lower legs with no involvement of the hands or feet. The few cases of parvovirus infection that have been reported with bulbous skin lesions in children generally were not associated with papular purpuric gloves-and-socks syndrome, which is widely considered a textbook manifestation of parvovirus infection, the authors wrote.
This case study was supported by a grant from National Center for Child Health and Development. No disclosures were reported.
SOURCE: Yoshii S et al. J Pediatr. 2018. doi: 10.1016/j.jpeds.2018.05.038.
reported Shoko Yoshii, MD, and his associates at the National Center for Child Health and Development in Tokyo.
In a case study, a 2-year-old boy was admitted to an ED with swelling of both lower limbs. In the 2 weeks previous, he had had a fever that lasted 3 days followed by erythema on the cheeks and limbs. A physical examination reveled edematous erythema on his lower limbs with a predominance of them on the left leg. Doctors analyzed his laboratory results and found that the boy’s white blood cell count was in the normal range, with C-reactive protein level of 3.2 mg/L. The boy was treated with cefazolin for suspected bacterial cellulitis, but this did little; erythema and edema progressed on the left leg and multiple bullae developed 2 days after admission. Within a week, the bullae spontaneously ruptured and resolved.
Parvovirus B19 infection was suspected, and parvovirus B19 IgM was positive on the first day of admission. The boy ultimately recovered and has had no further episodes within 1 year of follow-up.Bullae or vesicles are considered rare manifestations of parvovirus B19 infection, which more typically presents with a “slapped-cheek” appearance and lacy exanthema, sometimes called erythema infectiosum. In adults with parvovirus infection, bullae or vesicles develop at the same time as papular purpuric gloves-and-socks syndrome.
This case did not follow this pattern, with lesions appearing on the lower legs with no involvement of the hands or feet. The few cases of parvovirus infection that have been reported with bulbous skin lesions in children generally were not associated with papular purpuric gloves-and-socks syndrome, which is widely considered a textbook manifestation of parvovirus infection, the authors wrote.
This case study was supported by a grant from National Center for Child Health and Development. No disclosures were reported.
SOURCE: Yoshii S et al. J Pediatr. 2018. doi: 10.1016/j.jpeds.2018.05.038.
reported Shoko Yoshii, MD, and his associates at the National Center for Child Health and Development in Tokyo.
In a case study, a 2-year-old boy was admitted to an ED with swelling of both lower limbs. In the 2 weeks previous, he had had a fever that lasted 3 days followed by erythema on the cheeks and limbs. A physical examination reveled edematous erythema on his lower limbs with a predominance of them on the left leg. Doctors analyzed his laboratory results and found that the boy’s white blood cell count was in the normal range, with C-reactive protein level of 3.2 mg/L. The boy was treated with cefazolin for suspected bacterial cellulitis, but this did little; erythema and edema progressed on the left leg and multiple bullae developed 2 days after admission. Within a week, the bullae spontaneously ruptured and resolved.
Parvovirus B19 infection was suspected, and parvovirus B19 IgM was positive on the first day of admission. The boy ultimately recovered and has had no further episodes within 1 year of follow-up.Bullae or vesicles are considered rare manifestations of parvovirus B19 infection, which more typically presents with a “slapped-cheek” appearance and lacy exanthema, sometimes called erythema infectiosum. In adults with parvovirus infection, bullae or vesicles develop at the same time as papular purpuric gloves-and-socks syndrome.
This case did not follow this pattern, with lesions appearing on the lower legs with no involvement of the hands or feet. The few cases of parvovirus infection that have been reported with bulbous skin lesions in children generally were not associated with papular purpuric gloves-and-socks syndrome, which is widely considered a textbook manifestation of parvovirus infection, the authors wrote.
This case study was supported by a grant from National Center for Child Health and Development. No disclosures were reported.
SOURCE: Yoshii S et al. J Pediatr. 2018. doi: 10.1016/j.jpeds.2018.05.038.
FROM THE JOURNAL OF PEDIATRICS
ACIP votes to recommend new strains for the 2018-2019 flu vaccine
Thirteen members of the Advisory Committee on Immunization Practices (ACIP) voted to approve the influenza vaccine recommendations for 2018-2019, while one member abstained from voting at the summer ACIP meeting.
The 2018-2019 recommendation maintains the core recommendation that influenza vaccines should be administered to all persons 6 months or older who have no contraindications.
FluMist Quadrivalent (LAIV4) also is being updated for the 2018-2019 season. At the February meeting of ACIP, the committee approved language that providers may provide any licensed, age-appropriate influenza vaccine, and LAIV4 is considered in this set of vaccine options.
Prior to this approval, there was a discussion of the safety of the 2017-2018 vaccine. For many of the available vaccines, there were no new safety concerns raised from reports during the flu season. Monitoring during the 2018-2019 will yield more safety monitoring data concerning pregnancy and influenza vaccinations and anaphylaxis in persons with an egg allergy.
The committee’s recommendations must be approved by the Centers for Disease Control and Prevention’s director before they are considered official recommendations.
Thirteen members of the Advisory Committee on Immunization Practices (ACIP) voted to approve the influenza vaccine recommendations for 2018-2019, while one member abstained from voting at the summer ACIP meeting.
The 2018-2019 recommendation maintains the core recommendation that influenza vaccines should be administered to all persons 6 months or older who have no contraindications.
FluMist Quadrivalent (LAIV4) also is being updated for the 2018-2019 season. At the February meeting of ACIP, the committee approved language that providers may provide any licensed, age-appropriate influenza vaccine, and LAIV4 is considered in this set of vaccine options.
Prior to this approval, there was a discussion of the safety of the 2017-2018 vaccine. For many of the available vaccines, there were no new safety concerns raised from reports during the flu season. Monitoring during the 2018-2019 will yield more safety monitoring data concerning pregnancy and influenza vaccinations and anaphylaxis in persons with an egg allergy.
The committee’s recommendations must be approved by the Centers for Disease Control and Prevention’s director before they are considered official recommendations.
Thirteen members of the Advisory Committee on Immunization Practices (ACIP) voted to approve the influenza vaccine recommendations for 2018-2019, while one member abstained from voting at the summer ACIP meeting.
The 2018-2019 recommendation maintains the core recommendation that influenza vaccines should be administered to all persons 6 months or older who have no contraindications.
FluMist Quadrivalent (LAIV4) also is being updated for the 2018-2019 season. At the February meeting of ACIP, the committee approved language that providers may provide any licensed, age-appropriate influenza vaccine, and LAIV4 is considered in this set of vaccine options.
Prior to this approval, there was a discussion of the safety of the 2017-2018 vaccine. For many of the available vaccines, there were no new safety concerns raised from reports during the flu season. Monitoring during the 2018-2019 will yield more safety monitoring data concerning pregnancy and influenza vaccinations and anaphylaxis in persons with an egg allergy.
The committee’s recommendations must be approved by the Centers for Disease Control and Prevention’s director before they are considered official recommendations.
REPORTING FROM AN ACIP MEETING
Preterm infant GER is a normal phenomenon
Treatment of gastroesophageal reflux (GER) in preterm infants with traditional treatments, such as body positioning, and newer treatments with pharmacologic agents appear to be ineffective, and pharmacologic agents in particular may cause significant harm, according to a clinical report by the American Academy of Pediatrics Committee on Fetus and Newborn.
“I think that probably the most important point for any physician, including neonatologists, is that the committee concluded on the basis of the evidence that Eric Eichenwald, MD, lead author of the committee’s clinical report and chief of neonatology at Children’s Hospital of Philadelphia, said in an interview. “So really the bottom line of the clinical report is watchful waiting, conservative management, and patience is the most important approach to a baby that you think is suffering from reflux.”
Pharmacologic management
The committee members focused on four categories of pharmacologic interventions in their report in Pediatrics.
Prokinetic (promotility) agents, such as metoclopramide, domperidone, and erythromycin, are widely used in treating symptoms of GER in older infants and appear to improve gastric emptying, reduce regurgitation, and enhance lower esophageal sphincter tone, but they do not appear to reduce GER symptoms in preterm infants. In addition to not being effective in these infants, there is also a potential for significant adverse events, including cardiac arrhythmia and neurologic side effects. Another common pharmacologic treatment is the use of sodium alginate in combination with sodium bicarbonate. In the presence of gastric acid, sodium alginate precipitates as a gel that forms a physical barrier that protects the gastric mucosa. When sodium bicarbonate is added, a carbon dioxide foam forms that is less harmful to the esophagus than GER-related fluids. While this combination treatment has reduced the number of acidic GER exposures and esophageal acid exposure in preterm infants in small studies, the long-term safety has not been evaluated in this populations.
Histamine2 (H2) blockers, like famotidine and ranitidine, also are commonly prescribed to treat preterm infant gastroesophageal reflux. H2 blockers compete with H2 for the histamine receptors of the parietal cells, which causes a decrease in hydrochloric acid and a subsequent increase in intragastric pH. These are often prescribed on the premise that GER symptoms are secondary to acid reflux in the lower esophagus, but there is no research on the efficacy of H2 blockers on the symptom profile of GER in preterm infants. This class of drugs also has been linked with an increased risk of necrotizing enterocolitis and a higher incidence of late-onset infections and death. This is thought to be caused by alteration of the intestinal microbiome, according to the clinical report.
Proton pump inhibitors (PPIs) are another treatment for reducing acid secretion by the parietal cells, but are largely ineffective in relieving clinical signs of GER in preterm infants. PPIs also have been associated with a higher risk of bacterial overgrowth, gastroenteritis, and community-acquired pneumonia in older children. It is theorized that, because of the acid mitigating effects of PPIs, they will have the potential for adverse effects similar to those seen with H2 blockers, although this has not been investigated.
Traditional treatments
Dr. Eichenwald also was quick to point out that even traditional methods of treating preterm infant GER are not particularly effective.
“Some of the conservative approaches that have been advocated include head-up position and different ways of side-lying to enhance emptying of the stomach after feeding. And none of those have been shown to reduce clinically appreciated signs of reflux in preterm infants. If anything – in term babies – some of those positions have been shown to increase the amount of reflux,” he said in an interview.
“I think that the other important point to make about this is that there are many signs that clinicians attribute to reflux in preterm babies, which include wakefulness, irritability, arching after a feeding. And none of those behaviors have been shown to be associated with reflux when it’s critically examined using either a pH Probe or multichannel impedance monitoring. And therefore the treatments to try to decrease reflux don’t really have an effect on those behaviors either.”
Parental concern
Treating a pediatric issue is not as simple as diagnosis and treatment. Often, parents are justifiably concerned about their children. Dr. Eichenwald sees educating parents as an important facet of treating GER in preterm infants.
“Quite honestly I think that there’s some projection on the part of adults who say, ‘I know how I feel when I have heartburn, which is the adult equivalent of reflux, and the baby must be experiencing the same thing, and that’s why they’re acting uncomfortable,’ ” suggested Dr. Eichenwald. “I think that it’s important for clinicians to educate families that a lot of the signs that we typically have attributed to gastroesophageal reflux are not really related to it.”
With both traditional and pharmacological interventions failing to treat preterm infant GER, Dr. Eichenwald believes that the most effective treatment could be patiently waiting. “I think that the important thing to stress is that reflux is a normal physiologic phenomenon. It rarely causes pathology in preterm infants, and therefore, in treating it, you’re not treating any pathology. You should just be patient and it will likely just go away on its own.”
Dr. Eichenwald has no potential conflicts of interest or external funding to report.
SOURCE: Eichenwald E et al. Pediatrics. 2018 June. doi: 10.1542/peds.2018-1061 .
Treatment of gastroesophageal reflux (GER) in preterm infants with traditional treatments, such as body positioning, and newer treatments with pharmacologic agents appear to be ineffective, and pharmacologic agents in particular may cause significant harm, according to a clinical report by the American Academy of Pediatrics Committee on Fetus and Newborn.
“I think that probably the most important point for any physician, including neonatologists, is that the committee concluded on the basis of the evidence that Eric Eichenwald, MD, lead author of the committee’s clinical report and chief of neonatology at Children’s Hospital of Philadelphia, said in an interview. “So really the bottom line of the clinical report is watchful waiting, conservative management, and patience is the most important approach to a baby that you think is suffering from reflux.”
Pharmacologic management
The committee members focused on four categories of pharmacologic interventions in their report in Pediatrics.
Prokinetic (promotility) agents, such as metoclopramide, domperidone, and erythromycin, are widely used in treating symptoms of GER in older infants and appear to improve gastric emptying, reduce regurgitation, and enhance lower esophageal sphincter tone, but they do not appear to reduce GER symptoms in preterm infants. In addition to not being effective in these infants, there is also a potential for significant adverse events, including cardiac arrhythmia and neurologic side effects. Another common pharmacologic treatment is the use of sodium alginate in combination with sodium bicarbonate. In the presence of gastric acid, sodium alginate precipitates as a gel that forms a physical barrier that protects the gastric mucosa. When sodium bicarbonate is added, a carbon dioxide foam forms that is less harmful to the esophagus than GER-related fluids. While this combination treatment has reduced the number of acidic GER exposures and esophageal acid exposure in preterm infants in small studies, the long-term safety has not been evaluated in this populations.
Histamine2 (H2) blockers, like famotidine and ranitidine, also are commonly prescribed to treat preterm infant gastroesophageal reflux. H2 blockers compete with H2 for the histamine receptors of the parietal cells, which causes a decrease in hydrochloric acid and a subsequent increase in intragastric pH. These are often prescribed on the premise that GER symptoms are secondary to acid reflux in the lower esophagus, but there is no research on the efficacy of H2 blockers on the symptom profile of GER in preterm infants. This class of drugs also has been linked with an increased risk of necrotizing enterocolitis and a higher incidence of late-onset infections and death. This is thought to be caused by alteration of the intestinal microbiome, according to the clinical report.
Proton pump inhibitors (PPIs) are another treatment for reducing acid secretion by the parietal cells, but are largely ineffective in relieving clinical signs of GER in preterm infants. PPIs also have been associated with a higher risk of bacterial overgrowth, gastroenteritis, and community-acquired pneumonia in older children. It is theorized that, because of the acid mitigating effects of PPIs, they will have the potential for adverse effects similar to those seen with H2 blockers, although this has not been investigated.
Traditional treatments
Dr. Eichenwald also was quick to point out that even traditional methods of treating preterm infant GER are not particularly effective.
“Some of the conservative approaches that have been advocated include head-up position and different ways of side-lying to enhance emptying of the stomach after feeding. And none of those have been shown to reduce clinically appreciated signs of reflux in preterm infants. If anything – in term babies – some of those positions have been shown to increase the amount of reflux,” he said in an interview.
“I think that the other important point to make about this is that there are many signs that clinicians attribute to reflux in preterm babies, which include wakefulness, irritability, arching after a feeding. And none of those behaviors have been shown to be associated with reflux when it’s critically examined using either a pH Probe or multichannel impedance monitoring. And therefore the treatments to try to decrease reflux don’t really have an effect on those behaviors either.”
Parental concern
Treating a pediatric issue is not as simple as diagnosis and treatment. Often, parents are justifiably concerned about their children. Dr. Eichenwald sees educating parents as an important facet of treating GER in preterm infants.
“Quite honestly I think that there’s some projection on the part of adults who say, ‘I know how I feel when I have heartburn, which is the adult equivalent of reflux, and the baby must be experiencing the same thing, and that’s why they’re acting uncomfortable,’ ” suggested Dr. Eichenwald. “I think that it’s important for clinicians to educate families that a lot of the signs that we typically have attributed to gastroesophageal reflux are not really related to it.”
With both traditional and pharmacological interventions failing to treat preterm infant GER, Dr. Eichenwald believes that the most effective treatment could be patiently waiting. “I think that the important thing to stress is that reflux is a normal physiologic phenomenon. It rarely causes pathology in preterm infants, and therefore, in treating it, you’re not treating any pathology. You should just be patient and it will likely just go away on its own.”
Dr. Eichenwald has no potential conflicts of interest or external funding to report.
SOURCE: Eichenwald E et al. Pediatrics. 2018 June. doi: 10.1542/peds.2018-1061 .
Treatment of gastroesophageal reflux (GER) in preterm infants with traditional treatments, such as body positioning, and newer treatments with pharmacologic agents appear to be ineffective, and pharmacologic agents in particular may cause significant harm, according to a clinical report by the American Academy of Pediatrics Committee on Fetus and Newborn.
“I think that probably the most important point for any physician, including neonatologists, is that the committee concluded on the basis of the evidence that Eric Eichenwald, MD, lead author of the committee’s clinical report and chief of neonatology at Children’s Hospital of Philadelphia, said in an interview. “So really the bottom line of the clinical report is watchful waiting, conservative management, and patience is the most important approach to a baby that you think is suffering from reflux.”
Pharmacologic management
The committee members focused on four categories of pharmacologic interventions in their report in Pediatrics.
Prokinetic (promotility) agents, such as metoclopramide, domperidone, and erythromycin, are widely used in treating symptoms of GER in older infants and appear to improve gastric emptying, reduce regurgitation, and enhance lower esophageal sphincter tone, but they do not appear to reduce GER symptoms in preterm infants. In addition to not being effective in these infants, there is also a potential for significant adverse events, including cardiac arrhythmia and neurologic side effects. Another common pharmacologic treatment is the use of sodium alginate in combination with sodium bicarbonate. In the presence of gastric acid, sodium alginate precipitates as a gel that forms a physical barrier that protects the gastric mucosa. When sodium bicarbonate is added, a carbon dioxide foam forms that is less harmful to the esophagus than GER-related fluids. While this combination treatment has reduced the number of acidic GER exposures and esophageal acid exposure in preterm infants in small studies, the long-term safety has not been evaluated in this populations.
Histamine2 (H2) blockers, like famotidine and ranitidine, also are commonly prescribed to treat preterm infant gastroesophageal reflux. H2 blockers compete with H2 for the histamine receptors of the parietal cells, which causes a decrease in hydrochloric acid and a subsequent increase in intragastric pH. These are often prescribed on the premise that GER symptoms are secondary to acid reflux in the lower esophagus, but there is no research on the efficacy of H2 blockers on the symptom profile of GER in preterm infants. This class of drugs also has been linked with an increased risk of necrotizing enterocolitis and a higher incidence of late-onset infections and death. This is thought to be caused by alteration of the intestinal microbiome, according to the clinical report.
Proton pump inhibitors (PPIs) are another treatment for reducing acid secretion by the parietal cells, but are largely ineffective in relieving clinical signs of GER in preterm infants. PPIs also have been associated with a higher risk of bacterial overgrowth, gastroenteritis, and community-acquired pneumonia in older children. It is theorized that, because of the acid mitigating effects of PPIs, they will have the potential for adverse effects similar to those seen with H2 blockers, although this has not been investigated.
Traditional treatments
Dr. Eichenwald also was quick to point out that even traditional methods of treating preterm infant GER are not particularly effective.
“Some of the conservative approaches that have been advocated include head-up position and different ways of side-lying to enhance emptying of the stomach after feeding. And none of those have been shown to reduce clinically appreciated signs of reflux in preterm infants. If anything – in term babies – some of those positions have been shown to increase the amount of reflux,” he said in an interview.
“I think that the other important point to make about this is that there are many signs that clinicians attribute to reflux in preterm babies, which include wakefulness, irritability, arching after a feeding. And none of those behaviors have been shown to be associated with reflux when it’s critically examined using either a pH Probe or multichannel impedance monitoring. And therefore the treatments to try to decrease reflux don’t really have an effect on those behaviors either.”
Parental concern
Treating a pediatric issue is not as simple as diagnosis and treatment. Often, parents are justifiably concerned about their children. Dr. Eichenwald sees educating parents as an important facet of treating GER in preterm infants.
“Quite honestly I think that there’s some projection on the part of adults who say, ‘I know how I feel when I have heartburn, which is the adult equivalent of reflux, and the baby must be experiencing the same thing, and that’s why they’re acting uncomfortable,’ ” suggested Dr. Eichenwald. “I think that it’s important for clinicians to educate families that a lot of the signs that we typically have attributed to gastroesophageal reflux are not really related to it.”
With both traditional and pharmacological interventions failing to treat preterm infant GER, Dr. Eichenwald believes that the most effective treatment could be patiently waiting. “I think that the important thing to stress is that reflux is a normal physiologic phenomenon. It rarely causes pathology in preterm infants, and therefore, in treating it, you’re not treating any pathology. You should just be patient and it will likely just go away on its own.”
Dr. Eichenwald has no potential conflicts of interest or external funding to report.
SOURCE: Eichenwald E et al. Pediatrics. 2018 June. doi: 10.1542/peds.2018-1061 .
FROM PEDIATRICS
Pancreatic cancer has a pancreatopathy distinct from type 2 diabetes
WASHINGTON –
“The endocrinopathies associated with type 2 diabetes mellitus and pancreatic cancer are distinct, the former represented by an increase in glucagon and the latter characterized by a reduction in islet size,” said Sajan Nagpal, MD, of the Mayo Clinic in Rochester, Minn., at Digestive Disease Week 2018®. “These data lend insight to a unique pathophysiology of diabetes that results from pancreatic cancer.”
Prior to presenting his results, Dr. Nagpal pointed out an interesting relationship between pancreatic cancer and diabetes.
“Pancreatic cancer and diabetes have a very unique, two-way relationship. While long-standing diabetes [LSDM] increases the risk of developing pancreatic cancer by 1.5-2 times over a person’s lifetime, pancreatic cancer itself causes a paraneoplastic form of diabetes. A person with a new diagnosis of diabetes mellitus has a five to eight times increased risk of being diagnosed with pancreatic cancer as compared to the general population within 3 years.“
This form of diabetes is referred to as pancreatic cancer–induced new onset diabetes (PC-NOD).
Dr. Nagpal and his team conducted a study that included 46 patients: 16 patients with pancreatic cancer (5 with LSDM, 5 NOD, and 6 without diabetes mellitus), 15 patients with T2DM (9 LSDM, 6 NOD), and 15 controls matched for age and body mass index. NOD was defined as a diabetes mellitus diagnosis less than 3 years from the date of autopsy or pancreatic cancer diagnosis. All pancreatic specimens were resected from pancreatic cancer patients or obtained as autopsy specimens. Researchers performed islet morphometric studies utilizing immunofluorescence analysis with specific insulin and glucagon antibodies.
The results of the study showed that patients with pancreatic cancer had islet sizes that were about a third smaller than those in the patients with T2DM and the healthy controls (P = .005). This held true for both LSDM and NOD pancreatic cancer patients, compared with the T2DM and healthy control groups. Researchers also found that insulin to glucagon (I:G) ratios were preserved in pancreatic cancer patients, whereas they were lower in patients with T2DM because of a higher percentage of glucagon in the islets (P = .08). Additionally, islet amyloid was much higher in T2DM patients (66.7%) versus patients with diabetes associated with pancreatic cancer (55.6%) and healthy controls (13.3%; P = .01).
There were several limitations to this study, including the small number of patients in each group and how pancreatic islet characteristics can vary based on their location. Finally, ductal obstruction can cause changes to islet morphology.
Along with the pathological changes found by Dr. Nagpal and his research team, PC-NOD and T2DM also have unique clinical profiles. As patients with pancreatic cancer approach their diagnosis, they begin to lose weight. This begins about 1 year before the patient’s diagnosis of pancreatic cancer. Conversely, these patients have worsening fasting glucose levels despite the fact that they are losing weight. The paradoxical relationship between weight loss and hyperglycemia are what distinguishes PC-NOD from T2DM, according to Dr. Nagpal. In patients with PC-NOD, worsening hyperglycemia happens over a periods of months, compared with the gradual increase over the course of years seen in T2DM.
The differences between these diseases may be caused by differences in their pancreatopathy.
When discussing the pancreatopathy associated with T2DM, Dr. Nagpal pointed out that there is a decrease in the I:G ratio, compared with those seen in patients without diabetes. The prevailing theory is that this decrease in the I:G ratio is caused by beta-cell apoptosis and transdifferentiation to alpha-cells. T2DM patients also have increased amyloid deposits, the result of increased islet amyloid polypeptide.
”Pancreatic cancer provides subtle metabolic clues, such as worsening glucose tolerance and weight loss, that can serve as potential targets for its early detection.”
According to Dr. Nagpal, more research is needed on pathogenesis of PC-NOD. Identification of biomarkers for screening may be possible in patients with new onset diabetes.
Dr. Nagpal had no financial conflicts of interest to report.
SOURCE: Nagpal S et al. DDW 2018, Abstract 392.
WASHINGTON –
“The endocrinopathies associated with type 2 diabetes mellitus and pancreatic cancer are distinct, the former represented by an increase in glucagon and the latter characterized by a reduction in islet size,” said Sajan Nagpal, MD, of the Mayo Clinic in Rochester, Minn., at Digestive Disease Week 2018®. “These data lend insight to a unique pathophysiology of diabetes that results from pancreatic cancer.”
Prior to presenting his results, Dr. Nagpal pointed out an interesting relationship between pancreatic cancer and diabetes.
“Pancreatic cancer and diabetes have a very unique, two-way relationship. While long-standing diabetes [LSDM] increases the risk of developing pancreatic cancer by 1.5-2 times over a person’s lifetime, pancreatic cancer itself causes a paraneoplastic form of diabetes. A person with a new diagnosis of diabetes mellitus has a five to eight times increased risk of being diagnosed with pancreatic cancer as compared to the general population within 3 years.“
This form of diabetes is referred to as pancreatic cancer–induced new onset diabetes (PC-NOD).
Dr. Nagpal and his team conducted a study that included 46 patients: 16 patients with pancreatic cancer (5 with LSDM, 5 NOD, and 6 without diabetes mellitus), 15 patients with T2DM (9 LSDM, 6 NOD), and 15 controls matched for age and body mass index. NOD was defined as a diabetes mellitus diagnosis less than 3 years from the date of autopsy or pancreatic cancer diagnosis. All pancreatic specimens were resected from pancreatic cancer patients or obtained as autopsy specimens. Researchers performed islet morphometric studies utilizing immunofluorescence analysis with specific insulin and glucagon antibodies.
The results of the study showed that patients with pancreatic cancer had islet sizes that were about a third smaller than those in the patients with T2DM and the healthy controls (P = .005). This held true for both LSDM and NOD pancreatic cancer patients, compared with the T2DM and healthy control groups. Researchers also found that insulin to glucagon (I:G) ratios were preserved in pancreatic cancer patients, whereas they were lower in patients with T2DM because of a higher percentage of glucagon in the islets (P = .08). Additionally, islet amyloid was much higher in T2DM patients (66.7%) versus patients with diabetes associated with pancreatic cancer (55.6%) and healthy controls (13.3%; P = .01).
There were several limitations to this study, including the small number of patients in each group and how pancreatic islet characteristics can vary based on their location. Finally, ductal obstruction can cause changes to islet morphology.
Along with the pathological changes found by Dr. Nagpal and his research team, PC-NOD and T2DM also have unique clinical profiles. As patients with pancreatic cancer approach their diagnosis, they begin to lose weight. This begins about 1 year before the patient’s diagnosis of pancreatic cancer. Conversely, these patients have worsening fasting glucose levels despite the fact that they are losing weight. The paradoxical relationship between weight loss and hyperglycemia are what distinguishes PC-NOD from T2DM, according to Dr. Nagpal. In patients with PC-NOD, worsening hyperglycemia happens over a periods of months, compared with the gradual increase over the course of years seen in T2DM.
The differences between these diseases may be caused by differences in their pancreatopathy.
When discussing the pancreatopathy associated with T2DM, Dr. Nagpal pointed out that there is a decrease in the I:G ratio, compared with those seen in patients without diabetes. The prevailing theory is that this decrease in the I:G ratio is caused by beta-cell apoptosis and transdifferentiation to alpha-cells. T2DM patients also have increased amyloid deposits, the result of increased islet amyloid polypeptide.
”Pancreatic cancer provides subtle metabolic clues, such as worsening glucose tolerance and weight loss, that can serve as potential targets for its early detection.”
According to Dr. Nagpal, more research is needed on pathogenesis of PC-NOD. Identification of biomarkers for screening may be possible in patients with new onset diabetes.
Dr. Nagpal had no financial conflicts of interest to report.
SOURCE: Nagpal S et al. DDW 2018, Abstract 392.
WASHINGTON –
“The endocrinopathies associated with type 2 diabetes mellitus and pancreatic cancer are distinct, the former represented by an increase in glucagon and the latter characterized by a reduction in islet size,” said Sajan Nagpal, MD, of the Mayo Clinic in Rochester, Minn., at Digestive Disease Week 2018®. “These data lend insight to a unique pathophysiology of diabetes that results from pancreatic cancer.”
Prior to presenting his results, Dr. Nagpal pointed out an interesting relationship between pancreatic cancer and diabetes.
“Pancreatic cancer and diabetes have a very unique, two-way relationship. While long-standing diabetes [LSDM] increases the risk of developing pancreatic cancer by 1.5-2 times over a person’s lifetime, pancreatic cancer itself causes a paraneoplastic form of diabetes. A person with a new diagnosis of diabetes mellitus has a five to eight times increased risk of being diagnosed with pancreatic cancer as compared to the general population within 3 years.“
This form of diabetes is referred to as pancreatic cancer–induced new onset diabetes (PC-NOD).
Dr. Nagpal and his team conducted a study that included 46 patients: 16 patients with pancreatic cancer (5 with LSDM, 5 NOD, and 6 without diabetes mellitus), 15 patients with T2DM (9 LSDM, 6 NOD), and 15 controls matched for age and body mass index. NOD was defined as a diabetes mellitus diagnosis less than 3 years from the date of autopsy or pancreatic cancer diagnosis. All pancreatic specimens were resected from pancreatic cancer patients or obtained as autopsy specimens. Researchers performed islet morphometric studies utilizing immunofluorescence analysis with specific insulin and glucagon antibodies.
The results of the study showed that patients with pancreatic cancer had islet sizes that were about a third smaller than those in the patients with T2DM and the healthy controls (P = .005). This held true for both LSDM and NOD pancreatic cancer patients, compared with the T2DM and healthy control groups. Researchers also found that insulin to glucagon (I:G) ratios were preserved in pancreatic cancer patients, whereas they were lower in patients with T2DM because of a higher percentage of glucagon in the islets (P = .08). Additionally, islet amyloid was much higher in T2DM patients (66.7%) versus patients with diabetes associated with pancreatic cancer (55.6%) and healthy controls (13.3%; P = .01).
There were several limitations to this study, including the small number of patients in each group and how pancreatic islet characteristics can vary based on their location. Finally, ductal obstruction can cause changes to islet morphology.
Along with the pathological changes found by Dr. Nagpal and his research team, PC-NOD and T2DM also have unique clinical profiles. As patients with pancreatic cancer approach their diagnosis, they begin to lose weight. This begins about 1 year before the patient’s diagnosis of pancreatic cancer. Conversely, these patients have worsening fasting glucose levels despite the fact that they are losing weight. The paradoxical relationship between weight loss and hyperglycemia are what distinguishes PC-NOD from T2DM, according to Dr. Nagpal. In patients with PC-NOD, worsening hyperglycemia happens over a periods of months, compared with the gradual increase over the course of years seen in T2DM.
The differences between these diseases may be caused by differences in their pancreatopathy.
When discussing the pancreatopathy associated with T2DM, Dr. Nagpal pointed out that there is a decrease in the I:G ratio, compared with those seen in patients without diabetes. The prevailing theory is that this decrease in the I:G ratio is caused by beta-cell apoptosis and transdifferentiation to alpha-cells. T2DM patients also have increased amyloid deposits, the result of increased islet amyloid polypeptide.
”Pancreatic cancer provides subtle metabolic clues, such as worsening glucose tolerance and weight loss, that can serve as potential targets for its early detection.”
According to Dr. Nagpal, more research is needed on pathogenesis of PC-NOD. Identification of biomarkers for screening may be possible in patients with new onset diabetes.
Dr. Nagpal had no financial conflicts of interest to report.
SOURCE: Nagpal S et al. DDW 2018, Abstract 392.
REPORTING FROM DDW 2018
Key clinical point: Pancreatic cancer has a distinct endocrine pancreatopathy.
Major finding: Patients with pancreatic cancer had islet sizes that were about a third smaller than those in patients with type 2 diabetes and healthy controls (P = .005).
Study details: Small study analyzing the pathology of pancreatic cancer resections and autopsy specimens.
Disclosures: The authors of this study had no financial conflicts to disclose.
Source: Nagpal S et al. DDW 2018, Abstract 392.