User login
Cost, value of new cancer treatments rarely correlate
New high-priced cancer treatments rarely demonstrate value, compared with the prices being charged for them.
Researchers examined clinical trial data for new treatments using scoring frameworks developed by both the American Society of Clinical Oncology (ASCO) and the European Society for Medical Oncology (ESMO) that assess the value of cancer therapies by taking into consideration survival gains in relation to toxicity and quality. Findings were simultaneously published online June 2 in The Lancet Oncology (2017 June 2. doi: 10.1016/S1470-2045(17)30415-1) and presented at the annual meeting of the American Society of Clinical Oncology.
One of the findings from the research quantified the magnitude of how much benefit a new treatment offers patients.
“We were able to compare that across different treatments and we were able to calculate the drug cost per month of treatment with each new cancer treatment,” Christopher Booth, MD, of Queen’s University Cancer Research Institute, Kingston, Ont., and one of the report’s authors, said in an interview.
“We looked to see whether there is a relationship between cost and benefit. In most elements of our economy, if something is of higher value and better quality, we often pay more for it as opposed to something that offers less quality or less value,” he continued. “We found that that relationship does not hold true in the world of cancer drugs. In fact, if anything, we saw an inverse association, meaning that the drugs that are the most expensive actually have the smallest benefit for patients. That is probably the most important finding of the work.”
Dr. Booth suggested that this has to do with the fact that value is never a factor in pricing.
“In very general terms, the way that a new drug is priced is effectively the highest price the market will bear,” he said. “There really isn’t an approach currently to price drugs based on the return that they offer to patients and society. There is a conversation under way within the oncology community about whether we need to be shifting that conversation to something perhaps called value-based pricing where treatments that offer greater benefit to patients are priced higher than treatments that offer negligible benefit.”
He also noted that “there is not a lot of incentive for the research community or pharmaceutical companies to identify drugs that have larger and larger benefits, being that the financial return on their investment does not appear to be related to how much benefit the drug offers. If we shifted that conversation, it would hopefully, at least in some way, drive the research community and push us to find treatments that have large or meaningful benefits to patients instead of some of these treatments that are very expensive with important side effects that really offer very small improvements in patient outcomes.”
Dr. Booth continued: “I think it’s inevitable and I think what these score cards are doing, and even though they are not perfect, are getting the conversation into the mainstream and for the first time allowing oncologists and researchers and policy makers to start some kind of comparative analyses looking at one treatment compared to the other in the same disease setting as offering a greater or lesser benefit to patients,” which is an important conversation as health care systems are faced with stretching their limited resources to help the populations they serve.
The other key finding of the report was the lack of correlation between the scores yielded by the ASCO Value Framework and the ESMO Magnitude of Clinical Benefit Scale.
“We looked at a number of randomized trials of new cancer treatments and we scored them using the European approach and the American approach and found that there is actually fairly little agreement between the two systems,” Dr. Booth said.
The cause, he suggested, was tied to differences in methodology between the two systems, though he noted that both frameworks are evolving and “I suspect there will be convergence over time.”
New high-priced cancer treatments rarely demonstrate value, compared with the prices being charged for them.
Researchers examined clinical trial data for new treatments using scoring frameworks developed by both the American Society of Clinical Oncology (ASCO) and the European Society for Medical Oncology (ESMO) that assess the value of cancer therapies by taking into consideration survival gains in relation to toxicity and quality. Findings were simultaneously published online June 2 in The Lancet Oncology (2017 June 2. doi: 10.1016/S1470-2045(17)30415-1) and presented at the annual meeting of the American Society of Clinical Oncology.
One of the findings from the research quantified the magnitude of how much benefit a new treatment offers patients.
“We were able to compare that across different treatments and we were able to calculate the drug cost per month of treatment with each new cancer treatment,” Christopher Booth, MD, of Queen’s University Cancer Research Institute, Kingston, Ont., and one of the report’s authors, said in an interview.
“We looked to see whether there is a relationship between cost and benefit. In most elements of our economy, if something is of higher value and better quality, we often pay more for it as opposed to something that offers less quality or less value,” he continued. “We found that that relationship does not hold true in the world of cancer drugs. In fact, if anything, we saw an inverse association, meaning that the drugs that are the most expensive actually have the smallest benefit for patients. That is probably the most important finding of the work.”
Dr. Booth suggested that this has to do with the fact that value is never a factor in pricing.
“In very general terms, the way that a new drug is priced is effectively the highest price the market will bear,” he said. “There really isn’t an approach currently to price drugs based on the return that they offer to patients and society. There is a conversation under way within the oncology community about whether we need to be shifting that conversation to something perhaps called value-based pricing where treatments that offer greater benefit to patients are priced higher than treatments that offer negligible benefit.”
He also noted that “there is not a lot of incentive for the research community or pharmaceutical companies to identify drugs that have larger and larger benefits, being that the financial return on their investment does not appear to be related to how much benefit the drug offers. If we shifted that conversation, it would hopefully, at least in some way, drive the research community and push us to find treatments that have large or meaningful benefits to patients instead of some of these treatments that are very expensive with important side effects that really offer very small improvements in patient outcomes.”
Dr. Booth continued: “I think it’s inevitable and I think what these score cards are doing, and even though they are not perfect, are getting the conversation into the mainstream and for the first time allowing oncologists and researchers and policy makers to start some kind of comparative analyses looking at one treatment compared to the other in the same disease setting as offering a greater or lesser benefit to patients,” which is an important conversation as health care systems are faced with stretching their limited resources to help the populations they serve.
The other key finding of the report was the lack of correlation between the scores yielded by the ASCO Value Framework and the ESMO Magnitude of Clinical Benefit Scale.
“We looked at a number of randomized trials of new cancer treatments and we scored them using the European approach and the American approach and found that there is actually fairly little agreement between the two systems,” Dr. Booth said.
The cause, he suggested, was tied to differences in methodology between the two systems, though he noted that both frameworks are evolving and “I suspect there will be convergence over time.”
New high-priced cancer treatments rarely demonstrate value, compared with the prices being charged for them.
Researchers examined clinical trial data for new treatments using scoring frameworks developed by both the American Society of Clinical Oncology (ASCO) and the European Society for Medical Oncology (ESMO) that assess the value of cancer therapies by taking into consideration survival gains in relation to toxicity and quality. Findings were simultaneously published online June 2 in The Lancet Oncology (2017 June 2. doi: 10.1016/S1470-2045(17)30415-1) and presented at the annual meeting of the American Society of Clinical Oncology.
One of the findings from the research quantified the magnitude of how much benefit a new treatment offers patients.
“We were able to compare that across different treatments and we were able to calculate the drug cost per month of treatment with each new cancer treatment,” Christopher Booth, MD, of Queen’s University Cancer Research Institute, Kingston, Ont., and one of the report’s authors, said in an interview.
“We looked to see whether there is a relationship between cost and benefit. In most elements of our economy, if something is of higher value and better quality, we often pay more for it as opposed to something that offers less quality or less value,” he continued. “We found that that relationship does not hold true in the world of cancer drugs. In fact, if anything, we saw an inverse association, meaning that the drugs that are the most expensive actually have the smallest benefit for patients. That is probably the most important finding of the work.”
Dr. Booth suggested that this has to do with the fact that value is never a factor in pricing.
“In very general terms, the way that a new drug is priced is effectively the highest price the market will bear,” he said. “There really isn’t an approach currently to price drugs based on the return that they offer to patients and society. There is a conversation under way within the oncology community about whether we need to be shifting that conversation to something perhaps called value-based pricing where treatments that offer greater benefit to patients are priced higher than treatments that offer negligible benefit.”
He also noted that “there is not a lot of incentive for the research community or pharmaceutical companies to identify drugs that have larger and larger benefits, being that the financial return on their investment does not appear to be related to how much benefit the drug offers. If we shifted that conversation, it would hopefully, at least in some way, drive the research community and push us to find treatments that have large or meaningful benefits to patients instead of some of these treatments that are very expensive with important side effects that really offer very small improvements in patient outcomes.”
Dr. Booth continued: “I think it’s inevitable and I think what these score cards are doing, and even though they are not perfect, are getting the conversation into the mainstream and for the first time allowing oncologists and researchers and policy makers to start some kind of comparative analyses looking at one treatment compared to the other in the same disease setting as offering a greater or lesser benefit to patients,” which is an important conversation as health care systems are faced with stretching their limited resources to help the populations they serve.
The other key finding of the report was the lack of correlation between the scores yielded by the ASCO Value Framework and the ESMO Magnitude of Clinical Benefit Scale.
“We looked at a number of randomized trials of new cancer treatments and we scored them using the European approach and the American approach and found that there is actually fairly little agreement between the two systems,” Dr. Booth said.
The cause, he suggested, was tied to differences in methodology between the two systems, though he noted that both frameworks are evolving and “I suspect there will be convergence over time.”
FROM ASCO 2017
Health reform action shifts to Senate, exacerbated by poor AHCA CBO score
With a highly anticipated impact analysis from the nonpartisan Congressional Budget Office, the much maligned American Health Care Act seems relegated to a Capitol Hill recycling bin and repeal/replace focus has moved to the Senate.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee, has reached out to physicians’ organizations to learn their priorities.
The organization also called for the reduction of regulatory burdens and increased cost transparency.
Additional recommendations include
• Support for advanceable, refundable tax credits to help individuals purchase private health care coverage, with the current tax credit structure in the ACA maintained.
• Maintenance of the ACA cost-sharing reductions for 2017 and 2018.
• Enhanced tax credits for young adults aged 19-30 years and modest funding of health savings accounts to help counter high deductibles.
The AMA also supports maintenance of the current Medicaid expansion while offering states even more flexibility for innovation.
Similarly, the American Osteopathic Association noted that any policy changes “should be to expand or at least maintain access to comprehensive, affordable coverage and care. With that said, we are also concerned about the growing potential for market instability and the deleterious effect that a collapse would have on patients’ access to insurance coverage and health care services,” according to a May 23 letter from Boyd Buser, DO, president of AOA.
The organization called for continued coverage of preventive care services with no copayment and expressed concern that “the changes being considered for the Medicaid program as part of health reform discussions will significantly impact coverage for these Americans.”
The House-passed American Health Care Act (H.R. 1628) would repeal the ACA’s Medicaid expansion provisions and implement a per-capita funding scheme for state Medicaid programs. “The AOA is concerned that this will leave states with insufficient funds to provide care to the most vulnerable in our society,” Dr. Buser wrote.
AOA recommended a number of consumer protections, including adequate funding of an invisible risk-sharing program that is maintained by an organization outside of the government; efforts to improve health literacy, and other cost-containment recommendations, particularly the maintenance of the cost-sharing reduction payments.
Even if the Senate were able to incorporate these recommendations, its leaders face an uphill battle to get enough support for passage.
“If, on the Republican side, they can come to an agreement on the bill, I think they have a chance of passing it,” Julius Hobson, senior policy analyst at the Washington law firm Polsinelli, said in an interview. “The GOP is not taking up the House-passed AHCA but is proceeding with writing its own reform legislation.
However, he pointed out that there is very little margin for error because the party only holds a two-seat majority and moderates Republican senators have expressed concerns about cuts to Medicaid.
If Senate Republicans do pass a bill that appeals to its more moderate members, that legislation is likely to face stiff opposition in the House.
“Given what we just saw the House go through, I don’t know” if a more moderate bill could pass in that chamber, he said, adding that, if “they don’t do this by the end of the calendar year, you can forget it.”
The potential death blow to the AHCA came in the form of a financial impact “score” from the Congressional Budget Office (CBO).
The government budget watchdog estimated the AHCA would reduce the budget deficit by $119 billion from 2017 to 2026, with the largest savings coming from “reductions in outlays for Medicaid and from the replacement of the Affordable Care Act’s subsidies for nongroup health insurance with new tax credits for nongroup health insurance. Those savings would be partially offset by other changes in coverage provisions – spending for a new Patient and State Stability Fund, designed to reduce premiums, and a reduction in revenues from repealing penalties on employers who do not offer insurance and on people who do not purchase insurance.”
The CBO score also predicted that an additional 23 million patients would be uninsured by 2026 – for a total of 51 million – compared with a total of 28 million uninsured under the ACA.
CBO analysts predicted that nongroup health insurance markets would stabilize before 2020 under the AHCA, but instability could increased if states seek waivers to modify the essential health benefits and community rating requirements.
Although premiums overall would decrease under the AHCA, certain subpopulations could see substantial increases under state waivers.
Additionally, the waivers could also impact the provision of care.
Analysis of the impact of the waiving of essential health benefits is the part doctors should be paying most attention to, Laura Wooster, AOA senior vice president of public policy, said in an interview.
“They would start seeing patients who potentially would have insurance plans that only cover certain benefits,” she said. That would “prevent them from providing certain services or care for their patients under the patients’ coverage. Even a more immediate administrative aspect of it that things would become more complicated if there isn’t a uniform standard, then it is going to be even more complicated for patients to navigate what’s covered, what’s not, and, if the physician takes the insurance, which services are they able to provide.”
She added that, if states waive any or all of the essential health benefits, those benefits would no longer be subject to lifetime and annual caps on spending.
Mr. Hobson suggested that the biggest part of the CBO score that doctors should be worried about is the spike in uninsured that could result from any reform effort.
“The concern for physicians will be that they are more likely to see more patients who don’t have insurance depending on the specialty,” Mr. Hobson said. “Primary care will certainly see a lot of that. Physicians in emergency departments will see more of them because, as you well know, when people don’t have insurance, that’s where they show up when they are at their sickest.”
He added that a “patient can come in, a physician can diagnose the problem, but, if the patient doesn’t have the insurance, he or she may not have the ability to spend the money to do what they need to do, which means they will be back.”
With a highly anticipated impact analysis from the nonpartisan Congressional Budget Office, the much maligned American Health Care Act seems relegated to a Capitol Hill recycling bin and repeal/replace focus has moved to the Senate.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee, has reached out to physicians’ organizations to learn their priorities.
The organization also called for the reduction of regulatory burdens and increased cost transparency.
Additional recommendations include
• Support for advanceable, refundable tax credits to help individuals purchase private health care coverage, with the current tax credit structure in the ACA maintained.
• Maintenance of the ACA cost-sharing reductions for 2017 and 2018.
• Enhanced tax credits for young adults aged 19-30 years and modest funding of health savings accounts to help counter high deductibles.
The AMA also supports maintenance of the current Medicaid expansion while offering states even more flexibility for innovation.
Similarly, the American Osteopathic Association noted that any policy changes “should be to expand or at least maintain access to comprehensive, affordable coverage and care. With that said, we are also concerned about the growing potential for market instability and the deleterious effect that a collapse would have on patients’ access to insurance coverage and health care services,” according to a May 23 letter from Boyd Buser, DO, president of AOA.
The organization called for continued coverage of preventive care services with no copayment and expressed concern that “the changes being considered for the Medicaid program as part of health reform discussions will significantly impact coverage for these Americans.”
The House-passed American Health Care Act (H.R. 1628) would repeal the ACA’s Medicaid expansion provisions and implement a per-capita funding scheme for state Medicaid programs. “The AOA is concerned that this will leave states with insufficient funds to provide care to the most vulnerable in our society,” Dr. Buser wrote.
AOA recommended a number of consumer protections, including adequate funding of an invisible risk-sharing program that is maintained by an organization outside of the government; efforts to improve health literacy, and other cost-containment recommendations, particularly the maintenance of the cost-sharing reduction payments.
Even if the Senate were able to incorporate these recommendations, its leaders face an uphill battle to get enough support for passage.
“If, on the Republican side, they can come to an agreement on the bill, I think they have a chance of passing it,” Julius Hobson, senior policy analyst at the Washington law firm Polsinelli, said in an interview. “The GOP is not taking up the House-passed AHCA but is proceeding with writing its own reform legislation.
However, he pointed out that there is very little margin for error because the party only holds a two-seat majority and moderates Republican senators have expressed concerns about cuts to Medicaid.
If Senate Republicans do pass a bill that appeals to its more moderate members, that legislation is likely to face stiff opposition in the House.
“Given what we just saw the House go through, I don’t know” if a more moderate bill could pass in that chamber, he said, adding that, if “they don’t do this by the end of the calendar year, you can forget it.”
The potential death blow to the AHCA came in the form of a financial impact “score” from the Congressional Budget Office (CBO).
The government budget watchdog estimated the AHCA would reduce the budget deficit by $119 billion from 2017 to 2026, with the largest savings coming from “reductions in outlays for Medicaid and from the replacement of the Affordable Care Act’s subsidies for nongroup health insurance with new tax credits for nongroup health insurance. Those savings would be partially offset by other changes in coverage provisions – spending for a new Patient and State Stability Fund, designed to reduce premiums, and a reduction in revenues from repealing penalties on employers who do not offer insurance and on people who do not purchase insurance.”
The CBO score also predicted that an additional 23 million patients would be uninsured by 2026 – for a total of 51 million – compared with a total of 28 million uninsured under the ACA.
CBO analysts predicted that nongroup health insurance markets would stabilize before 2020 under the AHCA, but instability could increased if states seek waivers to modify the essential health benefits and community rating requirements.
Although premiums overall would decrease under the AHCA, certain subpopulations could see substantial increases under state waivers.
Additionally, the waivers could also impact the provision of care.
Analysis of the impact of the waiving of essential health benefits is the part doctors should be paying most attention to, Laura Wooster, AOA senior vice president of public policy, said in an interview.
“They would start seeing patients who potentially would have insurance plans that only cover certain benefits,” she said. That would “prevent them from providing certain services or care for their patients under the patients’ coverage. Even a more immediate administrative aspect of it that things would become more complicated if there isn’t a uniform standard, then it is going to be even more complicated for patients to navigate what’s covered, what’s not, and, if the physician takes the insurance, which services are they able to provide.”
She added that, if states waive any or all of the essential health benefits, those benefits would no longer be subject to lifetime and annual caps on spending.
Mr. Hobson suggested that the biggest part of the CBO score that doctors should be worried about is the spike in uninsured that could result from any reform effort.
“The concern for physicians will be that they are more likely to see more patients who don’t have insurance depending on the specialty,” Mr. Hobson said. “Primary care will certainly see a lot of that. Physicians in emergency departments will see more of them because, as you well know, when people don’t have insurance, that’s where they show up when they are at their sickest.”
He added that a “patient can come in, a physician can diagnose the problem, but, if the patient doesn’t have the insurance, he or she may not have the ability to spend the money to do what they need to do, which means they will be back.”
With a highly anticipated impact analysis from the nonpartisan Congressional Budget Office, the much maligned American Health Care Act seems relegated to a Capitol Hill recycling bin and repeal/replace focus has moved to the Senate.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee, has reached out to physicians’ organizations to learn their priorities.
The organization also called for the reduction of regulatory burdens and increased cost transparency.
Additional recommendations include
• Support for advanceable, refundable tax credits to help individuals purchase private health care coverage, with the current tax credit structure in the ACA maintained.
• Maintenance of the ACA cost-sharing reductions for 2017 and 2018.
• Enhanced tax credits for young adults aged 19-30 years and modest funding of health savings accounts to help counter high deductibles.
The AMA also supports maintenance of the current Medicaid expansion while offering states even more flexibility for innovation.
Similarly, the American Osteopathic Association noted that any policy changes “should be to expand or at least maintain access to comprehensive, affordable coverage and care. With that said, we are also concerned about the growing potential for market instability and the deleterious effect that a collapse would have on patients’ access to insurance coverage and health care services,” according to a May 23 letter from Boyd Buser, DO, president of AOA.
The organization called for continued coverage of preventive care services with no copayment and expressed concern that “the changes being considered for the Medicaid program as part of health reform discussions will significantly impact coverage for these Americans.”
The House-passed American Health Care Act (H.R. 1628) would repeal the ACA’s Medicaid expansion provisions and implement a per-capita funding scheme for state Medicaid programs. “The AOA is concerned that this will leave states with insufficient funds to provide care to the most vulnerable in our society,” Dr. Buser wrote.
AOA recommended a number of consumer protections, including adequate funding of an invisible risk-sharing program that is maintained by an organization outside of the government; efforts to improve health literacy, and other cost-containment recommendations, particularly the maintenance of the cost-sharing reduction payments.
Even if the Senate were able to incorporate these recommendations, its leaders face an uphill battle to get enough support for passage.
“If, on the Republican side, they can come to an agreement on the bill, I think they have a chance of passing it,” Julius Hobson, senior policy analyst at the Washington law firm Polsinelli, said in an interview. “The GOP is not taking up the House-passed AHCA but is proceeding with writing its own reform legislation.
However, he pointed out that there is very little margin for error because the party only holds a two-seat majority and moderates Republican senators have expressed concerns about cuts to Medicaid.
If Senate Republicans do pass a bill that appeals to its more moderate members, that legislation is likely to face stiff opposition in the House.
“Given what we just saw the House go through, I don’t know” if a more moderate bill could pass in that chamber, he said, adding that, if “they don’t do this by the end of the calendar year, you can forget it.”
The potential death blow to the AHCA came in the form of a financial impact “score” from the Congressional Budget Office (CBO).
The government budget watchdog estimated the AHCA would reduce the budget deficit by $119 billion from 2017 to 2026, with the largest savings coming from “reductions in outlays for Medicaid and from the replacement of the Affordable Care Act’s subsidies for nongroup health insurance with new tax credits for nongroup health insurance. Those savings would be partially offset by other changes in coverage provisions – spending for a new Patient and State Stability Fund, designed to reduce premiums, and a reduction in revenues from repealing penalties on employers who do not offer insurance and on people who do not purchase insurance.”
The CBO score also predicted that an additional 23 million patients would be uninsured by 2026 – for a total of 51 million – compared with a total of 28 million uninsured under the ACA.
CBO analysts predicted that nongroup health insurance markets would stabilize before 2020 under the AHCA, but instability could increased if states seek waivers to modify the essential health benefits and community rating requirements.
Although premiums overall would decrease under the AHCA, certain subpopulations could see substantial increases under state waivers.
Additionally, the waivers could also impact the provision of care.
Analysis of the impact of the waiving of essential health benefits is the part doctors should be paying most attention to, Laura Wooster, AOA senior vice president of public policy, said in an interview.
“They would start seeing patients who potentially would have insurance plans that only cover certain benefits,” she said. That would “prevent them from providing certain services or care for their patients under the patients’ coverage. Even a more immediate administrative aspect of it that things would become more complicated if there isn’t a uniform standard, then it is going to be even more complicated for patients to navigate what’s covered, what’s not, and, if the physician takes the insurance, which services are they able to provide.”
She added that, if states waive any or all of the essential health benefits, those benefits would no longer be subject to lifetime and annual caps on spending.
Mr. Hobson suggested that the biggest part of the CBO score that doctors should be worried about is the spike in uninsured that could result from any reform effort.
“The concern for physicians will be that they are more likely to see more patients who don’t have insurance depending on the specialty,” Mr. Hobson said. “Primary care will certainly see a lot of that. Physicians in emergency departments will see more of them because, as you well know, when people don’t have insurance, that’s where they show up when they are at their sickest.”
He added that a “patient can come in, a physician can diagnose the problem, but, if the patient doesn’t have the insurance, he or she may not have the ability to spend the money to do what they need to do, which means they will be back.”
Trump administration loosens up HealthCare.gov
Patients buying health insurance through an Affordable Care Act health insurance exchange will no longer have to complete the transaction via HealthCare.gov.
The move is intended to help bring stability to the health insurance market, Seema Verma, administrator of the Centers for Medicare & Medicaid Services, said in a statement.
“It is common sense to make it as simple and easy as possible for consumers to shop for and access health coverage,” she said. “It is time to get the federal government out of the way and give patients the best tools to make their own health care decision.”
The change will take effect with the open enrollment period for the 2018 coverage year.
Since the beginning of the health insurance exchanges, patients were required to complete their coverage applications via HealthCare.gov. Feedback from users indicated that “the process was confusing and made it harder to complete the application,” Ms. Verma said in a statement.
The move comes as the Republican-led Congress and the Trump Administration seek to repeal and replace the ACA. This move would deemphasize the government’s role in providing coverage as consumers could potentially avoid contact with HealthCare.gov altogether if they are using a third party to purchase coverage.
Patients buying health insurance through an Affordable Care Act health insurance exchange will no longer have to complete the transaction via HealthCare.gov.
The move is intended to help bring stability to the health insurance market, Seema Verma, administrator of the Centers for Medicare & Medicaid Services, said in a statement.
“It is common sense to make it as simple and easy as possible for consumers to shop for and access health coverage,” she said. “It is time to get the federal government out of the way and give patients the best tools to make their own health care decision.”
The change will take effect with the open enrollment period for the 2018 coverage year.
Since the beginning of the health insurance exchanges, patients were required to complete their coverage applications via HealthCare.gov. Feedback from users indicated that “the process was confusing and made it harder to complete the application,” Ms. Verma said in a statement.
The move comes as the Republican-led Congress and the Trump Administration seek to repeal and replace the ACA. This move would deemphasize the government’s role in providing coverage as consumers could potentially avoid contact with HealthCare.gov altogether if they are using a third party to purchase coverage.
Patients buying health insurance through an Affordable Care Act health insurance exchange will no longer have to complete the transaction via HealthCare.gov.
The move is intended to help bring stability to the health insurance market, Seema Verma, administrator of the Centers for Medicare & Medicaid Services, said in a statement.
“It is common sense to make it as simple and easy as possible for consumers to shop for and access health coverage,” she said. “It is time to get the federal government out of the way and give patients the best tools to make their own health care decision.”
The change will take effect with the open enrollment period for the 2018 coverage year.
Since the beginning of the health insurance exchanges, patients were required to complete their coverage applications via HealthCare.gov. Feedback from users indicated that “the process was confusing and made it harder to complete the application,” Ms. Verma said in a statement.
The move comes as the Republican-led Congress and the Trump Administration seek to repeal and replace the ACA. This move would deemphasize the government’s role in providing coverage as consumers could potentially avoid contact with HealthCare.gov altogether if they are using a third party to purchase coverage.
Physician-created APMs: Early recommendations offer insight
Three physician-created advanced alternative payment models have been recommended for approval by an advisory committee of the Health & Human Services department. Their path to this milestone can help guide organizations and groups who want to benefit from the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA)–based Quality Payment Program on a more intense scale.
Advanced alternative payment models (APMs) involve physicians taking on two-sided risk along with Medicare in exchange for the potential for higher bonus payments for delivering higher value care to patients. Officials at the Centers for Medicare & Medicaid Services have created seven APMs (some primary care and some specialty focused), but they may not appeal to everyone. That’s where physician-created APMs come in.
Proposals are routed through the Physician-focused Payment Model Technical Advisory Committee (PTAC), comprising physicians and experts in value-based health care systems. Commissioners are appointed by the Comptroller General of the United States.
Each proposals was assigned to three commissioners, including at least one physician, for review against 10 criteria:
- Scope of proposed PFPM (high priority)
- Quality and cost (high priority)
- Payment methodology (high priority)
- Value over volume
- Flexibility
- Ability to be evaluated
- Integration and care coordination
- Patient choice
- Patient safety
- Health information technology
While each proposal met a few of the criteria, none met all three high priority criteria and none were recommended for approval by its preliminary reviewers; however, after committee deliberation, two received provisional recommendation.
“We are recommending the two models for small-scale testing,” PTAC Vice-Chairman Elizabeth Mitchell said in an interview. “Even though we think they are very good ideas, we know that more experience and evidence is required before they may be ready.”
The two models that got the limited recommendation were
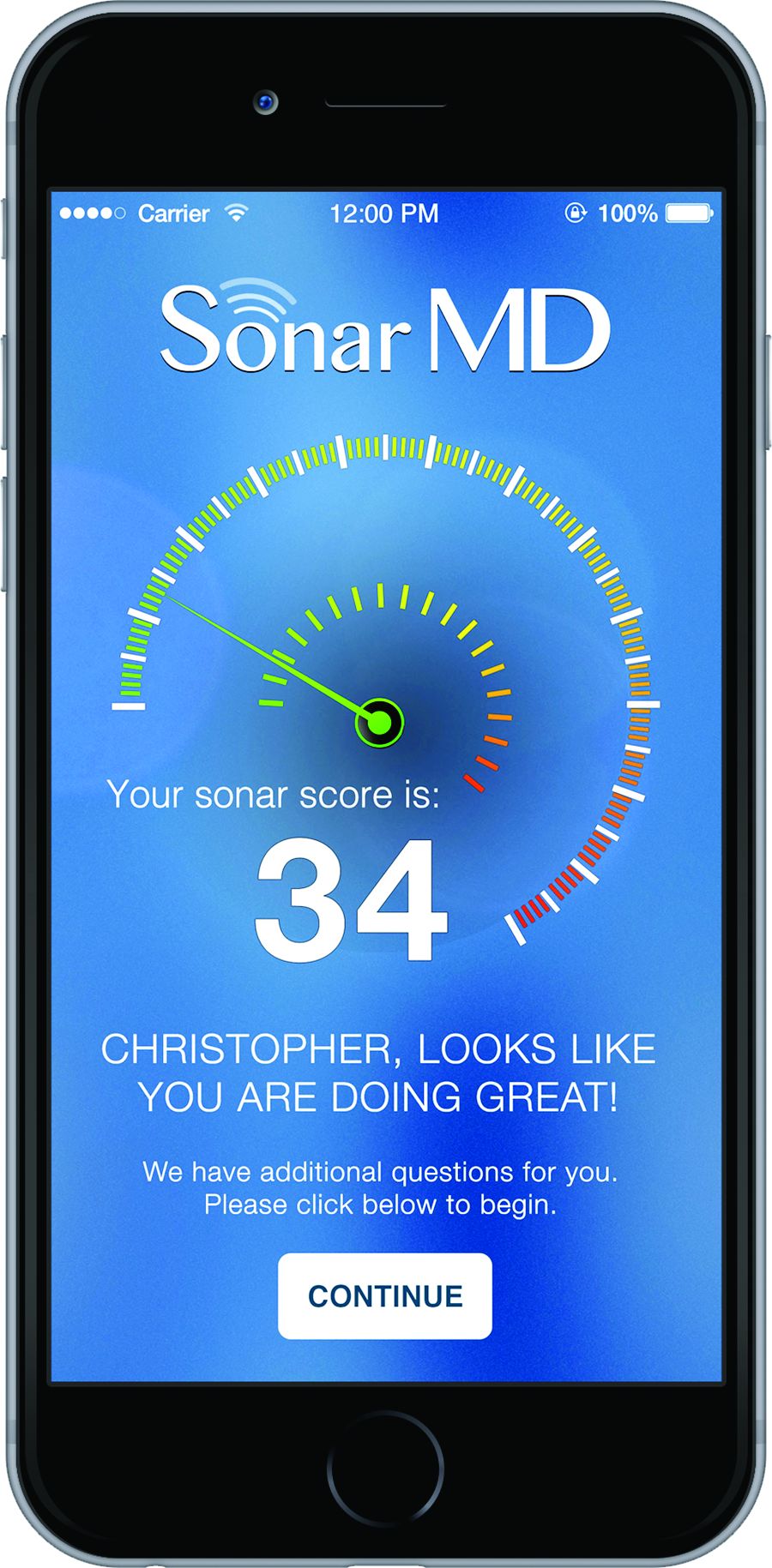
- Project Sonar, submitted by the Illinois Gastroenterology Group and SonarMD, a web-based platform that queries patients with inflammatory bowel disease monthly to determine which are in need of more hands-on care.
- APM, submitted by the American College of Surgeons, an episode-based payment model that uses claims data but expands on existing CMS value-based models by not requiring hospitalizations. It creates an episodic payment using outpatient settings, including acute and chronic care.
The COPD [chronic obstructive pulmonary disease] and Asthma Monitoring Project (CAMP), a smartphone app to remotely monitor and guide treatment of patients with asthma and chronic obstructive pulmonary disease, was not recommended. It was submitted by Pulmonary Medicine, Infectious Disease and Critical Care Consultants Medical Group of Sacremento, Calif.
PTAC has received more than 20 letters of intent from physicians and aims to hold another round of public hearings in September to determine their usefulness.
“I think it is very safe to say that our whole committee has been really gratified with the level of interest and engagement,” said Ms. Mitchell, president and CEO of Network for Regional Healthcare Improvement in Portland, Maine. The volume of applications “underscores the level of interest from the field. The entire reason PTAC was established was to get those good ideas from practicing physicians and others who are identifying better ways to deliver care but are facing barriers in the current payment system.”
She offered advice to those who are contemplating submission of a payment model.
“Really understand the criteria and review the request for proposals,” she said. “I think the committee lays out what we are looking for in terms of information, and we are hoping that it is really straight forward.”
She also stressed that successful models need to work broadly. “We are not talking about something that works for a single practice,” she said. “We are talking about models that are ready for inclusion in the whole CMS portfolio. It is helpful if there is experience to draw from that informs our deliberations, but we recognize that, in some cases, there has not been the opportunity to test these models broadly.”
Most of all, the highest priority when it comes to the models is related to quality of care and cost.
“We are not soliciting models that are essentially tweaks to fee-for-service. We are looking for changes that cannot be made without a new method of payment,” she said, adding that the models “have to either reduce cost while maintaining quality or improve quality without raising cost.”
Meeting transcripts and video are posted online and can help potential applicants see how the committee came to its recommendations.
“The committee does not deliberate on the proposals except in public,” Ms. Mitchell said. “So, those public meetings were the first time we had deliberated on any of the proposals we have considered. The preliminary review teams have discussed it [in depth], but the full committee can only deliberate in public.”
Three physician-created advanced alternative payment models have been recommended for approval by an advisory committee of the Health & Human Services department. Their path to this milestone can help guide organizations and groups who want to benefit from the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA)–based Quality Payment Program on a more intense scale.
Advanced alternative payment models (APMs) involve physicians taking on two-sided risk along with Medicare in exchange for the potential for higher bonus payments for delivering higher value care to patients. Officials at the Centers for Medicare & Medicaid Services have created seven APMs (some primary care and some specialty focused), but they may not appeal to everyone. That’s where physician-created APMs come in.
Proposals are routed through the Physician-focused Payment Model Technical Advisory Committee (PTAC), comprising physicians and experts in value-based health care systems. Commissioners are appointed by the Comptroller General of the United States.
Each proposals was assigned to three commissioners, including at least one physician, for review against 10 criteria:
- Scope of proposed PFPM (high priority)
- Quality and cost (high priority)
- Payment methodology (high priority)
- Value over volume
- Flexibility
- Ability to be evaluated
- Integration and care coordination
- Patient choice
- Patient safety
- Health information technology
While each proposal met a few of the criteria, none met all three high priority criteria and none were recommended for approval by its preliminary reviewers; however, after committee deliberation, two received provisional recommendation.
“We are recommending the two models for small-scale testing,” PTAC Vice-Chairman Elizabeth Mitchell said in an interview. “Even though we think they are very good ideas, we know that more experience and evidence is required before they may be ready.”
The two models that got the limited recommendation were
- Project Sonar, submitted by the Illinois Gastroenterology Group and SonarMD, a web-based platform that queries patients with inflammatory bowel disease monthly to determine which are in need of more hands-on care.
- APM, submitted by the American College of Surgeons, an episode-based payment model that uses claims data but expands on existing CMS value-based models by not requiring hospitalizations. It creates an episodic payment using outpatient settings, including acute and chronic care.
The COPD [chronic obstructive pulmonary disease] and Asthma Monitoring Project (CAMP), a smartphone app to remotely monitor and guide treatment of patients with asthma and chronic obstructive pulmonary disease, was not recommended. It was submitted by Pulmonary Medicine, Infectious Disease and Critical Care Consultants Medical Group of Sacremento, Calif.
PTAC has received more than 20 letters of intent from physicians and aims to hold another round of public hearings in September to determine their usefulness.
“I think it is very safe to say that our whole committee has been really gratified with the level of interest and engagement,” said Ms. Mitchell, president and CEO of Network for Regional Healthcare Improvement in Portland, Maine. The volume of applications “underscores the level of interest from the field. The entire reason PTAC was established was to get those good ideas from practicing physicians and others who are identifying better ways to deliver care but are facing barriers in the current payment system.”
She offered advice to those who are contemplating submission of a payment model.
“Really understand the criteria and review the request for proposals,” she said. “I think the committee lays out what we are looking for in terms of information, and we are hoping that it is really straight forward.”
She also stressed that successful models need to work broadly. “We are not talking about something that works for a single practice,” she said. “We are talking about models that are ready for inclusion in the whole CMS portfolio. It is helpful if there is experience to draw from that informs our deliberations, but we recognize that, in some cases, there has not been the opportunity to test these models broadly.”
Most of all, the highest priority when it comes to the models is related to quality of care and cost.
“We are not soliciting models that are essentially tweaks to fee-for-service. We are looking for changes that cannot be made without a new method of payment,” she said, adding that the models “have to either reduce cost while maintaining quality or improve quality without raising cost.”
Meeting transcripts and video are posted online and can help potential applicants see how the committee came to its recommendations.
“The committee does not deliberate on the proposals except in public,” Ms. Mitchell said. “So, those public meetings were the first time we had deliberated on any of the proposals we have considered. The preliminary review teams have discussed it [in depth], but the full committee can only deliberate in public.”
Three physician-created advanced alternative payment models have been recommended for approval by an advisory committee of the Health & Human Services department. Their path to this milestone can help guide organizations and groups who want to benefit from the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA)–based Quality Payment Program on a more intense scale.
Advanced alternative payment models (APMs) involve physicians taking on two-sided risk along with Medicare in exchange for the potential for higher bonus payments for delivering higher value care to patients. Officials at the Centers for Medicare & Medicaid Services have created seven APMs (some primary care and some specialty focused), but they may not appeal to everyone. That’s where physician-created APMs come in.
Proposals are routed through the Physician-focused Payment Model Technical Advisory Committee (PTAC), comprising physicians and experts in value-based health care systems. Commissioners are appointed by the Comptroller General of the United States.
Each proposals was assigned to three commissioners, including at least one physician, for review against 10 criteria:
- Scope of proposed PFPM (high priority)
- Quality and cost (high priority)
- Payment methodology (high priority)
- Value over volume
- Flexibility
- Ability to be evaluated
- Integration and care coordination
- Patient choice
- Patient safety
- Health information technology
While each proposal met a few of the criteria, none met all three high priority criteria and none were recommended for approval by its preliminary reviewers; however, after committee deliberation, two received provisional recommendation.
“We are recommending the two models for small-scale testing,” PTAC Vice-Chairman Elizabeth Mitchell said in an interview. “Even though we think they are very good ideas, we know that more experience and evidence is required before they may be ready.”
The two models that got the limited recommendation were
- Project Sonar, submitted by the Illinois Gastroenterology Group and SonarMD, a web-based platform that queries patients with inflammatory bowel disease monthly to determine which are in need of more hands-on care.
- APM, submitted by the American College of Surgeons, an episode-based payment model that uses claims data but expands on existing CMS value-based models by not requiring hospitalizations. It creates an episodic payment using outpatient settings, including acute and chronic care.
The COPD [chronic obstructive pulmonary disease] and Asthma Monitoring Project (CAMP), a smartphone app to remotely monitor and guide treatment of patients with asthma and chronic obstructive pulmonary disease, was not recommended. It was submitted by Pulmonary Medicine, Infectious Disease and Critical Care Consultants Medical Group of Sacremento, Calif.
PTAC has received more than 20 letters of intent from physicians and aims to hold another round of public hearings in September to determine their usefulness.
“I think it is very safe to say that our whole committee has been really gratified with the level of interest and engagement,” said Ms. Mitchell, president and CEO of Network for Regional Healthcare Improvement in Portland, Maine. The volume of applications “underscores the level of interest from the field. The entire reason PTAC was established was to get those good ideas from practicing physicians and others who are identifying better ways to deliver care but are facing barriers in the current payment system.”
She offered advice to those who are contemplating submission of a payment model.
“Really understand the criteria and review the request for proposals,” she said. “I think the committee lays out what we are looking for in terms of information, and we are hoping that it is really straight forward.”
She also stressed that successful models need to work broadly. “We are not talking about something that works for a single practice,” she said. “We are talking about models that are ready for inclusion in the whole CMS portfolio. It is helpful if there is experience to draw from that informs our deliberations, but we recognize that, in some cases, there has not been the opportunity to test these models broadly.”
Most of all, the highest priority when it comes to the models is related to quality of care and cost.
“We are not soliciting models that are essentially tweaks to fee-for-service. We are looking for changes that cannot be made without a new method of payment,” she said, adding that the models “have to either reduce cost while maintaining quality or improve quality without raising cost.”
Meeting transcripts and video are posted online and can help potential applicants see how the committee came to its recommendations.
“The committee does not deliberate on the proposals except in public,” Ms. Mitchell said. “So, those public meetings were the first time we had deliberated on any of the proposals we have considered. The preliminary review teams have discussed it [in depth], but the full committee can only deliberate in public.”
One-third of drug postmarket studies go unpublished
More than one-third of postmarket studies following drug approval that should be published are not, according to new research.
Investigators examined a Food and Drug Administration internal database to identify all postmarket drug studies between 2009 and 2013 identified by the agency as completed, with a follow-up search to find if/where the results of the studies were published.
“As of July 2016, 183 of the 288 postmarket studies (63.5%) meeting inclusion criteria were published in either the scientific literature or on the ClinicalTrials.gov website,” Marisa Cruz, MD, medical officer in the Food and Drug Administration’s Office of Public Health Strategy and Analysis, and her colleagues wrote in a researcher letter published online May 15 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2017.1313).
More studies were published in journals (175) than in the agency’s clinical trial registry (87), and the 183 interventional clinical trials had a higher overall publication rate (87.4%) than the other 105 studies combined (21.9%).
Of the 69 interventional clinical trials that were focused on efficacy, 86.2% were categorized as having results that were favorable to the trial sponsor. However, the 57 interventional clinical trials with positive results were no more likely to be published than the 12 trials with negative results, Dr. Cruz and colleagues noted.
The findings are consistent with previous research, the researchers noted, with the analysis demonstrating “that postmarket study results are not consistently disseminated, either through journal publication or trial registries.”
“Despite calls for data sharing and publication of all clinical trial results, publication rates for completed postmarket studies required by the FDA remain relatively low,” the researchers wrote.
While the FDA could publish the data itself, “this approach would likely require new regulations,” the authors noted. “Alternatively, increased sponsor commitment to submitting to journals and to publish all clinical trial results on trial registries, regardless of whether publication is legally required, may serve to promote dissemination of scientific knowledge.”
The researchers reported no conflicts of interest.
gtwachtman@frontlinemedcom.com
More than one-third of postmarket studies following drug approval that should be published are not, according to new research.
Investigators examined a Food and Drug Administration internal database to identify all postmarket drug studies between 2009 and 2013 identified by the agency as completed, with a follow-up search to find if/where the results of the studies were published.
“As of July 2016, 183 of the 288 postmarket studies (63.5%) meeting inclusion criteria were published in either the scientific literature or on the ClinicalTrials.gov website,” Marisa Cruz, MD, medical officer in the Food and Drug Administration’s Office of Public Health Strategy and Analysis, and her colleagues wrote in a researcher letter published online May 15 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2017.1313).
More studies were published in journals (175) than in the agency’s clinical trial registry (87), and the 183 interventional clinical trials had a higher overall publication rate (87.4%) than the other 105 studies combined (21.9%).
Of the 69 interventional clinical trials that were focused on efficacy, 86.2% were categorized as having results that were favorable to the trial sponsor. However, the 57 interventional clinical trials with positive results were no more likely to be published than the 12 trials with negative results, Dr. Cruz and colleagues noted.
The findings are consistent with previous research, the researchers noted, with the analysis demonstrating “that postmarket study results are not consistently disseminated, either through journal publication or trial registries.”
“Despite calls for data sharing and publication of all clinical trial results, publication rates for completed postmarket studies required by the FDA remain relatively low,” the researchers wrote.
While the FDA could publish the data itself, “this approach would likely require new regulations,” the authors noted. “Alternatively, increased sponsor commitment to submitting to journals and to publish all clinical trial results on trial registries, regardless of whether publication is legally required, may serve to promote dissemination of scientific knowledge.”
The researchers reported no conflicts of interest.
gtwachtman@frontlinemedcom.com
More than one-third of postmarket studies following drug approval that should be published are not, according to new research.
Investigators examined a Food and Drug Administration internal database to identify all postmarket drug studies between 2009 and 2013 identified by the agency as completed, with a follow-up search to find if/where the results of the studies were published.
“As of July 2016, 183 of the 288 postmarket studies (63.5%) meeting inclusion criteria were published in either the scientific literature or on the ClinicalTrials.gov website,” Marisa Cruz, MD, medical officer in the Food and Drug Administration’s Office of Public Health Strategy and Analysis, and her colleagues wrote in a researcher letter published online May 15 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2017.1313).
More studies were published in journals (175) than in the agency’s clinical trial registry (87), and the 183 interventional clinical trials had a higher overall publication rate (87.4%) than the other 105 studies combined (21.9%).
Of the 69 interventional clinical trials that were focused on efficacy, 86.2% were categorized as having results that were favorable to the trial sponsor. However, the 57 interventional clinical trials with positive results were no more likely to be published than the 12 trials with negative results, Dr. Cruz and colleagues noted.
The findings are consistent with previous research, the researchers noted, with the analysis demonstrating “that postmarket study results are not consistently disseminated, either through journal publication or trial registries.”
“Despite calls for data sharing and publication of all clinical trial results, publication rates for completed postmarket studies required by the FDA remain relatively low,” the researchers wrote.
While the FDA could publish the data itself, “this approach would likely require new regulations,” the authors noted. “Alternatively, increased sponsor commitment to submitting to journals and to publish all clinical trial results on trial registries, regardless of whether publication is legally required, may serve to promote dissemination of scientific knowledge.”
The researchers reported no conflicts of interest.
gtwachtman@frontlinemedcom.com
Value-based care didn’t trigger spikes in patient dismissals
Fears that the transition to value-based care could lead to doctors dismissing patients from their practice who could adversely affect their reimbursement didn’t come to fruition in a recent federal value-based initiative.
“Patient dismissal could be an unintended consequence of this shift as clinicians face (or perceive they face) pressure to limit their panel to patients for whom they can readily demonstrate value in order to maximize revenue,” Ann S. O’Malley, MD, senior fellow at Mathematica Policy Research, and her colleagues wrote in a research letter published online May 15 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2017.1309).
“A similar portion and distribution of CPC and comparison practices reported ever dismissing patients in the past 2 years,” 89% and 92%, respectively, the researchers reported.
CPC and comparison practices “dismissed patients for similar reasons,” Dr. O’Malley and colleagues added, noting the exception that more comparison practices reported dismissing patients for violating bill payment policies than CPC practices did – 43% vs. 35%, respectively.
Other reasons for dismissing patients included patients being extremely disruptive and/or behaving inappropriately toward clinicians or staff, patients violating chronic pain/controlled substances policies, patients repeatedly missing appointments, patients not following recommended lifestyle changes, and patients making frequent emergency department visits and/or frequent self-referrals to specialists.
Practices participating in the CPC initiative were also asked if participation in the value-based payment model would make them more or less likely to dismiss patients.
“According to most CPC practices, the initiative had no effect or made them less likely to dismiss patients,” the researchers found.
The CMS Centers for Medicare & Medicaid Innovation funded the study. The study authors reported no conflicts of interest.
Fears that the transition to value-based care could lead to doctors dismissing patients from their practice who could adversely affect their reimbursement didn’t come to fruition in a recent federal value-based initiative.
“Patient dismissal could be an unintended consequence of this shift as clinicians face (or perceive they face) pressure to limit their panel to patients for whom they can readily demonstrate value in order to maximize revenue,” Ann S. O’Malley, MD, senior fellow at Mathematica Policy Research, and her colleagues wrote in a research letter published online May 15 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2017.1309).
“A similar portion and distribution of CPC and comparison practices reported ever dismissing patients in the past 2 years,” 89% and 92%, respectively, the researchers reported.
CPC and comparison practices “dismissed patients for similar reasons,” Dr. O’Malley and colleagues added, noting the exception that more comparison practices reported dismissing patients for violating bill payment policies than CPC practices did – 43% vs. 35%, respectively.
Other reasons for dismissing patients included patients being extremely disruptive and/or behaving inappropriately toward clinicians or staff, patients violating chronic pain/controlled substances policies, patients repeatedly missing appointments, patients not following recommended lifestyle changes, and patients making frequent emergency department visits and/or frequent self-referrals to specialists.
Practices participating in the CPC initiative were also asked if participation in the value-based payment model would make them more or less likely to dismiss patients.
“According to most CPC practices, the initiative had no effect or made them less likely to dismiss patients,” the researchers found.
The CMS Centers for Medicare & Medicaid Innovation funded the study. The study authors reported no conflicts of interest.
Fears that the transition to value-based care could lead to doctors dismissing patients from their practice who could adversely affect their reimbursement didn’t come to fruition in a recent federal value-based initiative.
“Patient dismissal could be an unintended consequence of this shift as clinicians face (or perceive they face) pressure to limit their panel to patients for whom they can readily demonstrate value in order to maximize revenue,” Ann S. O’Malley, MD, senior fellow at Mathematica Policy Research, and her colleagues wrote in a research letter published online May 15 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2017.1309).
“A similar portion and distribution of CPC and comparison practices reported ever dismissing patients in the past 2 years,” 89% and 92%, respectively, the researchers reported.
CPC and comparison practices “dismissed patients for similar reasons,” Dr. O’Malley and colleagues added, noting the exception that more comparison practices reported dismissing patients for violating bill payment policies than CPC practices did – 43% vs. 35%, respectively.
Other reasons for dismissing patients included patients being extremely disruptive and/or behaving inappropriately toward clinicians or staff, patients violating chronic pain/controlled substances policies, patients repeatedly missing appointments, patients not following recommended lifestyle changes, and patients making frequent emergency department visits and/or frequent self-referrals to specialists.
Practices participating in the CPC initiative were also asked if participation in the value-based payment model would make them more or less likely to dismiss patients.
“According to most CPC practices, the initiative had no effect or made them less likely to dismiss patients,” the researchers found.
The CMS Centers for Medicare & Medicaid Innovation funded the study. The study authors reported no conflicts of interest.
Do you have to MIPS in 2017? CMS has a tool for that
Want to know if Medicare’s Merit-based Incentive Payment System (MIPS) is in your future?
The Centers for Medicare & Medicaid Services launched a Web tool on May 9. To see if you must participate in MIPS in 2017, just enter your national provider identifier. The agency is also in the process of mailing letters to update physicians on their status. The Web tool can be found at the CMS website.
Physicians who bill Medicare Part B more than $30,000 and see more than 100 Medicare patients must participate in MIPS this year. That threshold will be determined by means of claims submitted Sept. 1, 2015, through Aug. 31, 2016, and Sept. 1, 2016, through Aug. 31, 2017.
Those who don’t meet those criteria but want to participate may do so, but they won’t receive either a bonus or a penalty.
Under the MIPS “pick your pace” option, physicians who meet the threshold but are not ready to participate for either the 90-day period or the full year can report on one measure for 2017. Data on the lone measure need to be submitted to CMS no later than March 31, 2018.
Data need only be submitted for one patient, and, in 2017, all forms of submission – via registry, electronic health record, administrative claims, or attestation – are acceptable, though options may vary based on the performance option selected. Doing this minimum effort will result in no adjustment to Medicare payments in 2019.
Submitting no data at all for 2017, however, will mean a 4% Medicare pay cut in 2019.
To do the bare minimum to avoid any penalty, select a single data measurement from one of three categories: quality measures, improvement activity, or, in the case of Advancing Care Information, four or five base measures, depending on which certified EHR is being used.
There are 271 quality measures from which to choose, as well as 92 improvement activities. Improvement activities focus on care coordination, patient engagement, and patient safety.
For each measure, there is a downloadable spreadsheet that gives detailed information about the measure and how to meet it. The spreadsheet can also be used by physicians to track the data that are collected for submission.
Physicians who are new to Medicare in 2017 do not have to participate in MIPS in 2017.
Another way to be exempt from MIPS is to participate in the Advanced Alternative Payment Model track of the QPP. Doctors participating in APMs will have the opportunity to earn higher payment bonuses but will have to assume more risk and could see payment reductions if quality and value thresholds are not met.
Want to know if Medicare’s Merit-based Incentive Payment System (MIPS) is in your future?
The Centers for Medicare & Medicaid Services launched a Web tool on May 9. To see if you must participate in MIPS in 2017, just enter your national provider identifier. The agency is also in the process of mailing letters to update physicians on their status. The Web tool can be found at the CMS website.
Physicians who bill Medicare Part B more than $30,000 and see more than 100 Medicare patients must participate in MIPS this year. That threshold will be determined by means of claims submitted Sept. 1, 2015, through Aug. 31, 2016, and Sept. 1, 2016, through Aug. 31, 2017.
Those who don’t meet those criteria but want to participate may do so, but they won’t receive either a bonus or a penalty.
Under the MIPS “pick your pace” option, physicians who meet the threshold but are not ready to participate for either the 90-day period or the full year can report on one measure for 2017. Data on the lone measure need to be submitted to CMS no later than March 31, 2018.
Data need only be submitted for one patient, and, in 2017, all forms of submission – via registry, electronic health record, administrative claims, or attestation – are acceptable, though options may vary based on the performance option selected. Doing this minimum effort will result in no adjustment to Medicare payments in 2019.
Submitting no data at all for 2017, however, will mean a 4% Medicare pay cut in 2019.
To do the bare minimum to avoid any penalty, select a single data measurement from one of three categories: quality measures, improvement activity, or, in the case of Advancing Care Information, four or five base measures, depending on which certified EHR is being used.
There are 271 quality measures from which to choose, as well as 92 improvement activities. Improvement activities focus on care coordination, patient engagement, and patient safety.
For each measure, there is a downloadable spreadsheet that gives detailed information about the measure and how to meet it. The spreadsheet can also be used by physicians to track the data that are collected for submission.
Physicians who are new to Medicare in 2017 do not have to participate in MIPS in 2017.
Another way to be exempt from MIPS is to participate in the Advanced Alternative Payment Model track of the QPP. Doctors participating in APMs will have the opportunity to earn higher payment bonuses but will have to assume more risk and could see payment reductions if quality and value thresholds are not met.
Want to know if Medicare’s Merit-based Incentive Payment System (MIPS) is in your future?
The Centers for Medicare & Medicaid Services launched a Web tool on May 9. To see if you must participate in MIPS in 2017, just enter your national provider identifier. The agency is also in the process of mailing letters to update physicians on their status. The Web tool can be found at the CMS website.
Physicians who bill Medicare Part B more than $30,000 and see more than 100 Medicare patients must participate in MIPS this year. That threshold will be determined by means of claims submitted Sept. 1, 2015, through Aug. 31, 2016, and Sept. 1, 2016, through Aug. 31, 2017.
Those who don’t meet those criteria but want to participate may do so, but they won’t receive either a bonus or a penalty.
Under the MIPS “pick your pace” option, physicians who meet the threshold but are not ready to participate for either the 90-day period or the full year can report on one measure for 2017. Data on the lone measure need to be submitted to CMS no later than March 31, 2018.
Data need only be submitted for one patient, and, in 2017, all forms of submission – via registry, electronic health record, administrative claims, or attestation – are acceptable, though options may vary based on the performance option selected. Doing this minimum effort will result in no adjustment to Medicare payments in 2019.
Submitting no data at all for 2017, however, will mean a 4% Medicare pay cut in 2019.
To do the bare minimum to avoid any penalty, select a single data measurement from one of three categories: quality measures, improvement activity, or, in the case of Advancing Care Information, four or five base measures, depending on which certified EHR is being used.
There are 271 quality measures from which to choose, as well as 92 improvement activities. Improvement activities focus on care coordination, patient engagement, and patient safety.
For each measure, there is a downloadable spreadsheet that gives detailed information about the measure and how to meet it. The spreadsheet can also be used by physicians to track the data that are collected for submission.
Physicians who are new to Medicare in 2017 do not have to participate in MIPS in 2017.
Another way to be exempt from MIPS is to participate in the Advanced Alternative Payment Model track of the QPP. Doctors participating in APMs will have the opportunity to earn higher payment bonuses but will have to assume more risk and could see payment reductions if quality and value thresholds are not met.
House barely passes ACA repeal/replace bill
A few additional tweaks to the American Health Care Act helped garner just enough Republican votes to pass the first phase of the party’s three-part effort to repeal and replace the Affordable Care Act.
The bill passed May 4 by a 217-213 margin, with one Republican member not voting. The vote came after a false start in March when House Speaker Paul Ryan (R-Wisc.) canceled consideration because Republicans could not muster enough votes to pass it. All votes in favor of the bill came from GOP members, while all House Democrats plus 20 Republicans voted against passage.
Two amendments helped to make the bill palatable enough to gain enough votes for passage. New amendments from Rep. Gary Palmer (R-Ala.) and Rep. Fred Upton (R-Mich.) targeted high-risk pools. They were added to an April amendment from Rep. Tom MacArthur (R-N.J.) that would allow states to seek waivers for coverage of the essential health benefits and from community rating provisions to allow for higher premiums for those who are sicker or older.
The American Health Care Act (H.R. 1629) in its amended form has not been yet been scored by the Congressional Budget Office (CBO) to determine its effects on the federal budget. However, an earlier CBO analysis of the original, unamended bill predicted an estimated 58 million people would be uninsured by 2026, compared with 28 million under the Affordable Care Act. It is also predicting large premium increases for some groups of patients.
A CBO score is required of all legislation because, under Senate rules, anything that adds to the budget must be offset by additional revenue-generating provisions or cuts elsewhere in the federal budget. The bill, if passed and sent to the president’s desk for signature, is at minimum budget neutral if not deficit reducing.
The amended AHCA was roundly rejected by most physician organizations, including the American Medical Association and many specialty societies.
“The bill passed by the House today will result in millions of Americans losing access to quality, affordable health insurance and those with preexisting health conditions face the possibility of going back to the time when insurers could charge them premiums that made access to coverage out of the question,” AMA President Andrew Gurman, MD, said in a statement. “The AMA urges the Senate and the Administration to work with physician, patient, hospital, and other provider groups to craft bipartisan solutions so all American families can access affordable and meaningful coverage, while preserving the safety net for vulnerable patients.”
House Minority Leader Nancy Pelosi (D-Calif.), in addition to criticizing the bill for its predicted effects in increasing premiums and decreasing coverage for those with preexisting conditions, called out the bill for being nothing more than a means to help cover the cost of a separate tax bill when she described the AHCA as providing “tax cuts for the rich at the expense of health insurance for tens of millions of working families across America” during the debate prior to passage. “Trumpcare is a billionaire’s tax cut disguised as a health care bill.”
Speaker Ryan continued to highlight the continual coverage issues that have been growing in the individual health insurance marketplace, spotlighting Iowa, where insurer Medica has announced that it will likely discontinue providing coverage in 2018, leaving most counties in the state with no option to purchase coverage following the announced withdrawal of Aetna and Wellmark Blue Cross Blue Shield.
“This is a crisis,” Speaker Ryan said during the debate. “What protection is Obamacare if there is no health care plan to purchase in your state? This is the direction Obamacare is rapidly heading.”
In helping to get the AHCA barely over the final hurdle, the Palmer amendment creates an “invisible risk-sharing program” under which the federal government would subsidize insurers to the tune of $15 billion over 9 years. The program would allow insurers to make a prospective determination of who might be a cost-intensive user and move them to the high-risk pool with the federal funding joining insurer funding to help pay for coverage. The amendment also would change the ACA’s reinsurance provisions, which retroactively reimburse insurers for high-utilizing customers.
Neither invisible risk sharing nor retroactive reinsurance are “inherently superior at reducing premiums,” according to an April 12 blog post by the journal Health Affairs. “Premium reductions depend entirely on how much funding the program receives in relation to the risks being insured. Rep. Palmer’s amendment leaves all the critical details of this new, invisible program unspecified, making it hard to generate precise estimate.”
Authors Mark Hall, senior fellow at Brookings Institute, and Nicholas Bagely, law professor at the University of Michigan, Ann Arbor, note that the funding in the amendment “is no more than 2% of total premiums in the market.”
The Upton amendment would add an additional $8 billion in funding for high-risk pools, bringing the total amount potentially available to help cover people with preexisting conditions to $123 billion.
Analysis from Avalere finds that the funding specifically allocated to assist those with preexisting conditions ($23 billion, including the additional $8 billion from the Upton amendment) “will only cover 110,000 individuals with preexisting, chronic condition. If states were to allocate all the other funds [available in the AHCA] toward providing insurance to people with preexisting conditions ... 600,000 with preexisting chronic conditions could be covered.” The analysis notes approximately “2.2 million enrollees in the individual market today have some sort of preexisting chronic condition.”
“Given the amount of funding in the bill, the program can only afford a few small states to opt into medical underwriting,” Caroline Pearson, senior vice president at Avalere, said in a statement. “If any large states receive a waiver, many chronically ill individuals could be left without access to insurance.”
Because the AHCA focuses solely on reforming revenue-related aspects of the ACA and was passed using budget reconciliation procedures, it will need only a simple majority to pass the Senate. However, keeping the bill budget neutral will make it difficult to pass in its current form, even though Republicans hold 52 of the chamber’s 100 seats.
Phase two of the repeal and replace plan will be a full examination of federal regulations and phase three, which will require at least 60 votes in the Senate, will be changes to other provisions in the health care law that are not directly revenue generating. President Donald Trump in the past has suggested that this will include his goals of opening the sale of insurance across state lines and other key priorities.
A few additional tweaks to the American Health Care Act helped garner just enough Republican votes to pass the first phase of the party’s three-part effort to repeal and replace the Affordable Care Act.
The bill passed May 4 by a 217-213 margin, with one Republican member not voting. The vote came after a false start in March when House Speaker Paul Ryan (R-Wisc.) canceled consideration because Republicans could not muster enough votes to pass it. All votes in favor of the bill came from GOP members, while all House Democrats plus 20 Republicans voted against passage.
Two amendments helped to make the bill palatable enough to gain enough votes for passage. New amendments from Rep. Gary Palmer (R-Ala.) and Rep. Fred Upton (R-Mich.) targeted high-risk pools. They were added to an April amendment from Rep. Tom MacArthur (R-N.J.) that would allow states to seek waivers for coverage of the essential health benefits and from community rating provisions to allow for higher premiums for those who are sicker or older.
The American Health Care Act (H.R. 1629) in its amended form has not been yet been scored by the Congressional Budget Office (CBO) to determine its effects on the federal budget. However, an earlier CBO analysis of the original, unamended bill predicted an estimated 58 million people would be uninsured by 2026, compared with 28 million under the Affordable Care Act. It is also predicting large premium increases for some groups of patients.
A CBO score is required of all legislation because, under Senate rules, anything that adds to the budget must be offset by additional revenue-generating provisions or cuts elsewhere in the federal budget. The bill, if passed and sent to the president’s desk for signature, is at minimum budget neutral if not deficit reducing.
The amended AHCA was roundly rejected by most physician organizations, including the American Medical Association and many specialty societies.
“The bill passed by the House today will result in millions of Americans losing access to quality, affordable health insurance and those with preexisting health conditions face the possibility of going back to the time when insurers could charge them premiums that made access to coverage out of the question,” AMA President Andrew Gurman, MD, said in a statement. “The AMA urges the Senate and the Administration to work with physician, patient, hospital, and other provider groups to craft bipartisan solutions so all American families can access affordable and meaningful coverage, while preserving the safety net for vulnerable patients.”
House Minority Leader Nancy Pelosi (D-Calif.), in addition to criticizing the bill for its predicted effects in increasing premiums and decreasing coverage for those with preexisting conditions, called out the bill for being nothing more than a means to help cover the cost of a separate tax bill when she described the AHCA as providing “tax cuts for the rich at the expense of health insurance for tens of millions of working families across America” during the debate prior to passage. “Trumpcare is a billionaire’s tax cut disguised as a health care bill.”
Speaker Ryan continued to highlight the continual coverage issues that have been growing in the individual health insurance marketplace, spotlighting Iowa, where insurer Medica has announced that it will likely discontinue providing coverage in 2018, leaving most counties in the state with no option to purchase coverage following the announced withdrawal of Aetna and Wellmark Blue Cross Blue Shield.
“This is a crisis,” Speaker Ryan said during the debate. “What protection is Obamacare if there is no health care plan to purchase in your state? This is the direction Obamacare is rapidly heading.”
In helping to get the AHCA barely over the final hurdle, the Palmer amendment creates an “invisible risk-sharing program” under which the federal government would subsidize insurers to the tune of $15 billion over 9 years. The program would allow insurers to make a prospective determination of who might be a cost-intensive user and move them to the high-risk pool with the federal funding joining insurer funding to help pay for coverage. The amendment also would change the ACA’s reinsurance provisions, which retroactively reimburse insurers for high-utilizing customers.
Neither invisible risk sharing nor retroactive reinsurance are “inherently superior at reducing premiums,” according to an April 12 blog post by the journal Health Affairs. “Premium reductions depend entirely on how much funding the program receives in relation to the risks being insured. Rep. Palmer’s amendment leaves all the critical details of this new, invisible program unspecified, making it hard to generate precise estimate.”
Authors Mark Hall, senior fellow at Brookings Institute, and Nicholas Bagely, law professor at the University of Michigan, Ann Arbor, note that the funding in the amendment “is no more than 2% of total premiums in the market.”
The Upton amendment would add an additional $8 billion in funding for high-risk pools, bringing the total amount potentially available to help cover people with preexisting conditions to $123 billion.
Analysis from Avalere finds that the funding specifically allocated to assist those with preexisting conditions ($23 billion, including the additional $8 billion from the Upton amendment) “will only cover 110,000 individuals with preexisting, chronic condition. If states were to allocate all the other funds [available in the AHCA] toward providing insurance to people with preexisting conditions ... 600,000 with preexisting chronic conditions could be covered.” The analysis notes approximately “2.2 million enrollees in the individual market today have some sort of preexisting chronic condition.”
“Given the amount of funding in the bill, the program can only afford a few small states to opt into medical underwriting,” Caroline Pearson, senior vice president at Avalere, said in a statement. “If any large states receive a waiver, many chronically ill individuals could be left without access to insurance.”
Because the AHCA focuses solely on reforming revenue-related aspects of the ACA and was passed using budget reconciliation procedures, it will need only a simple majority to pass the Senate. However, keeping the bill budget neutral will make it difficult to pass in its current form, even though Republicans hold 52 of the chamber’s 100 seats.
Phase two of the repeal and replace plan will be a full examination of federal regulations and phase three, which will require at least 60 votes in the Senate, will be changes to other provisions in the health care law that are not directly revenue generating. President Donald Trump in the past has suggested that this will include his goals of opening the sale of insurance across state lines and other key priorities.
A few additional tweaks to the American Health Care Act helped garner just enough Republican votes to pass the first phase of the party’s three-part effort to repeal and replace the Affordable Care Act.
The bill passed May 4 by a 217-213 margin, with one Republican member not voting. The vote came after a false start in March when House Speaker Paul Ryan (R-Wisc.) canceled consideration because Republicans could not muster enough votes to pass it. All votes in favor of the bill came from GOP members, while all House Democrats plus 20 Republicans voted against passage.
Two amendments helped to make the bill palatable enough to gain enough votes for passage. New amendments from Rep. Gary Palmer (R-Ala.) and Rep. Fred Upton (R-Mich.) targeted high-risk pools. They were added to an April amendment from Rep. Tom MacArthur (R-N.J.) that would allow states to seek waivers for coverage of the essential health benefits and from community rating provisions to allow for higher premiums for those who are sicker or older.
The American Health Care Act (H.R. 1629) in its amended form has not been yet been scored by the Congressional Budget Office (CBO) to determine its effects on the federal budget. However, an earlier CBO analysis of the original, unamended bill predicted an estimated 58 million people would be uninsured by 2026, compared with 28 million under the Affordable Care Act. It is also predicting large premium increases for some groups of patients.
A CBO score is required of all legislation because, under Senate rules, anything that adds to the budget must be offset by additional revenue-generating provisions or cuts elsewhere in the federal budget. The bill, if passed and sent to the president’s desk for signature, is at minimum budget neutral if not deficit reducing.
The amended AHCA was roundly rejected by most physician organizations, including the American Medical Association and many specialty societies.
“The bill passed by the House today will result in millions of Americans losing access to quality, affordable health insurance and those with preexisting health conditions face the possibility of going back to the time when insurers could charge them premiums that made access to coverage out of the question,” AMA President Andrew Gurman, MD, said in a statement. “The AMA urges the Senate and the Administration to work with physician, patient, hospital, and other provider groups to craft bipartisan solutions so all American families can access affordable and meaningful coverage, while preserving the safety net for vulnerable patients.”
House Minority Leader Nancy Pelosi (D-Calif.), in addition to criticizing the bill for its predicted effects in increasing premiums and decreasing coverage for those with preexisting conditions, called out the bill for being nothing more than a means to help cover the cost of a separate tax bill when she described the AHCA as providing “tax cuts for the rich at the expense of health insurance for tens of millions of working families across America” during the debate prior to passage. “Trumpcare is a billionaire’s tax cut disguised as a health care bill.”
Speaker Ryan continued to highlight the continual coverage issues that have been growing in the individual health insurance marketplace, spotlighting Iowa, where insurer Medica has announced that it will likely discontinue providing coverage in 2018, leaving most counties in the state with no option to purchase coverage following the announced withdrawal of Aetna and Wellmark Blue Cross Blue Shield.
“This is a crisis,” Speaker Ryan said during the debate. “What protection is Obamacare if there is no health care plan to purchase in your state? This is the direction Obamacare is rapidly heading.”
In helping to get the AHCA barely over the final hurdle, the Palmer amendment creates an “invisible risk-sharing program” under which the federal government would subsidize insurers to the tune of $15 billion over 9 years. The program would allow insurers to make a prospective determination of who might be a cost-intensive user and move them to the high-risk pool with the federal funding joining insurer funding to help pay for coverage. The amendment also would change the ACA’s reinsurance provisions, which retroactively reimburse insurers for high-utilizing customers.
Neither invisible risk sharing nor retroactive reinsurance are “inherently superior at reducing premiums,” according to an April 12 blog post by the journal Health Affairs. “Premium reductions depend entirely on how much funding the program receives in relation to the risks being insured. Rep. Palmer’s amendment leaves all the critical details of this new, invisible program unspecified, making it hard to generate precise estimate.”
Authors Mark Hall, senior fellow at Brookings Institute, and Nicholas Bagely, law professor at the University of Michigan, Ann Arbor, note that the funding in the amendment “is no more than 2% of total premiums in the market.”
The Upton amendment would add an additional $8 billion in funding for high-risk pools, bringing the total amount potentially available to help cover people with preexisting conditions to $123 billion.
Analysis from Avalere finds that the funding specifically allocated to assist those with preexisting conditions ($23 billion, including the additional $8 billion from the Upton amendment) “will only cover 110,000 individuals with preexisting, chronic condition. If states were to allocate all the other funds [available in the AHCA] toward providing insurance to people with preexisting conditions ... 600,000 with preexisting chronic conditions could be covered.” The analysis notes approximately “2.2 million enrollees in the individual market today have some sort of preexisting chronic condition.”
“Given the amount of funding in the bill, the program can only afford a few small states to opt into medical underwriting,” Caroline Pearson, senior vice president at Avalere, said in a statement. “If any large states receive a waiver, many chronically ill individuals could be left without access to insurance.”
Because the AHCA focuses solely on reforming revenue-related aspects of the ACA and was passed using budget reconciliation procedures, it will need only a simple majority to pass the Senate. However, keeping the bill budget neutral will make it difficult to pass in its current form, even though Republicans hold 52 of the chamber’s 100 seats.
Phase two of the repeal and replace plan will be a full examination of federal regulations and phase three, which will require at least 60 votes in the Senate, will be changes to other provisions in the health care law that are not directly revenue generating. President Donald Trump in the past has suggested that this will include his goals of opening the sale of insurance across state lines and other key priorities.
Project Sonar brings gastroenterologists one step closer to a specialty-specific APM
Gastroenterologists wanting to participate in the advanced alternative payment model track of the new Quality Payment Program developed under the Medicare Access and CHIP Reauthorization Act (MACRA) may soon have an option as early as 2018.
Project Sonar, a program that helps gastroenterologists and their patients help manage inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis was the first physician-focused gastroenterology-specific payment model to receive a recommendation from the Physician-Focused Payment Model Technical Advisory Committee (PTAC). The proposal was supported by public comments from AGA and the American Medical Association. It now heads to the U.S. Department of Health & Human Services for final approval.
“The intensive medical home Blue Cross initiated with us because of the success of the pilot pays us a supplemental management fee for every patient that is enrolled,” Lawrence Kosinski, MD, MBA, managing partner at IGG, and a Practice Councillor for the AGA Institute Governing Board, said in an interview. “That management fee is adjusted based on how much savings we produce for the payer. It ultimately winds up being a shared savings program based on our ability to control the cost of care, but we get a management fee upfront in order to make it happen.”
And getting those savings was simply a matter of getting patients engaged in their care. The way Project Sonar works is patients are “pinged” once a month to report on their symptoms. They generally receive a text alert with a link to a secure website where they answer five questions that are derived from the Crohn’s Disease Activity Index. The first one asks how many bowel movements per day over the last 7 days. The second one asks for a rating of abdominal pain. The third one is a rating of the patient’s general state of well-being. Then they are asked whether they are taking drugs for diarrhea. Finally, there are some check boxes for whether they have any eye symptoms or skin rashes or joint pains.
The answers are then weighted and a score is given both to the patient and the doctor. Doctors are alerted to which patients might require more focused attention over those who have their symptoms well managed.
But what is making this program work is that IGG has been able to get an 80% sustained response rate from patients using the program.
“The entire savings that we are generating is coming solely from the patients who participate in the platform,” Dr. Kosinski said.
From an analysis of BCBS of Illinois’ claims data, Dr. Kosinski and his colleagues determined that “ it costs about $24,000 a year to take care of a Crohn’s patient, and over half the money that is spent is spent for inpatient care, complications, bad things happening to these patients.”
He continued: “The difference in annual costs between a pinger and a nonpinger is $6,300. That is a 25% drop in the cost of care.” He added that Project Sonar is leading to a 10% savings in the overall cost of care for these patients when total costs are factored in.
One surprise aspect that Dr. Kosinski found was that patients needed no additional incentive to respond to their pings.
“We had thought we were going to have to get into some gameification and we actually ran a few lotteries to reward people,” he said. “We haven’t had to do it. The patients have participated because I think they feel like they are getting excellent care this way, and I’m very impressed by the fact that the patients have not had to be stimulated to do it.”
At the end of the day, it’s all about improving patients’ lives.
“Patients are doing better,” he noted. “They are staying out of the hospital. They are staying out of the operating room. They are staying at work. They are staying with their families. We have to realize, we look at these as patients with diseases. These are human beings that just happen to have a disease, and they have a life, they have jobs, family, responsibility, and if our Sonar system is allowing them to have a more normal life, there is a lot of traction there.”
Dr. Kosinski is also an Associate Editor for GI & Hepatology News.
Gastroenterologists wanting to participate in the advanced alternative payment model track of the new Quality Payment Program developed under the Medicare Access and CHIP Reauthorization Act (MACRA) may soon have an option as early as 2018.
Project Sonar, a program that helps gastroenterologists and their patients help manage inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis was the first physician-focused gastroenterology-specific payment model to receive a recommendation from the Physician-Focused Payment Model Technical Advisory Committee (PTAC). The proposal was supported by public comments from AGA and the American Medical Association. It now heads to the U.S. Department of Health & Human Services for final approval.
“The intensive medical home Blue Cross initiated with us because of the success of the pilot pays us a supplemental management fee for every patient that is enrolled,” Lawrence Kosinski, MD, MBA, managing partner at IGG, and a Practice Councillor for the AGA Institute Governing Board, said in an interview. “That management fee is adjusted based on how much savings we produce for the payer. It ultimately winds up being a shared savings program based on our ability to control the cost of care, but we get a management fee upfront in order to make it happen.”
And getting those savings was simply a matter of getting patients engaged in their care. The way Project Sonar works is patients are “pinged” once a month to report on their symptoms. They generally receive a text alert with a link to a secure website where they answer five questions that are derived from the Crohn’s Disease Activity Index. The first one asks how many bowel movements per day over the last 7 days. The second one asks for a rating of abdominal pain. The third one is a rating of the patient’s general state of well-being. Then they are asked whether they are taking drugs for diarrhea. Finally, there are some check boxes for whether they have any eye symptoms or skin rashes or joint pains.
The answers are then weighted and a score is given both to the patient and the doctor. Doctors are alerted to which patients might require more focused attention over those who have their symptoms well managed.
But what is making this program work is that IGG has been able to get an 80% sustained response rate from patients using the program.
“The entire savings that we are generating is coming solely from the patients who participate in the platform,” Dr. Kosinski said.
From an analysis of BCBS of Illinois’ claims data, Dr. Kosinski and his colleagues determined that “ it costs about $24,000 a year to take care of a Crohn’s patient, and over half the money that is spent is spent for inpatient care, complications, bad things happening to these patients.”
He continued: “The difference in annual costs between a pinger and a nonpinger is $6,300. That is a 25% drop in the cost of care.” He added that Project Sonar is leading to a 10% savings in the overall cost of care for these patients when total costs are factored in.
One surprise aspect that Dr. Kosinski found was that patients needed no additional incentive to respond to their pings.
“We had thought we were going to have to get into some gameification and we actually ran a few lotteries to reward people,” he said. “We haven’t had to do it. The patients have participated because I think they feel like they are getting excellent care this way, and I’m very impressed by the fact that the patients have not had to be stimulated to do it.”
At the end of the day, it’s all about improving patients’ lives.
“Patients are doing better,” he noted. “They are staying out of the hospital. They are staying out of the operating room. They are staying at work. They are staying with their families. We have to realize, we look at these as patients with diseases. These are human beings that just happen to have a disease, and they have a life, they have jobs, family, responsibility, and if our Sonar system is allowing them to have a more normal life, there is a lot of traction there.”
Dr. Kosinski is also an Associate Editor for GI & Hepatology News.
Gastroenterologists wanting to participate in the advanced alternative payment model track of the new Quality Payment Program developed under the Medicare Access and CHIP Reauthorization Act (MACRA) may soon have an option as early as 2018.
Project Sonar, a program that helps gastroenterologists and their patients help manage inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis was the first physician-focused gastroenterology-specific payment model to receive a recommendation from the Physician-Focused Payment Model Technical Advisory Committee (PTAC). The proposal was supported by public comments from AGA and the American Medical Association. It now heads to the U.S. Department of Health & Human Services for final approval.
“The intensive medical home Blue Cross initiated with us because of the success of the pilot pays us a supplemental management fee for every patient that is enrolled,” Lawrence Kosinski, MD, MBA, managing partner at IGG, and a Practice Councillor for the AGA Institute Governing Board, said in an interview. “That management fee is adjusted based on how much savings we produce for the payer. It ultimately winds up being a shared savings program based on our ability to control the cost of care, but we get a management fee upfront in order to make it happen.”
And getting those savings was simply a matter of getting patients engaged in their care. The way Project Sonar works is patients are “pinged” once a month to report on their symptoms. They generally receive a text alert with a link to a secure website where they answer five questions that are derived from the Crohn’s Disease Activity Index. The first one asks how many bowel movements per day over the last 7 days. The second one asks for a rating of abdominal pain. The third one is a rating of the patient’s general state of well-being. Then they are asked whether they are taking drugs for diarrhea. Finally, there are some check boxes for whether they have any eye symptoms or skin rashes or joint pains.
The answers are then weighted and a score is given both to the patient and the doctor. Doctors are alerted to which patients might require more focused attention over those who have their symptoms well managed.
But what is making this program work is that IGG has been able to get an 80% sustained response rate from patients using the program.
“The entire savings that we are generating is coming solely from the patients who participate in the platform,” Dr. Kosinski said.
From an analysis of BCBS of Illinois’ claims data, Dr. Kosinski and his colleagues determined that “ it costs about $24,000 a year to take care of a Crohn’s patient, and over half the money that is spent is spent for inpatient care, complications, bad things happening to these patients.”
He continued: “The difference in annual costs between a pinger and a nonpinger is $6,300. That is a 25% drop in the cost of care.” He added that Project Sonar is leading to a 10% savings in the overall cost of care for these patients when total costs are factored in.
One surprise aspect that Dr. Kosinski found was that patients needed no additional incentive to respond to their pings.
“We had thought we were going to have to get into some gameification and we actually ran a few lotteries to reward people,” he said. “We haven’t had to do it. The patients have participated because I think they feel like they are getting excellent care this way, and I’m very impressed by the fact that the patients have not had to be stimulated to do it.”
At the end of the day, it’s all about improving patients’ lives.
“Patients are doing better,” he noted. “They are staying out of the hospital. They are staying out of the operating room. They are staying at work. They are staying with their families. We have to realize, we look at these as patients with diseases. These are human beings that just happen to have a disease, and they have a life, they have jobs, family, responsibility, and if our Sonar system is allowing them to have a more normal life, there is a lot of traction there.”
Dr. Kosinski is also an Associate Editor for GI & Hepatology News.
HHS Secretary Price promises reduced health IT burden for physicians
WASHINGTON – Reducing IT burden for doctors and fostering interoperability are two top tech priorities for Health and Human Services Secretary Tom Price, MD.
“We simply have to do a better job of reducing the burden of health IT on physicians and all health care providers,” Dr. Price said April 27 at Health Datapalooza, an annual conference on health data transparency. “The promise of big data and health information technology is so great and absolutely remarkable but we must not, we cannot continue to get this wrong.”
“Now we are seeing physicians leaving the practice of medicine when they are 60 or 55,” he said. “Many of my colleagues, my personal friends who have been practicing, right now they are looking for the exit doors. They are trying to figure out how to get out of practicing medicine and I think it is incredibly important for us as a society to step back and ask, why?”
A significant factor is the shift to electronic health records, which has caused doctors to spend much more time looking at screens and feeling more like data entry clerks than health care providers, he said.
“I know that we have lost more than one physician to retirement because of the kinds of burdens that have been placed on a lot of them and that simply ought to be unacceptable to us,” he said. “You think of the intellectual capital that has been lost by this nation because of the kinds of burdens that clinicians have seen.”
That said, “data is absolutely crucial,” Dr. Price said. “Don’t misunderstand me. It is absolutely critical that we have all the data that we can and that we use it in an evidence-based manner so that we can provide better care and better quality of care to patients.”
He challenged the health IT professionals at the meeting to make their products more user friendly.
“We will work on reducing the burdens at the federal level, but we also need clinicians and IT folks on the ground to help make certain that technology implementation is done in a way that it enhances usability and increases efficiency,” Dr. Price said.
He also called for true interoperability, a common goal that has persisted since electronic health records were mandated under the HITECH Act but remains an elusive target.
“This has always been the goal and it just seems so simple,” he said. “Somehow something has happened between the idea of interoperability and now that has made it so much more challenging.”
He placed that fault on current federal regulation around interoperability and pledged to create an environment that reduces regulatory roadblocks and allows the technology sector to innovate and foster the free flow of data.
“From my perspective it seems that what we ought to be doing is deciding the rules of the road,” Dr. Price said. “We are going to drive on the right side. We are going to stop at the red light. This is the language we are going to do. This is what a triangular sign looks like, as opposed to stipulating every single dot... all the way down the line.”
WASHINGTON – Reducing IT burden for doctors and fostering interoperability are two top tech priorities for Health and Human Services Secretary Tom Price, MD.
“We simply have to do a better job of reducing the burden of health IT on physicians and all health care providers,” Dr. Price said April 27 at Health Datapalooza, an annual conference on health data transparency. “The promise of big data and health information technology is so great and absolutely remarkable but we must not, we cannot continue to get this wrong.”
“Now we are seeing physicians leaving the practice of medicine when they are 60 or 55,” he said. “Many of my colleagues, my personal friends who have been practicing, right now they are looking for the exit doors. They are trying to figure out how to get out of practicing medicine and I think it is incredibly important for us as a society to step back and ask, why?”
A significant factor is the shift to electronic health records, which has caused doctors to spend much more time looking at screens and feeling more like data entry clerks than health care providers, he said.
“I know that we have lost more than one physician to retirement because of the kinds of burdens that have been placed on a lot of them and that simply ought to be unacceptable to us,” he said. “You think of the intellectual capital that has been lost by this nation because of the kinds of burdens that clinicians have seen.”
That said, “data is absolutely crucial,” Dr. Price said. “Don’t misunderstand me. It is absolutely critical that we have all the data that we can and that we use it in an evidence-based manner so that we can provide better care and better quality of care to patients.”
He challenged the health IT professionals at the meeting to make their products more user friendly.
“We will work on reducing the burdens at the federal level, but we also need clinicians and IT folks on the ground to help make certain that technology implementation is done in a way that it enhances usability and increases efficiency,” Dr. Price said.
He also called for true interoperability, a common goal that has persisted since electronic health records were mandated under the HITECH Act but remains an elusive target.
“This has always been the goal and it just seems so simple,” he said. “Somehow something has happened between the idea of interoperability and now that has made it so much more challenging.”
He placed that fault on current federal regulation around interoperability and pledged to create an environment that reduces regulatory roadblocks and allows the technology sector to innovate and foster the free flow of data.
“From my perspective it seems that what we ought to be doing is deciding the rules of the road,” Dr. Price said. “We are going to drive on the right side. We are going to stop at the red light. This is the language we are going to do. This is what a triangular sign looks like, as opposed to stipulating every single dot... all the way down the line.”
WASHINGTON – Reducing IT burden for doctors and fostering interoperability are two top tech priorities for Health and Human Services Secretary Tom Price, MD.
“We simply have to do a better job of reducing the burden of health IT on physicians and all health care providers,” Dr. Price said April 27 at Health Datapalooza, an annual conference on health data transparency. “The promise of big data and health information technology is so great and absolutely remarkable but we must not, we cannot continue to get this wrong.”
“Now we are seeing physicians leaving the practice of medicine when they are 60 or 55,” he said. “Many of my colleagues, my personal friends who have been practicing, right now they are looking for the exit doors. They are trying to figure out how to get out of practicing medicine and I think it is incredibly important for us as a society to step back and ask, why?”
A significant factor is the shift to electronic health records, which has caused doctors to spend much more time looking at screens and feeling more like data entry clerks than health care providers, he said.
“I know that we have lost more than one physician to retirement because of the kinds of burdens that have been placed on a lot of them and that simply ought to be unacceptable to us,” he said. “You think of the intellectual capital that has been lost by this nation because of the kinds of burdens that clinicians have seen.”
That said, “data is absolutely crucial,” Dr. Price said. “Don’t misunderstand me. It is absolutely critical that we have all the data that we can and that we use it in an evidence-based manner so that we can provide better care and better quality of care to patients.”
He challenged the health IT professionals at the meeting to make their products more user friendly.
“We will work on reducing the burdens at the federal level, but we also need clinicians and IT folks on the ground to help make certain that technology implementation is done in a way that it enhances usability and increases efficiency,” Dr. Price said.
He also called for true interoperability, a common goal that has persisted since electronic health records were mandated under the HITECH Act but remains an elusive target.
“This has always been the goal and it just seems so simple,” he said. “Somehow something has happened between the idea of interoperability and now that has made it so much more challenging.”
He placed that fault on current federal regulation around interoperability and pledged to create an environment that reduces regulatory roadblocks and allows the technology sector to innovate and foster the free flow of data.
“From my perspective it seems that what we ought to be doing is deciding the rules of the road,” Dr. Price said. “We are going to drive on the right side. We are going to stop at the red light. This is the language we are going to do. This is what a triangular sign looks like, as opposed to stipulating every single dot... all the way down the line.”
AT HEALTH DATAPALOOZA 2017