User login
All You Need Is Love
During their residency at Beth Israel Deaconess Medical Center in Boston, hospitalist Margaret Fang, MD, MPH, FHM, and her friends often talked about who they might want to marry: someone completely outside of the medical field? A violinist, perhaps? But when she interviewed for a faculty position at the University of California at San Francisco (UCSF), she met hospitalist Bradley Sharpe, MD, SFHM, then the chief resident in the Department of Medicine.
They married in 2010 and currently work as associate professors in the Department of Medicine at UCSF Medical Center—Margaret as a clinician-investigator and Brad as a clinician-educator and administrator. “I find that [being married to a hospitalist] makes many aspects of communication easier because you have a shared language,” she says.
A common language, a partner who “gets it” if you’re on service 16 days straight, a shared passion for the hospitalist movement: These are the advantages of being married to a fellow hospitalist, say five dual hospitalist couples.
“It is wonderful having a partner who understands where I’m coming from if I do have a rough day,” says Elizabeth “Liz” Gundersen, MD, FHM, who in 2004 tied the knot with hospitalist Jasen Gundersen, MD, MBA, CPE, SFHM.
Heather Wark, MD, who is married to SHM cofounder Win Whitcomb, MD, MHM, seconds that notion. “You don’t have to start from the beginning with anything,” says Dr. Wark, who works as a hospitalist (SNFist), at Farren Care Center, a skilled nursing facility in Turners Falls, Mass. “You can just launch right into whatever the crisis of the day is, and your partner completely understands.”
By and large, the advantages of marrying someone in the same profession outweigh the disadvantages, as a survey of female family physicians recently showed.1 But with those advantages come challenges. Among them:
- Aligning career and relationship goals;
- Juggling demanding schedules; and
- Carving out relationship and family time.
Threading through these issues requires transparent communication, flexibility, and mutual respect, according to these couples.
Career Negotiation
Liz Gundersen recently resigned her position as associate chief of the Division of Hospital Medicine at the University of Massachusetts (UMass) Medical School in Worcester, Mass. The reason? Jasen accepted a new job. As many hospitalists before them have done, the Gundersens pulled up roots and moved across the country, as Jasen started his new job as chief medical officer with TeamHealth Hospital Medicine in Fort Lauderdale, Fla.
“It was a pretty stressful job change,” Jasen says. Following the job offer from TeamHealth, the Gundersens spent “a couple of months” weighing all of their options. “My taking the job was a great promotion for me,” he says, “but Liz also had the opportunity for a great promotion at UMass. In the end, the decision came down to the fact that it was a great opportunity for me and a great opportunity for us, as a couple, to do something new. And I think we weathered it pretty well.”
Liz, who is in the midst of securing her credentials to work in Florida, agrees. She is continuing to work with UMass long-distance, completing the physician schedule and training the new scheduler.
Dr. Whitcomb, who is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., and Dr. Wark married 15 years ago and have worked to configure their relationship to accommodate both career and family. “For most of our relationship,” she explains, “I’ve had a part-time job that has stayed steady.”
Dr. Wark’s professional flexibility allows her to function as a full-time mother to their two children, Maela, 13, and Nicholas, 10. “Although my career has been very successful, Win has been more the one who has undergone career changes and advancements,” she says. “My staying steady has allowed that space in our relationship.”
Drs. Fang and Sharpe haven’t had to cross the bridge of different job offerings yet. But Dr. Sharpe asserts that he’s a firm believer that there should be no difference in how their careers are valued. The couple has an ongoing “transparent conversation,” adds Dr. Fang, about what’s important to each of them and the relative impact of future opportunities. In addition, her job as a researcher is somewhat portable, so the chances of simultaneous job offers might increase. For now, though, they are happily committed to UCSF and love the city of San Francisco.
Madhavi Dandu, MD, MPH, assistant clinical professor and associate director of Pathways to Discovery in Global Health at UCSF, and her husband, Nima Afshar, MD, an ED/hospitalist at UCSF and at the Veterans Affairs Medical Center in San Francisco, have been lucky, she says, because “we were both drawn to medicine for similar reasons.” Together since their second year of medical school, they also both wanted, early on, to pursue careers in academic medicine. “We definitely went through some difficult times, but mostly, we were on the same page,” Dr. Dandu says.
When it came time to apply to a match program for residency, they both applied to UCSF, where they successfully completed their residencies and began their academic careers. They made a conscious decision to wait to have children until their training was finished.
Still, in the first year or so after their daughter’s birth in 2008, Dr. Dandu felt the pull between career and parenthood. “As a physician, you’re driven to make sure you’re not dropping the ball on anything, and there were many weekends that I was away from my daughter,” she says.
A supportive family helped with a flexible childcare arrangement, but this past year, Dr. Dandu decided to scale back her work schedule to 80% of regular shifts in order to spend more time with her daughter. Now, she says, “It’s pretty rare” that she will alter a commitment with her daughter for last-minute calls from work.
Shared and Diverse Interests
Even if they work in the same division, dual-hospitalist couples say they thrive when they also have independent career interests. David O. Meltzer, MD, PhD, FHM, chief of the Division of Hospital Medicine at the University of Chicago’s Department of Medicine and director of the Center for Health and the Social Sciences in Chicago, and his wife, Vineet Arora, MD, MPP, SFHM, assistant dean of Pritzker School of Medicine in Chicago and associate program director of the internal-medicine residency program, pursue independent spheres in addition to occasional collaborations as hospitalist-researchers.
They recently were on clinical service together during a blizzard. “We also co-mentor several trainees,” Dr. Arora says, “which is actually really fun. For example, I can refer trainees to David if they’re interested in economics, and if someone has a quality/safety interest, he could refer that person to me” (see “Keys to Thriving as a Dual-Hospitalist Couple,” above).
The Gundersens’ professional interests forked when Jasen found his niche in administrative work and started to pursue an MBA in 2007. Meanwhile, Liz was finding her own niche doing quality improvement (QI) and became one of the physician quality officers at UMass Memorial.
continued below...
Drs. Fang and Sharpe have experienced similar career divisions with their hospitalist roots. Dr. Sharpe is focused on medical education, while Dr. Fang’s focus predominantly is clinical research. “Between the two of us, we capture many of the elements of academic hospitalist practice,” she says. “I think having our diverse interests gives us a lot of knowledge and expertise about our respective fields. I’m able to learn a lot about how the hospital works and about clinical teaching from Brad, and, hopefully, he can come to me for research advice.”
Drs. Dandu and Afshar have branched out, too. He completed additional residency training in emergency medicine and she acquired an MPH at the University of California at Berkeley. Subsequently, she became associate director of Pathways to Discovery in Global Health, the global health elective program for medical students.
“If you follow your passion in your career, that will allow you to bring a happier individual to your relationship,” Dr. Whitcomb adds.
Schedule Time Together
Communication is a major factor when dual-hospitalist couples plan and execute their weekly schedules. “We try to have an organizing conversation at the end of each weekend,” says Dr. Wark, who also is the keeper of the family calendar and “the glue” that keeps her family of four on track.
Marriage and family therapist Catherine Hastings, PhD, who practices in Lancaster, Pa., says it’s important for dual-hospitalist couples to remember that the relationship needs attention, just as physician careers do.
“It’s very easy to talk about your job when you are in the same profession, but you can easily get consumed by that and let your personal relationships take a back seat,” Dr. Hastings explains. “Couples may look upon conversation about work as ‘brainstorming’ or problem-solving together, but that can also take over.” Hospitalist couples need to be aware that they should plan to be a couple as rigorously as they plan for their jobs, she adds.
Dr. Meltzer doesn’t think that he and his wife consciously delineate between work and personal conversation. “We certainly talk about things that don’t involve work, but we do not say, ‘We will absolutely not talk about work,’ ” he says. “That’s like saying there is not an elephant in the room.”
It didn’t bother the Gundersens that their work came home to a certain extent, says Liz. Even so, to avoid the temptation to “try and churn through all of our work over dinner,” she began scheduling meetings through Jasen’s secretary to discuss work issues.
“When we’re working, we’re doing so full-on,” Jasen says. “But then, we are definitely known for taking recovery time,” which includes skiing vacations and spending weekends on their boat in order to recharge.
Drs. Meltzer and Arora have traveled extensively together for both work and fun. On a trip last year, they traveled to China to a medical school partnered with their own to give talks. They even lengthened their stay to visit the Great Wall of China and toured Beijing and Shanghai.
Dr. Fang considers her husband the “uber-scheduler” in their relationship. “We very consciously build quality time with each other into our schedules,” she says. Without children, for the moment, they also have the free time to grab dinner spontaneously.
Parents First, Physicians Second
Time together as a couple is a scarcer commodity when a dual-hospitalist couple has children. With a pair of pre-teens who are involved in competitive swimming, Drs. Wark and Whitcomb have a two-hour block of time they need plan into their schedule three to four evenings a week.
“We’ve got a built-in babysitter called the YMCA swim team,” Dr. Wark jokes. They also run together several times a week, an activity they use to reconnect. “You have to figure out ways to grow together, to develop and have interests and activities that are specific to the relationship and not related to the kids,” Dr. Whitcomb says. “And if you don’t grow together, you’ll grow apart.”
Drs. Dandu and Afshar, who married in 2003, are just beginning to reacquaint themselves with their adult social lives, she says, now that their daughter is two and a half. “Sometimes we make time to have ‘date night,’ but sometimes it’s just us getting together with our adult friends,” she says.
With or without children, dual-hospitalist couples’ passion for their profession is intertwined with their successful marriages. “Being a physician,” Jasen Gundersen says, “is not just a vocation; it’s part of who you are.”
Dr. Dandu describes it this way: “Our life at home and our life at work are very melded.”
Like Dr. Wang, Dr. Dandu had contemplated a long-term relationship with someone who wasn’t in medicine. But being married to a physician-hospitalist, she says, “turned out to be great for me, because I have someone I can really talk to about everything.” TH
Gretchen Henkel is a freelance writer based in California.
Reference
- Schrager S, Kolan A, Dottl SL. Is that your pager or mine: a survey of women academic family physicians in dual physician families. WMJ. 2007;106 (5):251-255.
During their residency at Beth Israel Deaconess Medical Center in Boston, hospitalist Margaret Fang, MD, MPH, FHM, and her friends often talked about who they might want to marry: someone completely outside of the medical field? A violinist, perhaps? But when she interviewed for a faculty position at the University of California at San Francisco (UCSF), she met hospitalist Bradley Sharpe, MD, SFHM, then the chief resident in the Department of Medicine.
They married in 2010 and currently work as associate professors in the Department of Medicine at UCSF Medical Center—Margaret as a clinician-investigator and Brad as a clinician-educator and administrator. “I find that [being married to a hospitalist] makes many aspects of communication easier because you have a shared language,” she says.
A common language, a partner who “gets it” if you’re on service 16 days straight, a shared passion for the hospitalist movement: These are the advantages of being married to a fellow hospitalist, say five dual hospitalist couples.
“It is wonderful having a partner who understands where I’m coming from if I do have a rough day,” says Elizabeth “Liz” Gundersen, MD, FHM, who in 2004 tied the knot with hospitalist Jasen Gundersen, MD, MBA, CPE, SFHM.
Heather Wark, MD, who is married to SHM cofounder Win Whitcomb, MD, MHM, seconds that notion. “You don’t have to start from the beginning with anything,” says Dr. Wark, who works as a hospitalist (SNFist), at Farren Care Center, a skilled nursing facility in Turners Falls, Mass. “You can just launch right into whatever the crisis of the day is, and your partner completely understands.”
By and large, the advantages of marrying someone in the same profession outweigh the disadvantages, as a survey of female family physicians recently showed.1 But with those advantages come challenges. Among them:
- Aligning career and relationship goals;
- Juggling demanding schedules; and
- Carving out relationship and family time.
Threading through these issues requires transparent communication, flexibility, and mutual respect, according to these couples.
Career Negotiation
Liz Gundersen recently resigned her position as associate chief of the Division of Hospital Medicine at the University of Massachusetts (UMass) Medical School in Worcester, Mass. The reason? Jasen accepted a new job. As many hospitalists before them have done, the Gundersens pulled up roots and moved across the country, as Jasen started his new job as chief medical officer with TeamHealth Hospital Medicine in Fort Lauderdale, Fla.
“It was a pretty stressful job change,” Jasen says. Following the job offer from TeamHealth, the Gundersens spent “a couple of months” weighing all of their options. “My taking the job was a great promotion for me,” he says, “but Liz also had the opportunity for a great promotion at UMass. In the end, the decision came down to the fact that it was a great opportunity for me and a great opportunity for us, as a couple, to do something new. And I think we weathered it pretty well.”
Liz, who is in the midst of securing her credentials to work in Florida, agrees. She is continuing to work with UMass long-distance, completing the physician schedule and training the new scheduler.
Dr. Whitcomb, who is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., and Dr. Wark married 15 years ago and have worked to configure their relationship to accommodate both career and family. “For most of our relationship,” she explains, “I’ve had a part-time job that has stayed steady.”
Dr. Wark’s professional flexibility allows her to function as a full-time mother to their two children, Maela, 13, and Nicholas, 10. “Although my career has been very successful, Win has been more the one who has undergone career changes and advancements,” she says. “My staying steady has allowed that space in our relationship.”
Drs. Fang and Sharpe haven’t had to cross the bridge of different job offerings yet. But Dr. Sharpe asserts that he’s a firm believer that there should be no difference in how their careers are valued. The couple has an ongoing “transparent conversation,” adds Dr. Fang, about what’s important to each of them and the relative impact of future opportunities. In addition, her job as a researcher is somewhat portable, so the chances of simultaneous job offers might increase. For now, though, they are happily committed to UCSF and love the city of San Francisco.
Madhavi Dandu, MD, MPH, assistant clinical professor and associate director of Pathways to Discovery in Global Health at UCSF, and her husband, Nima Afshar, MD, an ED/hospitalist at UCSF and at the Veterans Affairs Medical Center in San Francisco, have been lucky, she says, because “we were both drawn to medicine for similar reasons.” Together since their second year of medical school, they also both wanted, early on, to pursue careers in academic medicine. “We definitely went through some difficult times, but mostly, we were on the same page,” Dr. Dandu says.
When it came time to apply to a match program for residency, they both applied to UCSF, where they successfully completed their residencies and began their academic careers. They made a conscious decision to wait to have children until their training was finished.
Still, in the first year or so after their daughter’s birth in 2008, Dr. Dandu felt the pull between career and parenthood. “As a physician, you’re driven to make sure you’re not dropping the ball on anything, and there were many weekends that I was away from my daughter,” she says.
A supportive family helped with a flexible childcare arrangement, but this past year, Dr. Dandu decided to scale back her work schedule to 80% of regular shifts in order to spend more time with her daughter. Now, she says, “It’s pretty rare” that she will alter a commitment with her daughter for last-minute calls from work.
Shared and Diverse Interests
Even if they work in the same division, dual-hospitalist couples say they thrive when they also have independent career interests. David O. Meltzer, MD, PhD, FHM, chief of the Division of Hospital Medicine at the University of Chicago’s Department of Medicine and director of the Center for Health and the Social Sciences in Chicago, and his wife, Vineet Arora, MD, MPP, SFHM, assistant dean of Pritzker School of Medicine in Chicago and associate program director of the internal-medicine residency program, pursue independent spheres in addition to occasional collaborations as hospitalist-researchers.
They recently were on clinical service together during a blizzard. “We also co-mentor several trainees,” Dr. Arora says, “which is actually really fun. For example, I can refer trainees to David if they’re interested in economics, and if someone has a quality/safety interest, he could refer that person to me” (see “Keys to Thriving as a Dual-Hospitalist Couple,” above).
The Gundersens’ professional interests forked when Jasen found his niche in administrative work and started to pursue an MBA in 2007. Meanwhile, Liz was finding her own niche doing quality improvement (QI) and became one of the physician quality officers at UMass Memorial.
continued below...
Drs. Fang and Sharpe have experienced similar career divisions with their hospitalist roots. Dr. Sharpe is focused on medical education, while Dr. Fang’s focus predominantly is clinical research. “Between the two of us, we capture many of the elements of academic hospitalist practice,” she says. “I think having our diverse interests gives us a lot of knowledge and expertise about our respective fields. I’m able to learn a lot about how the hospital works and about clinical teaching from Brad, and, hopefully, he can come to me for research advice.”
Drs. Dandu and Afshar have branched out, too. He completed additional residency training in emergency medicine and she acquired an MPH at the University of California at Berkeley. Subsequently, she became associate director of Pathways to Discovery in Global Health, the global health elective program for medical students.
“If you follow your passion in your career, that will allow you to bring a happier individual to your relationship,” Dr. Whitcomb adds.
Schedule Time Together
Communication is a major factor when dual-hospitalist couples plan and execute their weekly schedules. “We try to have an organizing conversation at the end of each weekend,” says Dr. Wark, who also is the keeper of the family calendar and “the glue” that keeps her family of four on track.
Marriage and family therapist Catherine Hastings, PhD, who practices in Lancaster, Pa., says it’s important for dual-hospitalist couples to remember that the relationship needs attention, just as physician careers do.
“It’s very easy to talk about your job when you are in the same profession, but you can easily get consumed by that and let your personal relationships take a back seat,” Dr. Hastings explains. “Couples may look upon conversation about work as ‘brainstorming’ or problem-solving together, but that can also take over.” Hospitalist couples need to be aware that they should plan to be a couple as rigorously as they plan for their jobs, she adds.
Dr. Meltzer doesn’t think that he and his wife consciously delineate between work and personal conversation. “We certainly talk about things that don’t involve work, but we do not say, ‘We will absolutely not talk about work,’ ” he says. “That’s like saying there is not an elephant in the room.”
It didn’t bother the Gundersens that their work came home to a certain extent, says Liz. Even so, to avoid the temptation to “try and churn through all of our work over dinner,” she began scheduling meetings through Jasen’s secretary to discuss work issues.
“When we’re working, we’re doing so full-on,” Jasen says. “But then, we are definitely known for taking recovery time,” which includes skiing vacations and spending weekends on their boat in order to recharge.
Drs. Meltzer and Arora have traveled extensively together for both work and fun. On a trip last year, they traveled to China to a medical school partnered with their own to give talks. They even lengthened their stay to visit the Great Wall of China and toured Beijing and Shanghai.
Dr. Fang considers her husband the “uber-scheduler” in their relationship. “We very consciously build quality time with each other into our schedules,” she says. Without children, for the moment, they also have the free time to grab dinner spontaneously.
Parents First, Physicians Second
Time together as a couple is a scarcer commodity when a dual-hospitalist couple has children. With a pair of pre-teens who are involved in competitive swimming, Drs. Wark and Whitcomb have a two-hour block of time they need plan into their schedule three to four evenings a week.
“We’ve got a built-in babysitter called the YMCA swim team,” Dr. Wark jokes. They also run together several times a week, an activity they use to reconnect. “You have to figure out ways to grow together, to develop and have interests and activities that are specific to the relationship and not related to the kids,” Dr. Whitcomb says. “And if you don’t grow together, you’ll grow apart.”
Drs. Dandu and Afshar, who married in 2003, are just beginning to reacquaint themselves with their adult social lives, she says, now that their daughter is two and a half. “Sometimes we make time to have ‘date night,’ but sometimes it’s just us getting together with our adult friends,” she says.
With or without children, dual-hospitalist couples’ passion for their profession is intertwined with their successful marriages. “Being a physician,” Jasen Gundersen says, “is not just a vocation; it’s part of who you are.”
Dr. Dandu describes it this way: “Our life at home and our life at work are very melded.”
Like Dr. Wang, Dr. Dandu had contemplated a long-term relationship with someone who wasn’t in medicine. But being married to a physician-hospitalist, she says, “turned out to be great for me, because I have someone I can really talk to about everything.” TH
Gretchen Henkel is a freelance writer based in California.
Reference
- Schrager S, Kolan A, Dottl SL. Is that your pager or mine: a survey of women academic family physicians in dual physician families. WMJ. 2007;106 (5):251-255.
During their residency at Beth Israel Deaconess Medical Center in Boston, hospitalist Margaret Fang, MD, MPH, FHM, and her friends often talked about who they might want to marry: someone completely outside of the medical field? A violinist, perhaps? But when she interviewed for a faculty position at the University of California at San Francisco (UCSF), she met hospitalist Bradley Sharpe, MD, SFHM, then the chief resident in the Department of Medicine.
They married in 2010 and currently work as associate professors in the Department of Medicine at UCSF Medical Center—Margaret as a clinician-investigator and Brad as a clinician-educator and administrator. “I find that [being married to a hospitalist] makes many aspects of communication easier because you have a shared language,” she says.
A common language, a partner who “gets it” if you’re on service 16 days straight, a shared passion for the hospitalist movement: These are the advantages of being married to a fellow hospitalist, say five dual hospitalist couples.
“It is wonderful having a partner who understands where I’m coming from if I do have a rough day,” says Elizabeth “Liz” Gundersen, MD, FHM, who in 2004 tied the knot with hospitalist Jasen Gundersen, MD, MBA, CPE, SFHM.
Heather Wark, MD, who is married to SHM cofounder Win Whitcomb, MD, MHM, seconds that notion. “You don’t have to start from the beginning with anything,” says Dr. Wark, who works as a hospitalist (SNFist), at Farren Care Center, a skilled nursing facility in Turners Falls, Mass. “You can just launch right into whatever the crisis of the day is, and your partner completely understands.”
By and large, the advantages of marrying someone in the same profession outweigh the disadvantages, as a survey of female family physicians recently showed.1 But with those advantages come challenges. Among them:
- Aligning career and relationship goals;
- Juggling demanding schedules; and
- Carving out relationship and family time.
Threading through these issues requires transparent communication, flexibility, and mutual respect, according to these couples.
Career Negotiation
Liz Gundersen recently resigned her position as associate chief of the Division of Hospital Medicine at the University of Massachusetts (UMass) Medical School in Worcester, Mass. The reason? Jasen accepted a new job. As many hospitalists before them have done, the Gundersens pulled up roots and moved across the country, as Jasen started his new job as chief medical officer with TeamHealth Hospital Medicine in Fort Lauderdale, Fla.
“It was a pretty stressful job change,” Jasen says. Following the job offer from TeamHealth, the Gundersens spent “a couple of months” weighing all of their options. “My taking the job was a great promotion for me,” he says, “but Liz also had the opportunity for a great promotion at UMass. In the end, the decision came down to the fact that it was a great opportunity for me and a great opportunity for us, as a couple, to do something new. And I think we weathered it pretty well.”
Liz, who is in the midst of securing her credentials to work in Florida, agrees. She is continuing to work with UMass long-distance, completing the physician schedule and training the new scheduler.
Dr. Whitcomb, who is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., and Dr. Wark married 15 years ago and have worked to configure their relationship to accommodate both career and family. “For most of our relationship,” she explains, “I’ve had a part-time job that has stayed steady.”
Dr. Wark’s professional flexibility allows her to function as a full-time mother to their two children, Maela, 13, and Nicholas, 10. “Although my career has been very successful, Win has been more the one who has undergone career changes and advancements,” she says. “My staying steady has allowed that space in our relationship.”
Drs. Fang and Sharpe haven’t had to cross the bridge of different job offerings yet. But Dr. Sharpe asserts that he’s a firm believer that there should be no difference in how their careers are valued. The couple has an ongoing “transparent conversation,” adds Dr. Fang, about what’s important to each of them and the relative impact of future opportunities. In addition, her job as a researcher is somewhat portable, so the chances of simultaneous job offers might increase. For now, though, they are happily committed to UCSF and love the city of San Francisco.
Madhavi Dandu, MD, MPH, assistant clinical professor and associate director of Pathways to Discovery in Global Health at UCSF, and her husband, Nima Afshar, MD, an ED/hospitalist at UCSF and at the Veterans Affairs Medical Center in San Francisco, have been lucky, she says, because “we were both drawn to medicine for similar reasons.” Together since their second year of medical school, they also both wanted, early on, to pursue careers in academic medicine. “We definitely went through some difficult times, but mostly, we were on the same page,” Dr. Dandu says.
When it came time to apply to a match program for residency, they both applied to UCSF, where they successfully completed their residencies and began their academic careers. They made a conscious decision to wait to have children until their training was finished.
Still, in the first year or so after their daughter’s birth in 2008, Dr. Dandu felt the pull between career and parenthood. “As a physician, you’re driven to make sure you’re not dropping the ball on anything, and there were many weekends that I was away from my daughter,” she says.
A supportive family helped with a flexible childcare arrangement, but this past year, Dr. Dandu decided to scale back her work schedule to 80% of regular shifts in order to spend more time with her daughter. Now, she says, “It’s pretty rare” that she will alter a commitment with her daughter for last-minute calls from work.
Shared and Diverse Interests
Even if they work in the same division, dual-hospitalist couples say they thrive when they also have independent career interests. David O. Meltzer, MD, PhD, FHM, chief of the Division of Hospital Medicine at the University of Chicago’s Department of Medicine and director of the Center for Health and the Social Sciences in Chicago, and his wife, Vineet Arora, MD, MPP, SFHM, assistant dean of Pritzker School of Medicine in Chicago and associate program director of the internal-medicine residency program, pursue independent spheres in addition to occasional collaborations as hospitalist-researchers.
They recently were on clinical service together during a blizzard. “We also co-mentor several trainees,” Dr. Arora says, “which is actually really fun. For example, I can refer trainees to David if they’re interested in economics, and if someone has a quality/safety interest, he could refer that person to me” (see “Keys to Thriving as a Dual-Hospitalist Couple,” above).
The Gundersens’ professional interests forked when Jasen found his niche in administrative work and started to pursue an MBA in 2007. Meanwhile, Liz was finding her own niche doing quality improvement (QI) and became one of the physician quality officers at UMass Memorial.
continued below...
Drs. Fang and Sharpe have experienced similar career divisions with their hospitalist roots. Dr. Sharpe is focused on medical education, while Dr. Fang’s focus predominantly is clinical research. “Between the two of us, we capture many of the elements of academic hospitalist practice,” she says. “I think having our diverse interests gives us a lot of knowledge and expertise about our respective fields. I’m able to learn a lot about how the hospital works and about clinical teaching from Brad, and, hopefully, he can come to me for research advice.”
Drs. Dandu and Afshar have branched out, too. He completed additional residency training in emergency medicine and she acquired an MPH at the University of California at Berkeley. Subsequently, she became associate director of Pathways to Discovery in Global Health, the global health elective program for medical students.
“If you follow your passion in your career, that will allow you to bring a happier individual to your relationship,” Dr. Whitcomb adds.
Schedule Time Together
Communication is a major factor when dual-hospitalist couples plan and execute their weekly schedules. “We try to have an organizing conversation at the end of each weekend,” says Dr. Wark, who also is the keeper of the family calendar and “the glue” that keeps her family of four on track.
Marriage and family therapist Catherine Hastings, PhD, who practices in Lancaster, Pa., says it’s important for dual-hospitalist couples to remember that the relationship needs attention, just as physician careers do.
“It’s very easy to talk about your job when you are in the same profession, but you can easily get consumed by that and let your personal relationships take a back seat,” Dr. Hastings explains. “Couples may look upon conversation about work as ‘brainstorming’ or problem-solving together, but that can also take over.” Hospitalist couples need to be aware that they should plan to be a couple as rigorously as they plan for their jobs, she adds.
Dr. Meltzer doesn’t think that he and his wife consciously delineate between work and personal conversation. “We certainly talk about things that don’t involve work, but we do not say, ‘We will absolutely not talk about work,’ ” he says. “That’s like saying there is not an elephant in the room.”
It didn’t bother the Gundersens that their work came home to a certain extent, says Liz. Even so, to avoid the temptation to “try and churn through all of our work over dinner,” she began scheduling meetings through Jasen’s secretary to discuss work issues.
“When we’re working, we’re doing so full-on,” Jasen says. “But then, we are definitely known for taking recovery time,” which includes skiing vacations and spending weekends on their boat in order to recharge.
Drs. Meltzer and Arora have traveled extensively together for both work and fun. On a trip last year, they traveled to China to a medical school partnered with their own to give talks. They even lengthened their stay to visit the Great Wall of China and toured Beijing and Shanghai.
Dr. Fang considers her husband the “uber-scheduler” in their relationship. “We very consciously build quality time with each other into our schedules,” she says. Without children, for the moment, they also have the free time to grab dinner spontaneously.
Parents First, Physicians Second
Time together as a couple is a scarcer commodity when a dual-hospitalist couple has children. With a pair of pre-teens who are involved in competitive swimming, Drs. Wark and Whitcomb have a two-hour block of time they need plan into their schedule three to four evenings a week.
“We’ve got a built-in babysitter called the YMCA swim team,” Dr. Wark jokes. They also run together several times a week, an activity they use to reconnect. “You have to figure out ways to grow together, to develop and have interests and activities that are specific to the relationship and not related to the kids,” Dr. Whitcomb says. “And if you don’t grow together, you’ll grow apart.”
Drs. Dandu and Afshar, who married in 2003, are just beginning to reacquaint themselves with their adult social lives, she says, now that their daughter is two and a half. “Sometimes we make time to have ‘date night,’ but sometimes it’s just us getting together with our adult friends,” she says.
With or without children, dual-hospitalist couples’ passion for their profession is intertwined with their successful marriages. “Being a physician,” Jasen Gundersen says, “is not just a vocation; it’s part of who you are.”
Dr. Dandu describes it this way: “Our life at home and our life at work are very melded.”
Like Dr. Wang, Dr. Dandu had contemplated a long-term relationship with someone who wasn’t in medicine. But being married to a physician-hospitalist, she says, “turned out to be great for me, because I have someone I can really talk to about everything.” TH
Gretchen Henkel is a freelance writer based in California.
Reference
- Schrager S, Kolan A, Dottl SL. Is that your pager or mine: a survey of women academic family physicians in dual physician families. WMJ. 2007;106 (5):251-255.
ONLINE EXCLUSIVE: Listen to billing and coding consultants discuss the importance of provider buy-in
Click here to listen to Dr. Pinson
Click here to listen to Ms. Leong
Click here to listen to Dr. Pinson
Click here to listen to Ms. Leong
Click here to listen to Dr. Pinson
Click here to listen to Ms. Leong
ONLINE EXCLUSIVE: Listen to a dual-hospitalist couple talk about their shared and diverse interests
How to Find a Mentor in the Mentorship Gap
Looking for a mentor to help guide your career development? HM presents young physicians with unique challenges and opportunities.
As a relatively young field, HM hasn't yet accrued a depth of senior leaders. Protected time is in shorter supply in academic medicine, as hospitalists bridge the Accreditation Council for Graduate Medical Education (ACGME) duty-hour coverage gap. In community hospitals, hospitalists are expressly hired to provide clinical coverage, and rewards for career advancement might not be included in the hospital's contract with the program. (For more on career advancement, listen to experts talk about why hospitalists make great hospital leaders.)

—Jeff Wiese, MD, SFHM, professor, associate dean for Graduate Medical Education, Tulane University Health Sciences Center, New Orleans
Each is a reason Steven B. Deitelzweig, MD, MMM, FACP, SFHM, vice president of medical affairs and system chairman of the Department of Hospital Medicine at Ochsner Health System in New Orleans, concludes: "If you rely on hospital medicine to teach you hospital medicine, you're only going to get so far in this day and age."
Big Community Ops
Working a week on/week off schedule might be the preferred goal for some hospitalists in the community setting, says Erik DeLue, MD, MBA, SFHM, hospitalist medical director for the Virtua healthcare system, which runs four hospitals in southern New Jersey. But if you find yourself asking, "Is there more out there for me?" community settings offer lots of opportunities to explore.
For example, one PhD physician in Dr. DeLue's group is parlaying her interest in research to the next level by submitting an abstract to the SHM annual meeting's poster competition regarding care coordination and fragmentation rates. Two other hospitalists share a clinical position (each works 0.5 FTE). On their off time, one works in information technology (IT) for Virtua, which pays the other half of his salary; the other does IT work for two hospital systems in New York City.
Click here to read the full story.
Searching for a new opportunity? View hundreds of jobs at SHM's Career Center.
Looking for a mentor to help guide your career development? HM presents young physicians with unique challenges and opportunities.
As a relatively young field, HM hasn't yet accrued a depth of senior leaders. Protected time is in shorter supply in academic medicine, as hospitalists bridge the Accreditation Council for Graduate Medical Education (ACGME) duty-hour coverage gap. In community hospitals, hospitalists are expressly hired to provide clinical coverage, and rewards for career advancement might not be included in the hospital's contract with the program. (For more on career advancement, listen to experts talk about why hospitalists make great hospital leaders.)

—Jeff Wiese, MD, SFHM, professor, associate dean for Graduate Medical Education, Tulane University Health Sciences Center, New Orleans
Each is a reason Steven B. Deitelzweig, MD, MMM, FACP, SFHM, vice president of medical affairs and system chairman of the Department of Hospital Medicine at Ochsner Health System in New Orleans, concludes: "If you rely on hospital medicine to teach you hospital medicine, you're only going to get so far in this day and age."
Big Community Ops
Working a week on/week off schedule might be the preferred goal for some hospitalists in the community setting, says Erik DeLue, MD, MBA, SFHM, hospitalist medical director for the Virtua healthcare system, which runs four hospitals in southern New Jersey. But if you find yourself asking, "Is there more out there for me?" community settings offer lots of opportunities to explore.
For example, one PhD physician in Dr. DeLue's group is parlaying her interest in research to the next level by submitting an abstract to the SHM annual meeting's poster competition regarding care coordination and fragmentation rates. Two other hospitalists share a clinical position (each works 0.5 FTE). On their off time, one works in information technology (IT) for Virtua, which pays the other half of his salary; the other does IT work for two hospital systems in New York City.
Click here to read the full story.
Searching for a new opportunity? View hundreds of jobs at SHM's Career Center.
Looking for a mentor to help guide your career development? HM presents young physicians with unique challenges and opportunities.
As a relatively young field, HM hasn't yet accrued a depth of senior leaders. Protected time is in shorter supply in academic medicine, as hospitalists bridge the Accreditation Council for Graduate Medical Education (ACGME) duty-hour coverage gap. In community hospitals, hospitalists are expressly hired to provide clinical coverage, and rewards for career advancement might not be included in the hospital's contract with the program. (For more on career advancement, listen to experts talk about why hospitalists make great hospital leaders.)

—Jeff Wiese, MD, SFHM, professor, associate dean for Graduate Medical Education, Tulane University Health Sciences Center, New Orleans
Each is a reason Steven B. Deitelzweig, MD, MMM, FACP, SFHM, vice president of medical affairs and system chairman of the Department of Hospital Medicine at Ochsner Health System in New Orleans, concludes: "If you rely on hospital medicine to teach you hospital medicine, you're only going to get so far in this day and age."
Big Community Ops
Working a week on/week off schedule might be the preferred goal for some hospitalists in the community setting, says Erik DeLue, MD, MBA, SFHM, hospitalist medical director for the Virtua healthcare system, which runs four hospitals in southern New Jersey. But if you find yourself asking, "Is there more out there for me?" community settings offer lots of opportunities to explore.
For example, one PhD physician in Dr. DeLue's group is parlaying her interest in research to the next level by submitting an abstract to the SHM annual meeting's poster competition regarding care coordination and fragmentation rates. Two other hospitalists share a clinical position (each works 0.5 FTE). On their off time, one works in information technology (IT) for Virtua, which pays the other half of his salary; the other does IT work for two hospital systems in New York City.
Click here to read the full story.
Searching for a new opportunity? View hundreds of jobs at SHM's Career Center.
The Locums Litmus Test: Is Per Diem Work for You?
Family-medicine-trained hospitalist Benjamin Craig Hamilton, MD,mightrepresent the ideal locum tenens candidate. He’s single, enjoys the challenge of working in new environments, and has is licensed in six states. Currently based in Knoxville, Tenn., he values the professional and monetary rewards of per diem work.
“The beauty is that you can work three months and take three months off,” says Dr. Hamilton, one of thousands of physicians who contract to provide temporary coverage to fill staffing gaps at HM programs around the country. Dr. Hamilton works for Locum Leaders LLC, a national locums firm headquartered in Alpharetta, Ga., that focuses on hospitalists. “If you’re willing to go, you’re never without work. It’s the ultimate flexibility.”
Are You Suited?
Flexibilitytops the list of qualities locum tenens recruiters look for. “The more they [the candidates] can say ‘yes,’ the more likely that we can find a good fit for them,” says Andrea Oldendorf, physician recruiter for Nashville, Tenn.-based Cogent Healthcare. Oldendorfhandles locum tenens placements in the company’s central and western regions.
“We’re a very team-oriented company,” Oldendorf says, noting her objective is to integrate a locum physician into an HM group. “If someone comes in with a lot of limitations, such as ‘I won’t work nights’ or ‘I won’t cover ER admissions,’ that starts to narrow the pool of places where we can use them.”
Every HM program is a little different, according to Robert W. Harrington, MD, SFHM, chief medical officer at Locum Leaders LLC and chair of SHM’s Family Medicine Task Force. “Being able to work with new people, new systems, new computers, and new nursing staff is very important,” he says. Interestingly, the credentialing process provides his recruiters an avenue for gaugingcandidates’ flexibility.“There is so much paperwork, and there are certain parts of it that we can’t do. By the time they get through credentialing, we know whether they’re flexible or not.”
Temporary Work = Test Run
The monetary rewards of locums work often are cited as a major advantage. Locum physicians can gross 30% to 40% more per year (about $280,000 to $300,000) for the same number of shifts as a typical FTE hospitalist (median compensation for non-teaching hospitalists is $215,000 per year, according to the 2010 MGMA-SHM State of Hospital Medicine report). As contracted employees, locum physicians are self-employed and must report their own income and pay their own taxes; many times locum physicians need to hire an accountant.
Working locum tenens also offers a chance to sample a variety of hospital settings. “There’s a big difference between a small rural hospital and a big teaching hospital with a closed ICU,” points out Karen Belote, a physician recruiter for Locum Leaders. “[Working locums] is a great way to try some different locations and different hospitals before settling into a permanent position.”
Pitfalls and Cautions
The only pitfall Dr. Hamilton has observed is perception.“Some people have an initial gut reflex that a locums doctor is either running from something or is not of the same caliber as a permanent physician,” he says. But that notion is quickly dispelled, he says, when he or she demonstrates flexibility, competency, and eagerness to work with the team.
Dr. Hamilton has found a great fit with his current assignments and has no immediate plans to take a permanent position. “I’m learning every day,” he says. “Remember, you are the boss of your life.”
Gretchen Henkel is a freelance writer based in California.
Increase your hirability
Thinking of taking a locum tenens assignment? Consider acquiring additional procedural competencies during your third year of residency, Dr. Harrington advises.
“We are getting more and more requests for people who are comfortable with procedural skills, such as intubations, placing central lines, and vent management,” he says.
Your locum tenens agency might underwrite a procedures course, as Locum Leaders did for Dr. Hamilton. Just make sure you don’t misrepresent your abilities or your comfort level, he cautions. “Know your limits and realize that you are building your career every month,” he says.
SHM will offer a pre-course, “Medical Procedures for the Hospitalist,” at HM11 (May 9, 2011 in Grapevine, Texas), and at many of the HM regional meetings.—GH
Family-medicine-trained hospitalist Benjamin Craig Hamilton, MD,mightrepresent the ideal locum tenens candidate. He’s single, enjoys the challenge of working in new environments, and has is licensed in six states. Currently based in Knoxville, Tenn., he values the professional and monetary rewards of per diem work.
“The beauty is that you can work three months and take three months off,” says Dr. Hamilton, one of thousands of physicians who contract to provide temporary coverage to fill staffing gaps at HM programs around the country. Dr. Hamilton works for Locum Leaders LLC, a national locums firm headquartered in Alpharetta, Ga., that focuses on hospitalists. “If you’re willing to go, you’re never without work. It’s the ultimate flexibility.”
Are You Suited?
Flexibilitytops the list of qualities locum tenens recruiters look for. “The more they [the candidates] can say ‘yes,’ the more likely that we can find a good fit for them,” says Andrea Oldendorf, physician recruiter for Nashville, Tenn.-based Cogent Healthcare. Oldendorfhandles locum tenens placements in the company’s central and western regions.
“We’re a very team-oriented company,” Oldendorf says, noting her objective is to integrate a locum physician into an HM group. “If someone comes in with a lot of limitations, such as ‘I won’t work nights’ or ‘I won’t cover ER admissions,’ that starts to narrow the pool of places where we can use them.”
Every HM program is a little different, according to Robert W. Harrington, MD, SFHM, chief medical officer at Locum Leaders LLC and chair of SHM’s Family Medicine Task Force. “Being able to work with new people, new systems, new computers, and new nursing staff is very important,” he says. Interestingly, the credentialing process provides his recruiters an avenue for gaugingcandidates’ flexibility.“There is so much paperwork, and there are certain parts of it that we can’t do. By the time they get through credentialing, we know whether they’re flexible or not.”
Temporary Work = Test Run
The monetary rewards of locums work often are cited as a major advantage. Locum physicians can gross 30% to 40% more per year (about $280,000 to $300,000) for the same number of shifts as a typical FTE hospitalist (median compensation for non-teaching hospitalists is $215,000 per year, according to the 2010 MGMA-SHM State of Hospital Medicine report). As contracted employees, locum physicians are self-employed and must report their own income and pay their own taxes; many times locum physicians need to hire an accountant.
Working locum tenens also offers a chance to sample a variety of hospital settings. “There’s a big difference between a small rural hospital and a big teaching hospital with a closed ICU,” points out Karen Belote, a physician recruiter for Locum Leaders. “[Working locums] is a great way to try some different locations and different hospitals before settling into a permanent position.”
Pitfalls and Cautions
The only pitfall Dr. Hamilton has observed is perception.“Some people have an initial gut reflex that a locums doctor is either running from something or is not of the same caliber as a permanent physician,” he says. But that notion is quickly dispelled, he says, when he or she demonstrates flexibility, competency, and eagerness to work with the team.
Dr. Hamilton has found a great fit with his current assignments and has no immediate plans to take a permanent position. “I’m learning every day,” he says. “Remember, you are the boss of your life.”
Gretchen Henkel is a freelance writer based in California.
Increase your hirability
Thinking of taking a locum tenens assignment? Consider acquiring additional procedural competencies during your third year of residency, Dr. Harrington advises.
“We are getting more and more requests for people who are comfortable with procedural skills, such as intubations, placing central lines, and vent management,” he says.
Your locum tenens agency might underwrite a procedures course, as Locum Leaders did for Dr. Hamilton. Just make sure you don’t misrepresent your abilities or your comfort level, he cautions. “Know your limits and realize that you are building your career every month,” he says.
SHM will offer a pre-course, “Medical Procedures for the Hospitalist,” at HM11 (May 9, 2011 in Grapevine, Texas), and at many of the HM regional meetings.—GH
Family-medicine-trained hospitalist Benjamin Craig Hamilton, MD,mightrepresent the ideal locum tenens candidate. He’s single, enjoys the challenge of working in new environments, and has is licensed in six states. Currently based in Knoxville, Tenn., he values the professional and monetary rewards of per diem work.
“The beauty is that you can work three months and take three months off,” says Dr. Hamilton, one of thousands of physicians who contract to provide temporary coverage to fill staffing gaps at HM programs around the country. Dr. Hamilton works for Locum Leaders LLC, a national locums firm headquartered in Alpharetta, Ga., that focuses on hospitalists. “If you’re willing to go, you’re never without work. It’s the ultimate flexibility.”
Are You Suited?
Flexibilitytops the list of qualities locum tenens recruiters look for. “The more they [the candidates] can say ‘yes,’ the more likely that we can find a good fit for them,” says Andrea Oldendorf, physician recruiter for Nashville, Tenn.-based Cogent Healthcare. Oldendorfhandles locum tenens placements in the company’s central and western regions.
“We’re a very team-oriented company,” Oldendorf says, noting her objective is to integrate a locum physician into an HM group. “If someone comes in with a lot of limitations, such as ‘I won’t work nights’ or ‘I won’t cover ER admissions,’ that starts to narrow the pool of places where we can use them.”
Every HM program is a little different, according to Robert W. Harrington, MD, SFHM, chief medical officer at Locum Leaders LLC and chair of SHM’s Family Medicine Task Force. “Being able to work with new people, new systems, new computers, and new nursing staff is very important,” he says. Interestingly, the credentialing process provides his recruiters an avenue for gaugingcandidates’ flexibility.“There is so much paperwork, and there are certain parts of it that we can’t do. By the time they get through credentialing, we know whether they’re flexible or not.”
Temporary Work = Test Run
The monetary rewards of locums work often are cited as a major advantage. Locum physicians can gross 30% to 40% more per year (about $280,000 to $300,000) for the same number of shifts as a typical FTE hospitalist (median compensation for non-teaching hospitalists is $215,000 per year, according to the 2010 MGMA-SHM State of Hospital Medicine report). As contracted employees, locum physicians are self-employed and must report their own income and pay their own taxes; many times locum physicians need to hire an accountant.
Working locum tenens also offers a chance to sample a variety of hospital settings. “There’s a big difference between a small rural hospital and a big teaching hospital with a closed ICU,” points out Karen Belote, a physician recruiter for Locum Leaders. “[Working locums] is a great way to try some different locations and different hospitals before settling into a permanent position.”
Pitfalls and Cautions
The only pitfall Dr. Hamilton has observed is perception.“Some people have an initial gut reflex that a locums doctor is either running from something or is not of the same caliber as a permanent physician,” he says. But that notion is quickly dispelled, he says, when he or she demonstrates flexibility, competency, and eagerness to work with the team.
Dr. Hamilton has found a great fit with his current assignments and has no immediate plans to take a permanent position. “I’m learning every day,” he says. “Remember, you are the boss of your life.”
Gretchen Henkel is a freelance writer based in California.
Increase your hirability
Thinking of taking a locum tenens assignment? Consider acquiring additional procedural competencies during your third year of residency, Dr. Harrington advises.
“We are getting more and more requests for people who are comfortable with procedural skills, such as intubations, placing central lines, and vent management,” he says.
Your locum tenens agency might underwrite a procedures course, as Locum Leaders did for Dr. Hamilton. Just make sure you don’t misrepresent your abilities or your comfort level, he cautions. “Know your limits and realize that you are building your career every month,” he says.
SHM will offer a pre-course, “Medical Procedures for the Hospitalist,” at HM11 (May 9, 2011 in Grapevine, Texas), and at many of the HM regional meetings.—GH
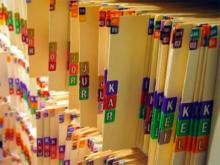
The Triple Crown: Collaboration with clinical documentation specialists can be a win-win for patients, hospitals, and HM
“Doctor, please clarify: Is this type of congestive heart failure acute or chronic, systolic or diastolic?” Most hospitalists have had patients’ charts flagged with these types of queries. And no, the people who write the questions are not trying to be difficult.
In fact, says Karen Bachman, BSN, MHSA, director of clinical documentation at 300-bed Good Samaritan Hospital in Suffern, N.Y., the specialists who place worksheets on hospitalists’ charts are sympathetic to the perceived disconnect between clinical processes and the language of the coding world. Even for nurses, the ICD-9-CM, the manual upon which Medicare bases its reimbursement structure, “is a different language,” she says. “You have to think like a coder.”
And in the coding world, as the saying goes, “if it’s not documented, it didn’t happen.”
That’s where clinical documentation specialists come in. Collaborating with documentation specialists can help boost patient quality, hospital reimbursement, and your hospital’s recognition of the value your HM group adds.
Stephanie Jensen, RN, BSN, coordinator of the Clinical Documentation Integrity (CDI) program at The Nebraska Medical Center in Omaha, summed it up this way: The chart has become more than what it was originally intended. It’s now the repository of “the patient’s story. We’re just trying to help physicians capture the quality of care that they’re giving, and to make sure that, in the medical record, the documentation supports the severity of illness, risk of mortality, and overall clinical picture.”
—Stephanie Jensen, RN, BSN, coordinator, Clinical Documentation Integrity (CDI) program, The Nebraska Medical Center, Omaha
For example, even though nurses can stage a pressure ulcer, the stage must be accompanied by the hospitalist’s diagnosis of decubitus ulcer in order for the coders in the Health Information Management and Services (HIMS) department to properly code the diagnosis, which affects the DRG submitted to Medicare/CMS.
The Challenge
Bachmann thinks the biggest challenge to proper documentation is time. Hospitalists are immersed in caring for their patients. They must balance different coding systems—the ICD-9-CM, as well as CPT and E/M coding for their own billing. They often feel pulled between taking extra time to clarify their working or discharge diagnoses and getting on to the next patient. The catch, though, is that hospital coders can rely only on what the treating physician documents.
At Good Samaritan, documentation specialists see themselves as allies in this process. They use the JA Thomas documentation system and print out worksheets to attach to patients’ charts; it’s intended to be a trigger so that the hospitalist will be as specific with documentation as possible. “As nurses,” Bachmann explains, “we understand what physicians need and what the coders need. We’re an intermediary between the two.”
At The Nebraska Medical Center, the hospital’s mortality committee initiated a systemwide CDI program in November 2009. Jensen explains that every new staff physician at the 689-bed facility now receives a CDI toolkit detailing the documentation program. The six CDI team members wear blue T-shirts, and documentation clarification worksheets are on blue paper.
Further Education
During monthly in-services at hospitalists’ meetings, says Bachmann, “we stress the importance of linking the etiology with the diagnosis. We illustrate how different diagnoses will be given different relative weights for DRGs.” The effort has proven to be an effective educational tool, she says.
Jensen admits that the semantic differences between the clinical and coding worlds can be challenging. But, she says, the more specific physicians can be, the more it will help all indicators in the long run: patient safety, physician profiles, and, yes, hospital reimbursement. And for demonstrating hospitalists’ value, that’s considerable return on investment of the time it takes to write a complete note.
Gretchen Henkel is a freelance writer based in California.
“Doctor, please clarify: Is this type of congestive heart failure acute or chronic, systolic or diastolic?” Most hospitalists have had patients’ charts flagged with these types of queries. And no, the people who write the questions are not trying to be difficult.
In fact, says Karen Bachman, BSN, MHSA, director of clinical documentation at 300-bed Good Samaritan Hospital in Suffern, N.Y., the specialists who place worksheets on hospitalists’ charts are sympathetic to the perceived disconnect between clinical processes and the language of the coding world. Even for nurses, the ICD-9-CM, the manual upon which Medicare bases its reimbursement structure, “is a different language,” she says. “You have to think like a coder.”
And in the coding world, as the saying goes, “if it’s not documented, it didn’t happen.”
That’s where clinical documentation specialists come in. Collaborating with documentation specialists can help boost patient quality, hospital reimbursement, and your hospital’s recognition of the value your HM group adds.
Stephanie Jensen, RN, BSN, coordinator of the Clinical Documentation Integrity (CDI) program at The Nebraska Medical Center in Omaha, summed it up this way: The chart has become more than what it was originally intended. It’s now the repository of “the patient’s story. We’re just trying to help physicians capture the quality of care that they’re giving, and to make sure that, in the medical record, the documentation supports the severity of illness, risk of mortality, and overall clinical picture.”
—Stephanie Jensen, RN, BSN, coordinator, Clinical Documentation Integrity (CDI) program, The Nebraska Medical Center, Omaha
For example, even though nurses can stage a pressure ulcer, the stage must be accompanied by the hospitalist’s diagnosis of decubitus ulcer in order for the coders in the Health Information Management and Services (HIMS) department to properly code the diagnosis, which affects the DRG submitted to Medicare/CMS.
The Challenge
Bachmann thinks the biggest challenge to proper documentation is time. Hospitalists are immersed in caring for their patients. They must balance different coding systems—the ICD-9-CM, as well as CPT and E/M coding for their own billing. They often feel pulled between taking extra time to clarify their working or discharge diagnoses and getting on to the next patient. The catch, though, is that hospital coders can rely only on what the treating physician documents.
At Good Samaritan, documentation specialists see themselves as allies in this process. They use the JA Thomas documentation system and print out worksheets to attach to patients’ charts; it’s intended to be a trigger so that the hospitalist will be as specific with documentation as possible. “As nurses,” Bachmann explains, “we understand what physicians need and what the coders need. We’re an intermediary between the two.”
At The Nebraska Medical Center, the hospital’s mortality committee initiated a systemwide CDI program in November 2009. Jensen explains that every new staff physician at the 689-bed facility now receives a CDI toolkit detailing the documentation program. The six CDI team members wear blue T-shirts, and documentation clarification worksheets are on blue paper.
Further Education
During monthly in-services at hospitalists’ meetings, says Bachmann, “we stress the importance of linking the etiology with the diagnosis. We illustrate how different diagnoses will be given different relative weights for DRGs.” The effort has proven to be an effective educational tool, she says.
Jensen admits that the semantic differences between the clinical and coding worlds can be challenging. But, she says, the more specific physicians can be, the more it will help all indicators in the long run: patient safety, physician profiles, and, yes, hospital reimbursement. And for demonstrating hospitalists’ value, that’s considerable return on investment of the time it takes to write a complete note.
Gretchen Henkel is a freelance writer based in California.
“Doctor, please clarify: Is this type of congestive heart failure acute or chronic, systolic or diastolic?” Most hospitalists have had patients’ charts flagged with these types of queries. And no, the people who write the questions are not trying to be difficult.
In fact, says Karen Bachman, BSN, MHSA, director of clinical documentation at 300-bed Good Samaritan Hospital in Suffern, N.Y., the specialists who place worksheets on hospitalists’ charts are sympathetic to the perceived disconnect between clinical processes and the language of the coding world. Even for nurses, the ICD-9-CM, the manual upon which Medicare bases its reimbursement structure, “is a different language,” she says. “You have to think like a coder.”
And in the coding world, as the saying goes, “if it’s not documented, it didn’t happen.”
That’s where clinical documentation specialists come in. Collaborating with documentation specialists can help boost patient quality, hospital reimbursement, and your hospital’s recognition of the value your HM group adds.
Stephanie Jensen, RN, BSN, coordinator of the Clinical Documentation Integrity (CDI) program at The Nebraska Medical Center in Omaha, summed it up this way: The chart has become more than what it was originally intended. It’s now the repository of “the patient’s story. We’re just trying to help physicians capture the quality of care that they’re giving, and to make sure that, in the medical record, the documentation supports the severity of illness, risk of mortality, and overall clinical picture.”
—Stephanie Jensen, RN, BSN, coordinator, Clinical Documentation Integrity (CDI) program, The Nebraska Medical Center, Omaha
For example, even though nurses can stage a pressure ulcer, the stage must be accompanied by the hospitalist’s diagnosis of decubitus ulcer in order for the coders in the Health Information Management and Services (HIMS) department to properly code the diagnosis, which affects the DRG submitted to Medicare/CMS.
The Challenge
Bachmann thinks the biggest challenge to proper documentation is time. Hospitalists are immersed in caring for their patients. They must balance different coding systems—the ICD-9-CM, as well as CPT and E/M coding for their own billing. They often feel pulled between taking extra time to clarify their working or discharge diagnoses and getting on to the next patient. The catch, though, is that hospital coders can rely only on what the treating physician documents.
At Good Samaritan, documentation specialists see themselves as allies in this process. They use the JA Thomas documentation system and print out worksheets to attach to patients’ charts; it’s intended to be a trigger so that the hospitalist will be as specific with documentation as possible. “As nurses,” Bachmann explains, “we understand what physicians need and what the coders need. We’re an intermediary between the two.”
At The Nebraska Medical Center, the hospital’s mortality committee initiated a systemwide CDI program in November 2009. Jensen explains that every new staff physician at the 689-bed facility now receives a CDI toolkit detailing the documentation program. The six CDI team members wear blue T-shirts, and documentation clarification worksheets are on blue paper.
Further Education
During monthly in-services at hospitalists’ meetings, says Bachmann, “we stress the importance of linking the etiology with the diagnosis. We illustrate how different diagnoses will be given different relative weights for DRGs.” The effort has proven to be an effective educational tool, she says.
Jensen admits that the semantic differences between the clinical and coding worlds can be challenging. But, she says, the more specific physicians can be, the more it will help all indicators in the long run: patient safety, physician profiles, and, yes, hospital reimbursement. And for demonstrating hospitalists’ value, that’s considerable return on investment of the time it takes to write a complete note.
Gretchen Henkel is a freelance writer based in California.
Rewards and Challenges of Two-Physician Marriages
For hospitalist Kirsten N. Kangelaris, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California at San Francisco (UCSF), there are several benefits to being married to a physician. "It's nice to be able to relate with your spouse on a professional, as well as a personal, level," she says.
Although coordinating schedules can be challenging, one of the pluses of being married to another physician is that your spouse understands the lifestyle, says Sarina B. Schrager, MD, associate professor in the Department of Family Medicine at the University of Wisconsin School of Medicine and Public Health in Madison. In 2007, Dr. Schrager surveyed female physicians (WMJ. 106(5);251-255) and found that most reported that there were benefits to having a physician partner.
Making Work Work
Keith Ashby, MD, is a hospitalist and intensivist at Rapides Regional Medical Center in Alexandria, La., and regional director for Hospitalists Management Group (HMG), supervising three other hospitals from Lafayette to Houston. He and his wife, Agnes, a rheumatologist in private practice, met in Chicago 17 years ago, when he was an attending and she a resident in rheumatology. "It truly does help to have your best friend as a support and also a colleague," he says, though the scheduling can sometimes be daunting. "It takes some creative planning and ingenuity to figure out how to couple work and family responsibilities so that neither comes up short."
One way Dr. Kangelaris and her husband, Gerald, a fourth-year resident in otolaryngology/head and neck surgery at UCSF, manage is to avoid compartmentalizing tasks: Each takes a part in childcare, preparing meals, and other household duties when the other is on duty at the hospital. On the advice of a mentor, Dr. Kangelaris and her husband hired a weekly housecleaning service—a boon for mental health and relationship time, she says.
Contingency Plans
Dr. Ashby and his wife moved away from "the comfort of family" when they left Chicago to embark on their dual careers. Without aunts, uncles, or grandparents to turn to for sharing the childcare load, they built a strong support network of friends and other working parents to help bridge the gap.
Dr. Kangelaris and her husband enrolled their now-2-year-old daughter in a university-sponsored childcare center when she was an infant. They also make an effort to stagger their clinical duties. She admits that most of the flexibility in work schedules is coming from her direction right now because her husband's time is "not his own.". There are many young families in the division at UCSF, and Dr. Kangelaris says most of her scheduling requests are honored.
"In a lot of ways, academic medicine does provide more flexibility," Dr. Schrager says. She advises job-seeking residents to anticipate future goals. "Look for a place that, regardless of what your life situation is now, might be flexible for you in the future."
Gretchen Henkel is a freelance writer based in California.
Protect Relationship Time
Instituting a “date night” is one popular strategy for staying in touch with your partner. Now that their teenagers have full social schedules, weekly date nights are a little bit challenging, Dr. Ashby admits, so he and his physician wife plan getaways: If one partner travels to a medical meeting, the other tags along; if the kids are at summer camp, they take an extended trip.
With a 2-year-old and a husband who is a surgical resident, Dr. Kangelaris says they struggle to reach a work-life balance, and look forward to a time when they can reinstitute their own date night.
Just be sure, advises Jim Bird, president and CEO of Atlanta-based training firm WorkLifeBalance.com, that you don’t inadvertently turn date night into meeting night. Table the conversations about work and bills until another time.
Dr. Schrager couldn’t agree more, noting most female physicians in her survey of dual-physician couples noted that they try to limit talk about work, then turn to other subjects.—GH
For hospitalist Kirsten N. Kangelaris, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California at San Francisco (UCSF), there are several benefits to being married to a physician. "It's nice to be able to relate with your spouse on a professional, as well as a personal, level," she says.
Although coordinating schedules can be challenging, one of the pluses of being married to another physician is that your spouse understands the lifestyle, says Sarina B. Schrager, MD, associate professor in the Department of Family Medicine at the University of Wisconsin School of Medicine and Public Health in Madison. In 2007, Dr. Schrager surveyed female physicians (WMJ. 106(5);251-255) and found that most reported that there were benefits to having a physician partner.
Making Work Work
Keith Ashby, MD, is a hospitalist and intensivist at Rapides Regional Medical Center in Alexandria, La., and regional director for Hospitalists Management Group (HMG), supervising three other hospitals from Lafayette to Houston. He and his wife, Agnes, a rheumatologist in private practice, met in Chicago 17 years ago, when he was an attending and she a resident in rheumatology. "It truly does help to have your best friend as a support and also a colleague," he says, though the scheduling can sometimes be daunting. "It takes some creative planning and ingenuity to figure out how to couple work and family responsibilities so that neither comes up short."
One way Dr. Kangelaris and her husband, Gerald, a fourth-year resident in otolaryngology/head and neck surgery at UCSF, manage is to avoid compartmentalizing tasks: Each takes a part in childcare, preparing meals, and other household duties when the other is on duty at the hospital. On the advice of a mentor, Dr. Kangelaris and her husband hired a weekly housecleaning service—a boon for mental health and relationship time, she says.
Contingency Plans
Dr. Ashby and his wife moved away from "the comfort of family" when they left Chicago to embark on their dual careers. Without aunts, uncles, or grandparents to turn to for sharing the childcare load, they built a strong support network of friends and other working parents to help bridge the gap.
Dr. Kangelaris and her husband enrolled their now-2-year-old daughter in a university-sponsored childcare center when she was an infant. They also make an effort to stagger their clinical duties. She admits that most of the flexibility in work schedules is coming from her direction right now because her husband's time is "not his own.". There are many young families in the division at UCSF, and Dr. Kangelaris says most of her scheduling requests are honored.
"In a lot of ways, academic medicine does provide more flexibility," Dr. Schrager says. She advises job-seeking residents to anticipate future goals. "Look for a place that, regardless of what your life situation is now, might be flexible for you in the future."
Gretchen Henkel is a freelance writer based in California.
Protect Relationship Time
Instituting a “date night” is one popular strategy for staying in touch with your partner. Now that their teenagers have full social schedules, weekly date nights are a little bit challenging, Dr. Ashby admits, so he and his physician wife plan getaways: If one partner travels to a medical meeting, the other tags along; if the kids are at summer camp, they take an extended trip.
With a 2-year-old and a husband who is a surgical resident, Dr. Kangelaris says they struggle to reach a work-life balance, and look forward to a time when they can reinstitute their own date night.
Just be sure, advises Jim Bird, president and CEO of Atlanta-based training firm WorkLifeBalance.com, that you don’t inadvertently turn date night into meeting night. Table the conversations about work and bills until another time.
Dr. Schrager couldn’t agree more, noting most female physicians in her survey of dual-physician couples noted that they try to limit talk about work, then turn to other subjects.—GH
For hospitalist Kirsten N. Kangelaris, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California at San Francisco (UCSF), there are several benefits to being married to a physician. "It's nice to be able to relate with your spouse on a professional, as well as a personal, level," she says.
Although coordinating schedules can be challenging, one of the pluses of being married to another physician is that your spouse understands the lifestyle, says Sarina B. Schrager, MD, associate professor in the Department of Family Medicine at the University of Wisconsin School of Medicine and Public Health in Madison. In 2007, Dr. Schrager surveyed female physicians (WMJ. 106(5);251-255) and found that most reported that there were benefits to having a physician partner.
Making Work Work
Keith Ashby, MD, is a hospitalist and intensivist at Rapides Regional Medical Center in Alexandria, La., and regional director for Hospitalists Management Group (HMG), supervising three other hospitals from Lafayette to Houston. He and his wife, Agnes, a rheumatologist in private practice, met in Chicago 17 years ago, when he was an attending and she a resident in rheumatology. "It truly does help to have your best friend as a support and also a colleague," he says, though the scheduling can sometimes be daunting. "It takes some creative planning and ingenuity to figure out how to couple work and family responsibilities so that neither comes up short."
One way Dr. Kangelaris and her husband, Gerald, a fourth-year resident in otolaryngology/head and neck surgery at UCSF, manage is to avoid compartmentalizing tasks: Each takes a part in childcare, preparing meals, and other household duties when the other is on duty at the hospital. On the advice of a mentor, Dr. Kangelaris and her husband hired a weekly housecleaning service—a boon for mental health and relationship time, she says.
Contingency Plans
Dr. Ashby and his wife moved away from "the comfort of family" when they left Chicago to embark on their dual careers. Without aunts, uncles, or grandparents to turn to for sharing the childcare load, they built a strong support network of friends and other working parents to help bridge the gap.
Dr. Kangelaris and her husband enrolled their now-2-year-old daughter in a university-sponsored childcare center when she was an infant. They also make an effort to stagger their clinical duties. She admits that most of the flexibility in work schedules is coming from her direction right now because her husband's time is "not his own.". There are many young families in the division at UCSF, and Dr. Kangelaris says most of her scheduling requests are honored.
"In a lot of ways, academic medicine does provide more flexibility," Dr. Schrager says. She advises job-seeking residents to anticipate future goals. "Look for a place that, regardless of what your life situation is now, might be flexible for you in the future."
Gretchen Henkel is a freelance writer based in California.
Protect Relationship Time
Instituting a “date night” is one popular strategy for staying in touch with your partner. Now that their teenagers have full social schedules, weekly date nights are a little bit challenging, Dr. Ashby admits, so he and his physician wife plan getaways: If one partner travels to a medical meeting, the other tags along; if the kids are at summer camp, they take an extended trip.
With a 2-year-old and a husband who is a surgical resident, Dr. Kangelaris says they struggle to reach a work-life balance, and look forward to a time when they can reinstitute their own date night.
Just be sure, advises Jim Bird, president and CEO of Atlanta-based training firm WorkLifeBalance.com, that you don’t inadvertently turn date night into meeting night. Table the conversations about work and bills until another time.
Dr. Schrager couldn’t agree more, noting most female physicians in her survey of dual-physician couples noted that they try to limit talk about work, then turn to other subjects.—GH
How to Get Ahead in Community-Based Hospital Medicine
What does it take to advance your career in the community hospital setting? Good communication and relationship skills top the list, according to Joe Metcalf, MD, director of the Hospital Medicine Service at Faith Regional Health Services in Norfolk, Neb. When Dr. Metcalf started the hospitalist service at the 227-bed regional referral center three and a half years ago, he was not looking for "brilliant" physicians. Instead, he says, "I was looking for excellent communicators."
"Patients are not interested in exceedingly smart clinicians," Dr. Metcalf says. "They are interested in clinicians who are willing to sit at the bedside, hold the elderly patient’s hand, listen to their concerns, and communicate the plans of care in ways they can understand."
Listening is a part of communication that is often neglected, he says.
Versatile and Teachable
Family-practice-trained, ED-hospitalist Joseph Babbitt, MD, works at 22-bed Blue Hill Memorial Hospital in Blue Hill, Maine. The key to success for hospitalists in the small-community-hospital setting is versatility, he says. It’s not unusual for hospitalists at Blue Hill to perform cardiac stress tests for a cardiology colleague or provide perioperative comanagement for surgical colleagues, he adds.
Dr. Babbitt underscores the willingness to acquire a broad range of skills. Dr. Metcalf agrees, and explains it’s one of the reasons he looks for "teachability" in hospitalist job candidates.
"It goes without saying that physicians must be proficient clinicians," he says, "but what I’m also listening for is whether they truly have a passion for patient-centered care."
Dr. Metcalf values honesty in his team members, and respects hospitalists who ask for help with their difficult cases.
Wired for Small
When it comes to community hospital settings, size matters. The hospital setting and job description should fit your preferences. Dr. Babbitt advises candidates to "listen to your gut" when interviewing for community hospital jobs. "If your reaction after checking out a job prospect is, ‘Well, I think I can make this work,’ then don’t try to make it work, because it probably won’t," he says. "You’re either ‘wired for small’ or you’re not."
Residents can prepare for a new job at a small community hospital. Dr. Babbitt recalls one young physician who, after a medical school rotation in a small hospital, realized that he was interested in becoming a "small-hospital hospitalist." He acquired additional training in emergency medicine because he identified it as a skill set that he needed to strengthen.
One thing is for sure: Variety is the order of the day in community settings. "You can bet," Dr. Babbitt says, "that the job you’re hired for is not going to be the job you’re doing in a year. Something about it will have changed."
Gretchen Henkel is a frequent contributor to The Hospitalist.
SOUND CAREER ADVICE
For more tips and strategies for advancing or establishing a career in hospital medicine, visit the SHM Career Center.
What does it take to advance your career in the community hospital setting? Good communication and relationship skills top the list, according to Joe Metcalf, MD, director of the Hospital Medicine Service at Faith Regional Health Services in Norfolk, Neb. When Dr. Metcalf started the hospitalist service at the 227-bed regional referral center three and a half years ago, he was not looking for "brilliant" physicians. Instead, he says, "I was looking for excellent communicators."
"Patients are not interested in exceedingly smart clinicians," Dr. Metcalf says. "They are interested in clinicians who are willing to sit at the bedside, hold the elderly patient’s hand, listen to their concerns, and communicate the plans of care in ways they can understand."
Listening is a part of communication that is often neglected, he says.
Versatile and Teachable
Family-practice-trained, ED-hospitalist Joseph Babbitt, MD, works at 22-bed Blue Hill Memorial Hospital in Blue Hill, Maine. The key to success for hospitalists in the small-community-hospital setting is versatility, he says. It’s not unusual for hospitalists at Blue Hill to perform cardiac stress tests for a cardiology colleague or provide perioperative comanagement for surgical colleagues, he adds.
Dr. Babbitt underscores the willingness to acquire a broad range of skills. Dr. Metcalf agrees, and explains it’s one of the reasons he looks for "teachability" in hospitalist job candidates.
"It goes without saying that physicians must be proficient clinicians," he says, "but what I’m also listening for is whether they truly have a passion for patient-centered care."
Dr. Metcalf values honesty in his team members, and respects hospitalists who ask for help with their difficult cases.
Wired for Small
When it comes to community hospital settings, size matters. The hospital setting and job description should fit your preferences. Dr. Babbitt advises candidates to "listen to your gut" when interviewing for community hospital jobs. "If your reaction after checking out a job prospect is, ‘Well, I think I can make this work,’ then don’t try to make it work, because it probably won’t," he says. "You’re either ‘wired for small’ or you’re not."
Residents can prepare for a new job at a small community hospital. Dr. Babbitt recalls one young physician who, after a medical school rotation in a small hospital, realized that he was interested in becoming a "small-hospital hospitalist." He acquired additional training in emergency medicine because he identified it as a skill set that he needed to strengthen.
One thing is for sure: Variety is the order of the day in community settings. "You can bet," Dr. Babbitt says, "that the job you’re hired for is not going to be the job you’re doing in a year. Something about it will have changed."
Gretchen Henkel is a frequent contributor to The Hospitalist.
SOUND CAREER ADVICE
For more tips and strategies for advancing or establishing a career in hospital medicine, visit the SHM Career Center.
What does it take to advance your career in the community hospital setting? Good communication and relationship skills top the list, according to Joe Metcalf, MD, director of the Hospital Medicine Service at Faith Regional Health Services in Norfolk, Neb. When Dr. Metcalf started the hospitalist service at the 227-bed regional referral center three and a half years ago, he was not looking for "brilliant" physicians. Instead, he says, "I was looking for excellent communicators."
"Patients are not interested in exceedingly smart clinicians," Dr. Metcalf says. "They are interested in clinicians who are willing to sit at the bedside, hold the elderly patient’s hand, listen to their concerns, and communicate the plans of care in ways they can understand."
Listening is a part of communication that is often neglected, he says.
Versatile and Teachable
Family-practice-trained, ED-hospitalist Joseph Babbitt, MD, works at 22-bed Blue Hill Memorial Hospital in Blue Hill, Maine. The key to success for hospitalists in the small-community-hospital setting is versatility, he says. It’s not unusual for hospitalists at Blue Hill to perform cardiac stress tests for a cardiology colleague or provide perioperative comanagement for surgical colleagues, he adds.
Dr. Babbitt underscores the willingness to acquire a broad range of skills. Dr. Metcalf agrees, and explains it’s one of the reasons he looks for "teachability" in hospitalist job candidates.
"It goes without saying that physicians must be proficient clinicians," he says, "but what I’m also listening for is whether they truly have a passion for patient-centered care."
Dr. Metcalf values honesty in his team members, and respects hospitalists who ask for help with their difficult cases.
Wired for Small
When it comes to community hospital settings, size matters. The hospital setting and job description should fit your preferences. Dr. Babbitt advises candidates to "listen to your gut" when interviewing for community hospital jobs. "If your reaction after checking out a job prospect is, ‘Well, I think I can make this work,’ then don’t try to make it work, because it probably won’t," he says. "You’re either ‘wired for small’ or you’re not."
Residents can prepare for a new job at a small community hospital. Dr. Babbitt recalls one young physician who, after a medical school rotation in a small hospital, realized that he was interested in becoming a "small-hospital hospitalist." He acquired additional training in emergency medicine because he identified it as a skill set that he needed to strengthen.
One thing is for sure: Variety is the order of the day in community settings. "You can bet," Dr. Babbitt says, "that the job you’re hired for is not going to be the job you’re doing in a year. Something about it will have changed."
Gretchen Henkel is a frequent contributor to The Hospitalist.
SOUND CAREER ADVICE
For more tips and strategies for advancing or establishing a career in hospital medicine, visit the SHM Career Center.
Generation Next
If imitation is the sincerest form of flattery, then hospitalists have a lot to crow about. For the same reasons that sparked the original hospital medicine movement, HM’s specialist colleagues are flocking to the HM model.
“I switched because your impact with consultation is limited,” says geriatrician-hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile Acute Care for the Elderly Service (MACE) at Mount Sinai Hospital in New York City. As the former director of the Department of Geriatrics’ consult service, Dr. Farber adds, “I like being able to call the shots and direct the care.”
He’s not the only one. Neurologists, surgeons, and even dermatologists and otolaryngologists have been establishing inpatient services based on the HM model. While many of these programs first begin in the academic setting, where resident work-hour limits necessitate faculty coverage, community hospitals increasingly are turning to specialist hospitalists to address patient-safety and treatment-innovation issues.
According to a leading surgical hospitalist, more than 250 such programs exist throughout the country.
Shaun Frost, MD, FACP, SFHM, chair of SHM’s Membership Committee and SHM’s Emergency Medicine Task Force, an SHM board member, and regional medical director for Brentwood, Tenn.-based Cogent Healthcare, views the growth of specialty hospitalist programs as a positive development. “In many ways, [this trend] is confirmatory regarding the key reasons for creation of the hospital movement,” he says.
For example, mirroring the performance of adult inpatient hospitalist programs, pediatric hospitalist programs have now documented improved throughput, increased efficiency, and increased patient satisfaction, especially when such programs combine pediatric emergency department and pediatric inpatient coverage.1
“We’ve all been inspired by the success of the medical hospitalist model, and we want to acknowledge and credit them for being the trailblazers and pioneers who are leading the way,” adds John Maa, MD, FACS, assistant professor in the Department of Surgery, assistant chair of the Surgery Quality Improvement Program, and director of the Surgical Hospitalist Program at the University of California at San Francisco (UCSF). Dr. Maa and colleagues introduced the surgical hospitalist program at UCSF in July 2005.

—David Likosky, MD, FHM, neurohospitalist, stroke program director, Evergreen Hospital Medical Center, Seattle
What’s Driving the Trend?
The impetus for adopting and adapting the HM model varies across medical specialties. For some, it was necessity; for others, it was a way to extend coverage or streamline the hospital stay; and for still others, it was a matter of personal choice.
“We couldn’t continue in the old paradigm and deliver safe care, because it was traditionally resident-dependent,” says Dr. Maa, explaining that the 80-hour resident workweek restriction mandated by the Accreditation Council for Graduate Medical Education (ACGME) “annihilated” the old-school model.
The goal in organizing the Society of Dermatology Hospitalists (SDH), according to SDH cofounder Lindy P. Fox, MD, assistant professor of clinical dermatology and director of the hospital consultation service at UCSF, was to ensure 24/7 coverage by a dedicated group of dermatologists whose skill set is focused on inpatient care, and who, because of their involvement with the university hospital, are probably more comfortable with the nuances of inpatient dermatologic care than their outpatient-based colleagues. The SDH currently has 20 members representing about 15 academic programs.
Innovations in stroke treatment caused a “sea change” for the field of neurology, says David Likosky, MD, SFHM, hospitalist and stroke program director at Evergreen Hospital Medical Center in Seattle. Dr. Likosky, who is board-certified in neurology and internal medicine, says the HM model allows neurohospitalists to enjoy a work-life balance.
“It used to be that neurologists didn’t have to get out of bed at night for most strokes. But with innovations in stroke treatments, that’s all changed,” Dr. Likosky says. “It really helped to give birth to the neurohospitalist movement.”
A recent survey on the current scope of neurohospitalists’ practice presented by Dr. Likosky and colleagues at the American Academy of Neurology found that 8% of those surveyed were full-time neurohospitalists. The number might seem small, but it might be a matter of perception. The same study showed 73% of neurologists surveyed listed inpatient neurology care as their primary practice focus.2
Another driver for the neurohospitalist movement was that it became unfeasible to staff inpatient neurology services with physicians who maintained offices “across town,” observes S. Andrew Josephson, MD, director of the neurohospitalist program and inpatient neurology at UCSF. “Stroke is just one example of a disease that has so many emergent therapies that hospitals decided they needed a neurologist on site to make those types of treatment decisions.”
At a quaternary-care center such as UCSF, the requirements for otolaryngology expertise have increased exponentially, says Andrew H. Murr, MD, FACS, vice-chair of the Department of Otolaryngology/Head and Neck Surgery at UCSF. “For instance, our hospital has a huge transplant volume. Often, patients are on immuno-compromising medications that create the specter of fungal sinusitis,” he says. “We also get called to the operating room or ICU when patients have breathing problems and require surgical airways or other complicated intubation schemes. All of these problems require a lot of time, effort, and special expertise.”
Since September of last year, Dr. Murr’s department has been using office space adjacent to the hospital as headquarters for a full-time otolaryngologist whose sole responsibility is to cover inpatient work. Increased complexity of otolaryngologic-related problems, increased ED commitment, and a simple matter of logistics prompted the move. The Department of Otolaryngology moved 10 minutes away from the hospital, so literally running across the street for an otolaryngology consult was no longer an option.
Today, the hospital duty is linked to the department’s call schedule. Dr. Murr anticipates the department soon will establish a full-time faculty position to create a hospitalist niche within the department.
Usefulness Affirmed
Good results already have been demonstrated for the hospitalist model in other specialties. In the first two years of the surgical hospitalist program at UCSF, response times for surgical consultations averaged less than 20 minutes; the average wait for patients with acute appendicitis to undergo surgery was cut in half; and the number of billable consults rose by almost 200%.3
Heidi Wald, MD, MSPH, FHM, a 2009 Health and Aging Policy Fellow, and two hospitalist colleagues studied the impact of hospitalist programs on acute-care geriatrics and found a paucity of geriatric-care approaches.4 “The employment of geriatrics-trained clinicians by hospitalist programs is one approach to supporting generalist-hospitalists and inclining group culture toward clinical geriatric concerns,” the authors wrote. “Programs that purposefully hired geriatricians and gerontology nurse-practitioners used them to staff geriatrics services.”
Dr. Wald, assistant professor of medicine in the division of Health Care Policy Research and a hospitalist at the University of Colorado Denver, says trends in patient demographics and patient-safety initiatives will drive the proliferation of more geriatrician-hospitalists and geriatrics-focused services in the future. “The median age of the hospital population is increasing,” she notes, “and there are not enough geriatricians to deal with every elderly patient.”
Mount Sinai’s Dr. Farber is in the process of submitting for publication two years’ worth of data about the MACE service at Mount Sinai, which will evaluate the effect of MACE on costs, length of stay, and rehospitalization rates.
Variations on a Theme
The dermatology HM model at UCSF more closely resembles a consultative practice model. UCSF’s dermatology hospitalists do not admit patients. Still, says SDH’s Dr. Fox, because of their conversance with inpatient care and round-the-clock availability, dermatology hospitalists are invaluable. They help colleagues “puzzle out” the causes of cutaneous manifestations of system disease, quickly initiate state of the art treatment for hospital-acquired skin conditions, and improve outcomes for hospitalized patients with skin diseases.
“We see our charge as being multifold,” Dr. Fox explains. “We provide continuity of care for patients who are frequently hospitalized; we keep up with the medical literature; we are comfortable with and know the nuances of hospital operations; and we provide education to residents, house staff, and colleagues.”
In Denver, the Acute Care for the Elderly (ACE) service operated by the internal-medicine hospitalist group has only informal ties to the Department of Medicine’s Geriatrics Division, Dr. Wald says. Although not a closed geriatric-care unit, the service concentrates elderly patients on one inpatient service and introduces the tenets of geriatric care—multidisciplinary approach, functional assessment, early discharge planning, mitigating the hazards of hospitalization, and patient and family-centered care—into a hospitalist milieu.
Surgical hospitalist models also vary by setting, and continue to evolve as surgeons examine processes to determine what works and what doesn’t. At UCSF, the original model relied on surgeons taking call for seven days running. “You probably couldn’t do that continuously for your career,” says Dr. Maa, who worked the seven-day call schedule for 3 1/2 years.
The program has been modified so that the surgical hospitalists now work three- or four-day stretches.
Another successful variation involves one surgeon taking all the daytime shifts, while others rotate in for the PM shifts and weekends.
A Win-Win for Hospitalists?
Does the proliferation of specialty hospitalists create competition for patients? That could be a possibility, says Dr. Frost, should other specialty hospitalists become interested in providing care for the “bread and butter” pathologies.
“For instance, if neurohospitalists were interested in evaluating and managing patients with TIAs (transient ischemic attacks), or cardiohospitalists were interested in managing patients with low-risk chest pain, then there could be some competition,” Dr. Frost says. Although possible, he senses it isn’t a likely scenario.
What’s more likely, according to neurohospitalist Dr. Likosky, is cross-fertilization between specialties, where hospitalists who interface with their specialty colleagues gain the benefit of on-site, in-service education. “Many hospitalists feel that they were not adequately trained in neurologic illnesses, and yet, by default, they have become the first-line providers of inpatient neurologic care nationally,” Dr. Likosky says. “The neurohospitalist model is a way of getting at that issue. I don’t think that we are in competition. I think we are welcome partners.”
Dr. Likosky and fellow neurohospitalists Dr. Josephson and W. David Freeman, MD, assistant professor in the department of neurology and critical care at the Mayo Clinic College of Medicine in Jacksonville, Fla., offered the first neurology precourse in April at HM10 in Washington, D.C., and more and more hospitalist meetings are including neurohospitalist courses on their schedules.
Increased education also is a benefit of Mount Sinai’s adaptation of the MACE concept, Dr. Farber says. Because the hospitalist-run MACE patients are located throughout the hospital, the team conducts nursing grand rounds to educate other hospital staff about geriatrics-centered HM principles.

—John Maa, MD, FACS, assistant professor, Department of Surgery; assistant chair, Surgery Quality Improvement Program; director, Surgical Hospitalist Program, University of California at San Francisco
Economies of Scale
Dr. Fox, the dermatology hospitalist, is the first to admit that UCSF’s practice model probably works best in a large, tertiary-care, academic medical center. However, the potential exists for extension into rural settings with telemedicine models and trained physician assistants or nurse practitioners, she notes.
Dr. Farber agrees the HM model is adaptable to a variety of medical specialties; he foresees geriatric hospitalists working in community settings. “Even in smaller hospitals with fewer discharges, there will be a sizable subset of admissions of patients at risk for high utilization of resources,” he says. “Many of Medicare’s hospital-acquired conditions are geriatrics-related, such as catheter-associated urinary tract infections, central-line infections, and falls. The investment [in geriatrician-hospitalist teams] could be justified if you track the outcomes of these high-risk patients over time and see whether you’re reducing length of stay, direct costs, and readmissions.”
Dr. Likosky says the benefits of the neurohospitalist model closely mirror those of the HM model, and although volumes are lower, the benefits “remain significant even in relatively small hospitals.” His American Academy of Neurology (AAN) survey backs up this observation: Neurohospitalists were about evenly split between academic and private settings (49% and 51%, respectively). “Unlike dermatology, neurologic diagnoses are very common as either a primary or secondary reason for admission to the hospital,” Dr. Likosky says.
In the community setting, surgical hospitalist programs provide a new answer for ED call coverage, Dr. Maa says. Surgical practices often approach the medical center leadership to negotiate a stipend, then contribute salary support so that a new surgeon can be recruited to join the practice. This physician—usually a younger surgeon—then is hired in the role of a surgicalist so that timely patient care and surgeon availability can be ensured.
In rural settings, however, even this model might not be feasible, Dr. Maa says, because surgical practices could be comprised of only one or two surgeons. “We will have to think differently about telemedicine, telesurgery, and having ERs equipped with video monitors so that the ED physician can examine the patient while a surgeon, at a remote centralized area, can provide input,” he says.
Adoption of the hospitalist model by other specialties shows no sign of slowing down. That’s good news for HM and patient care, Dr. Maa says.
“This represents a transformation of the way an academic medical center is structured,” he adds. “We’ve traditionally prioritized research ahead of patient care, but this model is inverting that. It is patient-centered, making them the priority, and answers the question, ‘How can we reconfigure what we have to take better care of patients?’ And that’s why I think we’ll succeed.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Krugman SD, Suggs A, Photowala HY, et al. Redefining the community pediatric hospitalist: the combined pediatric ED/inpatient unit. Ped Emerg Car. 2007;23(1):33-37.
- Likosky D. Is it time for neurohospitalists? Neurology. 2009;72(9):859-860.
- Maa J, Carter JT, Gosnell JE, et al. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1(1):29-35.
If imitation is the sincerest form of flattery, then hospitalists have a lot to crow about. For the same reasons that sparked the original hospital medicine movement, HM’s specialist colleagues are flocking to the HM model.
“I switched because your impact with consultation is limited,” says geriatrician-hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile Acute Care for the Elderly Service (MACE) at Mount Sinai Hospital in New York City. As the former director of the Department of Geriatrics’ consult service, Dr. Farber adds, “I like being able to call the shots and direct the care.”
He’s not the only one. Neurologists, surgeons, and even dermatologists and otolaryngologists have been establishing inpatient services based on the HM model. While many of these programs first begin in the academic setting, where resident work-hour limits necessitate faculty coverage, community hospitals increasingly are turning to specialist hospitalists to address patient-safety and treatment-innovation issues.
According to a leading surgical hospitalist, more than 250 such programs exist throughout the country.
Shaun Frost, MD, FACP, SFHM, chair of SHM’s Membership Committee and SHM’s Emergency Medicine Task Force, an SHM board member, and regional medical director for Brentwood, Tenn.-based Cogent Healthcare, views the growth of specialty hospitalist programs as a positive development. “In many ways, [this trend] is confirmatory regarding the key reasons for creation of the hospital movement,” he says.
For example, mirroring the performance of adult inpatient hospitalist programs, pediatric hospitalist programs have now documented improved throughput, increased efficiency, and increased patient satisfaction, especially when such programs combine pediatric emergency department and pediatric inpatient coverage.1
“We’ve all been inspired by the success of the medical hospitalist model, and we want to acknowledge and credit them for being the trailblazers and pioneers who are leading the way,” adds John Maa, MD, FACS, assistant professor in the Department of Surgery, assistant chair of the Surgery Quality Improvement Program, and director of the Surgical Hospitalist Program at the University of California at San Francisco (UCSF). Dr. Maa and colleagues introduced the surgical hospitalist program at UCSF in July 2005.

—David Likosky, MD, FHM, neurohospitalist, stroke program director, Evergreen Hospital Medical Center, Seattle
What’s Driving the Trend?
The impetus for adopting and adapting the HM model varies across medical specialties. For some, it was necessity; for others, it was a way to extend coverage or streamline the hospital stay; and for still others, it was a matter of personal choice.
“We couldn’t continue in the old paradigm and deliver safe care, because it was traditionally resident-dependent,” says Dr. Maa, explaining that the 80-hour resident workweek restriction mandated by the Accreditation Council for Graduate Medical Education (ACGME) “annihilated” the old-school model.
The goal in organizing the Society of Dermatology Hospitalists (SDH), according to SDH cofounder Lindy P. Fox, MD, assistant professor of clinical dermatology and director of the hospital consultation service at UCSF, was to ensure 24/7 coverage by a dedicated group of dermatologists whose skill set is focused on inpatient care, and who, because of their involvement with the university hospital, are probably more comfortable with the nuances of inpatient dermatologic care than their outpatient-based colleagues. The SDH currently has 20 members representing about 15 academic programs.
Innovations in stroke treatment caused a “sea change” for the field of neurology, says David Likosky, MD, SFHM, hospitalist and stroke program director at Evergreen Hospital Medical Center in Seattle. Dr. Likosky, who is board-certified in neurology and internal medicine, says the HM model allows neurohospitalists to enjoy a work-life balance.
“It used to be that neurologists didn’t have to get out of bed at night for most strokes. But with innovations in stroke treatments, that’s all changed,” Dr. Likosky says. “It really helped to give birth to the neurohospitalist movement.”
A recent survey on the current scope of neurohospitalists’ practice presented by Dr. Likosky and colleagues at the American Academy of Neurology found that 8% of those surveyed were full-time neurohospitalists. The number might seem small, but it might be a matter of perception. The same study showed 73% of neurologists surveyed listed inpatient neurology care as their primary practice focus.2
Another driver for the neurohospitalist movement was that it became unfeasible to staff inpatient neurology services with physicians who maintained offices “across town,” observes S. Andrew Josephson, MD, director of the neurohospitalist program and inpatient neurology at UCSF. “Stroke is just one example of a disease that has so many emergent therapies that hospitals decided they needed a neurologist on site to make those types of treatment decisions.”
At a quaternary-care center such as UCSF, the requirements for otolaryngology expertise have increased exponentially, says Andrew H. Murr, MD, FACS, vice-chair of the Department of Otolaryngology/Head and Neck Surgery at UCSF. “For instance, our hospital has a huge transplant volume. Often, patients are on immuno-compromising medications that create the specter of fungal sinusitis,” he says. “We also get called to the operating room or ICU when patients have breathing problems and require surgical airways or other complicated intubation schemes. All of these problems require a lot of time, effort, and special expertise.”
Since September of last year, Dr. Murr’s department has been using office space adjacent to the hospital as headquarters for a full-time otolaryngologist whose sole responsibility is to cover inpatient work. Increased complexity of otolaryngologic-related problems, increased ED commitment, and a simple matter of logistics prompted the move. The Department of Otolaryngology moved 10 minutes away from the hospital, so literally running across the street for an otolaryngology consult was no longer an option.
Today, the hospital duty is linked to the department’s call schedule. Dr. Murr anticipates the department soon will establish a full-time faculty position to create a hospitalist niche within the department.
Usefulness Affirmed
Good results already have been demonstrated for the hospitalist model in other specialties. In the first two years of the surgical hospitalist program at UCSF, response times for surgical consultations averaged less than 20 minutes; the average wait for patients with acute appendicitis to undergo surgery was cut in half; and the number of billable consults rose by almost 200%.3
Heidi Wald, MD, MSPH, FHM, a 2009 Health and Aging Policy Fellow, and two hospitalist colleagues studied the impact of hospitalist programs on acute-care geriatrics and found a paucity of geriatric-care approaches.4 “The employment of geriatrics-trained clinicians by hospitalist programs is one approach to supporting generalist-hospitalists and inclining group culture toward clinical geriatric concerns,” the authors wrote. “Programs that purposefully hired geriatricians and gerontology nurse-practitioners used them to staff geriatrics services.”
Dr. Wald, assistant professor of medicine in the division of Health Care Policy Research and a hospitalist at the University of Colorado Denver, says trends in patient demographics and patient-safety initiatives will drive the proliferation of more geriatrician-hospitalists and geriatrics-focused services in the future. “The median age of the hospital population is increasing,” she notes, “and there are not enough geriatricians to deal with every elderly patient.”
Mount Sinai’s Dr. Farber is in the process of submitting for publication two years’ worth of data about the MACE service at Mount Sinai, which will evaluate the effect of MACE on costs, length of stay, and rehospitalization rates.
Variations on a Theme
The dermatology HM model at UCSF more closely resembles a consultative practice model. UCSF’s dermatology hospitalists do not admit patients. Still, says SDH’s Dr. Fox, because of their conversance with inpatient care and round-the-clock availability, dermatology hospitalists are invaluable. They help colleagues “puzzle out” the causes of cutaneous manifestations of system disease, quickly initiate state of the art treatment for hospital-acquired skin conditions, and improve outcomes for hospitalized patients with skin diseases.
“We see our charge as being multifold,” Dr. Fox explains. “We provide continuity of care for patients who are frequently hospitalized; we keep up with the medical literature; we are comfortable with and know the nuances of hospital operations; and we provide education to residents, house staff, and colleagues.”
In Denver, the Acute Care for the Elderly (ACE) service operated by the internal-medicine hospitalist group has only informal ties to the Department of Medicine’s Geriatrics Division, Dr. Wald says. Although not a closed geriatric-care unit, the service concentrates elderly patients on one inpatient service and introduces the tenets of geriatric care—multidisciplinary approach, functional assessment, early discharge planning, mitigating the hazards of hospitalization, and patient and family-centered care—into a hospitalist milieu.
Surgical hospitalist models also vary by setting, and continue to evolve as surgeons examine processes to determine what works and what doesn’t. At UCSF, the original model relied on surgeons taking call for seven days running. “You probably couldn’t do that continuously for your career,” says Dr. Maa, who worked the seven-day call schedule for 3 1/2 years.
The program has been modified so that the surgical hospitalists now work three- or four-day stretches.
Another successful variation involves one surgeon taking all the daytime shifts, while others rotate in for the PM shifts and weekends.
A Win-Win for Hospitalists?
Does the proliferation of specialty hospitalists create competition for patients? That could be a possibility, says Dr. Frost, should other specialty hospitalists become interested in providing care for the “bread and butter” pathologies.
“For instance, if neurohospitalists were interested in evaluating and managing patients with TIAs (transient ischemic attacks), or cardiohospitalists were interested in managing patients with low-risk chest pain, then there could be some competition,” Dr. Frost says. Although possible, he senses it isn’t a likely scenario.
What’s more likely, according to neurohospitalist Dr. Likosky, is cross-fertilization between specialties, where hospitalists who interface with their specialty colleagues gain the benefit of on-site, in-service education. “Many hospitalists feel that they were not adequately trained in neurologic illnesses, and yet, by default, they have become the first-line providers of inpatient neurologic care nationally,” Dr. Likosky says. “The neurohospitalist model is a way of getting at that issue. I don’t think that we are in competition. I think we are welcome partners.”
Dr. Likosky and fellow neurohospitalists Dr. Josephson and W. David Freeman, MD, assistant professor in the department of neurology and critical care at the Mayo Clinic College of Medicine in Jacksonville, Fla., offered the first neurology precourse in April at HM10 in Washington, D.C., and more and more hospitalist meetings are including neurohospitalist courses on their schedules.
Increased education also is a benefit of Mount Sinai’s adaptation of the MACE concept, Dr. Farber says. Because the hospitalist-run MACE patients are located throughout the hospital, the team conducts nursing grand rounds to educate other hospital staff about geriatrics-centered HM principles.

—John Maa, MD, FACS, assistant professor, Department of Surgery; assistant chair, Surgery Quality Improvement Program; director, Surgical Hospitalist Program, University of California at San Francisco
Economies of Scale
Dr. Fox, the dermatology hospitalist, is the first to admit that UCSF’s practice model probably works best in a large, tertiary-care, academic medical center. However, the potential exists for extension into rural settings with telemedicine models and trained physician assistants or nurse practitioners, she notes.
Dr. Farber agrees the HM model is adaptable to a variety of medical specialties; he foresees geriatric hospitalists working in community settings. “Even in smaller hospitals with fewer discharges, there will be a sizable subset of admissions of patients at risk for high utilization of resources,” he says. “Many of Medicare’s hospital-acquired conditions are geriatrics-related, such as catheter-associated urinary tract infections, central-line infections, and falls. The investment [in geriatrician-hospitalist teams] could be justified if you track the outcomes of these high-risk patients over time and see whether you’re reducing length of stay, direct costs, and readmissions.”
Dr. Likosky says the benefits of the neurohospitalist model closely mirror those of the HM model, and although volumes are lower, the benefits “remain significant even in relatively small hospitals.” His American Academy of Neurology (AAN) survey backs up this observation: Neurohospitalists were about evenly split between academic and private settings (49% and 51%, respectively). “Unlike dermatology, neurologic diagnoses are very common as either a primary or secondary reason for admission to the hospital,” Dr. Likosky says.
In the community setting, surgical hospitalist programs provide a new answer for ED call coverage, Dr. Maa says. Surgical practices often approach the medical center leadership to negotiate a stipend, then contribute salary support so that a new surgeon can be recruited to join the practice. This physician—usually a younger surgeon—then is hired in the role of a surgicalist so that timely patient care and surgeon availability can be ensured.
In rural settings, however, even this model might not be feasible, Dr. Maa says, because surgical practices could be comprised of only one or two surgeons. “We will have to think differently about telemedicine, telesurgery, and having ERs equipped with video monitors so that the ED physician can examine the patient while a surgeon, at a remote centralized area, can provide input,” he says.
Adoption of the hospitalist model by other specialties shows no sign of slowing down. That’s good news for HM and patient care, Dr. Maa says.
“This represents a transformation of the way an academic medical center is structured,” he adds. “We’ve traditionally prioritized research ahead of patient care, but this model is inverting that. It is patient-centered, making them the priority, and answers the question, ‘How can we reconfigure what we have to take better care of patients?’ And that’s why I think we’ll succeed.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Krugman SD, Suggs A, Photowala HY, et al. Redefining the community pediatric hospitalist: the combined pediatric ED/inpatient unit. Ped Emerg Car. 2007;23(1):33-37.
- Likosky D. Is it time for neurohospitalists? Neurology. 2009;72(9):859-860.
- Maa J, Carter JT, Gosnell JE, et al. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1(1):29-35.
If imitation is the sincerest form of flattery, then hospitalists have a lot to crow about. For the same reasons that sparked the original hospital medicine movement, HM’s specialist colleagues are flocking to the HM model.
“I switched because your impact with consultation is limited,” says geriatrician-hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile Acute Care for the Elderly Service (MACE) at Mount Sinai Hospital in New York City. As the former director of the Department of Geriatrics’ consult service, Dr. Farber adds, “I like being able to call the shots and direct the care.”
He’s not the only one. Neurologists, surgeons, and even dermatologists and otolaryngologists have been establishing inpatient services based on the HM model. While many of these programs first begin in the academic setting, where resident work-hour limits necessitate faculty coverage, community hospitals increasingly are turning to specialist hospitalists to address patient-safety and treatment-innovation issues.
According to a leading surgical hospitalist, more than 250 such programs exist throughout the country.
Shaun Frost, MD, FACP, SFHM, chair of SHM’s Membership Committee and SHM’s Emergency Medicine Task Force, an SHM board member, and regional medical director for Brentwood, Tenn.-based Cogent Healthcare, views the growth of specialty hospitalist programs as a positive development. “In many ways, [this trend] is confirmatory regarding the key reasons for creation of the hospital movement,” he says.
For example, mirroring the performance of adult inpatient hospitalist programs, pediatric hospitalist programs have now documented improved throughput, increased efficiency, and increased patient satisfaction, especially when such programs combine pediatric emergency department and pediatric inpatient coverage.1
“We’ve all been inspired by the success of the medical hospitalist model, and we want to acknowledge and credit them for being the trailblazers and pioneers who are leading the way,” adds John Maa, MD, FACS, assistant professor in the Department of Surgery, assistant chair of the Surgery Quality Improvement Program, and director of the Surgical Hospitalist Program at the University of California at San Francisco (UCSF). Dr. Maa and colleagues introduced the surgical hospitalist program at UCSF in July 2005.

—David Likosky, MD, FHM, neurohospitalist, stroke program director, Evergreen Hospital Medical Center, Seattle
What’s Driving the Trend?
The impetus for adopting and adapting the HM model varies across medical specialties. For some, it was necessity; for others, it was a way to extend coverage or streamline the hospital stay; and for still others, it was a matter of personal choice.
“We couldn’t continue in the old paradigm and deliver safe care, because it was traditionally resident-dependent,” says Dr. Maa, explaining that the 80-hour resident workweek restriction mandated by the Accreditation Council for Graduate Medical Education (ACGME) “annihilated” the old-school model.
The goal in organizing the Society of Dermatology Hospitalists (SDH), according to SDH cofounder Lindy P. Fox, MD, assistant professor of clinical dermatology and director of the hospital consultation service at UCSF, was to ensure 24/7 coverage by a dedicated group of dermatologists whose skill set is focused on inpatient care, and who, because of their involvement with the university hospital, are probably more comfortable with the nuances of inpatient dermatologic care than their outpatient-based colleagues. The SDH currently has 20 members representing about 15 academic programs.
Innovations in stroke treatment caused a “sea change” for the field of neurology, says David Likosky, MD, SFHM, hospitalist and stroke program director at Evergreen Hospital Medical Center in Seattle. Dr. Likosky, who is board-certified in neurology and internal medicine, says the HM model allows neurohospitalists to enjoy a work-life balance.
“It used to be that neurologists didn’t have to get out of bed at night for most strokes. But with innovations in stroke treatments, that’s all changed,” Dr. Likosky says. “It really helped to give birth to the neurohospitalist movement.”
A recent survey on the current scope of neurohospitalists’ practice presented by Dr. Likosky and colleagues at the American Academy of Neurology found that 8% of those surveyed were full-time neurohospitalists. The number might seem small, but it might be a matter of perception. The same study showed 73% of neurologists surveyed listed inpatient neurology care as their primary practice focus.2
Another driver for the neurohospitalist movement was that it became unfeasible to staff inpatient neurology services with physicians who maintained offices “across town,” observes S. Andrew Josephson, MD, director of the neurohospitalist program and inpatient neurology at UCSF. “Stroke is just one example of a disease that has so many emergent therapies that hospitals decided they needed a neurologist on site to make those types of treatment decisions.”
At a quaternary-care center such as UCSF, the requirements for otolaryngology expertise have increased exponentially, says Andrew H. Murr, MD, FACS, vice-chair of the Department of Otolaryngology/Head and Neck Surgery at UCSF. “For instance, our hospital has a huge transplant volume. Often, patients are on immuno-compromising medications that create the specter of fungal sinusitis,” he says. “We also get called to the operating room or ICU when patients have breathing problems and require surgical airways or other complicated intubation schemes. All of these problems require a lot of time, effort, and special expertise.”
Since September of last year, Dr. Murr’s department has been using office space adjacent to the hospital as headquarters for a full-time otolaryngologist whose sole responsibility is to cover inpatient work. Increased complexity of otolaryngologic-related problems, increased ED commitment, and a simple matter of logistics prompted the move. The Department of Otolaryngology moved 10 minutes away from the hospital, so literally running across the street for an otolaryngology consult was no longer an option.
Today, the hospital duty is linked to the department’s call schedule. Dr. Murr anticipates the department soon will establish a full-time faculty position to create a hospitalist niche within the department.
Usefulness Affirmed
Good results already have been demonstrated for the hospitalist model in other specialties. In the first two years of the surgical hospitalist program at UCSF, response times for surgical consultations averaged less than 20 minutes; the average wait for patients with acute appendicitis to undergo surgery was cut in half; and the number of billable consults rose by almost 200%.3
Heidi Wald, MD, MSPH, FHM, a 2009 Health and Aging Policy Fellow, and two hospitalist colleagues studied the impact of hospitalist programs on acute-care geriatrics and found a paucity of geriatric-care approaches.4 “The employment of geriatrics-trained clinicians by hospitalist programs is one approach to supporting generalist-hospitalists and inclining group culture toward clinical geriatric concerns,” the authors wrote. “Programs that purposefully hired geriatricians and gerontology nurse-practitioners used them to staff geriatrics services.”
Dr. Wald, assistant professor of medicine in the division of Health Care Policy Research and a hospitalist at the University of Colorado Denver, says trends in patient demographics and patient-safety initiatives will drive the proliferation of more geriatrician-hospitalists and geriatrics-focused services in the future. “The median age of the hospital population is increasing,” she notes, “and there are not enough geriatricians to deal with every elderly patient.”
Mount Sinai’s Dr. Farber is in the process of submitting for publication two years’ worth of data about the MACE service at Mount Sinai, which will evaluate the effect of MACE on costs, length of stay, and rehospitalization rates.
Variations on a Theme
The dermatology HM model at UCSF more closely resembles a consultative practice model. UCSF’s dermatology hospitalists do not admit patients. Still, says SDH’s Dr. Fox, because of their conversance with inpatient care and round-the-clock availability, dermatology hospitalists are invaluable. They help colleagues “puzzle out” the causes of cutaneous manifestations of system disease, quickly initiate state of the art treatment for hospital-acquired skin conditions, and improve outcomes for hospitalized patients with skin diseases.
“We see our charge as being multifold,” Dr. Fox explains. “We provide continuity of care for patients who are frequently hospitalized; we keep up with the medical literature; we are comfortable with and know the nuances of hospital operations; and we provide education to residents, house staff, and colleagues.”
In Denver, the Acute Care for the Elderly (ACE) service operated by the internal-medicine hospitalist group has only informal ties to the Department of Medicine’s Geriatrics Division, Dr. Wald says. Although not a closed geriatric-care unit, the service concentrates elderly patients on one inpatient service and introduces the tenets of geriatric care—multidisciplinary approach, functional assessment, early discharge planning, mitigating the hazards of hospitalization, and patient and family-centered care—into a hospitalist milieu.
Surgical hospitalist models also vary by setting, and continue to evolve as surgeons examine processes to determine what works and what doesn’t. At UCSF, the original model relied on surgeons taking call for seven days running. “You probably couldn’t do that continuously for your career,” says Dr. Maa, who worked the seven-day call schedule for 3 1/2 years.
The program has been modified so that the surgical hospitalists now work three- or four-day stretches.
Another successful variation involves one surgeon taking all the daytime shifts, while others rotate in for the PM shifts and weekends.
A Win-Win for Hospitalists?
Does the proliferation of specialty hospitalists create competition for patients? That could be a possibility, says Dr. Frost, should other specialty hospitalists become interested in providing care for the “bread and butter” pathologies.
“For instance, if neurohospitalists were interested in evaluating and managing patients with TIAs (transient ischemic attacks), or cardiohospitalists were interested in managing patients with low-risk chest pain, then there could be some competition,” Dr. Frost says. Although possible, he senses it isn’t a likely scenario.
What’s more likely, according to neurohospitalist Dr. Likosky, is cross-fertilization between specialties, where hospitalists who interface with their specialty colleagues gain the benefit of on-site, in-service education. “Many hospitalists feel that they were not adequately trained in neurologic illnesses, and yet, by default, they have become the first-line providers of inpatient neurologic care nationally,” Dr. Likosky says. “The neurohospitalist model is a way of getting at that issue. I don’t think that we are in competition. I think we are welcome partners.”
Dr. Likosky and fellow neurohospitalists Dr. Josephson and W. David Freeman, MD, assistant professor in the department of neurology and critical care at the Mayo Clinic College of Medicine in Jacksonville, Fla., offered the first neurology precourse in April at HM10 in Washington, D.C., and more and more hospitalist meetings are including neurohospitalist courses on their schedules.
Increased education also is a benefit of Mount Sinai’s adaptation of the MACE concept, Dr. Farber says. Because the hospitalist-run MACE patients are located throughout the hospital, the team conducts nursing grand rounds to educate other hospital staff about geriatrics-centered HM principles.

—John Maa, MD, FACS, assistant professor, Department of Surgery; assistant chair, Surgery Quality Improvement Program; director, Surgical Hospitalist Program, University of California at San Francisco
Economies of Scale
Dr. Fox, the dermatology hospitalist, is the first to admit that UCSF’s practice model probably works best in a large, tertiary-care, academic medical center. However, the potential exists for extension into rural settings with telemedicine models and trained physician assistants or nurse practitioners, she notes.
Dr. Farber agrees the HM model is adaptable to a variety of medical specialties; he foresees geriatric hospitalists working in community settings. “Even in smaller hospitals with fewer discharges, there will be a sizable subset of admissions of patients at risk for high utilization of resources,” he says. “Many of Medicare’s hospital-acquired conditions are geriatrics-related, such as catheter-associated urinary tract infections, central-line infections, and falls. The investment [in geriatrician-hospitalist teams] could be justified if you track the outcomes of these high-risk patients over time and see whether you’re reducing length of stay, direct costs, and readmissions.”
Dr. Likosky says the benefits of the neurohospitalist model closely mirror those of the HM model, and although volumes are lower, the benefits “remain significant even in relatively small hospitals.” His American Academy of Neurology (AAN) survey backs up this observation: Neurohospitalists were about evenly split between academic and private settings (49% and 51%, respectively). “Unlike dermatology, neurologic diagnoses are very common as either a primary or secondary reason for admission to the hospital,” Dr. Likosky says.
In the community setting, surgical hospitalist programs provide a new answer for ED call coverage, Dr. Maa says. Surgical practices often approach the medical center leadership to negotiate a stipend, then contribute salary support so that a new surgeon can be recruited to join the practice. This physician—usually a younger surgeon—then is hired in the role of a surgicalist so that timely patient care and surgeon availability can be ensured.
In rural settings, however, even this model might not be feasible, Dr. Maa says, because surgical practices could be comprised of only one or two surgeons. “We will have to think differently about telemedicine, telesurgery, and having ERs equipped with video monitors so that the ED physician can examine the patient while a surgeon, at a remote centralized area, can provide input,” he says.
Adoption of the hospitalist model by other specialties shows no sign of slowing down. That’s good news for HM and patient care, Dr. Maa says.
“This represents a transformation of the way an academic medical center is structured,” he adds. “We’ve traditionally prioritized research ahead of patient care, but this model is inverting that. It is patient-centered, making them the priority, and answers the question, ‘How can we reconfigure what we have to take better care of patients?’ And that’s why I think we’ll succeed.” TH
Gretchen Henkel is a freelance writer based in California.
References
- Krugman SD, Suggs A, Photowala HY, et al. Redefining the community pediatric hospitalist: the combined pediatric ED/inpatient unit. Ped Emerg Car. 2007;23(1):33-37.
- Likosky D. Is it time for neurohospitalists? Neurology. 2009;72(9):859-860.
- Maa J, Carter JT, Gosnell JE, et al. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1(1):29-35.
ONLINE EXCLUSIVE: HM pioneer Bob Wachter, MD, MHM, discusses the growing trend of specialist-hospitalists
Bob Wachter, MD, MHM, has watched the hospitalist movement grow from its infancy in the mid-1990s to more than 30,000 hospitalists practicing nationwide today. As professor and chief of the Division of Hospital Medicine and associate chairman of the Department of Medicine at the University of California at San Francisco, and chief of the medical service at UCSF Medical Center, Dr. Wachter also has watched the HM model spread to other medical specialties, including a handful of departments in his own hospital. The Hospitalist caught up with Dr. Wachter and found out what he thinks about the spread of the HM model.
Question: Do specialist-hospitalist programs threaten to siphon off your medical hospitalist workforce, or are they a boon?
Answer: Having specialized physicians focus on hospital care is a powerful model. Not only are they available all the time, but they are keeping up with innovations in their field. More importantly, they get involved in system improvement in a way that the part-time hospital person will not.

—Bob Wachter, MD, MHM
Q: Are there direct benefits to the hospitalist on the floor?
A: I think it creates a vehicle for collegiality, interchange, and learning across the specialties, which is harder to come by when we’re in the hospital all the time, but the consults we’re interacting with may not be.
Q: Aren’t hospitalists already comanaging patients with neurosurgery, hematology/oncology, and orthopedics at your institution? How are specialist hospitalists different?
A: Neurohospitalists focus their professional practice on the hospitalized care of patients with neurological diseases—they perform the same function for those patients as we do for medical patients. That is, they admit patients, supervise their overall care, and discharge them. On our neurosurgery service, which has a census of 50 patients, the surgeons are in the operating room much of the day. Their post-surgical patients often have multiple medical comorbidities (heart failure, high blood pressures, diabetes, etc.), which is where the medical hospitalist comes in to comanage and coordinate their medical care.
We probably need new lingo to distinguish between medical hospitalists comanaging specialty patients and specialty hospitalists, because it can be confusing to people.
Q: Is this model sustainable in the community and rural settings, where specialists are in short supply?
A: There is a size below which you probably cannot support a specialty hospitalist. But larger places can, and their value is not only what they do at that individual hospital, but the fact that they can teach and do research and (quality improvement) that may help influence care beyond their organization’s walls.
—GH
Bob Wachter, MD, MHM, has watched the hospitalist movement grow from its infancy in the mid-1990s to more than 30,000 hospitalists practicing nationwide today. As professor and chief of the Division of Hospital Medicine and associate chairman of the Department of Medicine at the University of California at San Francisco, and chief of the medical service at UCSF Medical Center, Dr. Wachter also has watched the HM model spread to other medical specialties, including a handful of departments in his own hospital. The Hospitalist caught up with Dr. Wachter and found out what he thinks about the spread of the HM model.
Question: Do specialist-hospitalist programs threaten to siphon off your medical hospitalist workforce, or are they a boon?
Answer: Having specialized physicians focus on hospital care is a powerful model. Not only are they available all the time, but they are keeping up with innovations in their field. More importantly, they get involved in system improvement in a way that the part-time hospital person will not.

—Bob Wachter, MD, MHM
Q: Are there direct benefits to the hospitalist on the floor?
A: I think it creates a vehicle for collegiality, interchange, and learning across the specialties, which is harder to come by when we’re in the hospital all the time, but the consults we’re interacting with may not be.
Q: Aren’t hospitalists already comanaging patients with neurosurgery, hematology/oncology, and orthopedics at your institution? How are specialist hospitalists different?
A: Neurohospitalists focus their professional practice on the hospitalized care of patients with neurological diseases—they perform the same function for those patients as we do for medical patients. That is, they admit patients, supervise their overall care, and discharge them. On our neurosurgery service, which has a census of 50 patients, the surgeons are in the operating room much of the day. Their post-surgical patients often have multiple medical comorbidities (heart failure, high blood pressures, diabetes, etc.), which is where the medical hospitalist comes in to comanage and coordinate their medical care.
We probably need new lingo to distinguish between medical hospitalists comanaging specialty patients and specialty hospitalists, because it can be confusing to people.
Q: Is this model sustainable in the community and rural settings, where specialists are in short supply?
A: There is a size below which you probably cannot support a specialty hospitalist. But larger places can, and their value is not only what they do at that individual hospital, but the fact that they can teach and do research and (quality improvement) that may help influence care beyond their organization’s walls.
—GH
Bob Wachter, MD, MHM, has watched the hospitalist movement grow from its infancy in the mid-1990s to more than 30,000 hospitalists practicing nationwide today. As professor and chief of the Division of Hospital Medicine and associate chairman of the Department of Medicine at the University of California at San Francisco, and chief of the medical service at UCSF Medical Center, Dr. Wachter also has watched the HM model spread to other medical specialties, including a handful of departments in his own hospital. The Hospitalist caught up with Dr. Wachter and found out what he thinks about the spread of the HM model.
Question: Do specialist-hospitalist programs threaten to siphon off your medical hospitalist workforce, or are they a boon?
Answer: Having specialized physicians focus on hospital care is a powerful model. Not only are they available all the time, but they are keeping up with innovations in their field. More importantly, they get involved in system improvement in a way that the part-time hospital person will not.

—Bob Wachter, MD, MHM
Q: Are there direct benefits to the hospitalist on the floor?
A: I think it creates a vehicle for collegiality, interchange, and learning across the specialties, which is harder to come by when we’re in the hospital all the time, but the consults we’re interacting with may not be.
Q: Aren’t hospitalists already comanaging patients with neurosurgery, hematology/oncology, and orthopedics at your institution? How are specialist hospitalists different?
A: Neurohospitalists focus their professional practice on the hospitalized care of patients with neurological diseases—they perform the same function for those patients as we do for medical patients. That is, they admit patients, supervise their overall care, and discharge them. On our neurosurgery service, which has a census of 50 patients, the surgeons are in the operating room much of the day. Their post-surgical patients often have multiple medical comorbidities (heart failure, high blood pressures, diabetes, etc.), which is where the medical hospitalist comes in to comanage and coordinate their medical care.
We probably need new lingo to distinguish between medical hospitalists comanaging specialty patients and specialty hospitalists, because it can be confusing to people.
Q: Is this model sustainable in the community and rural settings, where specialists are in short supply?
A: There is a size below which you probably cannot support a specialty hospitalist. But larger places can, and their value is not only what they do at that individual hospital, but the fact that they can teach and do research and (quality improvement) that may help influence care beyond their organization’s walls.
—GH