User login
Antinuclear antibodies: When to test and how to interpret findings
› Reserve antinuclear antibody testing for instances of clinically suggestive connective tissue diseases (CTD) and for assessing CTD prognosis. It can also be useful in monitoring disease progression. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Antinuclear antibodies (ANA) are a spectrum of autoantibodies that react with various nuclear and cytoplasmic components of normal human cells. Their detection is important in the diagnosis of some connective tissue diseases (CTD)—eg, systemic lupus erythematosus (SLE), Sjögren’s syndrome (SS), scleroderma, polymyositis, or mixed connective tissue disease (MCTD). Unfortunately, ANA tests are often used indiscriminately in daily clinical practice.1
When is ANA testing warranted?
Indiscriminate use of ANA testing can yield positive results that falsely point to CTD in a high proportion of patients and thereby lead to further inappropriate testing and errant management decisions. To wit: The presence of ANA in the serum can be associated with any number of factors, such as genetic predisposition (eg, through histocompatibility locus DR3), environmental agents (viruses, drugs), chronic infections, neoplasms, and advancing age.1 Therefore, the test should not be ordered in a patient with low pre-test probability of CTD. Moreover, higher titers of ANA are more clinically significant than lower titers. In one multicenter study, 31.7% of healthy individuals were ANA-positive at a serum dilution of 1:40, but only 5% were ANA-positive at a dilution of 1:160.2
What is the clinical significance of different immunofluorescent patterns?
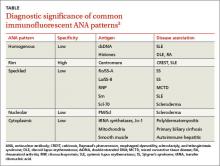
Immunofluorescent ANA testing not only determines if such antibodies are present in a patient’s serum but also reveals informative antibody patterns. Five distinct patterns of fluorescence are possible and can help differentiate between various CTDs (TABLE3):
1. Homogenous, in which the entire nucleus fluoresces, is seen in SLE and discoid lupus erythematosus (DLE).
2. Rim, in which the nuclear perimeter fluoresces, is seen most often in CREST (calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) syndrome and SLE.
3. Speckled, in which the nucleus fluoresces in a speckled pattern, can be seen in a variety of CTDs, including Sjögren’s syndrome, MCTD, SLE, and scleroderma.
4. Nucleolar, in which the nucleolus fluoresces, is associated with scleroderma.
5. Cytoplasmic, in which fluorescence occurs outside the nucleus, typically occurs with poly/dermatomyositis, primary biliary cirrhosis, or autoimmune hepatitis.
What is the next step if ANA is positive?
A positive ANA result warrants additional studies to identify specific autoantibodies suggested by the fluorescence pattern and by a patient’s signs and symptoms.
Following up diagnostic clues
Most systemic autoimmune diseases have a highly characteristic profile of autoantibodies to cellular antigens. A patient’s clinical features and ANA fluorescence pattern should direct additional testing.
Photosensitive butterfly rash, arthralgias/arthritis, pleuritic chest pain, fever of unknown cause, and urine sediment consistent with nephritis point to a diagnosis of SLE. Order an assay for anti-double-stranded DNA (dsDNA) antibodies, which, if present, confirm the diagnosis.4 Also order an assay for anti-Sm antibodies, which are highly specific for SLE but found only in 30% to 40% of SLE patients.4
Raynaud’s phenomenon, skin hardening or thickening, stiffness and tightening of the skin on the fingers, hands and forearms, tight and mask-like skin on the face, dry cough, shortness of breath, and difficulty in swallowing are features of scleroderma. If you suspect this disorder, order an assay for anti-Scl-70 antibodies. These antibodies are highly specific for scleroderma, but sensitivity of the assay is only 15% to 20%.5
Calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia indicate CREST syndrome. Anti-centromere antibodies are highly specific for CREST syndrome; sensitivity on assay is 50% to 90%.6
MCTD combines features of rheumatoid arthritis, SLE, myositis, and scleroderma. Order an assay of anti-RNP (ribonucleoprotein) antibodies. Although anti-RNP antibodies are also found in 25% to 30% of patients with SLE, they typically appear in the company of anti-Sm antibodies.7 Isolated high titers of anti-RNP antibodies point to MCTD, and sensitivity on assay is 100%.8 Their absence on testing, therefore, excludes the diagnosis of MCTD.
RNP, anti-Ro/SS-A, La/SS-B, and Sm are also referred to as extractable nuclear antigens (ENA). Assays of antibodies to ENA and anti-dsDNA are warranted only if the ANA assay result is positive. It is rare to have a positive anti-ENA antibody test (with the exception of antibodies to cytoplasmic antigens) in the absence of a positive ANA test.9
Dry eyes, dry mouth, joint pain and swelling, and swelling of parotid glands point to Sjögren’s syndrome. Anti-Ro/SS-A and La/SS-B antibodies are associated with Sjögren’s syndrome, but are also found in seronegative SLE.10 Therefore, if patients with features suggestive of SLE have a negative result on a dsDNA antibody assay, test for anti-Ro/SS-A and La/SS-B antibodies.
Muscle weakness and soreness, purplish discoloration of the upper eyelids, and purplish-red discoloration of the knuckles suggest dermatomyositis. Muscle biopsy and electromyography will clinch the diagnosis. Also test for anti–Jo-1 antibodies, which are associated with pulmonary involvement in polymyositis.11
ANA’s continuing role—prognosis and disease activity
Besides confirming a diagnosis of CTD in patients with suggestive clinical features, ANA testing serves 2 additional purposes: to help determine a patient’s prognosis and to monitor CTD activity. Consider the following:
- Patients with Sjögren’s syndrome who test positive for anti-Ro/SS-A antibodies have aggressive, extra-glandular disease that can cause vasculitis, purpura, lymphadenopathy, leukopenia, and thrombocytopenia.12
- The presence of anti-Ro/SS-A in the circulation of pregnant women with SLE confers a higher risk of neonatal lupus erythematosus and of congenital heart block in their newborns.13
- Severe interstitial lung disease is frequently found in scleroderma patients who test positive for anti-Scl-70.14 Antibodies to aminoacyl-tRNA synthetases—including anti–Jo-1, as mentioned earlier—are associated with pulmonary involvement in polymyositis patients.11
- A positive ANA test result in Raynaud’s phenomenon increases the likelihood that the patient will develop a systemic rheumatic disease; a negative result reduces this likelihood.15
- While the ANA test is not useful for diagnosing juvenile chronic arthritis (JCA), it is useful to test for ANA in patients with known JCA. A positive test result should prompt screening for uveitis.16
- An ANA test is not necessary for diagnosing antiphospholipid antibody syndrome (APS). However, the presence of ANA in a patient with APS increases the likelihood that APS is secondary to SLE.17
Monitoring disease activity
Documenting titers of anti-dsDNA antibodies may help in monitoring the disease activity of SLE in some patients. However, changes in titers of anti-dsDNA should be interpreted in the clinical context of the SLE Disease Activity Index.18
CORRESPONDENCE
Habib U. Rehman, MB, Department of Medicine, Regina Qu’Appelle Health Region, Regina General Hospital, 1440–14th Avenue, Regina, SK, S4P 0W5, Canada; habib31@sasktel.net
1. Volkmann ER, Taylor M, Ben-Artzi A. Using the antinuclear antibody test to diagnose rheumatic disease: when does a positive test warrant further investigation? South Med J. 2012;105:100-104.
2. Giannouli E, Chatzidimitriou D, Gerou S, et al. Frequency and specificity of antibodies against nuclear and cytoplasmic antigens in healthy individuals by classic and new methods. Clin Rheumatol. 2013;32:1541-1546.
3. O’Sullivan M, McLean-Tooke A, Loh RK. Antinuclear antibody test. Aust Fam Physician. 2013;42:718-721.
4. Kurien BT, Scofield RH. Autoantibody determination in the diagnosis of systemic lupus erythematosus. Scand J Immunol. 2006;64:227-235.
5. Basu D, Reveille JD. Ant-scl-70. Autoimmunity. 2005;38:65-72.
6. Caramaschi P, Biasi D, Manzo T, et al. Anticentromere antibody—clinical associations. A study of 44 patients. Rheumatol Int. 1995;14:253-255.
7. Migliorini P, Baldini C, Rocchi V, et al. Anti-Sm and anti-RNP antibodies. Autoimmunity. 2005;38:47-54.
8. Alarcón-Segovia D, Cardiel MH. Comparison between 3 diagnostic criteria for mixed connective tissue disease. Study of 593 patients. J Rheumatol. 1989;16:328-334.
9. Phan TG, Wong RC, Adelstein S. Autoantibodies to extractable nuclear antigens: making detection and interpretation more meaningful. Clin Diagn Lab Immunol. 2002;9:1-7.
10. Cross LS, Aslam A, Misbah SA. Antinuclear antibody-negative lupus as a distinct diagnostic entity—does it no longer exist? QJM. 2004;97:303-308.
11. Miller FW, Waite KA, Biswat T, et al. The role of an autoantigen, histidyl-tRNA synthetase, in the induction and maintenance of autoimmunity. Proc Natl Acad Sci USA. 1990;87:9933-9937.
12. Brito-Zerón P, Ramos-Casals M, Bove A, et al. Predicting adverse outcomes in primary Sjogren’s syndrome: identification of prognostic factors. Rheumatology. 2007;46:1359-1362.
13. Lindop R, Arentz G, Thurgood LA, et al. Pathogenicity and proteomic signatures of autoantibodies to Ro and La. Immunol Cell Biol. 2012;90:304-309.
14. Steen VD. Autoantibodies in systemic sclerosis. Semin Arthritis Rheum. 2005;35:35-42.
15. Spencer-Green G. Outcomes in primary Raynaud phenomenon: a meta-analysis of the frequency, rates, and predictors of transition to secondary diseases. Arch Intern Med. 1998;158:595-600.
16. Grassi A, Corona F, Casellato A, et al. Prevalence and outcome of juvenile idiopathic arthritis-associated uveitis and relation to articular disease. J Rheumatol. 2007;34:1139-1145.
17. Petri M. Diagnosis of antiphospholipid antibody syndrome. Rheum Dis Clin North Am. 1994;20:443.
18. Kavanaugh A, Tomar R, Reveille J, et al. Guidelines for clinical use of the antinuclear antibody test and tests for specific autoantibodies to nuclear antigens. American College of Pathologists. Arch Pathol Lab Med. 2000;124:71-81.
› Reserve antinuclear antibody testing for instances of clinically suggestive connective tissue diseases (CTD) and for assessing CTD prognosis. It can also be useful in monitoring disease progression. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Antinuclear antibodies (ANA) are a spectrum of autoantibodies that react with various nuclear and cytoplasmic components of normal human cells. Their detection is important in the diagnosis of some connective tissue diseases (CTD)—eg, systemic lupus erythematosus (SLE), Sjögren’s syndrome (SS), scleroderma, polymyositis, or mixed connective tissue disease (MCTD). Unfortunately, ANA tests are often used indiscriminately in daily clinical practice.1
When is ANA testing warranted?
Indiscriminate use of ANA testing can yield positive results that falsely point to CTD in a high proportion of patients and thereby lead to further inappropriate testing and errant management decisions. To wit: The presence of ANA in the serum can be associated with any number of factors, such as genetic predisposition (eg, through histocompatibility locus DR3), environmental agents (viruses, drugs), chronic infections, neoplasms, and advancing age.1 Therefore, the test should not be ordered in a patient with low pre-test probability of CTD. Moreover, higher titers of ANA are more clinically significant than lower titers. In one multicenter study, 31.7% of healthy individuals were ANA-positive at a serum dilution of 1:40, but only 5% were ANA-positive at a dilution of 1:160.2
What is the clinical significance of different immunofluorescent patterns?
Immunofluorescent ANA testing not only determines if such antibodies are present in a patient’s serum but also reveals informative antibody patterns. Five distinct patterns of fluorescence are possible and can help differentiate between various CTDs (TABLE3):
1. Homogenous, in which the entire nucleus fluoresces, is seen in SLE and discoid lupus erythematosus (DLE).
2. Rim, in which the nuclear perimeter fluoresces, is seen most often in CREST (calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) syndrome and SLE.
3. Speckled, in which the nucleus fluoresces in a speckled pattern, can be seen in a variety of CTDs, including Sjögren’s syndrome, MCTD, SLE, and scleroderma.
4. Nucleolar, in which the nucleolus fluoresces, is associated with scleroderma.
5. Cytoplasmic, in which fluorescence occurs outside the nucleus, typically occurs with poly/dermatomyositis, primary biliary cirrhosis, or autoimmune hepatitis.
What is the next step if ANA is positive?
A positive ANA result warrants additional studies to identify specific autoantibodies suggested by the fluorescence pattern and by a patient’s signs and symptoms.
Following up diagnostic clues
Most systemic autoimmune diseases have a highly characteristic profile of autoantibodies to cellular antigens. A patient’s clinical features and ANA fluorescence pattern should direct additional testing.
Photosensitive butterfly rash, arthralgias/arthritis, pleuritic chest pain, fever of unknown cause, and urine sediment consistent with nephritis point to a diagnosis of SLE. Order an assay for anti-double-stranded DNA (dsDNA) antibodies, which, if present, confirm the diagnosis.4 Also order an assay for anti-Sm antibodies, which are highly specific for SLE but found only in 30% to 40% of SLE patients.4
Raynaud’s phenomenon, skin hardening or thickening, stiffness and tightening of the skin on the fingers, hands and forearms, tight and mask-like skin on the face, dry cough, shortness of breath, and difficulty in swallowing are features of scleroderma. If you suspect this disorder, order an assay for anti-Scl-70 antibodies. These antibodies are highly specific for scleroderma, but sensitivity of the assay is only 15% to 20%.5
Calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia indicate CREST syndrome. Anti-centromere antibodies are highly specific for CREST syndrome; sensitivity on assay is 50% to 90%.6
MCTD combines features of rheumatoid arthritis, SLE, myositis, and scleroderma. Order an assay of anti-RNP (ribonucleoprotein) antibodies. Although anti-RNP antibodies are also found in 25% to 30% of patients with SLE, they typically appear in the company of anti-Sm antibodies.7 Isolated high titers of anti-RNP antibodies point to MCTD, and sensitivity on assay is 100%.8 Their absence on testing, therefore, excludes the diagnosis of MCTD.
RNP, anti-Ro/SS-A, La/SS-B, and Sm are also referred to as extractable nuclear antigens (ENA). Assays of antibodies to ENA and anti-dsDNA are warranted only if the ANA assay result is positive. It is rare to have a positive anti-ENA antibody test (with the exception of antibodies to cytoplasmic antigens) in the absence of a positive ANA test.9
Dry eyes, dry mouth, joint pain and swelling, and swelling of parotid glands point to Sjögren’s syndrome. Anti-Ro/SS-A and La/SS-B antibodies are associated with Sjögren’s syndrome, but are also found in seronegative SLE.10 Therefore, if patients with features suggestive of SLE have a negative result on a dsDNA antibody assay, test for anti-Ro/SS-A and La/SS-B antibodies.
Muscle weakness and soreness, purplish discoloration of the upper eyelids, and purplish-red discoloration of the knuckles suggest dermatomyositis. Muscle biopsy and electromyography will clinch the diagnosis. Also test for anti–Jo-1 antibodies, which are associated with pulmonary involvement in polymyositis.11
ANA’s continuing role—prognosis and disease activity
Besides confirming a diagnosis of CTD in patients with suggestive clinical features, ANA testing serves 2 additional purposes: to help determine a patient’s prognosis and to monitor CTD activity. Consider the following:
- Patients with Sjögren’s syndrome who test positive for anti-Ro/SS-A antibodies have aggressive, extra-glandular disease that can cause vasculitis, purpura, lymphadenopathy, leukopenia, and thrombocytopenia.12
- The presence of anti-Ro/SS-A in the circulation of pregnant women with SLE confers a higher risk of neonatal lupus erythematosus and of congenital heart block in their newborns.13
- Severe interstitial lung disease is frequently found in scleroderma patients who test positive for anti-Scl-70.14 Antibodies to aminoacyl-tRNA synthetases—including anti–Jo-1, as mentioned earlier—are associated with pulmonary involvement in polymyositis patients.11
- A positive ANA test result in Raynaud’s phenomenon increases the likelihood that the patient will develop a systemic rheumatic disease; a negative result reduces this likelihood.15
- While the ANA test is not useful for diagnosing juvenile chronic arthritis (JCA), it is useful to test for ANA in patients with known JCA. A positive test result should prompt screening for uveitis.16
- An ANA test is not necessary for diagnosing antiphospholipid antibody syndrome (APS). However, the presence of ANA in a patient with APS increases the likelihood that APS is secondary to SLE.17
Monitoring disease activity
Documenting titers of anti-dsDNA antibodies may help in monitoring the disease activity of SLE in some patients. However, changes in titers of anti-dsDNA should be interpreted in the clinical context of the SLE Disease Activity Index.18
CORRESPONDENCE
Habib U. Rehman, MB, Department of Medicine, Regina Qu’Appelle Health Region, Regina General Hospital, 1440–14th Avenue, Regina, SK, S4P 0W5, Canada; habib31@sasktel.net
› Reserve antinuclear antibody testing for instances of clinically suggestive connective tissue diseases (CTD) and for assessing CTD prognosis. It can also be useful in monitoring disease progression. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Antinuclear antibodies (ANA) are a spectrum of autoantibodies that react with various nuclear and cytoplasmic components of normal human cells. Their detection is important in the diagnosis of some connective tissue diseases (CTD)—eg, systemic lupus erythematosus (SLE), Sjögren’s syndrome (SS), scleroderma, polymyositis, or mixed connective tissue disease (MCTD). Unfortunately, ANA tests are often used indiscriminately in daily clinical practice.1
When is ANA testing warranted?
Indiscriminate use of ANA testing can yield positive results that falsely point to CTD in a high proportion of patients and thereby lead to further inappropriate testing and errant management decisions. To wit: The presence of ANA in the serum can be associated with any number of factors, such as genetic predisposition (eg, through histocompatibility locus DR3), environmental agents (viruses, drugs), chronic infections, neoplasms, and advancing age.1 Therefore, the test should not be ordered in a patient with low pre-test probability of CTD. Moreover, higher titers of ANA are more clinically significant than lower titers. In one multicenter study, 31.7% of healthy individuals were ANA-positive at a serum dilution of 1:40, but only 5% were ANA-positive at a dilution of 1:160.2
What is the clinical significance of different immunofluorescent patterns?
Immunofluorescent ANA testing not only determines if such antibodies are present in a patient’s serum but also reveals informative antibody patterns. Five distinct patterns of fluorescence are possible and can help differentiate between various CTDs (TABLE3):
1. Homogenous, in which the entire nucleus fluoresces, is seen in SLE and discoid lupus erythematosus (DLE).
2. Rim, in which the nuclear perimeter fluoresces, is seen most often in CREST (calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) syndrome and SLE.
3. Speckled, in which the nucleus fluoresces in a speckled pattern, can be seen in a variety of CTDs, including Sjögren’s syndrome, MCTD, SLE, and scleroderma.
4. Nucleolar, in which the nucleolus fluoresces, is associated with scleroderma.
5. Cytoplasmic, in which fluorescence occurs outside the nucleus, typically occurs with poly/dermatomyositis, primary biliary cirrhosis, or autoimmune hepatitis.
What is the next step if ANA is positive?
A positive ANA result warrants additional studies to identify specific autoantibodies suggested by the fluorescence pattern and by a patient’s signs and symptoms.
Following up diagnostic clues
Most systemic autoimmune diseases have a highly characteristic profile of autoantibodies to cellular antigens. A patient’s clinical features and ANA fluorescence pattern should direct additional testing.
Photosensitive butterfly rash, arthralgias/arthritis, pleuritic chest pain, fever of unknown cause, and urine sediment consistent with nephritis point to a diagnosis of SLE. Order an assay for anti-double-stranded DNA (dsDNA) antibodies, which, if present, confirm the diagnosis.4 Also order an assay for anti-Sm antibodies, which are highly specific for SLE but found only in 30% to 40% of SLE patients.4
Raynaud’s phenomenon, skin hardening or thickening, stiffness and tightening of the skin on the fingers, hands and forearms, tight and mask-like skin on the face, dry cough, shortness of breath, and difficulty in swallowing are features of scleroderma. If you suspect this disorder, order an assay for anti-Scl-70 antibodies. These antibodies are highly specific for scleroderma, but sensitivity of the assay is only 15% to 20%.5
Calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia indicate CREST syndrome. Anti-centromere antibodies are highly specific for CREST syndrome; sensitivity on assay is 50% to 90%.6
MCTD combines features of rheumatoid arthritis, SLE, myositis, and scleroderma. Order an assay of anti-RNP (ribonucleoprotein) antibodies. Although anti-RNP antibodies are also found in 25% to 30% of patients with SLE, they typically appear in the company of anti-Sm antibodies.7 Isolated high titers of anti-RNP antibodies point to MCTD, and sensitivity on assay is 100%.8 Their absence on testing, therefore, excludes the diagnosis of MCTD.
RNP, anti-Ro/SS-A, La/SS-B, and Sm are also referred to as extractable nuclear antigens (ENA). Assays of antibodies to ENA and anti-dsDNA are warranted only if the ANA assay result is positive. It is rare to have a positive anti-ENA antibody test (with the exception of antibodies to cytoplasmic antigens) in the absence of a positive ANA test.9
Dry eyes, dry mouth, joint pain and swelling, and swelling of parotid glands point to Sjögren’s syndrome. Anti-Ro/SS-A and La/SS-B antibodies are associated with Sjögren’s syndrome, but are also found in seronegative SLE.10 Therefore, if patients with features suggestive of SLE have a negative result on a dsDNA antibody assay, test for anti-Ro/SS-A and La/SS-B antibodies.
Muscle weakness and soreness, purplish discoloration of the upper eyelids, and purplish-red discoloration of the knuckles suggest dermatomyositis. Muscle biopsy and electromyography will clinch the diagnosis. Also test for anti–Jo-1 antibodies, which are associated with pulmonary involvement in polymyositis.11
ANA’s continuing role—prognosis and disease activity
Besides confirming a diagnosis of CTD in patients with suggestive clinical features, ANA testing serves 2 additional purposes: to help determine a patient’s prognosis and to monitor CTD activity. Consider the following:
- Patients with Sjögren’s syndrome who test positive for anti-Ro/SS-A antibodies have aggressive, extra-glandular disease that can cause vasculitis, purpura, lymphadenopathy, leukopenia, and thrombocytopenia.12
- The presence of anti-Ro/SS-A in the circulation of pregnant women with SLE confers a higher risk of neonatal lupus erythematosus and of congenital heart block in their newborns.13
- Severe interstitial lung disease is frequently found in scleroderma patients who test positive for anti-Scl-70.14 Antibodies to aminoacyl-tRNA synthetases—including anti–Jo-1, as mentioned earlier—are associated with pulmonary involvement in polymyositis patients.11
- A positive ANA test result in Raynaud’s phenomenon increases the likelihood that the patient will develop a systemic rheumatic disease; a negative result reduces this likelihood.15
- While the ANA test is not useful for diagnosing juvenile chronic arthritis (JCA), it is useful to test for ANA in patients with known JCA. A positive test result should prompt screening for uveitis.16
- An ANA test is not necessary for diagnosing antiphospholipid antibody syndrome (APS). However, the presence of ANA in a patient with APS increases the likelihood that APS is secondary to SLE.17
Monitoring disease activity
Documenting titers of anti-dsDNA antibodies may help in monitoring the disease activity of SLE in some patients. However, changes in titers of anti-dsDNA should be interpreted in the clinical context of the SLE Disease Activity Index.18
CORRESPONDENCE
Habib U. Rehman, MB, Department of Medicine, Regina Qu’Appelle Health Region, Regina General Hospital, 1440–14th Avenue, Regina, SK, S4P 0W5, Canada; habib31@sasktel.net
1. Volkmann ER, Taylor M, Ben-Artzi A. Using the antinuclear antibody test to diagnose rheumatic disease: when does a positive test warrant further investigation? South Med J. 2012;105:100-104.
2. Giannouli E, Chatzidimitriou D, Gerou S, et al. Frequency and specificity of antibodies against nuclear and cytoplasmic antigens in healthy individuals by classic and new methods. Clin Rheumatol. 2013;32:1541-1546.
3. O’Sullivan M, McLean-Tooke A, Loh RK. Antinuclear antibody test. Aust Fam Physician. 2013;42:718-721.
4. Kurien BT, Scofield RH. Autoantibody determination in the diagnosis of systemic lupus erythematosus. Scand J Immunol. 2006;64:227-235.
5. Basu D, Reveille JD. Ant-scl-70. Autoimmunity. 2005;38:65-72.
6. Caramaschi P, Biasi D, Manzo T, et al. Anticentromere antibody—clinical associations. A study of 44 patients. Rheumatol Int. 1995;14:253-255.
7. Migliorini P, Baldini C, Rocchi V, et al. Anti-Sm and anti-RNP antibodies. Autoimmunity. 2005;38:47-54.
8. Alarcón-Segovia D, Cardiel MH. Comparison between 3 diagnostic criteria for mixed connective tissue disease. Study of 593 patients. J Rheumatol. 1989;16:328-334.
9. Phan TG, Wong RC, Adelstein S. Autoantibodies to extractable nuclear antigens: making detection and interpretation more meaningful. Clin Diagn Lab Immunol. 2002;9:1-7.
10. Cross LS, Aslam A, Misbah SA. Antinuclear antibody-negative lupus as a distinct diagnostic entity—does it no longer exist? QJM. 2004;97:303-308.
11. Miller FW, Waite KA, Biswat T, et al. The role of an autoantigen, histidyl-tRNA synthetase, in the induction and maintenance of autoimmunity. Proc Natl Acad Sci USA. 1990;87:9933-9937.
12. Brito-Zerón P, Ramos-Casals M, Bove A, et al. Predicting adverse outcomes in primary Sjogren’s syndrome: identification of prognostic factors. Rheumatology. 2007;46:1359-1362.
13. Lindop R, Arentz G, Thurgood LA, et al. Pathogenicity and proteomic signatures of autoantibodies to Ro and La. Immunol Cell Biol. 2012;90:304-309.
14. Steen VD. Autoantibodies in systemic sclerosis. Semin Arthritis Rheum. 2005;35:35-42.
15. Spencer-Green G. Outcomes in primary Raynaud phenomenon: a meta-analysis of the frequency, rates, and predictors of transition to secondary diseases. Arch Intern Med. 1998;158:595-600.
16. Grassi A, Corona F, Casellato A, et al. Prevalence and outcome of juvenile idiopathic arthritis-associated uveitis and relation to articular disease. J Rheumatol. 2007;34:1139-1145.
17. Petri M. Diagnosis of antiphospholipid antibody syndrome. Rheum Dis Clin North Am. 1994;20:443.
18. Kavanaugh A, Tomar R, Reveille J, et al. Guidelines for clinical use of the antinuclear antibody test and tests for specific autoantibodies to nuclear antigens. American College of Pathologists. Arch Pathol Lab Med. 2000;124:71-81.
1. Volkmann ER, Taylor M, Ben-Artzi A. Using the antinuclear antibody test to diagnose rheumatic disease: when does a positive test warrant further investigation? South Med J. 2012;105:100-104.
2. Giannouli E, Chatzidimitriou D, Gerou S, et al. Frequency and specificity of antibodies against nuclear and cytoplasmic antigens in healthy individuals by classic and new methods. Clin Rheumatol. 2013;32:1541-1546.
3. O’Sullivan M, McLean-Tooke A, Loh RK. Antinuclear antibody test. Aust Fam Physician. 2013;42:718-721.
4. Kurien BT, Scofield RH. Autoantibody determination in the diagnosis of systemic lupus erythematosus. Scand J Immunol. 2006;64:227-235.
5. Basu D, Reveille JD. Ant-scl-70. Autoimmunity. 2005;38:65-72.
6. Caramaschi P, Biasi D, Manzo T, et al. Anticentromere antibody—clinical associations. A study of 44 patients. Rheumatol Int. 1995;14:253-255.
7. Migliorini P, Baldini C, Rocchi V, et al. Anti-Sm and anti-RNP antibodies. Autoimmunity. 2005;38:47-54.
8. Alarcón-Segovia D, Cardiel MH. Comparison between 3 diagnostic criteria for mixed connective tissue disease. Study of 593 patients. J Rheumatol. 1989;16:328-334.
9. Phan TG, Wong RC, Adelstein S. Autoantibodies to extractable nuclear antigens: making detection and interpretation more meaningful. Clin Diagn Lab Immunol. 2002;9:1-7.
10. Cross LS, Aslam A, Misbah SA. Antinuclear antibody-negative lupus as a distinct diagnostic entity—does it no longer exist? QJM. 2004;97:303-308.
11. Miller FW, Waite KA, Biswat T, et al. The role of an autoantigen, histidyl-tRNA synthetase, in the induction and maintenance of autoimmunity. Proc Natl Acad Sci USA. 1990;87:9933-9937.
12. Brito-Zerón P, Ramos-Casals M, Bove A, et al. Predicting adverse outcomes in primary Sjogren’s syndrome: identification of prognostic factors. Rheumatology. 2007;46:1359-1362.
13. Lindop R, Arentz G, Thurgood LA, et al. Pathogenicity and proteomic signatures of autoantibodies to Ro and La. Immunol Cell Biol. 2012;90:304-309.
14. Steen VD. Autoantibodies in systemic sclerosis. Semin Arthritis Rheum. 2005;35:35-42.
15. Spencer-Green G. Outcomes in primary Raynaud phenomenon: a meta-analysis of the frequency, rates, and predictors of transition to secondary diseases. Arch Intern Med. 1998;158:595-600.
16. Grassi A, Corona F, Casellato A, et al. Prevalence and outcome of juvenile idiopathic arthritis-associated uveitis and relation to articular disease. J Rheumatol. 2007;34:1139-1145.
17. Petri M. Diagnosis of antiphospholipid antibody syndrome. Rheum Dis Clin North Am. 1994;20:443.
18. Kavanaugh A, Tomar R, Reveille J, et al. Guidelines for clinical use of the antinuclear antibody test and tests for specific autoantibodies to nuclear antigens. American College of Pathologists. Arch Pathol Lab Med. 2000;124:71-81.
What caused elevated liver enzymes in this postpartum patient?
CASE › 38-year-old, previously healthy G2 P2 woman arrives at your office with sudden-onset epigastric pain, chills, and nausea, but no vomiting. She has had no fever, shortness of breath, or pruritis. Her appetite is good and her weight is stable. Three days earlier, she gave birth to a healthy baby. The course of pregnancy had been uncomplicated, and delivery was vaginal at 35 weeks gestation without any complications. Her blood pressure (BP) was normal throughout pregnancy, and she had no signs of preeclampsia.
She does not smoke. Although she usually drinks 1 beer daily, she avoided alcohol during her pregnancy. She does not use illicit drugs. She has received no blood transfusions and has no history of viral hepatitis.
On examination she is alert and oriented. She is afebrile and anicteric. Her vital signs are normal with a BP of 116/80 mm Hg and a pulse rate of 86/min. Respiratory rate is 20/min, and oxygen saturation is 98% while breathing ambient air. On palpation, her abdomen is soft and nontender without organomegaly. There is no ascites and bowel sounds are audible.
Initial laboratory investigation yields the following results:
• alkaline phosphatase 436 U/L (normal, 40-135)
• alanine aminotransferase 685 U/L (4-55)
• total bilirubin 27 mcmol/L (2-20)
• serum albumin 25 g/L (35-55)
• international normalized ratio 0.9 (0.9-1.3)
• amylase 47 U/L (20-110)
• hemoglobin 146 g/L (140-180)
• platelets 296 3 109/L (150-400)
• white blood cell count 9.7 3 109/L (4.0-10.0)
• urinalysis reveals no proteins
• transferrin 4.58 g/L (1.32-3.02)
• iron saturation 29% (15-50)
• ferritin 70 mcg/L (10-200)
• serum copper 43.9 mcmol/L (9.0-27.0)
• ceruloplasmin 594 mg/L (200-600)
• Alpha-1-antitrypsin levels 2.05 g/L (1.06-1.58).
What is the differential diagnosis of abnormally elevated liver enzymes in the peripartum period?
Possible underlying causes of the patient’s findings include pregnancy-related liver diseases such as hyperemesis gravidarum (HG), intrahepatic cholestasis of pregnancy, preeclampsia, eclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets), and acute fatty liver of pregnancy (AFLP); or liver diseases unrelated to pregnancy such as viral hepatitis, autoimmune liver disease, Wilson’s disease, Budd-Chiari syndrome, cholecystitis, and drug-induced hepatotoxicity.
Narrowing the field. HG usually presents between 4 to 13 weeks of the start of pregnancy and is characterized by severe nausea, vomiting, weight loss, and electrolyte disturbances, none of which are present in this patient. The patient does not have neuropsychiatric symptoms and signs typical of Wilson’s disease, and the high-normal ceruloplasmin level despite above-normal serum copper also weighs against this diagnosis.
Our patient was not taking any hepatotoxic drugs or over-the-counter medications that cause liver damage.
With intrahepatic cholestasis of pregnancy, aminotransferase levels can be as high as 20 times the upper limit of normal. However, with this disorder, elevated serum bile acids during the second half of pregnancy cause pruritis. Absence of pruritis, jaundice, and features of obstructive jaundice, including pale stools and dark urine, makes intrahepatic cholestasis of pregnancy unlikely. Moreover, patients with this disorder do not have constitutional symptoms.1
Preeclampsia is characterized by hypertension and proteinuria after 20 weeks of gestation or within 48 hours of delivery. Absence of seizures differentiates it from eclampsia. Right upper quadrant pain, nausea, and vomiting may be the presenting features. Aminotransferase levels can be up to 10 times the upper limit of normal. Bilirubin concentrations are usually normal. These abnormalities typically resolve within 2 weeks of delivery. Though atypical clinical presentations have been known with preeclampsia—particularly as extremes of maternal childbearing age have been associated with preeclampsia2—the patient’s normal BP and an absence of proteinuria make both preeclampsia and eclampsia unlikely.
HELLP syndrome usually arises in the second or third trimester of pregnancy but also can develop after delivery. Right upper quadrant and epigastric pain, nausea, and vomiting are usual presenting symptoms. Hypertension and proteinuria are found in 85% of cases.3 Absence of hypertension and proteinuria and normal microangiopathic blood smear and platelet count make HELLP syndrome unlikely in the patient.
AFLP usually presents in the third trimester of pregnancy with nausea, abdominal pain, jaundice, and hepatic encephalopathy. Hypoglycemia, lactic acidosis, hyperammonemia, and disseminated intravascular coagulation may complicate the clinical picture. Leukocytosis occurs in 98% of patients.4 Elevated concentrations of bilirubin, aminotransferases, and uric acid are commonly found. The biochemical picture in our patient does not match that of AFLP and makes this diagnosis unlikely.
Remaining potential diagnoses. Hepatitis B and C are possibilities and must be excluded by appropriate serologic tests. Hepatitis E viral infection usually follows a more severe course in pregnancy. Pregnant women are more likely to acquire hepatitis E in the second or third trimester. Also, though it is rare for autoimmune hepatitis to first appear during pregnancy, it too, must be ruled out.
Pregnancy is a prothrombotic state, so you must exclude Budd-Chiari syndrome. Up to 20% of cases of Budd-Chiari syndrome occur in women who are on oral contraceptives or are pregnant or 2 months postpartum.5 Right upper quadrant pain, jaundice, and ascites are the common clinical features.
Gallstones are strongly associated with higher parity in women. Pre-pregnancy obesity and high serum leptin levels are strong risk factors for pregnancy-associated gallbladder disease. Gallbladder sludge and stones are common in pregnancy and the postpartum period, and cholecystectomy is frequently done within the first year postpartum.6 Serum alkaline phosphatase is less helpful in diagnosing cholecystitis in pregnancy because of elevated levels from the placenta.
With hepatitis, Budd-Chiari syndrome, and gallstones remaining in the differential, what other investigations would you pursue to narrow the differential?
A test for hepatitis A virus immunoglobulin M (IgM) proves negative. Hepatitis B surface antigen is negative, and hepatitis B surface antibody is 11.5 mIU/L, suggesting borderline protective level of antibody. Hepatitis C virus antibody also is negative. Hepatitis E occurs in the Indian subcontinent, Africa, and the Middle East, and is therefore unlikely in this patient. Serologies for cytomegalovirus IgG and Epstein-Barr virus IgM are negative. Herpes simplex type-1 specific IgG antibody is present. These serologic results exclude viral causes of hepatitis.
Antinuclear (ANA) and antimitochondrial antibodies are negative. Antismooth muscle antibody (ASMA) is positive at a titer of 1:20. Quantitative IgG is 7.23 g/L (normal, 5.52-17.24), IgA is 1.36 g/L (0.87-3.94), and IgM is 1.19 g/L (0.44-2.47). Negative ANA, weakly positive ASMA, and normal levels of immunoglobulins in our patient do not support a diagnosis of autoimmune liver disease.
Imaging is the next step for this patient. Even during pregnancy, ultrasound and magnetic resonance imaging are safe and readily available. The diagnostic accuracy of ultrasound for detecting gallstones is 95%. When ultrasound findings are equivocal in a pregnant patient, magnetic resonance cholangiopancreatography provides an accurate evaluation of the biliary system and can substitute for endoscopic retrograde cholangiopancreatography (ERCP).7
An ultrasound examination of the patient shows a normal liver with no significant fatty infiltration. The gallbladder, however, is packed with calculi. The common hepatic duct measures 4.6 mm and the common bile duct measures 8.5 mm. The intrahepatic ducts are not dilated. Doppler ultrasound of the hepatic and portal veins demonstrates normal flow without evidence of thromboses. Absence of jaundice, ascites, and hepatic vein thrombosis on ultrasound excludes Budd-Chiari syndrome.
The diagnosis
History of sudden-onset epigastric pain, chills, and nausea in the postpartum period, no history of liver disease, and an uneventful pregnancy makes cholecystitis the most likely diagnosis for the patient.
Gallstones are common in pregnancy and more than 4% of pregnant women have incident gallbladder sludge or stones persisting to the early postpartum. Cholesterol secretion is increased in the second and third trimester of pregnancy, thus increasing the lithogenicity of the bile.8
The outcome
ERCP showed several stones in the common bile duct. We performed a papillotomy and removed 15 pale, almost white-faced, stones. Subsequent laparoscopic cholecystectomy removed a large gallbladder with multiple remaining stones. Microscopic examination of the gallbladder wall showed thickened muscularis propria and fibrosis of the subserosa, findings consistent with chronic cholecystitis.
CORRESPONDENCE
H.U. Rehman, MBBS, Clinical Associate Professor, Department of Medicine, Regina General Hospital, 1440 14th Avenue, Regina, SK, S4P 0W5, Canada; habib31@sasktel.net
1. Knox TA, Olans LB. Liver disease in pregnancy. N Engl J Med. 1996;335:569-576.
2. Joshi D, James A, Quaglia A, et al. Liver disease in pregnancy. Lancet. 2010;375:594-605.
3. Martin JN Jr, Rinehart BK, May WL, et al. The spectrum of severe preeclampsia: comparative analysis by HELLP (hemolysis, elevated liver enzyme levels, and low platelet count) syndrome classification. Am J Obstet Gynecol. 1999;180(6 pt 1):1373-1384.
4. Knight M, Nelson-Piercy C, Kurinczuk JJ, et al; UK Obstetric Surveillance System. A prospective national study of acute fatty liver of pregnancy in the UK. Gut. 2008;57:951–956.
5. Khuroo MS, Datta DV. Budd-Chiari syndrome following pregnancy. Report of 16 cases, with roentgenologic, hemodynamic and histologic studies of the hepatic outflow tract. Am J Med. 1980;68:113-121.
6. Ko CW, Beresford SA, Schulte SJ, et al. Incidence, natural history, and risk factors for biliary sludge and stones during pregnancy. Hepatology. 2005;41:359-365.
7. Oto A, Ernst R, Ghulmiyyah L, et al. The role of MR cholangiopancreatography in the evaluation of pregnant patients with acute pancreaticobiliary disease. Br J Radiol. 2009;82:279-285.
8. Donovan JM. Physical and metabolic factors in gallstone pathogenesis. Gastroenterol Clin North Am. 1999;28:75-97.
CASE › 38-year-old, previously healthy G2 P2 woman arrives at your office with sudden-onset epigastric pain, chills, and nausea, but no vomiting. She has had no fever, shortness of breath, or pruritis. Her appetite is good and her weight is stable. Three days earlier, she gave birth to a healthy baby. The course of pregnancy had been uncomplicated, and delivery was vaginal at 35 weeks gestation without any complications. Her blood pressure (BP) was normal throughout pregnancy, and she had no signs of preeclampsia.
She does not smoke. Although she usually drinks 1 beer daily, she avoided alcohol during her pregnancy. She does not use illicit drugs. She has received no blood transfusions and has no history of viral hepatitis.
On examination she is alert and oriented. She is afebrile and anicteric. Her vital signs are normal with a BP of 116/80 mm Hg and a pulse rate of 86/min. Respiratory rate is 20/min, and oxygen saturation is 98% while breathing ambient air. On palpation, her abdomen is soft and nontender without organomegaly. There is no ascites and bowel sounds are audible.
Initial laboratory investigation yields the following results:
• alkaline phosphatase 436 U/L (normal, 40-135)
• alanine aminotransferase 685 U/L (4-55)
• total bilirubin 27 mcmol/L (2-20)
• serum albumin 25 g/L (35-55)
• international normalized ratio 0.9 (0.9-1.3)
• amylase 47 U/L (20-110)
• hemoglobin 146 g/L (140-180)
• platelets 296 3 109/L (150-400)
• white blood cell count 9.7 3 109/L (4.0-10.0)
• urinalysis reveals no proteins
• transferrin 4.58 g/L (1.32-3.02)
• iron saturation 29% (15-50)
• ferritin 70 mcg/L (10-200)
• serum copper 43.9 mcmol/L (9.0-27.0)
• ceruloplasmin 594 mg/L (200-600)
• Alpha-1-antitrypsin levels 2.05 g/L (1.06-1.58).
What is the differential diagnosis of abnormally elevated liver enzymes in the peripartum period?
Possible underlying causes of the patient’s findings include pregnancy-related liver diseases such as hyperemesis gravidarum (HG), intrahepatic cholestasis of pregnancy, preeclampsia, eclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets), and acute fatty liver of pregnancy (AFLP); or liver diseases unrelated to pregnancy such as viral hepatitis, autoimmune liver disease, Wilson’s disease, Budd-Chiari syndrome, cholecystitis, and drug-induced hepatotoxicity.
Narrowing the field. HG usually presents between 4 to 13 weeks of the start of pregnancy and is characterized by severe nausea, vomiting, weight loss, and electrolyte disturbances, none of which are present in this patient. The patient does not have neuropsychiatric symptoms and signs typical of Wilson’s disease, and the high-normal ceruloplasmin level despite above-normal serum copper also weighs against this diagnosis.
Our patient was not taking any hepatotoxic drugs or over-the-counter medications that cause liver damage.
With intrahepatic cholestasis of pregnancy, aminotransferase levels can be as high as 20 times the upper limit of normal. However, with this disorder, elevated serum bile acids during the second half of pregnancy cause pruritis. Absence of pruritis, jaundice, and features of obstructive jaundice, including pale stools and dark urine, makes intrahepatic cholestasis of pregnancy unlikely. Moreover, patients with this disorder do not have constitutional symptoms.1
Preeclampsia is characterized by hypertension and proteinuria after 20 weeks of gestation or within 48 hours of delivery. Absence of seizures differentiates it from eclampsia. Right upper quadrant pain, nausea, and vomiting may be the presenting features. Aminotransferase levels can be up to 10 times the upper limit of normal. Bilirubin concentrations are usually normal. These abnormalities typically resolve within 2 weeks of delivery. Though atypical clinical presentations have been known with preeclampsia—particularly as extremes of maternal childbearing age have been associated with preeclampsia2—the patient’s normal BP and an absence of proteinuria make both preeclampsia and eclampsia unlikely.
HELLP syndrome usually arises in the second or third trimester of pregnancy but also can develop after delivery. Right upper quadrant and epigastric pain, nausea, and vomiting are usual presenting symptoms. Hypertension and proteinuria are found in 85% of cases.3 Absence of hypertension and proteinuria and normal microangiopathic blood smear and platelet count make HELLP syndrome unlikely in the patient.
AFLP usually presents in the third trimester of pregnancy with nausea, abdominal pain, jaundice, and hepatic encephalopathy. Hypoglycemia, lactic acidosis, hyperammonemia, and disseminated intravascular coagulation may complicate the clinical picture. Leukocytosis occurs in 98% of patients.4 Elevated concentrations of bilirubin, aminotransferases, and uric acid are commonly found. The biochemical picture in our patient does not match that of AFLP and makes this diagnosis unlikely.
Remaining potential diagnoses. Hepatitis B and C are possibilities and must be excluded by appropriate serologic tests. Hepatitis E viral infection usually follows a more severe course in pregnancy. Pregnant women are more likely to acquire hepatitis E in the second or third trimester. Also, though it is rare for autoimmune hepatitis to first appear during pregnancy, it too, must be ruled out.
Pregnancy is a prothrombotic state, so you must exclude Budd-Chiari syndrome. Up to 20% of cases of Budd-Chiari syndrome occur in women who are on oral contraceptives or are pregnant or 2 months postpartum.5 Right upper quadrant pain, jaundice, and ascites are the common clinical features.
Gallstones are strongly associated with higher parity in women. Pre-pregnancy obesity and high serum leptin levels are strong risk factors for pregnancy-associated gallbladder disease. Gallbladder sludge and stones are common in pregnancy and the postpartum period, and cholecystectomy is frequently done within the first year postpartum.6 Serum alkaline phosphatase is less helpful in diagnosing cholecystitis in pregnancy because of elevated levels from the placenta.
With hepatitis, Budd-Chiari syndrome, and gallstones remaining in the differential, what other investigations would you pursue to narrow the differential?
A test for hepatitis A virus immunoglobulin M (IgM) proves negative. Hepatitis B surface antigen is negative, and hepatitis B surface antibody is 11.5 mIU/L, suggesting borderline protective level of antibody. Hepatitis C virus antibody also is negative. Hepatitis E occurs in the Indian subcontinent, Africa, and the Middle East, and is therefore unlikely in this patient. Serologies for cytomegalovirus IgG and Epstein-Barr virus IgM are negative. Herpes simplex type-1 specific IgG antibody is present. These serologic results exclude viral causes of hepatitis.
Antinuclear (ANA) and antimitochondrial antibodies are negative. Antismooth muscle antibody (ASMA) is positive at a titer of 1:20. Quantitative IgG is 7.23 g/L (normal, 5.52-17.24), IgA is 1.36 g/L (0.87-3.94), and IgM is 1.19 g/L (0.44-2.47). Negative ANA, weakly positive ASMA, and normal levels of immunoglobulins in our patient do not support a diagnosis of autoimmune liver disease.
Imaging is the next step for this patient. Even during pregnancy, ultrasound and magnetic resonance imaging are safe and readily available. The diagnostic accuracy of ultrasound for detecting gallstones is 95%. When ultrasound findings are equivocal in a pregnant patient, magnetic resonance cholangiopancreatography provides an accurate evaluation of the biliary system and can substitute for endoscopic retrograde cholangiopancreatography (ERCP).7
An ultrasound examination of the patient shows a normal liver with no significant fatty infiltration. The gallbladder, however, is packed with calculi. The common hepatic duct measures 4.6 mm and the common bile duct measures 8.5 mm. The intrahepatic ducts are not dilated. Doppler ultrasound of the hepatic and portal veins demonstrates normal flow without evidence of thromboses. Absence of jaundice, ascites, and hepatic vein thrombosis on ultrasound excludes Budd-Chiari syndrome.
The diagnosis
History of sudden-onset epigastric pain, chills, and nausea in the postpartum period, no history of liver disease, and an uneventful pregnancy makes cholecystitis the most likely diagnosis for the patient.
Gallstones are common in pregnancy and more than 4% of pregnant women have incident gallbladder sludge or stones persisting to the early postpartum. Cholesterol secretion is increased in the second and third trimester of pregnancy, thus increasing the lithogenicity of the bile.8
The outcome
ERCP showed several stones in the common bile duct. We performed a papillotomy and removed 15 pale, almost white-faced, stones. Subsequent laparoscopic cholecystectomy removed a large gallbladder with multiple remaining stones. Microscopic examination of the gallbladder wall showed thickened muscularis propria and fibrosis of the subserosa, findings consistent with chronic cholecystitis.
CORRESPONDENCE
H.U. Rehman, MBBS, Clinical Associate Professor, Department of Medicine, Regina General Hospital, 1440 14th Avenue, Regina, SK, S4P 0W5, Canada; habib31@sasktel.net
CASE › 38-year-old, previously healthy G2 P2 woman arrives at your office with sudden-onset epigastric pain, chills, and nausea, but no vomiting. She has had no fever, shortness of breath, or pruritis. Her appetite is good and her weight is stable. Three days earlier, she gave birth to a healthy baby. The course of pregnancy had been uncomplicated, and delivery was vaginal at 35 weeks gestation without any complications. Her blood pressure (BP) was normal throughout pregnancy, and she had no signs of preeclampsia.
She does not smoke. Although she usually drinks 1 beer daily, she avoided alcohol during her pregnancy. She does not use illicit drugs. She has received no blood transfusions and has no history of viral hepatitis.
On examination she is alert and oriented. She is afebrile and anicteric. Her vital signs are normal with a BP of 116/80 mm Hg and a pulse rate of 86/min. Respiratory rate is 20/min, and oxygen saturation is 98% while breathing ambient air. On palpation, her abdomen is soft and nontender without organomegaly. There is no ascites and bowel sounds are audible.
Initial laboratory investigation yields the following results:
• alkaline phosphatase 436 U/L (normal, 40-135)
• alanine aminotransferase 685 U/L (4-55)
• total bilirubin 27 mcmol/L (2-20)
• serum albumin 25 g/L (35-55)
• international normalized ratio 0.9 (0.9-1.3)
• amylase 47 U/L (20-110)
• hemoglobin 146 g/L (140-180)
• platelets 296 3 109/L (150-400)
• white blood cell count 9.7 3 109/L (4.0-10.0)
• urinalysis reveals no proteins
• transferrin 4.58 g/L (1.32-3.02)
• iron saturation 29% (15-50)
• ferritin 70 mcg/L (10-200)
• serum copper 43.9 mcmol/L (9.0-27.0)
• ceruloplasmin 594 mg/L (200-600)
• Alpha-1-antitrypsin levels 2.05 g/L (1.06-1.58).
What is the differential diagnosis of abnormally elevated liver enzymes in the peripartum period?
Possible underlying causes of the patient’s findings include pregnancy-related liver diseases such as hyperemesis gravidarum (HG), intrahepatic cholestasis of pregnancy, preeclampsia, eclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets), and acute fatty liver of pregnancy (AFLP); or liver diseases unrelated to pregnancy such as viral hepatitis, autoimmune liver disease, Wilson’s disease, Budd-Chiari syndrome, cholecystitis, and drug-induced hepatotoxicity.
Narrowing the field. HG usually presents between 4 to 13 weeks of the start of pregnancy and is characterized by severe nausea, vomiting, weight loss, and electrolyte disturbances, none of which are present in this patient. The patient does not have neuropsychiatric symptoms and signs typical of Wilson’s disease, and the high-normal ceruloplasmin level despite above-normal serum copper also weighs against this diagnosis.
Our patient was not taking any hepatotoxic drugs or over-the-counter medications that cause liver damage.
With intrahepatic cholestasis of pregnancy, aminotransferase levels can be as high as 20 times the upper limit of normal. However, with this disorder, elevated serum bile acids during the second half of pregnancy cause pruritis. Absence of pruritis, jaundice, and features of obstructive jaundice, including pale stools and dark urine, makes intrahepatic cholestasis of pregnancy unlikely. Moreover, patients with this disorder do not have constitutional symptoms.1
Preeclampsia is characterized by hypertension and proteinuria after 20 weeks of gestation or within 48 hours of delivery. Absence of seizures differentiates it from eclampsia. Right upper quadrant pain, nausea, and vomiting may be the presenting features. Aminotransferase levels can be up to 10 times the upper limit of normal. Bilirubin concentrations are usually normal. These abnormalities typically resolve within 2 weeks of delivery. Though atypical clinical presentations have been known with preeclampsia—particularly as extremes of maternal childbearing age have been associated with preeclampsia2—the patient’s normal BP and an absence of proteinuria make both preeclampsia and eclampsia unlikely.
HELLP syndrome usually arises in the second or third trimester of pregnancy but also can develop after delivery. Right upper quadrant and epigastric pain, nausea, and vomiting are usual presenting symptoms. Hypertension and proteinuria are found in 85% of cases.3 Absence of hypertension and proteinuria and normal microangiopathic blood smear and platelet count make HELLP syndrome unlikely in the patient.
AFLP usually presents in the third trimester of pregnancy with nausea, abdominal pain, jaundice, and hepatic encephalopathy. Hypoglycemia, lactic acidosis, hyperammonemia, and disseminated intravascular coagulation may complicate the clinical picture. Leukocytosis occurs in 98% of patients.4 Elevated concentrations of bilirubin, aminotransferases, and uric acid are commonly found. The biochemical picture in our patient does not match that of AFLP and makes this diagnosis unlikely.
Remaining potential diagnoses. Hepatitis B and C are possibilities and must be excluded by appropriate serologic tests. Hepatitis E viral infection usually follows a more severe course in pregnancy. Pregnant women are more likely to acquire hepatitis E in the second or third trimester. Also, though it is rare for autoimmune hepatitis to first appear during pregnancy, it too, must be ruled out.
Pregnancy is a prothrombotic state, so you must exclude Budd-Chiari syndrome. Up to 20% of cases of Budd-Chiari syndrome occur in women who are on oral contraceptives or are pregnant or 2 months postpartum.5 Right upper quadrant pain, jaundice, and ascites are the common clinical features.
Gallstones are strongly associated with higher parity in women. Pre-pregnancy obesity and high serum leptin levels are strong risk factors for pregnancy-associated gallbladder disease. Gallbladder sludge and stones are common in pregnancy and the postpartum period, and cholecystectomy is frequently done within the first year postpartum.6 Serum alkaline phosphatase is less helpful in diagnosing cholecystitis in pregnancy because of elevated levels from the placenta.
With hepatitis, Budd-Chiari syndrome, and gallstones remaining in the differential, what other investigations would you pursue to narrow the differential?
A test for hepatitis A virus immunoglobulin M (IgM) proves negative. Hepatitis B surface antigen is negative, and hepatitis B surface antibody is 11.5 mIU/L, suggesting borderline protective level of antibody. Hepatitis C virus antibody also is negative. Hepatitis E occurs in the Indian subcontinent, Africa, and the Middle East, and is therefore unlikely in this patient. Serologies for cytomegalovirus IgG and Epstein-Barr virus IgM are negative. Herpes simplex type-1 specific IgG antibody is present. These serologic results exclude viral causes of hepatitis.
Antinuclear (ANA) and antimitochondrial antibodies are negative. Antismooth muscle antibody (ASMA) is positive at a titer of 1:20. Quantitative IgG is 7.23 g/L (normal, 5.52-17.24), IgA is 1.36 g/L (0.87-3.94), and IgM is 1.19 g/L (0.44-2.47). Negative ANA, weakly positive ASMA, and normal levels of immunoglobulins in our patient do not support a diagnosis of autoimmune liver disease.
Imaging is the next step for this patient. Even during pregnancy, ultrasound and magnetic resonance imaging are safe and readily available. The diagnostic accuracy of ultrasound for detecting gallstones is 95%. When ultrasound findings are equivocal in a pregnant patient, magnetic resonance cholangiopancreatography provides an accurate evaluation of the biliary system and can substitute for endoscopic retrograde cholangiopancreatography (ERCP).7
An ultrasound examination of the patient shows a normal liver with no significant fatty infiltration. The gallbladder, however, is packed with calculi. The common hepatic duct measures 4.6 mm and the common bile duct measures 8.5 mm. The intrahepatic ducts are not dilated. Doppler ultrasound of the hepatic and portal veins demonstrates normal flow without evidence of thromboses. Absence of jaundice, ascites, and hepatic vein thrombosis on ultrasound excludes Budd-Chiari syndrome.
The diagnosis
History of sudden-onset epigastric pain, chills, and nausea in the postpartum period, no history of liver disease, and an uneventful pregnancy makes cholecystitis the most likely diagnosis for the patient.
Gallstones are common in pregnancy and more than 4% of pregnant women have incident gallbladder sludge or stones persisting to the early postpartum. Cholesterol secretion is increased in the second and third trimester of pregnancy, thus increasing the lithogenicity of the bile.8
The outcome
ERCP showed several stones in the common bile duct. We performed a papillotomy and removed 15 pale, almost white-faced, stones. Subsequent laparoscopic cholecystectomy removed a large gallbladder with multiple remaining stones. Microscopic examination of the gallbladder wall showed thickened muscularis propria and fibrosis of the subserosa, findings consistent with chronic cholecystitis.
CORRESPONDENCE
H.U. Rehman, MBBS, Clinical Associate Professor, Department of Medicine, Regina General Hospital, 1440 14th Avenue, Regina, SK, S4P 0W5, Canada; habib31@sasktel.net
1. Knox TA, Olans LB. Liver disease in pregnancy. N Engl J Med. 1996;335:569-576.
2. Joshi D, James A, Quaglia A, et al. Liver disease in pregnancy. Lancet. 2010;375:594-605.
3. Martin JN Jr, Rinehart BK, May WL, et al. The spectrum of severe preeclampsia: comparative analysis by HELLP (hemolysis, elevated liver enzyme levels, and low platelet count) syndrome classification. Am J Obstet Gynecol. 1999;180(6 pt 1):1373-1384.
4. Knight M, Nelson-Piercy C, Kurinczuk JJ, et al; UK Obstetric Surveillance System. A prospective national study of acute fatty liver of pregnancy in the UK. Gut. 2008;57:951–956.
5. Khuroo MS, Datta DV. Budd-Chiari syndrome following pregnancy. Report of 16 cases, with roentgenologic, hemodynamic and histologic studies of the hepatic outflow tract. Am J Med. 1980;68:113-121.
6. Ko CW, Beresford SA, Schulte SJ, et al. Incidence, natural history, and risk factors for biliary sludge and stones during pregnancy. Hepatology. 2005;41:359-365.
7. Oto A, Ernst R, Ghulmiyyah L, et al. The role of MR cholangiopancreatography in the evaluation of pregnant patients with acute pancreaticobiliary disease. Br J Radiol. 2009;82:279-285.
8. Donovan JM. Physical and metabolic factors in gallstone pathogenesis. Gastroenterol Clin North Am. 1999;28:75-97.
1. Knox TA, Olans LB. Liver disease in pregnancy. N Engl J Med. 1996;335:569-576.
2. Joshi D, James A, Quaglia A, et al. Liver disease in pregnancy. Lancet. 2010;375:594-605.
3. Martin JN Jr, Rinehart BK, May WL, et al. The spectrum of severe preeclampsia: comparative analysis by HELLP (hemolysis, elevated liver enzyme levels, and low platelet count) syndrome classification. Am J Obstet Gynecol. 1999;180(6 pt 1):1373-1384.
4. Knight M, Nelson-Piercy C, Kurinczuk JJ, et al; UK Obstetric Surveillance System. A prospective national study of acute fatty liver of pregnancy in the UK. Gut. 2008;57:951–956.
5. Khuroo MS, Datta DV. Budd-Chiari syndrome following pregnancy. Report of 16 cases, with roentgenologic, hemodynamic and histologic studies of the hepatic outflow tract. Am J Med. 1980;68:113-121.
6. Ko CW, Beresford SA, Schulte SJ, et al. Incidence, natural history, and risk factors for biliary sludge and stones during pregnancy. Hepatology. 2005;41:359-365.
7. Oto A, Ernst R, Ghulmiyyah L, et al. The role of MR cholangiopancreatography in the evaluation of pregnant patients with acute pancreaticobiliary disease. Br J Radiol. 2009;82:279-285.
8. Donovan JM. Physical and metabolic factors in gallstone pathogenesis. Gastroenterol Clin North Am. 1999;28:75-97.