User login
Growth Spurt
Despite intravenous medication, a young boy in status epilepticus had the pediatric ICU team at the University of Wisconsin School of Medicine and Public Health in Madison stumped. The team called for a consult with the Integrative Medicine Program, which works with licensed acupuncturists and has been affiliated with the department of family medicine since 2001. Acupuncture’s efficacy in this setting has not been validated, but it has been shown to ease chemotherapy-induced nausea and vomiting, as well as radiation-induced xerostomia.1,2
Following several treatments by a licensed acupuncturist and continued conventional care, the boy’s seizures subsided and he was transitioned to the medical floor. Did the acupuncture contribute to bringing the seizures under control? “I can’t say that it was the acupuncture—it was probably a function of all the therapies working together,” says David P. Rakel, MD, assistant professor and director of UW’s Integrative Medicine Program.
The UW case illustrates both current trends and the constant conundrum that surrounds hospital-based complementary medicine: Complementary and alternative medicine’s use is increasing in some U.S. hospitals, yet the existing research evidence for the efficacy of its multiple modalities is decidedly mixed.
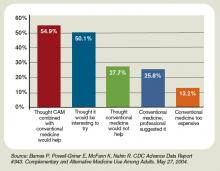
Even if your hospital does not offer complementary and alternative medicine (CAM), your patients are using CAM at ever-increasing rates. In 1993, 34% of Americans reported using some type of CAM (e.g., supplements, massage therapy, prayer, and so on). That number has almost doubled to 62%.3 Americans spend $47 billion a year—of their own money—for CAM therapies, chiropractors, acupuncturists, and massage therapists. And older patients with chronic conditions—the kind of patient hospitalists are most familiar with—tend to try CAM more than younger patients.4
These trends can directly affect hospitalists’ treatment decisions, but they also play a part in how you establish communication and trust with your patients, and how you keep your patients safe from adverse drug interactions. According to the National Academy of Sciences, in order to effectively counsel patients and ensure high-quality comprehensive care, conventional professionals need more CAM-related education.5

—Suzanne Bertisch, MD, MPH, fellow, Harvard Medical School’s Osher Research Center
What Trends Show
In 2007, according to the American Hospital Association, 20.8% of community hospitals offered some type of care or treatment not based on traditional Western allopathic medicine. That’s up from 8.6% of reporting hospitals that offered those services in 1998.
The 1990s saw rapid growth of integrative medicine centers at major research institutions, and the majority of U.S. cancer centers now offer some form of complementary therapy, says Barrie R. Cassileth, MS, PhD, the Laurance S. Rockefeller Chair in Integrative Medicine and chief of the Integrative Medicine Service at Memorial Sloan-Kettering Cancer Center in New York City.
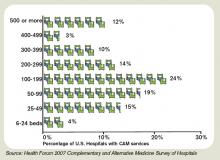
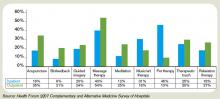
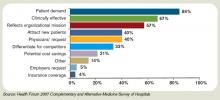
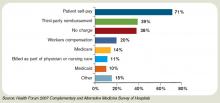
The 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals reported that complementary programs are more common in urban rather than rural hospitals; services vary by hospital size (see Figure 2, above); and the top six modalities offered on an inpatient basis are pet therapy, massage therapy, music/art therapy, guided imagery, acupuncture, and reiki (see “Glossary of Complementary Terms,” above). Eighty-four percent of hospitals offer complementary services due to patient demand, the survey showed.
Joseph Ming-Wah Li, MD, FHM, SHM board member and assistant professor of medicine at Harvard Medical School and director of the hospital medicine program and associate chief of the division of general medicine and primary care at Beth Israel Deaconess Medical Center in Boston, doesn’t see a problem with modalities that can make his patients feel better. Patients at his hospital have access to pet therapy, massage, and acupuncture. “I don’t think these modalities hurt our patients, and there is very little downside, except for potential cost,” says Dr. Li, an SHM board member. “What’s not clear is whether these therapies work or not.”
What’s in a Name?
Numerous therapies and modalities crowd under the CAM umbrella, but most experts classify “complementary” modalities as those used in conjunction with conventional medicine to mitigate symptoms of disease or treatment, whereas “alternative” connotes therapies claiming to treat or cure the underlying disease. Some harmful, dangerous, and dishonest practices fall into the “alternative” category, such as Hulda Clark’s “Zapper” device, which was promoted as a cure for liver flukes, something she says cause everything from diabetes to heart disease. (For more on questionable practices, visit www.quackwatch.com or the National Council Against Health Fraud’s Web site at www.ncahf.org.)
The National Institutes of Health’s National Center for Complementary and Alternative Medicine (NCCAM) defines CAM as a group of “diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.” Dr. Cassileth says the conflation of “complementary and alternative” into one neat acronym—CAM—causes confusion among patients and medical professionals. NCCAM will be changing its name soon, she says, to the National Center for Integrative Medicine, emphasizing the use of adjunctive modalities along with conventional medical treatments.
Hospitalist Suzanne Bertisch, MD, MPH, recently completed a research fellowship at Harvard Medical School’s Osher Research Center. She explains that integrative medicine uses a macro model of health, claiming a middle ground between the traditional, allopathic model of treating disease.
All Kinds of Evidence
Twenty years of complementary medicine research has yielded some information about safety—namely, what works and what doesn’t. For example, saw palmetto has not panned out as an effective treatment for benign prostatic hyperplasia; St. John’s wort, useful for mild depression, interferes with many medications, including cyclosporine and warfarin, and should be avoided at least five days prior to surgery.7,8
Since NCCAM’s inception in October 1998, its research portfolio has stirred debate in the scientific community. Part of the disagreement stems from the difficulty of fitting multidimensional interventions, some of which are provider-dependent (e.g., massage or acupuncture), into the gold standard of the randomized, double-blind, placebo-controlled trial, explains Darshan Mehta, MD, MPH, associate director of medical education at the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital in Boston. The manner in which the effectiveness of integrative techniques is assessed requires a higher sophistication of systems research, Dr. Mehta says.
“The way we construe evidence needs to change,” she adds.
Likely to Expand
Most private health plans do not cover complementary services, although Medicare and numerous insurance plans will reimburse treatment in conjunction with physical therapy (e.g., massage) in the outpatient setting. Twenty-three states cover chiropractic care under Medicaid, and Medicare has begun to assess the cost-effectiveness of including acupuncture—especially for postoperative and chemotherapy-associated nausea and vomiting—in its benefits package.9 Other modalities, ranging from aromatherapy to guided imagery training, are paid for largely out-of-pocket.10
Dr. Rakel notes that the delivery of integrative medicine services at UW entails conversations with patients about out-of-pocket payments. “It can pose a barrier to the clinician-patient relationship if you give them acupuncture to help with their chemotherapy-induced nausea and then ask for their credit card,” he says.
Hospitalist Preparation
Most complementary therapies are currently offered on an outpatient basis. Because of this trend, and because they deal with acute conditions, hospitalists are less likely to be involved with complementary or integrative medicine services, says Beth Israel Deaconess Medical Center hospitalist Andrew C. Ahn, MD, MPH. But that’s not to say complementary medicine is something hospitalists should ignore; patients arrive at the hospital with CAM regimens in tow. It’s the No. 1 reason, Dr. Ahn says, hospitalists should be knowledgeable and exposed to CAM therapies.
Physicians must understand patient patterns and preferences regarding allopathic and complementary medicine, says Sita Ananth, MHA, director of knowledge services and optimal healing environments at the Samueli Institute in Alexandria, Va., and author of the 2007 AHA report. She points to a 2006 survey conducted by AARP and NCCAM that found almost 70% of respondents did not tell their physicians about their complementary medicine approaches. These patients are within the age range most likely to be cared for by hospitalists, and failure to communicate about complementary treatment, such as supplemental vitamin use, could lead to safety issues. Moreover, without complete disclosure, the patient-physician relationship might not be as open as possible, Dr. Ananth says.
Many acute-care hospitalists do not have formal dietary supplement policies, and less than half of U.S. children’s hospitals require documentation of a check for drug or dietary supplement interaction.11,12 As a safety issue, it is always incumbent on hospitalists, says Dr. Li, to ask about any supplements or therapies patients are trying on their own as part of the history and physical examination. The policy at Memorial Sloan-Kettering Cancer Center, Dr. Cassileth says, is that patients on chemotherapy or who are undergoing radiation or facing surgery must avoid herbal dietary supplements.
Beyond Safety
Dr. Bertisch advises hospitalists to pose questions about complementary therapies in an open manner, avoiding antagonistic discussions. “Even when I disagree, I try to guide them to issues about safety and nonsafety, and coax in my concerns,” she says. “The most challenging part about complementary medicine is that patients’ beliefs in these therapies may be so strong that even if the doctor says it won’t work, that will not necessarily change that belief.” A 2001 study in the Archives of Internal Medicine revealed that 70% of respondents would continue to take supplements even if a major study or their physician told them they didn’t work.13
The attraction to complementary medicine often reflects patients’ preferences for a holistic approach to health, says Dr. Ahn, or it may emanate from traditions carried with them from their country of origin. “Once you do understand their reasons for using CAM, then the patient-physician relationship can be significantly strengthened,” he says. With nearly two-thirds of Americans using some form of CAM, hospitalists need to engage in this dialogue.
Dr. Rakel agrees understanding patient culture is vital to uncovering useful information. “Most clinicians would agree that if we can match a therapy to the patient culture and belief system, we are more likely to get buy-in from the patient,” he says.
Dr. Mehta also is a clinical instructor of medicine at Harvard Medical School. He teaches his residents to educate themselves about credentialing, certification, and licensure of complementary providers. He also asks them to maintain an open mind. He says the most important preparation for hospitalists right now is to help educate their patients to be more proactive in their own healthcare. “An engaged patient,” he says, “is better than a disengaged patient.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Deng G, Cassileth BR, Yeung KS. Complementary therapies for cancer-related symptoms. J Support Oncol. 2004;2(5):419-426.
- Kahn ST, Johnstone PA. Management of xerostomia related to radiotherapy for head and neck cancer. Oncology. 2005;19(14):1827-1832.
- Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;27(343):1-19.
- Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280(18):1569-1575.
- Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington, D.C: National Academies Press; 2005.
- Ananth S. 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals. Health Forum LLC. 2008.
- Bent S, Kane C, Shinohara K, et al. Saw palmetto for benign prostatic hyperplasia. N Engl J Med. 2006;354(6):557-566.
- Bauer BA. The herbal hospitalist. The Hospitalist. 2006;10(2);16-17.
- Ananth S. Applying integrative healthcare. Explore. 2009;5(2):119-120.
- Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246-52
- Bassie KL, Witmer DR, Pinto B, Bush C, Clark J, Deffenbaugh J Jr. National survey of dietary supplement policies in acute care facilities. Am J Health Syst Pharm. 2006;63(1):65-70.
- Gardiner P, Phillips RS, Kemper KJ, Legedza A, Henlon S, Woolf AD. Dietary supplements: inpatient policies in US children’s hospitals. Pediatrics. 2008;121(4):e775-781.
- Blendon RJ, DesRoches CM, Benson JM, Brodie M, Altman DE. Americans’ views on the use and regulation of dietary supplements. Arch Intern Med. 2001;161(6):805-810.
Top Image Source: TETRA IMAGES
Despite intravenous medication, a young boy in status epilepticus had the pediatric ICU team at the University of Wisconsin School of Medicine and Public Health in Madison stumped. The team called for a consult with the Integrative Medicine Program, which works with licensed acupuncturists and has been affiliated with the department of family medicine since 2001. Acupuncture’s efficacy in this setting has not been validated, but it has been shown to ease chemotherapy-induced nausea and vomiting, as well as radiation-induced xerostomia.1,2
Following several treatments by a licensed acupuncturist and continued conventional care, the boy’s seizures subsided and he was transitioned to the medical floor. Did the acupuncture contribute to bringing the seizures under control? “I can’t say that it was the acupuncture—it was probably a function of all the therapies working together,” says David P. Rakel, MD, assistant professor and director of UW’s Integrative Medicine Program.
The UW case illustrates both current trends and the constant conundrum that surrounds hospital-based complementary medicine: Complementary and alternative medicine’s use is increasing in some U.S. hospitals, yet the existing research evidence for the efficacy of its multiple modalities is decidedly mixed.
Even if your hospital does not offer complementary and alternative medicine (CAM), your patients are using CAM at ever-increasing rates. In 1993, 34% of Americans reported using some type of CAM (e.g., supplements, massage therapy, prayer, and so on). That number has almost doubled to 62%.3 Americans spend $47 billion a year—of their own money—for CAM therapies, chiropractors, acupuncturists, and massage therapists. And older patients with chronic conditions—the kind of patient hospitalists are most familiar with—tend to try CAM more than younger patients.4
These trends can directly affect hospitalists’ treatment decisions, but they also play a part in how you establish communication and trust with your patients, and how you keep your patients safe from adverse drug interactions. According to the National Academy of Sciences, in order to effectively counsel patients and ensure high-quality comprehensive care, conventional professionals need more CAM-related education.5

—Suzanne Bertisch, MD, MPH, fellow, Harvard Medical School’s Osher Research Center
What Trends Show
In 2007, according to the American Hospital Association, 20.8% of community hospitals offered some type of care or treatment not based on traditional Western allopathic medicine. That’s up from 8.6% of reporting hospitals that offered those services in 1998.
The 1990s saw rapid growth of integrative medicine centers at major research institutions, and the majority of U.S. cancer centers now offer some form of complementary therapy, says Barrie R. Cassileth, MS, PhD, the Laurance S. Rockefeller Chair in Integrative Medicine and chief of the Integrative Medicine Service at Memorial Sloan-Kettering Cancer Center in New York City.
The 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals reported that complementary programs are more common in urban rather than rural hospitals; services vary by hospital size (see Figure 2, above); and the top six modalities offered on an inpatient basis are pet therapy, massage therapy, music/art therapy, guided imagery, acupuncture, and reiki (see “Glossary of Complementary Terms,” above). Eighty-four percent of hospitals offer complementary services due to patient demand, the survey showed.
Joseph Ming-Wah Li, MD, FHM, SHM board member and assistant professor of medicine at Harvard Medical School and director of the hospital medicine program and associate chief of the division of general medicine and primary care at Beth Israel Deaconess Medical Center in Boston, doesn’t see a problem with modalities that can make his patients feel better. Patients at his hospital have access to pet therapy, massage, and acupuncture. “I don’t think these modalities hurt our patients, and there is very little downside, except for potential cost,” says Dr. Li, an SHM board member. “What’s not clear is whether these therapies work or not.”
What’s in a Name?
Numerous therapies and modalities crowd under the CAM umbrella, but most experts classify “complementary” modalities as those used in conjunction with conventional medicine to mitigate symptoms of disease or treatment, whereas “alternative” connotes therapies claiming to treat or cure the underlying disease. Some harmful, dangerous, and dishonest practices fall into the “alternative” category, such as Hulda Clark’s “Zapper” device, which was promoted as a cure for liver flukes, something she says cause everything from diabetes to heart disease. (For more on questionable practices, visit www.quackwatch.com or the National Council Against Health Fraud’s Web site at www.ncahf.org.)
The National Institutes of Health’s National Center for Complementary and Alternative Medicine (NCCAM) defines CAM as a group of “diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.” Dr. Cassileth says the conflation of “complementary and alternative” into one neat acronym—CAM—causes confusion among patients and medical professionals. NCCAM will be changing its name soon, she says, to the National Center for Integrative Medicine, emphasizing the use of adjunctive modalities along with conventional medical treatments.
Hospitalist Suzanne Bertisch, MD, MPH, recently completed a research fellowship at Harvard Medical School’s Osher Research Center. She explains that integrative medicine uses a macro model of health, claiming a middle ground between the traditional, allopathic model of treating disease.
All Kinds of Evidence
Twenty years of complementary medicine research has yielded some information about safety—namely, what works and what doesn’t. For example, saw palmetto has not panned out as an effective treatment for benign prostatic hyperplasia; St. John’s wort, useful for mild depression, interferes with many medications, including cyclosporine and warfarin, and should be avoided at least five days prior to surgery.7,8
Since NCCAM’s inception in October 1998, its research portfolio has stirred debate in the scientific community. Part of the disagreement stems from the difficulty of fitting multidimensional interventions, some of which are provider-dependent (e.g., massage or acupuncture), into the gold standard of the randomized, double-blind, placebo-controlled trial, explains Darshan Mehta, MD, MPH, associate director of medical education at the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital in Boston. The manner in which the effectiveness of integrative techniques is assessed requires a higher sophistication of systems research, Dr. Mehta says.
“The way we construe evidence needs to change,” she adds.
Likely to Expand
Most private health plans do not cover complementary services, although Medicare and numerous insurance plans will reimburse treatment in conjunction with physical therapy (e.g., massage) in the outpatient setting. Twenty-three states cover chiropractic care under Medicaid, and Medicare has begun to assess the cost-effectiveness of including acupuncture—especially for postoperative and chemotherapy-associated nausea and vomiting—in its benefits package.9 Other modalities, ranging from aromatherapy to guided imagery training, are paid for largely out-of-pocket.10
Dr. Rakel notes that the delivery of integrative medicine services at UW entails conversations with patients about out-of-pocket payments. “It can pose a barrier to the clinician-patient relationship if you give them acupuncture to help with their chemotherapy-induced nausea and then ask for their credit card,” he says.
Hospitalist Preparation
Most complementary therapies are currently offered on an outpatient basis. Because of this trend, and because they deal with acute conditions, hospitalists are less likely to be involved with complementary or integrative medicine services, says Beth Israel Deaconess Medical Center hospitalist Andrew C. Ahn, MD, MPH. But that’s not to say complementary medicine is something hospitalists should ignore; patients arrive at the hospital with CAM regimens in tow. It’s the No. 1 reason, Dr. Ahn says, hospitalists should be knowledgeable and exposed to CAM therapies.
Physicians must understand patient patterns and preferences regarding allopathic and complementary medicine, says Sita Ananth, MHA, director of knowledge services and optimal healing environments at the Samueli Institute in Alexandria, Va., and author of the 2007 AHA report. She points to a 2006 survey conducted by AARP and NCCAM that found almost 70% of respondents did not tell their physicians about their complementary medicine approaches. These patients are within the age range most likely to be cared for by hospitalists, and failure to communicate about complementary treatment, such as supplemental vitamin use, could lead to safety issues. Moreover, without complete disclosure, the patient-physician relationship might not be as open as possible, Dr. Ananth says.
Many acute-care hospitalists do not have formal dietary supplement policies, and less than half of U.S. children’s hospitals require documentation of a check for drug or dietary supplement interaction.11,12 As a safety issue, it is always incumbent on hospitalists, says Dr. Li, to ask about any supplements or therapies patients are trying on their own as part of the history and physical examination. The policy at Memorial Sloan-Kettering Cancer Center, Dr. Cassileth says, is that patients on chemotherapy or who are undergoing radiation or facing surgery must avoid herbal dietary supplements.
Beyond Safety
Dr. Bertisch advises hospitalists to pose questions about complementary therapies in an open manner, avoiding antagonistic discussions. “Even when I disagree, I try to guide them to issues about safety and nonsafety, and coax in my concerns,” she says. “The most challenging part about complementary medicine is that patients’ beliefs in these therapies may be so strong that even if the doctor says it won’t work, that will not necessarily change that belief.” A 2001 study in the Archives of Internal Medicine revealed that 70% of respondents would continue to take supplements even if a major study or their physician told them they didn’t work.13
The attraction to complementary medicine often reflects patients’ preferences for a holistic approach to health, says Dr. Ahn, or it may emanate from traditions carried with them from their country of origin. “Once you do understand their reasons for using CAM, then the patient-physician relationship can be significantly strengthened,” he says. With nearly two-thirds of Americans using some form of CAM, hospitalists need to engage in this dialogue.
Dr. Rakel agrees understanding patient culture is vital to uncovering useful information. “Most clinicians would agree that if we can match a therapy to the patient culture and belief system, we are more likely to get buy-in from the patient,” he says.
Dr. Mehta also is a clinical instructor of medicine at Harvard Medical School. He teaches his residents to educate themselves about credentialing, certification, and licensure of complementary providers. He also asks them to maintain an open mind. He says the most important preparation for hospitalists right now is to help educate their patients to be more proactive in their own healthcare. “An engaged patient,” he says, “is better than a disengaged patient.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Deng G, Cassileth BR, Yeung KS. Complementary therapies for cancer-related symptoms. J Support Oncol. 2004;2(5):419-426.
- Kahn ST, Johnstone PA. Management of xerostomia related to radiotherapy for head and neck cancer. Oncology. 2005;19(14):1827-1832.
- Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;27(343):1-19.
- Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280(18):1569-1575.
- Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington, D.C: National Academies Press; 2005.
- Ananth S. 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals. Health Forum LLC. 2008.
- Bent S, Kane C, Shinohara K, et al. Saw palmetto for benign prostatic hyperplasia. N Engl J Med. 2006;354(6):557-566.
- Bauer BA. The herbal hospitalist. The Hospitalist. 2006;10(2);16-17.
- Ananth S. Applying integrative healthcare. Explore. 2009;5(2):119-120.
- Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246-52
- Bassie KL, Witmer DR, Pinto B, Bush C, Clark J, Deffenbaugh J Jr. National survey of dietary supplement policies in acute care facilities. Am J Health Syst Pharm. 2006;63(1):65-70.
- Gardiner P, Phillips RS, Kemper KJ, Legedza A, Henlon S, Woolf AD. Dietary supplements: inpatient policies in US children’s hospitals. Pediatrics. 2008;121(4):e775-781.
- Blendon RJ, DesRoches CM, Benson JM, Brodie M, Altman DE. Americans’ views on the use and regulation of dietary supplements. Arch Intern Med. 2001;161(6):805-810.
Top Image Source: TETRA IMAGES
Despite intravenous medication, a young boy in status epilepticus had the pediatric ICU team at the University of Wisconsin School of Medicine and Public Health in Madison stumped. The team called for a consult with the Integrative Medicine Program, which works with licensed acupuncturists and has been affiliated with the department of family medicine since 2001. Acupuncture’s efficacy in this setting has not been validated, but it has been shown to ease chemotherapy-induced nausea and vomiting, as well as radiation-induced xerostomia.1,2
Following several treatments by a licensed acupuncturist and continued conventional care, the boy’s seizures subsided and he was transitioned to the medical floor. Did the acupuncture contribute to bringing the seizures under control? “I can’t say that it was the acupuncture—it was probably a function of all the therapies working together,” says David P. Rakel, MD, assistant professor and director of UW’s Integrative Medicine Program.
The UW case illustrates both current trends and the constant conundrum that surrounds hospital-based complementary medicine: Complementary and alternative medicine’s use is increasing in some U.S. hospitals, yet the existing research evidence for the efficacy of its multiple modalities is decidedly mixed.
Even if your hospital does not offer complementary and alternative medicine (CAM), your patients are using CAM at ever-increasing rates. In 1993, 34% of Americans reported using some type of CAM (e.g., supplements, massage therapy, prayer, and so on). That number has almost doubled to 62%.3 Americans spend $47 billion a year—of their own money—for CAM therapies, chiropractors, acupuncturists, and massage therapists. And older patients with chronic conditions—the kind of patient hospitalists are most familiar with—tend to try CAM more than younger patients.4
These trends can directly affect hospitalists’ treatment decisions, but they also play a part in how you establish communication and trust with your patients, and how you keep your patients safe from adverse drug interactions. According to the National Academy of Sciences, in order to effectively counsel patients and ensure high-quality comprehensive care, conventional professionals need more CAM-related education.5

—Suzanne Bertisch, MD, MPH, fellow, Harvard Medical School’s Osher Research Center
What Trends Show
In 2007, according to the American Hospital Association, 20.8% of community hospitals offered some type of care or treatment not based on traditional Western allopathic medicine. That’s up from 8.6% of reporting hospitals that offered those services in 1998.
The 1990s saw rapid growth of integrative medicine centers at major research institutions, and the majority of U.S. cancer centers now offer some form of complementary therapy, says Barrie R. Cassileth, MS, PhD, the Laurance S. Rockefeller Chair in Integrative Medicine and chief of the Integrative Medicine Service at Memorial Sloan-Kettering Cancer Center in New York City.
The 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals reported that complementary programs are more common in urban rather than rural hospitals; services vary by hospital size (see Figure 2, above); and the top six modalities offered on an inpatient basis are pet therapy, massage therapy, music/art therapy, guided imagery, acupuncture, and reiki (see “Glossary of Complementary Terms,” above). Eighty-four percent of hospitals offer complementary services due to patient demand, the survey showed.
Joseph Ming-Wah Li, MD, FHM, SHM board member and assistant professor of medicine at Harvard Medical School and director of the hospital medicine program and associate chief of the division of general medicine and primary care at Beth Israel Deaconess Medical Center in Boston, doesn’t see a problem with modalities that can make his patients feel better. Patients at his hospital have access to pet therapy, massage, and acupuncture. “I don’t think these modalities hurt our patients, and there is very little downside, except for potential cost,” says Dr. Li, an SHM board member. “What’s not clear is whether these therapies work or not.”
What’s in a Name?
Numerous therapies and modalities crowd under the CAM umbrella, but most experts classify “complementary” modalities as those used in conjunction with conventional medicine to mitigate symptoms of disease or treatment, whereas “alternative” connotes therapies claiming to treat or cure the underlying disease. Some harmful, dangerous, and dishonest practices fall into the “alternative” category, such as Hulda Clark’s “Zapper” device, which was promoted as a cure for liver flukes, something she says cause everything from diabetes to heart disease. (For more on questionable practices, visit www.quackwatch.com or the National Council Against Health Fraud’s Web site at www.ncahf.org.)
The National Institutes of Health’s National Center for Complementary and Alternative Medicine (NCCAM) defines CAM as a group of “diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.” Dr. Cassileth says the conflation of “complementary and alternative” into one neat acronym—CAM—causes confusion among patients and medical professionals. NCCAM will be changing its name soon, she says, to the National Center for Integrative Medicine, emphasizing the use of adjunctive modalities along with conventional medical treatments.
Hospitalist Suzanne Bertisch, MD, MPH, recently completed a research fellowship at Harvard Medical School’s Osher Research Center. She explains that integrative medicine uses a macro model of health, claiming a middle ground between the traditional, allopathic model of treating disease.
All Kinds of Evidence
Twenty years of complementary medicine research has yielded some information about safety—namely, what works and what doesn’t. For example, saw palmetto has not panned out as an effective treatment for benign prostatic hyperplasia; St. John’s wort, useful for mild depression, interferes with many medications, including cyclosporine and warfarin, and should be avoided at least five days prior to surgery.7,8
Since NCCAM’s inception in October 1998, its research portfolio has stirred debate in the scientific community. Part of the disagreement stems from the difficulty of fitting multidimensional interventions, some of which are provider-dependent (e.g., massage or acupuncture), into the gold standard of the randomized, double-blind, placebo-controlled trial, explains Darshan Mehta, MD, MPH, associate director of medical education at the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital in Boston. The manner in which the effectiveness of integrative techniques is assessed requires a higher sophistication of systems research, Dr. Mehta says.
“The way we construe evidence needs to change,” she adds.
Likely to Expand
Most private health plans do not cover complementary services, although Medicare and numerous insurance plans will reimburse treatment in conjunction with physical therapy (e.g., massage) in the outpatient setting. Twenty-three states cover chiropractic care under Medicaid, and Medicare has begun to assess the cost-effectiveness of including acupuncture—especially for postoperative and chemotherapy-associated nausea and vomiting—in its benefits package.9 Other modalities, ranging from aromatherapy to guided imagery training, are paid for largely out-of-pocket.10
Dr. Rakel notes that the delivery of integrative medicine services at UW entails conversations with patients about out-of-pocket payments. “It can pose a barrier to the clinician-patient relationship if you give them acupuncture to help with their chemotherapy-induced nausea and then ask for their credit card,” he says.
Hospitalist Preparation
Most complementary therapies are currently offered on an outpatient basis. Because of this trend, and because they deal with acute conditions, hospitalists are less likely to be involved with complementary or integrative medicine services, says Beth Israel Deaconess Medical Center hospitalist Andrew C. Ahn, MD, MPH. But that’s not to say complementary medicine is something hospitalists should ignore; patients arrive at the hospital with CAM regimens in tow. It’s the No. 1 reason, Dr. Ahn says, hospitalists should be knowledgeable and exposed to CAM therapies.
Physicians must understand patient patterns and preferences regarding allopathic and complementary medicine, says Sita Ananth, MHA, director of knowledge services and optimal healing environments at the Samueli Institute in Alexandria, Va., and author of the 2007 AHA report. She points to a 2006 survey conducted by AARP and NCCAM that found almost 70% of respondents did not tell their physicians about their complementary medicine approaches. These patients are within the age range most likely to be cared for by hospitalists, and failure to communicate about complementary treatment, such as supplemental vitamin use, could lead to safety issues. Moreover, without complete disclosure, the patient-physician relationship might not be as open as possible, Dr. Ananth says.
Many acute-care hospitalists do not have formal dietary supplement policies, and less than half of U.S. children’s hospitals require documentation of a check for drug or dietary supplement interaction.11,12 As a safety issue, it is always incumbent on hospitalists, says Dr. Li, to ask about any supplements or therapies patients are trying on their own as part of the history and physical examination. The policy at Memorial Sloan-Kettering Cancer Center, Dr. Cassileth says, is that patients on chemotherapy or who are undergoing radiation or facing surgery must avoid herbal dietary supplements.
Beyond Safety
Dr. Bertisch advises hospitalists to pose questions about complementary therapies in an open manner, avoiding antagonistic discussions. “Even when I disagree, I try to guide them to issues about safety and nonsafety, and coax in my concerns,” she says. “The most challenging part about complementary medicine is that patients’ beliefs in these therapies may be so strong that even if the doctor says it won’t work, that will not necessarily change that belief.” A 2001 study in the Archives of Internal Medicine revealed that 70% of respondents would continue to take supplements even if a major study or their physician told them they didn’t work.13
The attraction to complementary medicine often reflects patients’ preferences for a holistic approach to health, says Dr. Ahn, or it may emanate from traditions carried with them from their country of origin. “Once you do understand their reasons for using CAM, then the patient-physician relationship can be significantly strengthened,” he says. With nearly two-thirds of Americans using some form of CAM, hospitalists need to engage in this dialogue.
Dr. Rakel agrees understanding patient culture is vital to uncovering useful information. “Most clinicians would agree that if we can match a therapy to the patient culture and belief system, we are more likely to get buy-in from the patient,” he says.
Dr. Mehta also is a clinical instructor of medicine at Harvard Medical School. He teaches his residents to educate themselves about credentialing, certification, and licensure of complementary providers. He also asks them to maintain an open mind. He says the most important preparation for hospitalists right now is to help educate their patients to be more proactive in their own healthcare. “An engaged patient,” he says, “is better than a disengaged patient.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Deng G, Cassileth BR, Yeung KS. Complementary therapies for cancer-related symptoms. J Support Oncol. 2004;2(5):419-426.
- Kahn ST, Johnstone PA. Management of xerostomia related to radiotherapy for head and neck cancer. Oncology. 2005;19(14):1827-1832.
- Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;27(343):1-19.
- Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280(18):1569-1575.
- Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington, D.C: National Academies Press; 2005.
- Ananth S. 2007 Health Forum/AHA Complementary and Alternative Medicine Survey of Hospitals. Health Forum LLC. 2008.
- Bent S, Kane C, Shinohara K, et al. Saw palmetto for benign prostatic hyperplasia. N Engl J Med. 2006;354(6):557-566.
- Bauer BA. The herbal hospitalist. The Hospitalist. 2006;10(2);16-17.
- Ananth S. Applying integrative healthcare. Explore. 2009;5(2):119-120.
- Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246-52
- Bassie KL, Witmer DR, Pinto B, Bush C, Clark J, Deffenbaugh J Jr. National survey of dietary supplement policies in acute care facilities. Am J Health Syst Pharm. 2006;63(1):65-70.
- Gardiner P, Phillips RS, Kemper KJ, Legedza A, Henlon S, Woolf AD. Dietary supplements: inpatient policies in US children’s hospitals. Pediatrics. 2008;121(4):e775-781.
- Blendon RJ, DesRoches CM, Benson JM, Brodie M, Altman DE. Americans’ views on the use and regulation of dietary supplements. Arch Intern Med. 2001;161(6):805-810.
Top Image Source: TETRA IMAGES
Alpesh Amin: HM's History maker
Dedication to hard work, a passion for improving health outcomes and medical curricula, a background in business administration, and a knack for team-building have catapulted Alpesh Amin, MD, MBA, FACP, to the forefront of change at the University of California at Irvine Health Affairs, comprised of the UC Irvine Medical Center and School of Medicine. Those skill sets and determination have landed Dr. Amin an HM first: appointment as interim chair of an academic Department of Medicine.
Dr. Amin’s new role—he supervises 11 divisions and more than 200 faculty—means he’s responsible for the department’s budget and administration. He also is charged with advancing the department’s clinical, teaching, and research missions, demonstrating that it’s possible for hospitalists to rise through the department ranks through an HM track. And that, says Scott Flanders, SHM’s president-elect and associate professor of medicine and director of the HM program at the University of Michigan Health System in Ann Arbor, “bodes well for the future of academic hospitalists at many institutions across the country.”
Traditionally, lofty hospital appointments have gone to academics with a background in biomedical and basic science research. But as academic and teaching hospitals focus more and more on quality issues and improved performance, hospitalists are positioned to advance into department leadership positions.
Dr. Amin’s appointment could signal the first of many opportunities for academic hospitalists, according to Joseph Ming-Wah Li, MD, assistant professor of medicine at Harvard Medical School and director of the HM program at Beth Israel Deaconess Medical Center in Boston. Dr. Li, who served with Dr. Amin on SHM’s Board of Directors, was not surprised when Alpesh was named the first hospitalist to chair a department of medicine. “He is a very gregarious person, he’s bright, and he’s logical in his thinking,” Dr. Li says.
Career Foundation
Dr. Amin credits his family with instilling in him strong values and dedication to his work. Born in Baroda, India, he emigrated to the U.S. before his first birthday; he graduated from Northgate High School in Walnut Creek, Calif., in 1985, and from UC San Diego with a degree in bioengineering in 1989. He obtained his MD in 1994 from Northwestern University’s Feinberg School of Medicine in Chicago.
During his internship and residency at UC Irvine, Dr. Amin pondered the possibilities of a subspecialty within internal medicine. He opted to follow his interests in medical education and healthcare outcomes and research. The HM field intrigued him, he says, “because there was an opportunity to improve on systems and patient-care delivery.” Numerous mentors along the way encouraged his interests in curriculum development and design, quality improvement, and developing delivery models for patient care.
Trendsetter
As a medical resident, Dr. Amin demonstrated a desire to become a leader and change agent. “He was truly an outstanding resident, and then he joined the faculty and did spectacularly in organizing the hospitalist program, which has become very successful,” recalls Nosratola D. Vaziri, MD, chief of the division of nephrology and hypertension at UC Irvine’s School of Medicine. Dr. Amin founded the UC Irvine hospitalist program in 1998. At the same time, he acquired his MBA in healthcare administration, thus rounding out an already impressive skill set. “The MBA has been a valuable tool,” says Dr. Amin, “because I learned—among other skills—leadership, strategic planning, developing business plans, and improving on operations.”
He has applied those techniques throughout his career, serving in various leadership roles at his institution, including medicine clerkship director, associate program director for the internal medicine residency program, vice chair for clinical affairs and quality assurance, and chief of the division of general internal medicine.
By developing and nurturing the UC Irvine hospitalist program, Dr. Amin has exhibited a deep commitment to the core missions of hospital medicine. “Our multidisciplinary program has nine different specialties managed under one program,” he notes. He has structured the program in such a way that members hold dual appointments in the HM program and their individual departments or divisions, thus creating a bridge between the HM program and other departments.
“We have an integrated group that is working together for the focus of advancement in the hospital setting, in terms of clinical care, teaching, team-building, quality and systems improvement. As a result, we’ve had great outcomes in terms of length of stay, quality, and core measures,” Dr. Amin says. “I’ve been fortunate to work with a team of hospitalist faculty who are spectacular and collectively deserve kudos for the success of our group.”
Dr. Amin has shared his passion for quality improvement and curriculum development with all of hospital medicine. As chair of SHM’s education committee, he pushed for the first education summit in 2001, securing support to form a core-curriculum task force. Four years later, Dr. Amin and a small group of industry leaders published “Core Competencies in Hospital Medicine” in the Journal of Hospital Medicine (www.hospitalmedicine.org/corecomp).
“Dr. Amin has really set the trend [for improved hospital performance], not only here for the hospitalist program, but nationwide,” says David N. Bailey, MD, dean and vice chancellor for UC Irvine Health Affairs.
Bucking Tradition
Hospitalists have been advancing into leadership positions in the private sector for many years. It’s been a slower ascent in the academic medical center setting.
“Until recently, it would not have been possible to ascend to the level of chair at most academic centers unless your background was in biomedical and basic science research,” says Robert Wachter, MD, professor and chief of the division of HM at the University of California San Francisco, a former SHM president and author of the blog Wachter’s World (www.wachtersworld .com). “Quality, patient safety, and systems improvement were not considered to be legitimate enough academic work to garner the necessary credibility. I think that’s changing.”
Jeffrey Wiese, MD, FACP, professor of medicine and associate dean for graduate medical education at Tulane University Health Sciences Center in New Orleans and an SHM board member, believes Dr. Amin’s interim appointment “speaks in broad strokes to the new skill set—that is, financial and organizational abilities—that are increasingly becoming valued by academic medicine.” Agendas of patient safety, quality, and delivery of efficient, cost-effective, and safe healthcare are gaining parity, Dr. Wiese says, with academic research agendas. “For one to supercede the other is not a good thing, but for the two to be in balance, I think, is a very good thing,” he says.
“Renaissance Physician”
Dr. Bailey appointed Dr. Amin to what he describes as a “long-term” interim post last June. To make his decision, Dr. Bailey consulted with 11 division chiefs, and Dr. Amin emerged as the leading candidate. “Alpesh does it all, from clinical research to leading a department to running an outstanding hospitalist service,” Dr. Bailey says. “He’s really a renaissance physician.”
The promotion coincides with another of Dr. Amin’s recent accomplishments: He received the Laureate Award for the California Southern Region 2 of the American College of Physicians.
Ever energetic, Dr. Amin is not resting on his laurels. “I’m looking forward to helping the department continue to be a flagship within the UC Irvine School of Medicine,” he says. “This is a challenging and positive opportunity to balance systems-based practice, the business of medicine, and the science of medicine.”
Dr. Amin thinks his appointment signifies the new opportunities open to the growing number of U.S. hospitalists—now more than 28,000 strong and growing every day. “This [appointment] shows that hospitalists can move in the direction of being both academic leaders and healthcare administrative leaders.” TH
Gretchen Henkel is a freelance medical writer based in California.
Dedication to hard work, a passion for improving health outcomes and medical curricula, a background in business administration, and a knack for team-building have catapulted Alpesh Amin, MD, MBA, FACP, to the forefront of change at the University of California at Irvine Health Affairs, comprised of the UC Irvine Medical Center and School of Medicine. Those skill sets and determination have landed Dr. Amin an HM first: appointment as interim chair of an academic Department of Medicine.
Dr. Amin’s new role—he supervises 11 divisions and more than 200 faculty—means he’s responsible for the department’s budget and administration. He also is charged with advancing the department’s clinical, teaching, and research missions, demonstrating that it’s possible for hospitalists to rise through the department ranks through an HM track. And that, says Scott Flanders, SHM’s president-elect and associate professor of medicine and director of the HM program at the University of Michigan Health System in Ann Arbor, “bodes well for the future of academic hospitalists at many institutions across the country.”
Traditionally, lofty hospital appointments have gone to academics with a background in biomedical and basic science research. But as academic and teaching hospitals focus more and more on quality issues and improved performance, hospitalists are positioned to advance into department leadership positions.
Dr. Amin’s appointment could signal the first of many opportunities for academic hospitalists, according to Joseph Ming-Wah Li, MD, assistant professor of medicine at Harvard Medical School and director of the HM program at Beth Israel Deaconess Medical Center in Boston. Dr. Li, who served with Dr. Amin on SHM’s Board of Directors, was not surprised when Alpesh was named the first hospitalist to chair a department of medicine. “He is a very gregarious person, he’s bright, and he’s logical in his thinking,” Dr. Li says.
Career Foundation
Dr. Amin credits his family with instilling in him strong values and dedication to his work. Born in Baroda, India, he emigrated to the U.S. before his first birthday; he graduated from Northgate High School in Walnut Creek, Calif., in 1985, and from UC San Diego with a degree in bioengineering in 1989. He obtained his MD in 1994 from Northwestern University’s Feinberg School of Medicine in Chicago.
During his internship and residency at UC Irvine, Dr. Amin pondered the possibilities of a subspecialty within internal medicine. He opted to follow his interests in medical education and healthcare outcomes and research. The HM field intrigued him, he says, “because there was an opportunity to improve on systems and patient-care delivery.” Numerous mentors along the way encouraged his interests in curriculum development and design, quality improvement, and developing delivery models for patient care.
Trendsetter
As a medical resident, Dr. Amin demonstrated a desire to become a leader and change agent. “He was truly an outstanding resident, and then he joined the faculty and did spectacularly in organizing the hospitalist program, which has become very successful,” recalls Nosratola D. Vaziri, MD, chief of the division of nephrology and hypertension at UC Irvine’s School of Medicine. Dr. Amin founded the UC Irvine hospitalist program in 1998. At the same time, he acquired his MBA in healthcare administration, thus rounding out an already impressive skill set. “The MBA has been a valuable tool,” says Dr. Amin, “because I learned—among other skills—leadership, strategic planning, developing business plans, and improving on operations.”
He has applied those techniques throughout his career, serving in various leadership roles at his institution, including medicine clerkship director, associate program director for the internal medicine residency program, vice chair for clinical affairs and quality assurance, and chief of the division of general internal medicine.
By developing and nurturing the UC Irvine hospitalist program, Dr. Amin has exhibited a deep commitment to the core missions of hospital medicine. “Our multidisciplinary program has nine different specialties managed under one program,” he notes. He has structured the program in such a way that members hold dual appointments in the HM program and their individual departments or divisions, thus creating a bridge between the HM program and other departments.
“We have an integrated group that is working together for the focus of advancement in the hospital setting, in terms of clinical care, teaching, team-building, quality and systems improvement. As a result, we’ve had great outcomes in terms of length of stay, quality, and core measures,” Dr. Amin says. “I’ve been fortunate to work with a team of hospitalist faculty who are spectacular and collectively deserve kudos for the success of our group.”
Dr. Amin has shared his passion for quality improvement and curriculum development with all of hospital medicine. As chair of SHM’s education committee, he pushed for the first education summit in 2001, securing support to form a core-curriculum task force. Four years later, Dr. Amin and a small group of industry leaders published “Core Competencies in Hospital Medicine” in the Journal of Hospital Medicine (www.hospitalmedicine.org/corecomp).
“Dr. Amin has really set the trend [for improved hospital performance], not only here for the hospitalist program, but nationwide,” says David N. Bailey, MD, dean and vice chancellor for UC Irvine Health Affairs.
Bucking Tradition
Hospitalists have been advancing into leadership positions in the private sector for many years. It’s been a slower ascent in the academic medical center setting.
“Until recently, it would not have been possible to ascend to the level of chair at most academic centers unless your background was in biomedical and basic science research,” says Robert Wachter, MD, professor and chief of the division of HM at the University of California San Francisco, a former SHM president and author of the blog Wachter’s World (www.wachtersworld .com). “Quality, patient safety, and systems improvement were not considered to be legitimate enough academic work to garner the necessary credibility. I think that’s changing.”
Jeffrey Wiese, MD, FACP, professor of medicine and associate dean for graduate medical education at Tulane University Health Sciences Center in New Orleans and an SHM board member, believes Dr. Amin’s interim appointment “speaks in broad strokes to the new skill set—that is, financial and organizational abilities—that are increasingly becoming valued by academic medicine.” Agendas of patient safety, quality, and delivery of efficient, cost-effective, and safe healthcare are gaining parity, Dr. Wiese says, with academic research agendas. “For one to supercede the other is not a good thing, but for the two to be in balance, I think, is a very good thing,” he says.
“Renaissance Physician”
Dr. Bailey appointed Dr. Amin to what he describes as a “long-term” interim post last June. To make his decision, Dr. Bailey consulted with 11 division chiefs, and Dr. Amin emerged as the leading candidate. “Alpesh does it all, from clinical research to leading a department to running an outstanding hospitalist service,” Dr. Bailey says. “He’s really a renaissance physician.”
The promotion coincides with another of Dr. Amin’s recent accomplishments: He received the Laureate Award for the California Southern Region 2 of the American College of Physicians.
Ever energetic, Dr. Amin is not resting on his laurels. “I’m looking forward to helping the department continue to be a flagship within the UC Irvine School of Medicine,” he says. “This is a challenging and positive opportunity to balance systems-based practice, the business of medicine, and the science of medicine.”
Dr. Amin thinks his appointment signifies the new opportunities open to the growing number of U.S. hospitalists—now more than 28,000 strong and growing every day. “This [appointment] shows that hospitalists can move in the direction of being both academic leaders and healthcare administrative leaders.” TH
Gretchen Henkel is a freelance medical writer based in California.
Dedication to hard work, a passion for improving health outcomes and medical curricula, a background in business administration, and a knack for team-building have catapulted Alpesh Amin, MD, MBA, FACP, to the forefront of change at the University of California at Irvine Health Affairs, comprised of the UC Irvine Medical Center and School of Medicine. Those skill sets and determination have landed Dr. Amin an HM first: appointment as interim chair of an academic Department of Medicine.
Dr. Amin’s new role—he supervises 11 divisions and more than 200 faculty—means he’s responsible for the department’s budget and administration. He also is charged with advancing the department’s clinical, teaching, and research missions, demonstrating that it’s possible for hospitalists to rise through the department ranks through an HM track. And that, says Scott Flanders, SHM’s president-elect and associate professor of medicine and director of the HM program at the University of Michigan Health System in Ann Arbor, “bodes well for the future of academic hospitalists at many institutions across the country.”
Traditionally, lofty hospital appointments have gone to academics with a background in biomedical and basic science research. But as academic and teaching hospitals focus more and more on quality issues and improved performance, hospitalists are positioned to advance into department leadership positions.
Dr. Amin’s appointment could signal the first of many opportunities for academic hospitalists, according to Joseph Ming-Wah Li, MD, assistant professor of medicine at Harvard Medical School and director of the HM program at Beth Israel Deaconess Medical Center in Boston. Dr. Li, who served with Dr. Amin on SHM’s Board of Directors, was not surprised when Alpesh was named the first hospitalist to chair a department of medicine. “He is a very gregarious person, he’s bright, and he’s logical in his thinking,” Dr. Li says.
Career Foundation
Dr. Amin credits his family with instilling in him strong values and dedication to his work. Born in Baroda, India, he emigrated to the U.S. before his first birthday; he graduated from Northgate High School in Walnut Creek, Calif., in 1985, and from UC San Diego with a degree in bioengineering in 1989. He obtained his MD in 1994 from Northwestern University’s Feinberg School of Medicine in Chicago.
During his internship and residency at UC Irvine, Dr. Amin pondered the possibilities of a subspecialty within internal medicine. He opted to follow his interests in medical education and healthcare outcomes and research. The HM field intrigued him, he says, “because there was an opportunity to improve on systems and patient-care delivery.” Numerous mentors along the way encouraged his interests in curriculum development and design, quality improvement, and developing delivery models for patient care.
Trendsetter
As a medical resident, Dr. Amin demonstrated a desire to become a leader and change agent. “He was truly an outstanding resident, and then he joined the faculty and did spectacularly in organizing the hospitalist program, which has become very successful,” recalls Nosratola D. Vaziri, MD, chief of the division of nephrology and hypertension at UC Irvine’s School of Medicine. Dr. Amin founded the UC Irvine hospitalist program in 1998. At the same time, he acquired his MBA in healthcare administration, thus rounding out an already impressive skill set. “The MBA has been a valuable tool,” says Dr. Amin, “because I learned—among other skills—leadership, strategic planning, developing business plans, and improving on operations.”
He has applied those techniques throughout his career, serving in various leadership roles at his institution, including medicine clerkship director, associate program director for the internal medicine residency program, vice chair for clinical affairs and quality assurance, and chief of the division of general internal medicine.
By developing and nurturing the UC Irvine hospitalist program, Dr. Amin has exhibited a deep commitment to the core missions of hospital medicine. “Our multidisciplinary program has nine different specialties managed under one program,” he notes. He has structured the program in such a way that members hold dual appointments in the HM program and their individual departments or divisions, thus creating a bridge between the HM program and other departments.
“We have an integrated group that is working together for the focus of advancement in the hospital setting, in terms of clinical care, teaching, team-building, quality and systems improvement. As a result, we’ve had great outcomes in terms of length of stay, quality, and core measures,” Dr. Amin says. “I’ve been fortunate to work with a team of hospitalist faculty who are spectacular and collectively deserve kudos for the success of our group.”
Dr. Amin has shared his passion for quality improvement and curriculum development with all of hospital medicine. As chair of SHM’s education committee, he pushed for the first education summit in 2001, securing support to form a core-curriculum task force. Four years later, Dr. Amin and a small group of industry leaders published “Core Competencies in Hospital Medicine” in the Journal of Hospital Medicine (www.hospitalmedicine.org/corecomp).
“Dr. Amin has really set the trend [for improved hospital performance], not only here for the hospitalist program, but nationwide,” says David N. Bailey, MD, dean and vice chancellor for UC Irvine Health Affairs.
Bucking Tradition
Hospitalists have been advancing into leadership positions in the private sector for many years. It’s been a slower ascent in the academic medical center setting.
“Until recently, it would not have been possible to ascend to the level of chair at most academic centers unless your background was in biomedical and basic science research,” says Robert Wachter, MD, professor and chief of the division of HM at the University of California San Francisco, a former SHM president and author of the blog Wachter’s World (www.wachtersworld .com). “Quality, patient safety, and systems improvement were not considered to be legitimate enough academic work to garner the necessary credibility. I think that’s changing.”
Jeffrey Wiese, MD, FACP, professor of medicine and associate dean for graduate medical education at Tulane University Health Sciences Center in New Orleans and an SHM board member, believes Dr. Amin’s interim appointment “speaks in broad strokes to the new skill set—that is, financial and organizational abilities—that are increasingly becoming valued by academic medicine.” Agendas of patient safety, quality, and delivery of efficient, cost-effective, and safe healthcare are gaining parity, Dr. Wiese says, with academic research agendas. “For one to supercede the other is not a good thing, but for the two to be in balance, I think, is a very good thing,” he says.
“Renaissance Physician”
Dr. Bailey appointed Dr. Amin to what he describes as a “long-term” interim post last June. To make his decision, Dr. Bailey consulted with 11 division chiefs, and Dr. Amin emerged as the leading candidate. “Alpesh does it all, from clinical research to leading a department to running an outstanding hospitalist service,” Dr. Bailey says. “He’s really a renaissance physician.”
The promotion coincides with another of Dr. Amin’s recent accomplishments: He received the Laureate Award for the California Southern Region 2 of the American College of Physicians.
Ever energetic, Dr. Amin is not resting on his laurels. “I’m looking forward to helping the department continue to be a flagship within the UC Irvine School of Medicine,” he says. “This is a challenging and positive opportunity to balance systems-based practice, the business of medicine, and the science of medicine.”
Dr. Amin thinks his appointment signifies the new opportunities open to the growing number of U.S. hospitalists—now more than 28,000 strong and growing every day. “This [appointment] shows that hospitalists can move in the direction of being both academic leaders and healthcare administrative leaders.” TH
Gretchen Henkel is a freelance medical writer based in California.
Ethical Gray Zones
A distraught daughter demands you place a feeding tube in her father, your patient, who has not eaten in three days. The patient’s advanced dementia, anti-coagulation therapy, and other co-morbidities suggest such a move may not be in his best interest. How do you respond?
Ethical dilemmas rarely are simple or clear cut. They often involve revisiting the same issues time and again. That’s where an ethics committee comes in, says Maj. Heather Cereste, MD, U.S. Air Force, co-director of the geriatric medicine service and chair of the bioethics committee at Wilford Hall Medical Center, Lackland Air Force Base, San Antonio, Texas.
Ethics committees provide oversight and assist the institution in creating policies to guide staff through ethical dilemmas, Dr. Cereste says.
“Our job at the ethics committee—and we try to make this very clear—is not to solve people’s problems or dictate care,” she says. “Our job is to provide a perspective and a way of thinking about an issue to better equip people to get through it.”
Though it seems straightforward, the notion is fraught with myriad complications.
A Range of Issues
Pediatric Hospitalist Sheldon Berkowitz, MD, medical director, Minneapolis Children’s Clinic (MCC), Children’s Hospital and Clinics of Minnesota, has been involved with ethics issues for 24 years. He currently is the ethics committee chair at MCC. In his experience, he says “most [ethics committee] consults come from intensive care settings, relating to life-and-death issues.”
The issues become trickier for patients from cultures with specific traditions and beliefs surrounding death. Anita Gandhy, MD, a hospitalist board certified in hospice and palliative care, works at Saint Francis Memorial Hospital in San Francisco. The family of a patient she was treating wanted to continue care for its loved one despite the fact the patient was dying. “I later found out that a baby had recently been born into the family,” Dr. Gandhy says. “In the Chinese culture, if someone dies around the time that a baby is born, that spirit will follow the baby. So the family’s desire to prolong care was consistent with their cultural beliefs.”
Ethical dilemmas surface in a variety of situations—not just related to end-of-life treatment—and between a variety of parties: patient surrogates and medical staff, members of the care team, patients and family, or among family members themselves. Physicians will face many types of conflicts:
- Who makes decisions regarding the rights and preferences of unidentified patients without designated surrogates or advance directives;
- Whether to allow medical training on the newly dead;
- Whether to agree to requests for exorbitant or unorthodox treatments;
- Whether family members can ably deliver home care for a patient who is being discharged; or
- Whether to grant sterilization requests from families of adolescent children with Down syndrome.1
Underutilized Service?
With such a wide swath of potential ethical dilemmas, it would seem intuitive for physicians to use an ethics committee when one is available. Yet, a 2005 survey of 600 U.S. hospitals by The National Center for Ethics in Health Care tells a different story. The survey found 81% of the general hospitals responding to the survey had ethics consultation services, and 100% of hospitals with more than 400 beds had such services. However, the staff sought the ethics consultation services a median of only three times in the year prior to the survey.2
Hospitalist Olivia Wendy Zachary, MD, has worked for two years at California Pacific Medical Center in San Francisco. In that time, she has requested a total of four ethics consults. One recent consultation helped her determine the source of durable power of attorney for a patient who was a prisoner and who, because he was a felon and a ward of the state prison system, could not make his own healthcare decisions.
There are other situations, however, when Dr. Zachary refrains from asking for an ethics consult. For example, as a geriatrician conversant in the potential adverse outcomes of tube feeding patients with dementia, she makes the judgment calls in these instances.
“I feel very comfortable giving family members the data, in a way that they can understand, on the conflicts of tube feeding in demented patients,” Dr. Zachary says. “The role of the ethics committee, in my opinion, should be to answer conflicts for which you do not have the answers. … If that’s beyond your expertise—if you don’t know the studies and aren’t a geriatrician—then in that case, it might be appropriate.”
In other words, don’t call the ethics committee because you don’t have the time to clearly communicate with the family.
Call on the Committee
Medical ethics dilemmas aren’t always as straightforward as knowing the possible negative consequences of placing a feeding tube in a dementia patient. So when should you call on the ethics committee? Physicians at St. Joseph’s Hospital in St. Paul, Minn., fill out an ethics consultation request form to help the hospital determine the need for the consult.
Robert C. Moravec, MD, medical director, director of hospital medicine, and chair of the ethics committee at St. Joseph’s, says the form was created to prevent physicians from requesting consults prematurely, before they have attempted a family care conference or fully understand the issue at hand. For example, providers occasionally request ethics consults when the problem really is poor communication.
“Sometimes, when our ethics committee is consulted, we discover that there is so much emotional energy going into the issue that the participants are simply not communicating,” Dr. Cereste says. “We can help them identify that.”
Other times, the issue lies in a conflict between the physician and the patient’s family. The physician may want to move from aggressive care to a pain and palliative care approach. The family, of course, wants to stay the aggressive course. It’s not the committee’s job to resolve this conflict, Dr. Berkowitz cautions. “The role of the ethics committee should be helping to identify, delineate, and resolve ethics issues,” he explains. “The committee should not be there simply to help the attending physician accomplish their goals.”
Committee Credibility
Even if physicians know when to ask for help from an ethics committee, they only will do so if they trust the enterprise, Dr. Moravec says. Using a multidisciplinary approach has worked at St. Joseph’s, where the ethics committee is comprised of nursing clinical directors, physicians, social workers, chaplains, hospice and palliative care directors, and even dietitians, who meet monthly.
When the St. Joseph’s ethics committee convenes, members fill out a multi-page record for each patient. In addition to a summary of the patient’s medical history, goals of treatment, preferences, and expected quality of life with proposed treatments (or withdrawal thereof), the record documents the committee’s conclusions, Dr. Moravec says. One copy of the document gets incorporated into the patient’s chart, one is sent to hospital administration, and a third gets channeled to the hospital system’s organization-wide ethics committee. This reporting through the medical staff fosters physician buy-in, Dr. Moravec says.
Physicians are less likely to use the consultation services if they feel the ethics committee doesn’t have teeth, says Rachel George, MD, MBA, hospitalist at Aurora St. Luke’s Hospital in Milwaukee, and regional director of five west coast hospitalist programs for Cogent Healthcare, Inc.
The same is true for one Southern California hospitalist who preferred to remain anonymous. “I rarely call for an ethics consult because they’re rarely helpful,” she says. “Generally, the issues we bring to the ethics committee are those where the family is pushing us to provide care we think is futile, and the ethics committee really doesn’t make a decision. You don’t get the backup you need, and you end up very frustrated.”
Sometimes, the California hospitalist continues, the family needs permission from the hospital to halt futile care. Without a durable power of attorney, the care team may find itself bowing to the wishes of one family member—the outlier—who insists the patient be kept alive with aggressive measures. The inpatient palliative care team often fills the ethics gap, helping the medical team discuss end-of-life issues, goals, and desires with the family. Hospitalists, she says, sometimes need an authoritative body to say, “It is no longer ethical to do this to this patient.”
“Having a hospital committee say it’s OK to withdraw a feeding tube or stop dialysis gives a comfort level to physicians,” Dr. Moravec says, “especially if the committee involves clergy, as well as administration. That is powerful support for that doctor.”
Med Students & Residents
The key to making ethics committees more effectively and widely used is education, Dr. George says. “We need to be educating our medical students and residents a lot more aggressively than we are right now,” she asserts. “How to talk with families about end-of-life issues, what is appropriate or inappropriate care, how should you be using your ethics committees—none of that is taught.”
At Children’s Hospital and Clinics, Dr. Berkowitz meets with residents and medical students every six weeks to discuss cases with ethical dilemmas. He says house staffers have little background or experience with ethics. The American Medical Association’s Liaison Committee on Medical Education 2007-2008 survey of 126 U.S. medical colleges found medical ethics was included in one required course at all 126 colleges, and was an elective course in 61. For some perspective, a course in end-of-life care was required at 124 schools and was an elective at 69. A course in palliative care was required at 120 schools, and was an elective in 60.3
Dr. Berkowitz agrees outreach is one solution. “The longer you have an ethics committee available and doing consultations in an institution, the more you expand the knowledge about how to handle problems,” he says. “People who may have previously requested an ethics consult may now have the skills and ability to handle these issues on their own, without needing to call a consult.”
Dr. Gandhy, of Saint Francis Memorial, believes such additional knowledge helps her focus on a patient’s family, not her own plan. “If the family is not ready to withdraw the care, I realize that forcing my agenda on them can also cause suffering,” she says. “When I change my focus to ask, ‘What is going to help the patient and the family?’ sometimes I don’t even need the ethics committee, because I am then able to address the family’s concerns.”
And that’s when everybody gains. TH
Gretchen Henkel is a freelance writer based in California and a frequent contributor to The Hospitalist.
References
1. Snyder L, Leffler C;, for the Ethics and Human Rights Committee, American College of Physicians. Ethics Manual. 5th ed.,2005.
2. Fox E, Myers S, Pearlman RA. Ethics consultation in United States hospitals: a national survey. Am J Bioeth. 2007 Feb;7(2):13-25.
3. Barzansky B, Etze SI. 2007-2008 annual medical school questionnaire part II. JAMA 2008;300(10):1221.
A distraught daughter demands you place a feeding tube in her father, your patient, who has not eaten in three days. The patient’s advanced dementia, anti-coagulation therapy, and other co-morbidities suggest such a move may not be in his best interest. How do you respond?
Ethical dilemmas rarely are simple or clear cut. They often involve revisiting the same issues time and again. That’s where an ethics committee comes in, says Maj. Heather Cereste, MD, U.S. Air Force, co-director of the geriatric medicine service and chair of the bioethics committee at Wilford Hall Medical Center, Lackland Air Force Base, San Antonio, Texas.
Ethics committees provide oversight and assist the institution in creating policies to guide staff through ethical dilemmas, Dr. Cereste says.
“Our job at the ethics committee—and we try to make this very clear—is not to solve people’s problems or dictate care,” she says. “Our job is to provide a perspective and a way of thinking about an issue to better equip people to get through it.”
Though it seems straightforward, the notion is fraught with myriad complications.
A Range of Issues
Pediatric Hospitalist Sheldon Berkowitz, MD, medical director, Minneapolis Children’s Clinic (MCC), Children’s Hospital and Clinics of Minnesota, has been involved with ethics issues for 24 years. He currently is the ethics committee chair at MCC. In his experience, he says “most [ethics committee] consults come from intensive care settings, relating to life-and-death issues.”
The issues become trickier for patients from cultures with specific traditions and beliefs surrounding death. Anita Gandhy, MD, a hospitalist board certified in hospice and palliative care, works at Saint Francis Memorial Hospital in San Francisco. The family of a patient she was treating wanted to continue care for its loved one despite the fact the patient was dying. “I later found out that a baby had recently been born into the family,” Dr. Gandhy says. “In the Chinese culture, if someone dies around the time that a baby is born, that spirit will follow the baby. So the family’s desire to prolong care was consistent with their cultural beliefs.”
Ethical dilemmas surface in a variety of situations—not just related to end-of-life treatment—and between a variety of parties: patient surrogates and medical staff, members of the care team, patients and family, or among family members themselves. Physicians will face many types of conflicts:
- Who makes decisions regarding the rights and preferences of unidentified patients without designated surrogates or advance directives;
- Whether to allow medical training on the newly dead;
- Whether to agree to requests for exorbitant or unorthodox treatments;
- Whether family members can ably deliver home care for a patient who is being discharged; or
- Whether to grant sterilization requests from families of adolescent children with Down syndrome.1
Underutilized Service?
With such a wide swath of potential ethical dilemmas, it would seem intuitive for physicians to use an ethics committee when one is available. Yet, a 2005 survey of 600 U.S. hospitals by The National Center for Ethics in Health Care tells a different story. The survey found 81% of the general hospitals responding to the survey had ethics consultation services, and 100% of hospitals with more than 400 beds had such services. However, the staff sought the ethics consultation services a median of only three times in the year prior to the survey.2
Hospitalist Olivia Wendy Zachary, MD, has worked for two years at California Pacific Medical Center in San Francisco. In that time, she has requested a total of four ethics consults. One recent consultation helped her determine the source of durable power of attorney for a patient who was a prisoner and who, because he was a felon and a ward of the state prison system, could not make his own healthcare decisions.
There are other situations, however, when Dr. Zachary refrains from asking for an ethics consult. For example, as a geriatrician conversant in the potential adverse outcomes of tube feeding patients with dementia, she makes the judgment calls in these instances.
“I feel very comfortable giving family members the data, in a way that they can understand, on the conflicts of tube feeding in demented patients,” Dr. Zachary says. “The role of the ethics committee, in my opinion, should be to answer conflicts for which you do not have the answers. … If that’s beyond your expertise—if you don’t know the studies and aren’t a geriatrician—then in that case, it might be appropriate.”
In other words, don’t call the ethics committee because you don’t have the time to clearly communicate with the family.
Call on the Committee
Medical ethics dilemmas aren’t always as straightforward as knowing the possible negative consequences of placing a feeding tube in a dementia patient. So when should you call on the ethics committee? Physicians at St. Joseph’s Hospital in St. Paul, Minn., fill out an ethics consultation request form to help the hospital determine the need for the consult.
Robert C. Moravec, MD, medical director, director of hospital medicine, and chair of the ethics committee at St. Joseph’s, says the form was created to prevent physicians from requesting consults prematurely, before they have attempted a family care conference or fully understand the issue at hand. For example, providers occasionally request ethics consults when the problem really is poor communication.
“Sometimes, when our ethics committee is consulted, we discover that there is so much emotional energy going into the issue that the participants are simply not communicating,” Dr. Cereste says. “We can help them identify that.”
Other times, the issue lies in a conflict between the physician and the patient’s family. The physician may want to move from aggressive care to a pain and palliative care approach. The family, of course, wants to stay the aggressive course. It’s not the committee’s job to resolve this conflict, Dr. Berkowitz cautions. “The role of the ethics committee should be helping to identify, delineate, and resolve ethics issues,” he explains. “The committee should not be there simply to help the attending physician accomplish their goals.”
Committee Credibility
Even if physicians know when to ask for help from an ethics committee, they only will do so if they trust the enterprise, Dr. Moravec says. Using a multidisciplinary approach has worked at St. Joseph’s, where the ethics committee is comprised of nursing clinical directors, physicians, social workers, chaplains, hospice and palliative care directors, and even dietitians, who meet monthly.
When the St. Joseph’s ethics committee convenes, members fill out a multi-page record for each patient. In addition to a summary of the patient’s medical history, goals of treatment, preferences, and expected quality of life with proposed treatments (or withdrawal thereof), the record documents the committee’s conclusions, Dr. Moravec says. One copy of the document gets incorporated into the patient’s chart, one is sent to hospital administration, and a third gets channeled to the hospital system’s organization-wide ethics committee. This reporting through the medical staff fosters physician buy-in, Dr. Moravec says.
Physicians are less likely to use the consultation services if they feel the ethics committee doesn’t have teeth, says Rachel George, MD, MBA, hospitalist at Aurora St. Luke’s Hospital in Milwaukee, and regional director of five west coast hospitalist programs for Cogent Healthcare, Inc.
The same is true for one Southern California hospitalist who preferred to remain anonymous. “I rarely call for an ethics consult because they’re rarely helpful,” she says. “Generally, the issues we bring to the ethics committee are those where the family is pushing us to provide care we think is futile, and the ethics committee really doesn’t make a decision. You don’t get the backup you need, and you end up very frustrated.”
Sometimes, the California hospitalist continues, the family needs permission from the hospital to halt futile care. Without a durable power of attorney, the care team may find itself bowing to the wishes of one family member—the outlier—who insists the patient be kept alive with aggressive measures. The inpatient palliative care team often fills the ethics gap, helping the medical team discuss end-of-life issues, goals, and desires with the family. Hospitalists, she says, sometimes need an authoritative body to say, “It is no longer ethical to do this to this patient.”
“Having a hospital committee say it’s OK to withdraw a feeding tube or stop dialysis gives a comfort level to physicians,” Dr. Moravec says, “especially if the committee involves clergy, as well as administration. That is powerful support for that doctor.”
Med Students & Residents
The key to making ethics committees more effectively and widely used is education, Dr. George says. “We need to be educating our medical students and residents a lot more aggressively than we are right now,” she asserts. “How to talk with families about end-of-life issues, what is appropriate or inappropriate care, how should you be using your ethics committees—none of that is taught.”
At Children’s Hospital and Clinics, Dr. Berkowitz meets with residents and medical students every six weeks to discuss cases with ethical dilemmas. He says house staffers have little background or experience with ethics. The American Medical Association’s Liaison Committee on Medical Education 2007-2008 survey of 126 U.S. medical colleges found medical ethics was included in one required course at all 126 colleges, and was an elective course in 61. For some perspective, a course in end-of-life care was required at 124 schools and was an elective at 69. A course in palliative care was required at 120 schools, and was an elective in 60.3
Dr. Berkowitz agrees outreach is one solution. “The longer you have an ethics committee available and doing consultations in an institution, the more you expand the knowledge about how to handle problems,” he says. “People who may have previously requested an ethics consult may now have the skills and ability to handle these issues on their own, without needing to call a consult.”
Dr. Gandhy, of Saint Francis Memorial, believes such additional knowledge helps her focus on a patient’s family, not her own plan. “If the family is not ready to withdraw the care, I realize that forcing my agenda on them can also cause suffering,” she says. “When I change my focus to ask, ‘What is going to help the patient and the family?’ sometimes I don’t even need the ethics committee, because I am then able to address the family’s concerns.”
And that’s when everybody gains. TH
Gretchen Henkel is a freelance writer based in California and a frequent contributor to The Hospitalist.
References
1. Snyder L, Leffler C;, for the Ethics and Human Rights Committee, American College of Physicians. Ethics Manual. 5th ed.,2005.
2. Fox E, Myers S, Pearlman RA. Ethics consultation in United States hospitals: a national survey. Am J Bioeth. 2007 Feb;7(2):13-25.
3. Barzansky B, Etze SI. 2007-2008 annual medical school questionnaire part II. JAMA 2008;300(10):1221.
A distraught daughter demands you place a feeding tube in her father, your patient, who has not eaten in three days. The patient’s advanced dementia, anti-coagulation therapy, and other co-morbidities suggest such a move may not be in his best interest. How do you respond?
Ethical dilemmas rarely are simple or clear cut. They often involve revisiting the same issues time and again. That’s where an ethics committee comes in, says Maj. Heather Cereste, MD, U.S. Air Force, co-director of the geriatric medicine service and chair of the bioethics committee at Wilford Hall Medical Center, Lackland Air Force Base, San Antonio, Texas.
Ethics committees provide oversight and assist the institution in creating policies to guide staff through ethical dilemmas, Dr. Cereste says.
“Our job at the ethics committee—and we try to make this very clear—is not to solve people’s problems or dictate care,” she says. “Our job is to provide a perspective and a way of thinking about an issue to better equip people to get through it.”
Though it seems straightforward, the notion is fraught with myriad complications.
A Range of Issues
Pediatric Hospitalist Sheldon Berkowitz, MD, medical director, Minneapolis Children’s Clinic (MCC), Children’s Hospital and Clinics of Minnesota, has been involved with ethics issues for 24 years. He currently is the ethics committee chair at MCC. In his experience, he says “most [ethics committee] consults come from intensive care settings, relating to life-and-death issues.”
The issues become trickier for patients from cultures with specific traditions and beliefs surrounding death. Anita Gandhy, MD, a hospitalist board certified in hospice and palliative care, works at Saint Francis Memorial Hospital in San Francisco. The family of a patient she was treating wanted to continue care for its loved one despite the fact the patient was dying. “I later found out that a baby had recently been born into the family,” Dr. Gandhy says. “In the Chinese culture, if someone dies around the time that a baby is born, that spirit will follow the baby. So the family’s desire to prolong care was consistent with their cultural beliefs.”
Ethical dilemmas surface in a variety of situations—not just related to end-of-life treatment—and between a variety of parties: patient surrogates and medical staff, members of the care team, patients and family, or among family members themselves. Physicians will face many types of conflicts:
- Who makes decisions regarding the rights and preferences of unidentified patients without designated surrogates or advance directives;
- Whether to allow medical training on the newly dead;
- Whether to agree to requests for exorbitant or unorthodox treatments;
- Whether family members can ably deliver home care for a patient who is being discharged; or
- Whether to grant sterilization requests from families of adolescent children with Down syndrome.1
Underutilized Service?
With such a wide swath of potential ethical dilemmas, it would seem intuitive for physicians to use an ethics committee when one is available. Yet, a 2005 survey of 600 U.S. hospitals by The National Center for Ethics in Health Care tells a different story. The survey found 81% of the general hospitals responding to the survey had ethics consultation services, and 100% of hospitals with more than 400 beds had such services. However, the staff sought the ethics consultation services a median of only three times in the year prior to the survey.2
Hospitalist Olivia Wendy Zachary, MD, has worked for two years at California Pacific Medical Center in San Francisco. In that time, she has requested a total of four ethics consults. One recent consultation helped her determine the source of durable power of attorney for a patient who was a prisoner and who, because he was a felon and a ward of the state prison system, could not make his own healthcare decisions.
There are other situations, however, when Dr. Zachary refrains from asking for an ethics consult. For example, as a geriatrician conversant in the potential adverse outcomes of tube feeding patients with dementia, she makes the judgment calls in these instances.
“I feel very comfortable giving family members the data, in a way that they can understand, on the conflicts of tube feeding in demented patients,” Dr. Zachary says. “The role of the ethics committee, in my opinion, should be to answer conflicts for which you do not have the answers. … If that’s beyond your expertise—if you don’t know the studies and aren’t a geriatrician—then in that case, it might be appropriate.”
In other words, don’t call the ethics committee because you don’t have the time to clearly communicate with the family.
Call on the Committee
Medical ethics dilemmas aren’t always as straightforward as knowing the possible negative consequences of placing a feeding tube in a dementia patient. So when should you call on the ethics committee? Physicians at St. Joseph’s Hospital in St. Paul, Minn., fill out an ethics consultation request form to help the hospital determine the need for the consult.
Robert C. Moravec, MD, medical director, director of hospital medicine, and chair of the ethics committee at St. Joseph’s, says the form was created to prevent physicians from requesting consults prematurely, before they have attempted a family care conference or fully understand the issue at hand. For example, providers occasionally request ethics consults when the problem really is poor communication.
“Sometimes, when our ethics committee is consulted, we discover that there is so much emotional energy going into the issue that the participants are simply not communicating,” Dr. Cereste says. “We can help them identify that.”
Other times, the issue lies in a conflict between the physician and the patient’s family. The physician may want to move from aggressive care to a pain and palliative care approach. The family, of course, wants to stay the aggressive course. It’s not the committee’s job to resolve this conflict, Dr. Berkowitz cautions. “The role of the ethics committee should be helping to identify, delineate, and resolve ethics issues,” he explains. “The committee should not be there simply to help the attending physician accomplish their goals.”
Committee Credibility
Even if physicians know when to ask for help from an ethics committee, they only will do so if they trust the enterprise, Dr. Moravec says. Using a multidisciplinary approach has worked at St. Joseph’s, where the ethics committee is comprised of nursing clinical directors, physicians, social workers, chaplains, hospice and palliative care directors, and even dietitians, who meet monthly.
When the St. Joseph’s ethics committee convenes, members fill out a multi-page record for each patient. In addition to a summary of the patient’s medical history, goals of treatment, preferences, and expected quality of life with proposed treatments (or withdrawal thereof), the record documents the committee’s conclusions, Dr. Moravec says. One copy of the document gets incorporated into the patient’s chart, one is sent to hospital administration, and a third gets channeled to the hospital system’s organization-wide ethics committee. This reporting through the medical staff fosters physician buy-in, Dr. Moravec says.
Physicians are less likely to use the consultation services if they feel the ethics committee doesn’t have teeth, says Rachel George, MD, MBA, hospitalist at Aurora St. Luke’s Hospital in Milwaukee, and regional director of five west coast hospitalist programs for Cogent Healthcare, Inc.
The same is true for one Southern California hospitalist who preferred to remain anonymous. “I rarely call for an ethics consult because they’re rarely helpful,” she says. “Generally, the issues we bring to the ethics committee are those where the family is pushing us to provide care we think is futile, and the ethics committee really doesn’t make a decision. You don’t get the backup you need, and you end up very frustrated.”
Sometimes, the California hospitalist continues, the family needs permission from the hospital to halt futile care. Without a durable power of attorney, the care team may find itself bowing to the wishes of one family member—the outlier—who insists the patient be kept alive with aggressive measures. The inpatient palliative care team often fills the ethics gap, helping the medical team discuss end-of-life issues, goals, and desires with the family. Hospitalists, she says, sometimes need an authoritative body to say, “It is no longer ethical to do this to this patient.”
“Having a hospital committee say it’s OK to withdraw a feeding tube or stop dialysis gives a comfort level to physicians,” Dr. Moravec says, “especially if the committee involves clergy, as well as administration. That is powerful support for that doctor.”
Med Students & Residents
The key to making ethics committees more effectively and widely used is education, Dr. George says. “We need to be educating our medical students and residents a lot more aggressively than we are right now,” she asserts. “How to talk with families about end-of-life issues, what is appropriate or inappropriate care, how should you be using your ethics committees—none of that is taught.”
At Children’s Hospital and Clinics, Dr. Berkowitz meets with residents and medical students every six weeks to discuss cases with ethical dilemmas. He says house staffers have little background or experience with ethics. The American Medical Association’s Liaison Committee on Medical Education 2007-2008 survey of 126 U.S. medical colleges found medical ethics was included in one required course at all 126 colleges, and was an elective course in 61. For some perspective, a course in end-of-life care was required at 124 schools and was an elective at 69. A course in palliative care was required at 120 schools, and was an elective in 60.3
Dr. Berkowitz agrees outreach is one solution. “The longer you have an ethics committee available and doing consultations in an institution, the more you expand the knowledge about how to handle problems,” he says. “People who may have previously requested an ethics consult may now have the skills and ability to handle these issues on their own, without needing to call a consult.”
Dr. Gandhy, of Saint Francis Memorial, believes such additional knowledge helps her focus on a patient’s family, not her own plan. “If the family is not ready to withdraw the care, I realize that forcing my agenda on them can also cause suffering,” she says. “When I change my focus to ask, ‘What is going to help the patient and the family?’ sometimes I don’t even need the ethics committee, because I am then able to address the family’s concerns.”
And that’s when everybody gains. TH
Gretchen Henkel is a freelance writer based in California and a frequent contributor to The Hospitalist.
References
1. Snyder L, Leffler C;, for the Ethics and Human Rights Committee, American College of Physicians. Ethics Manual. 5th ed.,2005.
2. Fox E, Myers S, Pearlman RA. Ethics consultation in United States hospitals: a national survey. Am J Bioeth. 2007 Feb;7(2):13-25.
3. Barzansky B, Etze SI. 2007-2008 annual medical school questionnaire part II. JAMA 2008;300(10):1221.
When It Comes to Quality Measures, Size Matters
You work in a small rural hospital. In one year, you admit six patients with acute myocardial infarctions (AMI). You follow CMS and Hospital Quality Alliance guidelines for the eight process measures for AMI, and your hospital scores 100% for that year.
A neighboring hospital isn’t as lucky: One of its four AMI admits, a 99-year-old man, refuses a beta blocker at discharge. What could have been a perfect score (a beta blocker prescribed four out of a possible four times, or 100%), is now 75%.
A study released in June by Duke University Medical Center elucidates the challenges faced by small hospitals when they report performance measures. Smaller hospitals, according to the study, are more likely to rate as top performers when reporting on the eight AMI process measures.1 However, the authors conclude, reports such as those required by Medicare, which ignore denominator size when assessing process performance, can unfairly reward or penalize hospitals.
“The scores can be very misleading,” says Randy Ferrance, DC, MD, a hospitalist at the 67-bed Riverside Tappahannock Hospital in Tappahannock, Va. “If we miss aspirin on discharge for one patient and everything else was perfect, we have the potential to slide into a lower percentile, whereas larger hospitals can miss aspirin at discharge and do just fine.”
Small Denominators, Big Differences
Doug Koekkoek, MD, is in a unique position to see how performance and quality metrics vary by hospital size. As chief medical officer of the Providence Hospitalist Programs in Oregon, Dr. Koekkoek oversees two tertiary facilities, Providence Portland Medical Center (483 beds) and Providence St. Vincent Medical Center (523 beds), as well as a 77-bed community hospital (Providence Milwaukie Hospital), a 40-bed community hospital (Providence Newberg Medical Center), and a 24-bed critical access hospital (Providence Seaside Hospital).
“When we do a roll-up, looking at our appropriate care score, which looks at all the CMS metrics for AMI, congestive heart failure, and pneumonia, we can see that in the bigger institutions, where you have a much bigger denominator of patients who qualify for each diagnosis, the trends are fairly even,” Dr. Koekkoek says. “But in the smaller hospitals, there is much greater variability.”
Rather than focus on each month’s scores, he looks at trends for several months to get a better sense of how his hospitals rate. “You can run at 100% on the heart-failure measures for nine months and then, if your denominator is 10 cases in a quarter and you miss only two or three of the measures, all of a sudden, you’re in the 80% or 70% performance percentile,” he says. “You don’t get a full picture unless you’re looking back over the last six, eight, or 10 months.”
The American Hospital Association (AHA) recommends presenting data to consumers in the same way. “We encourage our hospitals to not let the data themselves tell the story, but to help set them in context and portray to the communities they serve exactly what the data mean,” says Nancy Foster, AHA’s vice president for quality and patient safety.
Foster concedes the issue raised in the Duke study, that quality data don’t reflect low case volumes, has plagued the data-reporting process, but the AHA believes the process should continue. “We firmly believe that all hospitals ought to be sharing good, reliable information on the quality of care they’re providing with the communities they serve,” she says.
Document Challenges
Conveying an accurate representation of your hospital starts with appropriate documentation, says Christian Voge, MD, a hospitalist with Central Coast Chest Consultants, which provides coverage to Sierra Vista Regional Medical Center and French Hospital Medical Center in San Luis Obispo, Calif.
He gives an example: An ACE inhibitor—one of the CMS care process measures for AMI—is contraindicated in a patient. “The way the rules are, if the physician does not document the reason for not giving the medication, this will look like you simply did not meet that measure and will show up as a deficiency.”
It’s similar to billing and coding processes, says hospitalist Joseph Babbitt, MD, who works at the 25-bed Blue Hill Memorial Hospital in Blue Hill, Maine, “It’s not about what you do. It’s about what you document,” he says. “You can provide ‘the best care,’ but if you didn’t write down why an ACE inhibitor was contraindicated and not given, this will not show up as ‘the best care.’ ”
Another complicating factor, in the opinion of Matthew Szvetecz, MD, a hospitalist at St. Mary Medical Center, a rural hospital with 142 beds in Walla Walla, Wash., is severity indexes for determining patients' underlying risk for complications and mortality “are very coarse–there could be small hospitals taking care of very sick patients that are not getting picked up because they do not have that level of detail in an interpretable format."
More Accurate Results
It’s true smaller hospitals are more vulnerable to large swings in performance ratings. However, with fewer staff who need to buy into the process, these hospitals may have an advantage over larger institutions when launching quality improvement initiatives. Case in point: Gifford Medical Center, a 25-bed critical access hospital in Randolph, Vt.
Hospitalist Josh Plavin, MD, MPH, who is board certified in internal medicine and pediatrics, serves as Gifford’s medical director. The current hospitalist program consists of one hospitalist and three physician assistants who provide round-the-clock coverage. For the hospital’s quality improvement effort, all admitting staff, including the eight emergency room providers, must use the hospital’s systemwide, CMS-compliant order set. In addition, quality management staff participate in multidisciplinary rounds and help track performance measures for patients admitted to the hospital. According to Dr. Plavin, the hospital has been 100% compliant with CMS measures the past three quarters since instituting this system.
Dr. Voge agrees smaller hospitals better lend themselves to quality improvement initiatives. “If you have only three or four hospitalists with a contractual arrangement with the hospital, they’re going to be a little more open to ensuring that their numbers–and the hospital’s numbers–look good,” he notes.
Reference
1. O’Brien SM, DeLong ER, and Peterson ED. Impact of case volume on hospital performance assessment. Arch Intern Med. June 2008;168(12):1277-1284.
You work in a small rural hospital. In one year, you admit six patients with acute myocardial infarctions (AMI). You follow CMS and Hospital Quality Alliance guidelines for the eight process measures for AMI, and your hospital scores 100% for that year.
A neighboring hospital isn’t as lucky: One of its four AMI admits, a 99-year-old man, refuses a beta blocker at discharge. What could have been a perfect score (a beta blocker prescribed four out of a possible four times, or 100%), is now 75%.
A study released in June by Duke University Medical Center elucidates the challenges faced by small hospitals when they report performance measures. Smaller hospitals, according to the study, are more likely to rate as top performers when reporting on the eight AMI process measures.1 However, the authors conclude, reports such as those required by Medicare, which ignore denominator size when assessing process performance, can unfairly reward or penalize hospitals.
“The scores can be very misleading,” says Randy Ferrance, DC, MD, a hospitalist at the 67-bed Riverside Tappahannock Hospital in Tappahannock, Va. “If we miss aspirin on discharge for one patient and everything else was perfect, we have the potential to slide into a lower percentile, whereas larger hospitals can miss aspirin at discharge and do just fine.”
Small Denominators, Big Differences
Doug Koekkoek, MD, is in a unique position to see how performance and quality metrics vary by hospital size. As chief medical officer of the Providence Hospitalist Programs in Oregon, Dr. Koekkoek oversees two tertiary facilities, Providence Portland Medical Center (483 beds) and Providence St. Vincent Medical Center (523 beds), as well as a 77-bed community hospital (Providence Milwaukie Hospital), a 40-bed community hospital (Providence Newberg Medical Center), and a 24-bed critical access hospital (Providence Seaside Hospital).
“When we do a roll-up, looking at our appropriate care score, which looks at all the CMS metrics for AMI, congestive heart failure, and pneumonia, we can see that in the bigger institutions, where you have a much bigger denominator of patients who qualify for each diagnosis, the trends are fairly even,” Dr. Koekkoek says. “But in the smaller hospitals, there is much greater variability.”
Rather than focus on each month’s scores, he looks at trends for several months to get a better sense of how his hospitals rate. “You can run at 100% on the heart-failure measures for nine months and then, if your denominator is 10 cases in a quarter and you miss only two or three of the measures, all of a sudden, you’re in the 80% or 70% performance percentile,” he says. “You don’t get a full picture unless you’re looking back over the last six, eight, or 10 months.”
The American Hospital Association (AHA) recommends presenting data to consumers in the same way. “We encourage our hospitals to not let the data themselves tell the story, but to help set them in context and portray to the communities they serve exactly what the data mean,” says Nancy Foster, AHA’s vice president for quality and patient safety.
Foster concedes the issue raised in the Duke study, that quality data don’t reflect low case volumes, has plagued the data-reporting process, but the AHA believes the process should continue. “We firmly believe that all hospitals ought to be sharing good, reliable information on the quality of care they’re providing with the communities they serve,” she says.
Document Challenges
Conveying an accurate representation of your hospital starts with appropriate documentation, says Christian Voge, MD, a hospitalist with Central Coast Chest Consultants, which provides coverage to Sierra Vista Regional Medical Center and French Hospital Medical Center in San Luis Obispo, Calif.
He gives an example: An ACE inhibitor—one of the CMS care process measures for AMI—is contraindicated in a patient. “The way the rules are, if the physician does not document the reason for not giving the medication, this will look like you simply did not meet that measure and will show up as a deficiency.”
It’s similar to billing and coding processes, says hospitalist Joseph Babbitt, MD, who works at the 25-bed Blue Hill Memorial Hospital in Blue Hill, Maine, “It’s not about what you do. It’s about what you document,” he says. “You can provide ‘the best care,’ but if you didn’t write down why an ACE inhibitor was contraindicated and not given, this will not show up as ‘the best care.’ ”
Another complicating factor, in the opinion of Matthew Szvetecz, MD, a hospitalist at St. Mary Medical Center, a rural hospital with 142 beds in Walla Walla, Wash., is severity indexes for determining patients' underlying risk for complications and mortality “are very coarse–there could be small hospitals taking care of very sick patients that are not getting picked up because they do not have that level of detail in an interpretable format."
More Accurate Results
It’s true smaller hospitals are more vulnerable to large swings in performance ratings. However, with fewer staff who need to buy into the process, these hospitals may have an advantage over larger institutions when launching quality improvement initiatives. Case in point: Gifford Medical Center, a 25-bed critical access hospital in Randolph, Vt.
Hospitalist Josh Plavin, MD, MPH, who is board certified in internal medicine and pediatrics, serves as Gifford’s medical director. The current hospitalist program consists of one hospitalist and three physician assistants who provide round-the-clock coverage. For the hospital’s quality improvement effort, all admitting staff, including the eight emergency room providers, must use the hospital’s systemwide, CMS-compliant order set. In addition, quality management staff participate in multidisciplinary rounds and help track performance measures for patients admitted to the hospital. According to Dr. Plavin, the hospital has been 100% compliant with CMS measures the past three quarters since instituting this system.
Dr. Voge agrees smaller hospitals better lend themselves to quality improvement initiatives. “If you have only three or four hospitalists with a contractual arrangement with the hospital, they’re going to be a little more open to ensuring that their numbers–and the hospital’s numbers–look good,” he notes.
Reference
1. O’Brien SM, DeLong ER, and Peterson ED. Impact of case volume on hospital performance assessment. Arch Intern Med. June 2008;168(12):1277-1284.
You work in a small rural hospital. In one year, you admit six patients with acute myocardial infarctions (AMI). You follow CMS and Hospital Quality Alliance guidelines for the eight process measures for AMI, and your hospital scores 100% for that year.
A neighboring hospital isn’t as lucky: One of its four AMI admits, a 99-year-old man, refuses a beta blocker at discharge. What could have been a perfect score (a beta blocker prescribed four out of a possible four times, or 100%), is now 75%.
A study released in June by Duke University Medical Center elucidates the challenges faced by small hospitals when they report performance measures. Smaller hospitals, according to the study, are more likely to rate as top performers when reporting on the eight AMI process measures.1 However, the authors conclude, reports such as those required by Medicare, which ignore denominator size when assessing process performance, can unfairly reward or penalize hospitals.
“The scores can be very misleading,” says Randy Ferrance, DC, MD, a hospitalist at the 67-bed Riverside Tappahannock Hospital in Tappahannock, Va. “If we miss aspirin on discharge for one patient and everything else was perfect, we have the potential to slide into a lower percentile, whereas larger hospitals can miss aspirin at discharge and do just fine.”
Small Denominators, Big Differences
Doug Koekkoek, MD, is in a unique position to see how performance and quality metrics vary by hospital size. As chief medical officer of the Providence Hospitalist Programs in Oregon, Dr. Koekkoek oversees two tertiary facilities, Providence Portland Medical Center (483 beds) and Providence St. Vincent Medical Center (523 beds), as well as a 77-bed community hospital (Providence Milwaukie Hospital), a 40-bed community hospital (Providence Newberg Medical Center), and a 24-bed critical access hospital (Providence Seaside Hospital).
“When we do a roll-up, looking at our appropriate care score, which looks at all the CMS metrics for AMI, congestive heart failure, and pneumonia, we can see that in the bigger institutions, where you have a much bigger denominator of patients who qualify for each diagnosis, the trends are fairly even,” Dr. Koekkoek says. “But in the smaller hospitals, there is much greater variability.”
Rather than focus on each month’s scores, he looks at trends for several months to get a better sense of how his hospitals rate. “You can run at 100% on the heart-failure measures for nine months and then, if your denominator is 10 cases in a quarter and you miss only two or three of the measures, all of a sudden, you’re in the 80% or 70% performance percentile,” he says. “You don’t get a full picture unless you’re looking back over the last six, eight, or 10 months.”
The American Hospital Association (AHA) recommends presenting data to consumers in the same way. “We encourage our hospitals to not let the data themselves tell the story, but to help set them in context and portray to the communities they serve exactly what the data mean,” says Nancy Foster, AHA’s vice president for quality and patient safety.
Foster concedes the issue raised in the Duke study, that quality data don’t reflect low case volumes, has plagued the data-reporting process, but the AHA believes the process should continue. “We firmly believe that all hospitals ought to be sharing good, reliable information on the quality of care they’re providing with the communities they serve,” she says.
Document Challenges
Conveying an accurate representation of your hospital starts with appropriate documentation, says Christian Voge, MD, a hospitalist with Central Coast Chest Consultants, which provides coverage to Sierra Vista Regional Medical Center and French Hospital Medical Center in San Luis Obispo, Calif.
He gives an example: An ACE inhibitor—one of the CMS care process measures for AMI—is contraindicated in a patient. “The way the rules are, if the physician does not document the reason for not giving the medication, this will look like you simply did not meet that measure and will show up as a deficiency.”
It’s similar to billing and coding processes, says hospitalist Joseph Babbitt, MD, who works at the 25-bed Blue Hill Memorial Hospital in Blue Hill, Maine, “It’s not about what you do. It’s about what you document,” he says. “You can provide ‘the best care,’ but if you didn’t write down why an ACE inhibitor was contraindicated and not given, this will not show up as ‘the best care.’ ”
Another complicating factor, in the opinion of Matthew Szvetecz, MD, a hospitalist at St. Mary Medical Center, a rural hospital with 142 beds in Walla Walla, Wash., is severity indexes for determining patients' underlying risk for complications and mortality “are very coarse–there could be small hospitals taking care of very sick patients that are not getting picked up because they do not have that level of detail in an interpretable format."
More Accurate Results
It’s true smaller hospitals are more vulnerable to large swings in performance ratings. However, with fewer staff who need to buy into the process, these hospitals may have an advantage over larger institutions when launching quality improvement initiatives. Case in point: Gifford Medical Center, a 25-bed critical access hospital in Randolph, Vt.
Hospitalist Josh Plavin, MD, MPH, who is board certified in internal medicine and pediatrics, serves as Gifford’s medical director. The current hospitalist program consists of one hospitalist and three physician assistants who provide round-the-clock coverage. For the hospital’s quality improvement effort, all admitting staff, including the eight emergency room providers, must use the hospital’s systemwide, CMS-compliant order set. In addition, quality management staff participate in multidisciplinary rounds and help track performance measures for patients admitted to the hospital. According to Dr. Plavin, the hospital has been 100% compliant with CMS measures the past three quarters since instituting this system.
Dr. Voge agrees smaller hospitals better lend themselves to quality improvement initiatives. “If you have only three or four hospitalists with a contractual arrangement with the hospital, they’re going to be a little more open to ensuring that their numbers–and the hospital’s numbers–look good,” he notes.
Reference
1. O’Brien SM, DeLong ER, and Peterson ED. Impact of case volume on hospital performance assessment. Arch Intern Med. June 2008;168(12):1277-1284.
Canadian Hospitalists: Time to Stand Up
In late June 2006, hospitalists in British Columbia (B.C.) were on the verge of walking out of their regions’ hospitals in protest over payment and workload. The strike was narrowly averted (see “Tough Negotiations Avert B.C. Hospitalist Walkout,” August 2006, p. 1), and chief negotiators for the B.C. hospitalists signed an interim agreement that left the door open for future pay hikes and an examination of workload among other issues.
Two years later, some progress in providing pay increases and adjusting workloads has happened, according to some B.C. hospitalists. David Wilton, MD, is one of the directors of the Vancouver Hospitalist Society, a nonprofit organization that contracts with Vancouver General Hospital and the University of British Columbia Hospital (both overseen by the Vancouver Coastal Health Authority). Although Dr. Wilton reports “things have been working at a snail’s pace,” he and his colleagues have made important inroads in developing more collegial relations with the British Columbia Medical Association (BCMA) and the Canadian College of Family Physicians (CCFP). By taking guidance from SHM, Canadian hospitalists are strengthening their own association by increasing awareness of the value of hospital medicine in Canada.
Where the Trouble Began
BC is divided into six regional health authorities—five of which have active hospitalist programs. Hospitals are administered by the health authorities, whose administrators have come to appreciate hospitalists’ value in increasing patient flow and thus reducing emergency room crowding. However, the health authority administrators do not determine hospitalists’ salaries. All B.C. physicians’ compensation is established through periodic negotiations between the BCMA and the province’s Ministry of Health (MOH).
A Letter of Agreement signed by the two sides in April 2006 revealed serious problems for the hospitalists. The association, dominated by establishment physicians, had (for purposes of the Letter of Agreement) placed hospitalists lower on the pay scale grid than community-based family physicians. Even though hospitalists in Canada predominantly are from a family practice background (the opposite of the United States, where the majority of hospitalists come from internal medicine backgrounds) the BCMA’s under-appreciation of hospitalists’ workloads led to a low base rate for calculating salary increases.
Subsequently, the B.C. hospitalists realized they needed to be proactive about their own interests and hired an attorney to attend meetings with the ministry. Although the ministry never agreed this second, public round of talks were negotiations, an agreement to re-examine contracts was reached.
—Wayne DeMott, MD, hospitalist at Royal Jubilee Hospital in Victoria, B.C.
The contract (signed in June 2006) stipulated timelines for a wind-down provision if there were no satisfactory outcomes with the alternate payments committee or the newly established tripartite Hospitalist Workload Model Working Group, comprised of MOH, local health authority, and hospitalist representatives. An interim contract was signed in September 2007 (retroactive to March 2007) and is again up for renewal since it is now past the April 1, 2008 deadline. The strategy for the near-term is to renew the compensation contract for shorter time periods and wait until the BCMA re-opens negotiations with the MOH in 2010 for an updated Letter of Agreement.
Repairing the Divide
In the meantime, B.C. hospitalists have delved into multiple initiatives they believe eventually will bear fruit. Chief among these is establishment of a hospitalist section within the BCMA. In 2006, the situation was “somewhat antagonistic” between hospitalists and the BCMA, says Geoff Appleton, MD, the current BCMA president.
“There has been friction between GPs and hospitalists because GPs have felt themselves pushed out of the hospital sector,” he says, “and they felt that hospitalists were getting paid more for hospital work than they were.”
Hospitalists, on the other hand, contend GPs were abandoning hospital-based practice, which created a new opportunity for those specializing in inpatient service delivery.
“Hospitalists did not feel they were represented as well as they should have been with the last round of [MOH] negotiations,” Dr. Appleton says. “They feel that they have been undervalued from a BCMA point of view, we don’t like to see that kind of conflict. I think once hospitalists help their colleagues understand the services that they are providing, then some of that resistance can go away. I’m hoping that they’re happier with what we’ve been doing and that their sectional status has improved things for them.”
Others in British Columbia agree with Dr. Appleton’s prognosis. “I think we’ve got optimism,” says Wayne DeMott, MD, a hospitalist at Royal Jubilee Hospital in Victoria, B.C. and chief negotiator for the BCMA’s Section of Hospitalist Medicine. “I think we’re trying to seek a much better representation of our issues from our parent organization that has struggled with figuring out what the heck to do with hospitalists. I do sense that they are trying to accommodate us a bit better and that they’re going to look at how they will represent us in the future.”
Understandably, though, Dr. DeMott also expresses wariness: “We had to go on a pretty tough journey in 2006 and we still haven’t forgotten how we were treated two years ago. We’re definitely going to continue to advocate strongly for ourselves.”
U.S.-Canadian Similarities, Differences
As U.S. hospitalists observe the growing pains of hospitalists in the Canadian healthcare system, it might look like deja vu all over again.
“In many ways, Canadian hospitalists are following a similar arc [as our U.S. HM colleagues] in carving out their niche,” says Dr. Wilton. The void created when family practice physicians abandoned hospital care in the late 1980s and early ’90s has turned into an opportunity for hospitalists. In turn, family practice physicians who at first were resistant have become accepting as they begin to appreciate the service hospitalists provide.
Even though U.S. and Canadian healthcare delivery and reimbursement systems differ, hospitalists “have a similar scope of practice” in the two countries, says Echo- Marie Enns, MD, CCFP, a hospitalist in Calgary, Alberta, and the first president of the Canadian chapter of SHM. John Nelson, MD, medical director of the Hospitalist Practice at Overlake Hospital in Bellevue, WA, a consultant for hospitalist practices with Nelson/Flores Associates, and co-founder and past president of SHM, agrees. “Eighty to ninety percent of the issues with hospitalists would apply to both settings,” he says. “There are ways in which they differ, but in broad strokes, they’re almost identical.”
Hospitalists’ situations and reimbursement agreements do vary from province to province, Dr. Enns notes. She was the lead hospitalist when the Calgary program started in 1998. She also worked in B.C. for a time and noticed that the MOH can be adversarial toward physicians at times. On the other hand, hospitalists in Alberta say they are “very well treated,” and have reported high satisfaction levels overall.
“The hospitalists here admit greater than fifty percent of the patients to medical beds in the region. So, we are the admitting force for the hospital,” she says. “We have a very cooperative relationship with the administration and have been able to initiate a lot of excellent initiatives to improve patient flow in moving patients to the most appropriate bed at the right time. As a result, we’re also getting to be more well known amongst the public.”
More Developments
Currently, the Hospitalist Workload Model Working Group awaits money to hire an external consultant to study hospitalists’ workloads across the province. B.C. hospitalists also are forging a new partnership with the Canadian College of Family Physicians (CCFP). Family practice physicians formerly were wedded to the “mantra of the full-service family physician who did everything—patients, obstetrics, pediatrics—and now they are recognizing that practice patterns are changing,” explains Dr. Wilton. “In order to remain relevant, they need to acknowledge hospital medicine, embrace it and regulate it, to make sure that it is done well.”
The CCFP is now partnering with hospitalists to establish a hospital medicine certification process. Another positive step: the University of Toronto is beginning a new one-year hospital medicine fellowship program. (www.sunnybrook.ca/education/Hospitalist).
Hospitalists across Canada are “in the middle stages” of forming their HM society, reports Dr. Wilton, who has led efforts to build a national database and to launch a survey of Canadian hospitalists. Dr. Enns, who initiated the first Canadian SHM chapter in 2000, thinks opportunities abound for increased collaborations across the border. For instance, she says, having Canadian hospitals involved in multicenter trials of DVT prophylaxis or diabetes initiatives could prove fruitful.
Dr. Nelson also agrees SHM and Canadian hospitalists should continue to consult and work with each other. “There are a number of Canadians who are active in SHM and I think that should continue,” he says. “We have a lot to learn from one another because for most of the issues we face the solutions are going to be the same.”
Drs. Wilton and DeMott invite their U.S. colleagues to attend the 6th annual Canadian Hospitalist Conference from Sept. 27-28, at the Morris J. Wosk Centre for Dialogue in Vancouver, BC. SHM CEO Larry Wellikson, MD, will be the keynote speaker. To register visit www.cpdkt.ubc.ca.
Stay Optimistic
Dr. Wilton notes that despite the slow rate of change for hospitalists, there are positive aspects to their work. “We all know—fundamentally—that we are essential to the functioning of the hospitals,” he says. “We know we’re needed and valued on the frontlines. The [government] bureaucracy and the medical establishment are slow to change, but they eventually will.”
Dr. DeMott considers the future of BCMA hopeful. “We’re going to have a bigger role at the BCMA. They’re going to come to completely appreciate us, and things will hopefully be less acrimonious in the future.”
Both physicians agree the crisis of June 2006 served to heighten awareness of hospitalists’ value.
“It was the hospitalists’ time to make people recognize what we do and that we need to be adequately compensated for it,” Dr. Wilton says. TH
Gretchen Henkel is a medical writer based in California.
In late June 2006, hospitalists in British Columbia (B.C.) were on the verge of walking out of their regions’ hospitals in protest over payment and workload. The strike was narrowly averted (see “Tough Negotiations Avert B.C. Hospitalist Walkout,” August 2006, p. 1), and chief negotiators for the B.C. hospitalists signed an interim agreement that left the door open for future pay hikes and an examination of workload among other issues.
Two years later, some progress in providing pay increases and adjusting workloads has happened, according to some B.C. hospitalists. David Wilton, MD, is one of the directors of the Vancouver Hospitalist Society, a nonprofit organization that contracts with Vancouver General Hospital and the University of British Columbia Hospital (both overseen by the Vancouver Coastal Health Authority). Although Dr. Wilton reports “things have been working at a snail’s pace,” he and his colleagues have made important inroads in developing more collegial relations with the British Columbia Medical Association (BCMA) and the Canadian College of Family Physicians (CCFP). By taking guidance from SHM, Canadian hospitalists are strengthening their own association by increasing awareness of the value of hospital medicine in Canada.
Where the Trouble Began
BC is divided into six regional health authorities—five of which have active hospitalist programs. Hospitals are administered by the health authorities, whose administrators have come to appreciate hospitalists’ value in increasing patient flow and thus reducing emergency room crowding. However, the health authority administrators do not determine hospitalists’ salaries. All B.C. physicians’ compensation is established through periodic negotiations between the BCMA and the province’s Ministry of Health (MOH).
A Letter of Agreement signed by the two sides in April 2006 revealed serious problems for the hospitalists. The association, dominated by establishment physicians, had (for purposes of the Letter of Agreement) placed hospitalists lower on the pay scale grid than community-based family physicians. Even though hospitalists in Canada predominantly are from a family practice background (the opposite of the United States, where the majority of hospitalists come from internal medicine backgrounds) the BCMA’s under-appreciation of hospitalists’ workloads led to a low base rate for calculating salary increases.
Subsequently, the B.C. hospitalists realized they needed to be proactive about their own interests and hired an attorney to attend meetings with the ministry. Although the ministry never agreed this second, public round of talks were negotiations, an agreement to re-examine contracts was reached.
—Wayne DeMott, MD, hospitalist at Royal Jubilee Hospital in Victoria, B.C.
The contract (signed in June 2006) stipulated timelines for a wind-down provision if there were no satisfactory outcomes with the alternate payments committee or the newly established tripartite Hospitalist Workload Model Working Group, comprised of MOH, local health authority, and hospitalist representatives. An interim contract was signed in September 2007 (retroactive to March 2007) and is again up for renewal since it is now past the April 1, 2008 deadline. The strategy for the near-term is to renew the compensation contract for shorter time periods and wait until the BCMA re-opens negotiations with the MOH in 2010 for an updated Letter of Agreement.
Repairing the Divide
In the meantime, B.C. hospitalists have delved into multiple initiatives they believe eventually will bear fruit. Chief among these is establishment of a hospitalist section within the BCMA. In 2006, the situation was “somewhat antagonistic” between hospitalists and the BCMA, says Geoff Appleton, MD, the current BCMA president.
“There has been friction between GPs and hospitalists because GPs have felt themselves pushed out of the hospital sector,” he says, “and they felt that hospitalists were getting paid more for hospital work than they were.”
Hospitalists, on the other hand, contend GPs were abandoning hospital-based practice, which created a new opportunity for those specializing in inpatient service delivery.
“Hospitalists did not feel they were represented as well as they should have been with the last round of [MOH] negotiations,” Dr. Appleton says. “They feel that they have been undervalued from a BCMA point of view, we don’t like to see that kind of conflict. I think once hospitalists help their colleagues understand the services that they are providing, then some of that resistance can go away. I’m hoping that they’re happier with what we’ve been doing and that their sectional status has improved things for them.”
Others in British Columbia agree with Dr. Appleton’s prognosis. “I think we’ve got optimism,” says Wayne DeMott, MD, a hospitalist at Royal Jubilee Hospital in Victoria, B.C. and chief negotiator for the BCMA’s Section of Hospitalist Medicine. “I think we’re trying to seek a much better representation of our issues from our parent organization that has struggled with figuring out what the heck to do with hospitalists. I do sense that they are trying to accommodate us a bit better and that they’re going to look at how they will represent us in the future.”
Understandably, though, Dr. DeMott also expresses wariness: “We had to go on a pretty tough journey in 2006 and we still haven’t forgotten how we were treated two years ago. We’re definitely going to continue to advocate strongly for ourselves.”
U.S.-Canadian Similarities, Differences
As U.S. hospitalists observe the growing pains of hospitalists in the Canadian healthcare system, it might look like deja vu all over again.
“In many ways, Canadian hospitalists are following a similar arc [as our U.S. HM colleagues] in carving out their niche,” says Dr. Wilton. The void created when family practice physicians abandoned hospital care in the late 1980s and early ’90s has turned into an opportunity for hospitalists. In turn, family practice physicians who at first were resistant have become accepting as they begin to appreciate the service hospitalists provide.
Even though U.S. and Canadian healthcare delivery and reimbursement systems differ, hospitalists “have a similar scope of practice” in the two countries, says Echo- Marie Enns, MD, CCFP, a hospitalist in Calgary, Alberta, and the first president of the Canadian chapter of SHM. John Nelson, MD, medical director of the Hospitalist Practice at Overlake Hospital in Bellevue, WA, a consultant for hospitalist practices with Nelson/Flores Associates, and co-founder and past president of SHM, agrees. “Eighty to ninety percent of the issues with hospitalists would apply to both settings,” he says. “There are ways in which they differ, but in broad strokes, they’re almost identical.”
Hospitalists’ situations and reimbursement agreements do vary from province to province, Dr. Enns notes. She was the lead hospitalist when the Calgary program started in 1998. She also worked in B.C. for a time and noticed that the MOH can be adversarial toward physicians at times. On the other hand, hospitalists in Alberta say they are “very well treated,” and have reported high satisfaction levels overall.
“The hospitalists here admit greater than fifty percent of the patients to medical beds in the region. So, we are the admitting force for the hospital,” she says. “We have a very cooperative relationship with the administration and have been able to initiate a lot of excellent initiatives to improve patient flow in moving patients to the most appropriate bed at the right time. As a result, we’re also getting to be more well known amongst the public.”
More Developments
Currently, the Hospitalist Workload Model Working Group awaits money to hire an external consultant to study hospitalists’ workloads across the province. B.C. hospitalists also are forging a new partnership with the Canadian College of Family Physicians (CCFP). Family practice physicians formerly were wedded to the “mantra of the full-service family physician who did everything—patients, obstetrics, pediatrics—and now they are recognizing that practice patterns are changing,” explains Dr. Wilton. “In order to remain relevant, they need to acknowledge hospital medicine, embrace it and regulate it, to make sure that it is done well.”
The CCFP is now partnering with hospitalists to establish a hospital medicine certification process. Another positive step: the University of Toronto is beginning a new one-year hospital medicine fellowship program. (www.sunnybrook.ca/education/Hospitalist).
Hospitalists across Canada are “in the middle stages” of forming their HM society, reports Dr. Wilton, who has led efforts to build a national database and to launch a survey of Canadian hospitalists. Dr. Enns, who initiated the first Canadian SHM chapter in 2000, thinks opportunities abound for increased collaborations across the border. For instance, she says, having Canadian hospitals involved in multicenter trials of DVT prophylaxis or diabetes initiatives could prove fruitful.
Dr. Nelson also agrees SHM and Canadian hospitalists should continue to consult and work with each other. “There are a number of Canadians who are active in SHM and I think that should continue,” he says. “We have a lot to learn from one another because for most of the issues we face the solutions are going to be the same.”
Drs. Wilton and DeMott invite their U.S. colleagues to attend the 6th annual Canadian Hospitalist Conference from Sept. 27-28, at the Morris J. Wosk Centre for Dialogue in Vancouver, BC. SHM CEO Larry Wellikson, MD, will be the keynote speaker. To register visit www.cpdkt.ubc.ca.
Stay Optimistic
Dr. Wilton notes that despite the slow rate of change for hospitalists, there are positive aspects to their work. “We all know—fundamentally—that we are essential to the functioning of the hospitals,” he says. “We know we’re needed and valued on the frontlines. The [government] bureaucracy and the medical establishment are slow to change, but they eventually will.”
Dr. DeMott considers the future of BCMA hopeful. “We’re going to have a bigger role at the BCMA. They’re going to come to completely appreciate us, and things will hopefully be less acrimonious in the future.”
Both physicians agree the crisis of June 2006 served to heighten awareness of hospitalists’ value.
“It was the hospitalists’ time to make people recognize what we do and that we need to be adequately compensated for it,” Dr. Wilton says. TH
Gretchen Henkel is a medical writer based in California.
In late June 2006, hospitalists in British Columbia (B.C.) were on the verge of walking out of their regions’ hospitals in protest over payment and workload. The strike was narrowly averted (see “Tough Negotiations Avert B.C. Hospitalist Walkout,” August 2006, p. 1), and chief negotiators for the B.C. hospitalists signed an interim agreement that left the door open for future pay hikes and an examination of workload among other issues.
Two years later, some progress in providing pay increases and adjusting workloads has happened, according to some B.C. hospitalists. David Wilton, MD, is one of the directors of the Vancouver Hospitalist Society, a nonprofit organization that contracts with Vancouver General Hospital and the University of British Columbia Hospital (both overseen by the Vancouver Coastal Health Authority). Although Dr. Wilton reports “things have been working at a snail’s pace,” he and his colleagues have made important inroads in developing more collegial relations with the British Columbia Medical Association (BCMA) and the Canadian College of Family Physicians (CCFP). By taking guidance from SHM, Canadian hospitalists are strengthening their own association by increasing awareness of the value of hospital medicine in Canada.
Where the Trouble Began
BC is divided into six regional health authorities—five of which have active hospitalist programs. Hospitals are administered by the health authorities, whose administrators have come to appreciate hospitalists’ value in increasing patient flow and thus reducing emergency room crowding. However, the health authority administrators do not determine hospitalists’ salaries. All B.C. physicians’ compensation is established through periodic negotiations between the BCMA and the province’s Ministry of Health (MOH).
A Letter of Agreement signed by the two sides in April 2006 revealed serious problems for the hospitalists. The association, dominated by establishment physicians, had (for purposes of the Letter of Agreement) placed hospitalists lower on the pay scale grid than community-based family physicians. Even though hospitalists in Canada predominantly are from a family practice background (the opposite of the United States, where the majority of hospitalists come from internal medicine backgrounds) the BCMA’s under-appreciation of hospitalists’ workloads led to a low base rate for calculating salary increases.
Subsequently, the B.C. hospitalists realized they needed to be proactive about their own interests and hired an attorney to attend meetings with the ministry. Although the ministry never agreed this second, public round of talks were negotiations, an agreement to re-examine contracts was reached.
—Wayne DeMott, MD, hospitalist at Royal Jubilee Hospital in Victoria, B.C.
The contract (signed in June 2006) stipulated timelines for a wind-down provision if there were no satisfactory outcomes with the alternate payments committee or the newly established tripartite Hospitalist Workload Model Working Group, comprised of MOH, local health authority, and hospitalist representatives. An interim contract was signed in September 2007 (retroactive to March 2007) and is again up for renewal since it is now past the April 1, 2008 deadline. The strategy for the near-term is to renew the compensation contract for shorter time periods and wait until the BCMA re-opens negotiations with the MOH in 2010 for an updated Letter of Agreement.
Repairing the Divide
In the meantime, B.C. hospitalists have delved into multiple initiatives they believe eventually will bear fruit. Chief among these is establishment of a hospitalist section within the BCMA. In 2006, the situation was “somewhat antagonistic” between hospitalists and the BCMA, says Geoff Appleton, MD, the current BCMA president.
“There has been friction between GPs and hospitalists because GPs have felt themselves pushed out of the hospital sector,” he says, “and they felt that hospitalists were getting paid more for hospital work than they were.”
Hospitalists, on the other hand, contend GPs were abandoning hospital-based practice, which created a new opportunity for those specializing in inpatient service delivery.
“Hospitalists did not feel they were represented as well as they should have been with the last round of [MOH] negotiations,” Dr. Appleton says. “They feel that they have been undervalued from a BCMA point of view, we don’t like to see that kind of conflict. I think once hospitalists help their colleagues understand the services that they are providing, then some of that resistance can go away. I’m hoping that they’re happier with what we’ve been doing and that their sectional status has improved things for them.”
Others in British Columbia agree with Dr. Appleton’s prognosis. “I think we’ve got optimism,” says Wayne DeMott, MD, a hospitalist at Royal Jubilee Hospital in Victoria, B.C. and chief negotiator for the BCMA’s Section of Hospitalist Medicine. “I think we’re trying to seek a much better representation of our issues from our parent organization that has struggled with figuring out what the heck to do with hospitalists. I do sense that they are trying to accommodate us a bit better and that they’re going to look at how they will represent us in the future.”
Understandably, though, Dr. DeMott also expresses wariness: “We had to go on a pretty tough journey in 2006 and we still haven’t forgotten how we were treated two years ago. We’re definitely going to continue to advocate strongly for ourselves.”
U.S.-Canadian Similarities, Differences
As U.S. hospitalists observe the growing pains of hospitalists in the Canadian healthcare system, it might look like deja vu all over again.
“In many ways, Canadian hospitalists are following a similar arc [as our U.S. HM colleagues] in carving out their niche,” says Dr. Wilton. The void created when family practice physicians abandoned hospital care in the late 1980s and early ’90s has turned into an opportunity for hospitalists. In turn, family practice physicians who at first were resistant have become accepting as they begin to appreciate the service hospitalists provide.
Even though U.S. and Canadian healthcare delivery and reimbursement systems differ, hospitalists “have a similar scope of practice” in the two countries, says Echo- Marie Enns, MD, CCFP, a hospitalist in Calgary, Alberta, and the first president of the Canadian chapter of SHM. John Nelson, MD, medical director of the Hospitalist Practice at Overlake Hospital in Bellevue, WA, a consultant for hospitalist practices with Nelson/Flores Associates, and co-founder and past president of SHM, agrees. “Eighty to ninety percent of the issues with hospitalists would apply to both settings,” he says. “There are ways in which they differ, but in broad strokes, they’re almost identical.”
Hospitalists’ situations and reimbursement agreements do vary from province to province, Dr. Enns notes. She was the lead hospitalist when the Calgary program started in 1998. She also worked in B.C. for a time and noticed that the MOH can be adversarial toward physicians at times. On the other hand, hospitalists in Alberta say they are “very well treated,” and have reported high satisfaction levels overall.
“The hospitalists here admit greater than fifty percent of the patients to medical beds in the region. So, we are the admitting force for the hospital,” she says. “We have a very cooperative relationship with the administration and have been able to initiate a lot of excellent initiatives to improve patient flow in moving patients to the most appropriate bed at the right time. As a result, we’re also getting to be more well known amongst the public.”
More Developments
Currently, the Hospitalist Workload Model Working Group awaits money to hire an external consultant to study hospitalists’ workloads across the province. B.C. hospitalists also are forging a new partnership with the Canadian College of Family Physicians (CCFP). Family practice physicians formerly were wedded to the “mantra of the full-service family physician who did everything—patients, obstetrics, pediatrics—and now they are recognizing that practice patterns are changing,” explains Dr. Wilton. “In order to remain relevant, they need to acknowledge hospital medicine, embrace it and regulate it, to make sure that it is done well.”
The CCFP is now partnering with hospitalists to establish a hospital medicine certification process. Another positive step: the University of Toronto is beginning a new one-year hospital medicine fellowship program. (www.sunnybrook.ca/education/Hospitalist).
Hospitalists across Canada are “in the middle stages” of forming their HM society, reports Dr. Wilton, who has led efforts to build a national database and to launch a survey of Canadian hospitalists. Dr. Enns, who initiated the first Canadian SHM chapter in 2000, thinks opportunities abound for increased collaborations across the border. For instance, she says, having Canadian hospitals involved in multicenter trials of DVT prophylaxis or diabetes initiatives could prove fruitful.
Dr. Nelson also agrees SHM and Canadian hospitalists should continue to consult and work with each other. “There are a number of Canadians who are active in SHM and I think that should continue,” he says. “We have a lot to learn from one another because for most of the issues we face the solutions are going to be the same.”
Drs. Wilton and DeMott invite their U.S. colleagues to attend the 6th annual Canadian Hospitalist Conference from Sept. 27-28, at the Morris J. Wosk Centre for Dialogue in Vancouver, BC. SHM CEO Larry Wellikson, MD, will be the keynote speaker. To register visit www.cpdkt.ubc.ca.
Stay Optimistic
Dr. Wilton notes that despite the slow rate of change for hospitalists, there are positive aspects to their work. “We all know—fundamentally—that we are essential to the functioning of the hospitals,” he says. “We know we’re needed and valued on the frontlines. The [government] bureaucracy and the medical establishment are slow to change, but they eventually will.”
Dr. DeMott considers the future of BCMA hopeful. “We’re going to have a bigger role at the BCMA. They’re going to come to completely appreciate us, and things will hopefully be less acrimonious in the future.”
Both physicians agree the crisis of June 2006 served to heighten awareness of hospitalists’ value.
“It was the hospitalists’ time to make people recognize what we do and that we need to be adequately compensated for it,” Dr. Wilton says. TH
Gretchen Henkel is a medical writer based in California.
The Patient Has Left the Building
The hospitalist service at the University of Wisconsin Hospital and Clinics in the Department of Medicine recently admitted a patient with altered sensorium, which the team determined most likely was narcotic-related. Going the extra distance, they did a spinal tap to rule out meningitis.
Within a day of changing the medication, the patient got better and was ready for discharge. However, says Julia S. Wright, MD, director of the Madison-based service, an important test remained from the spinal tap. “We thought that those results would not change the medical management of the case, but we knew if it were positive, it would be a big deal,” she recalls.
Not all medical-legal experts would agree the responsibility for patient care ends when patients leave the hospital. Often there are extenuating circumstances that may warrant the hospitalist’s continued communication and contact with patients and/or their providers and caregivers. Although there are no universally accepted standards of care that define these post-discharge issues, several hospitalists recently discussed their institutions’ and groups’ guiding principles for managing the nuances of post-discharge protocol.
Who’s Responsible?
Hospitalist Jeffrey Greenwald, MD, associate professor of medicine at Boston University School of Medicine, is a member of SHM’s Hospital Quality and Patient Safety Committee and also has been investigating pre- and post-discharge interventions through a grant-funded project from the Agency for Healthcare Research and Quality (AHRQ) called “Project RED” (the Re-Engineered Discharge, online at www.ahrq.gov/qual/pips).
One reason the post-discharge period is a “gray zone” of responsibility for care, he believes, is that the hospital system was designed to have a finite endpoint—the discharge. “This ‘out of sight, out of mind’ mentality has existed forever in the inpatient service, but it has become more highlighted in the post-hospitalist era,” he notes.
That mentality can sometimes take over in the hospitalists’ minds. “I think a lot of hospitalists are burying their heads [in the sand] about how these patients are being sent home and the chances for miscommunication and a ‘bounce-back,’ ” notes David Yu, MD, FACP, ABIM, medical director of hospitalist services, Decatur Memorial Hospital, Decatur, Ill., and clinical assistant professor of family and community medicine, Southern Illinois University School of Medicine. “This is going to be more of an issue as hospitalists become increasingly busy. The temptation is to squeeze time on discharges, because it takes an effort to reconcile medications and tie up loose ends at time of discharge. It is not acceptable to write, ‘resume current medications and follow up with PCP’ and think the job is done. It is magical thinking that discharge medications and follow-up instructions will be figured out somehow by the patient and discharging nurse.”
Cover the Gray Zone
Hospitalists describe differing approaches to ensuring patients get the care they need when they leave the hospital.
In the case of the UWHC patient who wanted to leave the hospital, the hospitalist team arranged to stay in touch with the patient. They watched for the test results during the next 24 hours. When the test came back positive, they called the patient back to the hospital, and began treatment.
“Although tracking test results may be out of the hospitalist’s purview, I think we have a strong obligation to make sure we look at some of that data,” Dr. Wright says. “I think there has to be some redundancy, otherwise, the patient probably would not have seen the primary care physician in time and would have become more ill.”
Attention to detail before discharge can avoid problems in the post-discharge period. Partnering with the pharmacy to achieve medication reconciliation has been shown to reduce risk of readmission, notes Tom Bookwalter, PharmD, associate professor of health sciences at the University of California San Francisco School of Medicine and formerly clinical pharmacist there. Using standardized templates and electronic medical records (EMR), hospitalists at many academic centers can furnish real-time discharge summaries to patients’ primary care physicians.
Dr. Yu is especially proud of the EMR system at his institution, by which discharge summaries are faxed to the primary care physician (PCP) in real time. “A patient can call their primary care physician right after discharge, and that physician will know exactly what happened during the hospital course, and what the medications and the discharge plan are,” he explains.
In addition, computerized entry and transmission eliminates the risk of error introduced when handwritten instructions are given to patients. “We believe that communication is the ‘mother’s milk’ of the hospitalist,” Dr. Yu says. Accordingly, his hospitalist service also makes a courtesy call to the PCP following transmission of the EMR for the patient.
Attorney Patrick T. O’Rourke of the Office of University Counsel at Colorado University in Denver and legal columnist for The Hospitalist, advises how to avoid inviting unintended legal consequences. “It’s important for hospitalists to understand that they are the conduit of information about what happened during the hospitalization,” he notes. “Failing to define everyone’s job in the discharge process can expose people to liability.”
In that vein, he urges hospitalists not to delegate the process of giving discharge instructions to the patient. Patients should hear directly from the hospitalist about their condition, the recommended course of action, and how to respond in case of emergency post-discharge. When returning the patient to their regular physician, the hospitalist should also touch base with the patient’s physician via e-mail or telephone to prevent gaps in communication.
Other Strategies
If budgets allow, some groups employ ancillary staff who call patients after discharge.
Hospitalist David Grace, MD, area medical officer for the Schumacher Group, Hospital Medicine Division, in Lafayette, La., reports that having a practice coordinator who calls patients within 48 hours of discharge “adds one more layer of safety to the process.” “Yes” answers to some questions (e.g., “Have your symptoms worsened? Do you have any new symptoms?”) trigger follow-up calls to the on-call hospitalist to take appropriate steps. However, O’Rourke cautions that midlevel providers should possess adequate training to be able to act appropriately upon patients’ information.
Hospitalist Randy Ferrance, DC, MD, medical director at Riverside Tappahannock Hospice in Tappahannock, Va., agrees follow-up calls to patients are a good idea. “I think more aggressive follow up in the short term, and then turning the patient over, for continuity reasons, to their primary care physician as quickly as possible is very important.” His hospitalist group, comprising only four staff, struggles with having the time to devote to such activities. However, with an average inpatient age of 72, their patients often transition to home healthcare. His group enjoys an “excellent relationship” with all the area home health agencies. Those agencies are asked to call the hospitalist group during their first visit with the patient, in addition to sending their usual report to the primary care physician. “At that first home health visit, we consider ourselves still responsible for the patient,” he says.
Beyond Liability Protection
Adhering to the “higher standard” of patient safety can improve transitions of care even further, Dr. Greenwald believes. Such actions might include a mechanism for patients to reach a member of the hospitalist team (nurse, pharmacist or physician) if they have post-discharge concerns; empowering patients and family members to know what to do if an adverse event occurs; and enabling patients to have copies of their own medical information (discharge summary, lab tests, medication reconciliations).
“In addition, we need to involve the nonmedical caregivers who are going to help the patient recuperate,” he asserts. Physicians can educate patients and their caregivers about what happened while they were in the hospital, what treatments are planned, and what information is pending at discharge. While these efforts might require that hospitalists shift their thinking about doctor-patient roles, they can help to create a more comprehensive approach to patient care.
Inherent Dangers
Ironically, what hospitalists do best—promote effective inpatient management—can also lead to a disconnect when the patient leaves the hospital. “Part of what we do, as hospitalists, is to drive down the patient’s length of stay and get them home sooner,” Dr. Grace says. “While unquestionably beneficial for a variety of reasons, it increases the chance that a patient can leave before a result comes back.”
“This change from the continuity of healthcare [provided by a physician who also saw his or her hospitalized patients] to a division of labor does have some inherent fragmentation,” agrees Dr. Wright. “We need to still look at the patient as a whole and be in communication with [our primary care colleagues] and supporting each other on both ends so that the patient does get this more comprehensive care.” TH
Gretchen Henkel is a medical writer based in California.
The hospitalist service at the University of Wisconsin Hospital and Clinics in the Department of Medicine recently admitted a patient with altered sensorium, which the team determined most likely was narcotic-related. Going the extra distance, they did a spinal tap to rule out meningitis.
Within a day of changing the medication, the patient got better and was ready for discharge. However, says Julia S. Wright, MD, director of the Madison-based service, an important test remained from the spinal tap. “We thought that those results would not change the medical management of the case, but we knew if it were positive, it would be a big deal,” she recalls.
Not all medical-legal experts would agree the responsibility for patient care ends when patients leave the hospital. Often there are extenuating circumstances that may warrant the hospitalist’s continued communication and contact with patients and/or their providers and caregivers. Although there are no universally accepted standards of care that define these post-discharge issues, several hospitalists recently discussed their institutions’ and groups’ guiding principles for managing the nuances of post-discharge protocol.
Who’s Responsible?
Hospitalist Jeffrey Greenwald, MD, associate professor of medicine at Boston University School of Medicine, is a member of SHM’s Hospital Quality and Patient Safety Committee and also has been investigating pre- and post-discharge interventions through a grant-funded project from the Agency for Healthcare Research and Quality (AHRQ) called “Project RED” (the Re-Engineered Discharge, online at www.ahrq.gov/qual/pips).
One reason the post-discharge period is a “gray zone” of responsibility for care, he believes, is that the hospital system was designed to have a finite endpoint—the discharge. “This ‘out of sight, out of mind’ mentality has existed forever in the inpatient service, but it has become more highlighted in the post-hospitalist era,” he notes.
That mentality can sometimes take over in the hospitalists’ minds. “I think a lot of hospitalists are burying their heads [in the sand] about how these patients are being sent home and the chances for miscommunication and a ‘bounce-back,’ ” notes David Yu, MD, FACP, ABIM, medical director of hospitalist services, Decatur Memorial Hospital, Decatur, Ill., and clinical assistant professor of family and community medicine, Southern Illinois University School of Medicine. “This is going to be more of an issue as hospitalists become increasingly busy. The temptation is to squeeze time on discharges, because it takes an effort to reconcile medications and tie up loose ends at time of discharge. It is not acceptable to write, ‘resume current medications and follow up with PCP’ and think the job is done. It is magical thinking that discharge medications and follow-up instructions will be figured out somehow by the patient and discharging nurse.”
Cover the Gray Zone
Hospitalists describe differing approaches to ensuring patients get the care they need when they leave the hospital.
In the case of the UWHC patient who wanted to leave the hospital, the hospitalist team arranged to stay in touch with the patient. They watched for the test results during the next 24 hours. When the test came back positive, they called the patient back to the hospital, and began treatment.
“Although tracking test results may be out of the hospitalist’s purview, I think we have a strong obligation to make sure we look at some of that data,” Dr. Wright says. “I think there has to be some redundancy, otherwise, the patient probably would not have seen the primary care physician in time and would have become more ill.”
Attention to detail before discharge can avoid problems in the post-discharge period. Partnering with the pharmacy to achieve medication reconciliation has been shown to reduce risk of readmission, notes Tom Bookwalter, PharmD, associate professor of health sciences at the University of California San Francisco School of Medicine and formerly clinical pharmacist there. Using standardized templates and electronic medical records (EMR), hospitalists at many academic centers can furnish real-time discharge summaries to patients’ primary care physicians.
Dr. Yu is especially proud of the EMR system at his institution, by which discharge summaries are faxed to the primary care physician (PCP) in real time. “A patient can call their primary care physician right after discharge, and that physician will know exactly what happened during the hospital course, and what the medications and the discharge plan are,” he explains.
In addition, computerized entry and transmission eliminates the risk of error introduced when handwritten instructions are given to patients. “We believe that communication is the ‘mother’s milk’ of the hospitalist,” Dr. Yu says. Accordingly, his hospitalist service also makes a courtesy call to the PCP following transmission of the EMR for the patient.
Attorney Patrick T. O’Rourke of the Office of University Counsel at Colorado University in Denver and legal columnist for The Hospitalist, advises how to avoid inviting unintended legal consequences. “It’s important for hospitalists to understand that they are the conduit of information about what happened during the hospitalization,” he notes. “Failing to define everyone’s job in the discharge process can expose people to liability.”
In that vein, he urges hospitalists not to delegate the process of giving discharge instructions to the patient. Patients should hear directly from the hospitalist about their condition, the recommended course of action, and how to respond in case of emergency post-discharge. When returning the patient to their regular physician, the hospitalist should also touch base with the patient’s physician via e-mail or telephone to prevent gaps in communication.
Other Strategies
If budgets allow, some groups employ ancillary staff who call patients after discharge.
Hospitalist David Grace, MD, area medical officer for the Schumacher Group, Hospital Medicine Division, in Lafayette, La., reports that having a practice coordinator who calls patients within 48 hours of discharge “adds one more layer of safety to the process.” “Yes” answers to some questions (e.g., “Have your symptoms worsened? Do you have any new symptoms?”) trigger follow-up calls to the on-call hospitalist to take appropriate steps. However, O’Rourke cautions that midlevel providers should possess adequate training to be able to act appropriately upon patients’ information.
Hospitalist Randy Ferrance, DC, MD, medical director at Riverside Tappahannock Hospice in Tappahannock, Va., agrees follow-up calls to patients are a good idea. “I think more aggressive follow up in the short term, and then turning the patient over, for continuity reasons, to their primary care physician as quickly as possible is very important.” His hospitalist group, comprising only four staff, struggles with having the time to devote to such activities. However, with an average inpatient age of 72, their patients often transition to home healthcare. His group enjoys an “excellent relationship” with all the area home health agencies. Those agencies are asked to call the hospitalist group during their first visit with the patient, in addition to sending their usual report to the primary care physician. “At that first home health visit, we consider ourselves still responsible for the patient,” he says.
Beyond Liability Protection
Adhering to the “higher standard” of patient safety can improve transitions of care even further, Dr. Greenwald believes. Such actions might include a mechanism for patients to reach a member of the hospitalist team (nurse, pharmacist or physician) if they have post-discharge concerns; empowering patients and family members to know what to do if an adverse event occurs; and enabling patients to have copies of their own medical information (discharge summary, lab tests, medication reconciliations).
“In addition, we need to involve the nonmedical caregivers who are going to help the patient recuperate,” he asserts. Physicians can educate patients and their caregivers about what happened while they were in the hospital, what treatments are planned, and what information is pending at discharge. While these efforts might require that hospitalists shift their thinking about doctor-patient roles, they can help to create a more comprehensive approach to patient care.
Inherent Dangers
Ironically, what hospitalists do best—promote effective inpatient management—can also lead to a disconnect when the patient leaves the hospital. “Part of what we do, as hospitalists, is to drive down the patient’s length of stay and get them home sooner,” Dr. Grace says. “While unquestionably beneficial for a variety of reasons, it increases the chance that a patient can leave before a result comes back.”
“This change from the continuity of healthcare [provided by a physician who also saw his or her hospitalized patients] to a division of labor does have some inherent fragmentation,” agrees Dr. Wright. “We need to still look at the patient as a whole and be in communication with [our primary care colleagues] and supporting each other on both ends so that the patient does get this more comprehensive care.” TH
Gretchen Henkel is a medical writer based in California.
The hospitalist service at the University of Wisconsin Hospital and Clinics in the Department of Medicine recently admitted a patient with altered sensorium, which the team determined most likely was narcotic-related. Going the extra distance, they did a spinal tap to rule out meningitis.
Within a day of changing the medication, the patient got better and was ready for discharge. However, says Julia S. Wright, MD, director of the Madison-based service, an important test remained from the spinal tap. “We thought that those results would not change the medical management of the case, but we knew if it were positive, it would be a big deal,” she recalls.
Not all medical-legal experts would agree the responsibility for patient care ends when patients leave the hospital. Often there are extenuating circumstances that may warrant the hospitalist’s continued communication and contact with patients and/or their providers and caregivers. Although there are no universally accepted standards of care that define these post-discharge issues, several hospitalists recently discussed their institutions’ and groups’ guiding principles for managing the nuances of post-discharge protocol.
Who’s Responsible?
Hospitalist Jeffrey Greenwald, MD, associate professor of medicine at Boston University School of Medicine, is a member of SHM’s Hospital Quality and Patient Safety Committee and also has been investigating pre- and post-discharge interventions through a grant-funded project from the Agency for Healthcare Research and Quality (AHRQ) called “Project RED” (the Re-Engineered Discharge, online at www.ahrq.gov/qual/pips).
One reason the post-discharge period is a “gray zone” of responsibility for care, he believes, is that the hospital system was designed to have a finite endpoint—the discharge. “This ‘out of sight, out of mind’ mentality has existed forever in the inpatient service, but it has become more highlighted in the post-hospitalist era,” he notes.
That mentality can sometimes take over in the hospitalists’ minds. “I think a lot of hospitalists are burying their heads [in the sand] about how these patients are being sent home and the chances for miscommunication and a ‘bounce-back,’ ” notes David Yu, MD, FACP, ABIM, medical director of hospitalist services, Decatur Memorial Hospital, Decatur, Ill., and clinical assistant professor of family and community medicine, Southern Illinois University School of Medicine. “This is going to be more of an issue as hospitalists become increasingly busy. The temptation is to squeeze time on discharges, because it takes an effort to reconcile medications and tie up loose ends at time of discharge. It is not acceptable to write, ‘resume current medications and follow up with PCP’ and think the job is done. It is magical thinking that discharge medications and follow-up instructions will be figured out somehow by the patient and discharging nurse.”
Cover the Gray Zone
Hospitalists describe differing approaches to ensuring patients get the care they need when they leave the hospital.
In the case of the UWHC patient who wanted to leave the hospital, the hospitalist team arranged to stay in touch with the patient. They watched for the test results during the next 24 hours. When the test came back positive, they called the patient back to the hospital, and began treatment.
“Although tracking test results may be out of the hospitalist’s purview, I think we have a strong obligation to make sure we look at some of that data,” Dr. Wright says. “I think there has to be some redundancy, otherwise, the patient probably would not have seen the primary care physician in time and would have become more ill.”
Attention to detail before discharge can avoid problems in the post-discharge period. Partnering with the pharmacy to achieve medication reconciliation has been shown to reduce risk of readmission, notes Tom Bookwalter, PharmD, associate professor of health sciences at the University of California San Francisco School of Medicine and formerly clinical pharmacist there. Using standardized templates and electronic medical records (EMR), hospitalists at many academic centers can furnish real-time discharge summaries to patients’ primary care physicians.
Dr. Yu is especially proud of the EMR system at his institution, by which discharge summaries are faxed to the primary care physician (PCP) in real time. “A patient can call their primary care physician right after discharge, and that physician will know exactly what happened during the hospital course, and what the medications and the discharge plan are,” he explains.
In addition, computerized entry and transmission eliminates the risk of error introduced when handwritten instructions are given to patients. “We believe that communication is the ‘mother’s milk’ of the hospitalist,” Dr. Yu says. Accordingly, his hospitalist service also makes a courtesy call to the PCP following transmission of the EMR for the patient.
Attorney Patrick T. O’Rourke of the Office of University Counsel at Colorado University in Denver and legal columnist for The Hospitalist, advises how to avoid inviting unintended legal consequences. “It’s important for hospitalists to understand that they are the conduit of information about what happened during the hospitalization,” he notes. “Failing to define everyone’s job in the discharge process can expose people to liability.”
In that vein, he urges hospitalists not to delegate the process of giving discharge instructions to the patient. Patients should hear directly from the hospitalist about their condition, the recommended course of action, and how to respond in case of emergency post-discharge. When returning the patient to their regular physician, the hospitalist should also touch base with the patient’s physician via e-mail or telephone to prevent gaps in communication.
Other Strategies
If budgets allow, some groups employ ancillary staff who call patients after discharge.
Hospitalist David Grace, MD, area medical officer for the Schumacher Group, Hospital Medicine Division, in Lafayette, La., reports that having a practice coordinator who calls patients within 48 hours of discharge “adds one more layer of safety to the process.” “Yes” answers to some questions (e.g., “Have your symptoms worsened? Do you have any new symptoms?”) trigger follow-up calls to the on-call hospitalist to take appropriate steps. However, O’Rourke cautions that midlevel providers should possess adequate training to be able to act appropriately upon patients’ information.
Hospitalist Randy Ferrance, DC, MD, medical director at Riverside Tappahannock Hospice in Tappahannock, Va., agrees follow-up calls to patients are a good idea. “I think more aggressive follow up in the short term, and then turning the patient over, for continuity reasons, to their primary care physician as quickly as possible is very important.” His hospitalist group, comprising only four staff, struggles with having the time to devote to such activities. However, with an average inpatient age of 72, their patients often transition to home healthcare. His group enjoys an “excellent relationship” with all the area home health agencies. Those agencies are asked to call the hospitalist group during their first visit with the patient, in addition to sending their usual report to the primary care physician. “At that first home health visit, we consider ourselves still responsible for the patient,” he says.
Beyond Liability Protection
Adhering to the “higher standard” of patient safety can improve transitions of care even further, Dr. Greenwald believes. Such actions might include a mechanism for patients to reach a member of the hospitalist team (nurse, pharmacist or physician) if they have post-discharge concerns; empowering patients and family members to know what to do if an adverse event occurs; and enabling patients to have copies of their own medical information (discharge summary, lab tests, medication reconciliations).
“In addition, we need to involve the nonmedical caregivers who are going to help the patient recuperate,” he asserts. Physicians can educate patients and their caregivers about what happened while they were in the hospital, what treatments are planned, and what information is pending at discharge. While these efforts might require that hospitalists shift their thinking about doctor-patient roles, they can help to create a more comprehensive approach to patient care.
Inherent Dangers
Ironically, what hospitalists do best—promote effective inpatient management—can also lead to a disconnect when the patient leaves the hospital. “Part of what we do, as hospitalists, is to drive down the patient’s length of stay and get them home sooner,” Dr. Grace says. “While unquestionably beneficial for a variety of reasons, it increases the chance that a patient can leave before a result comes back.”
“This change from the continuity of healthcare [provided by a physician who also saw his or her hospitalized patients] to a division of labor does have some inherent fragmentation,” agrees Dr. Wright. “We need to still look at the patient as a whole and be in communication with [our primary care colleagues] and supporting each other on both ends so that the patient does get this more comprehensive care.” TH
Gretchen Henkel is a medical writer based in California.
OR Opportunity
In this era of increasing synergy between the surgical and hospital medicine services, Minnesota hospitalist David Frenz, MD, has taken perioperative management of surgical patients a step further.
One or two days a week, Dr. Frenz can be found in the operating room (OR) of St. Joseph’s Hospital in St. Paul, assisting on multilevel spine surgery cases.
Although Dr. Frenz may be a one-of-a-kind hospitalist acting as first assistant in the OR, the approach offers many advantages to his hospital and hospital medicine service, says Robert C. Moravec, MD.
“It seems more efficient having one assistant surgeon [rather than several scrub technicians] who knows exactly what’s going to happen next,” says Dr. Moravec, medical director for both the hospital service and St. Joseph’s Hospital. “More importantly, it’s a way to develop some expertise in the perioperative arena and to develop collaborative relationships with the surgeons.” In addition, the hospital service is able to bill for an assistant surgeon’s fee, which covers much of Dr. Frenz’ salary. And when he’s not on the medical floors seeing patients, Dr. Frenz is engaged in a monthslong quality improvement (QI) project to improve perioperative care and reduce same-day surgery cancellations at his institution.
The effectiveness of this QI project, which Dr. Moravec believes will go to HealthEast’s other two acute care hospitals in nine months, would not be possible without Dr. Frenz’ conversance with problems in the OR.
“When you are involved in this type of process improvement project, you don’t want, as a do-gooder, to create more cancellations and delays,” says Dr. Frenz. “And you don’t want to screw up their referral relationships. You’ve got to be super-sensitive to those issues as you’re trying to slowly bring about change. The fact that I’m known to the surgeons and that I’m in the OR getting dirty lends credibility to our efforts to bring change.”
Value in Surgical Assisting?
In medical school, Dr. Frenz had considered becoming a general surgeon before switching to family-practice medicine, so he is comfortable in the OR and finds assisting to be a stimulating change of pace. Although this long-standing pilot project is unique, it raises provocative possibilities for other hospitalists.
“Having a hospitalist go into the OR to assist with cases creates an interesting situation,” says Richard Rohr, MD, vice president for medical affairs at Cortland Regional Medical Center in Cortland, N.Y. “The hospitalist is then able to engage with more surgical aspects of the case, as well as the medical management.” Adding surgical assisting to the hospitalist’s role—although it could complicate scheduling and malpractice coverage—might dovetail with some hospitals’ difficulties retaining general surgeons, he says.
Combining the two functions could add to the hospital medicine group’s bottom line if relevant malpractice costs could be worked out, says hospitalist Kenneth Patrick, MD, the ICU director at Chestnut Hill Hospital in Philadelphia. Dr. Frenz’ malpractice is provided by his hospital, and pre-certification for his assistance on cases is handled by the neurosurgeon’s office staff.
In Dr. Patrick’s experience, there could be benefits to the patient if the hospitalist has direct involvement in the OR. For instance, the hospitalist would be better able to anticipate and deal with pre- and post-operative problems.
—David Frenz, MD, hospitalist, St. Joseph’s Hospital, St. Paul, Minn.
Surgery and ‘Outer Space’
Whether or not surgical assisting could become a new frontier for hospitalists, it illustrates the multiple collaborative roles the specialty increasingly offers.
David A. Hoffmann, MD, is medical director of a hospitalist group in Chambersburg, Pa. The group is made up of half family practice and half internal medicine hospitalists. Like so many other hospitalists, he’s seen tremendous growth in the number of surgical co-management cases his group handles at Chambersburg Hospital (see “The Surgical Surge,” December 2007, p. 1). His group tries “to make inroads with the surgeons,” he says. “We send a member of our group to their meetings, and we work with them on management protocols [such as DVT prophylaxis]. I can see the benefits of getting to know what’s going on down there [in the OR]. The truth of matter is, [despite co-management], sending the patient to the OR is like sending someone into outer space for the hospitalist. The rocket goes off, and you don’t see the patient until they come back in for a landing.”
Depending on the location of hospitalist groups, involvement as first assistants could represent additional opportunities for family medicine physicians, Dr. Hoffmann believes.
Air Force Maj. Heather Cereste, MD, agrees that the degree of symbiosis between surgeons and hospitalists likely will continue to be a location - and hospital-specific phenomenon. While serving in Iraq, she had significant experience with surgical procedures, and felt that from an internist’s perspective, she was more valuable to the surgical team. During her third-year residency in Maine, she observed many who planned to go into family practice assisting with gastrointestinal procedures and the like. “Certainly, in a smaller setting, with fewer available resources, the more autonomous a hospitalist can be, the better,” says Dr. Cereste, co-director of the geriatric medicine service at Wilford Hall Medical Center, Lackland Air Force Base, Texas, and chair of the bioethics committee.
Cautionary Tales
Though surgical assisting is an intriguing idea, such a set up “could have its own set of unintended consequences,” especially for a private model hospitalist group, says Brian Bossard, MD, medical director of Inpatient Physician Associates in Lincoln, Neb.
Dr. Bossard has personal experience with this configuration. When an internist in his hospitalist group began to do surgical assisting, the privately owned group (which contracts with Bryan LGH Hospital in Lincoln to provide hospitalist services) did not find this advantageous. The physician’s surgical participation was at times disruptive for the group, since he was unable to be immediately available and on call or to run codes while in the OR.
“It’s not clear to me that there would be an advantage to have a hospitalist [assisting in the OR], as opposed to another physician extender such as a physician assistant or a nurse practitioner,” says Jack M. Percelay, MD, a pediatric hospitalist at Saint Barnabas Medical Center in Livingston, N.J. Co-management of surgical patients is another matter, however, and Dr. Percelay does see value in having hospitalists help with maintenance of lines, wound care, and other post-surgical management duties.
“There is a certain set of procedures we’re supposed to master, such as vascular access and airway support,” Dr. Percelay continues. “But our value as hospitalists is in our cognitive skill set. I don’t know any hospitalists who consider a scalpel as one of their routine tools.”
Bryan Fine, MD, a pediatric hospital at Children’s National Medical Center in Washington, D.C., recently joined a general hospitalist group after spending three and a half years as the hospitalist in charge of medical management for the gastroenterology service. His opinion of hospitalists assisting in surgery? “I think it’s definitely valuable if it’s done in the context of a larger goal and to gain credibility from a hospital administrative level,” he suggests. However, he said, professional satisfaction for a hospitalist might be limited since he or she essentially would be serving as a physician extender.
Barriers
Family-practice physicians often are differentiated from their internal medicine colleagues by their skill sets in procedures.
“To the extent that a family-medicine physician may want to demonstrate that they can have a skill set that adds value in order to be hired or accepted, I think surgical assisting could have very specific application in specific places,” says A. Neal Axon, MD, assistant professor in the departments of internal medicine and pediatrics at the Medical University of South Carolina in Charleston. “I’ve certainly tried to market myself as a med-peds person, and as somebody who’s good at more than one thing.”
Dr. Axon concedes hospitalists as surgical assistants would not work at his institution. “In academic medical centers, the dividing lines between divisions and disciplines are very concrete,” he explains. “I think many people carry those cultural barriers or dividers—even if they are somewhat artificial outside the academic environment—when they leave and go into community practice.”
Those divisions are not felt as keenly in the Midwest, according to Dr. Frenz, where “family medicine has a long tradition.” St. Joseph’s Hospital has a family - medicine residency program, and more than half the credentialed physicians there are family- medicine trained.
“We think that family-medicine physicians have a skill set that is valuable in certain clinical settings,” he says. “For example, we do a lot of work on the behavioral health floors and are the principal medical providers on a 28-bed chemical dependency unit.” Dr. Frenz had a patient who was pregnant and alcohol dependent. Because of his expertise in addiction medicine (another of his self-described “insurgencies”) and residency training in obstetrics, Dr. Frenz is managing the patient without incurring an ob/gyn consultation.
How to Prepare
Every hospitalist’s path and skill set is unique, but for those medical students or residents who might be interested in combining some surgical work with hospitalist skills, Dr. Frenz advises adopting a calculated approach to electives. Besides taking as many surgical electives as possible, trainees should try to pick small community hospitals where they will not have to compete with surgical residents for time in the OR.
Although she thinks expanding into surgical assisting could improve recruitment (offering a varied hospital experience), Dr. Cereste also emphasizes that many questions regarding training standards, care standards, and expense hurdles would have to be addressed.
The bottom line, says Dr. Hoffmann, is that hospitalists “need to be able to play a lot of different roles. I think we’re like a utility infielder. If [surgical assisting] improves patient care, is a valuable service to the health system, and is viewed by consultants, specialists, and family doctors as an additional skill, it’s clearly going to benefit your program and your hospital. The key is to see what works in everyone’s little pond and try to be a team builder.” TH
Gretchen Henkel is a medical writer based in California
In this era of increasing synergy between the surgical and hospital medicine services, Minnesota hospitalist David Frenz, MD, has taken perioperative management of surgical patients a step further.
One or two days a week, Dr. Frenz can be found in the operating room (OR) of St. Joseph’s Hospital in St. Paul, assisting on multilevel spine surgery cases.
Although Dr. Frenz may be a one-of-a-kind hospitalist acting as first assistant in the OR, the approach offers many advantages to his hospital and hospital medicine service, says Robert C. Moravec, MD.
“It seems more efficient having one assistant surgeon [rather than several scrub technicians] who knows exactly what’s going to happen next,” says Dr. Moravec, medical director for both the hospital service and St. Joseph’s Hospital. “More importantly, it’s a way to develop some expertise in the perioperative arena and to develop collaborative relationships with the surgeons.” In addition, the hospital service is able to bill for an assistant surgeon’s fee, which covers much of Dr. Frenz’ salary. And when he’s not on the medical floors seeing patients, Dr. Frenz is engaged in a monthslong quality improvement (QI) project to improve perioperative care and reduce same-day surgery cancellations at his institution.
The effectiveness of this QI project, which Dr. Moravec believes will go to HealthEast’s other two acute care hospitals in nine months, would not be possible without Dr. Frenz’ conversance with problems in the OR.
“When you are involved in this type of process improvement project, you don’t want, as a do-gooder, to create more cancellations and delays,” says Dr. Frenz. “And you don’t want to screw up their referral relationships. You’ve got to be super-sensitive to those issues as you’re trying to slowly bring about change. The fact that I’m known to the surgeons and that I’m in the OR getting dirty lends credibility to our efforts to bring change.”
Value in Surgical Assisting?
In medical school, Dr. Frenz had considered becoming a general surgeon before switching to family-practice medicine, so he is comfortable in the OR and finds assisting to be a stimulating change of pace. Although this long-standing pilot project is unique, it raises provocative possibilities for other hospitalists.
“Having a hospitalist go into the OR to assist with cases creates an interesting situation,” says Richard Rohr, MD, vice president for medical affairs at Cortland Regional Medical Center in Cortland, N.Y. “The hospitalist is then able to engage with more surgical aspects of the case, as well as the medical management.” Adding surgical assisting to the hospitalist’s role—although it could complicate scheduling and malpractice coverage—might dovetail with some hospitals’ difficulties retaining general surgeons, he says.
Combining the two functions could add to the hospital medicine group’s bottom line if relevant malpractice costs could be worked out, says hospitalist Kenneth Patrick, MD, the ICU director at Chestnut Hill Hospital in Philadelphia. Dr. Frenz’ malpractice is provided by his hospital, and pre-certification for his assistance on cases is handled by the neurosurgeon’s office staff.
In Dr. Patrick’s experience, there could be benefits to the patient if the hospitalist has direct involvement in the OR. For instance, the hospitalist would be better able to anticipate and deal with pre- and post-operative problems.
—David Frenz, MD, hospitalist, St. Joseph’s Hospital, St. Paul, Minn.
Surgery and ‘Outer Space’
Whether or not surgical assisting could become a new frontier for hospitalists, it illustrates the multiple collaborative roles the specialty increasingly offers.
David A. Hoffmann, MD, is medical director of a hospitalist group in Chambersburg, Pa. The group is made up of half family practice and half internal medicine hospitalists. Like so many other hospitalists, he’s seen tremendous growth in the number of surgical co-management cases his group handles at Chambersburg Hospital (see “The Surgical Surge,” December 2007, p. 1). His group tries “to make inroads with the surgeons,” he says. “We send a member of our group to their meetings, and we work with them on management protocols [such as DVT prophylaxis]. I can see the benefits of getting to know what’s going on down there [in the OR]. The truth of matter is, [despite co-management], sending the patient to the OR is like sending someone into outer space for the hospitalist. The rocket goes off, and you don’t see the patient until they come back in for a landing.”
Depending on the location of hospitalist groups, involvement as first assistants could represent additional opportunities for family medicine physicians, Dr. Hoffmann believes.
Air Force Maj. Heather Cereste, MD, agrees that the degree of symbiosis between surgeons and hospitalists likely will continue to be a location - and hospital-specific phenomenon. While serving in Iraq, she had significant experience with surgical procedures, and felt that from an internist’s perspective, she was more valuable to the surgical team. During her third-year residency in Maine, she observed many who planned to go into family practice assisting with gastrointestinal procedures and the like. “Certainly, in a smaller setting, with fewer available resources, the more autonomous a hospitalist can be, the better,” says Dr. Cereste, co-director of the geriatric medicine service at Wilford Hall Medical Center, Lackland Air Force Base, Texas, and chair of the bioethics committee.
Cautionary Tales
Though surgical assisting is an intriguing idea, such a set up “could have its own set of unintended consequences,” especially for a private model hospitalist group, says Brian Bossard, MD, medical director of Inpatient Physician Associates in Lincoln, Neb.
Dr. Bossard has personal experience with this configuration. When an internist in his hospitalist group began to do surgical assisting, the privately owned group (which contracts with Bryan LGH Hospital in Lincoln to provide hospitalist services) did not find this advantageous. The physician’s surgical participation was at times disruptive for the group, since he was unable to be immediately available and on call or to run codes while in the OR.
“It’s not clear to me that there would be an advantage to have a hospitalist [assisting in the OR], as opposed to another physician extender such as a physician assistant or a nurse practitioner,” says Jack M. Percelay, MD, a pediatric hospitalist at Saint Barnabas Medical Center in Livingston, N.J. Co-management of surgical patients is another matter, however, and Dr. Percelay does see value in having hospitalists help with maintenance of lines, wound care, and other post-surgical management duties.
“There is a certain set of procedures we’re supposed to master, such as vascular access and airway support,” Dr. Percelay continues. “But our value as hospitalists is in our cognitive skill set. I don’t know any hospitalists who consider a scalpel as one of their routine tools.”
Bryan Fine, MD, a pediatric hospital at Children’s National Medical Center in Washington, D.C., recently joined a general hospitalist group after spending three and a half years as the hospitalist in charge of medical management for the gastroenterology service. His opinion of hospitalists assisting in surgery? “I think it’s definitely valuable if it’s done in the context of a larger goal and to gain credibility from a hospital administrative level,” he suggests. However, he said, professional satisfaction for a hospitalist might be limited since he or she essentially would be serving as a physician extender.
Barriers
Family-practice physicians often are differentiated from their internal medicine colleagues by their skill sets in procedures.
“To the extent that a family-medicine physician may want to demonstrate that they can have a skill set that adds value in order to be hired or accepted, I think surgical assisting could have very specific application in specific places,” says A. Neal Axon, MD, assistant professor in the departments of internal medicine and pediatrics at the Medical University of South Carolina in Charleston. “I’ve certainly tried to market myself as a med-peds person, and as somebody who’s good at more than one thing.”
Dr. Axon concedes hospitalists as surgical assistants would not work at his institution. “In academic medical centers, the dividing lines between divisions and disciplines are very concrete,” he explains. “I think many people carry those cultural barriers or dividers—even if they are somewhat artificial outside the academic environment—when they leave and go into community practice.”
Those divisions are not felt as keenly in the Midwest, according to Dr. Frenz, where “family medicine has a long tradition.” St. Joseph’s Hospital has a family - medicine residency program, and more than half the credentialed physicians there are family- medicine trained.
“We think that family-medicine physicians have a skill set that is valuable in certain clinical settings,” he says. “For example, we do a lot of work on the behavioral health floors and are the principal medical providers on a 28-bed chemical dependency unit.” Dr. Frenz had a patient who was pregnant and alcohol dependent. Because of his expertise in addiction medicine (another of his self-described “insurgencies”) and residency training in obstetrics, Dr. Frenz is managing the patient without incurring an ob/gyn consultation.
How to Prepare
Every hospitalist’s path and skill set is unique, but for those medical students or residents who might be interested in combining some surgical work with hospitalist skills, Dr. Frenz advises adopting a calculated approach to electives. Besides taking as many surgical electives as possible, trainees should try to pick small community hospitals where they will not have to compete with surgical residents for time in the OR.
Although she thinks expanding into surgical assisting could improve recruitment (offering a varied hospital experience), Dr. Cereste also emphasizes that many questions regarding training standards, care standards, and expense hurdles would have to be addressed.
The bottom line, says Dr. Hoffmann, is that hospitalists “need to be able to play a lot of different roles. I think we’re like a utility infielder. If [surgical assisting] improves patient care, is a valuable service to the health system, and is viewed by consultants, specialists, and family doctors as an additional skill, it’s clearly going to benefit your program and your hospital. The key is to see what works in everyone’s little pond and try to be a team builder.” TH
Gretchen Henkel is a medical writer based in California
In this era of increasing synergy between the surgical and hospital medicine services, Minnesota hospitalist David Frenz, MD, has taken perioperative management of surgical patients a step further.
One or two days a week, Dr. Frenz can be found in the operating room (OR) of St. Joseph’s Hospital in St. Paul, assisting on multilevel spine surgery cases.
Although Dr. Frenz may be a one-of-a-kind hospitalist acting as first assistant in the OR, the approach offers many advantages to his hospital and hospital medicine service, says Robert C. Moravec, MD.
“It seems more efficient having one assistant surgeon [rather than several scrub technicians] who knows exactly what’s going to happen next,” says Dr. Moravec, medical director for both the hospital service and St. Joseph’s Hospital. “More importantly, it’s a way to develop some expertise in the perioperative arena and to develop collaborative relationships with the surgeons.” In addition, the hospital service is able to bill for an assistant surgeon’s fee, which covers much of Dr. Frenz’ salary. And when he’s not on the medical floors seeing patients, Dr. Frenz is engaged in a monthslong quality improvement (QI) project to improve perioperative care and reduce same-day surgery cancellations at his institution.
The effectiveness of this QI project, which Dr. Moravec believes will go to HealthEast’s other two acute care hospitals in nine months, would not be possible without Dr. Frenz’ conversance with problems in the OR.
“When you are involved in this type of process improvement project, you don’t want, as a do-gooder, to create more cancellations and delays,” says Dr. Frenz. “And you don’t want to screw up their referral relationships. You’ve got to be super-sensitive to those issues as you’re trying to slowly bring about change. The fact that I’m known to the surgeons and that I’m in the OR getting dirty lends credibility to our efforts to bring change.”
Value in Surgical Assisting?
In medical school, Dr. Frenz had considered becoming a general surgeon before switching to family-practice medicine, so he is comfortable in the OR and finds assisting to be a stimulating change of pace. Although this long-standing pilot project is unique, it raises provocative possibilities for other hospitalists.
“Having a hospitalist go into the OR to assist with cases creates an interesting situation,” says Richard Rohr, MD, vice president for medical affairs at Cortland Regional Medical Center in Cortland, N.Y. “The hospitalist is then able to engage with more surgical aspects of the case, as well as the medical management.” Adding surgical assisting to the hospitalist’s role—although it could complicate scheduling and malpractice coverage—might dovetail with some hospitals’ difficulties retaining general surgeons, he says.
Combining the two functions could add to the hospital medicine group’s bottom line if relevant malpractice costs could be worked out, says hospitalist Kenneth Patrick, MD, the ICU director at Chestnut Hill Hospital in Philadelphia. Dr. Frenz’ malpractice is provided by his hospital, and pre-certification for his assistance on cases is handled by the neurosurgeon’s office staff.
In Dr. Patrick’s experience, there could be benefits to the patient if the hospitalist has direct involvement in the OR. For instance, the hospitalist would be better able to anticipate and deal with pre- and post-operative problems.
—David Frenz, MD, hospitalist, St. Joseph’s Hospital, St. Paul, Minn.
Surgery and ‘Outer Space’
Whether or not surgical assisting could become a new frontier for hospitalists, it illustrates the multiple collaborative roles the specialty increasingly offers.
David A. Hoffmann, MD, is medical director of a hospitalist group in Chambersburg, Pa. The group is made up of half family practice and half internal medicine hospitalists. Like so many other hospitalists, he’s seen tremendous growth in the number of surgical co-management cases his group handles at Chambersburg Hospital (see “The Surgical Surge,” December 2007, p. 1). His group tries “to make inroads with the surgeons,” he says. “We send a member of our group to their meetings, and we work with them on management protocols [such as DVT prophylaxis]. I can see the benefits of getting to know what’s going on down there [in the OR]. The truth of matter is, [despite co-management], sending the patient to the OR is like sending someone into outer space for the hospitalist. The rocket goes off, and you don’t see the patient until they come back in for a landing.”
Depending on the location of hospitalist groups, involvement as first assistants could represent additional opportunities for family medicine physicians, Dr. Hoffmann believes.
Air Force Maj. Heather Cereste, MD, agrees that the degree of symbiosis between surgeons and hospitalists likely will continue to be a location - and hospital-specific phenomenon. While serving in Iraq, she had significant experience with surgical procedures, and felt that from an internist’s perspective, she was more valuable to the surgical team. During her third-year residency in Maine, she observed many who planned to go into family practice assisting with gastrointestinal procedures and the like. “Certainly, in a smaller setting, with fewer available resources, the more autonomous a hospitalist can be, the better,” says Dr. Cereste, co-director of the geriatric medicine service at Wilford Hall Medical Center, Lackland Air Force Base, Texas, and chair of the bioethics committee.
Cautionary Tales
Though surgical assisting is an intriguing idea, such a set up “could have its own set of unintended consequences,” especially for a private model hospitalist group, says Brian Bossard, MD, medical director of Inpatient Physician Associates in Lincoln, Neb.
Dr. Bossard has personal experience with this configuration. When an internist in his hospitalist group began to do surgical assisting, the privately owned group (which contracts with Bryan LGH Hospital in Lincoln to provide hospitalist services) did not find this advantageous. The physician’s surgical participation was at times disruptive for the group, since he was unable to be immediately available and on call or to run codes while in the OR.
“It’s not clear to me that there would be an advantage to have a hospitalist [assisting in the OR], as opposed to another physician extender such as a physician assistant or a nurse practitioner,” says Jack M. Percelay, MD, a pediatric hospitalist at Saint Barnabas Medical Center in Livingston, N.J. Co-management of surgical patients is another matter, however, and Dr. Percelay does see value in having hospitalists help with maintenance of lines, wound care, and other post-surgical management duties.
“There is a certain set of procedures we’re supposed to master, such as vascular access and airway support,” Dr. Percelay continues. “But our value as hospitalists is in our cognitive skill set. I don’t know any hospitalists who consider a scalpel as one of their routine tools.”
Bryan Fine, MD, a pediatric hospital at Children’s National Medical Center in Washington, D.C., recently joined a general hospitalist group after spending three and a half years as the hospitalist in charge of medical management for the gastroenterology service. His opinion of hospitalists assisting in surgery? “I think it’s definitely valuable if it’s done in the context of a larger goal and to gain credibility from a hospital administrative level,” he suggests. However, he said, professional satisfaction for a hospitalist might be limited since he or she essentially would be serving as a physician extender.
Barriers
Family-practice physicians often are differentiated from their internal medicine colleagues by their skill sets in procedures.
“To the extent that a family-medicine physician may want to demonstrate that they can have a skill set that adds value in order to be hired or accepted, I think surgical assisting could have very specific application in specific places,” says A. Neal Axon, MD, assistant professor in the departments of internal medicine and pediatrics at the Medical University of South Carolina in Charleston. “I’ve certainly tried to market myself as a med-peds person, and as somebody who’s good at more than one thing.”
Dr. Axon concedes hospitalists as surgical assistants would not work at his institution. “In academic medical centers, the dividing lines between divisions and disciplines are very concrete,” he explains. “I think many people carry those cultural barriers or dividers—even if they are somewhat artificial outside the academic environment—when they leave and go into community practice.”
Those divisions are not felt as keenly in the Midwest, according to Dr. Frenz, where “family medicine has a long tradition.” St. Joseph’s Hospital has a family - medicine residency program, and more than half the credentialed physicians there are family- medicine trained.
“We think that family-medicine physicians have a skill set that is valuable in certain clinical settings,” he says. “For example, we do a lot of work on the behavioral health floors and are the principal medical providers on a 28-bed chemical dependency unit.” Dr. Frenz had a patient who was pregnant and alcohol dependent. Because of his expertise in addiction medicine (another of his self-described “insurgencies”) and residency training in obstetrics, Dr. Frenz is managing the patient without incurring an ob/gyn consultation.
How to Prepare
Every hospitalist’s path and skill set is unique, but for those medical students or residents who might be interested in combining some surgical work with hospitalist skills, Dr. Frenz advises adopting a calculated approach to electives. Besides taking as many surgical electives as possible, trainees should try to pick small community hospitals where they will not have to compete with surgical residents for time in the OR.
Although she thinks expanding into surgical assisting could improve recruitment (offering a varied hospital experience), Dr. Cereste also emphasizes that many questions regarding training standards, care standards, and expense hurdles would have to be addressed.
The bottom line, says Dr. Hoffmann, is that hospitalists “need to be able to play a lot of different roles. I think we’re like a utility infielder. If [surgical assisting] improves patient care, is a valuable service to the health system, and is viewed by consultants, specialists, and family doctors as an additional skill, it’s clearly going to benefit your program and your hospital. The key is to see what works in everyone’s little pond and try to be a team builder.” TH
Gretchen Henkel is a medical writer based in California
To Serve in America
In the first part of this two-part series, we examined the implications of international medical graduates (IMGs) in hospital medicine groups (November 2007, p. 1). Part 2 features stories from hospitalist IMGs as they establish themselves as professionals in their communities.
December 2005 was a tough time for Charles Onunkwo, MD, and his wife. He had been working since July 1 as a hospitalist with St. Clare’s Hospital in Wausau, a small town in central Wisconsin, and had just received alarming news. His H1-B visa transfer, filed by his immigration attorney, had been denied.
His wife’s application to change from a visitor visa to an H-4 (dependent of an H1-B visa holder) was also denied. As a result, his wife was considered “unlawfully present” in the country. Dr. Onunkwo was now “out of status,” because the Naturalization and Immigration Service (INS) did not recognize St. Clare’s as exempt from caps on the annual number of H1-B visas granted. The couple was faced with a mandatory return trip to their native Nigeria, and no guarantee that the U.S. Consulate in Lagos would grant them permission to return to the United States to work as physicians.
“It was a bad time for us,” he recalls.
Barriers and Adjustments
The obstacles faced by IMGs in obtaining visas and eventual permanent employment status have been well documented.1 For the Onunkwos, the story had a good outcome: a new immigration attorney hired by St. Clare’s was able to establish the hospital as a “cap-exempt” organization. Intervention by the staff of Rep. David R. Obey, D-Wis., allowed them to secure new H-1B visas and a return to this country.
Dr. Onunkwo and the other hospitalist IMGs attest that immigration hurdles constitute their biggest challenges.
There can be other barriers as well. Mark Dotson, senior recruiter for Cogent Healthcare in Nashville, Tenn., has encountered resistance toward IMG candidates from hospital administrators in some communities. Concerns usually relate to candidates’ ability to communicate effectively and demonstrate appropriate bedside manner. “There are also some misperceptions about some residency programs that can hinder an international medical graduate,” he says. In addition, some communities “want the doctors to reflect the makeup of the local community.” That means in a community that is 95% Caucasian, hospital administrators may be reluctant to hire a physician of color.
Dotson says attention to communication skills should be the primary goal of IMGs, and that buy-in from hospital administrators or leaders of hospital medicine groups is critical for smooth transitions. “I think some of the best physicians we have out there are doctors who are international medical graduates who see this as their life calling,” he says. “And, I think that even people in the general population understand that IMGs are extremely intelligent, and that they work extremely hard.”
As the following stories affirm, communities in remote or medically underserved areas are often welcoming of physicians who offer much-needed primary care.
A Long Journey
In 1997, Emmanuel Fajardo, MD, medical director of the hospitalist program at St. Dominic-Jackson Memorial Hospital in Jackson, Miss., found himself “between the devil and the deep blue sea.” He had just been offered a chief residency position at the Meharry Medical College Affiliated Hospitals Internal Medicine residency program and was torn between accepting that job and a J-1 waiver offer in Shubuta, Miss., a federally designated Medically Underserved Area (MUSA).
He had been waiting a full year for the J-1 visa waiver, which allows IMGs to remain in the U.S. in exchange for five years of service in an MUSA. But, he also liked teaching and was attracted to the opportunity to pass on a legacy to the junior residents and incoming interns. He elected to proceed with the waiver because it offered the opportunity to “stay here in the States and to be able to practice medicine for good.”
Born in the Philippines, Dr. Fajardo says his family was wary about his locating to a remote area in Mississippi—but he wasn’t. “When I make a decision, I go for it 100%,” he says. “In everything I do I always do my best and leave the rest to God. I was very fortunate to find out that the community was very involved in and engaged with my waiver.
“Also, to my surprise, I didn’t feel discriminated against at all. They made me feel like I’m a part of the family. There is a strong sense of community here, indeed. The only problem then was, of course, being in a small town, that whatever you do, everybody knows about it.”
Although Dr. Onunkwo moved to Wausau, Wis., a small town in a predominantly white area, he says it was not difficult for him to adjust to life there. Part of the reason, he says, is that his first overseas experience was in Ireland, where he obtained a diploma in tropical medical at the Royal College of Surgeons in Dublin and practiced in a small village nearby. In addition, he and his wife were together in Wausau. “It was probably easier for both of us because we had each other,” he says.
And then there were their great neighbors, says Dr. Onunkwo. ”They made the transition seamless,” he says. “We have formed lifelong relationships with some of our neighbors in Wausau.” The strength of those relationships became apparent on Christmas Day 2005. “They really don’t know what they have done for us,” Dr. Onunkwo recalls warmly. “When we were going through our travails, they knew something was wrong, but we didn’t tell them exactly what we were going through. They made our day for us, because they just rang our bell and here they had the three-course Christmas dinner for us.”
Prove Yourself
Dr. Onunkwo has been aware of misperceptions about his professional competency. “Depending on what part of the country you find yourself in, you need to continually prove yourself,” he says. “There is this perception, maybe due to the accent or the way you express yourself. It’s unspoken, but it’s there and you don’t need to be a rocket scientist to observe that. You need to prove that you’re good to be able to survive.”
This is easier for some than others.
“I cannot say I have experienced any barriers in that respect,” reports Gunter Kurrle, MD, lead physician with the WellStar Kennestone Hospitalist Group in Atlanta. “I’m European, like most Americans with European background, so it has not been my personal experience to encounter prejudice.” Dr. Kurrle’s journey to his present post as lead hospitalist is also atypical compared with most IMGs who come to the U.S. He initially took his foreign medical graduate examination in the late 1980s, just before the United States Medical Licensing Examination was initiated. He then returned to Germany for five years of additional training after his residency in this country. He came back to the U.S. for personal reasons (his wife is a U.S. citizen and was starting her residency training here) and found that entering hospital medicine was “a better fit than trying to start a practice on my own.”
Hemant Patel, MD, president of the American Association of Physicians of Indian Origin (AAIP), based in Oak Brook, Ill., believes discrimination toward foreign-born physicians has been greatly reduced since the early 1980s, when he entered the country. AAPI, with membership of 45,000, was founded in 1982 to offer support to IMGs from India. Physicians of Indian origin constitute the largest group of IMGs.2
“At that time, it was very difficult to obtain residency slots due to competition, and we had a lot more physicians to occupy those slots,” says Dr. Patel.
Dr. Fajardo believes the inclination to discriminate is inherent in everyone: “It’s latent, but if you give them the reason to discriminate against you, then it will manifest.” With regards to the physician-patient relationship, Dr. Fajardo reports that initially, on rare occasions, he encountered resistance from patients who were reluctant to trust their care to him because of his name (“I can’t pronounce it—are you a terrorist?”) or his looks (“You look too young to be a doctor—are you sure you can take care of me?”).
“At the end of the day, it’s very fulfilling when you hear them say, ‘Thanks a lot, doc, for getting me better,’’ says Dr. Fajardo. “I believe that it isn’t where you come from that matters; it’s what you can do.” Overall, he says, the realities of the medical profession are that “the outcome of what we do speaks for itself, and that’s what matters most.”
Dr. Onunkwo is philosophical about the initial skepticism he sometimes senses from patients and other colleagues. “I understand that people are wary of the unknown, and I think it’s just natural,” he says. “Usually, what happens in my situation is that I feel the skepticism, but I don’t do anything about it. I still treat the person with the respect that they deserve and ultimately, I just let my work do the talking. Everybody gets the same level of respect and attention that they need and nine times out of 10, before patients are done with their hospital stay, their attitudes toward me have changed.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
References
- Leon LR Jr, Villar H, Leon CR, et al. The journey of a foreign-trained physician to a United States residency. J Am Coll Surg. 2007 Mar;204(3):486-494.
- Hart LG, Skillman SM, Fordyce M, et al. International medical graduate physicians in the United States: changes since 1981. Health Aff. 2007 Jul/Aug;26(4):1159-1169.
In the first part of this two-part series, we examined the implications of international medical graduates (IMGs) in hospital medicine groups (November 2007, p. 1). Part 2 features stories from hospitalist IMGs as they establish themselves as professionals in their communities.
December 2005 was a tough time for Charles Onunkwo, MD, and his wife. He had been working since July 1 as a hospitalist with St. Clare’s Hospital in Wausau, a small town in central Wisconsin, and had just received alarming news. His H1-B visa transfer, filed by his immigration attorney, had been denied.
His wife’s application to change from a visitor visa to an H-4 (dependent of an H1-B visa holder) was also denied. As a result, his wife was considered “unlawfully present” in the country. Dr. Onunkwo was now “out of status,” because the Naturalization and Immigration Service (INS) did not recognize St. Clare’s as exempt from caps on the annual number of H1-B visas granted. The couple was faced with a mandatory return trip to their native Nigeria, and no guarantee that the U.S. Consulate in Lagos would grant them permission to return to the United States to work as physicians.
“It was a bad time for us,” he recalls.
Barriers and Adjustments
The obstacles faced by IMGs in obtaining visas and eventual permanent employment status have been well documented.1 For the Onunkwos, the story had a good outcome: a new immigration attorney hired by St. Clare’s was able to establish the hospital as a “cap-exempt” organization. Intervention by the staff of Rep. David R. Obey, D-Wis., allowed them to secure new H-1B visas and a return to this country.
Dr. Onunkwo and the other hospitalist IMGs attest that immigration hurdles constitute their biggest challenges.
There can be other barriers as well. Mark Dotson, senior recruiter for Cogent Healthcare in Nashville, Tenn., has encountered resistance toward IMG candidates from hospital administrators in some communities. Concerns usually relate to candidates’ ability to communicate effectively and demonstrate appropriate bedside manner. “There are also some misperceptions about some residency programs that can hinder an international medical graduate,” he says. In addition, some communities “want the doctors to reflect the makeup of the local community.” That means in a community that is 95% Caucasian, hospital administrators may be reluctant to hire a physician of color.
Dotson says attention to communication skills should be the primary goal of IMGs, and that buy-in from hospital administrators or leaders of hospital medicine groups is critical for smooth transitions. “I think some of the best physicians we have out there are doctors who are international medical graduates who see this as their life calling,” he says. “And, I think that even people in the general population understand that IMGs are extremely intelligent, and that they work extremely hard.”
As the following stories affirm, communities in remote or medically underserved areas are often welcoming of physicians who offer much-needed primary care.
A Long Journey
In 1997, Emmanuel Fajardo, MD, medical director of the hospitalist program at St. Dominic-Jackson Memorial Hospital in Jackson, Miss., found himself “between the devil and the deep blue sea.” He had just been offered a chief residency position at the Meharry Medical College Affiliated Hospitals Internal Medicine residency program and was torn between accepting that job and a J-1 waiver offer in Shubuta, Miss., a federally designated Medically Underserved Area (MUSA).
He had been waiting a full year for the J-1 visa waiver, which allows IMGs to remain in the U.S. in exchange for five years of service in an MUSA. But, he also liked teaching and was attracted to the opportunity to pass on a legacy to the junior residents and incoming interns. He elected to proceed with the waiver because it offered the opportunity to “stay here in the States and to be able to practice medicine for good.”
Born in the Philippines, Dr. Fajardo says his family was wary about his locating to a remote area in Mississippi—but he wasn’t. “When I make a decision, I go for it 100%,” he says. “In everything I do I always do my best and leave the rest to God. I was very fortunate to find out that the community was very involved in and engaged with my waiver.
“Also, to my surprise, I didn’t feel discriminated against at all. They made me feel like I’m a part of the family. There is a strong sense of community here, indeed. The only problem then was, of course, being in a small town, that whatever you do, everybody knows about it.”
Although Dr. Onunkwo moved to Wausau, Wis., a small town in a predominantly white area, he says it was not difficult for him to adjust to life there. Part of the reason, he says, is that his first overseas experience was in Ireland, where he obtained a diploma in tropical medical at the Royal College of Surgeons in Dublin and practiced in a small village nearby. In addition, he and his wife were together in Wausau. “It was probably easier for both of us because we had each other,” he says.
And then there were their great neighbors, says Dr. Onunkwo. ”They made the transition seamless,” he says. “We have formed lifelong relationships with some of our neighbors in Wausau.” The strength of those relationships became apparent on Christmas Day 2005. “They really don’t know what they have done for us,” Dr. Onunkwo recalls warmly. “When we were going through our travails, they knew something was wrong, but we didn’t tell them exactly what we were going through. They made our day for us, because they just rang our bell and here they had the three-course Christmas dinner for us.”
Prove Yourself
Dr. Onunkwo has been aware of misperceptions about his professional competency. “Depending on what part of the country you find yourself in, you need to continually prove yourself,” he says. “There is this perception, maybe due to the accent or the way you express yourself. It’s unspoken, but it’s there and you don’t need to be a rocket scientist to observe that. You need to prove that you’re good to be able to survive.”
This is easier for some than others.
“I cannot say I have experienced any barriers in that respect,” reports Gunter Kurrle, MD, lead physician with the WellStar Kennestone Hospitalist Group in Atlanta. “I’m European, like most Americans with European background, so it has not been my personal experience to encounter prejudice.” Dr. Kurrle’s journey to his present post as lead hospitalist is also atypical compared with most IMGs who come to the U.S. He initially took his foreign medical graduate examination in the late 1980s, just before the United States Medical Licensing Examination was initiated. He then returned to Germany for five years of additional training after his residency in this country. He came back to the U.S. for personal reasons (his wife is a U.S. citizen and was starting her residency training here) and found that entering hospital medicine was “a better fit than trying to start a practice on my own.”
Hemant Patel, MD, president of the American Association of Physicians of Indian Origin (AAIP), based in Oak Brook, Ill., believes discrimination toward foreign-born physicians has been greatly reduced since the early 1980s, when he entered the country. AAPI, with membership of 45,000, was founded in 1982 to offer support to IMGs from India. Physicians of Indian origin constitute the largest group of IMGs.2
“At that time, it was very difficult to obtain residency slots due to competition, and we had a lot more physicians to occupy those slots,” says Dr. Patel.
Dr. Fajardo believes the inclination to discriminate is inherent in everyone: “It’s latent, but if you give them the reason to discriminate against you, then it will manifest.” With regards to the physician-patient relationship, Dr. Fajardo reports that initially, on rare occasions, he encountered resistance from patients who were reluctant to trust their care to him because of his name (“I can’t pronounce it—are you a terrorist?”) or his looks (“You look too young to be a doctor—are you sure you can take care of me?”).
“At the end of the day, it’s very fulfilling when you hear them say, ‘Thanks a lot, doc, for getting me better,’’ says Dr. Fajardo. “I believe that it isn’t where you come from that matters; it’s what you can do.” Overall, he says, the realities of the medical profession are that “the outcome of what we do speaks for itself, and that’s what matters most.”
Dr. Onunkwo is philosophical about the initial skepticism he sometimes senses from patients and other colleagues. “I understand that people are wary of the unknown, and I think it’s just natural,” he says. “Usually, what happens in my situation is that I feel the skepticism, but I don’t do anything about it. I still treat the person with the respect that they deserve and ultimately, I just let my work do the talking. Everybody gets the same level of respect and attention that they need and nine times out of 10, before patients are done with their hospital stay, their attitudes toward me have changed.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
References
- Leon LR Jr, Villar H, Leon CR, et al. The journey of a foreign-trained physician to a United States residency. J Am Coll Surg. 2007 Mar;204(3):486-494.
- Hart LG, Skillman SM, Fordyce M, et al. International medical graduate physicians in the United States: changes since 1981. Health Aff. 2007 Jul/Aug;26(4):1159-1169.
In the first part of this two-part series, we examined the implications of international medical graduates (IMGs) in hospital medicine groups (November 2007, p. 1). Part 2 features stories from hospitalist IMGs as they establish themselves as professionals in their communities.
December 2005 was a tough time for Charles Onunkwo, MD, and his wife. He had been working since July 1 as a hospitalist with St. Clare’s Hospital in Wausau, a small town in central Wisconsin, and had just received alarming news. His H1-B visa transfer, filed by his immigration attorney, had been denied.
His wife’s application to change from a visitor visa to an H-4 (dependent of an H1-B visa holder) was also denied. As a result, his wife was considered “unlawfully present” in the country. Dr. Onunkwo was now “out of status,” because the Naturalization and Immigration Service (INS) did not recognize St. Clare’s as exempt from caps on the annual number of H1-B visas granted. The couple was faced with a mandatory return trip to their native Nigeria, and no guarantee that the U.S. Consulate in Lagos would grant them permission to return to the United States to work as physicians.
“It was a bad time for us,” he recalls.
Barriers and Adjustments
The obstacles faced by IMGs in obtaining visas and eventual permanent employment status have been well documented.1 For the Onunkwos, the story had a good outcome: a new immigration attorney hired by St. Clare’s was able to establish the hospital as a “cap-exempt” organization. Intervention by the staff of Rep. David R. Obey, D-Wis., allowed them to secure new H-1B visas and a return to this country.
Dr. Onunkwo and the other hospitalist IMGs attest that immigration hurdles constitute their biggest challenges.
There can be other barriers as well. Mark Dotson, senior recruiter for Cogent Healthcare in Nashville, Tenn., has encountered resistance toward IMG candidates from hospital administrators in some communities. Concerns usually relate to candidates’ ability to communicate effectively and demonstrate appropriate bedside manner. “There are also some misperceptions about some residency programs that can hinder an international medical graduate,” he says. In addition, some communities “want the doctors to reflect the makeup of the local community.” That means in a community that is 95% Caucasian, hospital administrators may be reluctant to hire a physician of color.
Dotson says attention to communication skills should be the primary goal of IMGs, and that buy-in from hospital administrators or leaders of hospital medicine groups is critical for smooth transitions. “I think some of the best physicians we have out there are doctors who are international medical graduates who see this as their life calling,” he says. “And, I think that even people in the general population understand that IMGs are extremely intelligent, and that they work extremely hard.”
As the following stories affirm, communities in remote or medically underserved areas are often welcoming of physicians who offer much-needed primary care.
A Long Journey
In 1997, Emmanuel Fajardo, MD, medical director of the hospitalist program at St. Dominic-Jackson Memorial Hospital in Jackson, Miss., found himself “between the devil and the deep blue sea.” He had just been offered a chief residency position at the Meharry Medical College Affiliated Hospitals Internal Medicine residency program and was torn between accepting that job and a J-1 waiver offer in Shubuta, Miss., a federally designated Medically Underserved Area (MUSA).
He had been waiting a full year for the J-1 visa waiver, which allows IMGs to remain in the U.S. in exchange for five years of service in an MUSA. But, he also liked teaching and was attracted to the opportunity to pass on a legacy to the junior residents and incoming interns. He elected to proceed with the waiver because it offered the opportunity to “stay here in the States and to be able to practice medicine for good.”
Born in the Philippines, Dr. Fajardo says his family was wary about his locating to a remote area in Mississippi—but he wasn’t. “When I make a decision, I go for it 100%,” he says. “In everything I do I always do my best and leave the rest to God. I was very fortunate to find out that the community was very involved in and engaged with my waiver.
“Also, to my surprise, I didn’t feel discriminated against at all. They made me feel like I’m a part of the family. There is a strong sense of community here, indeed. The only problem then was, of course, being in a small town, that whatever you do, everybody knows about it.”
Although Dr. Onunkwo moved to Wausau, Wis., a small town in a predominantly white area, he says it was not difficult for him to adjust to life there. Part of the reason, he says, is that his first overseas experience was in Ireland, where he obtained a diploma in tropical medical at the Royal College of Surgeons in Dublin and practiced in a small village nearby. In addition, he and his wife were together in Wausau. “It was probably easier for both of us because we had each other,” he says.
And then there were their great neighbors, says Dr. Onunkwo. ”They made the transition seamless,” he says. “We have formed lifelong relationships with some of our neighbors in Wausau.” The strength of those relationships became apparent on Christmas Day 2005. “They really don’t know what they have done for us,” Dr. Onunkwo recalls warmly. “When we were going through our travails, they knew something was wrong, but we didn’t tell them exactly what we were going through. They made our day for us, because they just rang our bell and here they had the three-course Christmas dinner for us.”
Prove Yourself
Dr. Onunkwo has been aware of misperceptions about his professional competency. “Depending on what part of the country you find yourself in, you need to continually prove yourself,” he says. “There is this perception, maybe due to the accent or the way you express yourself. It’s unspoken, but it’s there and you don’t need to be a rocket scientist to observe that. You need to prove that you’re good to be able to survive.”
This is easier for some than others.
“I cannot say I have experienced any barriers in that respect,” reports Gunter Kurrle, MD, lead physician with the WellStar Kennestone Hospitalist Group in Atlanta. “I’m European, like most Americans with European background, so it has not been my personal experience to encounter prejudice.” Dr. Kurrle’s journey to his present post as lead hospitalist is also atypical compared with most IMGs who come to the U.S. He initially took his foreign medical graduate examination in the late 1980s, just before the United States Medical Licensing Examination was initiated. He then returned to Germany for five years of additional training after his residency in this country. He came back to the U.S. for personal reasons (his wife is a U.S. citizen and was starting her residency training here) and found that entering hospital medicine was “a better fit than trying to start a practice on my own.”
Hemant Patel, MD, president of the American Association of Physicians of Indian Origin (AAIP), based in Oak Brook, Ill., believes discrimination toward foreign-born physicians has been greatly reduced since the early 1980s, when he entered the country. AAPI, with membership of 45,000, was founded in 1982 to offer support to IMGs from India. Physicians of Indian origin constitute the largest group of IMGs.2
“At that time, it was very difficult to obtain residency slots due to competition, and we had a lot more physicians to occupy those slots,” says Dr. Patel.
Dr. Fajardo believes the inclination to discriminate is inherent in everyone: “It’s latent, but if you give them the reason to discriminate against you, then it will manifest.” With regards to the physician-patient relationship, Dr. Fajardo reports that initially, on rare occasions, he encountered resistance from patients who were reluctant to trust their care to him because of his name (“I can’t pronounce it—are you a terrorist?”) or his looks (“You look too young to be a doctor—are you sure you can take care of me?”).
“At the end of the day, it’s very fulfilling when you hear them say, ‘Thanks a lot, doc, for getting me better,’’ says Dr. Fajardo. “I believe that it isn’t where you come from that matters; it’s what you can do.” Overall, he says, the realities of the medical profession are that “the outcome of what we do speaks for itself, and that’s what matters most.”
Dr. Onunkwo is philosophical about the initial skepticism he sometimes senses from patients and other colleagues. “I understand that people are wary of the unknown, and I think it’s just natural,” he says. “Usually, what happens in my situation is that I feel the skepticism, but I don’t do anything about it. I still treat the person with the respect that they deserve and ultimately, I just let my work do the talking. Everybody gets the same level of respect and attention that they need and nine times out of 10, before patients are done with their hospital stay, their attitudes toward me have changed.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
References
- Leon LR Jr, Villar H, Leon CR, et al. The journey of a foreign-trained physician to a United States residency. J Am Coll Surg. 2007 Mar;204(3):486-494.
- Hart LG, Skillman SM, Fordyce M, et al. International medical graduate physicians in the United States: changes since 1981. Health Aff. 2007 Jul/Aug;26(4):1159-1169.
New Perspective
Chris Hamerski, MD, a third-year resident, was nervous. In Uganda with the Global Health Scholars Program at the University of California, San Francisco (UCSF), he and a fellow resident were scheduled to accompany a physician and a social worker on a Hospice Uganda home visit.
Now back at UCSF between shifts on his current inpatient rotation, Dr. Hamerski recalls his reluctance: “Going into someone’s home is such an intimate experience, and I was a little worried about how we were going to be viewed.”
He needn’t have worried. Despite the startled reactions from young village boys who stopped in their tracks and put down the water jugs they were carrying to stare at the visiting Caucasian doctors, the patients were “very welcoming and gracious, and happy that someone was there to look after them,” he says.
In addition to his time with Hospice Uganda, Dr. Hamerski also worked at Mulago Hospital in Kampala and the Reach-Out Mbuya Clinic, set up to serve patients with HIV/AIDS. “I found the clinic to be very uplifting and inspiring,” he says. “I think it actually works better than clinics in the U.S. because it was an all-in-one clinic, with a holistic approach to the patient.” Not only do patients see a doctor and obtain refills on the spot of their antiretroviral drugs, he explained, but they also have access to a social worker and can obtain money to send their children to school or a micro-loan to help start a business. “It was definitely inspiring to see patients living with HIV doing well in the community,” says Dr. Hamerski. “It made you feel that the clinic was making a difference and having a positive effect on the health of the community.”
Hospitalists, residents, and directors of global health programs stress that international health experiences not only broaden physicians’ perspectives but improve their approach to diagnosis and use of resources when they return to working in U.S. hospitals.
“In their one-month immersions, people have the ability to see and effect change in a more direct way,” points out hospitalist Madhavi Dandu, MD, MPH, assistant clinical professor of medicine and director of UCSF’s Global Health Scholars Program for the Internal Medicine Residency.
Nearly 60% of American medical schools offer global health electives, according to a 2004-2005 survey by the American Association of Medical Colleges—and demand is increasing. The value of a stint abroad for any physician is irrefutable, says hospitalist Tracy Minichiello, MD, who founded the UCSF Global Health Scholars program.
Dr. Hamerski chose to do the global health elective because he wanted to “be more excited about medicine. At the end of residency, it can be a little hard to keep that positive outlook.”
Residents and physicians who complete international health elective courses (typically lasting one or two months) say the experience can greatly influence career choice. Many participants choose to practice with underserved populations or go on to specialize in global medicine.1 But even physicians who do not continue on to a career in global health reap huge benefits as practitioners.
Dr. Dandu has experienced those benefits, both as a resident and now as a visiting director of programs. Through participation in global health electives, she observes, “there is a palpable rejuvenation that occurs, a reminder of some of the enthusiasm that comes from practicing medicine with a little less of the structural issues that make the U.S. healthcare system difficult.”
Less Can Teach More
The Global Health Track of the University of Pittsburgh Internal Medicine Residency Program emphasizes “a generalist perspective, cost-conscious practice and back-to-basics diagnosis”—competencies that dovetail with the mission of hospital medicine.
“The major component of an international health elective is to really improve their [residents’] clinical skills,” notes Thuy D. Bui, MD, director of UPMC’s Global Health Track and medical director of the Program for Health Care to Underserved Populations. This clinical skills improvement is facilitated by the often-limited resources in host countries. “There is no CT, and there are no fancy blood tests, so they [the residents] really have to rely on their clinical acumen to make the diagnosis,” she says.
Dr. Bui has observed that when residents return from a global health elective (the UPMC program has centers in Malawi, India, Japan, Honduras, and Italy), they are “better at picking the right test, knowing when to be more aggressive [with treatment], and are more comfortable with ‘watchful waiting,’ rather than following up every single abnormality they detect in blood work or other imaging studies.”
Franziska Jovin, MD, is medical director of inpatient services at the University of Pittsburgh Medical Center (UPMC) Hospital Medicine Program. Originally from Romania, Dr. Jovin attended medical school in Germany, did her internship in the United Kingdom, and completed her residency in the U.S. During her residency, she returned to Romania on an international elective.
“I think the biggest thing you gain from doing an outside elective is that you learn to really practice medicine the way it used to be in the old days,” she says. “You rely much more on your clinical exam—and get better at it—because at the end of your exam, you have to formulate a differential diagnosis and a treatment plan without always confirming your hypothesis with a test.”
Practicing in another healthcare delivery system can also expand physicians’ perspectives on use of resources. Even though healthcare is funded by the government in many developing countries, says Dr. Jovin, patients still have to pay a large fee for the tests doctors order. “When patients have to pay for the studies that you order, it is much less likely that you will order a battery of tests, and instead concentrate on the test with the highest likely yield first,” she says.
While on elective in Romania, Dr. Jovin practiced in both an outpatient clinic and a hospital setting. She learned that physicians can “stay basic” by using equivalent generic medications to treat conditions such as hypertension. “Here in the U.S., you can use the latest ACE inhibitor or calcium-channel blocker and spend a lot of your patient’s money,” she says. “When money becomes an issue in order to effectively treat a patient, you’re much more cost-conscious.”
On-the-Job Training
Another eye opener for those who go abroad is the chance to observe differences in practice and learn about physician training. “In many countries there is very little structured training after graduation from medical school,” notes Dr. Jovin. “Young doctors learn by following more senior doctors around; it is more an apprenticeship-type training. In many rural areas, fresh medical school graduates may be practicing alone with very limited diagnostic and treatment tools.”
Tanyaporn Wansom, MSIV, a fourth-year medical student at the University of Michigan Medical School in Ann Arbor, is the 2007-2008 chair of the Global Health Action Committee for the American Medical Student Association. During her 2006-2007 stay in Thailand (as an NIH/Fogarty Global Health and Clinical Research Fellow at the Research Institute for the Health Sciences, Chiang Mai University), she was especially impressed with the broad range of diagnostic skills possessed by her supervisor, an infectious diseases (ID) fellow. “For example, I know how to do a lumbar puncture if I am worried about the possibility of meningitis,” she says. “I know how to put the [cerebrospinal] fluid in a tube and send it to the lab. But there, my ID fellow knew how to do all the stains herself, and was able to make immediate diagnoses. There are strengths to the specialization of the American healthcare system, but it is amazing to go abroad and see what other doctors can do.”
This impression is echoed in evaluation forms from the UCSF Global Health Scholars Program, says Dr. Dandu. “One of the common comments is, ‘I’m incredibly impressed by my colleagues abroad because of their amazing physical exam skills,’ ” she says. She believes the exigencies of medical practice in the United States (reliance on testing, adherence to reporting, and regulatory requirements) often mean residents and physicians do not have “the space to focus on the physical exam or the patient’s history. And sometimes, with the way we practice medicine here, it can take longer to see the fruits of what we do and see. In their one-month immersions, people have the ability to see and effect change in a more direct way.”
Rare Encounters
Wansom, who is Thai-American, was motivated to work abroad by her curiosity about her ancestral roots and her commitment to working with people living with HIV/AIDS. She found the physician-patient relationship quite different in Thailand. “Patients look up to you, almost as they would a deity,” she says. “Sometimes it is hard to get their real input on what they are feeling. You may think, because they are nodding, that they are agreeing with everything you say and are totally compliant. In fact, the opposite may be true.”
It is this kind of sensitizing experience that can improve clinicians’ skills when they return to the States, says Dr. Bui. At tertiary care centers such as UPMC, a large transplant center, hospitalists are likely to encounter people from all over the world. “If they have interacted with people from a different culture, they can deal with our [mix of] inpatients better,” she says.
Another significant benefit of traveling to developing countries is that residents get a chance to treat diseases rarely seen in the United States, says Dr. Bui. For instance, she says: “A resident who had treated patients with dengue fever during his clinical elective in India would be quick to include this differential in a returning traveler from Central America admitted to our hospital with fever, headache, myalgia, and a rash. Having seen some of those diseases during their international elective, residents are more comfortable with managing those kinds of diseases, such as when treating travelers who come back with malaria.”
Integrated Care
“Global health electives have tremendous impact in terms of allowing people to experience firsthand the inequalities that exist in global health, and the social and political determinants that cause them,” says Wansom. Those who have the experience “get a snapshot as to how another healthcare system with limited resources is able to provide care to its people and [are] exposed to disease processes and situations that you may not be familiar with from training in the American medical system.”
International health programs at medical schools are growing to accommodate increased demand for overseas experience. UCSF’s residency program formalized residents’ experiences and developed partnership agreements with programs in other countries—ensuring sustainable benefits to hosting countries. The Global Health Scholars Program has sites in Uganda, Saipan, China, and Kenya.
Dr. Dandu believes electives abroad can also offer hospitalists and hospitalists-to-be insight into hand-offs. “One of the central issues for hospitalists is how we help people transition into and out of the hospital,” she explains. “Many of us, as hospitalists, struggle with the fact that we sometimes lose track of our patients when they leave the hospital. One beautiful aspect of many international programs is that residents have an experience with a more holistic approach to care.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ramsey AH, Haq C, Gjerde CL, et al. Career influence of an international health experience during medical school. Fam Med. 2004 June;36(6):412-416.
Chris Hamerski, MD, a third-year resident, was nervous. In Uganda with the Global Health Scholars Program at the University of California, San Francisco (UCSF), he and a fellow resident were scheduled to accompany a physician and a social worker on a Hospice Uganda home visit.
Now back at UCSF between shifts on his current inpatient rotation, Dr. Hamerski recalls his reluctance: “Going into someone’s home is such an intimate experience, and I was a little worried about how we were going to be viewed.”
He needn’t have worried. Despite the startled reactions from young village boys who stopped in their tracks and put down the water jugs they were carrying to stare at the visiting Caucasian doctors, the patients were “very welcoming and gracious, and happy that someone was there to look after them,” he says.
In addition to his time with Hospice Uganda, Dr. Hamerski also worked at Mulago Hospital in Kampala and the Reach-Out Mbuya Clinic, set up to serve patients with HIV/AIDS. “I found the clinic to be very uplifting and inspiring,” he says. “I think it actually works better than clinics in the U.S. because it was an all-in-one clinic, with a holistic approach to the patient.” Not only do patients see a doctor and obtain refills on the spot of their antiretroviral drugs, he explained, but they also have access to a social worker and can obtain money to send their children to school or a micro-loan to help start a business. “It was definitely inspiring to see patients living with HIV doing well in the community,” says Dr. Hamerski. “It made you feel that the clinic was making a difference and having a positive effect on the health of the community.”
Hospitalists, residents, and directors of global health programs stress that international health experiences not only broaden physicians’ perspectives but improve their approach to diagnosis and use of resources when they return to working in U.S. hospitals.
“In their one-month immersions, people have the ability to see and effect change in a more direct way,” points out hospitalist Madhavi Dandu, MD, MPH, assistant clinical professor of medicine and director of UCSF’s Global Health Scholars Program for the Internal Medicine Residency.
Nearly 60% of American medical schools offer global health electives, according to a 2004-2005 survey by the American Association of Medical Colleges—and demand is increasing. The value of a stint abroad for any physician is irrefutable, says hospitalist Tracy Minichiello, MD, who founded the UCSF Global Health Scholars program.
Dr. Hamerski chose to do the global health elective because he wanted to “be more excited about medicine. At the end of residency, it can be a little hard to keep that positive outlook.”
Residents and physicians who complete international health elective courses (typically lasting one or two months) say the experience can greatly influence career choice. Many participants choose to practice with underserved populations or go on to specialize in global medicine.1 But even physicians who do not continue on to a career in global health reap huge benefits as practitioners.
Dr. Dandu has experienced those benefits, both as a resident and now as a visiting director of programs. Through participation in global health electives, she observes, “there is a palpable rejuvenation that occurs, a reminder of some of the enthusiasm that comes from practicing medicine with a little less of the structural issues that make the U.S. healthcare system difficult.”
Less Can Teach More
The Global Health Track of the University of Pittsburgh Internal Medicine Residency Program emphasizes “a generalist perspective, cost-conscious practice and back-to-basics diagnosis”—competencies that dovetail with the mission of hospital medicine.
“The major component of an international health elective is to really improve their [residents’] clinical skills,” notes Thuy D. Bui, MD, director of UPMC’s Global Health Track and medical director of the Program for Health Care to Underserved Populations. This clinical skills improvement is facilitated by the often-limited resources in host countries. “There is no CT, and there are no fancy blood tests, so they [the residents] really have to rely on their clinical acumen to make the diagnosis,” she says.
Dr. Bui has observed that when residents return from a global health elective (the UPMC program has centers in Malawi, India, Japan, Honduras, and Italy), they are “better at picking the right test, knowing when to be more aggressive [with treatment], and are more comfortable with ‘watchful waiting,’ rather than following up every single abnormality they detect in blood work or other imaging studies.”
Franziska Jovin, MD, is medical director of inpatient services at the University of Pittsburgh Medical Center (UPMC) Hospital Medicine Program. Originally from Romania, Dr. Jovin attended medical school in Germany, did her internship in the United Kingdom, and completed her residency in the U.S. During her residency, she returned to Romania on an international elective.
“I think the biggest thing you gain from doing an outside elective is that you learn to really practice medicine the way it used to be in the old days,” she says. “You rely much more on your clinical exam—and get better at it—because at the end of your exam, you have to formulate a differential diagnosis and a treatment plan without always confirming your hypothesis with a test.”
Practicing in another healthcare delivery system can also expand physicians’ perspectives on use of resources. Even though healthcare is funded by the government in many developing countries, says Dr. Jovin, patients still have to pay a large fee for the tests doctors order. “When patients have to pay for the studies that you order, it is much less likely that you will order a battery of tests, and instead concentrate on the test with the highest likely yield first,” she says.
While on elective in Romania, Dr. Jovin practiced in both an outpatient clinic and a hospital setting. She learned that physicians can “stay basic” by using equivalent generic medications to treat conditions such as hypertension. “Here in the U.S., you can use the latest ACE inhibitor or calcium-channel blocker and spend a lot of your patient’s money,” she says. “When money becomes an issue in order to effectively treat a patient, you’re much more cost-conscious.”
On-the-Job Training
Another eye opener for those who go abroad is the chance to observe differences in practice and learn about physician training. “In many countries there is very little structured training after graduation from medical school,” notes Dr. Jovin. “Young doctors learn by following more senior doctors around; it is more an apprenticeship-type training. In many rural areas, fresh medical school graduates may be practicing alone with very limited diagnostic and treatment tools.”
Tanyaporn Wansom, MSIV, a fourth-year medical student at the University of Michigan Medical School in Ann Arbor, is the 2007-2008 chair of the Global Health Action Committee for the American Medical Student Association. During her 2006-2007 stay in Thailand (as an NIH/Fogarty Global Health and Clinical Research Fellow at the Research Institute for the Health Sciences, Chiang Mai University), she was especially impressed with the broad range of diagnostic skills possessed by her supervisor, an infectious diseases (ID) fellow. “For example, I know how to do a lumbar puncture if I am worried about the possibility of meningitis,” she says. “I know how to put the [cerebrospinal] fluid in a tube and send it to the lab. But there, my ID fellow knew how to do all the stains herself, and was able to make immediate diagnoses. There are strengths to the specialization of the American healthcare system, but it is amazing to go abroad and see what other doctors can do.”
This impression is echoed in evaluation forms from the UCSF Global Health Scholars Program, says Dr. Dandu. “One of the common comments is, ‘I’m incredibly impressed by my colleagues abroad because of their amazing physical exam skills,’ ” she says. She believes the exigencies of medical practice in the United States (reliance on testing, adherence to reporting, and regulatory requirements) often mean residents and physicians do not have “the space to focus on the physical exam or the patient’s history. And sometimes, with the way we practice medicine here, it can take longer to see the fruits of what we do and see. In their one-month immersions, people have the ability to see and effect change in a more direct way.”
Rare Encounters
Wansom, who is Thai-American, was motivated to work abroad by her curiosity about her ancestral roots and her commitment to working with people living with HIV/AIDS. She found the physician-patient relationship quite different in Thailand. “Patients look up to you, almost as they would a deity,” she says. “Sometimes it is hard to get their real input on what they are feeling. You may think, because they are nodding, that they are agreeing with everything you say and are totally compliant. In fact, the opposite may be true.”
It is this kind of sensitizing experience that can improve clinicians’ skills when they return to the States, says Dr. Bui. At tertiary care centers such as UPMC, a large transplant center, hospitalists are likely to encounter people from all over the world. “If they have interacted with people from a different culture, they can deal with our [mix of] inpatients better,” she says.
Another significant benefit of traveling to developing countries is that residents get a chance to treat diseases rarely seen in the United States, says Dr. Bui. For instance, she says: “A resident who had treated patients with dengue fever during his clinical elective in India would be quick to include this differential in a returning traveler from Central America admitted to our hospital with fever, headache, myalgia, and a rash. Having seen some of those diseases during their international elective, residents are more comfortable with managing those kinds of diseases, such as when treating travelers who come back with malaria.”
Integrated Care
“Global health electives have tremendous impact in terms of allowing people to experience firsthand the inequalities that exist in global health, and the social and political determinants that cause them,” says Wansom. Those who have the experience “get a snapshot as to how another healthcare system with limited resources is able to provide care to its people and [are] exposed to disease processes and situations that you may not be familiar with from training in the American medical system.”
International health programs at medical schools are growing to accommodate increased demand for overseas experience. UCSF’s residency program formalized residents’ experiences and developed partnership agreements with programs in other countries—ensuring sustainable benefits to hosting countries. The Global Health Scholars Program has sites in Uganda, Saipan, China, and Kenya.
Dr. Dandu believes electives abroad can also offer hospitalists and hospitalists-to-be insight into hand-offs. “One of the central issues for hospitalists is how we help people transition into and out of the hospital,” she explains. “Many of us, as hospitalists, struggle with the fact that we sometimes lose track of our patients when they leave the hospital. One beautiful aspect of many international programs is that residents have an experience with a more holistic approach to care.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ramsey AH, Haq C, Gjerde CL, et al. Career influence of an international health experience during medical school. Fam Med. 2004 June;36(6):412-416.
Chris Hamerski, MD, a third-year resident, was nervous. In Uganda with the Global Health Scholars Program at the University of California, San Francisco (UCSF), he and a fellow resident were scheduled to accompany a physician and a social worker on a Hospice Uganda home visit.
Now back at UCSF between shifts on his current inpatient rotation, Dr. Hamerski recalls his reluctance: “Going into someone’s home is such an intimate experience, and I was a little worried about how we were going to be viewed.”
He needn’t have worried. Despite the startled reactions from young village boys who stopped in their tracks and put down the water jugs they were carrying to stare at the visiting Caucasian doctors, the patients were “very welcoming and gracious, and happy that someone was there to look after them,” he says.
In addition to his time with Hospice Uganda, Dr. Hamerski also worked at Mulago Hospital in Kampala and the Reach-Out Mbuya Clinic, set up to serve patients with HIV/AIDS. “I found the clinic to be very uplifting and inspiring,” he says. “I think it actually works better than clinics in the U.S. because it was an all-in-one clinic, with a holistic approach to the patient.” Not only do patients see a doctor and obtain refills on the spot of their antiretroviral drugs, he explained, but they also have access to a social worker and can obtain money to send their children to school or a micro-loan to help start a business. “It was definitely inspiring to see patients living with HIV doing well in the community,” says Dr. Hamerski. “It made you feel that the clinic was making a difference and having a positive effect on the health of the community.”
Hospitalists, residents, and directors of global health programs stress that international health experiences not only broaden physicians’ perspectives but improve their approach to diagnosis and use of resources when they return to working in U.S. hospitals.
“In their one-month immersions, people have the ability to see and effect change in a more direct way,” points out hospitalist Madhavi Dandu, MD, MPH, assistant clinical professor of medicine and director of UCSF’s Global Health Scholars Program for the Internal Medicine Residency.
Nearly 60% of American medical schools offer global health electives, according to a 2004-2005 survey by the American Association of Medical Colleges—and demand is increasing. The value of a stint abroad for any physician is irrefutable, says hospitalist Tracy Minichiello, MD, who founded the UCSF Global Health Scholars program.
Dr. Hamerski chose to do the global health elective because he wanted to “be more excited about medicine. At the end of residency, it can be a little hard to keep that positive outlook.”
Residents and physicians who complete international health elective courses (typically lasting one or two months) say the experience can greatly influence career choice. Many participants choose to practice with underserved populations or go on to specialize in global medicine.1 But even physicians who do not continue on to a career in global health reap huge benefits as practitioners.
Dr. Dandu has experienced those benefits, both as a resident and now as a visiting director of programs. Through participation in global health electives, she observes, “there is a palpable rejuvenation that occurs, a reminder of some of the enthusiasm that comes from practicing medicine with a little less of the structural issues that make the U.S. healthcare system difficult.”
Less Can Teach More
The Global Health Track of the University of Pittsburgh Internal Medicine Residency Program emphasizes “a generalist perspective, cost-conscious practice and back-to-basics diagnosis”—competencies that dovetail with the mission of hospital medicine.
“The major component of an international health elective is to really improve their [residents’] clinical skills,” notes Thuy D. Bui, MD, director of UPMC’s Global Health Track and medical director of the Program for Health Care to Underserved Populations. This clinical skills improvement is facilitated by the often-limited resources in host countries. “There is no CT, and there are no fancy blood tests, so they [the residents] really have to rely on their clinical acumen to make the diagnosis,” she says.
Dr. Bui has observed that when residents return from a global health elective (the UPMC program has centers in Malawi, India, Japan, Honduras, and Italy), they are “better at picking the right test, knowing when to be more aggressive [with treatment], and are more comfortable with ‘watchful waiting,’ rather than following up every single abnormality they detect in blood work or other imaging studies.”
Franziska Jovin, MD, is medical director of inpatient services at the University of Pittsburgh Medical Center (UPMC) Hospital Medicine Program. Originally from Romania, Dr. Jovin attended medical school in Germany, did her internship in the United Kingdom, and completed her residency in the U.S. During her residency, she returned to Romania on an international elective.
“I think the biggest thing you gain from doing an outside elective is that you learn to really practice medicine the way it used to be in the old days,” she says. “You rely much more on your clinical exam—and get better at it—because at the end of your exam, you have to formulate a differential diagnosis and a treatment plan without always confirming your hypothesis with a test.”
Practicing in another healthcare delivery system can also expand physicians’ perspectives on use of resources. Even though healthcare is funded by the government in many developing countries, says Dr. Jovin, patients still have to pay a large fee for the tests doctors order. “When patients have to pay for the studies that you order, it is much less likely that you will order a battery of tests, and instead concentrate on the test with the highest likely yield first,” she says.
While on elective in Romania, Dr. Jovin practiced in both an outpatient clinic and a hospital setting. She learned that physicians can “stay basic” by using equivalent generic medications to treat conditions such as hypertension. “Here in the U.S., you can use the latest ACE inhibitor or calcium-channel blocker and spend a lot of your patient’s money,” she says. “When money becomes an issue in order to effectively treat a patient, you’re much more cost-conscious.”
On-the-Job Training
Another eye opener for those who go abroad is the chance to observe differences in practice and learn about physician training. “In many countries there is very little structured training after graduation from medical school,” notes Dr. Jovin. “Young doctors learn by following more senior doctors around; it is more an apprenticeship-type training. In many rural areas, fresh medical school graduates may be practicing alone with very limited diagnostic and treatment tools.”
Tanyaporn Wansom, MSIV, a fourth-year medical student at the University of Michigan Medical School in Ann Arbor, is the 2007-2008 chair of the Global Health Action Committee for the American Medical Student Association. During her 2006-2007 stay in Thailand (as an NIH/Fogarty Global Health and Clinical Research Fellow at the Research Institute for the Health Sciences, Chiang Mai University), she was especially impressed with the broad range of diagnostic skills possessed by her supervisor, an infectious diseases (ID) fellow. “For example, I know how to do a lumbar puncture if I am worried about the possibility of meningitis,” she says. “I know how to put the [cerebrospinal] fluid in a tube and send it to the lab. But there, my ID fellow knew how to do all the stains herself, and was able to make immediate diagnoses. There are strengths to the specialization of the American healthcare system, but it is amazing to go abroad and see what other doctors can do.”
This impression is echoed in evaluation forms from the UCSF Global Health Scholars Program, says Dr. Dandu. “One of the common comments is, ‘I’m incredibly impressed by my colleagues abroad because of their amazing physical exam skills,’ ” she says. She believes the exigencies of medical practice in the United States (reliance on testing, adherence to reporting, and regulatory requirements) often mean residents and physicians do not have “the space to focus on the physical exam or the patient’s history. And sometimes, with the way we practice medicine here, it can take longer to see the fruits of what we do and see. In their one-month immersions, people have the ability to see and effect change in a more direct way.”
Rare Encounters
Wansom, who is Thai-American, was motivated to work abroad by her curiosity about her ancestral roots and her commitment to working with people living with HIV/AIDS. She found the physician-patient relationship quite different in Thailand. “Patients look up to you, almost as they would a deity,” she says. “Sometimes it is hard to get their real input on what they are feeling. You may think, because they are nodding, that they are agreeing with everything you say and are totally compliant. In fact, the opposite may be true.”
It is this kind of sensitizing experience that can improve clinicians’ skills when they return to the States, says Dr. Bui. At tertiary care centers such as UPMC, a large transplant center, hospitalists are likely to encounter people from all over the world. “If they have interacted with people from a different culture, they can deal with our [mix of] inpatients better,” she says.
Another significant benefit of traveling to developing countries is that residents get a chance to treat diseases rarely seen in the United States, says Dr. Bui. For instance, she says: “A resident who had treated patients with dengue fever during his clinical elective in India would be quick to include this differential in a returning traveler from Central America admitted to our hospital with fever, headache, myalgia, and a rash. Having seen some of those diseases during their international elective, residents are more comfortable with managing those kinds of diseases, such as when treating travelers who come back with malaria.”
Integrated Care
“Global health electives have tremendous impact in terms of allowing people to experience firsthand the inequalities that exist in global health, and the social and political determinants that cause them,” says Wansom. Those who have the experience “get a snapshot as to how another healthcare system with limited resources is able to provide care to its people and [are] exposed to disease processes and situations that you may not be familiar with from training in the American medical system.”
International health programs at medical schools are growing to accommodate increased demand for overseas experience. UCSF’s residency program formalized residents’ experiences and developed partnership agreements with programs in other countries—ensuring sustainable benefits to hosting countries. The Global Health Scholars Program has sites in Uganda, Saipan, China, and Kenya.
Dr. Dandu believes electives abroad can also offer hospitalists and hospitalists-to-be insight into hand-offs. “One of the central issues for hospitalists is how we help people transition into and out of the hospital,” she explains. “Many of us, as hospitalists, struggle with the fact that we sometimes lose track of our patients when they leave the hospital. One beautiful aspect of many international programs is that residents have an experience with a more holistic approach to care.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ramsey AH, Haq C, Gjerde CL, et al. Career influence of an international health experience during medical school. Fam Med. 2004 June;36(6):412-416.
Transition Talk
Charles A. Crecelius, MD, of Saint Louis, has experienced best- and worst-case scenarios when his frail elderly patients have been admitted and discharged by local hospitalists.
Best case, he says: “My patient is admitted. I get a call. I’m told what is going on. I’m notified of meaningful changes, and at discharge, I get another call [from the hospitalist].”
But there are wide variations in hospitalist/nursing home relationships, notes Dr. Crecelius, a long-term care physician and president-elect of the American Medical Director’s Association (AMDA).
This was brought home by the case of a patient with a well-documented history of dystonic reaction to toxic lithium levels. The patient was later misdiagnosed as having tardive dyskinesia, a movement disorder. Her much-needed medication was discontinued, and the hospital transferred the patient back to the nursing home in worse condition than before.
“We wasted an entire hospitalization,” Dr. Crecelius recalls ruefully.
The above scenario underscores the importance of a thorough transfer of information when elderly patients move from facility to facility. Interaction between hospitalists and nursing home staff will become increasingly important in light of the growing frail elderly population and the Joint Commission on Accreditation of Health Care Organization’s (JCAHO) push for improved discharge communications.1
By applying a customer service model and continually upgrading transfer documentation, hospital medicine groups can “keep the level of communication where it needs to be,” says Susan S. Cumming, MD, associate medical director of Marin Hospitalist Medical Group at Marin General Hospital in Greenbrae, Calif.
Running a Risk
Dan Osterweil, MD, CMD, is familiar with the hospitalist model through his medical training in Israel during the late 1970s and early 1980s. Hospitalists there routinely handled inpatient care.
Dr. Osterweil, a clinical professor of medicine/geriatric medicine at UCLA, research associate with the UCLA Borun Center for Gerontological Research, and former medical director of the Jewish Home for the Aging in Reseda, Calif., has the opportunity to observe hospitalists deal with nursing homes in his current capacity as a consultant for managed care corporations in Southern California.
“Hospitalists have an excellent understanding of acute care management,” he says. “They do a good on-site job of dealing with immediate problems of the individual, and they’re very efficient and very responsive. But while hospitalists are providing higher competency in the management of intra-hospital care, I think that those I’ve interfaced with fall short on the transitions of care, which is so critical with the nursing home patient.”
Dr. Osterweil recalls one patient who had in place do not resuscitate (DNR) and do not intubate (DNI) orders. But when he was hospitalized, the patient was intubated. “If [the hospitalist] had asked one question of the individual or the caregiver—‘What is the goal of care?’—they would have been able to plan a much smoother transition for that person back to the facility.”
At Lower Bucks Hospital in Bristol, Pa., where long-term care physician Daniel Haimowitz, MD, CMD serves as chairman of internal medicine and chairs the utilization committee, the surrounding community of physicians has responded in a mostly positive way to a new hospitalist program.
However, Dr. Haimowitz has concerns that transitioning admissions of nursing home patients to hospitalists can hinder continuity of care.
Different hospitalists work each shift, and unless the patient has been on the hospitalist service in the past, the admitting hospitalist may know nothing about the patient—and most probably has no relationship with the patient’s family (as the primary care physician would have).
“The family doctor has seen the patient for 20 or 30 years and knows what he or she wants,” Dr. Haimowitz says. “But this patient is brand new to the hospitalist. Unless the hospitalist is really good with communication and takes the extra step to call the physician at the nursing home, I think you run the real risk of duplicating workup or actually not doing what is in the best interest of the patient.”
“While demonstrating improved quality of care for the acutely ill hospitalized patient, hospital medicine has struggled with the fact that it inherently adds more patient hand-offs into the mix,” says Bryce Gartland, MD, medical director for care coordination and director of hospital medicine for Emory University Hospital in Atlanta. “We experience this internally, within our facility and externally when transferring patients into or out of the hospital.”
There is always a potential for what has been called the “voltage drop” when hand-offs occur, agrees Dr. Cumming, whether they’re between hospitalists in the same facility or from hospitalist back to the primary care provider. “We function in a healthcare system that is very individualized,” she says. “When you’re dealing with many different community hospitals that may not be part of the same system, it’s very hard to standardize [transfer processes].”
The standard of care for transferring patients from Marin General Hospital to subacute rehabilitation facilities or to skilled nursing facilities entails a detailed inter-facility transfer form. The form includes a thorough discharge summary, with a separate medication reconciliation form, photocopies of any relevant consultations, and a list of pending lab tests. In concert with the hospital’s case managers, Dr. Cumming and hospitalists on her team also make every effort to speak with patients’ receiving providers to relay a synopsis of what has occurred during their patients’ stay in the hospital.
—Daniel Haimowitz, MD, CMD, chairman of internal medicine, Lower Bucks Hospital, Bristol, Pa.
Avoid Assumptions
Especially in the case of patients with dementia or severe illness prohibiting communication about their condition, a thorough transfer sheet or discharge summary—arriving with the patient or faxed in a timely manner—can help reduce errors and contribute to more seamless resumption of care at the next facility.
Without access to a patient’s history, the opportunity for errors increases. One of Dr. Crecelius’ pet peeves is seeing “history not obtainable” on the hospital’s patient transfer sheet. “A history is always obtainable,” Dr. Crecelius asserts. “You can call the nursing home, the family, or the patient’s physician. That phrase equals, ‘We didn’t bother to take the time.’ There is no such thing as ‘history not obtainable,’ and legally, that will not fly in a court of law.”
Missing or incomplete records necessitate communication between facilities. Dr. Crecelius has also found that hospitalists may not understand the nuances of medication prescription for the elderly—a situation that can be rectified with a phone call.
A case in point: Dr. Crecelius once prescribed theophylline for a bradycardic patient who refused a pacemaker but frequently lost consciousness when his pulse and blood pressure dropped. Although this was an obscure use of the drug, which is primarily a bronchodilator, “it worked to keep the patient’s pulse up so he was not passing out. When he went to the hospital, they stopped the drug, and it took forever to get him discharged. The patient came back to the nursing home in horrible shape. I assume the providers at the hospital thought I was crazy for prescribing theophylline to a frail old person!”
Dr. Crecelius’ prescription for avoiding the above scenario: “If you think the medicine is an odd choice, ask the prescriber why the patient is on it. We need to respect each other and get the information when there is a question.”
Cornerstones of Continuity
Medical directors have addressed continuity of care issues in their own ways. Whenever possible, Dr. Crecelius sees his patients in the hospital. He has also been working as a representative of the Missouri Association of Long-Term Care Physicians with a statewide transition planning committee. The committee is drafting new transfer forms for hospitals and post-acute care facilities.
The Asheville Hospitalist Group, PA has “gone to extraordinary lengths to address the issue of inter-facility transfers,” says Marc Westle, DO, FACP, president and managing partner for the large private group in N.C. His group has coordinated efforts with another group of hospitalists who specialize in managing patients in the Asheville area’s 20-plus nursing homes.
To facilitate transfers to a hospital, the nursing homes send paperwork (including history, physical, and medication records) with patients to the emergency department. When patients are ready for discharge, discharge summaries are dictated stat and faxed to the nursing home. Hospitalists discharging patients pre-order diagnostic tests that will be necessary when the patient returns to the nursing home by noting those tests on discharge orders. In addition, “The nursing home group has a list of all our beeper numbers for direct contact should a question arise,” says Dr. Westle.
Every patient transferred to another facility from Emory University Hospital in Atlanta is accompanied by a three-page transfer form, says Dr. Gartland. Included is a one-page summary of detailed nursing care; a second page listing hospitalization events, including pertinent consults, procedures, diagnoses, pending lab tests, and recommended follow-up; and a detailed medication sheet with discontinuation dates for such medication as antibiotics.
During his time as medical director at the Jewish Home for the Aging, Dr. Osterweil created what he calls his own “pseudo-hospitalist arrangement” to ensure continuity of care. He identified multiphysician groups comprising internists and nephrologists who, between them, could offer 24 hours on-call coverage.
When patients were transported to a local community hospital, Dr. Osterweil or his staff would call one of these physicians, who would take care of the patients when they were admitted to the floor. That arrangement is still in place.
“Any major decisions that are made, we are kept in the loop,” says Dr. Osterweil. “Twenty-four hours before readmission back to the skilled nursing facility, we receive a call letting us know the patient is coming back and his or her issues. The physician group executes a ‘stat’ dictated discharge summary, and the patient leaves the hospital with those orders. This ensures the continuity of care when the patient goes back to the nursing home or the board and care facility.”
Beef Up Communication
Dr. Crecelius concedes that certified medical directors (CMDs) are also often guilty of dropping the ball when it comes to communicating with inpatient provider colleagues.
Care of nursing home patients can be improved if hospitalists and medical directors of nursing homes talk directly on the phone, he says. “I met one wonderful hospitalist who actually showed up at the nursing home to see how the patients that he’d been sending out of the hospital were doing,’’ he recalls. “It was so nice to see the face behind the voice. You can’t get mad at a face!”
However, again demonstrating the range of practice techniques, another hospitalist group in Dr. Crecelius’ area does not do anything beyond faxing him the patient’s diagnosis. “Well, I knew the diagnosis, so that fax is not telling me anything,’’ he says. “And unfortunately, that is their idea of communication.”
The Marin Hospitalist Medical Group makes every effort to ensure communications with receiving facilities are timely and thorough. According to Dr. Cumming, the group has surveyed—and will continue to survey—its referring primary care physicians, whether office or facility-based, for feedback on their performance. Hospital case managers also relay feedback to the hospitalist group, she notes. “We’ve tried to use the customer service model across all the groups of physicians who transfer patients to us and to whom we transfer patients, to keep that level of communication where it needs to be,” she says. Some of the questions they ask of their facilities:
- Are we sending the information you need?
- Do you want to receive all documents with the patient when he or she is transferred, or just a small subset of documents?
- How do you want information delivered? Do you want forms, discharge summaries and other documents faxed to you? Would you prefer a phone call?
- What can we do better?
Dr. Haimowitz’s advice to hospitalists might parallel the advice he recently gave to local a hospital administrators who were considering starting an intensivist program. “If you’re going to do this right, you must have physicians who are sensitive to older patients and what they want,” he says. Quality of life, DNR orders, and goals of care take on subtle gradations when applied to the elderly, he emphasizes.
Absent the time to visit the area nursing homes, hospitalists can always at least call, Dr. Crecelius notes.
Just as a hospitalist or emergency department physician would contact the family to corroborate patient history, they should also call the nursing home. “Speaking with the nurse at the skilled nursing facility, you can access a wealth of information—and save time and effort,” he says.
Improve Transfers
Dr. Haimowitz believes communication—on a form or by phone—is essential. He sees even more opportunity for miscommunication between hospitals and nursing homes because of different recordkeeping systems.
Hospitals are moving increasingly to electronic health records, while nursing homes still rely on paper documentation. “How do you foster communication?” Dr. Haimowitz asks. “How do you get the right people on the same bus? The best transfer sheet in the world is no good if one, it’s not filled out, and two, if it’s not read.”
Disparate systems can be a barrier, but it does not mean you should not try to optimize communication within whatever system you have, says Dr. Cumming.
The Marin Hospitalist Medical Group is setting up a communication system to alert all primary care physicians of pending lab results so such tests do not fall through the cracks after patients are discharged.
In another initiative, the hospital will set up a system to note that any pneumonia or influenza vaccinations performed while the patient was hospitalized are communicated either to PCP or outside facility. The group is also working to urge all local nursing facilities to include records of patients’ recent vaccinations when they are transferred to the hospital.
It’s clear that effective transfers of elderly patients require a concerted effort by all involved. “If you perform a root cause analysis of [transfer] errors, most occur not because of any negligence, but because communication—written or verbal—was not handled as best as it could have been,” Dr. Gartland notes. “Oftentimes, we are just as frustrated as they [nursing facilities] are when patients return to the emergency room unable to communicate their medical conditions, wishes, and the like,” he says. As medical director of care coordination at Emory, he has worked to improve relationships with administrators and physicians in nursing facilities used most often by the hospital. “If people have a vested interest in a relationship, they are more likely to be diligent about the transfer of patients,” he asserts.
Above all, emphasizes Dr. Cumming, “it important to always solicit feedback from your primary care physician ‘clientele.’ They are your clients, much as your patients are, and your hospital is. We’re providing services to all these various groups. Quality patient care is the most important thing that we do, and part of that means that we have to have good transfer of information. Our group recognizes that we are far from perfect; we know we can always do better; and we always have to reassess to make sure that we’re on the right track.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ouslander JG, Osterweil D, Morley J. Medical Care in the Nursing Home. 2nd ed. New York, New York: McGraw-Hill Publishers;1997.
Charles A. Crecelius, MD, of Saint Louis, has experienced best- and worst-case scenarios when his frail elderly patients have been admitted and discharged by local hospitalists.
Best case, he says: “My patient is admitted. I get a call. I’m told what is going on. I’m notified of meaningful changes, and at discharge, I get another call [from the hospitalist].”
But there are wide variations in hospitalist/nursing home relationships, notes Dr. Crecelius, a long-term care physician and president-elect of the American Medical Director’s Association (AMDA).
This was brought home by the case of a patient with a well-documented history of dystonic reaction to toxic lithium levels. The patient was later misdiagnosed as having tardive dyskinesia, a movement disorder. Her much-needed medication was discontinued, and the hospital transferred the patient back to the nursing home in worse condition than before.
“We wasted an entire hospitalization,” Dr. Crecelius recalls ruefully.
The above scenario underscores the importance of a thorough transfer of information when elderly patients move from facility to facility. Interaction between hospitalists and nursing home staff will become increasingly important in light of the growing frail elderly population and the Joint Commission on Accreditation of Health Care Organization’s (JCAHO) push for improved discharge communications.1
By applying a customer service model and continually upgrading transfer documentation, hospital medicine groups can “keep the level of communication where it needs to be,” says Susan S. Cumming, MD, associate medical director of Marin Hospitalist Medical Group at Marin General Hospital in Greenbrae, Calif.
Running a Risk
Dan Osterweil, MD, CMD, is familiar with the hospitalist model through his medical training in Israel during the late 1970s and early 1980s. Hospitalists there routinely handled inpatient care.
Dr. Osterweil, a clinical professor of medicine/geriatric medicine at UCLA, research associate with the UCLA Borun Center for Gerontological Research, and former medical director of the Jewish Home for the Aging in Reseda, Calif., has the opportunity to observe hospitalists deal with nursing homes in his current capacity as a consultant for managed care corporations in Southern California.
“Hospitalists have an excellent understanding of acute care management,” he says. “They do a good on-site job of dealing with immediate problems of the individual, and they’re very efficient and very responsive. But while hospitalists are providing higher competency in the management of intra-hospital care, I think that those I’ve interfaced with fall short on the transitions of care, which is so critical with the nursing home patient.”
Dr. Osterweil recalls one patient who had in place do not resuscitate (DNR) and do not intubate (DNI) orders. But when he was hospitalized, the patient was intubated. “If [the hospitalist] had asked one question of the individual or the caregiver—‘What is the goal of care?’—they would have been able to plan a much smoother transition for that person back to the facility.”
At Lower Bucks Hospital in Bristol, Pa., where long-term care physician Daniel Haimowitz, MD, CMD serves as chairman of internal medicine and chairs the utilization committee, the surrounding community of physicians has responded in a mostly positive way to a new hospitalist program.
However, Dr. Haimowitz has concerns that transitioning admissions of nursing home patients to hospitalists can hinder continuity of care.
Different hospitalists work each shift, and unless the patient has been on the hospitalist service in the past, the admitting hospitalist may know nothing about the patient—and most probably has no relationship with the patient’s family (as the primary care physician would have).
“The family doctor has seen the patient for 20 or 30 years and knows what he or she wants,” Dr. Haimowitz says. “But this patient is brand new to the hospitalist. Unless the hospitalist is really good with communication and takes the extra step to call the physician at the nursing home, I think you run the real risk of duplicating workup or actually not doing what is in the best interest of the patient.”
“While demonstrating improved quality of care for the acutely ill hospitalized patient, hospital medicine has struggled with the fact that it inherently adds more patient hand-offs into the mix,” says Bryce Gartland, MD, medical director for care coordination and director of hospital medicine for Emory University Hospital in Atlanta. “We experience this internally, within our facility and externally when transferring patients into or out of the hospital.”
There is always a potential for what has been called the “voltage drop” when hand-offs occur, agrees Dr. Cumming, whether they’re between hospitalists in the same facility or from hospitalist back to the primary care provider. “We function in a healthcare system that is very individualized,” she says. “When you’re dealing with many different community hospitals that may not be part of the same system, it’s very hard to standardize [transfer processes].”
The standard of care for transferring patients from Marin General Hospital to subacute rehabilitation facilities or to skilled nursing facilities entails a detailed inter-facility transfer form. The form includes a thorough discharge summary, with a separate medication reconciliation form, photocopies of any relevant consultations, and a list of pending lab tests. In concert with the hospital’s case managers, Dr. Cumming and hospitalists on her team also make every effort to speak with patients’ receiving providers to relay a synopsis of what has occurred during their patients’ stay in the hospital.
—Daniel Haimowitz, MD, CMD, chairman of internal medicine, Lower Bucks Hospital, Bristol, Pa.
Avoid Assumptions
Especially in the case of patients with dementia or severe illness prohibiting communication about their condition, a thorough transfer sheet or discharge summary—arriving with the patient or faxed in a timely manner—can help reduce errors and contribute to more seamless resumption of care at the next facility.
Without access to a patient’s history, the opportunity for errors increases. One of Dr. Crecelius’ pet peeves is seeing “history not obtainable” on the hospital’s patient transfer sheet. “A history is always obtainable,” Dr. Crecelius asserts. “You can call the nursing home, the family, or the patient’s physician. That phrase equals, ‘We didn’t bother to take the time.’ There is no such thing as ‘history not obtainable,’ and legally, that will not fly in a court of law.”
Missing or incomplete records necessitate communication between facilities. Dr. Crecelius has also found that hospitalists may not understand the nuances of medication prescription for the elderly—a situation that can be rectified with a phone call.
A case in point: Dr. Crecelius once prescribed theophylline for a bradycardic patient who refused a pacemaker but frequently lost consciousness when his pulse and blood pressure dropped. Although this was an obscure use of the drug, which is primarily a bronchodilator, “it worked to keep the patient’s pulse up so he was not passing out. When he went to the hospital, they stopped the drug, and it took forever to get him discharged. The patient came back to the nursing home in horrible shape. I assume the providers at the hospital thought I was crazy for prescribing theophylline to a frail old person!”
Dr. Crecelius’ prescription for avoiding the above scenario: “If you think the medicine is an odd choice, ask the prescriber why the patient is on it. We need to respect each other and get the information when there is a question.”
Cornerstones of Continuity
Medical directors have addressed continuity of care issues in their own ways. Whenever possible, Dr. Crecelius sees his patients in the hospital. He has also been working as a representative of the Missouri Association of Long-Term Care Physicians with a statewide transition planning committee. The committee is drafting new transfer forms for hospitals and post-acute care facilities.
The Asheville Hospitalist Group, PA has “gone to extraordinary lengths to address the issue of inter-facility transfers,” says Marc Westle, DO, FACP, president and managing partner for the large private group in N.C. His group has coordinated efforts with another group of hospitalists who specialize in managing patients in the Asheville area’s 20-plus nursing homes.
To facilitate transfers to a hospital, the nursing homes send paperwork (including history, physical, and medication records) with patients to the emergency department. When patients are ready for discharge, discharge summaries are dictated stat and faxed to the nursing home. Hospitalists discharging patients pre-order diagnostic tests that will be necessary when the patient returns to the nursing home by noting those tests on discharge orders. In addition, “The nursing home group has a list of all our beeper numbers for direct contact should a question arise,” says Dr. Westle.
Every patient transferred to another facility from Emory University Hospital in Atlanta is accompanied by a three-page transfer form, says Dr. Gartland. Included is a one-page summary of detailed nursing care; a second page listing hospitalization events, including pertinent consults, procedures, diagnoses, pending lab tests, and recommended follow-up; and a detailed medication sheet with discontinuation dates for such medication as antibiotics.
During his time as medical director at the Jewish Home for the Aging, Dr. Osterweil created what he calls his own “pseudo-hospitalist arrangement” to ensure continuity of care. He identified multiphysician groups comprising internists and nephrologists who, between them, could offer 24 hours on-call coverage.
When patients were transported to a local community hospital, Dr. Osterweil or his staff would call one of these physicians, who would take care of the patients when they were admitted to the floor. That arrangement is still in place.
“Any major decisions that are made, we are kept in the loop,” says Dr. Osterweil. “Twenty-four hours before readmission back to the skilled nursing facility, we receive a call letting us know the patient is coming back and his or her issues. The physician group executes a ‘stat’ dictated discharge summary, and the patient leaves the hospital with those orders. This ensures the continuity of care when the patient goes back to the nursing home or the board and care facility.”
Beef Up Communication
Dr. Crecelius concedes that certified medical directors (CMDs) are also often guilty of dropping the ball when it comes to communicating with inpatient provider colleagues.
Care of nursing home patients can be improved if hospitalists and medical directors of nursing homes talk directly on the phone, he says. “I met one wonderful hospitalist who actually showed up at the nursing home to see how the patients that he’d been sending out of the hospital were doing,’’ he recalls. “It was so nice to see the face behind the voice. You can’t get mad at a face!”
However, again demonstrating the range of practice techniques, another hospitalist group in Dr. Crecelius’ area does not do anything beyond faxing him the patient’s diagnosis. “Well, I knew the diagnosis, so that fax is not telling me anything,’’ he says. “And unfortunately, that is their idea of communication.”
The Marin Hospitalist Medical Group makes every effort to ensure communications with receiving facilities are timely and thorough. According to Dr. Cumming, the group has surveyed—and will continue to survey—its referring primary care physicians, whether office or facility-based, for feedback on their performance. Hospital case managers also relay feedback to the hospitalist group, she notes. “We’ve tried to use the customer service model across all the groups of physicians who transfer patients to us and to whom we transfer patients, to keep that level of communication where it needs to be,” she says. Some of the questions they ask of their facilities:
- Are we sending the information you need?
- Do you want to receive all documents with the patient when he or she is transferred, or just a small subset of documents?
- How do you want information delivered? Do you want forms, discharge summaries and other documents faxed to you? Would you prefer a phone call?
- What can we do better?
Dr. Haimowitz’s advice to hospitalists might parallel the advice he recently gave to local a hospital administrators who were considering starting an intensivist program. “If you’re going to do this right, you must have physicians who are sensitive to older patients and what they want,” he says. Quality of life, DNR orders, and goals of care take on subtle gradations when applied to the elderly, he emphasizes.
Absent the time to visit the area nursing homes, hospitalists can always at least call, Dr. Crecelius notes.
Just as a hospitalist or emergency department physician would contact the family to corroborate patient history, they should also call the nursing home. “Speaking with the nurse at the skilled nursing facility, you can access a wealth of information—and save time and effort,” he says.
Improve Transfers
Dr. Haimowitz believes communication—on a form or by phone—is essential. He sees even more opportunity for miscommunication between hospitals and nursing homes because of different recordkeeping systems.
Hospitals are moving increasingly to electronic health records, while nursing homes still rely on paper documentation. “How do you foster communication?” Dr. Haimowitz asks. “How do you get the right people on the same bus? The best transfer sheet in the world is no good if one, it’s not filled out, and two, if it’s not read.”
Disparate systems can be a barrier, but it does not mean you should not try to optimize communication within whatever system you have, says Dr. Cumming.
The Marin Hospitalist Medical Group is setting up a communication system to alert all primary care physicians of pending lab results so such tests do not fall through the cracks after patients are discharged.
In another initiative, the hospital will set up a system to note that any pneumonia or influenza vaccinations performed while the patient was hospitalized are communicated either to PCP or outside facility. The group is also working to urge all local nursing facilities to include records of patients’ recent vaccinations when they are transferred to the hospital.
It’s clear that effective transfers of elderly patients require a concerted effort by all involved. “If you perform a root cause analysis of [transfer] errors, most occur not because of any negligence, but because communication—written or verbal—was not handled as best as it could have been,” Dr. Gartland notes. “Oftentimes, we are just as frustrated as they [nursing facilities] are when patients return to the emergency room unable to communicate their medical conditions, wishes, and the like,” he says. As medical director of care coordination at Emory, he has worked to improve relationships with administrators and physicians in nursing facilities used most often by the hospital. “If people have a vested interest in a relationship, they are more likely to be diligent about the transfer of patients,” he asserts.
Above all, emphasizes Dr. Cumming, “it important to always solicit feedback from your primary care physician ‘clientele.’ They are your clients, much as your patients are, and your hospital is. We’re providing services to all these various groups. Quality patient care is the most important thing that we do, and part of that means that we have to have good transfer of information. Our group recognizes that we are far from perfect; we know we can always do better; and we always have to reassess to make sure that we’re on the right track.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ouslander JG, Osterweil D, Morley J. Medical Care in the Nursing Home. 2nd ed. New York, New York: McGraw-Hill Publishers;1997.
Charles A. Crecelius, MD, of Saint Louis, has experienced best- and worst-case scenarios when his frail elderly patients have been admitted and discharged by local hospitalists.
Best case, he says: “My patient is admitted. I get a call. I’m told what is going on. I’m notified of meaningful changes, and at discharge, I get another call [from the hospitalist].”
But there are wide variations in hospitalist/nursing home relationships, notes Dr. Crecelius, a long-term care physician and president-elect of the American Medical Director’s Association (AMDA).
This was brought home by the case of a patient with a well-documented history of dystonic reaction to toxic lithium levels. The patient was later misdiagnosed as having tardive dyskinesia, a movement disorder. Her much-needed medication was discontinued, and the hospital transferred the patient back to the nursing home in worse condition than before.
“We wasted an entire hospitalization,” Dr. Crecelius recalls ruefully.
The above scenario underscores the importance of a thorough transfer of information when elderly patients move from facility to facility. Interaction between hospitalists and nursing home staff will become increasingly important in light of the growing frail elderly population and the Joint Commission on Accreditation of Health Care Organization’s (JCAHO) push for improved discharge communications.1
By applying a customer service model and continually upgrading transfer documentation, hospital medicine groups can “keep the level of communication where it needs to be,” says Susan S. Cumming, MD, associate medical director of Marin Hospitalist Medical Group at Marin General Hospital in Greenbrae, Calif.
Running a Risk
Dan Osterweil, MD, CMD, is familiar with the hospitalist model through his medical training in Israel during the late 1970s and early 1980s. Hospitalists there routinely handled inpatient care.
Dr. Osterweil, a clinical professor of medicine/geriatric medicine at UCLA, research associate with the UCLA Borun Center for Gerontological Research, and former medical director of the Jewish Home for the Aging in Reseda, Calif., has the opportunity to observe hospitalists deal with nursing homes in his current capacity as a consultant for managed care corporations in Southern California.
“Hospitalists have an excellent understanding of acute care management,” he says. “They do a good on-site job of dealing with immediate problems of the individual, and they’re very efficient and very responsive. But while hospitalists are providing higher competency in the management of intra-hospital care, I think that those I’ve interfaced with fall short on the transitions of care, which is so critical with the nursing home patient.”
Dr. Osterweil recalls one patient who had in place do not resuscitate (DNR) and do not intubate (DNI) orders. But when he was hospitalized, the patient was intubated. “If [the hospitalist] had asked one question of the individual or the caregiver—‘What is the goal of care?’—they would have been able to plan a much smoother transition for that person back to the facility.”
At Lower Bucks Hospital in Bristol, Pa., where long-term care physician Daniel Haimowitz, MD, CMD serves as chairman of internal medicine and chairs the utilization committee, the surrounding community of physicians has responded in a mostly positive way to a new hospitalist program.
However, Dr. Haimowitz has concerns that transitioning admissions of nursing home patients to hospitalists can hinder continuity of care.
Different hospitalists work each shift, and unless the patient has been on the hospitalist service in the past, the admitting hospitalist may know nothing about the patient—and most probably has no relationship with the patient’s family (as the primary care physician would have).
“The family doctor has seen the patient for 20 or 30 years and knows what he or she wants,” Dr. Haimowitz says. “But this patient is brand new to the hospitalist. Unless the hospitalist is really good with communication and takes the extra step to call the physician at the nursing home, I think you run the real risk of duplicating workup or actually not doing what is in the best interest of the patient.”
“While demonstrating improved quality of care for the acutely ill hospitalized patient, hospital medicine has struggled with the fact that it inherently adds more patient hand-offs into the mix,” says Bryce Gartland, MD, medical director for care coordination and director of hospital medicine for Emory University Hospital in Atlanta. “We experience this internally, within our facility and externally when transferring patients into or out of the hospital.”
There is always a potential for what has been called the “voltage drop” when hand-offs occur, agrees Dr. Cumming, whether they’re between hospitalists in the same facility or from hospitalist back to the primary care provider. “We function in a healthcare system that is very individualized,” she says. “When you’re dealing with many different community hospitals that may not be part of the same system, it’s very hard to standardize [transfer processes].”
The standard of care for transferring patients from Marin General Hospital to subacute rehabilitation facilities or to skilled nursing facilities entails a detailed inter-facility transfer form. The form includes a thorough discharge summary, with a separate medication reconciliation form, photocopies of any relevant consultations, and a list of pending lab tests. In concert with the hospital’s case managers, Dr. Cumming and hospitalists on her team also make every effort to speak with patients’ receiving providers to relay a synopsis of what has occurred during their patients’ stay in the hospital.
—Daniel Haimowitz, MD, CMD, chairman of internal medicine, Lower Bucks Hospital, Bristol, Pa.
Avoid Assumptions
Especially in the case of patients with dementia or severe illness prohibiting communication about their condition, a thorough transfer sheet or discharge summary—arriving with the patient or faxed in a timely manner—can help reduce errors and contribute to more seamless resumption of care at the next facility.
Without access to a patient’s history, the opportunity for errors increases. One of Dr. Crecelius’ pet peeves is seeing “history not obtainable” on the hospital’s patient transfer sheet. “A history is always obtainable,” Dr. Crecelius asserts. “You can call the nursing home, the family, or the patient’s physician. That phrase equals, ‘We didn’t bother to take the time.’ There is no such thing as ‘history not obtainable,’ and legally, that will not fly in a court of law.”
Missing or incomplete records necessitate communication between facilities. Dr. Crecelius has also found that hospitalists may not understand the nuances of medication prescription for the elderly—a situation that can be rectified with a phone call.
A case in point: Dr. Crecelius once prescribed theophylline for a bradycardic patient who refused a pacemaker but frequently lost consciousness when his pulse and blood pressure dropped. Although this was an obscure use of the drug, which is primarily a bronchodilator, “it worked to keep the patient’s pulse up so he was not passing out. When he went to the hospital, they stopped the drug, and it took forever to get him discharged. The patient came back to the nursing home in horrible shape. I assume the providers at the hospital thought I was crazy for prescribing theophylline to a frail old person!”
Dr. Crecelius’ prescription for avoiding the above scenario: “If you think the medicine is an odd choice, ask the prescriber why the patient is on it. We need to respect each other and get the information when there is a question.”
Cornerstones of Continuity
Medical directors have addressed continuity of care issues in their own ways. Whenever possible, Dr. Crecelius sees his patients in the hospital. He has also been working as a representative of the Missouri Association of Long-Term Care Physicians with a statewide transition planning committee. The committee is drafting new transfer forms for hospitals and post-acute care facilities.
The Asheville Hospitalist Group, PA has “gone to extraordinary lengths to address the issue of inter-facility transfers,” says Marc Westle, DO, FACP, president and managing partner for the large private group in N.C. His group has coordinated efforts with another group of hospitalists who specialize in managing patients in the Asheville area’s 20-plus nursing homes.
To facilitate transfers to a hospital, the nursing homes send paperwork (including history, physical, and medication records) with patients to the emergency department. When patients are ready for discharge, discharge summaries are dictated stat and faxed to the nursing home. Hospitalists discharging patients pre-order diagnostic tests that will be necessary when the patient returns to the nursing home by noting those tests on discharge orders. In addition, “The nursing home group has a list of all our beeper numbers for direct contact should a question arise,” says Dr. Westle.
Every patient transferred to another facility from Emory University Hospital in Atlanta is accompanied by a three-page transfer form, says Dr. Gartland. Included is a one-page summary of detailed nursing care; a second page listing hospitalization events, including pertinent consults, procedures, diagnoses, pending lab tests, and recommended follow-up; and a detailed medication sheet with discontinuation dates for such medication as antibiotics.
During his time as medical director at the Jewish Home for the Aging, Dr. Osterweil created what he calls his own “pseudo-hospitalist arrangement” to ensure continuity of care. He identified multiphysician groups comprising internists and nephrologists who, between them, could offer 24 hours on-call coverage.
When patients were transported to a local community hospital, Dr. Osterweil or his staff would call one of these physicians, who would take care of the patients when they were admitted to the floor. That arrangement is still in place.
“Any major decisions that are made, we are kept in the loop,” says Dr. Osterweil. “Twenty-four hours before readmission back to the skilled nursing facility, we receive a call letting us know the patient is coming back and his or her issues. The physician group executes a ‘stat’ dictated discharge summary, and the patient leaves the hospital with those orders. This ensures the continuity of care when the patient goes back to the nursing home or the board and care facility.”
Beef Up Communication
Dr. Crecelius concedes that certified medical directors (CMDs) are also often guilty of dropping the ball when it comes to communicating with inpatient provider colleagues.
Care of nursing home patients can be improved if hospitalists and medical directors of nursing homes talk directly on the phone, he says. “I met one wonderful hospitalist who actually showed up at the nursing home to see how the patients that he’d been sending out of the hospital were doing,’’ he recalls. “It was so nice to see the face behind the voice. You can’t get mad at a face!”
However, again demonstrating the range of practice techniques, another hospitalist group in Dr. Crecelius’ area does not do anything beyond faxing him the patient’s diagnosis. “Well, I knew the diagnosis, so that fax is not telling me anything,’’ he says. “And unfortunately, that is their idea of communication.”
The Marin Hospitalist Medical Group makes every effort to ensure communications with receiving facilities are timely and thorough. According to Dr. Cumming, the group has surveyed—and will continue to survey—its referring primary care physicians, whether office or facility-based, for feedback on their performance. Hospital case managers also relay feedback to the hospitalist group, she notes. “We’ve tried to use the customer service model across all the groups of physicians who transfer patients to us and to whom we transfer patients, to keep that level of communication where it needs to be,” she says. Some of the questions they ask of their facilities:
- Are we sending the information you need?
- Do you want to receive all documents with the patient when he or she is transferred, or just a small subset of documents?
- How do you want information delivered? Do you want forms, discharge summaries and other documents faxed to you? Would you prefer a phone call?
- What can we do better?
Dr. Haimowitz’s advice to hospitalists might parallel the advice he recently gave to local a hospital administrators who were considering starting an intensivist program. “If you’re going to do this right, you must have physicians who are sensitive to older patients and what they want,” he says. Quality of life, DNR orders, and goals of care take on subtle gradations when applied to the elderly, he emphasizes.
Absent the time to visit the area nursing homes, hospitalists can always at least call, Dr. Crecelius notes.
Just as a hospitalist or emergency department physician would contact the family to corroborate patient history, they should also call the nursing home. “Speaking with the nurse at the skilled nursing facility, you can access a wealth of information—and save time and effort,” he says.
Improve Transfers
Dr. Haimowitz believes communication—on a form or by phone—is essential. He sees even more opportunity for miscommunication between hospitals and nursing homes because of different recordkeeping systems.
Hospitals are moving increasingly to electronic health records, while nursing homes still rely on paper documentation. “How do you foster communication?” Dr. Haimowitz asks. “How do you get the right people on the same bus? The best transfer sheet in the world is no good if one, it’s not filled out, and two, if it’s not read.”
Disparate systems can be a barrier, but it does not mean you should not try to optimize communication within whatever system you have, says Dr. Cumming.
The Marin Hospitalist Medical Group is setting up a communication system to alert all primary care physicians of pending lab results so such tests do not fall through the cracks after patients are discharged.
In another initiative, the hospital will set up a system to note that any pneumonia or influenza vaccinations performed while the patient was hospitalized are communicated either to PCP or outside facility. The group is also working to urge all local nursing facilities to include records of patients’ recent vaccinations when they are transferred to the hospital.
It’s clear that effective transfers of elderly patients require a concerted effort by all involved. “If you perform a root cause analysis of [transfer] errors, most occur not because of any negligence, but because communication—written or verbal—was not handled as best as it could have been,” Dr. Gartland notes. “Oftentimes, we are just as frustrated as they [nursing facilities] are when patients return to the emergency room unable to communicate their medical conditions, wishes, and the like,” he says. As medical director of care coordination at Emory, he has worked to improve relationships with administrators and physicians in nursing facilities used most often by the hospital. “If people have a vested interest in a relationship, they are more likely to be diligent about the transfer of patients,” he asserts.
Above all, emphasizes Dr. Cumming, “it important to always solicit feedback from your primary care physician ‘clientele.’ They are your clients, much as your patients are, and your hospital is. We’re providing services to all these various groups. Quality patient care is the most important thing that we do, and part of that means that we have to have good transfer of information. Our group recognizes that we are far from perfect; we know we can always do better; and we always have to reassess to make sure that we’re on the right track.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ouslander JG, Osterweil D, Morley J. Medical Care in the Nursing Home. 2nd ed. New York, New York: McGraw-Hill Publishers;1997.